- 1Jorge Basadre Grohmann National University, Tacna, Peru
- 2School of Obstetrics and Childcare, Faculty of Medicine, Universidad Andrés Bello, Santiago, Chile
Background: Urinary incontinence (UI), which can be classified as stress, urgency, or mixed, represents a public health problem that mainly affects adult women. This study aimed to determine the prevalence, association of sociodemographic and obstetric factors with the types of UI as well as the perceived impact on quality of life of women attending primary health facilities in the Tacna region from Peru.
Methods: A quantitative, non-experimental, correlational, and cross-sectional study was conducted. Stratified sample. A total of 346 women aged 30 to 64 years were surveyed, applying two short version instruments: the Urinary Discomfort Inventory Questionnaire (UDI-6) and the Urinary Incontinence Impact Questionnaire (IIQ-7). Descriptive statistics, parameters of the multinomial logistic regression, with the B values, odds ratio (OR) and significance level (p < 0.05).
Results: The prevalence of UI was 80.9%, with mixed UI being more frequent (48.8%). A significant association was found between the sociodemographic factor of educational level and type of UI (p = 0.004). Obstetric factors: higher frequency of mixed urinary incontinence (MUI) in vaginal delivery (30.6%) and newborns weighing 2,500–3,999 grams (35.5%). Additionally, an association between quality of life and type of urinary incontinence was observed, with a greater impact on those who had MUI (18.2%).
Conclusion: There is a high prevalence of UI in women in the Tacna region, the sociodemographic associated is educational level. There is an association between quality of life and UI, with MUI being more frequent.
1 Introduction
The World Health Organization (WHO) recognizes UI as a major public health problem that affects millions of people worldwide, especially women (1). UI is not only a medical problem, it also has an impact on the psychological, social and economic aspects, due to the stigma and isolation it can cause, generating functional limitations and often negative relationships with people, couples and families (2–4).
The International Association of Urogynecology (IUGA) and the International Continence Society (ICS) have stablished standardized definitions of UI, considering it as an important medical issue that impacts quality of life. This regulatory framework facilitates the understanding and classification of UI, which is essential for its diagnosis, treatment and management. According to the ICS, UI is defined as “any involuntary loss of urine.” This definition includes different conditions, classified into types, according to the symptoms and circumstances that cause urine leakage (5), being more common in women (6). Among the types of UI are the urgency UI (UUI), effort UI (EUI) and mixed UI (MUI). EUI is characterized by involuntary urine leakage during activities that increase abdominal pressure, such as coughing, sneezing, or exercise; in contrast, UUI occurs along with an urgent need to urinate, while MUI has characteristics of both types (3, 5).
Furthermore, the ICS provides a clear framework regarding the prevalence of UI, highlighting its impact on public health and the importance of a comprehensive approach. The prevalence varies significantly according to the different studies and populations analyzed: in the United States, it was estimated that 61.8% of women experience some type of UI and more than 20% have moderate or severe UI (7). In Japan, the estimate for women between 20 and 64 years of age was 25.5% and increased with age (8). The percentage of women seeking help for the problem is low, 24% for Asia and 33% for Europe (9). Chile, Colombia, Mexico, and Costa Rica have policies and research that address their high prevalence and impact on quality of life (10–13). Finally, in southern Peru (14), a prevalence of 73.9% was found in pelvic floor dysfunction (PPD), with UI being the most frequent. UI tends to increase with age, being especially high in older women, due to factors such as aging, menopause and weakness in the pelvic floor musculature. This highlights the importance of well-designed epidemiological studies to better understand the magnitude of this condition and its effects on the affected population, especially since UI not only has physical implications, but also generates significant psychological and social problems (7).
The context of the study corresponds to the southern region of Peru (Tacna). This region presents geographical, sociodemographic, and healthcare access characteristics that affect the quality of life, especially among women, with diverse socioeconomic levels and a lack of specialized pelvic health care, which constitutes one of the main barriers. Additionally, 59.7% of the population are migrants, mainly from the Puno region (a high Andean area) (15), which has specific cultural characteristics, such as the presence of patriarchal families where women tend not to express their sexual health issues, as it is considered a taboo subject. These cultural dynamics perpetuate the lack of awareness and invisibility of health problems such as pelvic floor dysfunctions, which often remain unaddressed and untreated.
The main risk factors associated with UI in women include age (6, 7, 16), pregnancy and parity (14, 17, 18), history of hysterectomy, obesity, pelvic radiation, as well as pelvic floor affectation during childbirth (19, 20). Of these factors, parity is one of the most important, as childbirth can lead to pelvic muscle atrophy and nerve deterioration, increasing the risk of UI (3, 20). Weak connective tissue and high fetal weight at birth are important risk factors (21). In addition, being overweight has also been observed to be a risk factor for UI in women (14, 16), which highlights the importance of maintaining a healthy weight to prevent this condition, especially in young and middle-aged women (22). Strenuous exercise has been studied in recent years, and has been found to be a risk factor for UI, specially in women due to increased of intra-abdominal pressure and potential weakening of the pelvic floor (23). However, moderate physical activity and proper pelvic floor training can offer significant benefits and help prevent it. Pelvic floor muscle training (PFMT) is considered as the first choice treatment for women with UI, focusing on increasing strength and correcting their activation patterns (24). Recent evidence has demonstrated its effectiveness in the treatment of UI and other disorders (25).
The ICS has recommended the inclusion of a quality of life questionnaire in all UI-related studies, highlighting the importance of assessing the impact on individuals’ physical, psychological, and social well-being (26). Therefore, the adaptation of questionnaires and the validation of assessment tools in different populations, such as in Chile, reflect efforts to understand and address UI as a public health problem (11, 27). In addition, WHO’s recommendation to study and analyze the evolution of health systems, as demonstrated in the context of Peru, reflects a broader global perspective to address public health challenges, including UI (28).
The recognition and understanding of risk factors are essential for the design of strategies for the prevention, diagnosis and treatment of UI in women, as well as to promote pelvic floor health and improve quality of life in those affected. Therefore, the objective of the study was to determine the prevalence, association of sociodemographic and obstetric factors with the type of UI and to know the perception of its impact on the quality of life of women who attend first-level health facilities in the Tacna region—Peru.
2 Methodology
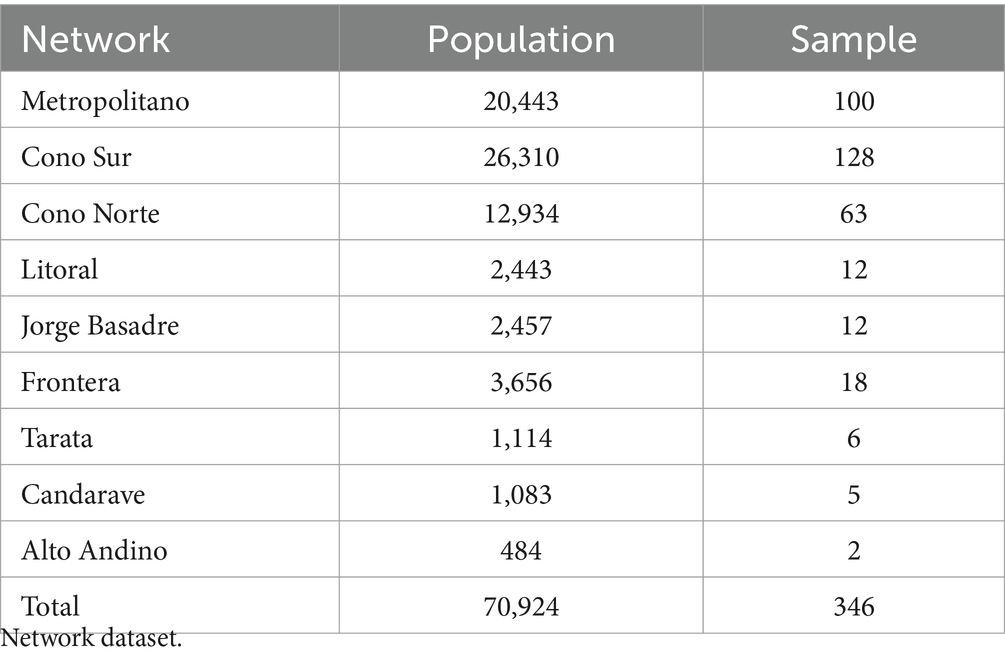
This study, with a quantitative approach, utilized a non-experimental and correlational cross-sectional design. The population consisted of 70,924 women aged 30 to 64 years, assigned to different healthcare networks of the Ministry of Health, from which a representative sample of 346 was selected. Each healthcare network was considered a stratum, and the following parameters were applied for sample calculation: population = 70,924, z = 1.96 (value of the normal distribution for 95% confidence), p = 0.5; q = 0.5, and a margin of error of 5.26%. Participants were randomly selected from each healthcare network. All women who agreed to participate in the study were included, regardless of their parity, without limitations in relation to the practice of sports and who signed the informed consent form. Those who presented psychic alterations or cognitive impairment were excluded. Below is the table detailing the study’s population and sample.
Ethical approval for the study was obtained from the Institutional Ethics and Research Committee of the Hipólito Unanue Hospital in Tacna, with the assigned code: 28-CIÉI-HHUT-2024.
2.1 Technique, instrument and data processing
Two measurement scales were used in short version: Urinary Discomfort Inventory Questionnaire (UDI-6), to determine prevalence and type of incontinence (29, 30) and the Impact of Urinary Incontinence (IIQ-7) on quality of life (31).
To determine the type of incontinence, specific questions from the UDI-6 questionnaire were used. Item 2 identified UUI, characterized by urinary leakage associated with a sudden and intense need to urinate. On the other hand, item 3 focused on EUI, which occurs when there is urinary leakage during physical activities or when pressure is exerted on the abdomen, such as coughing, sneezing, laughing, or lifting objects. When both items showed positive results, the person was considered to have MUI, which combines characteristics of the previous two types (30).
Various studies corroborate that both questionnaires have proven to be psychometrically valid and reliable, documenting key aspects such as validity, reliability and sensibility to change (29, 32, 33). Turning them in valuable tools in clinical practice and research. They were adapted to their short versions in 2005 and validated into other languages such as French, Swedish, Chinese, Arabic, Turkish and, Spanish in U.S. Spanish speakers (29, 34).
2.2 Procedure and statistical analysis
The analysis was executed using SSPS version 27 statistical software and Excel. To determine prevalence, type of UI and quality of life, descriptive statistics were used. For the association of variables, the parameters of the multinomial logistic regression, including the values of B, odds ratio (OR) and the significance level (p < 0.05) were determined.
3 Results
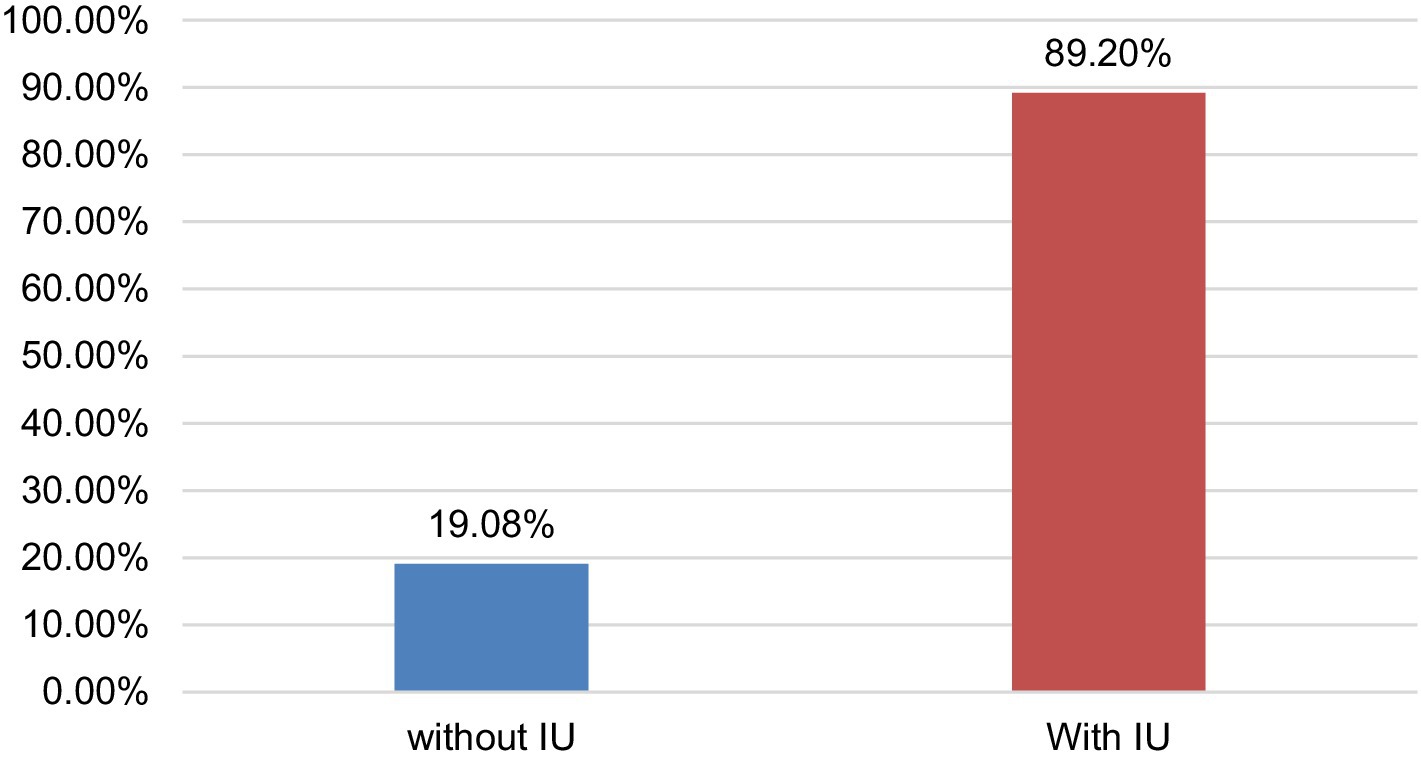
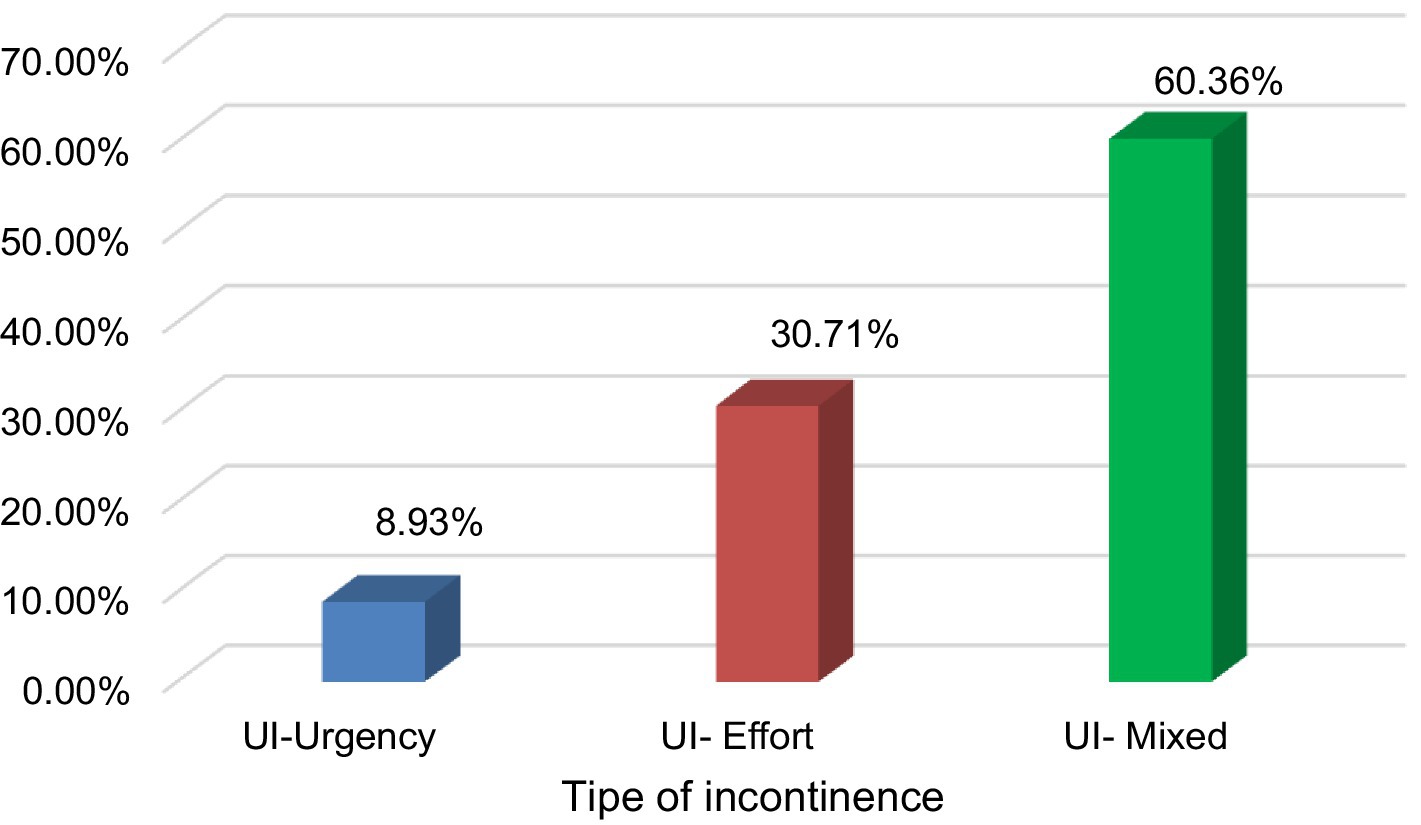
The prevalence of UI in women aged 30 to 64 years was 80.9% (Figure 1), with MU being the most frequent with 60.4% (Figure 2). This occurs in the group of 30 to 49 years old (35.8%) with overweight (21.4%) and obesity (18.5%); with secondary (23.7%) and higher (14.2%) levels of education, cohabiting (25.4%) and separated (12.4%), living in urban areas (41.3%). Educational level shows a significant association with stress urinary incontinence (OR = 4.431) and a possible association with mixed incontinence (OR = 2.441). Age has a slight relationship with stress incontinence (OR = 1.031), but it is not conclusive for other types of incontinence. Other factors, such as nutritional status, occupation, marital status, and place of origin, were not significant in most cases (Table 1).
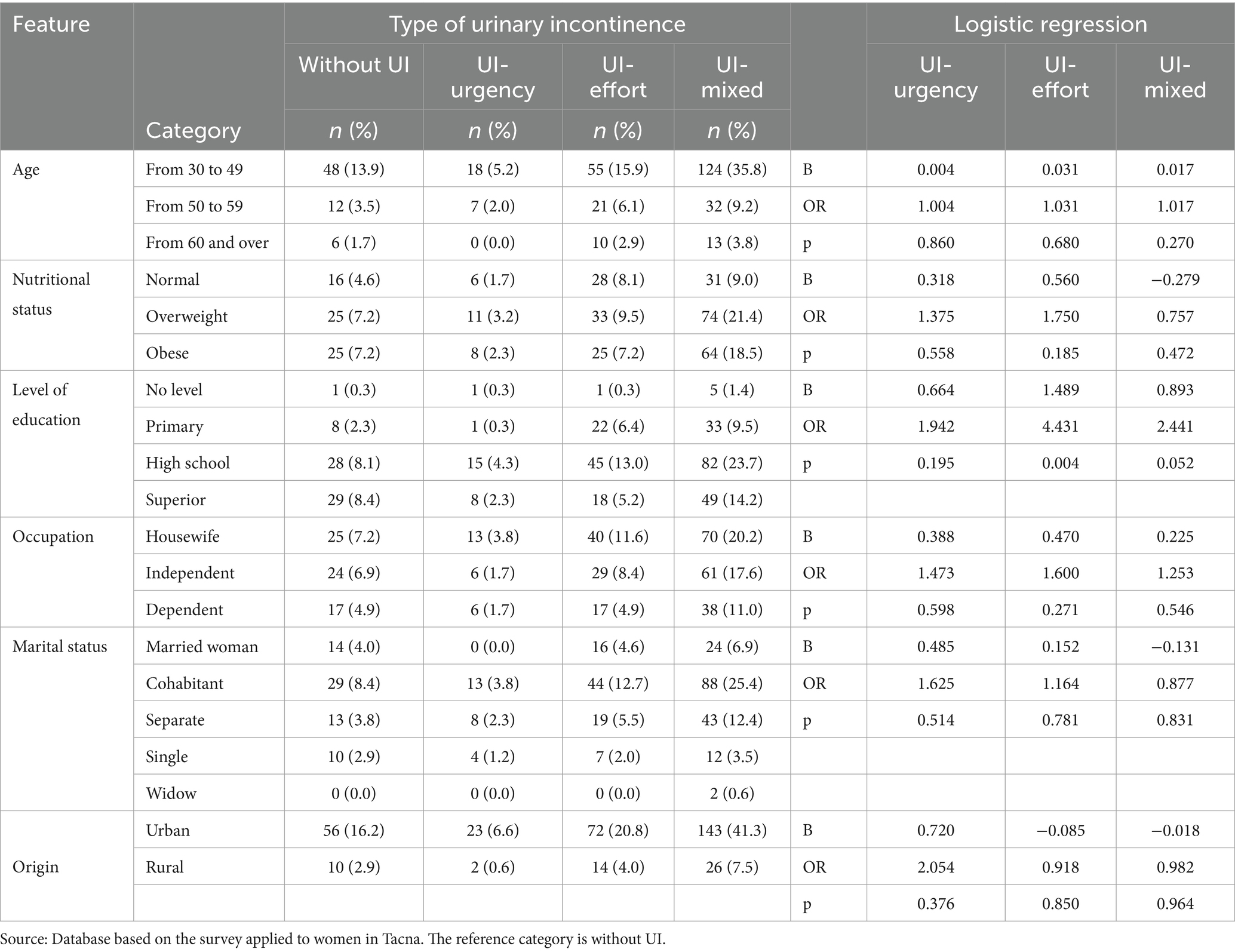
Table 1. Association of socioeconomic factors and types of urinary incontinence in women of the Tacna region—2023.
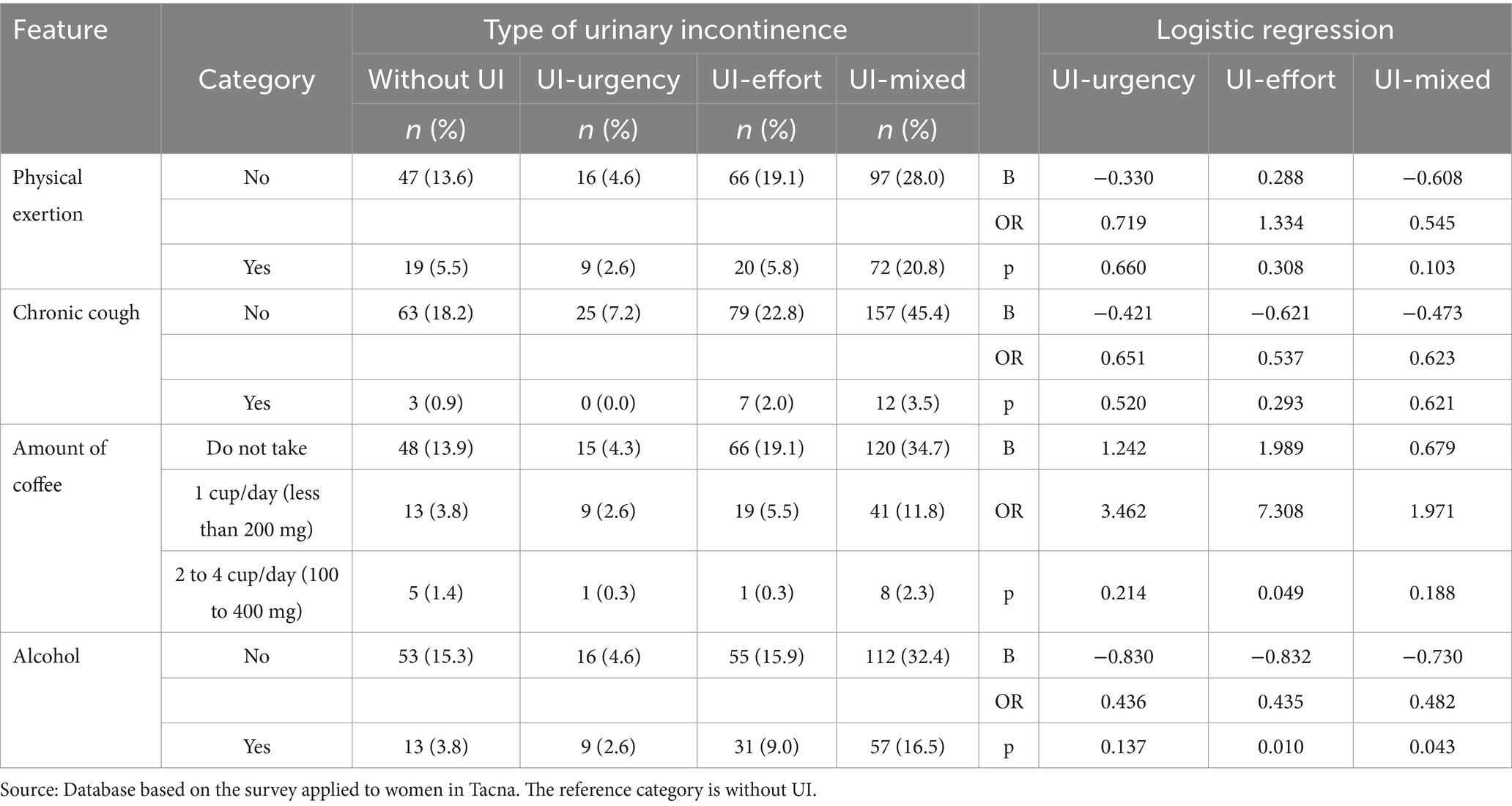
Regarding habits, alcohol consumption shows a significant negative association with mixed MUI (B = −0.730, OR = 0.482, p = 0.043) and with UUI (B = −0.832, OR = 0.435, p = 0.010). However, for SUI (B = −0.830, OR = 0.436, p = 0.137), no significant association was found. Coffee consumption (B = 0.679, OR = 1.971, p = 0.188) appears to be related to an increased likelihood of MUI, but this association is not significant. Although for UUI (B = 1.242, OR = 3.462, p = 0.214) the coefficient suggests a possible positive association. However, for EUI (B = 1.989, OR = 7.308, p = 0.049), this relationship is not significant (Table 2).
MUI predominated in women with a history of vaginal delivery (30.6%) and those with both cesarean and vaginal deliveries (7.8%). The mode of delivery (B = −1.270; OR = 0.281, p = 0.031) is significantly associated with a lower likelihood of having mixed urinary incontinence. However, for UUI (B = 1.163; OR = 3.200, p = 0.947), there is a trend towards increasing the likelihood, but it is not significant. Regarding SUI (B = −0.816; OR = 0.442, p = 0.240), the mode of delivery shows a trend towards reducing the likelihood, but this association is also not significant. A higher newborn weight tends to increase the likelihood of MUI (B = 0.565; OR = 1.760, p = 0.108), although this relationship is not significant (Table 3).
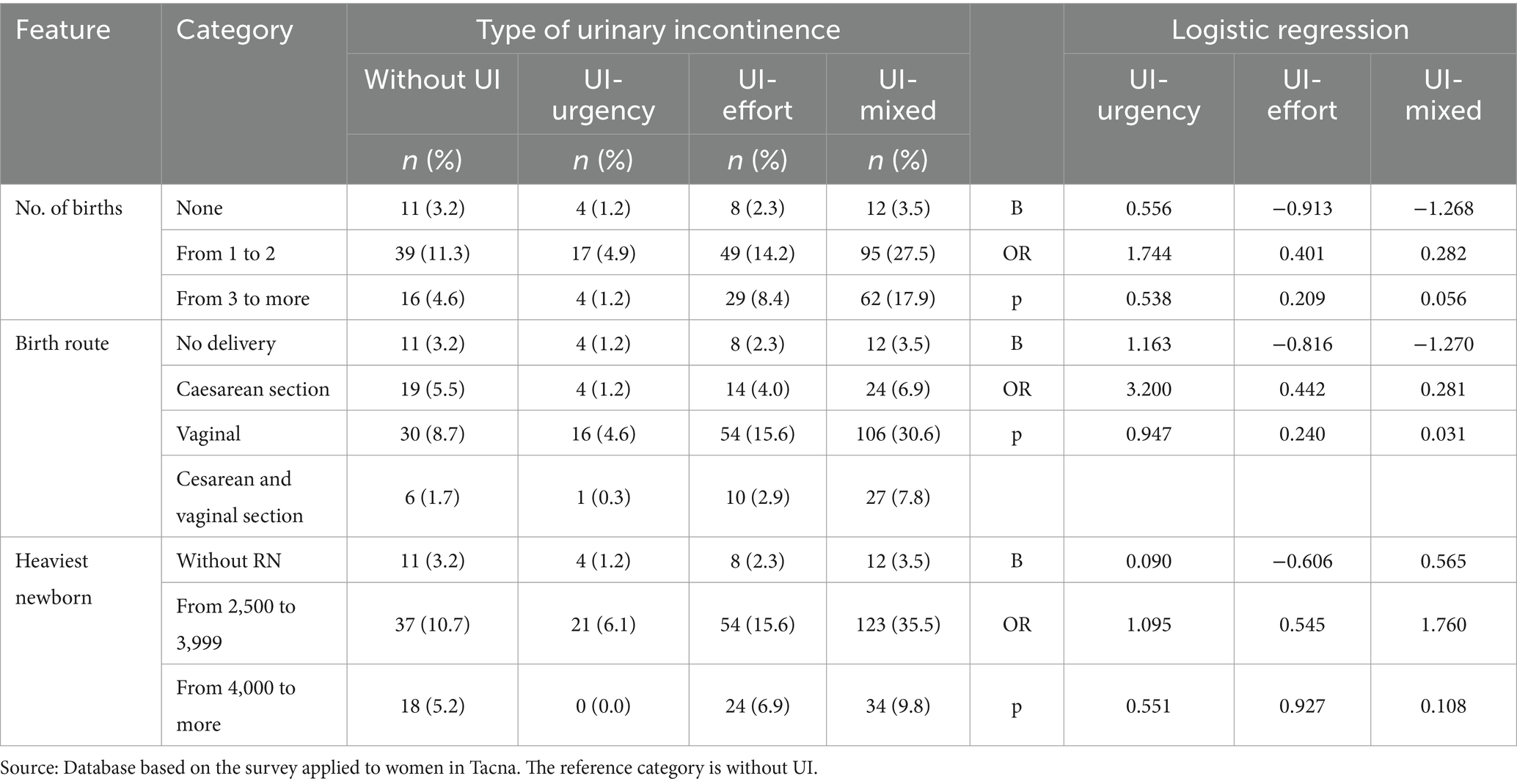
Table 3. Association of obstetric factors and types of urinary incontinence in women of the Tacna region—2023.
Likewise, it was found that women with urinary incontinence have a significantly higher likelihood of experiencing a mild impact on their quality of life (B = 2.658; OR = 14.264; p = 0.000), as well as a moderate impact (B = 2.188; OR = 8.915; p = 0.036) compared to those without urinary incontinence. This association is statistically significant (Table 4).
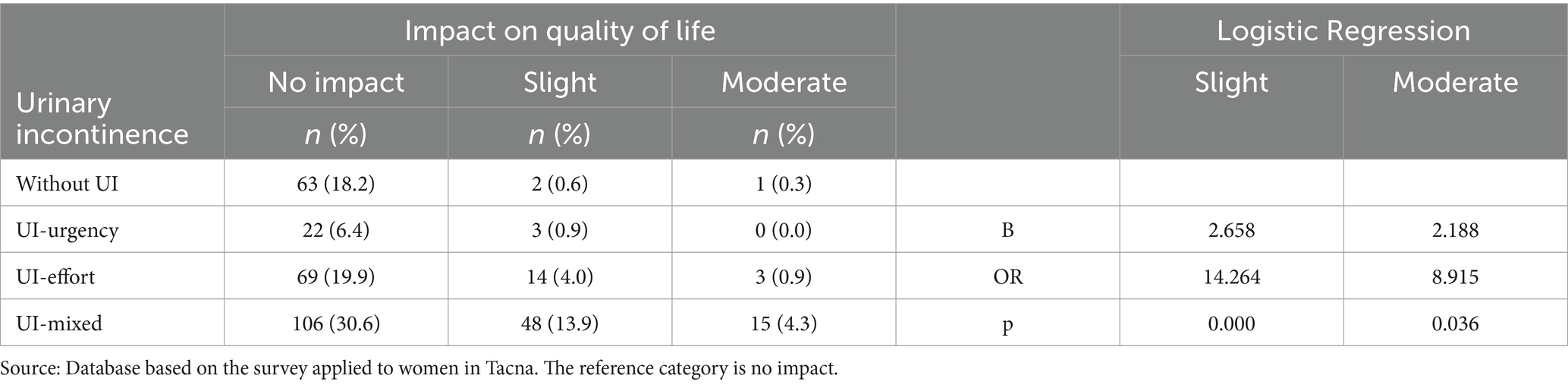
Table 4. Association of types of urinary incontinence and their impact on the quality of life of women of the Tacna region—2023.
4 Discussion
The study showed that out of every five women, four have UI, with MUI being more frequent; Milsom and Gyhagen (35), in a systematic review, argues that other studies have reported prevalences between 25 and 45% and that increase with age, exertional UI becoming more common. Llajaruna Zumaeta and Urbina Quispe (36) showed that this subtype of UI has a prevalence that varies between 40 and 50%. On the other hand, Khan et al. (37) in a study carried out in India found that the older the age, the more cases of MUI increase, unlike the present study where MUI occurs at younger ages (30 to 49 years). Salo et al. (38) found, using a logistic regression model, in a population from Finland, that MUI is associated with poor work capacity (OR 2.51, 95% CI 1.68–3.74), especially in young women. It should be noted that UI is a common condition among women. In this regard, Turk et al. (39) states that one in seven women suffer from some type of UI. Despite its high prevalence, about half of those with clinically significant UI are undiagnosed and untreated (40).
Regarding sociodemographic factors, the data suggest some trends, such as a higher frequency of MUI in women aged 30 to 49 years, with overweight and obesity, medium and high educational levels, housewives and self-employed women, cohabiting and separated, as well as coming from urban areas. Different authors found similar results where UI was be associated with factors such as age, obesity, menopause, rural area of residence, among others (37, 41, 42). Other research suggests that MUI it’s an underestimated problem (37, 43). Islam et al. (44), in a research conducted in Bangladesh identified that women in the highest wealth quintile (p = 0.009) and underweight women had a lower risk of emergency UI (p = 0.018), constituting protective factors. This research also found that educational level has a significant association with EUI, which may be due to the fact that women with higher educational levels tend to be more informed about health issues, are more likely to consult medical professionals when experiencing symptoms, and are more open to discussing these topics. Digging deeper into these findings could guide more targeted interventions based on the identified risk profiles.
MUI was more frequent in women with 1–2 deliveries, predominating in women with vaginal deliveries. Similar results were obtained in other studies where parity is an associated factor (6, 18, 45). Other researchers assert multiparity as a risk factor (3, 46). This condition, along with factors such as gestational age, history of miscarriages, and constipation, are significantly associated with UI during pregnancy (46–48). Physiological changes, such as increased abdominal pressure, progesterone levels, and pelvic floor injuries, can increase susceptibility to it (18, 48).
It was found that the mode of delivery (B = −1.270; OR = 0.281, p = 0.031) is significantly associated with a lower likelihood of developing MUI. This may be due to the fact that nearly a quarter of the sample had a cesarean delivery, which, by avoiding the birth canal, reduces the risk of damage to these structures.
UI is more common in multiparous women and can persist even after childbirth (7, 47). Therefore, it is crucial that health professionals recognize parity as a significant risk factor when evaluating and treating UI, especially during the prenatal and postpartum period.
Although no significant association was found with newborn weight, research suggested that vaginal delivery with higher birth weight infants may increase the risk of developing postpartum UI (21, 49). In addition, it has been observed that obstetric trauma during childbirth, particularly in cases of shoulder dystocia or instrumental births, could trigger it (45), determining that the weight of the newborn may be a relevant risk factor (50). Understanding this connection can be critical to improving its prevention, diagnosis, and treatment, providing comprehensive and personalized care to those who are affected by this condition. In this regard, the effectiveness of pelvic floor muscle training in the treatment of UI has been recognized, suggesting the potential for non-invasive interventions to address this issue (26). However, a study conducted in Japan found that less than 5% of individuals with UI had experience with pelvic floor muscle training and medical care (8). The literature also emphasizes the need for comprehensive care and support for individuals with UI, particularly among older adults, where physiotherapeutic treatment and pelvic floor muscle training can effectively improve muscle strength and quality of life (51, 52).
The findings suggest that UI has a significant negative impact on the quality of life of women in the Tacna region, who are approximately 14 times more likely to have their quality of life mildly affected and almost 9 times more likely to experience a moderate impact. This result coincides with the report by Moyolema Chicaiza (6), who points out that UI significantly affects the daily lives of women who suffer from it. The amount of urine leakage and frequency with which it occurs limit and impede personal, work, social and recreational activities (18, 48), and may even influence relationships, sexuality and general well-being (53). This observation coincides with previous research that has assessed quality of life in women with UI using standardized and validated questionnaires. For example, the “King’s Health Questionnaire,” adapted and validated for Portuguese women with UI, has shown how this condition negatively affects quality of life, reflecting similar limitations in social participation and general well-being (54). In addition, studies on strengthening the pelvic floor muscle have evidenced improvements in both quality of life and self-perception of women, highlighting the relevance of specific interventions in these cases (55). These results support and extend the understanding of the impact of UI on various aspects of daily life, aligning with the findings of this study.
Despite the negative impact of UI on quality of life, many women are reluctant to seek medical care for this condition (42, 56). The lack of open communication about UI is a clear issue, as a significant portion of those affected do not mention the condition, and only a minority seek professional care (9). Among the main reasons for not seeking medical advice are the embarrassment of discussing the issue, especially with male doctors, and the mistaken belief that it is a common or incurable condition. This reluctance is a complex phenomenon influenced by various factors (57). In this regard, Vallana Sala (58) mentions that it is not only due to cultural differences, but also to previous experiences with medicine, considering that the quality of medical care plays a crucial role in women’s willingness to seek treatment (59). The studies maintain that women with a lower level of education are at greater risk of not seeking medical attention. On the other hand, it has been observed that most of those affected do not seek medical attention, either because they consider it not to be serious or because they see it as a normal aging process, which contributes to normalizing UI (14, 60). Improving education about UI, treatment options, and promoting lifestyle changes offer significant opportunities (37). Consequently, the impact on women’s quality of life has been a focal point in several studies, emphasizing the need for comprehensive care and support for those affected (61). Despite its high prevalence, the discomfort caused by this condition is often accepted as normal by the general population, highlighting the urgent need to increase education on the subject (14).
UI can present itself in different forms (effort, urgency or mixed), mainly affecting women and older adults. A comprehensive approach, addressing both physical, emotional, and social aspects is essential to improve the quality of life of those affected.
Given that information about prior treatment was not included, there is a possibility that the results are underestimating or overestimating the true prevalence and its associated factors. This limitation should be considered when interpreting the findings, as women who received treatment might be less likely to present symptoms at the time of the study. In future studies, it would be important to collect data on UI treatment to adjust the analyses and account for this potentially confounding variable. It is recommended to continue researching and developing effective strategies to diagnose, treat and manage UI in women, in order to promote general well-being and health.
5 Conclusion
This study reveals a high prevalence of UI (80.9%), the most common form was MUI (48.8%). Regarding sociodemographic factors, an association was found with the level of education, obstetric risk factors were not associated with the types of UI: route of delivery, history of vaginal delivery, and newborn weight. Finally, an association was found between negative impact on quality of life and UI.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Institutional Committee of Ethics and Research of the Hipólito Unanue Hospital in Tacna. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
GS-G: Writing – original draft, Writing – review & editing. CL: Writing – original draft, Writing – review & editing. JF: Writing – original draft, Writing – review & editing. GE-B: Writing – original draft, Writing – review & editing. SS-G: Writing – original draft, Writing – review & editing. CF: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank all the women who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vogel, J, Jung, J, Lavin, T, Simpson, G, Kluwgant, D, Abalos, E, et al. Neglected medium-term and long-term consequences of labour and childbirth: a systematic analysis of the burden, recommended practices, and a way forward. Lancet Glob Health. (2024) 12:e317–30. doi: 10.1016/S2214-109X(23)00454-0
2. Alves, RA, Machado, M, Moura, T, Brazil, CA, Lemos, AQ, and Lordelo, P. Perfil Clínico de Mulheres Com Incontinência Urinária de Esforço Em Centro de Referência. Rev Pesqui Fisioter. (2021) 11:351–60. doi: 10.17267/2238-2704rpf.v11i2.3714
3. Choudhary, A, and Dadhich, R. Prevalence of different types of urinary incontinence and their association with age and parity. J Med Sci Clin Res. (2018) 6. doi: 10.18535/jmscr/v6i4.128
4. Razzaq, R, Muhammad, A, Shabbir, S, Naeem Malhi, M, Fatima, N, and Kiran, W. Prevalence of urinary incontinence in pregnant women: a cross sectional survey study: prevalence of urinary incontinence in pregnant women. Pak J Med Sci. (2022) 3:145–8. doi: 10.54393/pjhs.v3i04.61
5. Haylen, BT, de Ridder, D, Freeman, RM, Swift, SE, Berghmans, B, Lee, J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. (2010) 29:4–20. doi: 10.1002/nau.20798
6. Moyolema Chicaiza, PF, and Flores Chiliguano, LY. Incontinencia urinaria postparto en mujeres nulíparas y multíparas. Salud Cienc Tecnol. (2022) 2:90. doi: 10.56294/saludcyt202290
7. Patel, UJ, Godecker, AL, Giles, DL, and Brown, HW. Updated prevalence of urinary incontinence in women: 2015–2018 national population-based survey data. Female Pelvic Med Reconstr Surg. (2022) 28:181–7. doi: 10.1097/SPV.0000000000001127
8. Onishi, A, and Shibata, A. Prevalence and sociodemographic correlates of urinary incontinence in Japanese women: a web-based cross-sectional study. Women’s Health. (2023) 19:17455057231207754. doi: 10.1177/17455057231207754
9. Liang, S, Li, J, Chen, Z, Li, Y, Hao, F, and Cai, W. Prevalence and influencing factors of help-seeking behavior among women with urinary incontinence: a systematic review and meta-analysis. J Women’s Health. (2023) 32:1363–79. doi: 10.1089/jwh.2022.0482
10. de Monterrosa-Castro, ÁJ, Paternina-Caicedo, Á, Márquez-Vega, J, and Pérez, IR. Prevalencia de la sintomatología urogenital en mujeres indígenas colombianas en posmenopausia. Iatreia. (2012) 25:357–68. doi: 10.17533/udea.iatreia.13132
11. Busquets, CM, and Serra, TR. Validación del cuestionario International Consultation on Incontinence Questionnaire Short-Form (ICIQ-SF) en una población chilena usuaria del Fondo Nacional de Salud (FONASA). Rev Med Chile. (2012) 140:340–6. doi: 10.4067/S0034-98872012000300009
12. Chacón, GK, Zúñiga, AA, Umaña, AA, and Benavides, LA. Resultados del programa de terapia integral de incontinencia urinaria en personas adultos mayores, atendidos en la Uunidad de Incontinencia Urinaria del Hospital Nacional de Geriatrí y Gerontología, de Cosa Rica. Rev Clin Esc Med UCR-HSJD. (2020) 9:61–9. doi: 10.15517/rc_ucr-hsjd.v9i6.35330
13. Rincón, AO. Caracterización clínica de la incontinencia urinaria y factores asociados en usuarias de la Unidad de la Mujer del Centro de Salud Familiar “Ultraestación” en la ciudad de Chillán. Rev Med Chile. (2015) 143:203–12. doi: 10.4067/S0034-98872015000200008
14. Sologuren-García, G, Linares, CL, Flores, JR, Escobar-Bermejo, G, Sotelo-Gonzales, S, and Fagerstrom, CK. Epidemiology of pelvic floor dysfunction in the Tacna region of Peru, 2023. Int Urogynecol J. (2024) 35:1211–8. doi: 10.1007/s00192-024-05792-6
15. Instituto Nacional de Estadística e Informática. Compendio Estadístico, Tacna 2023. Lima-Perú: Instituto Nacional de Estadística e Informática (2023).
16. AlAzab, R, Alomari, RA, Khader, YS, and Gharaibeh, M. Stress urinary incontinence among Jordanian women living in rural areas: prevalence, associated factors and self-management behaviours. Arab J Urol. (2021) 19:469–72. doi: 10.1080/2090598X.2021.1926751
17. Åhlund, S, Rothstein, E, Rådestad, I, Zwedberg, S, and Lindgren, H. Urinary incontinence after uncomplicated spontaneous vaginal birth in primiparous women during the first year after birth. Int Urogynecol J. (2020) 31:1409–16. doi: 10.1007/s00192-019-03975-0
18. Wang, X, Jin, Y, Xu, P, and Feng, S. Urinary incontinence in pregnant women and its impact on health-related quality of life. Health Qual Life Outcomes. (2022) 20. doi: 10.1186/s12955-022-01920-2
19. Vázquez, IC, Rodríguez-Rodríguez, B, Hernández-Méndez, EA, López-Bravo, GM, Ortega-González, ME, Cortés-Raygoza, P, et al. Prospective analysis of obesity and the effect of bariatric surgery on urinary incontinence. Rev Mex Urol. (2019) 79:1–12. doi: 10.48193/revistamexicanadeurologa.v79i3.486
20. Maldonado, LAG, Erosa-Villareal, RA, Janssen-Aguilar, R, Laviada-Molina, HA, and Méndez-Domínguez, NI. Urinary incontinence: risk factors and frequency in women above 60 years of age in the southeast of Mexico. Rev Mex Urol. (2019) 79:1–14. doi: 10.48193/revistamexicanadeurologa.v79i3.408
21. Stroeder, R, Radosa, J, Clemens, L, Gerlinger, C, Schmidt, G, Sklavounos, P, et al. Urogynecology in obstetrics: impact of pregnancy and delivery on pelvic floor disorders, a prospective longitudinal observational pilot study. Arch Gynecol Obstet. (2021) 304:401–8. doi: 10.1007/s00404-021-06022-w
22. Alsannan, B, Alharmi, J, Alrahal, F, Al Mansoor, S, and Tulandi, T. Prevalence and quality of life among overweight and obese women with different severity and types of urinary incontinence. Med Princ Pract. (2024) 33:47–55. doi: 10.1159/000534651
23. Bø, K, and Nygaard, IE. Is physical activity good or bad for the female pelvic floor? A narrative review. Sports Med. (2020) 50:471–84. doi: 10.1007/s40279-019-01243-1
24. Lee, BA, Kim, SJ, Choi, DK, Kwon, O, Na, HR, and Cho, ST. Effects of pelvic floor muscle exercise on urinary incontinence in elderly women with cognitive impairment. Int Neurourol J. (2017) 21:295–301. doi: 10.5213/inj.1734956.478
25. Molina-Torres, G, Moreno-Muñoz, M, Rebullido, TR, Castellote-Caballero, Y, Bergamin, M, Gobbo, S, et al. The effects of an 8-week hypopressive exercise training program on urinary incontinence and pelvic floor muscle activation: a randomized controlled trial. Neurourol Urodyn. (2023) 42:500–9. doi: 10.1002/nau.25110
26. Weber-Rajek, M, Strączyńska, A, Strojek, K, Piekorz, Z, Pilarska, B, Podhorecka, M, et al. Assessment of the effectiveness of pelvic floor muscle training (PFMT) and extracorporeal magnetic innervation (ExMI) in treatment of stress urinary incontinence in women: a randomized controlled trial. Biomed Res Int. (2020) 2020:1019872–7. doi: 10.1155/2020/1019872
27. Viedma, CL, and Caruso, D. Adaptación transcultural del cuestionario “Barriers to Incontinence Care Seeking” en mujeres adultas mayores en el ámbito ambulatorio. Rev Fac Cien Med Univ Nac Cordoba. (2019) 76:3–10. doi: 10.31053/1853.0605.v76.n1.21088
28. Llanos Zavalaga, LF, Castro Quiroz, JA, Ortiz Fernández, J, and Ramírez Atencio, CW. Cuando crear sinergia no siempre es Salud: Análisis y propuesta en la evolución del Sistema de Salud en Perú. Rev Med Hered. (2020) 31:56–69. doi: 10.20453/rmh.v31i1.3730
29. Barber, MD, Walters, MD, and Bump, RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. (2005) 193:103–13. doi: 10.1016/j.ajog.2004.12.025
30. de Viñaspre, R, Hernández, R, Tomás Aznar, C, and Rubio, AE. Validación de la versión española de las formas cortas del Urogenital Distress Inventory (UDI-6) y del Incontinence Impact Questionnaire (IIQ-7) en mujeres embarazadas. Gac Sanit. (2011) 25:379–84. doi: 10.1016/j.gaceta.2011.05.010
31. Sánchez Sánchez, B, Torres Lacomba, M, Navarro Brazález, B, Cerezo Téllez, E, Pacheco Da Costa, S, and Gutiérrez Ortega, C. Responsiveness of the Spanish pelvic floor distress inventory and pelvic floor impact questionnaires short forms (PFDI-20 and PFIQ-7) in women with pelvic floor disorders. Eur J Obstet Gynecol Reprod Biol. (2015) 190:20–5. doi: 10.1016/j.ejogrb.2015.03.029
32. Ghroubi, S, El Fani, N, Elarem, S, Alila, S, Ben Ayed, H, Borgi, O, et al. Arabic (Tunisian) translation and validation of the Urogenital Distress Inventory short form (UDI-6) and Incontinence Impact Questionnaire short form (IIQ-7). Arab J Urol. (2020) 18:27–33. doi: 10.1080/2090598X.2019.1678000
33. Ip, PNP, Cheung, RYK, Wan, OYK, Choy, RKW, and Chan, SSC. Responsiveness of Urogenital Distress Inventory-6 and Incontinence Impact Questionnaire-7 after pelvic floor muscle training and surgical treatment. Hong Kong J Gynecol Obstet Midwif. (2022) 22:21–8. doi: 10.12809/hkjgom.22.1.01
34. Sánchez-Sánchez, B, Torres-Lacomba, M, Yuste-Sánchez, MJ, Navarro-Brazález, B, Pacheco-da-Costa, S, Gutiérrez-Ortega, C, et al. Cultural adaptation and validation of the Pelvic Floor Distress Inventory short form (PFDI-20) and Pelvic Floor Impact Questionnaire short form (PFIQ-7) Spanish versions. Eur J Obstet Gynecol Reprod Biol. (2013) 170:281–5. doi: 10.1016/j.ejogrb.2013.07.006
35. Milsom, I, and Gyhagen, M. The prevalence of urinary incontinence. Climacteric. (2019) 22:217–22. doi: 10.1080/13697137.2018.1543263
36. Llajaruna Zumaeta, E, and Urbina, QK. Incontinencia urinaria de esfuerzo femenina. Inter Méd. (2021) 11:12–21. doi: 10.56838/icmed.v11i3.14
37. Khan, S, Ansari, MA, Vasenwala, SM, and Mohsin, Z. The influence of menopause on urinary incontinence in the women of the community: a cross-sectional study from North India. Int J Reprod Contracept Obstet Gynecol. (2017) 6:911–8. doi: 10.18203/2320-1770.ijrcog20170555
38. Salo, H, Mäkelä-Kaikkonen, J, Sova, H, Piltonen, T, Laru, J, Ala-Mursula, L, et al. Urinary incontinence associates with poor work ability in middle-aged women: a northern Finland birth cohort 1966 study. Acta Obstet Gynecol Scand. (2024) 103:572–9. doi: 10.1111/aogs.14743
39. Turk, Q-U-a, Jadoon, IJ, Fareed, S, Shah, HU, Fareed, A, Bhutta, AH, et al. Prevalence ratio of urinary incontinence and its association with parity and gravidity: correlational study. J Women Med Dent Coll. (2023) 1:8–12. doi: 10.56600/jwmdc.v1i4.54
40. Sönmez, S, Eraydın, E, Arıcan, Y, and Sönmez, F. Factors associated with help seeking behavior of Turkish women with urinary incontinence; a single center cross-sectional study. Gynecol Obstet Reprod Med. (2017) 23:153–7. doi: 10.21613/GORM.2016.699
41. Alexander, MC, Londhe, V, Ebenezer, ED, Kekre, AN, and Jeyaseelan, V. Is hysterectomy a risk factor for urinary incontinence? Int J Reprod Contracept Obstet Gynecol. (2019) 8:1260–5. doi: 10.18203/2320-1770.ijrcog20191061
42. Al Kiyumi, MH, Al Belushi, ZI, Jaju, S, and Al Mahrezi, AM. Urinary incontinence among Omani women: prevalence, risk factors and impact on quality of life. Sultan Qaboos Univ Med J. (2020) 20:45–e53. doi: 10.18295/squmj.2020.20.01.007
43. Amanat Ali, M, Naeem, L, Asif, R, Imran, K, Noor, M, and Hafeez, M. Prevalence of urinary incontinence among married females in Sialkot Pakistan: prevalence of urinary incontinence among married females in Sialkot Pakistan. J Ther Rehabil Sci. (2022) 3:24–7. doi: 10.54393/tt.v3i1.37
44. Islam, RM, Bell, RJ, Hossain, MB, and Davis, SR. Types of urinary incontinence in Bangladeshi women at midlife: prevalence and risk factors. Maturitas. (2018) 116:18–23. doi: 10.1016/j.maturitas.2018.07.012
45. Moossdorff-Steinhauser, HFA, Berghmans, BCM, Spaanderman, MEA, and Bols, EMJ. Prevalence, incidence and bothersomeness of urinary incontinence between 6 weeks and 1 year post-partum: a systematic review and meta-analysis. Int Urogynecol J. (2021) 32:1675–93. doi: 10.1007/s00192-021-04877-w
46. Berhe, A, Alamer, A, Negash, K, and Assefa, B. Urinary incontinence and associated factors among pregnant women attending antenatal care in public health facilities of Mekelle city, Tigray, Ethiopia. Women’s Health. (2020) 16:1745506520952009. doi: 10.1177/1745506520952009
47. Liu, W, and Qian, L. Risk factors for postpartum stress urinary incontinence: a prospective study. BMC Urol. (2024) 24:42. doi: 10.1186/s12894-024-01430-x
48. Alshenqeti, AM, Almutairi, RE, and Keram, AM. Impact of urinary incontinence on quality of life among women of childbearing age in Al Madinah Al Munawara, Saudi Arabia. Cureus. (2022) 14:e24886. doi: 10.7759/cureus.24886
49. Gao, J, Liu, X, Zuo, Y, and Li, X. Risk factors of postpartum stress urinary incontinence in primiparas: what should we care. Medicine. (2021) 100:e25796. doi: 10.1097/MD.0000000000025796
50. Liang, C-C, Chao, M, Chang, S-D, and Chiu, SYH. Impact of prepregnancy body mass index on pregnancy outcomes, incidence of urinary incontinence and quality of life during pregnancy—an observational cohort study. Biom J. (2020) 43:476–83. doi: 10.1016/j.bj.2019.11.001
51. Cho, ST, and Kim, KH. Pelvic floor muscle exercise and training for coping with urinary incontinence. J Exerc Rehabil. (2021) 17:379–87. doi: 10.12965/jer.2142666.333
52. López-Pérez, MP, Afanador-Restrepo, DF, Rivas-Campo, Y, Hita-Contreras, F, Carcelén-Fraile, MC, Castellote-Caballero, Y, et al. Pelvic floor muscle exercises as a treatment for urinary incontinence in postmenopausal women: a systematic review of randomized controlled trials. Healthcare. (2023) 11:216. doi: 10.3390/healthcare11020216
53. Rendón-Galvez, N, and Tamayo-Perdomo, G. Physiotherapist role and the importance of comprehensive sex education in women. Rev Investig Innov Cienc Salud. (2022) 4:125–36. doi: 10.46634/riics.82
54. Viana, R, Viana, S, Neto, F, and Mascarenhas, T. Adaptation and validation of the King’s Health Questionnaire in Portuguese women with urinary incontinence. Int Urogynecol J. (2015) 26:1027–33. doi: 10.1007/s00192-015-2628-6
55. Pires, TF, Pires, PM, Costa, R, and Viana, R. Effects of pelvic floor muscle training in pregnant women. Porto Biomed J. (2020) 5:e077. doi: 10.1097/j.pbj.0000000000000077
56. Siyoum, M, Teklesilasie, W, Alelgn, Y, and Astatkie, A. Inequality in healthcare-seeking behavior among women with pelvic organ prolapse: a systematic review and narrative synthesis. BMC Womens Health. (2023) 23:222. doi: 10.1186/s12905-023-02367-3
57. Hammad, F. Prevalence, social impact and help-seeking behaviour among women with urinary incontinence in the Gulf countries: a systematic review. Eur J Obstet Gynecol Reprod Biol. (2021) 266:150–6. doi: 10.1016/j.ejogrb.2021.10.005
58. Vallana Sala, VV. “A enfermidade normal”: Aspectos históricos e políticos da medicalização do parto. Sex Salud Soc. (2020):90–107. doi: 10.1590/1984-6487.sess.2020.34.06.a
59. Jarbøl, DE, Haastrup, PF, Rasmussen, S, Søndergaaard, J, and Balasubramaniam, K. Women’s barriers for contacting their general practitioner when bothered by urinary incontinence: a population-based cross-sectional study. BMC Urol. (2021) 21:99. doi: 10.1186/s12894-021-00864-x
60. Garg, P, Goyal, LD, Goyal, S, and Verma, M. Utility of opportunistic screening to assess the impact of urinary incontinence on quality of life and barriers to seeking treatment among women attending a tertiary healthcare Centre in North India. BMC Urol. (2024) 24:50. doi: 10.1186/s12894-024-01434-7
Keywords: pelvic floor, prevalence, quality of life, urinary incontinence, women
Citation: Sologuren-García G, Linares CL, Flores JR, Escobar-Bermejo G, Sotelo-Gonzales S and Fagerstrom CK (2024) Associated factors and quality of life in women with urinary incontinence in southern Peru, 2023. Front. Public Health. 12:1487330. doi: 10.3389/fpubh.2024.1487330
Edited by:
Tracy Reibel, Murdoch University, AustraliaReviewed by:
Ilce Ferreira Da Silva, Fundação Oswaldo Cruz, BrazilRui Viana, Fernando Pessoa Foundation, Portugal
Copyright © 2024 Sologuren-García, Linares, Flores, Escobar-Bermejo, Sotelo-Gonzales and Fagerstrom. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gema Sologuren-García, Z3NvbG9ndXJlbmdAdW5qYmcuZWR1LnBl
†ORCID: Gema Sologuren-García, orcid.org/0000-0002-6675-0635
Carmen L. Linares, orcid.org/0000-0003-4111-6336
Jackeline R. Flores, orcid.org/0000-0002-1740-615X
Gloria Escobar-Bermejo, orcid.org/0000-0001-8818-4374
Soledad Sotelo-Gonzales, orcid.org/0000-0002-1301-575X
Cristhel K. Fagerstrom, orcid.org/0000-0003-4406-9862
 Gema Sologuren-García
Gema Sologuren-García Carmen L. Linares1†
Carmen L. Linares1†