
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 27 January 2025
Sec. Public Mental Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1458680
This article is part of the Research TopicSexual Violence in Times of ConflictView all 4 articles
 Lindsey Green1*
Lindsey Green1* Linda Kaljee2
Linda Kaljee2 Shahanoor Akter Chowdhury1
Shahanoor Akter Chowdhury1 Thomas McHale1
Thomas McHale1 Ranit Mishori1,3
Ranit Mishori1,3 Dahlia Fateen3
Dahlia Fateen3 Nima Sheth4
Nima Sheth4Background: In August 2017, the Rohingya population of northern Rakhine State in Myanmar fled to Bangladesh following “clearance operations” by the Myanmar security forces that were characterized by widespread and systematic violence, constituting severe human rights violations. The “clearance operations” were preceded by years of consistent denial of the human rights of the Rohingya people in Myanmar. This study examines the impact of these human rights violations on the trauma experiences of Rohingya survivors, their resulting mental health, and the availability and access to post-migration mental health services.
Methods: Qualitative one-on-one interviews were conducted with 26 health care professionals who cared for Rohingya refugees after their arrival in Bangladesh.
Results: Trauma experienced by the Rohingya spanned the period before, during, and following migration and was ongoing at the time of data collection. The impact of Rohingya survivors’ concurrent grief and trauma in relation to the violence they experienced in Myanmar as well as during and after their journey to Bangladesh that, at times, exacerbated survivors’ trauma presentation. There were limited mental health services available in Bangladesh and additional structural and procedural barriers to care that limited responsiveness to Rohingya survivors’ mental health needs.
Conclusion: The Rohingya experienced traumatic human rights violations in Myanmar that led to their forced migration to Bangladesh. The Rohingya continued to experience trauma during their forced migration to Bangladesh and were exposed to additional stressors in the post-migration settings in refugee camps, including lack of access to adequate mental health services. These experiences have resulted in a spectrum of stress-and trauma-related symptoms. These findings show the mental health impact of protracted human rights violations on the Rohingya, revealing how trauma is not a singular event but a continuous experience. Detailing the limited mental health infrastructure and structural barriers facing Rohingya refugees in Bangladesh, the findings underscore the urgent need for trauma-informed interventions that address the complex psychological consequences of systemic violence and displacement. The findings emphasize the critical importance of holistic mental health support in refugee settings, providing evidence-based recommendations for the public health and humanitarian sector to consider when designing programs to address the mental health and psychosocial support needs of sexual violence survivors living in conditions of displacement.
Current frameworks for understanding mental health outcomes for displaced and conflict-affected populations consider pre-migration, migration, and post-migration stressors as contributors to mental health outcomes and overall well-being (1, 2). Olcese et al.’s scoping review on migration and community resilience underscores that migrants face profound economic, social, and psychological hardships, which are further intensified by experiences of violence or displacement before migration (3). Resilience-building within these communities depends heavily on social capital, community competence, and adaptive attitudes, emphasizing the critical role of host contexts in fostering recovery. For refugee populations like the Rohingya, these insights underscore the need to address structural and systemic barriers while strengthening communal support mechanisms to mitigate cumulative stress and enhance mental health outcomes.
In August 2017, Myanmar security forces, accompanied by local civilians, launched “clearance operations” against the Rohingya population of northern Rakhine state (4). Serious human rights violations were widespread and systematic, including shootings, beatings, sexual violence, and destruction of property (4–8). Such human rights violations had been preceded by years of persistent human rights violations, including denial of citizenship, restrictions on movement, forced displacement, denial of the right to health and education, lack of religious freedom, looting and destruction of property, arbitrary and illegal detentions, killings, forced labor, and trafficking (5, 9, 10).
Following the ‘clearance operations,’ more than 720,000 Rohingya refugees1 fled to Bangladesh. After a long, treacherous journey, Rohingya refugees settled in camps near Cox’s Bazar. These camps quickly grew to become the largest refugee settlement in the world which put enormous strain on the existing social, cultural, and economic environment and infrastructure in this area of Bangladesh (11, 12). For the Rohingya, prolonged exposure to gross violations of human rights in Myanmar and on-going, systemic discrimination, deprivation of basic rights, and considerable safety concerns in Bangladesh, have increased their vulnerability to poor mental health outcomes (2, 13).
Challenges related to basic living conditions in within the refugee camp setting include access to health care and continued exposure to violence and crime and conflict. These challenges were exacerbated by the COVID-19 pandemic (14–20). In addition, the ongoing humanitarian crisis worsened barriers preventing access to essential health care services for women, girls, children and other vulnerable populations leading to increased distress and negative impacts (18, 21).
The Rohingya population in Bangladesh has experienced significant stressors related to the on-going and evolving political situation in Myanmar and limited prospects for return. In February 2021, the Myanmar miltary coup d’état and the ensuing violence and repression, have intensified the suffering of Rohingya and other minority communities within the country and caused significant social, political and economic instability (22–24). Increasing conflict since 2022 between the Myanmar Armed Forces and Arakan Army in Rakhine State has led to transportation blockages, displacement, and reduced humanitarian access, affecting livelihoods and increasing malnutrition rates (25). In the central region of Rakhine State, numerous internally displaced persons (IDPs) are compelled to return to areas that still pose significant protection and security risks (26). Due to ongoing insecurity, limited access to basic services, and the closure of IDP sites, some individuals are likely to experience multiple displacements (27–31).
Studies emphasize that the links among pre-migration trauma, displacement stressors, and post-migration living conditions to mental health outcomes, including PTSD and depression, are well-established (2, 32, 33). The Rohingya population have experienced prolonged exposure to violence, human rights violations, and statelessness, which are further compounded by post-migration adversities (15, 34). The accessibility and adequacy of mental health services in the post-migration context, particularly within refugee camps, remains underexplored. There is also limited research on healthcare workers’ perspectives to support more nuanced investigations into service gaps and tailored interventions.
With an understanding of Rohingya refugees’ experiences of forced migration and the particular mental health challenges faced by displaced, this study sought to capture trauma experiences in the periods before, during and after Rohingya survivors’ migration to Bangladesh and their resulting mental health presentations. The authors collected these data by speaking to health care workers who provided services to Rohingya survivors in Bangladesh to understand both the trauma experiences of survivors and post-migration mental health services within the Rohingya refugee camps during the period of data collection and analysis.
Qualitative one-on-one semi-structured interviews were conducted with health care professionals who cared for Rohingya refugees in Bangladesh between 2017 and 2020. The focus of the overall research project was to understand health care professionals’ experiences providing care to Rohingya survivors with an emphasis on patterns of perpetration of sexual violence and access to health care. In addition, data were obtained related to the impact of the COVID-19 pandemic on services for Rohingya survivors (8, 20). The data presented and analyzed here are specific to mental health presentation and access to services and represent a sub-set of the findings from this larger research project.
The study was intentionally designed to gather information from healthcare workers about the experiences of Rohingya refugees without directly interviewing survivors to avoid subjecting them to potential re-traumatization. Health care workers, through their clinical evaluations and interactions with numerous patients, can provide unique insights into both individual cases and can provide data to support overarching patterns and trends in survivors’ experiences. In addition, health care workers can provide information about both short-and long-term after-effects of trauma, offering a more comprehensive understanding that might not be available through direct survivor interviews alone.
The research team included social scientists, public health experts, and physicians from the United States and Bangladesh. Data were collected between November 2019 and August 2020. Due to several barriers, including the Covid-19 pandemic, all interviews but one were conducted virtually using Zoom, Skype, and phone. The in person interview was conducted in Cox’s Bazar with a participant still working there. Interviews were conducted in English and Bengali. All interviewers were established qualitative researchers and public health experts with extensive experience working on projects focused on sexual and reproductive health, conflict-related sexual violence, orphaned and vulnerable children, and displaced persons.
A purposive sampling strategy was used to recruit health professionals who fit the inclusion criteria: a healthcare worker of any nationality and any discipline and specialty who worked with Rohingya refugees in camps in Cox’s Bazar in Bangladesh between August 2017 and August 2020. Identification of participants included outreach to known contacts working with the Rohingya during the inclusion period and recommendations from those contacts and other professionals working in Cox Bazar. The cohort included physicians, nurses, midwives, community health workers, mental health and psychosocial support workers, case managers, SGBV and protection workers, and health volunteers. As is standard practice with qualitative research, data saturation, which is the point at which new themes or information cease to emerge from the data, was used to establish the final sample size (35). To help determine the point of ‘data saturation’ regular conference calls were conducted to provide an opportunity for the study team to discuss preliminary findings, data gaps, and identify potential participants to help fill in those gaps.
No compensation was provided for participation in the interview. All participants provided informed consent prior to starting interviews.
Data was collected via a semi-structured interview guide and a demographic form. The interview guide covered key areas, including professional background and contextual details of work with the Rohingya, general experiences treating Rohingya patients, experiences specific to physical violence, SGBV, and mental health status, and challenges in addressing trauma and health care. A summary of main themes for the interview were provided to respondents in advance of the interview.
All interviews were audio recorded and transcribed. Interviews in English were conducted by US-based researchers and transcribed verbatim by a professional service. Interviews in Bangla were conducted by a Bangladeshi researcher, fluent in both Bangla and English. These interviews were transcribed in Bangla and then translated into English with quality checks for accuracy. Transcribed data were uploaded into a qualitative data management program (Dedoose) (36). All transcripts were analyzed in English. The research team created a coding dictionary to ensure data were coded consistently by four study team members from the United States and Bangladesh. An intercoder reliability assessment was conducted on a sample of transcripts which indicated an overall consistency in the use of the codes. In addition, research team members met regularly during the data analysis project to review coding and determine if new codes were required for emergent themes. After completion of data coding, themes and sub-themes were identified and reviewed by the team. Illustrative examples of the themes and sub-themes were selected from the text. All interviewers were established qualitative researchers with extensive experience working on projects focused on sexual and reproductive health, orphaned and vulnerable children, and displaced persons.
The study received ethical approval from the Georgetown University IRB (STUDY00001282 and MOD00004144) and an exemption was given by PHR’s Ethical Review Board. Permission to conduct the study was also received from the Office of the Refugee Relief and Repatriation Commissioner (RRRC) in Cox’s Bazar, Bangladesh.
This research has several limitations. The study relied on health professionals’ experiences and observations of the physical and mental health status of a population that is different from them culturally and linguistically. While the study population represented different geographic, professional, and cultural backgrounds, it did not include Rohingya health care providers.
Observations must therefore be viewed as highly contextual and potentially affected by biases. The survivors’ stories recounted in these interviews were communicated through multiple cultural and linguistic filters, including interpretation. Additionally, our cohort was selected via snowball sampling and is not representative of all health professionals who worked in the camps.
Interviews were conducted in 2020, in some cases more than 3 years after respondents had had the experiences that they had described to the interviewers. Recall bias, therefore, must be considered. However, respondents were given a summary of the main research themes prior to the interview and some respondents reviewed written notes or journals from their time spent in Cox’s Bazar during the interviews. Clinicians who had worked in the camps in August or September 2017 may have observed the manifestation of more acute trauma, suggesting potential chronological bias. Participants interviewed had a wide range of time periods when they supported Rohingya survivors, some had been part of an acute response during 2017 and 2018 while others were still working with Rohingya refugees in Bangladesh at the time of the interview. This variety in participant experiences allowed us to observe more about the acute and long-term mental health challenges for Rohingya survivors.
Lastly, while some of the respondents interviewed were health care professionals with mental health specialization or experience, most respondents were not specialists in psychiatry, behavioral, or mental health.
Despite these limitations, there were significant similarities across the collected narratives reflecting on the experiences of the Rohingya.
As a qualitative study, the interpretation and analysis of data is subject to interpretation biases introduced by the researchers. The research team was multidisciplinary, drawn from a variety of cultural backgrounds, and worked collaboratively to address potential biases in the interpretation of results.
We recruited 26 health professionals who fit the inclusion criteria. Table 1 describes their characteristics.
Respondents recognized that Rohingya refugees’ trauma experiences were ongoing and spanned pre-, during, and post-migration periods. On arriving in the camps, however, health professionals tried to address Rohingya patients’ immediate health needs while recognizing the impact of their past and concurrent experiences of trauma and grief. Table 2 provides examples of the different phases during which Rohingya survivors experienced trauma, as noted by the respondents.
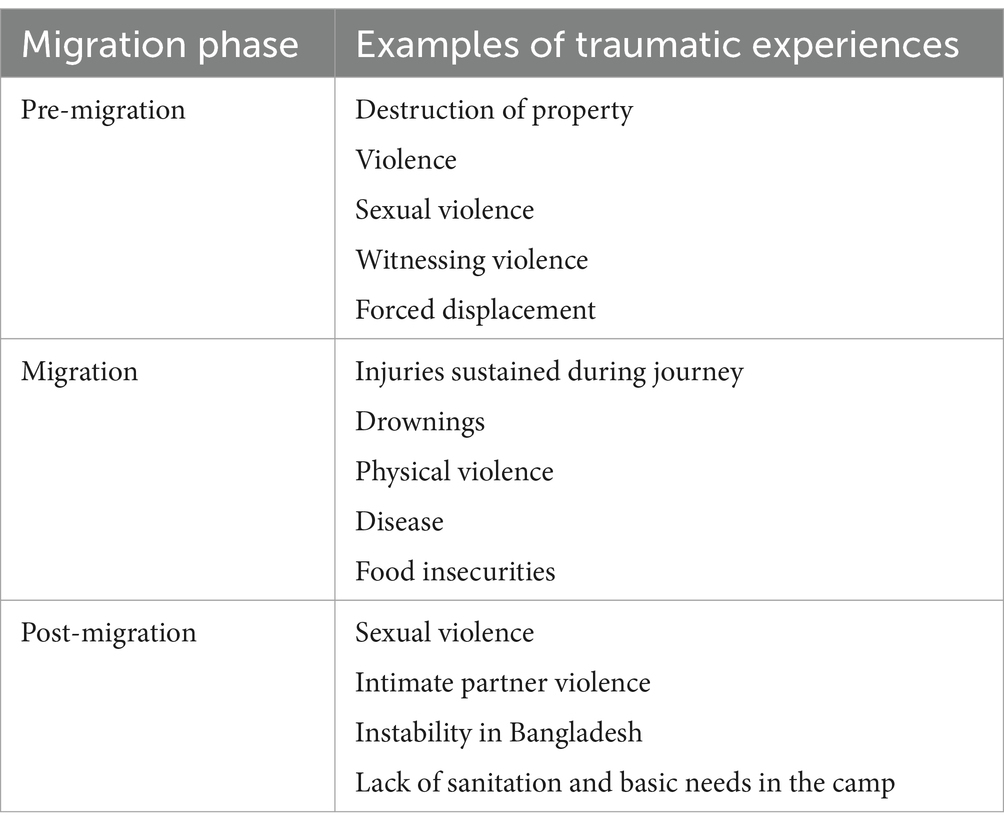
Table 2. Phases and types of traumatic experiences of Rohingya refugees who settled in camps in Bangladesh.
Health care workers were well-aware of the multiple traumas experienced by Rohingya refugees prior to leaving Myanmar. The health care workers described being alert to potential for their patients to disclose violent experiences, including those related to the destruction of villages, and killings.
We all knew they were fleeing Myanmar because there were the atrocities that were happening there. They were being killed, their villages were being burned, their homes were being burned..” A nurse working in Cox's Bazar in 2017.
“It was kind of like the understanding that everybody coming in had witnessed,… if not experienced, some level of abuse…. So, we were always on heightened alert looking for those types of things.” A nurse working at a primary health clinic in Kutupalong camp in 2018.
Health care workers also described specific instances in which patients or family members of patients described experiences of witnessing physical violence and death. Because of stigma, many health care workers’ heard indirect accounts of sexual violence from their patients or saw signs of sexual violence from those who did not disclose a history of sexual violence, such as from women coming into the clinic for to treat sexually transmitted infections or unwanted pregnancies.
One case … was this 11-year-old who came in because her mom said she stopped talking. That was striking to me because she had basically selective mutism as a manifestation of her PTSD. I suspected she was probably either raped or had some sort of gender-based violence, but she denied it. Then I interviewed the mom separately and found out that, actually, her father, his legs were chopped off in front of her by the military. A fellow Rohingya man saw and took the father, and they fled across the border into Bangladesh, and they took him immediately to the field hospital, and they have not seen him since, and that was like months ago …. She stopped talking since that experience.” A volunteer physician working in Cox’s Bazar in 2018.
“I did have an 11-year-old girl come in who brought in her … five-and seven-year-old [siblings].. She was the ‘mom.’ Both parents had been killed.” A pediatrician working in Cox’s Bazar in 2017 and 2018.
The arduous journey from the Rohingya refugees’ home villages in Myanmar to Bangladesh required several days of walking through difficult terrain and across the river border between the two countries. Refugees left their homes with no provisions and suffered injuries, illnesses, and death during migration. Families lost contact with one another including parents and their children (37). Health care workers heard about these experiences from their patients.
There were a lot of people who had like actual physical injuries from the journey or from the trauma and the events that were preceding that. We would see someone that had a laceration that they said was from a machete from that conflict or someone that was injured in the process of migrating, like while they were walking for forever without shoes.” An emergency nurse working in satellite health clinics in December 2017.
We saw lots and lots of parents or moms who had lost many kids who would say, ‘I had five kids trying to cross the river. This is the only one I could hold.’” A pediatrician working in Cox's Bazar in 2017 and 2018.
“I would say everybody.. we saw [was] suffering from the effects of the violence and the trip altogether.” A nurse working in Cox's Bazar in 2017.
The influx of almost 800,000 persons into Bangladesh over a short period of time meant that local, national, and international actors where not initially prepared for the arrival of this many people. The crowded Cox Bazar refugee sites were without basic sanitation and survival needs, including water and food. Access to healthcare was limited with a focus on immediate needs for those injured or suffering from infectious disease outbreaks including measles and diphtheria. In addition, this large population had endured extreme physical, psychological, and physical trauma, requiring complex, long-term care and treatment (38). On arrival and even years into resettlement, the Rohingya continued to experience sexual violence, intimate partner violence, and multiple physical and mental health challenges exacerbated by poor access to healthcare and economic, social, and political instability (39).
“I definitely saw gender-based violence. It was often within the community, from the camp itself, within the community…” A physician working with Rohingya refugees in 2017 and 2018.
“Hitting, punching, kicking on any part of the body, including the head, and even if you're pregnant, it could still be the abdomen. …. We've had women whose husbands have tried to hang them, whose husbands have tried to poison them, who have been burned. Yeah, we see all kinds but hitting and kicking and punching are definitely the most common.” A nurse practitioner working at an outpatient clinic in Kutupalong in 2017.
“I didn't see any domestic violence in November, but as the time goes on.. end of December or beginning of January we started to see some domestic violence.. The stress shows.. The direction of stress comes into the, inside of the house because the life there was very difficult.” A nurse midwife working in Kutupalong camp in 2017.
“They've moved from kind of crisis mode, from the things that happened there. It certainly still affects them, and they still think about it, but that's not why they're coming to the clinic.. They still bring it up sometimes during their visits, but it's more of the trauma that we would see now would be related to current situations.” A nurse working in Cox's Bazar in 2017.
While the violence sometimes left physical injuries and scars, other forms of trauma, such as sexual violence and psychological trauma, were primarily evident through the stories told to the health care providers during care for other conditions. In addition, health care workers experienced (Table 3).
When survivors shared their experiences with health professionals, the associated psychological trauma was sometimes expressed to them by patients explicitly, and at other times it was discernable from their behaviors, including their affect or lack of engagement or responsiveness.
“The thing that you did see was just overall deep, deep sadness in these women. The women would come in … [covered] …, so you could only see their eyes, but many of them, when I'd be taking care of their kids, would start to cry.” A pediatrician working in Cox's Bazar in 2017 and 2018.
Providers reported seeing a wide range of mental health and trauma related symptoms including hypervigilance, emotional numbing, re-experiencing, avoidance, lack of appetite, and co-occurring symptoms of depression, anxiety, and panic attacks.
“We had patients present regularly enough, like complaining of depression, anxiety, panic attacks, those were all fairly common complaints.” An emergency nurse working in satellite health clinics in December 2017.
Clinicians shared that patients regularly presented with somatic complaints, including physical pain, that the clinicians attributed to their psychological distress.
“A huge number of our patients had somatic complaints, like very vague. Like, ‘I've had a headache or a stomachache or backache.’ And then when you dig deeper into how long [they] have these things … it's been going on as long as they left their home or as long as they've been living in the camps. … we couldn't find anything wrong with them clinically and it seemed like the providers would attribute it to just a stress reaction that manifested in a physical way. And that was very, very common.” An emergency nurse working in satellite health clinics in December 2017.
Some survivors experienced such severe trauma responses that they stopped eating and speaking.
“And then there was a 15-year-old who had been raped and was mute and mostly catatonic. She wasn't talking, she wasn't eating. She had also seen her brothers killed and she had been raped. … Our clinic did have a psychologist, so when a patient came with severe problems and they didn't seem to have any physical problems, then we would have them come back every day and talk to a counselor. But this child was much too sick to stay with us.” A nurse working in Cox's Bazar in 2017.
Patients often disclosed trauma and traumatic experiences associated with sexual violence when seeking care for a wide range of services, including sexual and reproductive health.
“And then there was a woman who … had complaints of vaginal discharge. So, I asked her if I could examine her vaginally. And then when I did the exam it looked like she had some trauma, just from the scars on her perineum. So, I asked her a few questions about that, and then she started crying and talked to me about her experience of rape at the hands of the military, the Myanmar military… she and I think around 14 other women had been taken and locked into a house, and that they were all gang raped. And some of them did not survive, but she was able to survive.” A nurse practitioner working at an outpatient clinic in Kutupalong camp in 2017.
Clinicians also reported that patients who were seeking sexual and reproductive health care disclosed trauma from witnessing sexual violence, often against a relative.
“I remember an elderly lady who came in just with a bladder infection, a UTI. And then somehow the conversation devolved into the fact that she had watched her daughter-in-law get gang-raped by six soldiers in their home.” A volunteer physician working with Rohingya refugees in January 2018.
At the start of the humanitarian response in Cox’s Bazar in late 2017, there was limited mental health capacity within the health sector, especially a lack of inpatient capacity for acute or severe mental health case management. Respondents described numerous barriers that limited access to care and responsiveness to the refugees’ mental health needs. These barriers likely contributed to poor post-migration mental health outcomes. Barriers identified in this study included structural, legal, and medical/procedural issues.
Table 4 provides examples of the types of barriers faced by Rohingya refugees when seeking mental health services and support.
Respondents commented on the restrictions Rohingya refugees faced in their ability to leave the camps due to a lack of legal status in Bangladesh. These restriction affected access to health services and contributed to a sense of confinement and isolation. The size and number of refugee camps also limited access to care, sometimes requiring survivors to prioritize traveling to remote service points over other demands on their time such as accessing food or clean water.
“The nearest clinic that would offer mental health services by trained professionals would be a 20-minute walk from our clinic, so sometimes it's just too much effort.” A nurse practitioner working at an outpatient clinic in Kutupalong camp in 2017.
Many respondents noted the lack of private space for discussions about sensitive issues and/or for counseling sessions.
“It is very tough when we try to make confidentiality and rapport building, and sometimes [if] there is any secret issue. Lots of noises, so clients sometimes feel discomfort to give enough information …. Besides the room, there is another room, they are talking, working and even they are laughing sometimes …” A clinical psychologist working in Cox's Bazar in 2018.
For health care workers, long workdays in the clinics and high daily patient loads significantly impacted their time with each patient and thereby limited the time available to discuss mental health and SGBV issues or to conduct screenings and referrals.
“I think that some of the challenges are time. If I had time, I probably would have asked the trauma stories from every one of the patients because I think that's part of healing. I think that time was definitely a great limiting factor.” A volunteer physician working in Cox's Bazar in 2018.
Some healthcare workers also identified continuity of services for survivors as a barrier. Agencies providing services experienced inconsistent funding streams and, health care providers often served on short-term emergency response assignments. Available health services also had little to no access to providers with mental health training. Healthcare workers felt that inadequate resources and infrastructure, including telecommunication outages and blockages, limited their ability to make appropriate referrals and follow up with patient’s progress.
“The funding was always like short-term, very short-term funding. Like one-month, two-month, maximum three-month funding. So that hampered our program planning and design.” A public health administrator for a multilateral organization in Cox's Bazar in 2017.
Many respondents shared that standardized mental health screening protocols were not adapted for the Rohingya culture nor translated into the Rohingya language. These tools were also perceived to be too long and complex for use within the refugee health settings. One respondent identified challenges with the integration of mental health screening protocols during a clinical encounter, especially when patients presented with multiple health issues that needed to be addressed in and environment where follow-up visits were not guaranteed.
“I question where the most appropriate place to deploy the screening tool would be as far as like at what point during their exam? Typically, a lot of screening tools are kind of used towards the beginning …. If they have decided that they're going to come in with kind of generalized abdominal pain as a complaint and you ask them about sexual violence kind of before you'd gotten to that they might feel uncomfortable jumping the gun.” An emergency nurse working in satellite health clinics in December 2017.
Within the complex and limiting service delivery context, some health care professionals perceived that giving their patients a safe space to discuss their experiences was important, even while recognizing the limits of their ability to provide care.
“That's why my personal philosophy was if I had a minute or two or if I had even a little bit of extra time to spare, I would want to kind of serve as sort of a counselor role, even though that's not my training …. I'm not a psychologist, I'm not a clinical psychiatrist, but I felt like I had to act like one for a lot of the patients because they're coming in with vague symptoms like … muscle aches or stomach pain. That's sometimes somatization of trauma.” A volunteer physician working in Cox's Bazar in 2018.
Respondents also described the challenges faced in obtaining information from female survivors about sexual health, SGBV, and associated mental health when a majority of interpreters and providers were male. Additionally, they noted that it was often difficult for interpreters to discuss and translate questions and language related to mental health conditions to patients because of a lack of cultural understanding of mental health and medically trained interpreters.
“Probably it was just there and not disclosed for [a] multitude of reasons. Number one, I'm a western man, western white man speaking with a Rohingya woman patient and even if there was just kind of a simple gynecological complaint, many Rohingya women would prefer just to continue with their complaint than allowing a strange man to examine them, even with another woman in the room …. we wanted to train female English interpreters … [but] those female interpreters and their families were threatened with physical violence if they allowed their daughters to go be trained to be an English translator in the clinic.” An outpatient attending physician in Kutupalong camp in 2018 and 2019.
Health workers play a critical role in addressing the mental health challenges of forcibly displaced populations by serving as both frontline responders and community liaisons. Their responsibilities often extend beyond conventional care to include trauma-informed practices, cultural competence, and advocacy for improved access to essential health services. Given the intersection of migration-related stressors with pre-existing trauma, health professionals are uniquely positioned to mitigate the compounded psychological distress experienced by refugees. For example, they deliver culturally sensitive psychosocial interventions, often adapting to resource-scarce environments to provide meaningful support. In addition, health workers can help bridge the gap between displaced populations and host communities, promoting integration and resilience.
Interview data from health workers confirms previously documented information about the traumatic human rights violations in Myanmar that led to the forced migration of the Rohingya. These interviews further provide important data related to traumas associated with the migration journey and experiences post-migration within the Cox Bazar camps.
This study offers an important contribution to the recent literature that seeks to document the continuum of trauma experiences and associated mental health outcomes for refugee populations as well as barriers to general health care and mental health care in post-migration settings (13, 21, 34, 40–42). The study also provides a structured, phased approach to assessing these experiences and identifying the factors that contribute to Rohingya refugees’ psychological, emotional, physical, and social well-being. These data also provide insights into the logistical, economic, social, and cultural challenges in providing health care in the context of a large influx of persons in urgent need of a broad spectrum of medical interventions (43–47). In addition, through the perspectives of health care professionals, mental health services can be developed and adapted to address some of these limitations within refugee settings that negatively affect delivery and accessibility and acceptability.
Within the context of clinical care, many Rohingya refugees disclosed traumatic experiences, including sexual violence and killing of family members, to health care workers. In other instances, these experiences were disclosed by family or community members. In some cases, trauma was presented either somatically with physical pain or through subtle interpersonal changes such as lack of engagement or responsiveness. It is important to note that these specific manifestations of trauma may only capture a small fraction of trauma experiences within this population. However, the reported presentations of trauma are consistent with what would be expected and have been documented elsewhere (48).
Healthcare workers also helped to provide data on the multiple physical and psychological trauma associated with the migration process. These data are important to understanding the continuum of events which impact the mental health of the Rohingya and other refugees including the migration experience, on-going social and political upheaval within the Rohingya’s home country, and post-migration experiences within Bangladesh (49).
The instability in the post-migration environment of the Rohingya, from their stateless immigration status to scarcity of resources to dismantled social networks, left the community with added stress, continuous fear and a shared, collective, experienced trauma that affects the social fabric of the community (13, 50). Not having proper channels to address these experiences could have contributed to various other stressors, such as intimate partner violence, increased burden on children to assume care responsibilities, and suppression of pre-migration traumas for fear of social stigma. The continued trauma experienced by many likely affected their ability to readjust and find stability as individuals and as a group (13, 15, 21, 40, 51).
As noted, the narratives shared by the health care workers are consistent with other studies that have found mental health conditions to be prevalent among the Rohingya refugee population and with frameworks that outline factors that contribute to refugee mental health (5, 13, 21). In one study, Rohingya refugees in Bangladesh compared to those in Malaysia were more likely to experience PTSD, depression, anxiety, and functional impairment. Data from the Cox’s Bazar Panel Survey indicated 30.0% of respondents reported depressive symptoms and 4.9% reported symptoms associated with PTSD (15, 51). The healing of Rohingya refugees should be viewed within a context of potentially compounded and continued trauma at both the individual and community level (52). A study analyzing household survey responses of Rohingya refugees in Bangladesh from 2019 and 2020 revealed a high prevalence of severe post-traumatic stress symptoms (PTSSs), particularly among those who experienced physical or sexual abuse before displacement, with 46.6% reporting severe PTSSs (42). Findings from this study however also indicated that adequate humanitarian aid and opportunities for paid employment in refugee camps mitigated risks of PTSSs related to post-migration stressors.
Outcomes from this study can be used to further research and humanitarian efforts among other populations. The experiences of the Rohingya, although unique in many ways, are not entirely dissimilar from the experiences of other forcibly displaced populations including Bosnian, Cambodian, Cuban, Iraqi, Sudanese, Syrian, and Tamil communities. In each of these communities, the continuum of migration stressors may either compound or be mitigated by interventions (52–55).
This study substantiates reports about the lack of mental health infrastructure in Rohingya refugee camps in Bangladesh, especially during the initial humanitarian response, and the enormous difficulty accessing appropriate services. While improvements have been made to infrastructure, and more mental health services and programs have been added over time, there continues to be an inadequate mental health response (41). In a recent study, ongoing challenges to the availability of mental health services for Rohingya include inadequate numbers of skilled service providers and services for severe mental illness, lack of programs focused on children, and issues related to privacy and confidentiality of clients (56). In addition, Rohingya refugees ability to access to health services continues to be hampered by linguistic and socio-cultural barriers including perceptions and definition of health and illness, and lack of trust and fear of authority (57).
Evidence-based intervention approaches in the post-migration period may offer more effective and prompt healing spaces and should be explored to mitigate on-going stressors within the Rohingya community. Frameworks exist to address mental health issues in varying contexts (58). Leveraging multicomponent interventions that address survivors’ symptoms, culture, manifestations of trauma, social settlements, adaptations and interpersonal connectivity best support recovery for displaced populations with complex trauma exposure (59–64). Mental health and psychosocial support (MHPSS) services in the Rohingya humanitarian response have provided critical support to the Rohingya refugees However, the success of these interventions has been contingent on adaptation to account for the type of trauma experienced by the survivors, their symptoms, delivery logistics, and the socio-cultural and political contexts from which they came and to which they migrated (58, 59).
Interventions that should be prioritized for Rohingya survivors should be those that have worked best for other displaced populations in limited resource settings (59–64). In general, these interventions are characterized by: (1) low intensity mental health interventions that can be delivered to a variety of people with a wide range of diagnoses (trans-diagnostic), and (2) implementation through trained professionals with different skill levels (task-shifting) (61). Some of these interventions have been adapted in Rohingya populations including the Adaptation and Development After Persecution and Trauma (ADAPT) model, a version of which has been adapted for Rohingya refugees in both Malaysia and Bangladesh (60). Other interventions that should be considered are outlined in Table 5.
These interventions are designed to be easy to implement and scale up in low-and middle-income countries. However, medication management and individual trauma approaches are necessary to address the needs of those with a higher degree of psychopathology (59). It is also important to assess implementation conditions including stakeholder engagement, cultural adaptation, current barriers to care, and staff training, supervision, and monitoring. Special challenges can arise with high staff turnover and lack of sustainable supervision systems, all of which exist in the context of mental health support for Rohingya survivors (60).
Training health workers in trauma-informed care, survivor-centered approaches, cultural competence, and trust-building with refugee communities is essential to mitigate barriers such as stigma, linguistic challenges, and lack of trust. Programs like Self Help Plus (SH+) and Problem management Plus (PM+), which have proven effective in low-resource settings, should be tailored to address Rohingya-specific experiences, such as their collective trauma and intergenerational suffering (61, 62). Furthermore, sustainable support systems for health worker supervision and capacity-building are crucial to maintain service quality and address challenges like staff burnout and turnover. Stakeholder engagement, cultural adaptation, and strengthened inter-agency coordination should also be prioritized to create a holistic, accessible, and culturally resonant mental health response.
Focusing on pre-migration traumatic events in displaced populations can undermine the significance of traumas experienced during migration, the conditions in which displaced populations live, and how these conditions and post-migration stress, may also negatively impact mental health (65). Analyzing the mental health outcomes of displaced populations therefore necessitates a multi-pronged approach, acknowledging the nuanced experiences of such populations pre-, during, and post-migration.
This study shows persistent trauma related to experiences of conflict-related sexual violence years after the events of 2017 and offer insight into the long-term manifestations of trauma related to human rights violations experienced by Rohingya populations. Seven years since Rohingya survivors first experienced displacement and forced migration, this study demonstrates that the drivers for persistent trauma still exist, as do the opportunities to leverage existing models of mental health and psychosocial support for healing.
The findings of this research are consistent with well-documented and expected outcomes for forcibly displaced populations who have experienced trauma, violence, and prolonged displacement. These findings emphasize the importance of providing immediate low-resource psychological interventions as well as long-term individual trauma-focused psychotherapy for forced migrants to address pre-, during, and post-migration trauma.
This study highlights the ongoing mental health challenges faced by Rohingya refugees, stemming from traumatic pre-migration events, continued violence during migration, and persistent stressors in post-migration environments. To address these issues, healthcare workers and policymakers must prioritize culturally sensitive mental health services, such as Group Integrative Adapt Therapy (IAT-G) and Problem Management Plus (PM+), tailored to the unique needs of this population. Expanding access through mobile clinics, increasing the availability of trained professionals, and adopting task-shifting approaches can improve service delivery. Additionally, embedding mental health care into broader humanitarian assistance frameworks, supported by sustainable funding and inter-agency coordination, is essential to reduce barriers and foster resilience. These interventions can significantly enhance the well-being of Rohingya refugees and other displaced populations.
Findings from this study should be used to advocate for effective mental health services for Rohingya refugees specifically, and displaced populations more generally.
The datasets presented in this article are not readily available because of the studies informed consent process. The deidentified data used for this analysis can be made available upon reasonable request, in accordance with the study’s informed consent process. Requests to access the datasets should be directed to bGdyZWVuQHBoci5vcmc=.
The study involving humans were approved by Georgetown University Institutional Review Board (STUDY00001282 and MOD00004144) and an exemption was given by PHR’s Ethical Review Board. Permission to conduct the study was also received from the Office of the Refugee Relief and Repatriation Commissioner (RRRC) in Cox’s Bazar, Bangladesh. The study were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
LG: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. LK: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. SC: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. TM: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing, Conceptualization, Project administration. RM: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. DF: Writing – original draft, Writing – review & editing. NS: Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research received funding from an anonymous donor.
The authors would like to acknowledge and extend thanks to all the health care workers who were willing to share their experiences for this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ACT, Acceptance and Commitment Therapy; ADAPT, Adaption and Development After Persecution and Trauma; CBT, Cognitive Behavior Therapy; CETA, Common Elements Treatment Approach; EASE, Early Adolescent Skills for Emotions; EMDR, Eye Movement Desensitization and Reprocessing; IAT-G, Group Integrative Adapt Therapy; IPT, Interpersonal Therapy; MHPSS, Mental Health and Psychosocial Support; PM+, Problem Management Plus; PTSD, Post-traumatic Stress Disorder; RRRC, Office of the Refugee Relief and Repatriation Commissioner (Bangladesh); SGBV, Sexual and Gender-based Violence; SH+, Self Help Plus; TF-CBT, Trauma-focused Cognitive Behavioral Therapy; WHO, World Health Organization.
1. ^The Government of Bangladesh refers to the Rohingya as "Forcibly Displaced Myanmar Nationals" (FDMN).
1. Miller, KE, and Rasmussen, A. The mental health of civilians displaced by armed conflict: an ecological model of refugee distress. Epidemiol Psychiatr Sci. (2017) 26:129–38. doi: 10.1017/S2045796016000172
2. Hynie, M. The social determinants of refugee mental health in the post-migration context: a critical review. Can J Psychiatr. (2018) 63:297–303. doi: 10.1177/0706743717746666
3. Olcese, M, Cardinali, P, Madera, F, Camilleri, AP, and Migliorini, L. Migration and community resilience: a scoping review. Int J Intercult Relat. (2024) 98:101924. doi: 10.1016/j.ijintrel.2023.101924
4. Parmar, PK, Leigh, J, Venters, H, and Nelson, T. Violence and mortality in the northern Rakhine State of Myanmar, 2017: results of a quantitative survey of surviving community leaders in Bangladesh. Lancet Planet Health. (2019) 3:e144–53. doi: 10.1016/S2542-5196(19)30037-3
5. Haar, RJ, Wang, K, Venters, H, Salonen, S, Patel, R, Nelson, T, et al. Documentation of human rights abuses among Rohingya refugees from Myanmar. Confl Heal. (2019) 13:42. doi: 10.1186/s13031-019-0226-9
6. UN Human Rights Council. Report of the independent international fact-finding mission on Myanmar. UN human rights council; (2018). Report No.: A/HRC/39/64. Available from: https://www.ohchr.org/sites/default/files/Documents/HRBodies/HRCouncil/FFM-Myanmar/A_HRC_39_64.pdf (Accessed June 24, 2024).
7. Chynoweth, SK, Buscher, D, Martin, S, and Zwi, AB. Characteristics and impacts of sexual violence against men and boys in conflict and displacement: a multicountry exploratory study. J Interpers Violence. (2022) 37:NP7470–501. doi: 10.1177/0886260520967132
8. Green, L, McHale, T, Mishori, R, Kaljee, L, and Akter, CS. “Most of the cases are very similar.”: documenting and corroborating conflict-related sexual violence affecting Rohingya refugees. BMC Public Health. (2022) 22:700. doi: 10.1186/s12889-022-13038-7
9. Physicians for Human Rights. Where there is police, there is persecution: Government security forces and human rights abuses in Myanmar’s northern Rakhine state. New York, NY: Physicians for Human Rights (2016).
10. Physicians for Human Rights. Stateless and starving: Persecuted Rohingya flee Burma and starve in Bangladesh. Cambridge, Mass: Physicians for Human Rights (2010).
11. Strategic Executive Group. JRP for Rohingya humanitarian crisis: March-December 2018. (2018). Available from: https://reporting.unhcr.org/sites/default/files/JRP%20for%20Rohingya%20Humanitarian%20Crisis%20-%20March%202018.PDF (Accessed September 23, 2020).
12. Physicians for Human Rights. Situation Refugee Response in Bangladesh. Available from: https://data 2.unhcr.org/en/situations/myanmar_refugees (Accessed July 20, 2020).
13. Tay, AK, Riley, A, Islam, R, Welton-Mitchell, C, Duchesne, B, Waters, V, et al. The culture, mental health and psychosocial wellbeing of Rohingya refugees: a systematic review. Epidemiol Psychiatr Sci. (2019) 28:489–94. doi: 10.1017/S2045796019000192
14. Jubayer, F, Kayshar, S, Arifin, S, Parven, A, Khan, SI, and Meftaul, IM. Nutritional health of the Rohingya refugees in Bangladesh: conceptualizing a multilevel action framework focusing the COVID-19. Nutr Health. (2023) 30:21–5. doi: 10.1177/02601060231169372
15. Ritsema, H, and Armstrong-Hough, M. Associations among past trauma, post-displacement stressors, and mental health outcomes in Rohingya refugees in Bangladesh: a secondary cross-sectional analysis. Front Public Health. (2023) 10:1–20. doi: 10.3389/fpubh.2022.1048649
16. Shapna, KJ, Hasan, K, Kabir, KH, Li, J, and Hossain, ML. Water, sanitation and hygiene challenges of forcibly displaced Myanmar nationals in Rohingya camps in Bangladesh. J Water Health. (2023) 21:1385–403. doi: 10.2166/wh.2023.045
17. Anwar, A, Ali, ARMM, Yadav, UN, Huda, MN, Rizwan, AAM, Parray, AA, et al. Promotion of livelihood opportunities to address food insecurity in Rohingya refugee camps of Bangladesh. Glob. Public Health. (2024) 19:2295446. doi: 10.1080/17441692.2023.2295446
18. Palit, S, Yang, H, Li, J, Khan, MAS, and Hasan, MJ. The impact of the COVID-19 pandemic on the mental health of Rohingya refugees with pre-existing health problems in Bangladesh. Confl Heal. (2022) 16:10. doi: 10.1186/s13031-022-00443-3
19. Hossain, MA, Huda, MN, Ullah, AKMA, and Renzaho, A. Risk factors, contemporary challenges and psychological well-being of the Rohingya refugees in Bangladesh: policy implications. Int J Health Plann Manag. (2022) 37:1912–7. doi: 10.1002/hpm.3472
20. Chowdhury, SA, McHale, T, Green, L, Mishori, R, Pan, C, and Fredricks, I. Health professionals’ perspectives on the impact of COVID-19 on sexual and gender-based violence (SGBV) and SGBV services in Rohingya refugee communities in Bangladesh. BMC Health Serv Res. (2022) 22:743. doi: 10.1186/s12913-022-08122-y
21. Riley, A, Akther, Y, Noor, M, Ali, R, and Welton-Mitchell, C. Systematic human rights violations, traumatic events, daily stressors and mental health of Rohingya refugees in Bangladesh. Confl Heal. (2020) 14:60. doi: 10.1186/s13031-020-00306-9
22. United Nationa: Regional information center. Far from the headlines: Myanmar-the Rohingya crisis. (2024). Available from: https://unric.org/en/myanmar-the-rohingya-crisis/ (Accessed June 24, 2024).
23. Lindsay, Maizland. Myanmar’s troubled history: coups, military rule, and ethnic conflict. Counc Foreign Relat. (2022); Available from: https://www.cfr.org/backgrounder/myanmar-history-coup-military-rule-ethnic-conflict-rohingya (Accessed June 24, 2024).
24. AFP. Senior general min Aung Hlaing says new elections in two years. Frontier Myanmar. (2021); Available from: https://www.frontiermyanmar.net/en/senior-general-min-aung-hlaing-says-new-elections-in-two-years/ (Accessed June 24, 2024).
25. UN OCHA. Myanmar: escalation of conflict in Rakhine and southern Chin flash update. UN OCHA; (2022). Available from: https://reliefweb.int/report/myanmar/myanmar-escalation-conflict-rakhine-and-southern-chin-flash-update-5-september-2022 (Accessed June 24, 2024).
26. Thit, M. Military plans to force IDPs out of 25 camps in Rakhine State. Myanmar Now. (2023); Available from: https://myanmar-now.org/en/news/military-plans-to-force-idps-out-of-25-camps-in-rakhine-state/ (Accessed June 24, 2024).
27. UNHCR Regional Bureau for Asia and Pacific (RBAP). Myanmar emergency: external update. UNHCR; (2023). Available from: https://reliefweb.int/report/myanmar/unhcr-regional-bureau-asia-and-pacific-rbap-myanmar-emergency-external-update-10-april-2023 (Accessed June 24, 2024).
28. UN OCHA. Myanmar: Humanitarian Update No. 28. UN OCHA; (2023). Available from: https://themimu.info/sites/themimu.info/files/documents/Sitrep_Humanitarian_Update_No.28_OCHA_06Apr2023.pdf (Accessed June 24, 2024).
29. Dr. Nimrat Kaur. Denial of humanitarian assistance is a death sentence in Myanmar. The New Humanitarian. (2024); Available from: https://www.thenewhumanitarian.org/opinion/2024/06/11/denial-humanitarian-assistance-death-sentence-myanmar (Accessed June 24, 2024).
30. Chen, WT, Shiu, C, Lee, FR, Moolphate, S, and Aung, MN. Infrastructure collapsed, health care access disrupted, Myanmar people with chronic diseases are in danger. J Glob Health. (2023) 13:03002. doi: 10.7189/jogh.13.03002
31. UN Women, CARE. CARE rapid gender analysis Myanmar-Rakhine State. (2020). Available from: https://themimu.info/sites/themimu.info/files/assessment_file_attachments/Myanmar-RGA_Rakhine_CARE_4Aug2020.pdf (Accessed June 24, 2024).
32. Mundy, SS, Foss, SLW, Poulsen, S, Hjorthøj, C, and Carlsson, J. Sex differences in trauma exposure and symptomatology in trauma-affected refugees. Psychiatry Res. (2020) 293:113445. doi: 10.1016/j.psychres.2020.113445
33. Silove, D. The psychosocial effects of torture, mass human rights violations, and refugee trauma: toward an integrated conceptual framework. J Nerv Ment Dis. (1999) 187:200–7. doi: 10.1097/00005053-199904000-00002
34. Sudheer, N, and Banerjee, D. The Rohingya refugees: a conceptual framework of their psychosocial adversities, cultural idioms of distress and social suffering. Glob Ment Health. (2021) 8:1–15. doi: 10.1017/gmh.2021.43
35. Morse, JM. The significance of saturation. Qual Health Res. (1995) 5:147–9. doi: 10.1177/104973239500500201
36. Dedoose. Web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA: Socio Cultural Research Consultants, LLC (2020).
37. Medecins Sans Frontieres. Journeys of life and death: Rohingya refugees share their stories. (2018). Available from: https://www.doctorswithoutborders.org/latest/journeys-life-and-death-rohingya-refugees-share-their-stories (Accessed December 15, 2024).
38. Drožđek, B. Challenges in treatment of posttraumatic stress disorder in refugees: towards integration of evidence-based treatments with contextual and culture-sensitive perspectives. Eur J Psychotraumatol. (2015) 6:24750. doi: 10.3402/ejpt.v6.24750
39. Habib, M, Jubb, C, Ahmad, S, Rahman, M, and Pallard, H. Forced migration of Rohingya: An untold experience. Rochester, NY: Social Science Research Network (2018).
40. Christensen, LR, Ahsan, H, and Mandal, SK. Rohingya mHealth: investigating mental health in Kutupalong refugee camp. Intervention (2020) 18:99. doi: 10.4103/INTV.INTV_10_20,
41. Jeffries, R, Abdi, H, Ali, M, Bhuiyan, ATMRH, Shazly, ME, Harlass, S, et al. The health response to the Rohingya refugee crisis post august 2017: reflections from two years of health sector coordination in Cox’s bazar, Bangladesh. PLoS One. (2021) 16:e0253013. doi: 10.1371/journal.pone.0253013
42. Hossain, A, Baten, RBA, Sultana, ZZ, Rahman, T, Adnan, MA, Hossain, M, et al. Predisplacement abuse and Postdisplacement factors associated with mental health symptoms after forced migration among Rohingya refugees in Bangladesh. JAMA Netw Open. (2021) 4:e211801. doi: 10.1001/jamanetworkopen.2021.1801
43. Adrien, P, Francois, J, Parke, D, Bebekoski, T, Boncy, P, Corvil, S, et al. Establishing and utilizing strategic partnerships for vaccine-preventable diseases: best practices in Haiti. Infect Clin Pr. (2018) 26:252–7. doi: 10.1097/IPC.0000000000000644
44. UNHCR. UNHCR refugee statistics. Refugee data finder: Refugee hosting metrics. Available from: https://www.unhcr.org/refugee-statistics/insights/explainers/refugee-hosting-metrics.html (Accessed December 15, 2024).
45. Reihani, AR, Zimmerman, HG, Fernando, N, Saunders, DR, Edberg, M, and Carter, E. Barriers and facilitators to improving access to healthcare for recently resettled afghan refugees: a transformative qualitative study. J Health Soc Sci. (2021) 6:59–72. doi: 10.19204/2021/bbr5
46. Khanom, A, Alanazy, W, Couzens, L, Evans, BA, Fagan, L, Fogarty, R, et al. Asylum seekers’ and refugees’ experiences of accessing health care: a qualitative study. BJGP Open. (2021) 5:0059. doi: 10.3399/BJGPO.2021.0059
47. Mohiuddin, M, and Molderez, I. Rohingya influx and host community: a reflection on culture for leading socioeconomic and environmental changes in Bangladesh. Eur J Cult Manag Policy. (2023) 13:11559. doi: 10.3389/ejcmp.2023.11559
48. Center for Substance Abuse Treatment (US). Substance Abuse and Mental Health Services Administration. Understanding the impact of trauma. In: trauma-informed Care in Behavioral Health Services. Substance Abuse and Mental Health Services Administration (US); (2014). (Treatment Improvement Protocol (TIP) Series). Available from: https://www.ncbi.nlm.nih.gov/books/NBK207191/ (Accessed December 15, 2024).
49. Edberg, M, Benavides-Rawson, J, Rivera, I, Shaikh, H, Monge, R, and Grinker, R. Transnational determinants of health for central American migrants to the U.S.: results of a qualitative study. Glob. Public Health. (2021) 16:415–30. doi: 10.1080/17441692.2020.1779329
50. Kevers, R, Rober, P, Derluyn, I, and De Haene, L. Remembering collective violence: broadening the notion of traumatic memory in post-conflict rehabilitation. Cult Med Psychiatry. (2016) 40:620–40. doi: 10.1007/s11013-016-9490-y
51. Khan, S, and Haque, S. Trauma, mental health, and everyday functioning among Rohingya refugee people living in short-and long-term resettlements. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:497–512. doi: 10.1007/s00127-020-01962-1
52. Frost, R, Hyland, P, McCarthy, A, Halpin, R, Shevlin, M, and Murphy, J. The complexity of trauma exposure and response: profiling PTSD and CPTSD among a refugee sample. Psychol Trauma Theory Res Pract Policy. (2019) 11:165–75. doi: 10.1037/tra0000408
53. Schlaudt, VA, Bosson, R, Williams, MT, German, B, Hooper, LM, Frazier, V, et al. Traumatic experiences and mental health risk for refugees. Int J Environ Res Public Health. (2020) 17:1943. doi: 10.3390/ijerph17061943
54. Pumariega, AJ, Rothe, E, and Pumariega, JB. Mental health of immigrants and refugees. Community Ment Health J. (2005) 41:581–97. doi: 10.1007/s10597-005-6363-1
55. Assaf, SA, Nuwayhid, I, and Habib, RR. A conceptual framework on pre-and post-displacement stressors: the case of Syrian refugees. Front Public Health. (2024) 12:12. doi: 10.3389/fpubh.2024.1372334
56. Jahan, R, Amin, R, and Arafat, SMY. Practical challenges for mental health services among Rohingya refugee in Bangladesh. Asian J Psychiatr. (2024) 97:104069. doi: 10.1016/j.ajp.2024.104069
57. Haider, S, Maheen, A, Ansari, M, and Stolley, M. Health beliefs and barriers to healthcare of Rohingya refugees. J Racial Ethn Health Disparities. (2023) 10:1560–8. doi: 10.1007/s40615-022-01342-2
58. Elshazly, M, Budosan, B, Alam, ANMM, Khan, NT, and Ventevogel, P. Challenges and opportunities for Rohingya mental health and psychosocial support programming. Dermatol Int. (2019) 17:197. doi: 10.4103/INTV.INTV_49_19
59. Coventry, PA, Meader, N, Melton, H, Temple, M, Dale, H, Wright, K, et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: systematic review and component network meta-analysis. PLoS Med. (2020) 17:e1003262. doi: 10.1371/journal.pmed.1003262
60. Mahmuda, M, Miah, MAA, Elshazly, M, Khan, S, Tay, AK, and Ventevogel, P. Contextual adaptation and piloting of group integrative Adapt therapy (IAT-G) amongst Rohingya refugees living in Bangladesh. Dermatol Int. (2019) 17:149. doi: 10.4103/INTV.INTV_48_19
61. Dawson, KS, Bryant, RA, Harper, M, Kuowei Tay, A, Rahman, A, Schafer, A, et al. Problem management plus (PM+): a WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry. (2015) 14:354–7. doi: 10.1002/wps.20255
62. Epping-Jordan, JE, Harris, R, Brown, FL, Carswell, K, Foley, C, García-Moreno, C, et al. Self-help plus (SH+): a new WHO stress management package. World Psychiatry. (2016) 15:295–6. doi: 10.1002/wps.20355
63. Bolton, P, Bass, J, Betancourt, T, Speelman, L, Onyango, G, Clougherty, KF, et al. Interventions for depression symptoms among adolescent survivors of war and displacement in northern UgandaA randomized controlled trial. JAMA. (2007) 298:519–27. doi: 10.1001/jama.298.5.519
64. Fernandes, P, and Aiello, Y. Breaking the silence through MANTRA: empowering Tamil MAN survivors of torture and rape. Tor J Theol. (2018) 28:14–29. doi: 10.7146/torture.v28i3.111181
65. Einolf, C. Sexual torture among Arabic-speaking Shi’a Muslim men and women in Iraq: barriers to healing and finding meaning. Torture Q J Rehabil Torture Vict Prev Torture. (2018) 28:63–76. doi: 10.7146/torture.v28i3.111193
66. Tay, AK, and Silove, D. The ADAPT model: bridging the gap between psychosocial and individual responses to mass violence and refugee trauma. Epidemiol Psychiatr Sci. (2016) 26:142–5. doi: 10.1017/S2045796016000925
67. World Health Organization, Columbia University. Group interpersonal therapy (IPT) for depression (WHO generic field-trial version 1.0). WHO; (2016). Available from: https://www.who.int/publications-detail-redirect/WHO-MSD-MER-16.4 (Accessed March 16, 2022).
68. World Health Organization. Thinking healthy: a manual for psychosocial Management of Perinatal Depression. (WHO generic field-trial version 10) WHO; (2015). Available from: https://www.who.int/publications-detail-redirect/WHO-MSD-MER-15.1 (Accessed March 16, 2022).
Keywords: Rohingya, mental health, refugee mental health, humanitarian response, human rights, Myanmar, Bangladesh, sexual violence
Citation: Green L, Kaljee L, Chowdhury SA, McHale T, Mishori R, Fateen D and Sheth N (2025) Healthcare workers’ perspectives on trauma and mental health access for Rohingya refugees in Cox’s Bazar. Front. Public Health. 12:1458680. doi: 10.3389/fpubh.2024.1458680
Received: 02 July 2024; Accepted: 18 December 2024;
Published: 27 January 2025.
Edited by:
Thomas Wenzel, Medical University of Vienna, AustriaReviewed by:
Morufu Olalekan Raimi MNES, REHO, LEHO, FAIWMES, Federal University, NigeriaCopyright © 2025 Green, Kaljee, Chowdhury, McHale, Mishori, Fateen and Sheth. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lindsey Green, bGdyZWVuQHBoci5vcmc=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.