- 1Johns Hopkins University School of Nursing, Baltimore, MD, United States
- 2Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD, United States
- 3University of Pennsylvania School of Nursing, Philadelphia, PA, United States
- 4Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, PA, United States
Background: Despite increased insurance coverage since 2010, racial and ethnic minorities in the United States still receive less medical care than White counterparts. The Johns Hopkins School of Nursing’s Center for Community Programs, Innovation, and Scholarship (COMPASS Center) provides free wellness services, aiming to address healthcare disparities in the neighborhoods.
Objective: To delineate the types and cost of wellness services provided by the COMPASS Center.
Methods: The study employed a secondary analysis design, utilizing Qualtrics surveys to assess wellness service data from 2017 to 2022 at two main program sites—Wald center and House of Ruth, Maryland.
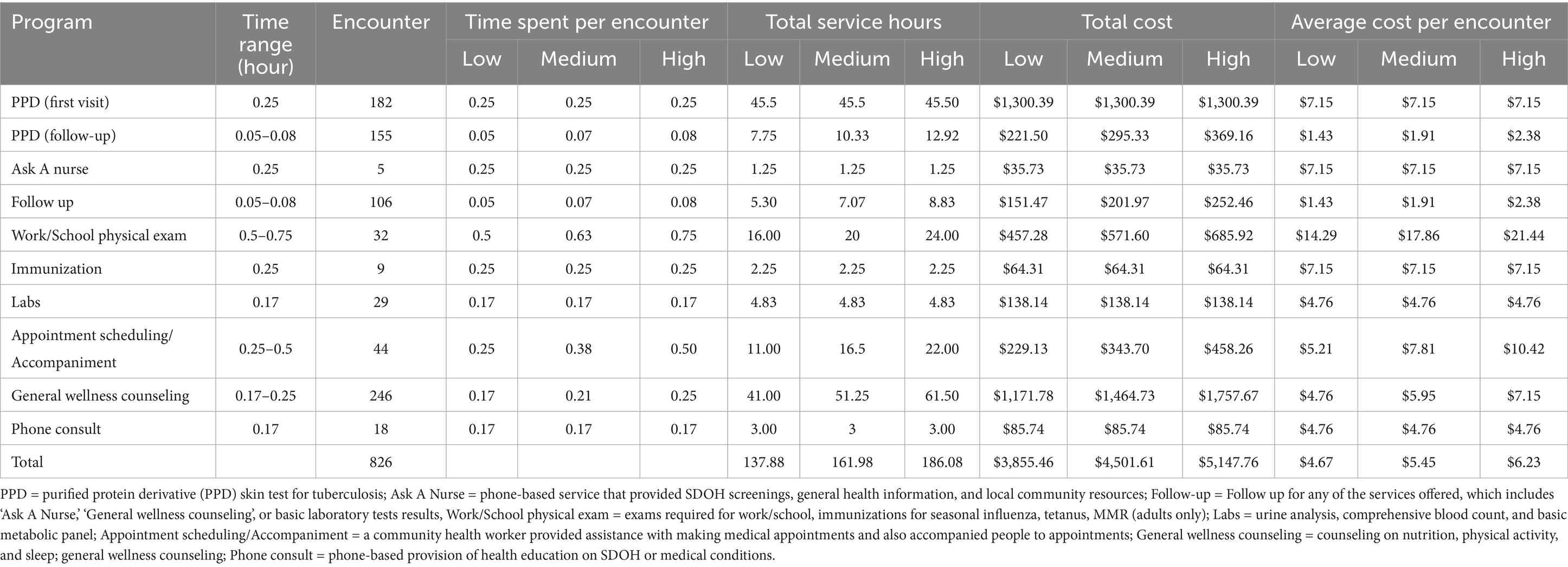
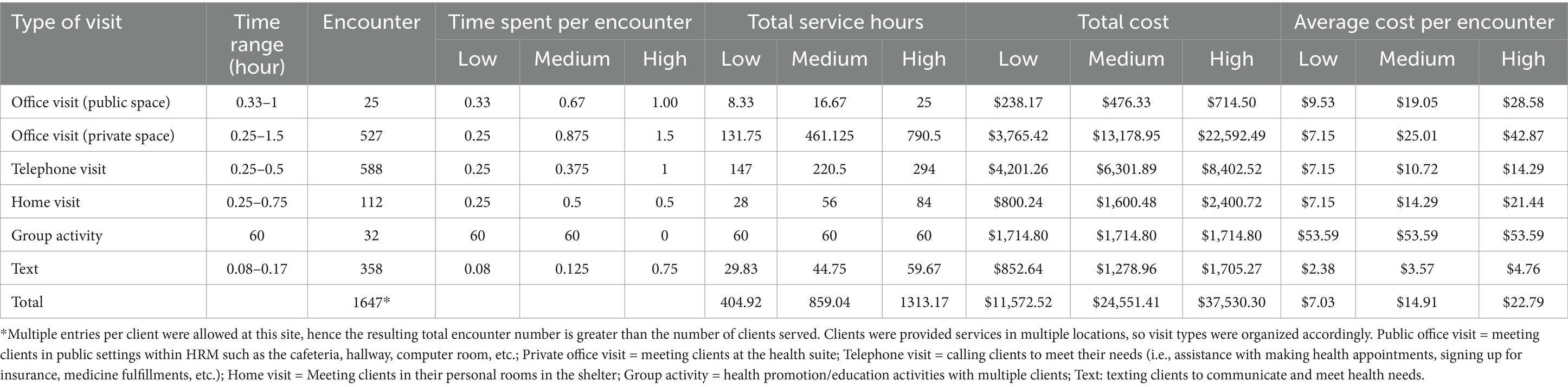
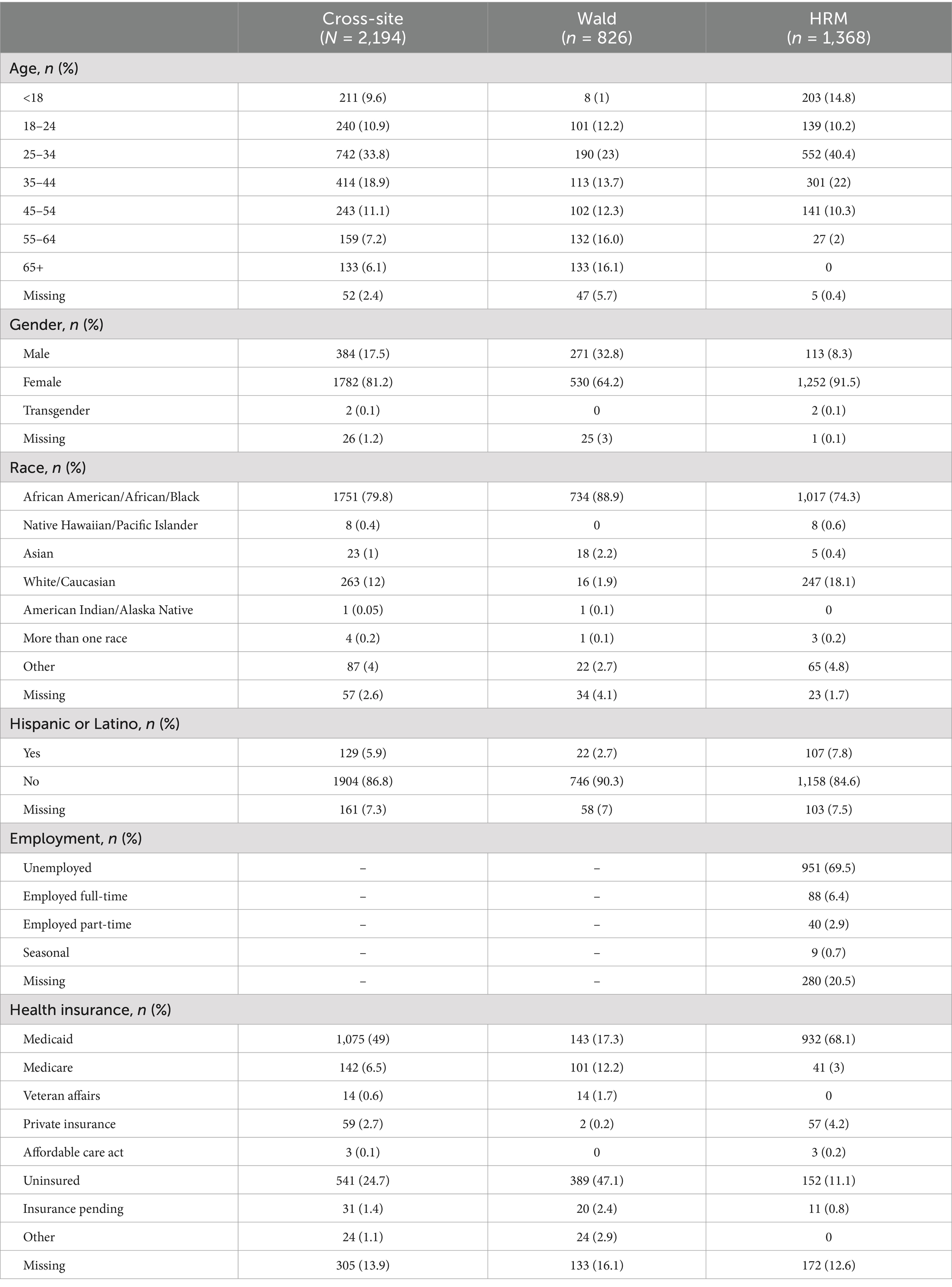
Results: The analysis covered 2,194 encounters (826 at Wald center and 1,368 at House of Ruth, Maryland). Most encounters at both sites served African American/African/Black and low-income individuals. Examples of wellness services included pre-employment exams and immunizations, health literacy and self-care management education, health insurance advice, parenting support, and referrals to community resources. Cost analysis revealed varying expenses per encounter, with medium costs ranging from $5.45 to $14.91 across sites, considering service type and duration, including staff salaries, encounter numbers, and service hours.
Conclusion: The COMPASS Center delivers essential wellness services supplementing traditional healthcare to disadvantaged community members through student engagement and academic support. The next generation of healthcare teams is learning with and from the community creating a holistic educational experience in building skills outside of institutional bedsides. Future plans involve structured training for students and center staff to provide wellness services, while expanding social service referrals. More work is needed to evaluate the impact of our wellness services on client satisfaction and wellness improvements.
Background
The healthcare model in the United States (U.S.) is diverse and dynamic with a mix of providers as well as private and public insurers. Since the enactment of the Affordable Care Act in 2010, the national uninsured rate has decreased from 16 to 8.5% (1). While governmental efforts have improved overall coverage rates in the U.S. population, this does not necessarily reflect equal access to healthcare. Racial and ethnic disparities are particularly pronounced, with studies showing that racial and ethnic minority groups often face limited access to care, lower quality of care, and, consequently, worse health outcomes compared to White individuals (2–4). These disparities are partly due to a number of institutional barriers, such as racial biases and the unequal distribution of the healthcare budget (5, 6). As the U.S. population becomes increasingly diverse, with projections indicating that people of color will represent over half of the population by 2050 (2), addressing these disparities has become a priority.
In an effort to mitigate these inequalities, community-level initiatives, such as federally qualified health centers and free clinics, have been shown to positively impact health outcomes among vulnerable populations (7). Acknowledging the impact of these community-centered efforts, the Johns Hopkins School of Nursing has made significant investments in the neighborhood, fulfilling part of its mission to promote ‘the health of individuals and diverse communities locally.’ In 1994, the school established the Lillian C. Wald Community Wellness Center to provide health screenings, health education and counseling, vaccinations, and referrals at no charge to low-income, uninsured, or underinsured residents (referred to as ‘wellness services’ hereafter). Since then, the school has expanded its community-based health promotion programs to include additional sites such as House of Ruth Maryland—a transitional housing facility for women escaping from domestic violence—and Northeast Market—a neighborhood market selling fresh products and other goods—in Baltimore, Maryland.
Currently, the school’s Center for Community Programs, Innovation, and Scholarship (COMPASS Center) serves as an operational umbrella for the school’s community wellness service initiatives (8). One unique aspect of COMPASS Center initiatives is that all activities are delivered by nursing students and nurses from the school’s academic programs (e.g., master’s entry into nursing, DNP and PhD programs), under the supervision of nursing faculty. One unique aspect of COMPASS Center initiatives is that all activities are delivered by nursing students and nurses from the school’s academic programs (e.g., master’s entry into nursing, DNP, and PhD programs), supervised by nursing faculty. This student-centered approach has proven to be a highly effective model for delivering services to communities (9). Although similar wellness programs are offered by other academic institutions (9, 10), our program provides a broader range of wellness services, extending beyond basic health screenings to include support for women experiencing domestic violence.
Given our sustained efforts to promote health and wellness among underserved individuals in the community, it is important to understand the impact of our work. While this program was intended to provide free healthcare services without profit, understanding its costs and benefits allows us to evaluate its impact on the community and assess the efficacy of the program model in comparison to alternatives (11–13). Therefore, the purposes of this analysis were two-fold: (1) To describe the types and nature of health and wellness services provided to the community, and (2) To estimate the cost associated with providing these services.
Methods
Design and data sources
The study design was a secondary analysis of the wellness service data captured through Qualtrics surveys. The first time a Qualtrics survey was created to enter wellness service-related encounters was in 2017. Since then, additional Qualtrics surveys were created for different years, sites, and initiatives. We pooled all available Qualtrics surveys at the time of this analysis, covering encounter data collected from January 2017 to March 2021 on the clients served at the Lillian C. Wald Community Wellness Center (Wald Center hereafter) (n = 1,382), and from January 2017 to March 2022 on the clients served at the House of Ruth Maryland (n = 1,378), yielding a total of 2,760 clients across sites (Note: Anonymous data is available upon request through https://livejohnshopkins.sharepoint.com/:x:/r/sites/SONCCIAS/_layouts/15/Doc.aspx?sourcedoc=%7BBDA248C7-3BD5-41E9-BB73-D6AADF2E89F0%7D&file=Wald_Clean.xlsx&action=default&mobileredirect=true).
Procedures
Upon the approval by the Johns Hopkins Medicine Institutional Review Board, the study team pooled the raw community health and wellness service data from the Qualtrics server. The Qualtrics surveys included questions about the date of service, client age, gender, race/ethnicity, medical history, any health problems addressed during the encounter, types of visits and services received, assisting staff during the encounter, and any referrals made. These surveys were completed by assisting staff (e.g., nursing student, licensed registered nurse, or community health worker) at the time of the visit. No personal identifiers were collected. Additionally, the team reached out to several faculty and staff who had working knowledge and experiences with wellness services offered by COMPASS Center to clarify types and nature of services while obtaining further details about staff who provided such services (e.g., nursing student, licensed registered nurse, or community health worker) or estimated time spent on each type of services as such level of detailed information was not collected as part of the encounter survey at the time of this analysis.
Analysis
Due to different types of wellness services provided, each site coded service encounters differently in the Qualtrics surveys. The team created shared data coding between the two sites to create a pooled dataset. After creating the pooled and cleaned dataset, we used descriptive statistics to summarize client characteristics and counts of wellness services. Of note, 486 of the 1,382 clients recorded at the Wald Center were research participants who came in for in-person data collection. Additionally, 80 clients (70 for Wald and 10 for House of Ruth Maryland) did not record encounter types and/or nature. After removing them, the final dataset included data from a total of 2,194 clients (n = 826 for Wald and n = 1,368 for House of Ruth Maryland).
For this cost analysis, the study team created a new variable—time spent on each service. The team used ranges of time spent on each service (as opposed to specific time values, unless standard time values were available) based on COMPASS Center faculty and staff recollection. The time range for each type of service is described in Tables 1, 2. For analysis purpose, if an encounter time range was 10–15 min, we assigned 10, 12.5, and 15 min for low, medium, and high time points, respectively. All minutes were then converted to hours to generate costs per service based on the hourly salary of the staff person who provided the service. Staff who provided wellness services were registered nurses and a community health worker at the school. The estimated hourly wage for community registered nurse was $28.58 per hour, which corresponds to the national mean wage for registered nurses reported in the 2021 U.S. Bureau of labor statistics national occupational wage estimates (14). The hourly wage of a community health worker was estimated as $20.83 per hour. Cumulative total cost per service was calculated by multiplying service encounter hours for each service type by the corresponding hourly wage. The average cost per encounter was estimated by total cost divided by total encounters.
Results
Characteristics of clients
The Wald Center and the House of Ruth Maryland served different clients and naturally, provided different types of wellness services. At the Wald Center, the majority of clients were adults aged between 25 and 34 years (23%). More women (64.2%) sought wellness services compared to men (32.8%). The majority of people were identified as African American/African/Black (88.9%), and as non-Hispanic or Latino (90.3%). Nearly half (47.1%) were uninsured and 17.3% had Medicaid. At House of Ruth Maryland, clients were often between the ages of 25 and 34 (40.4%) and almost all of the clients served were female (91.5%). More than two thirds of the clients identified as African American/African/Black (74.3%). About 69.5% of House of Ruth clients were unemployed and 68.1% had Medicaid (Table 3).
Description of types and nature of wellness services
Tables 1, 2 provide lists of services offered at Wald Center and House of Ruth Maryland, respectively. The types of services offered at Wald Center mainly consisted of pre-employment physical exams and vaccinations, whereas health maintenance and education were prioritized at the House of Ruth Maryland.
There were nine types of services provided at Wald, which included purified protein derivative (PPD) skin test for tuberculosis and/or follow-up (for reading of the skin test result), Ask A Nurse (a phone-based service that provided social determinants of health screening and general health information as well as connecting patients with local community resources), general follow-up for any of the services offered at the center, work/school physical examinations, immunizations for seasonal influenza, tetanus, and Measles, Mumps, and Rubella (MMR) (adults only), basic laboratory tests, medical appointment scheduling, general wellness counseling, and phone consultations. Basic laboratory tests (e.g., urine analysis, comprehensive blood count, and basic metabolic panel) were available for those who came for an initial physical examination. The appointment scheduling service was led by a community health worker who accompanied the patients to their necessary appointments for medical and/or social services. General wellness counseling embraced nutrition, physical activity, and sleep. Lastly, phone consultations were used to provide health education and referrals to address social determinants of health or ongoing medical care for patients.
At the House of Ruth Maryland, services were rendered in group and individual settings by community health nurses who operated the health suite within the transitional shelter. The nurses met with clients within the health suite, in public areas within the shelter, via phone or text communication, and in residents’ rooms. The nurses addressed episodic health concerns by conducting blood pressure and blood sugar screenings, providing over-the-counter medications per protocol or consultations for over-the-counter medications that were available on-site (e.g., pain or allergy relief medications, cortisone, calamine lotion, antacids, multi- and prenatal vitamins, and antifungal medications). The health suite had medications for both adult and pediatric populations. To address episodic concerns among clients at the House of Ruth, the nurses also administered seasonal flu vaccines and conducted physical exams to assess symptom acuity and need for referral to primary care or emergency care services. Health assessments were also performed on children in need of daycare and childcare approval. The nurses also assisted families with accessing pharmacies, obtaining health insurance, and connected them to primary care and other necessary health services. The nurses also facilitated “Health Talks” on different health topics such as self-breast examinations, nutrition, mental health, and personal hygiene to educate and promote the health of shelter clients.
Estimated costs associated with wellness services
Tables 1, 2 also outline the estimated costs associated with each type of visit, categorized by low, medium, and high ranges of service times at both sites. Services at the Wald Center were provided by community registered nurses and a community health worker to a total of 826 individuals, incurring a total cost ranging from $3,855.46 to $5,147.76, with the average cost per encounter across the various programs ranging from $4.67 to $6.23. For the PPD, patients completed intake forms and skin tests during the initial encounter and returned for result follow-ups. Initial visits (n = 182) lasted 15 min, while return visits (n = 155) lasted 3–5 min. Initial encounters cost $7.15, while subsequent visits ranged from $1.43 to $2.38 per encounter. The work/school physical exam required the longest service time at 30–45 min among the various programs. Despite the relatively small number of encounters (n = 32), this service had the highest average cost per encounter, ranging from $14.29 to $21.44. General wellness counseling had the highest total encounters (n = 246), with a cost per encounter ranging from $4.76 to $7.15 due to its shorter service time. Appointment scheduling had the second-highest cost at $10.42 per encounter. Lastly, despite the differences in encounter numbers and service durations, the immunization service, appointment scheduling, and Ask A Nurse program had the same average cost per encounter at $7.15. Similarly, labs and phone consult showed an identical cost per encounter at $4.76.
In contrast to Wald where single entry per encounter was recorded, multiple entries were allowed per encounter at the House of Ruth Maryland. Consequently, the number of encounters recorded (n = 1,647) was larger than the number of clients served at this site (n = 1,368). The total costs were estimated at $11,572.52 for the low estimated time, $24,551.41 for the medium time, and $37,530.30 for the high range of hours. The average costs per encounter across the various programs at this site ranged from a low of $7.03 to a high of $22.79. Looking at each program, community nurses provided office visits either in a public space or in a private space. For office visits in a public space, the service time per encounter was estimated to be between 20 and 60 min. With 25 encounters, the estimated costs ranged from $238.17 (low) to $714.50 (high). The mean cost per encounter was $9.53 (low), $19.05 (medium), and $28.58 (high) within each time range. On the other hand, office visits in a private space had a higher encounter count (n = 527) with a time range of 15 to 90 min. The total estimated cost for these encounters varied from $3765.42 to as high as $22,592.49. The average cost per encounter spanned from $7.15 to $42.87. Similar to office visits, home visits also addressed individual needs, with 112 recorded encounters. The total estimated cost for home visits varied between $800.24 and $2,400.72. The average cost per encounter ranged from $7.15 to $21.44. Telephone visits, highly demanded service with the highest encounter numbers (n = 588), had a time range of 15–30 min per encounter. The total estimated cost for telephone visits ranged between $4,201.26 and $8402.52. Despite the high encounter numbers, the relatively short encounter type resulted in an average cost per encounter ranging from $7.5 to $14.29. This site also provided group activity which involved 32 individuals, accounting for a total of 60 h. The average cost per encounter for group activities was $53.59. Counseling services through text messages, with a brief duration of 5–10 min per communication, totaled 358 encounters; the average cost per encounter ranged from $2.38 to $4.76.
Discussion
The current analysis revealed that a neighborhood-based nursing center affiliated with an academic institution has provided a wide ranges of wellness services to individuals in the neighborhood, most of whom were African American or Black, low-income, uninsured, and unemployed. It is particularly important to address the needs of these populations, as prior studies have shown that Black individuals experience a higher prevalence of lack of health insurance and unmet health needs compared to White individuals, due to both structural and racial/ethnic disparities (15). The historical segregation of minority groups across the U.S. means that Black individuals are more likely to live in medically underserved areas, where quality care is often unavailable, creating significant barriers to essential primary care services (16). By engaging nursing students and licensed registered nurses in the academic programs as the main providers of the wellness services, the costs were estimated to be low, with medium costs per encounter of $5.45 and $14.91 at Wald Center and House of Ruth Maryland, respectively.
By way of providing health screening and other types of wellness programs to local residents, our community nurses had a first-hand opportunity to understand and address the health needs of the community. The provision of service-learning activities has been noted as an innovative strategy for providing nursing and allied health students with a population perspective of health (17–19). Other community-oriented service models have been reported. For example, the mobile clinic model has served high-needs populations by offering health outreach, harm reduction services, and referrals at convenient community locations (20, 21). Our service model is academic center-based registered nurses who are in the graduate programs and are supervised by nursing faculty with advanced practice credentials and doctoral degrees. Student engagement in this type of service enhances empathy, knowledge, and the intent to practice in underserved populations—key aspects of future healthcare professionals’ development (10). One study also estimated the educational value provided to students in a student-run free clinic at $73,751 annually (22). Such service not only benefits the community but also provides significant value to the school. Research is warranted to investigate student perspectives and experiences to work as community nurses and how it impacts their orientation and skills to act as health agents in promoting health equity.
One of the key services offered was PPD testing. PPD testing (for Tuberculosis infection) is recommended or required for individuals who live or work in high-risk settings such as correctional facilities, nursing homes, or homeless shelters and healthcare workers (23). While it was not clearly documented in the Qualtrics forms as to in what context PPD testing was requested, it is likely that the testing was done as part of pre-employment health screenings as these tests were all onsite-based. Decades of research support the relationship between employment and better health (24). Individuals with low incomes have worse health status than the general U.S. population (25), due to limited or lack of resources that could bolster their health such as access to health insurance and necessary healthcare (24, 26). Pre-employment health screening is an essential step for certain individuals to whom it is required. Neighborhood-based pre-employment health screening such as ours may help promote employability among low-income and unemployed people who otherwise may not have access to such services. Future research should investigate if community-based nurse-led pre-employment health screening can affect individual’s economic viability through employment and subsequent health outcomes.
More than two thirds of the encounters at the House of Ruth Maryland were private office visits or phone visits where one-on-one services were provided. Similar to the wellness services offered at the Wald Center, the one-on-one services offered on site encompassed health screenings (e.g., PPD) and immunizations (e.g., hepatitis B) that are often required for employment (27). Of note, at this particular site, a homeless shelter and transitional housing facility for both women and their children escaping violence, our nurses also provided health assessments for children in need of daycare and childcare approval. Transitional or temporary housing offers people experiencing homelessness with interim housing stability and supportive services such as life skills training, mental health services, legal services, and employment assistance (28). Prior research has primarily addressed the outcomes of housing interventions on mental health, safety, and stress among women experiencing intimate partner violence (29). In contrast, the evidence gaps in investigating outcomes related to their children and/or how different types of supportive services are associated with long-term outcomes for these women such as employment. Financial stability was associated with higher odds of survivors transitioning into the ‘doing better’ class (as opposed to being in the ‘high abuse’ or ‘still affected’ class) over 6 months among survivors seeking services from domestic violence agencies (30). Taken together, it would be important to understand the impacts our wellness services may have on the lives of women and children in transitional housing.
Healthcare expenses are a major barrier to accessing care services. Policy changes that directly address the financing challenges faced by marginalized populations face are imperative. While the Affordable Care Act has provided much-needed insurance support to many, additional policies are needed to expand insurance plan coverage and advance home-based care services, making healthcare more affordable (31). Furthermore, care models that bring health services directly to the community, such as the efforts at the Wald Center and the health suite at the House of Ruth, may help make healthcare more available and accessible to those who need it most.
Limitations
The encounter data did not have specific information addressing time spent on each service. To enable comprehensive cost estimation, we created three different cost estimation models based on faculty and staff recollections. While those with prior knowledge and experience with the wellness services offered by COMPASS Center generally provided uniform responses, their recollections may have been influenced by recall bias. The dataset was also cross-sectional in nature. Whether these encounters resulted in health outcome changes remained unknown. It would be important to evaluate program outcomes in terms of increasing linkage to primary care services, emergency department overuse avoidance and delivering essential supplies, as has been reported for mobile clinics (21, 32). Additionally, we did not have access to data on non-personnel costs associated with wellness service encounters. A report commissioned by the Health Resources and Services Administration found that non-personnel costs at urban public health clinics accounted for approximately one-third (33.2%) of total healthcare delivery costs in 2021 (33). Based on this percentage, we estimate that our calculations may underestimate the total cost of student nurse encounters by approximately 50%. Lastly, the data were derived from one institution in a particular geographic area, limiting generalizability of the findings.
Conclusion
The COMPASS Center has provided wellness services to low-income, un/under-insured, and unemployed individuals. We found that the types and nature of services mainly included pre-employment physical exams, vaccinations, and health maintenance and education, with medium costs ranging from $5.45 to $14.91. Lack of trust being an independent factor in delays seeking health care (34, 35), our ongoing presence in the community might help build trust with the institution. To this end, our neighborhood-embedded center leveraging students in health professional programs may serve as a model to supplement the traditional health and social care systems for individuals and communities who—due to issues of trust and/or income, language, location, residency status—are “medically disenfranchised” (36). Since the COVID-19 pandemic, our team worked hard to recover and regain our service capacity by hiring new staff, while reconnecting with our partners. As we continue strengthening our endeavors, we envision our student and staff training will be more structured and expanded to allow further engagement with social service sectors, while continuing to promote coordinated primary care referrals and wellness services.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the anonymous data used for this analysis will be made available upon reasonable request. Requests to access these datasets should be directed to aGhhbjNAamh1LmVkdQ==.
Ethics statement
The studies involving humans were approved by Johns Hopkins Medicine Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because IT was deemed unnecessary given that the analysis pooled anonymous encounter records collected across community programs and sites.
Author contributions
H-RH: Conceptualization, Data curation, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. Y-JL: Formal analysis, Writing – original draft, Writing – review & editing. JL: Visualization, Writing – original draft, Writing – review & editing. C-AS: Data curation, Writing – original draft, Writing – review & editing. OD-G: Writing – original draft, Writing – review & editing. PW: Writing – original draft, Writing – review & editing. CL: Writing – original draft, Writing – review & editing. ES: Formal analysis, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Glover, L, and Woods, M. Health system overview. Australia: (2020). Available at: https://www.commonwealthfund.org/sites/default/files/2020-12/2020_IntlOverview_AUS.pdf (Accessed November 23, 2024).
2. Ndugga, N, Hill, L, Pillai, D, and Artiga, S. Race, inequality, and health. (2024). Health Policy 101. Available at: https://www.kff.org/health-policy-101-race-inequality-and-health/ (accessed November 23, 2024)
3. Radley, DC, Shah, A, Collins, SR, Powe, NR, and Zephyrin, LC. Advancing racial equity in U.S. health care: the Commonwealth Fund 2024 state health disparities report Commonwealth Fund (2024). Available at: https://www.commonwealthfund.org/publications/fund-reports/2024/apr/advancing-racial-equity-us-health-care (Accessed November 23, 2024).
4. National Healthcare Quality and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; (2023). AHRQ Pub. No. 23(24)-0091-EF. Available at: https://www.ahrq.gov/research/findings/nhqrdr/nhqdr23/index.html (Accessed November 24, 2024).
5. Volpe, VV, Schorpp, KM, Cacace, SC, Benson, GP, and Banos, NC. State- and provider-level racism and health Care in the U.S. Am J Prev Med. (2021) 61:338–47. doi: 10.1016/j.amepre.2021.03.008
6. Dieleman, JL, Chen, C, Crosby, SW, Liu, A, McCracken, D, Pollock, IA, et al. US health care spending by race and ethnicity, 2002-2016. JAMA. (2021) 326:649–59. doi: 10.1001/jama.2021.9937
7. Lee, EK, Donley, G, Ciesielski, TH, Freedman, DA, and Cole, MB. Spatial availability of federally qualified health centers and disparities in health services utilization in medically underserved areas. Soc Sci Med. (2023) 328:116009. doi: 10.1016/j.socscimed.2023.116009
8. Center for Community Programs, Innovation, and Scholarship. COMPASS Center. Johns Hopkins School of Nursing. Available at: https://nursing.jhu.edu/excellence/community/center-community-innovation-scholarship.html (Accessed November 14, 2023)
9. Stuhlmiller, CM, and Tolchard, B. Developing a student-led health and wellbeing clinic in an underserved community: collaborative learning, health outcomes and cost savings. BMC Nurs. (2015) 14:32. doi: 10.1186/s12912-015-0083-9
10. Fleischman, A, Vanden Heuvel, C, Tesfamichael, DH, Valley, TM, and Jones, K. Addressing social determinants of health in a free clinic setting: a student-run free clinic and community resource navigator program. J Stud Run Clin. (2023) 9. doi: 10.59586/jsrc.v9i1.227
11. Mitchell, D, Maloney, S, Robinson, L, Haines, T, and Foo, J. Costs and economic impact of student-led clinics-a systematic review. Med Educ. [Epub ahead of print] (2024). doi: 10.1111/medu.15550
12. Min, E, Ekeocha, C, Howarth, M, Keller, T, Shah, Z, Shah, S, et al. The costs of operating a student-run free clinic. J Community Health. (2023) 48:926–31. doi: 10.1007/s10900-023-01252-2
13. Hardik, P, Samuel, H, Megan, M, Marcus, C, David, S, and Hansel, T. Operational model and treatment costs of a student-run free clinic serving people who inject drugs. J Student-Run Clinics. (2022) 8:281. doi: 10.59586/jsrc.v8i1.281
14. U.S. Bureau of Labor Statistics. Occupational employment and wages, may 2021: Registered nurses. (2022). Available at: https://www.bls.gov/oes/2021/may/oes291141.htm (Accessed June 21, 2023)
15. Mahajan, S, Caraballo, C, Lu, Y, Valero-Elizondo, J, Massey, D, Annapureddy, AR, et al. Trends in differences in health status and health care access and affordability by race and ethnicity in the United States, 1999-2018. JAMA. (2021) 326:637–48. doi: 10.1001/jama.2021.9907
16. Bailey, ZD, Krieger, N, Agénor, M, Graves, J, Linos, N, and Bassett, MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. (2017) 389:1453–63. doi: 10.1016/S0140-6736(17)30569-X
17. Yoong, SQ, Liao, AWX, Goh, SH, and Zhang, H. Educational effects of community service-learning involving older adults in nursing education: an integrative review. Nurs Educ Today. (2022) 113:105376. doi: 10.1016/j.nedt.2022.105376
18. Howell, CK, Reveles, KR, Knodel, LC, Pattyn, NR, and Frei, CR. Know your medicine: a novel student-led community service learning program. Curr Phar Teach Learn. (2017) 9:353–9. doi: 10.1016/j.cptl.2017.01.006
19. Essa-Hadad, J, Murdoch-Eaton, D, and Rudolf, MCJ. What impact does community service learning have on medical students' appreciation of population health? Public Health. (2015) 129:1444–51. doi: 10.1016/j.puhe.2015.05.009
20. Dorans, J, Lepore, C, Mulroney, EM, and Chlebus, VA. Community wellness bus: a partner-led initiative to improve service integration and address unmet needs of underserved populations in Algoma district, Ontario. Healthc Q. (2023) 26:31–7. doi: 10.12927/hcq.2023.27054
21. Malone, NC, Williams, MM, Smith Fawzi, MC, Bennet, J, Hill, C, Katz, JN, et al. Mobile health clinics in the United States. Int J Equity Health. (2020) 19:40. doi: 10.1186/s12939-020-1135-7
22. Mazander, M, Rumenapp, J, Lee, D, Ong, C, Floramo, E, Benjamins, M, et al. Quantifying the educational value of a student-run free clinic. Fam Med. (2024) 56:176–9. doi: 10.22454/FamMed.2024.568265
23. Centers for Disease Control and Prevention. Who should be tested for TB infection. Available at: https://www.cdc.gov/tb/topic/testing/whobetested.htm (Accessed March 14, 2024)
24. Sama-Miller, E, Kleinman, R, Timmins, L, and Dahlen, H. Employment and health among low-income adults and their children: a review of the literature. Available at: https://www.acf.hhs.gov/opre/report/employment-and-health-among-low-income-adults-and-their-children-review-literature (Accessed March 21, 2024)
25. Antonisse, L, and Garfield, R. The relationship between work and health: Findings from a literature review. Henry J Kaiser Family Foundation; (2018). Available at: https://www.kff.org/medicaid/issue-brief/the-relationship-between-work-and-health-findings-from-a-literature-review/ (Accessed March 21, 2024)
26. U.S. Government Accountability Office. Behavioral health: options for low-income adults to receive treatment in selected states. (2015). Available at: https://www.gao.gov/products/gao-15-449 (Accessed March 21, 2024)
27. Centers for Disease Control and Prevention. Hepatitis B vaccination of adults. (2022). Available at: https://www.cdc.gov/hepatitis/hbv/vaccadults.htm (Accessed March 21, 2024)
28. U.S. Department of Justice. Transitional housing program. Available at: https://www.justice.gov/ovw/transitional-housing-program (Accessed March 21, 2024)
29. Yakubovich, AR, Bartsch, A, Metheny, N, Gesink, D, and O'Campo, P. Housing interventions for women experiencing intimate partner violence: a systematic review. Lancet Public Health. (2022) 7:e23–35. doi: 10.1016/s2468-2667(21)00234-6
30. Goodman-Williams, R, Simmons, C, Chiaramonte, D, Ayeni, OO, Guerrero, M, Sprecher, M, et al. Domestic violence survivors' housing stability, safety, and well-being over time: examining the role of domestic violence housing first, social support, and material hardship. Am J Orthopsychiatry. (2023) 93:402–14. doi: 10.1037/ort0000686
31. Shrank, WH, DeParle, N, Gottlieb, S, Jain, SH, Orszag, P, Powers, B, et al. Health costs and financing: challenges and strategies for a new administration. Health Aff. (2021) 40:235–42. doi: 10.1377/hlthaff.2020.01560
32. Paradis-Gagné, E, Kaszap, M, Ben Ahmed, HE, Pariseau-Legault, P, Jacques, MC, and Potcoava, S. Perceptions of mobile and acute healthcare services among people experiencing homelessness. Public Health Nurs. (2023) 40:36–43. doi: 10.1111/phn.13150
33. Capital Link. Rural federally qualified health centers financial and operational performance analysis 2018–2021. (2023). Available at: https://caplink.org/rural-trends-2023 (Accessed November 25, 2024)
34. Birkhäuer, J, Gaab, J, Kossowsky, J, Hasler, S, Krummenacher, P, Werner, C, et al. Trust in the health care professional and health outcome: a meta-analysis. PLoS One. (2017) 12:e0170988. doi: 10.1371/journal.pone.0170988
35. Taylor, LA, Nong, P, and Platt, J. Fifty years of trust research in health care: a synthetic review. Milbank Q. (2023) 101:126–78. doi: 10.1111/1468-0009.12598
Keywords: community center, wellness services, vulnerable population, nurses, cost
Citation: Han H-R, Lee Y-J, Lee JJ, Sun C-A, Dapaah-Gyimah O, Wilson P, Ling C and Slade E (2025) Types and cost of wellness services provided by a neighborhood-based academic nursing center. Front. Public Health. 12:1477436. doi: 10.3389/fpubh.2024.1477436
Edited by:
Minh-Hoang Nguyen, Phenikaa University, VietnamReviewed by:
Ni Putu Wulan Purnama Sari, Widya Mandala Catholic University Surabaya, IndonesiaNeti Juniarti, Padjadjaran University, Indonesia
Loren Wagner, Marquette University, United States
Copyright © 2025 Han, Lee, Lee, Sun, Dapaah-Gyimah, Wilson, Ling and Slade. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hae-Ra Han, aGhhbjNAamh1LmVkdQ==
 Hae-Ra Han
Hae-Ra Han Yoon-Jae Lee3,4
Yoon-Jae Lee3,4 Chun-An Sun
Chun-An Sun Catherine Ling
Catherine Ling