- 1Office of the Administrator, Centers for Medicare & Medicaid Services, Baltimore, MD, United States
- 2Department of Pediatric Dentistry, New York University College of Dentistry, New York, NY, United States
Introduction: There are ongoing concerns about opioid prescribing for surgical and non-surgical dental needs among adolescent/young adult and adult patients. Although there are known differences in the overall opioid prescription rates in rural areas compared to urban areas, the contribution of dental opioid prescriptions is still unclear. This study aims to examine the factors associated with receiving an opioid prescription following a dental visit.
Materials and methods: This cross-sectional study utilized the 2021 Centers for Medicare & Medicaid Services unredacted Transformed Medicaid Statistical Information System Analytic Files to examine Medicaid and CHIP adolescent/young adult beneficiaries aged 12–20 and adults aged 21–64 who are non-dually eligible for Medicare and had a dental visit in 2021. Multilevel logistic regression models were used to predict the odds of receiving a dental opioid prescription.
Results: The results of the adolescent/young adult models show that for every percentage point increase in the percentage of non-Hispanic Black residents in a county, the odds of receiving a dental opioid prescription increase by 0.8% in rural areas. However, with every percentage point increase in the Hispanic population, the odds of receiving a dental opioid prescription decrease by 0.3% in rural areas and 0.7% in urban areas. The adult models show that compared to non-Hispanic white beneficiaries, non-Hispanic Black beneficiaries are 8% more likely to receive a dental opioid prescription if they live in rural areas and 18% more likely if they live in urban areas, while all other racial and ethnic groups are significantly less likely to receive a dental opioid prescription. With every unit increase in the concentrated disadvantage index, the odds of receiving a dental opioid prescription increase by 17% among rural adults and 24% among urban adults.
Discussion: Our findings on rural–urban disparities in opioid prescriptions suggest that prescription patterns in dental settings are significant and inequitable across various beneficiary- and county-level factors and areas of residence. These variations in prescription patterns highlight the known disparities in access to preventive dental care and the need for targeted interventions to address the healthcare needs of rural residents.
Introduction
The overall rate of opioid prescribing in the United States (US) has steadily decreased since its peak in 2012 (1). Several initiatives, including prescription drug monitoring programs (PDMPs), clinical guidelines, and state opioid prescribing limits, have helped contribute to the overall decline in opioid prescriptions (2–5). Despite these efforts, opioid prescriptions remain elevated for specific populations and geographical areas, with prescription practices varying widely by practitioner specialty (6–9). While dentists typically prescribe opioids for analgesic purposes related to dental pain or after dental procedures such as tooth extraction or surgery, research and current guidelines now reflect that nonsteroidal anti-inflammatory drugs (NSAIDs) are more effective in a majority of cases (10, 11). Nevertheless, dentists remain one of the nation’s highest-prescribing healthcare specialties (12–14), second only to internal medicine (16.4%) (6). In particular, adolescent and young adult populations are significant recipients of dental opioid prescriptions (15). In 2009, dentists accounted for 31% of opioid prescriptions to children and adolescents aged 10 through 19 years (16). Moreover, from 2019 to 2015, the largest increase in dental opioid prescriptions was seen among 11 through 18 years olds (12). The effects of this are significant. Multiple studies have found that adolescents and young adults are often first exposed to opioids through dental providers and at increased risk for future opioid misuse and abuse (15, 17). Another study showed that adolescents and young adults receiving opioid prescriptions from dentists were at increased risk for subsequent substance-related morbidity (18). Additionally, studies have shown that dental-related prescriptions are often not fully used, which may increase the risk of opioid diversion and misuse of the leftover pills (19, 20).
Previous studies have primarily found higher overall opioid prescription rates in rural areas (21–23), but studies investigating dental opioid prescriptions have found no rural/urban differences (24, 25). However, these studies only examined oral maxillofacial surgeons (24, 25). Rural areas have been subject to many oral health challenges, with previous reports documenting higher rates of edentulism and poorer self-reported oral health scores for children (26, 27). In addition, there are several structural challenges that rural areas face, such as less access to dental care, higher rates of poverty, transportation difficulties, and lack of dental insurance (28, 29). Studies have identified similar structural challenges as reasons for higher opioid prescriptions and misuse in rural areas (30, 31).
Previous studies have explored provider-, procedure-, and beneficiary-specific factors associated with increased dental-related opioid prescriptions (15, 32–39). Studies examining beneficiary-level factors have found that higher opioid prescriptions differed by a wide variety of predictors. One study identified higher rates of opioid prescriptions among patients who were low-income, less educated, and insured by Medicaid (39). Other studies have reported that patients who are ‘young,’ ‘female,’ or ‘Non-Hispanic (NH) Black’ receive opioid prescriptions in dental settings at higher rates (15, 36–39). Further, several studies have investigated the complex interplay between beneficiary- and county-level factors within urban and rural settings and their associations with general opioid prescription rates (30, 31, 40, 41). However, to our knowledge, no studies examine the association between patient demographic factors, county characteristics, and dental opioid prescriptions. In addition, no studies explore how the association between patient demographic factors, county characteristics, and dental opioid prescriptions vary across urban and rural settings. This study aims to address these gaps in the literature by examining the factors associated with receiving a dental opioid prescription, considering both beneficiary and county characteristics. These characteristics will be examined separately for adolescents and adults, and how these characteristics differ across rural and urban areas will be considered.
Materials and methods
Data sources
This study utilized multiple data sources, including the 2021 Centers for Medicare & Medicaid Services (CMS) unredacted Transformed Medicaid Statistical Information System (T-MSIS) Analytic Files (TAF) Research Identifiable Files (RIF). Specifically, the Demographic and Eligibility, Other Services, and Pharmacy files were utilized and were accessed through the CMS Chronic Conditions Data Warehouse (CCW) (42). The American Dental Association (ADA) Dentist Data 2022 files were used to identify dental providers (43). The Economic Research Service Rural–Urban Commuting Area Codes were used to determine the rural/urban status of the beneficiary’s residence (44). This data was linked to the T-MSIS data using the beneficiary’s ZIP code. The US Census Bureau’s American Community Survey (ACS) 5-year (2008–2021) estimates were used to calculate the county characteristics measures (45). This data was linked to the T-MSIS data using the beneficiary’s Federal Information Processing Standard (FIPS) code. The study was covered by the Common Rule exemption, 45 CFR 46.104(d)(4)(iv), and did not require institutional review board review.
Cohort design and population
This study includes Medicaid and CHIP adolescent/young adult beneficiaries aged 12 to 20 and adults aged 21 to 64. All beneficiaries included in this study are non-dually eligible for Medicare. Beneficiaries must have had a dental visit in 2021. Beneficiaries are considered to have had a dental visit if they have a billed claim with any Code on Dental Procedures and Nomenclature (CDT code) for a dental procedure.
To be included in this study, beneficiaries must live in a state that does not need to be excluded for data quality concerns, according to the CMS DQ Atlas (46). States assigned as high concern or unusable on the following topics were excluded from all analyses: professional services claims volume, professional services procedure codes, prescription claims volume, prescription National Drug Codes (NDC), and linking claims to beneficiaries, resulting in beneficiaries from 9 states excluded from all analyses [Arkansas (AR), Florida (FL), Massachusetts (MA), Maine (ME), Minnesota (MN), Mississippi (MS), North Carolina (NC), New Jersey (NJ), and Utah (UT)] (46). Beneficiaries from 14 states are excluded due to race and ethnicity data quality concerns, 2 (MA and UT) of which were already excluded for claims data quality concerns [Arizona (AZ), Connecticut (CT), District of Columbia (DC), Hawaii (HI), Iowa (IA), Louisiana (LA), MA, New York (NY), Oregon (OR), Rhode Island (RI), South Carolina (SC), Tennes(see TN), UT, Wyoming (WY)] (46). Combining the claims data and race and ethnicity data quality exclusions, 21 states (AR, AZ, CT, DC, FL, HI, IA, LA, MA, ME, MN, MS, NC, NJ, NY, OR, RI, SC, TN, UT, WY) were excluded from all analyses stratified by race and ethnicity. After exclusions, 6,419,051 adolescent/young adult beneficiaries and 5,583,051 adult beneficiaries are included in the analyses that were not stratified by race and ethnicity, and a subset of 4,938,928 adolescent/young adult beneficiaries and 3,977,143 adult beneficiaries when stratified by race and ethnicity.
Outcome, demographic, and residential covariates
The outcome variable for this study is a dichotomous measure of whether a beneficiary received a dental opioid prescription. Opioid prescriptions were identified using NDC for prescriptions filled and paid by Medicaid, which are included in the pharmacy claims file. To be considered a dental opioid prescription, two requirements had to be met. First, the opioid had to be prescribed by a dental provider (a dental provider is defined as a dentist according to the ADA dentist data file (43) or as a provider with a dental taxonomy code according to the National Uniform Claim Committee’s (NUCC) Health Care Provider Taxonomy Code Set) (47). Second, the opioid prescription must have been filled within 7 days of a dental visit. To ensure that the opioid prescription is truly from a dental visit, all the beneficiary’s medical claims were also reviewed. If a provider billed for any medical visit or procedure and an opioid was prescribed within 7 days, the opioid prescription was excluded from the analysis. The reason for the exclusion is so that we can be extra confident that the opioid prescribed within 7 days of a dental visit did not come from a medical visit, which was also within 7 days of the dental visit.
This study includes beneficiary characteristics, including age, sex, race and ethnicity, as well as county characteristics, including rural/urban status, percentage of NH Black population, percentage of Hispanic population, concentrated disadvantage, and residential stability. Age is treated as a categorical variable using age 12–14 (reference group), age 15–17, and age 18–20. Sex is a categorical variable: male (reference group) and female. Race and ethnicity is treated as a categorical variable with the following racial/ethnic groups: American Indian/Alaskan Native (AI/AN), Asian/Pacific Islander (A/PI), Non-Hispanic (hereafter, NH) Black, Hispanic, NH White (reference group), and multiracial/other race/unknown race. Beneficiaries with missing race/ethnicity data are included in the multiracial/other race/unknown category. The percentage of NH Black and Hispanic population are continuous variables. Concentrated disadvantage is a continuous index variable calculated by applying principal components analysis to 5 variables from the ACS: logged median family income, unemployment rate, percentage of families headed by women, and percentage of the population receiving public assistance. All factor loadings are higher than 0.55, and this single factor accounts for 60 percent of the variance. Higher values suggest a higher concentrated disadvantage within the county. Residential stability is a continuous variable that is the average of two standardized indicators: the percentage of owner-occupied housing units and the percentage of households living in the same housing unit for at least 5 years. These county-level variables have been used in previous studies on opioid prescribing and opioid use disorder (41, 48–53).
Statistical analysis
The study population counts and rates per 1,000 Medicaid/CHIP beneficiaries who had a dental visit, as well as the opioid dental prescribing rate per 1,000 Medicaid/CHIP beneficiaries who had a dental visit, are presented for overall and by rural and urban status. Chi-square tests were used to test for significant differences in the rates across categories within each group, and whether the category-specific rates significantly differ across rural and urban areas. Multilevel logistic regression models were used to predict the odds of receiving a dental opioid prescription. The models include beneficiary characteristics in level-one and county characteristics in level-two. The county FIPS code is included in the models as a level-two random intercepts parameter to adjust for the similarity of beneficiaries residing within the same county. Separate multilevel logistic regression models were estimated for rural and urban beneficiaries. Wald tests were implemented to test whether the magnitude of the effects significantly differ across the rural and urban models. This approach is the equivalent of a full interaction model. Statistical significance was set at p ≤ 0.05; all p values were 2-tailed. Results are presented as adjusted odds ratios (aORs) and corresponding 95% confidence intervals (CI). Multicollinearity was assessed with variation inflation factors (VIF) and was identified in the models because no VIF were above 2. Analyses were conducted with SAS Enterprise Guide 7.1 and Stata 18.0 (54, 55). Maps were created with ESRI ArcGIS Pro 3.3.1 (56).
Results
Characteristics of study population and prevalence of opioid dental prescribing: adolescent/young adults
There are 6,419,051 adolescent/young adult beneficiaries in this study; of these, 2,756,216 (429 per 1,000) are 12–14 years old, followed by 2,291,730 (357 per 1,000) 15 to 17 years old (Table 1). There are more females (516 per 1,000) than males. Approximately one-third of adolescents and young adults are Hispanic (374 per 1,000), and another one-third are NH white (332 per 1,000).
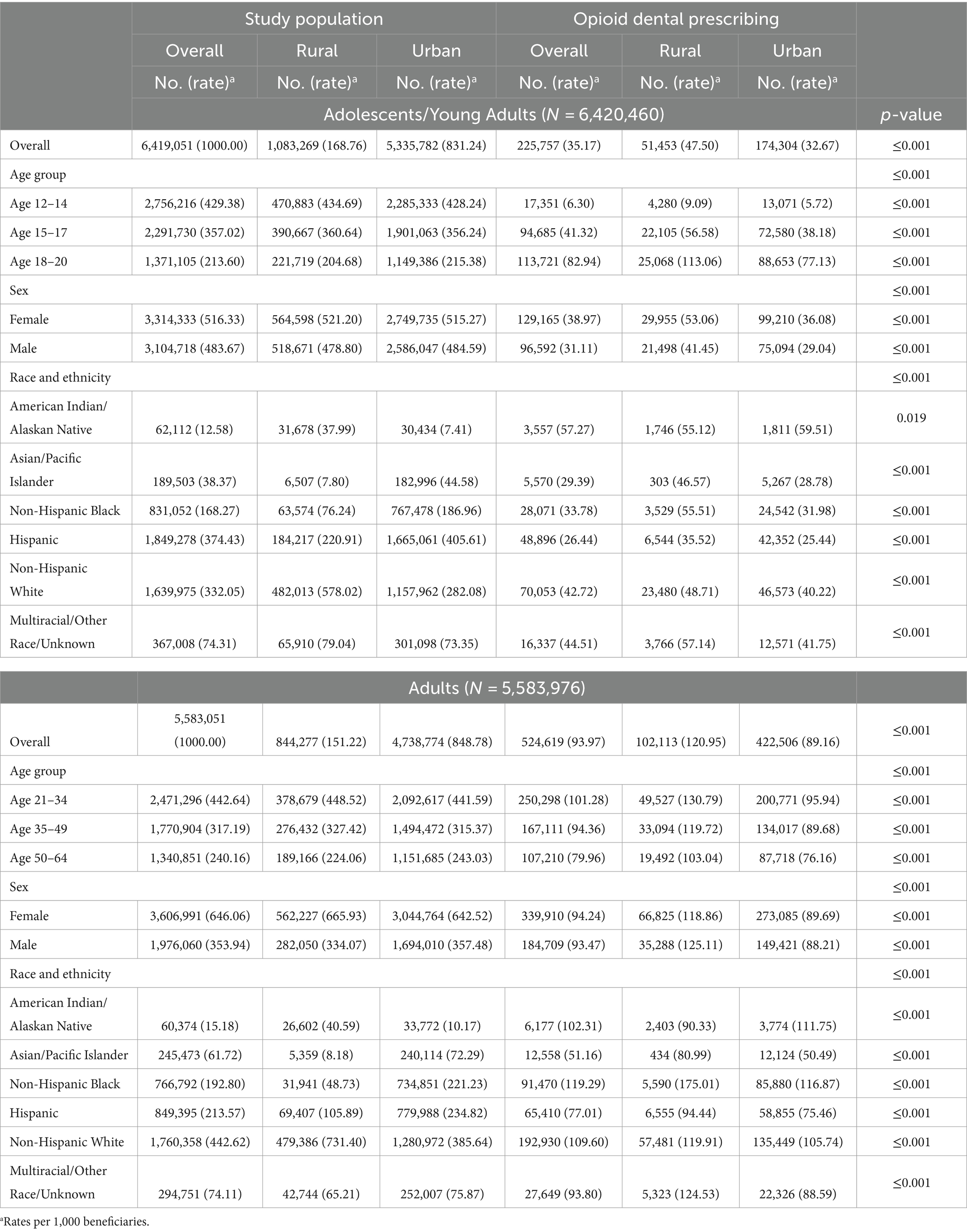
Table 1. Study population characteristics and opioid dental prescribing rates per 1,000 Medicaid/CHIP beneficiaries who had a dental visit, 2021.
Figures 1a–c display the rates of receiving a dental opioid prescription per 1,000 adolescent/young adult beneficiaries by state. The maps display the overall rate (Figure 1a), the rural rate (Figure 1b), and the urban rate (Figure 1c). The rates vary across states, with the lowest rate being 8 beneficiaries per 1,000 and the highest 96 beneficiaries per 1,000. The state-level rural rates are higher than the overall rates and urban rates.
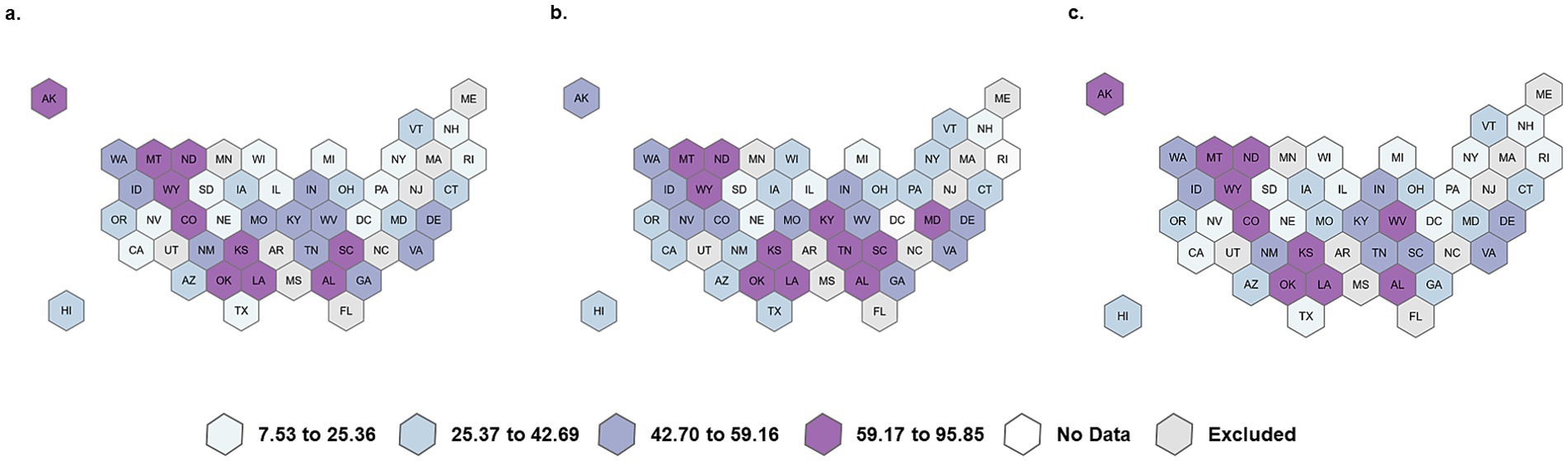
Figure 1. Overall, rural, and urban dental opioid prescribing rate per 1,000 adolescent/young adult Medicaid/CHIP beneficiaries. (a) Overall rate per 1,000, (b) Rural rate per 1,000, and (c) Urban rate per 1,000.
Table 1 shows the rates of opioid dental prescribing by age group, sex, and race and ethnicity, overall and by rural and urban status. The rates are significantly higher among older age groups (p ≤ 0.001). Among 12 to 14-year-olds, 6 beneficiaries per 1,000 received a dental opioid prescription compared to 41 beneficiaries per 1,000 for 15 to 17-year-olds and 83 per 1,000 for 18 to 20-year-olds. Among all age groups, the rates are significantly higher in rural areas compared to urban areas (p ≤ 0.001). For example, among beneficiaries 18 to 20 years of age, the rate is 113 per 1,000 in rural areas compared to 77 per 1,000 in urban areas.
Adolescent/young adult female beneficiaries have significantly higher dental opioid prescription rates than male beneficiaries, and these rates are significantly higher in rural areas than they are in urban areas (p ≤ 0.001). Among female beneficiaries living in rural areas, the rate is 53 per 1,000 compared to 36 per 1,000 for their urban counterparts. Among male beneficiaries, the rate is 41 per 1,000 in rural areas and 29 per 1,000 in urban areas.
The rates have statistically significant differences across all racial and ethnic groups. Looking at the overall rates, AI/AN beneficiaries have the highest rates at 57 beneficiaries per 1,000, followed by multiracial and other race beneficiaries at 45 per 1,000 and NH white beneficiaries at 43 per 1,000. Rural beneficiaries have higher rates than urban beneficiaries for every racial/ethnic group, except for AI/AN beneficiaries. In rural areas, the rates are highest among multiracial and other race beneficiaries at 57 per 1,000, followed by NH Black and AI/AN beneficiaries at 55 per 1,000. In urban areas, the rates are highest among AI/AN beneficiaries (60 per 1,000), followed by multiracial and other race beneficiaries (42 per 1,000) and NH white beneficiaries (40 per 1,000).
Characteristics of study population and prevalence of opioid dental prescribing: adults
There are 5,583,051 adult beneficiaries in this study; of these, 2,471,296 (443 per 1,000) are 21–34 years old, followed by 1,770,904 (317 per 1,000) 35–49 years old (Table 1). There are more females (646 per 1,000) than males. Almost half of the adults are NH white (443 per 1,000), followed by Hispanic (214 per 1,000) and NH Black (193 per 1,000). The dental opioid prescribing rates among adults are shown in Figures 2a–c. Among adult beneficiaries, the state-level rates vary from 23 per 1,000 to 347 per 1,000. States with the highest rates are generally located in the South and Southwest.
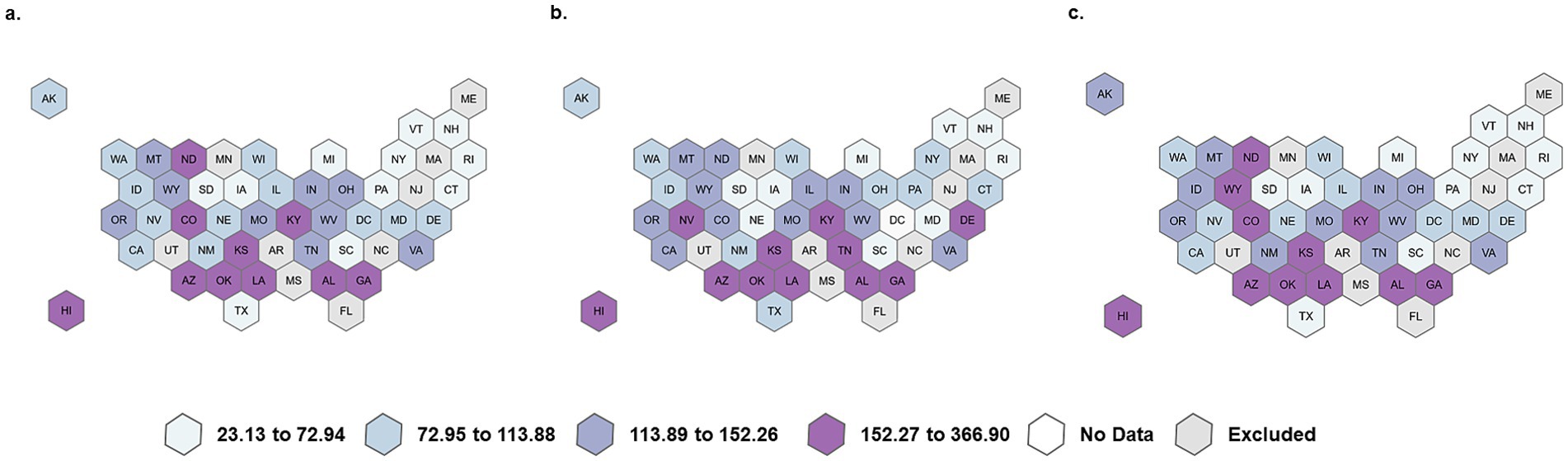
Figure 2. Overall, rural, and urban dental opioid prescribing rate per 1,000 adult Medicaid beneficiaries. (a) Overall rate per 1,000, (b) Rural rate per 1,000, (c) Urban rate per 1,000.
Among adult beneficiaries, the rates significantly decrease with each older age group. Beneficiaries aged 21 to 34 who live in rural areas have the highest dental opioid prescription rates at 131 per 1,000 beneficiaries. Among adults in general and adults living in urban areas, the rates of receiving a dental opioid prescription are higher for females than males. However, among adults living in rural areas, the rates of receiving a dental opioid prescription are significantly higher for males (125 per 1,000) than they are for females (119 per 1,000).
While AI/AN beneficiaries were the racial/ethnic group with the highest overall rates of dental opioid prescriptions for adolescent/young adult beneficiaries, among adults, NH Black beneficiaries have the highest rates (119 per 1,000). As was the case for adolescent/young adult beneficiaries, adult beneficiaries have higher rates in rural areas than in urban areas for every racial and ethnic group, except for AI/AN beneficiaries. In rural areas, the rates are highest among NH Black beneficiaries (175 per 1,000), followed by multiracial and other race beneficiaries at 125 per 1,000, and NH white beneficiaries at 120 per 1,000. In urban areas, the rates are highest among NH Black beneficiaries (117 per 1,000), followed by AI/AN beneficiaries at 112 per 1,000 and NH White beneficiaries (106 per 1,000).
Characteristics associated with receiving a dental opioid prescription: adolescent/young adults
The multilevel logistic regression model results are reported in Table 2. As shown in the adolescent/young adult models, compared to beneficiaries aged 12–14, beneficiaries aged 15–17 are 6.80 times (aOR, 6.80; 95% CI, 6.55–7.06) more likely to receive a dental opioid prescription if they live in a rural area and 7.22 times (aOr, 7.22; 95% CI, 7.06–7.37) more likely if they live in an urban area. Beneficiaries 18 to 20 years old are 14.59 times (aOR, 14.59; CI, 14.04–15.16) more likely to receive a dental opioid prescription compared to beneficiaries aged 12–14 if they live in a rural area and 15.95 times (aOR, 15.95; CI, 15.61–16.29) more likely if they live in an urban area. The odds of receiving a dental opioid prescription are 19% higher for females than they are for males among beneficiaries living in rural areas and 16% higher for females compared to males among beneficiaries living in urban areas. Among rural adolescent/young adult beneficiaries, the odds of receiving a dental opioid prescription are 21% lower for Hispanic beneficiaries compared to NH white beneficiaries. Among urban beneficiaries, when compared to NH white beneficiaries, all racial and ethnic groups are significantly less likely to receive a dental opioid prescription, except for AI/AN beneficiaries whose odds of receiving a dental opioid prescription are not significantly different from NH whites.
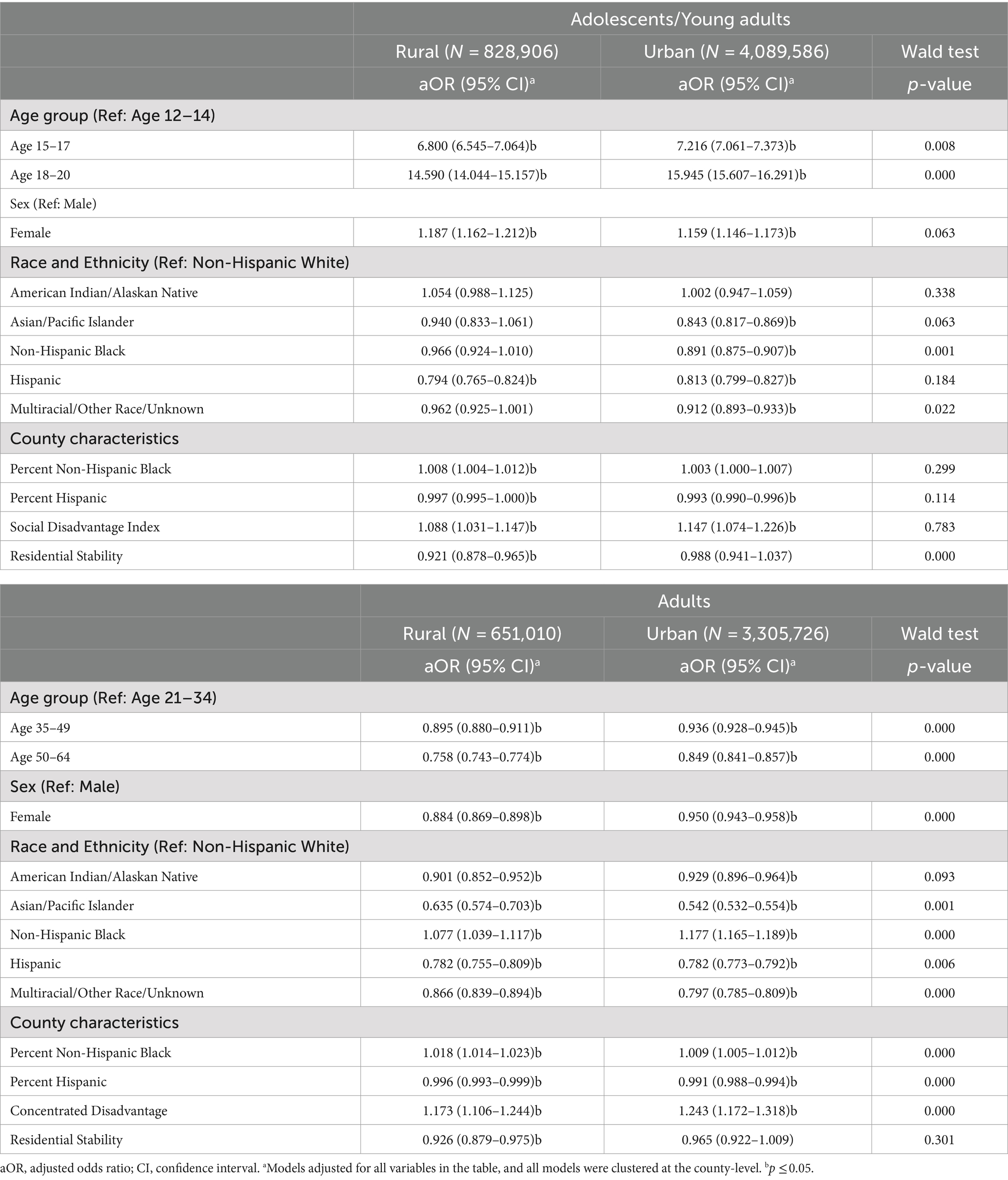
Table 2. Multilevel logistic regression model predicting the odds of receiving a dental opioid prescription among Medicaid/CHIP beneficiaries who had a dental visit, 2021.
As for the county characteristics, for every percentage point increase in the percentage of NH Black residents, the odds of receiving a dental opioid prescription increase by 0.8% in rural areas. However, with every percentage point increase in the Hispanic population, the odds of receiving a dental opioid prescription decrease by 0.3% in rural areas and 0.7% in urban areas. With every unit increase in the concentrated disadvantage index, the odds of receiving a dental opioid prescription increase by 9% in rural areas and 15% in urban areas. In rural areas, adolescents and young adults who live in counties with more residential stability have 8% lower odds of receiving a dental opioid prescription.
Characteristics associated with receiving a dental opioid prescription: adults
As shown in the adult rural and urban models, compared to adults aged 21 to 34, older beneficiaries are significantly less likely to receive a dental opioid prescription. Adult female beneficiaries are significantly less likely to receive a dental opioid prescription compared to males, and the odds are significantly lower for females living in rural areas (12%) than in urban areas (5%). The relationship between race and ethnicity and receiving a dental opioid prescription was different for adults than it was for adolescents and young adults. Among adults, compared to NH white beneficiaries, all racial and ethnic groups are significantly less likely to receive a dental opioid prescription except for NH Black beneficiaries, who are 8% more likely to receive a dental opioid prescription if they live in rural areas and 18% more likely if they live in urban areas.
The county characteristics results show similar patterns for adolescent/young adult beneficiaries. However, the effect of concentrated disadvantage is much stronger for adult beneficiaries. With every unit increase in the concentrated disadvantage index, the odds of receiving a dental opioid prescription increase by 17% among rural adults and 24% among urban adults.
Discussion
This study revealed that the relationship between age and the rate of beneficiaries receiving a dental opioid prescription is an inverted U-shape. The rates among adolescent/young adult beneficiaries increased with each age group, and among adult beneficiaries, the rates decreased with each age group. We also discover that racial disparities are age-dependent, with AI/AN adolescents/young adults and NH Black adults having the highest overall dental opioid prescription rates. Previous studies have primarily reported that patients who are NH white or NH Black have the highest opioid prescription rates (15, 36–39). Still, these studies did not analyze racial disparities by age group or include AI/AN beneficiaries in the analyses.
The finding that AI/AN adolescent/young adult beneficiaries have the highest dental opioid prescription rates highlights the alarming trend around the over-prescribing of opioids to AI/AN children that should be further explored. Almost half of AI/AN children live in dental care shortage areas, which can hinder access to regular and routine dental visits. Without periodic visits and early intervention, the progression of the disease can eventually lead to severe dental pain. If treatment can be rendered, follow-up appointments may still be challenging. While guidelines have demonstrated that NSAIDs are equally effective in managing dental pain, dental providers may still choose to prescribe opioids as a precautionary measure (57–59). Future investigations into dental opioid prescribing in AI/AN populations can better inform prescribing policies. They may also provide more insight into needed changes in the oral health care delivery system for AI/AN patients to decrease the need for analgesic prescriptions overall. Despite having the highest opioid prescription rates among adolescents/young adults, we did not find that AI/AN adolescent/young adults were significantly more likely to receive an opioid than their NH white counterparts, which previous studies for both general and dental opioid prescriptions concluded as well (60, 61).
Previous studies have primarily shown that overall opioid prescription rates are higher in rural areas (21–23). Our findings reveal higher dental opioid prescription rates in rural areas as well as provide additional perspective by demonstrating that the likelihood of receiving a dental opioid prescription in an urban vs. rural setting can significantly vary depending on beneficiary-level factors such as sex, age, and race and ethnicity. For example, among adolescents/young adults, the likelihood of receiving a dental opioid prescription was significantly lower among NH Black and multiracial/other race beneficiaries in urban areas than it was in rural areas. Among adults, the likelihood of receiving a dental opioid prescription was significantly higher among NH Black urban adults than it was for NH Black rural adults. It is beyond the scope of our study to explore causative drivers for these differences. Still, our findings confirm that the rurality or urbanicity of residence cannot solely predict the odds of receiving a dental opioid prescription and that beneficiary-level characteristics also need to be considered. These findings suggest that successfully addressing disparities in dental opioid prescribing must be sensitive to both individuals and their surrounding environment (62).
County-level predictors showed consistent effects across both adolescents/young adults and adults, but opposite effects were observed between areas with a higher percentage of NH Black residents (higher odds) and a higher percentage of Hispanic residents (lower odds); this finding suggests that race and ethnicity are not only significant at a beneficiary-level but also at a population level. Several studies have attributed racial disparities in opioid prescription patterns to factors such as providers’ conscious and unconscious racial biases as well as systemic structural racism such as segregated neighborhoods and lower density of healthcare providers (36, 63, 64). Our findings may reflect the broader impact these collective biases and disparities can have on entire communities’ dental and medical services access. When considering the impact of county-level factors, we found that residential stability is protective in rural areas for both adolescents/young adults and adults. Studies have shown that residential stability is more common in rural settings and has better health outcomes mediated by communal benefits such as greater social cohesion and community support (65–67). Our findings suggest that these social benefits may also facilitate a lower likelihood of receiving a dental opioid prescription. Yang et al. hypothesized that increased residential stability may not only decrease patient demand for opioids but may also disincentivize providers from prescribing opioids in these communities due to stronger communal ties (41). Future studies that further identify and investigate unique urban and rural characteristics that influence opioid prescribing may help better guide local and community-based initiatives seeking to curb the over-prescribing of opioids in dental settings.
Limitations
Our study has some noted limitations. First, our findings only account for Medicaid/CHIP beneficiaries and may not be generalizable to the US population. Future studies may investigate these disparities in the commercially insured and uninsured populations. Second, although our primary measure focused on whether a beneficiary was prescribed opioids, we did not consider other important aspects of opioid prescribing, such as the morphine milligram equivalents and the number of days supplied. Third, we are limited to the variables included in Medicaid administrative claims data, which could result in omitted variable bias.
Conclusion
Our findings on rural–urban disparities in dental opioid prescribing suggest that prescription patterns in dental settings are significant and inequitable across various beneficiary- and county-level factors as well as residence. These variations in prescription patterns indicate that there is not one solution that can address the disparities in opioid prescribing; in fact, developing interventions and policies that have identified targeted factors that account for the local populations and community structure may provide a more productive strategy that acknowledges the complex nature of the opioid crisis.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: this data is available through a signed data use agreement with the Centers for Medicare & Medicaid Services. Requests to access these datasets should be directed to https://www2.ccwdata.org/web/guest/home/.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
CS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. AS: Writing – original draft, Writing – review & editing. LQ: Data curation, Formal analysis, Methodology, Writing – review & editing. NC: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
CS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed in this article are those of the authors. No official endorsement by the Department of Health and Human Services, Centers for Medicare & Medicaid Services (CMS), or New York University College of Dentistry is intended or should be inferred.
References
1. U.S. Opioid Dispensing Rate Maps. Centers for Disease Control and Prevention (2021). Available at: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html. (Accessed January 15, 2024).
2. Dowell, D, Ragan, KR, Jones, CM, Baldwin, GT, and Chou, R. CDC clinical practice guideline for prescribing opioids for pain - United States, 2022. MMWR Recomm Rep. (2022) 71:1–95. doi: 10.15585/mmwr.rr7103a1
3. Townsend, T, Cerda, M, Bohnert, A, Lagisetty, P, and Haffajee, RL. CDC guideline for opioid prescribing associated with reduced dispensing to certain patients with chronic pain. Health Aff. (2021) 40:1766–75. doi: 10.1377/hlthaff.2021.00135
4. Prescription Drug Monitoring Programs (PDMPs). Centers for Disease Control and Prevention: 11/14.Available from: https://www.cdc.gov/drugoverdose/pdmp/index.html. (Accessed November 14, 2023).
5. Chua, KP, Nguyen, TD, Waljee, JF, Nalliah, RP, and Brummett, CM. Association between state opioid prescribing limits and duration of opioid prescriptions from dentists. JAMA Netw Open. (2023) 6:e2250409. doi: 10.1001/jamanetworkopen.2022.50409
6. Guy, GP, and Zhang, K. Opioid prescribing by specialty and volume in the U.S. Am J Prev Med. (2018) 55:e153–5. doi: 10.1016/j.amepre.2018.06.008
7. Khouja, T, Shah, NH, Suda, KJ, and Polk, DE. Trajectories of opioid prescribing by general dentists, specialists, and oral and maxillofacial surgeons in the United States, 2015-2019. J Am Dent Assoc. (2024) 155:7–16.e7. doi: 10.1016/j.adaj.2023.10.002
8. Olfson, M, Wang, S, Wall, MM, and Blanco, C. Trends in opioid prescribing and self-reported pain among US adults. Health Aff. (2020) 39:146–54. doi: 10.1377/hlthaff.2019.00783
9. Renny, MH, Yin, HS, Jent, V, Hadland, SE, and Cerdá, M. Temporal trends in opioid prescribing practices in children, adolescents, and younger adults in the US from 2006 to 2018. JAMA Pediatr. (2021) 175:1043–52. doi: 10.1001/jamapediatrics.2021.1832
10. Carrasco-Labra, A, Polk, DE, Urquhart, O, Aghaloo, T, Claytor, JW Jr, Dhar, V, et al. Evidence-based clinical practice guideline for the pharmacologic management of acute dental pain in adolescents, adults, and older adults: a report from the American dental association science and research institute, the University of Pittsburgh, and the University of Pennsylvania. J Am Dent Assoc. (2024) 155:102–117.e9. doi: 10.1016/j.adaj.2023.10.009
11. Thornhill, MH, Suda, KJ, Durkin, MJ, and Lockhart, PB. Is it time US dentistry ended its opioid dependence? J Am Dent Assoc. (2019) 150:883–9. doi: 10.1016/j.adaj.2019.07.003
12. Gupta, N, Vujicic, M, and Blatz, A. Opioid prescribing practices from 2010 through 2015 among dentists in the United States: what do claims data tell us? J Am Dent Assoc. (2018) 149:237–245.e6. doi: 10.1016/j.adaj.2018.01.005
13. Okunev, I, Frantsve-Hawley, J, and Tranby, E. Trends in national opioid prescribing for dental procedures among patients enrolled in Medicaid. J Am Dent Assoc. (2021) 152:622–630.e3. doi: 10.1016/j.adaj.2021.04.013
14. Zhang, J, Nalliah, RP, Waljee, JF, Brummett, CM, and Chua, KP. Association between the COVID-19 outbreak and opioid prescribing by U.S. dentists. PLoS One. (2023) 18:e0293621. doi: 10.1371/journal.pone.0293621
15. Schroeder, AR, Dehghan, M, Newman, TB, Bentley, JP, and Park, KT. Association of Opioid Prescriptions from Dental Clinicians for US adolescents and Young adults with subsequent opioid use and abuse. JAMA Intern Med. (2019) 179:145–52. doi: 10.1001/jamainternmed.2018.5419
16. Volkow, ND, McLellan, TA, Cotto, JH, Karithanom, M, and Weiss, SR. Characteristics of opioid prescriptions in 2009. JAMA. (2011) 305:1299–301. doi: 10.1001/jama.2011.401
17. Gupta, N, Vujicic, M, and Blatz, A. Multiple opioid prescriptions among privately insured dental patients in the United States: evidence from claims data. J Am Dent Assoc. (2018) 149:619–627.e1. doi: 10.1016/j.adaj.2018.02.025
18. Quinn, PD, Fine, KL, Rickert, ME, Sujan, AC, Boersma, K, Chang, Z, et al. Association of Opioid Prescription Initiation during Adolescence and Young Adulthood with Subsequent Substance-Related Morbidity. JAMA Pediatr. (2020) 174:1048–55. doi: 10.1001/jamapediatrics.2020.2539
19. Maughan, BC, Hersh, EV, Shofer, FS, Wanner, KJ, Archer, E, Carrasco, LR, et al. Unused opioid analgesics and drug disposal following outpatient dental surgery: a randomized controlled trial. Drug Alcohol Depend. (2016) 168:328–34. doi: 10.1016/j.drugalcdep.2016.08.016
20. McCabe, SE, West, BT, and Boyd, CJ. Leftover prescription opioids and nonmedical use among high school seniors: a multi-cohort national study. J Adolesc Health. (2013) 52:480–5. doi: 10.1016/j.jadohealth.2012.08.007
21. Garcia, MC, Heilig, CM, Lee, SH, Faul, M, Guy, G, Iademarco, MF, et al. Opioid prescribing rates in nonmetropolitan and metropolitan counties among primary care providers using an electronic health record system - United States, 2014-2017. MMWR Morb Mortal Wkly Rep. (2019) 68:25–30. doi: 10.15585/mmwr.mm6802a1
22. Heins, SE, Sorbero, MJ, Jones, CM, Dick, AW, and Stein, BD. High-risk prescribing to Medicaid enrollees receiving opioid analgesics: individual- and county-level factors. Subst Use Misuse. (2018) 53:1591–601. doi: 10.1080/10826084.2017.1416407
23. Prunuske, JP, St Hill, CA, Hager, KD, Lemieux, AM, Swanoski, MT, Anderson, GW, et al. Opioid prescribing patterns for non-malignant chronic pain for rural versus non-rural US adults: a population-based study using 2010 NAMCS data. BMC Health Serv Res. (2014) 14:563. doi: 10.1186/s12913-014-0563-8
24. Wang, TT, Nadella, S, Lee, CC, Hersh, EV, Tannyhill, RJ, and Panchal, N. Do patterns of opioid prescriptions to Medicare beneficiaries differ between Oral and maxillofacial surgeons practicing in urban and rural settings? J Oral Maxillofac Surg. (2022) 80:614–9. doi: 10.1016/j.joms.2021.10.018
25. Wang, TT, Chan, E, Lee, CC, Williams, RA, Young, LD, Keith, DA, et al. Are there differences in opioid prescriptions to urban and rural patients by Oral and maxillofacial surgeons in Massachusetts from 2011 to 2021? J Oral Maxillofac Surg. (2023) 81:831–7. doi: 10.1016/j.joms.2023.03.004
26. Mitchell, J, Bennett, K, and Brock-Martin, A. Edentulism in high poverty rural counties. J Rural Health. (2013) 29:30–8. doi: 10.1111/j.1748-0361.2012.00440.x
27. Crouch, E, Nelson, J, Merrell, MA, and Martin, A. The oral health status of America's rural children: an opportunity for policy change. J Public Health Dent. (2021) 81:251–60. doi: 10.1111/jphd.12444
28. Oral health in rural communities. Rural Health Information Hub: 11/15. (2022). Available at: https://www.ruralhealthinfo.org/topics/oral-health.
29. Musgrove, R. Improving Oral health Care Services in Rural America. Services NACoRHaH, (2018). Available at: https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/2018-oral-health-policy-brief.pdf. (Accessed February 15, 2024).
30. Luu, H, Slavova, S, Freeman, PR, Lofwall, M, Browning, S, and Bush, H. Trends and patterns of opioid analgesic prescribing: regional and rural-urban variations in Kentucky from 2012 to 2015. J Rural Health. (2019) 35:97–107. doi: 10.1111/jrh.12300
31. Monnat, SM, and Rigg, KK. Examining rural/urban differences in prescription opioid misuse among US adolescents. J Rural Health. (2016) 32:204–18. doi: 10.1111/jrh.12141
32. Chua, KP, Waljee, JF, Gunaseelan, V, Nalliah, RP, and Brummett, CM. Distribution of opioid prescribing and high-risk prescribing among U.S. dentists in 2019. Am J Prev Med. (2022) 62:317–25. doi: 10.1016/j.amepre.2021.09.017
33. Obadan-Udoh, E, Lupulescu-Mann, N, Charlesworth, CJ, Muench, U, Jura, M, Kim, H, et al. Opioid prescribing patterns after dental visits among beneficiaries of Medicaid in Washington state in 2014 and 2015. J Am Dent Assoc. (2019) 150:259–268.e1. doi: 10.1016/j.adaj.2018.12.030
34. Chua, KP, Hu, HM, Waljee, JF, Brummett, CM, and Nalliah, RP. Opioid prescribing patterns by dental procedure among US publicly and privately insured patients, 2013 through 2018. J Am Dent Assoc. (2021) 152:309–17. doi: 10.1016/j.adaj.2021.01.001
35. Yan, CH, Lee, TA, Sharp, LK, Hubbard, CC, Evans, CT, Calip, GS, et al. Trends in opioid prescribing by general dentists and dental specialists in the U.S., 2012-2019. Am J Prev Med. (2022) 63:3–12. doi: 10.1016/j.amepre.2022.01.009
36. Janakiram, C, Chalmers, NI, Fontelo, P, Huser, V, Lopez Mitnik, G, Iafolla, TJ, et al. Sex and race or ethnicity disparities in opioid prescriptions for dental diagnoses among patients receiving Medicaid. J Am Dent Assoc. (2018) 149:246–55. doi: 10.1016/j.adaj.2018.02.010
37. Lutfiyya, MN, Gross, AJ, Schvaneveldt, N, Woo, A, and Lipsky, MS. A scoping review exploring the opioid prescribing practices of US dental professionals. J Am Dent Assoc. (2018) 149:1011–23. doi: 10.1016/j.adaj.2018.07.017
38. Rindal, DB, Asche, SE, Kane, S, Truitt, AR, Worley, DC, Davin, LM, et al. Patient, provider type, and procedure type factors associated with opioid prescribing by dentists in a health care system. J Pain Res. (2021) 14:3309–19. doi: 10.2147/JPR.S330598
39. Steinmetz, CN, Zheng, C, Okunseri, E, Szabo, A, and Okunseri, C. Opioid analgesic prescribing practices of dental professionals in the United States. JDR Clin Trans Res. (2017) 2:241–8. doi: 10.1177/2380084417693826
40. Shoff, C, Yang, TC, and Kim, S. Rural/urban differences in the predictors of opioid prescribing rates among Medicare part D beneficiaries 65 years of age and older. J Rural Health. (2021) 37:5–15. doi: 10.1111/jrh.12497
41. Yang, TC, Kim, S, and Shoff, C. Income inequality and opioid prescribing rates: exploring rural/urban differences in pathways via residential stability and social isolation. Rural Sociol. (2021) 86:26–49. doi: 10.1111/ruso.12338
42. Chronic Conditions Data Warehouse (CCW). CCW t-MSIS TAF FRIP. Available at: https://www2.ccwdata.org/documents/10280/19002246/ccw-taf-rif-user-guide.pdf. (Accessed January 15, 2024).
43. American Dental Association. American dental association dentist data. Health Policy Institute. (2022)
45. U.S. Census Bureau. American community survey 5-Year County estimates 2016–2020 (2020). Available at: https://www.census.gov/data/developers/data-sets/acs-5year.2020.html#list-tab-1036221584. (Accessed January 15, 2024).
46. Centers for Medicare and Medicaid Services. DQ atlas. Medicaid and CHIP business information Solutions (2023). Available at: https://www.medicaid.gov/dq-atlas/welcome. (Accessed January 15, 2024).
47. National Uniform Claim Committee. Health care provider taxonomy code set. (2024). Available at: https://taxonomy.nucc.org/. (Accessed January 15, 2024).
48. Jones, CM, Shoff, C, Blanco, C, Losby, JL, Ling, SM, and Compton, WM. Overdose, behavioral health services, and medications for opioid use disorder after a nonfatal overdose. JAMA Intern Med. (2024) 184:954–62. doi: 10.1001/jamainternmed.2024.1733
49. Yang, T-C, Kim, S, Matthews, SA, and Shoff, C. Social vulnerability and the prevalence of opioid use disorder among older Medicare beneficiaries in U.S Counties. J Gerontol. (2023) 78:2111–21. doi: 10.1093/geronb/gbad146
50. Yang, T-C, Shoff, C, S-wE, C, and Sun, F. Multiscale dimensions of county-level disparities in opioid use disorder rates among older Medicare beneficiaries. Front Public Health. (2022) 10:993507. doi: 10.3389/fpubh.2022.993507
51. Yang, T-C, Shoff, C, and Kim, S. Social isolation, residential stability, and opioid use disorder among older Medicare beneficiaries: metropolitan and non-metropolitan county comparison. Soc Sci Med. (2022) 292:114605. doi: 10.1016/j.socscimed.2021.114605
52. Yang, T-C, Shoff, C, Kim, S, and Shaw, BA. County social isolation and opioid use disorder among older adults: a longitudinal analysis of Medicare data, 2013–2018. Soc Sci Med. (2022) 301:114971. doi: 10.1016/j.socscimed.2022.114971
53. Yang, T-C, Shoff, C, Shaw, BA, and Strully, K. Neighborhood characteristics and opioid use disorder among older Medicare beneficiaries: an examination of the role of the COVID-19 pandemic. Health Place. (2023) 79:102941. doi: 10.1016/j.healthplace.2022.102941
57. Moore, PA, Dionne, RA, Cooper, SA, and Hersh, EV. Why do we prescribe Vicodin? J Am Dent Assoc. (2016) 147:530–3. doi: 10.1016/j.adaj.2016.05.005
58. Moore, PA, and Hersh, EV. Just-in-case opioid prescribing. J Dent Educ. (2020) 84:1327–8. doi: 10.1002/jdd.12500
59. Carrasco-Labra, A, Polk, DE, Urquhart, O, Aghaloo, T, Claytor, JW Jr, Dhar, V, et al. Evidence-based clinical practice guideline for the pharmacologic management of acute dental pain in children: a report from the American dental association science and research institute, the University of Pittsburgh School of dental medicine, and the Center for Integrative Global Oral Health at the University of Pennsylvania. J Am Dent Assoc. (2023) 154:814–825 e2. doi: 10.1016/j.adaj.2023.06.014
60. Banks, J, Hill, C, and Chi, DL. Plan type and opioid prescriptions for children in Medicaid. Med Care. (2021) 59:386–92. doi: 10.1097/MLR.0000000000001504
61. Groenewald, CB, Rabbitts, JA, Hansen, EE, and Palermo, TM. Racial differences in opioid prescribing for children in the United States. Pain. (2018) 159:2050–7. doi: 10.1097/j.pain.0000000000001290
62. Jalali, MS, Botticelli, M, Hwang, RC, Koh, HK, and McHugh, RK. The opioid crisis: a contextual, social-ecological framework. Health Res Policy Syst. (2020) 18:87. doi: 10.1186/s12961-020-00596-8
63. Morden, NE, Chyn, D, Wood, A, and Meara, E. Racial inequality in prescription opioid receipt - role of individual health systems. N Engl J Med. (2021) 385:342–51. doi: 10.1056/NEJMsa2034159
64. Burgess, DJ, van Ryn, M, Crowley-Matoka, M, and Malat, J. Understanding the provider contribution to race/ethnicity disparities in pain treatment: insights from dual process models of stereotyping. Pain Med. (2006) 7:119–34. doi: 10.1111/j.1526-4637.2006.00105.x
65. Bures, RM. Childhood residential stability and health at midlife. Am J Public Health. (2003) 93:1144–8. doi: 10.2105/AJPH.93.7.1144
66. Swope, CB, and Hernandez, D. Housing as a determinant of health equity: a conceptual model. Soc Sci Med. (2019) 243:112571. doi: 10.1016/j.socscimed.2019.112571
67. Henning-Smith, C, Tuttle, M, Swendener, A, Lahr, M, and Yam, H. Differences in residential stability by rural/urban location and socio-demographic characteristics. August 2023. UMN Rural Health Research Center Policy Brief. 1–6. Available at: https://rhrc.umn.edu/wp-content/uploads/2023/07/UMN-Policy-Brief_residential-stability_8.2.pdf
Keywords: dental, opioid, prescribing, oral health, prescription, rural, urban, Medicaid
Citation: Shoff C, Sheen A, Qu L and Chalmers NI (2024) Rural–urban differences in dental opioid prescribing among adolescent/young adult and adult Medicaid beneficiaries. Front. Public Health. 12:1465206. doi: 10.3389/fpubh.2024.1465206
Edited by:
Tamanna Tiwari, University of Colorado Denver, United StatesReviewed by:
Naiya Patel, University of Louisville, United StatesHeather Taylor, Indiana University–Purdue University Indianapolis, United States
Copyright © 2024 Shoff, Sheen, Qu and Chalmers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Natalia I. Chalmers, TmF0YWxpYS5DaGFsbWVyczFAY21zLmhocy5nb3Y=
 Carla Shoff
Carla Shoff Alex Sheen
Alex Sheen Luping Qu
Luping Qu Natalia I. Chalmers
Natalia I. Chalmers