- 1School of Nursing and Rehabilitation, Shandong University, Jinan, China
- 2Department of Traditional Chinese Medicine, Qilu Hospital of Shandong University, Jinan, China
- 3Department of PICC Clinic, Qilu Hospital of Shandong University, Jinan, China
Introduction: Data about the impact of varying physical-activity therapy (PAT) intensities and the ideal duration of cognitive behavioral therapy (CBT) on older adults is inadequate. In this umbrella review, we seek to comprehensively synthesize and analyze findings from systematic reviews and meta-analyses regarding the optimal PAT intensity for lowering FOF and the duration of CBT interventions for effectively lowering FOF.
Methods: The PubMed, Web of Science, Cochrane Library, Medline, Embase, and CINAHL databases were searched up to April 2024. AMSTAR 2 was applied to assess the methodological and reporting quality. The quality of evidence for each intervention’s effect was evaluated using GRADE guidelines. A further meta-analysis of the primary studies was conducted to evaluate the effects of PAT intensity and CBT duration.
Results: In the 18 included studies, 12 were PAT interventions, 3 were multifactorial, and 3 were CBT interventions. The umbrella review found that PAT and CBT interventions can effectively manage FOF. Comparable improvements were reported with low- and moderate-intensity PAT intervention (p < 0.0001); Significant improvements were observed with CBT immediately post-intervention, in the short-term (<6 months), and in the long-term (≥6 months) (p < 0.0001).
Discussion: Our study revealed that a comprehensive intervention strategy combining low or moderate PAT with CBT interventions is more effective than isolated approaches, as it addresses the multifaceted nature of fear and fall risk. Future research should continue to track the long-term effects of synergistic interventions to optimize fall prevention strategies for older populations.
Systematic review registration: https://www.crd.york.ac.uk/prospero Identifier CRD42024557893.
1 Introduction
The phenomenon of falls among older adults is a significant public health concern, particularly as the global population ages. A large population-based study revealed that approximately 27.5% of 65 and older experience falls annually, increasing to 32.8–35.7% in individuals aged 85 and older (1). Su et al. (2) further demonstrated that the fall risk among individuals over 75 years was three times higher compared to those aged 65 to 74, and this risk escalated to nine times higher for individuals over 95 years. The accumulation of risk factors, including muscle weakness, balance deficits, and cognitive decline, is critical in fall susceptibility. For instance, Gale et al. (3) highlighted that intrinsic factors, such as muscle weakness and gait disorders, are prevalent among older adults and play a significant role in fall risk. Similarly, Nguyen et al. (4) found that body composition, interconnected with age, gender, health perception, and financial status, exacerbates the risk of falls.
While age is a significant fall risk factor, it is not the sole determinant. Environmental factors also play a critical role in fall risk among older adults. A review has shown that simple changes, such as improving lighting, removing clutter, and installing grab bars, can significantly reduce fall risk in hospital and home settings (5). The integration of wearable technologies into these modifications, such as smart belts equipped with airbag systems, has been developed to mitigate the impact of falls (6). Mobile applications also significantly advance fall risk management, especially in the COVID-19 pandemic, where physical distancing has become essential (7). Furthermore, Şimşek et al. (8) suggested that factors like living alone and fear of falling (FOF) are important contributors to fall risk. FOF is defined as low perceived self-efficacy in preventing falls during daily activities, with a prevalence of about 49.60%, ranging from 6.96 to 90.34% (9, 10).
FOF can increase fall risk in various ways. Firstly, older adults who experience FOF may avoid activities that they perceive as risky, leading to decreased muscle strength and impaired balance, both of which are significant predictors of falls. For instance, a study showed that older adults with limitations in lower limb exercises exhibited a markedly higher FOF, contributing to decreased physical performance (11). This avoidance behavior creates a vicious cycle in which FOF leads to inactivity, further weakening physical capabilities and increasing fall risk (12). In addition to physical factors, psychological conditions, such as anxiety and depression, are commonly associated with FOF, further heightening fall risk. For instance, Young et al. (13) noted that distressing thoughts can reduce the effectiveness of the reach-and-grasp balance response prior to a balance perturbation, thereby increasing falls. Similarly, Lin et al. (14) emphasized that emotional distress not only affects mental well-being but also negatively impacts physical health by mediating resilience.
The relationship between FOF and fall risk is characterized by a complex interplay of physical and psychological factors, and understanding these dynamics is crucial for developing effective prevention strategies. Physical-activity therapy (PAT), such as structured exercise programs, has been shown to improve balance, strength, and overall physical fitness, thereby reducing FOF. A recent study found that older adults who participated in structured exercise programs experienced significant reductions in FOF, particularly those who began with higher baseline fears (15). Moreover, eHealth-delivered exercise programs that combine PAT with educational components have proven particularly effective (16). Besides, Cognitive Behavioral Therapy (CBT) has shown promise in reducing FOF by addressing cognitive distortions and maladaptive beliefs that contribute to fear. A systematic review concluded that CBT-based interventions significantly reduce FOF among community-dwelling older adults, suggesting that psychological interventions can enhance self-efficacy and coping strategies (17).
In summary, PAT and CBT are essential components of a holistic approach to managing FOF in older adults. By addressing the fear’s physical and psychological factors, these interventions can significantly improve the quality of life and functional independence of older adult individuals. However, considering the previous reviews/meta-analysis, we raise two questions: (1) What intensity of PAT is most suitable for older adults? (2) Does CBT have a long-term effect on older adult FOF? Therefore, this overview was carried out to provide a comprehensive review of PAT and CBT interventions, evaluate which PAT intensity is most helpful for lowering FOF and determine the effective duration of CBT for reducing FOF in older adults.
2 Materials and methods
2.1 Design
This umbrella review of systematic reviews and meta-analyses adheres to the Preferred Reporting Items for Overviews of Reviews (PRIOR) guidelines (18). The review protocol was registered in the PROSPERO International Prospective Register of Systematic Reviews (Ref: CRD42024557893).
2.2 Criteria for considering reviews for inclusion
The inclusion and exclusion criteria were defined using the PICOS framework. The inclusion criteria were as follows: (1) P (population): Participants in the included reviews/meta-analyses were community-dwelling older adults who had a mean age of ≥60 years. (2) I (intervention): Reviews/meta-analyses that include CBT or any form of PAT, either as a primary or secondary intervention, were considered. (3) C (comparator): no intervention, standard care, or wait-list control. (4) O (outcomes): Included studies were required to utilize at least one measure related to FOF, such as the Falls Efficacy Scale (FES), FES-International (FES-I), Short FES-I, Activities-Specific Balance Confidence Scale (ABC), Survey of Activities and Fear of Falling in the older adult (SAFE), Geriatric Fear of Falling Measure (GFFM), Fear of Falling Questionnaire (FFQ), and a measure of balance confidence (CONFbal). (5) S (study design): Only published systematic reviews or meta-analyses were considered. The exclusion criteria were: (1) Literature written in languages other than English. (2) Studies with primary or secondary outcomes unrelated to FoF (e.g., fall self-efficacy, balance confidence).
2.3 Search methods for identification of reviews
Searches were conducted until April 2024 on PubMed, Web of Science, The Cochrane Library, Medline, Embase, and CINAHL. The Reference lists of relevant reviews and included studies were manually checked for additional citations not captured in the initial search. A combination of text words and MeSH phrases, such as “aged/older adult/older/senior,” “fear of falling/concern about falling/afraid of falling/worry about falling,” and “meta-analysis/systematic review” were employed.
2.4 Data extraction and management
Two independent reviewers screened the titles and abstracts derived from the database for eligibility; subsequently, all potentially includable articles were stored in Endnote X9 software, and duplicates were removed. For final inclusion, two researchers separately evaluated the full texts of the selected articles to ensure they met the eligibility criteria. In cases of disagreement, a third researcher participated in reaching a consensus. The author, year, country, study design, participants, number of studies, interventions, quality assessment, and principal conclusions were extracted from the included literature.
2.5 Assessment of methodological quality of included reviews
Two authors independently evaluated the quality of the included reviews using AMSTAR 2 (A Measurement Tool to Assess Systematic Reviews 2) (19). It contains 16 items, of which seven are critical domains (items 2, 4, 7, 9, 11, 13, and 15). Review methodological quality is classified into four levels: high, moderate, low, and critically low. The two researchers double-checked their evaluations after finishing the quality assessment. When there were disagreements, a third researcher helped to resolve the inconsistency.
2.6 Assessment of evidence quality of included reviews
Two authors independently evaluated the quality of the evidence using GRADE (Grades of Recommendations Assessment, Development, and Evaluation) guidelines (20). Evidence quality was assessed based on limitations in design, inconsistency, indirectness, imprecision, and publication bias. The evidence was subsequently rated as high, moderate, low, or very low. Finally, the two researchers cross-checked their evaluations of quality. In cases of discrepancies, a third researcher participated to reach a consensus.
2.7 Data synthesis
This study involved an umbrella review and a supplementary meta-analysis. Initially, the outcomes of PAT and CBT interventions were qualitatively summarized. Data were then taken from the meta-analyses to elucidate the effects of these interventions. Direct comparisons between CBT and PAT interventions were unfeasible due to insufficient data. Subsequently, a meta-analysis was conducted utilizing Review Manager 5.4.1 to determine which PAT intensity is most helpful for lowering FOF and explore the effects of CBT interventions’ duration on reducing FOF in older adults. Also, heterogeneity was quantified by I2, with a value exceeding 50% indicating substantial heterogeneity. During the sensitivity analysis, papers of low quality were removed, and the combined effect was calculated as the standardized mean difference (SMD) with a 95% confidence interval. Publication bias was evaluated using funnel plots if more than 10 original papers were incorporated.
3 Results
3.1 Search results
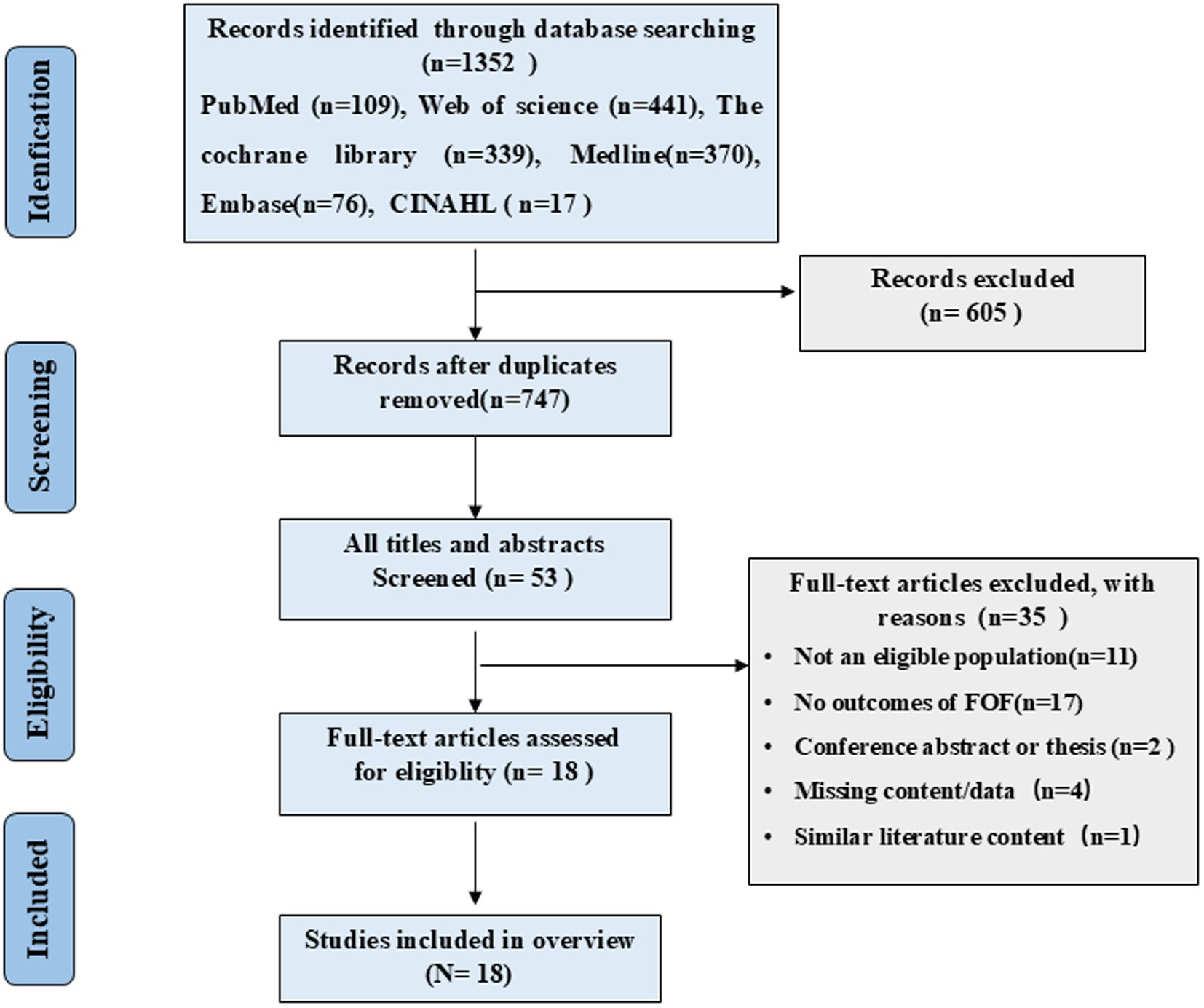
For our overview of reviews, we retrieved 1,352 papers, of which 747 remained after duplicates were removed. After browsing the titles and abstracts, 53 potentially relevant papers were identified. After reading the complete text, we removed 35 papers, leaving 18 reviews/meta-analyses (Figure 1).
3.2 General characteristics and outcomes of included studies
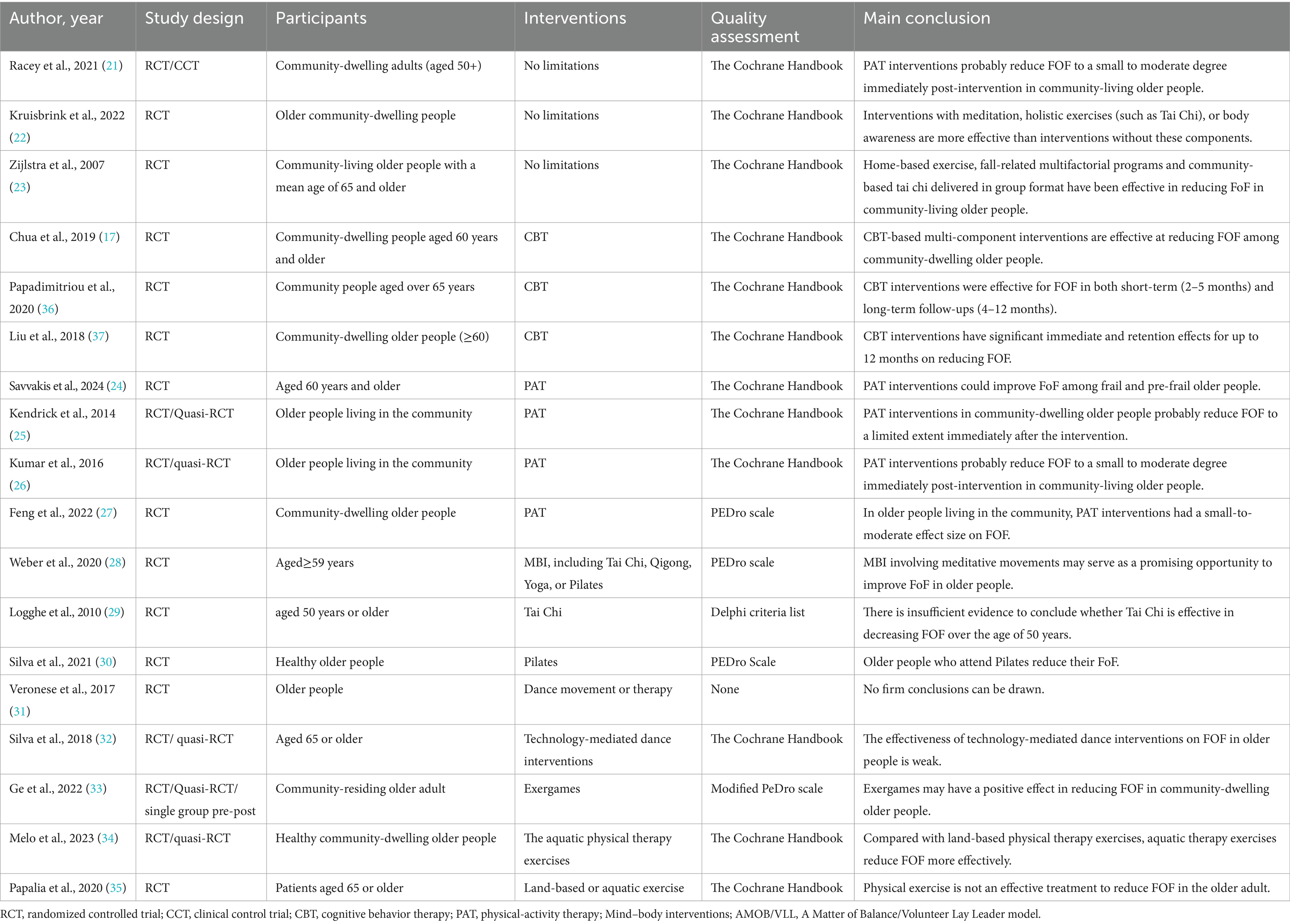
In the 18 included studies, three studies (21–23) reported multi-component interventions targeting FOF in community-dwelling older adults, while the remaining studies focused on single interventions, including PAT (n = 12) (24–35) and CBT (n = 3) (17, 36, 37). The main characteristics of the reviewed studies are summarized in Table 1.
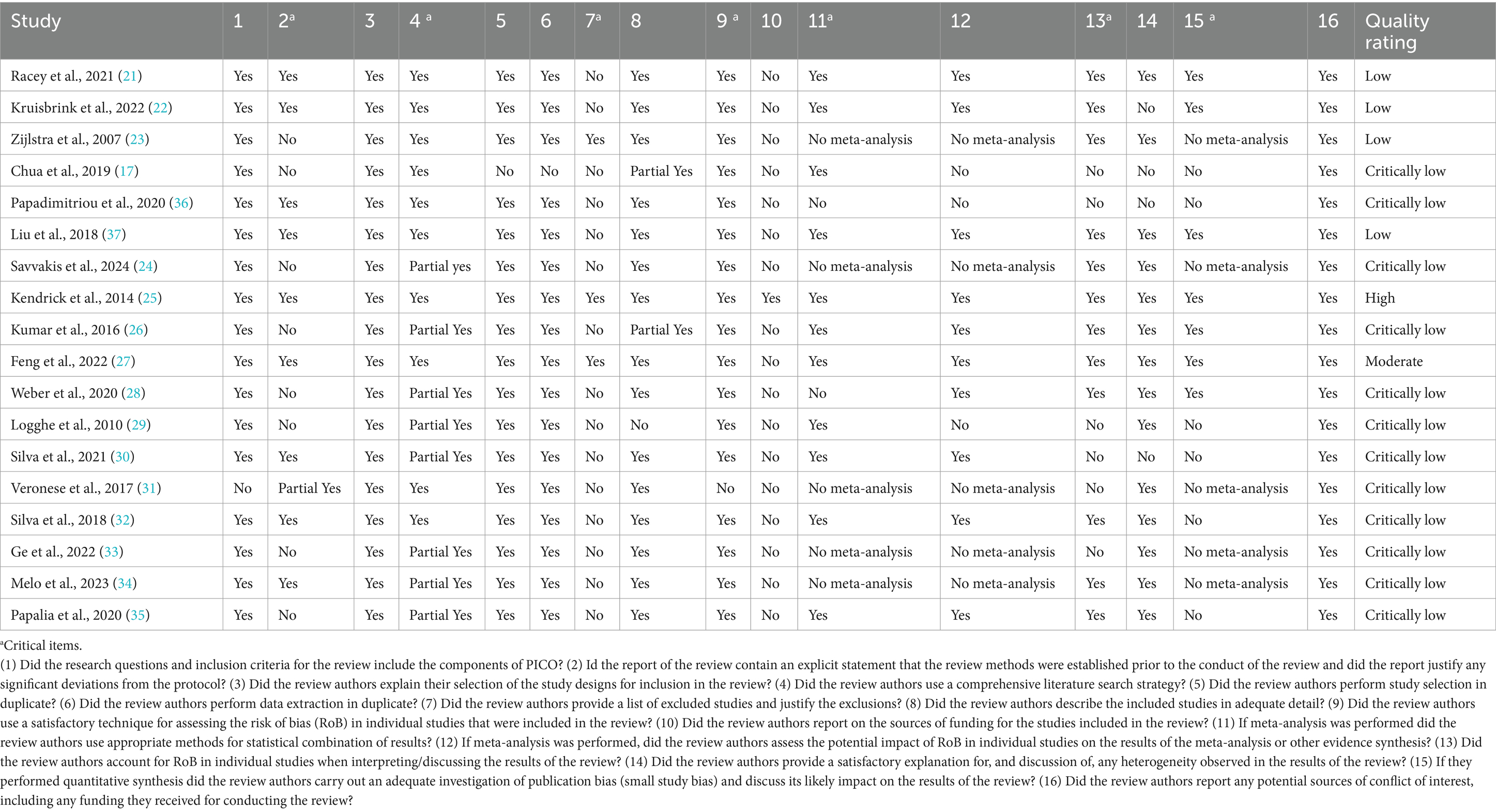
3.3 Quality of included reviews
The methodological quality of the 18 included studies was evaluated using AMSTAR 2. Of these, one study was rated as high quality (25), one as moderate quality (27), four as low quality (21–23, 37), and 12 as critically low quality (17, 24, 26, 28–36). The AMSTAR 2 assessment for these multiple-system reviews is presented in Table 2.
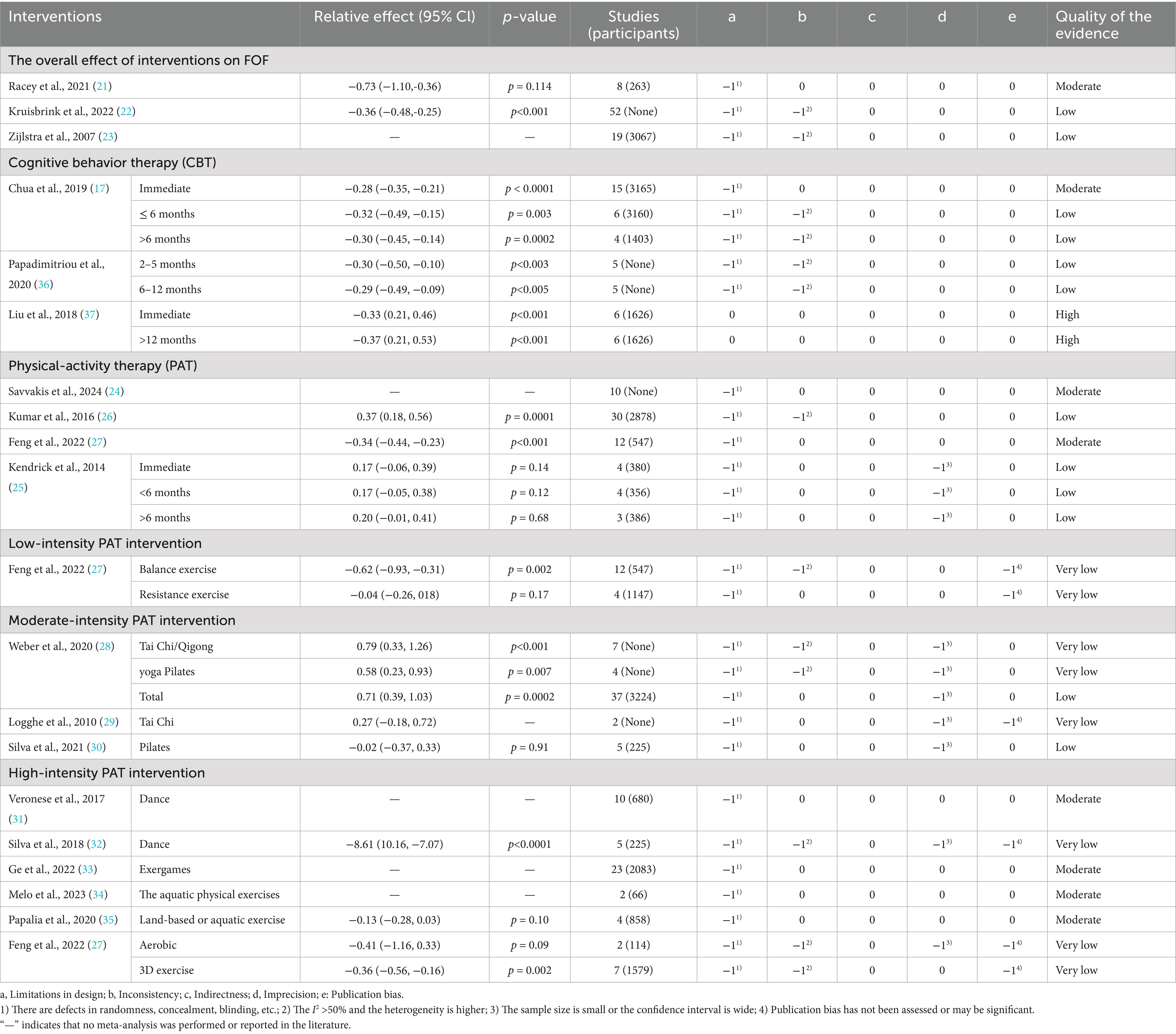
3.4 Quality of evidence
The quality of 31 pieces of evidence derived from the 18 included studies was evaluated using the GRADE system. Two pieces of evidence were rated as high quality, eight as moderate quality, 12 as low quality, and nine as very low quality. Table 3 displays the quality grade for intervention outcomes.
3.5 Effect of interventions on FOF
Three reviews were conducted to analyze and report on multi-component interventions for FOF systematically. According to Zijlstra et al. (23), 11 out of 19 preventive measures were found to decrease FOF, including Tai Chi (n = 3), exercise interventions (n = 2), fall-related multifactorial programs (n = 5), and hip protective interventions (n = 1). In a meta-analysis involving a large sample, it was found that combining PAT with CBT led to a significant reduction in FOF [SMD = −0.36, 95% CI (−0.48, −0.25), p < 0.0001] at the initial available assessment following the intervention (22). Furthermore, univariate meta-regression showed that interventions incorporating meditation, holistic exercise (such as Tai Chi or Pilates), or body awareness were significantly more effective than those without these components. Additionally, Racey et al. (21) evaluated the effectiveness of fall prevention interventions for community-dwelling adults with mild to moderate cognitive impairment. The results showed that PAT interventions are effective at improving FOF [SMD = −0.73, 95% CI (−1.10, −0.36), p < 0.05]. However, high-quality studies with longer follow-ups and adequate sample sizes are needed to determine their direct effectiveness on FOF.
3.5.1 PAT intervention on FOF
PAT is available in various formats and classified as low, moderate, and high-intensity based on global recommendations (38). Low-intensity PAT typically involves balance or resistance training; moderate-intensity PAT primarily comprises Tai Chi, Qigong, Yoga, Pilates, and other mind–body interventions; and high-intensity PAT can be land-based or aquatic, such as dance, exercise games, swimming, or other holistic exercises. The total impact of PAT on FOF was reported in two studies. Savvakis et al. (24) found that PAT interventions were associated with a small to moderate reduction in FOF immediately post-intervention [SMD = 0.37, 95% CI (0.18, 0.56), p < 0.0001], which was consistent with the findings of Feng et al. (27). Considering the susceptibility of older adults, we classified all PAT interventions as low, moderate, or high intensity based on the nature of the activities. The findings of the subgroup are as follows:
• Low-intensity PAT on FOF: Low-intensity PAT interventions include balance and resistance training. Feng’s study (27) found that balance PAT intervention had the most significant effect size [SMD = −0.62, 95% CI (−0.93, −0.31), p < 0.001], compared to studies using resistance PAT, aerobic PAT, or other forms of interventions, all of which also showed significant results.
• Moderate-intensity PAT on FOF: Three reviews reported the effects of moderate-intensity PAT, such as Tai Chi, Qigong, and Yoga/Pilates on FOF, with differing outcomes. In the study conducted by Weber et al. (28), moderate-intensity PAT interventions significantly reduced FOF compared to a non-PAT control group [SMD = 0.12, 95% CI (−0.16, −0.39), p = 0.08]. Similarly, Silva et al. (30) showed that the Pilates group had a lower FOF score, with statistically significant differences from the control group [MD = −8.61, 95% CI (−10.16, −7.07), p < 0.001]. However, a small sample meta-analysis suggested that moderate-intensity PAT for community-dwelling people with FOF did not show any improvement [SMD = 0.27, 95% CI (−0.18, 0.72), p > 0.05] compared to non-PAT controls (29).
• High-intensity PAT on FOF: Six studies reported the effect of high-intensity PAT on FOF. Silva et al. (32) demonstrated that technology-mediated dance systems showed little or no difference from the control groups [SMD = −0.02, 95% CI (−0.37, −0.33), p = 0.91]. A systematic review indicated that 15 of 23 trials (65%) involving exergame intervention, which mixes interactive features of video games with exercise, were associated with a statistically significant reduction in FOF (33). Another review yielded inconclusive results; however, two primary randomized controlled trials (RCTs) suggested that dancing may reduce FOF compared to the control group (31). Additionally, a systematic review indicated that aquatic PAT was more effective than land-based PAT in reducing FOF (34). In contrast, another meta-analysis concluded that land-based exercise interventions were ineffective relative to the control group [SMD = −0.13, 95% CI (−0.28, 0.03), p = 0.10] (35).
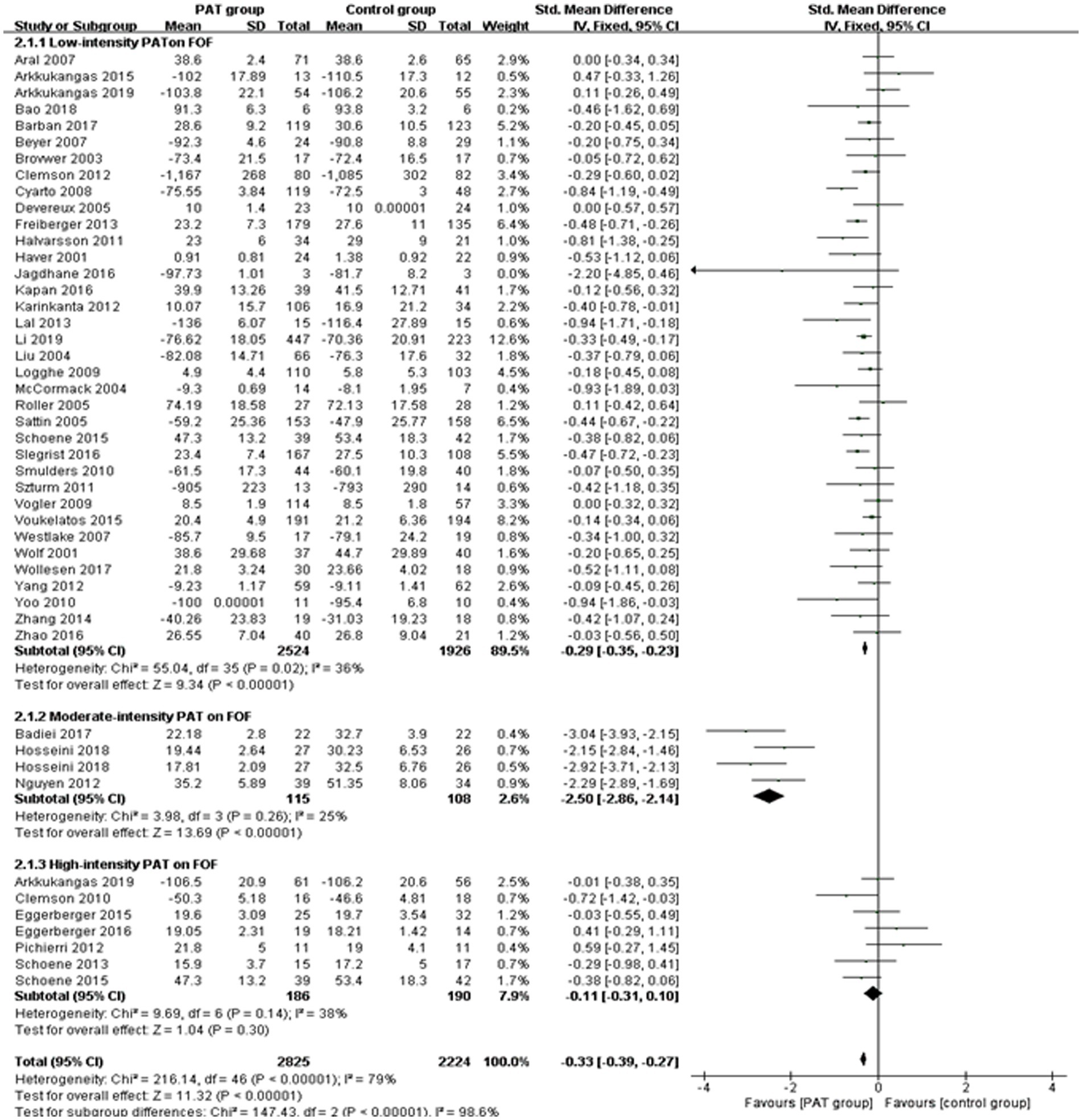
A supplementary meta-analysis of the principal RCT papers was performed. The results showed that both low-intensity PAT [SMD = −0.28, 95% CI (−0.37, −0.20), p < 0.0001] and moderate-intensity PAT [SMD = −2.52, 95% CI (−2.94, −2.11), p < 0.0001] can effectively reduce FOF incidence, while high-intensity PAT [SMD = −0.10, 95% CI (−0.37, 0.17), p = 0.48] was not significant. The comprehensive subgroup data are presented below, and the forest plots of the low-intensity, moderate-intensity, and high-intensity PAT on FOF are illustrated in Figure 2.
3.5.2 CBT intervention on FOF
The impact of CBT on FOF was reported in four studies. Chua et al. (17) found that CBT was effective in reducing FOF immediately post-intervention [SMD = −0.28, 95% CI (−0.35, −0.21), p < 0.0001], as well as in the short term (<6 months) [SMD = −0.32, 95% CI (−0.49, −0.15), p = 0.003], and in the long term (≥6 months) [SMD = −0.30, 95% CI (−0.45, −0.14), p = 0.002]. Papadimitriou et al. (36) consistently reported that CBT interventions were effective in reducing FOF in both short-term (2–5 months) [SMD = −0.30, 95% CI (−0.50, −0.10), p < 0.003] and long-term follow-ups (6–12 months) [SMD = −0.29, 95% CI (−0.49, −0.09), p < 0.005]. Similarly, Liu et al. (37) indicated that CBT interventions have substantial immediate [SMD = −0.33, 95% CI (0.21, 0.46), p < 0.001] and retention [SMD = −0.37, 95% CI (0.21, 0.53), p < 0.001] effects on reducing FOF for up to 12 months.
A supplementary meta-analysis was conducted, which included primary RCT evidence. The findings indicated that CBT can effectively decrease FOF [SMD = −0.30, 95% CI (−0.35, −0.25), p < 0.001] for at least 1 year, with its impact attaining the peaking in a short-term (<6 months). Details of the subgroup results are presented in Figure 3.
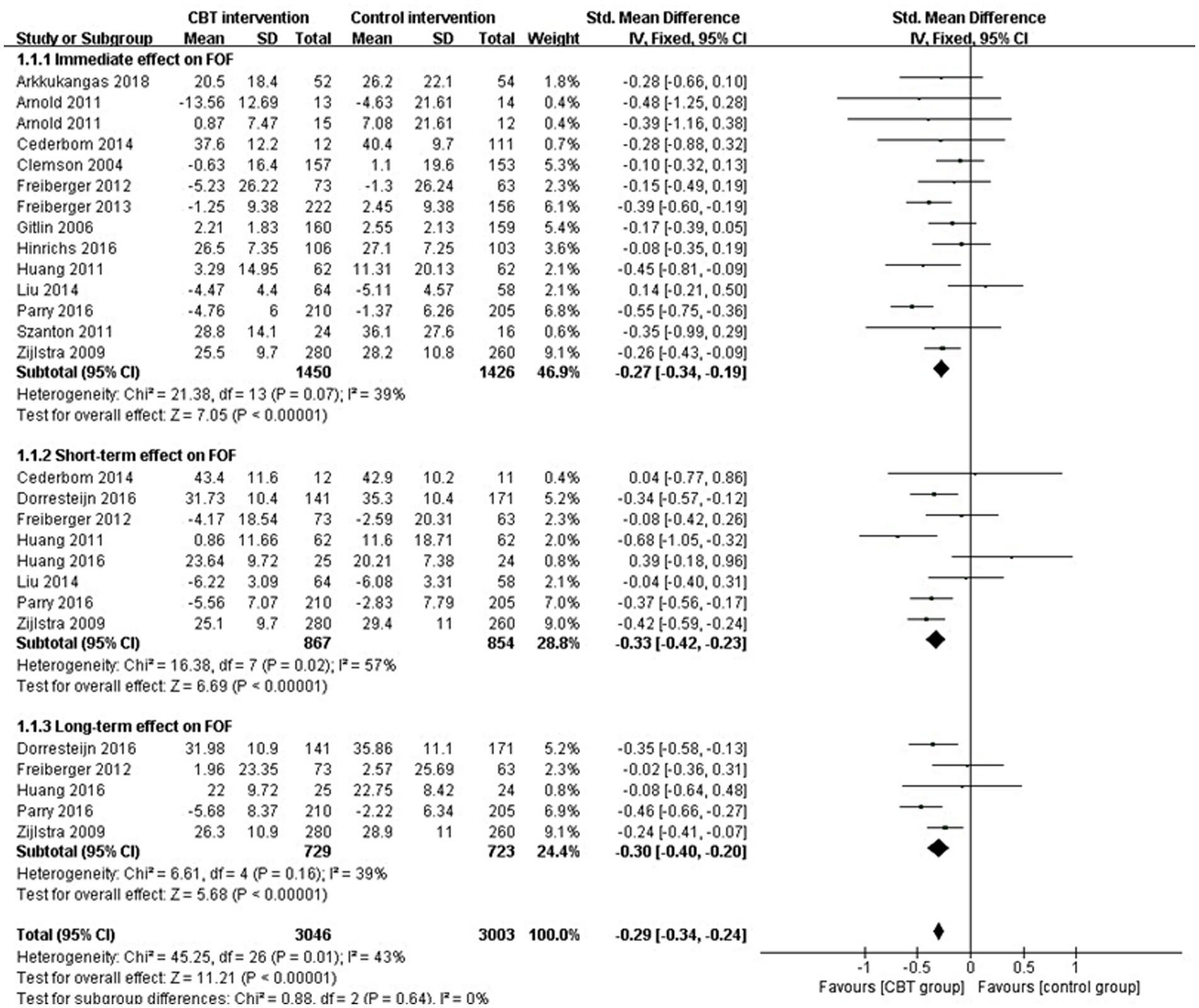
Figure 3. Forest plots of the immediate (1 month), short-term (<6 months), and long-term (>6 month) effects of CBT on FOF.
3.6 Publication bias
Funnel plots were employed to detect publication bias in the PAT and CBT intervention groups. The findings are illustrated in Figure 4. The funnel plots seemed symmetrical, showing minimal heterogeneity among the trials.
4 Discussion
4.1 Main findings
This umbrella review aimed to systematically overview the impacts of PAT and CBT interventions in reducing FOF among older adults. Based on the synthesis of the 18 included reviews, the majority focused on PAT interventions (n = 12), three papers mainly discussed CBT interventions, and three explored the overall effect of multi-component FOF interventions. Clear evidence supports the conclusion that a comprehensive intervention strategy that addresses physical and psychological factors is more effective than isolated approaches to managing FOF. Our supplementary meta-analysis indicates that low-to moderate-intensity PAT is more suitable for reducing FOF in older adults, and CBT effects may persist for up to 1 year.
4.2 Quality of the evidence
The GRADE evaluation revealed significant limitations in the quality of evidence. Of the 31 pieces of evidence assessed, two were classified as high quality, eight as moderate quality, 12 as low quality, and nine as very low quality. Firstly, most studies had defects in randomness, concealment, and blinding, leading to design limitations. Secondly, the inconsistency was primarily due to the heterogeneity among trials, stemming from variations in the intervention measures’ frequency, duration, and intensity. PAT interventions were classified into three subgroups according to exercise intensity: low-intensity, moderate-intensity, and high-intensity, with I2 values of 36, 25, and 38%, respectively, demonstrating no substantial heterogeneity within the subgroups. When combined, the I2 value was 79%, indicating that intervention intensity might be a key factor contributing to heterogeneity, confirming our analysis. Furthermore, the small sample sizes resulted in broad confidence intervals, which introduced imprecision and lowered the quality of evidence. Issues such as incomplete systematic review/meta-analysis retrieval, small sample sizes, and lacking funnel plots contributed to publication bias. Future studies should focus on designing robust research methodologies to provide stronger evidence for clinical practice.
4.3 Agreements and disagreements with other studies or reviews
The intensity of PAT intervention plays a crucial role in reducing FOF among older adults. Our main finding is that low-to-moderate-intensity PAT programs are particularly effective in reducing the FOF. One of the key advantages of low-to-moderate-intensity exercise programs is their accessibility and sustainability for older adults. For instance, a randomized controlled trial demonstrated that community-based Baduanjin exercise intervention for older adults is a safe, feasible, and acceptable exercise program that can be effective in alleviating vital exhaustion reduce FOF (39). Secondly, such programs are often more cost-effective and accessible than high-intensity alternatives, making them suitable for a broader range of participants, including those with varying fitness and health conditions (40). Moreover, psychological benefits also play an important role in these low-to moderate-intensity programs. For instance, group exercise settings such as Tai Chi can foster a sense of community and support, enhancing motivation and adherence, which enhances the positive effects on both physical and mental health (41).
Conversely, evidence suggests that high-intensity PAT may not effectively reduce FOF in older adults. Firstly, the physical condition of older adults is an important factor in their response to exercise. Lin et al. (42) emphasize that the type, intensity, and duration of exercise must be tailored to the individual’s physical condition to prevent falls effectively. Therefore, high-intensity PAT may not be suitable for those with pre-existing conditions or low baseline fitness, as it may lead to injury or falls during activity. Similarly, Barreto et al. (43) suggest that the notion of “more exercise is always better” does not apply universally to vulnerable older adults, as excessive exercise may lead to overtraining, diminished immunity, and negative psychological outcomes. In line with these findings, a systematic review indicated that traditional moderate or high-intensity physical resistance training alone did not significantly reduce the risk of falls (44). This suggests that while high-intensity PAT may improve specific physical capacities, it does not adequately address the multifaceted nature of fall prevention, including balance and functional training. Instead, focusing on low-to moderate-intensity PAT while incorporating balance and functional training is more beneficial for this population.
The study also identified CBT as a significant intervention for addressing FOF in older adults. However, more research is needed to determine whether regular intensive therapy is necessary to maintain treatment effects, as reflected in a recent systematic review (45). On one hand, CBT helps older adults reframe their thoughts about falling, viewing it as a manageable risk rather than an inevitable outcome, which significantly reduces anxiety and promotes engagement in physical activities (46). Besides, by addressing these psychological factors, CBT reduces FOF and promotes a more active and engaged lifestyle among older adults (33). On the other hand, whether CBT requires long-term continuous intervention is nuanced and may depend on individual circumstances and the complexity of the issues being addressed. For example, the systematic review by Jönsson et al. (47) supports the notion that psychological treatments, including CBT, can lead to long-term improvements in mental health outcomes for older adults, particularly in reducing depressive symptoms. Conversely, Kim et al. (48) highlighted that interventions lasting only 8 weeks might not affect lasting behavioral changes in older adults. Similarly, Lenouvel et al. (45) found that CBT with or without exercise interventions for FoF probably sustains improvements beyond 6 months, implying that addressing these underlying issues through initial intensive therapy may yield lasting benefits.
The Global Initiative World Guidelines recommend a multidisciplinary approach that includes PAT, CBT, and occupational therapy to reduce FOF among older adults (1B) (49). These findings suggest that integrating low-to-moderate PAT with CBT interventions provides a holistic approach to managing FOF. For example, a randomized controlled trial emphasized the importance of combining CBT with Tai Chi exercise to enhance mobility, manage FOF, and improve the quality of life among community-dwelling older adults (50). Moreover, Wetherell et al. (51) developed the ABLE intervention, which combines exposure therapy, cognitive restructuring and physical activity, demonstrating that such integrative approaches can significantly reduce FOF in older adults. Similarly, Yoshikawa et al. (52) developed the Matter of Balance Volunteer Lay Leader (AMOB/VLL) model by combining CBT with strength and balance exercises. In summary, Interventions combining PAT with CBT yield better outcomes in reducing FOF than PAT alone, as they tackle mental and physical barriers to activity. Future research should continue to explore the synergistic effects of these interventions to optimize fall prevention strategies for older populations.
4.4 Limitations and implications
This umbrella review has several limitations that should be noted. First, there is limited available evidence regarding the long-term effectiveness of CBT interventions for mitigating FOF. Although we have strengthened the theoretical basis for its effectiveness through its potential mechanisms, drawing definitive conclusions about its long-term impact remains challenging. Similarly, it remains unclear whether PAT effects are sustained over time, and limited data make direct comparisons between PAT and CBT interventions unfeasible. Nevertheless, it is clear that psychological improvements play a crucial role in reducing FOF, and combining PAT with CBT could offer a more comprehensive approach to managing this condition in older adults. Secondly, the FOF assessment tools for older adults have not been standardized; although the SMD effect size was used, the pooled effect size did not differ significantly among the various scales. Further, the results may have been affected by a high risk of performance bias due to the infeasibility of blinding participants and therapists, given the nature of the intervention.
Despite some limitations, several practical implications can be drawn from this study. Firstly, PAT serves as a foundational component in reducing FOF, as it directly addresses the physiological factors contributing to fall risk. CBT focuses on cognitive restructuring, helping individuals develop more realistic perceptions of their fall risk and enhancing their confidence in their physical abilities. Our study supports that a comprehensive intervention strategy is more effective than isolated approaches, as it addresses the multifaceted nature of fear and fall risk. Secondly, PAT programs should be flexible and adaptable. Low-to-moderate-intensity exercises are especially beneficial for frail individuals, while high-intensity programs may provide additional benefits regarding strength and balance improvement. Therefore, tailoring exercise interventions to the individual’s physical capabilities and fear levels is essential for maximizing their effectiveness in reducing FOF. Furthermore, CBT profoundly influences FOF in older adults by altering cognitive perceptions, enhancing coping strategies, and improving overall mental health. Integrating CBT with educational programs provides a comprehensive approach to managing FOF, ultimately promoting better health outcomes and quality of life for older adults. However, this psychological condition is not merely a transient concern; it often necessitates ongoing intervention to effectively manage and mitigate its effects on FOF, particularly in cognitively impaired older adults.
5 Conclusion
The umbrella review found that PAT and CBT interventions can effectively address FOF in older adults. While regular intensive CBT may not be universally necessary for all older adults with FOF, ongoing engagement in CBT and low-to moderate-intensity PAT interventions provide a comprehensive strategy for managing FOF and improving overall quality of life. Potential directions for future research include tracking the long-term effects of comprehensive intervention programs. Finally, we hope this study can provide valuable references for FOF intervention theory and practice while stimulating further discussions and research.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
YS: Writing – original draft, Writing – review & editing. CW: Methodology, Software, Validation, Writing – original draft. YW: Data curation, Methodology, Software, Writing – review & editing. LP: Formal analysis, Validation, Writing – review & editing. MZ: Formal analysis, Writing – review & editing. DL: Conceptualization, Funding acquisition, Writing – review & editing. WG: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Qilu School of Medicine Geriatric Diseases Chinese-Western Medicine Integration Academic Heritage Studio Project (NO.2022-93-1-10).
Acknowledgments
We thank Shandong University for providing the infrastructure and facilities.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Moreland, B, Kakara, R, and Henry, A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years - United States, 2012-2018. MMWR Morb Mortal Wkly Rep. (2020) 69:875–81. doi: 10.15585/mmwr.mm6927a5
2. Su, Q, Song, M, Mao, Y, Ku, H, Gao, Y, and Pi, H. An analysis of the associated factors for falls, recurrent falls, and fall-related injuries among the older adults in senior Chinese apartments: a cross-sectional study. Geriatr Nurs. (2023) 52:127–32. doi: 10.1016/j.gerinurse.2023.05.016
3. Gale, CR, Cooper, C, and Sayer, AA. Prevalence and risk factors for falls in older men and women: the English longitudinal study of ageing. Age Ageing. (2016) 45:789–94. doi: 10.1093/ageing/afw129
4. Nguyen, T, Thiamwong, L, Lou, Q, and Xie, R. Unveiling fall triggers in older adults: a machine learning graphical model analysis. Mathematics. (2024) 12:1271. doi: 10.3390/math12091271
5. Clemson, L, Stark, S, Pighills, AC, Fairhall, NJ, Lamb, SE, Ali, J, et al. Environmental interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. (2023) 2023:Cd013258. doi: 10.1002/14651858.CD013258.pub2
6. Yeoh Lui, CX, Yang, N, Tang, A, and Tam, WWS. Effectiveness evaluation of smart home Technology in Preventing and Detecting Falls in community and residential care settings for older adults: a systematic review and Meta-analysis. JAMA. (2024) 26:105347. doi: 10.1016/j.jamda.2024.105347
7. Hsieh, KL, Frechette, ML, Fanning, J, Chen, L, Griffin, A, and Sosnoff, JJ. The developments and iterations of a Mobile technology-based fall risk health application. Front digital. Health. (2022) 4:8686. doi: 10.3389/fdgth.2022.828686
8. Şimşek, H, Erkoyun, E, Akoz, A, Ergör, A, and Uçku, R. Falls, fear of falling and related factors in community-dwelling individuals aged 80 and over in Turkey. Australas J Ageing. (2019) 39:e16–23. doi: 10.1111/ajag.12673
9. Vo, MTH, Thonglor, R, Moncatar, TJR, Han, TDT, Tejativaddhana, P, and Nakamura, K. Fear of falling and associated factors among older adults in Southeast Asia: a systematic review. Public Health. (2022) 222:215–28. doi: 10.1016/j.puhe.2022.08.012
10. Xiong, W, Wang, D, Ren, W, Liu, X, Wen, R, and Luo, Y. The global prevalence of and risk factors for fear of falling among older adults: a systematic review and meta-analysis. BMC Geriatr. (2024) 24:321. doi: 10.1186/s12877-024-04882-w
11. Sebastião, E, Siqueira, V, Bakare, J, Bohn, L, and Gallo, LH. Fear of falling in older adults living in a community-dwelling facility: prevalence and its impact on activity behavior and physical function. J Appl Gerontol. (2024) 43:1015–22. doi: 10.1177/07334648241230403
12. World Health Organization. (2022). Ageing and health. Available at: (https://www.who.int/newsroom/factsheets/detail/ageing-and-health).
13. Akinlosotu, RY, Alissa, N, Waldstein, SR, Creath, RA, Wittenberg, GF, and Westlake, KP. Examining the influence of mental stress on balance perturbation responses in older adults. Exp Gerontol. (2021) 153:111495. doi: 10.1016/j.exger.2021.111495
14. Lin, H, Zhu, Y, Liu, Q, and Li, S. The mediating effect of resilience between physical activity and mental health: a meta-analytic structural equation modeling approach. Front Public Health. (2024) 12:1434624. doi: 10.3389/fpubh.2024.1434624
15. Mac Donald, M, Sénéchal, M, Leadbetter, B, and Bouchard, DR. Fear of falls following an online exercise program for aging adults. Gerontol Geriatr Med. (2023) 9:1357. doi: 10.1177/23337214231151357
16. Ambrens, M, Alley, S, Oliveira, JS, To, Q, Delbaere, K, Vandelanotte, C, et al. Effect of eHealth-delivered exercise programmes on balance in people aged 65 years and over living in the community: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. (2022) 12:e051377. doi: 10.1136/bmjopen-2021-051377
17. Chua, CHM, Jiang, Y, Lim, DS, Wu, VX, and Wang, W. Effectiveness of cognitive behaviour therapy-based multi-component interventions on fear of falling among community-dwelling older adults: a systematic review and Meta-analysis. J Adv Nurs. (2019) 75:3299–315. doi: 10.1111/jan.14150
18. Gates, M, Gates, A, Pieper, D, Fernandes, RM, Tricco, AC, Moher, D, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. BMJ. (2022) 378:e070849. doi: 10.1136/bmj-2022-070849
19. Shea, BJ, Reeves, BC, Wells, G, Thuku, M, Hamel, C, Moran, J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
20. Balshem, H, Helfand, M, Schünemann, HJ, Oxman, AD, Kunz, R, Brozek, J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. (2011) 64:401–6. doi: 10.1016/j.jclinepi.2010.07.015
21. Racey, M, Markle-Reid, M, Fitzpatrick-Lewis, D, Ali, MU, Gagne, H, Hunter, S, et al. Fall prevention in community-dwelling adults with mild to moderate cognitive impairment: a systematic review and meta-analysis. BMC Geriatr. (2021) 21:689. doi: 10.1186/s12877-021-02641-9
22. Kruisbrink, M, Crutzen, R, Kempen, G, Delbaere, K, Ambergen, T, Cheung, KL, et al. Disentangling interventions to reduce fear of falling in community-dwelling older people: a systematic review and meta-analysis of intervention components. Disabil Rehabil. (2022) 44:6247–57. doi: 10.1080/09638288.2021.1969452
23. Zijlstra, GA, van Haastregt, JC, van Rossum, E, van Eijk, JT, Yardley, L, and Kempen, GI. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc. (2007) 55:603–15. doi: 10.1111/j.1532-5415.2007.01148.x
24. Savvakis, I, Adamakidou, T, and Kleisiaris, C. Physical-activity interventions to reduce fear of falling in frail and pre-frail older adults: a systematic review of randomized controlled trials. Eur Geriatr Med. (2024) 15:333–44. doi: 10.1007/s41999-024-00944-9
25. Kendrick, D, Kumar, A, Carpenter, H, Zijlstra, GA, Skelton, DA, Cook, JR, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. (2014) 2014, 2015:Cd009848. doi: 10.1002/14651858.CD009848.pub2
26. Kumar, A, Delbaere, K, Zijlstra, GA, Carpenter, H, Iliffe, S, Masud, T, et al. Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing. (2016) 45:345–52. doi: 10.1093/ageing/afw036
27. Feng, C, Adebero, T, DePaul, VG, Vafaei, A, Norman, KE, and Auais, M. A systematic review and Meta-analysis of exercise interventions and use of exercise principles to reduce fear of falling in community-dwelling older adults. Phys Ther. (2022) 102:102. doi: 10.1093/ptj/pzab236
28. Weber, M, Schnorr, T, Morat, M, Morat, T, and Donath, L. Effects of mind-body interventions involving meditative movements on quality of life, depressive symptoms, fear of falling and sleep quality in older adults: a systematic review with Meta-analysis. Int J Environ Res Public Health. (2020) 17:186556. doi: 10.3390/ijerph17186556
29. Logghe, IH, Verhagen, AP, Rademaker, AC, Bierma-Zeinstra, SM, van Rossum, E, Faber, MJ, et al. The effects of tai chi on fall prevention, fear of falling and balance in older people: a meta-analysis. Prev Med. (2010) 51:222–7. doi: 10.1016/j.ypmed.2010.06.003
30. da Silva, LD, Shiel, A, and McIntosh, C. Pilates reducing falls risk factors in healthy older adults: a systematic review and Meta-analysis. Front Med. (2021) 8:708883. doi: 10.3389/fmed.2021.708883
31. Veronese, N, Maggi, S, Schofield, P, and Stubbs, B. Dance movement therapy and falls prevention. Maturitas. (2017) 102:1–5. doi: 10.1016/j.maturitas.2017.05.004
32. Silva, PA, Cochrane, A, and Farrell, H. The effectiveness of technology-mediated dance interventions and their impact on psychosocial factors in older adults: a systematic review and Meta-analysis. Games Health J. (2018) 7:347–61. doi: 10.1089/g4h.2017.0197
33. Ge, L, Su, TT, An, Y, and Mejía, ST. The effectiveness of exergames on fear of falling in community-dwelling older adults: a systematic review. Aging Ment Health. (2022) 26:1306–17. doi: 10.1080/13607863.2021.1950615
34. Melo, RS, Cardeira, CSF, Rezende, DSA, Guimarães-do-Carmo, VJ, Lemos, A, and de Moura-Filho, AG. Effectiveness of the aquatic physical therapy exercises to improve balance, gait, quality of life and reduce fall-related outcomes in healthy community-dwelling older adults: a systematic review and meta-analysis. PLoS One. (2023) 18:e0291193. doi: 10.1371/journal.pone.0291193
35. Papalia, GF, Papalia, R, Diaz Balzani, LA, Torre, G, Zampogna, B, Vasta, S, et al. The effects of physical exercise on balance and prevention of falls in older people: a systematic review and Meta-analysis. J Clin Med. (2020) 9:9. doi: 10.3390/jcm9082595
36. Papadimitriou, A, and Perry, M. Systematic review of the effects of cognitive and Behavioural interventions on fall-related psychological concerns in older adults. J Aging Phys Act. (2020) 28:155–68. doi: 10.1123/japa.2017-0408
37. Liu, TW, Ng, GYF, Chung, RCK, and Ng, SSM. Cognitive behavioural therapy for fear of falling and balance among older people: a systematic review and meta-analysis. Age Ageing. (2018) 47:520–7. doi: 10.1093/ageing/afy010
38. World Health Organization. WHO guidelines on physical activity and sedentary behaviour: at a glance. Geneva: World Health Organization (2020).
39. Tou, NX, Goh, SF, Harding, S, Tsao, MA, Ng, TP, and Wee, SL. Effectiveness of community-based Baduanjin exercise intervention for older adults with varying frailty status: a randomized controlled trial. Eur Rev Aging Phys Act. (2024) 21:28. doi: 10.1186/s11556-024-00363-6
40. Pinheiro, MB, Sherrington, C, Howard, K, Caldwell, P, Tiedemann, A, Wang, B, et al. Economic evaluations of fall prevention exercise programs: a systematic review. Br J Sports Med. (2022) 56:1353–65. doi: 10.1136/bjsports-2022-105747
41. Cui, Z, Xiong, J, Li, Z, and Yang, C. Tai chi improves balance performance in healthy older adults: a systematic review and meta-analysis. Front Public Health. (2024) 12:1443168. doi: 10.3389/fpubh.2024.1443168
42. Lin, X-z, Meng, R, Peng, D, Li, C, Zheng, X, Xu, H, et al. Cross-sectional study on prevalence and risk factors for falls among the elderly in communities of Guangdong Province, China. BMJ Open. (2022) 12:e062257. doi: 10.1136/bmjopen-2022-062257
43. Barreto, PS, Rolland, Y, Vellas, B, and Maltais, M. Association of Long-Term Exercise Training with Risk of falls, fractures, hospitalizations, and mortality in older adults. JAMA Intern Med. (2019) 179:394–405. doi: 10.1001/jamainternmed.2018.5406
44. Wang, Q, Jiang, X, Shen, Y-C, Yao, P, Chen, J, Zhou, Y, et al. Effectiveness of exercise intervention on fall-related fractures in older adults: a systematic review and Meta-analysis of randomized controlled trials. BMC Geriatr. (2020) 20:322. doi: 10.1186/s12877-020-01721-6
45. Lenouvel, E, Ullrich, P, Siemens, W, Dallmeier, D, Denkinger, M, Kienle, G, et al. Cognitive behavioural therapy (CBT) with and without exercise to reduce fear of falling in older people living in the community. Cochrane Database Syst Rev. (2023) 11:CD014666. doi: 10.1002/14651858.CD014666.pub2
46. Landers, MR, Oscar, S, Sasaoka, J, and Vaughn, K. Balance confidence and fear of falling avoidance behavior are Most predictive of falling in older adults: prospective analysis. Phys Ther. (2016) 96:433–42. doi: 10.2522/ptj.20150184
47. Jönsson, U, Bertilsson, G, Allard, P, Gyllensvärd, H, Söderlund, A, Tham, A, et al. Psychological treatment of depression in people aged 65 years and over: a systematic review of efficacy, safety, and cost-effectiveness. PLoS One. (2016) 11:e0160859. doi: 10.1371/journal.pone.0160859
48. Kim, M, Shin, E, Kim, S, and Sok, SR. The effectiveness of multi-component intervention on daily functioning among the community-dwelling elderly: a systematic review. Int J Environ Res Public Health. (2022) 19:7483. doi: 10.3390/ijerph19127483
49. Montero-Odasso, M, van der Velde, N, Martin, FC, Petrovic, M, Tan, MP, Ryg, J, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. (2022) 51:51. doi: 10.1093/ageing/afac205
50. Huang, TT, Yang, LH, and Liu, CY. Reducing the fear of falling among community-dwelling elderly adults through cognitive-behavioural strategies and intense tai chi exercise: a randomized controlled trial. J Adv Nurs. (2011) 67:961–71. doi: 10.1111/j.1365-2648.2010.05553.x
51. Wetherell, JL, Johnson, K, Chang, DG, Ward, SR, Bower, ES, Merz, C, et al. Activity, balance, learning, and exposure (ABLE): a new intervention for fear of falling. Int J Geriatr Psychiatry. (2016) 31:791–8. doi: 10.1002/gps.4393
Keywords: fear of falling, aged, physical-activity therapy, cognitive behavioral therapy, umbrella review
Citation: Sheng Y, Wang C, Wang Y, Pan L, Zhang M, Liu D and Gao W (2025) An umbrella review of physical-activity therapy and cognitive behavioral therapy in reducing fear of falling among community-dwelling older adults: insights on intervention intensity and duration. Front. Public Health. 12:1498451. doi: 10.3389/fpubh.2024.1498451
Edited by:
Ladda Thiamwong, University of Central Florida, United StatesReviewed by:
Adela Badau, Transilvania University of Brașov, RomaniaVeronica Decker, University of Central Florida, United States
Copyright © 2025 Sheng, Wang, Wang, Pan, Zhang, Liu and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Deshan Liu, c2R1bGRzQDE2My5jb20=; Wei Gao, Z2Fvd2Vpc2R1QDE2My5jb20=
†These authors have contributed equally to this work
 Yuan Sheng
Yuan Sheng Caili Wang
Caili Wang Yan Wang1
Yan Wang1