- 1Department of Rheumatology and Immunology, Jiujiang City Key Laboratory of Cell Therapy, JiuJiang NO.1 People’s Hospital, Jiujiang, China
- 2Department of Endocrinology, Jiujiang City Key Laboratory of Cell Therapy, JiuJiang NO.1 People’s Hospital, Jiujiang, China
Background: This study aims to assess the knowledge, attitudes, and practices (KAP) regarding dietary management among patients with rheumatoid arthritis (RA).
Methods: A cross-sectional survey was conducted at JiuJiang NO.1 People’s Hospital from November 2023 to May 2024. Data were gathered using structured questionnaires that solicited demographic information and measured KAP scores related to dietary management in RA patients.
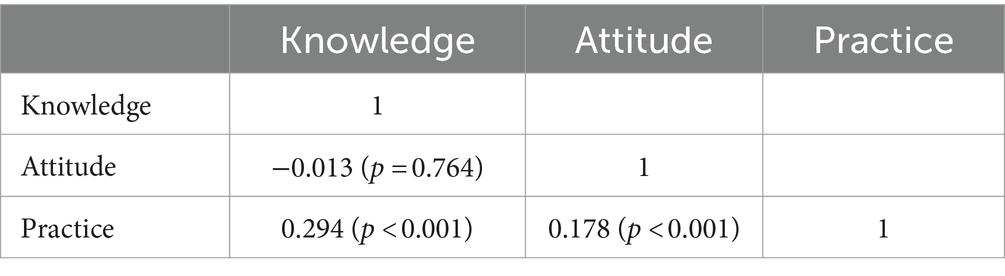
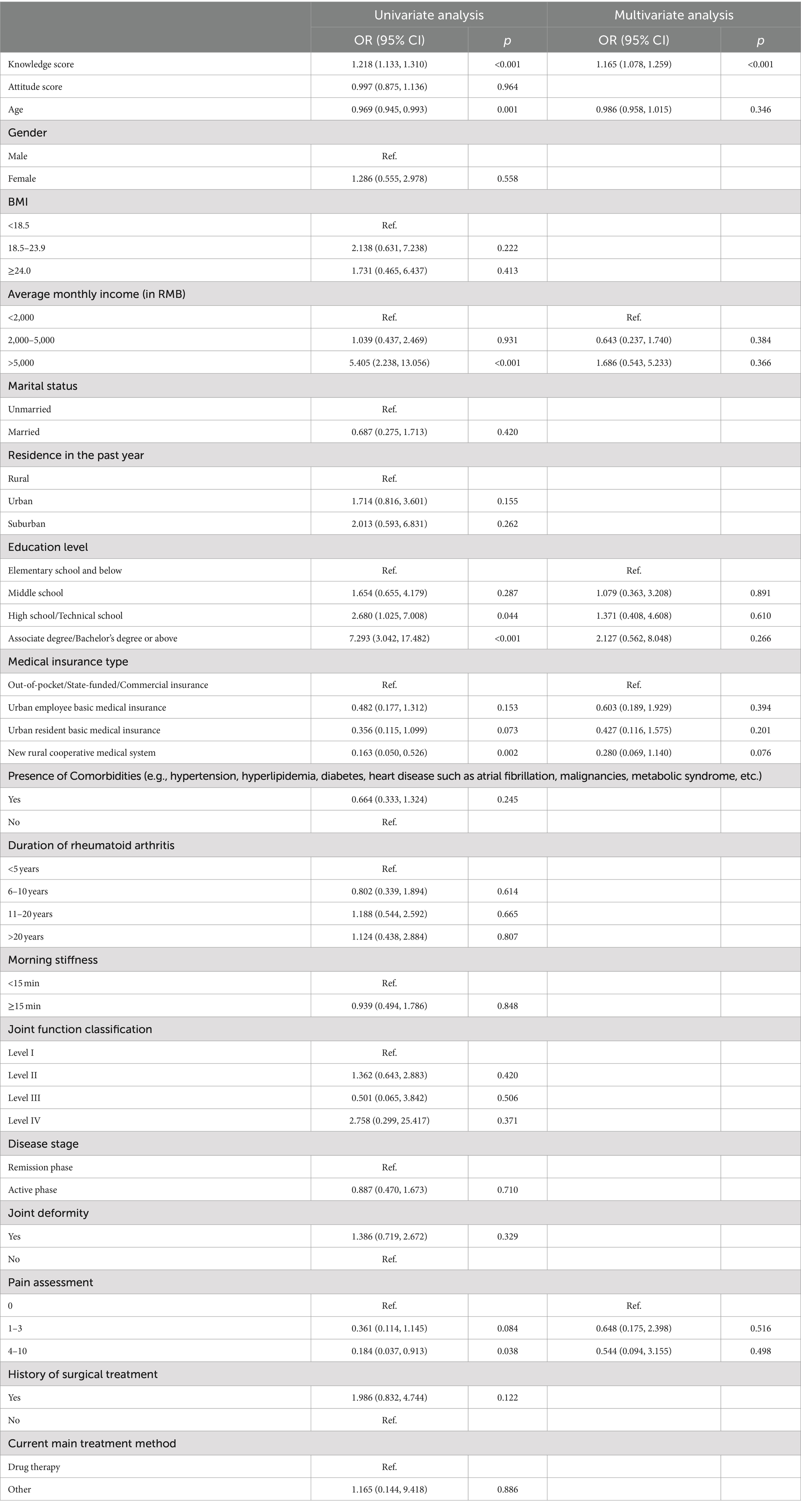
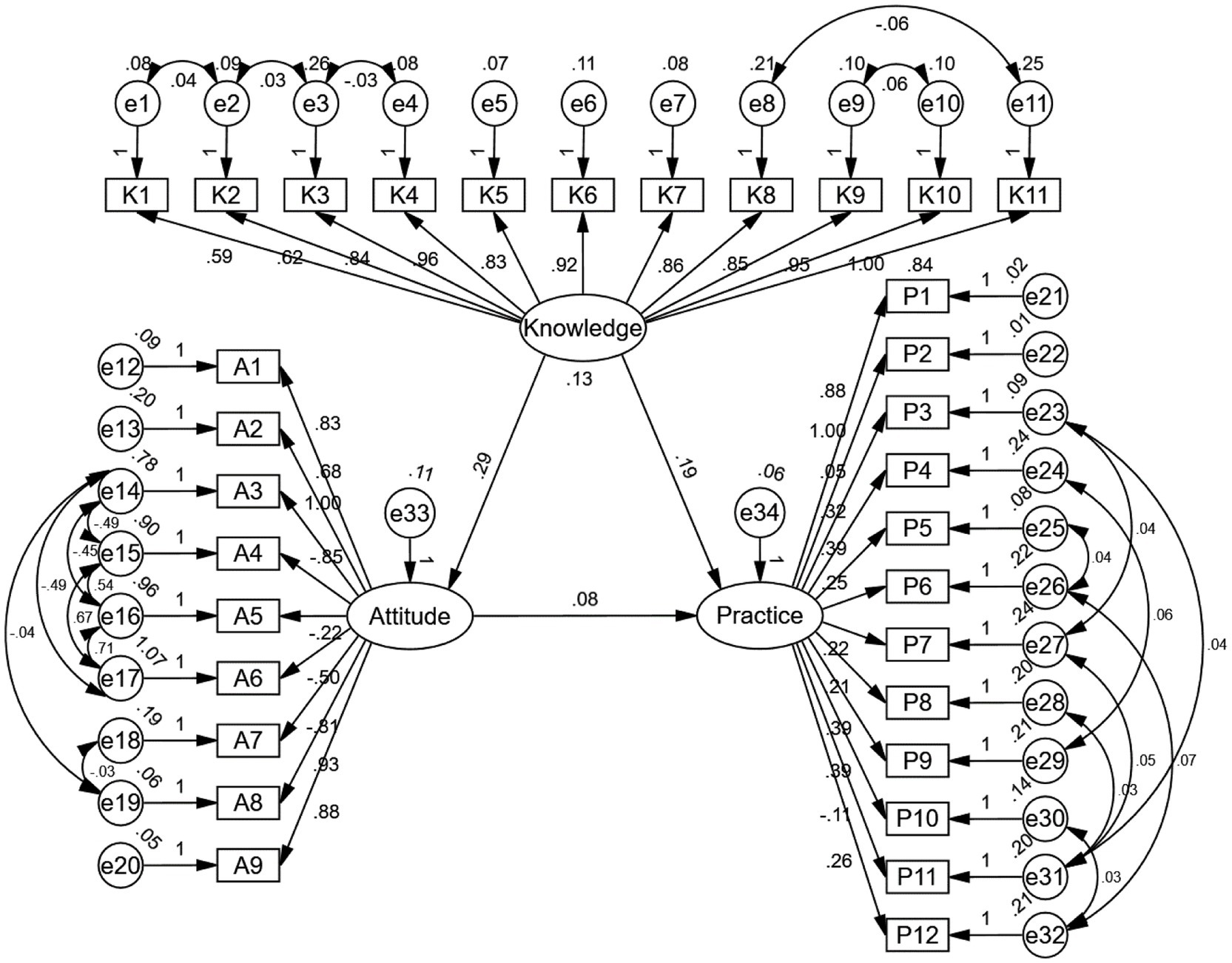
Results: The survey yielded 504 valid questionnaires. Of the respondents, 306 (60.71%) had a Body Mass Index (BMI) within the optimal range of 18.5–23.9 kg/m2. The mean scores for knowledge, attitude, and practice were 10.13 ± 3.58 (possible range: 0–22), 31.38 ± 2.38 (possible range: 9–45), and 4.46 ± 2.30 (possible range: 0–12), respectively. Correlation analysis revealed significant relationships between knowledge and practice (r = 0.294, p < 0.001) as well as between attitude and practice (r = 0.178, p < 0.001). Multivariate logistic regression showed that knowledge score (OR = 1.165, 95% CI: [1.078, 1.259], p < 0.001) was independently associated with proactive practice. The structural equation model (SEM) results showed that knowledge had direct effects on attitude (β = 0.291, p < 0.001) and practice (β = 0.188, p < 0.001). Meanwhile, attitude had a direct impact on practice (β = 0.081, p = 0.045).
Conclusion: This study indicates that patients with RA generally demonstrate inadequate knowledge but hold positive attitudes toward dietary management, despite relatively inactive practices in implementing such dietary changes. Healthcare providers should prioritize educational interventions that not only enhance patient understanding but also actively support the implementation of dietary management strategies in clinical settings.
Introduction
Rheumatoid arthritis (RA) is a chronic systemic autoimmune disease characterized by unknown etiology and significant joint damage. It globally affects approximately 460 individuals per 100,000 population (1), with a prevalence of 0.32–0.42% within the Chinese population (2). If RA is not adequately treated, it can lead to persistent synovitis and the erosion of articular cartilage and surrounding bone, resulting in reduced mobility, decreased quality of life, and complications including cardiovascular and other extra-articular issues (3, 4). In addition to these complications, RA is often associated with metabolic comorbidities such as diabetes. Studies have shown that patients with RA are at an increased risk of developing type 2 diabetes due to chronic inflammation and glucocorticoid use, which can impair insulin sensitivity and glycemic control. Managing these comorbidities requires a holistic approach, where diet plays a pivotal role not only in mitigating RA symptoms but also in controlling blood glucose levels in diabetic RA patients (5, 6).
Dietary management is essential in RA treatment, as specific foods can help reduce inflammation and improve patient outcomes (7). For instance, diets rich in anti-inflammatory components, such as omega-3 fatty acids, have been shown to alleviate RA symptoms, while unhealthy choices may worsen them (8). Understanding how RA patients approach dietary management is vital for effective care.
Management of RA involves a comprehensive approach that includes both pharmacologic and non-pharmacologic (9, 10). Pharmacologic treatments primarily consist of disease-modifying anti-rheumatic drugs (DMARDs), nonsteroidal anti-inflammatory drugs (NSAIDs), and glucocorticoids, which help manage the inflammation and pain associated with the disease (4). Complementarily, non-pharmacologic treatments such as patient education, physiotherapy, and nutritional therapy play critical roles in the overall management of RA (11).
The Knowledge-Attitude-Practice (KAP) model is a crucial framework in the healthcare domain, extensively used to assess the knowledge, attitudes, and practices of target populations (12). This model is founded on the premise that enhanced knowledge positively influences attitudes, which in turn, shape individual practices, a process integral to health literacy (13). The use of the KAP questionnaire alongside this model helps evaluate the demand and level of acceptance of health-related content (14).
Diet, as a key modifiable factor in chronic disease management, significantly impacts patient outcomes, with robust evidence supporting the benefits of dietary improvements (15). For patients with rheumatoid arthritis (RA), dietary choices are critical as they can influence symptoms significantly; certain foods, especially those rich in n-3 polyunsaturated fatty acids (PUFAs) from fish, have been shown to alleviate symptoms, while unhealthy options may exacerbate them. Additionally, evidence suggests that dietary management can play a crucial role in preventing and managing diabetes in RA patients, with anti-inflammatory and low-glycemic diets helping control both inflammation and blood sugar levels (16, 17).
Despite the established importance of diet in RA management, there is a notable gap in research focusing on the KAP regarding dietary management among these patients. While there have been studies examining KAP in patients with chronic conditions like diabetes, the specific area of dietary KAP in RA patients remains underexplored. By exploring how RA patients perceive and implement dietary recommendations, researchers can pinpoint knowledge gaps and barriers to effective management. This understanding is essential for creating targeted educational programs and interventions that enhance dietary habits, thereby improving the quality of life and health outcomes. Therefore, this study aims to assess the KAP regarding dietary management among patients with RA, addressing an underserved area of research with potential significant clinical implications.
Methods
Study design and participants
This cross-sectional study was conducted from November 2023 to May 2024 at JiuJiang NO.1 People’s Hospital. The study participants were patients with rheumatoid arthritis (RA). The study was approved by the Ethics Committee of JiuJiang NO.1 People’s Hospital (Ethic No. JJSDYRMYY-YXLL-2023-217), and written informed consent was obtained from all participants.
Inclusion criteria: Patients diagnosed with rheumatoid arthritis (meeting the 1987 ACR or 2010 ACR/EULAR criteria), who can communicate effectively in the local language, possess sufficient reading and writing skills, and are willing to participate.
Exclusion criteria: Patients with cognitive impairments, severe organic diseases or complications, or concurrent malignant tumors.
Questionnaire distribution: The survey was conducted via the Wenjuanxing platform and disseminated using WeChat and WeChat groups.
Questionnaire introduction
The questionnaire was developed in accordance with established guidelines and relevant literature (8, 18, 19), enriched by insights from multiple experts in the specified field. Prior to full implementation, it underwent a preliminary test involving a small cohort of 47 participants. The results from this pre-test demonstrated a robust overall reliability coefficient of 0.801. Specifically, the reliability coefficients for the knowledge, attitudes, and practices sections were 0.898, 0.680, and 0.759, respectively, indicating satisfactory internal consistency across both the overall questionnaire and its discrete sections.
The final version of the questionnaire, written in Chinese, comprised four distinct dimensions for collecting information, totaling 48 items. These dimensions included: Basic Information with 16 items, Knowledge with 11 items, Attitudes with 9 items, and Practices with 12 items.
For statistical analysis, the scoring for each item varied according to the dimension it belonged to. In the Knowledge Dimension (items K1 to K11), scoring was as follows: “Very familiar” earned 2 points, “Somewhat familiar” earned 1 point, and “Not familiar” received 0 points, with the total possible score ranging from 0 to 22 points. For the Attitude Dimension, scoring differed based on the nature of the statement: positive items (A1–A3, A7–A9) scored from 5 points for “Strongly agree” to 1 point for “Strongly disagree,” while negative items (A4–A6) scored inversely, with “Strongly agree” earning 1 point and “Strongly disagree” 5 points, leading to a total score range of 9–45 points. The Practice Dimension simply assigned 1 point for “Yes” responses and 0 points for “No,” with a potential score range from 0 to 12 points. A scoring threshold exceeding 60% for each dimension was set to determine adequate knowledge, positive attitudes, and proactive practices (20).
Sample size calculation
The sample size was calculated based on the minimum sample size formula for cross-sectional studies:
Where
• α = 0.05.
• = 1.96.
• δ = 0.05.
• p = 0.5
Using these values, the calculated minimum sample size was 384. This sample size is adequate to ensure a robust representation of the population and provide sufficient statistical power for the analysis. Considering an 80% effective response rate, at least 480 questionnaires were planned to be collected to account for potential non-responses or incomplete data.
Statistical analysis
Data analysis was conducted using SPSS 27.0 (IBM, Armonk, NY, USA) and AMOS 26.0 (IBM, Armonk, NY, USA). Continuous data are presented as means and standard deviations (SD), while categorical data are expressed as n (%). Continuous variables underwent a normality test, with the t-test for normally distributed data and the Wilcoxon Mann–Whitney test for non-normally distributed data when comparing two groups. For three or more groups with normally distributed continuous variables and uniform variance, ANOVA was used for comparisons, while the Kruskal–Wallis test was employed for non-normally distributed data. Univariate and multivariate logistic regression were performed to explore the risk factors associated with K, A, and P, with 60% of the total score was used as the cut-off value. Structural equation modeling (SEM) was utilized to explore the relationships between knowledge (K), attitude (A), and practice (P). Model fit was evaluated using root mean square error of approximation (RMSEA), incremental fit index (IFI), Tucker–Lewis index (TLI), and comparative fit index (CFI). A two-sided p-value less than 0.05 was considered statistically significant.
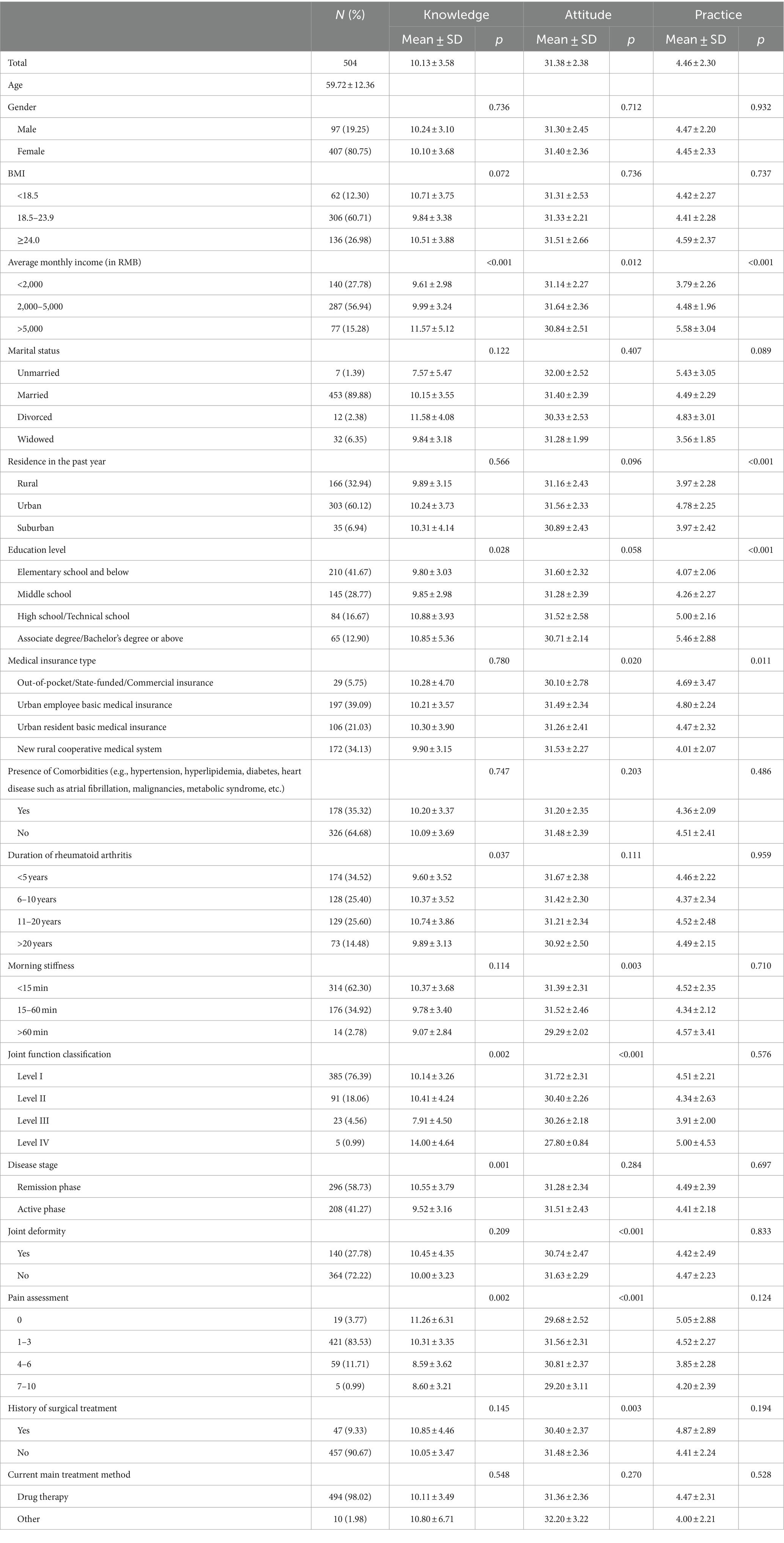
Results
Initially, this study collected a total of 507 questionnaires. Of these, one was excluded due to the respondent being underage (0.20%), and two were excluded due to incorrect age data (0.39%), resulting in 504 valid questionnaires. The validity rate was 99.41%. Among the respondents, 407 (80.75%) were female, with a mean age of 59.72 ± 12.36 years. A total of 306 participants (60.71%) reported a BMI within the range of 18.5–23.9 kg/m2. Regarding socioeconomic status, 287 respondents (56.94%) reported an average monthly income of 2,000–5,000 yuan, and 210 (41.67%) had attained an elementary school level education or lower. Furthermore, 174 participants (34.52%) had been diagnosed with rheumatoid arthritis for less than 5 years. Morning stiffness of less than 15 min was reported by 314 respondents (62.30%), while 296 (58.73%) were in the remission phase of the disease, 140 (27.78%) presented with joint deformity, and 494 (98.02%) were currently receiving pharmacological treatment as their primary form of management. The mean scores for knowledge, attitude, and practice were 10.13 ± 3.58, 31.38 ± 2.38, and 4.46 ± 2.30, respectively. Variations in knowledge scores were significantly associated with average monthly income (p < 0.001), educational attainment (p = 0.028), duration of rheumatoid arthritis (p = 0.037), joint function classification (p = 0.002), disease stage (p = 0.001), and pain assessment (p = 0.002). Attitude scores varied significantly across variables such as average monthly income (p = 0.012), type of medical insurance (p = 0.020), morning stiffness (p = 0.003), joint function classification (p < 0.001), joint deformity (p < 0.001), pain assessment (p < 0.001), and history of surgical treatment (p = 0.003). Practice scores showed significant variation based on average monthly income (p < 0.001), past year residence (p < 0.001), education level (p < 0.001), and medical insurance type (p = 0.011) (Table 1).
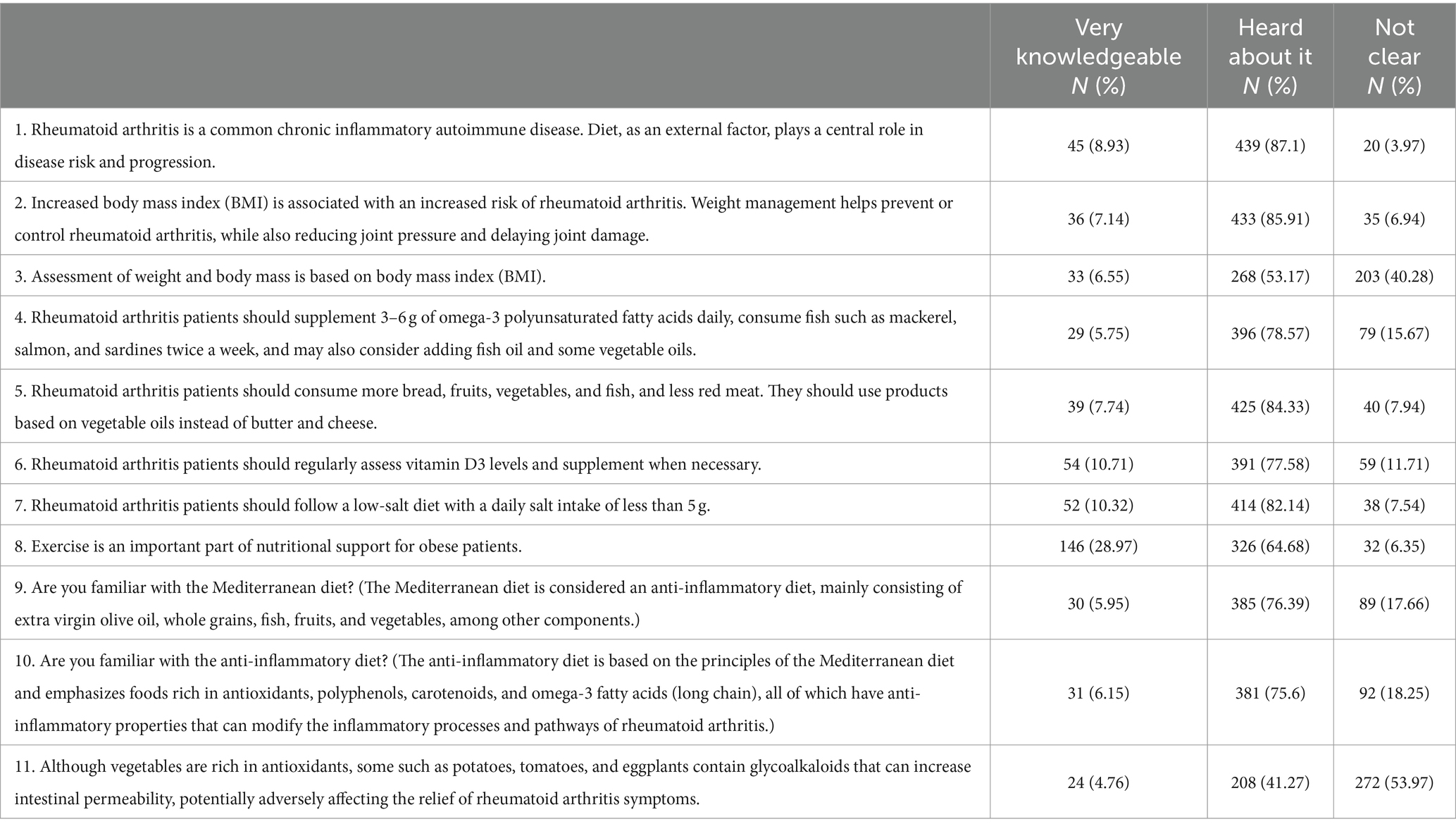
The distribution of knowledge dimensions shown that the three questions with the highest number of participants choosing the “Not clear” option were “Although vegetables are rich in antioxidants, some such as potatoes, tomatoes, and eggplants contain glycoalkaloids that can increase intestinal permeability, potentially adversely affecting the relief of rheumatoid arthritis symptoms.” (K11) with 53.97%, “Assessment of weight and body mass is based on body mass index (BMI).” (K3) with 40.28%, and “Are you familiar with the anti-inflammatory diet?” (K10) with 18.25% (Table 2).
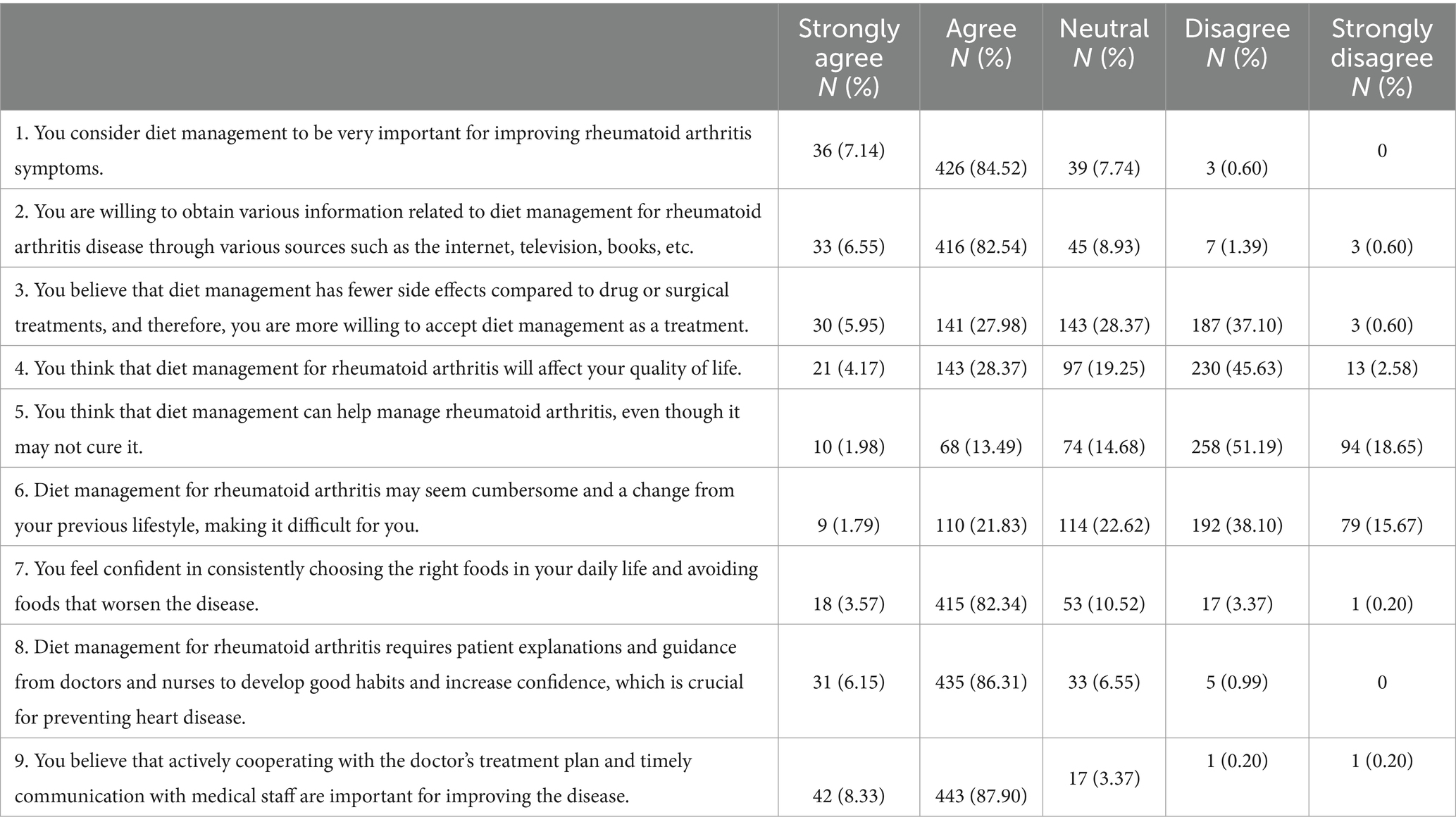
Responses to the attitudinal dimension showed that 37.10% disagreed that they would prefer to be treated with diet management (A3), 28.37% agreed that diet management would affect their quality of life (A4), and 21.83% agreed that diet management was too burdensome and changed habits, which was difficult for them (A6) (Table 3).
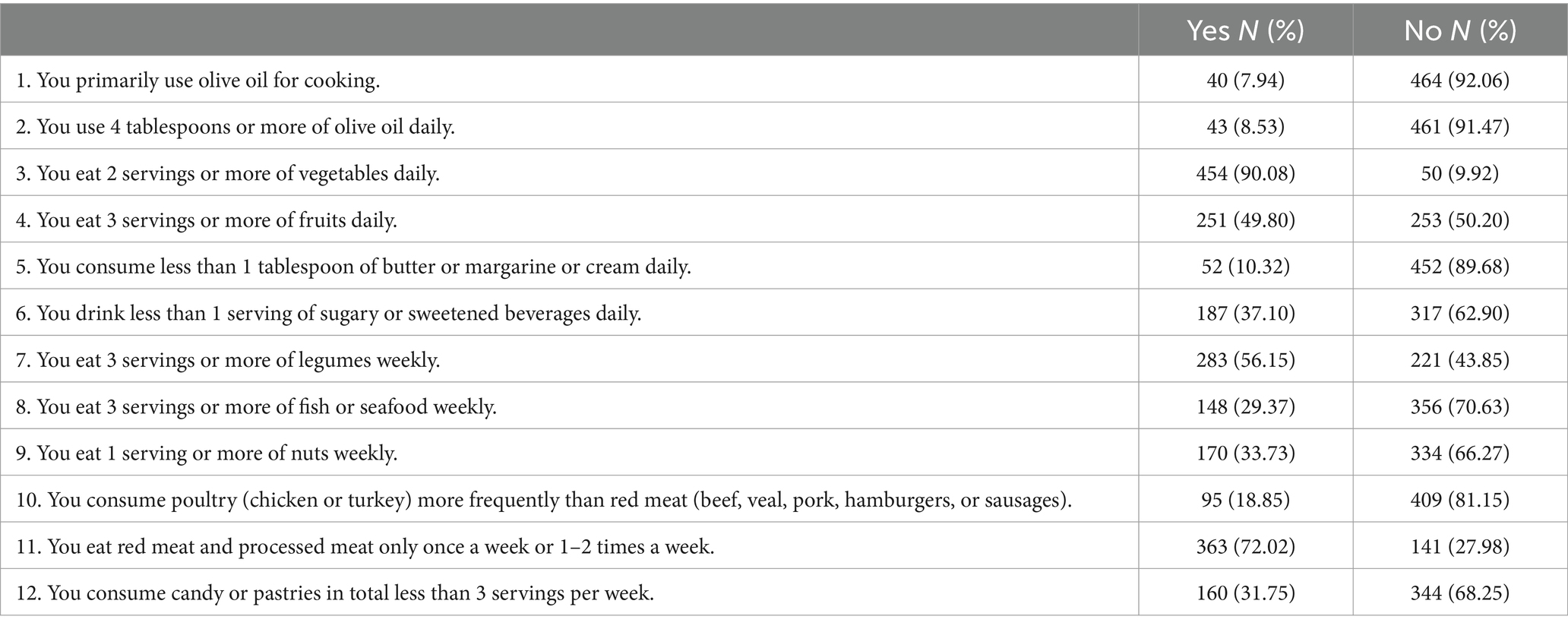
The distribution of practice dimensions shown that the three questions with the highest number of participants choosing the “No” option were “You primarily use olive oil for cooking.” (P1) with 92.06%, “You use 4 tablespoons or more of olive oil daily.” (P2) with 91.47%, and “You consume less than 1 tablespoon of butter or margarine or cream daily.” (P5) with 89.68% (Table 4).
Correlation analysis revealed significant relationships between knowledge and practice (r = 0.294, p < 0.001) as well as between attitude and practice (r = 0.178, p < 0.001) (Table 5).
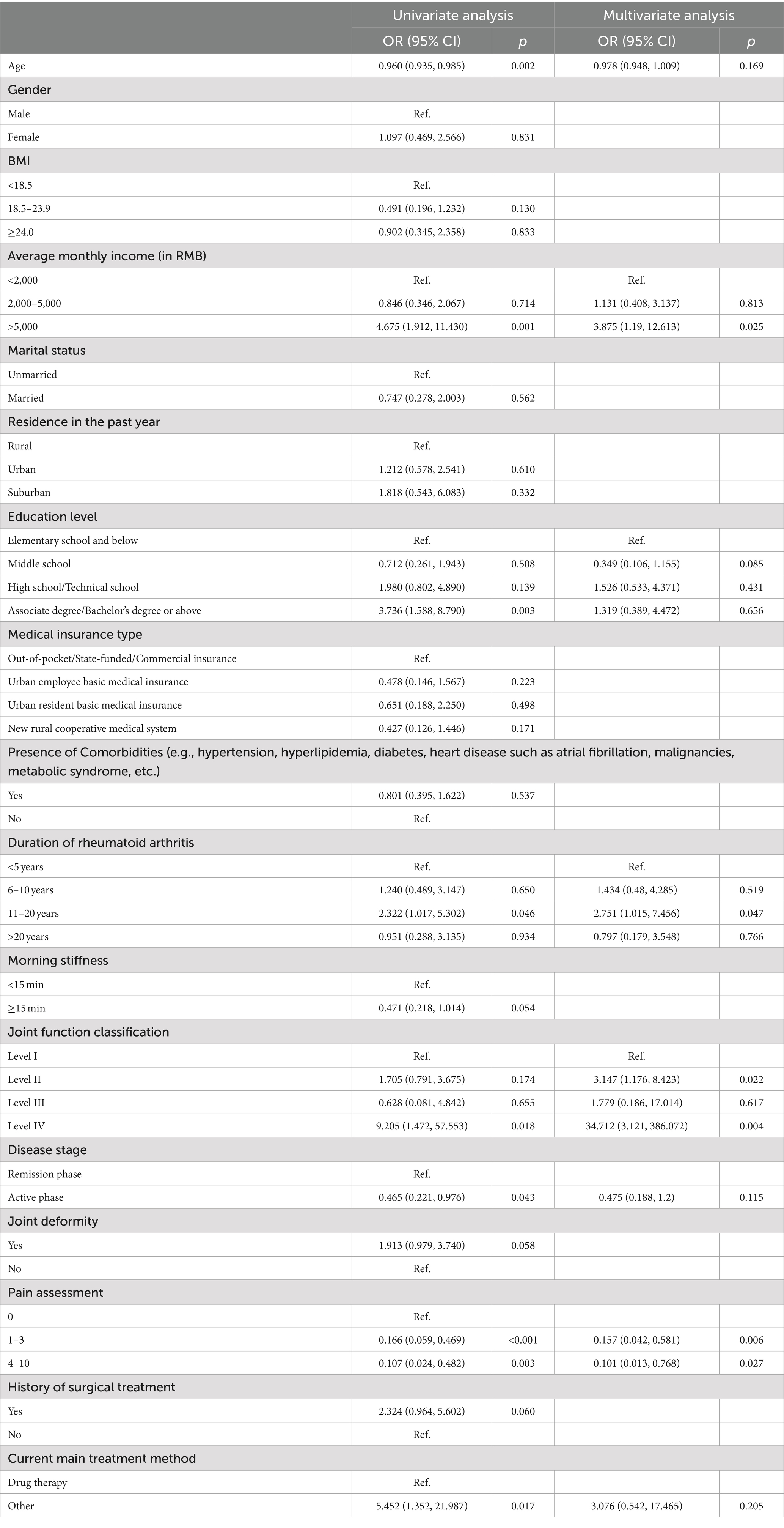
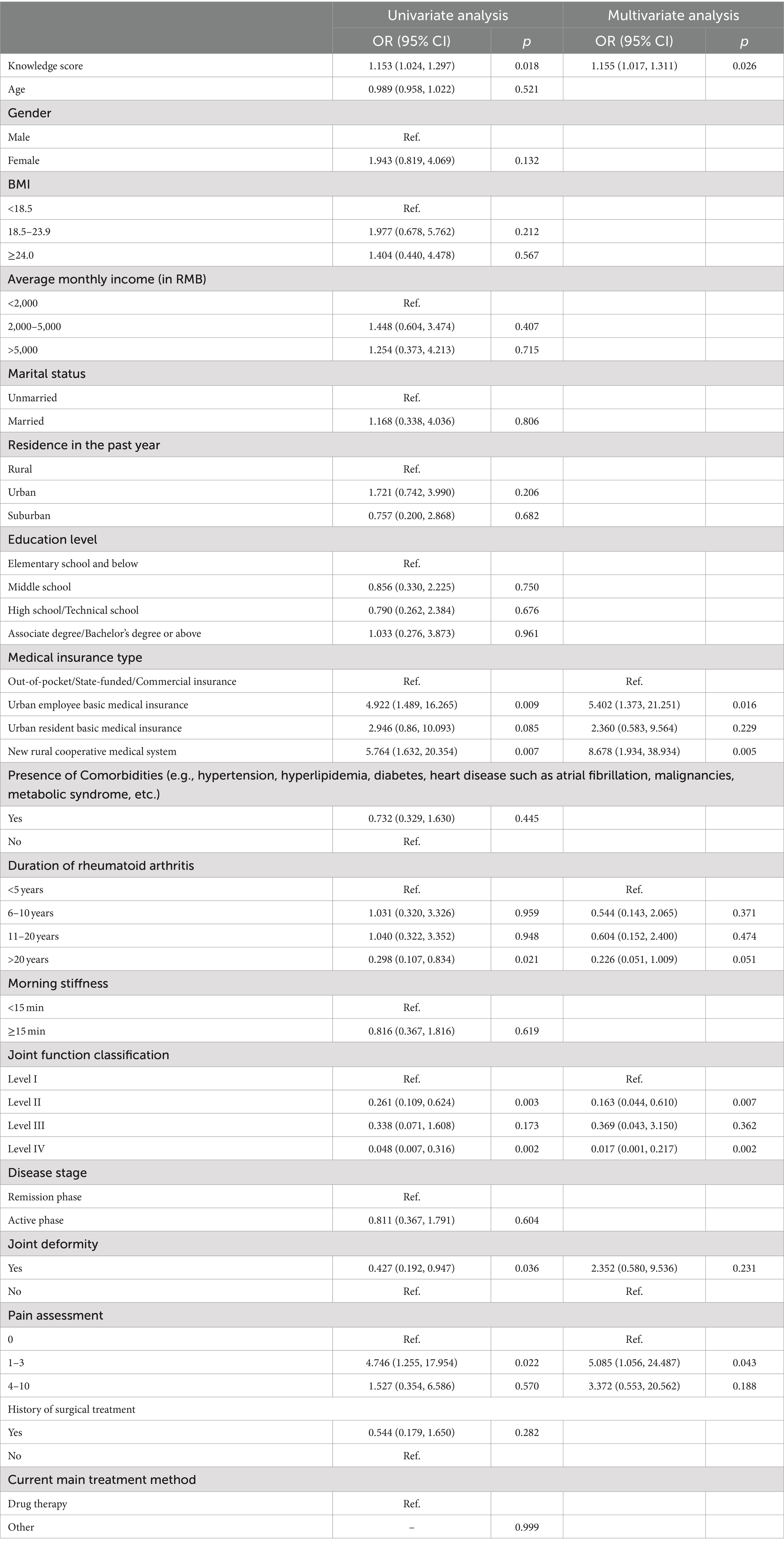
A cutoff value representing the top 60% of scores for each dimension was used to classify the participants, with 465 (92.26%) falling below this threshold for knowledge, 26 (5.16%) for attitude, and 460 (91.27%) for practice (Supplementary Table S1). Multivariate logistic regression showed that with average monthly income (OR = 3.875, 95% CI: [1.19, 12.613], p = 0.025), had rheumatoid arthritis for 11–20 years (OR = 2.751, 95% CI: [1.015, 7.456], p = 0.047), level II joint function (OR = 3.147, 95% CI: [1.176, 8.423], p = 0.022), level IV joint function (OR = 34.712, 95% CI: [3.121, 386.072], p = 0.004), pain assessment score 1–3 (OR = 0.157, 95% CI: [0.042, 0.581], p = 0.006), and pain assessment score 4–10 (OR = 0.101, 95% CI: [0.013, 0.768], p = 0.027) were independently associated with knowledge (Table 6). Concurrently, knowledge score (OR = 1.155, 95% CI: [1.017, 1.311], p = 0.026), with urban employee basic medical insurance (OR = 5.402, 95% CI: [1.373, 21.251], p = 0.016), with new rural cooperative medical system (OR = 8.678, 95% CI: [1.934, 38.934], p = 0.005), level II joint function (OR = 0.163, 95% CI: [0.044, 0.610], p = 0.007), level IV joint function (OR = 0.017, 95% CI: [0.001, 0.217], p = 0.002), pain assessment score 1–3 (OR = 5.085, 95% CI: [1.056, 24.487], p = 0.043) were independently associated with attitude (Table 7). Moreover, knowledge score (OR = 1.165, 95% CI: [1.078, 1.259], p < 0.001) was independently associated with proactive practice (Table 8).
The residual connection method was adopted to modify the SEM model so as to achieve a good fit (CMIN/DF value: 3.853, RMSEA value: 0.075, IFI value: 0.811, TLI value: 0.785, and CFI value: 0.810) (Supplementary Table S2), the results showed that knowledge had direct effects on attitude (β = 0.291, p < 0.001) and practice (β = 0.188, p < 0.001). Meanwhile, attitude had a direct impact on practice (β = 0.081, p = 0.045) (Supplementary Table S3 and Figure 1).
Discussion
The study highlights a significant discrepancy among patients with RA, demonstrating inadequate knowledge but relatively positive attitudes toward dietary management, which did not strongly translate into active practice. It is recommended that clinical programs for RA patients incorporate targeted educational interventions to enhance dietary management knowledge, aiming to bridge the gap between attitudes and actual practices to improve health outcomes.
This study underscores a significant discrepancy between the positive attitudes toward dietary management in RA patients and their relatively insufficient knowledge and suboptimal practices. This finding is consistent with other studies indicating that while patients may be receptive to managing their condition through diet, a lack of comprehensive knowledge often hinders effective implementation (21, 22).
Specific factors such as average monthly income and education level significantly impacted KAP scores. For instance, participants with higher incomes exhibited better knowledge and practices, a pattern also reflected in the regression analysis where higher income was associated with improved knowledge. This finding suggests that economic factors may influence access to resources or educational opportunities that can enhance self-management capabilities (23, 24). Similarly, educational attainment correlated with knowledge and practice outcomes, reinforcing the need for tailored educational interventions that consider the varied socioeconomic backgrounds of patients.
Interestingly, while variables such as joint function classification and pain assessment significantly affected knowledge and attitudes, they did not markedly influence practice outcomes. This could be due to a lag between changes in perception and the actual adoption of new behaviors, or it may reflect other unmeasured barriers to behavior change such as physical limitations or psychosocial factors (25, 26).
The correlation and multivariate logistic regression analyses, as well as SEM, suggest a complex interplay between knowledge, attitudes, and practices. Our findings indicate that better knowledge about RA directly enhances both attitudes and practices, supporting the notion that informed patients are more likely to adopt and maintain beneficial dietary habits (27, 28). These results were consistent with previous research that emphasizes the pivotal role of patient education in chronic disease management (29, 30).
The findings from the knowledge dimension reveal substantial gaps in the understanding of dietary management among RA patients. A significant portion of the cohort displayed limited awareness of the role of BMI in RA risk, the importance of omega-3 fatty acids, and the specifics of anti-inflammatory diets such as the Mediterranean diet. This lack of knowledge was particularly pronounced concerning the impact of certain vegetables like potatoes, tomatoes, and eggplants on intestinal permeability and RA symptoms. To address these deficiencies, healthcare providers should implement targeted educational programs that not only explain the importance of diet in managing RA but also clarify common misconceptions. Programs could include detailed patient brochures, interactive online platforms, and structured dietary counseling sessions that tailor content to individual knowledge gaps and cultural preferences (31, 32).
Attitudinal responses highlighted a general recognition of the importance of diet management in RA, yet there was notable reluctance regarding its practical application and potential impact on quality of life. Particularly, many patients viewed diet management as cumbersome and less preferable compared to pharmacological treatments. To enhance acceptance and willingness to engage in dietary management, it is crucial to foster a supportive environment that empowers patients. This could be achieved through regular motivational interviewing sessions that address personal barriers and benefits perceived by patients, as well as through the development of peer-led support groups that provide empathy and practical tips from shared experiences. Furthermore, incorporating mobile health technologies that track dietary intake and provide real-time feedback could improve patients’ engagement and adherence (7, 33).
Practical adherence to recommended dietary guidelines was low, particularly in the usage of olive oil, the consumption of fish, fruits, and legumes, as well as in the reduction of red meat intake. This poor adherence might be reflective of both a lack of conviction in the efficacy of dietary measures and the perceived difficulty in integrating these into daily life (34, 35). To promote better dietary practices among RA patients, practical and accessible interventions are needed. This could include working with dietitians to create personalized meal plans that accommodate individual preferences and limitations, offering cooking classes that focus on preparing anti-inflammatory meals, and establishing partnerships with local food services to provide discounts on healthful food options. Additionally, implementing community-based programs that emphasize the social aspect of eating could help normalize and reinforce dietary changes (36, 37).
This study has several limitations that warrant consideration. First, the cross-sectional design limits the ability to establish causal relationships between the knowledge, attitudes, and practices regarding dietary management and rheumatoid arthritis outcomes. Second, the lack of a control group, as suggested, limits the ability to directly compare RA patients with a healthy population. Future studies should incorporate a quasi-experimental design to address this gap. In addition, the data were collected from a single institution, which may restrict the generalizability of the findings to broader populations with diverse healthcare settings and cultural backgrounds. Lastly, self-reported measures were used to assess dietary practices, which might introduce response biases and may not accurately reflect actual dietary behaviors.
Conclusion
In conclusion, this study indicates that patients with RA demonstrate a discrepancy between a positive attitude toward dietary management and both insufficient knowledge and suboptimal practices. Significant predictors of better knowledge and attitudes include socioeconomic status, duration of RA, joint function, and type of medical insurance, which also influence dietary practices. These findings highlight the need for healthcare providers to integrate more robust dietary education into patient care. By offering clearer guidance on anti-inflammatory diets and providing continuous support, clinicians can help patients better manage RA symptoms, ultimately leading to improved treatment outcomes. Adjusting care plans to include routine dietary counseling may enhance the overall effectiveness of RA management.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by JiuJiang NO.1 People’s Hospital (Ethic No. JJSDYRMYY-YXLL-2023-217). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XL: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. JL: Conceptualization, Formal analysis, Visualization, Writing – original draft, Writing – review & editing. JY: Data curation, Formal analysis, Resources, Writing – original draft, Writing – review & editing. LD: Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1490189/full#supplementary-material
References
1. Almutairi, K, Nossent, J, Preen, D, Keen, H, and Inderjeeth, C. The global prevalence of rheumatoid arthritis: a meta-analysis based on a systematic review. Rheumatol Int. (2021) 41:863–77. doi: 10.1007/s00296-020-04731-0
2. Jin, S, Li, M, Fang, Y, Li, Q, Liu, J, Duan, X, et al. Chinese registry of rheumatoid arthritis (CREDIT): II. Prevalence and risk factors of major comorbidities in Chinese patients with rheumatoid arthritis. Arthritis Res Ther. (2017) 19:251. doi: 10.1186/s13075-017-1457-z
3. McInnes, IB, and Schett, G. The pathogenesis of rheumatoid arthritis. N Engl J Med. (2011) 365:2205–19. doi: 10.1056/NEJMra1004965
4. Smolen, JS, Aletaha, D, Barton, A, Burmester, GR, Emery, P, Firestein, GS, et al. Rheumatoid arthritis. Nat Rev Dis Primers. (2018) 4:18001. doi: 10.1038/nrdp.2018.1
5. Papakonstantinou, E, Oikonomou, C, Nychas, G, and Dimitriadis, GD. Effects of diet, lifestyle, Chrononutrition and alternative dietary interventions on postprandial glycemia and insulin resistance. Nutrients. (2022) 14:823. doi: 10.3390/nu14040823
6. Papamichou, D, Panagiotakos, DB, and Itsiopoulos, C. Dietary patterns and management of type 2 diabetes: a systematic review of randomised clinical trials. Nutr Metab Cardiovasc Dis. (2019) 29:531–43. doi: 10.1016/j.numecd.2019.02.004
7. Gioia, C, Lucchino, B, Tarsitano, MG, Iannuccelli, C, and Di Franco, M. Dietary habits and nutrition in rheumatoid arthritis: can diet influence disease development and clinical manifestations? Nutrients. (2020) 12:1456. doi: 10.3390/nu12051456
8. Philippou, E, Petersson, SD, Rodomar, C, and Nikiphorou, E. Rheumatoid arthritis and dietary interventions: systematic review of clinical trials. Nutr Rev. (2021) 79:410–28. doi: 10.1093/nutrit/nuaa033
9. Mishra, V, Pandey, RP, Priyadarshini, A, Chang, CM, and Leal, E eds. Nanotherapeutics for inflammatory arthritis: design, diagnosis, and treatment. 1st ed. Boca Raton: CRC Press (2024).
10. Rani, M, Ranjan, KR, and Mishra, V. Nanotherapeutics and rheumatoid arthritis In: Nanotherapeutics for inflammatory arthritis: design, diagnosis, and treatment : CRC Press (2024). 143–59.
11. Genel, F, Kale, M, Pavlovic, N, Flood, VM, Naylor, JM, and Adie, S. Health effects of a low-inflammatory diet in adults with arthritis: a systematic review and meta-analysis. J Nutr Sci. (2020) 9:e37. doi: 10.1017/jns.2020.31
12. Li, L, Zhang, J, Qiao, Q, Wu, L, and Chen, L. Development, reliability, and validity of the “knowledge-attitude-practice” questionnaire of foreigners on traditional Chinese medicine treatment. Evid Based Complement Alternat Med. (2020) 2020:8527320. doi: 10.1155/2020/8527320
13. Khalid, A, Haque, S, Alvi, S, Ferdous, M, Genereux, O, Chowdhury, N, et al. Promoting health literacy about cancer screening among Muslim immigrants in Canada: perspectives of imams on the role they can play in community. J Prim Care Community Health. (2022) 13:21501319211063051. doi: 10.1177/21501319211063051
14. Tan, J, Luo, L, Zhang, M, Chen, H, Zhang, D, Dong, C, et al. A Chinese and Western medication adherence scale in patients with chronic kidney disease. Patient Prefer Adherence. (2019) 13:1487–95. doi: 10.2147/PPA.S207693
15. Mastronuzzi, T, and Grattagliano, I. Nutrition as a health determinant in elderly patients. Curr Med Chem. (2019) 26:3652–61. doi: 10.2174/0929867324666170523125806
16. Parke, AL, and Hughes, GR. Rheumatoid arthritis and food: a case study. Br Med J (Clin Res Ed). (1981) 282:2027–9. doi: 10.1136/bmj.282.6281.2027
17. Rondanelli, M, Perdoni, F, Peroni, G, Caporali, R, Gasparri, C, Riva, A, et al. Ideal food pyramid for patients with rheumatoid arthritis: a narrative review. Clin Nutr. (2021) 40:661–89. doi: 10.1016/j.clnu.2020.08.020
18. England, BR, Smith, BJ, Baker, NA, Barton, JL, Oatis, CA, Guyatt, G, et al. 2022 American College of Rheumatology Guideline for exercise, rehabilitation, diet, and additional integrative interventions for rheumatoid arthritis. Arthritis Rheumatol. (2023) 75:1299–311. doi: 10.1002/art.42507
19. England, BR, Smith, BJ, Baker, NA, Barton, JL, Oatis, CA, Guyatt, G, et al. 2022 American College of Rheumatology Guideline for exercise, rehabilitation, diet, and additional integrative interventions for rheumatoid arthritis. Arthritis Care Res. (2023) 75:1603–15. doi: 10.1002/acr.25117
20. ALruwaili, BF, Thirunavukkarasu, A, Alsaidan, AA, Al-Ruwaili, AM, Alanazi, RBS, Alruwaili, AMB, et al. Knowledge, attitude, and practice towards evidence-based medicine among northern Saudi primary care physicians: a cross-sectional study. Healthcare (Basel). (2022) 10:2285. doi: 10.3390/healthcare10112285
21. Areri, H, Marshall, A, and Harvey, G. Factors influencing self-management of adults living with HIV on antiretroviral therapy in Northwest Ethiopia: a cross-sectional study. BMC Infect Dis. (2020) 20:879. doi: 10.1186/s12879-020-05618-y
22. Lim, JY, Rajikan, R, Amit, N, Ali, NM, Hamid, HA, Leong, HY, et al. Exploring the barriers and motivators to dietary adherence among caregivers of children with disorders of amino acid metabolism (AAMDs): a qualitative study. Nutrients. (2022) 14:2535. doi: 10.3390/nu14122535
23. Islam, MA, AlShayban, DM, Nisa, ZU, Al-Hawaj, GAM, Al-Eid, GHA, Alenazi, AMM, et al. What is the current state of awareness, knowledge, and attitudes toward breast cancer? A cross-sectional survey among health and non-health college students. Front Public Health. (2022) 10:838579. doi: 10.3389/fpubh.2022.838579
24. Sun, M, Xiong, L, Li, L, Chen, Y, Tang, J, Hua, W, et al. Digital divide in online education during the COVID-19 pandemic: a cosmetic course from the view of the regional socioeconomic distribution. Front Public Health. (2021) 9:796210. doi: 10.3389/fpubh.2021.800852
25. Lorlowhakarn, K, Kitphati, S, Songngerndee, V, Tanathaipakdee, C, Sinphurmsukskul, S, Siwamogsatham, S, et al. Thyrotoxicosis-induced cardiomyopathy complicated by refractory cardiogenic shock rescued by extracorporeal membrane oxygenation. Am J Case Rep. (2022) 23:e935029. doi: 10.12659/AJCR.935029
26. Wang, WC, Zou, SM, Ding, Z, and Fang, JY. Nutritional knowledge, attitude and practices among pregnant females in 2020 Shenzhen China: a cross-sectional study. Prev Med Rep. (2023) 32:102155. doi: 10.1016/j.pmedr.2023.102155
27. Asoudeh, F, Djafarian, K, Akhalghi, M, Mahmoudi, M, Jamshidi, AR, Farhadi, E, et al. The effect of probiotic cheese consumption on inflammatory and anti-inflammatory markers, disease severity, and symptoms in patients with rheumatoid arthritis: study protocol for a randomized, double-blind, placebo-controlled trial. Trials. (2022) 23:180. doi: 10.1186/s13063-022-06113-2
28. Şengelen, A, and Önay-Uçar, E. Rosmarinic acid and siRNA combined therapy represses Hsp27 (HSPB1) expression and induces apoptosis in human glioma cells. Cell Stress Chaperones. (2018) 23:885–96. doi: 10.1007/s12192-018-0896-z
29. Choi, JY, Kim, KI, and Kim, CH. Effect of home blood pressure monitoring for blood pressure control in hypertensive patients taking multiple antihypertensive medications including fimasartan (the FORTE study). Clin Hypertens. (2020) 26:24. doi: 10.1186/s40885-020-00154-y
30. Tang, S, Liu, M, Yang, T, Ye, C, Gong, Y, Yao, L, et al. Association between falls in elderly and the number of chronic diseases and health-related behaviors based on CHARLS 2018: health status as a mediating variable. BMC Geriatr. (2022) 22:374. doi: 10.1186/s12877-022-03055-x
31. Sparks, JA. Rheumatoid arthritis. Ann Intern Med. (2019) 170:Itc1–itc16. doi: 10.7326/AITC201901010
32. Zhao, SS, Holmes, MV, Zheng, J, Sanderson, E, and Carter, AR. The impact of education inequality on rheumatoid arthritis risk is mediated by smoking and body mass index: mendelian randomization study. Rheumatology (Oxford). (2022) 61:2167–75. doi: 10.1093/rheumatology/keab654
33. Nikiphorou, E, and Philippou, E. Nutrition and its role in prevention and management of rheumatoid arthritis. Autoimmun Rev. (2023) 22:103333. doi: 10.1016/j.autrev.2023.103333
34. Bárdos, H, Llanaj, E, Vincze, F, Diószegi, J, Pikó, P, Kósa, Z, et al. Diet quality as assessed by healthy eating index-2015 among Hungarian Roma living in settlements of Northeast Hungary. Sci Rep. (2022) 12:19213. doi: 10.1038/s41598-022-23670-3
35. Ramón-Arbués, E, Granada-López, JM, Martínez-Abadía, B, Echániz-Serrano, E, Antón-Solanas, I, and Jerue, BA. The association between diet and sleep quality among Spanish university students. Nutrients. (2022) 14:3291. doi: 10.3390/nu14163291
36. Chehade, L, Jaafar, ZA, El Masri, D, Zmerly, H, Kreidieh, D, Tannir, H, et al. Lifestyle modification in rheumatoid arthritis: dietary and physical activity recommendations based on evidence. Curr Rheumatol Rev. (2019) 15:209–14. doi: 10.2174/1573397115666190121135940
Keywords: knowledge, attitude, practice, dietary management, patients, rheumatoid arthritis
Citation: Li X, Liu J, Yu J and Dong L (2024) Knowledge, attitudes, and practices of dietary management among patients with rheumatoid arthritis in China. Front. Public Health. 12:1490189. doi: 10.3389/fpubh.2024.1490189
Edited by:
Vivek Mishra, Amity University, IndiaReviewed by:
Ramendra Pati Pandey, SRM University (Delhi-NCR), IndiaAnil Kumar Mavi, University of Delhi, India
Vikas Shukla, All India Institute of Medical Sciences, India
Copyright © 2024 Li, Liu, Yu and Dong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xueyong Li, anhseHkyMDA2QDEyNi5jb20=
 Xueyong Li
Xueyong Li Ju Liu1
Ju Liu1 Jie Yu
Jie Yu