- 1School of Nursing and Health Studies, University of Missouri-Kansas City, Kansas City, MO, United States
- 2Department of Biomedical and Health Informatics, School of Medicine, University of Missouri-Kansas City, Kansas City, MO, United States
- 3Department of Pediatrics, School of Medicine, University of Missouri-Kansas City, Kansas City, MO, United States
- 4Health Services and Outcomes Research, Children's Mercy Kansas City, Kansas City, MO, United States
- 5Bloch School of Management, University of Missouri-Kansas City, Kansas City, MO, United States
- 6Department of Internal Medicine, University of Missouri-Kansas City School of Medicine, Kansas City, MO, United States
- 7Graduate School of the Stowers Institute for Medical Research, Kansas City, MO, United States
- 8Department of Internal Medicine, University Health, Kansas City, MO, United States
- 9Seattle Children's Research Institute, Seattle, WA, United States
- 10Department of Pediatrics, University of Washington School of Medicine, Seattle, WA, United States
- 11Social Determinants of Obesity and Cardiovascular Risk Laboratory, Cardiovascular Branch, Division of Intramural Research, National Heart, Lung, and Blood Institute, and Intramural Research Program, National Institute on Minority Health and Health Disparities, National Institutes of Health, Bethesda, MD, United States
- 12Center for Children’s Healthy Lifestyles and Nutrition, Kansas City, MO, United States
- 13Children’s Mercy, Kansas City, MO, United States
- 14The University of Kansas Medical Center, Kansas City, KS, United States
- 15BikeWalkKC, Kansas City, MO, United States
- 16Kansas City Area Transportation Authority, Kansas City, MO, United States
Population-level efforts are needed to increase levels of physical activity and healthy eating to reduce and manage chronic diseases such as obesity, cardiovascular disease, and type 2 diabetes. Interventions to increase public transit use may be one promising strategy, particularly for low-income communities or populations of color who are disproportionately burdened by health disparities and transportation barriers. This study employs a natural experiment design to evaluate the impacts of a citywide zero-fare transit policy in Kansas City, Missouri, on ridership and health indicators. In Aim 1, comparison to 9 similar cities without zero-fare transit is used to examine differential changes in ridership from 3 years before to 4 years after the adoption of zero-fare. In Aim 2, Kansas City residents are being recruited from a large safety net health system to compare health indicators between zero-fare riders and non- riders. Longitudinal data on BMI, cardiometabolic markers, and economic barriers to health are collected from the electronic health record from 2017 to 2024. Cross-sectional data on healthy eating and device-measured physical activity are collected from a subsample of participants as part of the study procedures (N = 360). Numerous baseline characteristics are collected to account for differences between Kansas City and comparison city bus routes (Aim 1) and between zero-fare riders and non-riders within Kansas City (Aim 2). Evidence on how zero-fare transit shapes population health through mechanisms related to improved economic factors, transportation, physical activity, and healthy eating among low-income groups is expected.
1 Introduction
Wide-reaching efforts are needed to increase population levels of physical activity and healthy eating in low-income groups for obesity and type 2 diabetes prevention/control. Some evidence suggests public transit can benefit health by creating opportunities for physical activity (e.g., walking to/from the bus) and improving access to healthy food and health services (1–7). Thus, approaches aiming to increase the reach and use of public transit have promise for improving population health. Transit-based opportunities may also support health equity given groups that have been economically or historically marginalized experience significant health disparities and rely more on public transit than their counterparts (8–12).
Previous research on the health impacts of transit policy/environmental changes has primarily focused on increasing access to transit via new or improved transit lines, such as the expansion of a bus line to rapid transit or construction of a new light rail line (13–17). Findings have been mixed. Some findings indicated no overall effect on transit use or overall physical activity (15–18), whereas others showed an increase in the proportion of nearby residents using transit (15), more walking around transit stops (19), improvements in overall physical activity and body mass index (BMI) among transit users (15), and a decrease in health care costs among some individuals (18). Gaps in previous research are that the type of policy or environmental changes investigated have been limited in scope (e.g., limited geographical coverage, only addressing new/expanded transit lines), and few studies have investigated impacts on economic barriers to health (18, 20) or health markers other than physical activity (15). Additionally, few studies have evaluated whether increases in transit use may correspond with unintended negative outcomes such as increased crime or pedestrian-related crashes (21–24).
Fare-free transit has been primarily studied outside the U.S., particularly for city-wide initiatives. Several studies have been conducted examining the city-wide, fare-free transit in Tallinn, Estonia (25–28). An increase in transit mode (25, 26) share and demand (27), a decrease in car use (25, 26), and increased mobility for lower-income groups (28) were associated with the fare-free policy. However, these studies are limited by the study design as there were no prospective studies and no studies included a control group. Studies on fare-free policies for specific populations (i.e., older adults, women) have found increases in physical activity among older adults (29–31), and increased access to jobs, improved income, and access to quality healthcare for women (20). To our knowledge, no studies have investigated the impacts of fare-free transit on BMI, obesity, or other cardiometabolic health markers.
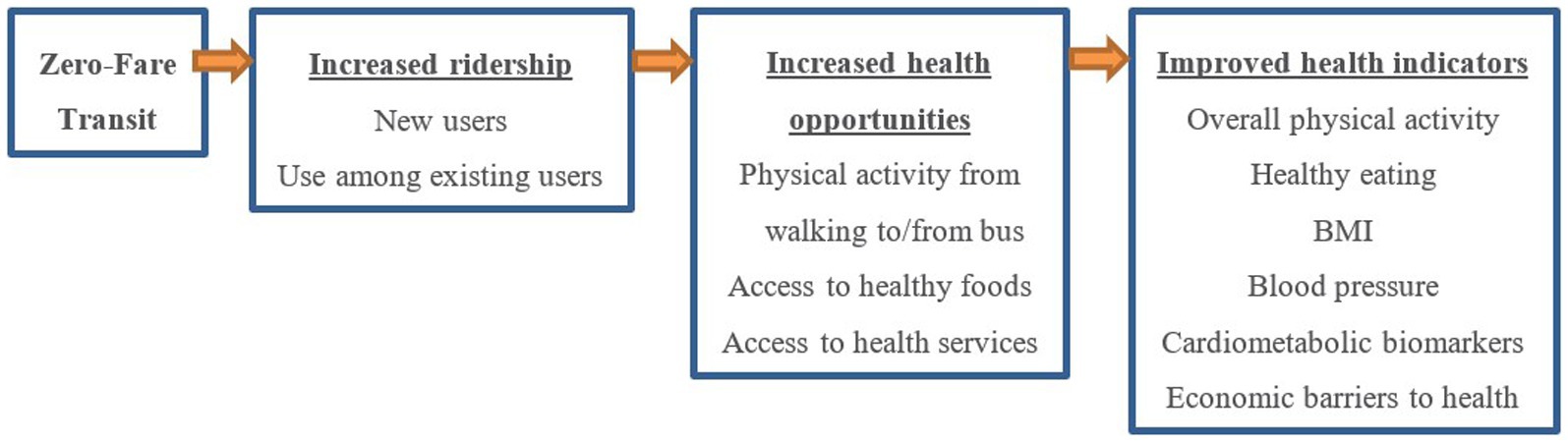
The current study aims to investigate one US city’s novel transit policy that eliminates bus fares for all users, referred to as zero-fare transit. In 2020, Kansas City, MO (KCMO), became the first major city in the U.S. to adopt an ongoing citywide zero-fare policy. This transit intervention differed from prior interventions in that it comprised a system-wide change largely intended to benefit low-income groups. As shown in Figure 1, zero-fare is posited to support increased ridership by providing a financial incentive (cost savings) for non-transit users to switch from using private vehicles to using the city bus for a portion of their trips (i.e., mode shift) and for existing transit users to use the city bus more often (i.e., increased mobility/access). Zero-fare riders may experience cardiometabolic health benefits through increased physical activity from walking to/from bus stops, increased access to health-related opportunities (e.g., places for engaging in healthy eating and active living, places for receiving health services), and reduced economic barriers to health (e.g., having sufficient money for transportation, medications, and nutrition). This publication presents the sample, design, and procedures for the Zero-Fare Bus Transit (ZBT) evaluation study. The ZBT study is testing the following aims:
1. To compare changes in bus ridership between Kansas City (zero-fare city) and non-zero-fare city bus routes.
2. To compare health indicators between zero-fare riders and non-riders.
2 Methods
2.1 Overview, design, and setting
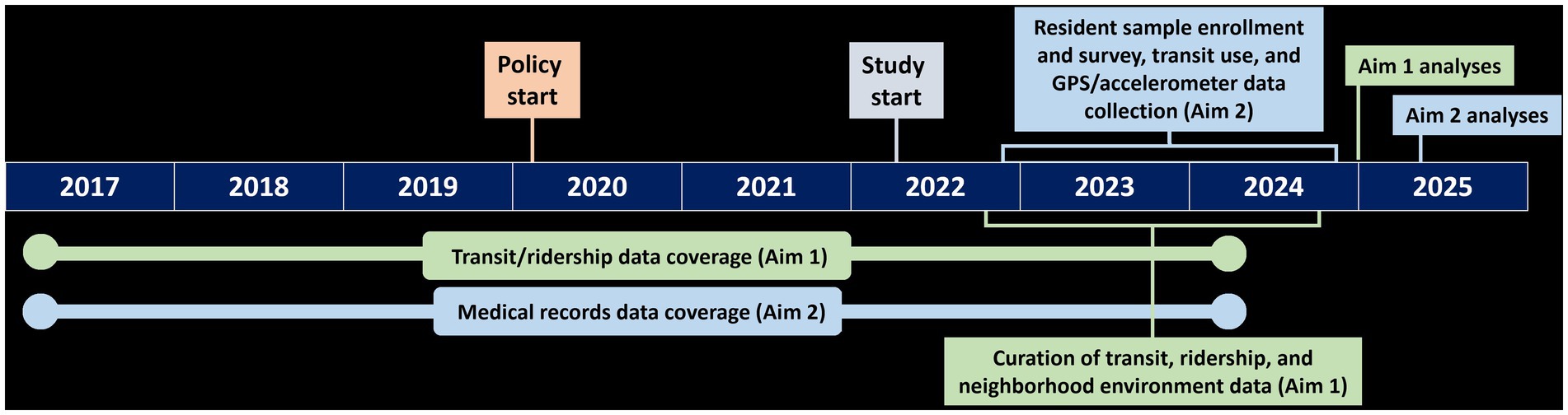
The ZBT study uses a quasi-experimental design. In Aim 1, longitudinal data from transit agencies are being used to compare ridership between KCMO bus routes (cases) and bus routes from comparison cities (controls). In Aim 2, KCMO residents are being enrolled to compare health indicators between zero-fare riders (i.e., those who use zero-fare bus transit; cases) and non-riders (controls) using longitudinal (i.e., BMI [primary outcome], biomarkers, economic barriers) and cross-sectional (i.e., physical activity, healthy eating) data. Given the quasi-experimental design, numerous neighborhood environment and transit characteristics (Aims 1–2) and participant characteristics (Aim 2) are being collected to account for baseline differences between the cases and controls. The study timeline (Figure 2) includes data spanning from 3 years prior to zero-fare to 4 years after. The 3-year baseline period helps show temporal trajectories in study variables prior to zero-fare and the 4-year follow up helps assess sustained impacts. The study was approved by the Institutional Review Boards at the sponsoring institutions and all study participants provided informed consent.
The zero-fare policy was adopted in March 2020 by the city of KCMO, which has a population of 491,158 residents and is the 6th largest city in the Midwest and 5th most economically and racially segregated city in the U.S. (32). As a result, communities in KCMO with a large proportion of non-White or Hispanic residents have a life expectancy up to 17 years lower than other communities (33). In 2019, the Kansas City Area Transportation Authority (KCATA) serviced 53 bus lines and an average daily weekday ridership of 33,000 trips. A majority of its service is provided within KCMO, with some routes extending to other cities in the metropolitan area. According to a 2019 KCATA Customer Survey, 44.5% of riders identified as Black, 28.5% as White non-Hispanic, and 9.3% as Hispanic; 67% did not have a working vehicle; 45% were between 13 and 32 years of age and 23% were between 33 and 42 years of age; 64% were male; and 77.1% had an annual income <$30 K. The city’s motivation to move to zero-fare was largely to improve transportation access, equity, and economic benefits among low-income communities, while also improving transit services by allowing for faster boarding and operations through fare elimination. All buses became zero-fare except for on-demand buses and a small number of micro-mobility services located outside of KCMO.
2.2 Sample and recruitment
2.2.1 Ridership sample (Aim 1)
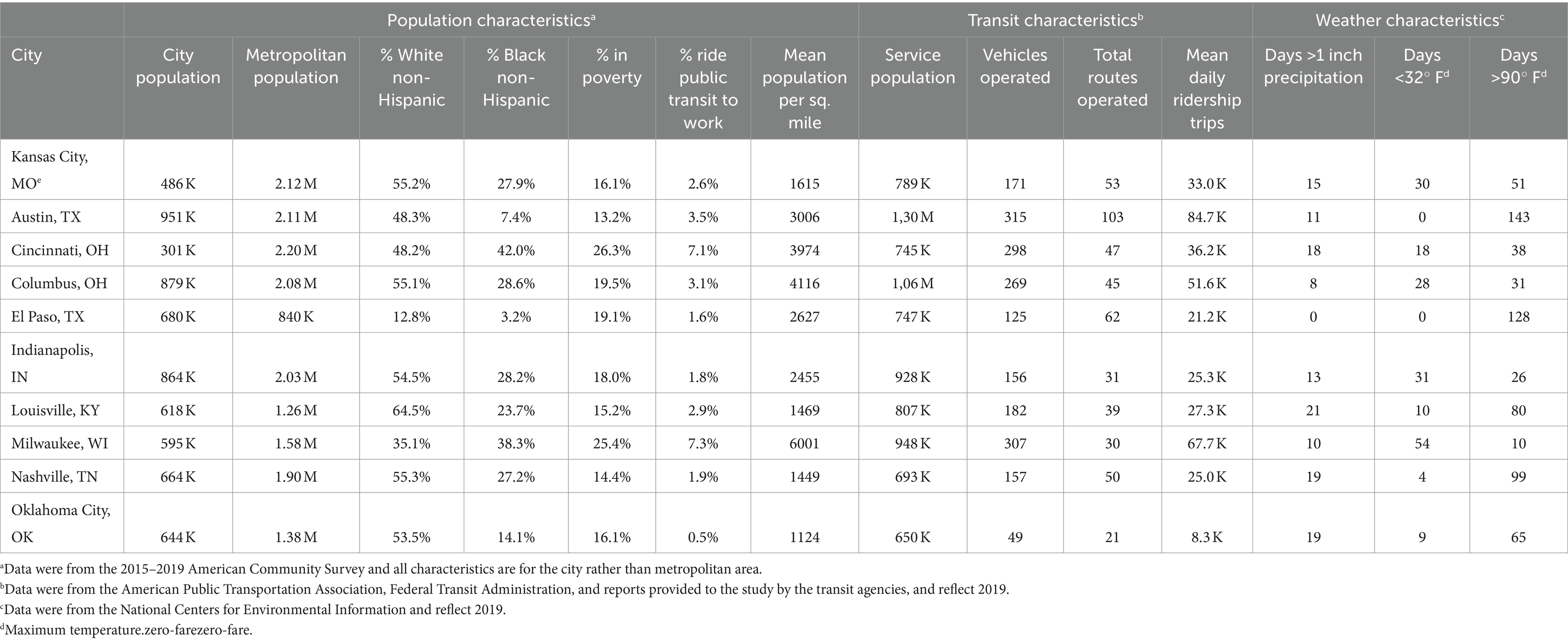
In partnership with the KCATA, the study team identified 9 cities that did not have a zero-fare policy and were comparable to KCMO across a number of demographic, transit, and climate characteristics (Table 1).
2.2.2 Resident sample and procedures (Aim 2)
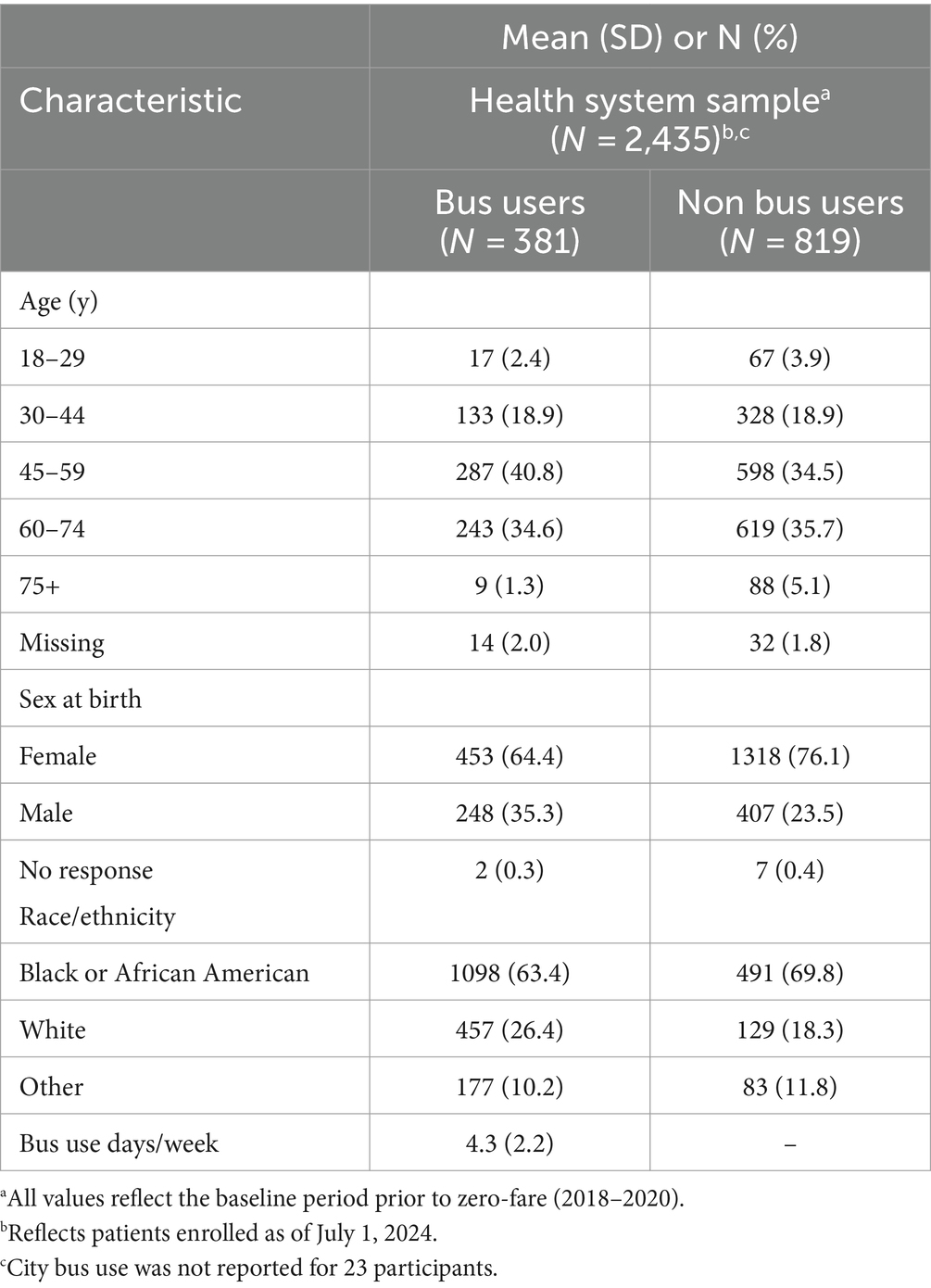
KCMO residents (Table 2) are being recruited from patients served by the University Health system, which is a large academic health system and safety-net provider in KCMO. The system comprises 10 hospital- and community-based primary care clinics located in the metropolitan area and serves a large portion of the city’s low-income residents. Patients are invited to participate if they reside in KCMO, are ≥18 years of age, speak English or Spanish, and had ≥1 visit to the health system between 3/1/2018 and 2/28/2020 and ≥ 1 visit between 4/1/2020 and 3/31/2022, which reflects the 2-year period before and after zero-fare began. Both visits must have included a weight and height measurement (to calculate BMI), not had a recorded pregnancy, and had a home address within the city limit. Recruitment spanned from December 2022 to December 2024, with a target goal of enrolling 480 bus users and ≥ 960 non-bus users. A total of 28,165 eligible patients were identified from the electronic health record and are being recruited through multiple contact methods (e.g., letters, phone calls, flyers). Participation involves completing a brief study survey to identify bus use. A subsample of 180 bus users matched to 180 non-bus users are invited to complete a second survey and an accelerometer assessment. Enrollment for this subsample is occurring from July 2023 to December 2024. Bus users are those who report using the KCATA city bus on ≥1 day during the past week. Propensity scores are used to identify matches (i.e., pairs of bus users and non-bus users to recruit into the subsample) based on sociodemographic characteristics and zip code as well as distance to the nearest bus stop, which are collected in the initial survey as detailed below. The propensity scores are computed using the R (34) package MatchIt (35).
2.3 Measures
2.3.1 Ridership and transit information (Aim 1)
The ridership data being collected from each city’s transit agency span March 1, 2017 to February 28, 2024, from 3 years prior to KCMO’s zero-fare policy to 4 years after. The data indicate, per each bus route, the number of unlinked passenger trips each month based on the number of riders boarding the bus. Yearly General Transit Feed Specification (36) data were then used to identify the route and associated bus stop locations to support geospatial analyses. At the end of the study period, a key informant from each transit agency is invited to complete a survey to capture more information about their transit system, including ridership tracking methods, bus fares, periods of zero-fare (e.g., start of pandemic), and major changes that occurred during the study period (e.g., new bus lines).
2.3.2 Neighborhood environment variables
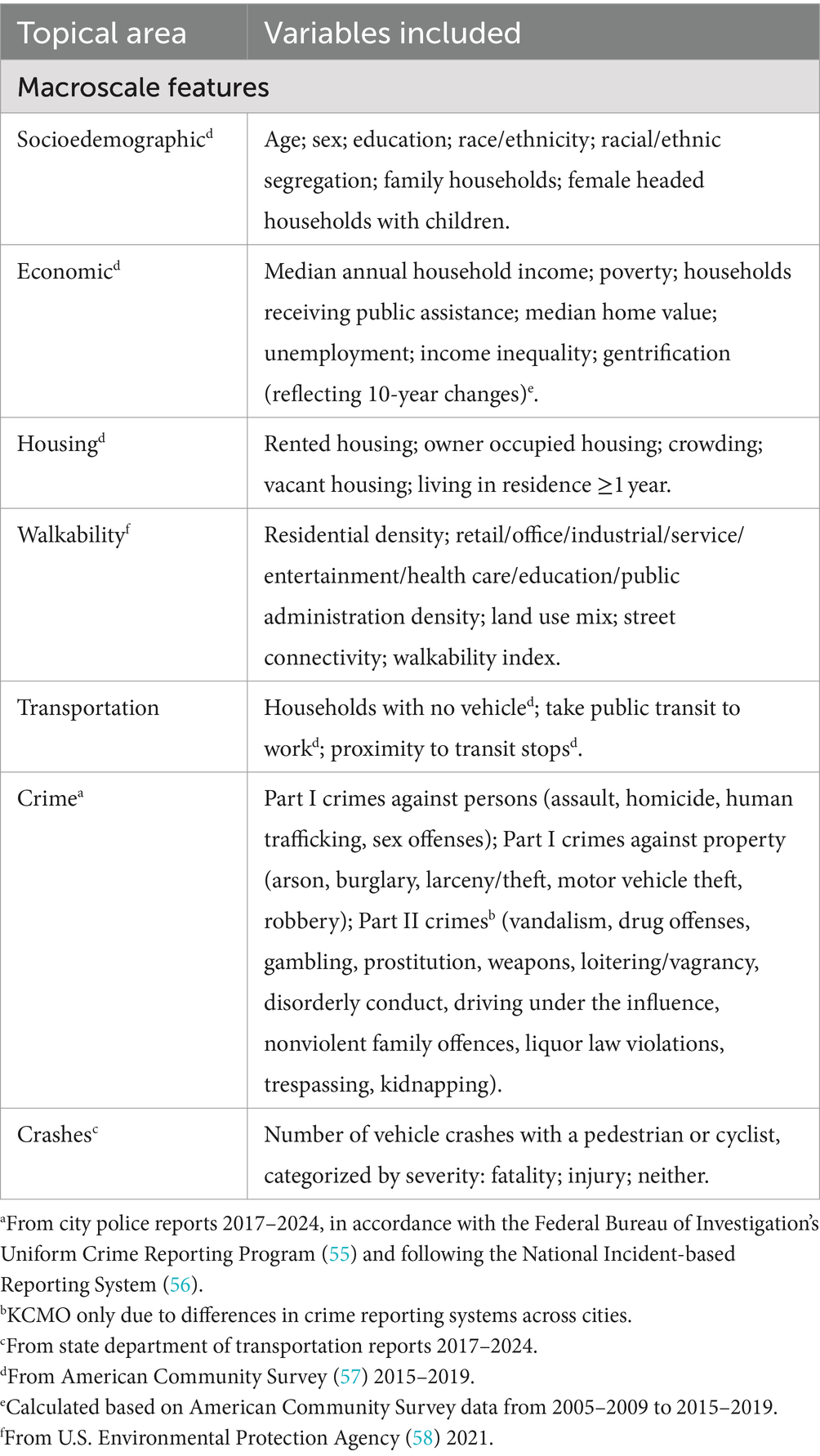
Neighborhood-level information on safety, built environment, and sociodemographic factors are being collected as detailed in Table 3. Variables were selected for inclusion based on their association with transit use or physical activity in prior research and availability and consistency across all included cities. All data except crime and crashes were collected from national sources. The crime and crash data were collected for each city with available data and processed to indicate the monthly number of crimes and crashes of different types. Geospatial analysis was performed to derive a version of each neighborhood variable that was specific to the included bus routes (Aim 1) and participant home addresses (Aim 2). The former set of variables were processed using a 500 m radial buffer around each bus stop in all included cities. The second set were based on a 500 m and 1 km street network buffer around each participant’s home.
2.3.3 Participant surveys (Aim 2)
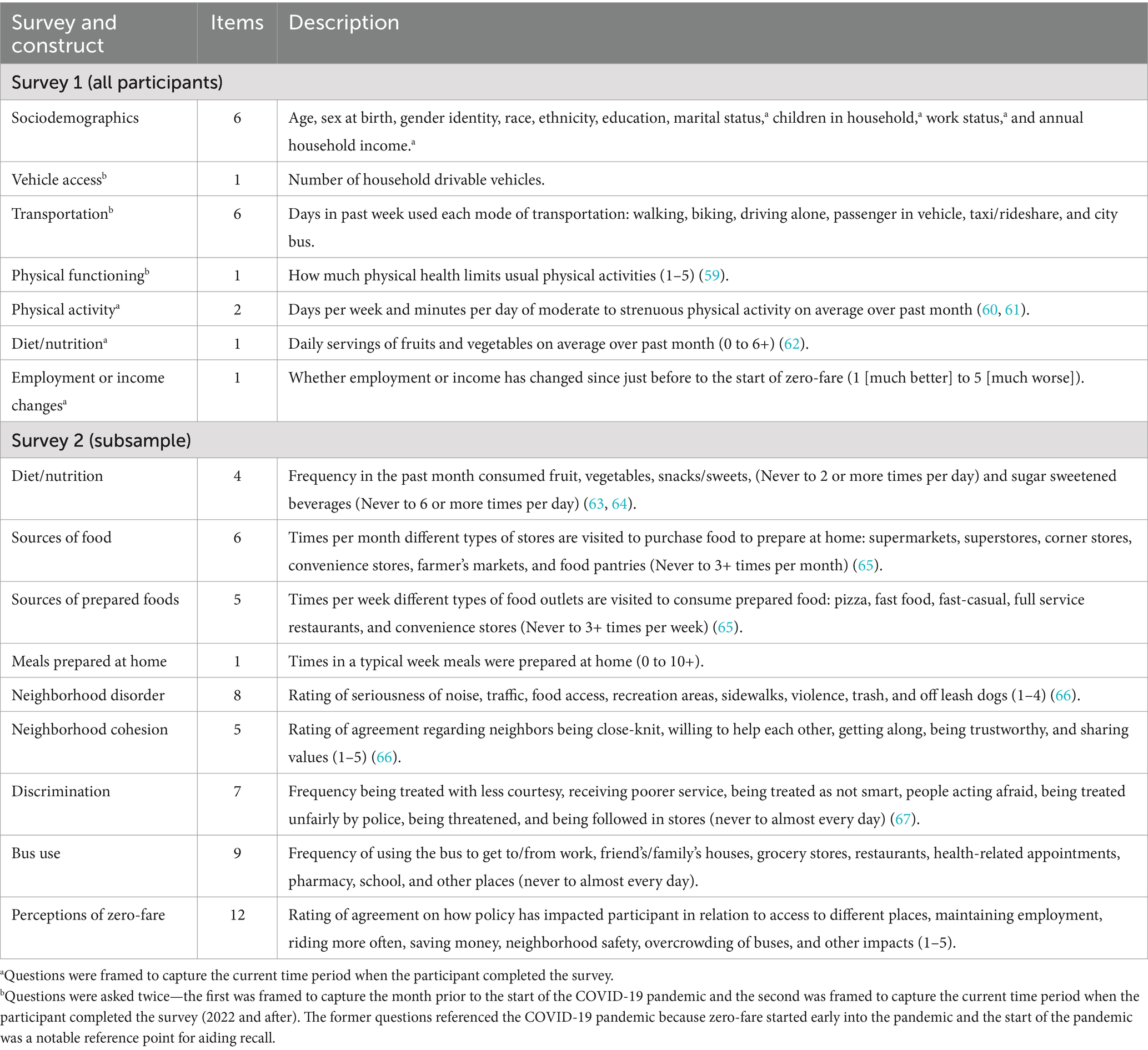
All participants are asked to complete Survey 1 (Table 4), which is primarily used to collect sociodemographic characteristics and bus use, and to identify participants to enroll into the 360-participant accelerometer subsample. Subsample participants are asked to complete Survey 2 to measure healthy eating (Aim 2) and factors to support exploratory analyses such as neighborhood perceptions, discrimination, destinations when using the bus, and perceptions of zero-fare.
2.3.4 Device-measured physical activity and trips (Aim 2 subsample)
Participants in the accelerometer subsample are instructed to wear an ActiGraph wGT3X-BT accelerometer (ActiGraph LLC, Pensacola, FL) on the right iliac crest and a QStarz BT-Q1000XT GPS monitor (QStarz, Taipei, Taiwan) (37, 38) attached to the same belt for 7 days during waking hours. Accelerometer nonwear is determined using the Choi algorithm with a 90 min window, 30 min streamframe, and 2 min tolerance (39). Days with ≥10 h of wear time are considered valid days (40, 41). Moderate-to-vigorous physical activity (MVPA) is scored using the widely accepted Freedson 60s cut points for adults (42). The GPS records participants’ geo-coordinates (latitude and longitude) every 30s a GPS satellite signal is available. Trips are identified using the Physical Activity Location Measurement System (PALMS) trip classification algorithms, which have good validity for assessing pedestrian, bicycle, and vehicle trips (43, 44). To distinguish bus trips from other vehicle trips and identify pedestrian and cycling trips occurring just before or after each bus trip the GPS data will be integrated with transit logs, as has been done in prior research (3), and with geospatial data for bus routes and bus stop locations. Because transit logs may be incomplete for some participants, we aim to develop a decision tree approach for categorizing whether each trip is bus related (yes/no) using only GPS and bus stop location data. The approach will be evaluated using transit logs and visual inspections of a subset of data. The final derived variables include daily minutes spent in MVPA, bus trips, vehicle trips (excluding bus trips), walking trips, bus-related walking trips, cycling trips, and bus-related cycling trips.
2.3.5 Transit log (Aim 2 subsample)
Participants in the accelerometer subsample also complete a transit log while wearing the study devices to record the number of bus trips they take each day, which will be integrated with the accelerometer and GPS data to identify missed and false trips.
2.3.6 Health markers and economic barriers to health (Aim 2 all participants)
Upon the completion of enrollment, participant data will be obtained from all clinic visits occurring from March 1, 2017 to February 28, 2024. Height, weight, blood pressure, cardiometabolic biomarkers (i.e., insulin, blood glucose, hemoglobin A1c, high- and low-density lipoprotein cholesterol, and triglycerides), and economic barriers to health were collected by University Health providers during patient visits as part of usual care and obtained through the electronic health record. BMI was calculated as kg/m2. The economic barriers survey asked patients whether over the past 12 months they have (1) missed doctor’s appointments or going to the pharmacy because of transportation barriers, (2) skipped medications to save money, and (3) eaten less than they thought they should because there wasn’t enough money for food. All responses were recorded as yes/no.
2.4 Statistical considerations
2.4.1 Analytic approach
Broadly, planned analyses involve two high-level considerations. First, inference of associations underlying each aim will be estimated utilizing generalized linear mixed models, to account for repeated timepoints (Aim 1), and nesting of participants within block groups (Aim 2). Second, synthetic controls will be generated specific to each aim for group-wise comparisons. This approach leverages a large sample of bus routes from non-zero-fare cities (Aim 1) and non-riders in KCMO (Aim 2) to create weighted (synthetic) control instances matched on baseline transit, neighborhood, and/or participant characteristics of the exposed/treatment group (45). The synthetic controls are used to account for differences between the cases and controls that arise from the quasi-experimental design. Additional models will be explored in which these baseline factors are adjusted as covariates.
To compare changes in bus ridership between Kansas City (zero-fare city) and non-zero-fare city bus routes in Aim 1, monthly route-level ridership will be modeled as a function of group (KCMO versus comparison cities), time (post- versus pre-zero-fare), and group × time interaction. Bus routes from the comparison cities, including their baseline ridership and macroscale neighborhood characteristics, will be used to create a synthetic comparison route for each KCMO bus route. Sensitivity analyses will be performed to comparing KCMO to each city individually and including baseline factors as covariates as opposed to creating synthetic controls.
To compare health indicators between zero-fare riders and non-riders in Aim 2, prospective analyses involve modeling participant BMI (primary), cardiometabolic markers, and economic barriers to health as a function of study group (zero-fare riders versus non-riders), time (post- versus pre-zero-fare), and group × time interaction. Among the accelerometer subsample, cross-sectional analyses (post-zero-fare) will model participant MVPA, travel behaviors, and healthy eating measures as a function of study group (zero-fare riders versus non-riders). Again, synthetic control and associated sensitivity analysis will be used based on the macroscale neighborhood factors shown in Table 3 and baseline participant characteristics collected in Survey 1.
2.4.2 Power
The study was powered based on Aims 1 and 2. All analyses are powered at 80% with an alpha level of 0.05 for two-tailed tests. For Aim 1, with 53 bus routes in KCMO and 53 synthetic control routes, the minimal detectable effect is an increase in ridership in KCMO by 1,200 daily riders (3.6%) as compared to the comparison cities. This assumes a correlation of 0.5 between pre- and post-zero-fare ridership and an ICC = 0.25 reflecting the repeated time points within bus routes (84 months within each route).
For Aim 2, power analysis indicated 480 bus users and at least as many non-bus users need to be enrolled in the health system sample to detect a minimal effect size of d = 0.31 in changes between group means. Given a standard deviation of 2.6 in BMI changes over time based on prior transit research (15), this effect size reflects a minimal detectable difference BMI change between groups (bus users and non-bus users) of 0.81 units. This assumes 25% attrition by 4-years post-baseline, a correlation of 0.5 between pre and post BMI, and an ICC of 0.10 based on prior studies of BMI and physical activity in participants nested within block groups (46, 47).
The minimal detectable effect size for MVPA, which is only collected at a single time point post-baseline, is d = 0.43 for the health system subsample of 360 participants assuming an ICC of 0.10. Based on a standard deviation of 30 min/day from prior studies of transit and non-transit users (3, 16, 48), this effect size equates to a difference of 13 min/day of MVPA between bus users and non-bus users.
3 Discussion
This study builds upon previous health-focused natural experiment transit studies that have capitalized on a large-scale public transit interventions (14, 15, 18, 19, 25, 49). Each of these previous studies examined health impacts of an expanded transit line rather than a city-wide initiative and therefore only have the capacity to impact a subsample of the city population. To our knowledge the present study is the first in the US to examine the health impacts of a city-wide transit initiative through a natural experiment study. Because the current study is examining a zero-fare initiative, the positive impacts may be greater than previous studies as the intervention may be more likely to be utilized by low-income populations compared to fee for service initiatives. We are using similar accelerometer and GPS measures of physical activity to three of the aforementioned studies (15, 48, 49). Our study is enhanced by our approach using synthetic controls to more accurately reflect a comparable control group.
Similar zero-fare transit policy interventions have been conducted outside of the U.S., with Tallinn, Estonia as the largest city globally with citywide zero-fare transit. While there are differences in the two cities’ populations, we expect similar outcomes. These outcomes include increase ridership, increase mode share of public transit, and decrease miles traveled by car (25, 26) and an increase in demand for public transit (27). The policy was also linked with decreases in transportation inequity, showing increased mobility among lower income groups (28). The results of the present study will expand upon the available evidence for citywide zero-fare transit by presenting the impact on health markers.
Several other cities have implemented zero-fare interventions for sub-groups of the populations, including zero-fare for older adults and college/university students. In several studies, transit use increased (50–52). For older adults, past studies suggest that access to zero-fare transit increases physical activity (29, 52, 53) and improves overall wellbeing and social connection (29, 52). We expect similar results for these sub-populations from this project.
3.1 Strengths and limitations
Study strengths include the use of a large sample of controls (comparison cities and non-riders) to support rigorous synthetic control methods accounting for baseline differences between groups (45); the inclusion of neighborhood sociodemographic, environment, and transit factors; and the use of historical ridership and electronic health record data to enable pre-post evaluations. Limitations include the inability to collect individual-level device-based measures of baseline (before zero-fare was implemented) physical activity and healthy eating, lack of health data from individual participants in comparison cities, and overlap between the study period and COVID-19 pandemic, which impacted health behavior, transit, and economic factors (54).
4 Conclusion
Large-scale policy and environment systems approaches are needed to increase opportunities for incorporating active living and healthy eating into the daily routines of individuals from disadvantaged communities. The ZBT study will provide novel information on how zero-fare transit shapes population health through mechanisms related to improved economic factors, transportation, physical activity, and healthy eating among low-income groups. In doing so, the study aims to inform the prioritization of health impacts in public policy decision making.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the University of Missouri-Kansas City Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because written consent was waived to increase confidentiality.
Author contributions
AG: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. JB-P: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. JA: Data curation, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. JL: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. KF: Methodology, Writing – original draft, Writing – review & editing. BN: Methodology, Writing – original draft, Writing – review & editing. BD: Data curation, Supervision, Writing – original draft, Writing – review & editing. BS: Writing – original draft, Writing – review & editing. TP-W: Writing – original draft, Writing – review & editing. LF: Writing – original draft, Writing – review & editing. CB: Project administration, Writing – original draft, Writing – review & editing. MP: Investigation, Writing – original draft, Writing – review & editing. KR: Investigation, Writing – original draft, Writing – review & editing. CS: Data curation, Writing – original draft, Writing – review & editing. EC: Data curation, Writing – original draft, Writing – review & editing. ER: Funding acquisition, Project administration, Resources, Writing – original draft, Writing – review & editing. CB: Resources, Writing – original draft, Writing – review & editing. JC: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Environmental Protection Agency (EC -97791001-0) and the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (R01DK132350). Powell-Wiley was funded by the Division of Intramural Research in the National Heart, Lung, and Blood Institute and the Intramural Research Program of the National Institute on Minority Health and Health Disparities.
Acknowledgments
The authors would like to thank the following groups and individuals for their contributions to this project: the study participants; Kansas City Area Transportation Authority; Kansas City Public Works; BikeWalkKC; the transit authorities from the other metropolitan areas included in this study; Coletta Hummel from BikeWalkKC; Carole Bowe Thompson, Sammi Ford, and Ryan Trickey from the University of Missouri-Kansas City; and Karynn Glover, Natalie Kane, Qianxia Jiang, Mallory Moon, Vincent Staggs, and Cory Yeager from Children’s Mercy.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Besser, LM, and Dannenberg, AL. Walking to public transit: steps to help meet physical activity recommendations. Am J Prev Med. (2005) 29:273–80. doi: 10.1016/j.amepre.2005.06.010
2. Lachapelle, U, Frank, L, Saelens, BE, Sallis, JF, and Conway, TL. Commuting by public transit and physical activity: where you live, where you work, and how you get there. J Phys Act Health. (2011) 8:S72–82. doi: 10.1123/jpah.8.s1.s72
3. Saelens, BE, Vernez Moudon, A, Kang, B, Hurvitz, PM, and Zhou, C. Relation between higher physical activity and public transit use. Am J Public Health. (2014) 104:854–9. doi: 10.2105/ajph.2013.301696
4. Farber, S, Morang, MZ, and Widener, MJ. Temporal variability in transit-based accessibility to supermarkets. Appl Geogr. (2014) 53:149–59. doi: 10.1016/j.apgeog.2014.06.012
5. Widener, MJ, Farber, S, Neutens, T, and Horner, M. Spatiotemporal accessibility to supermarkets using public transit: an interaction potential approach in Cincinnati, Ohio. J Transp Geogr. (2015) 42:72–83. doi: 10.1016/j.jtrangeo.2014.11.004
6. Abel, KC, and Faust, FM. Modeling food desert disruptors: impact of public transit systems on food access. (2018).
7. Syed, ST, Gerber, BS, and Sharp, LK. Traveling towards disease: transportation barriers to health care access. J Community Health. (2013) 38:976–93. doi: 10.1007/s10900-013-9681-1
8. Kuai, X, and Wang, F. Global and localized neighborhood effects on public transit ridership in Baton Rouge, Louisiana. Appl Geogr. (2020) 124:102338. doi: 10.1016/j.apgeog.2020.102338
9. Ogden, CL, Fakhouri, TH, Carroll, MD, Hales, CM, Fryar, CD, Li, X, et al. Prevalence of obesity among adults, by household income and education—United States, 2011–2014. MMWR Morb Mortal Wkly Rep. (2017) 66:1369–73. doi: 10.15585/mmwr.mm6650a1
10. Katz, SF, Rodriguez, F, and Knowles, JW. Health disparities in cardiometabolic risk among black and Hispanic youth in the United States. Am J Prevent Cardiol. (2021) 6:100175. doi: 10.1016/j.ajpc.2021.100175
11. Beckles, GL, and Chou, C-F. Disparities in the prevalence of diagnosed diabetes—United States, 1999–2002 and 2011–2014. Morb Mortal Wkly Rep. (2016) 65:1265–9. doi: 10.15585/mmwr.mm6545a4
12. Kim, S, Lee, B, Park, M, Oh, S, Chin, HJ, and Koo, H. Prevalence of chronic disease and its controlled status according to income level. Medicine. (2016) 95:e5286. doi: 10.1097/MD.0000000000005286
13. Frank, LD, Kuntz, JL, Chapman, JE, Fox, EH, Dickerson, JF, Meenan, RT, et al. The health and economic effects of light rail lines: design, methods, and protocol for a natural experiment. BMC Public Health. (2019) 19:1–13. doi: 10.1186/s12889-019-6518-6
14. Durand, CP, Oluyomi, AO, Gabriel, KP, Salvo, D, Sener, IN, Hoelscher, DM, et al. The effect of light rail transit on physical activity: design and methods of the travel-related activity in neighborhoods study. Front Public Health. (2016) 4:103. doi: 10.3389/fpubh.2016.00103
15. Brown, BB, Werner, CM, Tribby, CP, Miller, HJ, and Smith, KR. Transit use, physical activity, and body mass index changes: objective measures associated with complete street light-rail construction. Am J Public Health. (2015) 105:1468–74. doi: 10.2105/AJPH.2015.302561
16. Saelens, BE, Hurvitz, PM, Zhou, C, Colburn, T, Marchese, A, and Moudon, A. Impact of a light rail transit line on physical activity: findings from the longitudinal travel assessment and community (TRAC) study. J Transp Health. (2022) 27:101527. doi: 10.1016/j.jth.2022.101527
17. McCormack, GR, Ghoneim, D, Frehlich, L, Blackstaffe, A, Turley, L, and Bracic, B. A 12-month natural experiment investigating the impacts of replacing a traditional bus service with bus rapid transit on physical activity. J Transp Health. (2021) 22:101239. doi: 10.1016/j.jth.2021.101239
18. Wali, B, Frank, LD, Young, DR, Meenan, RT, Saelens, BE, Dickerson, JF, et al. Causal evaluation of the health effects of light rail line: a natural experiment. J Transp Health. (2022) 24:101292. doi: 10.1016/j.jth.2021.101292
19. Huang, R, Moudon, AV, Zhou, C, Stewart, OT, and Saelens, BE. Light rail leads to more walking around station areas. J Transp Health. (2017) 6:201–8. doi: 10.1016/j.jth.2017.02.002
20. Kiruthika, S, and Ravi, G. Impact of women free bus operation in Tamil Nadu state transport corporation (TNSTC) on Tamilnadu. Int J Early Childh Spec Educ. (2022) 14:1815–20. doi: 10.9756/intjecse/v14I5.189
21. Phillips, DC, and Sandler, D. Does public transit spread crime? Evidence from temporary rail station closures. Reg Sci Urban Econ. (2015) 52:13–26. doi: 10.1016/j.regsciurbeco.2015.02.001
22. Hess, PM, Moudon, AV, and Matlick, JM. Pedestrian safety and transit corridors. J Public Transp. (2004) 7:73–93. doi: 10.5038/2375-0901.7.2.5
23. Ridgeway, G, and MacDonald, JM. Effect of rail transit on crime: a study of Los Angeles from 1988 to 2014. J Quant Criminol. (2017) 33:277–91. doi: 10.1007/s10940-016-9296-7
24. Wu, Y, and Ridgeway, G. Effect of public transit on crime: evidence from SEPTA strikes in Philadelphia. J Exp Criminol. (2020) 17:267–86. doi: 10.1007/s11292-020-09416-z
25. Hess, DB. Decrypting fare-free public transport in Tallinn, Estonia. Case Stu Transport Policy. (2017) 5:690–8. doi: 10.1016/j.cstp.2017.10.002
26. Cats, O, Susilo, YO, and Reimal, T. The prospects of fare-free public transport: evidence from Tallinn. Transportation. (2017) 44:1083–104. doi: 10.1007/s11116-016-9695-5
27. Cats, O, Reimal, T, and Susilo, Y. Public transport pricing policy: empirical evidence from a fare-free scheme in Tallinn, Estonia. Transp Res Rec. (2014) 2415:89–96. doi: 10.3141/2415-10
28. Gabaldón-Estevan, D, Orru, K, Kaufmann, C, and Orru, H. Broader impacts of the fare-free public transportation system in Tallinn. Int J Urban Sustain Dev. (2019) 11:332–45. doi: 10.1080/19463138.2019.1596114
29. Jackson, SE, Firth, JA, Firth, J, Veronese, N, Gorely, T, Grabovac, I, et al. Social isolation and physical activity mediate associations between free bus travel and wellbeing among older adults in England. J Transp Health. (2019) 13:274–84. doi: 10.1016/j.jth.2019.03.006
30. Rambaldini-Gooding, D, Molloy, L, Parrish, A-M, Strahilevitz, M, Clarke, R, and Perez, P. Free public transport and older people: an ethnographic study of an Australian bus service. Australas J Ageing. (2023) 42:409–16. doi: 10.1111/ajag.13158
31. Webb, E, Laverty, A, Mindell, J, and Millett, C. Free bus travel and physical activity, gait speed, and adiposity in the English longitudinal study of ageing. Am J Public Health. (2016) 106:136–42. doi: 10.2105/AJPH.2015.302907
32. Urban Institute. Location and inequality: are the income gaps real? Available at: https://www.urban.org/urban-wire/location-and-inequality-are-income-gaps-real
33. Kansas City Health Department. Life expectancy by zip code. Available at: https://dashboards.mysidewalk.com/kansas-city-mo-chip-dashboard/
34. R Core Team. A language and environment for statistical computing R Foundation for Statistical Computing Available at: http://www.R-project.org.
35. Stuart, EA, King, G, Imai, K, and Ho, D. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. (2011) 42:1–28. doi: 10.18637/jss.v042.i08
36. OpenMobilityData. Available at: https://transitfeeds.com/
37. Schipperijn, J, Kerr, J, Duncan, S, Madsen, T, Klinker, CD, and Troelsen, J. Dynamic accuracy of GPS receivers for use in health research: a novel method to assess GPS accuracy in real-world settings. Front Public Health. (2014) 2:21. doi: 10.3389/fpubh.2014.00021
38. Hurvitz, PM, Moudon, AV, Kang, B, Saelens, BE, and Duncan, GE. Emerging technologies for assessing physical activity behaviors in space and time. Front Public Health. (2014) 2:2. doi: 10.3389/fpubh.2014.00002
39. Choi, L, Liu, Z, Matthews, CE, and Buchowski, MS. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. (2011) 43:357–64. doi: 10.1249/MSS.0b013e3181ed61a3
40. Troiano, RP. Large-scale applications of accelerometers: new frontiers and new questions. Med Sci Sports Exerc. (2007) 39:1501–1. doi: 10.1097/mss.0b013e318150d42e
41. Masse, LC, Fuemmeler, BF, Anderson, CB, Matthews, CE, Trost, SG, Catellier, DJ, et al. Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc. (2005) 37:S544–54. doi: 10.1249/01.mss.0000185674.09066.8a
42. Freedson, PS, Melanson, E, and Sirard, J. Calibration of the computer science and applications, Inc. accelerometer. Med Sci Sports Exerc. (1998) 30:777–81.
43. Carlson, JA, Jankowska, MM, Meseck, K, Godbole, S, Natarajan, L, Raab, F, et al. Validity of PALMS GPS scoring of active and passive travel compared with SenseCam. Med Sci Sports Exerc. (2015) 47:662–7. doi: 10.1249/mss.0000000000000446
44. Steel, C, Crist, K, Grimes, A, Bejarano, C, Ortega, A, Hibbing, PR, et al. Validity of a global positioning system-based algorithm and consumer wearables for classifying active trips in children and adults. J Meas Phys Behav. (2021) 4:321–32. doi: 10.1123/jmpb.2021-0019
45. Abadie, A, Diamond, A, and Hainmueller, J. Synthetic control methods for comparative case studies: estimating the effect of California’s tobacco control program. J Am Stat Assoc. (2010) 105:493–505. doi: 10.1198/jasa.2009.ap08746
46. Sallis, JF, Conway, TL, Cain, KL, Carlson, JA, Frank, LD, Kerr, J, et al. Neighborhood built environment and socioeconomic status in relation to physical activity, sedentary behavior, and weight status of adolescents. Prev Med. (2018) 110:47–54. doi: 10.1016/j.ypmed.2018.02.009
47. Frank, LD, Sallis, JF, Saelens, BE, Leary, L, Cain, K, Conway, TL, et al. The development of a walkability index: application to the neighborhood quality of life study. Br J Sports Med. (2010) 44:924–33. doi: 10.1136/bjsm.2009.058701
48. Knell, G, Durand, CP, Shuval, K, Kohl Iii, HW, Salvo, D, Sener, IN, et al. Transit use and physical activity: findings from the Houston travel-related activity in neighborhoods (TRAIN) study. Prev Med Rep. (2018) 9:55–61. doi: 10.1016/j.pmedr.2017.12.012
49. Li, W, Lee, C, Zhong, S, Xu, M, Towne, SD Jr, Zhu, X, et al. Examining the impacts of public transit on healthy aging through a natural experiment: study protocols and lessons learned from the active El Paso project. Front Public Health. (2023) 11:1132190. doi: 10.3389/fpubh.2023.1132190
50. Shin, EJ. Exploring the causal impact of transit fare exemptions on older adults’ travel behavior: evidence from the Seoul metropolitan area. Transp Res A Policy Pract. (2021) 149:319–38. doi: 10.1016/j.tra.2021.05.007
51. Reinhard, E, Carrino, L, Courtin, E, van Lenthe, FJ, and Avendano, M. Public transportation use and cognitive function in older age: a quasiexperimental evaluation of the free bus pass policy in the United Kingdom. Am J Epidemiol. (2019) 188:1774–83. doi: 10.1093/aje/kwz149
52. Zhang, Y, Yao, E, Zhang, R, and Xu, H. Analysis of elderly people's travel behaviours during the morning peak hours in the context of the free bus programme in Beijing, China. J Transp Geogr. (2019) 76:191–9. doi: 10.1016/j.jtrangeo.2019.04.002
53. Green, J, Jones, A, and Roberts, H. More than a to B: the role of free bus travel for the mobility and wellbeing of older citizens in London. Age Soc. (2014) 34:472–94. doi: 10.1017/S0144686X12001110
54. Lohse, B, Ramirez, A, Hickey, J, Bailey-Davis, L, Drees, B, Masters, KS, et al. Peer reviewed: changes in depressive symptoms, perceived stress, and food security among study participants with metabolic syndrome during a COVID-19–mandated research pause. Prev Chronic Dis. (2022) 19:E88. doi: 10.5888/pcd19.220206
55. History of and general information about the FBI's Uniform Crime Reporting (UCR) Program. Available at: https://ucr.fbi.gov/crime-in-the-u.s/2010/crime-in-the-u.s.-2010/aboutucrmain#:~:text=In%20January%201930%2C%20400%20cities,General%20to%20gather%20crime%20information
56. Ferderal Bureau of Investigation. National incident-based reporting system. Available at: https://www.fbi.gov/how-we-can-help-you/more-fbi-services-and-information/ucr/nibrs
57. United States Census Bureau. American Community Survey. Available at: https://www.census.gov/programs-surveys/acs
58. United States Enviromental Protection Agency. Smart location database version 3.0. smart location mapping. Available at: https://www.epa.gov/smartgrowth/smart-location-mapping
59. Ware, JE, Kosinski, M, Dewey, JE, and Gandek, B. How to score and interpret single-item health status measures: a manual for users of the SF-8 health survey. Lincoln. (2001) 15:5.
60. American College of Sports Medicine Physical activity vital sign. (2021). Available at: https://www.exerciseismedicine.org/assets/page_documents/The%20Physical%20Activity%20Vital%20Sign%20without%20Strength_2015_07_09_PDF.pdf
61. Kuntz, JL, Young, DR, Saelens, BE, Frank, LD, Meenan, RT, Dickerson, JF, et al. Validity of the exercise vital sign tool to assess physical activity. Am J Prev Med. (2021) 60:866–72. doi: 10.1016/j.amepre.2021.01.012
62. Peterson, KE, Hebert, JR, Hurley, TG, Resnicow, K, Thompson, FE, Greene, GW, et al. Accuracy and precision of two short screeners to assess change in fruit and vegetable consumption among diverse populations participating in health promotion intervention trials. J Nutr. (2008) 138:218S–25S. doi: 10.1093/jn/138.1.218S
63. National Cancer Institute. Dietary screener module (DTQ). Available at: https://epi.grants.cancer.gov/nhanes/dietscreen/questionnaires.html
64. Center for Disease Control and Prevention. Behavioral risk factor surveillance system (BRFSS). Available at: https://www.cdc.gov/brfss/pdf/fruits_vegetables.pdf
65. Saelens, BE, Sallis, JF, Frank, LD, Couch, SC, Zhou, C, Colburn, T, et al. Obesogenic neighborhood environments, child and parent obesity: the neighborhood impact on kids study. Am J Prev Med. (2012) 42:e57–64. doi: 10.1016/j.amepre.2012.02.008
66. Earls, FJ, Brooks-Gunn, J, Raudenbush, SW, and Sampson, RJ. Project on human development in Chicago neighborhoods: community survey, 1994–1995. (1999) doi: 10.3886/ICPSR02766.v3
Keywords: zero-fare transit, natural experiment, physical activity, social determinants of health, transportation
Citation: Grimes A, Berkley-Patton J, Allsworth JE, Lightner JS, Feldman K, Never B, Drees BM, Saelens BE, Powell-Wiley TM, Fitzpatrick L, Bowe Thompson C, Pilla M, Ross K, Steel C, Cramer E, Rogers E, Baker C and Carlson JA (2024) Impacts of zero-fare transit policy on health and social determinants: protocol for a natural experiment study. Front. Public Health. 12:1458137. doi: 10.3389/fpubh.2024.1458137
Edited by:
Ozgur Karcioglu, University of Health Sciences, TürkiyeReviewed by:
Andrew Kaczynski, University of South Carolina, United StatesHanish Kodali, City University of New York, United States
Tony Kuo, University of California, Los Angeles, United States
Copyright © 2024 Grimes, Berkley-Patton, Allsworth, Lightner, Feldman, Never, Drees, Saelens, Powell-Wiley, Fitzpatrick, Bowe Thompson, Pilla, Ross, Steel, Cramer, Rogers, Baker and Carlson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amanda Grimes, Z3JpbWVzYUB1bWtjLmVkdQ==
 Amanda Grimes
Amanda Grimes Jannette Berkley-Patton2
Jannette Berkley-Patton2 Joseph S. Lightner
Joseph S. Lightner Brent Never
Brent Never Brian E. Saelens
Brian E. Saelens Tiffany M. Powell-Wiley
Tiffany M. Powell-Wiley Lauren Fitzpatrick
Lauren Fitzpatrick Eric Rogers
Eric Rogers Jordan A. Carlson
Jordan A. Carlson