- 1Hepatobiliary Pancreatic Surgery, Banan Hospital Affiliated of Chongqing Medical University, Chongqing, China
- 2Xiangya School of Medicine, Central South University, Changsha, China
Background: This study aimed to quantify the global impact of pneumoconiosis resulting from occupational exposure to particulate matter, gasses, and fumes from 1990 to 2021, utilizing data from the Global Burden of Disease Study 2021.
Method: The analysis evaluated the global, regional, and national burden of pneumoconiosis attributable to workplace exposure to particulate matter, gasses, and fumes. It explored variations in disease impact across different demographics, including age and gender, and analyzed the relationship between disease burden and the Socio-Demographic Index (SDI). Furthermore, an ARIMA model was employed to forecast future trends of pneumoconiosis up to 2050.
Result: The year 2021 saw pneumoconiosis from occupational particulate matter, gasses, and fumes account for roughly 4,775 deaths and 117.80 thousand disability-adjusted life years (DALYs). Over the past three decades, there was a notable decline in the disease’s burden. The condition predominantly affected males and those aged above 60. Future projections suggest a decrease in mortality rates in low to middle SDI regions, while high SDI regions may experience an increase in ASMR. Additionally, both ASMR and ASDR are anticipated to rise globally. Nationally, the Czech Republic, France, and the United States are expected to show relatively higher mortality rates in 2030 and 2050. Countries like Kazakhstan, Egypt, Mongolia, and Peru are projected to experience elevated levels of ASMR, DALY rates, and ASDR.
Conclusion: The findings underscore the urgent need for policymakers to create and improve targeted preventive strategies to reduce the incidence of pneumoconiosis among specific populations.
1 Introduction
Pneumoconiosis was a chronic occupational disease resulting from prolonged inhalation of solid phase particulate matter, which led to lung dysfunction (1). According to types of occupational dust inhaled, pneumoconiosis was classified into asbestosis, silicosis, coal worker pneumoconiosis (CWP), and other pneumoconiosis (2), especially in developing countries where coal was the main energy source. Millions of workers were regularly exposed to coal dust (including dust from coal mining or pure coal dust) during their working hours, thus having great risk to suffer from pneumoconiosis. Besides, individual behavioral factors such as smoking could be an associated factor due to many cohort studies, indicating that smoking workers had an obviously higher risk than non-smoking workers to develop pneumoconiosis (15). Furthermore, indoor air pollution may contribute to the incidence and exacerbation of hut lung, a domestically acquired pneumoconiosis of mixed etiology (3, 4). Despite decades of prevention efforts, pneumoconiosis remained a global public health problem, constituting a significant portion of occupational diseases (5).
Despite ongoing prevention efforts, coal worker pneumoconiosis (CWP) continues to pose a significant public health challenge globally, representing a substantial fraction of occupational diseases (5). Global Burden of Disease studies indicate a downward trend in pneumoconiosis prevalence since 2015, yet it still affects a significant population, with current figures showing around 527,500 cases and an annual death toll surpassing 21,000 (6–13). Currently, no effective treatment exists for the lung damage caused by pneumoconiosis, with care mostly aimed at symptomatic relief and rehabilitation (1). Understanding and addressing modifiable risk factors is crucial for the global prevention and management of pneumoconiosis.
Risk factors for pneumoconiosis include being male, smoking, older age, and occupational exposure to substances like silica, particulate matter (PM), gasses, fumes, and asbestos (14, 15). Numerous studies confirm the strong correlation between occupational exposures and the development of pneumoconiosis (16, 17). The inhalable fraction of PM can bypass the upper respiratory defenses, damaging lung tissues and cells through mechanisms such as cell apoptosis, oxidative stress, and inflammation, which contribute to the onset of pneumoconiosis (17). Additionally, workers who smoke are at a significantly higher risk of developing pneumoconiosis compared to non-smokers (15). However, a comprehensive evaluation of the impact of occupational particulate matter, gasses, and fumes on pneumoconiosis remains lacking.
Our study analyzed trends in mortality and disability-adjusted life years (DALYs) across different demographics and socio-economic indicators (SDI) from 1990 to 2021, forecasting future trends with the autoregressive integrated moving average (ARIMA) model, drawing on previous research (18, 19). The insights from this study aim to enhance global awareness of occupational hazards like particulate matter, gasses, and fumes, and assist in devising prevention and intervention strategies for coal workers worldwide.
2 Method
2.1 Study population
Our research utilized data from the 2021 Global Burden of Disease Study, analyzing 369 diseases and injuries and 87 risk factors across 204 countries from 1990 to 2021 (20).
To evaluate the effects of pneumoconiosis, we adopted methodologies from prior studies. Data gathered from various sources such as health surveys and verbal autopsies were refined to increase accuracy. This refined data was analyzed using the Cause of Death Ensemble model (CODEm), which yielded yearly, regional estimates of pneumoconiosis mortality by age and gender. We conducted a comparative risk assessment to identify major risk factors for pneumoconiosis and calculated population attributable fractions (PAF) to assess the impact of occupational hazards on pneumoconiosis rates. These PAFs were crucial for estimating pneumoconiosis-related mortality and disability-adjusted life years (DALYs) across various demographics and periods. DALYs were calculated by summing years lost due to premature death from lower respiratory infections (LRIs) and years lived with disability (YLDs), with adjustments based on disease severity. The Socio-Demographic Index (SDI), formulated from factors such as fertility under age 25 (TFU25), education level for individuals over 15 (EDU15+), and per capita income, classified 204 regions into five SDI categories.
The diagnosis of pneumoconiosis can be found in the https://www.healthdata.org/research-analysis/gbd.
2.2 Statistical analysis
Age-adjusted rates (AAR) were employed to standardize mortality and DALY statistics across diverse population demographics and age structures. Linear regression was conducted on the natural logs of these measures, modeled as y = α + βx + ε, where x represents the year, and y is the natural log of the rate. The estimated annual percentage change (EAPC) was calculated with the formula 100 * (e^β - 1), including a 95% confidence interval (CI). An increase in AAR was determined if both the EAPC and the lower 95% CI limit were positive, a decrease if both the EAPC and the upper 95% CI limit were negative, and stability if neither condition was met. The relationship between AAR and SDI was examined using Gaussian process regression with Loess smoothing, with the correlation assessed via Spearman rank correlation tests (Figure 1).
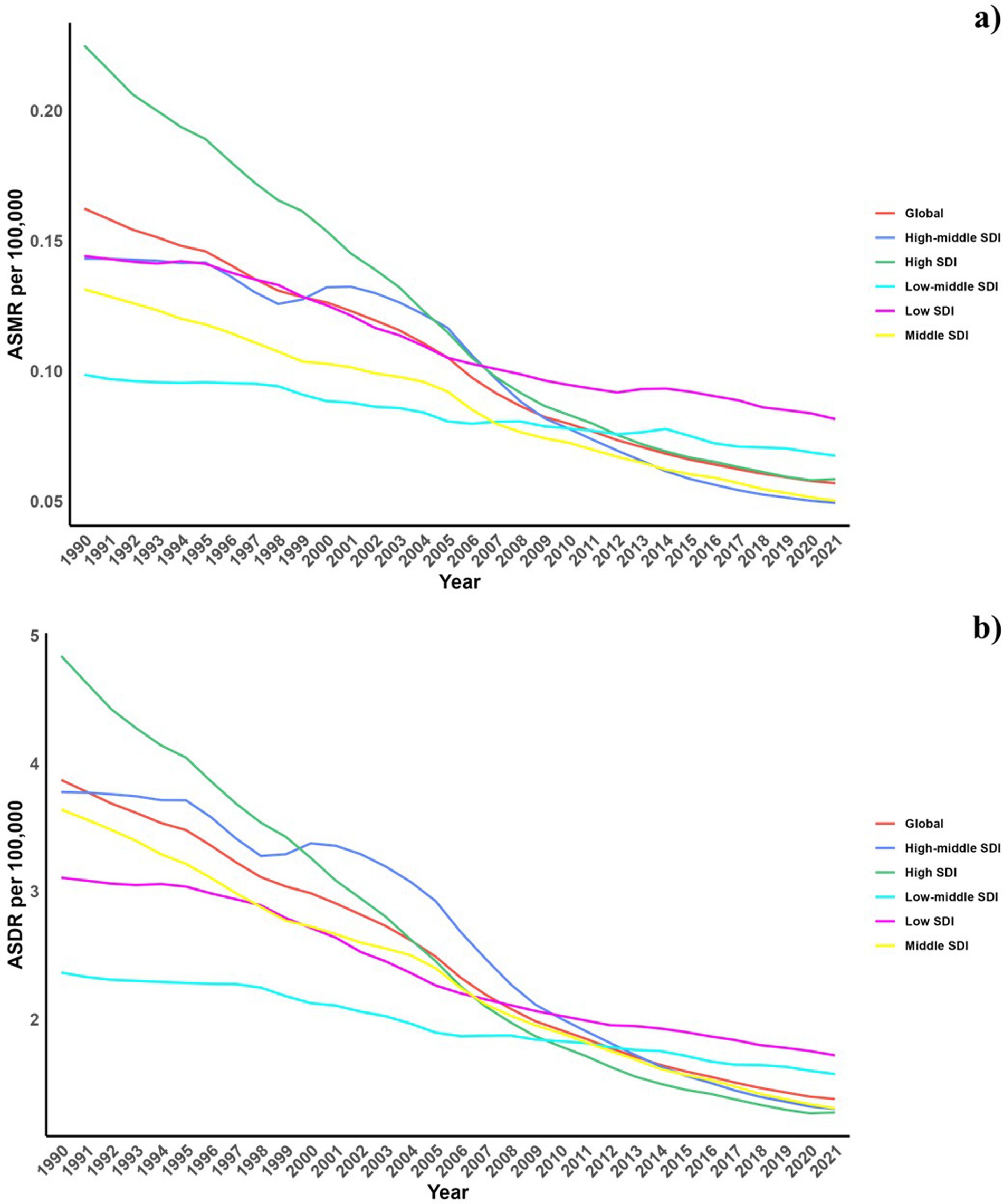
Figure 1. Temporal trends of ASMR and ASDR of Pneumoconiosis attributable to occupational particulate matter, gases, and fumes from1990 to 2021 in different SDI regions.
Furthermore, an ARIMA (Autoregressive Integrated Moving Average) model was used to study and forecast the impact of low vegetable consumption on pneumoconiosis trends globally, regionally, and nationally from 2020 to 2050. The configuration of the ARIMA model (p, d, q) includes ‘p’ as the number of lag observations in the autoregressive part, ‘q’ as the lag of forecast errors in the moving average component, and ‘d’ as the differencing needed for data stabilization. Model selection was informed by the Akaike Information Criterion (AIC) and the Bayesian Information Criterion (BIC).
All statistical analyses were performed using R. p < 0.05 was considered statistically significant (21–25).
3 Results
3.1 Spatiotemporal patterns of pneumoconiosis attributable to occupational particulate matter, gasses, and fumes
In 2021, exposure to occupational particulate matter, gasses, and fumes resulted in approximately 4,775 deaths and 117.80 thousand disability-adjusted life years (DALYs) due to pneumoconiosis. The age-standardized mortality rate (ASMR) for this condition was 0.0570, with a 95% uncertainty interval (UI) of 0.0487–0.0738, and the age-standardized DALY rate (ASDR) was 1.3771, with a 95% UI of 1.1831–1.7650 per 100,000 people. The data indicate a general decline in the burden of pneumoconiosis from occupational exposures over the last 30 years, as documented in Table 1 and Supplementary Table S1.
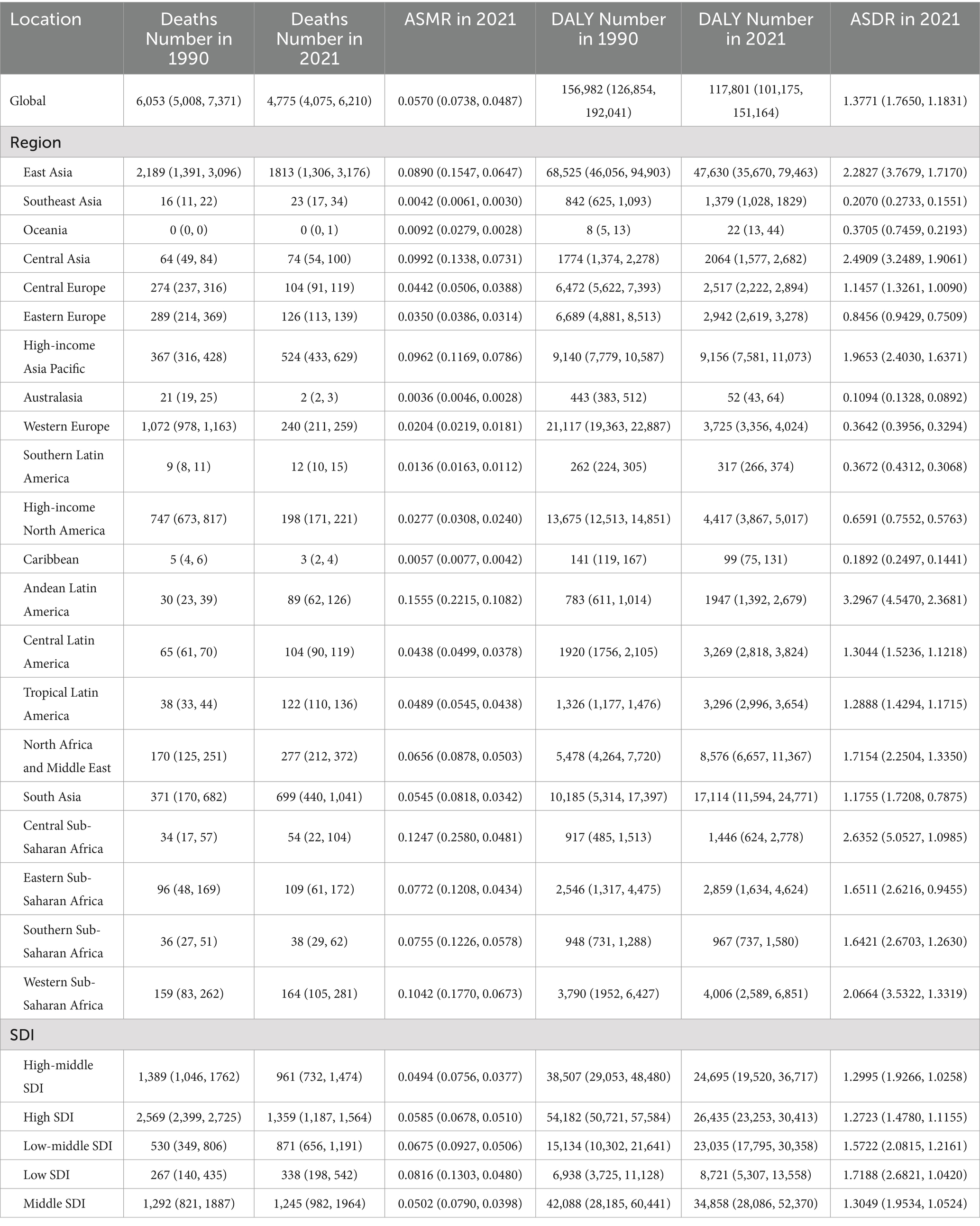
Table 1. Global and regional deaths and DALYs of pneumoconiosis attributable to occupational particulate matter, gasses, and fumes in 1990 and 2021 in 27 global regions.
Across different Socio-demographic Index (SDI) regions, there has been a reduction in pneumoconiosis burden. Notably, regions with high and high-middle SDI saw a significant drop, whereas the decline was more gradual in low and low-middle SDI areas.
Regionally, the highest number of pneumoconiosis deaths attributable to occupational exposures in 2021 was recorded in East Asia with 1813.2812 (95% UI: 3175.8013–1305.6708) and South Asia with 699.2660 (95% UI: 1041.0488–439.6702), while the lowest were in Australasia at 2.0019 (95% UI: 2.5319–1.5265) and the Caribbean at 3.0230 (95% UI: 4.0778–2.2664). Conversely, Andean Latin America, Central Sub-Saharan Africa, and Western Sub-Saharan Africa experienced the highest burdens in terms of ASMR and ASDR.
Nationally, China recorded the highest number of deaths from pneumoconiosis attributable to occupational exposures with 1690.4515 (95% UI: 3044.7846–1186.3571), followed by India with 604.2741 (95% UI: 896.0656–383.4427). Kazakhstan and Egypt reported the highest ASMRs, with Kazakhstan at 0.3288 (95% UI: 0.4798–0.2169) and Egypt at 0.3064 (95% UI: 0.4460–0.2094). Over the past thirty years, nations such as Australia, China, and those in Western Europe and North America have seen substantial reductions in ASMR, while the Russian Federation and Iran have witnessed increases (Table 1; Figure 2; Supplementary Table S1).
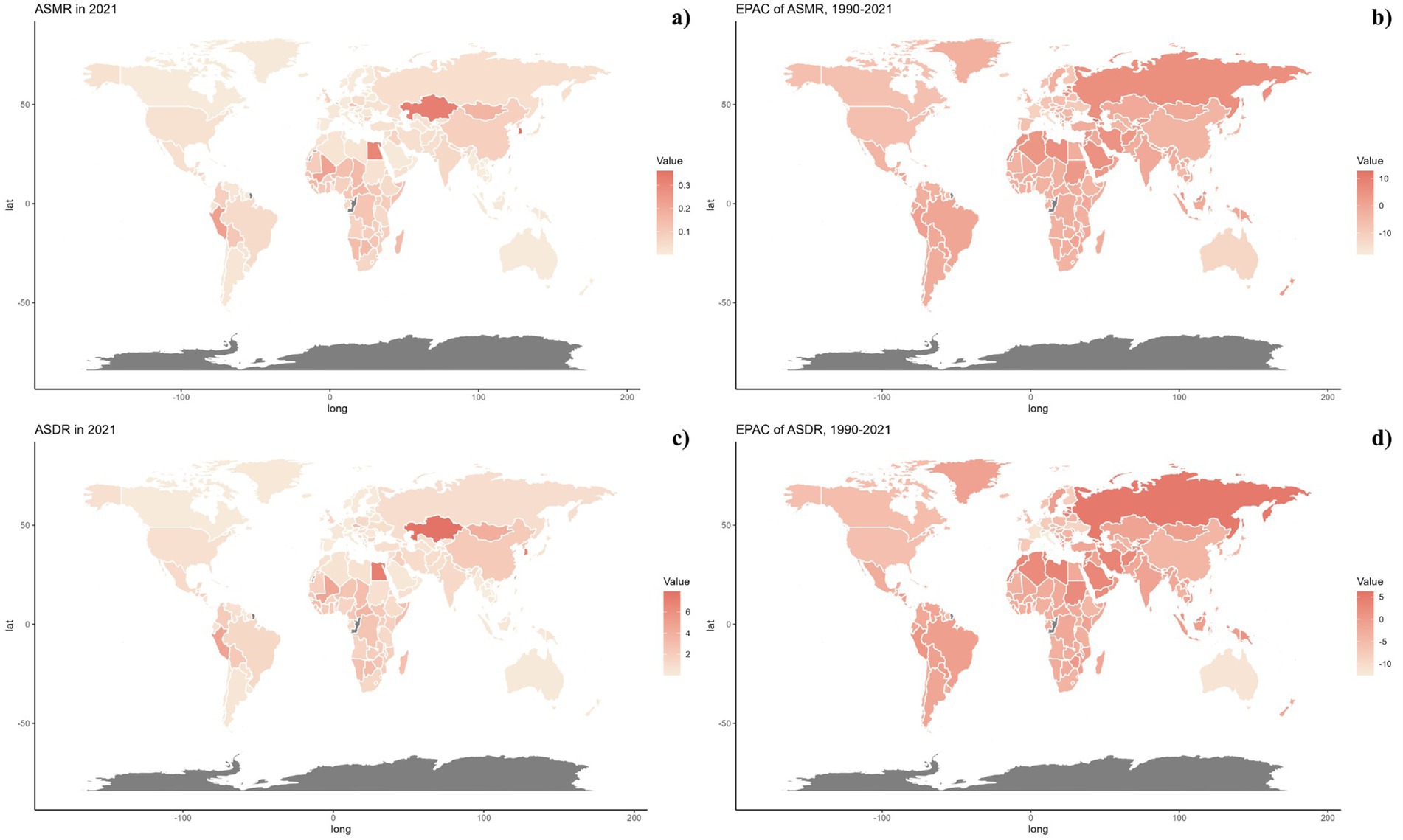
Figure 2. Global distribution of ASMR (A) and ASDR (C) of pneumoconiosis attributable to occupational particulate matter, gases, and fumes for both sexes in 2021 in 204 countries and territories. EAPC of ASMR (B) and ASDR (D) of pneumoconiosis attributable to occupational particulate matter, gases, and fumes from 1990 to 2021 in 204 countries and territories.
3.2 Age and gender pattern
Figure 3 illustrated the global mortality and DALY rates for pneumoconiosis across various ages in 2021, as well as trends since 1990. The analysis showed a J-shaped pattern with increasing mortality and DALY rates beginning in the early age groups and escalating sharply from age 60 onwards, reaching peaks in the 90–94 age group for males and 95+ for females. Across all ages, males consistently showed higher mortality and DALY rates compared to females. The estimated annual percentage change (EAPC) varied between −2 and −5, with a steady decrease beginning at age 40–44 for females and 65–69 for males. This gender disparity persisted across all Socio-demographic Index (SDI) regions as illustrated in Figure 4.
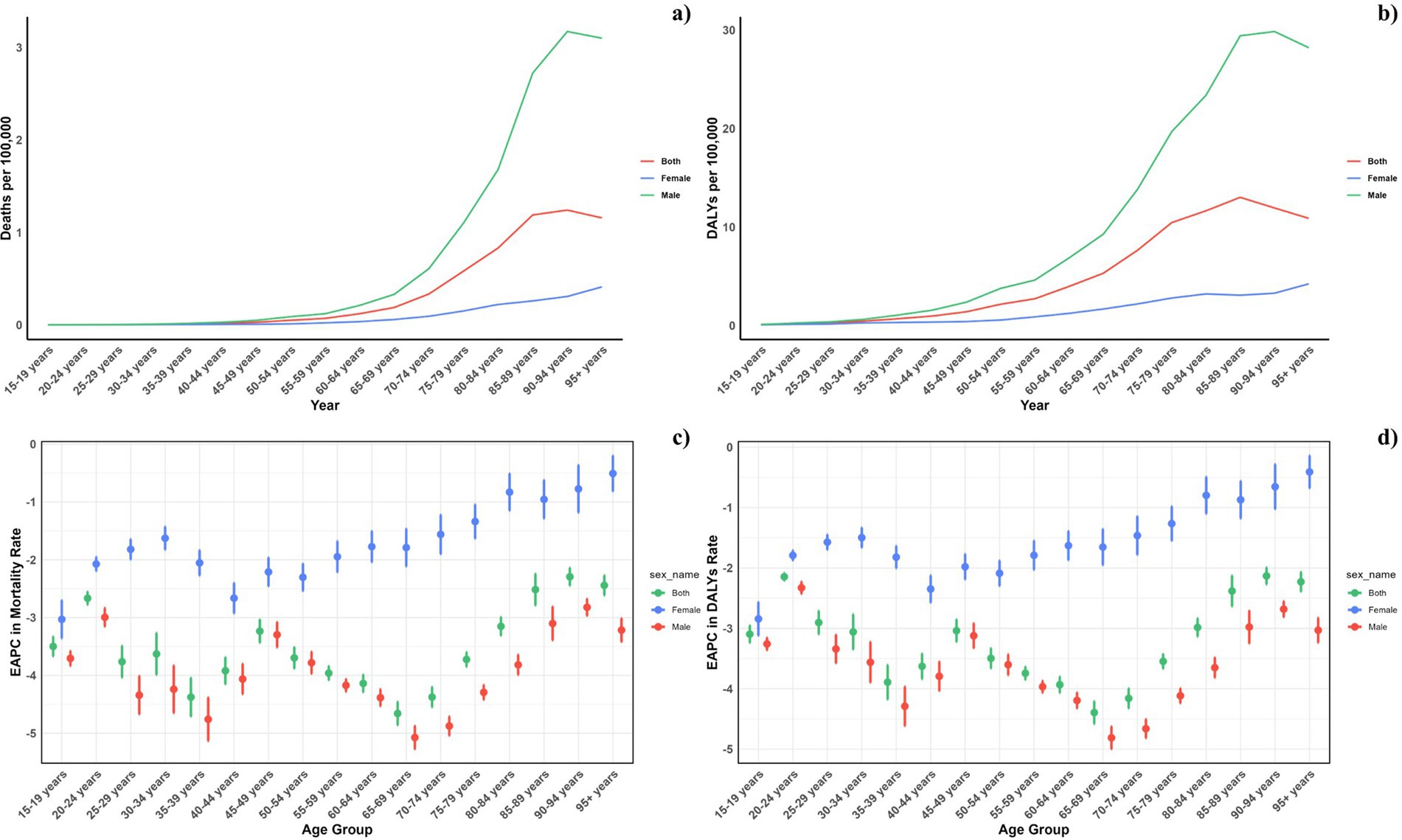
Figure 3. Age-specific rates of global deaths (A) and DALYs (B) of pneumoconiosis attributable to occupational particulate matter, gases, and fumes, by sex, in 2021 and the corresponding EAPC of global deaths (C) and DALYs (D) from 1990 to 2021.
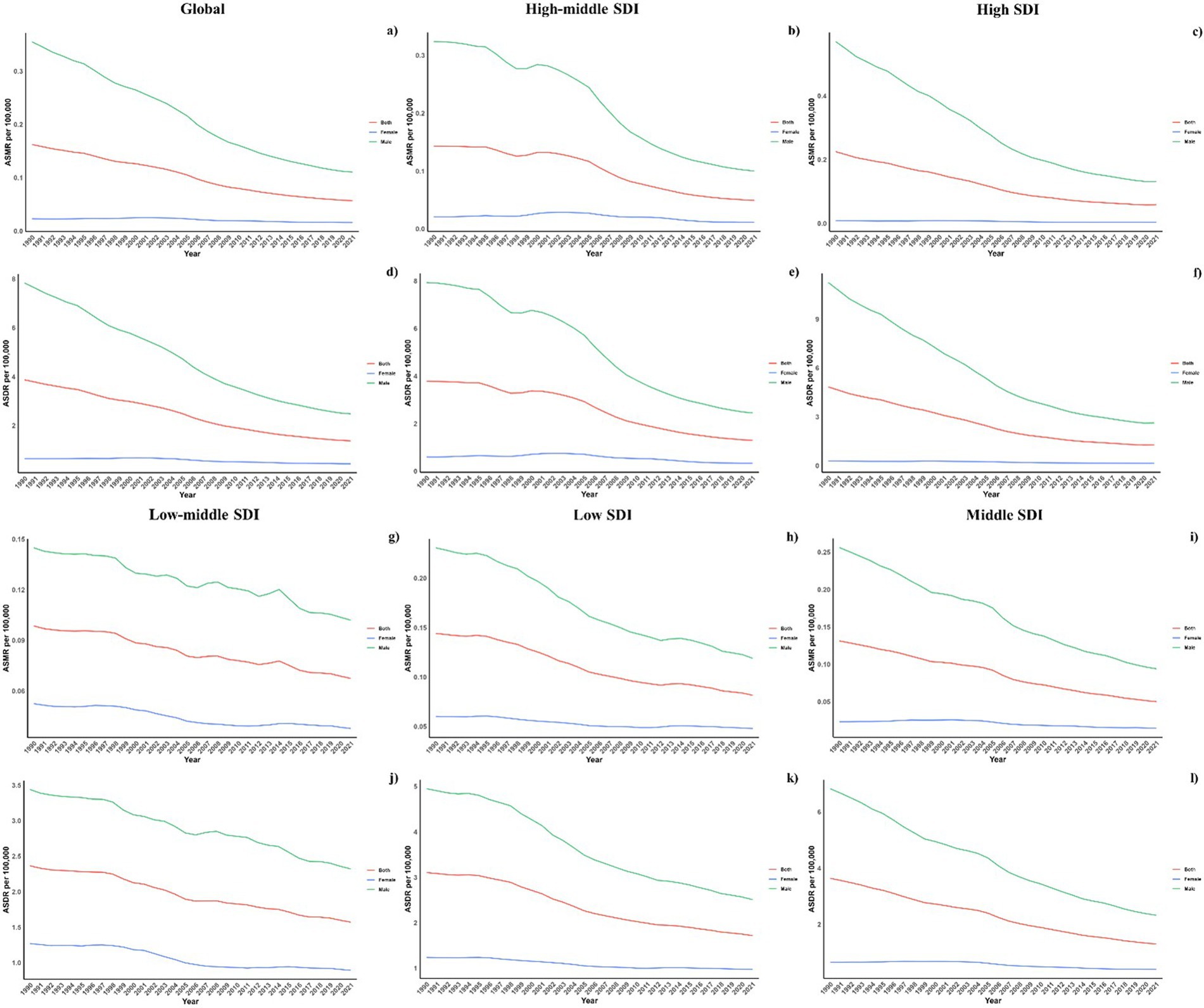
Figure 4. Sex disparity in pneumoconiosis attributable to occupational particulate matter, gases, and fumes across SDI Regions. Note: Global (a, d), high-middle SDI (b, e), high SDI (c, f), low-middle SDI (g, j), low SDI (h, k), middle SDI (i, l); ASMR (a, b, c, g, h, i), ASDR (d, e, f, j, k, l).
3.3 Association with the socio-demographic index
Our research evaluated the relationship between the ASDR and ASMR from occupational exposures and SDI values at regional and national levels from 1990 to 2021, as shown in Figure 5. We observed a non-linear relationship between ASDR and SDI (R = −0.23), where ASDR generally declined with increasing SDI but showed fluctuations within middle SDI ranges (0.4 to 0.8). Regions like Western Sub-Saharan Africa, Central Sub-Saharan Africa, Andean Latin America, Central Asia, East Asia, and High-income Asia Pacific reported higher than expected ASDR. Conversely, regions such as Eastern Sub-Saharan Africa, South Asia, Oceania, Tropical Latin America, Southeast Asia, the Caribbean, Southern Latin America, and Australasia had lower than forecasted ASDR. The observed trends in ASMR and ASDR aligned with SDI at regional levels. The 2021 data displayed an inverse relationship between observed and projected ASDR and ASMR at the national level, as depicted in Figure 5.
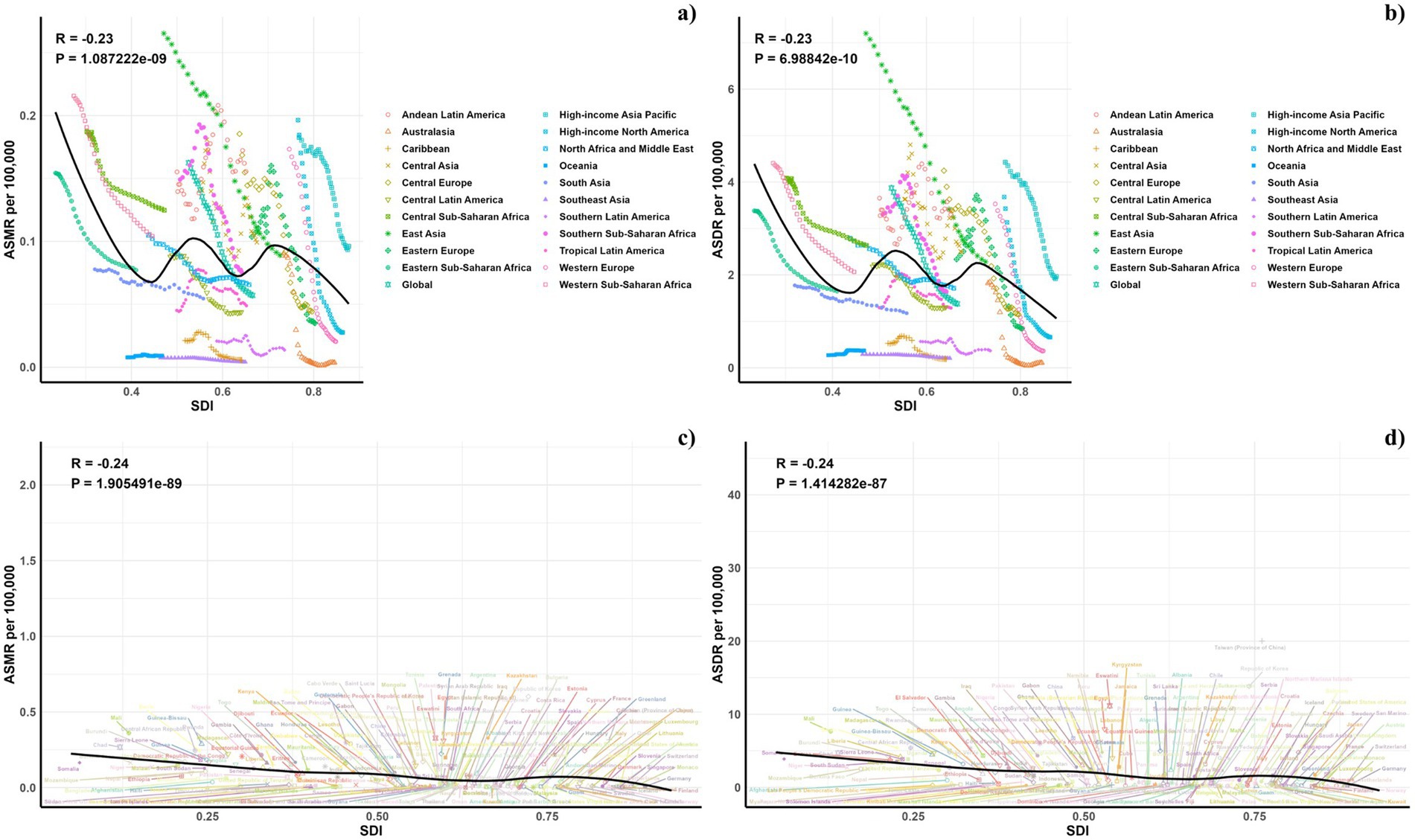
Figure 5. Correlations between ASMR (A,C) and ASDR (B,D) of pneumoconiosis attributable to occupational particulate matter, gases, and fumes and SDI at the regional level (A,B) and the national level (C,D).
3.4 Forecasts for the mortality, DALYs rate, ASMR, and ASDR of pneumoconiosis attributable to occupational particulate matter, gasses, and fumes in global (2022–2050)
Projections for mortality rates, DALY rates, ASMR, and ASDR related to pneumoconiosis from occupational particulate matter, gasses, and fumes were outlined in Figures 6–8. Forecasts indicate a significant increase in all four indicators in the high SDI regions, whereas a gradual decline is expected in the middle and low SDI regions. The high-middle and low-middle SDI regions are projected to maintain stable rates (Figure 6).
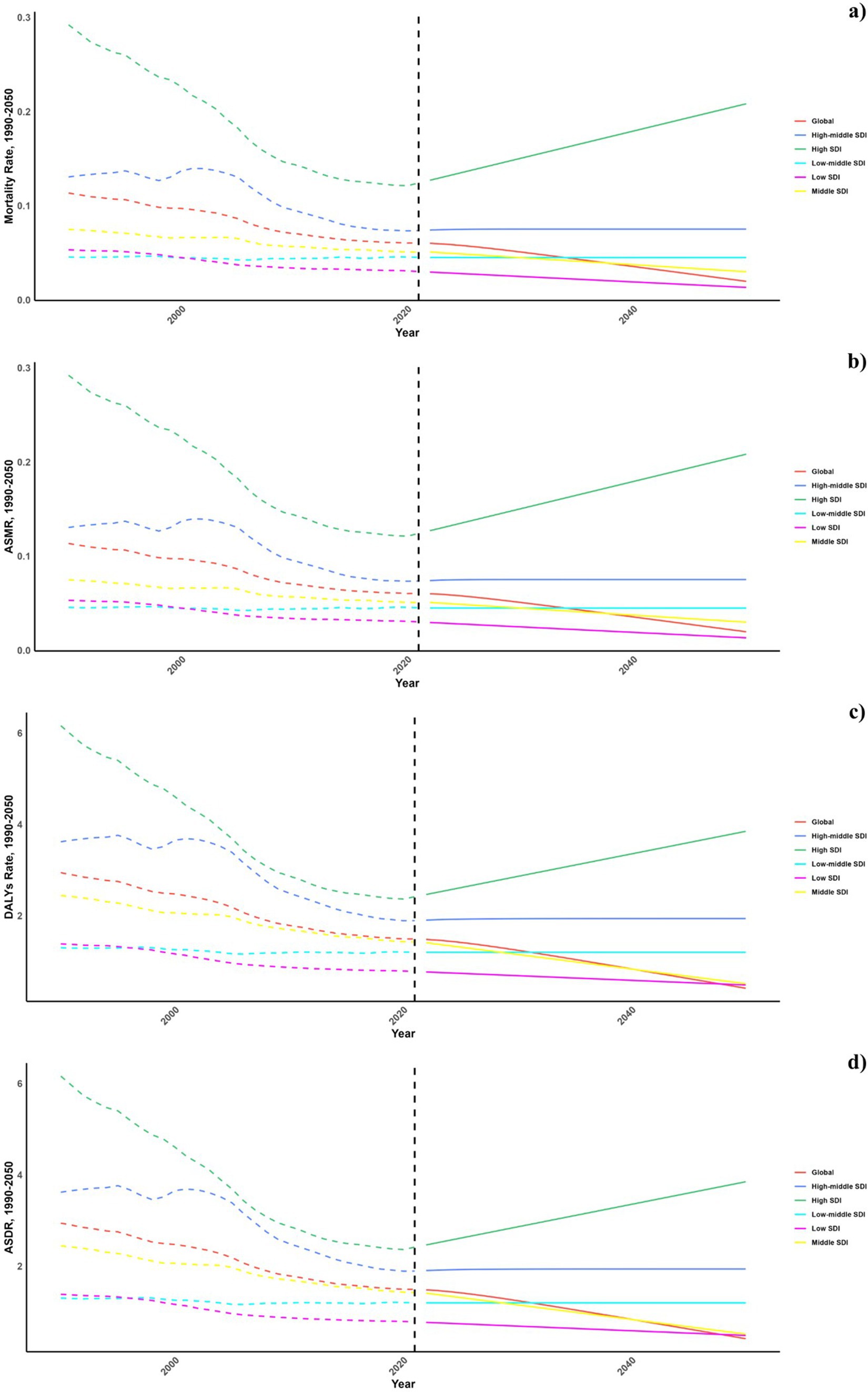
Figure 6. Estimated trends of mortality rate (A), DALYs Rate (B), ASMR (C), and ASDR (D), 1990-2050 at the regional level.
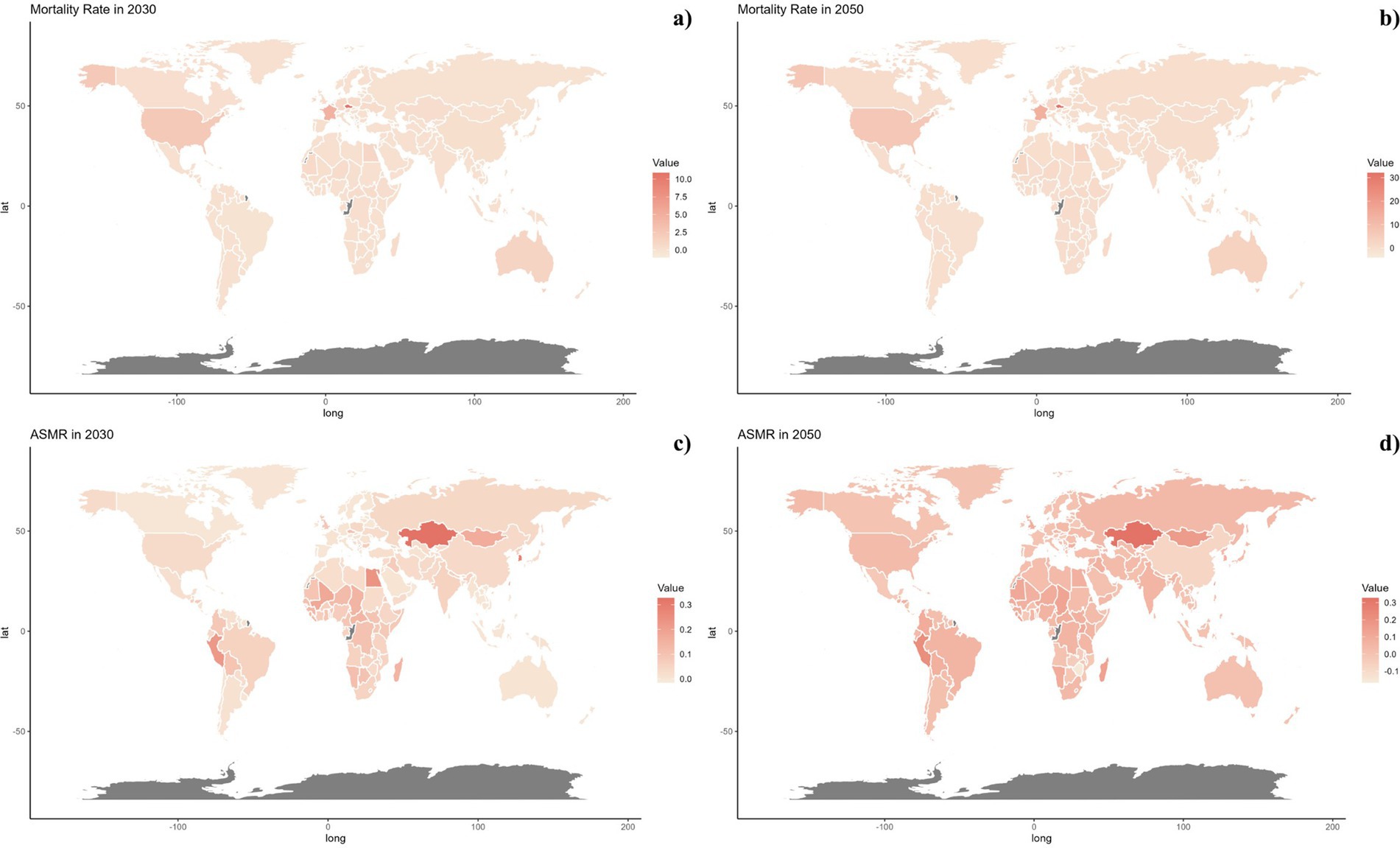
Figure 7. Estimated trends of mortality rate (A,B) and ASMR (C,D) in 2030 (A,C) and 2050 (B,D) at the national level.
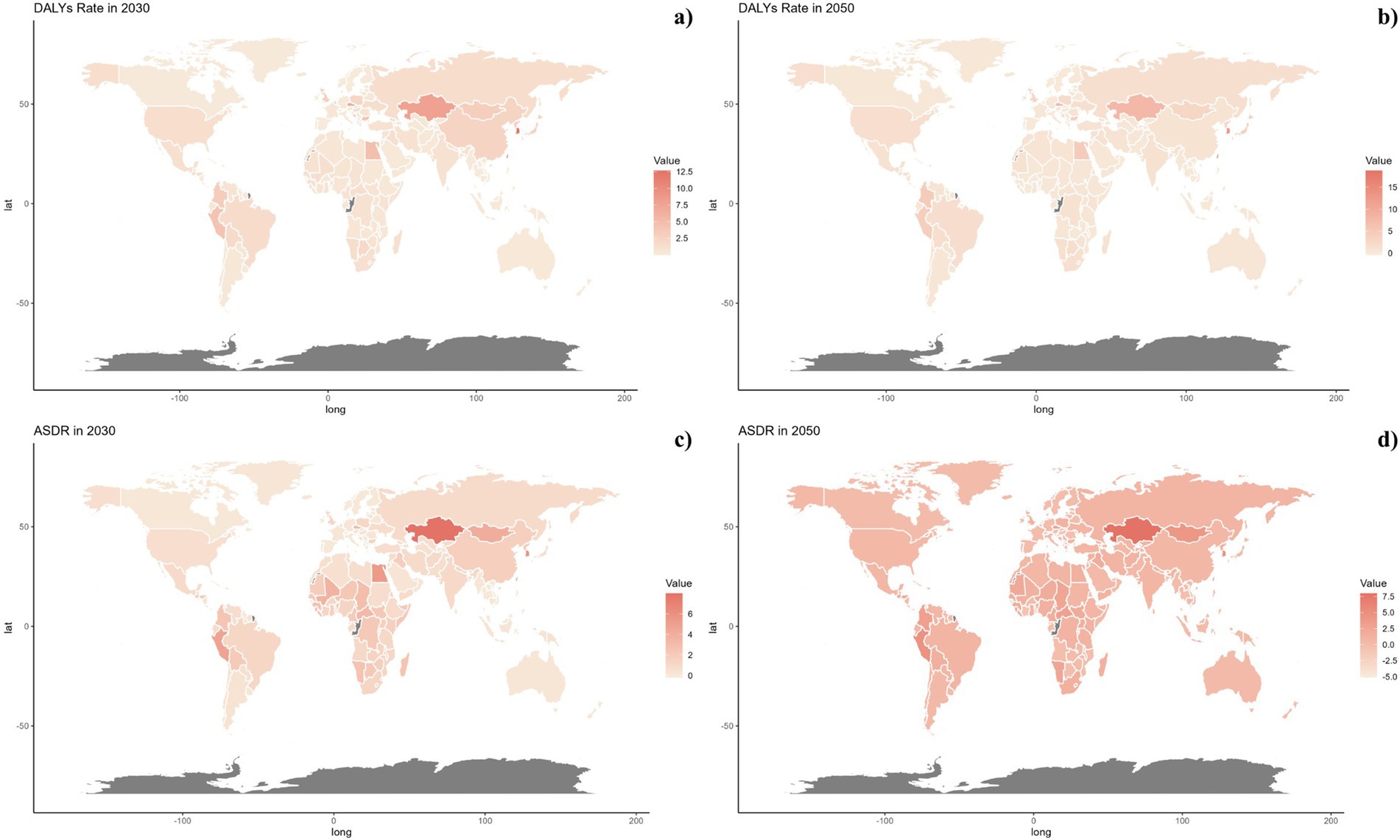
Figure 8. Estimated trends of DALYs Rate (A,B) and ASDR (C,D) in 2030 (A,C) and 2050 (B,D) at the national level.
Nationally, projected mortality rates from pneumoconiosis attributable to occupational exposures were notably higher in the Czech Republic, France, and America for both 2030 and 2050. Kazakhstan, Egypt, Mongolia, and Peru are expected to display higher levels of ASMR, DALY rates, and ASDR. It is also significant that ASMR and ASDR are trending upwards globally (Figures 7, 8).
4 Discussion
This study was carried out to assess the global burden of pneumoconiosis caused by occupational particulate matter, gasses, and fumes. It comes out that the global mortality rates, DALY rates, ASMR and ASDR of pneumoconiosis showed a declining trend from 1991 to 2021. From a demographic point of view, males and population aged over 60 suffered from pneumoconiosis more seriously. As projections suggested, mortality rates, DALY rates, ASMR, and ASDR would exhibit an increasing trend in the high SDI region while present a decreasing trend in the middle SDI region and low SDI region. In addition, projections also indicate that ASMR and ASDR would be on the rise worldwide. To the best of our knowledge, this study represented the first comprehensive assessment of the impact of pneumoconiosis resulting from occupational particulate matter, gasses, and fumes.
Occupational exposures to asbestos, silica and coal dust (defined as pure coal dust and dust from coal mining) were already recognized as risk factors for pneumoconiosis. As the Global Burden of Disease Study 2016 showed, asbestosis (as a separate outcome from coal workers’ pneumoconiosis and other pneumoconiosis) and silicosis were entirely attributed to occupational exposure to asbestos and silica, respectively, and the burden of coal workers’ pneumoconiosis and other pneumoconiosis was 100% attributable to the risk factors of exposure to occupational particulate matter, gasses, and fumes (2). A cross-sectional study for migrant workers with pneumoconiosis indicated that workers who smoked in the workplace and were exposed to dust were more likely to develop pneumoconiosis (26). Besides, another cohort study subjected on workers exposed to dusts in an iron mine suggested that cumulative exposure dose has an obvious dose-effect relationship with pneumoconiosis incidence (27). Moreover, chronic exposure to high concentrations of fumes during aluminum arc welding could lead to severe pneumoconiosis (28). Besides, benchtop fabrication from quartz conglomerate is also a potentially dangerous occupation. Recent research has highlighted new forms of multiorgan accelerated silicosis could be misdiagnosed as sarcoidosis in workers exposed to quartz conglomerate dust due to atypical clinical presentation (29). Therefore, general practitioners and physicians should have comprehensive understanding of various occupational hazard, especially newly described ones. And accurate occupational history is critical in avoiding misdiagnosis. To sum up, these findings suggested that exposure to particulate matter, gasses, and fumes in the workplace can have significant and lasting effects on lung health, potentially contributing to the onset of pneumoconiosis.
In regard to mechanisms of the pathogenesis of pneumoconiosis, there are already enough studies. Inhaled particle matters were often scavenged by alveolar macrophages, which were activated to produce ROS and RNS, overwhelming the lung’s antioxidant capabilities, resulting in inflammation, which caused disease (30). In response to inhaled PM, airway and alveolar epithelial cells, macrophages produced a variety of cytokines and growth factors, including IL-1β, IL-6, TNF-α, macrophage inflammatory proteins (MIP1, MIP2) etc., thus, recruiting other immune cells to the lungs, which produced inflammatory mediators and cell damage (31). Furthermore, some studies have found that accelerated biological aging, as indicated by increased DNA methylation age (DNAmAge) and shortened telomere length (TL), could play a role in patients with lung diseases (32). Additionally, Another research by Plaat et al. implied that occupational exposures might lead to differential methylation of genes involved in regulating gene expression, which could result in other adverse health consequences (32).
In 2017, occupational particulate matter, gasses, and fumes were responsible for 7,000 deaths and 178 thousand DALYs of pneumoconiosis globally, which showed an increase compared to 2007, probably due to population growth in the last decade (33). While age-standardized rates (ASRs) of deaths and DALYs presented a declining trend (33), which might be due to the fact that the prevention policy of pneumoconiosis has been established during these decades. To name a few, in 2016, the Occupational Safety and Health Administration (OSHA) revised standards for occupational exposure to respirable crystalline silica (RCS), limiting permissible exposure to 50 μg/m3 and imposing stricter limits on certain industries, which was estimated to reduce health risks significantly. Furthermore, a handful of nations worldwide, namely China, the United States, the United Kingdom, New Zealand, Germany, and Finland, have established robust data collection systems relating to occupational disease, providing more comprehensive data of pneumoconiosis for efficient prevention measures (34). Besides, advancements in dust control technology substantially reduced cumulative dust exposure dose of workers, such as utilizing wet operations to diminish the production and transmission of industrial dust (35), creating a trapezoidal protection area by air curtain to separate the dust-producing surface from the operator (36), etc.
According to the results of our research, ASDR and SDI are negatively correlated roughly. SDI is a composite measure of income per capita, years of education, and total fertility rate. Therefore, this could be due to the fact that areas with low SDI, such as India and Brazil, would likely stem from the poor working conditions, lack of awareness, and underdeveloped healthcare systems prevalent in these regions (37–38), while areas with high SDI possibly had highly developed healthcare systems, high standards of workplace safety procedures, and highly mechanized mining practices that reduced workers’ exposure to particle matters (39). Moreover, we also found that the ASMR and ASDR of pneumoconiosis attributable to occupational particulate matter, gasses, and fumes rose with age in both sexes. This can be attributed to the fact that pneumoconiosis typically had a lengthy latency period, which means that it can take several years or even decades for the disease to develop following exposure to those risk factors (40). The period of exposure to particulate matter, gasses, and fumes that can result in pneumoconiosis may vary based on a range of factors, including the frequency, duration, and intensity of exposure, as well as individual factors such as genetics and overall health. Further research is needed to fully understand the specific mechanisms involved.
In our prediction model, ASMR and ASDR exhibited an increasing trend worldwide, indicating the global burden of pneumoconiosis caused by occupational particulate matter, gasses, and fumes may escalate in the coming decades. However, the International Labor Organization and the World Health Organization were seeking to eradicate this disease by 2030 (41). Therefore, there are still great challenges on the prevention and treatment work of pneumoconiosis. For instance, some countries, like India, had imperfect laws and regulations about the prevention of pneumoconiosis, and other countries, such as China, despite of relevant laws and regulations, there were also problems of lax enforcement of laws and poor supervision (42). Secondly, due to inadequate education and training, some workers lacked basic knowledge of pneumoconiosis and its prevention and control measures (43). Thirdly, many areas lacked regular health checks and early screening measures for pneumoconiosis, and early cases were not detected and treated in a timely manner (43–44). Fourthly, safety measures in the workplace were inadequate. The problem of the shortage of protective equipment and poor ventilation still existed (44–46). As a consequence, policymakers should adopt multiple approaches, including legislation, intensifying supervision, supporting safe work practices, increasing awareness, and offering assistance to affected persons, etc.
Our research confronts several significant constraints. Initially, there is a paucity of primary data from less developed regions, particularly in Sub-Saharan Africa, where evaluations principally rely on mathematical modeling, resulting in extensive variability and uncertainty. Secondly, the statistics regarding pneumoconiosis caused by occupational particulate matter, gasses, and fumes are subject to inconsistencies and biases due to the reliance on self-reports as a data source. Thirdly, detailed quantitative data regarding occupational exposure of workers or occupational categories to particulate matter, gasses, and smoke are lacking.
5 Conclusion
This study conducted a detailed analysis of the global impact of pneumoconiosis caused by occupational exposure to particulate matter, gasses, and fumes from 1990 to 2021, showing a notable decline over this period. Men and those over 60 years old bore a higher burden from these exposures. Our forecasts indicate that low to middle SDI regions might experience reductions in mortality rates, whereas high SDI regions could see an uptick in standardized mortality rates. At the country level, projections pointed to particularly high mortality rates in the Czech Republic, France, and the United States for both 2030 and 2050. Additionally, Kazakhstan, Egypt, Mongolia, and Peru are expected to exhibit elevated ASMR, DALY rates, and ASDR.
These findings underscore the critical need for policymakers to craft and enhance specific preventive measures that safeguard and guide workers exposed to hazardous substances for long periods, aiming to reduce the incidence of pneumoconiosis in targeted groups effectively.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
MQ: Data curation, Formal analysis, Investigation, Writing – original draft. RX: Formal analysis, Writing – original draft. WY: Data curation, Investigation, Writing – original draft. XW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. YK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1494942/full#supplementary-material
References
1. Qi, XM, Luo, Y, Song, MY, Liu, Y, Shu, T, Liu, Y, et al. Pneumoconiosis: current status and future prospects. Chin Med J. (2021) 134:898–907. doi: 10.1097/CM9.0000000000001461
2. GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioral, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390:1345–422. doi: 10.1016/S0140-6736(17)32366-8
3. Su, X, Kong, X, Yu, X, and Zhang, X. Incidence and influencing factors of occupational pneumoconiosis: a systematic review and meta-analysis. BMJ Open. (2023) 13:e065114. doi: 10.1136/bmjopen-2022-065114
4. Grobbelaar, JP, and Bateman, ED. Hut lung: a domestically acquired pneumoconiosis of mixed aetiology in rural women. Thorax. (1991) 46:334–40. doi: 10.1136/thx.46.5.334
5. Mukhopadhyay, S, Gujral, M, Abraham, JL, Scalzetti, EM, and Iannuzzi, MC. A case of hut lung: scanning electron microscopy with energy dispersive x-ray spectroscopy analysis of a domestically acquired form of pneumoconiosis. Chest. (2013) 144:323–7. doi: 10.1378/chest.12-2085
6. Han, L, Han, R, Ji, X, Wang, T, Yang, J, Yuan, J, et al. Prevalence characteristics of coal Workers' pneumoconiosis (CWP) in a state-owned mine in eastern China. Int J Environ Res Public Health. (2015) 12:7856–67. doi: 10.3390/ijerph120707856
7. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/s0140-6736(18)32279-7
8. Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2015) 386:743–800. doi: 10.1016/s0140-6736(15)60692-4
9. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/s0140-6736(16)31678-6
10. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390:1211–59. doi: 10.1016/S0140-6736(17)32154-2
11. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet. (2015) 385:117–71. doi: 10.1016/S0140-6736(14)61682-2
12. GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1459–544. doi: 10.1016/s0140-6736(16)31012-1
13. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2017) 390:1151–210. doi: 10.1016/s0140-6736(17)32152-9
14. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
15. GBD 2019 Chronic Respiratory Diseases Collaborators. Global burden of chronic respiratory diseases and risk factors, 1990-2019: an update from the global burden of disease study 2019. EClinicalMedicine. (2023) 59:101936. doi: 10.1016/j.eclinm.2023.101936
16. Schlünssen, V, Mandrioli, D, Pega, F, Momen, NC, Ádám, B, Chen, W, et al. The prevalences and levels of occupational exposure to dusts and/or fibres (silica, asbestos and coal): a systematic review and meta-analysis from the WHO/ILO joint estimates of the work-related burden of disease and injury. Environ Int. (2023) 178:107980. doi: 10.1016/j.envint.2023.107980
17. Vanka, KS, Shukla, S, Gomez, HM, James, C, Palanisami, T, Williams, K, et al. Understanding the pathogenesis of occupational coal and silica dust-associated lung disease. Eur Respir Rev. (2022) 31:210250. doi: 10.1183/16000617.0250-2021
18. Wafa, HA, Marshall, I, Wolfe, CDA, Xie, W, Johnson, CO, Veltkamp, R, et al. Burden of intracerebral haemorrhage in Europe: forecasting incidence and mortality between 2019 and 2050. The Lancet Regional Health Europe. (2024) 38:100842:100842. doi: 10.1016/j.lanepe.2024.100842
19. Gong, Y, Jiang, Q, Zhai, M, Tang, T, and Liu, S. Thyroid cancer trends in China and its comparative analysis with G20 countries: projections for 2020-2040. J Glob Health. (2024) 14:04131. doi: 10.7189/jogh.14.04131
20. Mao, Q, Zhu, X, Zhang, X, and Kong, Y. Effect of air pollution on the global burden of cardiovascular diseases and forecasting future trends of the related metrics: a systematic analysis from the global burden of disease study 2021. Front Med. (2024) 11:1472996. doi: 10.3389/fmed.2024.1472996
21. Mao, Q, Zhu, X, Zhang, X, and Kong, Y. Triglyceride-glucose index and its combination with obesity indicators mediating the association between 2-hydroxyfluorene and the prevalence of cardiovascular disease: evidence from the NHANES (2005-2018). Ecotoxicol Environ Saf. (2024) 287:117283. doi: 10.1016/j.ecoenv.2024.117283
22. Mao, Q, Zhu, X, and Kong, Y. Sleep duration mediates the association between heavy metals and the prevalence of depression: an integrated approach from the NHANES (2005-2020). Front Psych. (2024) 15:1455896. doi: 10.3389/fpsyt.2024.1455896
23. Kong, Y, Zhu, X, Yang, Y, Xu, H, Ma, L, and Zuo, Y. Knowledge, attitudes, practice, and public health education demand regarding PARI prevention: a cross-sectional study among Chinese undergraduates. Front Public Health. (2024) 12:1387789. doi: 10.3389/fpubh.2024.1387789
24. Kong, Y, Xu, H, Li, C, Yang, Y, Zhu, X, and Zuo, Y. Construction of PARI public health education programs for Chinese undergraduates: a Delphi study. Front Public Health. (2024) 12:1390011. doi: 10.3389/fpubh.2024.1390011
25. Cheng, Z, Kong, Y, Yang, W, Xu, H, Tang, D, and Zuo, Y. Association between serum copper and blood glucose: a mediation analysis of inflammation indicators in the NHANES (2011-2016). Front Public Health. (2024) 12:1401347. doi: 10.3389/fpubh.2024.1401347
26. Chen, J, Ye, S, Mao, L, Xie, W, Nie, H, and Su, M. Characteristics and factors associated with morbidity of migrant workers with pneumoconiosis: a cross-sectional study. BMJ Open. (2022) 12:e064596. doi: 10.1136/bmjopen-2022-064596
27. Guan, HY, Zhang, H, Su, LP, Liu, YW, Weng, SF, and Chen, WH. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. Chinese J Industrial Hyg Occup Dis. (2012) 30:36–40.
28. Hull, MJ, and Abraham, JL. Aluminum welding fume-induced pneumoconiosis. Hum Pathol. (2002) 33:819–25. doi: 10.1053/hupa.2002.125382
29. Guarnieri, G, Bizzotto, R, Gottardo, O, Velo, E, Cassaro, M, Vio, S, et al. Multiorgan accelerated silicosis misdiagnosed as sarcoidosis in two workers exposed to quartz conglomerate dust. Occup Environ Med. (2019) 76:178–80. doi: 10.1136/oemed-2018-105462
30. Pinho, RA, Bonatto, F, Andrades, M, Frota, MLC Jr, Ritter, C, Klamt, F, et al. Lung oxidative response after acute coal dust exposure. Environ Res. (2004) 96:290–7. doi: 10.1016/j.envres.2003.10.006
31. Beckett, EL, Stevens, RL, Jarnicki, AG, Kim, RY, Hanish, I, Hansbro, NG, et al. A new short-term mouse model of chronic obstructive pulmonary disease identifies a role for mast cell tryptase in pathogenesis. J Allergy Clin Immunol. (2013) 131:752–762.e7. doi: 10.1016/j.jaci.2012.11.053
32. Campisi, M, Liviero, F, Maestrelli, P, Guarnieri, G, and Pavanello, S. DNA methylation-based age prediction and telomere length reveal an accelerated aging in induced sputum cells compared to blood leukocytes: a pilot study in COPD patients. Front Med. (2021) 8:690312. doi: 10.3389/fmed.2021.690312
33. van der Plaat, DA, Vonk, JM, Terzikhan, N, de Jong, K, de Vries, M, La Bastide-van Gemert, S, et al. Occupational exposure to gases/fumes and mineral dust affect DNA methylation levels of genes regulating expression. Hum Mol Genet. (2019) 28:2477–85. doi: 10.1093/hmg/ddz067
34. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1923–94. doi: 10.1016/S0140-6736(18)32225-6
35. International Labour Organization. National system for recording and notification of occupational diseases: Practical guide. Geneva: International Labour Office (2013).
36. Reed, WR, Shahan, M, Ross, G, and Blackwell, D. Peters S field comparison of a roof bolter dry dust collection system with an original designed wet collection system for dust control. Min Metall Explor. (2020) 37:1885–98. doi: 10.1007/s42461-020-00290-x
37. Nie, W, Zhang, X, Peng, HT, Chen, DW, Du, T, Yang, B, et al. Research on air curtain dust control technology for environmental protection at fully mechanized working faces. Environ Sci Pollut Res Int. (2022) 29:43371–84. doi: 10.1007/s11356-022-18775-1
38. Govindagoudar, MB, Singh, PK, Chaudhry, D, Chaudhary, R, Sachdeva, A, Dhankhar, S, et al. Burden of silicosis among stone crushing workers in India. Occup Med (Lond). (2022) 72:366–71. doi: 10.1093/occmed/kqab146
39. Souza, TP, van Tongeren, M, and Monteiro, I. Respiratory health and silicosis in artisanal mine workers in southern Brazil. Am J Ind Med. (2021) 64:511–8. doi: 10.1002/ajim.23242
40. Morgan, J. Black lung is still a threat [published correction appears in Lancet]. Lancet Respir Med. (2018) 6:745–6. doi: 10.1016/S2213-2600(18)30283-2
41. Ross, MH, and Murray, J. Occupational respiratory disease in mining. Occup Med (Lond). (2004) 54:304–10. doi: 10.1093/occmed/kqh073
42. Pingle, S. Occupational safety and health in India: now and the future. Ind Health. (2012) 50:167–71. doi: 10.2486/indhealth.ms1366
43. Wang, H, Ye, Q, Zhang, H, Sun, X, and Li, T. Prevention and treatment of pneumoconiosis in the context of healthy China 2030. China CDC Wkly. (2023) 5:927–32. doi: 10.46234/ccdcw2023.162
44. Rupani, MP. Challenges and opportunities for silicosis prevention and control: need for a national health program on silicosis in India. J Occup Med Toxicol. (2023) 18:11. doi: 10.1186/s12995-023-00379-1
45. Li, T, Yang, X, Xu, H, and Liu, H. Early identification, accurate diagnosis, and treatment of silicosis. Can Respir J. (2022) 2022:1–6. doi: 10.1155/2022/3769134
46. Moyo, D, Kavenga, F, Ncube, RT, Macheri, FP, Mando, TC, Moyo, F, et al. Knowledge, attitudes, and practices of artisanal and small-scale miners regarding tuberculosis, human immunodeficiency virus, and silicosis in Zimbabwe. Int J Environ Res Public Health. (2023) 20:7116. doi: 10.3390/ijerph20237116
Keywords: pneumoconiosis, occupational risk, mortality forecasting, epidemiology, disease burden
Citation: Qingsong M, Xiao R, Yang W, Wang X and Kong Y-z (2025) Global burden of pneumoconiosis attributable to occupational particulate matter, gasses, and fumes from 1990~2021 and forecasting the future trends: a population-based study. Front. Public Health. 12:1494942. doi: 10.3389/fpubh.2024.1494942
Edited by:
Sheikh M. Alif, Federation University Australia, AustraliaReviewed by:
Filippo Liviero, University of Padua, ItalyXin Liu, Jiangsu Provincial Center for Disease Control and Prevention, China
Copyright © 2025 Qingsong, Xiao, Yang, Wang and Kong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinyi Wang, ODMwMTIyMDIwN0Bjc3UuZWR1LmNu; Yu-zhe Kong, Y3N1eXV6aGVrb25nQGZveG1haWwuY29t
 Mao Qingsong
Mao Qingsong Ruijie Xiao2
Ruijie Xiao2 Wenqi Yang
Wenqi Yang Xinyi Wang
Xinyi Wang Yu-zhe Kong
Yu-zhe Kong