- 1Department of Movement and Training Science, University of Wuppertal, Wuppertal, Germany
- 2Department of Intervention Research in Exercise Training, German Sport University Cologne, Cologne, Germany
- 3Department of Sports Medicine and Exercise Physiology, Institute of Occupational, Social and Environmental Medicine, Goethe University Frankfurt, Frankfurt/Main, Germany
Introduction: This study investigated potential health status differences among forging, manufacturing, and logistics workers.
Methods: We included 403 participants (age: 41 ± 12 years) from a medium-sized steel company (forge: 64, manufacturing: 299, logistics: 99). Health status was multifactorial assessed: (1) Frequency of musculoskeletal complaints (German Pain Questionnaire). (2) Pain intensity, physical and psychological load [visual analog scales (VAS) 0–100 points]. (3) Occupational moderate-to-vigorous physical activity (MVPA), total MVPA, and sedentary behavior [Global Physical Activity Questionnaire (GPAQ)]. (4) Quality of life [Short Form Health Survey (SF-36)]. Between-group effects were analyzed via one-way ANOVAs with post-hoc Tukey correction.
Results: 308 workers (76.4%) reported at least one musculoskeletal issue. A significant between-group difference was revealed for left shoulder [F(2,40) = 5.40; p = 0.008; ω2 = 0.17], occupational MVPA [F(2,368) = 9.49; p < 0.001; ω2 = 0.04] and total MVPA [F(2,368) = 6.90; p = 0.001; ω2 = 0.03]. Post-hoc tests revealed a difference (p ≤ 0.007) between manufacturing (left shoulder: n = 22; 42.5 ± 24.8; occupational MVPA: n = 219; 6,978 ± 5,137 METs min/week; total MVPA: n = 219; 8,471 ± 5,390 METs min/week) and logistics workers (left shoulder: n = 14; 70.4 ± 26.3 au; occupational MVPA: n = 96; 9,640 ± 4,605 METs min/week; total MVPA: n = 96; 10,856 ± 4,680 METs min/week). No other between-group differences were observed.
Discussion: Variations in health disparities across work conditions were observed. Yet, clear distinctions between work conditions and health outcomes remain a challenge. Effective interventions should be focused on job-specific and personalized health profiles rather than a stratification of work conditions to enhance health, productivity, and workforce sustainability.
1 Introduction
Industrial work is recognized as one of the most physically demanding and mentally challenging occupational sectors (1). Beyond the physical demands, workers are frequently exposed to various occupational hazards, including dust, noise, vibration, awkward postures, repetitive movements, high-force exertion, and high impacts (1–4). These demands affect workers’ health, increasing the risk of illnesses, injuries, and chronic diseases (5, 6). Among these, work-related musculoskeletal disorders remain a major global concern among industrial workers, characterized by high prevalence rates and a tendency for persistent, long-term complaints despite low incidence ratios (7–9). For instance, in 2019, more than 50% of manufacturing workers in the EU reported absences due to work-related musculoskeletal disorders, exceeding those caused by flu-related absences (8, 10). Regarding body zones, the back is the most frequently affected body region, followed by the shoulder/neck, wrist, and knee, underscoring the widespread burden across multiple body regions in this population (7–9).
Addressing these challenges requires a proactive approach to workplace health promotion, which has been shown to enhance worker health and productivity by targeting factors that influence well-being (11, 12). For instance, the early detection of external factors influencing health status is crucial for timely diagnosis and preventive care, leading to long-term benefits (13). According to the International Labor Organization (ILO), global trends such as globalization, technological advancements, demographic shifts, and climate change are reshaping the nature of work (14), further emphasizing the importance of workplaces as a platform for promoting healthy habits from a public health perspective to address these challenges (11).
Despite these efforts, standardized health promotion programs often fail to address the complexity of the industrial work environments. Previous research suggests that a one-size-fits-all approach may be too simplistic, and health interventions should consider the diverse working conditions and health disparities within industrial sectors (15–17). A distinction based on working conditions may be a viable approach for assessing health-related factors. This cross-sectional study aimed to determine whether different working conditions among industrial workers influence health outcomes. These findings intend to guide stakeholders in developing tailored promotion strategies to address the specific needs of the workforce (18).
2 Materials and methods
2.1 Design and ethics
This cross-sectional study investigated industrial workers of a medium-sized steel company in Germany. The local ethics committee approved the study, including all described procedures (SK/AE240527). Before starting data collection, all participants were informed of the study procedure and aim. Then, they voluntarily signed a written informed consent form.
2.2 Population and setting
Data collection for this study was conducted between April 2022 and March 2023 by a team of trained research students led by experienced investigators. The team visited the company and screened potentially eligible workers, independent of any company representatives. None of the team members had any personal relationship with the participants.
The inclusion criteria for this study were: (I) age between 18 and 65 years, and (II) current full-time employment as a rotating shift worker in one of three working conditions. Work conditions are physical, environmental, and organizational factors specific to each department, reflecting the cumulative demands and exposure characteristics. The company was stratified into three conditions: forging (high physical and environmental stress, such as heat and noise), manufacturing (moderate physical demands with repetitive tasks), and logistics (dynamic physical activities like lifting and transporting). Participants were excluded if they worked across multiple conditions or were employed as temporary workers.
A total of 1.116 industrial workers were invited to participate in this study. Within the described company’s stratum, 206 workers were engaged in forging, 577 in manufacturing, and 333 in logistics.
2.3 Procedure
An initial interview was followed by a survey. The procedure encompassed five domains: demographic/anthropometric information, orthopedic complaints, physical activity, quality of life, and assessment of physical and psychological load. Subsequently, all participants provided a paper-and-pencil-based version of the surveys presented in German.
2.4 Measurements and outcomes
2.4.1 Pain frequency and intensity
A Part of the German Pain Questionnaire, a validated and reliable tool for assessing musculoskeletal complaints (19), was used to evaluate the location and frequency of orthopedic issues. Participants were presented with a body diagram and instructed to circle any anatomical regions where they experienced pain. The reported pain locations were sorted into the following regions: neck, upper back, right/left shoulder, right/left elbow, right/left wrist, right/left hand, lower back, hip, right/left knee, and foot. Pain frequency was quantified by counting the total number of anatomical regions with reported pain, providing a cumulative measure of musculoskeletal burden for each participant. In addition, pain intensity of each region was graded using a visual analog scale (VAS), ranging from 0 to 10 cm at regular intervals. The VAS is a recognized and reliable tool for measuring pain intensity (20).
2.4.2 Physical activity
The Global Physical Activity Questionnaire (GPAQ) is one of the World Health Organisation’s (WHO) stepwise approaches to surveillance of non-communicable disease factors that assess physical activity levels using 16 questions (21). The questionnaire can calculate the overall physical activity levels by assessing each domain’s contribution to overall physical activity (22). Total moderate-to-vigorous physical activity (MVPA) was calculated for occupational and total day as Metabolic Equivalent (METs) minutes per week. Therefore, when calculating METs using GPAQ data, moderate activity equals 4 METs and 8 METs to the time spent on vigorous activity (23); additionally, one extra item collected information about the amount of time spent on sedentary behavior (24). The GPAQ is a suitable and acceptable instrument for monitoring physical activity, and its validity and reliability have been assessed in several countries (24).
2.4.3 Quality of life
The Short Form Health Survey 36 (SF-36) is a questionnaire with 36 items that measure health-related quality of life on eight scales. Principal component analysis revealed two dimensions: the physical dimension represented by the Physical Component Summary (PCS) and the mental dimension represented by the Mental Component Summary (MSC) (25). The scores ranged from 0 to 100, with 0 being the worst and 100 being the best health status (26). The German version of the survey is reliable and valid (27).
2.4.4 Physical and psychological load
Subjective physical and psychological loads were assessed using VAS scales, ranging from 0 to 10 cm (0–100 points), to evaluate physical and psychological loads, which have proven helpful in research (28). Participants were asked to rate the perceived demands of their typical workday by answering the following questions (1): Physical load: “On a typical workday, how physically demanding do you perceive your job to be?” (2); Psychological load: “On a typical workday, how mentally demanding do you perceive your job to be?”
2.5 Data processing and statistical analysis
All data were transferred to an Excel spreadsheet (Microsoft Excel for Mac, Version 16.85, Redmond, WA, USA). Normal distribution was verified using a combination of visual inspection and Shapiro–Wilk tests (29). Variance homogeneity was visually checked by plotting residuals and using Levene-Test. Potential between-group effects were analyzed via one-way ANOVA with post-hoc Tukey’s correction for each outcome. Furthermore, effect sizes using omega square were calculated. The level of significance was set at p = 0.05 for all analyses. Statistical analysis was performed with R (version 4.0.3).
3 Results
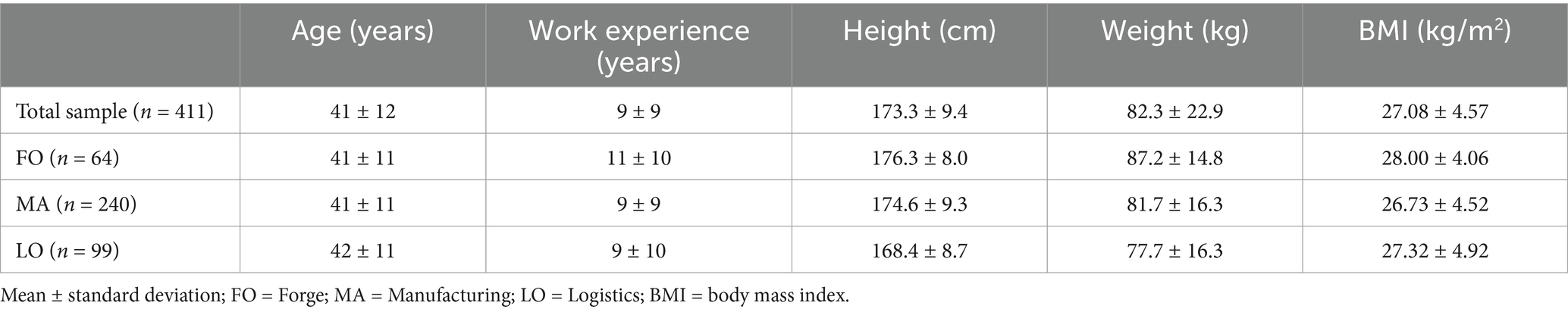
Characteristics of the participants are presented in Table 1. A total of 403 participants completed the interview and questionnaires, giving a response rate of 36%. About 67% of the respondents were men, and 33% were women. The majority (31%) of respondents were aged between 30 and 39 years.
Some workers only partially completed the questionnaire; all available data were included in the analysis. 32 participants did not answer the GPAQ, one did not answer the physical and psychological load, and three did not answer the SF-36.
3.1 Pain frequency and intensity
308 workers (76.4%) reported at least one orthopedic issue, compared to 11% reporting at least four problems. The underlying values are presented in Table 2.
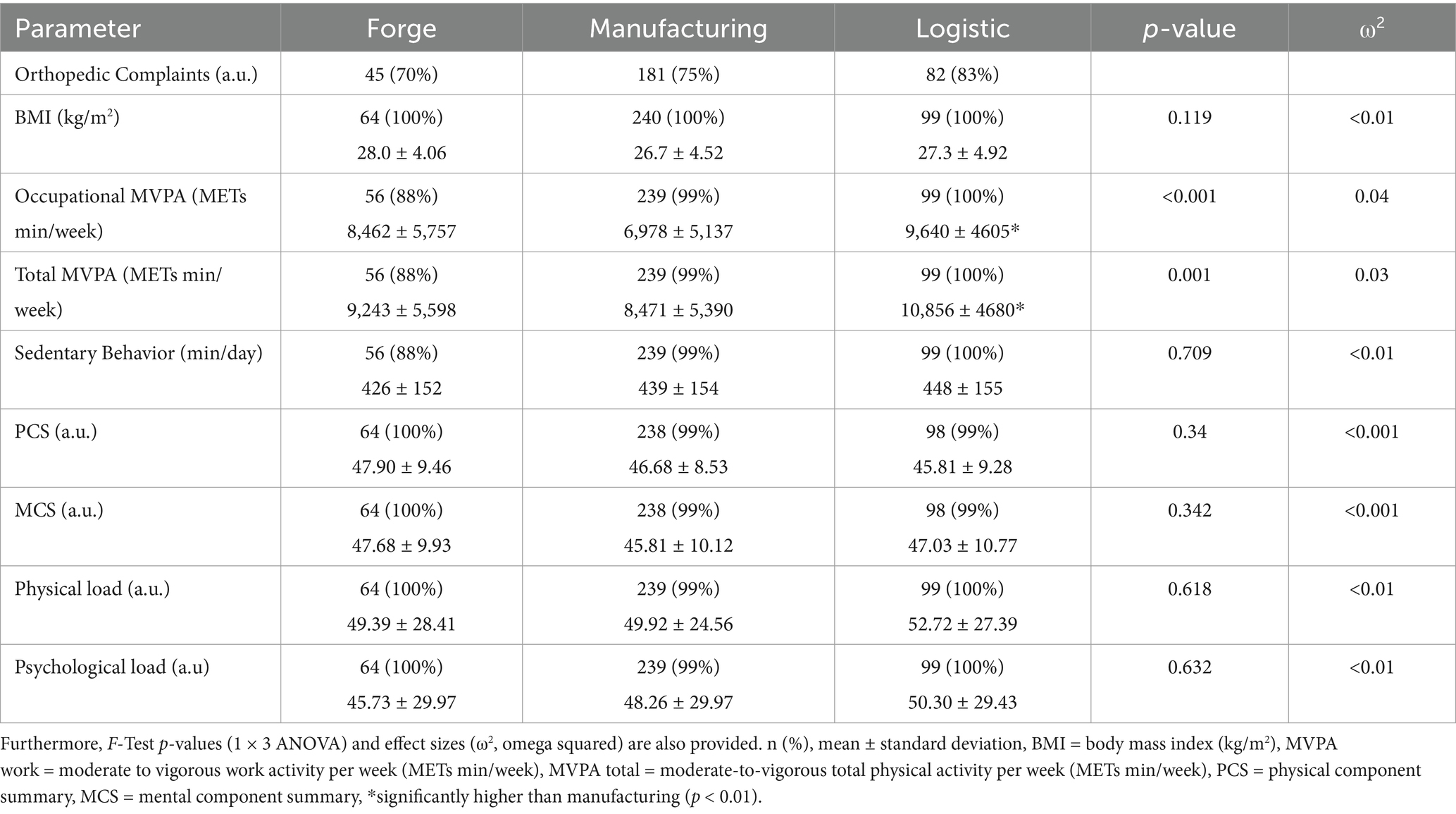
Table 2. Orthopedic complaints, BMI, self-reported physical activity, quality of life, physiological and psychological load of the three different working conditions.
For pain intensity, only the left shoulder showed a significant effect [F(2,40) = 5.40; p = 0.008; ω2 = 0.17]. Post-hoc tests revealed a difference (p = 0.007) between the manufacturing group (n = 22; 42.5 ± 24.8 au) and the logistic group (n = 14; 70.4 ± 26.3 au), but not between the forge group and any other group. For neck [F(2,64) = 0.76; p = 0.472; ω2 = 0.00], upper back [F(2,75) = 1.89; p = 0.158; ω2 = 0.02], shoulder right [F(2,57) = 3.16; p = 0.05; ω2 = 0.07], elbow right [F(2,31) = 3.18; p = 0.055; ω2 = 0.11], elbow left [F(2,3) = 6.58; p = 0.08; ω2 = 0.65], wrist right [F(2,47) = 0.87; p = 0.426; ω2 = 0.00], wrist left [F(2,32) = 2.35; p = 0.112; ω2 = 0.07], low back [F(2,188) = 0.98; p = 0.378; ω2 = 0.00], knee right [F(2,42) = 3.18; p = 0.052; ω2 = 0.09], knee left [F(2,32) = 2.70; p = 0.083; ω2 = 0.09], foot [F(2,18) = 0.82; p = 0.457; ω2 = 0.00], no group effect was found. Furthermore, the orthopedic frequencies of the right hand, left hand, and hip were not represented in all groups. Therefore, no further analysis was performed. The values are shown in Figure 1.
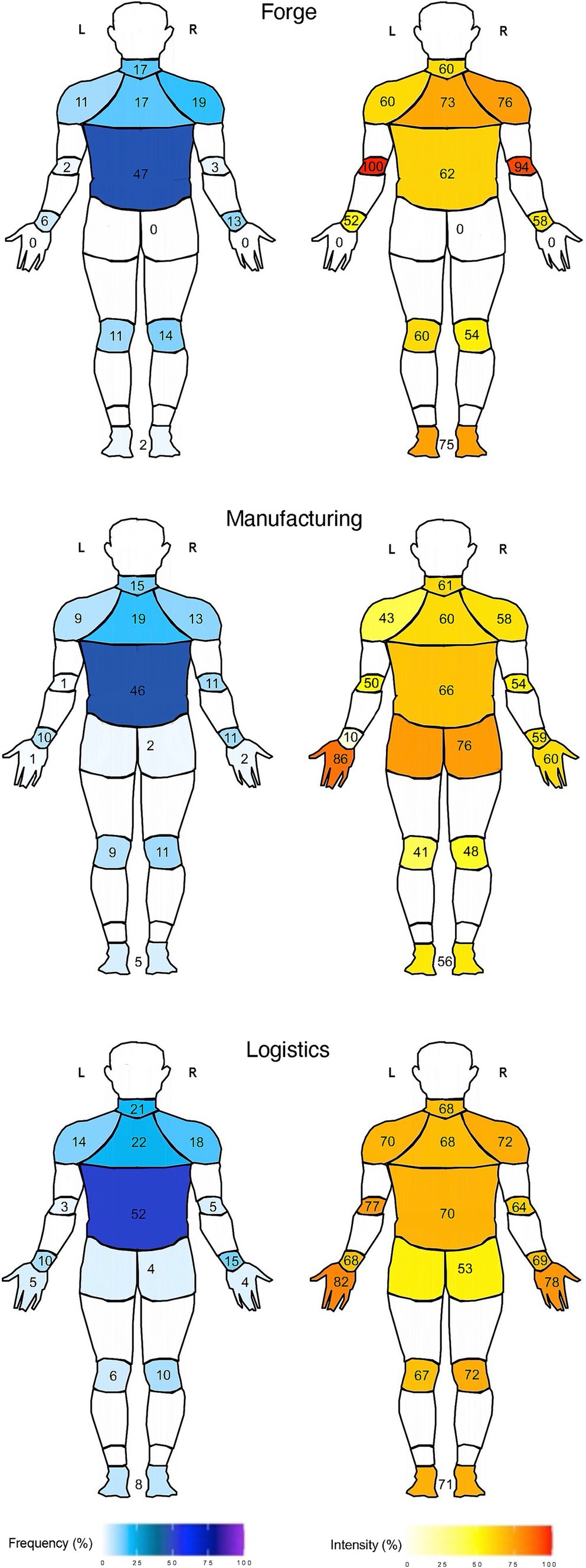
Figure 1. Frequency and pain-intensity of orthopedic complaints of industrial workers in the work conditions forge, manufacturing, and logistics [dorsal view (87)].
3.2 Physical activity
Occupational MVPA [F(2,368) = 9.49; p < 0.001; ω2 = 0.04] and total MVPA [F(2,368) = 6.90; p = 0.001; ω2 = 0.03] showed a significant between-group difference. Post-hoc testing revealed a significant difference (p ≤ 0.001) between the manufacturing group (n = 219; 6.978 ± 5.137 METs min/week) and the logistic group (n = 96; 9.640 ± 4.605 METs min/week) for occupational MVPA, and between the manufacturing group (n = 219; 8.471 ± 5.390 METs min/week) and the logistic group (n = 96; 10.856 ± 4.680 METs min/week) for total MVPA. No significant group difference was found for sedentary behavior [F(2,368) = 0.34; p = 0.709; ω2 = 0.00].
3.3 Body composition
No significant group differences were detected in BMI [F(2,400) = 2.14; p = 0.119; ω2 < 0.00].
3.4 Quality of life
There were no significant group differences in MCS [F(2,397) = 1.08; p = 0.342; ω2 < 0.00] or PCS [F(2,397) = 1.08; p = 0.34; ω2 < 0.00].
3.5 Perceived load
No significant differences were observed in physical load [F(2,399) = 0.48; p = 0.618; ω2 < 0.00] or psychological load [F(2,399) = 0.46; p = 0.632; ω2 = 0.00].
4 Discussion
This cross-sectional study aimed to examine whether different industrial work conditions influence the health status of industrial workers. The main findings are (I) a high number of orthopedic complaints with high variability in every group and one significant difference in orthopedic complaints between the manufacturing and logistic conditions; (II) a significant difference between the manufacturing and logistic conditions on physical activity; and (III) no significant differences across all other collected data.
4.1 Orthopedic complaints
The literature highlights the significant burden of musculoskeletal disorders in industrial settings (30, 31), driven by various risk factors for their development (8). Our findings align with this; over 76% of the analyzed workers reported at least one orthopedic issue. This high prevalence reflects similar trends in the literature (7–9) and underscores the critical need for targeted interventions within this population. Research indicates that the interaction of biomechanical and psychosocial risk factors increases the likelihood of developing musculoskeletal disorders (32, 33).
Low back pain emerged as the most frequently reported issue among participants in our study, aligning with prior research (5, 7, 8, 10, 34). Meta-analyses revealed a mean prevalence between 37 to 51% (7–9), which is consistent with our findings. The strong correlation between workload and the prevalence of low back pain (35, 36) further highlights the need to address these factors through targeted interventions. Additionally, individual factors such as obesity, educational level, and sex have been identified as contributors to a high prevalence of musculoskeletal disorders in the lower back (7).
In addition to the lower back, a systematic review and meta-analysis identified the shoulder, neck, and wrist as the most prevalent sites for musculoskeletal disorders, with a 12-month prevalence ranging from 42 to 60% (8). Our findings align closely with these observations, highlighting similar patterns of affected body regions. In contrast, another review emphasized that the back, wrist, and elbow are the most common anatomical regions of musculoskeletal disorders (34). Furthermore, a systematic review and meta-analysis of construction workers identified the lower back, knee, shoulder, and wrist as the most affected body regions (9). Lower limb musculoskeletal disorders were reported to be less prevalent than back or upper limb, as documented in the literature (7, 8), which aligns with our findings. These variations in the literature reflect the high variability in musculoskeletal disorders, influenced by individual characteristics and work-related factors.
Notably, our study identified significant differences in pain intensity between manufacturing and logistics workers, particularly in the left shoulder. Although the specific cause for this unilateral pain remains unclear, it is plausible that task-specific physical demands or individual biomechanical factors may play a role. Other authors have recognized that there are different tasks and organizations in manufacturing than in logistics, where logistics workers must frequently bend, twist, and stand for a long period of time (37). Both conditions involve repetitive tasks with low load and high work pace (38), and physically demanding activities such as heavy lifting (38, 39). These factors are established contributors to musculoskeletal disorders (8, 31).
However, these findings underscore the complexity of addressing musculoskeletal disorders in industrial settings, where workers’ tasks and conditions can differ significantly. Therefore, the observed pain in the left shoulder might be attributed to a combination of individual and job-specific factors. The high variability in orthopedic complaints and adverse working conditions pose challenges to the development of generalized interventions. As a result, translating findings into effective solutions requires a focus on tailored strategies that consider individual worker characteristics and specific job demands (40, 41).
Beyond the physical health implications, musculoskeletal disorders affect workability (6, 32), particularly in the low back area (42), prolonged absences (8), and substantial financial costs (39). They are also one of the leading causes of permanent incapacity (43), productivity loss, and early retirement (11).
Interventions such as ergonomic adaptations and innovative technologies, including robots and exoskeletons (44), might help prevent work-related musculoskeletal disorders by alleviating the physical strain associated with industrial tasks. These approaches are particularly relevant in countries experiencing demographic shifts that challenge the sustainability of physically demanding jobs (3) and human decline in musculoskeletal mass, leading to reduced adaptation strategies (7).
4.2 Body composition
A higher prevalence of overweight and obesity among industrial workers than among the general population is known (30). With a BMI of approximately 27 kg/m2, our findings fall within the WHO classification of overweight (45). However, we did not find a significant difference between the conditions, but there was a high variance in the data.
Generally, an increased BMI and musculoskeletal disorders are associated with each other (7), and both negatively impact work-related outcomes (30). Additionally, obesity is related to musculoskeletal pain (46). Furthermore, obesity with fat depots is recognized as a significant pro-inflammatory factor in modern society that contributes to modern diseases such as cancer, metabolic disorders, cardiovascular diseases, and dementia (47). Prevention and, if reasonable, therapy are necessary to improve health and increase healthspan, ideally targeting multiple health factors such as musculoskeletal disorders and obesity (48).
4.3 Physical activity
Promoting physical activity in the workplace has been a well-established health strategy for decades (49). According to prevailing guidelines, optimal physical activity is at least 600 METs min/week (50). Individuals falling below this WHO recommendations threshold may be classified as physically inactive (22). In our study, the manufacturing group exhibited the lowest level of occupational MVPA, at 6.978 METs min/week; only four individuals were labeled as physically inactive. However, self-reported data may lead to overestimation of physical activity, particularly in urban areas (51). In addition, participants appeared to overestimate their MVPA and underestimate their sedentary behavior when using the GPAQ, suggesting that the results should be interpreted with caution (24).
Occupational physical activity exceeds the recommended threshold 11-fold and can be considered a physical health paradox (52–54). While the positive association between leisure-time physical activity, orthopedic issues, and cardiovascular disease mortality is well documented (53), occupational physical activity did not have a beneficial association with mortality or orthopedic complaints (53, 54). On the contrary, high levels of occupational physical activity increase the risk for adverse health outcomes, mortality, and orthopedic complaints (53, 54). Consequently, promoting decreased physical activity among industrial workers could improve workplace health. While leisure-time physical activity is important for overall health (55), our study found that non-occupational activity accounted for only a modest difference in total physical activity. Given the potential health risks of occupational physical activity, it is essential to consider individual lifestyle factors.
Regarding sedentary behavior, no differences were observed across work conditions, which ranged between 426 and 448 min. Despite high physical activity levels, participants sit for over 7.5 h daily, exceeding the recommended limit for high sedentary behavior (56). However, sitting for long periods may be a relevant health factor, including posture during sitting from an evolutionary perspective (57).
A notable difference in the manufacturing and logistics groups was observed for both occupational MVPA and total MVPA, with differences of over 660 min and approximately 600 min, respectively. To contextualize these differences, the WHO recommends at least 150 to 300 min of moderate physical activity per week (58). However, the data showed that job profiles and individual lifestyle factors must be considered when planning and implementing workplace health promotion, especially for those with high physical activity.
4.4 Quality of life
Previous research has established a positive correlation between factors such as workability, nutritional intake, and sleep quality on quality of life (59–61). While these studies highlighted the influence of various factors on quality of life, our study found no significant differences across work conditions. However, our mental and physical scores were lower than those found in other studies with comparable populations (59), and similar to the data from Lim and colleagues (61) for night-shift workers, who comprised most of our participants.
Moreover, our quality of life scores were lower in terms of MCS (50.04) than those of patients with low back pain or disc herniation but higher in PCS (44.51) (62). Compared to adults in Germany, our results were lower in both categories (MCS: 51.40; PCS:49.30) (63). Orthopedic complaints could contribute to PCS scores across a range of patients with low back pain to general adults in Germany, but this remains speculative.
Of all participants, 56% had a mental and physical score below 50, which matches the percentage reported by Ghasemi and colleagues (64) (59%). Others have found that one-third of construction workers experience a mental health condition, resulting in high losses in work time and high economic costs (65). The number of sick days taken due to mental health concerns in the workplace has increased, which is in line with the rising trend of mental illnesses (66, 67). In particular, shift workers are affected by this trend, with a higher prevalence of poor mental health, particularly depressive symptoms (68, 69). Workers’ exposure to psychosocial hazards is influenced by the interplay between job demands and resources (70), whereas job control may be a possible influencing factor in the manufacturing context (40).
4.5 Practical applications
This study offers valuable insights and practical implications for workplace health promotion. Our analysis confirmed the diversity of job profiles among industrial workers. The nature of these job profiles is influenced by factors such as work environment, activities, and human factors (71, 72). While ergonomic concerns, particularly orthopedic issues, have historically been the focus of workplace health initiatives, our findings underscore the critical need to address psychosocial factors (35). Unpredictable work hours, for example, hinder workers’ access to medical care, contributing to undetected health conditions, poor overall health, and an increased risk of workplace injuries (73). These challenges negatively affect worker safety and contribute to organizational issues, such as productivity, absenteeism, and rising healthcare costs (14).
Companies strive to meet the increasing expectations of their workers by implementing progressively more comprehensive measures to address these demands (74). This reinforces the importance of aligning health promotion strategies with specific needs and expectations of the workforce. In this regard, recent reviews highlighted that workplace interventions, particularly in high-risk industries, are associated with a measurable reduction in musculoskeletal disorders (31) and stress-related absenteeism (68). Studies have demonstrated that health promotion programs reduce the prevalence of physical ailments like low back pain and alleviate mental stress, contributing to a healthier workforce (32, 75). Besides ergonomics, education is essential and plays a vital role in managing health by equipping workers with skills to adopt a healthier behavior (76).
To address these challenges, practical interventions should adopt a dual approach that combines preventive and rehabilitative strategies tailored to the unique worker and individual and job-specific needs. Strategies such as structured duty schedules, modified working postures, job rotation strategies, and targeted training programs are required to manage workplace health issues effectively (3, 77, 78). Given the substantial variability in job demands and individual health conditions, frameworks such as the Goldilocks principle (79), which seeks to balance workload demands, and the IGLO framework (80), which targets health promotion at the individual, group, leader, and organizational levels, offer valuable guidance in this regard.
Technological advances can further enhance these strategies. For instance, advanced monitoring technologies, such as wearable devices, allow real-time monitoring of individual health status (81), provide precise data (82), and enable tailored intervention recommendations (83). Moreover, after identifying specific job profiles and individual health conditions, e-health platforms offer a promising solution for delivering accessible interventions that accommodate irregular work among industrial shift workers (84). These tools can facilitate personalized health management, improve resource accessibility, and foster proactive health behaviors (85).
Future workplace interventions should systematically integrate these frameworks and technologies to classify health states and develop tailored health-management strategies. For example, task rotation schemes (86) customized with individual psychosocial support (67) can help workers meet their roles’ physical and mental demands. The cross-sector applications of such interventions could further validate their effectiveness and adaptability across various industries.
4.6 Limitations
Nonetheless, this study had several limitations. A cross-sectional design restricts the ability to infer causality from observed relationships between work conditions and health outcomes. Furthermore, the participants were drawn from a single mid-sized steel company, which restricts the generalizability of our findings to other industrial sectors and broader occupational populations. Potential confounding variables, such as age, sex, and lifestyle habits, were not comprehensively accounted for and may influence the observed relationships. Additionally, the response rate introduces a possible bias that could affect the validity of the findings.
Another notable limitation is the lack of longitudinal data, which prevents the tracking of health outcomes and evaluating their progression. Future research should prioritize longitudinal designs to assess the durability of health improvements and their influence on organizational outcomes. Moreover, the literature has reported a higher prevalence of musculoskeletal disorders in certain body regions when specific tools are used (8). This highlights the potential variability in reported outcomes based on the methodology employed. Similarly, reliance on self-defined musculoskeletal disorders has been associated with higher incidence rates (7), indicating the need for standardized definitions and assessments in future studies.
In terms of methodology, while we utilized personal interviews to address the inherent challenges of self-reported data, this approach remains subject to recall and reporting bias. Complementing self-reported measures with objective health data or workplace observations in future studies could enhance the reliability of findings.
For broader applicability, systematic reviews comparing interventions across different cultural and regulatory settings could provide valuable insights into a global adaptation of workplace health strategies. Future research should explore how parameters at the individual level, such as physical activity, impact health-related outcomes (55), particularly under more homogenous or task-specific work conditions. This highlights the potential impact of such interventions, particularly in shaping specific job profiles and addressing work-related health issues. Additionally, emphasis should be placed on fostering adequate work conditions within a broader health-related system and ensuring the sustainability and scalability of these approaches.
5 Conclusion
This study provides valuable insights into working conditions and health status of industrial shift workers. We observed a high prevalence of orthopedic complaints, low quality of life scores, and significant differences in physical activity across work conditions. However, the variability within each work condition suggests that more than stratifying workers based solely on work conditions may be required for effective workplace health interventions. While clear distinctions between work conditions and health outcomes remain challenging, our findings emphasize the importance for a comprehensive approach to workplace health promotion. Successful preventive and rehabilitative programs should focus on an individual level by implementing job-specific profiles and regular health assessments, including adequate screening and monitoring procedures among industrial shift workers. This approach can potentially improve workers’ health, enhance productivity, and support a more sustainable workforce.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by local ethical committee of the University of Wuppertal. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SJ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. LR: Data curation, Formal analysis, Software, Visualization, Writing – review & editing. CB: Writing – review & editing. DN: Writing – review & editing. LH: Writing – review & editing. JF: Project administration, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank the company Knipex Gustav Putsch KG for their contribution to this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
VAS, Visual analogue scale; GPAQ, Global physical activity questionnaire; WHO, World Health Organisation; MVPA, Moderate-to-vigorous physical activity; MET, Metabolic Equivalent; SF-36, Short Form Health Survey-36; PCS, Physical Component Summary; MCS, Mental Component Summary; BMI, Body Mass Index.
References
1. Ranasinghe, U, Tang, LM, Harris, C, Li, W, Montayre, J, de Almeida, NA, et al. A systematic review on workplace health and safety of ageing construction workers. Saf Sci. (2023) 167:106276. doi: 10.1016/j.ssci.2023.106276
2. Xu, X, Zhong, M, Wan, J, Yi, M, and Gao, T. Health monitoring and Management for Manufacturing Workers in adverse working conditions. J Med Syst. (2016) 40:222. doi: 10.1007/s10916-016-0584-4
3. Anagha, R. A review on ergonomic risk factors causing musculoskeletal disorders among construction workers. Int J Eng Res. (2020) V9:887. doi: 10.17577/ijertv9is060887
4. Javanmardi, S, Rappelt, L, Heinke, L, Niederer, D, Zemke, JA, Freiwald, J, et al. Impact of work pace on cardiorespiratory outcomes, perceived effort and carried load in industrial workers: a randomised cross-over trial. Occup Environ Med. (2024) 81:456–61. doi: 10.1136/oemed-2024-109563
5. Abrar, A, Cheema, KJ, Saif, S, and Mahmood, A. Health status assessment of workers during construction phase of highway rehabilitation projects around Lahore, Pakistan. J Occup Health. (2017) 59:74–80. doi: 10.1539/joh.16-0123-FS
6. Nguyen, TT, Nguyen, HV, Vu, HM, Chiu, RG, Nguyen, QN, Nguyen, TTP, et al. Factors correlated with neuropathic pain among industrial workers in Vietnam: a multi-site cross-sectional study. Front Public Health. (2023) 11:1007483. doi: 10.3389/fpubh.2023.1007483
7. He, X, Xiao, B, Wu, J, Chen, C, Li, W, and Yan, M. Prevalence of work-related musculoskeletal disorders among workers in the automobile manufacturing industry in China: a systematic review and meta-analysis. BMC Public Health. (2023) 23:2042. doi: 10.1186/s12889-023-16896-x
8. Govaerts, R, Tassignon, B, Ghillebert, J, Serrien, B, De Bock, S, Ampe, T, et al. Prevalence and incidence of work-related musculoskeletal disorders in secondary industries of 21st century Europe: a systematic review and meta-analysis. BMC Musculoskelet Disord. (2021) 22:751. doi: 10.1186/s12891-021-04615-9
9. Umer, W, Antwi-Afari, MF, Li, H, Szeto, GPY, and Wong, AYL. The prevalence of musculoskeletal symptoms in the construction industry: a systematic review and meta-analysis. Int Arch Occup Environ Health. (2018) 91:125–44. doi: 10.1007/s00420-017-1273-4
10. Cimarras-Otal, C, Marcen-Cinca, N, Rabal-Pelay, J, Lacrcel-Tejero, B, Alczar-Crevilln, A, Villalba-Ruete, J, et al. Adapted exercises versus general exercise recommendations on chronic low back pain in industrial workers: a randomized control pilot study. Work. (2020) 67:733–40. doi: 10.3233/WOR-203322
11. Andersen, LL, Persson, R, Jakobsen, MD, and Sundstrup, E. Psychosocial effects of workplace physical exercise among workers with chronic pain: randomized controlled trial. Medicine (Baltimore). (2017) 96:e5709. doi: 10.1097/MD.0000000000005709
12. Moreira-Silva, I, Santos, R, Abreu, S, and Mota, J. The effect of a physical activity program on decreasing physical disability indicated by musculoskeletal pain and related symptoms among workers: a pilot study. Int J Occup Saf Ergon. (2014) 20:55–64. doi: 10.1080/10803548.2014.11077028
13. de Walque, D, Chukwuma, A, Ayivi-Guedehoussou, N, and Koshkakaryan, M. Invitations, incentives, and conditions: a randomized evaluation of demand-side interventions for health screenings. Soc Sci Med. (2022) 296:114763. doi: 10.1016/j.socscimed.2022.114763
14. Sorensen, G, Dennerlein, JT, Peters, SE, Sabbath, EL, Kelly, EL, and Wagner, GR. The future of research on work, safety, health and wellbeing: a guiding conceptual framework. Soc Sci Med. (2021) 269:113593. doi: 10.1016/j.socscimed.2020.113593
15. Aikas, A, Absetz, P, Hirvensalo, M, and Pronk, N. Eight-year health risks trend analysis of a comprehensive workplace health promotion program. Int J Environ Res Public Health. (2020) 17:9426. doi: 10.3390/ijerph17249426
16. Pega, F, Momen, NC, Abubakar, AHA, Al-Emam, R, Hassan, MN, Howard, J, et al. Monitoring workers' health: focus on rights, determinants, and equity. Lancet. (2023) 402:1306–8. doi: 10.1016/S0140-6736(23)02049-4
17. Cui, P, Zhao, H, Dong, Z, Ju, X, Zou, P, and Zhou, S. Modeling the occupational health risk of workers caused by environmental release during the production of PC components. Front Public Health. (2022) 10:1076461. doi: 10.3389/fpubh.2022.1076461
18. Cancelliere, C, Cassidy, JD, Ammendolia, C, and Cote, P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health. (2011) 11:395. doi: 10.1186/1471-2458-11-395
19. Nagel, B, Gerbershagen, HU, Lindena, G, and Pfingsten, M. Development and evaluation of the multidimensional German pain questionnaire. Schmerz. (2002) 16:263–70. doi: 10.1007/s00482-002-0162-1
20. Gallagher, EJ, Bijur, PE, Latimer, C, and Silver, W. Reliability and validity of a visual analog scale for acute abdominal pain in the ED. Am J Emerg Med. (2002) 20:287–90. doi: 10.1053/ajem.2002.33778
21. WHO (2021). Global physical activity questionnaire (GPAQ). Available at: https://www.who.int/publications/m/item/global-physical-activity-questionnaire (Accessed June 10, 2024).
22. Guthold, R, Louazani, SA, Riley, LM, Cowan, MJ, Bovet, P, Damasceno, A, et al. Physical activity in 22 African countries: results from the World Health Organization STEPwise approach to chronic disease risk factor surveillance. Am J Prev Med. (2011) 41:52–60. doi: 10.1016/j.amepre.2011.03.008
23. Chu, AH, Ng, SH, Koh, D, and Muller-Riemenschneider, F. Reliability and validity of the self- and interviewer-administered versions of the global physical activity questionnaire (GPAQ). PLoS One. (2015) 10:e0136944. doi: 10.1371/journal.pone.0136944
24. Keating, XD, Zhou, K, Liu, X, Hodges, M, Liu, J, Guan, J, et al. Reliability and concurrent validity of global physical activity questionnaire (GPAQ): a systematic review. Int J Environ Res Public Health. (2019) 16:4128. doi: 10.3390/ijerph16214128
25. Lins, L, and Carvalho, FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. (2016) 4:2050312116671725. doi: 10.1177/2050312116671725
26. Barranco-Ruiz, Y, Paz-Viteri, S, and Villa-Gonzalez, E. Dance fitness classes improve the health-related quality of life in sedentary women. Int J Environ Res Public Health. (2020) 17:3771. doi: 10.3390/ijerph17113771
27. Bullinger, M. German translation and psychometric testing of the SF-36 health survey: preliminary results from the IQOLA project. International quality of life assessment. Soc Sci Med. (1995) 41:1359–66. doi: 10.1016/0277-9536(95)00115-N
28. Lesage, FX, and Berjot, S. Validity of occupational stress assessment using a visual analogue scale. Occup Med (Lond). (2011) 61:434–6. doi: 10.1093/occmed/kqr037
29. Mohd Razali, N, and Yap, B. Power comparisons of Shapiro-Wilk, Kolmogorov-Smirnov, Lilliefors and Anderson-Darling tests. J Stat Model Anal. (2011) 2:21–33.
30. Viester, L, Verhagen, EA, Bongers, PM, and van der Beek, AJ. The effect of a health promotion intervention for construction workers on work-related outcomes: results from a randomized controlled trial. Int Arch Occup Environ Health. (2015) 88:789–98. doi: 10.1007/s00420-014-1007-9
31. Sundstrup, E, Seeberg, KGV, Bengtsen, E, and Andersen, LL. A systematic review of workplace interventions to rehabilitate musculoskeletal disorders among employees with physical demanding work. J Occup Rehabil. (2020) 30:588–612. doi: 10.1007/s10926-020-09879-x
32. Blafoss, R, Aagaard, P, Clausen, T, and Andersen, LL. Effects of consecutive workdays and days off on low back pain, fatigue and stress: prospective cohort study among warehouse and construction workers. Occup Environ Med. (2023) 80:650–8. doi: 10.1136/oemed-2023-109043
33. Chaiklieng, S, and Suggaravetsiri, P. Low Back pain (LBP) incidence, ergonomics risk and Workers' characteristics in relations to LBP in electronics assembly manufacturing. Indian J Occup Environ Med. (2020) 24:183–7. doi: 10.4103/ijoem.IJOEM_4_20
34. Wang, D, Dai, F, and Ning, X. Risk assessment of work-related musculoskeletal disorders in construction: state-of-the-art review. J Constr Eng Manag. (2015) 141:979. doi: 10.1061/(ASCE)CO.1943-7862.0000979
35. Bezzina, A, Austin, E, Nguyen, H, and James, C. Workplace psychosocial factors and their association with musculoskeletal disorders: a systematic review of longitudinal studies. Workplace Health Saf. (2023) 71:578–88. doi: 10.1177/21650799231193578
36. Nappo, N. Is there an association between working conditions and health? An analysis of the sixth European working conditions survey data. PLoS One. (2019) 14:e0211294. doi: 10.1371/journal.pone.0211294
37. Gajšek, B, Ðukić, G, Butlewski, M, Opetuk, T, Cajner, H, and Kač, SM. The impact of the applied technology on health and productivity in manual "picker-to-part" systems. Work. (2020) 65:525–36. doi: 10.3233/WOR-203107
38. Santos, J, Baptista, JS, Monteiro, PRR, Miguel, AS, Santos, R, and Vaz, MAP. The influence of task design on upper limb muscles fatigue during low-load repetitive work: a systematic review. Int J Ind Ergon. (2016) 52:78–91. doi: 10.1016/j.ergon.2015.09.010
39. Antwi-Afari, MF, Li, H, Edwards, DJ, Pärn, EA, Seo, J, and Wong, AYL. Biomechanical analysis of risk factors for work-related musculoskeletal disorders during repetitive lifting task in construction workers. Autom Constr. (2017) 83:41–7. doi: 10.1016/j.autcon.2017.07.007
40. Rosen, PH, and Wischniewski, S. Scoping review on job control and occupational health in the manufacturing context. Int J Adv Manuf Technol. (2019) 102:2285–96. doi: 10.1007/s00170-018-03271-z
41. Tersa-Miralles, C, Bravo, C, Bellon, F, Pastells-Peiró, R, Rubinat Arnaldo, E, and Rubí-Carnacea, F. Effectiveness of workplace exercise interventions in the treatment of musculoskeletal disorders in office workers: a systematic review. BMJ Open. (2022) 12:e054288. doi: 10.1136/bmjopen-2021-054288
42. Arora, NK, Donath, L, Owen, PJ, Miller, CT, Saueressig, T, Winter, F, et al. The impact of exercise prescription variables on intervention outcomes in musculoskeletal pain: an umbrella review of systematic reviews. Sports Med. (2024) 54:711–25. doi: 10.1007/s40279-023-01966-2
43. Bevan, S. Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Pract Res Clin Rheumatol. (2015) 29:356–73. doi: 10.1016/j.berh.2015.08.002
44. Coccia, A, Capodaglio, EM, Amitrano, F, Gabba, V, Panigazzi, M, Pagano, G, et al. Biomechanical effects of using a passive exoskeleton for the upper limb in industrial manufacturing activities: a pilot study. Sensors (Basel). (2024) 24:1445. doi: 10.3390/s24051445
45. Purnell, JQ. Definitions, classification, and epidemiology of obesity In: KR Feingold, B Anawalt, MR Blackman, A Boyce, G Chrousos, and E Corpas, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc. (2000)
46. Vincent, HK, Adams, MC, Vincent, KR, and Hurley, RW. Musculoskeletal pain, fear avoidance behaviors, and functional decline in obesity: potential interventions to manage pain and maintain function. Reg Anesth Pain Med. (2013) 38:481–91. doi: 10.1097/AAP.0000000000000013
47. Trumble, BC, and Finch, CE. The Exposome in human evolution: from dust to diesel. Q Rev Biol. (2019) 94:333–94. doi: 10.1086/706768
48. Wasser, JG, Vasilopoulos, T, Zdziarski, LA, and Vincent, HK. Exercise benefits for chronic low Back pain in overweight and obese individuals. PM R. (2017) 9:181–92. doi: 10.1016/j.pmrj.2016.06.019
49. Sertel, M, Üçsular, FD, and Uğurlu, Ü. The effects of worksite exercises on physical capabilities of workers in an industry of a developing country: a randomized controlled study. Isokinet Exerc Sci. (2016) 24:247–55. doi: 10.3233/IES-160624
50. Sjogaard, G, Mann, S, Jensen, JSD, Oestergaard, AS, and Dalager, T. The elixir of muscle activity and kinesiology in a health perspective: evidence of worksite tailored exercise training alleviating muscle disorders. J Electromyogr Kinesiol. (2021) 61:102600. doi: 10.1016/j.jelekin.2021.102600
51. Lim, S, Wyker, B, Bartley, K, and Eisenhower, D. Measurement error of self-reported physical activity levels in New York City: assessment and correction. Am J Epidemiol. (2015) 181:648–55. doi: 10.1093/aje/kwu470
52. Holtermann, A, Coenen, P, and Krause, N. The paradoxical health effects of occupational versus leisure-time physical activity In: T Theorell, editor. Handbook of socioeconomic determinants of occupational health, Handbook Series in Occupational Health Sciences. Cham: Springer International Publishing (2020). 241–67.
53. Cillekens, B, Huysmans, MA, Holtermann, A, van Mechelen, W, Straker, L, Krause, N, et al. Physical activity at work may not be health enhancing. A systematic review with meta-analysis on the association between occupational physical activity and cardiovascular disease mortality covering 23 studies with 655 892 participants. Scand J Work Environ Health. (2022) 48:86–98. doi: 10.5271/sjweh.3993
54. Coenen, P, Huysmans, MA, Holtermann, A, Krause, N, van Mechelen, W, Straker, LM, et al. Do highly physically active workers die early? A systematic review with meta-analysis of data from 193 696 participants. Br J Sports Med. (2018) 52:1320–6. doi: 10.1136/bjsports-2017-098540
55. Amatori, S, Gobbi, E, Sisti, D, Pivato, G, Giombini, G, Rombaldoni, R, et al. Physical activity, musculoskeletal disorders, burnout, and work engagement: a cross-sectional study on Italian white-collar employees. Front Public Health. (2024) 12:1375817. doi: 10.3389/fpubh.2024.1375817
56. Jelsma, JGM, Gale, J, Loyen, A, van Nassau, F, Bauman, A, and van der Ploeg, HP. Time trends between 2002 and 2017 in correlates of self-reported sitting time in European adults. PLoS One. (2019) 14:e0225228. doi: 10.1371/journal.pone.0225228
57. Raichlen, DA, Pontzer, H, Zderic, TW, Harris, JA, Mabulla, AZP, Hamilton, MT, et al. Sitting, squatting, and the evolutionary biology of human inactivity. Proc Natl Acad Sci USA. (2020) 117:7115–21. doi: 10.1073/pnas.1911868117
58. Bull, FC, Al-Ansari, SS, Biddle, S, Borodulin, K, Buman, MP, Cardon, G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
59. Tavakoli-Fard, N, Mortazavi, SA, Kuhpayehzadeh, J, and Nojomi, M. Quality of life, work ability and other important indicators of women's occupational health. Int J Occup Med Environ Health. (2016) 29:77–84. doi: 10.13075/ijomeh.1896.00329
60. Manoogian, ENC, Zadourian, A, Lo, HC, Gutierrez, NR, Shoghi, A, Rosander, A, et al. Feasibility of time-restricted eating and impacts on cardiometabolic health in 24-h shift workers: the healthy heroes randomized control trial. Cell Metab. (2022) 34:1442–1456.e7. doi: 10.1016/j.cmet.2022.08.018. 1
61. Lim, YC, Hoe, VCW, Darus, A, and Bhoo-Pathy, N. Association between night-shift work, sleep quality and health-related quality of life: a cross-sectional study among manufacturing workers in a middle-income setting. BMJ Open. (2020) 10:e034455. doi: 10.1136/bmjopen-2019-034455
62. Morfeld, M, Kirchberger, I, and Bullinger, M. (2011). SF-36 Fragebogen zum Gesundheitszustand: Deutsche Version des Short Form-36 Health Survey.
63. Ellert, U, and Kurth, BM. Health related quality of life in adults in Germany: results of the German health interview and examination survey for adults (DEGS1). Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. (2013) 56:643–9. doi: 10.1007/s00103-013-1700-y
64. Ghasemi, SR, Khezeli, M, Rajabi-Gilan, N, Koulani, M, Moloudi-Safa, N, Hemati, A, et al. Sleep quality and health-related quality of life in Workers of Kermanshah Industrial Town: a correlation study. Indian J Occup Environ Med. (2020) 24:72–7. doi: 10.4103/ijoem.IJOEM_219_19
65. Burki, T. Mental health in the construction industry. Lancet Psychiatry. (2018) 5:303. doi: 10.1016/S2215-0366(18)30108-1
66. Holmlund, L, Tinnerholm Ljungberg, H, Bultmann, U, Holmgren, K, and Bjork, BE. Exploring reasons for sick leave due to common mental disorders from the perspective of employees and managers - what has gender got to do with it? Int J Qual Stud Health Well-being. (2022) 17:2054081. doi: 10.1080/17482631.2022.2054081
67. Rakhshani, T, Saeedi, P, Kashfi, SM, Bazrafkan, L, Kamyab, A, and Khani, JA. The relationship between spiritual health, quality of life, stress, anxiety and depression in working women. Front Public Health. (2024) 12:1366230. doi: 10.3389/fpubh.2024.1366230
68. Torquati, L, Mielke, GI, Brown, WJ, Burton, NW, and Kolbe-Alexander, TL. Shift work and poor mental health: a meta-analysis of longitudinal studies. Am J Public Health. (2019) 109:e13–20. doi: 10.2105/AJPH.2019.305278
69. Yan, T, Ji, F, Bi, M, Wang, H, Cui, X, Liu, B, et al. Occupational stress and associated risk factors among 13,867 industrial workers in China. Front Public Health. (2022) 10:945902. doi: 10.3389/fpubh.2022.945902
70. Amoadu, M, Ansah, EW, and Sarfo, JO. Influence of psychosocial safety climate on occupational health and safety: a scoping review. BMC Public Health. (2023) 23:1344. doi: 10.1186/s12889-023-16246-x
71. de Negreiros, AWFTRW, Rodrigues da Silva, P, Arezes, PMFM, Dangelino, R, and Padula, RS. Manufacturing assembly serial and cells layouts impact on rest breaks and workers’ health. Int J Ind Ergon. (2019) 70:22–7. doi: 10.1016/j.ergon.2019.01.005
72. Katiraee, N, Calzavara, M, Finco, S, Battini, D, and Battaïa, O. Consideration of workers’ differences in production systems modelling and design: state of the art and directions for future research. Int J Prod Res. (2021) 59:3237–68. doi: 10.1080/00207543.2021.1884766
73. Howard, ME, Wolkow, AP, Wilkinson, V, Swann, P, Jordan, AS, O'Donoghue, FJ, et al. Feasibility of cardiovascular risk and sleep health screening in the transport industry. J Transp Health. (2020) 18:100878. doi: 10.1016/j.jth.2020.100878
74. Foncubierta-Rodríguez, MJ, Poza-Méndez, M, and Holgado-Herrero, M. Workplace health promotion programs: the role of compliance with workers' expectations, the reputation and the productivity of the company. J Saf Res. (2024) 89:56–63. doi: 10.1016/j.jsr.2024.02.008
75. Kaveh, MH, Mehrazin, F, Cousins, R, and Mokarami, H. Effectiveness of a transactional model-based education programme for enhancing stress-coping skills in industrial workers: a randomized controlled trial. Sci Rep. (2023) 13:5076. doi: 10.1038/s41598-023-32230-2
76. Schaller, A, Stassen, G, Baulig, L, and Lange, M. Physical activity interventions in workplace health promotion: objectives, related outcomes, and consideration of the setting—a scoping review of reviews. Front Public Health. (2024) 12:1353119. doi: 10.3389/fpubh.2024.1353119
77. Cheng, S, and Wang, Y. The impact of perceived environmental competitiveness on employee mental health: a moderated mediation model of job crafting and work–family conflict. Frontiers. Public Health. (2024) 12:2024-August-16;12. doi: 10.3389/fpubh.2024.1433215
78. Wei, W, and Li, L. The impact of artificial intelligence on the mental health of manufacturing workers: the mediating role of overtime work and the work environment. Frontiers. Public Health. (2022) 10:10lish. doi: 10.3389/fpubh.2022.862407
79. Straker, L, Mathiassen, SE, and Holtermann, A. The 'Goldilocks Principle': designing physical activity at work to be 'just right' for promoting health. Br J Sports Med. (2018) 52:818–9. doi: 10.1136/bjsports-2017-097765
80. Gupta, N, Wahlin-Jacobsen, CD, Abildgaard, JS, Henriksen, LN, Nielsen, K, and Holtermann, A. Effectiveness of a participatory physical and psychosocial intervention to balance the demands and resources of industrial workers: a cluster-randomized controlled trial. Scand J Work Environ Health. (2018) 44:58–68. doi: 10.5271/sjweh.3689
81. Zhang, X, Schall, MC Jr, Chen, H, Gallagher, S, Davis, GA, and Sesek, R. Manufacturing worker perceptions of using wearable inertial sensors for multiple work shifts. Appl Ergon. (2022) 98:103579. doi: 10.1016/j.apergo.2021.103579
82. Zhang, Y, Weaver, RG, Armstrong, B, Burkart, S, Zhang, S, and Beets, MW. Validity of wrist-worn photoplethysmography devices to measure heart rate: a systematic review and meta-analysis. J Sports Sci. (2020) 38:2021–34. doi: 10.1080/02640414.2020.1767348
83. Murray, JM, Magee, M, Giliberto, ES, Booker, LA, Tucker, AJ, Galaska, B, et al. Mobile app for personalized sleep-wake management for shift workers: a user testing trial. Digit Health. (2023) 9:20552076231165972. doi: 10.1177/20552076231165972
84. Miguel, C, Amarnath, A, Akhtar, A, Malik, A, Baranyi, G, Barbui, C, et al. Universal, selective and indicated interventions for supporting mental health at the workplace: an umbrella review of meta-analyses. Occup Environ Med. (2023) 80:225–36. doi: 10.1136/oemed-2022-108698
85. Zahrt, OH, Evans, K, Murnane, E, Santoro, E, Baiocchi, M, Landay, J, et al. Effects of wearable fitness trackers and activity adequacy mindsets on affect, behavior, and health: longitudinal randomized controlled trial. J Med Internet Res. (2023) 25:e40529. doi: 10.2196/40529
86. Padula, RS, Comper, MLC, Sparer, EH, and Dennerlein, JT. Job rotation designed to prevent musculoskeletal disorders and control risk in manufacturing industries: a systematic review. Appl Ergon. (2017) 58:386–97. doi: 10.1016/j.apergo.2016.07.018
Keywords: workplace health promotion, occupational health, occupational hazards, musculoskeletal disorders, job-profile
Citation: Javanmardi S, Rappelt L, Baumgart C, Niederer D, Heinke L and Freiwald J (2025) Work conditions and determinants of health status among industrial shift workers: a cross-sectional study. Front. Public Health. 12:1489178. doi: 10.3389/fpubh.2024.1489178
Edited by:
Karen Søgaard, University of Southern Denmark, DenmarkReviewed by:
Stefano Amatori, University of eCampus, ItalyEbrahim Darvishi, Kurdistan University of Medical Sciences, Iran
Philippe Gorce, International Institute of Biomechanics and Occupational Ergonomics, France
Copyright © 2025 Javanmardi, Rappelt, Baumgart, Niederer, Heinke and Freiwald. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sasha Javanmardi, cy5qYXZhbm1hcmRpQHVuaS13dXBwZXJ0YWwuZGU=
 Sasha Javanmardi
Sasha Javanmardi Ludwig Rappelt
Ludwig Rappelt Christian Baumgart
Christian Baumgart Daniel Niederer
Daniel Niederer Lars Heinke
Lars Heinke Jürgen Freiwald
Jürgen Freiwald