- 1Institute for Health Behavioural Research, Ministry of Health, Setia Alam, Malaysia
- 2Faculty of Social Sciences and Humanities, Open University Malaysia, Kuala Lumpur, Malaysia
Introduction: COVID-19 has triggered significant disruptions globally, necessitating swift adaptations in individuals’ health behaviors.
Methods: This cross-sectional study was conducted during Phase Four of Malaysia’s National Recovery Plan and examines how the pandemic has affected health behaviors among adult Malaysians. The study gathered data online using convenience sampling with 1,004 respondents aged 18 and above. The research focused on diverse health domains, including eating habits, physical activity, smoking, alcohol consumption, and sleep patterns. The Wilcoxon Signed Rank test and descriptive statistics were employed to compare health behaviors before and after COVID-19.
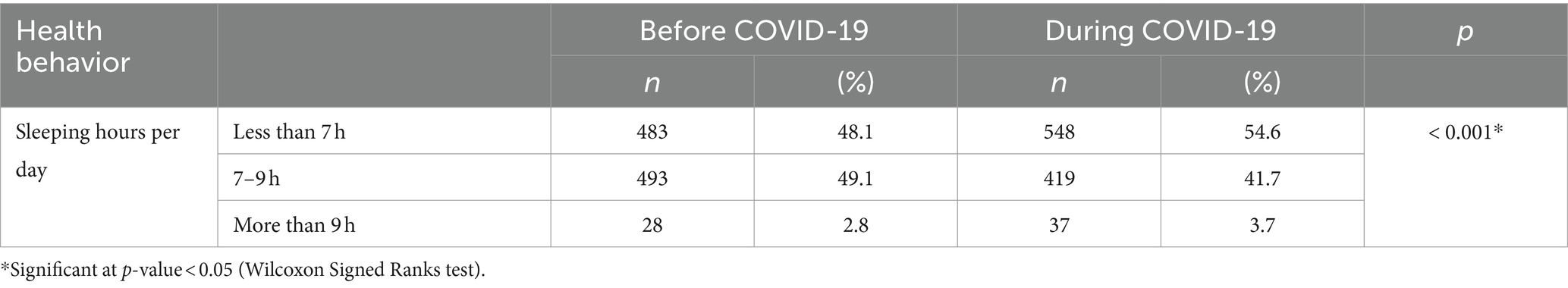
Results: Findings indicate noteworthy shifts in eating behaviors, with increased water and fruit consumption (p < .001). The frequency of home-cooked meals stayed relatively stable despite declining dinner preference and increasing daily snacks. Physical activity declined, marked by increased sedentary behavior and screen time (p < .001). There were differences in the patterns of smoking and alcohol consumption; some had started these behaviors during the pandemic. Notably, intentions to quit smoking among respondents were more prominent than attempts to stop drinking. Respondents’ sleep patterns also changed, with more sleeping fewer than seven hours daily (p < .001).
Conclusion: The study emphasizes the need for focused interventions to address new challenges by highlighting the impact on health behaviors. As Malaysia navigates the post-pandemic landscape, understanding and mitigating the persisting effects on health behaviors are crucial for promoting overall well-being.
Introduction
In late 2019, the highly contagious COVID-19 virus emerged, quickly spreading to 114 countries, territories, and places worldwide, causing an unparalleled global health emergency. By March 2020, the World Health Organization (WHO) declared the outbreak a pandemic. Numerous nations implemented lockdowns and mobility restrictions to curb the spread of the virus. As of September 2024, there have been almost 6 million deaths worldwide. In Malaysia, reports indicated approximately 5.3 million COVID-19 infections, with an estimated 36,652 deaths attributed to the virus (1).
Although the virus has continued to spread, many aspects of life have gradually improved since the onset of the pandemic. One notable advancement is the significant decrease in the risk of severe disease and death due to the introduction of vaccinations and boosters. Immunization has allowed more Malaysians to return to their regular lives over the past year. However, the COVID-19 pandemic has resulted in substantial adverse health, economic, and psychological effects that continue to affect the community, even as many of the pandemic’s restrictions have been loosened and transmission rates have declined.
At the beginning of the pandemic, Malaysia, like many other countries, implemented the Movement Control Order (MCO) to restrict social contact and physical movement to lower the spread of the virus among the broader public. However, COVID-19-related preventative measures and restrictions (such as confinement) were shown to negatively impact the health and well-being of the adult population (2). Additionally, it is particularly concerning when individuals engage in unhealthy behaviors, given the potential influence on COVID-19-related risks and consequences (3).
Previous research suggested that during the COVID-19 lockdown, lower psychological well-being and mental health were linked to the adoption of unhealthy lifestyle habits, such as using tobacco products (2), eating an unhealthy diet (4, 5), getting less sleep (4), and not exercising (6). These habits can contribute to mental health issues, including post-traumatic stress disorder (PTSD) and other stress-related conditions (2). Additionally, they can lead to metabolic disorders, such as overweight and obesity, which are associated with a range of health complications.
Despite the ongoing presence of COVID-19, individuals must adapt to coexisting with the virus. Many people remain at heightened risk of engaging in unhealthy behaviors. Therefore, this study compares health behaviors among adult Malaysians before and during the COVID-19 pandemic in the following domains: eating habits, physical activity, smoking, alcohol consumption, and sleep patterns. The study’s results will show how adult Malaysians’ health behaviors changed before and during the COVID-19 pandemic.
Method
Study design
This cross-sectional study was conducted from January to March 2022, during Phase Four of the National Recovery Plan (PPN), focusing on Malaysian citizens’ health and health-related behaviors. The minimum sample size required for this study was 385 respondents, calculated using a power analysis based on a 95% confidence level (5). This calculation assumed that the sample proportion would be within 0.05 of the population proportion, which was estimated to be 0.50, reflecting a population size of 29.1 million Malaysians (Department of Statistics, Malaysia, DOSM 2020). To ensure robust results and account for potential non-responses or incomplete surveys, we added a 30% contingency to the initial sample size. As a result, we targeted a minimum of 500 respondents for the study.
A convenience sampling technique was employed to recruit potential study respondents through various online platforms, including Facebook, Twitter, Instagram, WhatsApp, and some internet websites. WhatsApp was the most used platform, with 88% of respondents using it at least once a week. During the COVID-19 pandemic, social media platforms, especially Facebook, are an effective and cost-efficient research strategy for collecting large-scale nationwide surveys (7).
Data collection procedure
An anonymous online questionnaire was created using Google Forms, allowing respondents to fill in without signing in. The form provided information about the study and required informed consent. Respondents could choose to agree or disagree, and they could withdraw midway. The survey was anonymous, preserving privacy by not collecting personal identifying information. Data was stored for 5 years before being destroyed. Data was entered into an offline document after being retrieved from the Google Form and then destroyed. Participants were selected based on the following inclusion criteria: Malaysian citizens aged 18 years and above, capable of reading and writing in Malay, and proficient in using computers and mobile devices. Exclusion criteria included non-Malaysian citizens, individuals under 18 years of age, and those unable to understand the survey instructions.
Study instrument
The questionnaire used in this study comprised questions regarding health behaviors both before and during the pandemic, organized into five categories: (a) sociodemographic information, (b) eating behavior, (c) physical activity, (d) alcohol and tobacco use, and (e) sleep quality. Respondents were asked to indicate whether their behaviors had improved, worsened, or remained the same since the onset of the pandemic. These responses were based on the concept of “Self-Perceived Changes” to ascertain variations in health behavior before and during COVID-19 (2, 4–6). The questionnaire was developed in Malay, the national language.
To ensure the questionnaire’s validity and reliability, it underwent a review process by several experts, who provided recommendations for specific changes. Additionally, a hard copy of the questionnaire was pretested with 10 respondents to assess the clarity of the wording and the average time required for completion. The finalized version was then converted into an online format using Google Forms. Subsequently, a pilot study involving 30 respondents was conducted to evaluate the online survey’s formatting and the instrument’s reliability. The reliability scores from the pilot study indicated good consistency, with scores of 0.716 for items related to family relationships and 0.914 for those concerning psychological health. Overall, this rigorous process of development, expert review, pretesting, and pilot study ensured that the questionnaire was both appropriate and effective for the objectives of this research.
Ethical approval and consent form
The Medical Review & Ethics Committee (MREC) granted ethical approval for this study (NMRR-21-1866-61534). All respondents were informed of the study’s purpose, potential risks, and benefits before the start of the survey. Additionally, they were free to leave the study at any time. The informed consent form will be signed by those who consent to participate.
Data analysis
All completed Google Form questionnaires were downloaded into a Microsoft Excel sheet for data editing, sorting, and coding. The SPSS Statistical Package Programme Version 20.0 for Windows (SPSS Inc., Chicago, IL, USA) was then used to analyze the data. Next, the Wilcoxon Signed Rank test and descriptive statistics were employed to compare health behaviors before and after COVID-19.
Results
Demographic profile of the respondents
The online survey received 1,004 responses from Malaysia’s 16 states and federal territories. The majority of them were females (69.0%), Malays (74.4%), between the ages of 36 and 45 (38.9%), had a tertiary education (79.2%) and worked in government (83.3%). Table 1 shows that 35.5% of the respondents earned between RM 4001 and 8,000 monthly.
Changes in health behavior
This section aimed to investigate the changes in health behaviors, including eating habits, physical activity, smoking, alcohol consumption, and sleep quality among Malaysian adults before and during the COVID-19 pandemic.
Eating behavior
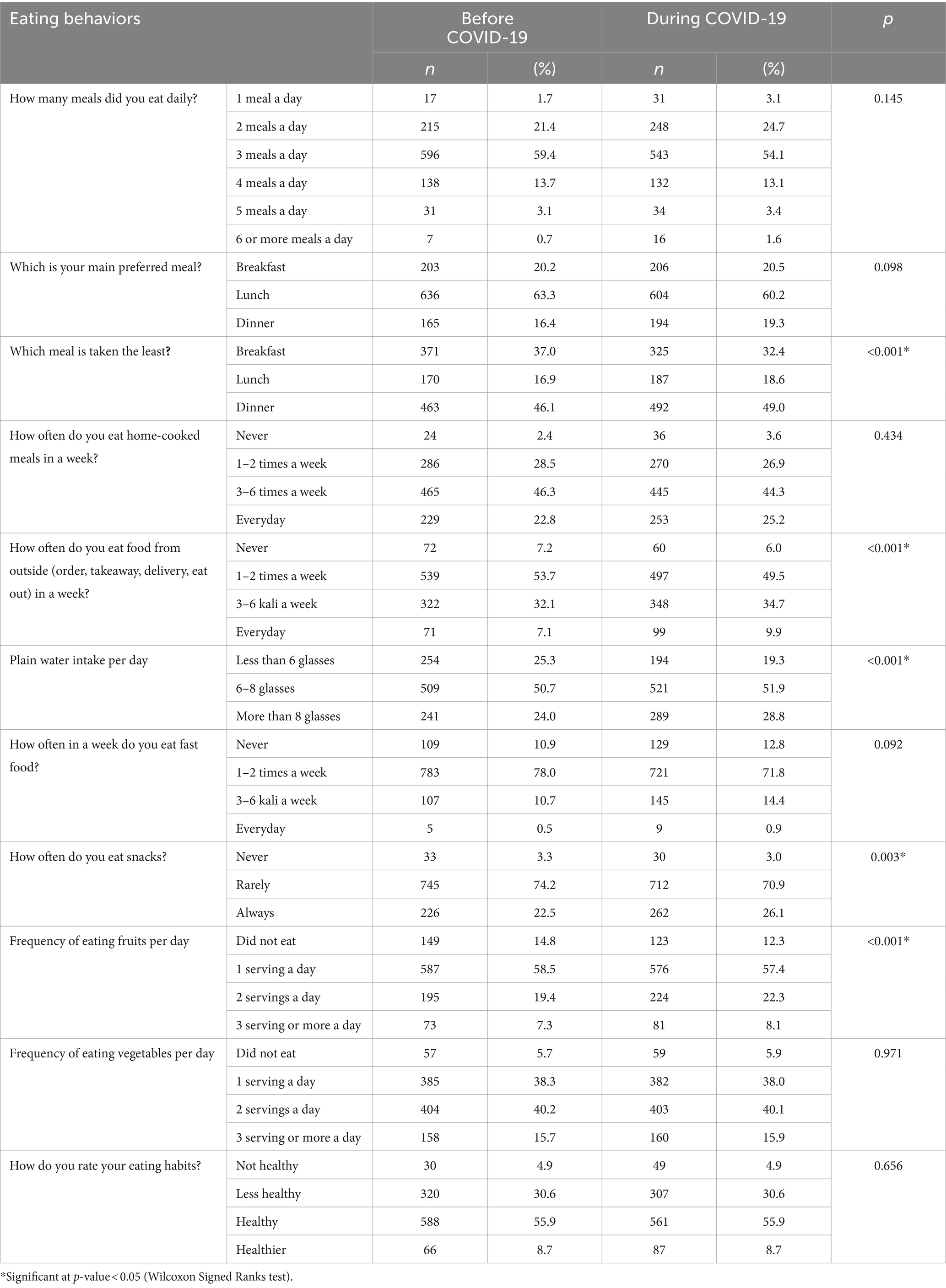
Table 2 presents the significant changes in the respondents’ eating behaviors throughout the pandemic. Although the frequency of eating four to six times a day increased, the reported percentage of people who ate three meals a day decreased slightly from 59.4 to 54.1%; however, this difference was not statistically significant. Dinner remained the least preferred meal, rising marginally from 46.1 to 49.0% (p < 0.001) during the pandemic. On the other hand, lunch continued to be the respondents’ main meal, both before and during COVID-19. More importantly, the percentage of respondents who ate their main meals outside their homes three to six times a week increased from 32.1 to 34.7%. This increase is likely because the data was collected during Phase 4 of the National Recovery Plan when all social and economic sectors had resumed operations.
Furthermore, the respondents were more likely to eat snacks during COVID-19 than before the pandemic (22.5 to 26.1%, p < 0.001). Additionally, there was a statistically significant increase in the daily consumption of fruits (two servings per day) and plain water (drinking more than eight glasses) from 24.0 and 19.34% to 28.8 and 22.3%, respectively. Conversely, no significant differences were found in the number of vegetables and fast food consumed. This may be because, even before the pandemic, a sizable portion of the population did not consume the recommended number of fruits and vegetables. All these findings should be considered when recommending dietary practices.
Comparison of physical activity before and during COVID-19
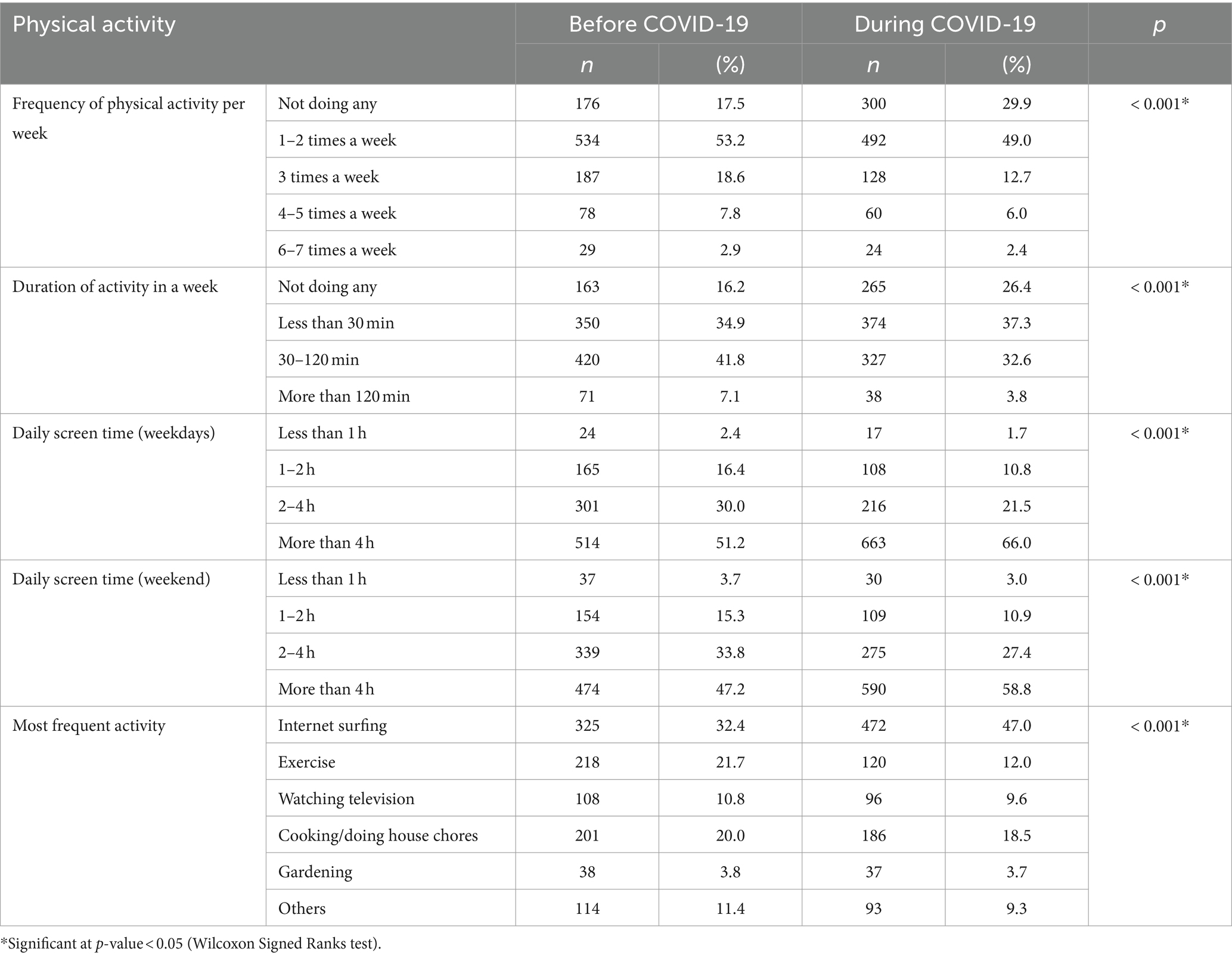
Table 3 compares the respondents’ physical activity levels before and during COVID-19. All five questions had a significant difference (p < 0.001). During the COVID-19 pandemic, there was an increase in respondents who did not engage in any physical activity (17.5 to 29.9%) as well as those who spent more than 4 h of screen time on weekdays and weekends (51.2 to 66.0% and 47.2 to 58.8%, respectively). There was also a slight decrease in those who engaged in 30–120 min of weekly physical activity, from 41.8% before the pandemic to 32.6% during it. Similarly, the proportion of people who did not engage in physical activity increased from 16.2 to 26.4%. Internet use became the most popular activity both before and during the pandemic. Furthermore, the time spent on the Internet increased from 32.4 to 47.0%. Those who engaged in physical activity, on the other hand, fell from 21.7 to 12.0% during the pandemic.
Self-perceived changes in physical activity and screen time due to COVID-19
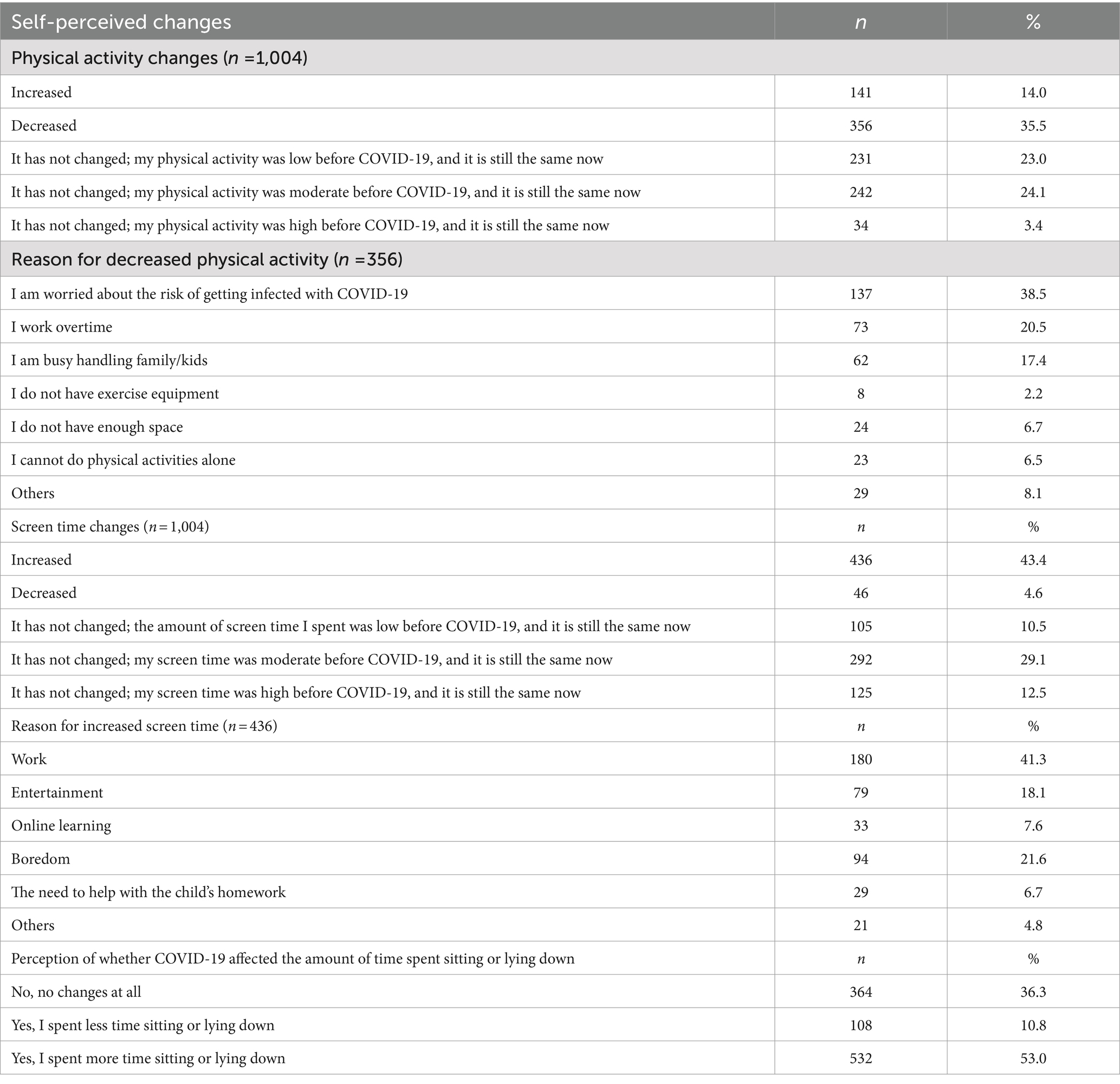
This study revealed that 35.5% of respondents reported decreased physical activity for various reasons, including being concerned about the risk of contracting COVID-19, needing to work overtime, or being preoccupied with family and children. Additionally, 43.4% of respondents said they had increased their screen time, with the most common reasons cited being work, boredom, and entertainment. Because of the COVID-19 pandemic, half of the respondents (53.0%) believed they spent more time sitting and lying down (Table 4).
Smoking and alcohol consumption
Of all the respondents, 77 were smokers during the survey. 3.9% of them stated that COVID-19 was when they first started smoking. Of the smokers who began before the pandemic, half (56.8%) said they had not changed their smoking habits. In comparison, the remaining smokers (21.6%) showed a similar percentage of either an increase or decrease in smoking habits. Furthermore, compared to smokers who merely intended to stop, 32.5% of current smokers (42.9%) had made attempts to quit (Table 5).
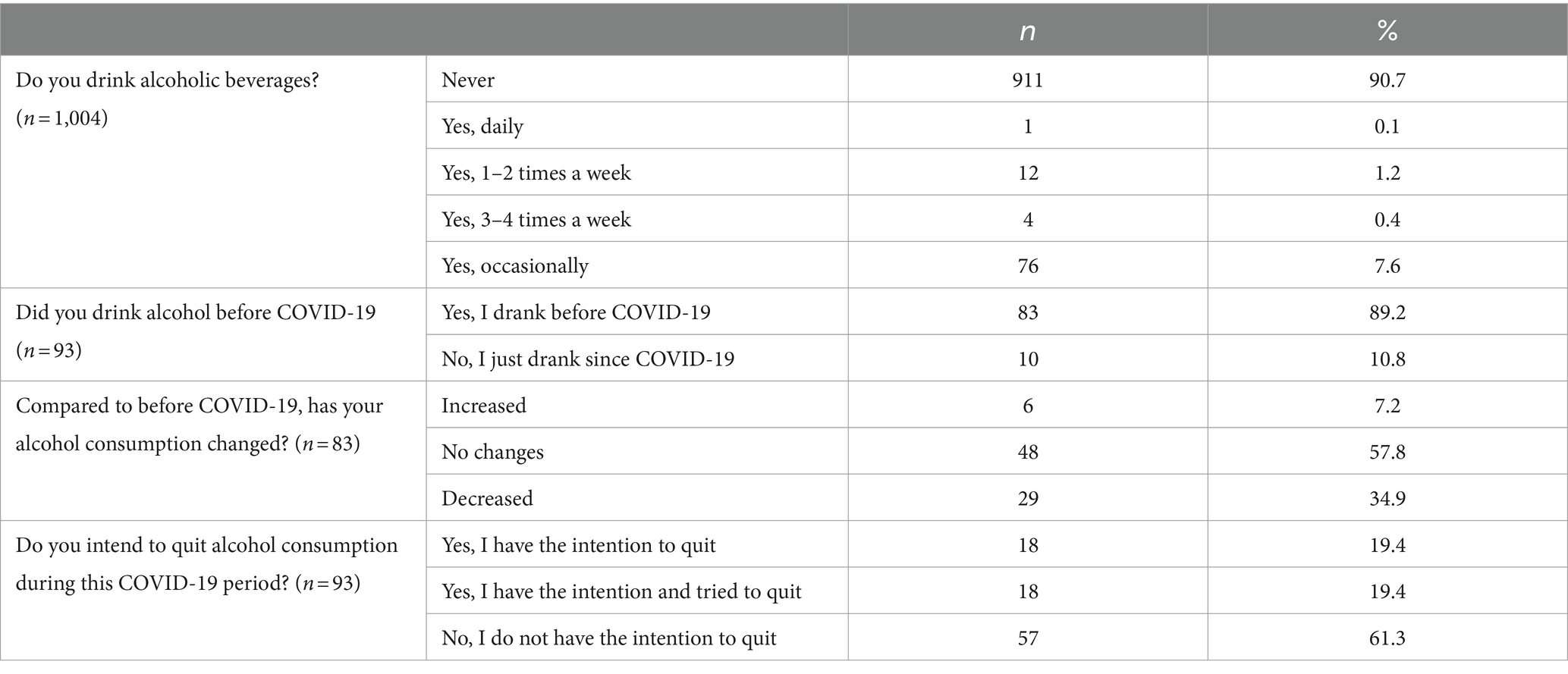
Regarding alcohol intake, 93 respondents reported having a current alcohol intake (Table 6). Of these, 10.8% stated that their first drinking experience occurred during COVID-19. Of this group of drinkers, 34.9% reported drinking less, 7.2% reported drinking more, and 57.8% reported no changes in alcohol consumption. Furthermore, most drinkers (61.3%) stated they had no intention of quitting.
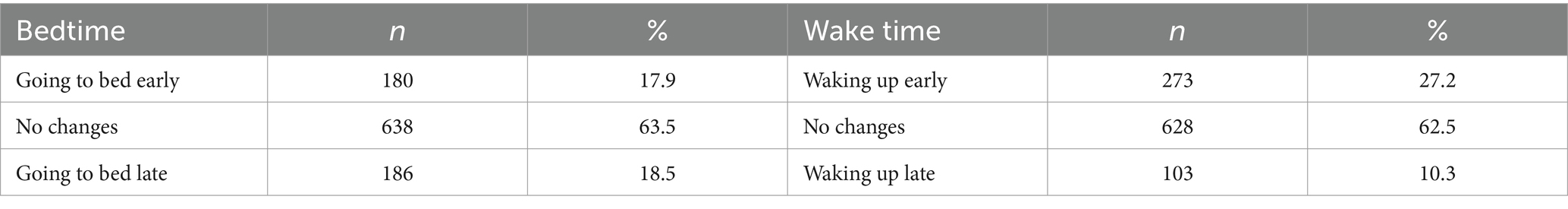
Sleep pattern
There was a significant difference in sleeping hours before and during the COVID-19 pandemic (p < 0.001). Approximately half of the respondents (54.6%) reported sleeping less than 7 hours during the COVID-19 pandemic, compared to 48.1% before the pandemic (Table 7). Most respondents (63.5%) and (32.5%) stated that their bedtime and wake-up times remained the same (Table 8).
Discussion
The COVID-19 pandemic has caused numerous changes in people’s health-related behaviors, which provides a unique lens through which to view the dynamics of lifestyle modifications during this historical period. Overall, the findings of this study are crucial due to the significant disruptions caused by the COVID-19 pandemic, which necessitated rapid changes in health behaviors globally. This study, conducted during Phase Four of Malaysia’s National Recovery Plan, sheds light on the pandemic’s impact on Malaysians’ eating habits, physical activity, smoking, alcohol consumption, and sleep patterns. These insights are vital for developing effective public health interventions and policies to address these behavior changes’ immediate and potentially long-lasting effects.
In regards to eating habits, the results of this study demonstrate that during the pandemic, over half of the respondents drank the recommended six to eight glasses of plain water per day, as advised by the Ministry of Health (MOH) Malaysia (8). Additionally, there was an increase in the frequency of the recommended fruit intake, which is two servings per day, and this result was consistent with a study conducted in Hong Kong (4). Some people ate more fruits during the pandemic to bolster their immune systems (9). On the other hand, the psychological impact of the pandemic, including stress coping mechanisms, may contribute to these changes, as individuals may resort to eating as a means of alleviating stress. The psychological impact of the pandemic may have influenced changes in dietary habits, with some individuals increasing their fruit intake as a potential coping mechanism for stress. While this shift could be viewed positively, it is important to consider that nearly 80% of respondents still consumed fewer than three servings of vegetables daily, indicating a consistent low intake of vegetables both before and during the pandemic. This aligns with national data showing that 94.9% of Malaysians do not meet the recommended vegetable intake (10). Additionally, although there was an increase in snack consumption, this finding alone does not imply negative dietary changes, as it depends on the type and quantity of snacks consumed. Overall, while fruit intake may have increased, the persistent low vegetable consumption remains a concern (10).
The findings of this study also indicate a concerning decrease in physical activity during the pandemic, accompanied by a rise in sedentary behaviors and screen time, aligning with findings from other studies (5, 11). Given the well-established links between physical inactivity and adverse health outcomes, this shift raises significant public health considerations (12). According to a review of 21 studies about the impact of physical activity on mental health during COVID-19, people who regularly engaged in physical activity (high volume and frequency) and adhered to a regular schedule of physical activity reported fewer symptoms of anxiety and depression (13). The study also emphasizes the impact of increased screen time on work, boredom, and entertainment, reflecting the broader trend of heightened digital engagement in the COVID-19 era.
Noteworthy trends emerged in smoking and alcohol consumption, with a percentage of respondents initiating these behaviors during COVID-19. According to this study, 3.9 and 10.8% of respondents, respectively, began smoking and consuming alcohol after COVID-19. Previous research found that during COVID-19, higher rates of alcohol and tobacco use were associated with depressive symptoms, sadness, financial hardship, future uncertainty, and stress (14–16). Remarkably, this study shows that 34.9% of alcohol consumers reported reducing their alcohol use since COVID-19, which is consistent with findings from previous studies (17). The prohibition of social gatherings during the pandemic may be one of the causes. In addition to closing bars and other establishments that served alcohol, the social gathering ban prohibited interacting socially with friends, family, or coworkers (18). Nonetheless, 61.3% of those who drank alcohol stated they had no intention of quitting. As Malaysia navigates the post-pandemic landscape, the insights from this study are critical for informing targeted health interventions. The data showing changes in smoking and alcohol consumption patterns, with some individuals starting these behaviors during the pandemic and notable intentions to quit smoking, underscore the need for focused support services. Tailoring interventions to address these specific behaviors can enhance their effectiveness, improving public health outcomes.
Furthermore, compared to 32.5% of smokers who had the intention but made no attempts to quit, nearly half (42.9%) of current smokers had the intention to quit and had tried to quit. There is evidence that the COVID-19 pandemic would influence smokers’ attitudes toward giving up. According to a survey conducted in the US, most smokers cut back on their use because they intended to stop smoking (19). Health concerns associated with COVID-19 could be used to highlight the dangers of smoking because they could make cessation efforts more successful in persuading individuals to give up the habit during the pandemic (20). Thus, this study sheds light on intentions to quit smoking, influenced by COVID-19-related health concerns, presenting an opportunity for targeted intervention strategies.
Regarding sleeping patterns, the proportion of respondents who slept for less than 7 hours during the pandemic increased compared to before. On the other hand, a few studies found that people slept longer during the pandemic. However, along with the extended period came a shift in sleep schedule and a deterioration in sleep quality (21). Changes in wakefulness and sleep patterns can majorly impact one’s health. In addition to increasing the risk of diabetes, cardiovascular disease, and mental health issues, it has been shown that getting too little sleep is linked to poorer cognitive function and diminished physical performance (22). However, almost half of the study’s respondents said their wake and bedtimes remained the same. Our findings contradicted those of a prior study (23), which documented a significant shift in sleep timing during COVID-19, with respondents staying longer and going to bed earlier. This discussion critically examines the nuanced shifts in health behaviors amid the pandemic, providing valuable insights into the complex interplay of individual choices and external factors during the global health crisis.
The publication of this manuscript is critically important now as it is essential for guiding post-pandemic health interventions, policies, and public awareness efforts. It offers an overview of the change in health behaviors among Malaysians during the pandemic. For example, by understanding how the pandemic has specifically altered health behaviors, individuals can make more informed decisions regarding their health. This knowledge can also foster community support for adopting healthier lifestyles during recovery. Not only that, this study contributes to the global body of knowledge, providing valuable comparative data for researchers and public health officials worldwide. It highlights Malaysia’s unique challenges and responses, offering lessons that can inform global health strategies. Understanding and addressing these shifts will help Malaysia and other countries better navigate the post-pandemic landscape, promoting overall well-being and resilience against future public health challenges.
Limitation and recommendation
The study’s results have notable limitations that warrant further discussion. Primarily, the cross-sectional design captures health behaviors before and during the pandemic at a single point in time. This raises concerns about the accuracy of participants’ recollections, particularly given the varying stress levels they may have experienced during the pandemic. Although the study acknowledges the potential for recall bias, this significant limitation deserves more in-depth consideration, as the validity of the findings heavily relies on how accurately individuals can recall their health behaviors during such a tumultuous period.
As societies continue to adapt to the ongoing presence of COVID-19, understanding shifts in health behaviors remains crucial. The findings provide valuable insights into how adult Malaysians’ health behaviors changed during the pandemic, but they also raise critical questions about the sustainability of these changes moving forward. In 2024, many individuals may be navigating a “new normal” where previous adaptations could either persist or revert to pre-pandemic patterns. The absence of data on current (post-pandemic) health behaviors complicates our understanding of whether the observed changes are lasting or merely temporary responses to the pandemic. Given that health behaviors may have continued to evolve since data collection in 2022, future research should adopt longitudinal approaches to effectively capture these dynamics over time.
To address these considerations, the implications of this study in the current post-pandemic context could be articulated more clearly. While the findings contribute valuable insights into health behavior changes during the pandemic, their relevance to present-day public health interventions and policies may be limited. However, it is essential for policymakers and public health professionals to recognize the long-term impacts of the COVID-19 pandemic on community health and well-being. By understanding how past behaviors were influenced by the pandemic, strategies can be developed that not only address current health needs but also promote sustained healthy practices.
The study emphasizes the importance of considering the long-term effects of the COVID-19 pandemic and enhancing health promotion strategies that effectively engage the population in positive health behaviors. Leveraging approaches such as “nudges,” as introduced by Thaler (24), could play a key role in encouraging adherence to health-enhancing behaviors (25–30). By implementing subtle interventions that influence decision-making without restricting choices, public health efforts can foster lasting behavior change. Overall, a comprehensive understanding of health behavior trends in the evolving post-pandemic landscape will be essential for guiding future interventions and improving community health.
Conclusion
The study’s conclusions show notable variations in the respondents’ health-related behaviors before and during the COVID-19 pandemic. There were positive changes in the amount of fruit and plain water consumed daily and the intention to stop smoking. On the other hand, detrimental alterations included decreased physical activity, more screen time, frequent snacking, extended sitting and lying down, and shorter sleep duration.
Maintaining healthy behaviors and changing harmful ones is vital to fend off pandemics and forestall diseases in the future. Therefore, public education is necessary to promote healthy lifestyles actively. The general well-being and resilience of the population can be protected in advance of any future health issues by assisting people in forming and maintaining healthy lifestyles.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Medical Research & Ethics Committee (MREC). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NI: Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. RK: Conceptualization, Data curation, Resources, Writing – original draft, Writing – review & editing. NA: Conceptualization, Data curation, Resources, Writing – original draft, Writing – review & editing. SA: Conceptualization, Data curation, Resources, Writing – original draft, Writing – review & editing. MK: Conceptualization, Project administration, Supervision, Visualization, Writing – review & editing. AP: Conceptualization, Data curation, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work is financial support for the publication of this article was provided by the Ministry of Health of Malaysia.
Acknowledgments
We would like to thank the Director-General of Health and Deputy Director-General of Health (Research and Technical Support), Ministry of Health Malaysia, for the permission to publish this paper.
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization, WHO COVID-19 dashboard. Available at:https://data.who.int/dashboards/covid19/cases. Accessed 1 Oct. 2024.
2. Rossinot, H, Fantin, R, and Venne, J. Behavioral changes during COVID-19 confinement in France: a web-based study. Int J Environ Res Public Health. (2020) 17:8444. doi: 10.3390/ijerph17228444
3. Romm, KF, Patterson, B, Wysota, CN, Wang, Y, and Berg, CJ. Predictors of negative psychosocial and health behavior impact of covid-19 among young adults. Health Educ Res. (2021) 36:385–97. doi: 10.1093/her/cyab026
4. Wang, J, Yeoh, EK, Yung, TKC, Wong, MCS, Dong, D, Chen, X, et al. Change in eating habits and physical activities before and during the COVID-19 pandemic in Hong Kong: a cross-sectional study via random telephone survey. J Int Soc Sports Nutr. (2021) 18:33. doi: 10.1186/s12970-021-00431-7
5. Husain, W, and Ashkanani, F. Does COVID-19 change dietary habits and lifestyle behaviours in Kuwait: a community-based cross-sectional study. Environ Health Prev Med. (2020) 25:61. doi: 10.1186/s12199-020-00901-5
6. Watson, KB, Whitfield, GP, Huntzicker, G, Omura, JD, Ussery, E, Chen, TJ, et al. Cross-sectional study of changes in physical activity behavior during the COVID-19 pandemic among us adults. Int J Behav Nutr Phys Act. (2021) 18:91. doi: 10.1186/s12966-021-01161-4
7. Ali, SH, Foreman, J, Tozan, Y, Capasso, A, Jones, AM, and DiClemente, RJ. Trends and predictors of COVID-19 information sources and their relationship with knowledge and beliefs related to the pandemic: Nationwide cross-sectional study. JMIR Public Health Surveill. (2020) 6:e21071. doi: 10.2196/21071
8. NCCFN. Malaysian dietary guidelines 2020. Ministry of Health Malaysia: National Coordinating Committee on Food and Nutrition (2021).
9. di Renzo, L, Gualtieri, P, Pivari, F, Soldati, L, Attinà, A, Cinelli, G, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. (2020) 18:229. doi: 10.1186/s12967-020-02399-5
10. Institute for Public Health (IPH), National Institutes of Health, Ministry of Health Malaysia (2020). “National Health and morbidity survey (NHMS) 2019: Vol. I: NCDs – Non-communicable diseases: Risk factors and other health problems ”
11. Ammar, A, Brach, M, Trabelsi, K, Chtourou, H, Boukhris, O, Masmoudi, L, et al. Effects of covid-19 home confinement on eating behaviour and physical activity: results of the ECLB-covid19 international online survey. Nutrients. (2020) 12:1583. doi: 10.3390/nu12061583
12. Sallis, R, Young, DR, Tartof, SY, Sallis, JF, Sall, J, Li, Q, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. (2021) 55:1099–105. doi: 10.1136/bjsports-2021-104080
13. Wolf, S, Seiffer, B, Zeibig, JM, Welkerling, J, Brokmeier, L, Atrott, B, et al. Is physical activity associated with less depression and anxiety during the COVID-19 pandemic? A rapid systematic review. Sports Med. (2021) 51:1771–83. doi: 10.1007/s40279-021-01468-z
14. Rehm, J, Kilian, C, Ferreira-Borges, C, Jernigan, D, Monteiro, M, Parry, CDH, et al. Alcohol use in times of the COVID 19: implications for monitoring and policy. Drug Alcohol Rev. (2020) 39:301–4. doi: 10.1111/dar.13074
15. Schäfer, AA, Santos, LP, Quadra, MR, Dumith, SC, and Meller, FO. Alcohol consumption and smoking during covid-19 pandemic: association with sociodemographic, behavioral, and mental health characteristics. J Community Health. (2022) 47:588–97. doi: 10.1007/s10900-022-01085-5
16. Keng, S-L, Stanton, MV, Haskins, LAB, Almenara, CA, Ickovics, J, Jones, A, et al. Covid-19 stressors and health behaviors: a multilevel longitudinal study across 86 countries. Prev Med Rep. (2022) 27:101764. doi: 10.1016/j.pmedr.2022.101764
17. Clare, PJ, Aiken, A, Yuen, WS, Upton, E, Kypri, K, Degenhardt, L, et al. Alcohol use among young Australian adults in may–June 2020 during the COVID-19 pandemic: a prospective cohort study. Addiction. (2021) 116:3398–407. doi: 10.1111/add.15599
18. Bade, R, Simpson, BS, Ghetia, M, Nguyen, L, White, JM, and Gerber, C. Changes in alcohol consumption associated with social distancing and self-isolation policies triggered by Covid-19 in South Australia: a wastewater analysis study. Addiction. (2020) 116:1600–5. doi: 10.1111/add.15256
19. Kowitt, SD, Cornacchione Ross, J, Jarman, KL, Kistler, CE, Lazard, AJ, Ranney, LM, et al. Tobacco quit intentions and behaviors among cigar smokers in the United States in response to COVID-19. Int J Environ Res Public Health. (2020) 17:5368. doi: 10.3390/ijerph17155368
20. Phetphum, C, Prajongjeep, A, Keeratisiroj, O, and Thawatchaijareonying, K. Communication intervention to improve perceived threat of smoking-related covid-19 and intentions to quit smoking during the COVID-19 pandemic in Thailand. Tob Induc Dis. (2022) 20:1–12. doi: 10.18332/tid/150363
21. Neculicioiu, VS, Colosi, IA, Costache, C, Sevastre-Berghian, A, and Clichici, S. Time to sleep?—a review of the impact of the COVID-19 pandemic on sleep and mental health. Int J Environ Res Public Health. (2022) 19:3497. doi: 10.3390/ijerph19063497
22. Chattu, V, Manzar, MD, Kumary, S, Burman, D, Spence, DW, and Pandi-Perumal, SR. The global problem of insufficient sleep and its serious public health implications. Healthcare. (2019) 7:1. doi: 10.3390/healthcare7010001
23. Cellini, N, Canale, N, Mioni, G, and Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. (2020) 29:e13074. doi: 10.1111/jsr.13074
24. Thaler, RH, and Sunstein, CR. Nudge: Improving decisions about health, wealth and happiness. London, UK: Allen Lane (2021).
25. Dudas, G, Hong, SL, Potter, BI, Calvignac-Spencer, S, Niatou-Singa, FS, Tombolomako, TB, et al. Emergence and spread of SARS-COV-2 lineage B.1.620 with variant of concern-like mutations and deletions. Nat Commun. (2021) 12, 1:5769. doi: 10.1038/s41467-021-26055-8
26. Dai, H, Saccardo, S, Han, MA, Roh, L, Raja, N, Vangala, S, et al. Behavioural nudges increase COVID-19 vaccinations. Nature. (2021) 597:404–9. doi: 10.1038/s41586-021-03843-2
27. Wisdom, J, Downs, J, and Loewenstein, G. Promoting healthy choices: information vs. convenience. American Economic Journal: Applied Economics. (2010) 2:164–78. doi: 10.1257/app.2.2.164
28. Forberger, S, Reisch, L, Kampfmann, T, and Zeeb, H. Nudging to move: a scoping review of the use of choice architecture interventions to promote physical activity in the general population. Int J Behav Nutr Phys Act. (2019) 16:77. doi: 10.1186/s12966-019-0844-z
29. Laiou, E, Rapti, I, Schwarzer, R, Fleig, L, Cianferotti, L, Ngo, J, et al. Review: nudge interventions to promote healthy diets and physical activity. Food Policy. (2021) 102:102103. doi: 10.1016/j.foodpol.2021.102103
30. Papandreou, P, Gioxari, A, Daskalou, E, Grammatikopoulou, MG, Skouroliakou, M, and Bogdanos, DP. Mediterranean diet and physical activity nudges versus usual care in women with rheumatoid arthritis: results from the Madeira randomized controlled trial. Nutrients. (2023) 15:676. doi: 10.3390/nu15030676
Keywords: health behaviors, COVID-19, Malaysia, eating behaviors, physical activity, smoking, alcohol, sleep patterns
Citation: Ithnain N, Kassim R, Amirudin N, Aimanan SNM, Krishnan M and Panting AJ (2024) A cross-sectional study on health behavior changes during COVID-19 among adults in Malaysia. Front. Public Health. 12:1465996. doi: 10.3389/fpubh.2024.1465996
Edited by:
Wing Fai Yeung, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Oksana Zayachkivska, Danylo Halytsky Lviv National Medical University, UkraineKerry Sudom, Department of National Defence (DND), Canada
Copyright © 2024 Ithnain, Kassim, Amirudin, Aimanan, Krishnan and Panting. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Norbaidurah Ithnain, ZHVycmFoQG1vaC5nb3YubXk=
 Norbaidurah Ithnain
Norbaidurah Ithnain Rosnani Kassim1
Rosnani Kassim1