- 1The Health and Risk Communication Lab, School of Public Health, University of Haifa, Haifa, Israel
- 2Department of Psychological Sciences, Kent State University, Kent, OH, United States
It is important to identify psychological correlates of vaccine hesitancy, including among people not from the United States (U.S.). College students were recruited between March–June 2023 in the US (n = 330, Mage = 20.21, 79.5% female) and in Israel (n = 204, Mage = 23.45, 92.6% female) to complete a cross-sectional survey on vaccine attitudes, emotions, and behavior. A 2 (Nation: US, Israel) × 2 (Vaccine Status: Vaccinated, Unvaccinated) factorial design was used. Individual ANCOVAS controlling for sociodemographic factors were conducted to test main effects of nation and vaccine status, and their interaction, across various psychological correlates of health behavior. Consistent with hypotheses, unvaccinated (vs. vaccinated) individuals reported higher perceived ambiguity, reactance, and anger as well as perceived lower susceptibility, severity, worry, and intentions to vaccinate. Unvaccinated (vs. vaccinated) individuals also reported lower positive emotion. Contrary to hypotheses, unvaccinated individuals reported greater fear. Israeli (vs. American) participants reported higher perceived ambiguity, worry, fear, and anger, as well as lower perceived susceptibility. Vaccinated Americans reported higher intentions to vaccinate again in the future (M = 2.89, SE = 0.08) compared to vaccinated Israelis (M = 2.36, SE = 0.08). However, unvaccinated Americans reported lower intentions to vaccinate (M = 1.80, SE = 0.15) than unvaccinated Israelis (M = 1.95, SE = 0.21). Findings provide insight into correlates to target for vaccine promotion and emphasize the need for cultural tailoring.
Introduction
Prior to the onset of the COVID-19 pandemic, vaccines prevented approximately 4–5 million deaths a year (1). More recent estimates indicate that at least 14.4 million deaths were prevented in 1 year by the COVID-19 vaccine (2). Additional deaths across all vaccine-preventable illnesses (e.g., Measles, Pertussis, and COVID-19) could be averted if vaccination rates increased. However, vaccine hesitancy—the delay or refusal to receive available vaccines (3)—serves as a barrier to vaccination. The purpose of the present research is to examine psychological correlates of vaccine hesitancy in a cross-cultural sample of Americans and Israelis.
Various behavioral theories provide insight into why people do not engage in protective health behavior, such as vaccination. According to the Health Belief Model (4), Theory of Planned Behavior (5), Extended Parallel Processing Model (71), the Appraisal Tendency Framework (6–8), Reactance Theory (9), PRECEDE PROCEED Model (10), and Transtheoretical Model of Behavior Change (11), several cognitive, affective, and behavioral constructs are at play in health decisions. Some of the many constructs involved in health decisions include risk perceptions, emotions, knowledge, reactance, and intentions. Other psychological variables relevant to health behavior that are often overlooked in major theories of health behavior include ambiguity and positive emotions. In the next section, we provide an overview of each of these variables, including a brief description and selected research pertaining to vaccination.
Psychological correlates of vaccine hesitancy
Risk perceptions refers to subjective beliefs pertaining to an outcome, such as illness. Individuals can hold beliefs about: their susceptibility or likelihood of contracting an illness, how severe or harmful the illness may be, as well as how worried they are about the illness (12, 13). Higher perceptions of risk about illness often predict greater vaccine use (14). However, higher perceptions of risk about vaccination, rather than the illness itself, can promote vaccine hesitancy or refusal (15).
In addition to risk perceptions, perceived ambiguity is another important psychological determinant of vaccine hesitancy. Ambiguity refers to the experience of uncertainty that specifically arises from perceiving information to be unreliable, low in credibility, or inadequate, which is often the case when information is conflicting, imprecise, or incomplete (16, 17). Perceiving ambiguity about vaccination (e.g., about side effects or the efficacy of the vaccine) can lead to avoidance of vaccination (18–20).
Next, emotions are important in understanding health behavior, as health behaviors likely occur within an emotional context (21). For example, individuals may deny or refuse vaccination because they experience fear about potential side effects of vaccination (22, 23). Anger is another emotion that may lead to hesitation to vaccinate (24, 25). Indeed, anger may activate schemas of distrust in others and lead to greater mistrust in the medical system (26). As for positive emotions (e.g., happiness, relaxation, etc.), more research is needed to understand the relationship between positive emotions and health behavior (27). However, related to vaccination, researchers have demonstrated that vaccine hesitant individuals are less likely to experience positive emotions compared to their counterparts who are more inclined to vaccinate (28). Further, there are various positive experiences (affective and cognitive) that may contribute to positive emotion—such as experiences of hope, optimism, trust, and altruism—that can, in turn, promote vaccination (25, 29–33). Indeed, vaccines may offer hope and optimism, such as in the case of a cancer vaccine or an AIDS vaccine that can improve survival outcomes and reduce transmission (34, 35). Further, fostering trust and altruistic motives may increase willingness to vaccinate (36, 37). Future cross-cultural research on vaccination behavior should assess these factors. Another factor relevant to health behavior engagement is knowledge. In particular, those who have a better understanding of what actually presents a health risk are more likely to engage in behaviors aimed at avoiding that health risk. Indeed, adults who are more knowledgeable about preventive health behaviors (e.g., handwashing or avoiding crowds) are more likely to engage in these behaviors during a pandemic (38, 39). Further, researchers have demonstrated a relationship between higher knowledge about vaccination and a positive attitude toward vaccination (40).
Finally, intentions are an especially important component of health behavior because intentions to engage in a behavior, or lack thereof, often precede the decision to engage in health behavior (41). However, experiencing reactance—a motivational state in which people attempt to re-establish autonomy in the face of feeling like their freedom is threatened (9)—can decrease intentions to vaccinate (42).
Importantly, no singular health behavior theory provides a comprehensive model of all psychological factors relevant to vaccination, and including all variables across health behavior theories would be beyond the scope of the present research. With our aim to examine psychological correlates of vaccine hesitancy, including some afforded less attention in major theories of health behavior, we selected correlates for inclusion based on variables that overlap across many different theories of health behavior (e.g., risk perception, knowledge, and intentions) or have received less attention across major theories of health behavior (e.g., ambiguity and emotions). We also included psychological reactance because this variable can be especially relevant in contexts with government involvement (43)—as was the case during the COVID-19 pandemic—that may lead individuals to feel a threat to their freedom. Thus, we expected that the real-world occurrence of the COVID-19 pandemic would be a fitting context to evaluate this psychological correlate of health behavior.
Sociodemographic factors and individual level differences relevant to vaccination
Prior research has demonstrated a relationship between general and COVID-19 specific vaccination behavior with various sociodemographic factors (44). For example, in one study conducted with US respondents, individuals who were more vaccine hesitant for COVID-19 were younger and more likely to be female and Black and American Indian or Alaskan Native (45). The direction of the relationship between various sociodemographic factors and vaccination behavior is not always consistent, such as in the case of education or religious affiliation (46).
Various individual level differences may also play a role in health behavior and thus may be relevant to vaccine hesitancy. A meta-analysis of research on health literacy—skills required for people to access, understand, and make use of health information (47) — indicated that health literacy is positively, but weakly, associated with healthier behaviors (48). In another meta-analysis on dispositional optimism, or the tendency to expect outcomes to be good (49), optimism was associated with various physical health outcomes with a small to moderate effect size (50). Another relevant and important construct is tolerance for uncertainty. Although additional research is needed to determine the extent and strength of relationships, tolerance for uncertainty has been associated with medical decision making across several studies (51). In the present study, we assessed these sociodemographic factors and individual level differences because we considered them to also be relevant to vaccination.
The present research
Although several research studies have examined the relationship among various factors relevant to health behavior and vaccination, further research is needed to include diverse populations. Including diverse populations would lead to a better understanding of what predicts vaccine behavior among different samples, which in turn, would inform strategic approaches to encourage vaccination (e.g., tailoring of health communications). Indeed, researchers concluded from a systematic review of the literature on vaccine hesitancy that most research on this topic is derived from Europe and the Americas (52).
Importantly, the present research extends upon decades of prior work on predictors of vaccine hesitancy by exploring the role of the cultural context. The goal of this research was not to test a specific health behavior theory, but rather to apply what we might expect based on major theories of health behavior to better understand psychological correlates of vaccine hesitancy in a cross-cultural context. Specifically, in the present research, we collected separate samples of American and Israeli participants in order to conduct a cross-cultural comparison of psychological correlates of vaccine hesitancy. Indeed, additional research on psychological correlates of vaccine hesitancy is needed among non-US samples. We use a 2 (Nation: US, Israel) × 2 (Vaccine Status: Vaccinated, Unvaccinated) factorial design. Further, the present research was specifically conducted in the context of the COVID-19 pandemic. However, what is learned in the present context can also provide insight for various other vaccination campaigns as well as during a future pandemic.
Hypotheses
1. Consistent with various theories of health behavior and research, we hypothesized that unvaccinated individuals (compared with vaccinated individuals) would report higher levels of perceived ambiguity and higher reactance, as well as lower risk perceptions of COVID-19, lower perceived knowledge about COVID-19 and COVID-19 vaccination, and lower intentions to vaccinate.
2. Next, we hypothesized that unvaccinated individuals (compared with vaccinated individuals) would report higher levels of anger and lower levels of fear while thinking about COVID-19 vaccination. Importantly, we included generalized measures of emotion—that is, we did not assess why individuals experienced anger or fear about COVID-19 vaccination—however, we based our hypotheses on possible reasons these emotions may have been experienced. That is, we expected that unvaccinated individuals would report experiencing higher anger in response to government mandates of vaccination, but lower fear about COVID-19 vaccination, consistent with lower risk perceptions from Hypothesis 1 (e.g., “COVID-19 is not severe and so there is no reason to feel fear from the COVID-19 vaccine as it’s unnecessary”).
3. We treated analyses regarding positive emotions as exploratory due to less research on positive emotions in the literature on health behavior.
4. Further, although we expected to observe cultural differences in the prevalence of psychological correlates of health behaviors across samples, we treated these analyses as exploratory. For example, perceptions of ambiguity or risk may differ among cultures but we did not have specific hypotheses for sample differences relevant to nationality. Rather, we examined differences across cultures to inform culture-specific interventions.
General methods
Overview
Data were collected in March–June 2023 from two studies with the same design and measures that separately took place in the United States and Israel. Recruitment occurred for each study simultaneously at Kent State University in the United States and at University of Haifa in Israel. Each university provided IRB approval. Eligibility criteria included being age 18 years or older, a resident of either the United States or Israel, and fluency in either English or Hebrew depending on respective location. Of note, although participants were not directly asked if they were an American or Israeli citizen, they were categorized as American or Israeli depending on their respective university, where they indicated living, and their language fluency. It is possible that non-citizens were incorporated into the sample, although they would likely comprise a small percentage of the overall sample. Analyses concerning relationships of perceived ambiguity with risk perceptions, emotions, intentions, and information seeking are reported elsewhere (72).
Study design and procedure
Participants were recruited using the SONA system subject pool through the Department of Psychological Sciences at Kent State University and the School of Public Health at University of Haifa. Each study was administered online through Qualtrics as a survey on attitudes and beliefs regarding vaccination. Participants first completed a screener to confirm they were eligible to participate followed by informed consent. After this step, participants completed a survey of measures including vaccination history, perceptions of ambiguity and risk, emotion, behavioral intentions, individual level differences, and demographic items.
Participants
Data collection occurred until the end of the academic semester across each university. Data were collected from 234 Israeli participants and 336 American participants. Data from 36 participants (6 Americans and 30 Israelis) were then removed due to low responsiveness (i.e., less than half the survey was completed). The final sample for analyses included 330 American and 204 Israeli participants (combined n = 534).
Measures
The survey underwent pilot testing with American and Israeli participants to confirm that participants understood each measure. Of note, all measures were translated from English to Hebrew for use with Israeli participants. To guarantee that measures were translated accurately, 3 bilingual, native Hebrew speakers reviewed the translation of measures. Measures that are relevant to hypotheses are reported below.
Vaccination status
Vaccination status was assessed with one item (created for this study): “Are you fully vaccinated against COVID-19, which means that you received either a single-dose vaccine (such as Johnson & Johnson) or a two-dose series vaccine such as Pfizer or Moderna? The names of authorized vaccines include: Pfizer, AstraZeneca, Moderna, Johnson & Johnson, Sinopharm BIBP, CoronaVac, Covaxin, Novavax, Convidecia, and Sputnik V” (coded as 0 = No, 1 = Yes). Participants were also given the option to respond “Do not know,” and those who did were recoded as missing data for this item (this only applied to 3 Israeli participants).
Psychological correlates
Three measures of risk perception were used: perceived susceptibility (adapted from (53); average of 3 items; αAmerican = 0.77, αIsraeli = 0.59), worry (adapted from (53, 54); average of 3 items; αAmerican = 0.95, αIsraeli = 0.96), and perceived severity (adapted from (55); average of 12 items; αAmerican = 0.90, αIsraeli = 0.88). Items assessing perceived susceptibility were: “I feel very vulnerable to being infected with COVID-19 in the next year” (1 = strongly disagree to 7 = strongly agree), “Overall, how likely is it that you will be infected with COVID-19 in the next year?” (1 = extremely unlikely to 7 = extremely likely) and “Overall, how do you think your chance of being infected with COVID-19 in the next year compares to other [women/men] of your age in [United States/Israel]?” Items assessing worry were: “How [anxious are you/much do you worry/much are you concerned/about being infected with COVID-19?” (1 = not at all to 7 = a lot)]. Finally, items assessing perceived severity were: “COVID-19 is [a serious condition/ dangerous/ life-threatening] for [immunocompromised individuals/older adult individuals/young adults/children] without any pre-existing health conditions”” (1 = strongly disagree to 4 = strongly agree). For the perceived severity items, participants could select “do not know,” and those who did were recoded as missing data (no participants responded “do not know” for this measure).
Perceived ambiguity (adapted from (56, 57); average of 3 items; αAmerican = 0.80, αIsraeli = 0.82) was assessed with, “There are many limitations of the existing information about COVID-19 vaccines,” “There is a lot that is unknown about COVID-19 vaccines” and “Leading scientists and experts have conflicting opinions about COVID-19 vaccines” (1 = strongly disagree, 4 = strongly agree).
Emotions (58) included subscales for fear (average of 4 items; αAmerican = 0.90, αIsraeli = 0.89), anger (average of 4 items; αAmerican = 0.92, αIsraeli = 0.95), happiness (average of 4 items; αAmerican = 0.89, αIsraeli = 0.83), and relaxed (average taken from 4 items; αAmerican = 0.89, αIsraeli = 0.85). In this measure, participants were asked to indicate the extent to which they experience specific affective states when they think about COVID-19 vaccination (1 = not at all to 7 = an extreme amount). Items used to assess fear include “fear,” “worry,” “panic,” and “scared.” Items used to assess anger include “anger,” “rage,” “mad,” and “pissed off.” Items used to assess happiness include “happy,” “enjoyment,” “satisfaction,” and “liking.” Finally, items used to assess relaxation include: “calm,” “relaxation,” “chilled out,” and “easygoing.”
Two separate items were used to assess perceived knowledge: perceived knowledge about COVID-19 (59) and perceived knowledge about COVID-19 vaccination [modified from (59)]. The former was assessed with: “Overall, how would you rate your level of knowledge about COVID-19 (for example, what it is, how it is transmitted, how to protect yourself, etc.)?” and the latter was assessed with: “Overall, how would you rate your level of knowledge about COVID-19 vaccination (for example, what options there are, what are the benefits and side effects, etc.)?” (1 = no knowledge at all to 4 = a lot of knowledge; 5 = do not know). Responses of “do not know” were again coded as missing data (for the perceived knowledge about COVID-19 item, this only applied to 10 American participants and 7 Israeli participants, and for the perceived knowledge about COVID-19 vaccination item, this only applied to 9 American participants and 9 Israeli participants.
Reactance [adapted from (60); average of 3 items; αAmerican = 92, αIsraeli = 87] included items such as “Vaccination recommendations from the government annoy me” and “The government is trying to manipulate me with these vaccination recommendations” (1 = strongly disagree; 5 = strongly agree).
Intentions (created for this study) consisted of a single item: “I intend to get vaccinated against COVID-19 at some point in the future” (1 = strongly disagree; 4 = strongly agree).
Sociodemographic factors and individual level differences
Standard demographic items were measured: age (continuous), gender (coded as 0 = female, 1 = male), year in school (coded as 1 = freshman, 2 = sophomore, 3 = junior, 4 = senior, and 5 = graduate student), race (in the American sample only; coded as 0 = non-white, 1 = white) and religious affiliation (in the Israeli sample only; coded as 0 = non-Jewish, 1 = Jewish). Participants also reported individual level differences. Tolerance for ambiguity (61) was assessed as the average of 6 items (1 = strongly disagree to 4 = strongly agree; αAmerican = 0.73, αIsraeli = 0.76). In this measure, participants were asked to imagine they are “considering having a medical test that checks for cancer,” but conflicting opinions about the test exist. They were then asked to rate their agreement with statements such as “I would be afraid of trying the test” (1 = strongly disagree, 4 = strongly agree). Health literacy (62) was assessed as the average of 3 items, such as “How often do you have problems learning about a medical condition because of difficulty understanding written information?” (1 = none of the time to 5 = all of the time; αAmerican = 0.57, αIsraeli = 0.23). Finally, dispositional optimism (63) was assessed as the average of 6 items, such as “I rarely count on good things happening to me” (scored so that higher values indicate greater optimism; 1 = strongly disagree to 5 = strongly agree; αAmerican = 0.85, αIsraeli = 0.65).
Overview of analyses
All analyses were conducted in IBM SPSS Statistics Version 27. First, we conducted chi square tests and ANOVAs (depending on whether the dependent measure was a categorical or continuous variable), to determine whether American and Israeli participants differed on any sociodemographic and individual level difference variables. Sociodemographic and individual level difference variables that were not equally distributed across groups were then controlled for in subsequent ANCOVAs that were used to test hypotheses. Next, 12 ANCOVAs controlling for gender, age, education, health literacy, and dispositional optimism were conducted to test main effects of nation and vaccine status, and their interaction, across various psychological correlates of health behavior including: health cognitions (perceived ambiguity, perceived susceptibility, worry, perceived severity, perceived knowledge about COVID-19, perceived knowledge about COVID-19 vaccination, and reactance), emotion (fear, anger, happiness and relaxation), and vaccination intentions.
Results
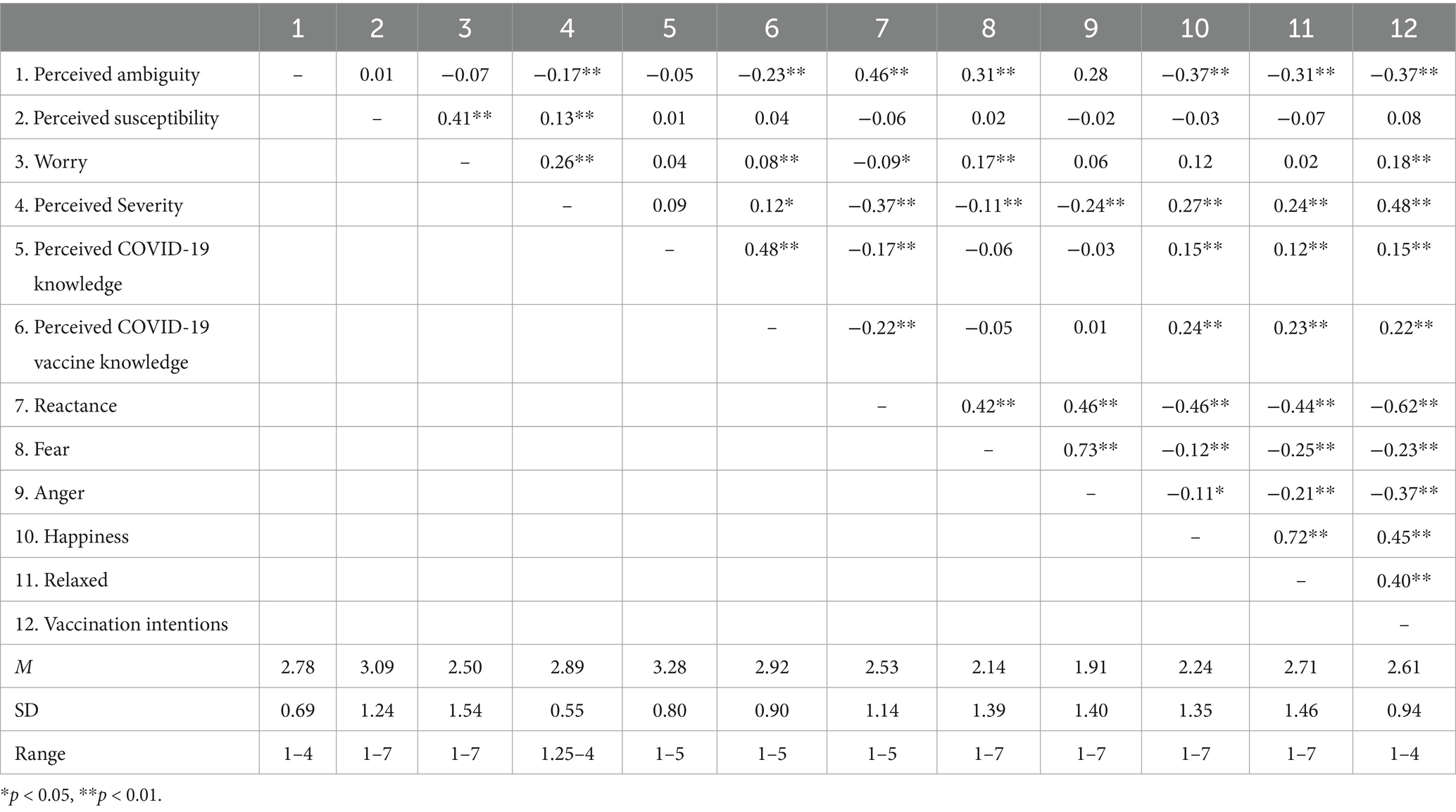
See Table 1 for bivariate correlations among study variables. The nature of these correlations was generally consistent with expectations. For example, individuals who reported higher worry about COVID-19, perceived higher severity of COVID-19, and higher knowledge about COVID-19 and COVID-19 vaccines also reported higher intentions to vaccinate. Further, individuals who experienced higher reactance reported lower intentions to vaccinate. With respect to variables that are not generally considered in major theories of health behavior, such as perceived ambiguity and emotion, we note that people who perceived higher ambiguity about COVID-19 vaccines also perceived COVID-19 to be less severe, reported lower knowledge about COVID-19 vaccines, experienced higher reactance, had lower intentions to vaccinate, and also reported higher fear, lower happiness, and lower relaxation. In the interest of brevity, we do not provide an extensive discussion of all correlations, because these analyses were secondary to the others reported and discussed in more detail.
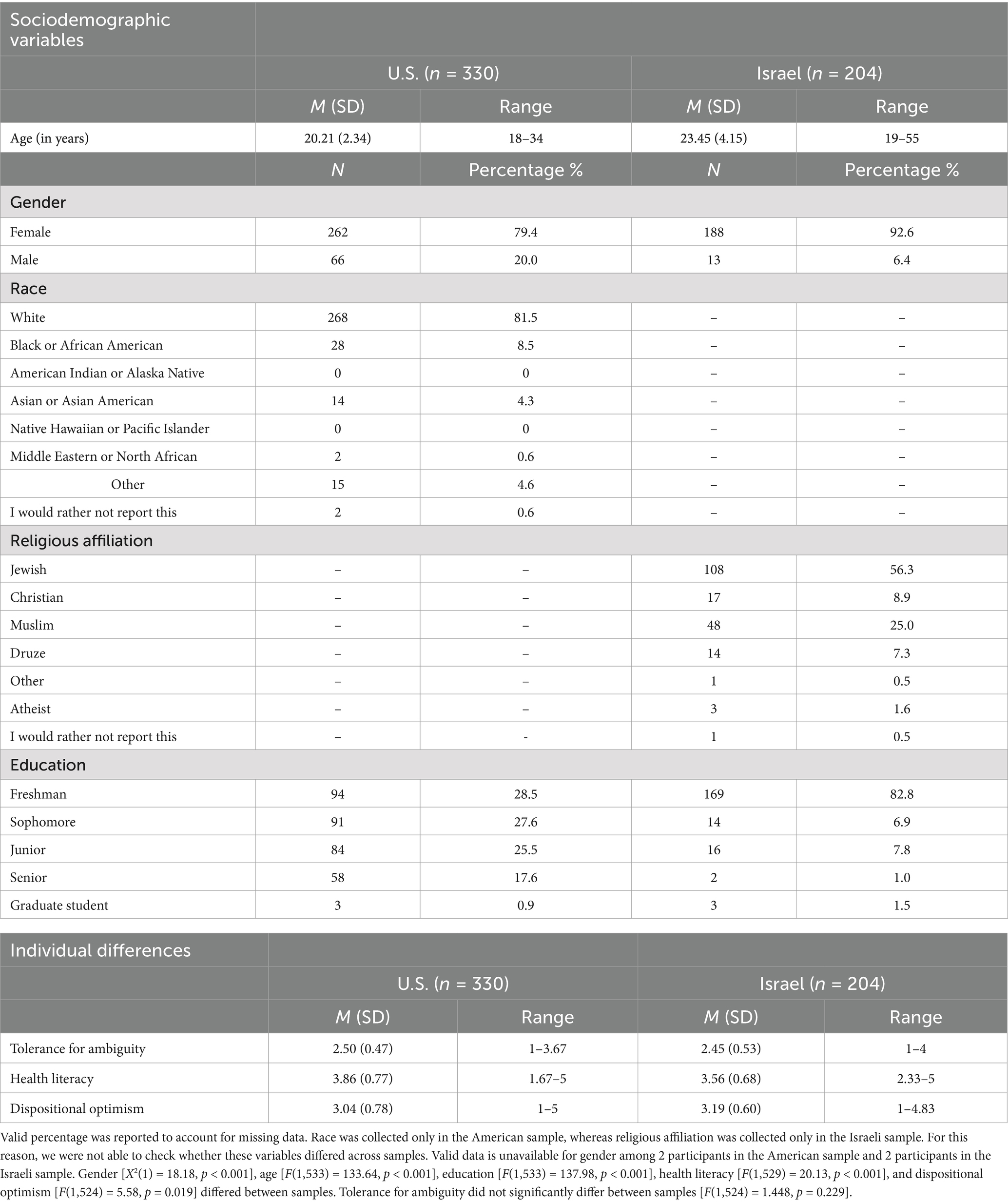
See Table 2 for the distribution of sociodemographic characteristics and individual level differences among samples. Findings from preliminary chi square tests and ANOVAs demonstrated that the samples of American and Israeli participants differed on several sociodemographic and individual level difference factors: gender [X2(1) = 18.18, p < 0.001], age [F(1,533) = 133.64, p < 0.001], education [F(1,533) = 137.98, p < 0.001], health literacy [F(1,529) = 20.13, p < 0.001], and dispositional optimism [F(1,524) = 5.58, p = 0.019]. Compared with the Israeli sample, the American sample was younger, had a greater proportion of males (21.5% male in the American sample versus 7.4% male in the Israeli sample), and had a higher level of education (i.e., there were more Americans at a later year in school). Further, compared with the Israeli sample, the American sample self-reported higher health literacy, but lower levels of dispositional optimism. Thus, these factors were controlled for in subsequent ANCOVAs.
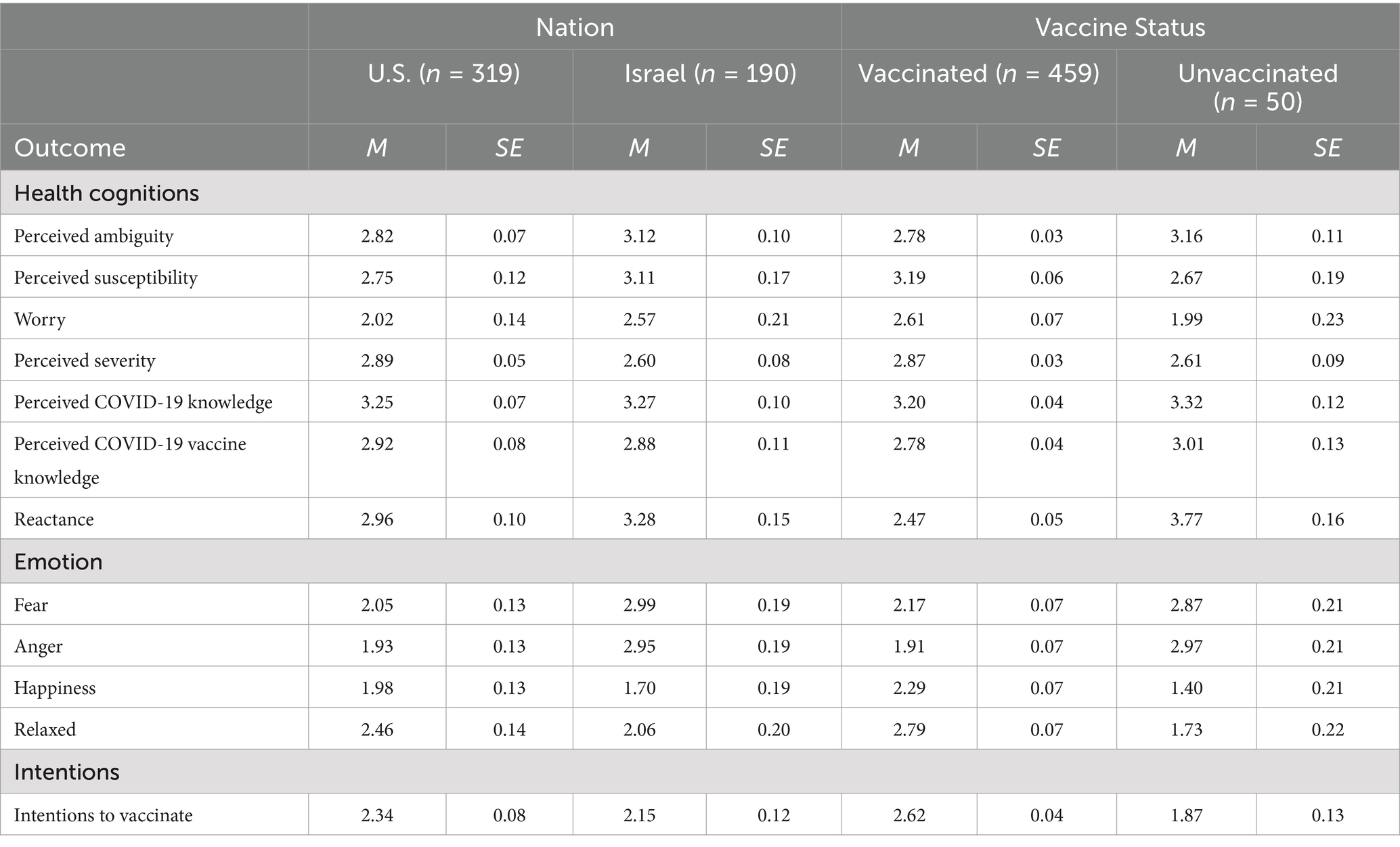
See Table 3 for descriptive statistics and Table 4 for inferential statistics from ANCOVAs. When reviewing the main effects of Nation (US, Israel) on various psychological correlates of health behavior, Israeli participants reported higher perceptions of ambiguity, higher worry, higher fear, and higher anger compared to American participants. However, Israeli participants reported lower perceived severity of COVID-19 compared to American participants. There were no significant differences in perceived susceptibility, perceived knowledge about COVID-19 and COVID-19 vaccination, reactance, happiness, relaxation, or vaccination intentions as a function of nation. When reviewing the main effects of Vaccination Status (Vaccinated, Unvaccinated) on various psychological correlates of health behavior, there were significant differences between vaccinated and unvaccinated participants on perceptions of ambiguity, perceptions of susceptibility, perceptions of severity, worry, reactance, fear, anger, happiness, relaxation, and intentions to vaccinate. Of note, significant differences between vaccinated and unvaccinated individuals on these factors were mostly consistent with hypotheses and theoretically expected relationships. Consistent with hypotheses, unvaccinated individuals reported higher perceptions of ambiguity, higher reactance, and higher anger compared to vaccinated participants. Further, unvaccinated individuals reported lower perceptions of susceptibility, lower perceptions of severity, lower worry about getting COVID-19, lower positive emotion (happiness and relaxation), and lower intentions to vaccinate in the future for COVID-19 compared to their vaccinated counterparts. Inconsistent with hypotheses, unvaccinated individuals reported higher fear compared with vaccinated participants. There were no significant differences in perceived knowledge about COVID-19 or COVID-19 vaccination as a function of vaccination status.
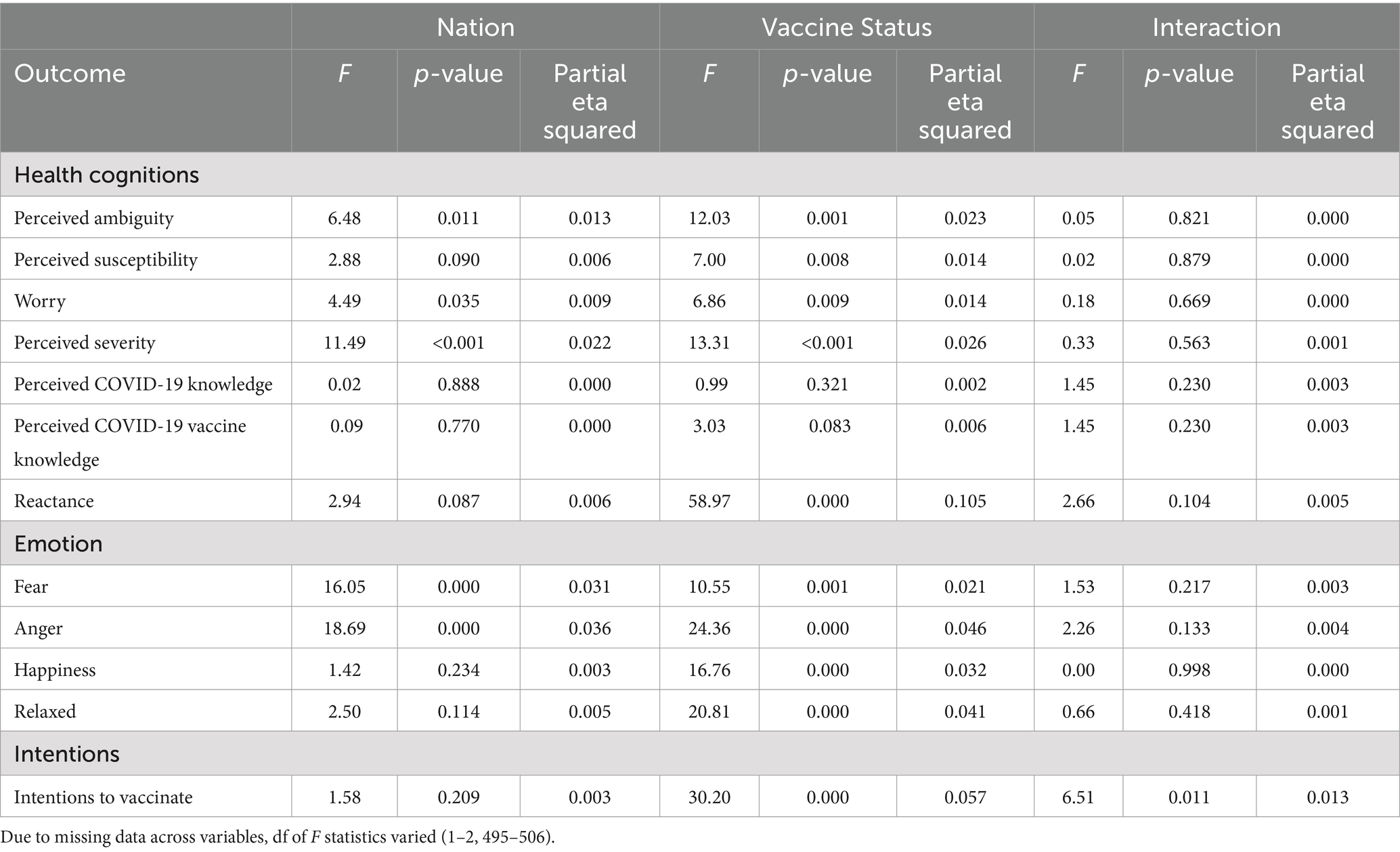
Table 4. Inferential statistics of nation, vaccine status, and their interaction on health cognitions, emotions, and intentions.
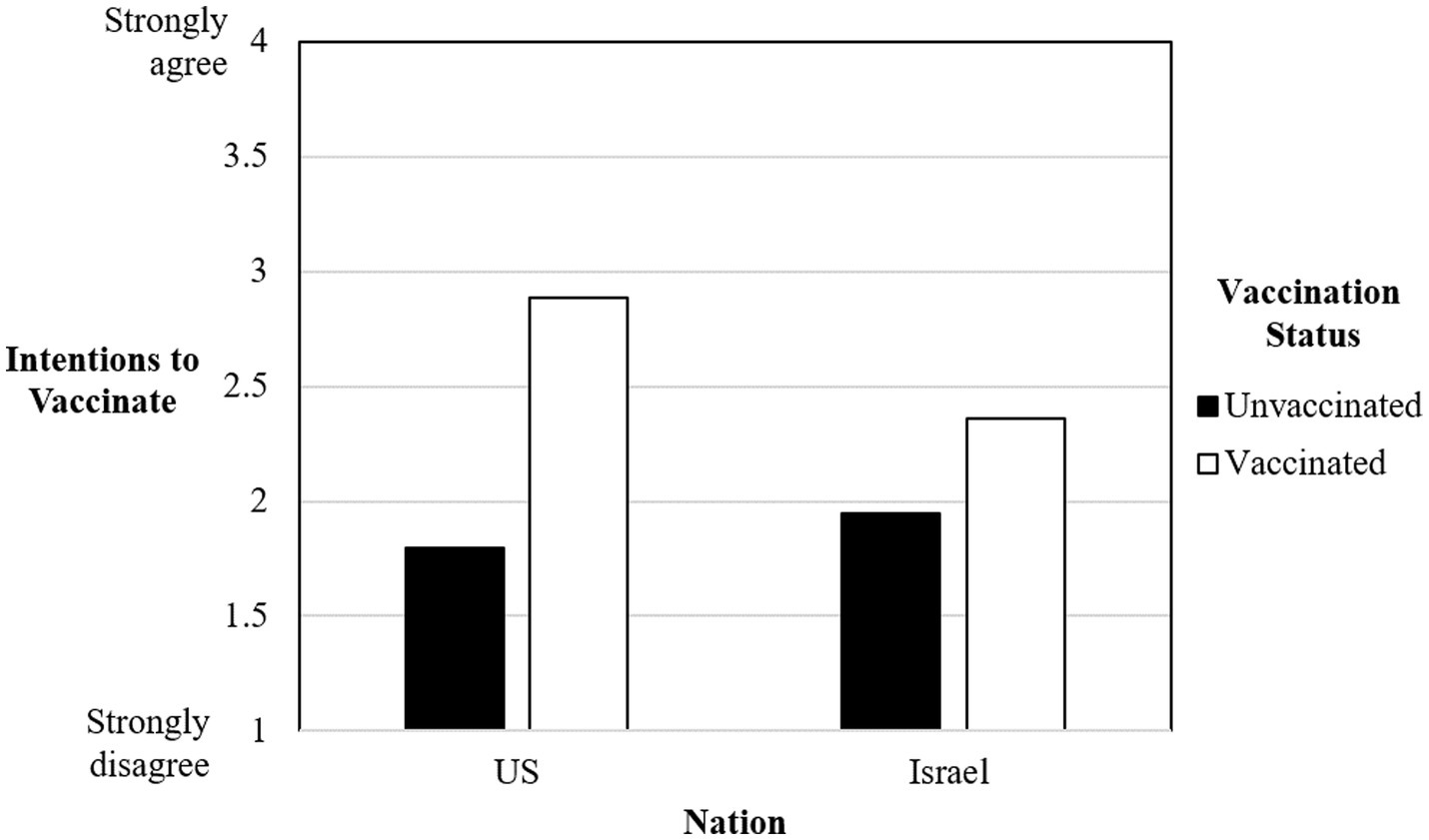
There was only one significant interaction between nation and vaccination status, and this was in regard to intentions to vaccinate. Vaccinated Americans reported higher intentions to vaccinate (M = 2.89, SE = 0.08) compared to vaccinated Israelis (M = 2.36, SE = 0.08). However, unvaccinated Americans reported lower intentions to vaccinate (M = 1.80, SE = 0.15) compared to unvaccinated Israelis (M = 1.95, SE = 0.21). See Figure 1 for a depiction of this relationship.
Discussion
Vaccine hesitancy is considered one of the top threats to global health (64). Thus, it is important to better understand vaccine hesitant individuals to appropriately intervene. Beyond a broad need to better understand vaccine hesitancy, there is a more immediate need to understand cultural differences and tailor behavioral health interventions appropriately. In the present study, we examined psychological correlates of vaccine hesitancy in a cross-cultural sample of Americans and Israelis. Although findings across samples were mostly consistent with hypotheses and theory, there were differences across cultures.
Psychological correlates of vaccine hesitancy
Compared with participants who self-reported that they were vaccinated, those who self-reported that they were not vaccinated also reported in the present research that they perceived higher ambiguity about the COVID-19 vaccines, felt higher negative emotion and lower positive emotion about the COVID-19 vaccines, experienced higher reactance about vaccination recommendations, thought they were less susceptible to be infected with COVID-19, thought that getting COVID-19 was less severe, felt less worry about getting COVID-19, and indicated lower intentions to receive a future COVID-19 vaccination. Overall, findings are consistent with how these psychological correlates of health behavior are expected to operate across various theoretical frameworks. These results are also mostly consistent with hypotheses, with the exception of one finding. Inconsistent with the hypothesis that unvaccinated individuals would report lower fear when thinking about COVID-19 vaccines compared with vaccinated individuals, we instead found that unvaccinated individuals reported higher fear. This result may have occurred if unvaccinated individuals were unvaccinated in part due to fear of the vaccines themselves.
Overall, a different profile of thoughts and feelings between vaccinated and unvaccinated individuals emerged. Importantly, findings provide concrete areas for intervention when it comes to vaccine hesitancy. That is, public health officials and practitioners might focus on changing these thoughts and feelings of unvaccinated individuals to match those held by vaccinated individuals. For example, focusing on decreasing perceptions of ambiguity with “normalization of uncertainty” interventions [(e.g., 20, 65)] may prove useful. Further, applying a self-affirmation intervention can reduce the effects of reactance [(e.g., 66)]. Indeed, the present research provides tangible areas to focus on for vaccination interventions.
Despite several differences, vaccinated and unvaccinated participants did not differ in their perceptions of knowledge about COVID-19 and COVID-19 vaccination. It is possible that the timing of data collection and the saturation of information about COVID-19 led to similar levels of perceived knowledge among vaccinated and unvaccinated individuals across both countries. More specifically, the pandemic had been ongoing for several years at the time of data collection. Further, technology had increased the availability and overwhelm of several voices on COVID-19, referred to as a “saturation” effect (67). In turn, people across countries may have generally felt knowledgeable about COVID-19 and COVID-19 vaccination. Indeed, the average responses to the perceived knowledge measures were above the midpoint for both American and Israeli participants.
Cross-cultural differences
Israeli participants reported higher perceptions of ambiguity about COVID-19 vaccines, higher fear and higher anger about COVID-19 vaccines, as well as higher worry about COVID-19, compared to American participants. Further, Israeli participants reported lower perceptions of COVID-19 severity compared to American participants. Although exact reasons for these cultural level differences is unknown, these differences underscore the need to examine health behavior within a cultural context. One interpretation for these cultural differences may be related to politicization of the vaccine. Indeed, the vaccines were highly politicized in both countries, but there was stronger involvement of authorities and limits to freedom in Israel during the vaccine rollout. COVID-19 vaccines were disseminated in Israel earlier than other countries due to a deal with Pfizer that allowed Pfizer to collect individuals’ personal vaccine data. Additionally, this deal also made Pfizer the dominant vaccine available in Israel, compared with more options that were available in the United States and elsewhere around the world. The United States and much of the world followed the data on vaccine efficacy and rollout from Israel’s vaccination campaign (73). This arrangement and subsequent debates among Israeli experts regarding vaccination policy may have created more vaccine reluctance and hesitation among the Israeli sample (68). Further, Israel also offered a “green pass” incentive at a federal level to allow people who were fully vaccinated, participating in a vaccine trial, or who recently recovered from COVID-19 to have access to locations that were otherwise closed off to prevent the spread of infection [i.e., businesses; (69)]. This restriction on movement at a federal level, although done to help prevent spread of infection, may have contributed to more negative sentiment among the Israeli sample.
Beyond the political context, several additional factors may help explain the observed differences between Israeli and American participants. First, differences in socio-cultural characteristics may have played a role. Israel’s more collectivist society with dense social networks (74) may have amplified the spread of both emotions and opinions about vaccination among community members. In contrast, a stronger emphasis on individualism and personal rights in the United States (75) may have led to more varied reactions to COVID-19 vaccines. Second, differences in media environment may have been important. Israel’s small size may have facilitated more uniform media coverage of vaccination issues through mainstream channels. The more diverse media landscape and multiple information sources in the United States (see for example (76))—including the prevalence of social media as a source of COVID-19 news (77)—and the polarization of trust in various news outlets (78) may have created less unified social norms around vaccination, allowing for a broader range of perspectives and potentially influencing emotional responses. Third, Israel’s centralized healthcare system, while enabling rapid and uniform policy implementation, may have intensified feelings of institutional control. The decentralized U.S. system allowed for more flexibility in vaccine rollout and policy enforcement, potentially reducing feelings of systemic pressure. Fourth, the historical context between countries may also explain differences in results. Israel’s previous experience with national emergencies may have influenced both institutional trust and emotional responses to government mandates. The United States has a longer history of vaccine debates predating COVID-19 (79), which may have positioned the COVID-19 vaccine within an existing framework of vaccine attitudes. Finally, demographic differences in average age, population density, and family structure between the countries may have influenced risk perception and vaccine attitudes. Additionally, varying levels of ethnic and cultural diversity between the nations may have affected institutional trust and response to health policies.
Indeed, paying greater attention to cross-cultural differences in vaccine hesitancy can allow the respective health ministries in each country to then frame health communications based on the needs of their respective populations. Future researchers may even consider whether these higher perceptions of ambiguity, fear, and anger about COVID-19 vaccines or lower perceptions of COVID-19 severity may have had an unintended spillover effect among Israelis toward other vaccines and vaccine-preventable illnesses.
Interaction effect
In the present research, whether individuals were vaccinated or not was associated with whether individuals also reported they were interested in receiving a future COVID-19 vaccination. First, vaccinated Americans reported higher intentions to receive a COVID-19 vaccine in the future compared to vaccinated Israelis. Second, unvaccinated Americans reported lower intentions to vaccinate in the future compared to unvaccinated Israelis. Thus, again, it is important to examine how health behavior might differ in different cultural contexts.
Limitations
There are limitations of the present research. First, we recruited convenience samples from universities, and the samples are not nationally representative. Indeed, as demonstrated by Table 2, most of the participants in the present research were young adult females, with limited diversity in gender and age. Indeed, males and females differ in COVID-19 risk perceptions and vaccine hesitancy, such that females perceive higher COVID-19 risk, but also tend to be more hesitant toward vaccination (70). Future research should include a more diverse sample in terms of age and gender, and also consider factors such as socioeconomic status. Second, there were also more vaccinated than unvaccinated participants, and future research should increase efforts to recruit unvaccinated participants. Third, data were collected while the pandemic was ongoing for several years (i.e., March–June 2023) rather than at the start of the pandemic in March 2020. Thus, associations among variables may have been weaker than at the start of the pandemic. Fourth, we cannot identify why certain cross-cultural differences exist, as this requires more in-depth research. Indeed, qualitative work may be beneficial for interviewing individuals and isolating themes relevant to their vaccination decisions. Fourth, we examined emotions about COVID-19 vaccination generally, and the exact target of negative and positive emotions (i.e., why participants experienced the specific emotions in regard to COVID-19 vaccination) was not examined. Future research should delve further into understanding these emotions. Additionally, the intentions item was written to be broad to apply to both vaccinated and unvaccinated individuals’ experiences (i.e., “I intend to get vaccinated against COVID-19 at some point in the future”). Thus, it is unknown how participants specifically interpreted this measure. Indeed, individuals may have a difference in opinion regarding the primary vaccination vs. additional booster shots, and this may have been reflected in their answers. Future research might consider these differences.
Conclusion
In the present research, we use cross-sectional data to provide a description of public perceptions about COVID-19 vaccination among vaccinated and unvaccinated Israeli and American adults. Findings revealed cross-cultural differences between the United States and Israel on psychological correlates of vaccine hesitancy. Continued cross-cultural research is necessary for increased vaccination efforts through tailoring of vaccination materials.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Kent State University IRB (approval number 20-166) and the University of Haifa IRB (approval number 463/22). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NS: Conceptualization, Formal analysis, Methodology, Resources, Writing – original draft, Writing – review & editing. AG-E: Conceptualization, Methodology, Resources, Supervision, Writing – review & editing. JT: Conceptualization, Methodology, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
Dr. Simonovic gratefully acknowledges financial support for a postdoctoral fellowship during the time of this research from the Fulbright U.S. Scholars Program, which is sponsored by the U.S. Department of State and the Fulbright Israel Commission. The contents of this publication are solely the responsibility of the author and do not necessarily represent the official views of the Fulbright Program, the Government of the United States, or the Fulbright Israel Commission.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization (2019). Immunization. Available at: https://www.who.int/news-room/facts-in-pictures/detail/immunization (Accessed July 1, 2024).
2. Watson, OJ, Barnsley, G, Toor, J, Hogan, AB, Winskill, P, and Ghani, AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Diseases. (2022) 22:1293–302. doi: 10.1016/S1473-3099(22)00320-6
3. World Health Organization, (2015). Vaccine hesitancy: a growing challenge for immunization programmes. Retrieved from https://www.who.int/news/item/18-08-2015-vaccine-hesitancy-a-growing-challenge-for-immunization-programmes (Accessed July 1, 2024).
4. Rosenstock, IM, Strecher, VJ, and Becker, MH. Social learning theory and the health belief model. Health Educ Q. (1988) 15:175–83.
6. Lerner, JS, and Keltner, D. Beyond valence: toward a model of emotion-specific influences on judgement and choice. Cognit Emot. (2000) 14:473–93. doi: 10.1080/026999300402763
7. Lerner, JS, and Keltner, D. Fear, anger, and risk. J Personal Soc Psychol. (2001) 81:146. doi: 10.1037/0022-3514.81.1.146
8. Lerner, JS, and Tiedens, LZ. Portrait of the angry decision maker: How appraisal tendencies shape anger's influence on cognition. J Behav Decision Making. (2006) 19:115–37. doi: 10.1002/bdm.515
10. Green, LW. Toward cost-benefit evaluations of health education: some concepts, methods, and examples. Health Educ Monographs. (1974) 2:34–64.
11. Prochaska, JO. Decision making in the transtheoretical model of behavior change. Med Decision Making. (2008) 28:845–9. doi: 10.1177/0272989X08327068
12. El-Toukhy, S. Parsing susceptibility and severity dimensions of health risk perceptions. J Health Commun. (2015) 20:499–511. doi: 10.1080/10810730.2014.989342
13. Ferrer, RA, and Klein, WM. Risk perceptions and health behavior. Curr Opinion Psychol. (2015) 5:85–9. doi: 10.1016/j.copsyc.2015.03.012
14. Brewer, NT, Chapman, GB, Gibbons, FX, Gerrard, M, McCaul, KD, and Weinstein, ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. (2007) 26:136–45. doi: 10.1037/0278-6133.26.2.136
15. Dubé, E, Laberge, C, Guay, M, Bramadat, P, Roy, R, and Bettinger, J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. (2013) 9:1763–73. doi: 10.4161/hv.24657
16. Han, PKJ. Uncertainty and ambiguity in health decisions In: MA Diefenbach, S Miller-Halegoua, and DJ Bowen, editors. Handbook of health decision science. New York, NY: Springer (2016). 133–44.
17. Ellsberg, D. Risk, ambiguity, and the Savage axioms. Q J Econ. (1961) 75:643–69. doi: 10.2307/1884324
18. Azarpanah, H, Farhadloo, M, Vahidov, R, and Pilote, L. Vaccine hesitancy: evidence from an adverse events following immunization database, and the role of cognitive biases. BMC Public Health. (2021) 21:1686. doi: 10.1186/s12889-021-11745-1
19. Courbage, C, and Peter, R. On the effect of uncertainty on personal vaccination decisions. Health Econ. (2021) 30:2937–42. doi: 10.1002/hec.4405
20. Han, PKJ, Zikmund-Fisher, BJ, Duarte, CW, Knaus, M, Black, A, Scherer, AM, et al. Communication of scientific uncertainty about a novel pandemic health threat: ambiguity aversion and its mechanisms. J Health Commun. (2018) 23:435–44. doi: 10.1080/10810730.2018.1461961
21. Ferrer, RA, and Mendes, WB. Emotion, health decision making, and health behaviour. Psychol Health. (2018) 33:1–16. doi: 10.1080/08870446.2017.1385787
22. Facciolà, A, Visalli, G, Orlando, A, Bertuccio, MP, Spataro, P, Squeri, R, et al. Vaccine hesitancy: an overview on parents' opinions about vaccination and possible reasons of vaccine refusal. J Public Health Res. (2019) 8:1436. doi: 10.4081/jphr.2019.1436
23. Loehr, J, and Savoy, M. Strategies for addressing and overcoming vaccine hesitancy. Am Fam Physician. (2016) 94:94–6.
24. Stevens, H, Rasul, ME, and Oh, YJ. Emotions and incivility in vaccine mandate discourse: natural language processing insights. JMIR Infodemiol. (2022) 2:e37635. doi: 10.2196/37635
25. Chou, WS, and Budenz, A. Considering Emotion in COVID-19 Vaccine Communication: Addressing Vaccine Hesitancy and Fostering Vaccine Confidence. Health Commun. (2020) 35:1718–22. doi: 10.1080/10410236.2020.1838096
26. Tselebis, A, Sikaras, C, Milionis, C, Sideri, EP, Fytsilis, K, Papageorgiou, SM, et al. A moderated mediation model of the influence of cynical distrust, medical mistrust, and anger on vaccination hesitancy in nursing staff. Eur J Investig Health Psychol Educ. (2023) 13:2373–87. doi: 10.3390/ejihpe13110167
27. Cameron, DS, Bertenshaw, EJ, and Sheeran, P. The impact of positive affect on health cognitions and behaviours: a meta-analysis of the experimental evidence. Health Psychol Rev. (2015) 9:345–65. doi: 10.1080/17437199.2014.923164
28. Zhou, Y, Li, R, and Shen, L. Psychological profiles of COVID vaccine-hesitant individuals and implications for vaccine message design strategies. Vaccine. (2023) X, 13:100279. doi: 10.1016/j.jvacx.2023.100279
29. Baumgaertner, B, Carlisle, JE, and Justwan, F. The influence of political ideology and trust on willingness to vaccinate. PLoS ONE. (2018) 13:e0191728. doi: 10.1371/journal.pone.0191728
30. Delporte, M, Luyts, M, Molenberghs, G, Verbeke, G, Demarest, S, and Hoorens, V. Do optimism and moralization predict vaccination? A five-wave longitudinal study. Health Psychol. (2023) 42:603–14. doi: 10.1037/hea0001272
31. Marlow, LA, Waller, J, and Wardle, J. Trust and experience as predictors of HPV vaccine acceptance. Human Vaccines. (2007) 3:171–5. doi: 10.4161/hv.3.5.4310
32. Petersen, MB, Christiansen, LE, Bor, A, et al. Communicate hope to motivate the public during the COVID-19 pandemic. Sci Rep. (2022) 12:2502. doi: 10.1038/s41598-022-06316-2
33. Soveri, A, Karlsson, LC, Mäki, O, Antfolk, J, Waris, O, Karlsson, H, et al. Trait reactance and trust in doctors as predictors of vaccination behavior, vaccine attitudes, and use of complementary and alternative medicine in parents of young children. PLoS ONE. (2020) 15:e0236527. doi: 10.1371/journal.pone.0236527
34. Drew, L. Cancer-vaccine trials give reasons for optimism. Nature. (2024) 627:S33. doi: 10.1038/d41586-024-00840-z
35. Robinson, H. New hope for an aids vaccine. Nat Rev Immunol. (2002) 2:239–50. doi: 10.1038/nri776
36. Bonafide, KE, and Vanable, PA. Male human papillomavirus vaccine acceptance is enhanced by a brief intervention that emphasizes both male-specific vaccine benefits and altruistic motives. Sex Transm Dis. (2015) 42:76–80. doi: 10.1097/OLQ.0000000000000226
37. Make, J, and Lauver, A. Increasing trust and vaccine uptake: offering invitational rhetoric as an alternative to persuasion in pediatric visits with vaccine-hesitant parents (VHPs). Vaccine. (2022) 10:100129. doi: 10.1016/j.jvacx.2021.100129
38. Rincón Uribe, FA, Godinho, RCS, Machado, MAS, Oliveira, KRDSG, Neira Espejo, CA, de Sousa, NCV, et al. Health knowledge, health behaviors and attitudes during pandemic emergencies: a systematic review. PLoS One. (2021) 16:e0256731. doi: 10.1371/journal.pone.0256731
39. Clavel, N, Badr, J, Gautier, L, Lavoie-Tremblay, M, and Paquette, J. Risk perceptions, knowledge and behaviors of general and high-risk adult populations towards COVID-19: a systematic scoping review. Public Health Rev. (2021) 42:1603979. doi: 10.3389/phrs.2021.1603979
40. Bălan, A, Bejan, I, Bonciu, S, Eni, CE, and Ruță, S. Romanian medical students' attitude towards and perceived knowledge on COVID-19 vaccination. Vaccine. (2021) 9:854. doi: 10.3390/vaccines9080854
41. Webb, TL, and Sheeran, P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. (2006) 132:249–68. doi: 10.1037/0033-2909.132.2.249
42. Verpaalen, IAM, Ritter, SM, van Hooff, MLM, van Stekelenburg, A, Fransen, ML, and Holland, RW. Psychological reactance and vaccine uptake: a longitudinal study. Psychol Health. (2023):1–21. doi: 10.1080/08870446.2023.2190761
43. Laurin, K, Kay, AC, and Fitzsimons, GJ. Reactance versus rationalization: divergent responses to policies that constrain freedom. Psychol Sci. (2012) 23:205–9. doi: 10.1177/0956797611429468
44. McElfish, PA, Willis, DE, Shah, SK, Bryant-Moore, K, Rojo, MO, and Selig, JP. Sociodemographic determinants of COVID-19 vaccine hesitancy, fear of infection, and protection self-efficacy. J Prim Care Commun Health. (2021) 12:21501327211040746. doi: 10.1177/21501327211040746
45. Reece, S, CarlLee, S, Scott, AJ, Willis, DE, Rowland, B, Larsen, K, et al. Hesitant adopters: COVID-19 vaccine hesitancy among diverse vaccinated adults in the United States. Inf Med. (2023) 2:89–95. doi: 10.1016/j.imj.2023.03.001
46. Ayyalasomayajula, S, Dhawan, A, Karattuthodi, M, Thorakkattil, SA, Suhaj, A, Elnaem, M, et al. A systematic review on sociodemographic, financial and psychological factors associated with COVID-19 vaccine booster hesitancy among adult population. Vaccine. (2023) 11:623. doi: 10.3390/vaccines11030623
47. World Health Organization (2009). Track 2: Health literacy and health behaviour. Available at: https://www.who.int/teams/health-promotion/enhanced-wellbeing/seventh-global-conference/health-literacy (Accessed July 1, 2024)
48. Elkin, N. The relationship between health literacy and healthy lifestyle behaviors: a meta-analysis. Medicine. (2024) 103:e40260. doi: 10.1097/MD.0000000000040260
49. Scheier, MF, and Carver, CS. Dispositional optimism and physical health: a long look back, a quick look forward. Am Psychol. (2018) 73:1082–94. doi: 10.1037/amp0000384
50. Rasmussen, HN, Scheier, MF, and Greenhouse, JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. (2009) 37:239–56. doi: 10.1007/s12160-009-9111-x
51. Strout, TD, Hillen, M, Gutheil, C, Anderson, E, Hutchinson, R, Ward, H, et al. Tolerance of uncertainty: a systematic review of health and healthcare-related outcomes. Patient Educ Couns. (2018) 101:1518–37. doi: 10.1016/j.pec.2018.03.030
52. Larson, HJ, Jarrett, C, Eckersberger, E, Smith, DM, and Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. (2014) 32:2150–9. doi: 10.1016/j.vaccine.2014.01.081
53. Taber, JM, McQueen, A, Simonovic, N, and Waters, E. Adapting a self-affirmation intervention for use in a mobile application for smokers. J Behav Med. (2019) 42:1050–61. doi: 10.1007/s10865-019-00028-1
54. Weinstein, ND, Kwitel, A, McCaul, KD, Magnan, RE, Gerrard, M, and Gibbons, FX. Risk perceptions: assessment and relationship to influenza vaccination. Health Psychol. (2007) 26:146–51. doi: 10.1037/0278-6133.26.2.146
55. Lipkus, IM, Green, LG, and Marcus, A. Manipulating perceptions of colorectal cancer threat: implications for screening intentions and behaviors. J Health Commun. (2003) 8:213–28. doi: 10.1080/10810730305684
56. Simonovic, N, and Taber, JM. Perceptions of ambiguity about cigarettes and e-cigarettes among users and non-users. Ann Behav Med. (2020) 54:S665–5.
57. Simonovic, N, and Taber, JM. Psychological impact of ambiguous health messages about COVID-19. J Behav Med. (2021) 45:159–71. doi: 10.1007/s10865-021-00266-2
58. Harmon-Jones, C, Bastian, B, and Harmon-Jones, E. The discrete emotions questionnaire: a new tool for measuring state self-reported emotions. PLoS ONE. (2016) 11:e0159915. doi: 10.1371/journal.pone.0159915
59. Thompson, CA, Taber, JM, Sidney, PG, Fitzsimmons, CJ, Mielicki, MK, Matthews, PG, et al. Math matters: A novel, brief educational intervention decreases whole number bias when reasoning about COVID-19. J Experiment Psychol. (2021) 27:632. doi: 10.1037/xap0000403
60. Hall, MG, Sheeran, P, Noar, SM, Ribisl, KM, Boynton, MH, and Brewer, NT. A brief measure of reactance to health warnings. J Behav Med. (2017) 40:520–9. doi: 10.1007/s10865-016-9821-z
61. Han, PK, Reeve, BB, Moser, RP, and Klein, WM. Aversion to ambiguity regarding medical tests and treatments: measurement, prevalence, and relationship to sociodemographic factors. J Health Commun. (2009) 14:556–72. doi: 10.1080/10810730903089630
62. Chew, LD, Bradley, KA, and Boyko, EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. (2004) 36:588–94.
63. Carver, CS, and Scheier, MF. Dispositional optimism. Trends Cogn Sci. (2014) 18:293–9. doi: 10.1016/j.tics.2014.02.003
64. World Health Organization (2019). Ten threats to global health in 2019. Available at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (Accessed July 1, 2024).
65. Han, P, Scharnetzki, E, Scherer, AM, Thorpe, A, Lary, C, Waterston, LB, et al. Communicating scientific uncertainty about the COVID-19 pandemic: online experimental study of an uncertainty-normalizing strategy. J Med Internet Res. (2021) 23:e27832. doi: 10.2196/27832
66. Schüz, N, Schüz, B, and Eid, M. When risk communication backfires: randomized controlled trial on self-affirmation and reactance to personalized risk feedback in high-risk individuals. Health Psychol. (2013) 32:561–70. doi: 10.1037/a0029887
67. Lloyd, A, and Hicks, A. Saturation, acceleration and information pathologies: the conditions that influence the emergence of information literacy safeguarding practice in COVID-19-environments. J Document. (2022) 78:1008–26. doi: 10.1108/JD-08-2021-0162
68. Gesser-Edelsburg, A, Zemach, M, and Hijazi, R. Who are the “real” experts? The debate surrounding COVID-19 health risk management: an Israeli Case Study. Risk Manage Healthcare Policy. (2021):2553–69. doi: 10.2147/RMHP.S311334
69. Kamin-Friedman, S, and Peled Raz, M. Lessons from Israel's COVID-19 green pass program. Israel J Health Policy Res. (2021) 10:1–6. doi: 10.1186/s13584-021-00496-4
70. Toshkov, D. Explaining the gender gap in COVID-19 vaccination attitudes. Eur J Public Health. (2023) 33:490–5. doi: 10.1093/eurpub/ckad052
71. Witte, K. Putting the fear back into fear appeals: The extended parallel process model. Commun. Monogr. (1992). 59:329–349. doi: 10.1080/03637759209376276
72. Simonovic, N, Gesser-Edelsburg, A, and Taber, JM. Testing psychological correlates of ambiguity aversion in the context of COVID-19 vaccination: Evidence for motivated reasoning and the appraisal tendency framework. (2024). [Manuscript submitted for publication].
73. Feuer, W. Israeli data suggest mass vaccinations led to drop in severe Covid cases, CDC study finds. (2001). Available at: https://www.cnbc.com/2021/02/26/israeli-data-suggest-mass-vaccinations-led-to-drop-in-severe-covid-cases-cdc-study-finds.html (Accessed November 25, 2024).
74. Fischer, CS, and Shavit, Y. Natiodal differences in network density: Israel and the United States. Social Networks, (1995). 17, 129–145. doi: 10.1016/0378-8733(94)00251-5
75. Hofstede, G. Culture’s consequences: Comparing values, behaviors, institutions and organizations across nations. (2nd ed.) Thousand Oaks, CA: Sage. (2001). doi: 10.1016/S0005-7967(02)00184-5
76. Young, C, Feldman, S, and Mendez, B. How media sources distort Americans’ understanding of reality. (2024). Available at: https://www.ipsos.com/en-us/how-media-sources-distort-americans-understanding-reality. (Accessed November 25, 2024).
77. Mitchell and Liedke, About four-in-ten Americans say social media is an important way of following COVID-19 vaccine news. (2021). Available at: https://www.pewresearch.org/short-reads/2021/08/24/about-four-in-ten-americans-say-social-media-is-an-important-way-of-following-covid-19-vaccine-news/ (Accessed November 25, 2024).
78. Orth, T., and Bialik, C. Trust in Media 2024: Which news sources Americans trust — and which they think lean left or right. (2024). Available at: https://today.yougov.com/politics/articles/49552-trust-in-media-2024-which-news-outlets-americans-trust (Accessed November 25, 2024).
Keywords: vaccine hesitancy, health behavior, risk perception, emotions, ambiguity, intentions
Citation: Simonovic N, Gesser-Edelsburg A and Taber JM (2025) Examining psychological correlates of vaccine hesitancy: a comparative study between the US and Israel. Front. Public Health. 12:1480419. doi: 10.3389/fpubh.2024.1480419
Edited by:
Carlos Alberto De Oliveira Magalhães Júnior, State University of Maringá, BrazilReviewed by:
Brittany Shoots-Reinhard, The Ohio State University, United StatesAlberto dos Santos de Lemos, Oswaldo Cruz Foundation (Fiocruz), Brazil
Copyright © 2025 Simonovic, Gesser-Edelsburg and Taber. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicolle Simonovic, bmljb2xsZXNAYmd1LmFjLmls
†Present addressNicolle Simonovic,Department of Nursing,Recanati School for Community Health Professions, Ben-Gurion University of the Negev, Beer-Sheva, Israel
Nicolle Simonovic, orcid.org/0000-0003-0384-7103
Anat Gesser-Edelsburg, orcid.org/0000-0003-4467-8799
Jennifer M. Taber, orcid.org/0000-0003-3285-4871
 Nicolle Simonovic
Nicolle Simonovic Anat Gesser-Edelsburg
Anat Gesser-Edelsburg Jennifer M. Taber
Jennifer M. Taber