- 1Division of Epidemiology and Biostatistics, St. John’s Research Institute, Bangalore, India
- 2Department of Statistical Sciences, Kannur University, Kannur, Kerala, India
- 3Division of Nutrition, St. John’s Research Institute, Bangalore, India
- 4Department of Physiology, St. John’s Medical College, Bangalore, India
- 5Department of Biostatistics, St. John’s Medical College, Bangalore, India
Background: National survey data show that age- and sex-standardized weight and length measurements decline early in Indian children. In population-level longitudinal data, early detection of growth trajectories is important for the implementation of interventions. We aimed to identify and characterize distinct growth trajectories of Indian children from birth to 12 months of age residing in urban and rural areas.
Methods: Pooled data from four interventional and non-interventional longitudinal studies across India were used for the analysis. Latent class mixed modeling (LCMM) was employed to identify groups of children with similar trajectories over age. The trajectories named Classes of Children were created for length-for-age Z scores (LAZ) and weight-for-age Z scores (WAZ) based on place of birth, residential area, and maternal education.
Results: We identified two latent classes for LAZ in boys and three latent classes for LAZ in girls, and four classes for WAZ were identified in both boys and girls. The first class for LAZ, with the highest proportion of children (>80% of children), did not decline or increase with age; In boys, Class 1 was close to the WHO median, whereas in girls, Class 1 was lower than the WHO median from birth. The LAZ classes of remaining boys and girls declined with age (slope,
Conclusion: There is heterogeneity in the growth of Indian children in the first year of life, which was identified by distinct types of growth trajectories. The predominant trajectories of both LAZ and WAZ did not decline with age, while most other trajectories demonstrated an initial decline.
Introduction
Low- and middle-income countries (LMICs) continue to report a high prevalence of suboptimal growth (1); for example, 38% of under-five children are stunted in India (2). The first 2 years of a child’s life are crucial to determining their future health and metabolic outcomes. Linear growth faltering and undernutrition in the first 2 years have been linked to poor cognitive, sensory-motor, and social–emotional development, which may reduce economic productivity in adulthood (3–5). Even mild cases of growth faltering have been associated with suboptimal development or delay in developmental milestones (6). Furthermore, there is emerging evidence that growth faltering in early life could also increase cardiovascular risk factors such as glucose intolerance, dyslipidemia, and hypertension in adulthood (7, 8).
Growth in early life can be influenced by multiple factors, including institutional birth, exclusive breastfeeding for the first 6 months, appropriate infant and young child feeding (IYCF) practices, exposure to adequate hygiene and sanitation, maternal education, and morbidities (1, 9, 10). In clinical settings, the growth of children is observed longitudinally, allowing for the assessment of their development over time. However, in public health research, growth has been studied using single or limited anthropometric measurements that can obscure the heterogeneity within population and the ability of children to grow differently, indicating the need for assessing distinct growth trajectories (11). A comparison of weight and height trajectories between well-nourished Pakistani and British children showed differences in these trajectories (12). Indeed, existing evidence suggests that growth trajectories can predict future health-related risks better than a single-point anthropometry-based assessment (13–15).
Cross-sectional growth surveys of Indian children have revealed a significant 0.3 SD decline in World Health Organization (WHO) standard-based length-for-age Z scores (LAZ) from birth to 12 months of age (16), accompanied by a notable decrease in weight-for-age Z-scores (WAZ) from −1.2 SD at birth with a decline of 0.14 SD at 12 months of life. On average, these patterns result in a greater reduction in growth standards at 24 months (mean LAZ at 12 months was −1.07 SD and − 1.32 SD at 24 months, mean WAZ at 12 months was −1.3 SD and − 1.4 SD at 24 months) (16). However, methods examining the association between growth and diet and environmental factors assume that all children are drawn from a single underlying population defined by a set of parameters. Therefore, the present analysis was aimed at comparing the growth velocity of Indian children with the WHO growth velocity standards and characterizing the growth trajectories of Indian children from birth to 12 months of age residing in urban slums and rural areas through multiple longitudinal studies conducted between 1995 and 2006. Additionally, this study focused on identifying potential heterogeneous yet hidden growth patterns. The association between model-based growth trajectory membership and stunting and underweight status at 2 years of age was examined in a subgroup of children. This study aims to inform public health researchers about the use of advanced statistical modeling to identify underlying trajectories such that customized interventions can be considered.
Methods
Data sources
The data for the study were accessed through the Healthy Birth, Growth, and Development Knowledge Integration-India (HBGDki) (17), a platform funded by the Bill & Melinda Gates Foundation. This platform enables the researchers to easily access datasets related to Indian children and cohorts. The platform contains 29 survey datasets conducted between 1995 and 2018, focusing on childbirth, growth, and development, including both cross-sectional and longitudinal studies. To model the longitudinal growth of children, we selected four studies from these datasets based on the availability of longitudinal data on anthropometric measures of children, along with related information such as place of residence, mother’s education, and type of delivery.
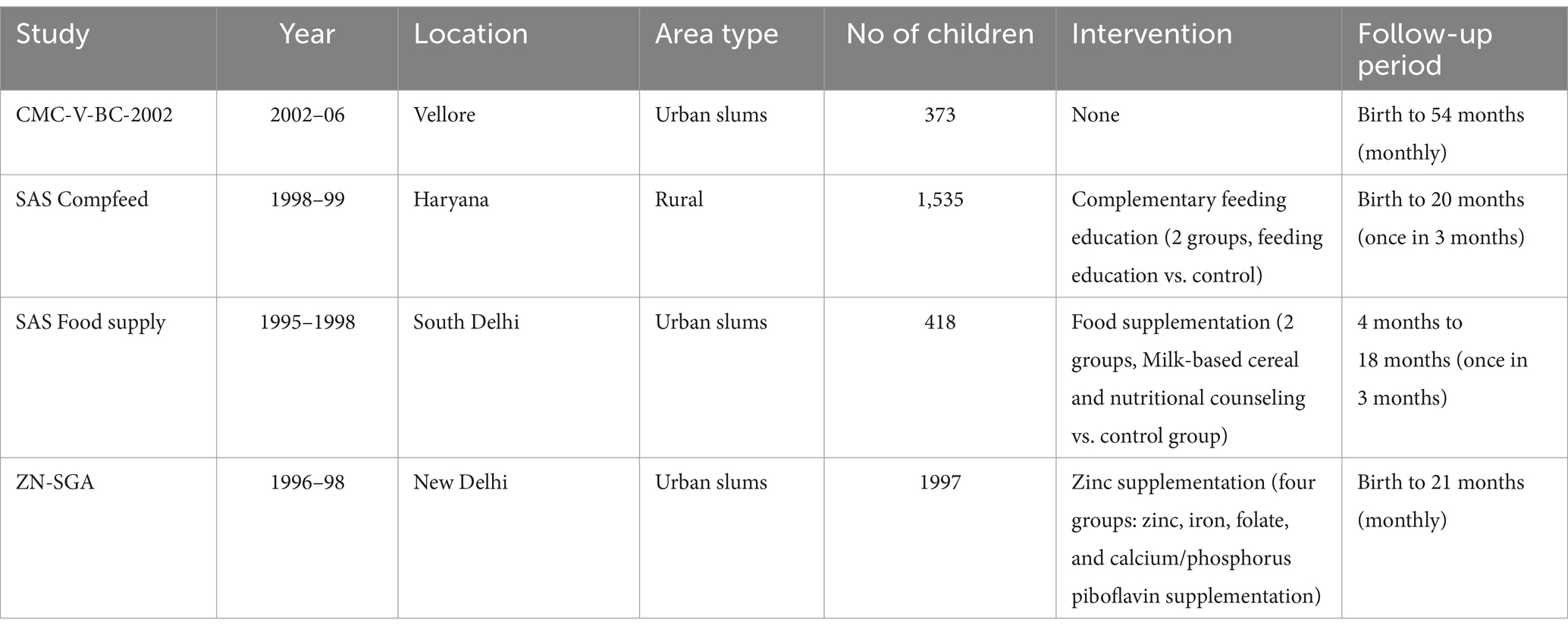
Longitudinal data at more than two time points from birth to 12 months of age were obtained from the following studies. The data from CMC-V-BC-2002 (Christian Medical College Vellore birth cohort study) (18, 19), SAS Compfeed (SAS Complementary Feeding Practices) (20), SAS Food Supply (SAS-Food supplementation) (21), and ZN-SGA (zinc supplementation in infants born small for gestational age) (22) were combined to form a single dataset; details of individual studies are provided in Table 1. The figure indicating the sample size selection is also in Supplementary Figure 1.
The final analytical sample consisted of 2,540 participants for LAZ analysis and 2,690 participants for WAZ analysis, after removing outliers in accordance with WHO standards (23). Outliers were defined as children with LAZ or WAZ beyond 6SD at any point in time, as unreliable data at any time point could influence growth trajectories. We opted to examine the growth progression of infants during their first 12 months only, as information was sparse after 12 months of age (17).
Measurements
Anthropometric measurements
Anthropometric measurements of participants from birth to 12 months were considered for growth trajectory analyses. The LAZ and WAZ for each child in the sample were obtained using the WHO growth standards (23). The weight of children was measured using the SECA scale in all studies (accuracy: 0.1 kg), and length was measured using a standardized infantometer (accuracy: 0.1 cm).
Early life characteristics
We identified early life characteristics, including institutional birth, maternal education level, residential area, and sex of the child. Residence locations were classified as urban slums and rural areas. Low birth weight was classified as birthweight<2,500 grams. Institutional births were defined as the births that occurred in health facilities. We classified maternal education level based on years of formal education the mother received, where education of more than 12 years was considered ‘college-level,’ less than 12 years was considered ‘school-level,’ and zero years of education was considered ‘not educated.’
Statistical models
Comparison of growth velocity with WHO standards
The longitudinal growth data were compared with WHO growth trajectory standards to understand how the current data were positioned in the trajectory centiles. 1-month weight increments and 2-month length increments were obtained using smoothed monthly anthropometry data. These were compared with the WHO growth velocity standards (23). We calculated the monthly Z-score of weight and length velocities, separately for boys and girls, using the WHO LMS (lambda-mu-sigma) parameters. These parameters are part of the Box-Cox power exponential transformation used in growth standard data construction and we plotted them alongside the WHO standard for visual examination.
Growth trajectory analysis
We used latent class mixed models (LCMM) to identify distinct latent trajectories of LAZ or WAZ in longitudinal data from birth to 12 months for boys and girls separately (24). The LCMM assumes that the population of children is heterogeneous in terms of z-scores, and G latent classes are used to represent these groups. Latent growth trajectories that represent a pattern of change in z-scores were identified as follows.
The procedure to define the growth trajectory of infants is as follows. Consider 𝑁 children followed up on multiple and different occasions up to the age of 12 months. Let, be the anthropometry Z scores for follow-ups of the child. Let be the covariates (early life characteristics) with fixed effects, and be the independent variables (age in months as linear or non-linear terms) whose effect is assumed to vary for each child and each latent group.
Let be the probability that the child is included in a latent group . Considering the Gth class as the reference class, the probability of ith child belonging to the gth class is described using a multinomial logistic model according to .
Based on the maximum class membership probability, each child was classified into either of the G latent growth classes. In an LCMM framework, is given by:
,
,
,
Here, is the intercept for the gth trajectory class and is the slope. is the early life characteristics considered for the analysis (place of birth, residential area, and maternal education), and we selected d as 2, assuming that age is linearly and quadratically assumed to vary for each child and each trajectory. We obtained the estimates of model parameters within a maximum likelihood framework using the modified Marquardt algorithm (25). Bayesian Information Criteria (BIC) and Log-likelihood were the criteria used to determine the number of trajectories (26). We also considered a minimum trajectory membership of 5% in the smallest group as another criterion for determining distinct trajectories (27). Visualization of growth trajectories was useful in determining the number of classes, assessing the quality of classification, and understanding the growth pattern of children in different classes (28). All available data were considered in the mixed effects model with individuals as the random effect, and missing data were not imputed.
Association of trajectories with anthropometric outcomes
The following analysis was performed to examine how the outcome of latent class trajectories of LAZ and WAZ until 12 months of age affect the poor nutritional status of the children at 2 years. Logistic regression models were used to predict the nutritional status at 2 years with the latent class membership of the children based on the LCMM model. According to the LCMM model, the child’s LAZ trajectory class was considered the predictor in the logistic regression model for stunting, and the WAZ trajectory class to which the child belonged was considered as the predictor in the logistic regression model for underweight status. The child’s birth weight and maternal education were considered covariates in the analysis. A receiver operating characteristic (ROC) analysis of prediction probability from the logistic regression model was used to determine the optimal threshold to classify children as either stunted, underweight, or normal. Sensitivity, specificity, and accuracy (overall % of correct classification) of nutritional status classification were used to assess the model’s predictive performance. K-fold cross-validation was used to validate the logistic model. All analyses were carried out using the packages LCMM v1.9.2 and R v4.0.2 software.
Results
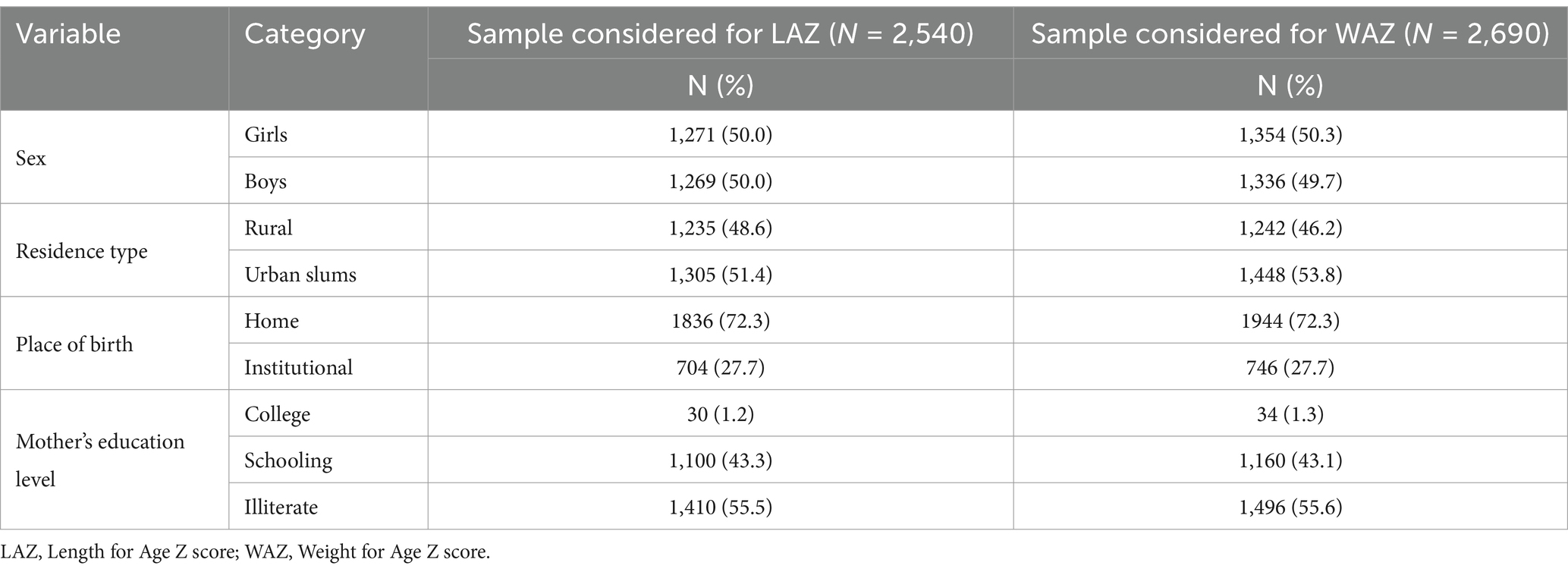
The characteristics of the children included in this study are summarized in Table 2. In the data considered for LAZ modeling, 50% of the children were girls, 51% were from urban slums, 72% were delivered at home, and 55% of the mothers were ‘not educated.’ The distribution of LAZ and WAZ in the four cohorts is given in Supplementary Figure 2. The average LAZ of the children at birth were − 0.98 1.25 for boys and − 0.93 1.18 for girls, while the average WAZ of the children at birth were − 1.29 1.09 for boys and − 1.42 1.12 for girls.
Comparison of growth velocity with WHO standards
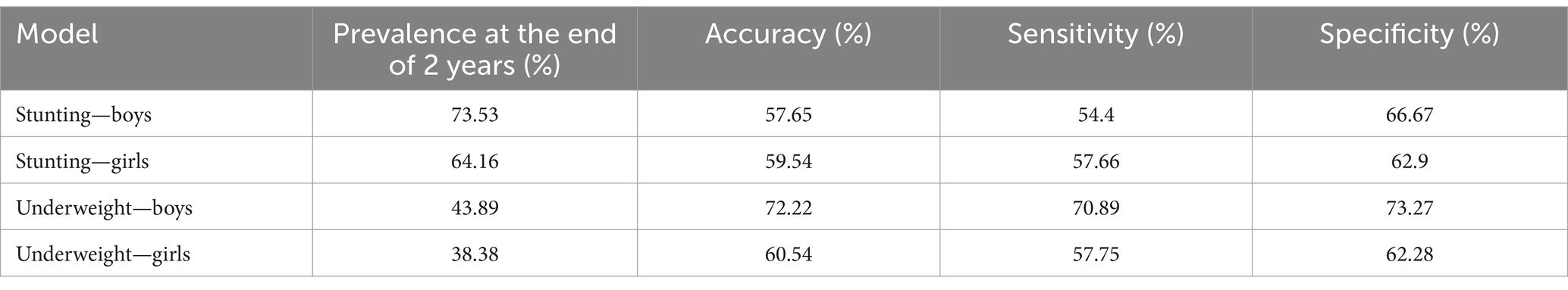
The 2-month length velocity calculated based on WHO standard LMS parameters was found to be low ( -2SD) until 3 months of age with subsequent improvement (Supplementary Table 1) for both boys and girls. However, this improvement fails to reach the median or even the 25th percentile of standard velocity recommended for infants in this age group as per WHO standards (Figures 1A,B). The monthly average weight velocity improved from 1 month to 12 months of age based on WHO growth velocity standards, with the z-score mostly remaining -1.0SD up to 4 months of age and eventually improving to −0.35 SD at 12 months of age (Supplementary Table 2) for boys and − 0.3 SD for girls. The smoothed 50th percentile values for one-month weight gain remained below the median WHO growth velocity standards at all ages for both boys and girls. This gain in weight can be observed in Figures 1C,D.
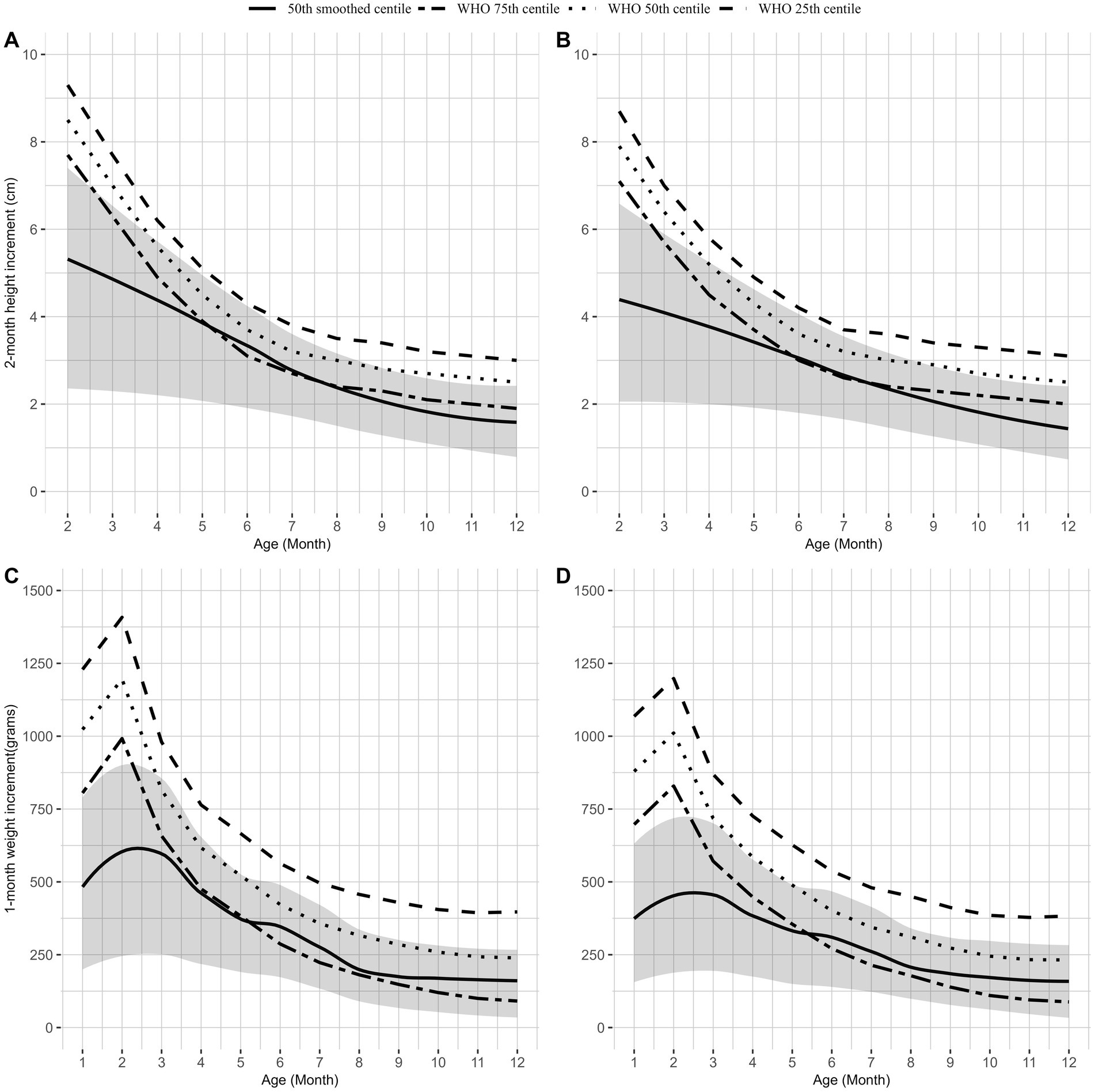
Figure 1. Comparison of WHO length velocity percentiles and percentiles of length velocity for boys (A) and girls (B). Comparison of WHO weight velocity percentiles and percentiles of weight velocity for boys (C) and girls (D). The dotted line represents the 50th percentile WHO growth velocities of weight and length, and the dot-dashed line represents the 25th percentile and 75th percentile of WHO weight and length velocities. The solid line represents the 50th percentile weight and length velocity from our data with a shaded confidence interval (25th percentile and 75th percentile).
Growth trajectory analysis
The trajectory model fit statistics for LAZ and WAZ are given in Supplementary Table 3. Latent models with three trajectories fulfilled the criteria of minimum BIC value and the minimum 5% trajectory membership criteria for both LAZ and WAZ in boys and girls.
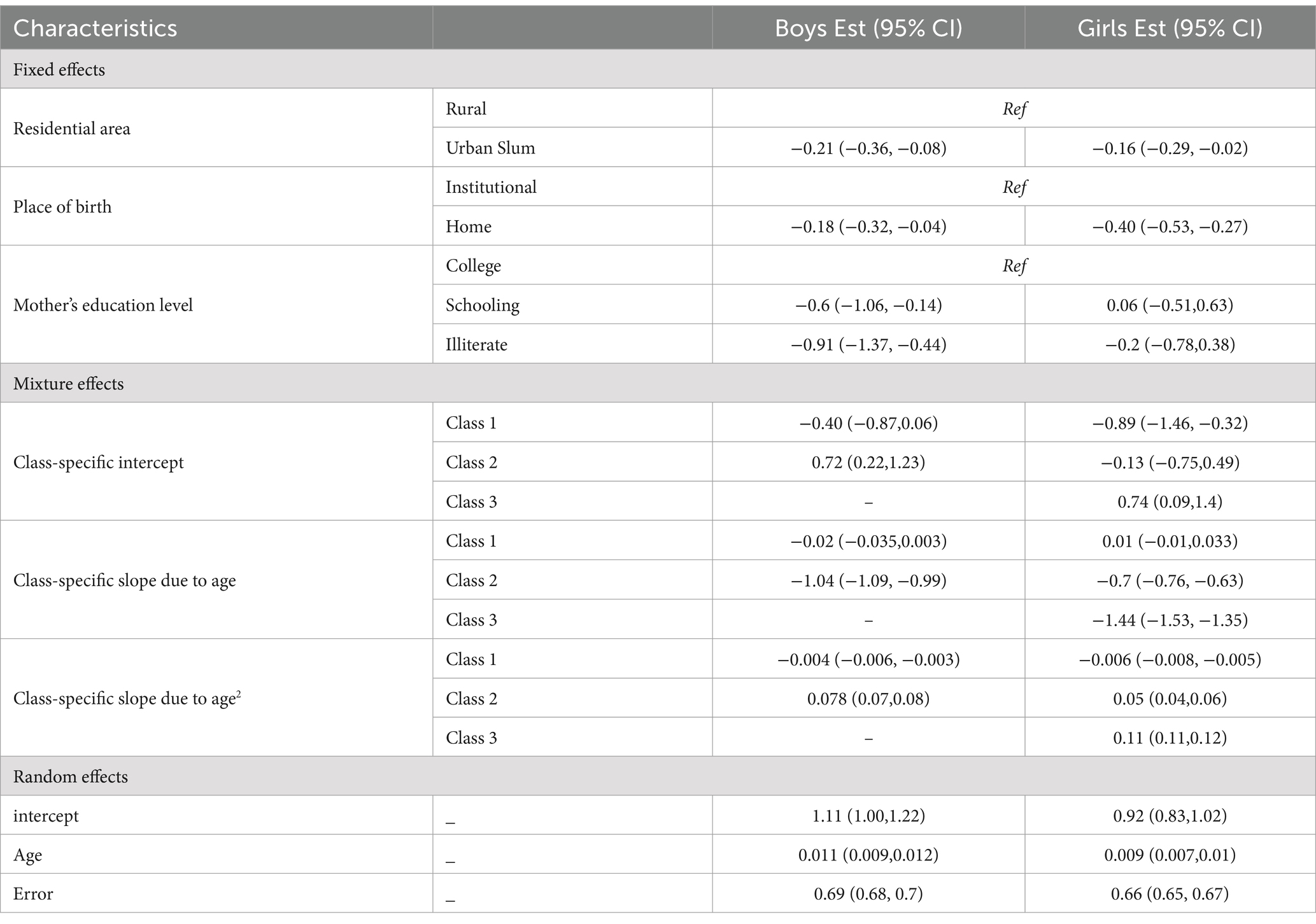
For boys LAZ, 83.7% belonged to Class 1 (Supplementary Table 3), characterized by LAZ at birth that was close to the WHO median −0.4 SD, p > 0.05) with no decline over time ( = − 0.02; 95% CI: −0.035, 0.003) as they aged (Table 3; Figure 2A). The remaining 16.3% belonged to Class 2, who had higher LAZ at birth ( =0.72), but this score declined with age = − 1.04; 95% CI: −1.09, −0.99).
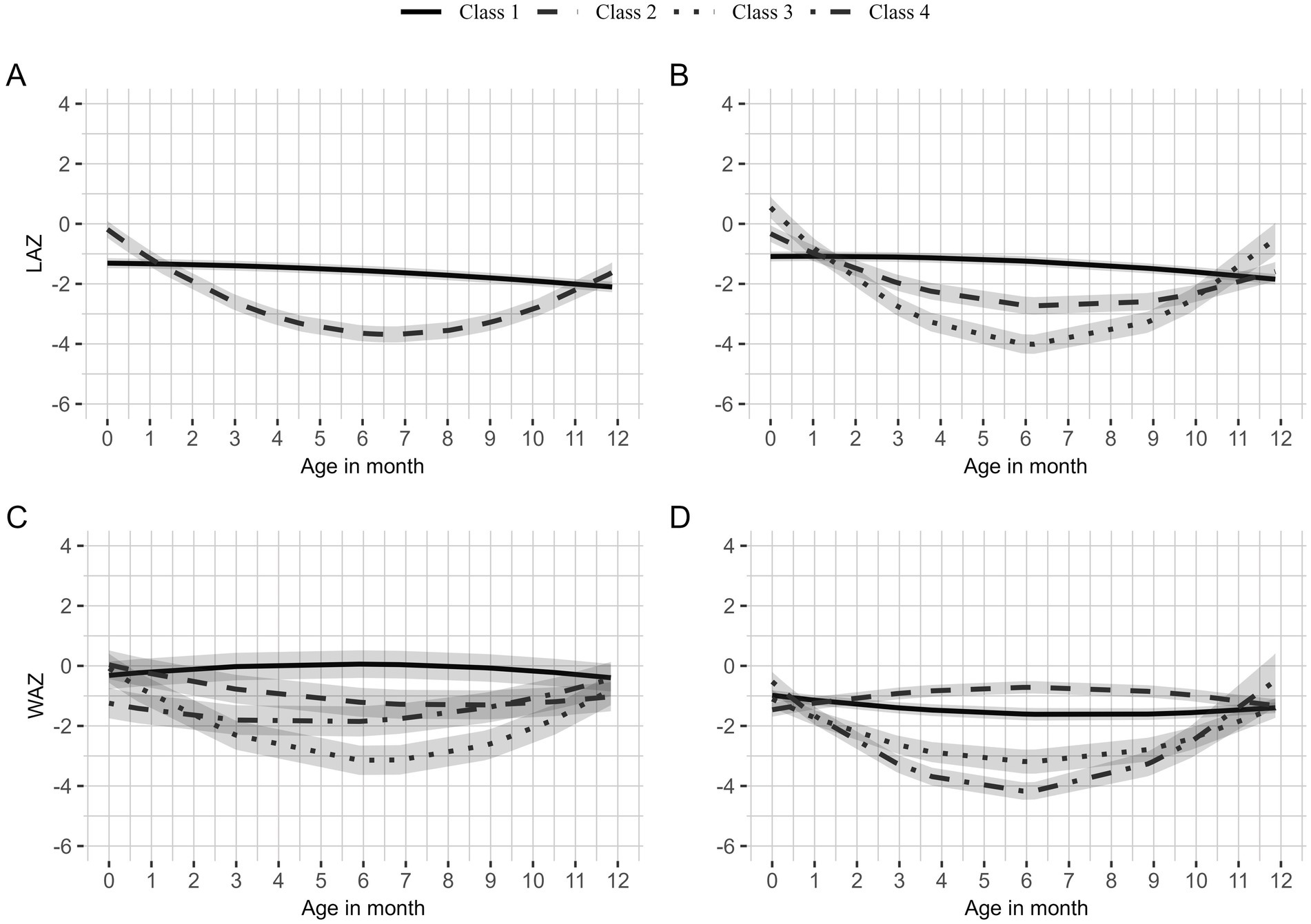
Figure 2. Latent class growth trajectories of length-for-age z-scores (LAZ) for boys (A) and girls (B) and weight-for-age z-scores (WAZ) for boys (C) and girls (D). Solid lines represent the first class with the highest proportion; dashed lines represent the second class with the second-highest proportion; dotted lines represent the third class with the third-highest proportion; and dot-dashed lines represent the last class with the lowest proportion of children.
The LAZ for girls was categorized into three classes. Class 1 comprised 80.2% and Class 2 comprised 13.3% of the girls (Supplementary Table 3). Class 1 (Table 3; Figure 2B) had a low LAZ at birth ( −0.9 SD) and no decline with age ( =0.01; 95% CI: −0.01, 0.033), while Class 2 had LAZ close to WHO median ( −0.13 SD, p > 0.05) at birth and this declined with age ( = − 0.7; 95% CI: −0.76, −0.63) until 6 months, after which there was a slight improvement ( =0.05; 95% CI: 0.04, 0.06). Finally, Class 3 (which constituted 6.5% of the girls) had a high LAZ ( 0.74 SD) at birth and experienced a significant decline with age until 6 months ( = − 1.44; 95% CI: −1.53, −1.35) and catch-up growth by 12 months ( = 0.11; 0.11, 0.12) as observed from the quadratic model.
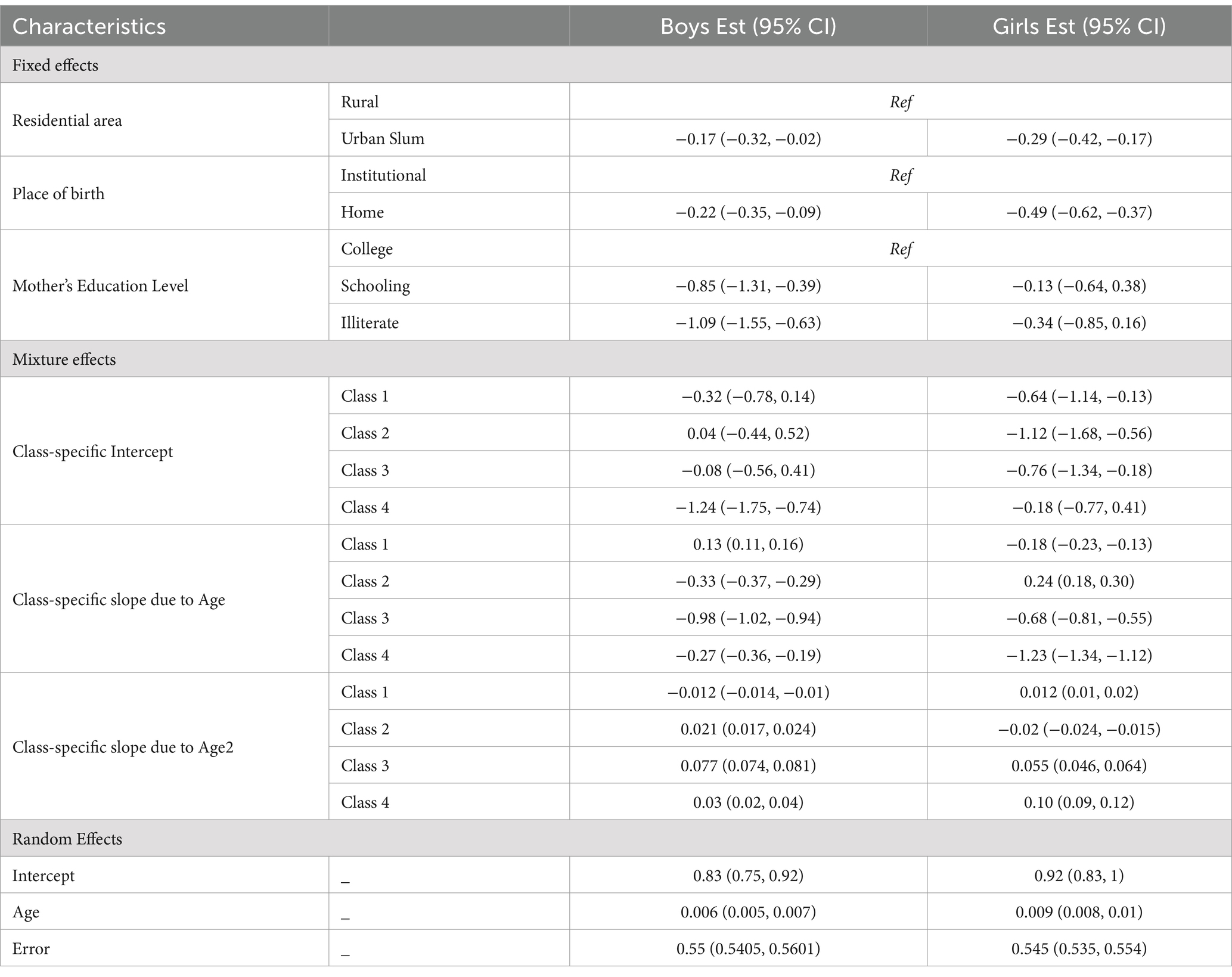
Four WAZ trajectory classes were identified for boys and girls from birth to 12 months of age (Supplementary Table 3). For boys, the WAZ at birth for Class 1 (46.1%) was close to the WHO median ( −0.32 SD, p > 0.05) and slightly increased (Table 4; Figure 2C) with age ( =0.13; 95% CI: 0.11, 0.16). Class 2 also had WAZ close to the WHO median at birth, but this declined significantly with age ( = − 0.33; 95% CI: −0.37, −0.29). Class 3 was similar to class 2 but significantly declined with age ( = − 0.98; 95% CI: −1.02, −0.94). Class 4 comprised only 5.8% of infants with low WAZ at birth = − 1.24; 95% CI: −1.75, −0.74), and it declined with age = − 0.27; 95% CI: −0.36, −0.19). All classes showed slight improvement in WAZ after 6 months except Class 1.
The Class 1 trajectory (52.8%) for girls was similar to the Class 1 WAZ trajectory for boys (Table 4; Figure 2D). Although Class 2 had a low WAZ at birth, an increment was observed with age ( =0.24, 95% CI: 0.18, 030). Class 3 (13.5%) had a low WAZ at birth ( −0.76 SD), which declined with age = − 0.68; 95% CI: −0.81, −0.55). Class 4 (6.9%) of girls had WAZ close to the WHO median at birth, which significantly declined with age = − 1.23; 95% CI: −1.34, −1.12). All classes demonstrated a slight improvement in WAZ after 6 months except Class 1 and Class 2.
We compared the latent class assignment of the children between the intervention groups of the three included studies separately. It was observed that latent class assignment was not associated with the intervention the children received in the different studies, except for LAZ in girls of the Zinc study (see Supplementary Table 4).
Predictors of growth trajectories
According to the LCMM analysis, residential location (urban slum vs. rural) and place of birth were significant predictors for identifying both boys’ and girls’ LAZ and WAZ trajectories (Tables 3, 4). Additionally, maternal education was a significant predictor of LAZ and WAZ trajectories only in boys. The covariates contributing to LAZ and WAZ class-specific membership of the infants are given in Supplementary Tables 5, 6. The distribution of covariates by latent classes of LAZ and WAZ are given in Supplementary Tables 7, 8. In general, the classes in which an initial decline in LAZ and WAZ was observed (Class 2 and above) consisted mostly of urban slum children (>90%). Additionally, these classes mostly included children who had ‘not educated’ mothers (>60% for LAZ and nearly 50% for WAZ).
Association between trajectories and anthropometric outcomes
Length data at 2 years were available for 170 boys and 173 girls, and weight data was available for 180 boys and 185 girls (24th or 25th month). The prevalence of stunting was 73.5% and that of underweight was 43.9% in boys. In girls, the prevalence of stunting and underweight was 64.2 and 38.4%, respectively. The latent classes of LAZ and WAZ were not associated with stunting and underweight at 2 years (Supplementary Table 9). The sensitivity of stunting and underweight classification based on the growth trajectory followed was low (Table 5), at <60%, except for the prediction of underweight in boys. The specificity was >60% for both stunting and underweight in boys and girls.
Discussion
The present analysis showed a lower growth velocity for both length and weight than the normative WHO growth velocity among Indian infants. There were two and three distinct LAZ trajectories for boys and girls, respectively, while there were four WAZ trajectories for both boys and girls. The LAZ of children in the predominant trajectory did not decline with age, while the WAZ of children in the predominant trajectory increased with age. Residential area and institutional delivery were the predictors of LAZ and WAZ trajectories for both boys and girls. Maternal characteristics, such as height and BMI, significantly influenced child growth outcomes and trajectories of LAZ in children from LMICs (29). In this analysis, maternal education was also identified as a critical factor in shaping both LAZ and WAZ trajectories in boys.
The classification of growth using the WHO growth standards indicates growth deprivation at the population level but may overlook children with the potential for improvement. The growth velocity observed in this study was comparable to that reported in secondary analyses of cohorts across LMICs (30). Therefore, we attempted to identify if different trajectories could differentiate children with the potential to grow better in a group of children who were born and brought up in suboptimal conditions for growth. Our analysis suggests that infants who showed a declining trend in LAZ and WAZ scores for the initial months of their life had improvement in these z-scores after 6 months. There were two distinct LAZ trajectories for both boys and girls, while for WAZ, four distinct growth trajectories were observed for both boys and girls, with an initial decline and a later increase in WAZ beyond 6 months. Other studies have observed an increase in WAZ. WAZ growth trajectories that were assessed using latent growth curve models in British and Pakistani children also observed a similar increase after 6 months (31). A similar trend was observed in a study on European children, where children with low birth weight had been shown to catch up after birth (32). This was also similar to growth trajectories observed for BMI z-scores in an Australian birth cohort (15). On the contrary, among Bangladeshi children, there was a declining trend in approximately 95% of the children for LAZ (33). Thus, in general, longitudinal studies have observed an acceleration in growth among children who have started with lower anthropometric measures. This finding contrasts with cross-sectional national surveys, which indicate a decline in growth standards with increasing age and are often used to inform policies for supplementary feeding (1, 16).
We employed latent class mixed models for the latent trajectory identification, which estimates the latent classification based on the cohort being examined and may not be extrapolated to any other population. A similar approach was used to identify growth trajectories in Guatemalan and Australian children (11, 15). Similar to the current study, multiple growth trajectories were identified in the earlier studies. In Guatemalan children, three linear growth trajectories were identified, but all of them had an initial declining slope indicating growth faltering, while in the current study, the predominant trajectory was one without faltering, and this could be because the average LAZ of the Indian children was higher (approximately 1SD at birth) compared to the Guatemalan children (approximately -2SD).
Inadequate child growth has been reported in both urban slums and rural areas of India. An analysis of the National Family Health Survey 4th round (NFHS-4) (2) data showed that a third of the stunted and underweight children belonged to slum areas (34). In NFHS-5, the prevalence of stunting (37% vs. 30%) and wasting (34% vs. 27%) was higher in rural areas compared to urban slums (16). Urban slums and rural areas in India are often associated with poor hygiene and sanitation, which lead to an increased risk of infections and other morbidities. Improper water, sanitation, and hygiene practices have been linked to repeated diarrheal episodes, infections, and environmental enteropathy disease (EED) (35). EED manifests as a subclinical inflammation of the intestines with villous atrophy, potentially leading to poor absorption of nutrients. These episodes of morbidity in children may either reduce the absorption of nutrients or increase their daily nutrient needs.
As discussed earlier, multiple factors influence growth in children. Therefore, exploring these factors can help predict the growth trajectories of infants. In the present analysis, residential location (such as urban and rural settings) and place of birth were found to be significant predictors of LAZ and WAZ trajectories for both boys and girls. The residential area is an important factor for growth as it is linked to hygiene, sanitation, and access to clean drinking water, which could impact episodes of infection and the duration of infection. A study conducted on children (under 24 months) from rural Cambodia (36) showed associations between growth faltering and water, sanitation, and hygiene practices, indicating potential predictors for growth trajectory. Furthermore, in the case of boys, maternal education was found to be a significant predictor for LAZ and WAZ trajectories. Similarly, in other studies, formal education of mothers has been shown to be inversely related to growth faltering (13, 33). Educated mothers are more likely to make informed choices (37) on infant feeding practices that are essential for growth and development. Maternal education was a significant predictor in Indian children, while maternal height was also a significant predictor in Guatemalan children. The Australian children had four trajectories of linear growth.
Although the infants included in these analyses belonged to urban slums and rural areas—environments that may not be conducive to optimal growth—distinct growth trajectories could be identified, which is a notable strength of this study. The predominant trajectories did show a decline in LAZ but showed an increase in WAZ. This contradicts cumulative declining growth curves drawn based on cross-sectional national survey data sets. The data clearly highlight the need for exploring growth patterns with trajectory models to identify subgroups of children with a decline in growth and to implement targeted interventions. The accuracy of the latent trajectories to predict stunting and underweight at 2 years in the same children was found to be poor. Earlier analyses have not explored the ability of latent growth trajectories to predict later nutritional outcomes in children.
Limitations
Our analysis was limited to the data available from the four selected studies. Therefore, we could not analyze other factors that could impact growth in infants, such as pre-pregnancy weight or BMI, duration of exclusive breastfeeding, complementary feeding practices, duration of infection, parity, maternal age, gestational diabetes, and gestational hypertension. A considerable portion of the original data from the studies were excluded based on the stringent WHO guidelines for cleaning survey data (23) during the data cleaning process (Supplementary Figure 1) because these studies were conducted in populations with a high prevalence of undernutrition.
Another limitation was that the analysis of trajectories with anthropometric outcomes was restricted to a subset of the data, which came from a single study in which data at 2 years were available. Future research with larger and more diverse samples and additional covariates is needed to further investigate the predictive power of early life growth trajectories on later nutritional and health outcomes.
The data used in this study are approximately 20 years old, which limits the interpretation of the results and the implications of our findings for contemporary India. Changes in healthcare, nutrition, and socioeconomic factors over time could impact the relevance of our results. However, this study clearly demonstrates that there is heterogeneity in growth patterns of children in India, and future analysis using more recent data is needed to confirm the applicability of our findings to present-day India.
Conclusion
In conclusion, our study identified multiple distinct types or classes of longitudinal growth trajectories in Indian children in their first year of life, utilizing a latent class mixed model approach. This finding highlights the heterogeneity of growth patterns, with the predominant class being those who did not experience a decline in LAZ and WAZ. This result contrasts with traditional curve-fit analyses of cross-sectional summary data, where an overall decline in LAZ and WAZ over time is noted in the entire sample of children, disregarding the heterogeneity in growth patterns. These findings demonstrate the growth patterns at a population level, and there is a need for further exploration of growth trajectories using longitudinal cohort data. Future research should focus on validating these trajectories and exploring their predictive value in health outcomes in later life. This research underscores the need for context-sensitive public health interventions with efficient precision public health strategies to improve child nutrition and health outcomes in diverse Indian populations.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: data for the study was accessed through the Healthy Birth, Growth, and Development Knowledge integration (HBGD Ki) platform on 23rd August 2020. Requests to access these datasets should be directed to https://www.kiglobalhealth.org/publications/introduction-to-hbgdki/.
Ethics statement
The studies involving humans were approved by the Institutional Ethics Committee, St. John’s Medical College & Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
AS: Conceptualization, Data curation, Formal analysis, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. JB: Conceptualization, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing, Investigation. PA: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Formal analysis, Investigation, Software. SS: Investigation, Writing – original draft, Writing – review & editing. SB: Investigation, Writing – original draft, Writing – review & editing. JJ: Writing – original draft, Writing – review & editing. AK: Writing – review & editing, Conceptualization. TT: Conceptualization, Writing – review & editing, Investigation, Methodology, Supervision, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The project described was funded by grant number BT/kiData0374/06/18 from the Grand Challenges India at BIRAC, an operating division of jointly supported DBT-BMGF-BIRAC.
Acknowledgments
The authors thank the members of the Ki community for their efforts in collating data from various sites, as well as data contributors for their valuable input. Data for the study was accessed through the Healthy Birth, Growth, and Development Knowledge integration (HBGD Ki) platform on 23rd August 2020. Visit the website https://www.kiglobalhealth.org/publications/understanding-ki-data-contributions-india/ for more details.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1474222/full#supplementary-material
Abbreviations
LCMM, Latent Class Mixed Modeling; LAZ, Length-for-Age; WAZ, Weight-for-Age; LMICs, Low- and Middle-Income Countries; IYCF, Infant and Young Child Feeding; BIC, Bayesian Information Criteria; EED, Environmental Enteropathy Disease; BMI, Body Mass Index; NFHS, National Family Health Survey.
References
1. Roth, DE, Krishna, A, Leung, M, Shi, J, Bassani, DG, and Barros, AJD. Early childhood linear growth faltering in low-income and middle-income countries as a whole-population condition: analysis of 179 demographic and health surveys from 64 countries (1993–2015). Lancet Glob Health. (2017) 5:e1249–57. doi: 10.1016/S2214-109X(17)30418-7
2. Sciences II for P. National family health survey (NFHS-4), 2015–2016: India. Mumbai: IIPS. (2017)1–671.
3. Collaborators LB of DCGF. Mapping child growth failure across low- and middle-income countries. Nature. (2020) 577:231–4. doi: 10.1038/s41586-019-1878-8
4. Grantham-McGregor, S, Cheung, YB, Cueto, S, Glewwe, P, Richter, L, and Strupp, B. Developmental potential in the first 5 years for children in developing countries. Lancet. (2007) 369:60–70. doi: 10.1016/S0140-6736(07)60032-4
5. Black, RE, Victora, CG, Walker, SP, Bhutta, ZA, Christian, P, De Onis, M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
6. Sudfeld, CR, McCoy, DC, Fink, G, Muhihi, A, Bellinger, DC, Masanja, H, et al. Malnutrition and its determinants are associated with suboptimal cognitive, communication, and motor development in Tanzanian children. J Nutr. (2015) 145:2705–14. doi: 10.3945/jn.115.215996
7. Martins, VJB, Toledo Florêncio, TMM, Grillo, LP, Do, CP, Franco, M, Martins, PA, et al. Long-lasting effects of undernutrition. Int J Environ Res Public Health. (2011) 8:1817–46. doi: 10.3390/ijerph8061817
8. DeBoer, MD, Lima, AAM, Oría, RB, Scharf, RJ, Moore, SR, Luna, MA, et al. Early childhood growth failure and the developmental origins of adult disease: do enteric infections and malnutrition increase risk for metabolic syndrome? Nutr Rev. (2012) 70:642–53. doi: 10.1111/j.1753-4887.2012.00543.x
9. Cumming, O, and Cairncross, S. Can water, sanitation and hygiene help eliminate stunting? Current evidence and policy implications: water, sanitation and hygiene, and stunting. Matern Child Nutr. (2016) 12:91–105. doi: 10.1111/mcn.12258
10. Bhutta, ZA, Das, JK, Rizvi, A, Gaffey, MF, Walker, N, Horton, S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. (2013) 382:452–77. doi: 10.1016/S0140-6736(13)60996-4
11. Ramírez-Luzuriaga, MJ, Hoddinott, J, Martorell, R, Patel, SA, Ramírez-Zea, M, Waford, R, et al. Linear growth trajectories in early childhood and adult cognitive and socioemotional functioning in a Guatemalan cohort. J Nutr. (2021) 151:206–13. doi: 10.1093/jn/nxaa337
12. Fairley, L, Petherick, ES, Howe, LD, Tilling, K, Cameron, N, Lawlor, DA, et al. Describing differences in weight and length growth trajectories between white and Pakistani infants in the UK: analysis of the born in Bradford birth cohort study using multilevel linear spline models. Arch Dis Child. (2013) 98:274–9. doi: 10.1136/archdischild-2012-302778
13. Li, C, Goran, MI, Kaur, H, Nollen, N, and Ahluwalia, JS. Developmental trajectories of overweight during childhood: role of early life factors*. Obesity. (2007) 15:760–71. doi: 10.1038/oby.2007.585
14. Rodriguez-Martinez, A, Zhou, B, Sophiea, MK, Bentham, J, Paciorek, CJ, Iurilli, MLC, et al. Height and body-mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: a pooled analysis of 2181 population-based studies with 65 million participants. Lancet. (2020) 396:1511–24. doi: 10.1016/S0140-6736(20)31859-6
15. Giles, LC, Whitrow, MJ, Davies, MJ, Davies, CE, Rumbold, AR, and Moore, VM. Growth trajectories in early childhood, their relationship with antenatal and postnatal factors, and development of obesity by age 9 years: results from an Australian birth cohort study. Int J Obes. (2015) 39:1049–56. doi: 10.1038/ijo.2015.42
16. Sciences II for P. National Family Health Survey (NFHS-5), 2019–2021: India. Mumbai: IIPS (2022).
17. Healthy Birth, Growth, and Development knowledge Integration-India (HBGDki). (2020). Available at: https://www.kiglobalhealth.org/publications/introduction-to-hbgdki/ (Accessed August 23, 2020).
18. Sarkar, R, Kang, G, and Naumova, EN. Rotavirus seasonality and age effects in a birth cohort study of southern India. PLoS One. (2013) 8:e71616–11. doi: 10.1371/journal.pone.0071616
19. Gladstone, BP, Ramani, S, Mukhopadhya, I, Muliyil, J, Sarkar, R, Rehman, AM, et al. Protective effect of natural rotavirus infection in an Indian birth cohort. N Engl J Med. (2011) 365:337–46. doi: 10.1056/NEJMoa1006261
20. Group IFSBhandari, N, Mazumder, S, Bahl, R, Martines, J, Black, RE, et al. An educational intervention to promote appropriate complementary feeding practices and physical growth in infants and young children in rural Haryana, India. J Nutr. (2004) 134:2342–8. doi: 10.1093/jn/134.9.2342
21. Bhandari, N, Bahl, R, Nayyar, B, Khokhar, P, Rohde, JE, and Bhan, MK. Food supplementation with encouragement to feed it to infants from 4 to 12 months of age has a small impact on weight gain. J Nutr. (2001) 131:1946–51. doi: 10.1093/jn/131.7.1946
22. Sazawal, S, Black, RE, Menon, VP, Dinghra, P, Caulfield, LE, Dhingra, U, et al. Zinc supplementation in infants born small for gestational age reduces mortality: a prospective, randomized, Controlled Trial. Pediatrics. (2001) 108:1280–6. doi: 10.1542/peds.108.6.1280
23. World Health Organization. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization (2006).
24. Proust-Lima, C, Philipps, V, and Liquet, B. Estimation of extended mixed models using latent classes and latent processes: the R package lcmm. J Stat Softw. (2017) 78:1–56. doi: 10.18637/jss.v078.i02
25. Marquardt, DW. An algorithm for least-squares estimation of nonlinear parameters. J Soc Ind Appl Math. (1963) 11:431–41. doi: 10.1137/0111030
26. Wen, X, Kleinman, K, Gillman, MW, Rifas-Shiman, SL, and Taveras, EM. Childhood body mass index trajectories: modeling, characterizing, pairwise correlations and socio-demographic predictors of trajectory characteristics. BMC Med Res Methodol. (2012) 12:38. doi: 10.1186/1471-2288-12-38
27. Lennon, H, Kelly, S, Sperrin, M, Buchan, I, Cross, AJ, Leitzmann, M, et al. Framework to construct and interpret latent class trajectory modeling. BMJ Open. (2018) 8:e020683. doi: 10.1136/bmjopen-2017-020683
28. International Institute for Population Sciences (IIPS) and ICF. A life course perspective on health trajectories and transitions. Cham: Springer International Publishing (2015).
29. Mertens, A, Benjamin-Chung, J, Colford, JM, Coyle, J, van der Laan, MJ, Hubbard, AE, et al. Causes and consequences of child growth faltering in low-resource settings. Nature. (2023) 621:568–76. doi: 10.1038/s41586-023-06501-x
30. Benjamin-Chung, J, Mertens, A, Colford, JM, Hubbard, AE, van der Laan, MJ, Coyle, J, et al. Early-childhood linear growth faltering in low- and middle-income countries. Nature. (2023) 621:550–7. doi: 10.1038/s41586-023-06418-5
31. Mebrahtu, TF, Feltbower, RG, Petherick, ES, and Parslow, RC. Growth patterns of white British and Pakistani children in the born in Bradford cohort: a latent growth modelling approach. J Epidemiol Community Health (1978). (2015) 69:368–73. doi: 10.1136/jech-2014-204571
32. Eriksson, JG, Forsen, TJ, Osmond, C, and Barker, DJP. Pathways of infant and childhood growth that Lead to type 2 diabetes. Diabetes Care. (2003) 26:3006–10. doi: 10.2337/diacare.26.11.3006
33. Zhang, Y, Zhou, J, Niu, F, Donowitz, JR, Haque, R, Petri, WA, et al. Characterizing early child growth patterns of height-for-age in an urban slum cohort of Bangladesh with functional principal component analysis. BMC Pediatr. (2017) 17:84–11. doi: 10.1186/s12887-017-0831-y
34. Kundu, D, Maiti, KD, Mishra, R, and Kar, B. Children and adolescents in urban India. (2022). Available at: https://www.unicef.org/india/reports/children-and-adolescents-urban-india (Accessed March 4, 2022).
35. Budge, S, Parker, AH, Hutchings, PT, and Garbutt, C. Environmental enteric dysfunction and child stunting. Nutr Rev. (2019) 77:240–53. doi: 10.1093/nutrit/nuy068
36. Lai, A, Velez, I, Ambikapathi, R, Seng, K, Cumming, O, and Brown, J. Risk factors for early childhood growth faltering in rural Cambodia: a cross-sectional study. BMJ Open. (2022) 12:e058092. doi: 10.1136/bmjopen-2021-058092
Keywords: growth trajectory, length-for-age Z score, weight-for-age Z score, longitudinal data, infants
Citation: Saji A, Baby J, Antony P, Sinha S, Bandyopadhyay S, Jose JK, Kurpad AV and Thomas T (2025) Growth dynamics of Indian infants using latent trajectory models in pooled survey datasets. Front. Public Health. 12:1474222. doi: 10.3389/fpubh.2024.1474222
Edited by:
Renaud Becquet, Global Health in the Global South (GHiGS), Bordeaux Population Health Research Centre (Inserm, IRD, Bordeaux University), FranceReviewed by:
Prema Ramachandran, Nutrition Foundation of India, IndiaHarvinder Kaur, Post Graduate Institute of Medical Education and Research (PGIMER), India
Philip T. James, Emergency Nutrition Network, United Kingdom
Copyright © 2025 Saji, Baby, Antony, Sinha, Bandyopadhyay, Jose, Kurpad and Thomas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tinku Thomas, dGlua3Uuc2FyYWhAc2pyaS5yZXMuaW4=
 Aswathi Saji1
Aswathi Saji1 Srishti Sinha
Srishti Sinha Sulagna Bandyopadhyay
Sulagna Bandyopadhyay Joby K. Jose
Joby K. Jose Anura V. Kurpad
Anura V. Kurpad Tinku Thomas
Tinku Thomas