- 1School of Nursing, Jinzhou Medical University, Jinzhou, Liaoning, China
- 2School of Nursing, Shanxi Medical University, Taiyuan, Shanxi, China
- 3School of Nursing, Wannan Medical College, Wuhu, Anhui, China
Background: The active coping strategies of family members can help breast cancer patients better handle the crisis, and family adaptation is a manifestation of the family's active coping with the crisis. In the study of breast cancer, a disease that predominantly affects women, we explored the influence of spouses on patients' family adaptation. This aspect has not been explored in previous studies.
Purpose: In recent years, with the development of family stress coping theory, cancer coping styles have shifted from an individual focus to a whole-family approach. This shift has the potential to help families of cancer patients adapt to the crisis. This study aimed to explore the correlation between dyadic coping, family adaptation, and benefit finding in couples with breast cancer.
Methods: Using convenience sampling, the study included 325 pairs consisting of breast cancer patients and their spouses who attended breast surgery, oncology, and chemotherapy sessions between April and November 2023. The survey utilized the General Information Questionnaire for patients and spouses, the Dyadic Coping Scale, the Benefit Finding Scale, and the Family Adaptability and Cohesion Evaluation Scales. Data analysis was conducted using SPSS 25.0 and Amos 24.0 software.
Results: In the actor effect of dyadic coping on family adaptation, the benefit finding of patients and their spouses played a mediating role. Regarding the partner effect (B = 0.019, 95% CI = 0.003–0.045, P < 0.05), the dyadic coping of spouses indirectly affected the family adaptation of patients through the benefit findings of patients. The patient's dyadic coping can directly affect the spouse's family adaptation. The spouse's dyadic coping can influence the patient's benefit finding.
Conclusion: There is a partial interaction between breast cancer patients and their spouses' dyadic coping, benefit finding, and family adaptation. Therefore, clinical staff should promptly identify patients and spouses with poor coping abilities and provide them with positive psychological interventions to enhance the dyadic coping abilities of both partners and assist them in overcoming the problems encountered during the treatment process, ultimately helping them better cope with family crises.
Introduction
According to the data released by the International Agency for Research on Cancer in 2020, the number of new cancer cases reached 19.3 million worldwide. Notably, breast cancer cases accounted for 2.3 million of these cases, surpassing lung cancer to become the most common cancer globally (1). In 2020, there were an estimated 4.82 million new cancer cases in China. Among these, the number of new cases of female breast cancer reached 357,200, making it the most common cancer among Chinese women after lung, rectal, thyroid, and liver cancers (2).
The diagnosis and treatment of cancer can often be extremely stressful for patients, resulting in severe negative emotions and other adverse consequences (3). More seriously, such stressful events may adversely affect the family adaptation of cancer patients (4). Previous research has shown that couples dealing with illness together can enhance their feelings of closeness and reduce the stress and psychological burden associated with the illness (5). In the face of crisis events, families of cancer patients adopt different coping styles, which may affect the family's adaptation (6).
Family adaptation is the family's direct response to a stressful event, indicating that the family needs to readjust its structure to restore stability and improve overall happiness and satisfaction (7). Studies have shown that stressful events reduce the family's capacity to adapt for both the patient and the primary caregiver (8). In the course of breast cancer treatment, the adaptive capacity of the patient's family is closely related to the caregiver's perceived stress; the higher the perceived level of stress, the worse the adaptive capacity of the family (9). Good family adaptation can reduce the incidence of suicidal ideation in patients (10), and the incidence of anxiety and depression is relatively low in patients with good family adaptation (11).
Benefit finding is a cognitive way of actively coping with adverse external circumstances, manifested as benefits finding from traumatic or unfortunate life events (12). In studies of cancer in men, it has been confirmed that benefit finding is a cognitive strategy to cope with cancer actively; the higher the level of benefit finding, the higher the level of quality of life (13). This cognitive approach not only reduces caregivers' negative emotions, such as anxiety and depression, improves mental health (14), but also improves overall quality of life (15). However, some studies have found that the extent of benefit finding may decrease as the patient's condition worsens (16). A study observed that the level of caregiver benefit findings was strongly correlated with family adaptation (17). In the dyadic study, it was noted that for older patients with physical impairments and their caregivers, low levels of benefit finding may produce mental and emotional distress, which in turn reduces the level of family adaptation (18). Therefore, it is necessary to study further the effect of benefit finding between couples on family adaptation.
In recent years, with the development of the family stress coping theory, the coping style of cancer has shifted from an individual focus to the couple's experience, that is, dyadic coping (19). Research has shown that couples who adopt good dyadic coping strategies can regulate their stress levels more effectively and navigate difficult situations with ease (20). This ability to cope constructively can enhance mutual communication and dependence between couples, foster a more intimate relationship, and improve their ability to resist the illness together (21). Families with better coping styles are more capable of overcoming difficulties and increasing their confidence in dealing with the disease (22). In a dyadic study, it was found that couples facing breast cancer exhibited inefficient coping styles, which not only causes serious psychological distress for both spouses but also may lead to a coping crisis within the family (23). A good dyadic coping style between a husband and wife not only helps effectively manage the disease and overcome the illness but also contributes to a more stable and harmonious family environment (24). Therefore, whether the dyadic coping style between couples has a positive or negative impact on family adaptation needs further research.
Conceptual framework
This study uses the ABC-X theory and the actor–partner interdependence model for analysis. Reuben Hill, founder of family stress theory, proposed the ABC-X stress theory model in 1949 (25). It is a relatively comprehensive family stress theory model. The model contains four factors: A represents the stressor event; B represents the resources to cope with; C represents the cognition or evaluation of the stressful event; and X represents the outcome, that is, the degree of harm caused by the stress or crisis to the individual. In this study, A is a cancer stress event, B is dyadic coping, C is benefit finding, and X is family adaptation. The actor–partner interdependence model (APIM) is a data analysis method proposed by Kenny and Cook in 1999 that allows researchers to analyze how dependent variables are affected by the predictor variables of another party (the partner effect) as well as their predictor (the actor effect) (26). The actor–partner interdependent mediation model (APIMeM) is an APIM-based model proposed by Kenny and Ledermann, which includes mediation variables (27). This model allows estimation of the mediating effects of benefit finding in patient–spouse dyadic relationships (see Figure 1).
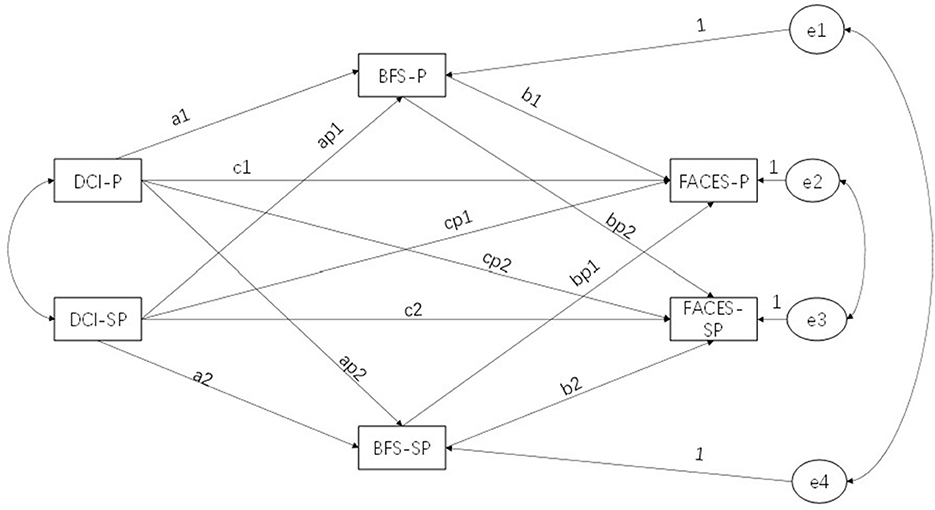
Figure 1. Basic model structure. DCI, Dyadic Coping Inventory; BFS, Benefit Finding Scale; FACES, Family Adaptability and Cohesion Evaluation Scales; P, patient; SP, spouse.
Materials and methods
Participants
A cross-sectional survey method was employed in this study. We surveyed breast cancer patients and their spouses who attended breast surgery, radiotherapy, and chemotherapy sessions in three Grade III hospitals in Liaoning Province from April to November 2023 using a convenient sampling method. The inclusion criteria were as follows: (1) age ≥ 20 years and married; (2) pathological diagnosis of breast cancer; (3) the patient must be aware of the diagnosis of her disease; (4) the patient must be able to communicate normally and have no diagnosed mental disorder according to Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). The exclusion criteria were as follows: (1) widowed or divorced status (patient or spouse); (2) have the intention to withdraw from the survey (patient or spouse); and (3) history of mental problems (patient or spouse).
In this study, Gpower3.1 software was used to calculate the sample size. According to the literature review, α value was set to 0.05, the statistical power (1 – β) to 0.90, and the effect size to 0.25 (28). The calculation showed that a minimum of 275 pairs (including patients and spouses) were required, and we collected 325 valid data pairs (see Figure 2).
Data collection
Before data collection, researchers received uniform training to ensure that the instructions communicated to study subjects remained consistent. The researchers explained the purpose and significance of the study to the subjects and guided them to sign a written informed consent. To ensure data reliability, the subjects were instructed to complete the survey in two different locations and were not allowed to discuss it with one another. At the same time, the researchers made sure to be always available to help study subjects who had difficulty reading, writing, or understanding the survey. Immediately after the survey was completed, the questionnaires were collected and checked to ensure that no missing items were present and that invalid questionnaires were removed. To protect the privacy of research subjects, all information was anonymized. The research followed the ethical principles of the Declaration of Helsinki and was approved by the Ethics Committee of Jinzhou Medical University (approval number: JZMULL2023026).
Measurements
Dyadic coping inventory
DCI was developed by Bodenmann (29) in 2008 to assess how effectively couples cope with stress. In 2016, Chinese scholar Xu et al. (30) translated the DCI scale into Chinese. The scale consists of 37 items divided into five dimensions using a 5-point Likert score with an overall range of 35–175 points. A score below 111 indicates a low level of binary coping, a score between 111 and 145 represents a moderate level, and a score above 145 indicates a high level of binary coping, with a higher score representing a better ability to cope. In this study, the value of Cronbach's α was 0.942 for the patient and 0.916 for the spouse.
Benefit finding scale
BFS was originally compiled by Antoni et al. (31) in 2001 for breast cancer patients. The higher the total score, the greater the level of benefit finding. In this study, the Chinese version of the Benefit Finding Scale adapted by Liu et al. (32) was used to assess the level of benefit finding in breast cancer patients. The scale contains 22 items covering six dimensions and uses a 5-point Likert score, with a higher score indicating greater benefit finding. In this study, the value of Cronbach's α was 0.923 for patients and 0.889 for spouses.
Family Adaptability and Cohesion Evaluation Scales
FACES is the most commonly used family adaptation scale. FACES was developed by Olson et al. (33) in 1979. Chinese scholars translated the FACES scale into Chinese. They revised it to form the Chinese version of the FACES II-CV scale (34), which contains 30 items divided into two subscales: family intimacy and family adaptability. The intimacy subscale includes 16 items, while adaptability contains 14 items, with each item scored on a five-point Likert scale. The content of the family adaptability dimension is more appropriate, as it better reflects the individual's satisfaction with family adaptation. In this study, the value of Cronbach's α was 0.957 for the patient and 0.965 for the spouse.
Sociodemographic and clinical characteristics
The demographic information of patients and spouses was collected using self-made questionnaires. At the same time, clinical characteristics of patients and their spouses were obtained through medical record review. All the contents of our investigation were approved by the patients and patients provided their informed consent.
Quality assurance
Under the tutor's guidance, we edited and standardized the questionnaire and two members of the research team were selected to administer the questionnaire. The study group members distributed questionnaires to protect patients' privacy and encourage their active participation. The responses were put through a double-input and verified using Excel software to ensure the effectiveness and accuracy of the questionnaire.
Statistical analysis
Descriptive statistical methods, including frequency distribution, mean, and standard deviation, were used to summarize demographic characteristics, cancer-related factors, family adaptation, benefit finding, and dyadic coping. We used the paired-sample t-test to describe the differences between patients and spouses regarding the primary study variables, and Pearson's correlation analysis was performed to describe the associations between patients and spouses on the key variables. In this study, we treated patients and spouses as distinguishable data sets. Using APIMeM, we studied the effect of dyadic coping between patients and their spouses on family adaptation and the mediating role of benefit finding. The APIMeM (27, 35) was used to test the hypotheses using bootstrap analysis with 5,000 bootstrap samples and a 95% confidence interval. The dyadic model was verified using χ2/df (value < 3), comparative fit index (CFI value ≥ 0.90), Tucker–Lewis index (TLI value ≥ 0.90), and root mean square error of approximation (RMSEA value ≤ 0.08). SPSS25.0 and AMOS24.0 were used for conducting statistical analysis. A P-value of <0.05 was considered statistically significant.
Results
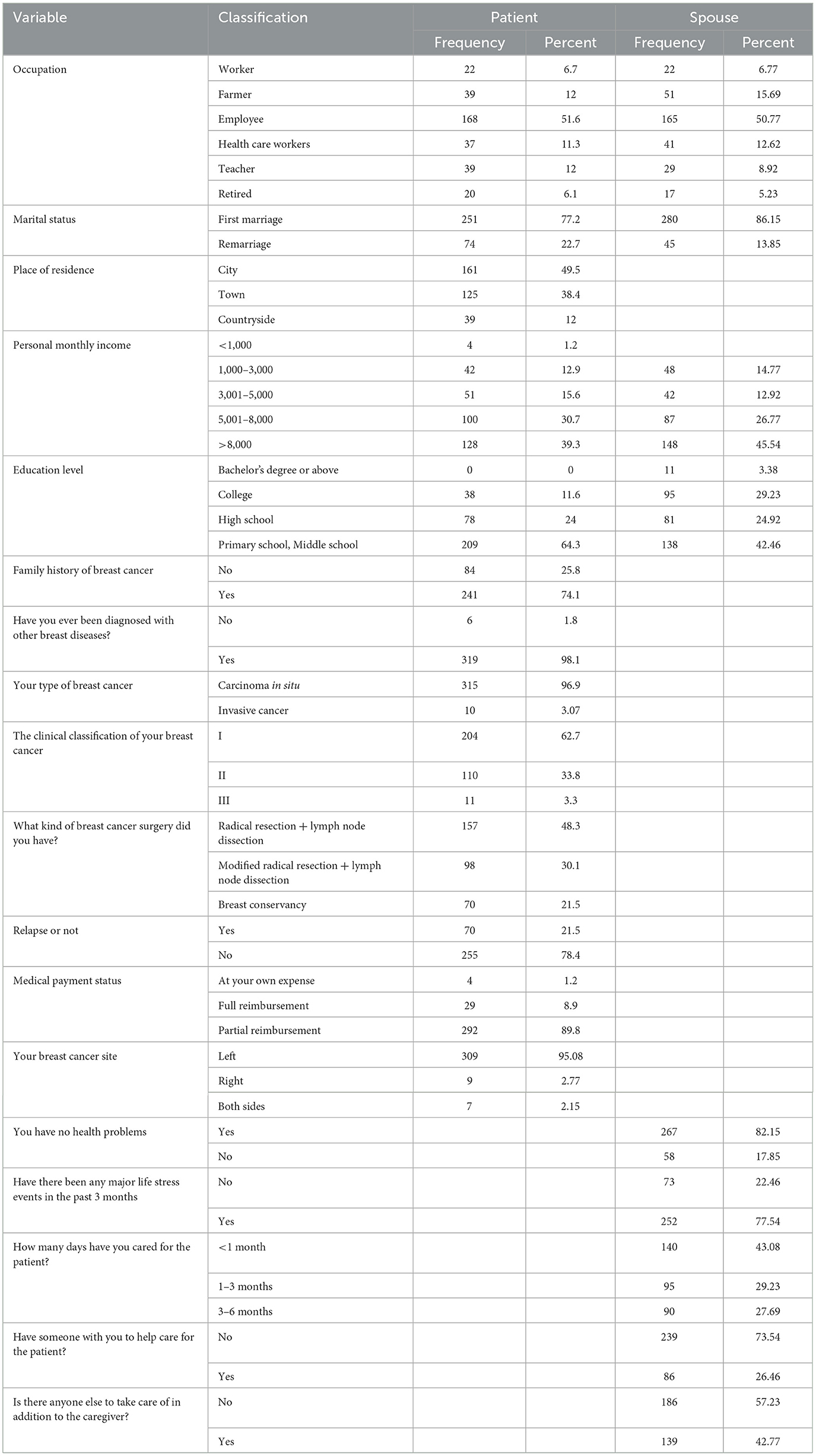
The demographic characteristics of breast cancer patients and their spouses showed that the majority of participants were office workers (51.6% of patients and 50.8% of spouses). Regarding marital status, the majority were married for the first time (77.2% of patients and 86.2% of spouses). Individual monthly income was predominantly in the range of 8,000 yuan and above (39.3% of patients and 45.5% of spouses). Regarding education, the majority of them had attained at least a primary or middle school level (64.3% of patients and 42.5% of spouses). In the majority of families with breast cancer patients, the spouse was in good health, with no health problems, accounting for 82.2%. Additionally, the majority of spouses cared for patients for <1 month (43.1%). In addition, a vast majority of breast cancer patients had a family history of the disease (74.1%), and the main type of breast cancer was in situ, accounting for 96.9%. See Table 1 for more detailed data.
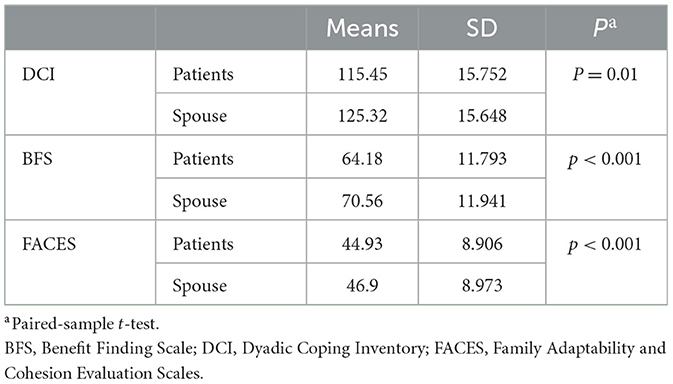
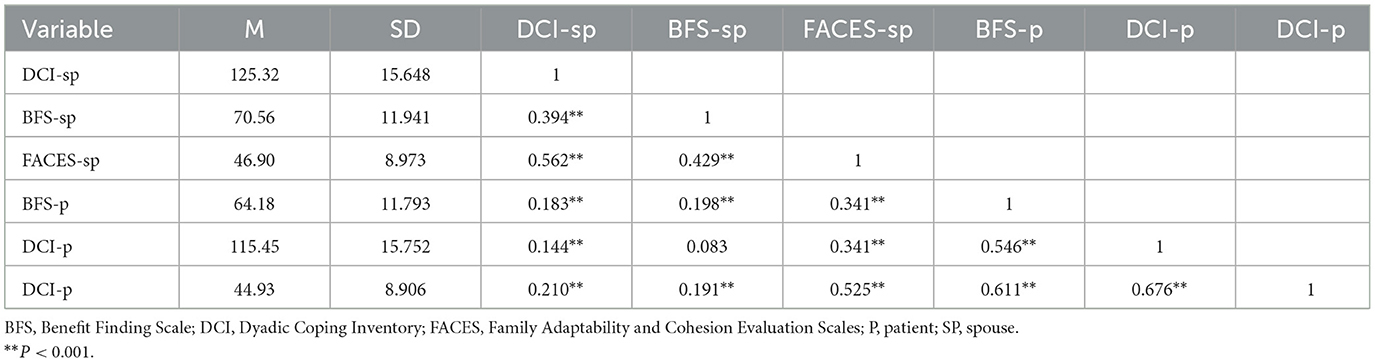
Table 2 describes the mean value of the variables, the standard deviation, and whether each variable is different in the patient–spouse binary. The paired-sample T-test showed significant differences between patients and spouses in dyadic coping, benefit finding, and family adaptation. Patients' binary coping (115.45 ± 15.752), benefit finding (64.18 ± 11.793), and family adaptation (44.93 ± 8.906) were significantly lower than spouses' binary coping (125.32 ± 15.648), benefit finding (70.56 ± 11.941), and family adaptation (46.90 ± 8.973). Table 3 shows the correlation of the study variables. In the correlation analysis, significant associations were found between patient–spouse binary coping (r = 0.144, p < 0.001), benefit finding (r = 0.198, p < 0.001), and family adaptation (r = 0.525, p < 0.001), suggesting that patient–spouse binary relationships were not independent.
Actor–partner interdependence mediation model
In this study, we constructed a subjective and actor–partner mediation model of benefit finding, dyadic coping, and family adaptation for breast cancer patients and their spouses. The results showed that the model fit well (CMIN/DF = 2.754, CFI = 0.984, TLI = 0.961, IFI = 0.985, GFI = 0.983, RMSEA = 0.074).
The results in Tables 4, 5 show that the dyadic coping of patients (B = 0.276; P < 0.05; lower = 0.188; upper = 0.354) and spouses (B = 0.244; P < 0.05; lower = 0.163; upper = 0.317) impacts family adaptation. In addition, in the actor effect, the dyadic coping of patients (B = 0.397; P < 0.001; lower = 0.31; upper = 0.477) and spouses (B = 0.298; P < 0.001; lower = 0.191; upper = 0.402) impacts the benefit finding. In the partner effect, the patient's dyadic coping does not affect the partner's benefit finding (B = 0.02; P = 0.608), but the spouse's dyadic coping affects the patient's benefit finding (B = 0.08; P = 0.03; lower = 0.008; upper = 0.153).

Table 5. Bootstrap test for indirect effects for the actor–partner interdependence mediation model with dyadic coping inventory as an independent variable, benefit finding as a mediator, and family adaptability as outcome.
In families of breast cancer patients, we have shown that benefit finding plays a mediating role between couples' dyadic coping and family adaptation. Specifically, we observe that the dyadic coping of patients (B = 0.096, P < 0.001; B = 0.05, P < 0.001) and their spouses (B = 0.050, 95% CI = 0.022–0.093, P < 0.001) has an actor effect on family adaptation and that this effect is partly mediated by benefit finding. In other words, the higher the level of dyadic coping of patients and their spouses, the more significant their benefit finding, leading to better family adaptation. In addition, we also found a partner effect: the dyadic coping of spouses can affect the patient's benefit finding and then affect the patient's family adaptation (B = 0.019, 95% CI = 0.003–0.045, P < 0.05). However, spouses' dyadic coping did not directly affect patients' family adaptation, possibly because patient benefit finding plays a mediating role (see Figure 3).
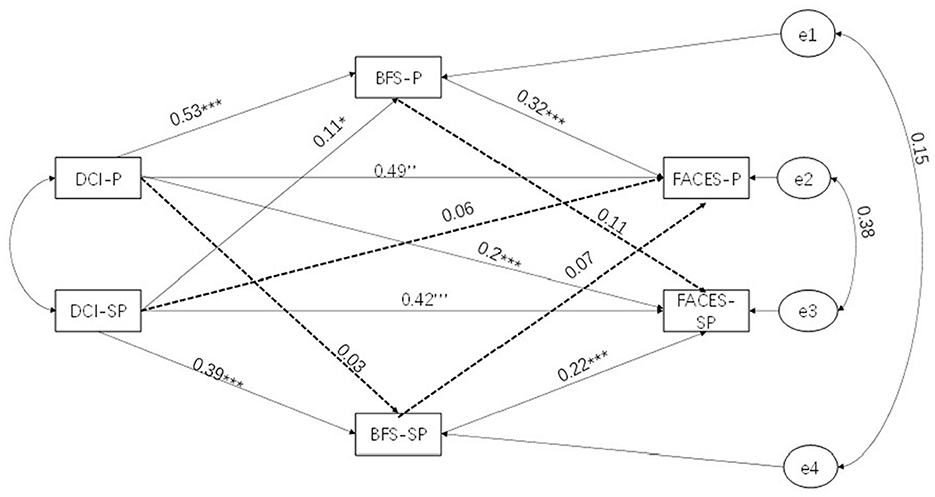
Figure 3. Actor–partner interdependence mediation model. DCI, Dyadic Coping Inventory; BFS, Benefit Finding Scale; FACES, Family Adaptability and Cohesion Evaluation Scales; P, patient; SP, spouse; ***p < 0.001, **p < 0.01, *p < 0.05.
The percentage of explanatory variation for the benefit finding in patients and spouses was 30.89 and 15.6%, respectively. The percentage of explanatory variation for family adaptation in patients and spouses was 55.03 and 44.05%, respectively.
Discussion
Previous studies have focused on the factors influencing family adaptation (36, 37) and the impact of coping styles on family adaptation (38). This study further expands on these frameworks, exploring the actor–partner effect of dyadic coping on family adaptation from a dyadic perspective and examining the mediating role of benefit finding in this effect. This is the first study to examine the effects of binary coping and benefit finding on family adaptation.
In this study, the positive dyadic coping of patients and spouses can directly affect their family adaptation. Previous studies have shown that good dyadic coping between couples can promote effective communication, enhance emotional stability, and contribute to family harmony (39). Effective dyadic coping enables couples to think from each other's perspective and understand one another when facing challenges, thereby enhancing family stability (40). For patients, the positive support, companionship, and care provided by the spouse can reduce the emotional pressure on the patient, convey love and care, and improve the confidence to overcome the disease and find the beauty of life (41). For spouses, good dyadic coping is considered an intrinsic resource for managing family crisis, which helps reduce caregivers' stress and burden (42, 43). This allows the spouse to work with the patient to overcome the challenges of the disease and have a positive experience.
A high level of dyadic coping is key for families to survive the crisis smoothly. The latest study confirms the conclusions of previous studies that the coping styles of patients and spouses impact the benefits finding (44, 45). When coping becomes a support system, good dyadic coping allows patients to trust that they will have support within the family when they encounter challenges (29). This support helps to enhance the individual's ability to overcome difficulties and thus find benefits in life. In addition, our findings show that the degree of benefit finding in patients and spouses can predict their family adaptation. Previous research has shown that individuals with higher levels of benefit finding are more inclined to cope with illness positively (46). Benefit finding helps individuals alleviate anxiety and depression while enhancing their ability to overcome difficulties so that families can better cope with crises and show good adaptability (41). Our study also found that the dyadic coping of breast cancer patients and their spouses indirectly affects their family finding through benefit findings. In the presence of negative emotions such as pessimism, good dyadic coping can be used as a resource within the family to help cope with crises and maintain family stability (47).
Limitations
There are some limitations to this study. First, it is impossible to infer a causal relationship between benefit finding, dyadic coping, and family adaptation using a cross-sectional design. At the same time, there is no restriction on the timing of the cancer diagnosis, which may lead to confounding factors affecting the outcome. Future longitudinal study designs are recommended to explore the relationship between these variables in depth and to understand the mechanisms by which patients at different stages of cancer interact with their spouses. Second, the data in this study are based on self-reports and there is a risk of reporting bias. The couples involved in the study may have had good family relationships, limiting the generalizability of the results. Future studies may consider using other data collection methods to explore couples with a less positive family atmosphere. Third, the study focused solely on breast cancer in women and did not take into account gender differences, other types of cancer, or the racial demographics of the population. Therefore, it is not possible to explore in depth the differences between various cancer types and the differences between various ethnic groups. Future studies are suggested to provide a more specific analysis of different cancer types and to consider the effects of gender and ethnicity. Finally, the majority of spouses in our study cared for patients for a shorter period of time and their coping styles changed over time (some spouses had better coping styles at first, but these changed as they became bored or disappointed during the course of caring). In addition, the duration of a breast cancer patient's marriage to their spouse is also a factor to consider. Therefore, in future studies, we need to conduct longitudinal studies to explore how dyadic coping, benefit finding, and family adaptation evolve during the course of patient care.
Conclusion
This study highlights a codependent relationship between breast cancer patients and their spouses. Dyadic coping in spouses is associated with beneficial findings for patients and further influences the adaptation of patients' families. Therefore, clinical staff can use the Dyadic Coping Scale to identify patients and spouses with poor coping abilities and provide positive psychological interventions to enhance the dyadic coping ability between couples to help them overcome the problems encountered during treatment and better cope with family crises. At the same time, clinicians should encourage the patient's spouse to participate actively in the cancer treatment process to help the couple develop good coping abilities. Through combined psychological interventions, communication and understanding between cancer couples can be improved. This, in turn, helps them find good things in life, cope more effectively with family crises, and improve family adaptation. In implementing this measure, clinicians should provide comprehensive support and education for patients and their spouses, along with timely and effective adjustments of intervention strategies to prevent placing unnecessary burden on the patients' families. Encouraging patients and their spouses to participate in developing and implementing the care plan can improve communication and understanding between couples, strengthen their ability to cope with the crisis, and help the entire family better adapt to the crisis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Jinzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZD: Data curation, Formal analysis, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing. YF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing. GZ: Conceptualization, Data curation, Formal analysis, Resources, Software, Writing – review & editing. XZ: Conceptualization, Investigation, Software, Writing – review & editing. XL: Conceptualization, Investigation, Writing – review & editing. YQ: Investigation, Writing – review & editing. HC: Funding acquisition, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the doctoral research Fund of Wannan Medical College (Approval No. WYRCQD202304). Funders have no role in research design, data collection and analysis, publication decisions, or manuscript preparation.
Acknowledgments
The authors sincerely thank the 650 participants who responded to the surveys and the nursing administrators from the collaborating hospitals for their support in this investigation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Zheng RS, Chen R, Han BF, Wang SM Li L, Sun KX, Zeng HM, et al. Cancer incidence and mortality in China, 2022. Chin J Oncol. (2024) 46:221–31. doi: 10.3760/cma.j.cn112152-20240119-00035
3. Mitchell AJ, Ferguson DW, Gill J, Paul J, Symonds P. Depression and anxiety in long-term cancer survivors compared with spouses and healthy controls: a systematic review and meta-analysis. Lancet Oncol. (2013) 14:721–32. doi: 10.1016/S1470-2045(13)70244-4
4. Mao S, Lu H, Zhang Y, Yu J, Li X, Peng J, et al. Evaluation of psychosocial pathways to family adaptation of Chinese patients with liver cancer using the McCubbin's Family Resilience Model. Front Psychiatry. (2021) 12:703137. doi: 10.3389/fpsyt.2021.703137
5. Li J, Liu L, Chen M, Su W, Yao T, Li X. Effect of intimacy and dyadic coping on psychological distress in pancreatic cancer patients and spousal caregivers. Front Psychol. (2023) 14:1040460. doi: 10.3389/fpsyg.2023.1040460
6. Chen W, Li H, Cai JZ, Qin N. Association between dyadic coping and quality of life in breast cancer patients and their spouses: an actor-partner interdependence mediation model. Asian Nurs Res. (2024) 18:44–50. doi: 10.1016/j.anr.2024.01.007
7. Wang N, Wang K, Lu X, Zhang S, Sun X, Zhang Y. Effects of family dignity interventions combined with standard palliative care on family adaptability, cohesion, and anticipatory grief in adult advanced cancer survivors and their family caregivers: a randomized controlled trial. Heliyon. (2024) 10:e28593. doi: 10.1016/j.heliyon.2024.e28593
8. Yeom HE, Park DS. Mediating and moderating effects of uncertainty on the relationship between family function, self-care, and depression among blood cancer survivors. Behav Sci. (2024) 14:170. doi: 10.3390/bs14030170
9. Park YY, Jeong YJ, Lee J, Moon N, Bang I, Kim H, et al. The influence of family adaptability and cohesion on anxiety and depression of terminally ill cancer patients. Support Care Cancer. (2018) 26:313–21. doi: 10.1007/s00520-017-3912-4
10. Huang BS, Lin CY, Hung TM, Chung CF, Chang YL, Chen SC. Factors influencing family function in spousal caregivers of head and neck cancer patients within 6 months posttreatment. Support Care Cancer. (2022) 30:7313–22. doi: 10.1007/s00520-022-07158-4
11. Zhou Y, Hu D, Zhang K, Mao J, Teng F, Yu T, et al. The mechanism of family adaptability and cohesion in suicidal ideation among Chinese cancer patients. J Psychosoc Oncol. (2020) 38:612–26. doi: 10.1080/07347332.2020.1757799
12. Li Y, Wang K, Yin Y, Li Y, Li S. Relationships between family resilience, breast cancer survivors' individual resilience, and caregiver burden: a cross-sectional study. Int J Nurs Stud. (2018) 88:79–84. doi: 10.1016/j.ijnurstu.2018.08.011
13. Mei YX, Xiang DD, Zhang ZX, Twumwaah Budu J, Lin BL, Chen SY. Family function, self-efficacy, care hours per day, closeness and benefit finding among stroke caregivers in China: a moderated mediation model. J Clin Nurs. (2023) 32:506–16. doi: 10.1111/jocn.16290
14. Jahnen M, Bayer P, Meissner VH, Schiele S, Schulwitz H, Gschwend JE, et al. Benefit finding in men affected by prostate cancer prior to and following radical prostatectomy - a cross-sectional study with a stratified sample. BMC Cancer. (2023) 23:508. doi: 10.1186/s12885-023-11018-7
15. Cao Q, Gong J, Chen M, Lin Y, Li Q. The dyadic effects of self-efficacy on quality of life in advanced cancer patient and family caregiver dyads: the mediating role of benefit finding, anxiety, and depression. J Oncol. (2022) 2022:3073358. doi: 10.1155/2022/3073358
16. Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. J Consult Clin Psychol. (2006) 74:797–816. doi: 10.1037/0022-006X.74.5.797
17. Ding Z, Fan Y, Li E, Ai F, Cui H. Latent profile analysis of family adaptation in breast cancer patients-cross-sectional study. Sci Rep. (2024) 14:21357. doi: 10.1038/s41598-024-72410-2
18. Abulaiti B, Zhang X, Guan T, Wang M, Jia S, Wang A. The dyadic care experiences of elderly individuals with disabilities and caregivers in the home setting from the perspective of family resilience: a qualitative study. Front Psychiatry. (2022) 13:963101. doi: 10.3389/fpsyt.2022.963101
19. Randall AK, Bodenmann G. Stress and its associations with relationship satisfaction. Curr Opin Psychol. (2017) 13:96–106. doi: 10.1016/j.copsyc.2016.05.010
20. Zimmermann T. Intimate relationships affected by breast cancer: interventions for couples. Breast Care. (2015) 10:102–8. doi: 10.1159/000381966
21. Lau N, Ramos KJ, Aitken ML, Goss CH, Barton KS, Kross EK, et al. “We'll deal with it as it comes”: a qualitative analysis of romantic partners' dyadic coping in cystic fibrosis. J Soc Pers Relat. (2024) 41:689–705. doi: 10.1177/02654075231190617
22. Van Schoors M, Loeys T, Goubert L, Berghmans G, Ooms B, Lemiere J, et al. Couples dealing with pediatric blood cancer: a study on the role of dyadic coping. Front Psychol. (2019) 10:402. doi: 10.3389/fpsyg.2019.00402
23. Liu W, Lewis FM, Oxford M, Kantrowitz-Gordon I. Common dyadic coping and its congruence in couples facing breast cancer: the impact on couples' psychological distress. Psychooncology. (2024) 33:e6314. doi: 10.1002/pon.6314
24. Ruark A, Bidwell JT, Butterfield R, Weiser SD, Neilands TB, Mulauzi N, et al. “I too have a responsibility for my partner's life”: Communal coping among Malawian couples living with HIV and cardiometabolic disorders. Soc Sci Med (1982). (2024) 342:116540. doi: 10.1016/j.socscimed.2023.116540
25. Schock-Giordano AM. Ethnic families and mental health: application of the ABC-X model of family stress. Sage Open. (2013) 3:2158244013478015. doi: 10.1177/2158244013478015
26. Kenny DA, Cook W. Partner effects in relationship research: conceptual issues, analytic difficulties, and illustrations. Pers Relatsh. (1999) 6:433–48. doi: 10.1111/j.1475-6811.1999.tb00202.x
27. Kenny DA, Ledermann T. Detecting, measuring, and testing dyadic patterns in the actor-partner interdependence model. J Fam Psychol. (2010) 24:359–66. doi: 10.1037/a0019651
28. Kang H. Sample size determination and power analysis using the G*Power software. J Educ Eval Health Prof. (2021) 18:17. doi: 10.3352/jeehp.2021.18.17
29. Bodenmann G. A systemic-transactional conceptualization of stress and coping in couples. Swiss J Psychol. (1995) 54:34–49. doi: 10.1111/j.1749-6632.1995.tb38155.x
30. Xu F, Hilpert P, Randall AK Li Q, Bodenmann G. Validation of the dyadic coping inventory with Chinese couples: factorial structure, measurement invariance, and construct validity. Psychol Assess. (2016) 28:e127–40. doi: 10.1037/pas0000329
31. Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. (2001) 20:20–32. doi: 10.1037/0278-6133.20.1.20
32. Liu Z, Zhang F, Gudenkauf L. Cross-cultural adaptation of the Benefit Finding Scale(BFS) in Chinese Cancer Patients. Chin J Nurs. (2015) 50:561–6. doi: 10.3761/j.issn.0254-1769.2015.05.010
33. Olson DH, Sprenkle DH, Russell CS. Circumplex model of marital and family system: I. Cohesion and adaptability dimensions, family types, and clinical applications. Fam Process. (1979) 18:3–28. doi: 10.1111/j.1545-5300.1979.00003.x
34. Phillips MR, West CL, Shen Q, Zheng Y. Comparison of schizophrenic patients' families and normal families in China, using Chinese versions of FACES-II and the Family Environment Scales. Fam Process. (1998) 37:95–106. doi: 10.1111/j.1545-5300.1998.00095.x
35. Priem JS. Actor–Partner Interdependence Model. The International Encyclopedia of Interpersonal Communication. New York, NY (2015). p. 1–6.
36. Guyard A, Michelsen SI, Arnaud C, Fauconnier J. Family adaptation to cerebral palsy in adolescents: a European multicenter study. Res Dev Disabil. (2017) 61:138–50. doi: 10.1016/j.ridd.2016.11.010
37. Park M, Choi EK Lyu CJ, Han JW, Hahn SM. Family resilience factors affecting family adaptation of children with cancer: a cross-sectional study. Eur J Oncol Nurs. (2022) 56:102078. doi: 10.1016/j.ejon.2021.102078
38. Hesamzadeh A, Dalvandi A, Bagher Maddah S, Fallahi Khoshknab M, Ahmadi F. Family adaptation to stroke: a metasynthesis of qualitative research based on double ABCX model. Asian Nurs Res. (2015) 9:177–84. doi: 10.1016/j.anr.2015.03.005
39. Li T, Liu RX, Lau EYY. Companionship goals and marital goal concordance contribute to relationship satisfaction partly through dyadic coping in dating couples. Anxiety Stress Coping. (2024) 37:685–98. doi: 10.1080/10615806.2024.2338107
40. Bröning S, Wartberg L. Attachment orientations: associations with romantic partners' self-regulation and dyadic coping. J Sex Marit Ther. (2024) 50:512–26. doi: 10.1080/0092623X.2024.2322566
41. Wen X, Wang D, Li N, Qin X, Gu D. The construction of the structural equation model of burden, benefit finding, and anxiety-depression of esophageal cancer caregivers based on Lazarus stress and coping theory. Ann Palliat Med. (2021) 10:7644–52. doi: 10.21037/apm-21-1466
42. Gardner MH, Mrug S, Schwebel DC, Phipps S, Whelan K, Madan-Swain A. Demographic, medical, and psychosocial predictors of benefit finding among caregivers of childhood cancer survivors. Psychooncology. (2017) 26:125–32. doi: 10.1002/pon.4014
43. Ferraris G, Gérain P, Zarzycki M, Elayan S, Morrison V, Sanderman R, et al. The associations of dyadic coping strategies with caregiver's willingness to care and burden: a weekly diary study. J Health Psychol. (2024) 29:935–49. doi: 10.1177/13591053231223838
44. Li L, Zhong HY, Xiao T, Xiao RH, Yang J, Li YL, et al. Association between self-disclosure and benefit finding of Chinese cancer patients caregivers: the mediation effect of coping styles. Support Care Cancer. (2023) 31:684. doi: 10.1007/s00520-023-08158-8
45. Liu Z, Zhang L, Cao Y, Xia W, Zhang L. The relationship between coping styles and benefit finding of Chinese cancer patients: the mediating role of distress. Eur J Oncol Nurs. (2018) 34:15–20. doi: 10.1016/j.ejon.2018.03.001
46. Yang J, Yan HL Li YQ, Zhang L, Qiu XY, Tian YH, Gong YL, et al. Benefit finding in chronic kidney disease patients receiving hemodialysis: a cross-sectional study. BMC Nephrol. (2024) 25:46. doi: 10.1186/s12882-024-03480-7
Keywords: dyadic coping, family adaptation, benefit finding, family stress coping theory, actor-partner
Citation: Ding Z, Fan Y, Zhong G, Zhang X, Li X, Qiao Y and Cui H (2024) A dyadic analysis of family adaptation among breast cancer patients and their spouses based on the framework of family stress coping theory. Front. Public Health 12:1453830. doi: 10.3389/fpubh.2024.1453830
Received: 24 June 2024; Accepted: 04 November 2024;
Published: 25 November 2024.
Edited by:
Edmund Howe, Uniformed Services University of the Health Sciences, United StatesReviewed by:
Aristea Ilias Ladas, University of York Europe Campus, GreeceSemra Bulbuloglu, Istanbul Aydın University, Türkiye
Copyright © 2024 Ding, Fan, Zhong, Zhang, Li, Qiao and Cui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huixia Cui, MTMxOTQ0NzM2N0BxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Zhangyi Ding
Zhangyi Ding Yarong Fan2†
Yarong Fan2† Gaoxiang Zhong
Gaoxiang Zhong