- 1Department of Social Work and Health, University of Emden/Leer, Emden, Germany
- 2Countway Library, Harvard Medical School, Harvard University, Boston, MA, United States
- 3Department of Palliative Care, Brandenburg Medical School Theodor Fontane (MHB), Brandenburg an der Havel, Germany
Background: Little is known about the mental health consequences of human rights violations in forcibly displaced populations. Objective: The objectives of this systematic review are to examine: (1) the prevalence of mental health conditions among forcibly displaced persons; (2) to investigate methodological factors contributing to mental health conditions; and (3) associations between mental health conditions and human rights violations.
Methods: We conducted a systematic review with meta-analyses on the prevalence of anxiety, depression, and posttraumatic stress disorder among forcibly displaced populations and factors contributing to it by searching in databases MEDLINE (Ovid), Embase, Web of Science Core Collection (Clarivate), PsycINFO (EBSCO), Sociological Abstracts (ProQuest), and PTSDPubs (ProQuest). Additionally, we assessed the Global Peace Index. Pooled associations were calculated using a random-effects meta-analysis model. Subgroup analyses were performed for the Global Peace Index, sampling methodology, also we assessed risk of bias.
Results: Of the 8,555 records screened, 55 with n = 31,573 participants met the inclusion criteria (n = 15,714 males, females, n = 15,859 females). Most studies were cross-sectional (n = 49). The pooled prevalence rates were 38.90% (95% CI: 29.63; 48.17) for anxiety, 38.16% (95% CI: 32.16; 44.15) for depression and 39.62% (95% CI: 32.87; 46.36) for posttraumatic stress disorder. Analyses by level of human rights violations show anxiety, and depression prevalence rates were higher in countries with very low Global Peace Index than countries with high, moderate and low Global Peace Index (39.84% vs. 16.09%; 41.07% vs. 26.67%). Analyses by risk of bias indicate that the prevalence rate of PTSD was higher in studies with a high risk of bias compared to those with a very high risk of bias (49.27% vs. 29.79%). For anxiety, the prevalence rate was greater with random sampling compared to convenience sampling (44.71% vs. 36.87%). Depression and PTSD prevalence rates were higher with convenience sampling than with random sampling (38.67% vs. 37.70%; 42.83% vs. 35.50%).
Conclusion: Our review suggests that systematic continuous human rights violations are associated with mental health conditions in forcibly displaced persons. To prevent mental health conditions, it is necessary to reduce exposure to human rights violations in the countries forcibly displaced persons come from.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42017076535, PROSPERO registration: CRD42017076535.
Introduction
Mental health conditions among forcibly displaced populations (FDPs) are a public mental health challenge given the prevalence of mental health conditions and the number of FDPs worldwide (1). Forcibly displaced persons include refugees as defined by the 1951 Refugee Convention (2). We use in this paper the term forcibly displaced persons as an umbrella term which includes refugees and asylum seekers. The number of FDPs was 89.3 million in 2021 (3) and is estimated to be more than 130 million by the end of 2024 (4). A broad range of factors contribute to mental health conditions among FDPs (5, 6). These factors are among other socioeconomic conditions including low household income and poverty (7), food insecurity (8), unemployment and job insecurity (9), financial difficulties (5), violence, conflicts and traumatic events including access to basic human rights such as secure housing and healthcare (10). However, studies suggest, heterogeneous prevalence rates of mental health conditions among FDPs between 1 and 77% for PTSD 4–74% for depression, and anxiety disorders between 2 and 50% (11). Yet, few studies investigated associations between human rights violations and mental health conditions of forcibly displaced persons. This could be because of human rights violations (e.g., restricting the freedom of movement and residence; freedom of thought, expression, religion; and rights to food, health, and livelihood, policies restricting the ability to marry, have children, or travel) have been assessed in few studies (12).
Human rights are fundamental entitlements inherent to every individual, irrespective of factors such as race, gender, nationality, ethnicity, language, or religion. These rights encompass essential freedoms, including the right to life, liberty, freedom from slavery and torture, freedom of expression, and access to education, work and health. They apply universally without any form of discrimination (13). To the best of our knowledge, no systematic review so far investigated the association of human rights violations with FDP’s mental health.
The objectives of this systematic review are therefore to evaluate (1) the prevalence of mental health conditions among FDPs; (2) investigate methodological factors contributing to study results; and (3) evaluate associations between mental health conditions and human rights violations. This study represents a novel contribution to the literature on FDPs mental health. This systematic review is registered with PROSPERO, identifier CRD42017076535.
Methods
Search strategy
In this systematic review and meta-analysis, undertaken according to both MOOSE and PRISMA standards, a health-science librarian (PB) developed the search strategy in consultation with the principal investigator (JL). The search included studies on forcibly displaced persons published until June 2022. We searched MEDLINE, Embase, PsycINFO, Scopus, and Web of Science for publications on FDPs and mental health conditions, as defined using a combination of keywords and controlled vocabulary terms applicable to each database in April 2017 and the search was updated in June 2022 (Supplementary Table 1), with no publication type or language restrictions at this stage. Articles with FDPs were identified using MeSH and text keywords for “FDPs,” while “mental health” content in articles was identified using MeSH and text keywords for “mental health” and specifically for “depression,” “anxiety,” and “PTSD.” These terms were adapted for each database. We supplemented the bibliographic database searches by checking the reference lists of identified relevant studies for additional relevant research. We managed the references using ENDNOTE 21.2 through which duplicates were removed. An additional search with a focus on individuals displaced by the war in Ukraine was was performed in the database PubMed in October 2024, however no study provided data on individuals fleeing from the territories occupied by Russia.
Inclusion and exclusion criteria
Firstly, we developed a study protocol. Based on the protocol, four reviewers (FS, PC, JL and HK) screened titles and abstracts of all potentially eligible publications. We excluded case reports, experimental studies, and studies with no prevalence information on mental health conditions, studies on internally displaced persons, study samples fewer than 100 participants, studies with clinical settings, studies on internally displaced populations as well as studies with populations aged below 18 years. All studies included at this stage were published in English, reported original research using an observational study design (cross-sectional or cohort) and with information on the mental health conditions (anxiety disorders; depressive disorders; trauma and stressor-related disorders). We chose this threshold to enable us to draw on the maximum amount of information in the current literature and to sample broadly to minimize bias. In the second step, following the above criteria, full-text articles were assessed for inclusion by the same reviewers and the same was followed for exclusion of studies. Disagreements between reviewers were solved by consensus (Supplementary Figure 1).
Data extraction
A standardized data extraction sheet was developed. We extracted (1) study characteristics (e.g., author, year of publication), (2) participants’ characteristics [e.g., age, gender, sample size(s)], (3) study participant’s country by origin and settlement, (4) study design, sampling method (5) measurements (e.g., exposure measure, adjustment/control of confounders, outcome measure for anxiety, depression and PTSD). Three reviewers (FS, PC, HK) extracted and cross-checked data independently for included full-text articles, including study information, participant characteristics, and information needed to calculate pooled estimates of prevalences for each co-occurring mental health condition.
Assessment of human rights violations
Human rights violations can be assessed in a variety of ways. We used an external dataset, the Global Peace Index (GPI). The GPI uses 23 quantitative and qualitative indicators and measures the status of peace across three domains: the level of societal safety and security, the extent of ongoing domestic and international conflict, and the degree of militarization. These indicators were first selected with the assistance of an expert panel in 2007 and are evaluated by the expert panel on a yearly basis. The scores for each indicator are standardized on a scale of 1–5, whereby qualitative indicators are banded into five groups, while quantitative ones are scored from 1–5 (14). The GPI ranks 172 states and territories (collectively accounting for 99.7 per cent of the world’s population) according to their levels of peacefulness. In the last years, the GPI showed an increase in violence and a decrease in peace (15).
Data analyses
Prevalence estimates of mental health outcomes are calculated with 95% confidence intervals (CIs) in the pooled data. Random-effects meta-analyses were calculated using the DerSimonian and Laird estimator based on inverse variance weights (16). Heterogeneity was anticipated because of between-study variations in study, design, sampling methods, country of origin, type of exposure and country of settlement. Hence random-effects meta-analysis was used to aggregate the prevalence rates. The heterogeneity among studies was described by I2-statistic. I2 is not affected by sample size and thus was considered useful for comparisons (17). Additionally, we evaluated potential sources of heterogeneity across studies in three subgroup analyses. First, we investigated the potential effects of human rights violations using the Global Peace Index ranking of countries. The indices of human rights violations were divided into three groups where low, moderate and high GPI countries were compared with very low GPI countries. Studies with samples from more than three countries were excluded from subgroup analysis by GPI in all three outcomes. Further, we analyzed the prevalence rates by risk of bias and sampling method (random and convenience sampling). All analyses were performed using Stata software version 18.5 [Stata Corp].
Sensitivity analysis
Sensitivity analysis was conducted based on the study quality or risk of bias for 55 studies included. The risk of bias was assessed by two reviewers (FS and PC) using a modified version of quality assessment for quantitative genocide studies (18). This tool evaluates eight domains: ethical approval, external validity and selection bias, misclassification bias, study design, confounders, data collection methods, withdrawals and dropouts, and data analysis. Each domain is rated as strong (1 point), moderate (2 points), or weak (3 points). Based on the cumulative score, studies are categorized into quality ratings: strong, moderate, weak, or very weak. Additionally, the risk of bias was determined based on these quality ratings, with strong-rated studies associated with very low to low risk, moderate-rated studies considered moderate risk, weak-rated studies indicating high risk, and very weak-rated studies reflecting very high risk of bias. We used this tool which is based on the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies (EPHPP), as it allows to evaluate the potential risk of bias for populations affected by mass violence and human rights violations (19).
In the subgroup analysis, we considered the level of human rights violations b by human rights violations by GPI score of the FDPs country of origin and study conducted year. We excluded studies that represented samples from more than three countries (20–27), and one study due to lack of GPI score (28). As a result, the number of studies in each subgroup was limited to the number of studies included in the meta-analysis. Therefore, subgroups in all three outcomes were merged when there were three or fewer studies in each category. Further, in anxiety subgroup analysis, study from Carta et al., 2018 (29) was not included due to negative lower bound confidence intervals in the prevalence rates for high, moderate and low GPI subgroups. This is likely because of the large prevalence within the studies in this category. After excluding this study, our analysis yielded a positive confidence interval and presented. In the subgroup analysis by sampling method, the study from Bogic et al., 2012 (28) was not included due to the mixed method sampling method.
Results
The search yielded 8,555 articles, with 611 articles being added from other sources. After abstract title and abstract screening, 8,314 records were excluded. Another 186 studies were excluded after full-text screening. Overall, 55 studies were included, providing data for 31,573 adult FDPs (Table 1). The additional search on individuals displaced by the war in Ukraine yielded 470 studies. Of those no study fulfilled the inclusion criteria. Supplementary Figure 1 shows the search, inclusion and exclusion process in detail. Characteristics including gender and age distribution, country of origin, study design, sampling strategy, exposure and exposure measures, outcome and outcome measures, confounder and confounder measures as well as prevalence rates of anxiety, depression and PTSD of selected studies are shown in Table 1. 18 of the 55 studies investigated anxiety, 38 depression and 41 PTSD. 49 studies used a cross-sectional study design (20–26, 28–70), three studies a longitudinal study design (27, 71, 72) and one study cohort study design (73) was used.
Country of origin of FDPs varied: with FDPs from Africa [Congo (31, 44), Eritrea (35, 73), Mali (29), Rwanda (55), Somalia (45, 72)]; eight studies from Asia [Bhutan (68), Cambodia (36), China (69), North Korea (47, 50, 53, 58), Sri Lanka (34)]; 28 studies from Middle East [Iran (72), Iraq (41, 54, 59, 64, 66, 70), Syria (30, 32, 33, 37–43, 46, 48, 49, 52, 54, 56, 57, 60–62, 65, 67, 71, 74), Afghanistan (72)], and two studies from Europe (Bosnia (63), former Yugoslavia (28)). The age range of participants ranged from 18 years to 97 years. All studies included male and female participants (49.83% vs. 50.17%) except one study which was conducted among Yazidi women in Iraq.
Anxiety, depression and PTSD were reported in 18, 38 and 41 studies, respectively. Most studies used diagnostic measures HTQ (27, 33, 36, 38–40, 42, 44, 46, 48, 60, 67, 68, 72) and HSCL (21, 23, 24, 26, 30, 36, 51, 54, 59, 64, 67–70). Studies also collected data on potential covariates such as socio-demographics (e.g., age, gender, education, marital status, employment status) (21–23, 25–51, 53–58, 60–72), religiosity (57), duration of displacement (49, 66), duration of stay in camp (51, 54), asylum duration (32, 48), family history of mental health diseases (32, 35), personal history of mental health treatment (30), mental health care use (25), difficulty in access to mental health care (27), migration status (23), social support (23, 44, 46), racism and food insecurity (23).
The studies Acarturk et al., 2020 (30) and Fuhr DC et al., 2019 (74) used the same sample and analyzed similar outcomes of anxiety, depression and PTSD. Therefore, only one study was included in the meta-analysis. In the studies by Gottvall et al., 2019 (46) and Tinghög et al., 2017 (67), although study samples were similar, the differences in exposure and outcome measurement scales, study outcomes, and prevalence rates justified the inclusion of both studies in the meta-analysis.
Anxiety among FDPs in included studies
Studies reporting anxiety disorders were 17 with a total of n = 9,407 FDPs. Of these studies, Bogic et al., 2012 (28) found the lowest prevalence rate of 8.67% (95% CI: 6.78; 10.55) in a study of n = 854 FDPs from former Yugoslavia living in Germany, Italy, United Kingdom (Figure 1). The highest prevalence of anxiety 74.82% (95% CI: 70.61; 79.02) was reported in a study by Carta et al., 2018 (29) of n = 409 FDPs from Mali living in Burkina Faso. The overall prevalence rate was 38.90% (95% CI: 29.63; 48.17) with a substantial heterogeneity of I2 = 99.08% between studies included in the meta-analysis.
Figure 1. Study authors, year, sample size, anxiety prevalence rate with 95% confidence intervals and random % weight. *Studies (Acarturk et al., 2020, Fuhr et al., 2019) were conducted using the same sample and analyzed the same outcomes, so only one study was considered for meta-analysis.
Depression among FDPs in included studies
A total of 37 studies investigated depression with a total number of participants of n = 21,706. For depression, the range of prevalence rate was broad among included studies reporting the lowest prevalence of 3.68% (95% CI: 0.51; 6.84) in a study Berthold et al., 2014 (36) of n = 136 FDPs from Cambodia to the highest prevalence rate of 71.65% (95% CI: 48.67; 79.49) in a study from Yang & Mutchler, 2020 (69) of n = 127 FDPs from China. The overall pooled prevalence rate was 38.16% (95% CI: 32.16; 44.15) showing a high heterogeneity of I2 = 99.18% (Figure 2).
Figure 2. Study authors, year, sample size, depression prevalence rate with 95% confidence intervals and random % weight. *Studies (Acarturk et al., 2020, Fuhr et al., 2019) were conducted using the same sample and analyzed the same outcomes. Therefore, only one study was considered for meta-analysis.
PTSD among FDPs in included studies
Overall, 40 studies reported PTSD in a study population n = 21,764 of which 8,007 forcibly displaced populations were diagnosed with PTSD with a pooled prevalence rate of 39.62% (95% CI: 32.87; 46.36). The lowest PTSD prevalence rates were reported in studies by both Rasmussen et al., 2012 (25) (n = 345) and Berthold et al., 2014 (36) (n = 136) with prevalence rates of 4.70% (95% CI: 3.08; 6.31) and 5.15% (95% CI: 1.43; 8.86) respectively. The highest prevalence rate of 87.68% (95% CI: 84.12; 91.26) was found in a study by Ainamani et al., 2020 (31) of n = 325 FDPs from DRC. There was substantial heterogeneity between studies reporting PTSD (I2 = 99.60%; Figure 3).
Figure 3. Study authors, year, sample size, PTSD prevalence rate with 95% confidence intervals and random % weight. *Studies (Acarturk et al., 2020, Fuhr et al., 2019) conducted using the same sample and analyzed the same outcomes. Therefore, only one study was considered for meta-analysis; **Studies conducted using the same sample with different outcomes.
Subgroup analysis by study and sample characteristics
Human rights violations by GPI ranking and mental conditions among FDPs
For countries with very low GPI, the prevalence of anxiety was 39.84% (95% CI: 34.20; 45.49) compared to countries with high, moderate and low GPI, where the prevalence of anxiety was 16.09% (95% CI: 10.83; 21.35). The test of group difference yielded a Chi-square statistic of 36.40, (p = <0.05) indicating a significant difference in anxiety prevalence rates between these two groups (Figure 4).
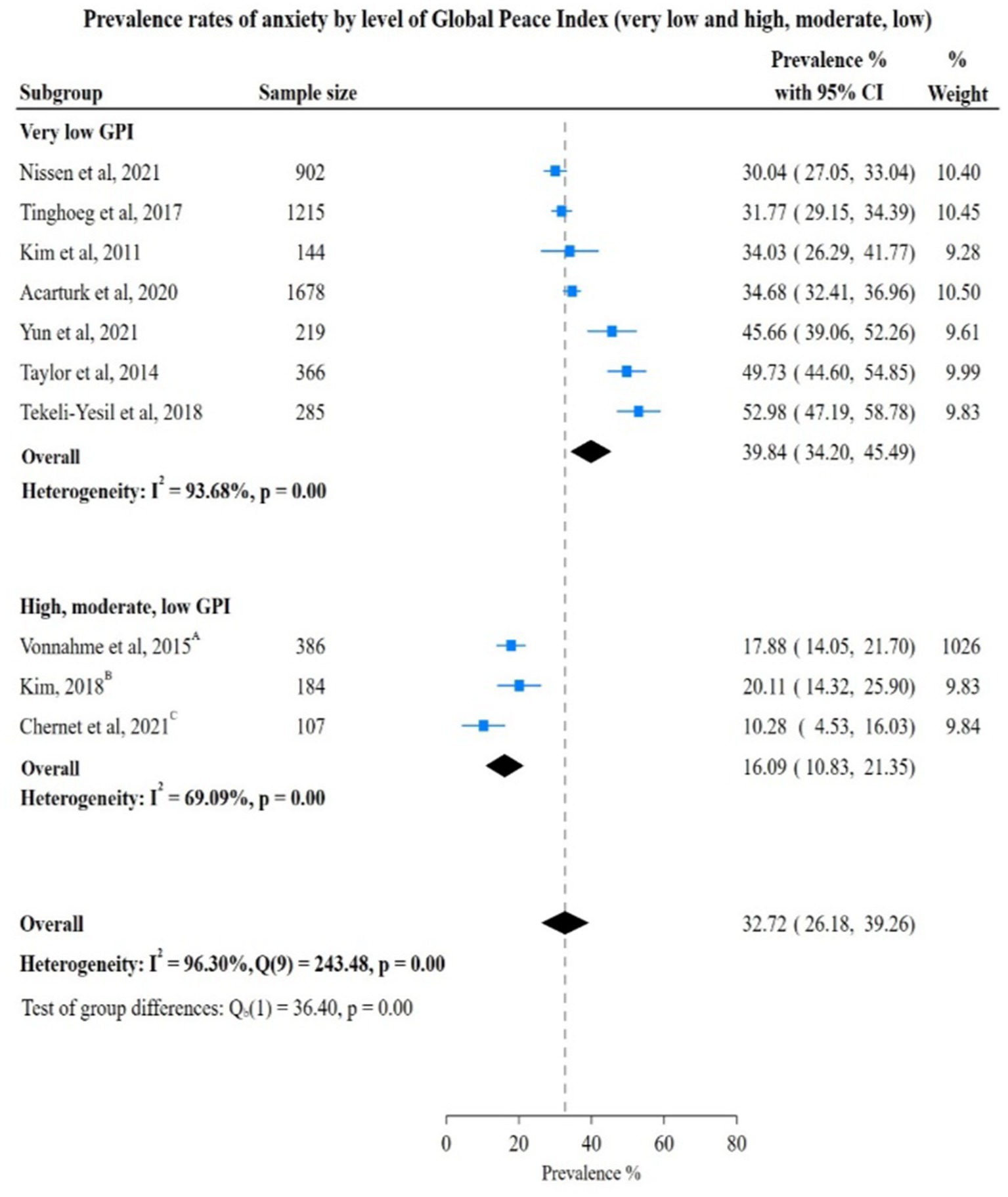
Figure 4. Study authors, year, sample size, anxiety prevalence rates with 95% confidence intervals and random % weight by very low versus all other categoreis of GPI. GPI, Global Peace Index; AHigh GPI; BModerate GPI; CLow GPI.
Depression prevalence rate among countries with very low GPI was higher at 41.07% (95% CI: 32.03%; 50.12%) than the pooled rate of depression in low GPI countries at 26.67% (95% CI: 9.74%; 43.60%). The difference in the pooled rate was not significant between very low GPI vs. moderate, high GPI countries 40.00% (95% CI: 31.05; 48.95) vs. 41.30% (95% CI: 22.67; 59.92). However, the test for group differences was not statistically significant [very low vs. low: Chi-square 2.16, (p = 0.14); very low vs. moderate and high: Chi-square 0.02, (p = 0.90)], showing no significant difference in depression prevalence rates between these subgroups (Figures 5, 6).
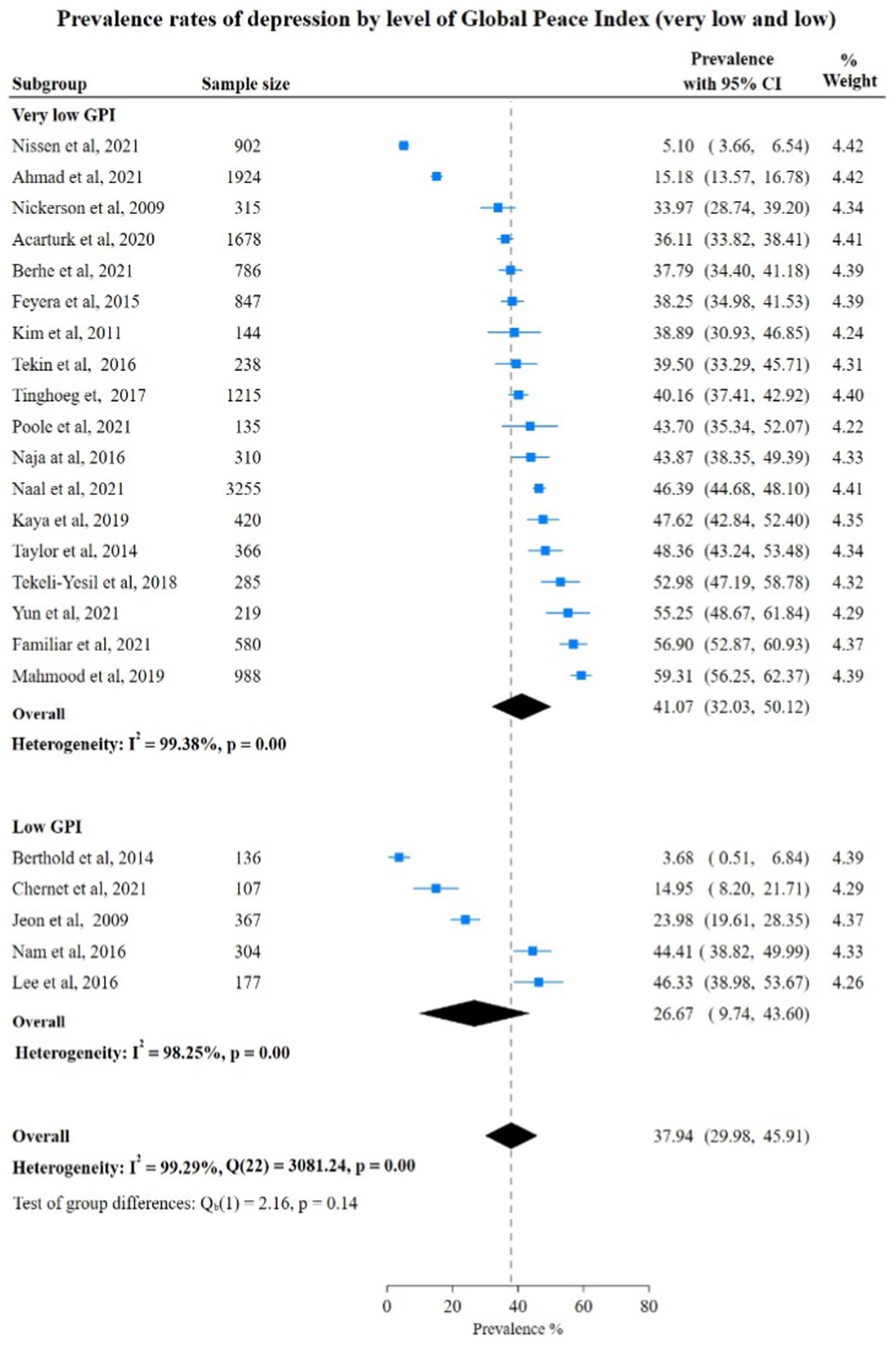
Figure 5. Study authors, year, sample size, depression prevalence rates with 95% confidence intervals and random % weight by very low versus versus low GPI. GPI, Global Peace Index.

Figure 6. Study authors, year, sample size, depression prevalence rates with 95% confidence intervals and random % weight by very low versus moderate, high categoreis of GPI. GPI, Global Peace Index; AModerate GPI; BHigh GPI.
In contrast to anxiety and depression, PTSD prevalence rates were higher in countries with moderate and high GPI than in countries with low GPI at 48.41% (95% CI: 5.18; 91.64), 40.58% (95% CI: 31.13; 50.02) respectively. Also, the pooled rate in low GPI countries was 39.32% (95% CI: 6.14%; 72.91%) which did not show a significant difference from the pooled rate of PTSD in very low GPI countries. However, the test for group differences was not statistically significant (very low vs. low: Chi-square 40.40, p = 0.95) very low vs. moderate and high: Chi-square 41.66, (p = 0.73), indicating no significant difference in PTSD prevalence rates between various subgroups (Figures 7, 8).
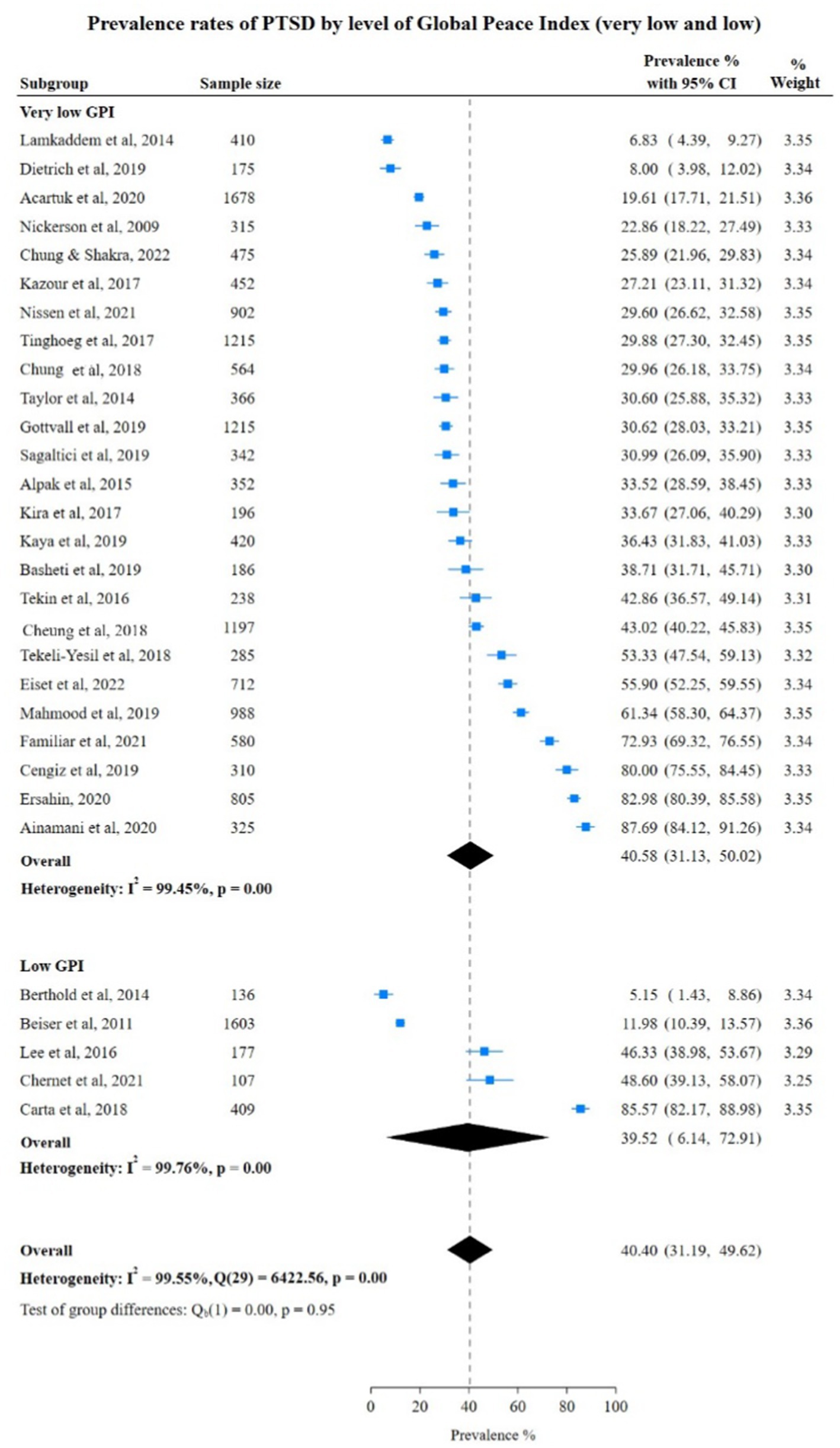
Figure 7. Study authors, year, sample size, PTSD prevalence rates with 95% confidence intervals and random % weight by very low versus low GPI. GPI, Global Peace Index.
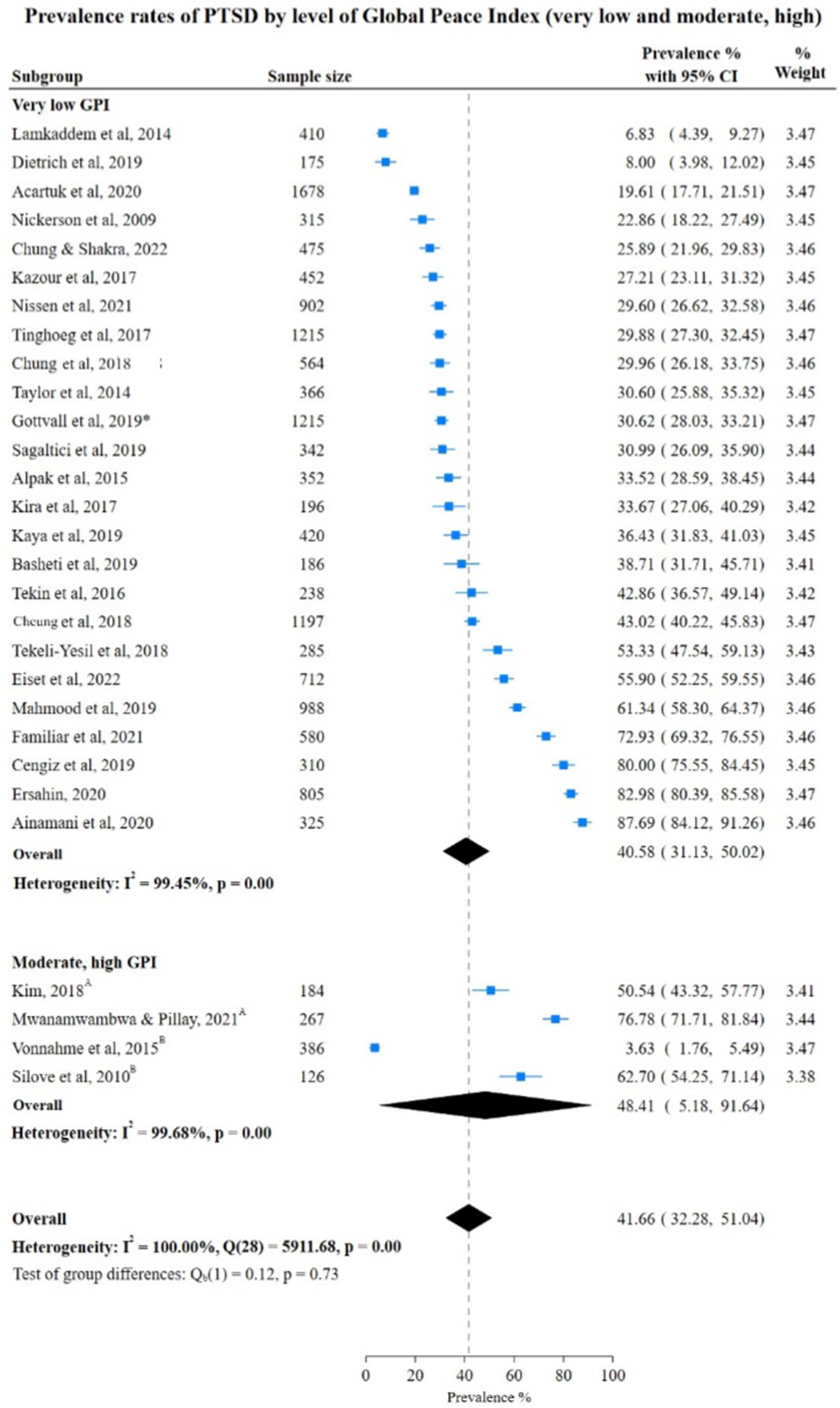
Figure 8. Study authors, year, sample size, PTSD prevalence rates with 95% confidence intervals and random % weight by very low versus low GPI. GPI, Global Peace Index; AModerate GPI; BHigh GPI.
Prevalence rates of mental health conditions in FDPs by risk of bias
We compared prevalence rates of anxiety and depression by risk of bias probability (moderate and low vs. high and very high) (Supplementary Figures 2–6). For anxiety we did not identify differences by risk fo bias subgroups (p = 0.74 for anxiety and p = 0.30 for depression).
For PTSD, overall prevalence was high in the high risk of bias subgroup at 49.27% (95% CI: 37.18; 61.35). Also, a comparison between the risk of bias subgroups, very high vs. high, revealed a pooled rate of 42.12% (95% CI: 31.66; 52.59) with a Chi-square statistic of 4.55, (p = 0.03) indicating a significant difference in PTSD prevalence rates between these two groups. Whereas comparison of the risk of bias subgroups, very high vs. moderate and low, showed a pooled rate of 32.23% (95% CI: 23.39; 41.07) and a non-significant difference in PTSD prevalence rates between these two groups with a Chi-square statistic of 0.42, (p = 0.52; Supplementary Figures 7, 8).
Prevalence rates of mental health conditions in FDPs by study sampling methods
Comparison of prevalence rates of anxiety, depression and PTSD by sampling methods (random and convenience) showed no significant difference: anxiety 40.79% (95% CI: 32.84; 48.75) Chi-square statistic 0.92, (p = 0.34); depression 38.27% (95% CI: 32.09; 44.45), Chi-square statistic 0.02 (p = 0.88); PTSD 40.01% (95% CI: 31.79; 48.23), Chi-square statistic 0.75, (p = 0.39; Supplementary Figures 9–11).
However, observation of prevalence rates by individual sampling method showed that anxiety prevalence rates by random sampling was 44.71% (95% CI: 32.08; 57.35) which was higher than the overall anxiety prevalence of 38.90 (95% CI: 29.63; 48.17). Whereas PTSD prevalence rate was higher by convenience sampling at 42.83% (95% CI: 31.23, 54.44) compared to the overall PTSD prevalence of 39.62% (95% CI: 32.87; 46.36). Similarly, for depression, there was a slight difference in prevalence rate between by the convenience sampling method of 38.67% (95% CI: 30.45; 46.89) and the depression pooled rate of 38.16% (95% CI: 32.16; 44.15).
Discussion
In this systematic review with meta-analysis, we found pooled prevalence rates of 38.90% for anxiety, 38.16% for depression and 39.62% for PTSD in FDPs. Additionally, the study results also showed a positive association between the level of peace in the country of origin and the mental health conditions of FDPs. For countries with very high human rights violations, prevalence rates of anxiety (39.84%), depression (41.07%) and PTSD (40.58%) were higher compared to countries with low human rights violations. These findings underscore that repeated and enduring human rights violations, rather than isolated traumatic event, contribute substantially to psychopathology and related findings are suggested by studies on the impact of child maltreatment (75, 76).
The experience of multiple traumatic events can be assumed in states of human rights violations. This is in line with studies suggesting that the number of traumatic events is a main predictor of mental health conditions (77, 78). These associations are potentially mediated by neurobiological mechanisms (79) involving changes in the hypothalamic–pituitary–adrenal (HPA) axis activity. Stress events stimulate the HPA axis and sympathetic nervous system (SNS), resulting in an increase in cortisol, alpha-amylase, and heart rate (80), which is positively associated with increased levels of heart rate, mood changes also mental health (81–83).
For the first time ever to the best of our knowledge, we identified an association between the level of human rights violations and the prevalence of anxiety, depression, and PTSD. Human rights violations can be understood as an act of exclusion disrupting the individual’s sense of safety and belonging in society making them more vulnerable to mental health conditions. Human rights violations have been found to be significant determinants of poor mental health in some populations but are outside the usual scope of psychiatric and social epidemiology (84). Few studies have advocated a comprehensive assessment of human rights violation’s impact on health (85, 86). Our findings challenge the traditional understanding of refugee health, which often emphasizes traumatic experiences during forced migration over political and social determinants embodied prior to displacement.
Furthermore, in the subgroup analysis based on risk of bias, studies with moderate and low risk of bias showed higher prevalence rates of anxiety (40.76%). However, the number of studies meeting the criteria for subgroup analysis was limited. On the other hand, for depression and PTSD, studies with a high risk of bias had higher prevalence rates (43.34 and 49.27%) compared to studies with a very high risk of bias. The difference could be due to the higher number of studies qualifying for the high risk of bias category. In the subgroup analysis based on study sampling methods, anxiety prevalence rate was high (44.71%) by random sampling while the prevalence rate of PTSD (42.83%) was high by convenience sampling.
The study is not without limitations, including reliance on self-report measures at a single time point, lack of data on the duration and timing of human rights violations, and potential exclusion of relevant studies.
We did an additional search on individuals fleeing from territories occupied by Russia. However, due to the difficulties in the territories occupied by Russia no study provided data on refugees from these areas. In case of countries occupied it is almost impossible to conduct a representative study. Recent studies on the impact of the Ukraine conflict from the occupied territories are not available. In the future it might be possible to use technology for collecting real time data in territories occupied. However, these data can only be obtained if data protection and safety of the study participants is possible. We acknowledge that new wars, such as the war in Ukraine and in Sudan, are happening at the moment. The current review aimed to synthesize data from the time period January1994 – June 2022. As it is difficult to keep up to date as new wars are emerging almost on a regular basis we acknowledge that our review might provide knowledge for a certain time period (January 1994 – October 2024) and needs a regular update. Further approaches such as a living systematic review may build on our review. This living review could evaluate the association of human rights violations and mental health conditions and integrate continuously data on emerging human rights violations. One limitation of the review is that we did not include grey literature which could include further groups of forcibly displaced persons. Further research could involve conducting a systematic search of the grey literature. Grey literature could help incorporate information about additional groups of forcibly displaced individuals.
Additionally, we conducted subgroup analyses to investigate potential sources of heterogeneity. Subgroups were combined when the number of studies in each subgroup category was less than four which would have affected the pooled prevalence rates and effect sizes in corresponding analysis. Also, some subgroup analyses were not feasible due to a lack of data availability. Furthermore, our review might have missed some relevant studies. Nevertheless, our review provides the first empirical evidence on the association between human rights violations and mental health conditions. Future research should expand the scope of assessment to include detailed information on the nature, duration, and type of human rights violations. Additionally, further studies are needed to interpret the pathways through which human rights violations impact mental health and to address the existing knowledge gaps in this area.
Conclusion
To summarize, the results of this study add to the knowledge of mental health conditions of FDPs. The findings highlight the association between human rights violations and mental health conditions among forcibly displaced populations. The study results are relevant for other conflict-affected and persecuted communities where basic human rights are systematically violated. It might be of value to conduct in the future a scoping review on this topic including grey literature. While mental health services are crucial for addressing anxiety, depression, and PTSD, they alone cannot fully alleviate the burden. To make an impact, policymakers, politicians, and service providers must continue to provide mental health services aimed at reducing the mental health conditions among these population groups. However, addressing mental health conditions alone is not sufficient to reduce the burden of mental health conditions among these populations. Further research is required to study the effects of systematic continuous human rights violations in conflict prone areas is essential to identify methods to alleviate the burden of these mental health conditions in FDPs. This effort will require substantial resources and long-term advocacy by all major stakeholders involved in this area.
Data availability statement
The datasets presented in this article are not readily available because datasets are available on request from the corresponding author. Requests to access the datasets should be directed to Jutta Lindert, anV0dGEubGluZGVydEBocy1lbWRlbi1sZWVyLmRl.
Author contributions
FS: Data curation, Formal analysis, Investigation, Software, Validation, Writing – review & editing. PC: Formal analysis, Investigation, Software, Validation, Visualization, Data curation, Writing – review & editing. PB: Investigation, Methodology, Writing – review & editing. HK: Investigation, Writing – review & editing. JL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors acknowledge using the free version of Grammarly AI writing and grammar checker (version 14.1214.0) for grammar checks.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1454331/full#supplementary-material
References
1. Silove, D . Challenges to mental health services for refugees: a global perspective. World Psychiatry. (2021) 20:131–2. doi: 10.1002/wps.20818
2. UNHCR . (2019). Refugee definition. Available at: https://emergency.unhcr.org/protection/legal-framework/refugee-definition [Accessed Jun 6, 2024]
3. Global Trends (2021). UNHCR. Available at: https://www.unhcr.org/publications/global-trends-2021[Accessed May 23, 2024]
4. Global Focus . (2024). Global Focus 2024. Available at: https://reporting.unhcr.org/global-appeal-2024. [Accessed May 23, 2024]
5. Kivimaki, M, Batty, GD, Pentti, J, Shipley, MJ, Sipila, PN, Nyberg, ST, et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health. (2020) 5:e140–9. doi: 10.1016/S2468-2667(19)30248-8
6. Lund, C, Brooke-Sumner, C, Baingana, F, Baron, EC, Breuer, E, Chandra, P, et al. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. (2018) 5:357–69. doi: 10.1016/S2215-0366(18)30060-9
7. Chang, Q, Peng, C, Guo, Y, Cai, Z, and Yip, PSF. Mechanisms connecting objective and subjective poverty to mental health: serial mediation roles of negative life events and social support. Soc Sci Med. (2020) 265:113308. doi: 10.1016/j.socscimed.2020.113308
8. Elgar, FJ, Pickett, W, Pfortner, TK, Gariepy, G, Gordon, D, Georgiades, K, et al. Relative food insecurity, mental health and wellbeing in 160 countries. Soc Sci Med. (2021) 268:113556. doi: 10.1016/j.socscimed.2020.113556
9. Bartelink, VHM, Zay Ya, K, Guldbrandsson, K, and Bremberg, S. Unemployment among young people and mental health: A systematic review. Scand J Public Health. (2020) 48:544–58. doi: 10.1177/1403494819852847
10. Charlson, F, van Ommeren, M, Flaxman, A, Cornett, J, Whiteford, H, and Saxena, S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. (2019) 394:240–8. doi: 10.1016/S0140-6736(19)30934-1
11. Morina, N, Akhtar, A, Barth, J, and Schnyder, U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: A systematic review. Front Psychol. (2018) 9:433. doi: 10.3389/fpsyt.2018.00433
12. Priebe, S, Bogic, M, Ashcroft, R, Franciskovic, T, Galeazzi, GM, Kucukalic, A, et al. Experience of human rights violations and subsequent mental disorders - a study following the war in the Balkans. Soc Sci Med. (2010) 71:2170–7. doi: 10.1016/j.socscimed.2010.09.029
13. Human Rights . (n.d.). United Nations. Available at: https://www.un.org/en/global-issues/human-rights [Accessed May 23, 2024]
14. Institute for Economics & Peace . Global peace index 2023: Measuring peace in a complex world, Sydney; (2023). Available at: https://www.visionofhumanity.org/resources/ [Accessed May 23, 2024]
15. Institute for Economics & Peace. Vision of Humanity (2024). Global peace index map, the Most & least peaceful countries. Available at: https://www.visionofhumanity.org/maps/ [Accessed May 23, 2024]
16. DerSimonian, R, and Laird, N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
17. Lipsey, MW, and Wilson, DB. Practical meta-analysis, vol. ix. Thousand oaks, CA, US: Sage publications, Inc (2001). 345 p.
18. Lindert, J, Knobler, HY, Kawachi, I, Bain, PA, Abramowitz, MZ, McKee, C, et al. Psychopathology of children of genocide survivors: a systematic review on the impact of genocide on their children’s psychopathology from five countries. Int J Epidemiol. (2017) 46:246–57. doi: 10.1093/ije/dyw161
19. Effective Public Healthcare Panacea Project . (2024). Quality assessment tool for quantitative studies. Available at: https://www.ephpp.ca/quality-assessment-tool-for-quantitative-studies/. [Accessed May 23, 2024]
20. Bapolisi, AM, Song, SJ, Kesande, C, Rukundo, GZ, and Ashaba, S. Post-traumatic stress disorder, psychiatric comorbidities and associated factors among refugees in Nakivale camp in southwestern Uganda. BMC Psychiatry. (2020) 20:53. doi: 10.1186/s12888-020-2480-1
21. Garoff, F, Skogberg, N, Klemettilä, A, Lilja, E, Ahmed Haji Omar, A, Snellman, O, et al. Mental health and traumatization of newly arrived asylum seeker adults in Finland: A population-based study. Int J Environ Res Pu. (2021) 18:7160. doi: 10.3390/ijerph18137160
22. Lin, S, Kobayashi, K, Tong, H, Davison, KM, SRA, A, and Fuller-Thomson, E. Close relations matter: the association between depression and refugee status in the Canadian longitudinal study on aging (CLSA). J Immigr Minor Health. (2020) 22:946–56. doi: 10.1007/s10903-020-00980-0
23. Maharaj, V, Tomita, A, Thela, L, Mhlongo, M, and Burns, JK. Food insecurity and risk of depression among refugees and immigrants in South Africa. J Immigr Minor Health. (2017) 19:631–7. doi: 10.1007/s10903-016-0370-x
24. Nesterko, Y, Jäckle, D, Friedrich, M, Holzapfel, L, and Glaesmer, H. Prevalence of post-traumatic stress disorder, depression and somatisation in recently arrived refugees in Germany: an epidemiological study. Epidemiol Psych Sci. (2020) 29:e40. doi: 10.1017/S2045796019000325
25. Rasmussen, A, Crager, M, Baser, RE, Chu, T, and Gany, F. Onset of posttraumatic stress disorder and major depression among refugees and voluntary migrants to the United States. J Trauma Stress. (2012) 25:705–12. doi: 10.1002/jts.21763
26. Winkler, JG, Brandl, EJ, Bretz, HJ, Heinz, A, and Schouler-Ocak, M. Psychische Symptombelastung bei Asylsuchenden in Abhängigkeit vom Aufenthaltsstatus. Psychiatr Prax. (2019) 46:191–9. doi: 10.1055/a-0806-3568
27. Lenferink, LIM, Liddell, BJ, Byrow, Y, O’Donnell, M, Bryant, RA, Mau, V, et al. Course and predictors of posttraumatic stress and depression longitudinal symptom profiles in refugees: A latent transition model. J Psychiatr Res. (2022) 146:1–10. doi: 10.1016/j.jpsychires.2021.12.009
28. Bogic, M, Ajdukovic, D, Bremner, S, Franciskovic, T, Galeazzi, GM, Kucukalic, A, et al. Factors associated with mental disorders in long-settled war refugees: refugees from the former Yugoslavia in Germany, Italy and the UK. Br J Psychiatry. (2012) 200:216–23. doi: 10.1192/bjp.bp.110.084764
29. Carta, MG, Moro, D, Wallet Oumar, F, Moro, MF, Pintus, M, Pintus, E, et al. A follow-up on psychiatric symptoms and post-traumatic stress disorders in Tuareg refugees in Burkina Faso. Front. Psychiatry. (2018) 9:9. doi: 10.3389/fpsyt.2018.00127
30. Acarturk, C, Cetinkaya, M, Senay, I, Gulen, B, Aker, T, and Hinton, D. Prevalence and predictors of posttraumatic stress and depression symptoms among Syrian refugees in a refugee camp. The. J Nerv Ment Dis. (2018) 206:40–5. doi: 10.1097/NMD.0000000000000693
31. Ainamani, HE, Elbert, T, Olema, DK, and Hecker, T. Gender differences in response to war-related trauma and posttraumatic stress disorder – a study among the Congolese refugees in Uganda. BMC Psychiatry. (2020) 20:17. doi: 10.1186/s12888-019-2420-0
32. Alpak, G, Unal, A, Bulbul, F, Sagaltici, E, Bez, Y, Altindag, A, et al. Post-traumatic stress disorder among Syrian refugees in Turkey: a cross-sectional study. Int J Psychiatry Clin Pract. (2015) 19:45–50. doi: 10.3109/13651501.2014.961930
33. Basheti, IA, Ayasrah, SM, Basheti, MM, Mahfuz, J, and Chaar, B. The Syrian refugee crisis in Jordan: a cross sectional pharmacist-led study assessing post-traumatic stress disorder. Pharm Pract (Granada). (2019) 17:1475. doi: 10.18549/PharmPract.2019.3.1475
34. Beiser, M, Simich, L, Pandalangat, N, Nowakowski, M, and Tian, F. Stresses of passage, balms of resettlement, and posttraumatic stress disorder among Sri Lankan Tamils in Canada. Can J Psychiatr. (2011) 56:333–40. doi: 10.1177/070674371105600604
35. Berhe, SM, Azale, T, Fanta, T, Demeke, W, and Minyihun, A. Prevalence and predictors of depression among Eritrean refugees in Ethiopia: A cross-sectional survey. Psychol Res Behav Manag. (2021) 14:1971–80. doi: 10.2147/PRBM.S337255
36. Berthold, SM, Kong, S, Mollica, RF, Kuoch, T, Scully, M, and Franke, T. Comorbid mental and physical health and health access in Cambodian refugees in the US. J Community Health. (2014) 39:1045–52. doi: 10.1007/s10900-014-9861-7
37. Cengiz, İ, Ergün, D, and Çakici, E. Posttraumatic stress disorder, posttraumatic growth and psychological resilience in Syrian refugees: Hatay. Turkey Anadolu Psikiyatri Dergisi. (2019) 20:1–76. doi: 10.5455/apd.4862
38. Chung, MC, and Shakra, M. The association between trauma centrality and posttraumatic stress among Syrian refugees: the impact of cognitive distortions and trauma-coping self-efficacy. J Interpers Violence. (2022) 37:1852–77. doi: 10.1177/0886260520926311
39. Cheung Chung, M, AlQarni, N, AlMazrouei, M, Al Muhairi, S, Shakra, M, Mitchell, B, et al. The impact of trauma exposure characteristics on post-traumatic stress disorder and psychiatric co-morbidity among Syrian refugees. Psychiatry Res. (2018) 259:310–5. doi: 10.1016/j.psychres.2017.10.035
40. Chung, MC, Shakra, M, Al-Qarni, N, Al-Mazrouei, M, Al-Mazrouei, S, and Al-Hashimi, S. Posttraumatic stress among Syrian refugees: trauma exposure characteristics, trauma centrality, and emotional suppression. Psychiatry. (2018) 81:54–70. doi: 10.1080/00332747.2017.1354620
41. Dietrich, H, Ali, RA, Tagay, S, Hebebrand, J, and Reissner, V. Screening for posttraumatic stress disorder in young adult refugees from Syria and Iraq. Compr Psychiatry. (2019) 90:73–81. doi: 10.1016/j.comppsych.2018.11.001
42. Eiset, AH, Aoun, MP, Stougaard, M, Gottlieb, AG, Haddad, RS, Frydenberg, M, et al. The association between long-distance migration and PTSD prevalence in Syrian refugees. BMC Psychiatry. (2022) 22:363. doi: 10.1186/s12888-022-03982-4
43. Ersahin, Z . Post-traumatic growth among Syrian refugees in Turkey: the role of coping strategies and religiosity. Curr Psychol. (2022) 41:2398–407. doi: 10.1007/s12144-020-00763-8
44. Familiar, I, Muniina, PN, Dolan, C, Ogwal, M, Serwadda, D, Kiyingi, H, et al. Conflict-related violence and mental health among self-settled Democratic Republic of Congo female refugees in Kampala, Uganda – a respondent driven sampling survey. Confl Heal. (2021) 15:42. doi: 10.1186/s13031-021-00377-2
45. Feyera, F, Mihretie, G, Bedaso, A, Gedle, D, and Kumera, G. Prevalence of depression and associated factors among Somali refugee at Melkadida camp, Southeast Ethiopia: a cross-sectional study. BMC Psychiatry. (2015) 15:171. doi: 10.1186/s12888-015-0539-1
46. Gottvall, M, Vaez, M, and Saboonchi, F. Social support attenuates the link between torture exposure and post-traumatic stress disorder among male and female Syrian refugees in Sweden. BMC Int Health Hum R. (2019) 19:28. doi: 10.1186/s12914-019-0214-6
47. Jeon, BH, Kim, MD, Hong, SC, Kim, NR, Lee, CI, Kwak, YS, et al. Prevalence and correlates of depressive symptoms among north Korean defectors living in South Korea for more than one year. Psychiatry Investig. (2009) 6:122–30. doi: 10.4306/pi.2009.6.3.122
48. Kaya, E, Kiliç, C, Karadağ Çaman, Ö, and Üner, S. Posttraumatic stress and depression among Syrian refugees living in Turkey: findings from an urban sample. J Nerv Ment Dis. (2019) 207:995–1000. doi: 10.1097/NMD.0000000000001104
49. Kazour, F, Zahreddine, NR, Maragel, MG, Almustafa, MA, Soufia, M, Haddad, R, et al. Post-traumatic stress disorder in a sample of Syrian refugees in Lebanon. Compr Psychiatry. (2017) 72:41–7. doi: 10.1016/j.comppsych.2016.09.007
50. Kim, HH, Lee, YJ, Kim, HK, Kim, JE, Kim, SJ, Bae, SM, et al. Prevalence and correlates of psychiatric symptoms in north korean defectors. Psychiatry Investig. (2011) 8:179–85. doi: 10.4306/pi.2011.8.3.179
51. Kim, I . Behavioral health symptoms among refugees from Burma: examination of sociodemographic and migration-related factors. Asian Am J Psychol. (2018) 9:179–89. doi: 10.1037/aap0000103
52. Kira, IA, Shuwiekh, H, Rice, K, Al Ibraheem, B, and Aljakoub, J. A threatened identity: the mental health status of Syrian refugees in Egypt and its etiology. Identity: Int J Theory Res. (2017) 17:176–90. doi: 10.1080/15283488.2017.1340163
53. Lee, YJ, Jun, JY, Lee, YJ, Park, J, Kim, S, Lee, SH, et al. Insomnia in north Korean refugees: association with depression and post-traumatic stress symptoms. Psychiatry Investig. (2016) 13:67–73. doi: 10.4306/pi.2016.13.1.67
54. Mahmood, HN, Ibrahim, H, Goessmann, K, Ismail, AA, and Neuner, F. Post-traumatic stress disorder and depression among Syrian refugees residing in the Kurdistan region of Iraq. Confl Heal. (2019) 13:51. doi: 10.1186/s13031-019-0238-5
55. Mwanamwambwa, V, and Pillay, BJ. Posttraumatic stress disorder and psychological distress in Rwandan refugees living in Zambia. S Afr J Psychol. (2022) 52:175–88. doi: 10.1177/00812463211031812
56. Naal, H, Nabulsi, D, El Arnaout, N, Abdouni, L, Dimassi, H, Harb, R, et al. Prevalence of depression symptoms and associated sociodemographic and clinical correlates among Syrian refugees in Lebanon. BMC Public Health. (2021) 21:217. doi: 10.1186/s12889-021-10266-1
57. Naja, WJ, Aoun, MP, El Khoury, EL, Abdallah, FJ, and Haddad, RS. Prevalence of depression in Syrian refugees and the influence of religiosity. Compr Psychiatry. (2016) 68:78–85. doi: 10.1016/j.comppsych.2016.04.002
58. Nam, B, Kim, JY, DeVylder, JE, and Song, A. Family functioning, resilience, and depression among north Korean refugees. Psychiatry Res. (2016) 245:451–7. doi: 10.1016/j.psychres.2016.08.063
59. Nickerson, A, Bryant, RA, Brooks, R, Steel, Z, and Silove, D. Fear of cultural extinction and psychopathology among Mandaean refugees: an exploratory path analysis. CNS Neurosci Ther. (2009) 15:227–36. doi: 10.1111/j.1755-5949.2009.00094.x
60. Nissen, A, Cauley, P, Saboonchi, F, and Andersen, J. Mental health in adult refugees from Syria resettled in Norway between 2015 and 2017: a nationwide, questionnaire-based, cross-sectional prevalence study. Eur J Psychotraumatol. (2021) 12:1994218. doi: 10.1080/20008198.2021.1994218
61. Poole, DN, Raymond, NA, Berens, J, Latonero, M, Ricard, J, and Hedt-Gauthier, B. A combination sampling approach for epidemiologic research in humanitarian settings: a case analysis of a study of depressive disorder prevalence among refugees in Greece. BMC Public Health. (2021) 21:272. doi: 10.1186/s12889-021-10342-6
62. Sagaltici, E, Alpak, G, and Altindag, A. Traumatic life events and severity of posttraumatic stress disorder among Syrian refugees residing in a camp in Turkey. J Loss Trauma. (2020) 25:47–60. doi: 10.1080/15325024.2019.1654691
63. Silove, D, Momartin, S, Marnane, C, Steel, Z, and Manicavasagar, V. Adult separation anxiety disorder among war-affected Bosnian refugees: comorbidity with PTSD and associations with dimensions of trauma. J Trauma Stress. (2010) 23:169–72. doi: 10.1002/jts.20490
64. Taylor, EM, Yanni, EA, Pezzi, C, Guterbock, M, Rothney, E, Harton, E, et al. Physical and mental health status of Iraqi refugees resettled in the United States. J Immigr Minor Health. (2014) 16:1130–7. doi: 10.1007/s10903-013-9893-6
65. Tekeli-Yesil, S, Isik, E, Unal, Y, Aljomaa Almossa, F, Konsuk Unlu, H, and Aker, AT. Determinants of mental disorders in Syrian refugees in Turkey versus internally displaced persons in Syria. Am J Public Health. (2018) 108:938–45. doi: 10.2105/AJPH.2018.304405
66. Tekin, A, Karadag, H, Suleymanoglu, M, Tekin, M, Kayran, Y, Alpak, G, et al. Prevalence and gender differences in symptomatology of posttraumatic stress disorder and depression among Iraqi Yazidis displaced into Turkey. Eur J Psychotraumatol. (2016) 7:28556. doi: 10.3402/ejpt.v7.28556
67. Tinghög, P, Malm, A, Arwidson, C, Sigvardsdotter, E, Lundin, A, and Saboonchi, F. Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: a population-based survey. BMJ Open. (2017) 7:e018899. doi: 10.1136/bmjopen-2017-018899
68. Vonnahme, LA, Lankau, EW, Ao, T, Shetty, S, and Cardozo, BL. Factors associated with symptoms of depression among Bhutanese refugees in the United States. J Immigr Minor Health. (2015) 17:1705–14. doi: 10.1007/s10903-014-0120-x
69. Yang, MS, and Mutchler, JE. The high prevalence of depressive symptoms and its correlates with older Hmong refugees in the United States. J Aging Health. (2020) 32:660–9. doi: 10.1177/0898264319844088
70. Yun, S, Ahmed, SR, Hauson, AO, and Al-Delaimy, WK. The relationship between acculturative stress and Postmigration mental health in Iraqi refugee women resettled in San Diego. California Community Ment Hlt J. (2021) 57:1111–20. doi: 10.1007/s10597-020-00739-9
71. Ahmad, F, Othman, N, Hynie, M, Bayoumi, AM, Oda, A, and McKenzie, K. Depression-level symptoms among Syrian refugees: findings from a Canadian longitudinal study. J Ment Health. (2021) 30:246–54. doi: 10.1080/09638237.2020.1765998
72. Lamkaddem, M, Stronks, K, Devillé, WD, Olff, M, Gerritsen, AA, and Essink-Bot, ML. Course of post-traumatic stress disorder and health care utilisation among resettled refugees in the Netherlands. BMC Psychiatry. (2014) 14:90. doi: 10.1186/1471-244X-14-90
73. Chernet, A, Probst-Hensch, N, Sydow, V, Paris, DH, and Labhardt, ND. Mental health and resilience among Eritrean refugees at arrival and one-year post-registration in Switzerland: a cohort study. BMC Res Notes. (2021) 14:281. doi: 10.1186/s13104-021-05695-5
74. Fuhr, DC, Acarturk, C, McGrath, M, Ilkkursun, Z, Sondorp, E, Sijbrandij, M, et al. Treatment gap and mental health service use among Syrian refugees in Sultanbeyli, Istanbul: a cross-sectional survey. Epidemiol Psych Sci. (2020) 29:e70. doi: 10.1017/S2045796019000660
75. De Bellis, MD . Developmental traumatology: the psychobiological development of maltreated children and its implications for research, treatment, and policy. Dev Psychopathol. (2001) 13:539–64. doi: 10.1017/S0954579401003078
76. Heim, C, and Nemeroff, CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. (2001) 49:1023–39. doi: 10.1016/S0006-3223(01)01157-X
77. Kessler, RC, Aguilar-Gaxiola, S, Alonso, J, Benjet, C, Bromet, EJ, Cardoso, G, et al. Trauma and PTSD in the WHO world mental health surveys. Eur J Psychotraumatol. (2017) 8:1353383. doi: 10.1080/20008198.2017.1353383
78. Neuner, F, Schauer, M, Klaschik, C, Karunakara, U, and Elbert, T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. J Consult Clin Psychol. (2004) 72:579–87. doi: 10.1037/0022-006X.72.4.579
79. Foley, P, and Kirschbaum, C. Human hypothalamus–pituitary–adrenal axis responses to acute psychosocial stress in laboratory settings. Neurosci Biobehav Rev. (2010) 35:91–6. doi: 10.1016/j.neubiorev.2010.01.010
80. Kudielka, BM, Buske-Kirschbaum, A, Hellhammer, DH, and Kirschbaum, C. Differential heart rate reactivity and recovery after psychosocial stress (TSST) in healthy children, younger adults, and elderly adults: the impact of age and gender. Int J Behav Med. (2004) 11:116–21. doi: 10.1207/s15327558ijbm1102_8
81. van Eck, M, Berkhof, H, Nicolson, N, and Sulon, J. The effects of perceived stress, traits, mood states, and stressful daily events on salivary cortisol. Psychosom Med. (1996) 58:447–58. doi: 10.1097/00006842-199609000-00007
82. Moylan, S, Maes, M, Wray, NR, and Berk, M. The neuroprogressive nature of major depressive disorder: pathways to disease evolution and resistance, and therapeutic implications. Mol Psychiatry. (2013) 18:595–606. doi: 10.1038/mp.2012.33
83. Teicher, MH, and Samson, JA. Childhood maltreatment and psychopathology: A case for ecophenotypic variants as clinically and neurobiologically distinct subtypes. Am J Psychiatry. (2013) 170:1114–33. doi: 10.1176/appi.ajp.2013.12070957
84. Krieger, N . Theories for social epidemiology in the 21st century_an ecosocial perspective. Int J Epidemiol. (2001) 30:668–77. doi: 10.1093/ije/30.4.668
85. Weathers, FW, and Keane, TM. The criterion A problem revisited: controversies and challenges in defining and measuring psychological trauma. J Trauma Stress. (2007) 20:107–21. doi: 10.1002/jts.20210
Keywords: forcibly displaced persons, depression, anxiety, PTSD, human rights violations, global peace index, systematic review, meta-analysis
Citation: Sisenop F, Chatarajupalli P, Bain PA, Kaade H and Lindert J (2025) Human rights violations are associated with forcibly displaced population’s mental health—a systematic review and meta-analysis. Front. Public Health. 12:1454331. doi: 10.3389/fpubh.2024.1454331
Edited by:
Gülseren Keskin, Ege University, TürkiyeReviewed by:
Barton Buechner, Adler School of Professional Psychology, United StatesPaola Cardinali, Mercatorum University, Italy
Copyright © 2025 Sisenop, Chatarajupalli, Bain, Kaade and Lindert. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jutta Lindert, anV0dGEubGluZGVydEBocy1lbWRlbi1sZWVyLmRl
†These authors have contributed equally to this work
 Felix Sisenop
Felix Sisenop Pallavi Chatarajupalli
Pallavi Chatarajupalli Paul A. Bain
Paul A. Bain Hanna Kaade
Hanna Kaade Jutta Lindert
Jutta Lindert