- 1School of Nursing, Beijing University of Chinese Medicine, Beijing, China
- 2Institute of Basic Research in Clinical Medicine, China Academy of Chinese Medical Sciences, Beijing, China
- 3Department of Vascular Surgery, Beijing Hospital, National Center of Gerontology, Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, China
- 4Institute of Encephalopathy, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
Objective: To develop a patient version of guidelines (PVG) for rehabilitation nursing (RN) in stroke patients with limb dysfunction, aiming to enhance patients’ awareness, self-management skills, and adherence to rehabilitation programs.
Methods: This guideline was developed based on the cultural and healthcare context of China, and was guided on the Minimum standards for the Development Process, Content and Governance of Patient-Directed Knowledge Tools and the PVG tool book of the Guidelines International Network. The guideline was constructed through a normative process involving clarifying priority questions, assessing and integrating evidence, detailing and contextualizing recommendations, and evaluating the prototype of PVG.
Results: Fifteen priority RN issues were identified, and eight articles (four guidelines and four evidence summaries) were included, all demonstrating robust methodological quality. The final guideline encompassed five themes: disease knowledge, functional assessment, symptom prevention and nursing, rehabilitation training, and traditional Chinese medicine nursing - a specialized approach integrating traditional Chinese medicine principles with modern nursing practices, including 26 recommendations.
Conclusion: This patient-centered guideline, grounded in a robust scientific framework and tailored to patient needs, serves as a valuable reference for the RN of stroke patients with limb dysfunction. The development of context-specific patient guidelines that integrate best available evidence remains an area requiring continued effort and refinement. Further research is warranted to evaluate the implementation and effectiveness of this guideline within diverse Chinese healthcare context.
1 Introduction
Stroke, a prevalent acute cerebrovascular disorder, is the second leading cause of adult mortality globally and a primary contributor to long-term severe disability (1). Limb function impairment is a common sequela, with epidemiological studies showing high incidence rates. In the United States, over 80% of stroke patients experience lower limb dysfunction, with 25% retaining residual disabilities despite rehabilitation (2, 3). Similarly, in China, 85% of patients initially present with upper limb dysfunction, and 30–36% continue to exhibit impairments 6 months post-onset (4). Rehabilitation nursing (RN) has been empirically validated as an efficacious approach to mitigating disability rates in these patients (5), demonstrating potential in alleviating functional deficits, enhancing functional status, preventing complications, and improving daily living activities (6).
RN plays a crucial role in promoting limb function recovery in stroke patients through various interventions. In China, economic and geographical constraints commonly necessitate home-based rehabilitation (7, 8), potentially limiting patients’ access to professional, systematic therapy during the critical early rehabilitation phase (9). Despite stroke patients’ desire to learn rehabilitation skills, they often lack awareness of sustained care needs (10). While online health education has emerged as a solution, existing materials frequently lack scientific rigor or contain outdated information. There is an urgent need for evidence-based RN knowledge specific to stroke-induced limb function impairment to enhance patient and caregiver awareness and adherence.
Clinical practice guidelines (CPGs) are widely recognized as the most scientifically rigorous source of health recommendations (11). However, the professional terminology and complex medical knowledge they contain often render them difficult for patients and the general public to comprehend and apply. To address this issue, patient versions of guideline (PVG) have emerged as a solution. PVG (12) refer to documents that “translate” the recommendations and underlying principles of CPGs into a format more accessible and applicable for patients and the general public. The Guidelines International Network (GIN) published its first handbook for developing PVGs in 2015, with an updated version released in 2021 (13). In 2018, the National Institute of Health Care of Southern Netherlands (14) established the Minimum Criteria for the Development Process, Content and Governance of Patient-Directed Knowledge Tools [PDKT(MC-PCG)]. In 2021, GIN (15) formulated a reporting checklist for PVGs. These methodological resources provide researchers with guidance for developing PVGs.
Although there are currently no specific CPGs or PVGs for RN of stroke with limb dysfunction, relevant content has been addressed in existing guidelines. For instance, the American Heart Association/American Stroke Association (AHA/ASA) published “Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association” in 2016 (16), which outlines general principles and strategies for stroke rehabilitation. Similarly, the “Clinical Management Guidelines for Cerebrovascular Diseases” (17), released by the Chinese Stroke Association in 2019, emphasizes the importance of early and continuous rehabilitation. These guidelines provide substantial evidence-based support for the RN of patients with stroke-induced limb function impairment.
This study aims to develop a PVG specifically for the RN of stroke patients with limb dysfunction. Guided by international PVG development standards and considering the Chinese context, this research will construct a patient-centered, comprehensive, and practical PVG for the RN of stroke patients with limb dysfunction. This PVG will fill a critical gap in China, providing evidence-based guidance for limb RN in stroke patients, thereby enhancing rehabilitation outcomes and quality of life. Additionally, the PVG will serve as a reference for healthcare providers, facilitating patient-provider communication and improving RN services.
2 Methods
This study employs the PDKT(MC-PCG) and the GIN’s PVG toolkit as theoretical frameworks. The GIN toolkit outlines key elements in PVG development, including stakeholder engagement and content presentation. The PDKT(MC-PCG), as the first internationally applicable tool for PVG development, provides a systematic approach covering team formation, scope definition, patient needs identification, and content determination. As PDKT(MC-PCG) primarily targets patient versions of individual CPGs, and no specific CPG exists for RN of stroke patients with limb dysfunction, our team, based on a literature review (18–20) and expert consultations, opted to systematically search for evidence meeting identified patient needs. We will integrate the best evidence using guideline adaptation methods (21, 22), aiming to synthesize current best practices in RN for stroke-induced limb function impairment and translate them into a PVG.
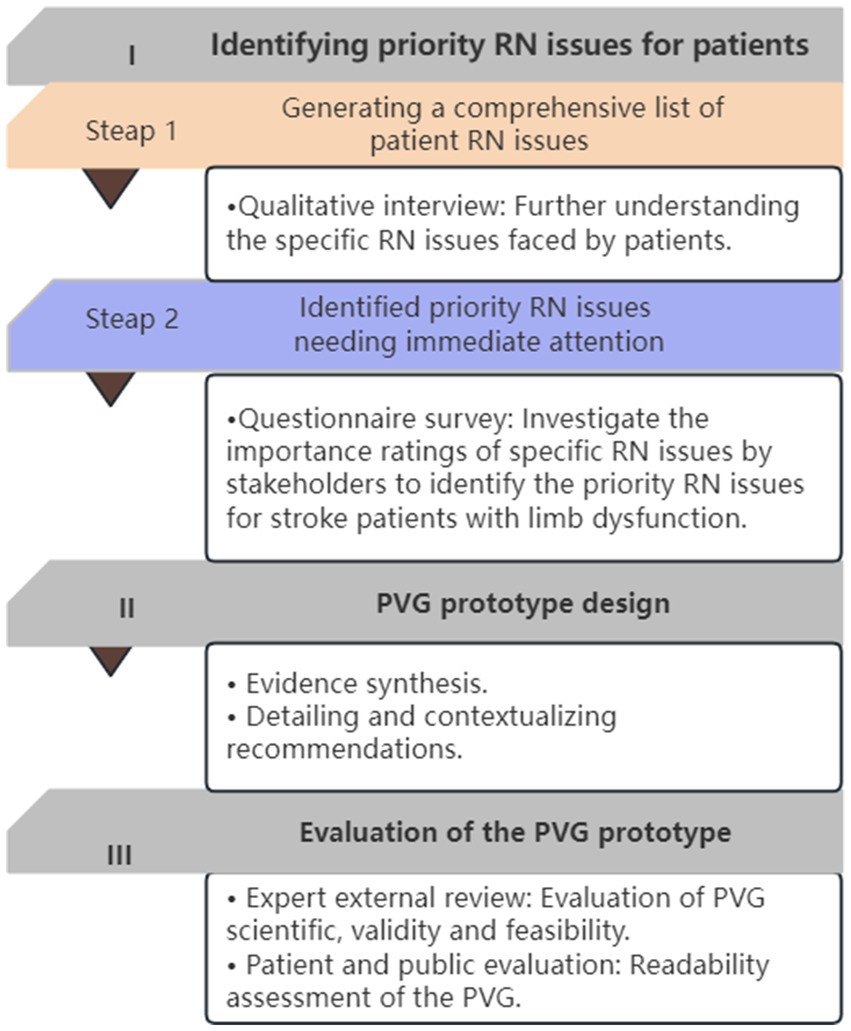
The study comprises three phases (see Figure 1): (1) Identifying priority RN issues for patients; (2) Developing a prototype of the PVG content based on the identified issues; and (3) evaluating the prototype of the PVG for readability, comprehensibility, and usability. This PVG has been registered on the International Practice Guidelines Registry Platform1 with the registration number IPGRP-2020CN203.
At the start, we established a 25 member guideline development team, comprising five functional groups: development, consensus, evidence evaluation and translation, patient and public, and external review. Team members included healthcare providers, research experts, patient representatives, and health education editors. Detailed information on group members and their responsibilities is available in Appendix A.
2.1 Identifying priority RN issues for patients
This phase began with semi-structured interviews to identify RN issues faced by patients, generating a comprehensive list. We then developed a questionnaire based on this list and surveyed patients and healthcare providers, asking them to rank the importance of each issue. This process identified priority RN issues needing immediate attention.
2.1.1 Qualitative interview
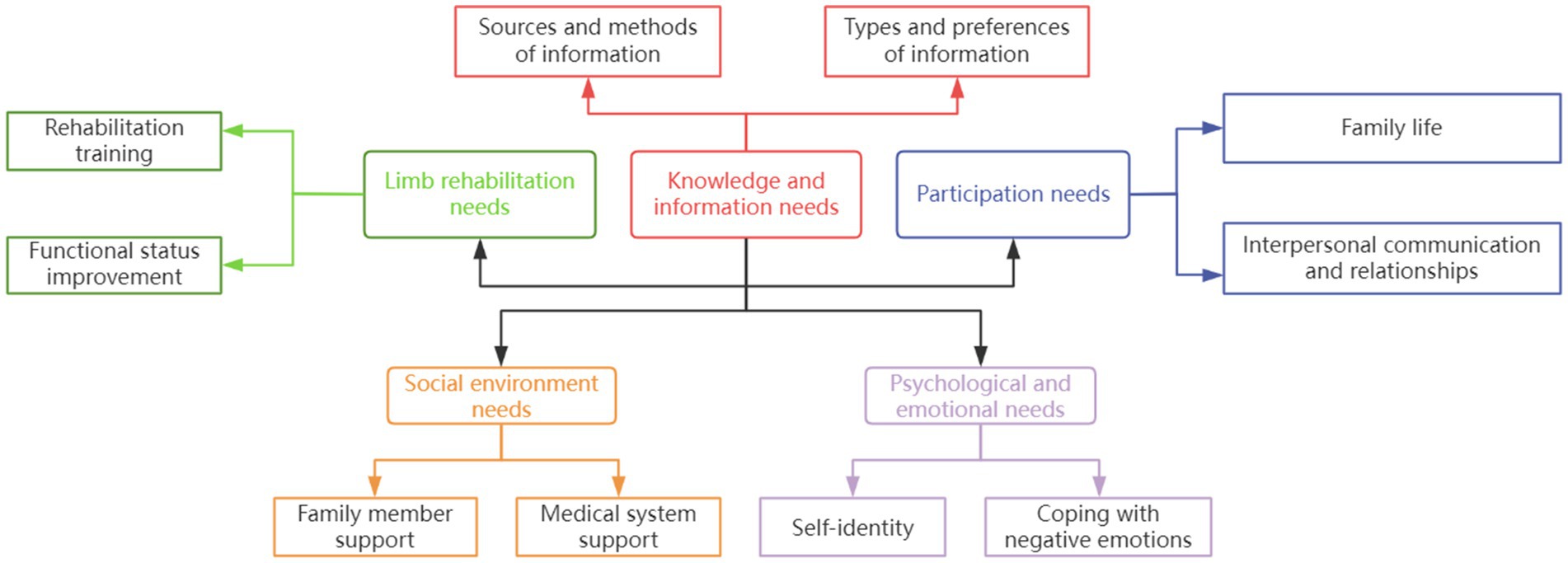
A semi-structured interview guide was developed based on RN themes from previous literature (23), comprising five primary and 10 secondary themes (Figure 2). Stroke patients with limb dysfunction (and their caregivers) and healthcare providers were purposively sampled from Beijing Dongzhimen Hospital’s Encephalopathy Department (August–September 2021). Each interview lasted approximately 40 min. The sample size for our interviews was determined by the principle of information saturation, whereby sampling was discontinued when no new codes emerged from the interview data (24). Deductive content analysis (25) was used, with an initial coding framework based on the International Classification of Functioning, Disability and Health (ICF). This process generated a comprehensive list of RN issues, described using evidence-based question formulation (26). The ICF (27, 28), widely used to classify functioning, disability, and health, facilitated a holistic analysis of patients’ rehabilitation needs, encompassing functional disabilities and contextual factors.
2.1.2 Questionnaire survey
Using purposive sampling, stroke patients with limb function impairment, caregivers, and healthcare providers from Dongzhimen Hospital’s Encephalopathy Department were surveyed (October–November 2021). A self-designed questionnaire based on the RN issue list used a 5-point Likert scale (1 = not important, 5 = crucial). SPSS 26.0 was used for descriptive analysis, with 10–15 priority issues identified through expert consensus (29).
2.2 PVG prototype design
This phase involved designing the PVG prototype through targeted literature review and expert consultation. It comprised two main components: evidence synthesis, and the detailing and contextualization of recommendations.
2.2.1 Evidence synthesis
2.2.1.1 Evidence search and quality appraisal
A systematic search (30) based on identified RN issues was conducted across international guideline websites, Chinese and English databases, and stroke-specific professional association websites from January 2016 to December 2021 (search strategies and criteria in Appendix B). Two evidence-based medicine experts independently screened the literature, with disagreements resolved through discussion. Included literature was independently evaluated using appropriate quality assessment tools: AGREE II (31) for CPG and CASE worksheet (32) for evidence summaries.
2.2.1.2 Evidence integration and analysis
Due to the diverse sources of eligible evidence, we established principles for evidence integration (33): (1) Select concise, clear evidence when consistent; (2) Combine complementary evidence logically; (3) Prioritize high - quality, latest authoritative literature when contradictory; (4) Retain original statements for independent evidence. The SIGN PVG (34) recommendation grading system was used for presentation. Two researchers integrated evidence, with five clinical experts evaluating synthesis results and applicability. Modifications were made based on feedback. The overall expert authority coefficient (sum of individual coefficients divided by number of experts) was assessed, with >0.7 indicating acceptable expert consensus.
2.2.2 Detailing and contextualizing recommendations
The evidence detailing phase aimed to supplement recommendations while maintaining consistency with original guidelines. Following GIN’s PVG toolkit principles (20), two researchers refined content focusing on structure rationality, appropriateness, clinical significance, and accuracy. The evidence translation phase then aligned detailed content with patients’ needs and enhanced comprehensibility. Guided by the Patient Education Materials Assessment Tool (PEMAT) (35), we emphasized ‘understandability’ and ‘actionability’. Healthcare providers, patient representatives, and science communicators evaluated the results, with researchers incorporating feedback for improvements. (Detailed principles and methods in Appendix C). This process ensured scientifically robust recommendations tailored to patients’ practical needs and understanding levels.
2.3 Evaluation of the PVG prototype
An external review panel (peer experts, patient representatives, and health science communicators) assessed the PVG content and development process. Revisions were made based on their feedback.
2.3.1 Evaluation of PVG scientific, validity. and feasibility
An expert panel of evidence-based methodology specialists and stroke experts evaluated the PVG using a custom-designed “Expert Consultation Form.” The evaluation covered: (1) Significance of identified RN questions. (2)Evidence synthesis and translation processes. (3)Guideline recommendations’ usability, using the JBI FAME framework (36) (rated as “Agree,” “Unclear,” or “Disagree”). And(4)PVG reporting quality, using the Reporting checklist for public versions of guidelines (RIGHT-PVG) (15) (four domains, 12 topics, 17 items; rated as “Fully met,” “Partially met,” or “Not met”).
2.3.2 Readability assessment of the PVG
Patient representatives and health science communicators evaluated the guideline’s readability using the Suitability Assessment of Materials (SAM) scale. This scale, developed by Doak et al. (37) and translated into Chinese by Li (38), assesses the readability of health education materials. Notably, the SAM scale has also been applied to evaluate the readability of PVG in previous studies (39).
3 Results
3.1 Priority RN issues for patients
3.1.1 Qualitative interviews
We interviewed nine stroke patients with limb functional impairment (six males, three females; mean age 58 ± 9.04 years) and six neurology specialist healthcare providers (mean specialized experience 13.33 ± 6.19 years). Combining interview findings with literature review results, we synthesized a refined categorization of rehabilitation nursing needs. This resulted in five primary themes, 10 secondary themes, and 26 specific rehabilitation nursing issues for stroke patients with limb functional impairment (detailed list in Appendix D).
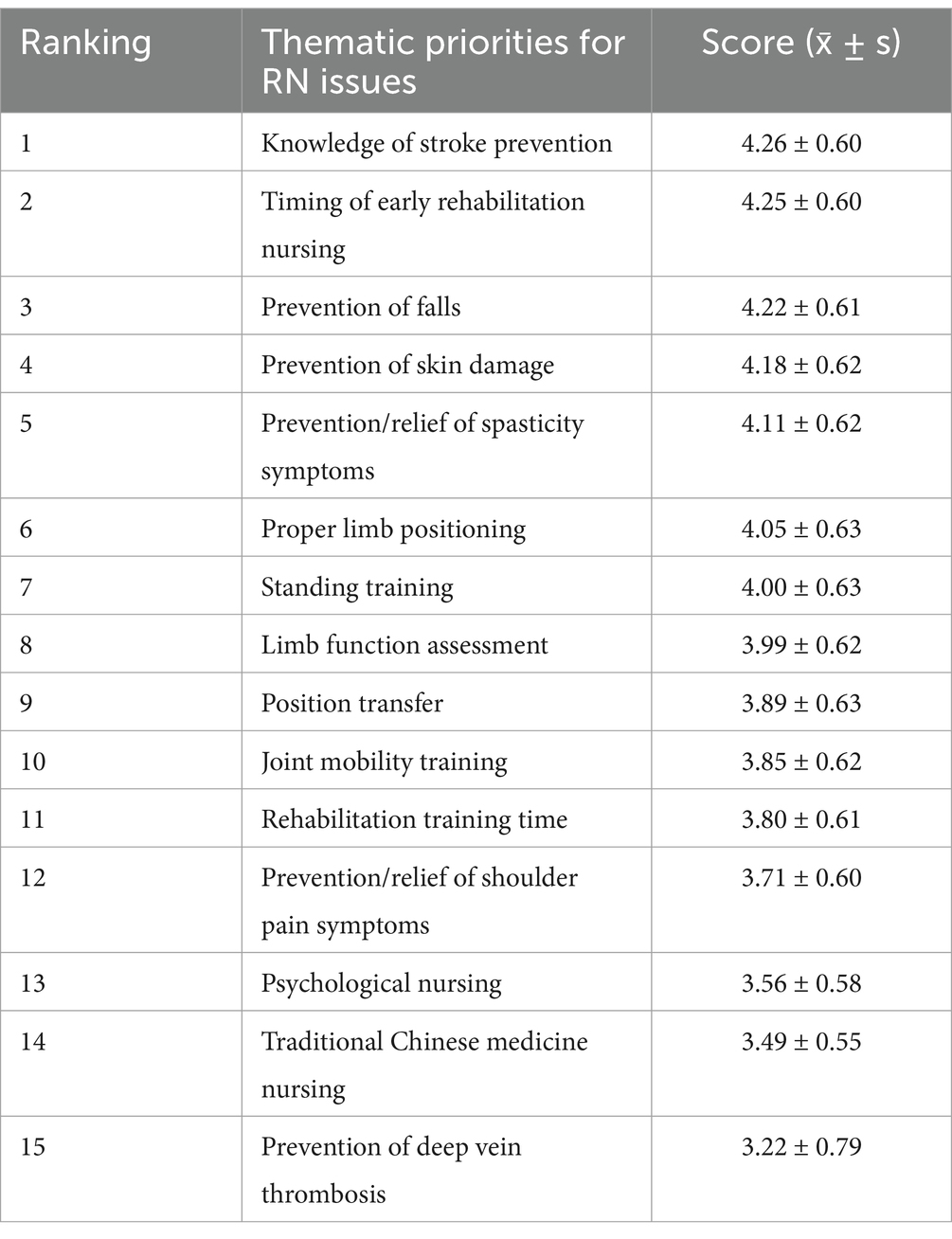
3.1.2 Questionnaire survey
A total of 140 distributed questionnaires among three groups: caregivers, patients, and healthcare providers. Of these, 134 valid responses were received, resulting in an overall response rate of 95.71%. The valid responses were distributed as follows: 58 from caregivers (43.28% of valid responses), 44 from patients (32.84% of valid responses), and 32 from healthcare providers (23.88% of valid responses). Based on these responses, the guideline development group identified the top 15 priority RN issues for stroke patients with limb dysfunction. Detailed scoring results are in Table 1.
3.2 PVG prototype
3.2.1 Evidence synthesis
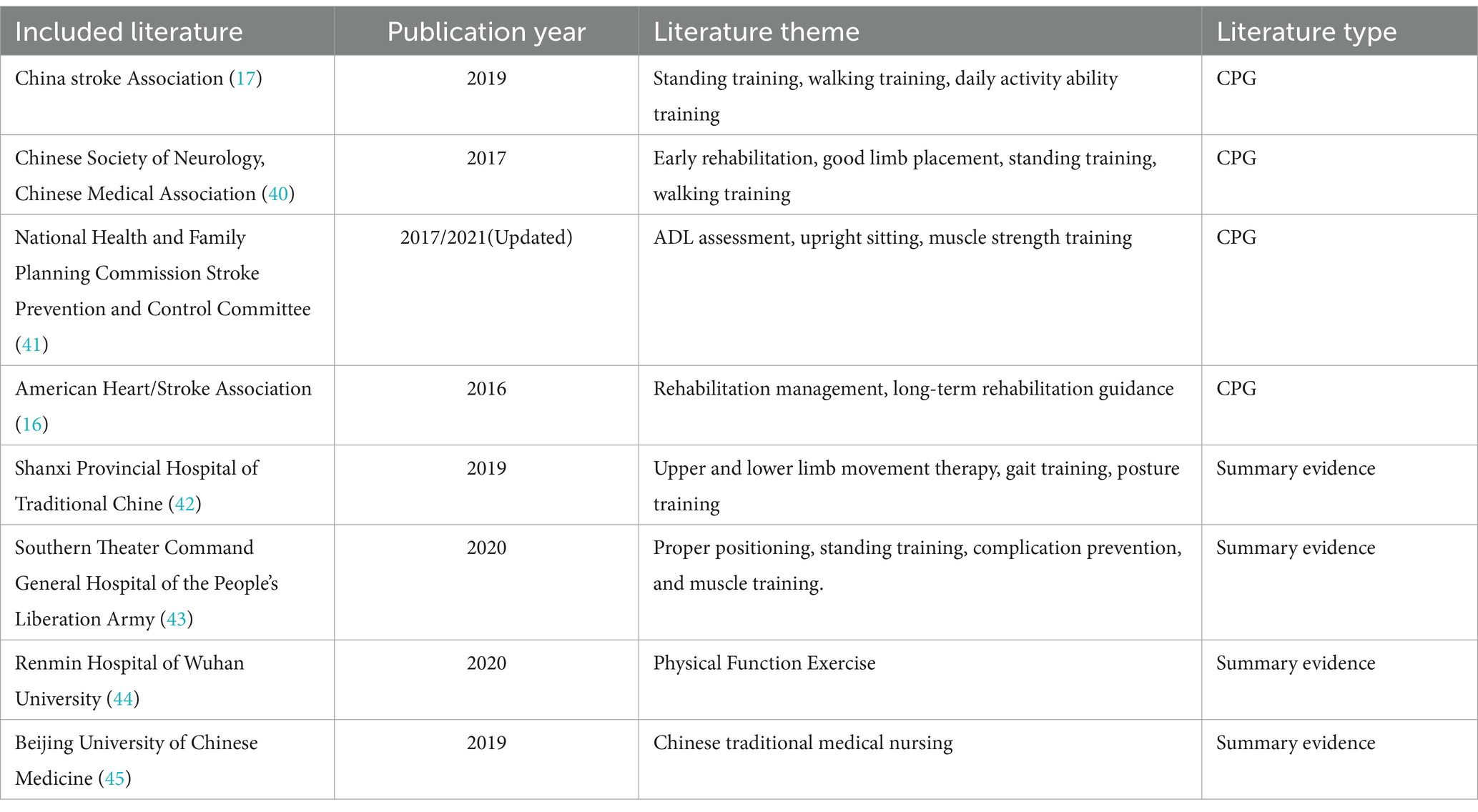
The initial literature search yielded 205 articles. After applying inclusion and exclusion criteria, four guidelines (16, 17, 40, 41) and 4 evidence summaries (42–45) were ultimately included (see Table 2). All selected materials demonstrated good quality of evidence and were incorporated following intra-group discussions. (The included evidence and evaluation results are detailed in Appendix E).
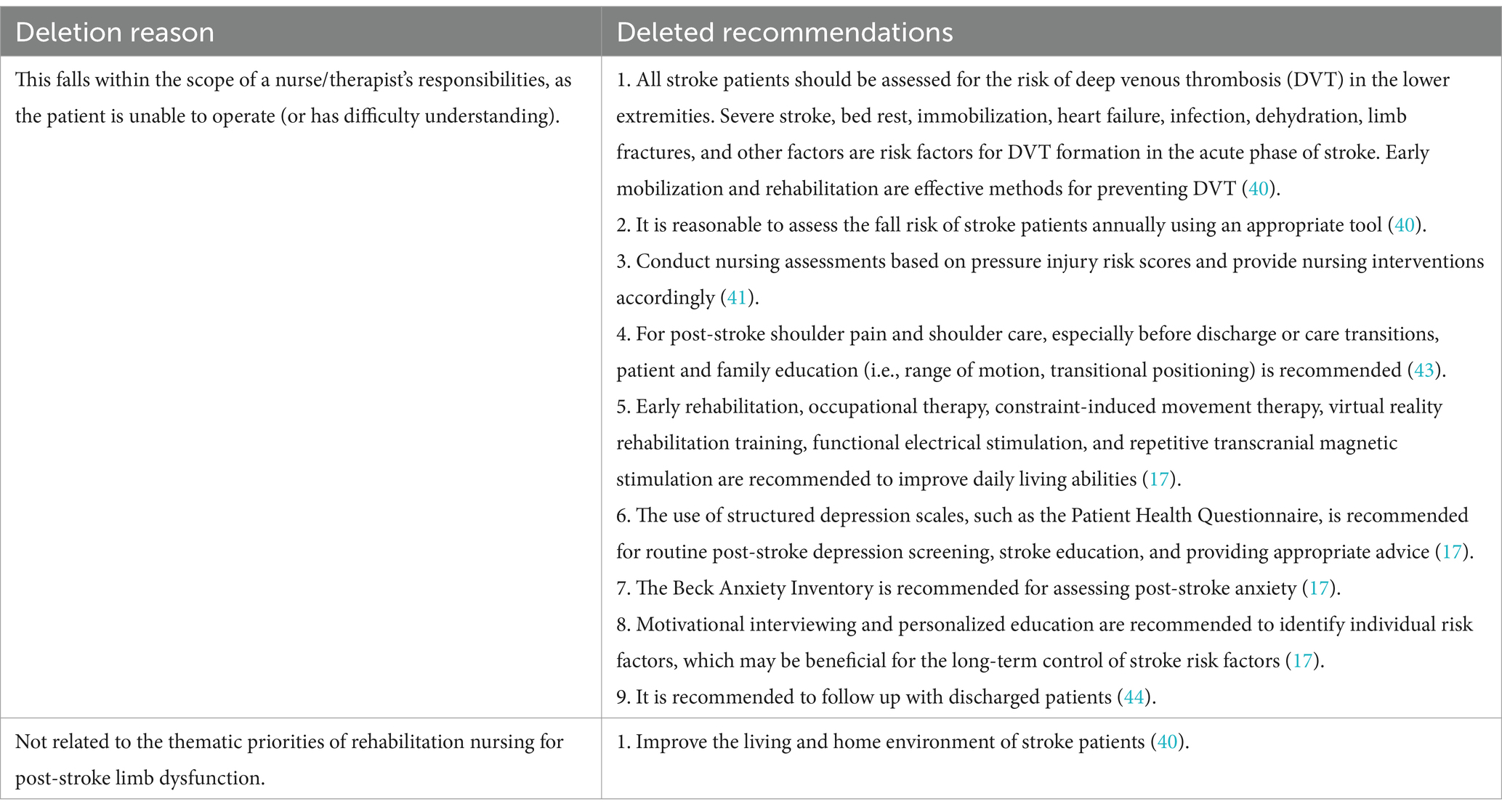
3.2.1.1 Results of recommendation extraction
Three specialists from the study’s expert consensus group conducted the consultation, with an overall expert authority coefficient of 0.90. From 83 initial recommendations, 10 were excluded: nine for being beyond patient implementation scope and one for irrelevance to post-stroke limb functional impairment rehabilitation (details in Table 3), which resulted in 73 preliminarily included recommendations.
3.2.1.2 Integration of recommendations
Through extraction, classification, synthesis, and expert consultation, a final set of 26 recommendations was formulated, comprising: one on functional assessment, 10 on symptom prevention and care, 10 on rehabilitation training series, three on traditional Chinese medicine nursing, and two on disease knowledge. Detailed information is provided in Appendix E.
3.2.2 Detailing and contextualizing recommendations
Consultations were conducted with four experts (authority coefficient: 0.88), two patient representatives, and one health science communicator.
Experts validated the accuracy and clinical significance of the detailed recommendations. However, they advised removing “Chinese herbal fumigation” and “muscle strength assessment” as unsuitable for home use or self-assessment. For the remaining recommendations, experts suggested considering specific application scenarios and adjusting according to contextual environments during implementation. (Final detailed recommendations are presented in Appendix F).
Regarding the contextualization of the detailed recommendations, experts confirmed the accuracy of the adapted content. They suggested presenting training procedures predominantly through a combination of text, images/videos, and step-by-step explanations, and providing more specific descriptions of recommendation strengths. Patient representatives and the communicator, while noting good readability, suggested: (1) explaining stroke-related limb impairment causes, (2) highlighting key information visually, and (3) detailing recommendation strengths to indicate relative importance. These inputs informed the PVG prototype development (Appendix G).
3.3 Evaluation of the PVG prototype
3.3.1 Expert evaluation results
Five experts in evidence-based medicine/nursing and clinical management/nursing evaluated the study (expert authority coefficient: 0.87).
3.3.1.1 PVG priority issues assessment results
Experts rated all 15 RN issues as highly important (mean scores ≥4; details in Appendix H).
3.3.1.2 Evaluation results of PVG recommendation integration, detailing and contextualizing recommendations
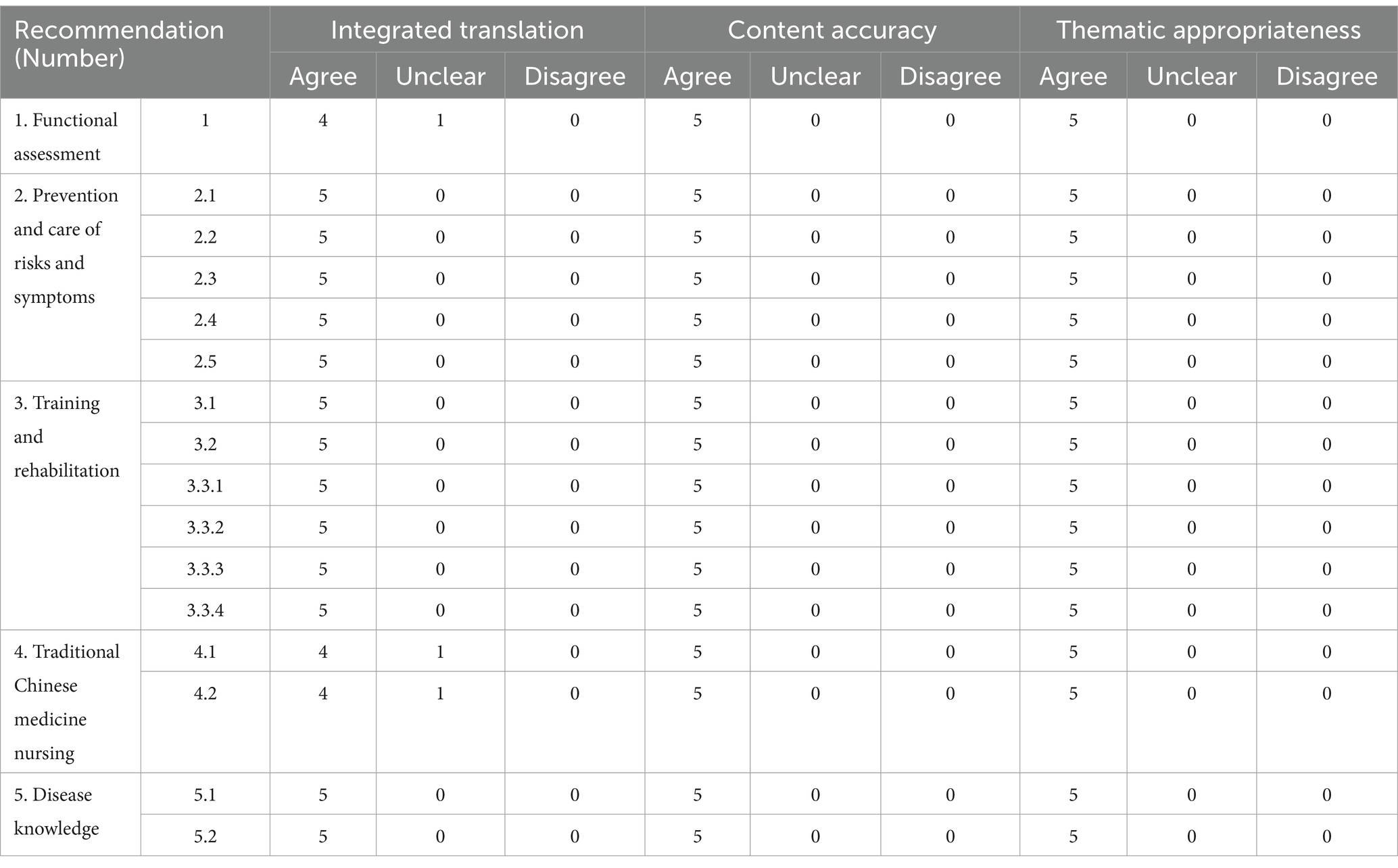
Experts highly agreed on the content accuracy and theme appropriateness of the synthesized, detailed, and contextualized recommendations. They emphasized the importance of professional guidance when implementing nursing procedures from this PVG (details in Table 4).
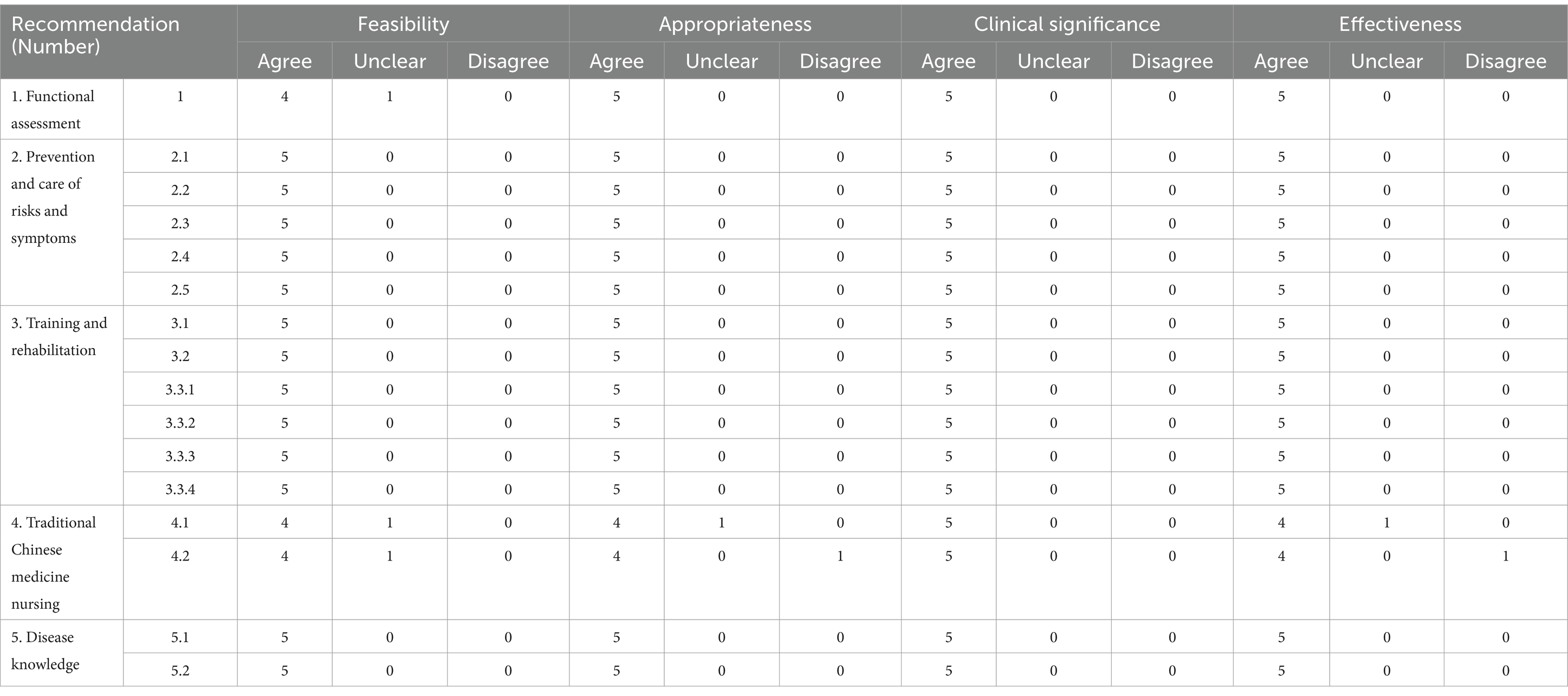
3.3.1.3 Applicability assessment results of recommendations
Experts highly agreed on the recommendations’ feasibility, appropriateness, clinical significance, and effectiveness, indicating their alignment with Chinese clinical practice and potential for widespread application (details in Table 5).
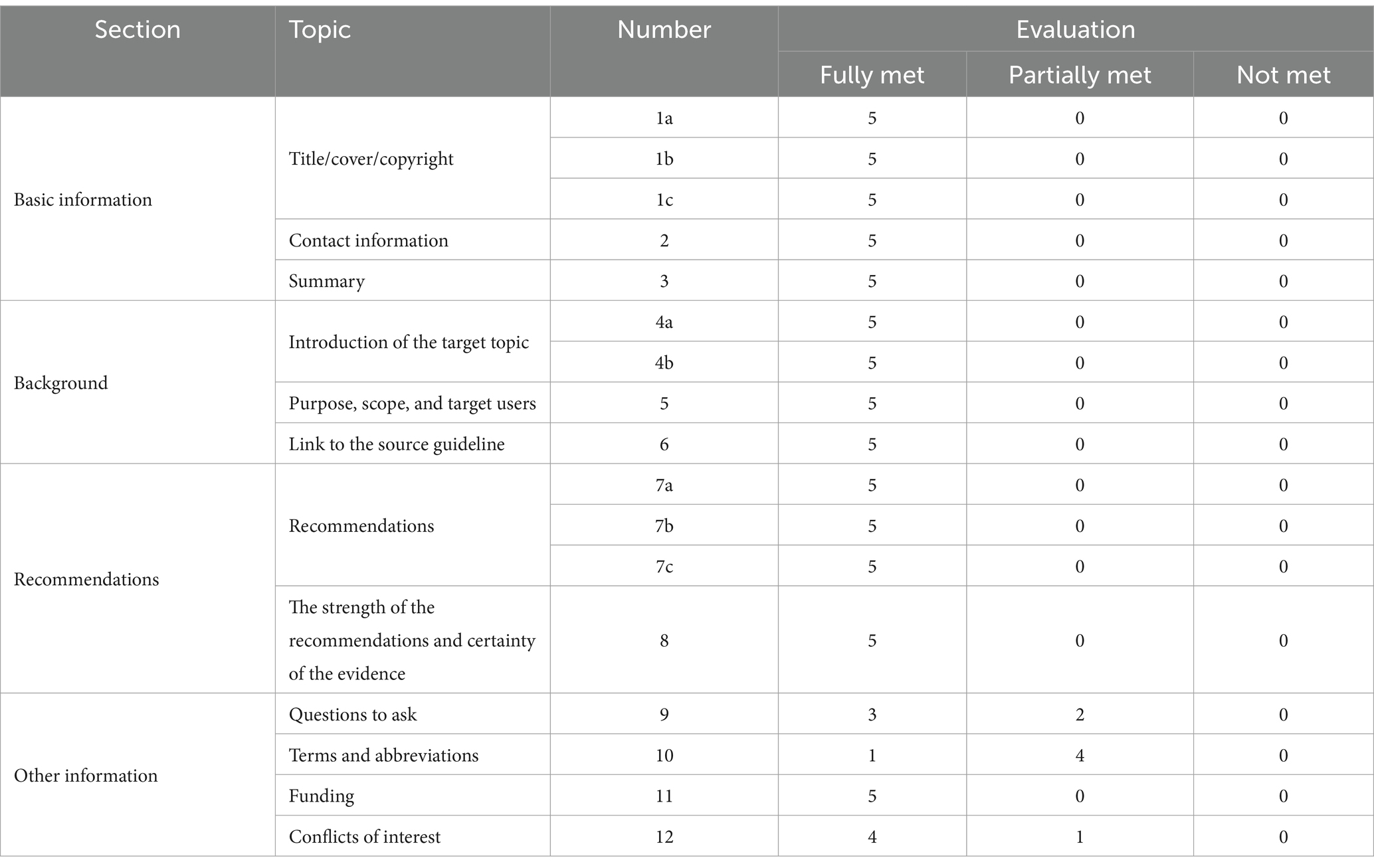
3.3.1.4 Evaluation results of PVG Reporting
Experts highly agreed on most reporting standards of the RN PVG for stroke patients with limb functional impairment, but suggested refinements in terminology, abbreviations, and question framing (details in Table 6).
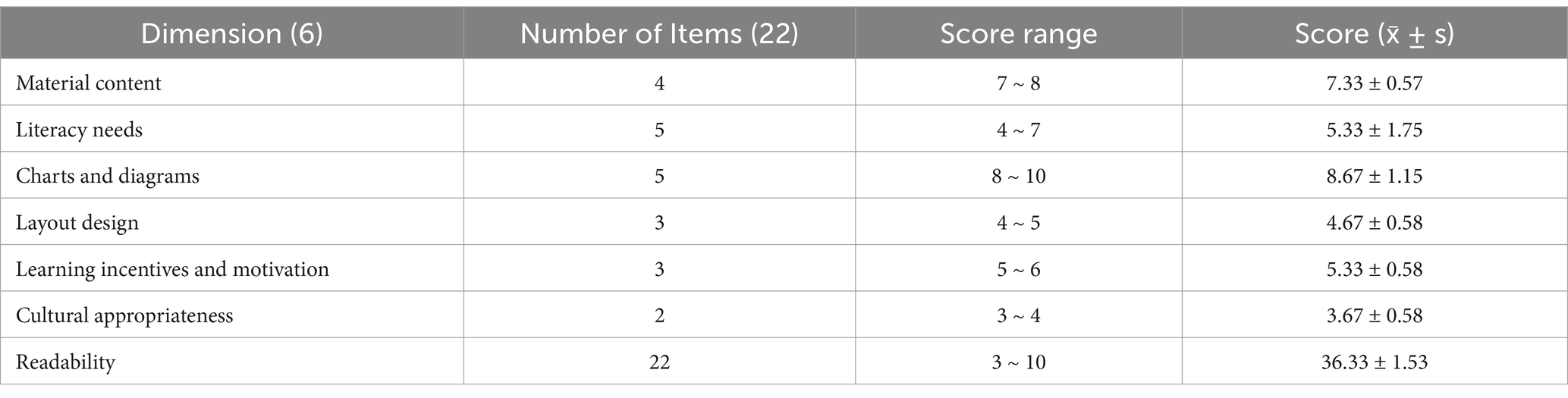
3.3.2 Readability evaluation results of PVG by patients and health science communicator
Two patients and one health science communicator evaluated the readability of the PVG. The overall readability score for the PVG textual materials was (36.33 ± 1.53), with individual overall score percentages of 79.54, 81.81, and 86.36%, respectively. All three reviewers rated the PVG as excellent (evaluation results are presented in Table 7).
3.3.3 Improvement of PVG prototype
Incorporating expert, patient, and public feedback, the team revised the initial PVG draft, producing the ‘2022 Patient Guideline for RN of Stroke-Related Limb Functional Impairment’ with a WeChat version (Appendix I). Main contents are in Table 8.
4 Discussion
4.1 Principal findings
This study presents the first PVG for RN of stroke-related limb dysfunction in mainland China. Developed using a mixed-methods approach guided by PDKT (MC-PCG) and GIN’s PVG toolkit, this evidence-based guideline is available in both online and print formats. Unlike traditional health education, it offers evidence-based recommendations and decision support for patients (34). Key stakeholders, including patients, caregivers, health communicators, and healthcare providers, were involved from early stages. The application of the ICF framework ensured that the guideline development better addressed the RN information needs of stroke patients with limb functional impairment. Continuous stakeholder collaboration throughout the guideline development process is expected to enhance its adoption and usability in home rehabilitation for stroke patients with limb functional impairment.
4.2 Comparison with prior work
This study adopts an innovative method in the development process of Patient Version Guideline (PVG), which is different from the existing international model. We do not fully follow the guidance of the PVG reference book of the International Guidelines Network (GIN), but are patient oriented, based on a comprehensive assessment and identification of patient needs, a comprehensive search of multiple high-quality clinical guidelines to extract the best evidence to meet the needs of patients. Subsequently, we adopted a scientifically rigorous approach to integrate, detailing and contextualizing recommendations, and finally formed a patient-centered PVG. This approach takes into account the use of a single clinical practice guideline as the basis for PVG and may be limited in meeting patient needs. This view is consistent with the findings of Lijiao et al. (46).
Reasonable and standardized determination of the priority health problems of PVG is a necessary condition for the construction of PVG, which determines the scope of evidence retrieval and whether PVG can scientifically answer the health problems of patients. However, there is currently no unified methodological standard to guide the identification of priority PVG issues, and there is commonly a lack of focus on priority health issues in existing published PVG (47). In this study, a mixed research method was adopted to determine the health problems covered by PVG in the RN of stroke limb dysfunction. Based on the ICF framework, the study was organized on the basis of literature research and qualitative interviews, and then the demand level of RN was investigated through questionnaires, which avoided overly broad or specific limitations of the scope of problems to a certain extent.
In terms of the transformation of demand questions, we innovatively classified patient demand questions first, and then find clinical questions in relevant studies and guidelines according to the types of problems, so that the focus of demand questions is clear and not too broad. Studies have shown that the importance assessment of the overall problem can meet the need for the importance assessment of the guidelines (48). Therefore, the score on the importance of health problems related to RN for stroke limb dysfunction in this study can be used as the basis for evaluating the importance of PVG health problems, which is consistent with the research results of Xing (49).
Patient guidelines aim to facilitate shared decision-making by translating complex medical information into understandable language. However, the process of converting specialized RN knowledge into patient-friendly content remains challenging, with few studies detailing specific methods (50). Guided by the GIN Reference Book and the Patient Educational Materials Evaluation Tool (PEMAT) (35), this study adopted a systematic approach to content translation. PEMAT, a widely used and reliable tool for assessing patient education materials (35), provided both evaluation criteria and conversion principles for our Patient Version Guide (PVG). This methodology enhances the readability and practicality of the guide while offering a replicable approach for future research.
5 Limitation
This study acknowledges several methodological limitations. Primarily, participant recruitment was confined to the Beijing area of China, potentially limiting the generalizability of findings to diverse regional contexts. Future research should include a more geographically heterogeneous sample to enhance external validity across varied socio-geographic landscapes. Furthermore, while the Patient Version Guide (PVG) developed in this study shows promise in enhancing comprehension and engagement in RN knowledge among stroke patients and caregivers, its practical efficacy requires empirical validation. The hypothesized outcomes, including improved patient adherence and optimized rehabilitation practices, necessitate rigorous evaluation through longitudinal clinical studies. These should encompass analyses of implementation contexts and extended follow-up periods to ascertain the PVG’s effectiveness and guide its refinement. Systematic assessment of the PVG’s impact in diverse clinical settings is crucial to substantiate its utility and inform its broader dissemination. This approach will not only validate the tool’s effectiveness but also contribute to patient-centered rehabilitation care knowledge, potentially influencing future stroke rehabilitation guidelines.
6 Conclusion
Based on GIN handbooks and patient-oriented knowledge tools, this study developed a “Patient Guideline for RN of Post-Stroke limb dysfunction” through systematic evidence synthesis. This PVG serves as a practical resource for healthcare providers, patients, and caregivers, facilitating the implementation of evidence-based practices. However, the optimal methodology for developing such guides and their clinical value require continuous evaluation, given the complex factors involved in patients’ self-rehabilitation. Future research should focus on standardizing the development timing of patient guides, improving evidence evaluation methods, and assessing their application in real clinical settings. This study’s standardized approach provides a beneficial model for future research in this field.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Ethics Committee of Beijing University of Chinese Medicine, Beijing University of Chinese Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
DY: Writing – original draft, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation. JZ: Writing – original draft, Formal analysis, Methodology. MM: Writing – review & editing, Validation. XL: Writing – review & editing, Data curation. LY: Writing – review & editing, Data curation. JF: Writing – review & editing, Data curation. ZW: Writing – review & editing, Investigation. SC: Writing – review & editing, Investigation. XZ: Writing – review & editing, Validation. YH: Writing – review & editing, Supervision, Methodology. FW: Writing – review & editing, Supervision.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank and appreciate all patients, health-care team members and experts participating in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1482771/full#supplementary-material
Footnotes
References
1. Kuriakose, D, and Xiao, Z. Pathophysiology and treatment of stroke: present status and future perspectives. Int J Mol Sci. (2020) 21:7609. doi: 10.3390/ijms21207609
2. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. (2022);9:137–150. doi: 10.1016/S2215-0366(21)00395
3. Duncan, PW, Zorowitz, R, Bates, B, Choi, JY, Glasberg, JJ, Graham, GD, et al. Management of Adult Stroke Rehabilitation Care: a clinical practice guideline. Stroke. (2005) 36:e100–43. doi: 10.1161/01.STR.0000180861.54180.FF
4. Alberts, MJ, Latchaw, RE, Selman, WR, Shephard, T, Hadley, MN, Brass, LM, et al. Recommendations for comprehensive stroke centers: a consensus statement from the brain attack coalition. Stroke. (2005) 36:1597–616. doi: 10.1161/01.STR.0000170622.07210.b4
5. Huang, X, and Yan, T. Rehabilitation medicine. 5th ed. Beijing: People’s Medical Publishing House (2013).
6. Wang, J, Zhang, Y, Chen, Y, Li, M, Yang, H, Chen, J, et al. Effectiveness of rehabilitation nursing versus usual therapist-led treatment in patients with acute ischemic stroke: a randomized non-inferiority trial. Clin Interv Aging. (2021) 16:1173–84. doi: 10.2147/CIA.S306255
7. Yan, A, Qi, L, and Wang, W. Research progress on application of home rehabilitation nursing for elderly stroke patients in recovery period. Chin Nurs Res. (2017) 31:1541–4. doi: 10.3969/j.issn.1009-6493.2017.13.002
8. Hu, M, and Zhong, M. Community family recovery nursing intervenes after the apoplexy patient leaves the hospital the mind and body recovery to affect. Chin Manipulat Rehabil Med. (2010) 1:19–20.
9. Wan, Y, Zhou, J, and Xue, L. Rehabilitation exercise compliance in patients with ischemic stroke and influencing factors in a third-grade class-a hospital in Xinjiang. Med Soc. (2019) 32:123–6. doi: 10.13723/j.yxysh.2019.05.030
10. Dong, K, Wang, Y, Tao, C, Ding, S, and Gao, F. Continuing care willingness and influencing factors in discharged stroke patients under the policy of the regional medical consortium. Modern. Prev Med. (2019) 46:3910–3913+3924.
11. IOM (Institute of Medicine). Clinical practice guidelines we can trust. Washington, DC: The National Academies Press (2011).
12. G-I-N PUBLIC (2021). Patient information, Communicating guidelines to patients and the public. https://g-i-n.net/toolkit/communicating-guidelines-to-patients-and-the-public (Accessed July 17, 2024).
13. G-I-N PUBLIC (2021). G-I-N PUBLIC Toolkit: Patient and Public Involvement in Guidelines, https://g-i-n.net/wp-content/uploads/2023/07/Toolkit-combined.pdf; 2021 (Accessed July 17, 2024).
14. van der Weijden, T, Dreesens, D, Faber, MJ, Bos, N, Drenthen, T, Maas, I, et al. Developing quality criteria for patient-directed knowledge tools related to clinical practice guidelines. A development and consensus study. Health Expect. (2019) 22:201–8. doi: 10.1111/hex.12843
15. Wang, X, Chen, Y, Akl, EA, Tokalic, R, Marusic, A, Qaseem, A, et al. The reporting checklist for public versions of guidelines: RIGHT-PVG. Implement Sci. (2021) 16:10. doi: 10.1186/s13012-020-01066-z
16. Winstein, CJ, Stein, J, Arena, R, Bates, B, Cherney, LR, Cramer, SC, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2016) 47:e98–e169. doi: 10.1161/STR.0000000000000098
17. Liping, L, Weiqi, C, Hongyu, Z, Wanying, D, Shujuan, L, Xiaochuan, H, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of ischaemic cerebrovascular diseases. Stroke Vasc Neurol. (2020) 5:159–76. doi: 10.1136/svn-2020-000378
18. Yang, Y, Yang, K, Lu, Q, Zheng, Y, Huang, C, Li, Z, et al. Practice guideline for patients with ankylosing spondylitis/spondyloarthritis. Chin J Int Med. (2020) 59:511–8. doi: 10.3760/cma.j.cn112138-20200505-00448
19. Li, Y, Chen, Y, Chen, J, Shang, H, Yang, K, Guo, G, et al. Guideline protocol of non-pharmacological secondary prevention for myocardial infarction. Chin J Evid Based Med. (2016) 16:617–20. doi: 10.7507/1672-2531.20160095
20. Ma, J. A study on the construction of guidelines for patients with high-risk foot management of diabetes mellitus. Beijing Univ Chin Med. (2019). doi: 10.26973/d.cnki.gbjzu.2019.000219
21. Harrison, MB, Graham, ID, van den Hoek, J, Dogherty, EJ, Carley, ME, and Angus, V. Guideline adaptation and implementation planning: a prospective observational study. Implement Sci. (2013) 8:49. doi: 10.1186/1748-5908-8-49
22. Fu, L, Hu, Y, Zhou, Y, Zhang, X, Gu, Y, and Xing, W. CAN-IMPLEMENT: guide to integration and application methods. Chin J Evid Based Pediat. (2017) 12:69–73. doi: 10.3969/j.issn.1673-5501.2017.01.014
23. Yang, D. Construction of guidelines for patients in rehabilitation nursing of limb dysfunction after stroke Beijing University of Chinese Medicine (2022).
24. Hennink, MM, Kaiser, BN, and Marconi, VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. (2017) 27:591–608. doi: 10.1177/1049732316665344
25. Elo, S, and Kyngäs, H. The qualitative content analysis process. J Adv Nurs. (2008) 62:107–15. doi: 10.1111/j.1365-2648.2007.04569.x
26. Hosseini, M, Jahanshahlou, F, Akbarzadeh, MA, Zarei, M, and Gharamaleki, Y. Formulating research questions for evidence-based studies. J Med Surg Public Health. (2024) 2:100046. doi: 10.1016/j.glmedi.2023.10004
27. WHO (2002). International classification of functioning, Disability and Health (ICF). https://cdn.who.int/media/docs/default-source/classification/icf/icfbeginnersguide.pdf?sfvrsn=eead63d3_4&download=true (Accessed 17 July 2024).
28. Abdi, S, Spann, A, Borilovic, J, de Witte, L, and Hawley, M. Understanding the care and support needs of older people: a scoping review and categorisation using the WHO international classification of functioning, disability and health framework (ICF). BMC Geriatr. (2020) 19:195. doi: 10.1186/s12877-019-1189-9
29. Huang, Y, Yang, K, Chen, S, Xie, Y, Huang, C, and Qing, Y. Practice guideline for patients with hyperuricemia/gout. Chin J Int Med (2020);59:519–527. doi: 10.3760/cma.j.cn112138-20200505-00449
30. Dicenso, A, Bayley, L, and Haynes, RB. Accessing pre-appraised evidence: fine-tuning the 5S model into a 6S model. Evid Based Nurs. (2009) 12:99.2–99.101. doi: 10.1136/ebn.12.4.99-b
31. Chen, Y. Application of GRADE to systematic reviews and practice guidelines. 2nd ed. Beijing: Peking Union Medical College Press (2021).
32. Foster, MJ, and Shurtz, S. Making the critical appraisal for summaries of evidence (CASE) for evidence-based medicine (EBM): critical appraisal of summaries of evidence. J Med Libr Assoc. (2013) 101:192–8. doi: 10.3163/1536-5050.101.3.008
33. Meng, M, Li, X, Peng, K, Zhang, X, Yang, D, Zhang, J, et al. Cultural adaptation of the Pan-Canadian oncology symptom triage and remote support practice guide for cancer-related fatigue in China: integration of traditional Chinese medicine nursing evidence. Asia Pac J Oncol Nurs. (2023) 10:100252. Published 2023 May 31. Doi:10.1016/j.apjon.2023.100252. doi: 10.1016/j.apjon.2023.100252
34. SGIN (2022). Epilepsy in Children: Young Persons Booklet. Available at: https://www.sign.ac.uk/patient-and-public-involvement/patient-publications/epilepsy-in-children/ (Accessed July 17, 2024).
35. Shoemaker, SJ, Wolf, MS, and Brach, C. Development of the patient education materials assessment tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns. (2014) 96:395–403. doi: 10.1016/j.pec.2014.05.027
36. Pearson, A, Wiechula, R, Court, A, and Lockwood, C. The JBI model of evidence-based healthcare. Int J Evid Based Healthc. (2005) 3:207–15. doi: 10.1111/j.1479-6988.2005.00026.x
37. Doak, CC, Doak, LG, and Root, JH. Teaching patients with low literacy skills. 2nd Ed. Philadelphia: J. B. Lippincott Company, pages 49–59.
38. Li, X. Suitability evaluation of the health education text material and the health literacy intervention of Korean-Chinese older adults with hypertension. Yanbian Univ. (2013). doi: 10.7666/d.D01180415
39. Fang, J. Construction of guidelines for patients in children with refractory epilepsy on a ketogenic diet in the initial stage. Beijing Univ Chin Med. (2022). doi: 10.26973/d.cnki.gbjzu.2022.000844
40. Zhang, T, and Zhao, J. Guidelines for early rehabilitation of stroke in China. Chin J Neurol. (2017) 50:405–12. doi: 10.3760/cma.j.issn.1006-7876.2017.06.002
41. Stroke Prevention and Control Engineering Committee of the National Health and Family Planning Commission (2021). Chinese Stroke Nursing Guidelines. Available at: https://www.nhc.gov.cn/yzygj/s3593/202108/50c4071a86df4bfd9666e9ac2aaac605.shtml (Accessed July 17, 2024).
42. Li, G, Chen, H, Liu, Y, Song, X, and Jia, L. Evidence summary for good limb position Management in Hemiplegic Patients with cerebral infarction. J Nurs. (2019) 26:22–7. doi: 10.16460/j.issn1008-9969.2019.24.022
43. Chen, H, Xie, H, Li, W, Luo, Q, and Ji, Y. Evidence summary for early rehabilitation nursing of stroke patients with limb dysfunction. Milit Nurs. (2020) 37:6–10. doi: 10.3969/j.issn.1008-9993.2020.06.002
44. Liu, X, Zhu, G, Cai, Y, Yi, M, and Li, L. Synthesis of the evidence regarding functional exercise for stroke survivors. Chin Nurs Manag. (2020) 20:1689–94. doi: 10.3969/j.issn.1672-1756.2020.11.020
45. Li, X. Evidence-based optimization of TCM nursing programs for stroke Beijing University of Chinese Medicine (2019).
46. Yan, LJ, Li, SA, Jin, XJ, Yang, D, Scott, SE, Wang, ZJ, et al. Development of patient versions of guidelines in Chinese mainland: a systematic survey of current practices and methods. Patient Educ Couns. (2022) 105:3410–21. doi: 10.1016/j.pec.2022.09.009
47. Wang, R, Zhu, S, Zhou, L, Cai, J, Yan, L, and Jiang, Y. Construction of patient version of guidelines for secondary prevention of ischemic stroke. Chin Nurs Res. (2021) 35:4351–7. doi: 10.12102/j.issn.1009-6493.2021.24.003
48. Wiercioch, W, Nieuwlaat, R, Zhang, Y, Alonso-Coello, P, Dahm, P, Iorio, A, et al. New methods facilitated the process of prioritizing questions and health outcomes in guideline development. J Clin Epidemiol. (2022) 143:91–104. doi: 10.1016/j.jclinepi.2021.11.031
49. Xing, N, Zhou, Y, Fang, Y, and Li, L. Identification of health questions based on social choice theory for patient version guideline on non-pharmacological management of ges-tational diabetes mellitus. J Nurs Sci. (2022) 37:26–30. doi: 10.3870/j.issn.1001-4152.2022.16.026
Keywords: patient version of guidelines, rehabilitation care, stroke, evidence based nursing, limb dysfunction
Citation: Yang D, Zhang J, Meng M, Li X, Yan L, Fang J, Wang Z, Chen S, Zhang X, Hao Y and Wang F (2025) Empowering Stroke Survivors: developing a patient version of guidelines to facilitate patient rehabilitation nursing of stroke patients with limb dysfunction in China. Front. Public Health. 12:1482771. doi: 10.3389/fpubh.2024.1482771
Edited by:
Hammad Nazeer, Air University, PakistanReviewed by:
Fauzia Fatima Gilani, National University of Science and Technology, PakistanFarrukh Shahzad, Care Plus Medical Center, Pakistan
Copyright © 2025 Yang, Zhang, Meng, Li, Yan, Fang, Wang, Chen, Zhang, Hao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yufang Hao, YnVjbW51cnNpbmdAMTYzLmNvbQ==; Fang Wang, d2FuZ2Zhbmc4MTk4MkAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Dan Yang
Dan Yang Jingyuan Zhang1†
Jingyuan Zhang1† Meiqi Meng
Meiqi Meng Jiaxin Fang
Jiaxin Fang Sihan Chen
Sihan Chen Yufang Hao
Yufang Hao