- 1Department of HIV/AIDS Control and Prevention, Guangzhou Center for Disease Control and Prevention, Guangzhou, China
- 2School of Public Health, Guangzhou Medical University, Guangzhou, China
- 3Huangpu District Center for Disease Control and Prevention, Guangzhou, China
- 4Guangdong Association of STD & AIDS Prevention and Control, Guangzhou, China
- 5Lingnan Partner Community Support Center, Guangzhou, China
Background: China has been exploring HIV self-testing (HIVST) among men who have sex with men (MSM) since 2014. Currently, both non-profit and commercial initiatives HIVST services have achieved comprehensive coverage. Investigating the factors influencing the initial adoption of HIVST among MSM in this context can help develop tailored HIVST service strategies of and further promote HIVST adoption among MSM communities.
Methods: We selected 230 participants from a prospective cohort on HIV infection among MSM population in Guangzhou, China, who had no prior experience of HIVST. Among the study participants, 43 who initially adopted HIVST during the follow-up period were designated as the case group, while the rest comprised the control group. Electronic questionnaires were used for baseline and follow-up surveys to collect demographic information, sexual behavior characteristics and HIVST utilization in the past 6 months. Logistic regression models were applied to analyze the factors influencing the initial adoption of HIVST.
Results: Among the study participants, 18.7% (43/230) initially adopted HIVST during the follow-up period. Multivariate logistic regression analysis revealed that individuals who primarily sought sexual partners through offline venues in the past 6 months (aOR = 5.28, 95% CI: 1.01–27.79), had more than one sexual partner in the past 6 months (aOR = 2.76, 95% CI: 1.33–5.74), engaged with more than two casual partners in the past 6 months (aOR = 3.02, 95% CI: 1.35–6.78), or had more than one regular partner (aOR = 3.37, 95% CI: 1.51–7.51) exhibited an increased likelihood of initiating HIVST.
Conclusion: In the context of comprehensive promotion and coverage of HIVST service, the development of personalized, adaptable, and innovative HIVST strategies for MSM with a higher number of sexual partners, particularly those in regular partnerships and those seeking partners offline, may further increase the adoption of HIVST among MSM.
1 Introduction
Epidemiological surveillance data from the Chinese Center for Disease Control and Prevention indicate that, as of the end of 2022, China had approximately 1.22 million people living with HIV/AIDS (PLWHA). The majority of newly reported HIV infection cases stem from sexual transmission, wherein male-to-male sexual transmission constitutes 25.6% (1). Located in southern China, Guangzhou is a major city with a population of 14 million. In Guangzhou, male-to-male sexual transmission has emerged as the predominant pathway of HIV transmission, accounting for over half of the newly reported cases annually. Consequently, interventions aimed at men who have sex with men (MSM) are imperative due to their heightened susceptibility to HIV, rendering them among the most heavily impacted populations in China. Comprehensive interventions, encompassing mobilization of testing among MSM and promotion of treatment for PLWHA among MSM, play a pivotal role in curbing HIV transmission and stemming the epidemic’s dissemination. These endeavors hold paramount significance in managing the HIV epidemic, spanning beyond Guangzhou to the entirety of China (1).
HIV self-testing (HIVST) entails individuals independently collecting samples, conducting self-tests with HIV rapid test kits, and autonomously interpreting the results (2). Due to its convenient and private nature, HIVST has considerable potential for promoting testing in regions and demographics with insufficient offline HIV testing services (3–5). Previous studies suggest that HIVST enhances MSM populations’ inclination and frequency for HIV testing (6), diminishes risky behaviors (7), and heightens awareness of individual HIV infection status (8). Since 2014, the World Health Organization (WHO) has been fostering worldwide endeavors to investigate and advance HIVST within pivotal groups, including MSM (2). The WHO released guidelines on HIVST in 2016, specifically endorsing the incorporation of HIVST as a complementary strategy to conventional HIV testing services (9). By 2020, the utilization and implementation of HIVST had received official approval in a total of 57 countries and regions across the globe (10).
In 2014, China embarked on the exploration of HIVST. The Guangzhou Center for Disease Control and Prevention (Guangzhou CDC), along with the Lingnan Partners Community Support Center, a community-based organization (CBO), collaborated to offer an online platform for MSM individuals to apply for HIVST kits, submit their results, and receive interpretation and consultation (11–13). Consequently, this non-profit HIVST model was extensively promoted nationwide. Consequently, different CBOs in various regions effectively facilitated HIV testing among local MSM populations through this service model of HIVST (14, 15). Following its explicit incorporation in China’s “Thirteenth Five-Year Plan for HIV/AIDS Prevention and Control,” issued by the State Council Office in 2017 (16), which outlined the expansion of HIVST services through diverse channels like pharmacies and online test kit sales, the first urine-based HIVST kit secured regulatory approval and was introduced to the Chinese market in 2019 (17). In the same year, China published its inaugural “Guidebook for HIVST” (5), coinciding with the emergence of commercially-driven HIVST services spearheaded by test kit manufacturers and e-commerce platforms. Capitalizing on substantial advantages in supply channels and marketing, commercial HIVST services have progressively risen to prominence, comprising a substantial proportion of HIVST utilization in China. Consumption data indicates an approximate sale of 400 HIVST kits per hour on e-commerce platforms (18–20). A specific test kit manufacturer in China disclosed an annual sale of 1 million HIVST kits on a designated e-commerce platform (14).
Propelled by both non-profit and commercial initiatives, and facilitated through a range of online and offline channels, China’s HIVST services have transformed into a varied and accessible framework, characterized by wide coverage and significant adoption. Being among the pioneering adopters of HIVST in China, MSM individuals have attained remarkable levels of awareness, acceptance, and utilization (21, 22).
Studies have demonstrated that service accessibility significantly affects the utilization of HIVST (23). Nevertheless, despite the broad range of service provision channels and comprehensive coverage, some MSM individuals have not yet embraced the use of HIVST. This underscores the need, at the present juncture of widespread HIVST service availability, to elevate the utilization rate among MSM individuals. This requires a strategic transition from mere supply augmentation to the cultivation of tailored, inventive, and flexible service models designed for MSM with varying attributes (24–26). These models are intended to address the specific HIVST requirements of diverse subgroups within the MSM population.
Previous investigations into the determinants of HIVST utilization have predominantly consisted of cross-sectional studies, which possess a restricted capacity for causal inference. Many of these studies were conducted when HIVST coverage was relatively limited. The central emphasis was on strategies to achieve significant enhancements in HIVST rates (23, 27–29). Consequently, the majority of research findings provide minimal assistance for advancing promotion, especially after the marginal effects of HIVST service utilization have been attained.
Guangzhou, an early advocate of HIVST services for MSM in China, is additionally a bustling international trade center. At present, the provisioning and coverage of HIVST among the MSM population in Guangzhou have nearly reached a state of saturation. Therefore, this study employs a prospective cohort established within the MSM population in Guangzhou, adopting a nested case-control design. The study aims to investigate factors impacting the initial adoption of HIVST among MSM individuals. The objective is to produce scientific evidence guiding the development of tailored strategies aimed at further bolstering HIVST adoption among MSM communities. In turn, this endeavor fosters the cultivation of consistent testing habits and mitigates HIV transmission within the MSM population.
2 Methods
2.1 Study population and design
We employed a non-matched nested case-control design, the case and control groups were extracted from a prospective cohort on HIV infection among MSM population in Guangzhou.
This cohort was conducted between June 2019 to April 2022, utilizing HIV voluntary counseling and testing (VCT) clinics from 12 CDC and 2 CBO in Guangzhou as field sites. The recruitment process targeted HIV antibody-negative males, aged 18 or above, residing in Guangzhou, who had engaged in male-to-male sexual behavior within the past 6 months. Participants who voluntarily provided informed consent and completed the baseline questionnaire were included in the study. Every 3–6 months, participants were mobilized to return to VCT clinics for follow-up questionnaire surveys and HIV antibody tests. The follow-up ended for individuals who tested positive for HIV antibodies. This study obtained ethical approval from the Ethics Committee of Guangzhou CDC (Approval No: GZCDC-ECHR-2020P0044). All methods were performed in accordance with the relevant guidelines and regulations.
From this cohort, we selected all 230 participants who had no prior experience of HIVST during the baseline survey as the study subjects. Among them, 43 who initial adoption of HIVST during the follow-up period were designated as the case group. The control group consisted of 187 participants who going non-utilize of HIVST throughout the follow-up period.
2.2 Collection of demographic and behavioral information
Both baseline and follow-up data were gathered through electronic questionnaires that we designed ourselves. Trained interviewers conducted surveys with study participants, adhering to standardized protocols. The survey covered demographic information, sexual behavior characteristics from the previous 6 months, utilization of HIVST in the past 6 months, as well as pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) utilization within the same timeframe.
(1) Definition of behavioral characteristics variables for the case group: The questionnaire responses from the latest follow-up survey prior to the initial adoption of HIVST were employed to establish the variables related to behavioral characteristics for the case group. (2) Definition of behavioral characteristics variables for the control group: The questionnaire responses from the most recent follow-up survey were utilized to determine the variables related to behavioral characteristics for the control group participants.
2.3 Statistical analysis
Statistical analyses were performed using SPSS 26.0 software. Descriptive statistics included means and standard deviations for quantitative data in both the case and control groups, while categorical data were presented using frequencies and proportions. Non-matched nested case-control data analysis was performed using a non-conditioned logistic regression model. Preliminary univariate analysis was conducted to explore factors influencing the initial adoption of HIVST. The significant variables identified through univariate analysis were incorporated into separate multivariate models, with each predictor factor analyzed individually while controlling for potential confounders, to prevent multicollinearity from affecting our results. A significance level of p < 0.05 indicated statistical significance for differences.
2.4 Quality control
Prior to data collection, standardized training was provided to interviewers and follow-up personnel to ensure their familiarity with recruitment methods and procedures. Only those who successfully completed the training assessment were allowed to proceed. Baseline and follow-up surveys were administered using electronic questionnaires to prevent omissions, logical errors, and potential issues arising from alterations to paper-based questionnaires or data entry errors. Survey questionnaires were labeled with unique participant codes, and baseline and follow-up questionnaires were consistently archived. Designated personnel were responsible for verification and quality control of the questionnaires. The study did not involve patient names or identifiable information, and all data were treated with strict confidentiality measures.
3 Results
3.1 Demographic characteristics
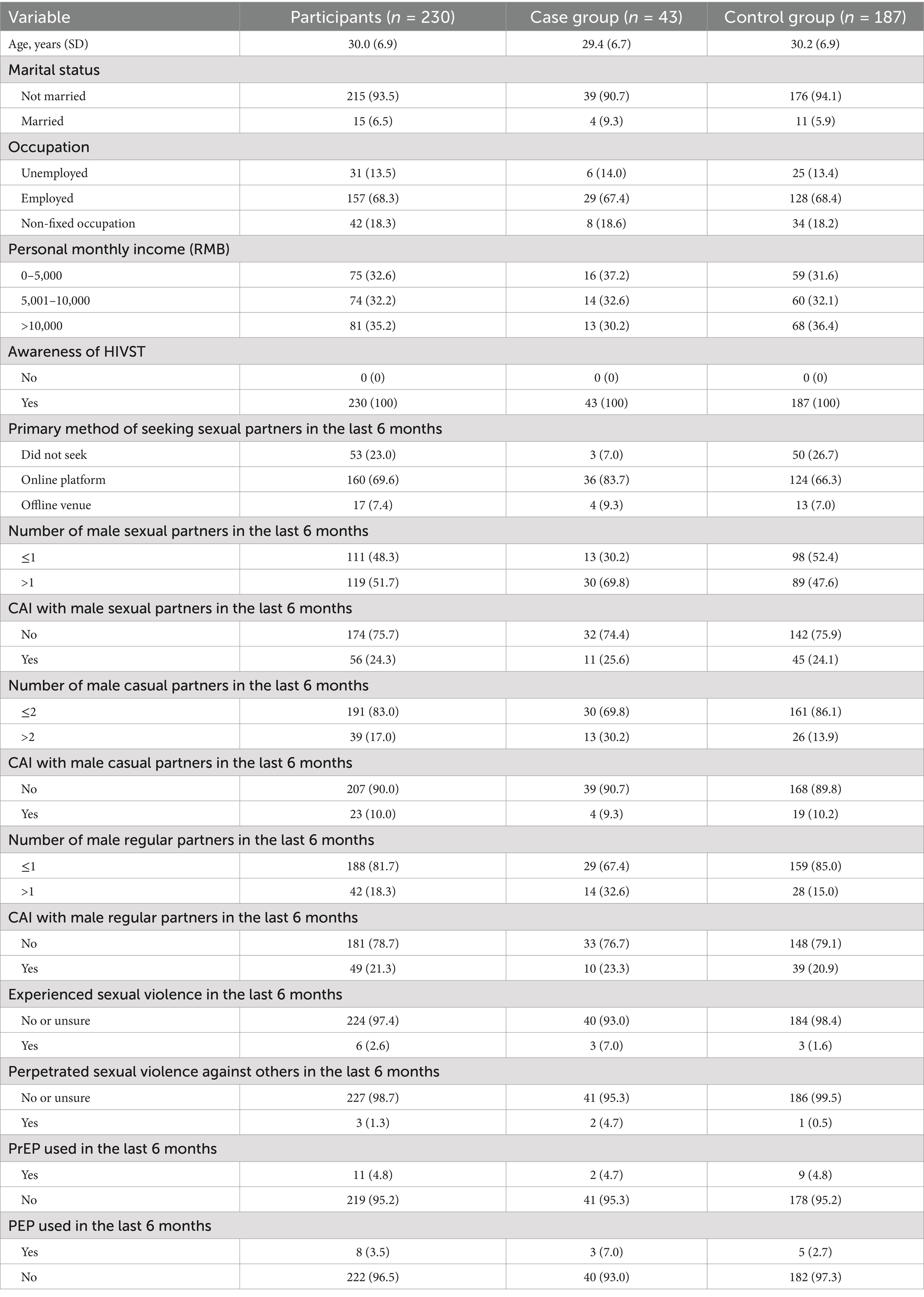
A total of 230 MSM with no prior experience of HIVST were included in this study. The participants had an average age of 30.0 (SD 6.9) years, with the majority being unmarried (93.5%, 215/230) and employed (68.3%, 157/230). Among the study participants, 18.7% (43/230) initially adopted HIVST during the follow-up period and were classified as the case group; the remaining 81.3% (187/230) consistently did not use HIVST and were classified as the control group. Refer to Table 1 for details.
3.2 Sexual behavioral characteristics
All 230 MSM participants demonstrated complete knowledge of HIVST. In the preceding 6 months, 24.3% (56/230) of participants engaged in male-to-male condomless anal intercourse (CAI). Furthermore, 10.0% (23/230) had CAI with male casual partners, and 21.3% (49/230) with male regular partners. Moreover, 51.7% (119/230) reported having more than one male sexual partner during this time. Among them, 17.0% (39/230) had over two male casual partners, and 18.3% (42/230) had more than one male regular partner within the same period.
In the previous 6 months, 2.6% (6/230) of participants reported experiencing sexual violence, and 1.3% (3/230) admitted perpetrating sexual violence against others during the same period. Utilization rates for PrEP and PEP in the past 6 months were 4.8% (11/230) and 3.5% (8/230), respectively.
3.3 Logistic regression analysis of factors influencing the initial adoption of HIVST
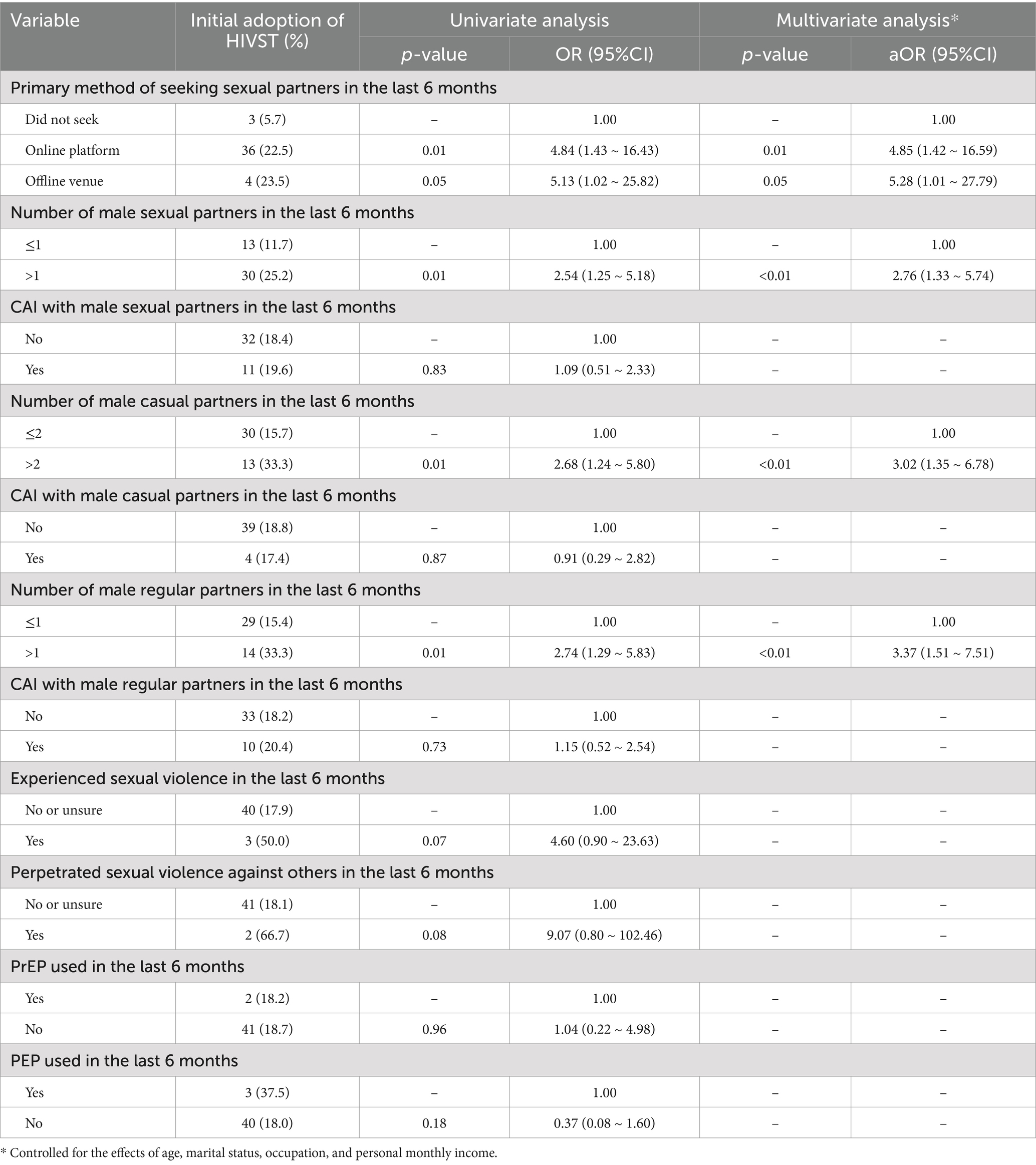
Univariate logistic regression analysis indicated that several factors were linked to the initial adoption of HIVST. These factors included seeking sexual partners through online platforms (OR = 4.84, 95%CI: 1.43–16.43) or offline venues (OR = 5.13, 95%CI: 1.02–25.82), having more than one male sexual partners in the past 6 months (OR = 2.54, 95% CI: 1.25–5.18), having more than two male casual partners in the past 6 months (OR = 2.68, 95% CI: 1.24–5.80), and having more than one male regular partner in the past 6 months (OR = 2.74, 95% CI: 1.29–5.83) (see Table 2).
The results of the multivariate logistic regression analysis, which adjusted for demographic factors, demonstrated that in comparison to those who did not seek sexual partners within the preceding 6 months, seeking sexual partners through online platforms (aOR = 4.85, 95%CI: 1.42–16.59) and offline venues (aOR = 5.28, 95% CI: 1.01–27.79) both appeared to positively influence the initial adoption of HIVST. Importantly, among MSM, those who predominantly sought sexual partners offline exhibited a heightened likelihood of initiating HIVST. Furthermore, individuals with more than one male sexual partners (aOR = 2.76, 95%CI: 1.33–5.74), more than two male casual partners (aOR = 3.02, 95%CI: 1.35–6.78), or more than one male regular partner (aOR = 3.37, 95%CI: 1.51–7.51) demonstrated an elevated probability of initiating HIVST, underscoring a moderately stronger inclination toward HIVST usage among those with a relatively higher number of sexual partners. Refer to Table 2 for details.
We performed an additional stratification of the variable “primary method of seeking sexual partners in the last 6 months” into two categories (online platforms, offline venues) to assess differences in the initial adoption of HIVST. However, the univariate logistic regression analysis revealed no statistically significant difference between those who sought sexual partners offline and those who used online platforms (OR = 1.06, 95% CI: 0.33–3.45).
4 Discussion
Since 2014, global efforts, including those in China, have been dedicated to the widespread promotion and exploration of HIVST services among key populations like MSM (2, 9, 10, 17). Previous research has highlighted the primary challenges in promoting HIVST among China’s MSM population as awareness, accessibility, and financial factors (30–32). However, the past decade has witnessed a significant transformation in the availability of HIVST services. Both public health and commercial sectors now offer a diverse range of HIVST services through online and offline channels, including local CDCs, CBOs, pharmacies, and e-commerce platforms. This expansion has substantially increased awareness and accessibility of HIVST within the Chinese MSM community. As a result, this group can now conveniently access a range of HIVST services that suit their preferences and financial means (11, 14, 18). Despite these advancements, there is a research gap regarding the factors, including barriers and facilitators, that could further enhance HIVST promotion within the context of comprehensive service coverage.
It is crucial to highlight that the follow-up periods for assessing outcomes in both the case and control groups were aligned with the operational phase of VCT services in Guangzhou, avoiding overlap with the service disruptions caused by the COVID-19 pandemic in early 2020. Consequently, participants in both groups were able to freely access HIVST and VCT services. The adoption of HIVST was not exclusively driven by the unavailability of VCT services during the pandemic. Among the prospective cohort of MSM, from which our study sample was derived, only 10.9% (230/2,115) of participants reported having no prior experience with HIVST in the baseline survey. While prior studies have highlighted the role of HIVST awareness in shaping utilization behaviors (33), the 230 MSM included in our study, all of whom with no prior HIVST experience, had already established awareness regarding the availability and access to HIVST services during the baseline survey. This observation further supports the assumption that HIVST service accessibility among MSM in Guangzhou has reached a saturation point (11–13). Despite earlier studies suggesting that service accessibility influences utilization rates positively (23), our findings indicate that merely 18.7% of participants attempted initial HIVST during the follow-up period. This rate is significantly lower than the results of surveys conducted during the initial phase of HIVST promotion in various Chinese cities (15). This disparity suggests that while conventional promotional strategies can somewhat improve MSM awareness of HIVST, their effectiveness in continuously increasing utilization rates might be limited. Consequently, it is crucial to explore innovative and tailored HIVST service models that address the unique characteristics of specific subgroups (24–26).
This study utilized a nested case-control analysis and discovered that MSM exhibiting a higher number of male sexual partners tended to be more inclined toward initially embracing HIVST, aligning with conclusions drawn from earlier cross-sectional investigations and meta-analysis (34–37). Among MSM who recently disclosed having over two male casual partners, the probability of adopting HIVST initially was significantly higher. This heightened probability may arise from their involvement in frequent informal liaisons, fostering increased risk sensitivity and incentivizing them toward HIVST contemplation. Furthermore, this inclination might stem from an arrangement with male casual partners to undertake self-testing either before or after sexual interactions, confirming the HIV-negative status of both parties (38, 39). Moreover, MSM who recently reported having more than one male regular partners were more inclined to initially embrace HIVST. This increased likelihood among individuals having more than one male regular partners could be linked to the comparatively stable and lasting nature of relationships among them. MSM engaged in several male regular partnerships frequently opt to withhold information about other sexual partners from certain partners. To avoid potential conflicts within relationships, they might choose for private HIV testing methods, such as self-testing, to monitor their risk and infection status. These findings indicate the possibility of creating customized HIVST services designed specifically for MSM engaged in several male sexual partnerships. For example, product designs could center on situations that involve testing prior to engaging in sexual activities with male casual partners. Additionally, promotional and marketing strategies could be targeted at MSM engaged in a greater number of regular male-to-male sexual relationships to cater to their distinct testing needs and preferences.
The results of this study also demonstrate that MSM primarily seeking sexual partners offline experience have a significantly higher likelihood of initiating HIVST. MSM who seek sexual partners in places such as parks, public restrooms, clubs, and bathhouses, and engage in sexual behaviors within those venues, are more prone to neglect safety precautions due to factors like on-site conditions and peer influences. This could even lead to condomless group sexual activities (40–42). Furthermore, when they are active in offline settings and forming connections with sexual partners, MSM face challenges in reducing HIV infection risks through awareness of their infection status or pre-sexual behavior testing. Thus, compared to the Internet and social networking platforms, seeking sexual partners offline inherently exposes MSM to a higher risk of HIV infection (43, 44). Perhaps MSM who habitually seek sexual partners through offline venues might overlook risks in the heat of the moment during sexual encounters, but may subsequently express health-related concerns upon recalling their actions or encountering relevant health educational materials. Recognizing the potential risks of HIV infection associated with condomless behavior during that time could act as a motivation for embracing HIVST. These findings indicate a requirement for investigating appropriate HIVST service models in offline contexts. For example, deploying Internet of Things (IoT)-based HIVST services in offline venues frequented by MSM or providing HIVST with the support of key individuals like operators or volunteers in these venues. Furthermore, tailoring the HIVST application and registration process to suit the routines and educational levels of typical offline venue attendees is essential. This approach ensures a direct connection with potential HIVST users, proving more effective than generic online campaigns. By streamlining the process, we can reduce the learning curve and actively engage MSM, thereby enhancing their willingness to adopt these services. Beyond behavioral factors, structural barriers significantly impede the accessibility and utilization of HIVST (45). Despite the extensive HIVST services offered by both non-profit and commercial sectors, the predominant online marketing approach disenfranchises older adult or low-educated MSM who are unfamiliar with Internet operations. This highlights an urgent need to develop services specifically tailored to accommodate the needs of this population.
This study has some limitations. Firstly, our study design did not fully account for potential confounders like healthcare access and participants’ socioeconomic status, which might impact the results. Additionally, the participants were selected from a prospective cohort focusing on HIV infection, with recruitment occurring at VCT clinics. This recruitment strategy could introduce a selection bias, potentially limiting the representativeness of our sample to the broader MSM population. Specifically, our study predominantly includes young-to-middle-aged MSM and may not fully account for those lacking testing experience or practicing irregular testing behaviors. Furthermore, the nested case-control design may not conclusively establish causality among the variables.
In conclusion, directing efforts toward MSM with a higher number of sexual partners, especially those involved in regular partnerships and those seeking partners offline, through the creation of personalized, adaptable, and inventive HIVST strategies, may enhance the adoption of HIVST among MSM. This strategy may offer advantages, particularly considering the existing high awareness and extensive service availability of HIVST for this demographic.
Data availability statement
The datasets presented in this article are not readily available because our institution has a data access and sharing policy that outlines the procedures for data storage, access, and eventual sharing or archiving of data. We are bound by these policies. Requests to access the datasets should be directed to Yuzhou Gu, eXVjaG91a29vQGZveG1haWwuY29t.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Guangzhou CDC (Approval No: GZCDC-ECHR-2020P0044). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their electronic informed consent to participate in this study.
Author contributions
YG: Conceptualization, Data curation, Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing, Methodology. JY: Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing. YeL: Investigation, Methodology, Supervision, Validation, Writing – original draft. LZ: Data curation, Investigation, Writing – original draft. FL: Investigation, Supervision, Writing – original draft. WZ: Investigation, Writing – original draft. HX: Project administration, Writing – review & editing. YoL: Investigation, Writing – review & editing. YC: Project administration, Resources, Supervision, Writing – review & editing. ZH: Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by National Natural Science Foundation of China (72204059, 71974212), Scientific Research Plan Project of Guangzhou (202201010078), and Guangdong Basic and Applied Basic Research Foundation (2020A1515010737). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Acknowledgments
We thank 12 district disease control and prevention centers and 2 MSM community based organizations in Guangzhou for supporting this study and giving their permission to publish these data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Han, MJ. Analysis of the epidemic situation of AIDS and prospect of prevention and control in China. Chin J AIDS STD. (2023) 29:247–50. doi: 10.13419/j.cnki.aids.2023.03.01
2. World Health Organization. (2019). Consolidated guidelines on HIV testing services. Available at: https://www.who.int/publications/i/item/978-92-4-155058-1 (Accessed July 15, 2023).
3. Ren, XL, Lu, MY, Liu, GW, Zhao, X, and Lu, HY. Progress on self-testing of HIV among men who have sex with men. Capital J Public Health. (2019) 13:42–4. doi: 10.16760/j.cnki.sdggws.2019.01.011
4. Ma, ZH, Yang, YL, and Xing, WG. WHO recommends AIDS self-test. Chin J AIDS STD. (2018) 24:211–2. doi: 10.13419/j.cnki.aids.2018.02.29
5. Chinese Center for Disease Control and Prevention, STD/AIDS prevention and control center. HIV self-testing guidance manual (first edition). (2019).
6. Witzel, TC, Eshun-Wilson, I, Jamil, MS, Tilouche, N, Figueroa, C, Johnson, CC, et al. Comparing the effects of HIV self-testing to standard HIV testing for key populations: a systematic review and meta-analysis. BMC Med. (2020) 18:381. doi: 10.1186/s12916-020-01835-z
7. Ren, XL. The influence of HIV self-testing on seeking facility-based HIV service and risk sexual behaviors among men who have sex with men in Beijing In: Chinese Center for Disease Control and Prevention (2017)
8. United States Center for Disease Control and Prevention. (2022). Notice of funding opportunity PS22-2210: Mass mailing of HIV self-tests to persons disproportionately affected by HIV in the U.S. Available at: https://www.cdc.gov/hiv/funding/announcements/ps22-2210/ (Accessed July 15, 2023).
9. World Health Organization. (2016). Guidelines on HIV self-testing and partner notification: Supplement to consolidated guidelines on HIV testing services. Available at: https://www.who.int/hiv/pub/self-testing/hiv-self-testing-guidelines/en/ (Accessed July 15, 2023).
10. HIV Self-Testing Research and Policy Hub. Data from: Country-level policy and regulatory data. (2020). Available at: https://hivst.fjelltopp.org/policy.
11. Cai, YS, Gu, YZ, Zhong, F, Fan, LX, Zhao, YT, Luo, YF, et al. Applicability and feasibility of “Lingnanzhun”-an “internet plus-based HIV self-testing tool” targeting MSM in Guangzhou. Chin J Epidemiol. (2019) 40:1212–6. doi: 10.3760/cma.j.issn.0254-6450.2019.10.008
12. Wu, QM, Cheng, WB, Zhong, F, Liu, Q, Cai, YS, Lin, P, et al. Lingnanzhun, a HIV self-testing model targeting men who have sex with men. Chin J AIDS STD. (2016) 22:391–3. doi: 10.13419/j.cnki.aids.2016.05.27
13. Zhong, F, Tang, WM, Cheng, WB, Lin, P, Wu, QM, Cai, YS, et al. Acceptability and feasibility of a social entrepreneurship testing model to promote HIV self-testing and linkage to care among men who have sex with men. HIV Med. (2017) 18:376–82. doi: 10.1111/hiv.12437
14. Tang, W, and Wu, D. Opportunities and challenges for HIV self-testing in China. Lancet HIV. (2018) 5:e611–2. doi: 10.1016/s2352-3018(18)30244-3
15. Xiu, XF, Qin, YY, Bao, YG, Chen, YK, Wu, H, Huang, XJ, et al. The practice and potential role of HIV self-testing in China: systematic review and Meta-analysis. JMIR Public Health Surveill. (2022) 8:e41125. doi: 10.2196/41125
16. State Council General Office. (2017). Notice of the state council general office on the issuance of the "thirteenth five-year" action plan for containing and preventing AIDS in China. Available at: https://www.gov.cn/zhengce/zhengceku/2017-02/05/content_5165514.htm (Accessed July 15, 2023).
17. Ministry of Science and Technology of the People's Republic of China. (2019). The world's first HIV (AIDS virus) urine self-test kit approved for market release. Available at: https://www.most.gov.cn/gnwkjdt/201910/t20191024_149514.html [Accessed July 15, 2023].
18. IVD Information. (2022). National medical products administration: HIV self-test kits included in innovative medical device approval! Available at: https://mp.weixin.qq.com/s/g5VrfyQh37lLc08GADGZYg [Accessed July 15, 2023].
19. Shan, D, Xiong, R, Xiao, D, Li, J, Shi, YJ, Pan, L, et al. A survey on current situation of HIV self-testing kits use. Chin J AIDS STD. (2021) 27:166–9. doi: 10.13419/j.cnki.aids.2021.02.13
20. Bao, HY, Xiong, Y, Gifty, M, and Tang, WM. Current status of HIV self-testing application. Chin J Epidemiol. (2021) 42:258–62. doi: 10.3760/cma.j.cn112338-20200624-00881
21. Tang, YY, Xu, ZL, Yuan, JH, and Long, DX. Analysis of willingness and influencing factors of HIV self-testing among men who have sex with men in Shenzhen. Chin J AIDS STD. (2022) 28:416–9. doi: 10.13419/j.cnki.aids.2022.04.08
22. Li, PL, Tang, HL, Li, DM, Ge, L, Yang, J, Qiu, YC, et al. HIV self-testing and related factors in men who have sex with men in Shijiazhuang. Chin J Epidemiol. (2023) 44:797–801. doi: 10.3760/cma.j.cn112338-20220526-00466
23. Njau, B, Covin, C, Lisasi, E, Damian, D, Mushi, D, Boulle, A, et al. A systematic review of qualitative evidence on factors enabling and deterring uptake of HIV self-testing in Africa. BMC Public Health. (2019) 19:1289. doi: 10.1186/s12889-019-7685-1
24. World Health Organization. (2019). WHO recommends HIV self-testing: evidence update and considerations for success. Available at: https://pesquisa.bvsalud.org/portal/resource/pt/who-329968 (Accessed July 15, 2023).
25. Meehan, SA, Draper, HR, Burger, R, and Beyers, N. What drives 'first-time testers' to test for HIV at community-based HIV testing services? Public Health Action. (2017) 7:304–6. doi: 10.5588/pha.17.0064
26. Lyons, CE, Coly, K, Bowring, AL, Liestman, B, Diouf, D, Wong, VJ, et al. Use and acceptability of HIV self-testing among first-time testers at risk for HIV in Senegal. AIDS Behav. (2019) 23:130–41. doi: 10.1007/s10461-019-02552-2
27. Krause, J, Subklew-Sehume, F, Kenyon, C, and Colebunders, R. Acceptability of HIV self-testing: a systematic literature review. BMC Public Health. (2013) 13:735. doi: 10.1186/1471-2458-13-735
28. Myers, JE, Bodach, S, Cutler, BH, Shepard, CW, Philippou, C, and Branson, BM. Acceptability of home self-tests for HIV in new York City, 2006. Am J Public Health. (2014) 104:e46–8. doi: 10.2105/AJPH.2014.302271
29. Lippman, SA, Périssé, AR, Veloso, VG, Sullivan, PS, Buchbinder, S, Sineath, RC, et al. Acceptability of self-conducted home-based HIV testing among men who have sex with men in Brazil: data from an on-line survey. Cad Saude Publica. (2014) 30:724–34. doi: 10.1590/0102-311x00008913
30. Lu, TY, Mao, X, Gao, YY, Zhang, J, Chu, ZX, and Xu, JJ. Research progress on HIV testing in MSM by using HIV self-testing strategy. Chin J AIDS STD. (2019) 25:648–51. doi: 10.13419/j.cnki.aids.2019.06.28
31. Liu, Y, Wu, G, Lu, R, Ou, R, Hu, L, Yin, Y, et al. Facilitators and barriers associated with uptake of HIV self-testing among men who have sex with men in Chongqing, China: a cross-sectional survey. Int J Environ Res Public Health. (2020) 17:1634. doi: 10.3390/ijerph17051634
32. Zhang, C, Li, X, Heilemann, MV, Chen, X, Wang, H, and Koniak-Griffin, D. Facilitators and barriers of HIV self-testing among Chinese men who have sex with men: a qualitative study. J Assoc Nurses AIDS Care. (2021) 32:599–609. doi: 10.1097/JNC.0000000000000218
33. Wong, HT, Tam, HY, Chan, DP, and Lee, SS. Usage and acceptability of HIV self-testing in men who have sex with men in Hong Kong. AIDS Behav. (2015) 19:505–15. doi: 10.1007/s10461-014-0881-1
34. Jin, X, Xu, JJ, Smith, MK, Xiao, D, Rapheal, ER, Xiu, XF, et al. An internet-based self-testing model (easy test): cross-sectional survey targeting men who have sex with men who never tested for HIV in 14 provinces of China. J Med Internet Res. (2019) 21:e11854. doi: 10.2196/11854
35. Mwangi, J, Miruka, F, Mugambi, M, Fidhow, A, Chepkwony, B, Kitheka, F, et al. Characteristics of users of HIV self-testing in Kenya, outcomes, and factors associated with use: results from a population-based HIV impact assessment, 2018. BMC Public Health. (2022) 22:643. doi: 10.1186/s12889-022-12928-0
36. Ren, XL, Wu, ZY, Mi, GD, McGoogan, J, Rou, KM, and Zhao, Y. Uptake of HIV self-testing among men who have sex with men in Beijing, China: a cross-sectional study. Biomed Environ Sci. (2017) 30:407–17. doi: 10.3967/bes2017.054
37. Li, N, Lel, Q, Wang, YX, She, GF, and Sun, HY. Meta-analysis of HIV self-testing status and influencing factors among MSM in China. Occup Health. (2023) 39:2700–4. doi: 10.13329/j.cnki.zyyjk.2023.0484
38. Wood, BR, Ballenger, C, and Stekler, JD. Arguments for and against HIV self-testing. HIV AIDS (Auckl). (2014) 6:117–26. doi: 10.2147/HIV.S49083
39. Lyu, H, Feng, Y, Zhou, Y, Guo, Z, Wang, Y, Cui, M, et al. Factors associated with first-time HIV testing among MSM via secondary distribution of HIV self-test kits in Zhuhai, China. AIDS Behav. (2023) 27:1942–9. doi: 10.1007/s10461-022-03927-8
40. Zheng, JT, Zhang, XF, Lu, CX, Fu, JH, and Ma, W. Characteristics of homosexual behaviors and relationship between high-risk sexual behaviors and seeking sex partners through the internet in men who have sex with men among university students. J Shandong Univ (Health Sci). (2017) 55:115–23. doi: 10.6040/j.issn.1671-7554.0.2017.016
41. Liu, Y, Wang, J, Qian, HZ, Liu, HJ, Yin, L, Lu, HY, et al. Seeking male sexual partners via internet and traditional venues among Chinese men who have sex with men: implications for HIV risk reduction interventions. AIDS Behav. (2016) 20:2222–30. doi: 10.1007/s10461-016-1371-4
42. Chen, YT, Bowles, K, An, Q, DiNenno, E, Finlayson, T, Hoots, B, et al. Surveillance among men who have sex with men in the United States: a comparison of web-based and venue-based samples. AIDS Behav. (2018) 22:2104–12. doi: 10.1007/s10461-017-1837-z
43. Tsui, HY, and Lau, JT. Comparison of risk behaviors and socio-cultural profile of men who have sex with men survey respondents recruited via venues and the internet. BMC Public Health. (2010) 10:232. doi: 10.1186/1471-2458-10-232
44. Qin, YL, Liu, FY, Tang, WM, Tang, SY, Liu, CC, Jessica, M, et al. HIV self-testing among high-risk men who have sex with men in China: a cross-sectional study. Lancet. (2016) 388:S76. doi: 10.1016/S0140-6736(16)32003-7
Keywords: self-testing, HIV, men who have sex with men, Guangzhou, nested case-control
Citation: Gu Y, Yang J, Luo Y, Zhan L, Liu F, Zeng W, Xu H, Lu Y, Cai Y and Han Z (2025) Nested case-control study investigating factors affecting initial adoption of HIV self-testing among men who have sex with men in Guangzhou, China: amidst comprehensive service coverage. Front. Public Health. 12:1483671. doi: 10.3389/fpubh.2024.1483671
Edited by:
Weiming Tang, University of North Carolina at Chapel Hill, United StatesReviewed by:
Huanyu Bao, Nanyang Technological University, SingaporeMeizhen Liao, Shandong Center for Disease Control and Prevention, China
Copyright © 2025 Gu, Yang, Luo, Zhan, Liu, Zeng, Xu, Lu, Cai and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuzhou Gu, eXVjaG91a29vQGZveG1haWwuY29t; Zhigang Han, emhpZ2FuZ2hhbjYxNkAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Yuzhou Gu
Yuzhou Gu JiaLi Yang
JiaLi Yang Yefei Luo
Yefei Luo Lishan Zhan1
Lishan Zhan1 Yanshan Cai
Yanshan Cai Zhigang Han
Zhigang Han