- 1Ministry of Health Holding (MOHH), Singapore, Singapore
- 2Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 3Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 4Department of Neonatology, Khoo Teck Puat-National University Children’s Medical Institute, National University Hospital, Singapore, Singapore
Introduction: The incidence of pediatric tracheostomy is on the rise. More children are undergoing tracheostomy at a younger age and living longer and cared for at home. Caring for children with tracheostomy affects the caregivers’ Quality of Life (QOL) and caregiver burden. We undertook a systematic review and meta-analysis to determine the impact of pediatric tracheostomy on caregivers’ QOL and caregiver burden.
Methods: We performed a search for quantitative studies measuring QOL, caregiver burden and related factors such as psychological distress, coping, stress, and financial strain using validated instruments, reported by caregivers of children with tracheostomy. We searched PubMed, Embase, Cochrane Central Register of Clinical Trials, CINAHL, and PsycINFO with the following search terms: “pediatrics,” “tracheostomy,” “quality of life,” “caregivers,” “care burden” from the inception of respective databases to 23rd May 2024. Meta-analysis was conducted using R (version 4.3.1).
Results: Twenty-three studies (1,299 caregivers) were included in systematic review. Seven studies (469 caregivers) using Pediatric Quality of Life Family Integrated Module underwent meta-analysis. The pooled mean total family impact score, parental health-related QOL, family functioning score were 70.29 [95% CI, 61.20–79.37], 69.27 [95% CI, 60.88–77.67], and 72.96 [95% CI, 65.92–80.00] respectively. Other key instruments were the Pediatric Tracheostomy Health Status Instrument and Zarit Burden Interview. Qualitative synthesis identified several risk factors for lower QOL and higher caregiver burden: comorbidities in children, younger age at tracheostomy, need for additional medical equipment, presence of older siblings, higher financial strain, being the sole caregiver or being unmarried, and maternal depression. Caregivers’ QOL correlated positively with coping and negatively with stress which is, in turn, associated with medical complications in the first year and the duration of tracheostomy. About 40% of mothers experienced moderate to severe caregiver burden while caring for their children with tracheostomy and this was significantly correlated with depression. Encouragingly, parents also reported positive experience including closeness of the family, feeling stronger, and having a strong sense of mastery.
Discussion: Caregivers of children with tracheostomy experience low QOL and high caregiver burden, which were exacerbated by various medical and psychosocial factors. QOL should be assessed during clinical encounters to identify caregivers who require additional support which includes learning coping and stress reduction strategies.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=334457, identifier CRD42022334457.
1 Introduction
The incidence of pediatric tracheostomy is on the rise in many countries (1). The common indications for pediatric tracheostomy have shifted from treatment of acute airway obstruction to respiratory care of children with medically complex conditions. More children are undergoing tracheostomy at a younger age and living longer and cared for at home (2). After the hospital discharge, these children are looked after by family caregivers, typically their parents, with variable support from the healthcare services (3).
Caregivers of children with tracheostomies are required to perform multiple tasks at home, including cleaning, changing, suctioning the tracheostomy, and administering medications (4). These tasks are typically performed by trained professionals in hospital settings. Caregivers of a pediatric tracheostomy patient must remain in a constant state of vigilance, monitoring the child for emergencies such as accidental dislodgement, tube blockage by secretions, and equipment malfunctions. The duration of a tracheostomy varies depending on the child’s underlying medical condition. For certain conditions, such as neuromuscular disabilities, the need for a tracheostomy can be lifelong. In contrast, some pediatric conditions, such as chronic lung disease of prematurity, tend to improve over time, allowing for the successful reversal of the tracheostomy (5).
Caregiver burden is an individual’s measure of impact on their physical, psychological, emotional and financial wellbeing when taking care of the patient (6) and the caregiver’s perception of how well they are coping with their duties in response to the demands by the person receiving the care (7). Caregiver burden has many negative consequences on the wellbeing of the caregivers (8). For example, in a study involving caregivers of children with cerebral palsy, risk factors for caregiver burden were single parenthood, perceived ability to cope with caregiving, perceived family functioning, financial status, community support and child’s needs (9). In the context of tracheostomy care, caregiver burden affects several aspects of their wellbeing: physical (e.g., higher home care responsibilities), psychological (e.g., constant worry about emergencies), emotional (e.g., child’s inability to speak like other children) and financial (e.g., increased cost of frequent medical visits, consumables, and equipment) (10).
Quality of Life (QOL), as an overlapping concept to caregiver burden, is defined as an “individual’s perception of their position in life in the context of the culture and value systems in which they live in, and in relation to their goals, expectations, standards and concerns” (11). It is an important marker of functional abilities associated with an illness (12). A recent review determined that caregiver burden integrates the impact on all facets of caregiver wellbeing with higher specificity compared to QOL measures, while QOL is better at integrating different facets of caregiver wellbeing but with less specificity than caregiver burden (13).
A systematic review of adult patients with tracheostomies and their caregivers reported a range of mostly negative experiences related to the care, support, and management of a tracheostomy, speech and communication, wellbeing and QOL, disfigurement and body image, stigma and social withdrawal (14). Qualitative studies of caregivers of ventilator-dependent children, many with tracheostomies, reported high levels of caregiver stress, emotional strains, negative impact on family relationship, decision regret, living with daily threats of death, and need to devote extraordinary care and attention to their children’s need (15, 16).
However, there is a paucity of systematic reviews and meta-analyses on quantitative studies of QOL and burden experienced by caregivers of pediatric tracheostomy patients. Therefore, we undertook this systematic review and meta-analysis with the primary aim of synthesizing the effect of caring for tracheostomized children on caregivers’ QOL and caregiver burden. We chose to include both QOL and caregiver burden in our review to comprehensively capture various facets that can impact caregiver wellbeing. Our secondary aim is to identify factors associated with lower QOL and higher caregiver burden, in order to propose measures to improve caregiver QOL.
2 Methods
2.1 Search strategy
We conducted this systematic review and meta-analysis according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (17) and Meta-analysis of Observational Studies in Epidemiology or MOOSE (Supplementary material 1) (18). We registered the protocol with the International Prospective Register of Systematic Reviews (PROSPERO) in June 2022 (PROSPERO registration: CRD42022334457).
We searched PubMed, Embase, Cochrane Central Register of Clinical Trials, CINAHL, and PsycINFO from the inception of respective databases to 23rd May 2024. We also searched grey literature and bibliography of included articles. The search strategy was devised in conjunction with a medical librarian with expertise in systematic review (Supplementary material 2).
2.2 Inclusion and exclusion criteria
We included studies reporting on quantitative QOL data or caregiver burden among caregivers of children with tracheostomy using validated instruments completed by caregivers. Studies investigating the relationship between caregiver burden and QOL with other related factors (e.g., psychological distress, coping, stress, financial burden) were included. We excluded articles that primarily studied cost of care, medical issues such as death and complications, outcomes of interventions, and validation of instruments. We also excluded review articles, conference reports, dissertations, abstracts, and articles in non-English languages.
2.3 Study selection and data extraction
Two review authors independently performed two-step process of screening—first by title and abstract, followed by full text of articles for study eligibility. Two review authors independently extracted relevant data from the included studies. We contacted authors of primary studies for missing data and clarifications. Discrepancies were resolved through team discussions.
2.4 Quality appraisal
Two review authors independently performed quality appraisal using a modified version of Newcastle-Ottawa Scale (NOS) for cross sectional studies (19).
2.5 Data synthesis and meta-analysis
We performed meta-analysis using R (version 4.3.1) if analyzable data were available from four or more studies. A random effects model was used due to heterogeneity of studies. We evaluated I2 statistics according to the Cochrane guidelines (0–40% = no heterogeneity; 30–60% = moderate heterogeneity; 50–90% = substantial heterogeneity; and 75–100% = considerable heterogeneity) (20). All studies underwent qualitative synthesis.
3 Results
A total of 2,726 studies were found from database search. After de-duplication, title and abstract screening, 103 full text articles were retrieved. One article was found from citation search. Finally, 23 studies involving 1,299 caregivers were included in this review (Figure 1). Seven studies (469 caregivers) using Pediatric Quality of Life Family Integrated Module underwent meta-analysis.
We categorized all these studies as cross-sectional studies. Two studies, October et al. (21) and Wyning et al. (22), collected data at two time points but reported comparison using aggregated data (21) or a modeling method (22) instead of tracking individual participant’s data.
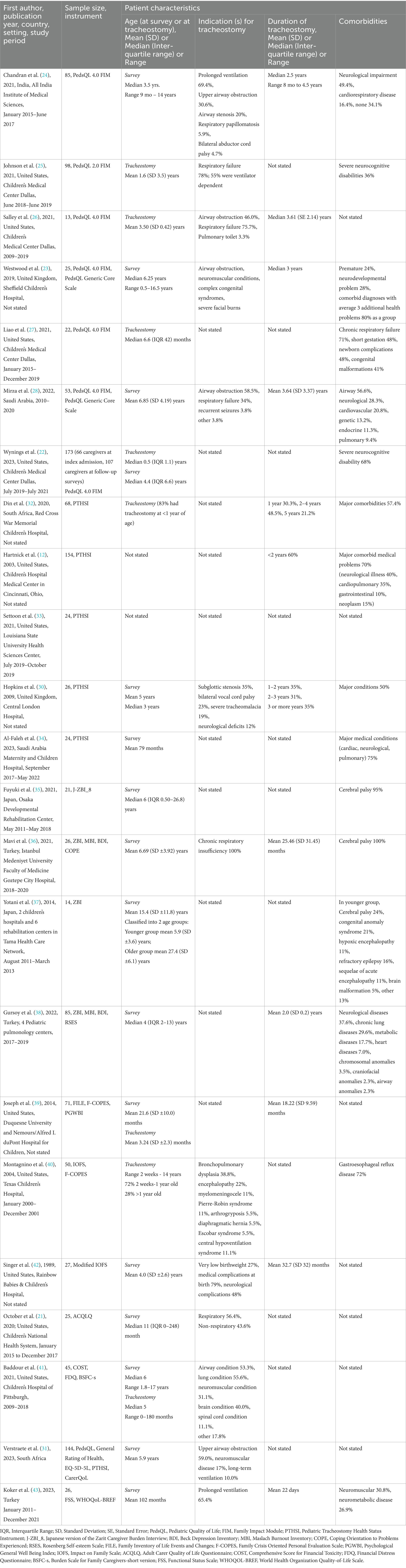
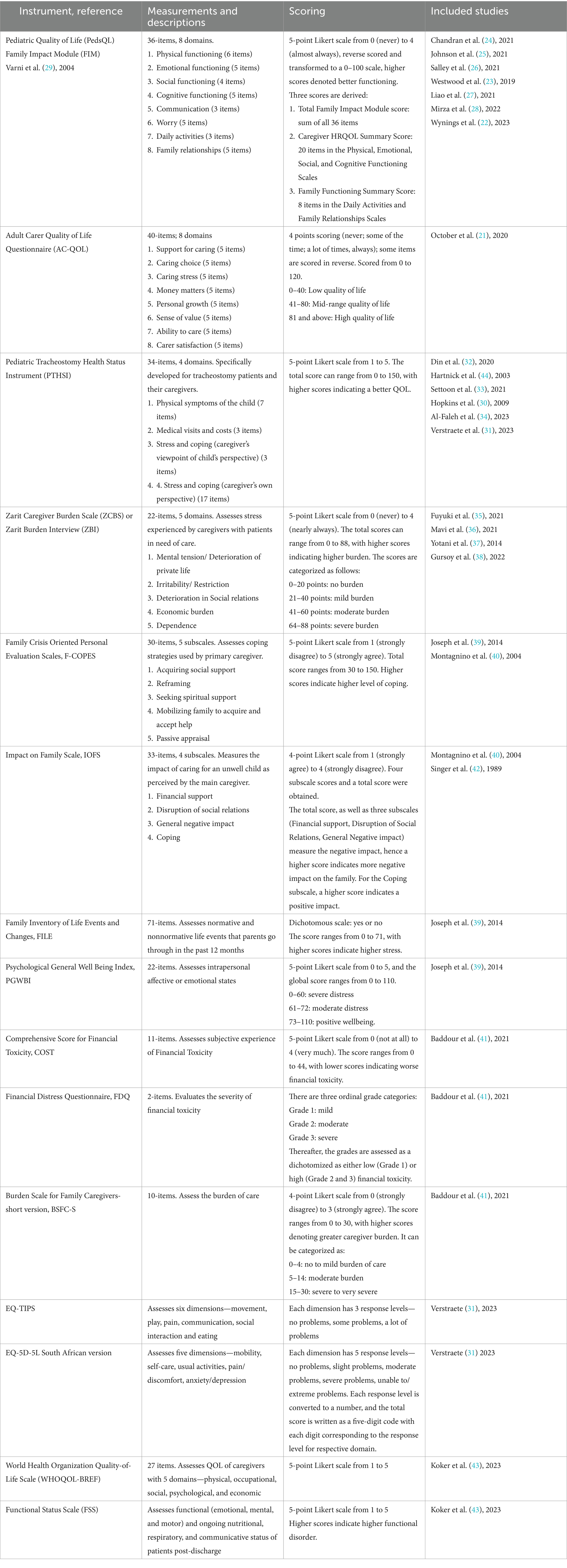
Table 1 displays the studies’ main characteristics which include country, study period, sample size, QOL tool, patient demographics, indication for and duration of tracheostomy and patient comorbidities. Table 2 describes the QOL instruments used, interpretation of scores, and studies which utilized the instruments.
3.1 Quality of the studies
The quality of 22 studies were good or very good, and one was satisfactory (Supplementary material 3). We included all studies in the review.
3.1.1 Meta-analysis of studies using pediatric quality of life family impact module (PedsQL FIM)
We performed meta-analysis on PedsQL FIM scores from seven studies involving 469 caregivers (22–28).
Figure 2 shows the results of meta-analysis on three summary scores. The pooled mean total family impact score was 70.29 (95% CI, 61.20–79.37), mean parental health-related QOL was 69.27 (95% CI, 60.88–77.67), and mean family functioning score (average of 8 items under daily activities and family relationships domains) was 72.96 (95% CI, 65.92–80.00). There was substantial heterogeneity between the studies (I2 = 93–97%, p < 0.01). As a comparison, the PedsQL FIM validation study on medically fragile children with complex chronic diseases in the home setting reported mean total family impact score of 62.49 (SD 17.26); parental health related QOL of 62.94 (SD 19.83); and family functioning score of 68.81 (SD 24.11) (29).
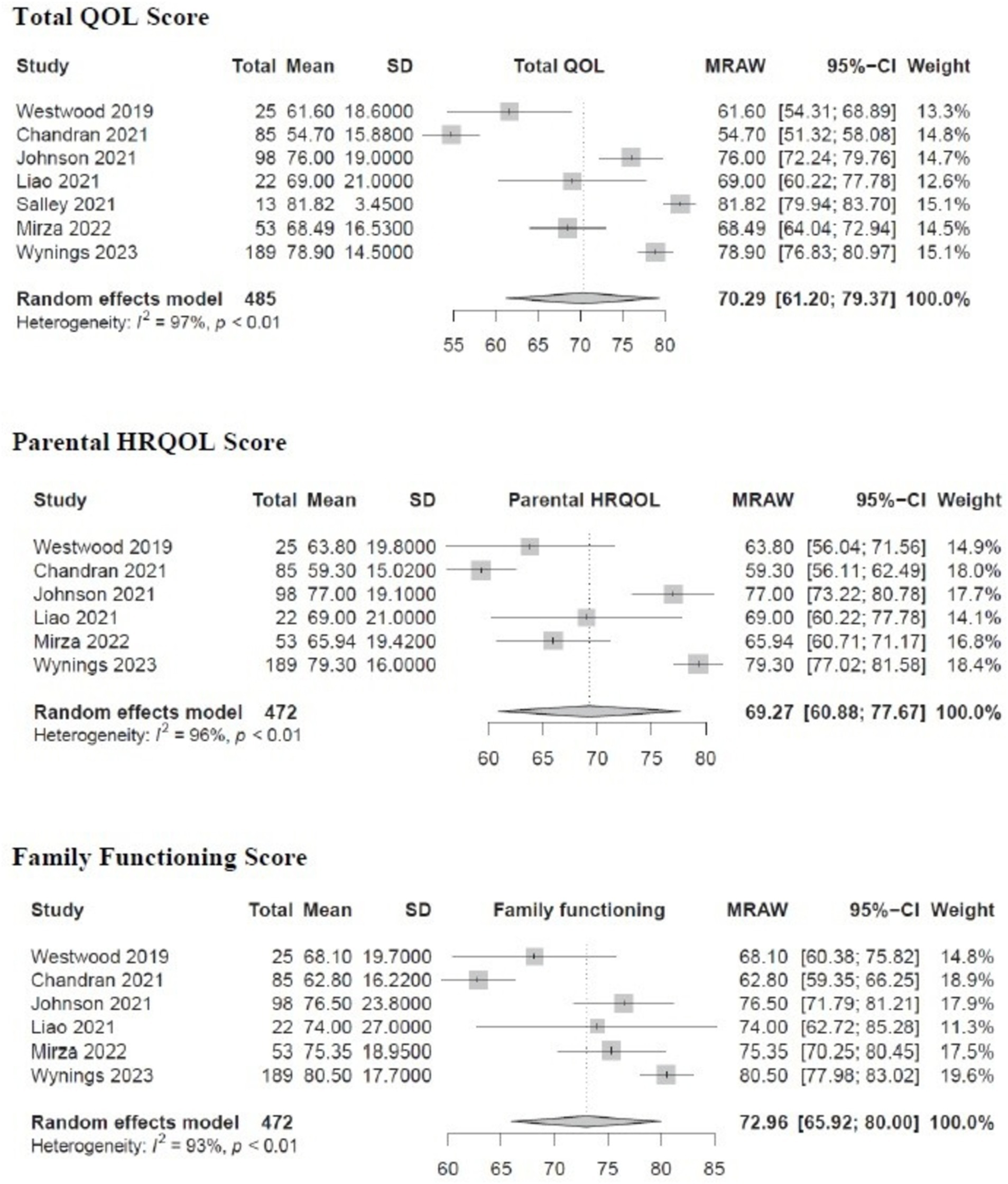
Figure 2. Pooled analysis of total QOL, parental HRQOL and family functioning scores in PedsQL FIM studies.
Supplementary material 4 displays the results of meta-analysis on the eight PedsQL FIM subdomains. The subdomain with the lowest score was worry 61.90 (95% CI, 51.69–72.11), followed by daily activities 64.60 (95% CI, 55.12–74.07). Corresponding scores from PedsQL FIM validation study were: worry 56.82 (SD 25.52) and daily activities 51.89 (SD 31.48) (29). The subdomains with the highest scores were cognitive functioning 80.92 (95% CI, 76.91–84.93) and family relationship 80.38 (95% CI, 70.36–90.40) with the corresponding scores from the validation study: cognitive functioning 74.09 (SD 18.95) and family relationship 78.95 (SD 27.62) (29). There was substantial heterogeneity between the studies (I2 = 79–99%, p < 0.01).
The result from our meta-analysis show higher values in total and sub-domain scores than corresponding values from the original PedsQL FIM validation study by Varni et al. (29). There are several plausible reasons for this finding. The validation study was conducted among families with medically fragile children with complex medical conditions; whereas, more families in this meta-analysis had children with fewer medical comorbidities. Secondly, the validation study was performed in early 2000s when medical care and support system might not have been well developed, whereas studies in this meta-analysis were more recent, published in the last 5 years. Nevertheless, the scores from our meta-analysis are similar to family caregivers caring for children with other chronic medical conditions such as sickle cell diseases, nephrotic syndrome, childhood cancers and congenital cyanotic heart disease (Supplementary material 5) indicating both groups of family caregivers experience low QOL.
3.1.2 Qualitative synthesis of PedsQL FIM studies
Chandran et al. determined that caregivers performed well in the cognitive functioning subdomain. Despite lower scores in other areas, caregiving seemed to have less impact on caregivers’ concentration, memory, and thought processes (24). Salley et al. reported higher overall QOL scores, with the family relationship subdomain scoring the highest (26). However, this finding might be influenced by response bias due to a small sample size (only 13 out of 337 parents participated) (26). Similarly, Westwood et al. also reported higher scores in cognitive functioning and family relationships (23).
Chandran et al. (24) and Johnson et al. (25) found no significant association between indications for tracheostomy and QOL scores. Chandran et al. highlighted significantly poorer QOL across all three summary scores (total family impact score, parental Health-Related QOL (HR-QOL) and family functioning score) in caregivers of children with co-morbidities. Additionally, caregivers of children ≤6 years old had lower parental HR-QOL and family functioning scores (24). Liao et al. observed no significant differences in scores between socioeconomically ‘less disadvantaged’ and ‘more disadvantaged’ groups (27). Wynings et al. studied the largest cohort (255 patients) and found that emotional functioning improved over time (22). Caregivers’ wellbeing had the most significant impact on QOL, regardless of the child’s underlying conditions (22). Mirza et al. found that the highest scores were in cognitive functioning, followed by communication. Within the family functioning summary score, which consists of two domains, parents reported higher scores in family relationships than in daily activities. This indicates that while parents are burdened with the additional daily activities required to care for children with tracheostomies, their family relationships remain better preserved (28).
In summary, these studies show that caregivers of tracheostomized children have better QOL in the cognitive functioning and family relationships subdomains. There is no association between tracheostomy indications and QOL scores. However, caregivers of younger children or those with co-morbidities tend to have lower QOL and family functioning scores.
3.2 Qualitative synthesis of remaining studies measuring QOL and caregiver burden
We performed qualitative synthesis on the remaining 16 studies involving 830 caregivers. Six studies (12, 30–34) used the Pediatric Tracheostomy Health Status Instrument (PTHSI), four studies (35–38) used the Zarit Burden Interview (ZBI) which is also known as Zarit Caregiver Burden Score (ZCBS), and six studies (21, 39–43) used a combination of other instruments. We could not perform any meta-analysis due to incomplete data and heterogeneity of the instruments used.
3.2.1 Studies based on PTHSI
PTHSI is a specific tool to assess QOL of tracheotomized children in four domains: physical symptoms of the child, medical visits and cost, caregiver’s viewpoint of child’s psychological health, and parent’s perspective of caregiver burden (44). The last domain represents caregiver burden which is analyzed in this review.
Hartnick et al. (12) and Hopkins et al. (30) found that caregiver burden was significantly related to the parent’s perception of the child’s health and the economic cost of care (12). Din et al. (32), Settoon et al. (33), and Al-Faleh et al. (34) found that parents of tracheotomized children with major medical conditions experienced a higher burden, but this burden did not differ according to family income. Verstraete et al. found that many caregivers derived some fulfillment from caring for their children, but were unable to focus on their own needs (31). Overall, these studies suggest that caregivers’ QOL is deeply intertwined with their children’s illness severity and QOL, indicating an improvement in children’s health status may have a positive impact on their parents’ QOL.
3.2.2 Studies based on ZBI
Fuyuki et al. found that the quality of patient’s relationship with other family members besides the main caregiver was better in low care burden groups than in high care burden groups, suggesting the level of care burden can affect familial relationships (35). Yotani et al. reported age-related differences in caregiver burden. For caregivers of younger patients (<15 years), there was no link between caregiver burden and need for home mechanical ventilation. However, caregiver burden increased with the presence of older siblings, indicating that family dynamics play a role in caregiver stress (37).
Mavi et al. studied mothers of children with cerebral palsy and chronic respiratory insufficiency and identified differences in coping mechanisms. Mothers of children without tracheostomy showed more active coping, utilized emotional/social support networks, and demonstrated more acceptance than mothers of children with tracheostomy (36). Gursoy et al. examined the correlation between caregiver burden and mental health (38). They found that 40% of mothers experienced moderate to severe caregiver burden, and this was significantly correlated with depression. Caregiver burden did not significantly differ based on maternal education, occupation, tracheostomy duration, or child’s age (38).
3.2.3 Studies using other instruments
Joseph et al. studied the impact of stress and coping on caregiver’s QOL (39). They found that caregiver QOL correlated positively with coping strategies and negatively with stress levels, indicating that effective coping mechanisms can mitigate the distress experienced by caregivers. Singer et al. assessed the impact of a tracheotomized child’s disability on family life and maternal perception of stress (42). There was a significant association between financial stress, younger age at tracheostomy, and medical complications during the first year. Maternal stress was associated with medical complications in the first year and the duration of tracheostomy. Encouragingly, parents also reported positive experience including closeness of the family, feeling stronger, and having a strong sense of mastery (42)—similar to findings in meta-analysis of PedsQL FIM studies which demonstrated high family functioning score.
Montagnino et al. found a positive correlation between a family’s economic status and their ability to access community resources, suggesting that financial stability can enhance support for caregivers (40). October et al. reported minimal changes in caregiver QOL scores shortly after the decision for tracheostomy, implying that caregivers may need time to adjust to the new care demands (21). Baddour et al. explored the concept of financial toxicity and determined higher financial toxicity was associated with increased caregiver burden (41). Lastly, Koker et al. found that a child’s worsening functional status negatively affected caregiver QOL across various domains (43).
In summary, these studies highlight how the complex interplay of stress, coping mechanisms, financial stability, adjustment period, and the child’s functional status influence the QOL of caregivers of children with tracheostomy. They underscore the need for comprehensive support systems and targeted interventions to improve caregivers’ QOL.
4 Discussion
To the best of our knowledge, this is the first comprehensive systematic review and meta-analysis on caregiving burden and QOL of family caregivers of children with tracheostomy. Caring for young children with tracheostomy negatively affects caregivers’ QOL, imposes additional burden on them, results in high level of stress and depression, and impairs their family functioning. Among the subdomains, ‘worry’ and ‘daily activities’ were the most negatively affected domains, while ‘cognitive functioning’ and ‘family relationship’ were the least affected domains.
Risk factors for poorer QOL and higher caregiver burden include caring for children with associated comorbidities (12, 24, 32), younger age at tracheostomy (24), poor functional status (43), need for additional therapeutic interventions (35), having a healthy school-going older sibling (37), higher financial strain (41), being the sole caregiver and being unmarried (41), and maternal depression (38). Indication for tracheostomy (24, 25, 28) and duration of tracheostomy (32, 38) did not have a consistent association with caregiver’s QOL and caregiver burden. Moderate and severe caregiver burden was associated with maternal depression, but not correlated with educational level, duration of tracheostomy and age of children (38).
We found correlations between stress, coping, and caregiver burden. Previous studies in caregivers of medically vulnerable children established a close link between caregivers’ wellbeing and health, and psychosocial outcomes which included higher risks of child abuse and neglect (45). Tracheostomy adversely impacts family’s finances, employment opportunity of the family caregivers, and the family’s ability to provide required services to the patients (41), which can result in suboptimal care of the tracheotomized child. Conversely, higher QOL scores are associated with better coping and lower stress levels (39) and improved psychosocial health in caregivers (28).
Although worry was the worst affected sub-domain, it is encouraging to note that the study with the largest cohort reported improvement in worry and emotional functioning over time (28). Family caregivers of a child with tracheostomy struggle to balance performing multiple tasks associated with tracheostomy care while assuming the typical role of parents. However, parents’ worry lessens as they become more competent with tracheostomy care and when provided with additional support. As psychosocial health has the largest impact on caregivers’ QOL (28), medical providers should target interventions to allay parental anxiety and worry and counsel them about active coping strategies.
Measurements of both generic QOL and disease/condition specific-QOL are useful. Generic QOL instruments allow comparison with caregivers of healthy children or children with other chronic medical conditions. Condition specific QOL instruments can provide deeper and relevant insights into caregiver experiences (44). For example, studies using PTHSI revealed associations between caregiver burden with cost of care (12), parental perception of child’s health (12), and caregiver’s perspective of child’s QOL (30) which may not be captured efficiently by generic instruments.
4.1 Strengths and limitations
We included both caregiver burden and QOL to broadly assess the impact of tracheostomy on family caregivers. Our work builds up on the knowledge base synthesized in a recent systematic review by Acorda et al. whose primary objective was to identify instruments used to measure psychosocial outcomes of caregivers of children with tracheostomy (46). In comparison, our principal objective was to synthesize the findings from primary studies with a secondary objectives of identifying factors affecting caregiver burden and QOL. Our review includes additional primary studies and a meta-analysis.
We would like to highlight several limitations. Studies were heterogeneous due to the variations in instruments used, age of patients, indications and duration of tracheostomy, and presence of concomitant conditions. Majority of caregivers were females (i.e., mothers) with underrepresentation of other family caregivers. There was a paucity of studies that evaluated QOL longitudinally over time. Our review focused on parental QOL and caregiver burden and did not explore the effect of tracheostomy on issues such as disfigurement, body-image, self-confidence, guilt and social isolation which have been reported among adults with tracheostomy (14).
4.2 Implications for practice, research and education
Our review suggests that assessment of QOL and caregiver burden should be a routine part of comprehensive assessment of tracheostomy patients at every touch point. Findings from this review can be used to counsel parents in preparing for their child’s tracheostomy and aid in the process of consent taking.
Based on our review, we identified the following risk factors of poorer caregiver QOL: presence of associated comorbidities in the children, early age of tracheostomy, longer duration of tracheostomy and a lack of social support. The risk factors for higher caregiver burden include need for additional medical equipment, older patients with home mechanical ventilation, having a healthy school going older sibling, being the sole caregiver and being unmarried. These risk factors can be used as a screening tool by healthcare providers to identify caregivers at high risk for poor QOL and caregiver burden (Table 3). As caregivers are integral to the patient’s recovery; efforts should be made to ensure caregiver’s coping so that they feel supported in this journey.
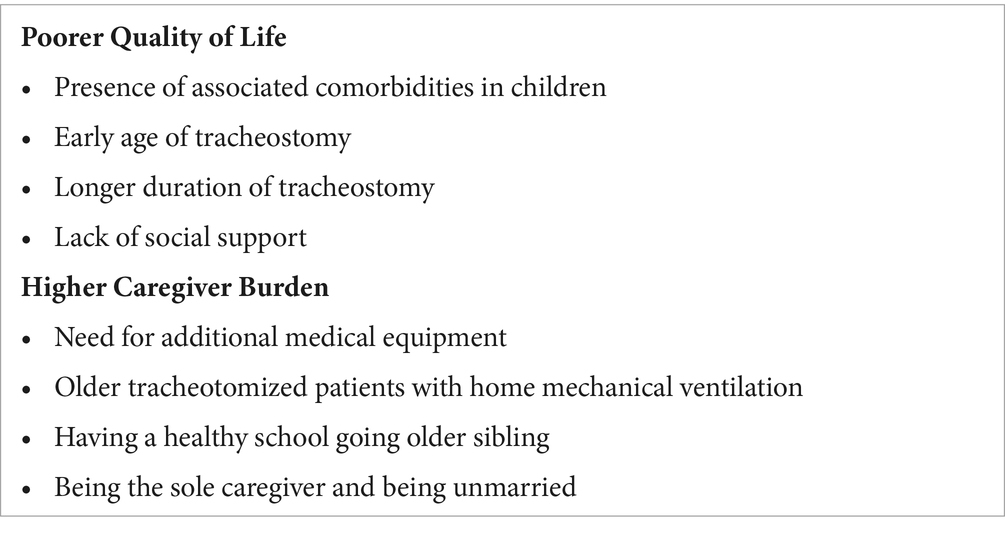
Table 3. Screening tool for providers to identify caregivers at risk of poor QOL and caregiver burden.
4.3 Conclusion
We suggest that longitudinal assessment of QOL and caregiver burden should be routinely performed for comprehensive management of children with tracheostomy. This will identify caregivers who need additional assistance and enable relevant stakeholders to implement targeted interventions to improve caregiver’s QOL. Both generic QOL tools and tracheostomy-specific QOL tools are useful to assess parental QOL. We also recommend teaching family caregivers coping and stress reduction strategies, as better coping and reduced stress result in higher caregiver QOL, which in turn may improve family’s wellbeing and outcomes of children with tracheostomies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
WA: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. NO: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. SY: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. NJ: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. GK: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. N-AL: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. ZA: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. YN: Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1485544/full#supplementary-material
References
1. Mahida, JB, Asti, L, Boss, EF, Shah, RK, Deans, KJ, Minneci, PC, et al. Tracheostomy placement in children younger than 2 years: 30-day outcomes using the national surgical quality improvement program pediatric. JAMA Otolaryngol Head Neck Surg. (2016) 142:241–6. doi: 10.1001/jamaoto.2015.3302
2. Parrilla, C, Scarano, E, Guidi, ML, Galli, J, and Paludetti, G. Current trends in paediatric tracheostomies. Int J Pediatr Otorhinolaryngol. (2007) 71:1563–7. doi: 10.1016/j.ijporl.2007.06.009
3. Family Caregivers Alliance. Definitions: what do we mean by [internet]. Family Caregivers Alliance. (1996). Available at: https://www.caregiver.org/resource/definitions-0/ (Accessed December 30, 2024).
4. McCormick, ME, Ward, E, Roberson, DW, Shah, RK, Stachler, RJ, and Brenner, MJ. Life after tracheostomy: patient and family perspectives on teaching, transitions, and multidisciplinary teams. Otolaryngol Head Neck Surg. (2015) 153:914–20. doi: 10.1177/0194599815599525
5. Lee, DMX, Tan, AKS, Ng, YPM, and Amin, Z. Quality of life of patients and caregivers affected by bronchopulmonary dysplasia: a systematic review. Qual Life Res. (2023) 32:1859–69. doi: 10.1007/s11136-022-03311-y
6. Chiao, C-Y, Wu, H-S, and Hsiao, C-Y. Caregiver burden for informal caregivers of patients with dementia: a systematic review. Int Nurs Rev. (2015) 62:340–50. doi: 10.1111/inr.12194
7. Montgomery, RJV, and Borgatta, EF. The effects of alternative support strategies on family caregiving. The Gerontologist. (1989) 29:457–64. doi: 10.1093/geront/29.4.457
8. Liu, Z, Heffernan, C, and Tan, J. Caregiver burden: a concept analysis. Int J Nurs Sci. (2020) 7:438–45. doi: 10.1016/j.ijnss.2020.07.012
9. Raina, P, O’Donnell, M, Rosenbaum, P, Brehaut, J, Walter, SD, Russell, D, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. (2005) 115:e626–36. doi: 10.1542/peds.2004-1689
10. Flynn, AP, Carter, B, Bray, L, and Donne, AJ. Parents’ experiences and views of caring for a child with a tracheostomy: a literature review. Int J Pediatr Otorhinolaryngol. (2013) 77:1630–4. doi: 10.1016/j.ijporl.2013.07.020
11. World Health Organization. The World Health Organization Quality of Life (WHOQOL) [internet]. World Health Organization. (2012). Available at: https://www.who.int/tools/whoqol (Accessed December 30, 2024).
12. Hartnick, CJ, Bissell, C, and Parsons, SK. The impact of pediatric tracheotomy on parental caregiver burden and health status. Arch Otolaryngol Head Neck Surg. (2003) 129:1065–9. doi: 10.1001/archotol.129.10.1065
13. Mosquera, I, Vergara, I, Larrañaga, I, Machón, M, Del Río, M, and Calderón, C. Measuring the impact of informal elderly caregiving: a systematic review of tools. Qual Life Res. (2016) 25:1059–92. doi: 10.1007/s11136-015-1159-4
14. Nakarada-Kordic, I, Patterson, N, Wrapson, J, and Reay, SD. A systematic review of patient and caregiver experiences with a tracheostomy. Patient. (2018) 11:175–91. doi: 10.1007/s40271-017-0277-1
15. Falkson, S, Knecht, C, Hellmers, C, and Metzing, S. The perspective of families with a ventilator-dependent child at home. A literature review. J Pediatr Nurs. (2017) 36:213–24. doi: 10.1016/j.pedn.2017.06.021
16. Carnevale, FA, Alexander, E, Davis, M, Rennick, J, and Troini, R. Daily living with distress and enrichment: the moral experience of families with ventilator-assisted children at home. Pediatrics. (2006) 117:e48–60. doi: 10.1542/peds.2005-0789
17. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 Statement: an updated guideline for reporting systematic reviews. BMJ. (2020) 2021:n71. doi: 10.1136/bmj.n71
18. Stroup, DF, Berlin, JA, Morton, SC, Olkin, I, Williamson, GD, Rennie, D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
19. Wells, G, Shea, B, O’Connell, D, Peterson, J, Welch, V, Losos, M, et al. (2021). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [internet]. Department of Epidemiology and Community Medicine, University of Ottawa; Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed December 30, 2024).
20. Higgins, J, Thomas, J, Chandler, J, Cumpston, M, Li, T, Page, M, et al. Cochrane handbook for systematic reviews of interventions version 6.4 (updated August 2023). [Internet] Cochrane. (2023). Available at: www.training.cochrane.org/handbook (Accessed December 30, 2024).
21. October, TW, Jones, AH, Greenlick Michals, H, Hebert, LM, Jiang, J, and Wang, J. Parental conflict, regret, and short-term impact on quality of life in tracheostomy decision-making. Pediatr Crit Care Med. (2020) 21:136–42. doi: 10.1097/PCC.0000000000002109
22. Wynings, EM, Chorney, SR, Brooks, RL, Brown, AF, Sewell, A, Bailey, CH, et al. Caregiver quality of life after pediatric tracheostomy. Int J Pediatr Otorhinolaryngol. (2023) 164:111416. doi: 10.1016/j.ijporl.2022.111416
23. Westwood, EL, Hutchins, JV, and Thevasagayam, R. Quality of life in paediatric tracheostomy patients and their caregivers – a cross-sectional study. Int J Pediatr Otorhinolaryngol. (2019) 127:109606. doi: 10.1016/j.ijporl.2019.109606
24. Chandran, A, Sikka, K, Thakar, A, Lodha, R, Irugu, DVK, Kumar, R, et al. The impact of pediatric tracheostomy on the quality of life of caregivers. Int J Pediatr Otorhinolaryngol. (2021) 149:110854. doi: 10.1016/j.ijporl.2021.110854
25. Johnson, RF, Brown, A, and Brooks, R. The family impact of having a child with a tracheostomy. Laryngoscope. (2021) 131:911–5. doi: 10.1002/lary.29003
26. Salley, JR, Kou, Y, Shah, GB, and Johnson, RF. Comparing long-term outcomes in tracheostomy placed in the first year of life. Laryngoscope. (2021) 131:2115–20. doi: 10.1002/lary.29440
27. Liao, K, Chorney, SR, Brown, AB, Brooks, RL, Sewell, A, Bailey, C, et al. The impact of socioeconomic disadvantage on pediatric tracheostomy outcomes. Laryngoscope. (2021) 131:2603–9. doi: 10.1002/lary.29576
28. Mirza, B, Marouf, A, Abi Sheffah, F, Marghlani, O, Heaphy, J, Alherabi, A, et al. Factors influencing quality of life in children with tracheostomy with emphasis on home care visits: a multi-centre investigation. J Laryngol Otol. (2023) 137:1102–9. doi: 10.1017/S002221512200202X
29. Varni, JW, Sherman, SA, Burwinkle, TM, Dickinson, PE, and Dixon, P. The PedsQL family impact module: preliminary reliability and validity. Health Qual Life Outcomes. (2004) 2:55. doi: 10.1186/1477-7525-2-55
30. Hopkins, C, Whetstone, S, Foster, T, Blaney, S, and Morrison, G. The impact of paediatric tracheostomy on both patient and parent. Int J Pediatr Otorhinolaryngol. (2009) 73:15–20. doi: 10.1016/j.ijporl.2008.09.010
31. Verstraete, J, Booth, C, Booth, J, Peer, S, McGuire, J, Kritzinger, F, et al. Fighting to breathe and fighting for health-related quality of life: measuring the impact of being dependent on technology for breathing on the child and their caregiver. Patient. (2024) 17:65–82. doi: 10.1007/s40271-023-00657-4
32. Din, TF, McGuire, J, Booth, J, Lytwynchuk, A, Fagan, JJ, and Peer, S. The assessment of quality of life in children with tracheostomies and their families in a low to middle income country (LMIC). Int J Pediatr Otorhinolaryngol. (2020) 138:110319. doi: 10.1016/j.ijporl.2020.110319
33. Settoon, C, and Evans, AK. Health literacy rates among pediatric tracheostomy caregivers. Int J Pediatr Otorhinolaryngol. (2021) 142:110560. doi: 10.1016/j.ijporl.2020.110560
34. Al-Faleh, M, Alsheef, H, Al-Anzi, O, Jabaan, R, AlQahtani, SM, and Alabdulmhsin, M. Pediatric tracheostomy: a quality-of-life assessment study in Saudi Arabia. Cureus. (2023) 15:e47235. doi: 10.7759/cureus.47235
35. Fuyuki, M, Yotani, N, Kondo, M, Iijima, Y, Wada, H, Takemoto, K, et al. Factors associated with high care burden of primary caregivers of children with medical complexity after completing a discharge-support program in a recovery center. Brain Dev. (2021) 43:988–96. doi: 10.1016/j.braindev.2021.06.003
36. Mavi, D, Onay, ZR, Karatoprak, EY, Oksay, SC, Ayhan, Y, Bulut, I, et al. Effects of tracheostomy on mothers of children with cerebral palsy. Pediatr Pulmonol. (2021) 56:3991–4000. doi: 10.1002/ppul.25635
37. Yotani, N, Ishiguro, A, Sakai, H, Ohfuji, S, Fukushima, W, and Hirota, Y. Factor-associated caregiver burden in medically complex patients with special health-care needs. Pediatr Int. (2014) 56:742–7. doi: 10.1111/ped.12339
38. Gursoy, TR, Eyuboglu, TS, Aslan, AT, Pekcan, S, Buyukkaya, EZ, Hangul, M, et al. The associations between the clinical course of children with tracheostomy and their mothers’ depression, burnout, burden, and self-esteem. J Clin Nurs. (2023) 32:3412–20. doi: 10.1111/jocn.16450
39. Joseph, RA, Goodfellow, LM, and Simko, LM. Parental quality of life: caring for an infant or toddler with a tracheostomy at home. Neonatal Netw. (2014) 33:86–94. doi: 10.1891/0730-0832.33.2.86
40. Montagnino, BA, and Mauricio, RV. The child with a tracheostomy and gastrostomy: parental stress and coping in the home--a pilot study. Pediatr Nurs. (2004) 30:373–80, 401.
41. Baddour, K, Mady, LJ, Schwarzbach, HL, Sabik, LM, Thomas, TH, McCoy, JL, et al. Exploring caregiver burden and financial toxicity in caregivers of tracheostomy-dependent children. Int J Pediatr Otorhinolaryngol. (2021) 145:110713. doi: 10.1016/j.ijporl.2021.110713
42. Singer, L, and Farkas, KJ. The impact of infant disability on maternal perception of stress. Fam Relat. (1989) 38:444–9. doi: 10.2307/585751
43. Koker, A, Tekerek, NÜ, Nalbant, GŞE, Çebişli, E, and Dursun, O. Factors affecting the quality of life of parents caring for pediatric patients with a tracheostomy. J Pediatr Intensive Care. (2023) 12:330–6. doi: 10.1055/s-0043-1771345
44. Hartnick, CJ, Giambra, BK, Bissell, C, Fitton, CM, Cotton, RT, and Parsons, SK. Final validation of the pediatric tracheotomy health status instrument (PTHSI). Otolaryngol Head Neck Surg. (2002) 126:228–33. doi: 10.1067/mhn.2002.122634
45. Hibbard, RA, and Desch, LWthe Committee on Child Abuse and Neglect, and Council on Children With Disabilities. Maltreatment of children with disabilities. Pediatrics. (2007) 119:1018–25. doi: 10.1542/peds.2007-0565
Keywords: psychological distress, financial burden, stress, coping, parents
Citation: Aung WT, Ong NY, Yeo SQC, Juhari NSB, Kong G, Lim N-A, Amin Z and Ng YPM (2025) Impact of pediatric tracheostomy on family caregivers’ burden and quality of life: a systematic review and meta-analysis. Front. Public Health. 12:1485544. doi: 10.3389/fpubh.2024.1485544
Edited by:
Ali Nawaz Khan, Hubei Engineering University, ChinaReviewed by:
Kathleen Leask Capitulo, Icahn School of Medicine at Mount Sinai, United StatesMina Rostami, Zanjan University of Medical Sciences, Iran
Copyright © 2025 Aung, Ong, Yeo, Juhari, Kong, Lim, Amin and Ng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zubair Amin, cGFlemFAbnVzLmVkdS5zZw==
†ORCID ID: Win Thu Aung, orcid.org/0009-0007-7406-1673
Natasha Yixuan Ong, orcid.org/0000-0001-9537-4539
Shina Qing Chun Yeo, orcid.org/0009-0007-1603-1740
Nur Syahindah Binti Juhari, orcid.org/0009-0002-4727-8600
Gwyneth Kong, orcid.org/0000-0002-3385-5078
Nicole-Ann Lim, orcid.org/0000-0001-8097-6262
Zubair Amin, orcid.org/0000-0002-4430-5012
Yvonne Peng Mei Ng, orcid.org/0000-0003-0497-0306
 Win Thu Aung1†
Win Thu Aung1† Gwyneth Kong
Gwyneth Kong Zubair Amin
Zubair Amin Yvonne Peng Mei Ng
Yvonne Peng Mei Ng