- 1Department of Vector Genomics, ICMR-National Institute of Malaria Research, Sector-8, New Delhi, India
- 2ICMR-National Institute of Malaria Research, Field Unit, Nadiad, Gujarat, India
- 3Vector Borne Diseases Control Program, Government of Gujarat, Gandhinagar, Gujarat, India
Objectives: Surveillance is the backbone for the control of malaria and its elimination. In the state of Gujarat, situated in the western region of India, some of the districts reported a high annual blood examination rate (ABER) for malaria. Therefore, a study was conducted to identify the underlying reasons for the increase in the ABER for malaria.
Methods: Planned investigations were carried out in three of the state districts, scrutinizing records of malaria forms and other epidemiological data collected during health worker surveillance, assessment of laboratory services, and rapid fever surveys.
Results: The rate of fever ranged from 8 to 57% in the primary health centers that were surveyed. Analysis of epidemiological data revealed that malaria parasite positivity was more from passive than active surveillance. Increased ABER was accounted for by multiple factors, including blood slides collected during the mass survey and contact smears, which were included in the ABER and not mentioned separately. Blood slides prepared for the migrant population were included in the ABER, but the migrant population was not counted while calculating the ABER.
Conclusion: The ABER in villages surveyed varied from 1.6 to 78%, which is mainly due to indiscriminate preparation of blood slides, i.e., without fever symptoms. Addressing the key gaps identified in data recording may aid in channeling the limited resources efficiently, thereby progressing toward malaria elimination. Adequate surveillance activities, along with systematic data recording, will enable timely, informed decision-making for the effective allocation of resources, ultimately supporting malaria elimination efforts in the state.
1 Introduction and rationale
The period of success in global malaria control has been followed by a plateau in further advancements. Despite being preventable and curable, malaria remains a major public health issue worldwide (1). However, India has made significant progress in reducing malaria incidence, with a consistent decline in malaria cases across the country since 2000 (2). Malaria remains unstable in certain regions of the country, with Gujarat state being one of them, contributing significantly to cases caused by Plasmodium vivax (3). Effective malaria case detection through robust surveillance and comprehensive treatment is vital for vector-borne disease control programs aimed at reducing the disease burden in the state. This process provides crucial evidence for policymakers to identify areas and population groups most susceptible to malaria, facilitating the monitoring of changes in disease patterns. Consequently, this enables health authorities to design appropriate interventions. Additionally, evaluating and assessing surveillance systems is vital for their continued improvement (16, 17). In India, the surveillance of malaria cases is conducted through active and passive case detection as per the operational manual of the National Center for Vector-Borne Disease Control (NCVBDC) (4). In passive detection, patients visit the healthcare provider/facility for evaluation. In contrast, active case detection involves health service providers visiting households to detect malaria cases. Fortnightly, active surveillance is essential for interrupting malaria transmission. Timely collection and investigation of blood smears are crucial strategies of the government's “early diagnosis and prompt treatment” policy.
In Gujarat state, blood smear examination/collection has increased gradually from 12.68 million in 2013 to 14.78 million in 2016 (data from the state). An annual blood examination rate (ABER) of 10% is considered adequate, but a few districts of Gujarat state have reported a high annual blood examination rate (ABER). The Joint Director of the Vector Borne Disease Control Program (VBDCP) in Gujarat requested the National Institute of Malaria Research (NIMR), a Central Government agency, to independently assess surveillance and laboratory services at primary health centers (PHCs). Hence, a study was undertaken to evaluate the quality of surveillance and laboratory services in three districts of Gujarat state, viz., Anand, Ahmedabad, and Gandhinagar districts. The study aimed to assess the performance of active and passive surveillance agencies through scrutiny of records, conducting personal discussions with staff, carrying out field visits, and assessing the quality of laboratory services to patients in the study area.
2 Methodology
2.1 Study area
The study was carried out in Gujarat state, situated in the western region of India, which shares its international border with Pakistan in the northwest and national borders with the states of Rajasthan, Madhya Pradesh, and Maharashtra.
The state's three-tier public healthcare delivery system is structured into primary, secondary, and tertiary levels. The primary healthcare system is further subdivided into three categories: (i) sub-centers (SCs)/sub-health centers (SHCs) at the base level, catering to a population of 3,000–5,000; (ii) primary health centers (PHCs) serving a population of 20,000–30,000; and (iii) community health centers (CHCs) catering to a population of 80,000–1,20,000.
According to the State Programme Office, seven districts, viz., Anand, Ahmedabad, Gandhinagar, Surendranagar, Patan, Banaskantha, and Dahod, have reported >25% ABER in 2016. The ICMR-NIMR, Nadiad team, planned an investigation in three districts (Anand, Ahmedabad, and Gandhinagar). A team consisting of scientists, a technical officer, a laboratory technician, and a field and laboratory assistant visited four PHCs in each of the three districts in 2017. The study area is shown in Figure 1.
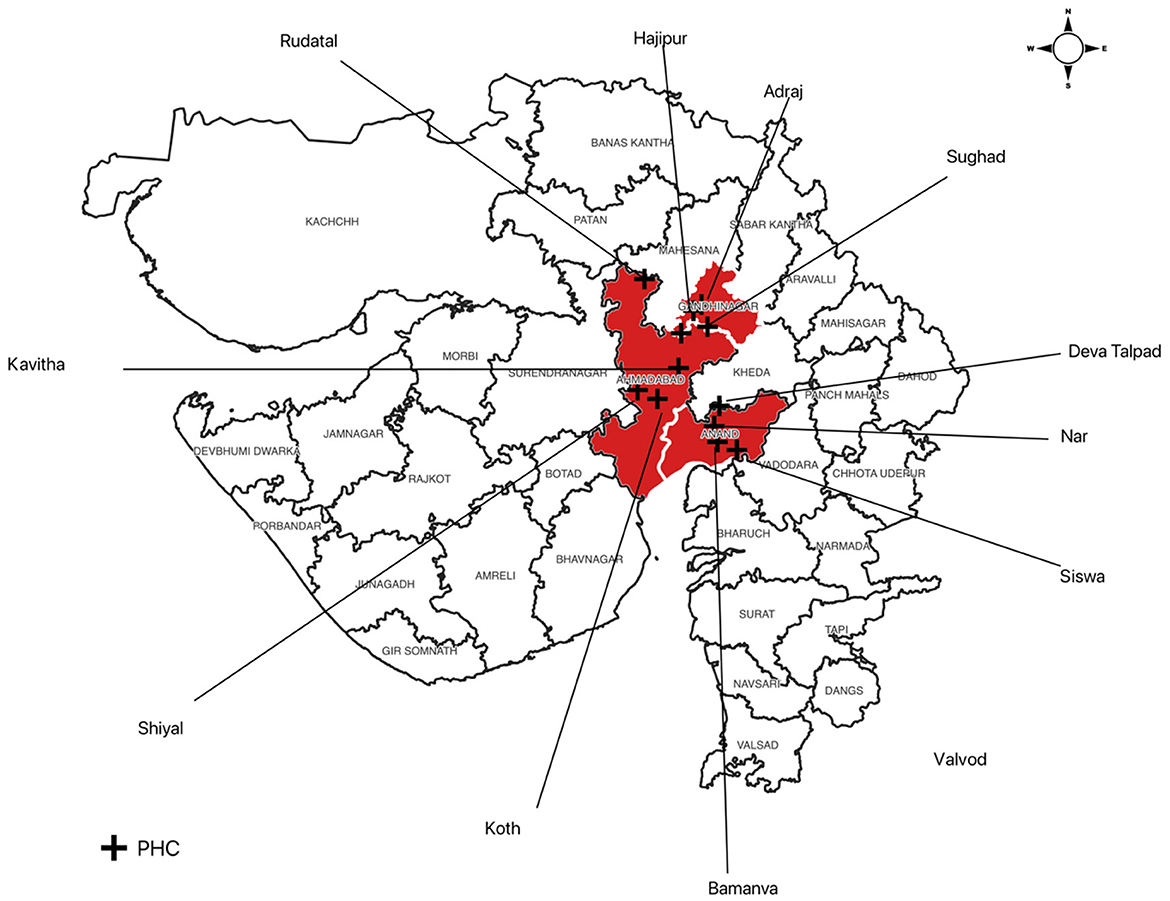
Figure 1. Map of Gujarat state showing the study area of 12 primary health centers (PHCs) in three districts, + representing the location of PHCs.
2.2 Selection of PHCs and villages
Based on the annual blood examination rate (ABER) in 2016, four PHCs each in three districts, namely, Ahmedabad, Anand, and Gandhinagar, showing both high and low ABERs were included in the study (Table 1). The teams conducted the rapid fever survey and visited PHCs with low and high ABERs in each district. The rapid fever survey was carried out in one village of each PHC to assess the quality of domiciliary visits of the concerned multipurpose health worker.
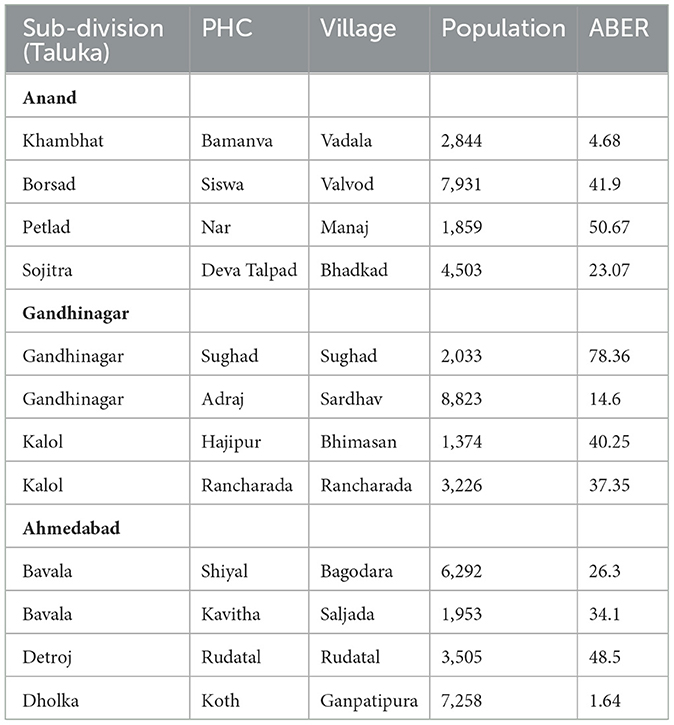
Table 1. Data on population and annual blood examination rate (ABER) of primary health centers (PHCs) and villages included in the study.
2.3 Discussion with officers and staff
The team discussed the surveillance plan, activities, and data with medical officers, laboratory technicians, supervisors, multipurpose health workers (MPHW-M), and Accredited Social Health Activists (ASHA) of the concerned PHCs. Apart from this, malaria forms, M-1, M-2, M-3, and M-4, as well as records of MPHW (M) and ASHA, were also scrutinized to determine the sources of blood smear collection, examination, and recording/reporting.
2.4 Assessment of laboratory services
The malaria microscopy laboratory at each primary health center (PHC) was inspected, focusing on the available equipment, logistics, methodology, records, and cross-checked reports of blood slides.
2.5 Malaria surveillance in villages
According to the NVBDCP manual, active case detection (ACD) should be carried out by assigning a multipurpose health worker male [MPHW (M)] to each PHC, following the advanced tour program of the worker (4). The fortnightly domiciliary visits using “reporting formats for malaria” are the technical requirement of malaria disease management. Active case detection ensures uninterrupted linkage between the communities and the peripheral health delivery system. The main components of the door-to-door active surveillance are as follows: (a) searching for individuals with fever or those who had a fever since the last visit by the MPW, (b) collection and examination of blood smears from such cases, and (c) administration of appropriate anti-malarial(s) as per the national malaria drug policy.
Furthermore, all individuals with fever attending the PHC should be screened for malaria, and blood smears collected by MPHW (F), ASHAs, Anganwadi workers, and other agencies should be included in passive case detection. The malaria forms and records of the health facility were examined, and discussions were held regarding the schedule and methods of activities carried out by supervisors, MPHW (M), and ASHAs. The treatment of confirmed malaria cases provided by staff was also scrutinized using radical treatment cards.
2.6 Rapid fever survey
The NIMR teams along with local health staff (MPHW) of the village and ASHAs carried out a rapid fever survey in one village of each PHC visited during the investigation, covering a minimum of 300–500 population. A blood smear of each febrile person was prepared. The blood smear was processed, stained, and examined at the NIMR laboratory.
2.7 Data collection and analysis
Retrospective data on malaria surveillance, diagnosis, and treatment were obtained from each PHC and sent to Medical Officers in a prescribed format before the PHC visit.
3 Results
3.1 Surveillance and record examination
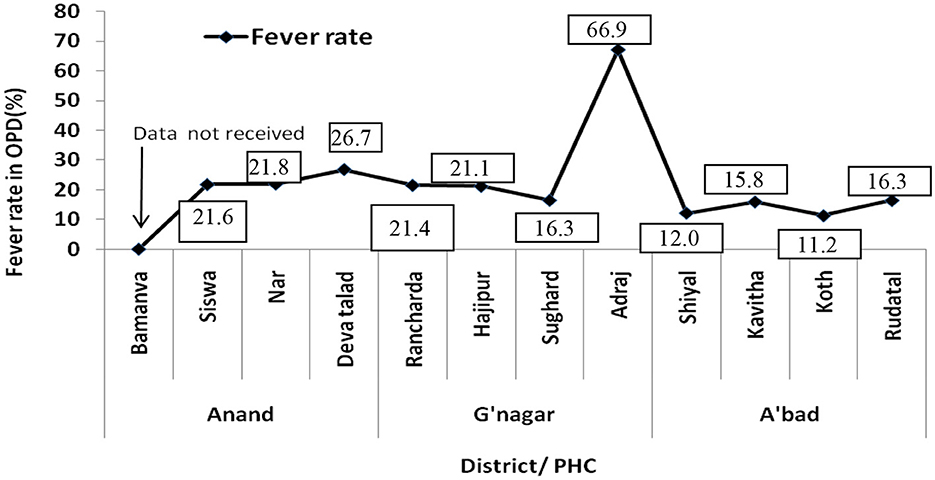
Data on monthly OPD attendance and febrile patients in four PHCs in each of Anand, Gandhinagar, and Ahmedabad districts were obtained to determine the fever rate in each district. It has been observed that the Gandhinagar district reported the highest fever rate/febrile patients (31.7–57.26%) throughout the year, followed by Anand (11.83–35.2%) and Ahmedabad (8.1–20.03%; Figure 2).
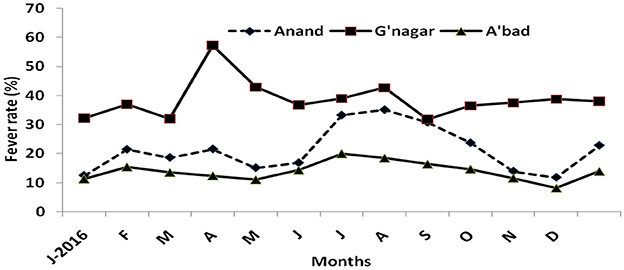
Figure 2. Fever rate in Anand, Gandhinagar, and Ahmedabad, based on four primary health centers in each district.
The PHC-wise analysis of OPD revealed > 21% of febrile patients in Anand and 16–21% in Gandhinagar except in Adraj PHC where 66.9% of OPD patients were febrile in 2016. In Ahmedabad, all four PHCs reported < 17% of febrile patients in OPD (Figure 3).
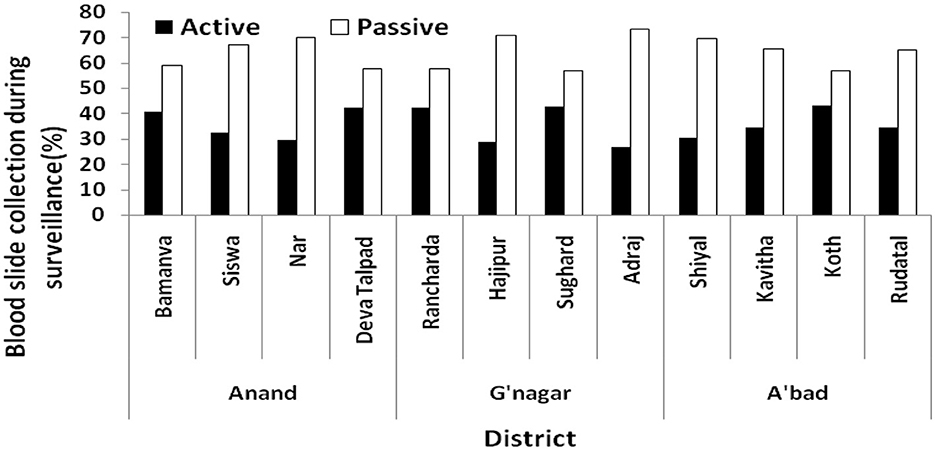
3.2 Agency wise blood slide collection/examination
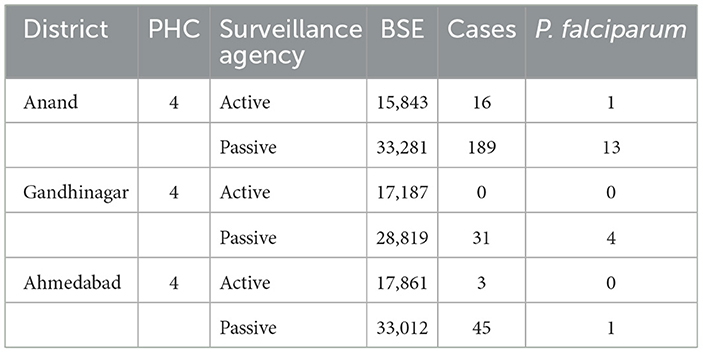
Data on blood slide collection/examination (BSC/E) were obtained from each PHC visited in the study districts. In general, a large proportion of blood slides were collected by the passive agencies (ASHA, MPHW (F), and PHC OPD (Figure 4). The passive collection among 12 PHCs in three districts ranged from 56 to 73%. In Anand, active collection ranged from 29 to 42% among four PHCs, 26–42% in Gandhinagar, and 30–43% in Ahmedabad. In all the PHCs, the passive collection was more than the active collection, ranging from 56 to 82.5%.
Table 2 reveals that active collection in each PHC was nearly 40% of the total BSE but the positivity was very low, indicating poor quality of surveillance. In Gandhinagar, not even a single malaria case could be detected from the active collection in four PHCs (Table 2).
3.3 Annual blood examination rate
Table 3 shows the ABERs and SPRs of the study districts over a period of time, whereas Table 4 shows the ABERs of the PHCs visited; The ABERs for PHCs visited are given in Table 3, it has been seen that the ABERs in 12 PHCs of three districts were ≥25% except in Bamanva (12.30%) PHC of Anand and Shiyal (19.91%) PHC of Ahmedabad district.

Table 3. Annual blood examination rate (ABER) and slide positivity rate (SPR) of study districts (12).
The ABERs in most of the villages in the same PHC varied to a very high level and remained higher throughout the year. In all three districts, the village-to-village variation in ABERs was quite high.
3.4 Scrutiny of records and factors for high ABER
During discussions with laboratory technicians, multipurpose health workers (MPHWs), and multipurpose health supervisors (MPHSs) from different PHCs, along with a review of records, it was observed that the blood smears collected during various focal and mass surveys under health programs have been incorrectly incorporated into active surveillance. This practice dilutes the importance of surveillance. Areas such as brick kilns, construction sites, and new projects, if included in routine surveillance, should have their populations accounted for separately when calculating the ABER. The objectives of these focal surveys differ; hence, the data must be recorded and analyzed separately to improve control strategies in particular areas and to identify the high-risk foci. Another reason for high ABER is when confirmed malaria cases were followed by PHC staff for 28 days to assess the drug efficacy. Blood slides were prepared on day 3 and weekly during the patient's follow-up. Thus, five additional blood smears of the same patient were prepared. The workers assigned fresh serial numbers to each follow-up slide, enhancing the ABER. However, several factors contributed to a high ABER, including indiscriminate blood smear preparation during antenatal check-ups, which were subsequently added to the active or passive collections. Furthermore, high variation in the ABER has been observed due to indiscriminate blood slide preparation and discrepancies in data recording by local health workers.
3.5 Status of laboratory services in PHCs
The NIMR team visited 12 laboratories in the three districts to assess the services provided to patients attending the PHCs, the logistics, and the conditions of the equipment related to malaria microscopy. During surveys, it was noticed that each laboratory had separate space, adequate furniture, and availability of antimalarials. The microscope of all primary health centers was found to be in working condition except in one PHC where servicing and replacement of the lenses of the microscope were required. The team suggested that a standard operating procedure (SOP) should be provided to the Laboratory Technician to maintain the microscope. Cross-checking of blood smears collected from different PHCs was performed. A few negative (119) and positive (23) slides examined by laboratory technicians of various PHCs were taken and cross-checked at the NIMR laboratory, and no discrepancy was observed. During a rapid fever survey by the team in one village of each study PHC, 82 blood smears were collected, processed, and examined at the NIMR Lab. None of them was found positive for the malaria parasite. The results have been communicated to the medical officer of the concerned PHC. A final report was prepared, and the recommendations made were transmitted to the state Health authority.
4 Discussion
Malaria parasite load in the community is governed by multiple parameters, such as individual immunity (5), the presence of infected individuals, the local vector population, and environmental conditions (13). The detection and treatment of malaria cases are important requisites for the elimination of malaria (6). Early identification of cases and their radical treatment aid in reducing human reservoirs and infective vectors, thus reducing malaria transmission in the community (7). Therefore, timely collection and examination of blood smears are key elements in the malaria control strategy.
Primary health centers are responsible for various programs and additional services rendered by field staff. Enhancing focused laboratory services and ensuring staff are adequately trained will enhance the performance of PHCs (15). Therefore, it is recommended that state health authorities prioritize filling all vacant positions. The involvement of the Medical Officer of the primary health center in vector control is important for arranging timely and complete surveillance in the villages. The fortnight advance tour program of the supervisor, MPHW (M), ASHAs, and other workers should be prepared under the guidance of MO to cover the entire area in time. The fortnightly door-to-door visits are a technical requirement of malaria disease management. The domiciliary active surveillance should be conducted by MPHW (M) or ASHA by visiting each family at their homes. The blood smear of only febrile patients/persons with a history of fever within the last fortnight must be prepared, and complete details, including symptoms, should be recorded in the case recording form. Furthermore, the blood slides collected by MPHW (F), ASHAs, and Anganwadi workers or during any unscheduled visit are considered a passive collection. All PHC staff should follow the standard operative procedure for surveillance. Assessment of ASHA in a tribal setting has revealed that training needs to be provided to ASHA workers for malaria surveillance and treatment (8).
The present study elucidated reasons for the high ABER reported in some districts, which is mainly due to the issues with data recording practices. There are many brick kilns, construction sites, and developmental projects in several villages where many migrant laborers camped in temporary shelters. Such construction sites and developmental projects provide ideal conditions for vectors to breed and malaria to spread (9). Usually, slides are prepared from migrants in these areas, but their population is not considered while calculating the ABER, thereby potentially augmenting the ABER. Furthermore, during follow-up of malaria cases, PHC workers prepare additional blood smears, labeling each slide with continuous serial numbers. Whereas, the follow-up slides of an individual should bear the original registration number along-with a descendant such as A, B, C (example: if original serial number is 101, then follow-up slides number may be 101-A, 101-B). To achieve this activity's objective, the results of the follow-up slides should have been analyzed separately to determine the status of drug efficacy in the community. In addition, when blood smears prepared during unscheduled surveillance activities by ASHAs, ANMs, and other agencies are included in active surveillance, it leads to an increase in the BSC and the ABER at PHCs.
In general, the laboratory services at each PHC were found to be satisfactory. However, there is scope for improvement by providing staining coupling jars with lids, microscope servicing, and replacement of damaged lenses for laboratory technicians. Excellent logistics support will also enhance the efficacy of laboratory technicians and reduce the time lag in reporting. Availability of antimalarials (2.5 mg PQ and ACT) and RDT at PHC should be monitored, and arrangements should be made to fulfill the requirement. A brief standard operating procedure for malaria laboratory maintenance should be developed and distributed to laboratory technicians for good laboratory practices.
Studies have highlighted that adequate surveillance activities performed over some time along with proper data recording (10, 14) can impact the malaria burden in the area. Furthermore, it has also been suggested that surveillance activities indicated by ABER can have an impact on other metrics used in malaria, such as annual parasite incidence (API) (11), thereby highlighting the importance of ABER and surveillance activities. The present study has a few limitations. The study was conducted at a limited number of sites primarily due to the restricted availability of data from different sites and time constraints. Another limitation is that recent data from various PHCs could not be analyzed and included in the study. In spite of these limitations, the study has provided essential insights into the factors responsible for augmented ABER in various PHCs of different districts of Gujarat state. We have identified vital gaps that, when addressed, will help build an effective surveillance system, thereby facilitating malaria elimination in the state.
5 Conclusion
The analysis of OPD attendance and febrile patients showed that fever rates ranged between 16 and 26% in different primary health centers except one. However, the indiscriminate blood smear preparation in each PHC has exaggerated the ABERs in the studied districts. The study analyzed the factors exaggerating the ABERs in different districts of Gujarat state and identified the gaps that need to be addressed through state health authorities. Proper surveillance activities, along with an appropriate recording of data, will aid in monitoring the disease progression and channel the use of limited resources. This approach will help reduce malaria transmission and achieve zero indigenous cases in the state, leading toward malaria elimination in the near future.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. RB: Data curation, Formal analysis, Investigation, Supervision, Writing – original draft, Writing – review & editing. MD: Data curation, Investigation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study acknowledges funding from ICMR-NIMR, Delhi and State Vector Borne Diseases Control Program, Government of Gujarat, India.
Acknowledgments
We extend our gratitude to the Vector Borne Disease Control Program, Government of Gujarat, India, for their support in facilitating the smooth execution of this study. The authors are thankful to ICMR-NIMR for providing support. The excellent technical support provided by the staff of the ICMR-NIMR Field Unit, Nadiad, Gujarat, is gratefully acknowledged. During the editing and revision of manuscript, the authors used ChatGPT to re-frame a few sentences. The authors take full responsibility for the content of the publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ABER, annual blood examination rate; MO, medical officer; BSC/BSE, blood slide collected/examined; PHC, primary health center; RDT, rapid diagnostic test; ASHA, Accredited Social Health Activist, ANM, auxiliary nurse midwifery; MPHW (M), multipurpose health worker (male); MPHW (F), multipurpose health worker (female).
References
1. WHO. World Malaria Report 2022 (2022). Geneva: WHO. Available at: https://www.who.int/publications/i/item/9789240064898 (accessed July 29, 2023).
2. WHO. World Malaria Report 2020: India Continues to Make Impressive Gains in Reduction of Malaria Burden (2020). Available at: https://pib.gov.in/Pressreleaseshare.aspx?PRID=1677601 (accessed July 15, 2024).
3. National Center for Vector Borne Diseases Control. Malaria Situation in India (2019). Available at: https://ncvbdc.mohfw.gov.in/WriteReadData/l892s/70565888431728538345.pdf (accessed September 28, 2024).
4. National Vector Borne Disease Control Programme. Operational Manual for Implementation of Malaria Programme (2009). Available at: https://ncvbdc.mohfw.gov.in/WriteReadData/l892s/Malaria-Operational-Manual-2009.pdf (accessed July 15, 2024).
5. Gonzales SJ, Reyes RA, Braddom AE, Batugedara G, Bol S, Bunnik EM. Naturally acquired humoral immunity against Plasmodium falciparum malaria. Front Immunol. (2020) 11:2809. doi: 10.3389/fimmu.2020.594653
6. National Vector Borne Disease Control Programme. Operational Manual for Malaria Elimination in India 2016 (Version-1) (2016). Available at: https://nvbdcp.gov.in/WriteReadData/l892s/5232542721532941542.pdf (accessed July 15, 2024).
7. Hsiang MS, Ntuku H, Roberts KW, Dufour MSK, Whittemore B, Tambo M, et al. Effectiveness of reactive focal mass drug administration and reactive focal vector control to reduce malaria transmission in the low malaria-endemic setting of Namibia: a cluster-randomised controlled, open-label, two-by-two factorial design trial. Lancet. (2020) 395:1361. doi: 10.1016/S0140-6736(20)30470-0
8. Rajvanshi H, Saha KB, Shukla MM, Nisar S, Jayswar H, Mishra AK, et al. Assessment of ASHA for knowledge, diagnosis and treatment on malaria in Mandla district of Madhya Pradesh as part of the malaria elimination demonstration project. Malar J. (2021) 20:78. doi: 10.1186/s12936-021-03610-8
9. Baeza A, Santos-Vega M, Dobson A, Pascual M. The rise and fall of malaria under land-use change in frontier regions. Nat Ecol Evol. (2017) 1:e0108. doi: 10.1038/s41559-017-0108
10. Agbemafle EE, Kubio C, Bandoh D, Odikro MA, Azagba CK, Issahaku RG, et al. Evaluation of the malaria surveillance system—Adaklu District, Volta Region, Ghana, 2019. Public Health Pract. (2023) 6:100414. doi: 10.1016/j.puhip.2023.100414
11. Yadav CP, Gupta S, Bharti PK, Rahi M, Faizi N, Sharma A. India may need an additional metric to assess the endemicity of malaria in low surveillance districts. PLoS Glob Public Health. (2022) 2:e0000326. doi: 10.1371/journal.pgph.0000326
12. National Center for Vector Borne Diseases Control. District Level Data Malaria Cases and Death (2024). Available at: https://ncvbdc.mohfw.gov.in/index1.php?lang=1&level=1&sublinkid=5784&lid=3689 (accessed September 28, 2024).
13. Bennett A, Yukich J, Miller JM, Keating J, Moonga H, Hamainza B, et al. The relative contribution of climate variability and vector control coverage to changes in malaria parasite prevalence in Zambia 2006–2012. Parasit Vect. (2016) 9:431. doi: 10.1186/s13071-016-1693-0
14. Chalageri VH, Marinaik SB, Nath SN, Singhal R, Rawat S, Ravikumar K, et al. Malaria control—lessons learned from trends of Malaria indices over three decades in Karnataka, India. Malar J. (2023) 22:353. doi: 10.1186/s12936-023-04774-1
15. Jain R, Rao B. Role of laboratory services in primary health center (PHC) outpatient department performance: an Indian case study. Prim Health Care Res Dev. (2019) 20:e112. doi: 10.1017/S1463423619000537
16. Lourenço C, Tatem AJ, Atkinson PM, et al. Strengthening surveillance systems for malaria elimination: a global landscaping of system performance, 2015–2017. Malar J. (2019) 18:315. doi: 10.1186/s12936-019-2960-2
Keywords: malaria surveillance, active case detection, passive surveillance, annual blood examination rate (ABER), assessment of laboratory services
Citation: Kaur J, Baharia R and Dattani M (2024) Assessment of the quality of malaria surveillance and laboratory services for diagnosis in three districts of Gujarat state, India. Front. Public Health 12:1465228. doi: 10.3389/fpubh.2024.1465228
Received: 15 July 2024; Accepted: 23 October 2024;
Published: 15 November 2024.
Edited by:
C. P. Yadav, ICMR-National Institute of Cancer Prevention and Research, IndiaReviewed by:
Adilson José Depina, CCS-SIDA/MoH, Cabo VerdeAnuj Kumar, ICMR-National Institute of Cancer Prevention and Research, India
Kakoli Borkotoky, National Institute of Cancer Prevention and Research (ICMR), India
Copyright © 2024 Kaur, Baharia and Dattani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jaspreet Kaur, a2F1ci5qYXNwcmVldDA3MDhAZ21haWwuY29t; ZHJqYXNwcmVldC5rYXVyQGljbXIuZ292Lmlu
†These authors share first authorship
 Jaspreet Kaur
Jaspreet Kaur Rajendra Baharia2†
Rajendra Baharia2†