- 1College of Sports, Nanjing Tech University, Nanjing, China
- 2School of Athletic Performance, Shanghai University of Sport, Shanghai, China
Objective: The 2-fold objective of this research is to investigate machine learning's (ML) predictive value for the incidence of depression among China's older adult population and to determine the noteworthy aspects resulting in depression.
Methods: This research selected 7,880 older adult people by utilizing data from the 2020 China Health and Retirement Longitudinal Study. Thereafter, the dataset was classified into training and testing sets at a 6:4 ratio. Six ML algorithms, namely, logistic regression, k-nearest neighbors, support vector machine, decision tree, LightGBM, and random forest, were used in constructing a predictive model for depression among the older adult. To compare the differences in the ROC curves of the different models, the Delong test was conducted. Meanwhile, to evaluate the models' performance, this research performed decision curve analysis (DCA). Thereafter, the Shapely Additive exPlanations values were utilized for model interpretation on the bases of the prediction results' substantial contributions.
Results: The range of the area under the curve (AUC) of each model's ROC curves was 0.648–0.738, with significant differences (P < 0.01). The DCA results indicate that within various probability thresholds, LightGBM's net benefit was the highest. Self-rated health, nighttime sleep, gender, age, and cognitive function are the five most important characteristics of all models in terms of predicting the occurrence of depression.
Conclusion: The occurrence of depression among China's older adult population and the critical factors leading to depression can be predicted and identified, respectively, by ML algorithms.
Introduction
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) defines depression as a persistent state of low mood accompanied by various psychological and physiological symptoms, significantly impairing an individual's daily functioning. Among the older adult, depression is a typical and serious issue concerning mental health (1). Given that about 300 million people globally are affected by depression, this condition is among the general population's most common mental illnesses and in the top three of the causes of disability (2, 3). In terms of global disease burden, the projection is that depression will be ranked first by 2023 (3). According to accumulating evidence, depression among the older adult is suggested to be a potential risk factor for the start of diseases related to aging, including dementia, cardiovascular, and metabolic diseases (4, 5). Depression that is mild and severe are substantially related with considerably high rates of suicide (6, 7), low-quality life (8), high death rates (9), and an increase in the cost of health care (8). In addition, inadequacy in treating depression among the older adult has been observed (10, 11). Although depression is viewed to be typically related to aging, concerns have been raised whether or not treatments for depression are effective (12). In 2021, a mere 0.5% of patients in China suffering from depression received sufficient treatment, according to the China Mental Health Survey (13). To identify high-risk people and implement appropriate early interventions, a crucial undertaking is risk prediction for depression (14). Therefore, preventing and treating depression among the older adult necessitate the identification of the characteristics and risk factors of this condition.
Machine learning (ML) has achieved critical developments in recent years, particularly in mental health diagnosis (15). ML is a crucial computer science branch, the objective of which is the performance improvement of a variety of tasks (e.g., prediction) via pattern extraction from data. To comprehend the mental disorder properties and the related risk and prognostic factors, researchers in clinical psychology and psychiatry are extensively performing wide-ranging and varied evaluations, including self-report measures, physiological factors, and imaging data. Current datasets normally comprise thousands of measurements often gathered frequently over time. ML methods can be utilized for complex data structures, thereby enabling an improved understanding and conceptualization of mental disorders, detection and prediction of symptoms' risk and trajectory, and investigation of outcomes of treatments and differential treatment responses. A research conducted data gathering from 1,617 participants in the China Health and Retirement Longitudinal Study (CHARLS) registry from 2011 to 2018, using three data balancing techniques and four ML algorithms to build predictive models for classifying depression prognosis (16). In another research, depression-related data were used from 2,548 home-dwelling Chinese older adult individuals in CHARLS (2011–2018); depression outcomes were estimated by utilizing three ML classification algorithms: gradient boosting decision tree (DT), support vector machine (SVM), and random forest (RF) (17). Even though prior research has developed models on depression risk prediction by utilizing longitudinal questionnaire data, information obtained in previous studies were gathered pre-COVID-19 pandemic (18). Evidently, society had been severely impacted by the pandemic, including the people's lifestyle and health status. According to studies, a correlation exists between the COVID-19 pandemic and an increase in depression symptoms (19, 20). A research conducted regarding the occurrence of depression in the older adult in low- and middle-income countries indicates that the incidence of symptoms of depression reported at the height of the COVID-19 pandemic was comparatively higher than pre-pandemic estimates (21, 22). In a research assessing changes in the symptoms of depression among older adult type 2 diabetes patients in the US from 2016 to 2020, the results indicated that the pervasiveness of mild or markedly severe symptoms of depression among these patients during the COVID-19 pandemic was over 1.6 times higher than prior to the pandemic (23).
The current research analyzed the updated CHARLS data gathered during the COVID-19 pandemic. The reason for selecting this dataset is that it substantially embodies depression's characteristics at this stage among the older adult. To predict depression and determine the related influencing factors leading to this condition among the older adult in China, the following six models were established: k-nearest neighbors (KNN), logistic regression, DT, RF, LightGBM, and SVM.
Research data and methods
Data sources
CHARLS was the first nationally representative survey of middle-aged and older adult people in China and used the multi-stage, stratified probability proportional to size (PPS) sampling method to select samples. The PPS sampling method guarantees the reasonable representation in the sample of individuals from different regions and of varying types (24). Through face-to-face interviews, including the use of questionnaire surveys and biomarker collection, data were collected through CHARLS. Investigators with professional training often conduct surveys, presenting data from a variety of modules, including sociodemography, lifestyle habits, psychological status, and health conditions, thereby guaranteeing data accuracy and consistency. This method presents dependable data support for developing a model for depression prediction for China's older adult. The Biomedical Ethics Committee of Peking University approved the 2020 CHARLS survey (approval number IRB00001052-11015.1.2). For the field survey, respondents who agreed to participate in the survey were asked to sign two informed consent forms; one copy for the respondents and the other is kept in the CHARLS office. Before being released, all data were strictly cleaned and anonymized. A follow-up survey every 2 years is planned by the CHARLS survey, the objective of which was to gather data from middle-aged and older adult people in China over time. However, the 2020 CHARLS data are the latest publicly released data owing to the time required for data collection, cleaning, verification, and release. Accordingly, the current study uses the 2020 CHARLS data. Criteria for inclusion are as follows: (1) individuals aged ≥ 60 years and (2) data on whether or not there are explanatory variables for the depression dimension. Criteria for exclusion are as follows: (1) people aged < 60 years and (2) over 10% missing values in the variables of interest. Moreover, replacing missing values (< 10%) entails using the median method.
Outcome variable
To screen depressive symptoms, CHARLS uses as a common tool the Center for Epidemiological Studies Depression Scale-10 (CESD-10) from the Chinese Center for Epidemiological Studies (25). CESD-10 is selected to test the respondents' depressive symptoms. Moreover, CESD-10, which is reliable and valid, is appropriate for use in large-scale epidemiological surveys. A total of 10 questions are included in the questionnaire to test the past week's individual depressive symptom frequency. The questions include various facets, including depressive mood, sleep disorders, appetite changes, loss of interest, fatigue, difficulty concentrating, and feelings of inferiority (26). A four-level scoring system is typically used for the answers: rarely (under 1 day), sometimes (1–2 days), more than half the time (3–4 days), and almost every day (5–7 days). On the bases of the respondents' answers, each question's scores will be added to obtain the total CESD-10 score, in which the range of the total score is 0–30 points. Total scores of ≥10 or < 10 points indicate having and no depressive symptoms, respectively. The higher the score, the more severe the depressive symptoms (27).
Sociodemographic factors
Variables for the sociodemographic data selected by this study comprise age, gender, education level, region, marital status, and living alone. Moreover, the variables were categorized as follows: gender: female or male; education level: illiterate, primary school, or junior high school and above; region: urban or rural; marital status: married, divorced, widowed, or unmarried; and living alone: yes or no. Age is considered a continuous variable.
Health status
This study chose the following variables for health status: self-rated health (28), multimorbidity (29), Katz-ADL score (30), and Lawton-IADL score (30). The variables were specifically categorized as follows: self-rated health: very poor, poor, fair, good, or very good; and multimorbidity: yes or no. Meanwhile, Katz-ADL and Lawton-IADL scores were used to assess independent living ability and instrumental daily living function, respectively, in which higher scores indicate poorer ability. The Katz-ADL and Lawton-IADL scores are considered continuous variables.
Behavioral factors
Smoking, drinking, nighttime sleep, nap time, social activities, and weekly physical exercise are included in the behavioral factors. Nighttime sleep is categorized as short (< 6 h), moderate (6–8 h; reference group), and long (>8 h) (31, 32). Nap time is evaluated based on the following question: “How long do you usually nap in the past month?” The respondents were divided into 4 groups: no nap (0 min), short nap (< 30 min), moderate nap (30–90 min), and long nap (>90 min) (33). Smoking, drinking, and social activities are categorized as yes or no. Lastly, weekly physical exercise is categorized as 0 times per week, 1–4 times per week, or more than 4 times per week.
Mental health factors
Cognitive function scores are included in the mental health factors. The American Health and Retirement Study (HRS) methods are used to measure the cognitive function scores (34). The participants underwent face-to-face assessments from four dimensions of cognitive function: orientation, memory, calculation, and drawing. The total cognitive score is the sum of orientation (five points), calculation (five points), memory (20 points), and drawing (one point), with a total score of 31 points (35).
Statistical analysis
SPSS23.0 and Python3.8 were used for data analysis. Continuous variables were characterized. In addition, the Kolmogorov-Smirnov test was performed to determine if the normal distribution was followed by the test data. Meanwhile (x ± s), depicted the econometrics conforming to the normal distribution. T-test and analysis of variance (ANOVA) were used for mean comparisons between two groups and across multiple groups, respectively. M(Q1, Q3) indicates measures not adhering to a normal distribution or variance. For comparisons within or between groups, rank-sum tests were utilized. In addition, n (%) depicted categorical data. Lastly, chi-square or exact Fisher's test was utilized for analyzing across at least two groups, with a statistically significant difference of P < 0.05.
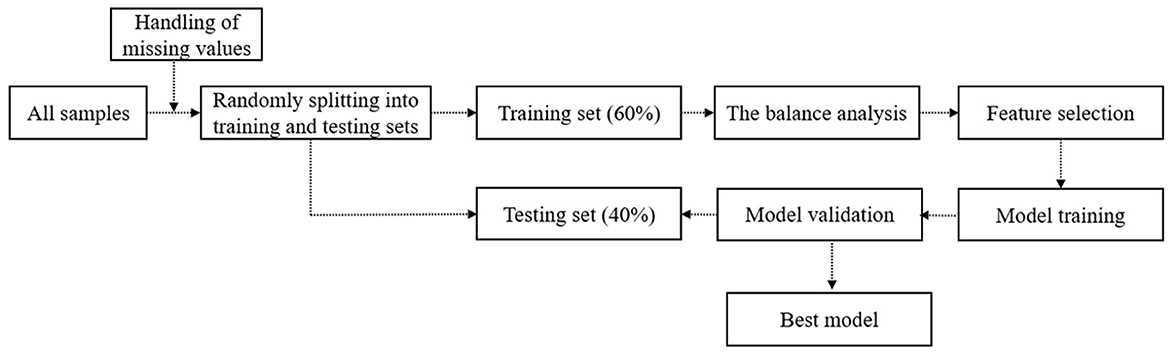
The schematic of the depression prediction framework is presented in Figure 1, which outlines the different steps comprising data preprocessing and model development. Data were divided randomly into training and tests at a 6:4 ratio, thereby guaranteeing similar distribution across both datasets (36). Various methods were also used to fill in missing data values. This study specifically used the training set data's preprocessed data feature screening, in which imbalance was first addressed, followed by balance analysis. The data were then sampled t in the modeling for the unbalanced data. Thereafter, we utilized the SMOTE algorithm to oversample the training set's minority samples. The RF algorithm was utilized for feature selection as the classification model for recursive feature elimination. For the discrete variants, the chi-square detection was performed. For the continuous variables, point-two sequence correlation analysis was conducted. Eventually, characteristic variables with P-values below 0.05 were selected as model inputs.
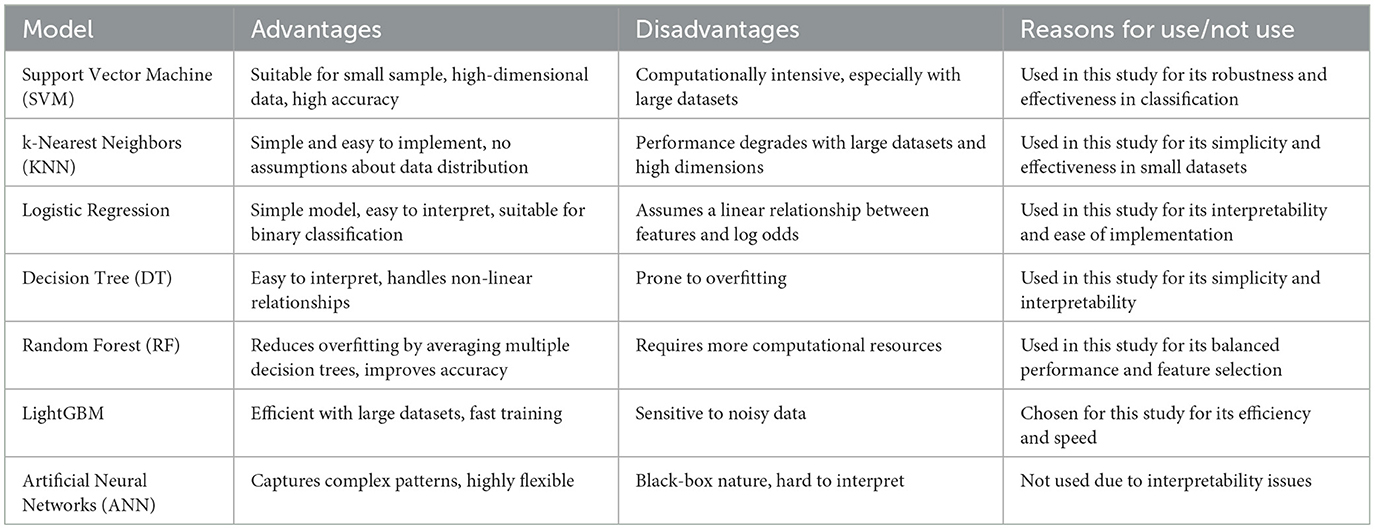
Six models were constructed and forecast by this study: SVM, KNN, logistic regression, DT, RF, and LightGBM (Table 1). The ROC and AUC values via grid search and 5-fold cross-validation were utilized to evaluate the scores, resulting in the selection of the hyperparameters of the model. We selected evaluation metrics (e.g., precision, AUC area, sensitivity, true positives, and false positives) for the model's assessment on the training set. Thereafter, the Delong test was utilized for the comparison of the differences of the ROC curves across models. Decision curve analysis (DCA) was used to assess the performance of the model, in which the true and false positives of a model are used to compute an analytical measure called net benefit, thereby placing the advantages and disadvantages of the model on a comparable scale (37). This study used the Brier score, defined as the mean squared difference between the observed and predicted outcomes, to assess the top-performing model's probabilistic accuracy. In general, the range of the Brier score is from 0 to 1.00, with 0 indicating the best calibration (38). Given the ML model's black-box nature, the current research utilized the SHapely Additive exPlanations (SHAP) value to underscore the significance of the prediction results of the model. The summary graph provides a visual depiction of the contribution of each feature to the prediction results of the model.
Findings
Descriptive analysis results
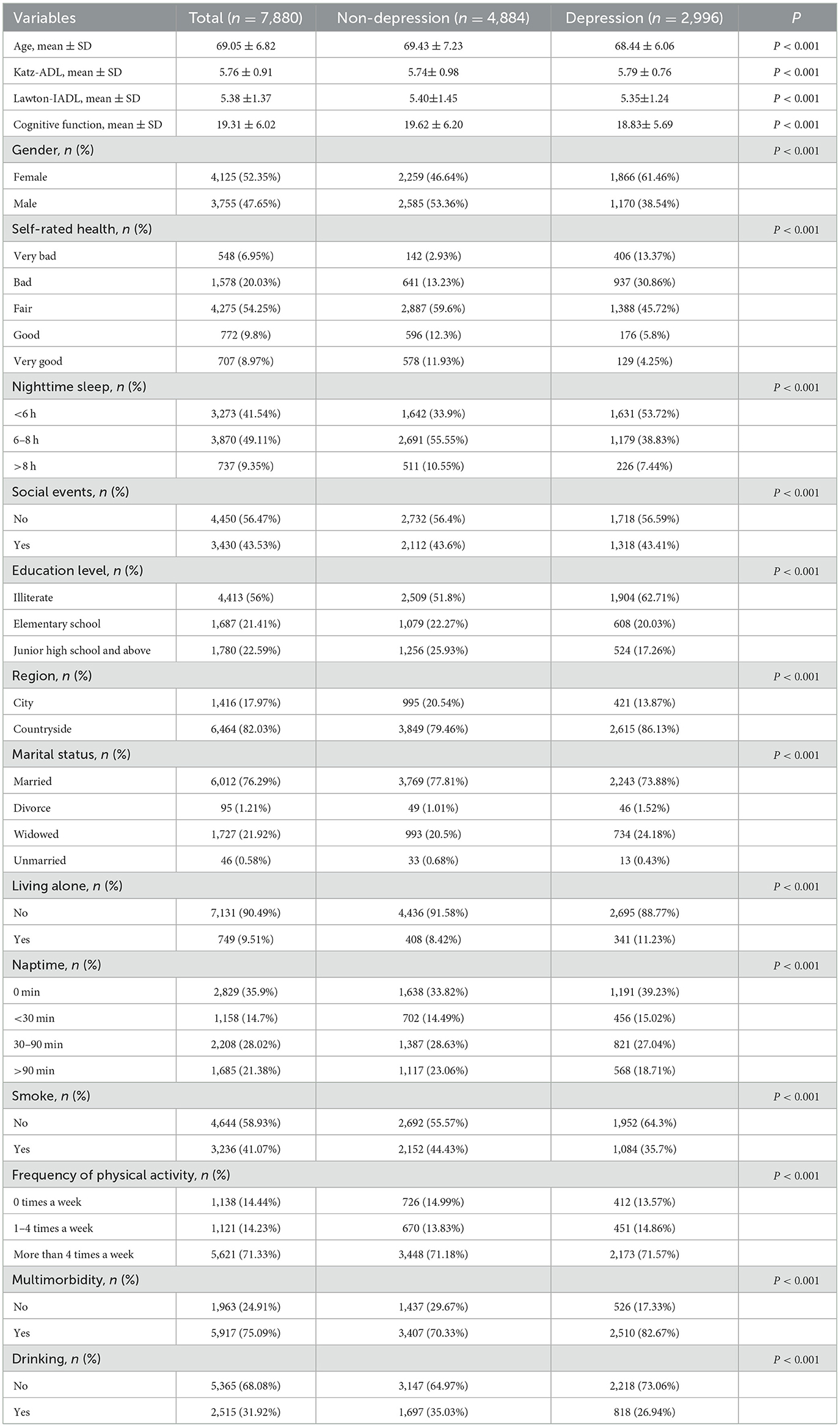
This study's final effective sample includes 7,880 older adult people: 4,125 females (52.35%), with average age of 69.05 ± 6.82 years, and 2,996 (38.5%) suffering from depression. Moreover, there are 4,413 illiterates (56.0%), 1,416 urban residents (17.97%), 6,012 married individuals (76.29%), 749 living alone (9.51%), 548 with extremely poor self-rated health (6.95%), 5,917 with multimorbidity (75.09%), 4,450 not participating in any social activities (56.47%), 737 with a night sleep duration of over 8 h (9.35%), and 2,829 without a nap habit (35.9%). Differences between each variable are statistically significant (P < 0.001). Table 2 shows the specific basic characteristics.
Predicting depression in Chinese older adults using the ML models
The SMOTE algorithm was used to oversample the minority samples. Thereafter, the dataset was partitioned into training and test sets at a 6:4 ratio. The model was trained on the training set, and its ability to generalize was evaluated on the test set. Using the RF algorithm as the classification model, recursive feature elimination was performed on the training set. Three-fold cross-validation was used to derive AUC area scores from various feature selection combinations, in which 16 was identified as the optimal number of features. According to the rank-sum test, no significant difference was noted in the continuous variables between the training and test sets (P > 0.05). The chi-square test also indicated no significant difference for the other categorical variables (P > 0.05).
For depression prediction, KNN and LightGBM had the lowest (AUC = 0.647) and highest (AUC = 0.738) AUC values, respectively, among the six ML models (Figure 2). Moreover, the Delong statistical comparison indicated that the performance of the different models' ROC curves vary (P < 0.01, Table 3).
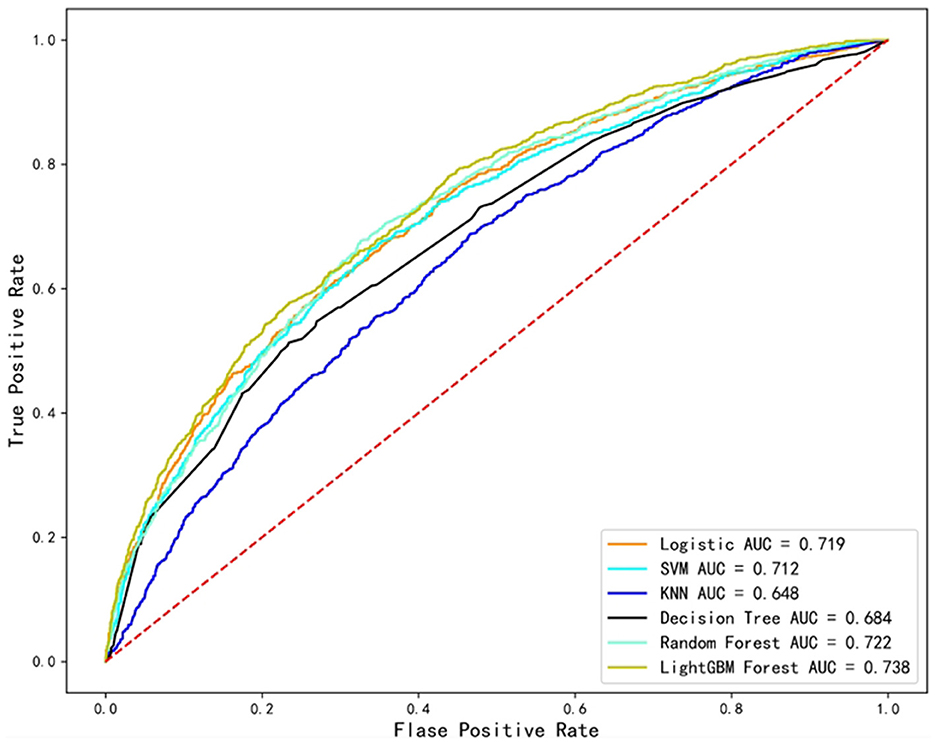
Figure 2. Predictive performance of six machine learning models for depression in older adults. ROC curve (the x-axis indicates the false positive rate, and the y-axis represents the true positive rate).
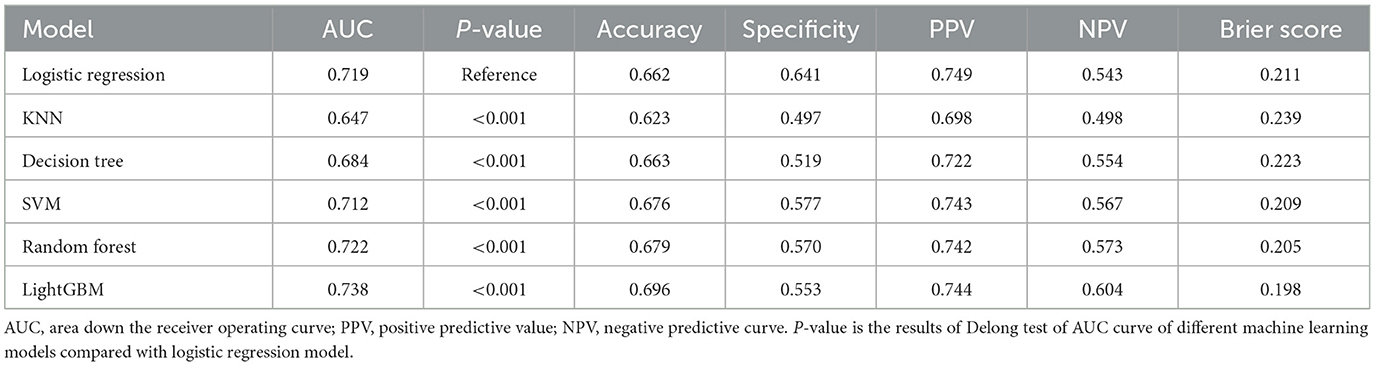
Table 3. Prediction performance of depression in Chinese older adults using six machine learning models.
According to the DCA curve (Figure 3), if the threshold probability of depression among Chinese older adults exceeds 0, then the LightGBM model outperforms the other models in the 0.00–0.85 range. From the results, the LightGBM model's Brier score was 0.198, which was the lowest among all models. Therefore, the best performance was demonstrated by the LightGBM model.
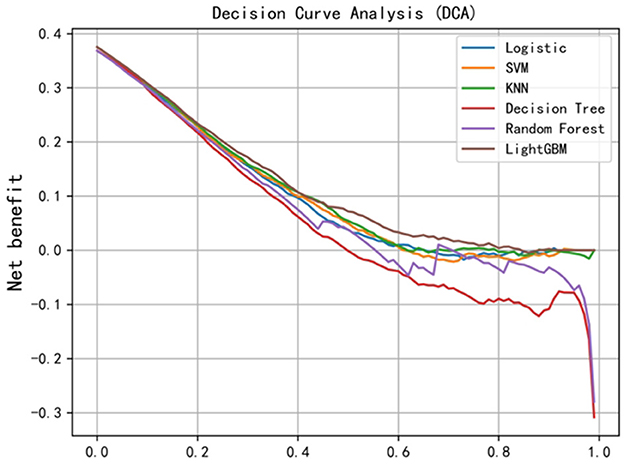
Figure 3. DCA curve (the x-axis indicates the threshold probability, and the y-axis represents net benefit).
Feature importance and variables interpretation
In depression prediction, the LightGBM model ranks feature importance (see Figure 4). The model indicates that the five most important features for predicting depression are self-assessment of health, nighttime sleep, gender, age, and cognitive function. Note that self-rated health, nighttime sleep, and age are negatively correlated with depression occurrence. Moreover, older women have a higher probability of experiencing depression than older men. The findings are significant for early identification and intervention in depression.
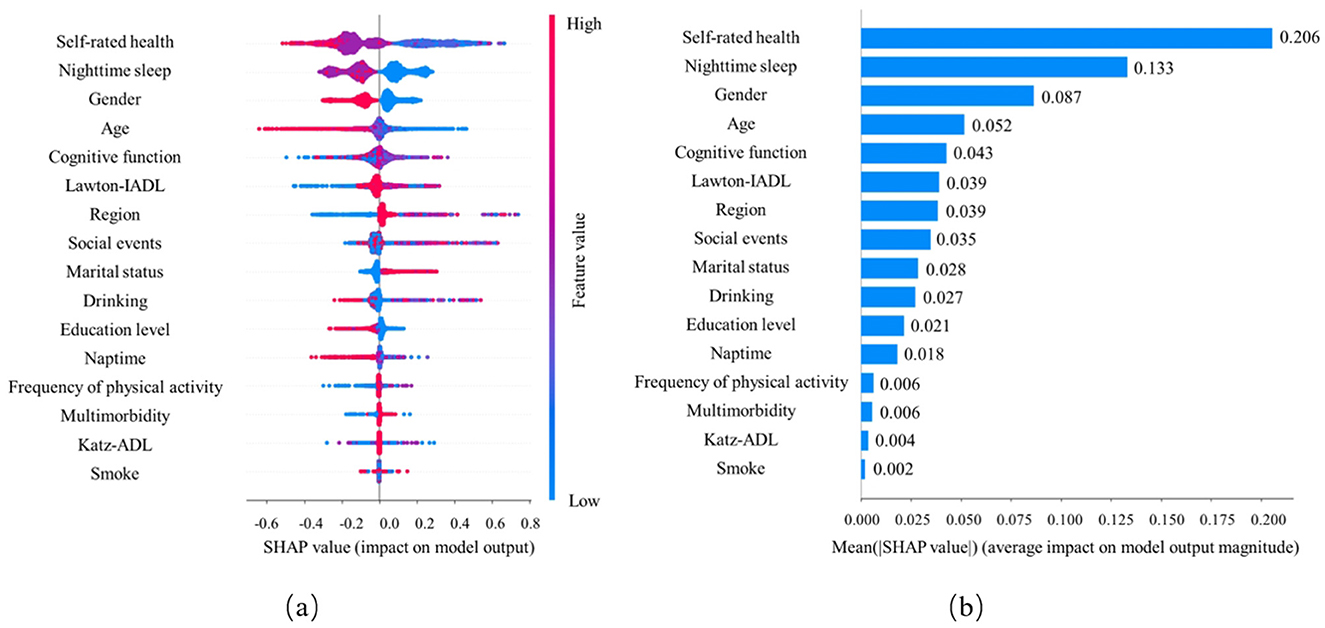
Figure 4. Visual explanation of predictive behavior of depression in older adults based on machine learning prediction models. (A) Each dot represents an individual prediction, dot's position on the x-axis shows the impact that predictor has on the model's prediction for that individual. When multiple dots land on the same x position, they pile up to show density. The color of the dot represents the level of the predictor related to that individual (color reference on the tight). (B) Bar chart of average feature importance based on SHAP value magnitude.
Discussion
Major findings
The newly released 2020 CHARLS data was used by the current research to conduct a depression-prediction task on the older adult under the decision support of six ML algorithms. For feature selection recursive feature elimination, the RF algorithm was used as classification model. Meanwhile, constructing and validating the model feature the use of 16 important feature variables. According to the results, the LightGBM model shows the best performance in terms of the AUC value and outperforms other models in predictive performance. The important contributions of the model prediction results are explained by the SHAP analysis, indicating that the five most important features for predicting depression are self-rated health, nighttime sleep, gender, age, and cognitive function. The contribution of each feature to the model prediction results is intuitively presented by the summary graph. The findings present the key factors affecting the occurrence of depression, which is critical in the early identification and intervention of depression.
Identifying key predictors of depression in the older adult
Social demographic factors, health status, behavioral factors, mental health factors, and other dimensions of the older adult are the variables selected in this study. Previous research has studied these indicators for their impact on depression, thereby showing the credibility and validity of the selected predictive factors. As a predictive factor, self-rated health contributes the most, which is consistent with a previous study that has considered this factor as the most important predictive factor for depression in the older adult (39). Moreover, numerous previous studies have indicated that a lower level of self-rated health is a risk factor for the occurrence of depression among the older adult (40–42). Previous research has likewise shown relationship between depression and the older adult's sleep duration (43). Sleep duration and depression have a U-shaped relationship, and the likelihood of depression is lowest for the older adult sleeping 6– 8 h at night (44). The result of a meta-analysis indicates that considered risk factors of depression are short and long sleep durations (45). Happiness can increase with an increase in sleep duration, which is closely related to a reduction in the occurrence of depression (46). A sharp decrease in sleep duration is associated with an increase in unhealthy behaviors such as obesity, smoking, and drinking, which can affect the older adult's psychology (47). Excessive sleep duration (>9 h) is associated with depression (48). A decrease in physical activity is associated with excessive sleep duration, which may reduce the production of key hormones that regulate emotions (e.g., serotonin or dopamine), thereby increasing the likelihood of depression among the older adult (49).
According to the current research, older adult women are likely to suffer from depression compared with older adult men. This finding is consistent with most previous studies' outcomes (50–53). For the longest time, women have been found to have a higher prevalence of depression. Epidemiological studies have indicated that the pervasiveness of depression among women is nearly twice that of men. Genetically determined susceptibility, hormone fluctuations related to various aspects of reproductive function, and hypersensitivity to hormone fluctuations mediating depressive states are among the reasons for this phenomenon (54). However, other findings have shown lack of association between gender and the occurrence of depression (55–57). The most common predictive factors for the occurrence of depression among the older adult are age, physical health, and cognitive function (18). According to previous studies, age is a risk factor for the occurrence of depression among the older adult (58–60), or it is not associated with the occurrence of depression (61–63). The current research presents a novel finding that age is negatively correlated with the occurrence of depression, which deviates from a few previous research results. This outcome possibly shows that during the COVID-19 pandemic, age might be associated with other protective factors (e.g., life experience and coping strategies), thereby potentially assisting in the reduction of depression risks (64). Accordingly, age may be a protective factor (65).
The relationship between cognitive function and depression remains mired in controversy. Two studies have shown the lack of effect of cognitive impairment on the depressed population (66, 67). Meanwhile, two other studies have reported that the risk of depression among the older adult increases owing to cognitive impairment (68, 69). Researchers have analyzed data from 8,382 men and women aged at least 65 years who participated in the US Health and Retirement Study from 1998 to 2010. Low depression and high depression categories are associated with rapid cognitive decline and estimated impact after adjusting for the interaction of depression and time (70).
Optimizing older adult depression prediction with lightGBM and SHAP
According to 20 studies that systematically evaluated the prediction model of older adult depression risk, 55% of the prediction models were built using ML technology, while seven models (35%) used multivariate logistic regression and two models (10%) used linear regression (18). First, to establish a prediction model for the occurrence of depression in the older adult, the current study used the SMOTE sampling technique to balance the “depression” sample ratio of 0 and 1. Accordingly, the model's prediction accuracy and stability are improved by balancing the number of older adult people in the dataset's different categories. Second, AUC is the indicator most commonly used for evaluating the prediction model's performance, while DCA is likewise utilized to assess the model's clinical value and has been applied in numerous medical studies, showing immense clinical utility (71). This study's results indicate that the LightGBM model performs best in terms of the AUC value. The possible reason is that LightGBM can handle numerous features and has good handling ability for unbalanced datasets. This model is further assessed using the DCA method. The net benefit of LightGBM is the largest when the net return is compared on the decision curve. If depression's threshold probability surpasses 0, then the performance of the LightGBM model is better than that of the other models in the 0.00–0.85 range. This finding is crucial because it indicates that the LightGBM model has excellent performance under most clinical decision thresholds. The LightGBM model's The Brier score is 0.198, the lowest among all models. The Brier score is an indicator to measure prediction accuracy. The lower the value, the higher the accuracy of prediction, thereby further confirming the LightGBM model's superiority.
By contrast, complex patterns and interactions are revealed by ML methods; however, these methods are often criticized for their “black box” nature. Accordingly, the SHAP technology can be used to solve this problem. The reason is that they can empirically indicate the importance of each feature to the model output, thereby enabling the combination of features and non-linear interactions, while providing insights into the current relationships among variables, which are considered correlations instead of causal relationships. Prior studies have successfully utilized SHAP values for ML interpretation in medical research (72). Ballester et al. analyzed the suicide risk of young people by using the gradient tree boosting model and SHAP values (73). Although the aforementioned method has been utilized in various fields of ML interpretation, to our knowledge, the SHAP value has yet to be applied to investigate the predictive research of depression's occurrence among the older adult in China. Therefore, this study's results can present a reference for enhancing the prediction model of depression's occurrence among the older adult in China.
Limitations
Several limitations characterize this research. First, the current study only uses CES-D to evaluate depression's symptoms among the older adult. While CES-D is not the gold standard technique for depression diagnosis, which may lead to bias in the evaluation results, the CESD-10 tool has been validated in the Chinese population and shows good validity, potentially improving the credibility and validity of the results. Second, this research is based on cross-sectional data, preventing the determination of the causal direction of the observed associations. Longitudinal studies are needed to establish causal relationships. Third, the data survey was conducted during the COVID-19 pandemic in 2020. This unique stressor may have influenced both predictors (e.g., sleep patterns) and the outcome (depression), acting as a collider and introducing bias into the model. New data after the pandemic have not yet been released, and a new longitudinal data model can be constructed subsequent to the data release post-pandemic. Fourth, reporting bias is possible from the study participants because self-reported data may not always accurately reflect their true state of health and wellbeing. Participants may underreport or overreport their symptoms due to social desirability or recall bias. Information bias could also occur due to inaccuracies in the collected data, which may affect the results. Specifically, the 2020 CHARLS data may have inaccuracies due to data entry errors, participants' misinterpretation of survey questions, or inconsistencies in data collection processes across different regions. Fifth, variables such as gender, age, and cognitive function, while strong predictors of depression, may correlate with other unmeasured factors like socioeconomic status or life stress, potentially confounding the results. Cognitive impairment might indirectly reflect life-stage factors or cumulative health burdens and also be a symptom of depression, particularly in older populations (“pseudo-dementia”). Self-rated health, identified as the most significant predictor, could act as a proxy for unmeasured variables such as chronic disease burden or healthcare access, leading to residual confounding. Sixth, the use of the SMOTE algorithm to oversample minority depression cases helps balance the dataset but may inadvertently create artificial correlations or inflate the importance of less influential variables, introducing collider bias. Lastly, although measures have been taken to ensure the good performance of the model, it still necessitates validation with an independent external cohort once it is established. This step is crucial to confirm the model's generalizability and robustness. Notwithstanding these limitations, the current research indicates that the constructed model can be utilized for predicting and providing further interventions for the occurrence of depression among the older adult.
Conclusion
This research uses six ML algorithms to build a prediction model for the occurrence of depression among the older adult in China. Moreover, the LightGBM algorithm-based predictive model has superior comprehensive performance compared with other models. Therefore, the research results can provide a theoretical reference for the accurate identification of high-risk groups from multiple dimensions and the implementation of the necessary early interventions. The proposed model identifies key influencing factors (i.e., self-rated health, nighttime sleep duration, gender, age, and cognitive function) and some potential influencing factors. These factors should be continuously enhanced in future model construction research.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: (China Health and Retirement Longitudinal Study, CHARLS) 2020 Data Access Links: https://charls.charlsdata.com/pages/data/111/zh-cn.html. If the database is not available, you can obtain the data directly from the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or the patients'/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
YS: Conceptualization, Data curation, Funding acquisition, Investigation, Writing – original draft. LC: Formal analysis, Project administration, Writing – review & editing. HL: Data curation, Supervision, Validation, Writing – review & editing. YL: Funding acquisition, Resources, Software, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This project was supported by the Foundation project [supported by research project of Shanghai University of Sport (2023STD015) and Ministry of Education Project of Humanities and Social Sciences for young scholars (22YJC890027)].
Acknowledgments
The authors would like to thank the National School of Development at Peking University for providing the CHARLS data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CHARLS, China Health and Retirement Longitudinal Study; AUC, Area under the curve; ROC, Receiver operating characteristic; SHAP, SHapley Additive exPlanations; SVM, Support Vector Machine; PPV, Positive predictive value; ML, machine learning; NP, Negative predictive value; KNN, K-Nearest Neighbors; RF, Random Forest; DT, Decision Tree; SMOTE, Synthetic Minority Oversampling Technique; DCA, Decision Curve Analysis; Katz-ADL, Katz activities of daily living; Lawton-IADL, Lawton instrumental activities of daily living; CESD10, Center for Epidemiological Studies Depression Scale.
References
1. Alexopoulos GS. Depression in the elderly. Lancet. (2005) 365:1961–70. doi: 10.1016/S0140-6736(05)66665-2
2. Herrman H, Kieling C, McGorry P, Horton R, Sargent J, Patel V. Reducing the global burden of depression: a Lancet-World Psychiatric Association Commission. Lancet. (2019) 393:e42–3. doi: 10.1016/S0140-6736(18)32408-5
4. Bennett S, Thomas AJ. Depression and dementia: cause, consequence or coincidence? Maturitas. (2014) 79:184–90. doi: 10.1016/j.maturitas.2014.05.009
5. Valkanova V, Ebmeier KP. Vascular risk factors and depression in later life: a systematic review and meta-analysis. Biol Psychiatry. (2013) 73:406–13. doi: 10.1016/j.biopsych.2012.10.028
6. Meeks TW, Dunn LB, Kim DS, Golshan S, Sewell DD, Atkinson JH, et al. Chronic pain and depression among geriatric psychiatry inpatients. Int J Geriatr Psychiatry. (2008) 23:637–42. doi: 10.1002/gps.1954
7. Kim JM, Shin IS, Yoon JS, Stewart R. Prevalence and correlates of late-life depression compared between urban and rural populations in Korea. Int J Geriatr Psychiatry. (2002) 17:409–15. doi: 10.1002/gps.622
8. Loughlin A. Depression and social support: effective treatments for homebound elderly adults. J Gerontol Nurs. (2004) 30:11–5. doi: 10.3928/0098-9134-20040501-05
9. Gallo JJ, Bogner HR, Morales KH, Post EP, Ten Have T, Bruce ML. Depression, cardiovascular disease, diabetes, and two-year mortality among older, primary-care patients. Am J Geriatr Psychiatry. (2005) 13:748–55. doi: 10.1097/00019442-200509000-00002
10. Briggs R, Tobin K, Kenny RA, Kennelly SP. What is the prevalence of untreated depression and death ideation in older people? Data from the Irish Longitudinal Study on aging. Int Psychogeriatr. (2018) 30:1393–401. doi: 10.1017/S104161021700299X
11. Kok RM, Reynolds CF 3rd. Management of depression in older adults: a review. JAMA. (2017) 317:2114–22. doi: 10.1001/jama.2017.5706
12. Wuthrich VM, Frei J. Barriers to treatment for older adults seeking psychological therapy. Int Psychogeriatr. (2015) 27:1227–36. doi: 10.1017/S1041610215000241
13. Lu J, Xu X, Huang Y, Li T, Ma C, Xu G, et al. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2021) 8:981–90. doi: 10.1016/S2215-0366(21)00251-0
14. Reynolds CF 3rd, Cuijpers P, Patel V, Cohen A, Dias A, Chowdhary N, et al. Early intervention to reduce the global health and economic burden of major depression in older adults. Annu Rev Public Health. (2012) 33:123–35. doi: 10.1146/annurev-publhealth-031811-124544
15. Bota PJ, Wang C, Fred ALN, Da Silva HP. A review, current challenges, and future possibilities on emotion recognition using machine learning and physiological signals. IEEE Access. (2019) 7:140990–1020. doi: 10.1109/ACCESS.2019.2944001
16. Chen X, Lin S, Zheng Y, He L, Fang Y. Long-term trajectories of depressive symptoms and machine learning techniques for fall prediction in older adults: evidence from the China Health and Retirement Longitudinal Study (CHARLS). Arch Gerontol Geriatr. (2023) 111:105012. doi: 10.1016/j.archger.2023.105012
17. Lin S, Wu Y, Fang Y. A hybrid machine learning model of depression estimation in home-based older adults: a 7-year follow-up study. BMC Psychiatry. (2022) 22:816. doi: 10.1186/s12888-022-04439-4
18. Tan J, Ma C, Zhu C, Wang Y, Zou X, Li H, et al. Prediction models for depression risk among older adults: systematic review and critical appraisal. Ageing Res Rev. (2023) 83:101803. doi: 10.1016/j.arr.2022.101803
19. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
20. Alqahtani IM, Al-Garni AM, Abumelha MS, Alsagti SA, Alshehri FAD, Alqahtani AA, et al. Prevalence of depression, anxiety, and stress among the general population during COVID-19 pandemic: a systematic review. J Family Med Prim Care. (2023) 12:1030–7. doi: 10.4103/jfmpc.jfmpc_1943_22
21. Rahman MS, Rahman MA, Ali M, Rahman MS, Maniruzzaman M, Yeasmin MA, et al. Determinants of depressive symptoms among older people in Bangladesh. J Affect Disord. (2020) 264:157–62. doi: 10.1016/j.jad.2019.12.025
22. Wahlin Å, Palmer K, Sternäng O, Hamadani JD, Kabir ZN. Prevalence of depressive symptoms and suicidal thoughts among elderly persons in rural Bangladesh. Int Psychogeriatr. (2015) 27:1999–2008. doi: 10.1017/S104161021500109X
23. Chao AM, Wadden TA, Clark JM, Hayden KM, Howard MJ, Johnson KC, et al. Changes in the prevalence of symptoms of depression, loneliness, and insomnia in US older adults with type 2 diabetes during the COVID-19 pandemic: the Look AHEAD Study. Diabetes Care. (2022) 45:74–82. doi: 10.2337/dc21-1179
24. Xue J, Li J, Liang J, Chen S. The prevalence of mild cognitive impairment in China: a systematic review. Aging Dis. (2018) 9:706–15. doi: 10.14336/AD.2017.0928
25. Lei X, Sun X, Strauss J, Zhang P, Zhao Y. Depressive symptoms and SES among the mid-aged and elderly in China: evidence from the China Health and Retirement Longitudinal Study national baseline. Soc Sci Med. (2014) 120:224–32. doi: 10.1016/j.socscimed.2014.09.028
26. Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. (1999) 14:608–17. doi: 10.1002/(SICI)1099-1166(199908)14:8<608::AID-GPS991>3.0.CO;2-Z
27. Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. (1991) 20:149–66. doi: 10.1007/BF01537606
28. Bazargan M, Smith J, Saqib M, Helmi H, Assari S. Associations between polypharmacy, self-rated health, and depression in African American older adults; mediators and moderators. Int J Environ Res Public Health. (2019) 16:1574. doi: 10.3390/ijerph16091574
29. Ansari S, Anand A, Hossain B. Multimorbidity and depression among older adults in India: mediating role of functional and behavioural health. PLoS ONE. (2022) 17:e0269646. doi: 10.1371/journal.pone.0269646
30. Zhao L, Wang J, Deng H, Chen J, Ding D. Depressive symptoms and ADL/IADL disabilities among older adults from low-income families in Dalian, Liaoning. Clin Interv Aging. (2022) 17:733–43. doi: 10.2147/CIA.S354654
31. Kwok CS, Kontopantelis E, Kuligowski G, Gray M, Muhyaldeen A, Gale CP, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc. (2018) 7:e008552. doi: 10.1161/JAHA.118.008552
32. Lo JC, Groeger JA, Cheng GH, Dijk DJ, Chee MW. Self-reported sleep duration and cognitive performance in older adults: a systematic review and meta-analysis. Sleep Med. (2016) 17:87–98. doi: 10.1016/j.sleep.2015.08.021
33. Li J, Cacchione PZ, Hodgson N, Riegel B, Keenan BT, Scharf MT, et al. Afternoon napping and cognition in chinese older adults: findings from the China health and retirement longitudinal study baseline assessment. J Am Geriatr Soc. (2017) 65:373–80. doi: 10.1111/jgs.14368
34. Crimmins EM, Kim JK, Langa KM, Weir DR. Assessment of cognition using surveys and neuropsychological assessment: the Health and Retirement Study and the Aging, Demographics, and Memory Study. J Gerontol B Psychol Sci Soc Sci. (2011) 66(Suppl. 1):i162–71. doi: 10.1093/geronb/gbr048
35. Cao L, Zhao Z, Ji C, Xia Y. Association between solid fuel use and cognitive impairment: a cross-sectional and follow-up study in a middle-aged and older Chinese population. Environ Int. (2021) 146:106251. doi: 10.1016/j.envint.2020.106251
37. Wei Z, Wang X, Ren L, Liu C, Liu C, Cao M, et al. Using machine learning approach to predict depression and anxiety among patients with epilepsy in China: a cross-sectional study. J Affect Disord. (2023) 336:1–8. doi: 10.1016/j.jad.2023.05.043
38. Karhade AV, Thio QCBS, Ogink PT, Bono CM, Ferrone ML, Oh KS, et al. Predicting 90-day and 1-year mortality in spinal metastatic disease: development and internal validation. Neurosurgery. (2019) 85:E671–81. doi: 10.1093/neuros/nyz070
39. Conde-Sala JL, Garre-Olmo J, Calvó-Perxas L, Turró-Garriga O, Vilalta-Franch J. Course of depressive symptoms and associated factors in people aged 65+ in Europe: a two-year follow-up. J Affect Disord. (2019) 245:440–50. doi: 10.1016/j.jad.2018.10.358
40. iang J, Xu X, Quiñones AR, Bennett JM, Ye W. Multiple trajectories of depressive symptoms in middle and late life: racial/ethnic variations. Psychol Aging. (2011) 26:761–77. doi: 10.1037/a0023945
41. Makizako H, Shimada H, Doi T, Yoshida D, Anan Y, Tsutsumimoto K, et al. Physical frailty predicts incident depressive symptoms in elderly people: prospective findings from the Obu Study of Health Promotion for the Elderly. J Am Med Dir Assoc. (2015) 16:194–9. doi: 10.1016/j.jamda.2014.08.017
42. Luppa M, Luck T, König HH, Angermeyer MC, Riedel-Heller SG. Natural course of depressive symptoms in late life. An 8-year population-based prospective study. J Affect Disord. (2012) 142:166–71. doi: 10.1016/j.jad.2012.05.009
43. Song Y, Liu H, Liu Y. The association between nap time, nighttime sleep and depression in Chinese older adults: a cross-sectional study. PLoS ONE. (2024) 19:e0302939. doi: 10.1371/journal.pone.0302939
44. Liu BP, Wang XT, Liu ZZ, Wang ZY, An D, Wei YX, et al. Depressive symptoms are associated with short and long sleep duration: a longitudinal study of Chinese adolescents. J Affect Disord. (2020) 263:267–73. doi: 10.1016/j.jad.2019.11.113
45. Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. (2015) 32:664–70. doi: 10.1002/da.22386
46. Tang NK, Fiecas M, Afolalu EF, Wolke D. Changes in sleep duration, quality, and medication use are prospectively associated with health and well-being: analysis of the UK household longitudinal study. Sleep. (2017) 40:zsw079. doi: 10.1093/sleep/zsw079
47. Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. (2012) 22:939–43. doi: 10.1016/j.cub.2012.03.038
48. Supartini A, Honda T, Basri NA, Haeuchi Y, Chen S, Ichimiya A, et al. The impact of sleep timing, sleep duration, and sleep quality on depressive symptoms and suicidal ideation amongst Japanese freshmen: the EQUSITE Study. Sleep Disord. (2016) 2016:8737654. doi: 10.1155/2016/8737654
49. Stranges S, Dorn JM, Shipley MJ, Kandala NB, Trevisan M, Miller MA, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. (2008) 168:1353–64. doi: 10.1093/aje/kwn337
50. Gureje O, Oladeji B, Abiona T. Incidence and risk factors for late-life depression in the Ibadan Study of Ageing. Psychol Med. (2011) 41:1897–906. doi: 10.1017/S0033291710002643
51. Lue BH, Chen LJ, Wu SC. Health, financial stresses, and life satisfaction affecting late-life depression among older adults: a nationwide, longitudinal survey in Taiwan. Arch Gerontol Geriatr. (2010) 50(Suppl. 1):S34–8. doi: 10.1016/S0167-4943(10)70010-8
52. Yokoyama E, Kaneita Y, Saito Y, Uchiyama M, Matsuzaki Y, Tamaki T, et al. Association between depression and insomnia subtypes: a longitudinal study on the elderly in Japan. Sleep. (2010) 33:1693–702. doi: 10.1093/sleep/33.12.1693
53. Chen R, Wei L, Hu Z, Qin X, Copeland JR, Hemingway H. Depression in older people in rural China. Arch Intern Med. (2005) 165:2019–25. doi: 10.1001/archinte.165.17.2019
54. Noble RE. Depression in women. Metabolism. (2005) 54(5 Suppl. 1):49–52. doi: 10.1016/j.metabol.2005.01.014
55. Weyerer S, Eifflaender-Gorfer S, Wiese B, Luppa M, Pentzek M, Bickel H, et al. Incidence and predictors of depression in non-demented primary care attenders aged 75 years and older: results from a 3-year follow-up study. Age Ageing. (2013) 42:173–80. doi: 10.1093/ageing/afs184
56. Weissgram S, Zehetmayer S, Jungwirth S, Rainer M, Tragl KH, Fischer P. Late-onset depression in elderly subjects from the Vienna Transdanube Aging (VITA) study. J Clin Psychiatry. (2009) 70:500–8. doi: 10.4088/JCP.08m04265
57. Schoevers RA, Deeg DJ, van Tilburg W, Beekman AT. Depression and generalized anxiety disorder: co-occurrence and longitudinal patterns in elderly patients. Am J Geriatr Psychiatry. (2005) 13:31–9. doi: 10.1097/00019442-200501000-00006
58. Chou KL. Reciprocal relationship between pain and depression in older adults: evidence from the English Longitudinal Study of Ageing. J Affect Disord. (2007) 102:115–23. doi: 10.1016/j.jad.2006.12.013
59. Chou KL. Combined effect of vision and hearing impairment on depression in older adults: evidence from the English Longitudinal Study of Ageing. J Affect Disord. (2008) 106:191–6. doi: 10.1016/j.jad.2007.05.028
60. Lampinen P, Heikkinen E. Reduced mobility and physical activity as predictors of depressive symptoms among community-dwelling older adults: an eight-year follow-up study. Aging Clin Exp Res. (2003) 15:205–11. doi: 10.1007/BF03324501
61. Yang YT, Wang YH, Chiu HT, Wu CR, Handa Y, Liao YL, et al. Functional limitations and somatic diseases are independent predictors for incident depressive disorders in seniors: findings from a nationwide longitudinal study. Arch Gerontol Geriatr. (2015) 61:371–7. doi: 10.1016/j.archger.2015.07.005
62. Dong Y, Yang FM. Insomnia symptoms predict both future hypertension and depression. Prev Med. (2019) 123:41–7. doi: 10.1016/j.ypmed.2019.02.001
63. Schoevers RA, Beekman AT, Deeg DJ, Geerlings MI, Jonker C, Van Tilburg W. Risk factors for depression in later life; results of a prospective community based study (AMSTEL). J Affect Disord. (2000) 59:127–37. doi: 10.1016/S0165-0327(99)00124-X
64. Cohen M. Depression, anxiety, and somatic symptoms in older cancer patients: a comparison across age groups. Psychooncology. (2014) 23:151–7. doi: 10.1002/pon.3383
65. Hurria A, Li D, Hansen K, Patil S, Nelson C, Lichtman SM, et al. Distress in older patients with cancer. J Clin Oncol. (2009) 27:4346–51. doi: 10.1200/JCO.2008.19.9463
66. Andreescu C, Chang CC, Mulsant BH, Ganguli M. Twelve-year depressive symptom trajectories and their predictors in a community sample of older adults. Int Psychogeriatr. (2008) 20:221–36. doi: 10.1017/S1041610207006667
67. Kuo SY, Lin KM, Chen CY, Chuang YL, Chen WJ. Depression trajectories and obesity among the elderly in Taiwan. Psychol Med. (2011) 41:1665–76. doi: 10.1017/S0033291710002473
68. Kuchibhatla MN, Fillenbaum GG, Hybels CF, Blazer DG. Trajectory classes of depressive symptoms in a community sample of older adults. Acta Psychiatr Scand. (2012) 125:492–501. doi: 10.1111/j.1600-0447.2011.01801.x
69. Montagnier D, Dartigues JF, Rouillon F, Pérès K, Falissard B, Onen F. Ageing and trajectories of depressive symptoms in community-dwelling men and women. Int J Geriatr Psychiatry. (2014) 29:720–9. doi: 10.1002/gps.4054
70. Donovan NJ, Wu Q, Rentz DM, Sperling RA, Marshall GA, Glymour MM. Loneliness, depression and cognitive function in older US adults. Int J Geriatr Psychiatry. (2017) 32:564–73. doi: 10.1002/gps.4495
71. Hijazi Z, Oldgren J, Lindbäck J, Alexander JH, Connolly SJ, Eikelboom JW, et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet. (2016) 387:2302–11. doi: 10.1016/S0140-6736(16)00741-8
72. Booth AL, Abels E, McCaffrey P. Development of a prognostic model for mortality in COVID-19 infection using machine learning. Mod Pathol. (2021) 34:522–31. doi: 10.1038/s41379-020-00700-x
Keywords: depression, machine learning, health promotion, CHARLS, China
Citation: Song YLQ, Chen L, Liu H and Liu Y (2025) Machine learning algorithms to predict depression in older adults in China: a cross-sectional study. Front. Public Health 12:1462387. doi: 10.3389/fpubh.2024.1462387
Received: 10 July 2024; Accepted: 10 December 2024;
Published: 07 January 2025.
Edited by:
Zahir Vally, United Arab Emirates University, United Arab EmiratesReviewed by:
Mariusz Stanisław Wiglusz, Medical University of Gdansk, PolandVimal Satodiya, California Department of Corrections and Rehabilitation (CDCR), United States
Copyright © 2025 Song, Chen, Liu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Liu, bHl1ZWNlQDE2My5jb20=
†ORCID: Yan Li Qing Song orcid.org/0009-0000-3725-714X
Yue Liu orcid.org/0000-0001-9428-9615
 Yan Li Qing Song
Yan Li Qing Song Lin Chen1
Lin Chen1 Yue Liu
Yue Liu