- 1Washington DC VA Medical Center, Washington, DC, United States
- 2Biomedical Informatics Center, The George Washington University, Washington, DC, United States
- 3VA Connecticut Healthcare System, West Haven, CT, United States
- 4Yale School of Medicine, Yale University, New Haven, CT, United States
Objectives: This study aims to analyze differences between lesbian, gay, bisexual, transgender, and queer (LGBTQ+) and non-LGBTQ+ Veterans with post-traumatic stress disorder (PTSD) in terms of demographics, comorbidities, and medical care usage, including differences by sex of record, including separate analyses for transgender and non-transgender Veterans.
Methods: Chi-square, t-test, ANOVA Welch one-way testing, and absolute standardized difference analyses were conducted on a cohort of 277,539 Veterans diagnosed with PTSD.
Results: The study found significant differences, particularly concerning positive LGBTQ+ status and sex of record. There were significant differences found in age, marital status, and medical care usage, as well as pain, mental health, and substance use disorder diagnoses. Differences in having experienced military sexual trauma, crime, or maltreatment were especially significant, with increased percentages among LGBTQ+ individuals, and sex of record females. In separate analyses, there were similar differences among transgender and non-transgender Veterans, with similar increased risks for sex of record females.
Conclusion: Our findings suggest an intersectionality of LGBTQ+ status and sex of record in the context of PTSD. These findings may help guide future research, policy, and interventions.
Introduction
Post-traumatic stress disorder (PTSD) is a condition people may develop after experiencing or witnessing a life-threatening event (1). It is defined as “exposure to actual or threatened death, serious injury, or sexual violence” through direct experience, witnessing, or finding that a close associate, friend, or family member has experienced this type of event (2). It is characterized by recurrent, intrusive memories and dreams, dissociative reactions such as flashbacks, psychological distress from cues that are reminiscent of the event, and other attributes (2). PTSD can last for months or years with lasting symptoms.
Approximately 12 million people in the United States experience PTSD each year; this includes 4% of men and 8% of women (3). Individuals who have experienced a traumatic brain injury (TBI) are at greater risk, especially military personnel (4). PTSD is also associated with other mental health disorders, particularly depression, anxiety (5), and substance abuse disorders (5–7). Substance abuse co-occurs in approximately 40% of individuals with PTSD (8–10). Pain is also associated with PTSD (11–13), including in Veterans with PTSD (14). Veterans often experience a higher rate of PTSD, particularly among women, and rates vary by deployment (15, 16). Even when combat is a factor, PTSD can be a complex condition, affected by other traumatic experiences, particularly for women (17–19).
Previous research has examined PTSD with respect to sexual orientation and gender identity. Lesbian, gay, bisexual, transgender, and queer (LGBTQ+) individuals are 2.2 times more likely to experience PTSD than their heterosexual/cisgender peers (20), with rates among lesbian/bisexual/gay individuals as high as 47.6%, and rates among transgender individuals ranging from 17.8 to 42.0% (21–26). LGBTQ+ individuals have an increased prevalence of PTSD-connected events such as physical and sexual assault, and child abuse (27). Transgender individuals are 2.52 times more likely, and bisexual individuals are 2.44 times more likely, to experience PTSD than other LGBTQ+ subgroups (20).
Studies addressing PTSD in Veterans in terms of LGBTQ+ status indicate PTSD may be more prevalent among LGBTQ+ Veterans than non-LGBTQ+ Veterans (28, 29). LGBTQ+ Veterans experience several kinds of traumatic and stressful events, including assault, verbal abuse, discrimination, social isolation, shame, and microaggressions such as slights and inaccurate pronoun usage (30). PTSD is more prevalent among transgender Veterans than matched non-transgender Veterans (31, 32). Transgender Veterans are also more likely to experience PTSD as well as depression, suicidality, serious mental illness, military sexual trauma (MST), incarceration, and homelessness (32). Veterans with minoritized sexual orientation are 2.35 times more likely to have “likely PTSD” (33). PTSD, depression, anxiety, binge eating, problematic anger, multiple somatic symptoms, and insomnia are more prevalent among lesbian, gay, and bisexual Veterans and service members (34).
Less is known about the prevalence and effects of PTSD among LGBTQ+ Veterans who are women. The risk for PTSD among women LGBTQ+ Veterans may be multiplicative, meaning the combined effect of sexual orientation and gender is larger than the product of their individual effects. Gorman et al. (35) found that, while sexual minority female Veterans have comparable PTSD rates as their heterosexual peers, deployment-related stressors were less likely to be associated with PTSD. While there are some previous studies on transgender Veterans with PTSD, there are knowledge gaps regarding transgender Veterans compared to other LGBTQ+ and non-LGBTQ+ individuals with PTSD. Data that can potentially address these and other knowledge gaps can be found in the U.S. Department of Veterans Affairs (VA) electronic health records (EHRs).
In this study of Veterans with PTSD, our objectives were (1) to analyze and describe the differences between LGBTQ+ and non-LGBTQ+ Veterans in terms of demographics, comorbidities, and medical care usage; and (2) to analyze differences between male and female LGBTQ+ and non-LGBTQ+ Veterans using sex of record. Because sex of record values in VA EHR data indicate birth sex and not gender or gender identity and noting that the experience of transgender Veterans with PTSD may be different, we also conducted the same analyses for transgender Veterans in the cohort. The specific gender identities and sexual orientations of the transgender Veterans in the cohort are unknown. We included selected comorbidities in order to gain greater insight in terms of previous research. We hypothesized there would be differences between LGBTQ+ Veterans and non-LGBTQ+ Veterans, as well as between male and female sex of record, and transgender Veterans vs. non-transgender Veterans. These results could help characterize the PTSD experience for all Veterans and possibly provide insight for future interventions.
Methods
Data/cohort
Veterans Affairs EHR records, stored within the VA central data warehouse (CDW), served as the data source for this cross-sectional study, and we accessed these data within the secure VA Informatics and Computing Infrastructure (VINCI) research platform (36).
Using an established cohort from a previous study (37) that classified patients as LGBTQ+ or non-LGBTQ+, we identified those who had received two or more PTSD diagnoses (ICD-10 F43.1) in the 5 years between 1 January 2017 and 31 December 2021 in outpatient care encounters. We limited the PTSD diagnosis count to a maximum of one per day, to ensure individual diagnoses were at least 1 day apart. Transgender Veterans (with two or more PTSD diagnoses) were identified in an additional process, using both natural language processing (NLP) (37) and ICD codes to determine transgender status.
Covariates
The baseline covariates were demographics (age at first diagnosis of PTSD, race, ethnicity, marital status, and sex of record) and selected comorbidities of interest based on the International Classification of Diseases (ICD) 9th and 10th revision codes, or clinical structural data element [pain diagnosis, alcohol and drug use, mental illness (e.g., bipolar disorder), traumatic brain injury (TBI), violent crime/maltreatment, and MST], and medical care usage (i.e., outpatient visits). ICD codes identifying comorbid diagnoses were previously established by the VA Musculoskeletal Diagnosis Cohort (38), Headache Centers of Excellence (39), the VA Northeast Program Evaluation Center, and Kaiser Permanente, with the exception of violent crime/maltreatment. In the case of violent crime/maltreatment, we used ICD-9 codes 995.54, 995.80–85, E960-E966, E968-, and E969-and ICD-10 codes X92-X99; Y00-Y04, Y08-Y09, Z04.41, Z65.4, Z91.41-, and T74-. For MST, we used EHR flag administrative data.
Statistical analysis
For this descriptive study, chi-square testing was applied to the categorical covariates, t-test was applied to continuous covariates in comparing two samples, and ANOVA Welch one-way testing was applied to continuous covariates in comparing four samples to detect statistically significant differences by (1) LGBTQ+ status, (2) LGBTQ+ status and sex of record, (3) transgender status, and (4) transgender status and sex of record. As an additional significance test, we calculated absolute standardized difference (ASD). An ASD > 10% indicates an imbalance between two groups (40, 41) considered clinically meaningful. A difference with a p-value of <0.05 and ASD of >10 was considered significant. Statistical analyses were conducted with SAS, version 9.4., and Python (version 3.6.10) for ASD.
Results
There were 277,539 patients with PTSD between calendar years 2017 and 2021, of whom 76,080 (27.4%) were LGBTQ+, 56,986 (20.5%) were female, 220,553 (79.5%) were male, and 17,278 (6.2%) were transgender Veterans.
LGBTQ+ status in Veterans with PTSD
There are several significant statistical differences between LGBTQ+ Veterans compared to non-LGBTQ+ Veterans (Table 1). LGBTQ+ Veterans compared to non-LGBTQ+ Veterans were less likely to be married (39.7% vs. 49.5%) and more likely to be female (32.9% vs. 15.9%) and have a diagnosis for drug use disorder (36.7% vs. 29.8%), bipolar disorder (22.1% vs. 14.8%), general anxiety disorder (20.6% vs. 16.2%), and major depressive disorder (67.0% vs. 57.9%). LGBTQ+ Veterans were also more likely to be victims of violent crime/maltreatment (10.4% vs. 5.4%), and MST (40.4% vs. 23.2%). LGBTQ+ Veterans also had more outpatient care encounters on average.
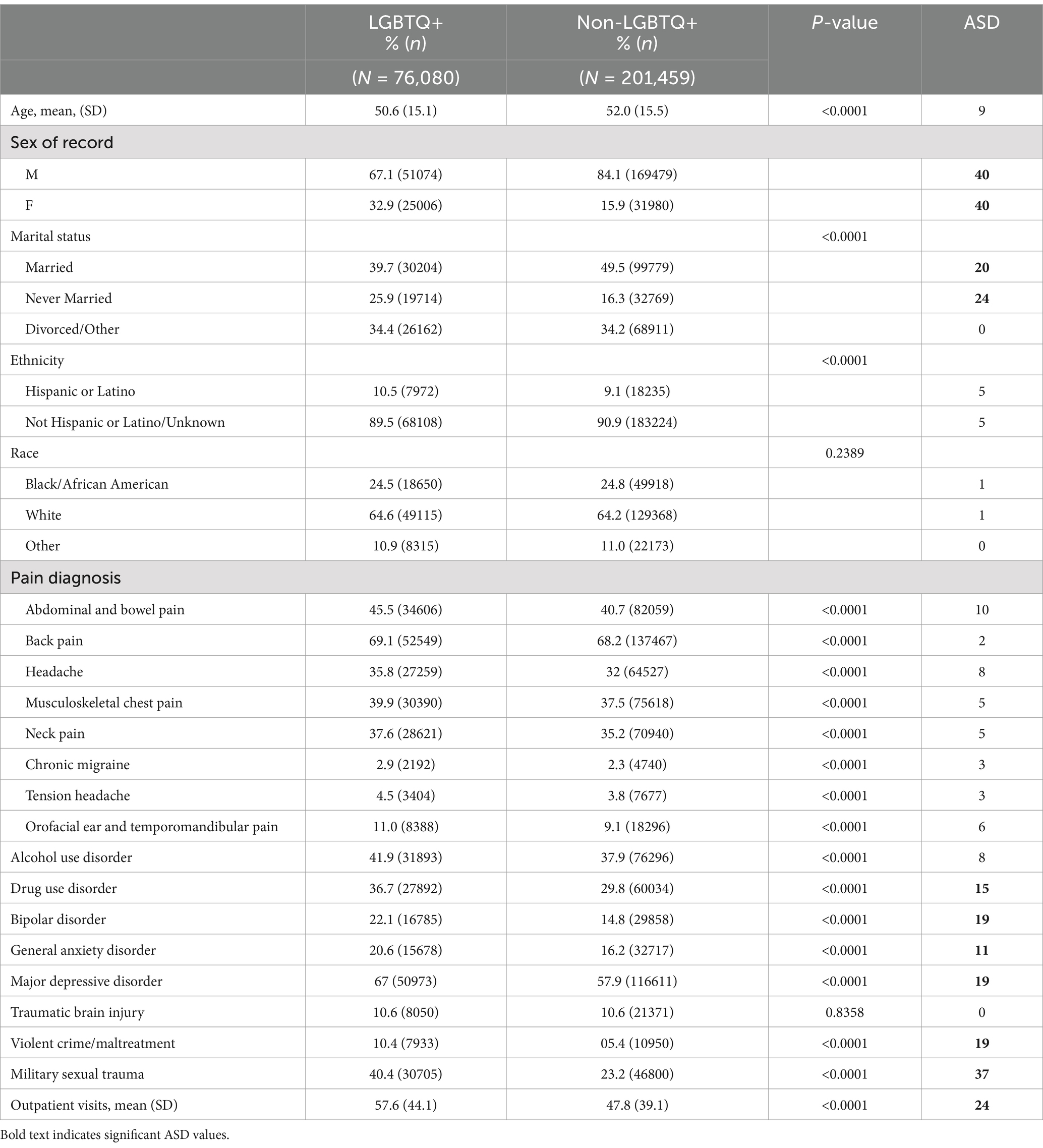
Table 1. Demographics, comorbidities, and mean outpatient encounters by LGBTQ+ Veterans with PTSD vs. non-LGBTQ+ Veterans with PTSD.
LGBTQ+ status and sex of record in Veterans with PTSD
Among LGBTQ+ Veterans, females compared to males were on average significantly younger (44.9 vs. 53.4 years old), less likely to be married (29.5% vs. 44.7%), more likely to be Black/African American (28.1% vs. 22.8%), to have had a diagnosis for abdominal and bowel pain (49.4% vs. 43.6%), headache (41.8% vs. 32.9%), chronic migraine (5.0% vs. 1.8%), orofacial ear and temporomandibular pain (13.7% vs. 9.7%), and to have experienced violent crime/maltreatment (17.5% vs. 6.9%) or MST (69.1% vs. 26.3%). Male LGBTQ+ Veterans with PTSD were more likely to be white (66.9% vs. 59.8%) and have a diagnosis of alcohol (47% vs. 31.5%) or drug use disorders (40.6% vs. 28.6%) (Table 2). Similar results were observed among non-LGBTQ+ Veterans, with a few notable exceptions. Non-LGBTQ+ female Veterans were more likely to have a diagnosis of tension headache (5.9% vs. 3.4%), bipolar disorder (20.2% vs. 13.8%), general anxiety disorder (21.1% vs. 15.3%), and major depressive disorder (67.6% vs. 56.1%) than non-LGBTQ+ male Veterans. Non-LGBTQ+ male Veterans were more likely to have a diagnosis for TBI (11.4% vs. 6.6%) than non-LGBTQ+ female Veterans.
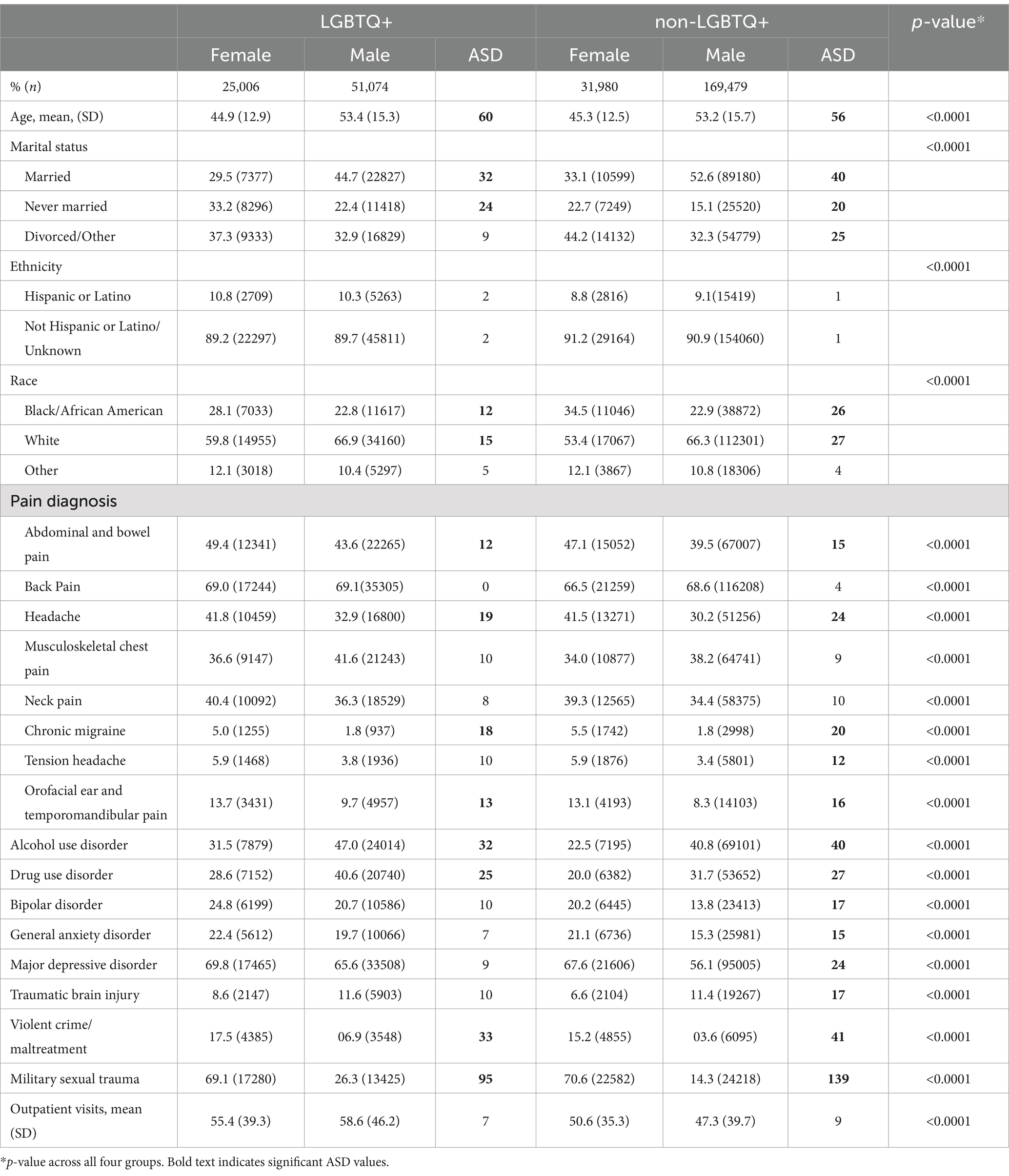
Table 2. Demographics, comorbidities, and mean outpatient encounters by LGBTQ+ status and sex of record of Veterans with PTSD.
Transgender status in Veterans with PTSD
Transgender Veterans with PTSD compared to non-transgender Veterans with PTSD were younger (49.7 vs. 51.7 years old), less likely to be married (37.2% vs. 47.5%), more likely to have had a diagnosis of bipolar disorder (22.7% vs. 16.4%), major depressive disorder (67.2% vs. 59.9%), drug use disorder (38.2% vs. 31.3%), and to have experienced violent crime/maltreatment (10.8% vs. 6.5%), and MST (40% vs. 27.1%) (Table 3). They also had higher outpatient visits (62.5 vs. 49.7).
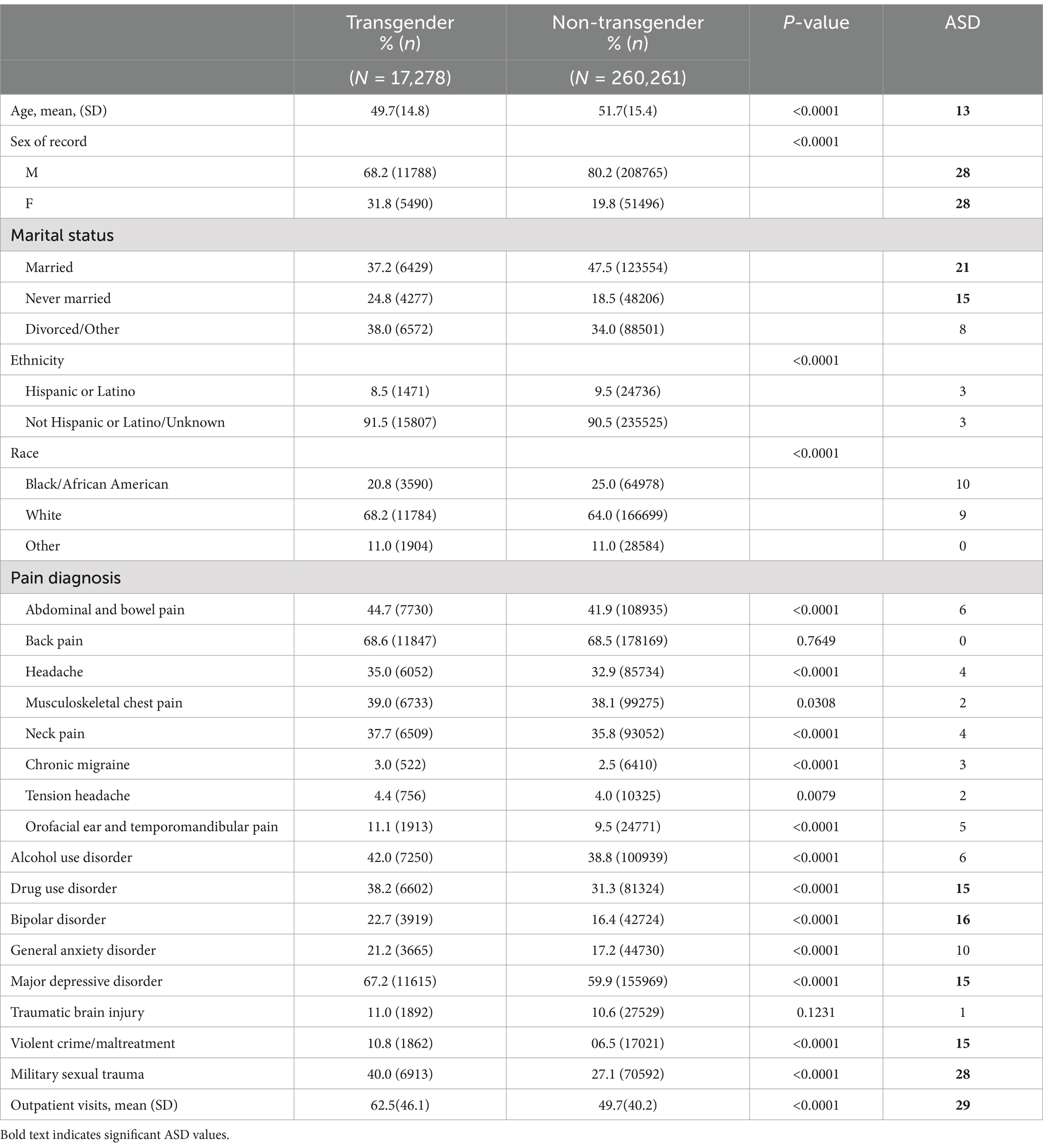
Table 3. Demographics, comorbidities, and mean outpatient encounters by transgender Veterans with PTSD vs. non-transgender Veterans with PTSD.
Transgender status and sex of record in Veterans with PTSD
Veterans recorded as female sex of record had significantly higher percentages of abdominal and bowel pain, headache, chronic migraine, and orofacial ear and temporomandibular pain diagnoses in both transgender and non-transgender groups (Table 4). Transgender female sex of record Veterans had a significantly higher percentage of neck pain (41.9% vs. 35.7%) than transgender male sex of record Veterans. Non-transgender female sex of record Veterans had a significantly higher percentage of tension headaches (5.9% vs. 3.5%) than non-transgender male sex of record Veterans. Female sex of record also had higher percentages of violent crime/maltreatment and MST in both transgender and non-transgender groups. For alcohol and drug use disorder, male sex of record had higher percentages in both transgender and non-transgender groups. Transgender Veterans had more outpatient visits than their non-transgender counterparts, but among transgender Veterans, there was no difference by sex of record. A higher percentage of Veterans recorded as male sex of record in both transgender and non-transgender groups were married. Non-transgender male Veterans were more likely to have a diagnosis of TBI (11.4% vs. 7.3%) than non-transgender female Veterans.
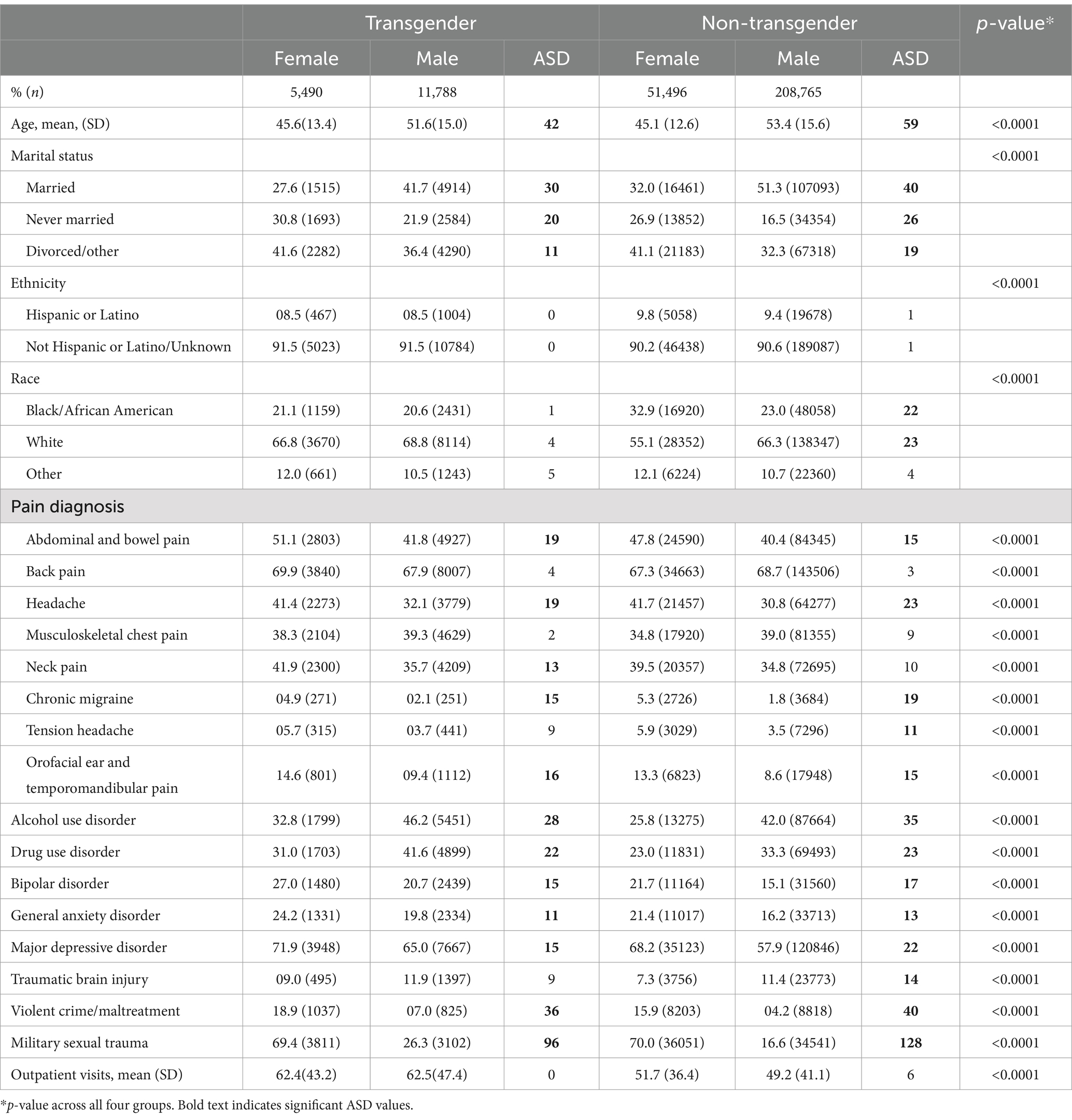
Table 4. Demographics, comorbidities, and mean outpatient encounters by transgender status and sex of record of Veterans with PTSD.
Discussion
In a large diverse nationwide cohort of Veterans in care, more LGBTQ+ Veterans were diagnosed with PTSD (36.6%) than non-LGBTQ+ Veterans (21.1%). The findings from this study suggest there are demographics, comorbidities, and outpatient care differences between LGBTQ+ Veterans with PTSD and non-LGBTQ+ Veterans with PTSD. The results also suggest an intersectionality of LGBTQ+ status and sex of record in the context of PTSD.
The study’s findings both align with and add to the literature. Overall, these results suggest that issues known to be generally associated with PTSD (i.e., pain, mental health issues, and substance abuse) may be accentuated in some Veteran populations, and while there may be differences among groups for some forms of pain in the wider population, this does not fully explain our study’s findings. For example, rates in transition from episodic to chronic migraine in men and women vary by study (42), with one study (43) finding that the percentage in men was slightly higher (5.4% vs. 4.4%). Individuals with female sex of record in our study reported significantly more chronic migraine. Abdominal/belly pain is associated with PTSD symptom severity and depression in Veterans (13) which may to a degree correlate with the results from our study. As in previous studies (17–19), our study’s findings also suggest that PTSD for some groups may be grounded in aspects outside of combat. Webermann et al. (44) found that one in three women Veterans reports MST and that MST was associated with PTSD. Our findings illustrated a striking difference at the intersection of LGBTQ+ status and sex of record; females compared to males were 3-fold more likely to have MST. Studies on marital status and PTSD have yielded mixed results (45); however, the support of a partner has been shown to mitigate PTSD (46), and in this study, there were significant differences in marital status. TBI was not statistically significant, except in comparing non-transgender male and female sex of record, and non-LGBTQ+ male and female sex of record.
These findings further characterize the PTSD experience for all Veterans and may help guide future research and policy. The findings also suggest tailoring treatment by sex of record, gender identity, sexual orientation minority status, and other factors may be of value and possibly enhance outcomes. Overall, more research is warranted.
Limitations
Our study has some limitations. Patients were largely male who were in care and may not be generalizable. Because this study relied on EHR data, it was reliant on correct data entry in the recording process. The natural language process could have misclassified Veterans, but this misclassification would have been small and non-differential (37). Additionally, we are unable to identify the sexual orientations and gender identities of transgender Veterans. Transgender status was paired with sex of record, which does not accurately represent the gender identities of these Veterans for multiple reasons. Within the VA, Veterans are permitted to update their sex of record to better align with their gender identity, though this practice is not adopted by all transgender Veterans. We acknowledge that having complete information on the sexual orientations and gender identities of transgender Veterans could provide more detailed data on specific differences within this group. Identifying transgender Veterans in EHR is problematic regardless of the EHR data source (47). Moreover, we did not separate the subgroups of L, G, and B which may have additional informative differences, but that level of granularity is beyond the scope of this study.
Future work
Future studies will address interventions, and policies regarding PTSD, LGBTQ+ status, and sex of record.
Conclusion
Veterans, as well as LGBTQ+ individuals and women, are disproportionately at risk for PTSD. In this descriptive statistical analysis, we compared Veterans who had been diagnosed as having PTSD, by LGBTQ+ status and sex of record, with separate analyses specific to transgender status. We found significant differences at the intersection of LGBTQ+ status and sex of record. These findings can potentially enhance future interventions, policy, and research.
Data availability statement
The data analyzed in this study are subject to the following licenses/restrictions: the data include protected health information (PHI), therefore, they are not publicly available.
Ethics statement
The studies involving humans were approved by The Washington DC VA Medical Center (Washington, DC) and West Haven VA Medical Center (West Haven, CT). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
TEW: Conceptualization, Data curation, Investigation, Formal analysis, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. KG: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. JG: Funding acquisition, Project administration, Writing – review & editing. CB: Supervision, Writing – review & editing. MS: Data curation, Writing – review & editing. JO’L: Data curation, Writing – review & editing. QT-Z: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by VA Health Research and Development Services (grant IIR 18-035, I01HX002679) and NIH National Center for Advancing Translational Sciences (grant UL1TR001876).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. National Center for PTSD. PTSD Basics: Department of Veterans Affairs; Veterans Health Administration. Available at: https://www.ptsd.va.gov/understand/what/ptsd_basics.asp (accessed August 13, 2024)
2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA, USA: American Psychiatric Association Publishing (2022).
3. National Center for PTSD. How Common Is PTSD in Adults?: U.S. Department of Veterans Affairs; Veterans Health Administration. Available at: https://www.ptsd.va.gov/understand/common/common_adults.asp#:~:text=About%206%20out%20of%20every,have%20gone%20through%20a%20trauma (accessed August 13, 2024)
4. Loignon, A, Ouellet, MC, and Belleville, G. A systematic review and Meta-analysis on PTSD following TBI among military/veteran and civilian populations. J Head Trauma Rehabil. (2020) 35:E21–35. doi: 10.1097/HTR.0000000000000514
5. Brady, KT, Killeen, TK, Brewerton, T, and Lucerini, S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. (2000) 61:22–32.
6. Driessen, M, Schulte, S, Luedecke, C, Schaefer, I, Sutmann, F, Ohlmeier, M, et al. Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcohol Clin Exp Res. (2008) 32:481–8. doi: 10.1111/j.1530-0277.2007.00591.x
7. Mills, KL, Teesson, M, Ross, J, and Peters, L. Trauma, PTSD, and substance use disorders: findings from the Australian National Survey of mental health and well-being. Am J Psychiatry. (2006) 163:652–8. doi: 10.1176/ajp.2006.163.4.652
8. Pietrzak, RH, Goldstein, RB, Southwick, SM, and Grant, BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from wave 2 of the National Epidemiologic Survey on alcohol and related conditions. J Anxiety Disord. (2011) 25:456–65. doi: 10.1016/j.janxdis.2010.11.010
9. Blanco, C, Xu, Y, Brady, K, Perez-Fuentes, G, Okuda, M, and Wang, S. Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: results from National Epidemiological Survey on alcohol and related conditions. Drug Alcohol Depend. (2013) 132:630–8. doi: 10.1016/j.drugalcdep.2013.04.016
10. Petrakis, IL, Rosenheck, R, and Desai, R. Substance use comorbidity among veterans with posttraumatic stress disorder and other psychiatric illness. Am J Addict. (2011) 20:185–9. doi: 10.1111/j.1521-0391.2011.00126.x
11. Fishbain, DA, Pulikal, A, Lewis, JE, and Gao, J. Chronic pain types differ in their reported prevalence of post-traumatic stress disorder (PTSD) and there is consistent evidence that chronic pain is associated with PTSD: an evidence-based structured systematic review. Pain Med. (2017) 18:711–35. doi: 10.1093/pm/pnw065
12. Siqveland, J, Hussain, A, Lindstrom, JC, Ruud, T, and Hauff, E. Prevalence of posttraumatic stress disorder in persons with chronic pain: a meta-analysis. Front Psych. (2017) 8:164. doi: 10.3389/fpsyt.2017.00164
13. Kearney, DJ, Kamp, KJ, Storms, M, and Simpson, TL. Prevalence of gastrointestinal symptoms and irritable bowel syndrome among individuals with symptomatic posttraumatic stress disorder. J Clin Gastroenterol. (2022) 56:592–6. doi: 10.1097/MCG.0000000000001670
14. Benedict, TM, Keenan, PG, Nitz, AJ, and Moeller-Bertram, T. Post-traumatic stress disorder symptoms contribute to worse pain and health outcomes in veterans with PTSD compared to those without: a systematic review with Meta-analysis. Mil Med. (2020) 185:e1481–91. doi: 10.1093/milmed/usaa052
15. Xue, C, Ge, Y, Tang, B, Liu, Y, Kang, P, Wang, M, et al. A meta-analysis of risk factors for combat-related PTSD among military personnel and veterans. PLoS One. (2015) 10:e0120270. doi: 10.1371/journal.pone.0120270
16. National Center for PTSD. How Common is PTSD in Veterans?. Available at: https://www.ptsd.va.gov/understand/common/common_veterans.asp (accessed August 13, 2024)
17. Zerach, G. The contribution of childhood adversity and potentially traumatic events during military service to PTSD and complex PTSD symptoms among Israeli women veterans. Psychol Trauma. (2023) 66:S179. doi: 10.1192/j.eurpsy.2023.430
18. Zerach, G, and Levi-Belz, Y. Exposure to potentially morally injurious events, disruption in assumptive world, moral injury symptoms, and psychological distress among Israeli female veterans. Stress Health. (2022) 39:651–62. doi: 10.1002/smi.3214
19. Fontana, A, Rosenheck, R, and Desai, R. Female veterans of Iraq and Afghanistan seeking care from VA specialized PTSD programs: comparison with male veterans and female war zone veterans of previous eras. J Womens Health. (2010) 19:751–7. doi: 10.1089/jwh.2009.1389
20. Marchi, M, Travascio, A, Uberti, D, De Micheli, E, Grenzi, P, Arcolin, E, et al. Post-traumatic stress disorder among LGBTQ people: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2023) 32:e44. doi: 10.1017/S2045796023000586
21. D'Augelli, AR, Grossman, AH, and Starks, MT. Childhood gender atypicality, victimization, and PTSD among lesbian, gay, and bisexual youth. J Interpers Violence. (2006) 21:1462–82. doi: 10.1177/0886260506293482
22. Gilman, SE, Cochran, SD, Mays, VM, Hughes, M, Ostrow, D, and Kessler, RC. Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. Am J Public Health. (2001) 91:933–9. doi: 10.2105/AJPH.91.6.933
23. Roberts, AL, Austin, SB, Corliss, HL, Vandermorris, AK, and Koenen, KC. Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. Am J Public Health. (2010) 100:2433–41. doi: 10.2105/AJPH.2009.168971
24. Roberts, AL, Rosario, M, Corliss, HL, Koenen, KC, and Austin, SB. Childhood gender nonconformity: a risk indicator for childhood abuse and posttraumatic stress in youth. Pediatrics. (2012) 129:410–7. doi: 10.1542/peds.2011-1804
25. Whitbeck, LB, Chen, X, Hoyt, DR, Tyler, KA, and Johnson, KD. Mental disorder, subsistence strategies, and victimization among gay, lesbian, and bisexual homeless and runaway adolescents. J Sex Res. (2004) 41:329–42. doi: 10.1080/00224490409552240
26. Shipherd, JC, Maguen, S, Skidmore, WC, and Abramovitz, SM. Potentially traumatic events in a transgender sample: frequency and associated symptoms. Traumatology. (2011) 17:56–67. doi: 10.1177/1534765610395614
27. Balsam, KF, Rothblum, ED, and Beauchaine, TP. Victimization over the life span: a comparison of lesbian, gay, bisexual, and heterosexual siblings. J Consult Clin Psychol. (2005) 73:477–87. doi: 10.1037/0022-006X.73.3.477
28. Lehavot, K, and Simpson, TL. Trauma, posttraumatic stress disorder, and depression among sexual minority and heterosexual women veterans. J Couns Psychol. (2014) 61:392–403. doi: 10.1037/cou0000019
29. Ray-Sannerud, BN, Bryan, CJ, Perry, NS, and Bryan, AO. High levels of emotional distress, trauma exposure, and self-injurious thoughts and behaviors among military personnel and veterans with a history of same sex behavior. Psychol Sex Orientat Gend Divers. (2015) 2:130–7. doi: 10.1037/sgd0000096
30. Livingston, NA, Berke, DS, Ruben, MA, Matza, AR, and Shipherd, JC. Experiences of trauma, discrimination, microaggressions, and minority stress among trauma-exposed LGBT veterans: unexpected findings and unresolved service gaps. Psychol Trauma. (2019) 11:695–703. doi: 10.1037/tra0000464
31. Livingston, NA, Lynch, KE, Hinds, Z, Gatsby, E, DuVall, SL, and Shipherd, JC. Identifying posttraumatic stress disorder and disparity among transgender veterans using nationwide veterans health administration electronic health record data. LGBT Health. (2022) 9:94–102. doi: 10.1089/lgbt.2021.0246
32. Brown, GR, and Jones, KT. Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the veterans health administration: a case-control study. LGBT Health. (2016) 3:122–31. doi: 10.1089/lgbt.2015.0058
33. Shipherd, JC, Lynch, K, Gatsby, E, Hinds, Z, DuVall, SL, and Livingston, NA. Estimating prevalence of PTSD among veterans with minoritized sexual orientations using electronic health record data. J Consult Clin Psychol. (2021) 89:856–68. doi: 10.1037/ccp0000691
34. Carey, FR, LeardMann, CA, Lehavot, K, Jacobson, IG, Kolaja, CA, Stander, VA, et al. Health disparities among lesbian, gay, and bisexual service members and veterans. Am J Prev Med. (2022) 63:521–31. doi: 10.1016/j.amepre.2022.04.034
35. Gorman, KR, Kearns, JC, Pantalone, DW, Bovin, MJ, Keane, TM, and Marx, BP. The impact of deployment-related stressors on the development of PTSD and depression among sexual minority and heterosexual female veterans. Psychol Trauma. (2022) 14:747–50. doi: 10.1037/tra0001102
36. VA Informatics and Computing Infrastructure (VINCI). Available at: https://www.hsrd.research.va.gov/for_researchers/vinci/ (accessed August 13, 2024)
37. Workman, TE, Goulet, JL, Brandt, C, Skanderson, M, Wang, R, Warren, AR, et al., eds. A prototype application to identify LGBT patients in clinical notes. 2020 IEEE International Conference on Big Data (Big Data); (2020): IEEE.
38. Goulet, JL, Kerns, RD, Bair, M, Becker, WC, Brennan, P, Burgess, DJ, et al. The musculoskeletal diagnosis cohort: examining pain and pain care among veterans. Pain. (2016) 157:1696–703. doi: 10.1097/j.pain.0000000000000567
39. VHA Headache Centers of Excellence Program Washington, DC, USA: U.S. Department of Veteran Affairs; (2022). Available at: https://www.polytrauma.va.gov/headache/ (accessed August 13, 2024)
40. Austin, PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. (2009) 28:3083–107. doi: 10.1002/sim.3697
41. Cohen, J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates Publishers (1988).
42. Vetvik, KG, and MacGregor, EA. Sex differences in the epidemiology, clinical features, and pathophysiology of migraine. Lancet Neurol. (2017) 16:76–87. doi: 10.1016/S1474-4422(16)30293-9
43. Munakata, J, Hazard, E, Serrano, D, Klingman, D, Rupnow, MF, Tierce, J, et al. Economic burden of transformed migraine: results from the American migraine prevalence and prevention (AMPP) study. Headache. (2009) 49:498–508. doi: 10.1111/j.1526-4610.2009.01369.x
44. Webermann, AR, Nester, MS, Gianoli, MO, Black, AC, Rosen, MI, Mattocks, KM, et al. Compensation and pension exams for military sexual trauma-related posttraumatic stress disorder: examiner perspectives, clinical impacts on veterans, and strategies. Womens Health Issues. (2023) 33:428–34. doi: 10.1016/j.whi.2023.02.002
45. Averill, LA, Eubanks Fleming, CJ, Holens, PL, and Larsen, SE. Research on PTSD prevalence in OEF/OIF veterans: expanding investigation of demographic variables. Eur J Psychotraumatol. (2015) 6:27322. doi: 10.3402/ejpt.v6.27322
46. Dinenberg, RE, McCaslin, SE, Bates, MN, and Cohen, BE. Social support may protect against development of posttraumatic stress disorder: findings from the heart and soul study. Am J Health Promot. (2014) 28:294–7. doi: 10.4278/ajhp.121023-QUAN-511
47. Wolfe, HL, Reisman, JI, Yoon, SS, Blosnich, JR, Shipherd, JC, Vimalananda, VG, et al. Validating data-driven methods for identifying transgender individuals in the veterans health administration of the US Department of veterans affairs. Am J Epidemiol. (2021) 190:1928–34. doi: 10.1093/aje/kwab102
Keywords: Veterans, sex of record, PTSD - post-traumatic stress disorder, LGBTQ+, comorbidities
Citation: Workman TE, Goulet JL, Brandt CA, Skanderson M, O’Leary J, Gordon KS and Treitler-Zeng Q (2025) LGBTQ+ status and sex of record in Veterans with post-traumatic stress disorder: demographics, comorbidities, and outpatient encounters. Front. Public Health. 12:1487866. doi: 10.3389/fpubh.2024.1487866
Edited by:
Piotr Karniej, WSB Merito University in Wroclaw, PolandReviewed by:
Lukasz Pietrzykowski, Nicolaus Copernicus University in Toruń, PolandAgnieszka Walendzik-Ostrowska, Akademia Humanitas, Poland
Copyright © 2025 Workman, Goulet, Brandt, Skanderson, O’Leary, Gordon and Treitler-Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Terri Elizabeth Workman, bGl6d29ya21hbkBnd3UuZWR1
†These authors share senior authorship
 Terri Elizabeth Workman
Terri Elizabeth Workman Joseph L. Goulet
Joseph L. Goulet Cynthia A. Brandt3,4
Cynthia A. Brandt3,4 Qing Treitler-Zeng
Qing Treitler-Zeng