- 1Department of Health Research, ICMR-Regional Medical Research Centre, Bhubaneswar, Odisha, India
- 2South Asian Institute of Health Promotion, Bhubaneswar, Odisha, India
Introduction: The increase in the prevalence of obesity has become a common public health issue worldwide, with low- and middle-income countries (LMICs) like India witnessing an equal rise. It makes a considerable contribution to chronic diseases as it is a major risk factor for other chronic illnesses. Multimorbidity, or the presence of two or more chronic illnesses, is becoming more common in LMICs, resulting in poor health outcomes. However, research on obesity and multimorbidity in younger populations in LMICs is scarce, with most studies focusing on older persons. The study analyzed sex differences in the prevalence of obesity among reproductive-aged persons and its association with multimorbidity, as well as investigated their health-seeking behaviors.
Methods: Data from the National Family Health Survey (NFHS-5) involving 751,831 females and 100,656 males were analyzed. Multimorbidity was defined by the presence of two or more chronic conditions out of the eight included chronic conditions. Multivariable logistic regression was applied to identify factors associated with obesity.
Result: The prevalence of obesity was 48.90% (95% CI: 48.60–49.20%) among males and 57.10% (95% CI: 57.00–57.22%) among females. Waist-to-Hip Ratio (WHR) revealed higher obesity rates in females with multiple chronic conditions (70.8%) compared to males (65.1%). Males with multimorbidity had a 47% higher likelihood of having obesity (AOR: 1.47, 95% CI: 1.13–1.89, p < 0.003) compared to individuals without obesity.
Conclusion: The study highlights high obesity prevalence among reproductive-aged individuals in India, with females having higher obesity rates overall. However, males with multimorbidity exhibit a significantly greater likelihood of obesity than males without. These findings emphasize the need for gender-specific public health strategies addressing obesity and multimorbidity, including promoting healthier diets, increasing physical activity, and improving disease management for both women and men.
Introduction
Obesity has arisen as a major public health issue, with critical levels in many countries, including low- and middle-income countries (LMICs). It is a major risk factor for chronic illnesses such as cardiovascular disease, diabetes, musculoskeletal problems, and some malignancies (1). The World Health Organization (WHO) estimates that 890 million persons globally, representing 16% of the global adult population have obesity, including 18.3% of females and 13.7% of males (1). Waist-hip ratio (WHR) of ≥0.90 cm for males and ≥ 0.85 cm for females defined as obesity. WHR, measured as the ratio of waist circumference to hip circumference, is a commonly used body composition measurement that is a powerful predictor of obesity-related health consequences (2). Studies have shown that the WHR is a more accurate predictor for chronic diseases than body mass index (BMI), commonly used to measure obesity. This provides insight into body composition and contributes to chronic diseases due to their correlation with excess body fat (3, 4). A high WHR is closely linked to an increased risk of having obesity-related health diseases such as type 2 diabetes mellitus (T2DM), site-specific malignancies, cardiovascular events, chronic renal disease, musculoskeletal disorders, and infections (5, 6).
Multimorbidity, defined as the presence of two or more chronic illnesses in one person without focusing on a specific index disease, has become a norm in LMICs. It is increasingly associated with negative health outcomes such as disabilities, deaths, hospitalizations, lower quality of life, and increased use of healthcare services (7). Unhealthy lifestyle choices, such as insufficient physical exercise, poor food, smoking, and excessive alcohol consumption, have all contributed to the increasing prevalence of non-communicable diseases (NCDs), including obesity (8, 9).
Despite the significant healthcare expenses associated with multimorbidity and obesity, little is known about their prevalence in low- and middle-income countries (LMICs) (10). In India, obesity affects 40.3% of the population, with females having a greater prevalence (41.88%) than males (38.67%). Obesity rates are greater in cities (44.17%) than in rural areas (36.08%), and people over 40 had a higher prevalence (45.81%) than those under 40 (34.58%) (11). A Chinese study found a link between obesity and an increased risk of multimorbidity among people 65 and older, with the risk increasing with age (12).
Given the potential long-term impacts of early multimorbidity on both individuals and society, the reproductive-aged population is particularly vulnerable to the adverse effects of obesity. Studying sex differences in obesity and early onset of multimorbidity among Indian females of reproductive age provides valuable insights. Sex-specific analysis is crucial for understanding the progression of chronic conditions and implementing timely interventions. Such information is essential for shaping public health policies to reduce the incidence of these conditions and improve health outcomes. Thus, we examined sex differences in obesity prevalence and its correlates among reproductive-aged individuals (15–49 years for females, 15–54 years for males). Additionally, we explored the association between obesity and multimorbidity and investigated healthcare utilization among participants.
Materials and methods
Overview of data
In partnership with the Ministry of Health and Family Welfare, the International Institute for Population Sciences (IIPS) conducted the nationwide Family Health Survey (NFHS) in India, an extensively representative nationwide survey. The most recent survey, NFHS-5, collected information from 29 states and 7 Union Territories (UTs) between 2019 and 2021.
Study design and study population
This study uses secondary data from the NFHS-5 dataset. The study included females aged 15–49 who were not pregnant and had not given birth in the 2 months before the survey, as well as males aged 15–54 years.
Sample size and sampling technique
A two-stage selection procedure was employed to choose villages in rural areas and Census Enumeration Blocks (CEBs) in cities. Data were gathered using Computer-Assisted Personal Interviewing (CAPI) to ensure accuracy and efficiency. The sampling process used in NFHS-5 was a methodical approach to select households, assuring national and district-level representation. 751,831 females and 100,656 males of reproductive age took part in face-to-face interviews. The precise sample techniques and data collection methods utilized in NFHS-5 have already been published, providing methodological transparency and reproducibility (13).
Data variable
Outcome characteristics
Anthropometric data, such as waist and hip circumferences, were obtained using Gulick Tape to act as a biomarker for obesity. These measures were used to compute the waist-to-hip ratio (WHR), which is a good indicator of body fat distribution and a predictor of abdominal obesity. Obesity was defined as a WHR of more than 0.9 for males and 0.85 for females.
Sociodemographic characteristics
The sociodemographic details collected from respondents encompassed age, sex, residence type (urban or rural), caste (classified into four categories), educational background (divided into four stages), employment status (employed or unemployed), wealth index (segmented into five quintiles), and current relationship status. The age for females was categorized as 15–19, 20–29, 30–39, and 40–49 years, while for males they were 15–19, 20–29, 30–39, 40–49, and 50–54 years. Marital status was categorized into “married” (currently married), “formerly/ever married” (including divorced, widowed, or separated), and “unmarried” (never married). Educational attainment was categorized as “no education” (no formal schooling), “up to primary” (less than 5 years of schooling), “up to secondary” (5 to 9 years of schooling), and “higher” (more than 10 years of schooling). Employment status was divided into “employed” (engaged in any form of occupation including professional, technical, managerial, clerical, sales, service, agricultural, skilled, or unskilled labor) and “unemployed” (not engaged in any work). The geographical region was classified into “north,” “central,” “east,” “northeast,” “west,” and “south.” Wealth categories included “poorest,” “poorer,” “middle,” “wealthier,” “richer,” and “richest,” based on household assets. Healthcare usage was categorized by facility type: “public,” “private,” “NGO/trust hospitals/clinics,” and “others” (such as pharmacies, home treatment, or alternative sources). Health insurance status was divided into “has a health insurance scheme” and “does not have a health insurance scheme. The parity of females was categorized into “nulliparous,” “primiparous,” and “multiparous.”
Multimorbidity
Multimorbidity was assessed through self-reported information on the presence of eight chronic conditions, including diabetes, hypertension, asthma, goiter or other thyroid disorders, cardiac disease, cancer, chronic kidney disease, and HIV. For the study, multimorbidity was classified into two groups: “absent” (having none or one chronic condition) and “present” (having two or more chronic conditions).
Statistical analysis
The statistical analysis was carried out using STATA 16 (StataCorp, College Station, Texas, USA). Data that were flagged, missing, or incomplete were removed before analysis, and variables were recoded as necessary. To overcome the differential probabilities of participant selection, NFHS sampling weights were used, ensuring the findings’ correctness and representativeness. The prevalence of chronic illnesses, obesity, and their predictors was calculated using weighted proportions, and the results were provided with 95% confidence intervals (CIs) to express uncertainty. All independent factors were subjected to unadjusted logistic regression, with findings presented as odds ratios (OR) and 95% confidence intervals. Following that, multivariable logistic regression was performed. The findings were presented as adjusted odds ratios (AOR) with 95% confidence intervals and significance determined by p-values less than 0.001.
Ethical consideration
This study posed no risk to participants, as it utilized secondary, anonymized data from the NFHS. Informed consent was obtained from all respondents during the original survey. Proper acknowledgment and citation of the dataset used in the analysis were ensured, following ethical guidelines.
Results
Sociodemographic characteristics
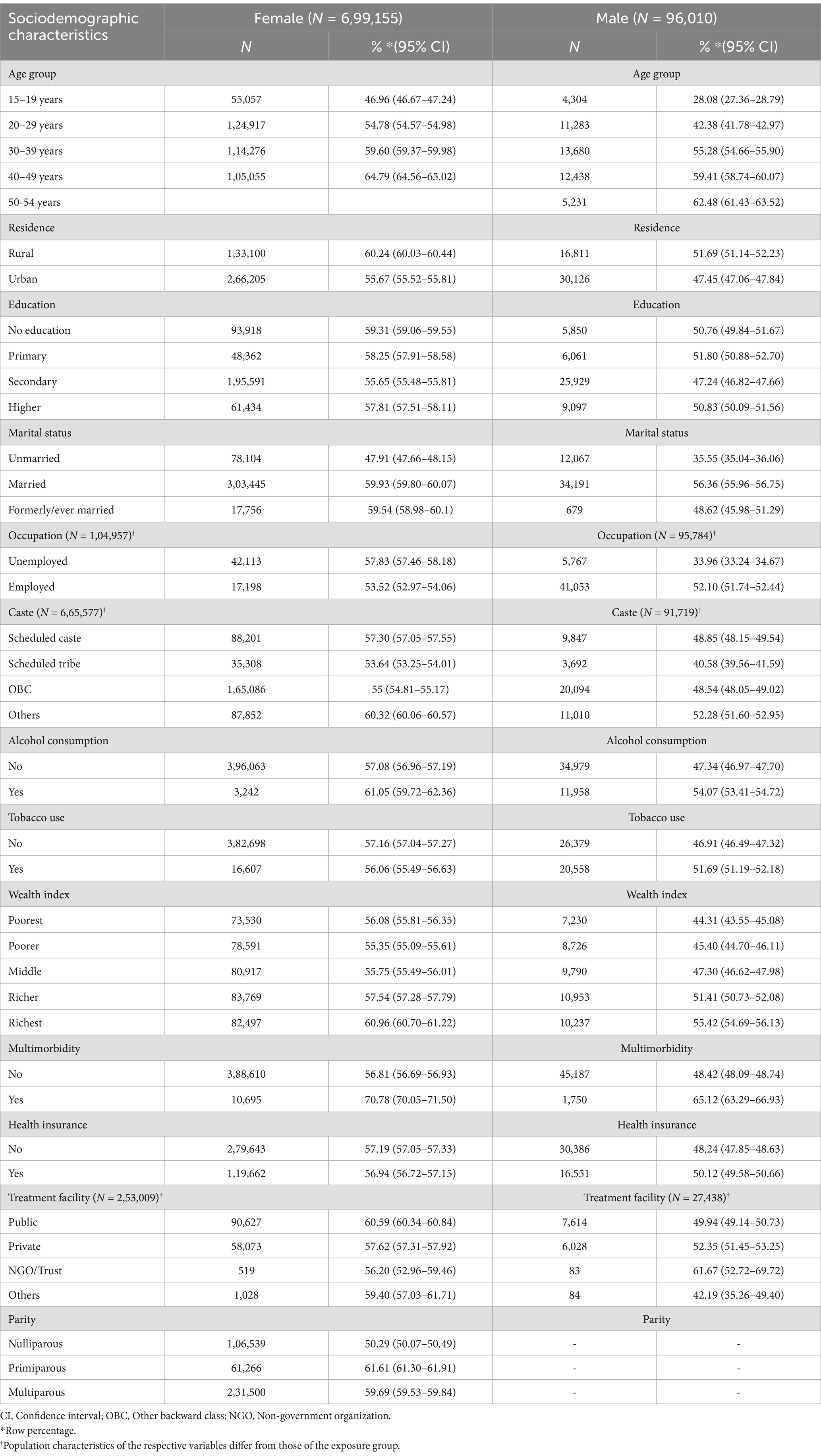
The average age of male respondents was 32.21 ± 11.21 years, ranging from 15 to 54 years, while that for the female respondents was 30.40 ± 9.88 years, ranging from 15 to 49 years. The majority of participants were between 20 and 29 years old. Around 75% of respondents lived in metropolitan areas, and more than half had completed secondary school. A significant 67.8% of females were unemployed, while 81.1% of males worked. The majority of individuals did not smoke tobacco. Furthermore, 63.4% of males and 67.9% of females did not have health insurance. Over half of the participants used public health services. Additional information is provided in Table 1.
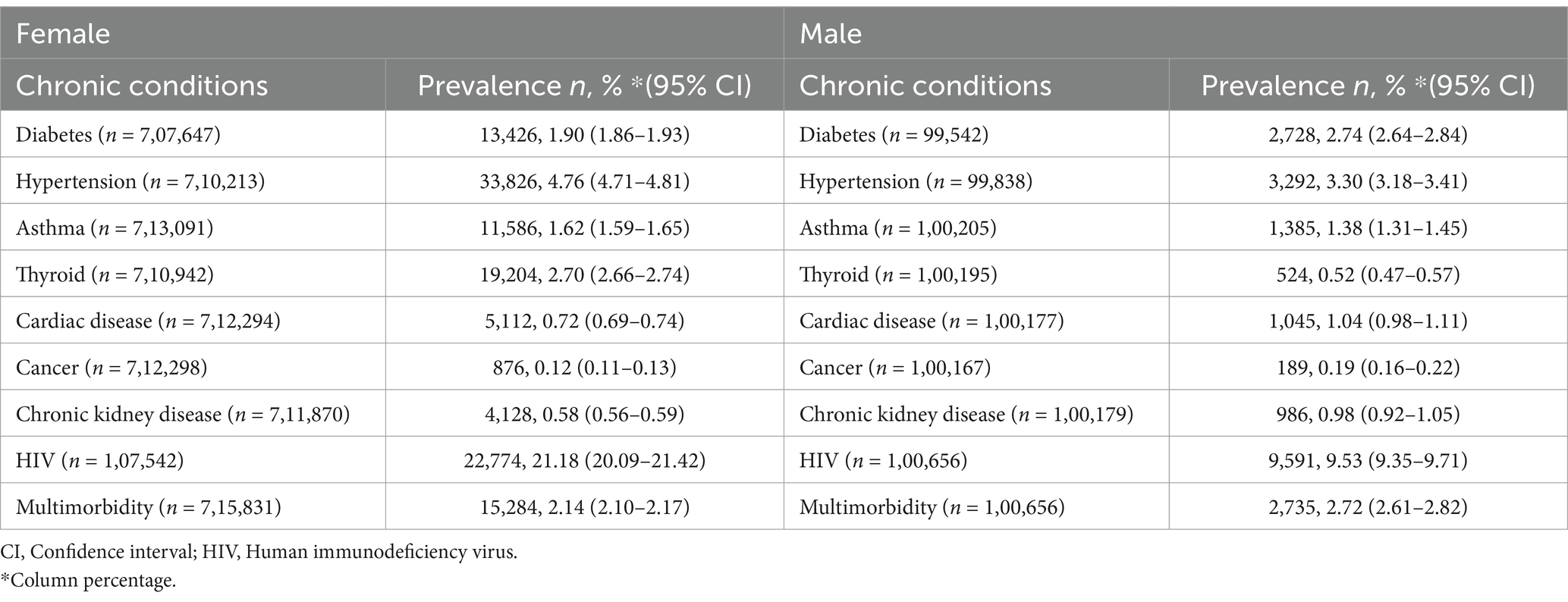
Profile of various chronic conditions
The prevalence of multimorbidity was 2.72% in males and 2.14% in females. HIV emerged as the most common chronic disease, affecting 21.18% of females (95% CI: 20.09–21.42) and 9.53% of males (95% CI: 9.35–9.71). Hypertension was the second most prevalent condition, affecting 4.76% of females (95% CI: 4.71–4.81) and 3.30% of males (95% CI: 3.18–3.41). Cancer had the lowest prevalence, affecting 0.12% of females (95% CI: 0.11–0.13) and 0.19% of males (95% CI: 0.16–0.22). Table 2 provides a full summary of chronic illnesses.
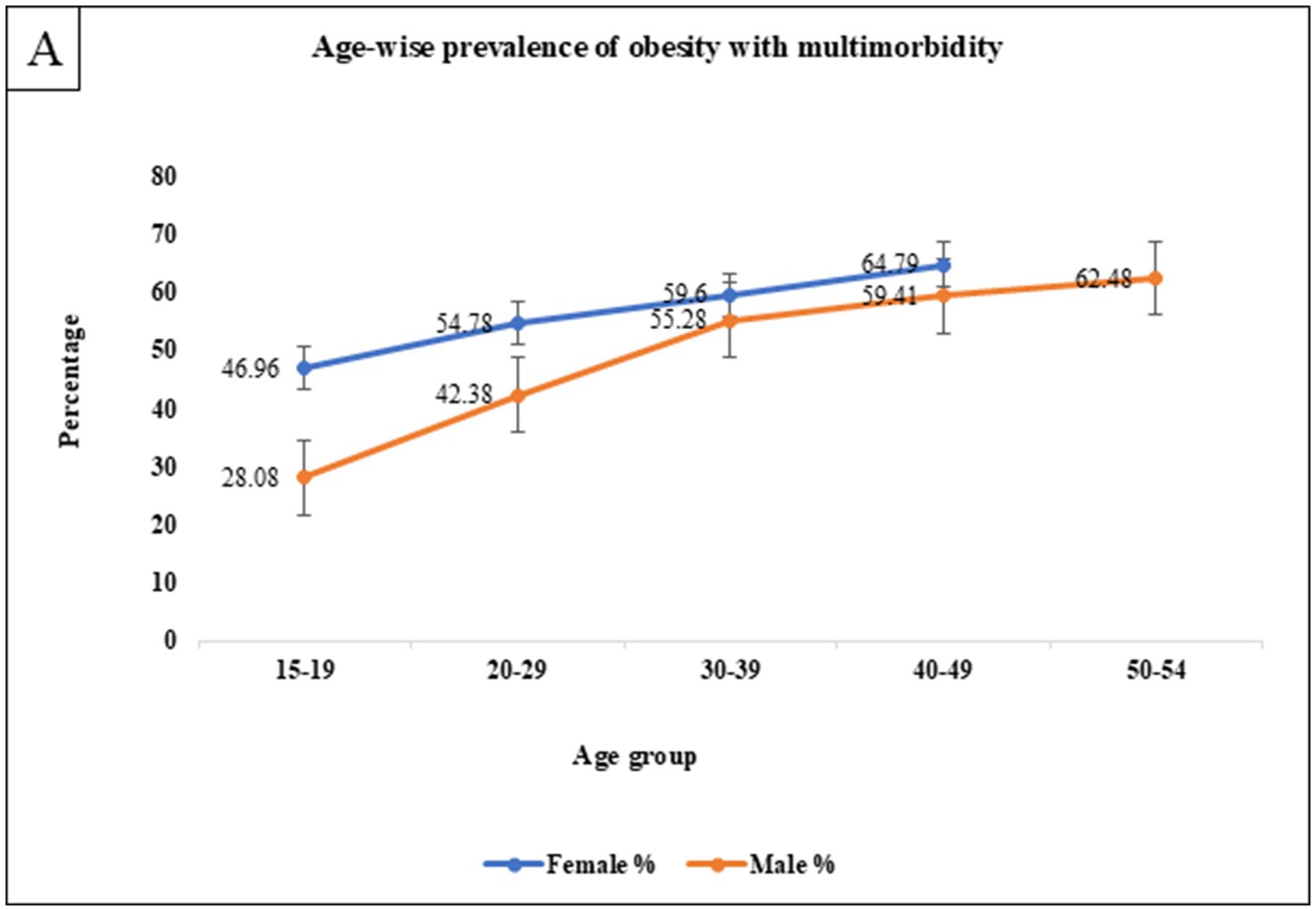
Prevalence of obesity with sociodemographic characteristics
The overall prevalence of obesity was 48.89% (95% CI: 48.57–49.20) among males and 57.11% (95% CI: 57.00–57.23) among females. As detailed in Table 3, obesity rates increased with age, peaking at 62.48% for males aged 50 to 54 years and 64.79% for females aged 40 to 49 years. Obesity was more prevalent among rural residents and women without formal education (59.31%). Higher rates were observed among unemployed women (57.83%) and employed men (52.10%). Alcohol consumption was strongly associated with obesity, with 61.05% of males and 54.07% of females affected. Additionally, individuals in the richest wealth quintile exhibited higher obesity rates, with 55.42% of males and 60.96% of females classified as people having obesity. Multimorbidity further amplified the prevalence of obesity, affecting 65.12% of males and 70.78% of females, indicating a slight predominance among females. Nulliparous women constituted a smaller proportion (50.29%, n = 1,06,539) compared to both primiparous (61.61%, n = 61,266) and multiparous (59.69%, n = 2,31,500). The predominance of multiparous women underscores the potential influence of parity on obesity and multimorbidity outcomes (Figure 1).
Association of obesity with multimorbidity
A univariate logistic regression analysis revealed significant associations of obesity with various factors, including age, marital status, residence, occupation, caste, and wealth index, in both men and women. Married women were 1.70 times more likely to have obesity [OR: 1.70, (95% CI: 1.48–1.95)] than unmarried women, while married men had 1.54 times greater chances [OR: 1.70, (95% CI: 1.32–1.81)] of having obesity than their unmarried counterparts. Furthermore, unemployment was linked to a 2.11-fold higher incidence of obesity in women [OR: 2.11, (95% CI: 1.99–2.25)].
Women aged 40 to 49 had 1.95 times higher risks of having obesity [AOR: 1.95, (95% CI: 1.68–2.28), p < 0.001] than those aged 15 to 19. Men aged 50–54 had 3.27 times greater risks [AOR: 3.27, (95% CI: 2.52–4.25), p < 0.001]. Women living in urban areas were 15% more likely to have obesity [AOR: 1.15, (95% CI: 1.07–1.25), p < 0.001] than those living in rural areas.
Marriage was found to be a significant predictor of obesity, with married women having 1.70 times higher chances [AOR: 1.70, (95% CI: 1.48–1.95), p < 0.001] and married men displaying 1.54 times larger odds [AOR: 1.54, (95% CI: 1.32–1.81), p < 0.001] than their unmarried counterparts. Men with the highest wealth index were 1.44 times more prone to have obesity [AOR: 1.44, (95% CI: 1.22–1.72)].
Men with multimorbidity were 47% more likely to have obesity [AOR: 1.47, (95% CI: 1.13–1.89), p < 0.003] than those without it. In contrast, tobacco use exhibited a negative connection with obesity, as male tobacco users were 9% less likely to have obesity compared to non-users [AOR: 0.91, (95% CI: 0.82–1.00), p = 0.052]. Multiparous women had 16% lower odds of having obesity [AOR: 0.84, (95% CI: 0.77–0.92), p < 0.001] compared to both nulliparous and primiparous women (Table 4).
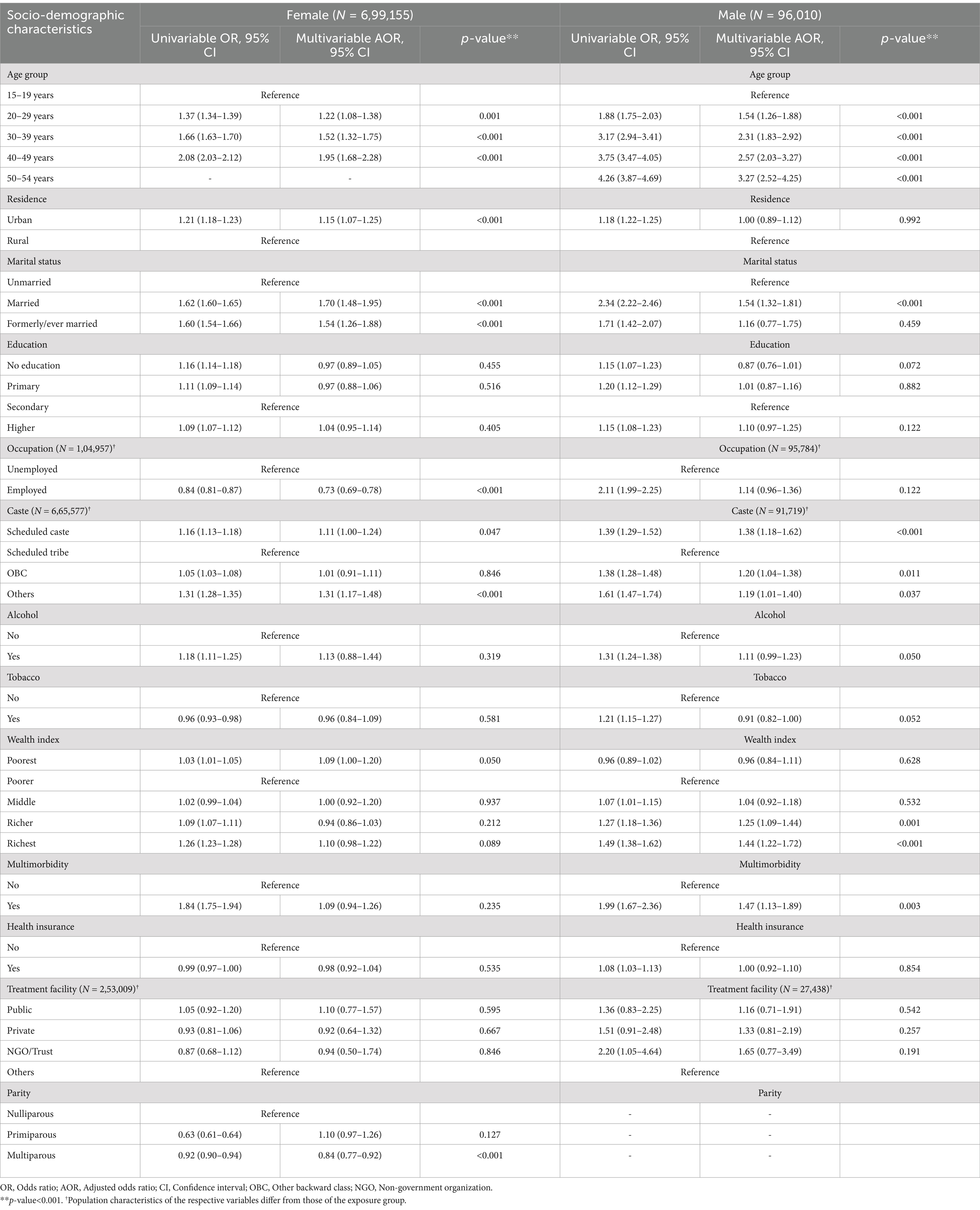
Table 4. Association of obesity with sociodemographic characteristics using univariable and multivariable regression.
Discussion
Our analysis reveals that obesity affects 48.89% of men (95% CI: 48.57–49.20) and 57.11% of women (95% CI: 57.00–57.23) in India. Significant risk factors for obesity identified include age, with the highest prevalence observed among women aged 40–49 and men aged 50–54; urban residency for women; the wealthiest quintile for men; marital status; and multimorbidity in men. Hypertension and HIV were identified as the most common chronic condition followed by diabetes and asthma across both genders.
The observed gender disparity in obesity aligns with earlier studies. Sinha et al. found that obesity was more prevalent among women (54.20%) compared to men (45.80%) (14), a trend also reported by Ruopeng An and Wang et al. (15–17). This difference may be attributed to the combination of hormonal, genetic, lifestyle, and cultural factors. For instance, estrogen promotes fat storage in women (18), while genetic predispositions may increase their vulnerability to obesity (19). Additionally, gendered lifestyle factors such as poor dietary habits, physical inactivity, and stress are known contributors to elevated obesity rates among women (20, 21). Health disparity has been similarly observed in LMICs, as evidenced by a study in Nepal and among tribal older adults reporting that one-fourth of the population experienced multimorbidity, highlighting the challenges of health conditions in these settings (22, 23). The escalating obesity rates in India can be linked to rapid urbanization, increased mechanized transport, consumption of processed foods, sedentary behaviors, and diets high in calories but low in nutrients (24).
Age also emerged as a critical factor in obesity, with older age being a recognized risk for having obesity and related non-communicable diseases (15). Venkatrao et al. reported that obesity rates were notably higher among individuals over 40 years (45.81%) compared to those under 40 years (34.58%) (11). This underscores the importance of addressing both immutable factors like age and biological sex, as well as modifiable factors such as educational attainment and physical activity, in obesity prevention strategies.
Alcohol consumption was significantly associated with obesity, with 61.05% of women and 54.07% of men affected. This aligns with evidence linking alcohol’s high caloric content and metabolic effects to weight gain, particularly in women (25, 26). Conversely, tobacco use was inversely related to obesity among men, with 51.69% of men having obesity reporting tobacco use. This aligns with previous studies indicating that smoking may suppress appetite and increase energy expenditure, thereby contributing to lower body weight (27). However, the health risks associated with tobacco use complicate its role in obesity management, suggesting a need for comprehensive public health strategies that address both tobacco cessation and obesity prevention (28, 29).
The study also highlights a positive association between wealth, urban residence, and obesity in reproductive-aged women. Higher obesity rates among wealthier individuals are likely influenced by dietary changes, reduced physical activity associated with urban living, and other related factors (30, 31). The increasing prevalence of abdominal obesity can be linked to the adoption of sedentary lifestyles and Western dietary patterns high in sugars, fats, and preservatives (32–34). Our findings demonstrate that sociodemographic factors such as education and employment contribute to sex-specific obesity trends. For women, the protective effect of employment likely reflects increased physical activity in certain occupational roles. Conversely, higher education does not confer substantial protection against obesity, likely due to behavioral and cultural influences. These findings align with studies by Anekwe et al. and Wang D et al., emphasizing the complex, multifactorial nature of obesity determinants (35, 36). Parity significantly influences reproductive health outcomes, particularly weight retention and obesity risk among women. The physiological changes during pregnancy and the postpartum period often result in weight gain, which can persist and become more pronounced with multiple pregnancies. Makama et al. report that 20% of women experience postpartum weight retention, emphasizing its public health relevance and the need for sex-sensitive interventions (37).
Our study confirms a strong association between obesity and multimorbidity, especially in men. Kivimaki et al. showed that a higher BMI markedly raises the risk of developing various cardiovascular and metabolic conditions, with overweight individuals being twice as likely and those who are severely obese more than 10 times as likely to encounter these conditions compared to those with a normal BMI (38). Obesity is a major contributor to various health issues, with recent research suggesting that people with obesity tend to experience multimorbidity earlier than those of normal weight (39–42).
Policy implication
The observed connection between obesity and multimorbidity in both sexes underscores the necessity for sex- and gender-sensitive policies and strategies to address this issue effectively. To reduce the risk of multimorbidity, it is essential to implement early interventions and preventive measures, particularly in regions with limited healthcare resources. Strategies could include integrating nutrition education into public health campaigns, implementing stricter food labeling regulations, promoting access to healthy food in workplaces, and designing culturally relevant educational programs to encourage healthier lifestyles (43, 44). Public health policies must also account for family-level interventions, as multimorbidity tends to cluster in urban, affluent populations, increasing healthcare expenditures (45). Integrating NCD risk reduction into medical training and fostering preventive practices in clinical settings can prepare healthcare professionals to tackle these challenges more effectively (46). A comprehensive approach that incorporates sex- and gender-sensitive and family-centered strategies is essential to mitigate the burden of obesity and multimorbidity among reproductive-age groups in India. Policymakers should prioritize improving healthcare access and affordability while promoting physical activity. This study underscores the importance of a holistic, gender-focused framework for addressing obesity and multimorbidity, particularly in India and other low- and middle-income countries (LMICs).
Strength and limitation
A major strength of this study is its use of anthropometric measurements, such as hip and waist circumference, to assess obesity, providing accurate indications of the disease. Furthermore, using data from a nationally representative survey increases the applicability of the findings. However, the cross-sectional nature of the data limits the ability to identify causal links. Furthermore, relying on self-reported chronic diseases may add bias, reducing the precision of prevalence estimates.
Conclusion
This study reveals a significant sex and gender disparity in obesity and multimorbidity among India’s reproductive-aged population, with females disproportionately affected by obesity. These findings call for sex- and gender-specific public health strategies to address the rising burden of NCDs. Targeted interventions promoting healthier diets, increased physical activity, and lifestyle changes are crucial for women. Policies must address root causes such as sedentary behavior and poor nutrition. The higher prevalence of obesity among females underscores the need for targeted interventions addressing female-specific factors such as hormonal influences, sociocultural norms, and lifestyle patterns. The stronger association between multimorbidity and obesity in males highlights that males with existing chronic conditions may require more tailored strategies for weight management and prevention of further complications. Strengthening healthcare systems to ensure equitable, accessible care, particularly for women from disadvantaged backgrounds, is essential. Integrating prevention with better healthcare delivery will improve health outcomes and reduce the burden on the healthcare system.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: International Institute for Population Sciences (IIPS) - https://www.iipsindia.ac.in/.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
JM: Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources. AS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. RA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. BR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. SK: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. SP: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank the National Family Health Survey (NFHS) for assembling and publishing meticulous, nationally depictive data on various health, biomarkers, and healthcare utilization indicators for females aged 15-49 and males aged 15-54. The authors are also grateful to NFHS’s project partners, the International Institute for Population Sciences (IIPS), Mumbai.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, Adjusted Odds Ratio; CAPI, Computer-assisted personal interview; CI, Confidence Interval; CEB, Census Enumeration Blocks; DHS, Demographic Health Survey; HIV, Human Immunodeficiency Virus; IEC, Information education communication; IIPS, International Institute for Population Sciences; LMIC, Low-and middle-income countries; NCDs, Non-communicable diseases; NFHS, National Family Health Survey; NGO, Non-government organization; T2DM, Type II Diabetes Mellitus; WHR, Waist to Hip Ratio.
References
1. World Health Organization. (2024). Obesity and overweight. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed January 05, 2024).
2. Sruthi, KG, John, SM, and David, SM. Assessment of obesity in the Indian setting: a clinical review. Clinical epidemiology and global. Health. (2023) 23:101348. doi: 10.1016/j.cegh.2023.101348
3. Tewari, A, Kumar, G, Maheshwari, A, Tewari, V, and Tewari, J. Comparative evaluation of waist-to-height ratio and BMI in predicting adverse cardiovascular outcome in people with diabetes: a systematic review. Cureus. (2023) 15:e38801. doi: 10.7759/cureus.38801
4. Khanna, D, Peltzer, C, Kahar, P, and Parmar, MS. Body mass index (BMI): a screening tool analysis. Cureus. (2022) 14:e22119. doi: 10.7759/cureus.22119
5. Powell-Wiley, TM, Poirier, P, Burke, LE, Després, JP, Gordon-Larsen, P, Lavie, CJ, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. (2021) 143:e984–e1010. doi: 10.1161/CIR.0000000000000973
6. Ashwell, M, and Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. (2016) 6:e010159. doi: 10.1136/bmjopen-2015-010159
7. Sinha, A, Kerketta, S, Ghosal, S, Kanungo, S, Lee, JT, and Pati, S. Multimorbidity and complex multimorbidity in India: findings from the 2017–2018 longitudinal ageing study in India (LASI). Int J Environ Res Public Health. (2022) 19:9091. doi: 10.3390/ijerph19159091
8. Harridge, SD, and Lazarus, NR. Physical activity, aging, and physiological function. Physiology. (2017) 32:152–61. doi: 10.1152/physiol.00029.2016
9. Varanasi, R, Sinha, A, Bhatia, M, Nayak, D, Manchanda, RK, Janardhanan, R, et al. Epidemiology and impact of chronic disease multimorbidity in India: a systematic review and meta-analysis. J Multimorb Comorb. (2024) 14:26335565241258851. doi: 10.1177/26335565241258851
10. Romano, E, Ma, R, Vancampfort, D, Firth, J, Felez-Nobrega, M, Haro, JM, et al. Multimorbidity and obesity in older adults from six low-and middle-income countries. Prev Med. (2021) 153:106816. doi: 10.1016/j.ypmed.2021.106816
11. Venkatrao, M, Nagarathna, R, Majumdar, V, Patil, SS, Rathi, S, and Nagendra, H. Prevalence of obesity in India and its neurological implications: a multifactor analysis of a nationwide cross-sectional study. Ann Neurosci. (2020) 27:153–61. doi: 10.1177/0972753120987465
12. Zhang, L, Ma, L, Sun, F, Tang, Z, and Chan, P. A multicentre study of multimorbidity in older adult inpatients in China. J Nutr Health Aging. (2020) 24:269–76. doi: 10.1007/s12603-020-1311-x
13. Chenrayudu, N, and Chandrasekarayya, T. (2021). Sex composition of population: an analysis of NFHS – 5 data. Available at: https://sciresol.s3.us-east-2.amazonaws.com/srs-j/bu_journals/GA/pdf/Volume-10/issue-2/GA_v10i2_1.pdf (Accessed January 05, 2024).
14. Sinha, A, Puri, P, and Pati, S. Social determinants of diabesity and its association with multimorbidity among older adults in India: a population-based cross-sectional study. BMJ Open. (2022) 12:e061154. doi: 10.1136/bmjopen-2022-061154
15. An, R. Diet quality and physical activity in relation to childhood obesity. Int J Adolesc Med Health. (2017) 29:45. doi: 10.1515/ijamh-2015-0045
16. Wang, T, Lu, Q, Zhang, H, Xue, H, Wang, J, Li, D, et al. Study on the prevalence and relationship of obesity and hypertension in southern mountain areas of Ningxia. Chin J Endocrinol Metab. (2018) 12:281–6.
17. Vrettos, I, Voukelatou, P, Pappa, E, Beletsioti, C, and Niakas, D. Gender differences in health-related quality of life (HRQL) of overweight and obese adults in a representative sample of Greek urban population. Iran J Public Health. (2021) 50:2038. doi: 10.18502/ijph.v50i10.7504
18. Ko, SH, and Jung, Y. Energy metabolism changes and dysregulated lipid metabolism in postmenopausal women. Nutrients. (2021) 13:4556. doi: 10.3390/nu13124556
19. Utkirzhonovna, SN. Main risk factors for overweight and obesity in young people. Eurasian Med. Res. Period. (2022) 7:141–6.
20. Sabra, AA, Taha, AZ, Al-Sebiany, AM, Al-Kurashi, NY, and Al-Zubier, AG. Coronary heart disease risk factors: prevalence and behavior among male university students in Dammam City, Saudi Arabia. J Egypt Public Health Assoc. (2007) 82:21–42.
21. Khabaz, MN, Bakarman, MA, Baig, M, Ghabrah, TM, Gari, MA, Butt, NS, et al. Dietary habits, lifestyle pattern and obesity among young Saudi university students. JPMA. The. J Pak Med Assoc. (2017) 67:1541–6.
22. Sinha, A, Suman, SS, Subedi, N, Sahoo, KC, Poudel, M, Chauhan, A, et al. Epidemiology of multimorbidity in Nepal: a systematic review and meta-analysis. J Multimorb Comorb. (2024) 14:26335565241284022. doi: 10.1177/26335565241284022
23. Sinha, A, Kanungo, S, Bhattacharya, D, Kaur, H, and Pati, S. Non-communicable disease multimorbidity among tribal older adults in India: evidence from study on global AGEing and adult health, 2015. Front Public Health. (2023) 11:1217753. doi: 10.3389/fpubh.2023.1217753
24. Misra, A, Singhal, N, and Khurana, L. Obesity, the metabolic syndrome, and type 2 diabetes in developing countries: role of dietary fats and oils. J Am Coll Nutr. (2010) 29:289S–301S. doi: 10.1080/07315724.2010.10719844
25. Traversy, G, and Chaput, JP. Alcohol consumption and obesity: an update. Curr Obes Rep. (2015) 4:122–30. doi: 10.1007/s13679-014-0129-4
26. Åberg, F, Byrne, CD, Pirola, CJ, Männistö, V, and Sookoian, S. Alcohol consumption and metabolic syndrome: clinical and epidemiological impact on liver disease. J Hepatol. (2023) 78:191–206. doi: 10.1016/j.jhep.2022.08.030
27. Taylor, AE, Richmond, RC, Palviainen, T, Loukola, A, Wootton, RE, Kaprio, J, et al. The effect of body mass index on smoking behaviour and nicotine metabolism: a Mendelian randomization study. Hum Mol Genet. (2019) 28:1322–30. doi: 10.1093/hmg/ddy434
28. Murmu, J, Agrawal, R, Manna, S, Pattnaik, S, Ghosal, S, Sinha, A, et al. Social determinants of tobacco use among tribal communities in India: evidence from the first wave of longitudinal ageing study in India. PLoS One. (2023) 18:e0282487. doi: 10.1371/journal.pone.0282487
29. Tsikrika, S, Dai, S, Dilektasli, A, Katsaounou, P, and Dagli, E. Challenges and perspectives of tobacco cessation in special groups of patients and populations. Breathe. (2023) 19:220224. doi: 10.1183/20734735.0224-2022
30. Ntandou, G, Delisle, H, Agueh, V, and Fayomi, B. Abdominal obesity explains the positive rural-urban gradient in the prevalence of the metabolic syndrome in Benin, West Africa. Nutr Res. (2009) 29:180–9. doi: 10.1016/j.nutres.2009.02.001
31. BeLue, R, Okoror, TA, Iwelunmor, J, Taylor, KD, Degboe, AN, Agyemang, C, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Glob Health. (2009) 5:1–2. doi: 10.1186/1744-8603-5-10
32. Seo, MH, Lee, WY, Kim, SS, Kang, JH, Kang, JH, Kim, KK, et al. 2018 Korean society for the study of obesity guideline for the management of obesity in Korea. J Obes Metab Syndr. (2019) 28:40–5. doi: 10.7570/jomes.2019.28.1.40
33. Saklayen, MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. (2018) 20:1–8. doi: 10.1007/s11906-018-0812-z
34. Shin, JH, Jung, S, Kim, SA, Kang, MS, Kim, MS, Joung, H, et al. Differential effects of typical Korean versus American-style diets on gut microbial composition and metabolic profile in healthy overweight Koreans: a randomized crossover trial. Nutrients. (2019) 11:2450. doi: 10.3390/nu11102450
35. Anekwe, CV, Jarrell, AR, Townsend, MJ, Gaudier, GI, Hiserodt, JM, and Stanford, FC. Socioeconomics of obesity. Curr Obes Rep. (2020) 9:272–9. doi: 10.1007/s13679-020-00398-7
36. Wang, D, Dai, X, Mishra, SR, Lim, CC, Carrillo-Larco, RM, Gakidou, E, et al. Association between socioeconomic status and health behaviour change before and after non-communicable disease diagnoses: a multicohort study. Lancet Public Health. (2022) 7:e670–82. doi: 10.1016/S2468-2667(22)00157-8
37. Makama, M, Skouteris, H, Moran, LJ, and Lim, S. Reducing postpartum weight retention: a review of the implementation challenges of postpartum lifestyle interventions. J Clin Med. (2021) 10:1891. doi: 10.3390/jcm10091891
38. Kivimaki, M, Kuosma, E, Ferrie, JE, Luukkonen, R, Nyberg, ST, Alfredsson, L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. (2017) 2:e277–85. doi: 10.1016/S2468-2667(17)30074-9
39. Agborsangaya, CB, Majumdar, SR, Sharma, AM, Gregg, EW, and Padwal, RS. Multimorbidity in a prospective cohort: prevalence and associations with weight loss and health status in severely obese patients. Obesity. (2015) 23:707–12. doi: 10.1002/oby.21008
40. Badley, EM, Canizares, M, Perruccio, AV, Hogg-Johnson, S, and Gignac, MA. Benefits gained, benefits lost: comparing baby boomers to other generations in a longitudinal cohort study of self-rated health. Milbank Q. (2015) 93:40–72. doi: 10.1111/1468-0009.12105
41. Robinson, WR, Utz, RL, Keyes, KM, Martin, CL, and Yang, Y. Birth cohort effects on abdominal obesity in the United States: the silent generation, baby boomers and generation X. Int J Obes. (2013) 37:1129–34. doi: 10.1038/ijo.2012.198
42. Sinha, A, Varanasi, R, and Pati, S. Kaleidoscopic use of World Health Organization's study on global ageing and adult health data set to explore multimorbidity and its outcomes in low and middle-income countries: An insider view. J Family Med Prim Care. (2021) 10:4623–5. doi: 10.4103/jfmpc.jfmpc_1598_21
43. Silva, P, Araújo, R, Lopes, F, and Ray, S. Nutrition and food literacy: framing the challenges to health communication. Nutrients. (2023) 15:4708. doi: 10.3390/nu15224708
44. Pineda, E, Atanasova, P, Wellappuli, NT, Kusuma, D, Herath, H, Segal, AB, et al. Policy implementation and recommended actions to create healthy food environments using the healthy food environment policy index (food-EPI): a comparative analysis in South Asia. Lancet Reg Health Southeast Asia. (2024) 26:100428. doi: 10.1016/j.lansea.2024.100428
45. Pati, S, Sinha, A, Ghosal, S, Kerketta, S, Lee, JT, and Kanungo, S. Family-level multimorbidity among older adults in India: looking through a syndemic lens. Int J Environ Res Public Health. (2022) 19:9850. doi: 10.3390/ijerph19169850
Keywords: reproductive-aging population, India, multimorbidity, chronic conditions, obesity, sex, gender, NFHS-5
Citation: Murmu J, Sinha A, Agrawal R, Rout B, Kanungo S and Pati S (2025) Sex and gender differentials in the prevalence of obesity and its association with multimorbidity among reproductive-aged individuals in India. Front. Public Health. 12:1496522. doi: 10.3389/fpubh.2024.1496522
Edited by:
Elena Marbán-Castro, Women in Global Health Spain, SpainReviewed by:
Xiyu Feng, Australian National University, AustraliaJohn Taormina, University of Colorado Anschutz Medical Campus, United States
Copyright © 2025 Murmu, Sinha, Agrawal, Rout, Kanungo and Pati. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Srikanta Kanungo, c3Jpa2FudGFrMTA5QGdtYWlsLmNvbQ==; Sanghamitra Pati, ZHJzYW5naGFtaXRyYTEyQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
‡ORCID: Jogesh Murmu, orcid.org/0000-0001-9428-9113
Abinav Sinha, orcid.org/0000-0001-7702-3671
Ritik Agrawal, orcid.org/0000-0001-5345-1559
Bhagyashree Rout, orcid.org/0009-0009-8785-8061
Sanghamitra Pati, orcid.org/0000-0002-7717-5592
 Jogesh Murmu
Jogesh Murmu Abhinav Sinha
Abhinav Sinha Ritik Agrawal
Ritik Agrawal Bhagyashree Rout
Bhagyashree Rout Srikanta Kanungo
Srikanta Kanungo Sanghamitra Pati
Sanghamitra Pati