- 1Department of Community Medicine, Rawalpindi Medical University, Rawalpindi, Pakistan
- 2Health Services Academy, Islamabad, Islamabad, Pakistan
- 3Department of Family and Community Medicine, Faculty of Medicine in Rabigh, King Abdulaziz University, Jeddah, Saudi Arabia
- 4Department of Biochemistry, Faculty of Medicine in Rabigh, King Abdulaziz University, Jeddah, Saudi Arabia
Background: Cervical cancer burden in South Asia is among the highest globally. Due to the lack of national immunization programs, the prevalence of human papillomavirus (HPV) infection and vaccine uptake remains unknown. This systematic review and meta-analysis aim to determine the prevalence of HPV vaccine uptake in South Asia.
Methods: We conducted a comprehensive search of MEDLINE (via PubMed), Embase, the Cochrane Library, and the Web of Science, covering the period from inception to May 20, 2024. We included observational studies reporting HPV vaccine uptake in South Asia, without any language filters or restrictions. The search strategy involved MeSH terms and relevant keywords related to “Papillomavirus Infections,” “Vaccination,” and “Uptake.” MetaXL and STATA were used to perform a proportional meta-analysis and meta-regression analysis.
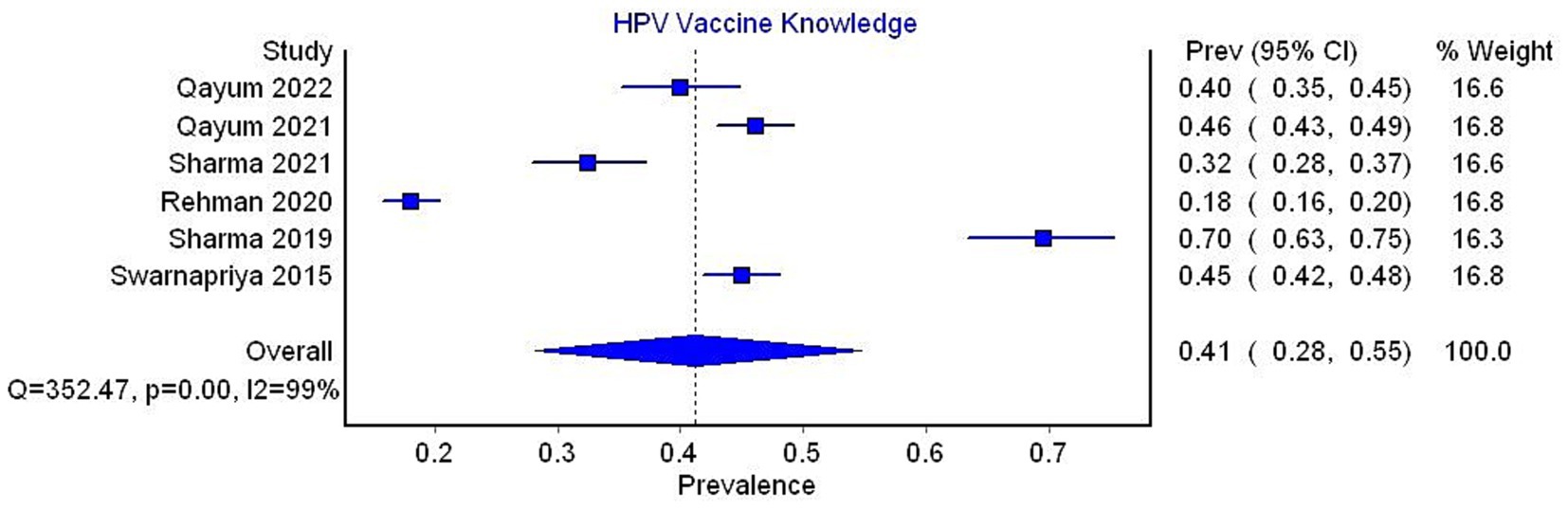
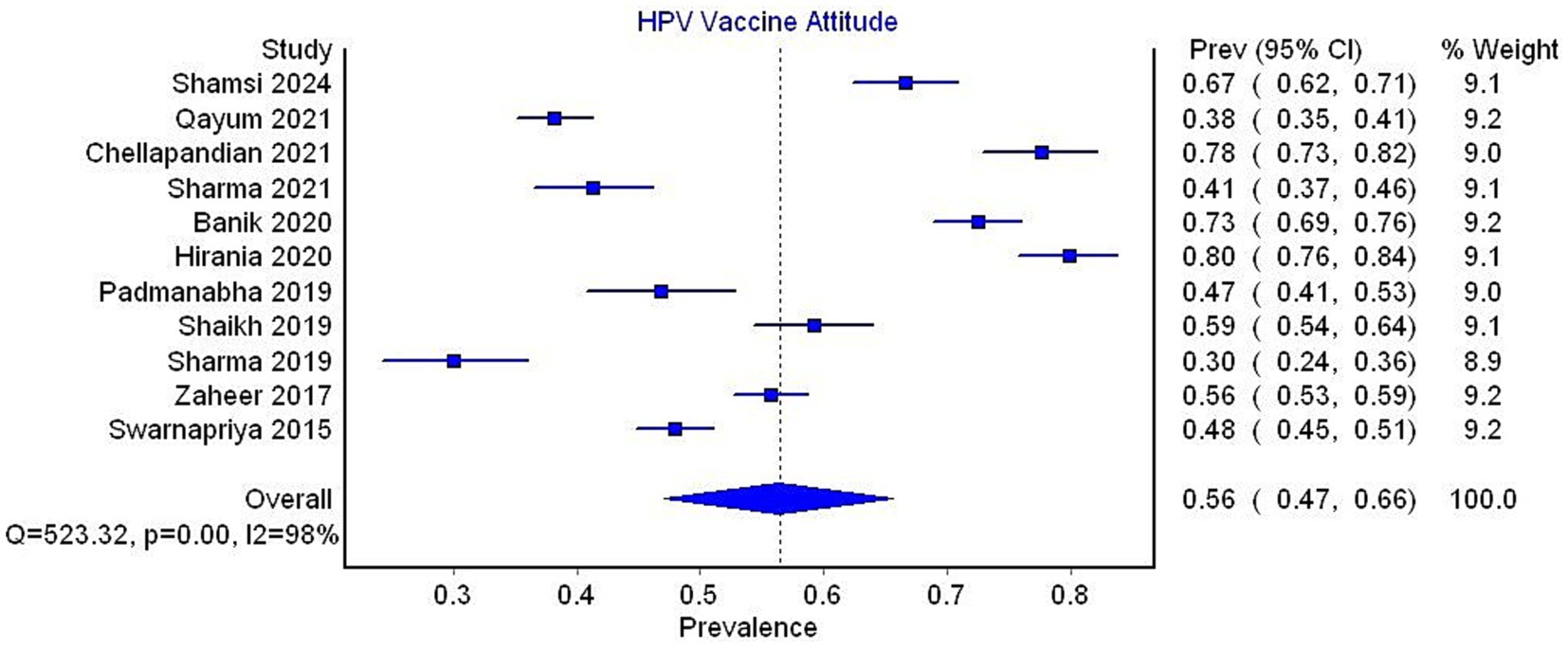
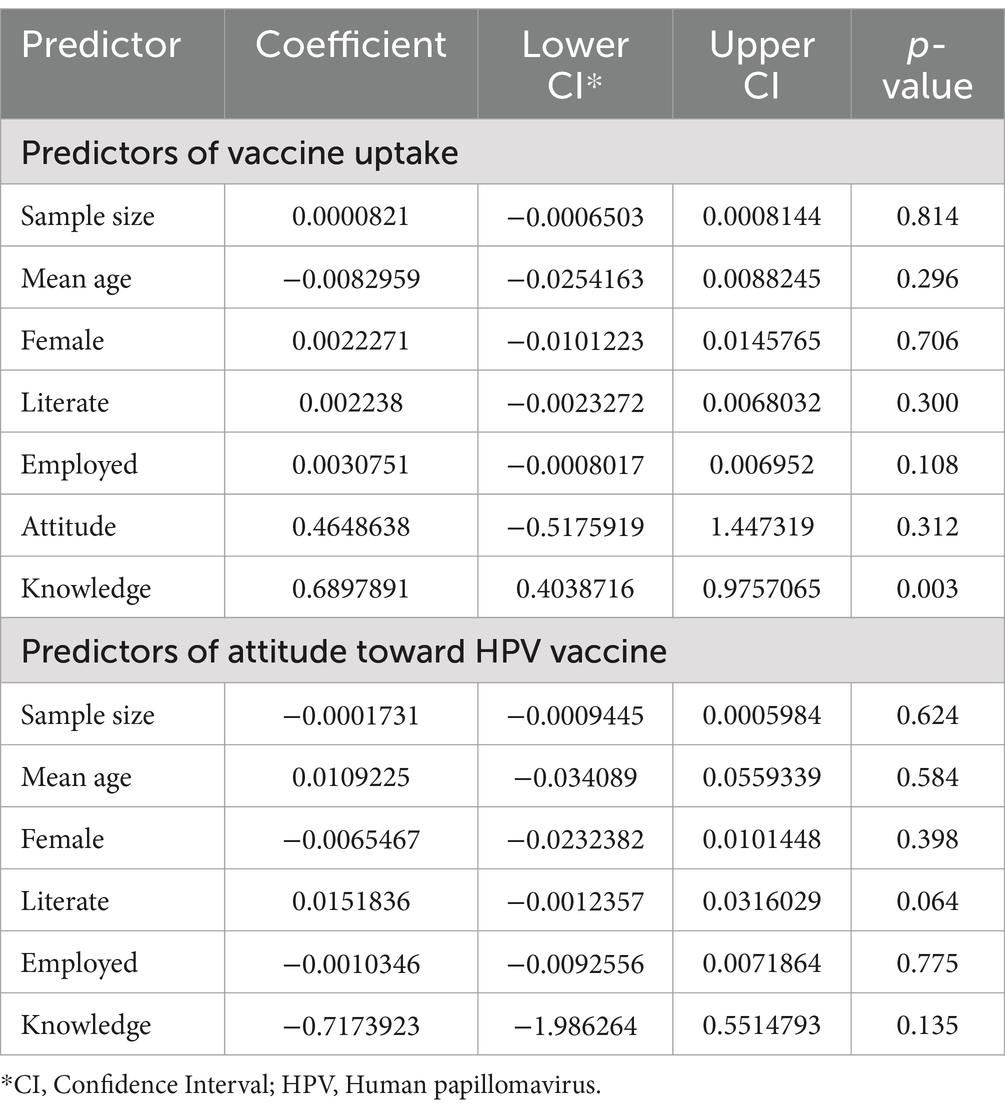
Results: Out of 3,913 articles identified, 17 articles (10,585 participants) were included in the systematic review. The pooled prevalence of vaccine uptake was 8% (95% CI 1–21). There was high heterogeneity between studies (I2 = 100%). The pooled prevalence of adequate knowledge of the HPV vaccine was 41% (95% CI 28–55, I2 = 99%). The pooled prevalence of a favorable attitude toward the HPV vaccine was 56% (95% CI 47–66, I2 = 98%). In the univariate meta-regression model, good knowledge significantly predicted HPV vaccine uptake (p = 0.003), while no covariates were found to be significant predictors of attitudes toward HPV vaccine uptake.
Conclusion: The findings of this meta-analysis indicate a low pooled prevalence of HPV vaccine uptake (8%) in South Asian countries. The pooled prevalence of adequate knowledge and a favorable attitude toward the vaccine were 41 and 56%, respectively. In the univariate meta-regression model, knowledge of the HPV vaccine uptake was the only significant predictor of vaccine uptake.
Systematic review registration: Systematic review is registered at Prospero through the link
Introduction
According to the GLOBOCAN 2020 database, there were over six million new cases and 340,000 deaths attributed to cervical cancer in 2020, making up nearly 3 % of both global cancer incidence and mortality (1). Cervical cancer is the fourth most common cancer in women, following breast, colorectal, and lung cancers. Low and middle-income countries carry the largest burden, accounting for almost 80% of new cases and 90% of deaths from cervical cancer (2).
Several risk factors have been identified for cervical cancer, including tobacco use, immunodeficiency, multiple pregnancies, and family history. However, the primary cause is widely accepted to be human papillomavirus (HPV) infection (3–5). HPV is one of the most prevalent sexually transmitted diseases in both men and women (6). There are over 130 serotypes of HPV, with high-risk serotypes 16 and 18 being most commonly associated with cervical cancer (7). The central role of HPV in cervical cancer pathogenesis makes this disease highly preventable.
The introduction of HPV vaccines, such as Gardasil and Cervarix, represents a groundbreaking advancement in the prevention of cervical cancer and other HPV-related diseases (8, 9). These vaccines offer long-term immunity with high efficacy but have potential side effects and require multiple doses. Following promising clinical trial results, 64 countries have launched national immunization programs with the goal of vaccinating 90% of girls by age 15 by 2030 (10, 11). The widespread rollout of the HPV vaccine in most developed countries has shifted the global burden of the disease toward low and middle-income countries (12). Currently, 85% of high-income countries, 25% of upper-middle-income countries, 30% of lower-middle-income countries, and 60% of low-income countries have national immunization programs (10).
The South Asian region, which includes India, Pakistan, Bangladesh, Nepal, Afghanistan, Sri Lanka, Bhutan, and Maldives, is home to 21% of the world’s population (13). Most countries in this region fall under the “low-middle-income country (LMIC)” classification. Despite the World Health Organization (WHO) highlighting strategies for cervical cancer eradication in LMICs, the uptake of the HPV vaccine in South Asia has been inadequate, with India alone accounting for a fifth of the global burden of the disease (10). Only Bhutan, Sri Lanka, and Maldives have included HPV vaccination in their national immunization programs (14).
Some progress has been made recently, with the completion of pilot projects for a vaccination program in Bangladesh and the launch of India’s first locally produced HPV vaccine (15). However, several sociocultural factors pose significant obstacles to the rapid rollout of vaccination programs across the region (16, 17). Data on the uptake of the HPV vaccine and attitudes toward vaccination are scarce and inconclusive. Therefore, systematic review is conducted and proportional meta-analysis to determine the pooled prevalence of HPV vaccine uptake and its determinants in South Asia.
Methods
The present systematic review and meta-analysis followed the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and was registered with PROSPERO (CRD42024547393) (18).
Search strategy
MEDLINE (via PubMed), Embase, the Cochrane Library, and the Web of Science from inception to May 20, 2024, without any language filters or restrictions were searched. The search strategy included MeSH terms and relevant keywords for “Papillomavirus Infections,” “Vaccination,” and “Uptake.” Detailed search strategy include Boolean operators ‘OR’ and ‘AND’ (“Papillomavirus Infections” [Mesh] OR Papillomavirus Infection OR Human Papillomavirus Infection OR Human Papillomavirus Infections OR HPV Infection OR HPV Infections) AND (“Vaccination” [Mesh] OR Vaccinations OR Active Immunization OR Active Immunizations) AND (“Uptake” [All Fields] OR “Practice” [All Fields] OR “utilization” [All Fields]). We also hand-searched the reference lists of relevant articles for additional references.
(“Papillomavirus” [Mesh] OR Human Papillomavirus OR Human Papillomavirus OR HPV) AND (“Vaccination” [Mesh] OR Vaccinations OR Active Immunization OR Active Immunizations) AND (“Uptake” [All Fields] OR “Practice” [All Fields] OR “utilization” [All Fields]) AND (India OR Pakistan OR Bangladesh OR Nepal OR Afghanistan OR Sri Lanka OR Bhutan OR Maldives).
Study selection and eligibility criteria
The search strategy imported the references into Endnote version 20. Two authors (KN and SN) independently screened the articles, with disagreements resolved by other authors (MAM, MBM, and SAK). The eligibility requirements were as follows: (1) The population consists of South Asian nationals who have not received a cervical cancer diagnosis, (2) the outcome is the prevalence of HPV vaccine uptake, and (3) the study design is observational studies.
Data extraction and outcomes
Data was extracted data on study characteristics (author name, publication year, study setting, and sample size), participant sociodemographic characteristics (age, sex, marital status, literacy, and employment), and our outcomes using Microsoft Excel. The primary outcome of interest was the prevalence of HPV vaccine uptake. The secondary outcomes were the prevalence of good knowledge of HPV vaccination and a positive attitude toward HPV vaccination. Two authors (KN and SN) independently extracted data, and disagreements were resolved by other authors (MAM, MB, and SAK).
Quality assessment
The “National Institute of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross-sectional Studies” was used for quality assessment (19). Two authors (KN and SN) independently assessed the quality of the included studies, with disagreements settled by a third author (MAM, MB, and SAK). The traffic light plots was constructed using Robvis (20).
Data analysis
As all outcomes were prevalence, we performed a meta-analysis of proportions. The Freeman-Tukey double arcsine transformation was used to stabilize variances. The random-effects model with the DerSimonian Laird method to pool transformed proportions before back-transforming them. The forest plots and computed I2 statistics were constructed to assess heterogeneity. The subgroup analysis was conducted based on the country of study and occupation. Meta-regression was also performed to determine predictors of the prevalence of HPV vaccine uptake and attitude toward the HPV vaccine. All statistical analyses were performed in MetaXL and STATA.
Results
Search results
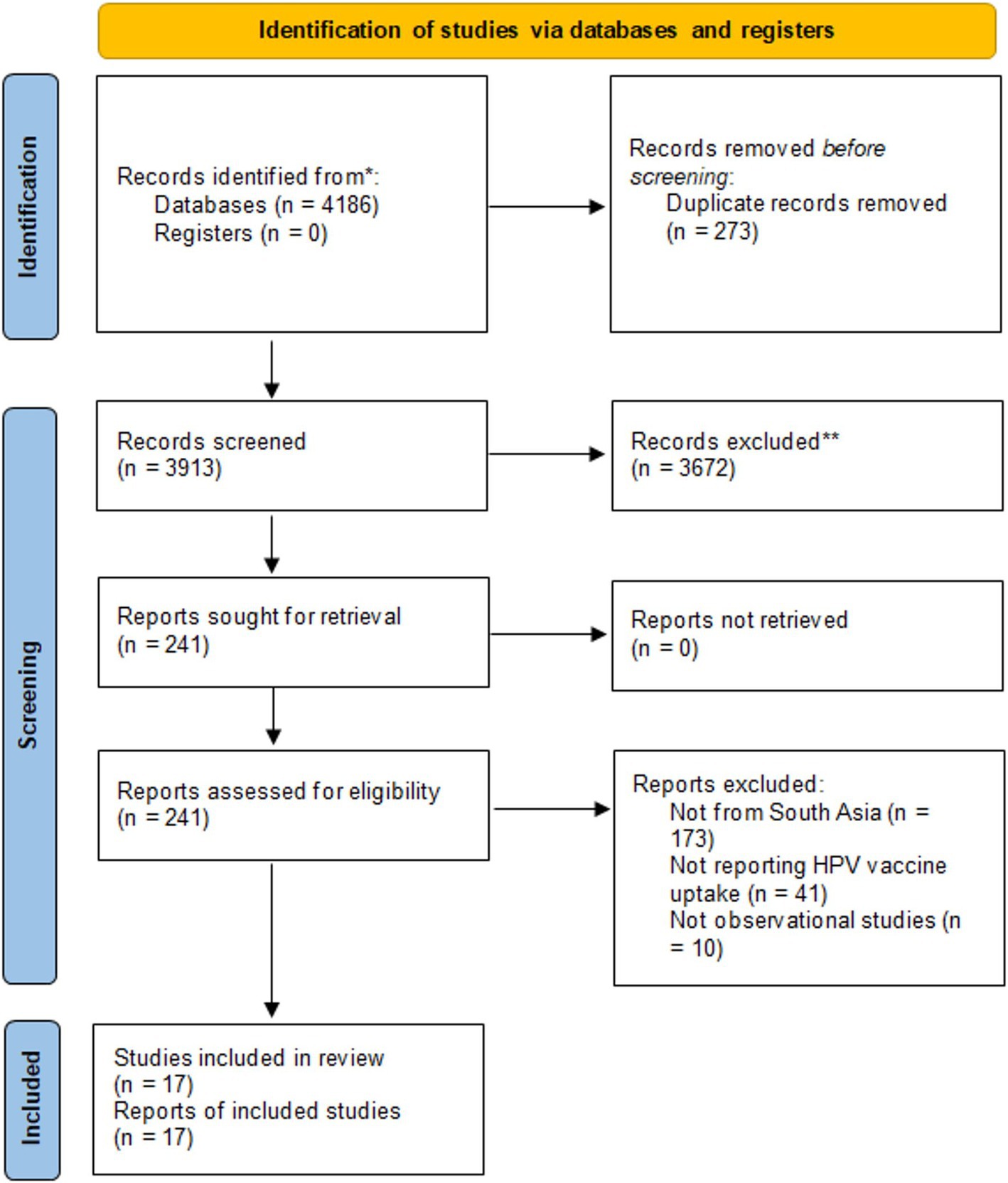
The initial search retrieved 4,186 articles. After removing 273 duplicates, we assessed the remaining 3,913 articles for eligibility. The titles and abstracts were reviewed and excluded 3,672 articles. Full texts of the remaining 241 articles were assessed against the eligibility criteria. Finally, 17 articles were included. Figure 1 provides details of the screening process.
Study characteristics
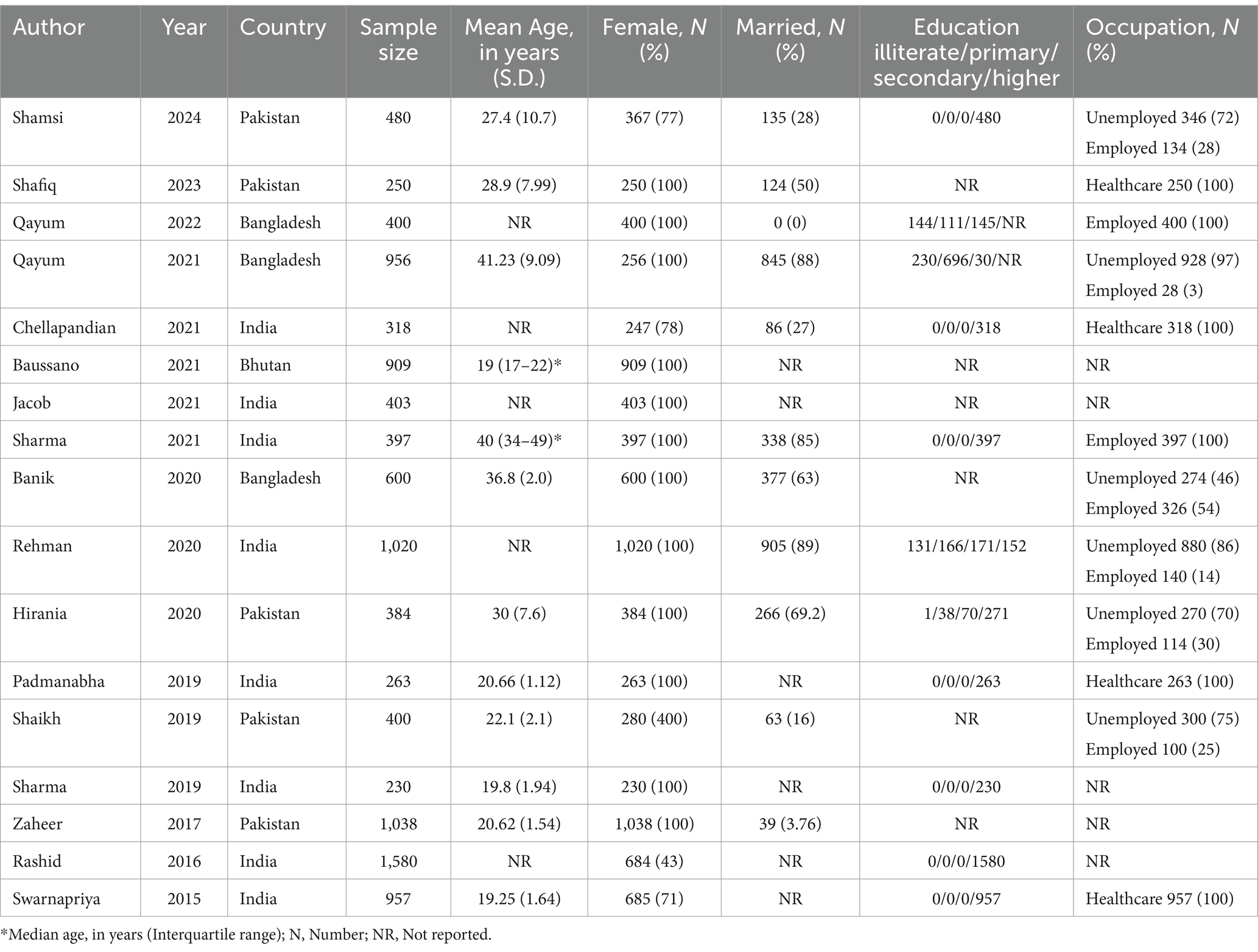
Of the 17 studies included in our review, 8 were conducted in India (21–28), 5 in Pakistan (29–33), 3 in Bangladesh (34–36), and 1 in Bhutan (37). The publication years ranged from 2015 to 2024. A total of 10,585 participants were included, with 8,413 (79.5%) being females. The mean age ranged from 19 to 40 years. Table 1 summarizes the characteristics of the included studies.
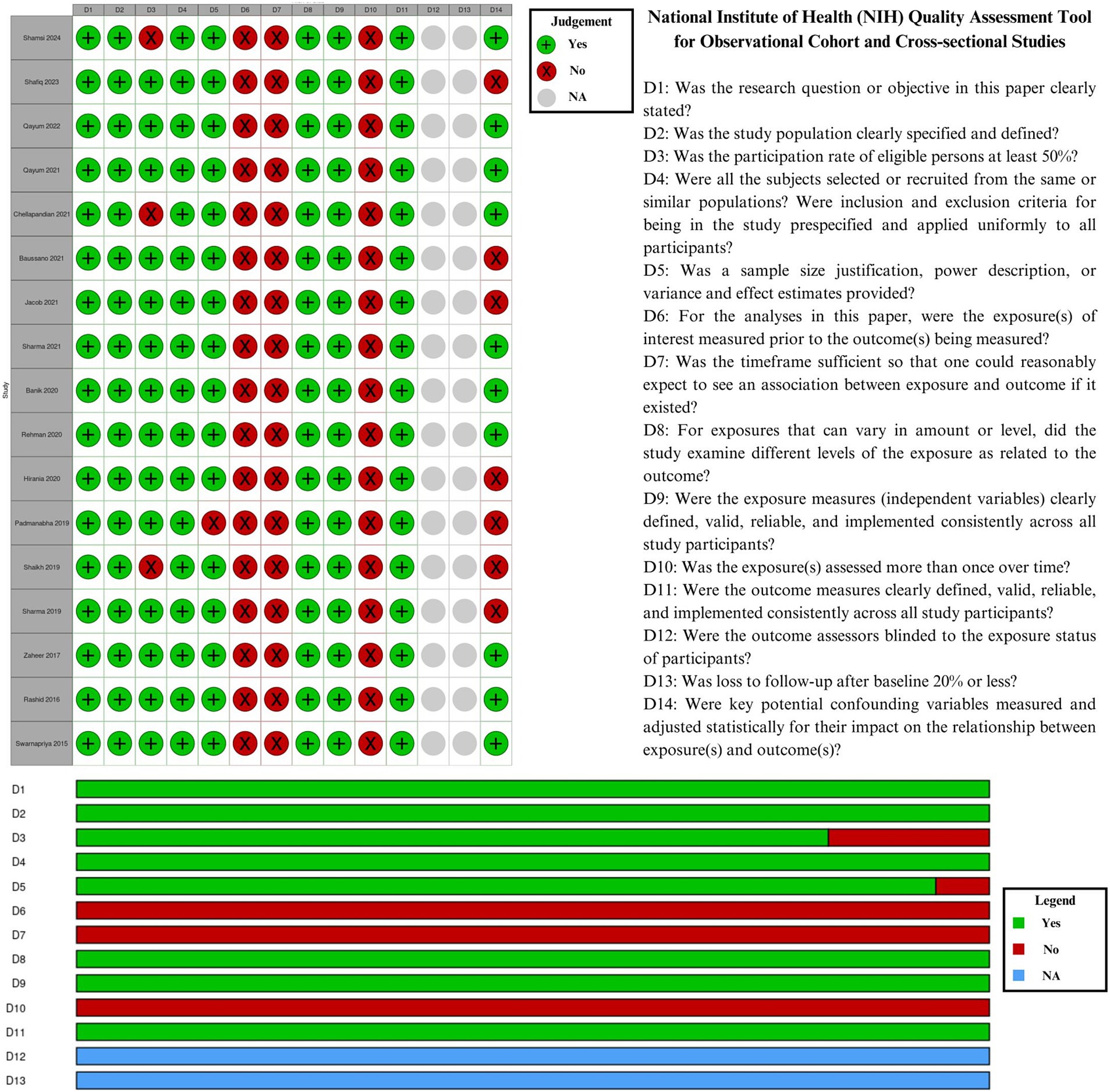
Quality assessment of included studies
In Figure 2, the quality assessment of the included studies was presented as a traffic light plot and a summary plot. Due to their cross-sectional nature, all studies scored poorly in D6 (exposures measured before outcomes), D7 (sufficient timeframe), and D10 (exposures assessed over time). D12 (blinding) and D13 (loss to follow-up) were considered not applicable exclusively to cohort studies.
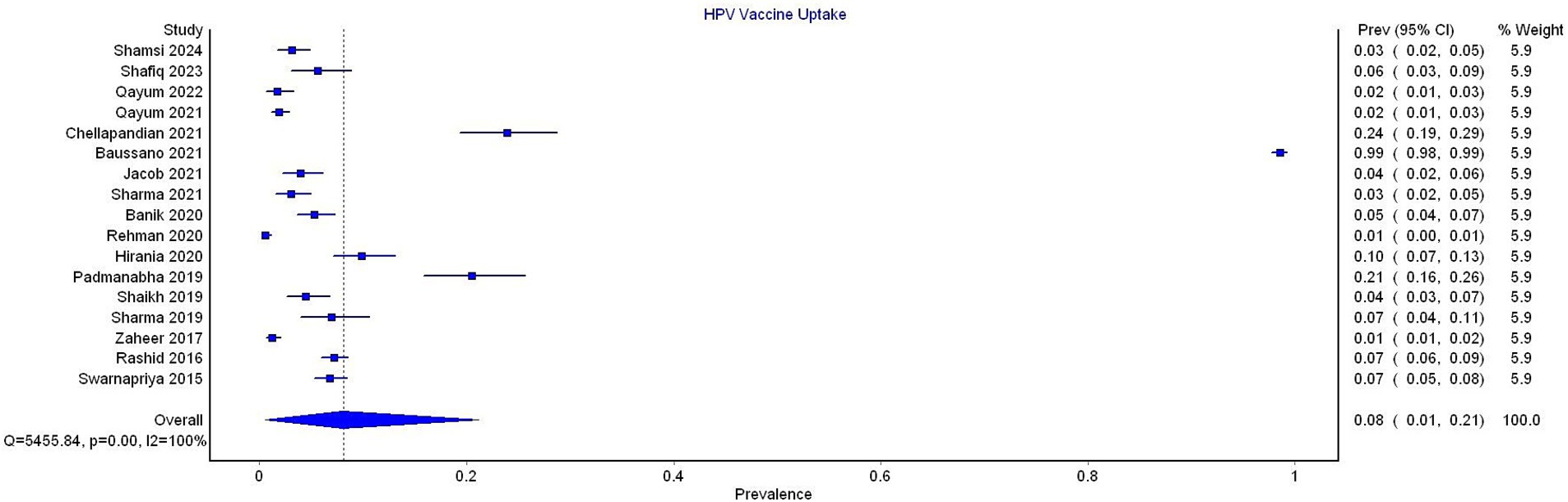
Proportional meta-analysis for vaccine uptake
All 17 studies reported data on HPV vaccine uptake. The pooled prevalence of vaccine uptake was 8% (95% CI 1–21). The substantial heterogeneity was noted (I2 = 100%) (Figure 3).
In the subgroup analysis by country, the pooled prevalence was 6% (95% CI 3–13, 8 studies, I2 = 97%) for India, 4% (95% CI 2–8, 5 studies, I2 = 93%) for Pakistan, and 3% (95% CI 1–5%, 3 studies, I2 = 87%) for Bangladesh. Only one study reported data from Bhutan, which showed a prevalence of 99% (Figure 4).
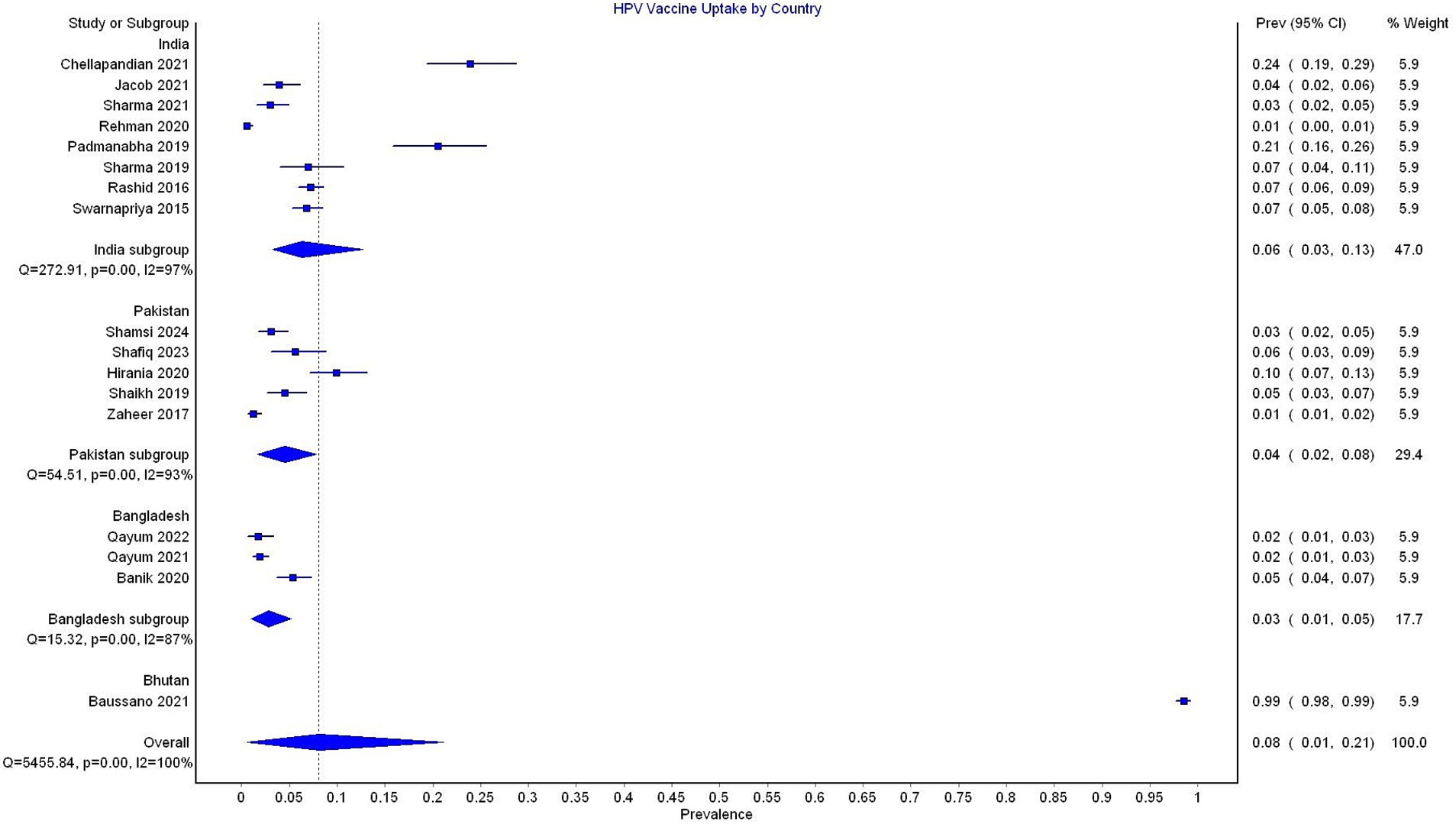
Figure 4. Forest plot depicting subgroup analysis by country for the prevalence of HPV vaccine uptake.
In the subgroup analysis by occupation, studies reporting data exclusively on healthcare workers reported a pooled prevalence of 12% (95% CI 5–23, 4 studies, I2 = 97%), compared to a prevalence of 7% (95% CI 0–23, 13 studies, I2 = 100%) reported in studies not exclusively focusing on healthcare workers (Figure 5).
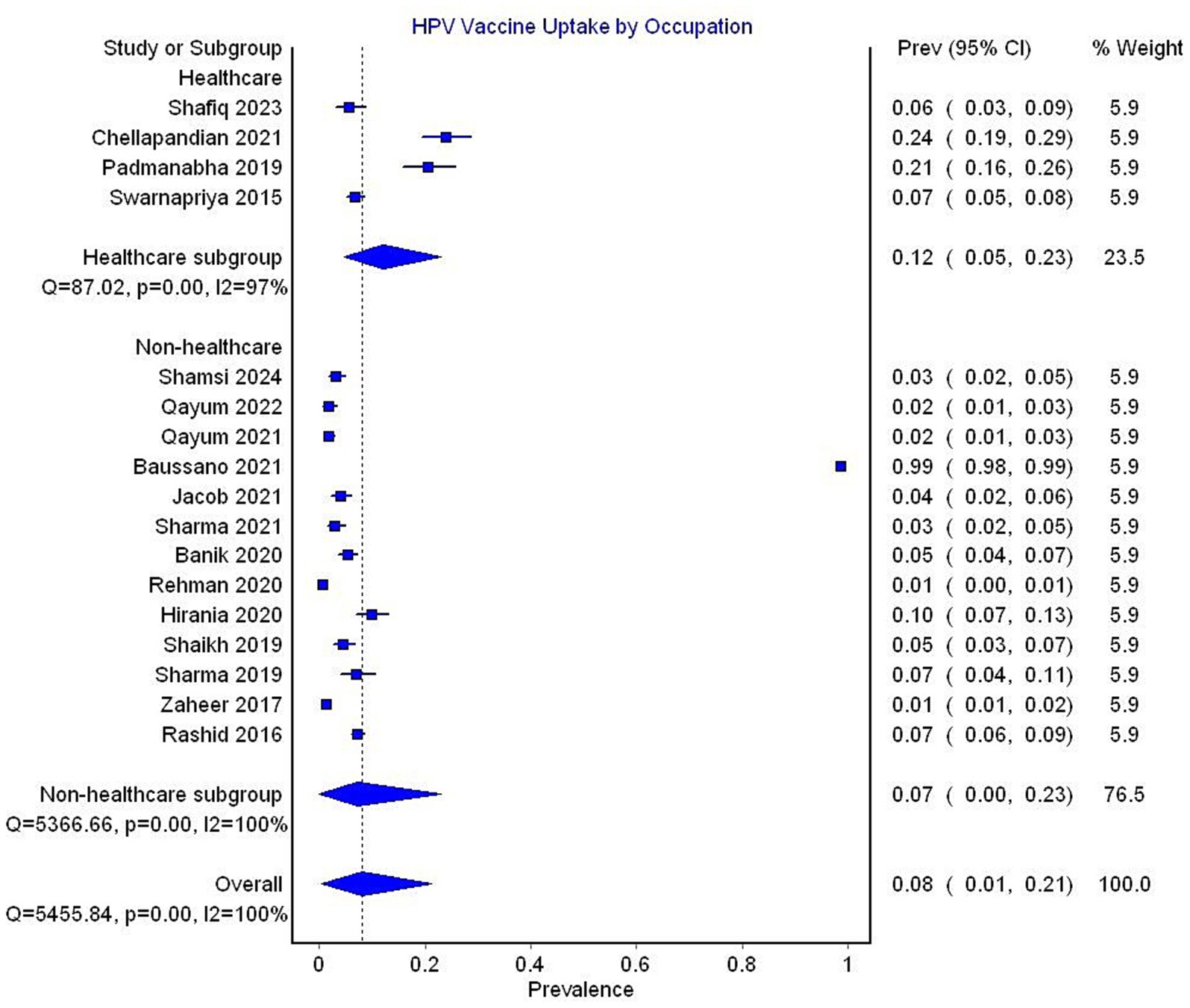
Figure 5. Forest plot depicting subgroup analysis by occupation for the prevalence of HPV vaccine uptake.
Proportional meta-analysis for knowledge of HPV vaccine
The pooled prevalence of adequate knowledge of the HPV vaccine was 41% (95% CI 28–55, I2 = 99%), based on data from 6 studies (Figure 6).
In the subgroup analysis by country, HPV vaccine knowledge was reported to be 40% (95% CI 21–61, 4 studies, I2 = 99%) in India and 43% (95% CI 37–49, 2 studies, I2 = 77%) in Bangladesh (Figure 7).
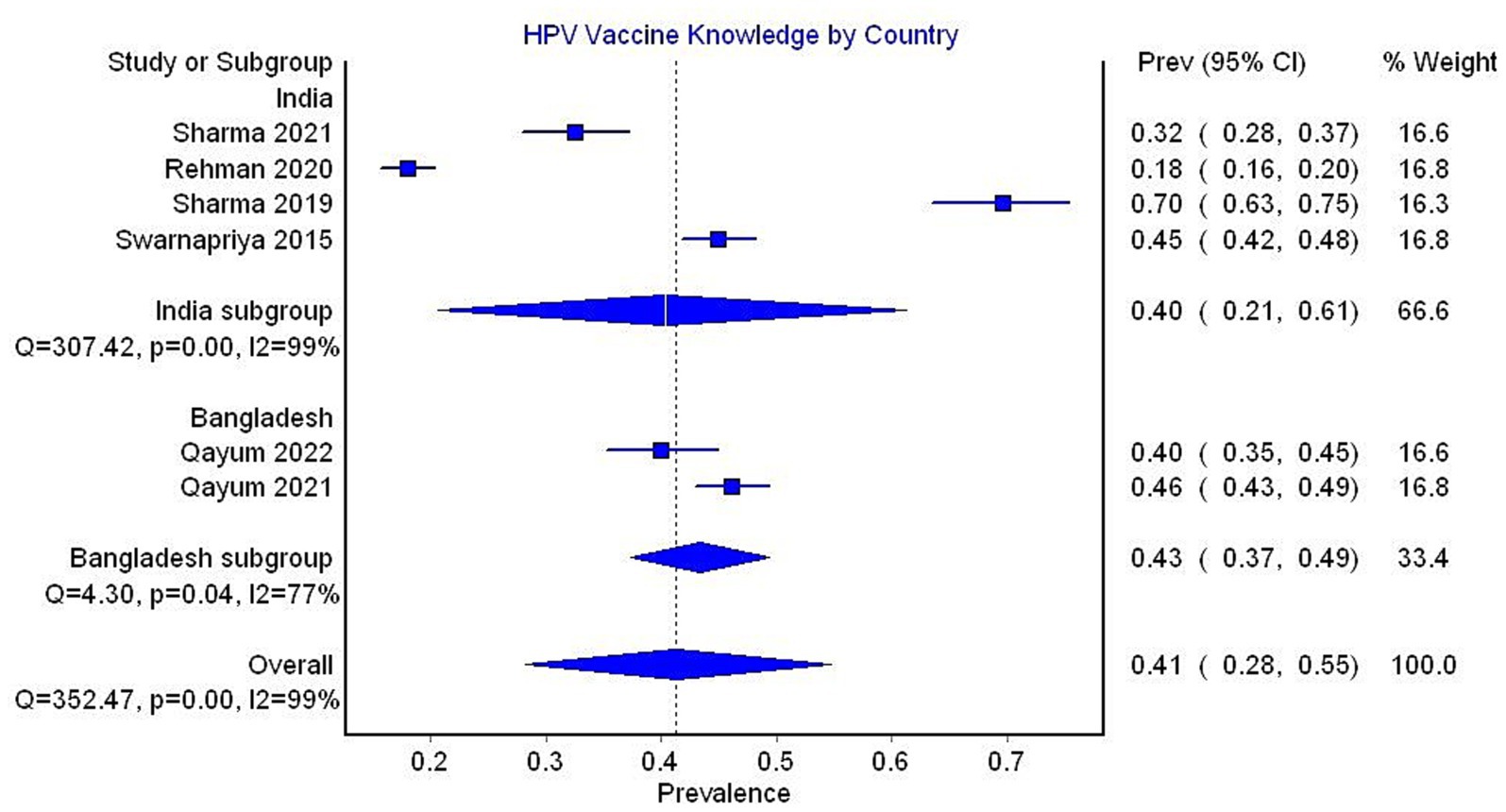
Figure 7. Forest plot depicting subgroup analysis by country for the prevalence of HPV vaccine knowledge.
In the subgroup analysis by occupation, only one study reporting data on healthcare professionals was included, with 45% of the sample having adequate knowledge. The pooled prevalence for non-healthcare studies was 40% (95% CI 24–57, 5 studies, I2 = 99%) (Figure 8).
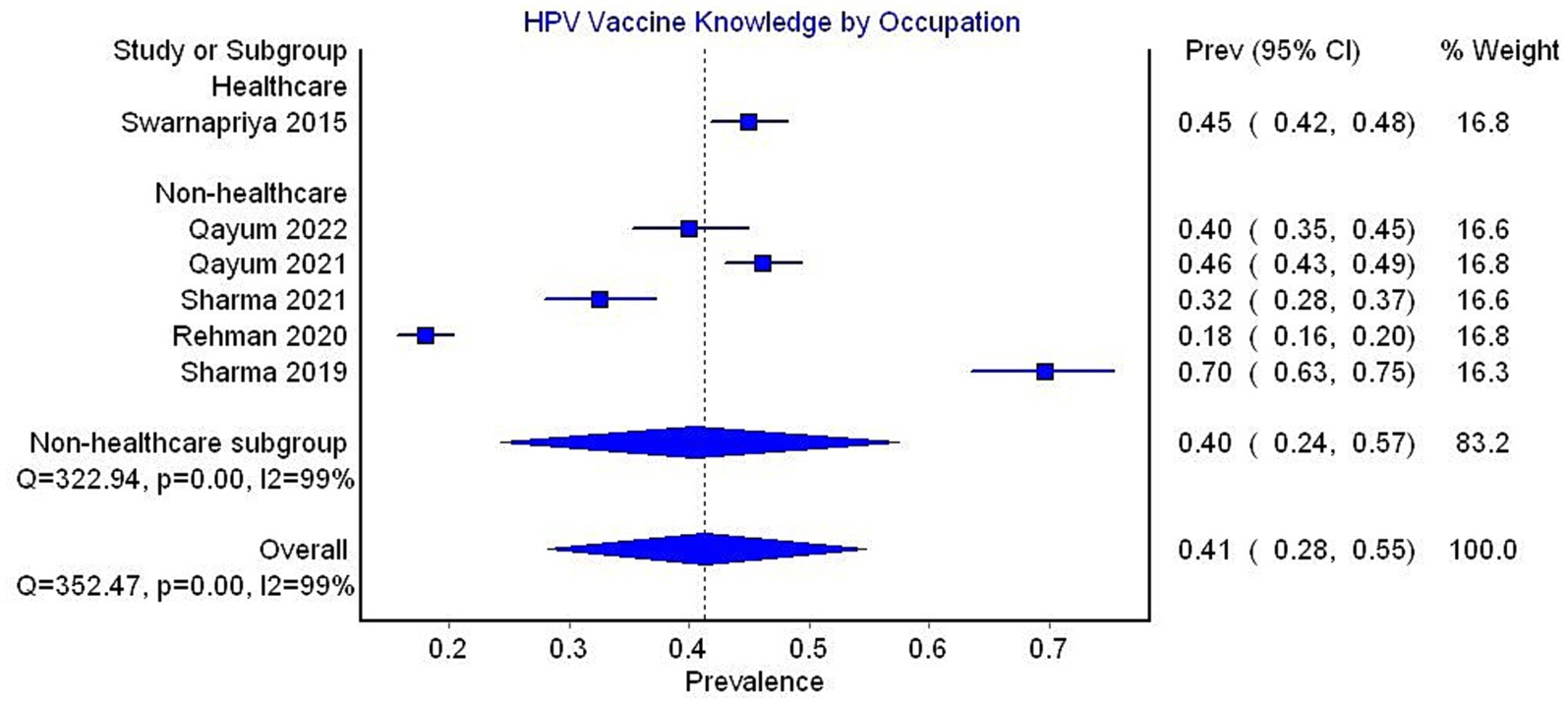
Figure 8. Forest plot depicting subgroup analysis by occupation for the prevalence of HPV vaccine knowledge.
Proportional meta-analysis for attitudes toward HPV vaccine
Eleven studies were included in the analysis and found that the pooled prevalence of a favorable attitude toward the HPV vaccine was 56% (95% CI 47–66, I2 = 98%) (Figure 9).
In the subgroup analysis by country, the pooled prevalence of a favorable attitude toward the HPV vaccine was 49% (95% CI 35–63, 5 studies, I2 = 98%) for India, 66% (95% CI 55–76, 4 studies, I2 = 96%) for Pakistan, and 56% (95% CI 20–90, 2 studies, I2 = 99%) for Bangladesh (Figure 10).
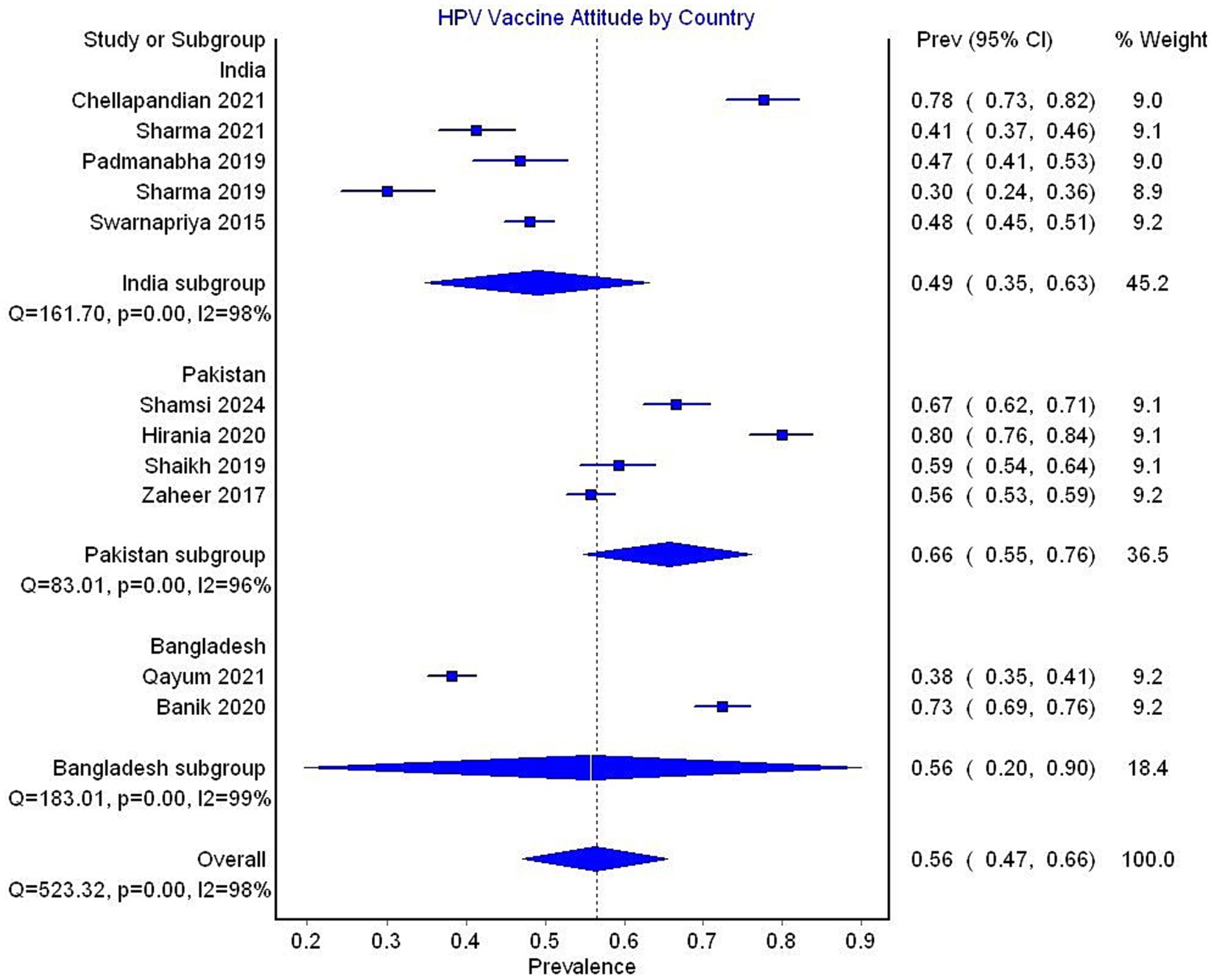
Figure 10. Forest plot depicting subgroup analysis by country for the prevalence of attitude toward HPV vaccine.
In the subgroup analysis by occupation, studies exclusively reporting data on healthcare workers showed a pooled prevalence of a favorable attitude toward the HPV vaccine of 58% (95% CI 38–77, 3 studies, I2 = 98%), compared to a prevalence of 56% (95% CI 44–67, 8 studies, I2 = 98%) reported in studies that did not exclusively focus on healthcare workers (Figure 11).
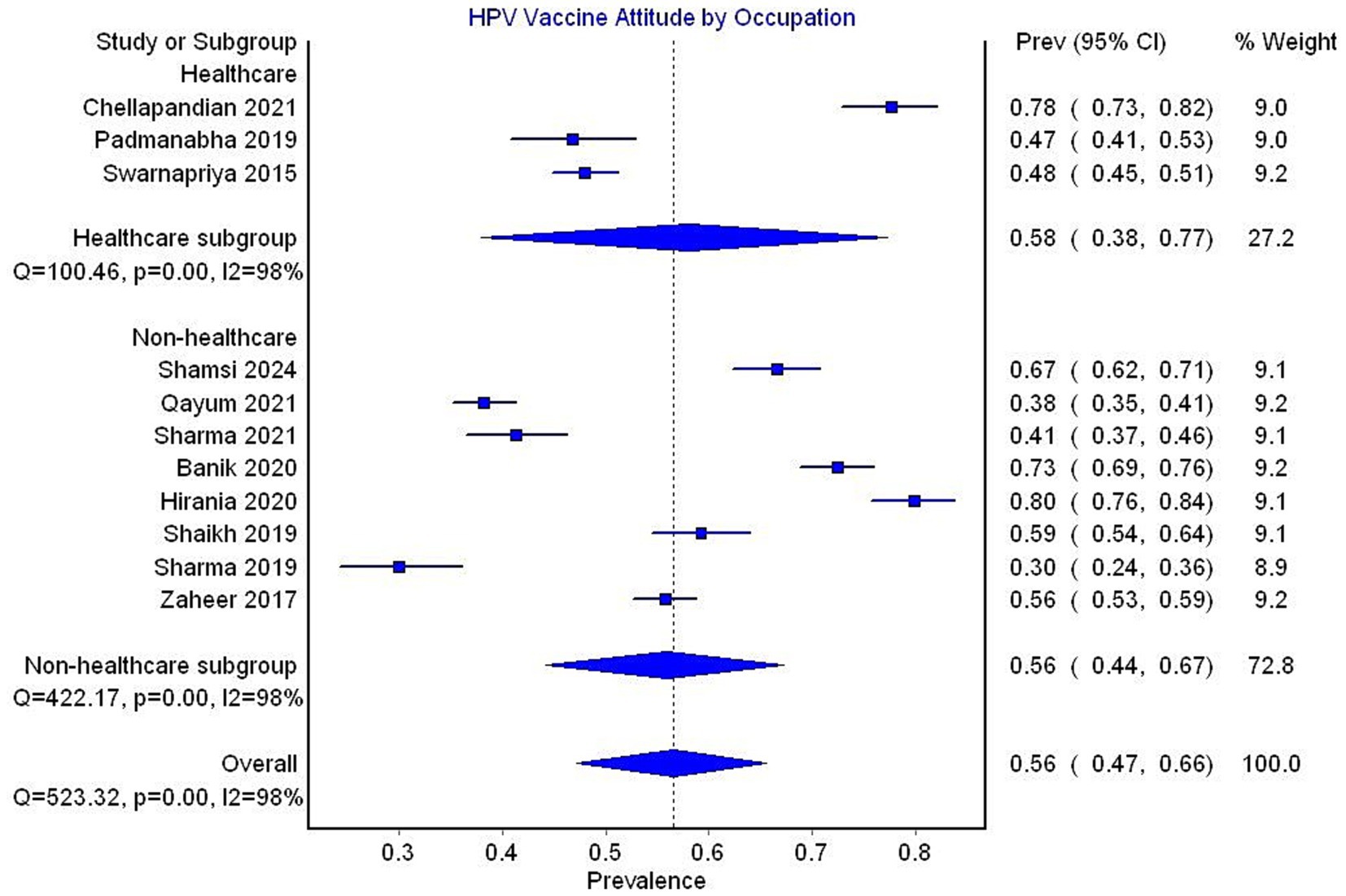
Figure 11. Forest plot depicting subgroup analysis by occupation for prevalence of attitude toward HPV vaccine.
Meta-regression analysis was conducted to assess factors affecting HPV vaccine uptake and attitude toward the vaccine. Covariates considered in the analysis included sample size, mean age, percentage of the sample that was female, employed, literate, knowledge of the HPV vaccine, and attitude toward the HPV vaccine. In the univariate meta-regression model, knowledge of the HPV vaccine uptake was found to be the only significant predictor for vaccine uptake (p = 0.003) (Table 2 and Figure 12).
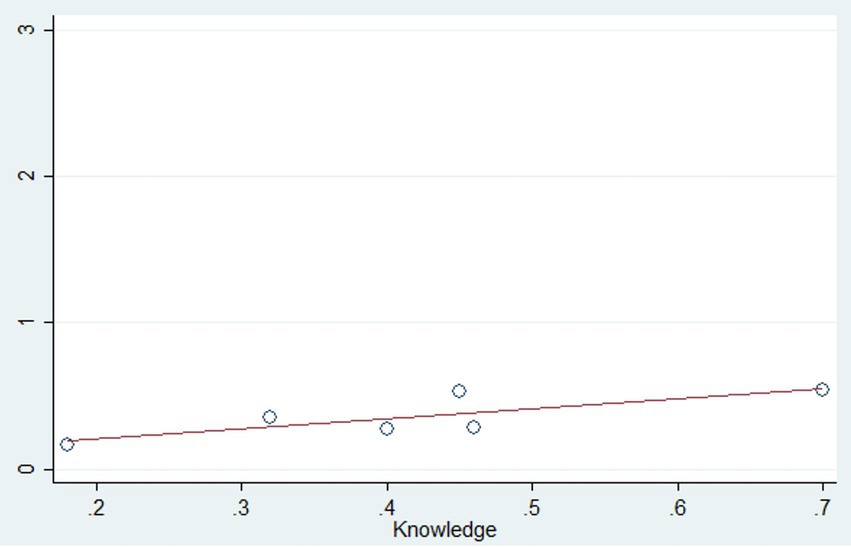
Figure 12. Bubble plot depicting the significant association between knowledge of HPV vaccine and vaccine uptake (p = 0.003).
Similarly, in the univariate meta-regression model for attitude toward the HPV vaccine, covariates such as sample size, mean age, percentage of the sample that was female, employed, literate, and knowledge of the HPV vaccine were considered, but none of these factors were found to be significant predictors (Table 2).
Discussion
This systematic review and meta-analysis aims to determine the estimated prevalence of HPV vaccine uptake in the South Asian region. Additionally, we assessed the proportion of participants who reported good knowledge and a positive attitude toward the vaccine. This meta-analysis is the first to report these metrics from the South Asian region and provides insights into effective strategies to increase HPV vaccine uptake.
Our study reveals a pooled prevalence of 8% (95% CI 1–21) based on data from over ten thousand participants. This estimate is significantly lower than those reported by similar meta-analyses focusing on other regions. Agimas et al. pooled data from 29 articles conducted in East Africa and reported a vaccine uptake of 35% (95% CI 26–45%) (38). Similarly, Addisu et al. pooled data from eight studies conducted in Ethiopia involving 3,936 participants and reported a vaccine uptake of 42.05% (95% CI 26.36–58.95) (39). Meanwhile, Bruni et al. conducted a pooled analysis of data from 64 countries and reported an uptake of 2.7% (95% CI 1.8–3.6), which aligns more closely with our findings (40). It’s worth noting that the global estimate of vaccine coverage is 77%, while a recent study reported a vaccine uptake of 62.8% in a low vaccination region of the United States (41, 42).
These findings underscore the alarming lack of progress in HPV vaccination and cervical cancer prevention in the South Asian region, particularly when compared to global efforts, developed countries, and even certain African regions (43). Sub-Saharan Africa, historically considered the center of HPV infection and cervical cancer, is home to 19 out of the top 20 countries with the greatest burden of cervical cancer (44). However, in recent years, 22 out of the 54 African countries have implemented national immunization programs (45). These efforts have undeniably provided a potential roadmap for South Asian countries to follow (46–48).
We report an estimated pooled prevalence for good knowledge of 41% (95% CI 28–55). This finding was in line with Addisu et al., who reported a prevalence of 55.12% (95% 30.8–79.4) (39). A meta-analysis reporting data from 58 Chinese studies reported lower knowledge (17.55, 95% CI 12.38–24.88) (49). While it is difficult to determine the exact cause for these discrepancies, one potential explanation is the relative recency of the studies included by our meta-analysis as well as by Addisu et al., compared to the Chinese study. Cervical cancer and HPV vaccination have gained increased attention globally in recent years (50–53). Another possible explanation is that several studies in our meta-analysis focused on healthcare professionals, who are generally expected to be more knowledgeable (54). However, only one such study could be included in the knowledge analysis. In the subgroup analysis of non-healthcare studies, 40% of participants still exhibited good knowledge. Despite this relatively high knowledge level, the low uptake of vaccines suggests that vaccine unavailability or high costs may be major factors contributing to the lack of vaccination (55–57).
Our study showed a significant association between the proportion of participants with good knowledge and the prevalence of vaccine uptake. These results are supported by previously published systematic reviews. Agimas et al. found good knowledge to be significantly associated with vaccine uptake (OR 1.6, 95% CI 1.43–1.8) (38). This was further corroborated by Addisu et al., who reported an odds ratio of 6.70 (95% CI 3.43, 13.07) (39). This association was also qualitatively reported by Kessels et al., who reviewed 25 studies, 20 of which were conducted in the United States (58). Greater knowledge of HPV and HPV vaccination likely enables individuals to make evidence-based decisions regarding vaccine uptake, as they become more receptive to national screening and vaccination efforts when aware of the consequences of HPV infection, as well as the relative efficacy, safety, and cost-effectiveness of vaccination (59, 60). Additionally, studies have shown that even just having heard of the HPV vaccine significantly increases vaccine uptake (61). These findings highlight the potential impact of mass awareness campaigns in significantly improving vaccine uptake, particularly in rural and low-literacy communities (62–65).
Our review indicates a positive attitude toward HPV vaccination in 56% of participants (95% CI 47–66). This is comparable to estimates of positive attitudes in Ethiopia (45.34%) and Germany (61.5%) (39, 66). Similar to knowledge, the South Asian region exhibits a comparable positive attitude toward vaccination compared to regions with higher vaccine uptake. This suggests that the limited vaccination is due to inadequate inclusion of HPV vaccination in national immunization programs (67–69). Although our study did not find attitude to be a significant predictor of vaccine uptake, substantial literature highlights a strong association between the two (70–73). In a meta-analysis conducted by Agimas et al., attitude was shown to be a significant predictor of uptake, with a reported OR of 2.54 (95% CI 2.13–3.03) (38). Similarly, Addisu et al. found a significant association with an OR of 2.04 (95% CI 1.51–2.74) (39). A Canadian focus group-based study revealed that poor knowledge and attitude were the most frequently observed barriers to vaccination (74). These results suggest that individuals with positive attitudes toward vaccines are more likely to have greater trust in vaccination programs. Furthermore, a longitudinal study conducted by Hofman et al. in the Netherlands demonstrated that a positive attitude was associated with increased trust in the vaccine and decreased ambivalence over time (75).
When comparing vaccine uptake across different countries, it is evident that Bhutan had a significantly higher uptake rate (99%) compared to India (6%), Pakistan (4%), and Bangladesh (3%). This difference can be attributed to Bhutan’s decision to implement a national HPV vaccination program in 2010, which achieved a coverage rate of 96.1% (76). Furthermore, Bhutan’s switch from health center-based to school-based immunization programs significantly improved coverage from 73 to 90% (76). Interestingly, data from Ethiopia, as reported by Addisu et al., also showed a relatively high uptake rate of 42%, mainly due to the implementation of school-based immunization programs (39). These findings suggest that school-based programs may be more effective in low-middle-income countries than health center programs. Bhutan’s success can also be attributed to various incentives employed, such as involving community leaders, providing token incentives like t-shirts, and offering financial incentives, which proved effective in their conservative and religious population (77). Other countries may achieve similar success by incorporating local cultural and traditional values, although this may pose challenges for culturally diverse countries like India and Pakistan.
It is important to interpret the findings of our systematic review, and meta-analysis needs to be interpreted with caution due to several limitations. Firstly, significant heterogeneity was observed in the pooled analysis. Despite undertaking subgroup and meta-regression analyses, we could not identify the source of heterogeneity. Secondly, despite conducting a thorough search, only 17 studies met the criteria for inclusion in the final analysis. The limited number of studies conducted may not comprehensively represent the wide range of HPV vaccine uptake in all South Asian nations, which could restrict the generalizability of the results. Thirdly, publication bias may exist due to the higher likelihood of studies with significant findings being published. We did a comprehensive search across many databases without any language limitations, it is possible that unpublished research or studies published in less widely available publications were inadvertently overlooked.
In conclusion, our study reveals that the prevalence of HPV vaccine uptake in South Asia is low (8%). The pooled prevalence of adequate knowledge and a favorable attitude toward the vaccine were 41 and 56%, respectively. In the univariate meta-regression model, knowledge of the HPV vaccine uptake was the only significant predictor of vaccine uptake. Based on these findings, we strongly recommend implementing awareness drives and social media campaigns to increase awareness about the HPV vaccine. Additionally, we suggest including the HPV vaccine in national immunization programs to prevent the region from lagging further behind the rest of the world in HPV vaccination rates and, ultimately, eradicate cervical cancer.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
KN: Methodology, Writing – original draft, Writing – review & editing. SN: Supervision, Writing – review & editing. MM: Software, Writing – original draft. MB: Supervision, Writing – original draft. SK: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1453704/full#supplementary-material
References
1. Singh, D, Vignat, J, Lorenzoni, V, Eslahi, M, Ginsburg, O, Lauby-Secretan, B, et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO global cervical Cancer elimination initiative. Lancet Glob Health. (2023) 11:e197–206. doi: 10.1016/S2214-109X(22)00501-0
2. Torre, LA, Bray, F, Siegel, RL, Ferlay, J, Lortet-Tieulent, J, and Jemal, A. Global cancer statistics, 2012. CA Cancer J Clin. (2015) 65:87–108. doi: 10.3322/caac.21262
3. Cohen, PA, Jhingran, A, Oaknin, A, and Denny, L. Cervical cancer. Lancet. (2019) 393:169–82. doi: 10.1016/S0140-6736(18)32470-X
4. Okunade, KS. Human papillomavirus and cervical cancer. J Obstet Gynaecol. (2020) 40:602–8. doi: 10.1080/01443615.2019.1634030
5. Siokos, AG, Siokou-Siova, O, and Tzafetas, I. Correlation between cervical carcinogenesis and tobacco use by sexual partners. Hell J Nucl Med. (2019) 2:184–90.
6. Bruni, L, Albero, G, Rowley, J, Alemany, L, Arbyn, M, Giuliano, AR, et al. Global and regional estimates of genital human papillomavirus prevalence among men: a systematic review and meta-analysis. Lancet Glob Health. (2023) 11:e1345–62. doi: 10.1016/S2214-109X(23)00305-4
7. Forster, AS. The human papillomavirus immunisation programme and sexual behaviour. London: University Coll London (2011).
8. Jørgensen, L, Gøtzsche, PC, and Jefferson, T. Benefits and harms of the human papillomavirus (HPV) vaccines: systematic review with meta-analyses of trial data from clinical study reports. Syst Rev. (2020) 9:1–23. doi: 10.1186/s13643-019-0983-y
9. Arbyn, M, Xu, L, Simoens, C, and Martin-Hirsch, PPL. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst Rev. (2018) 2020:CD009069. doi: 10.1002/14651858.CD009069.pub3
10. World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. Geneva: World Health Organization. (2020)1–56.
11. Schiller, JT, Castellsagué, X, and Garland, SM. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine. (2012) 30:F123–38. doi: 10.1016/j.vaccine.2012.04.108
12. Ebrahimi, N, Yousefi, Z, Khosravi, G, Malayeri, FE, Golabi, M, Askarzadeh, M, et al. Human papillomavirus vaccination in low- and middle-income countries: progression, barriers, and future prospective. Front Immunol. (2023) 14:1150238. doi: 10.3389/fimmu.2023.1150238
13. International Monetory Fund. (2024). World economic outlook databases. Available at: https://www.imf.org/en/Publications/SPROLLS/world-economic-outlook-databases#sort=%40imfdate_descending (Accessed June 26, 2024).
14. World Health Organization. (2022). Global HPV vaccine introduction overview. Available at:. (https://media.path.org)
15. Business Standard. (2022). DCGI approves India’s first qHPV vaccine to treat cervical cancer. Available at:. (https://www.business-standard.com/article/current-affairs/dcgi-approves-india-s-first-qhpv-vaccine-to-treat-cervical-cancer-122071201479_1.html)
16. Dutta, T, Agley, J, Meyerson, BE, Barnes, PA, Sherwood-Laughlin, C, and Nicholson-Crotty, J. Perceived enablers and barriers of community engagement for vaccination in India: using socioecological analysis. PLoS One. (2021) 16:e0253318. doi: 10.1371/journal.pone.0253318
17. Jain, RB, Kumar, A, Sharma, E, and Goel, PK. Barriers to childhood vaccination as perceived by accredited social health activists and multipurpose health workers in Mewat, Haryana India: a qualitative research. J Family Med Prim Care. (2020) 9:4134–8. doi: 10.4103/2249-4863.293044
18. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:372. doi: 10.1136/bmj.n71
19. NHLBI, NIH. (2021). Study quality assessment tools. Available at:. (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools)
20. McGuinness, LA, and Higgins, JPT. Risk-of-bias VISualization (robvis): an R package and shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. (2021) 12:55–61. doi: 10.1002/jrsm.1411
21. Swarnapriya, K, Kavitha, D, and Reddy, GM. Knowledge, attitude and practices regarding HPV vaccination among medical and Para medical in students, India a cross sectional study. Asian Pac J Cancer Prev. (2015) 16:8473–7. doi: 10.7314/APJCP.2015.16.18.8473
22. Rashid, S, Labani, S, and Das, BC. Knowledge, awareness and attitude on HPV, HPV vaccine and cervical Cancer among the college students in India. PLoS One. (2016) 11:e0166713. doi: 10.1371/journal.pone.0166713
23. Sharma, P, Bhilwar, M, Tiwari, P, Parija, PP, Saha, SK, and Mehra, K. Inadequate awareness of cervical cancer and its prevention among young women of Delhi, India: public health policy implications. Int J Adolesc Med Health. (2022) 34:20190108. doi: 10.1515/ijamh-2019-0108
24. Rehman, A, Srivastava, S, Garg, PR, Garg, R, Kurian, K, Shumayla, S, et al. Awareness about human papillomavirus vaccine and its uptake among women from North India: evidence from a cross-sectional study. Asian Pac J Cancer Prev. (2022) 23:4307–13. doi: 10.31557/APJCP.2022.23.12.4307
25. Sharma, A, Biswas, B, and Sati, B. Attributes of screening and vaccination for cervical cancer: insights of an online survey among female school teachers of Kota, Rajasthan, India. Health Promot Perspect. (2021) 11:45–53. doi: 10.34172/hpp.2021.07
26. Jacob, RA, Abraham, PS, Thomas, FR, Navya, V, Sebastian, J, Ravi, MD, et al. Impact of indirect education on knowledge and perception on cervical cancer and its prevention among the parents of adolescent girls: an interventional school-based study. Ther Adv Vaccines Immunother. (2021) 9:9. doi: 10.1177/2515135521990268
27. Chellapandian, P, Myneni, S, Ravikumar, D, Padmanaban, P, James, KM, Kunasekaran, VM, et al. Knowledge on cervical cancer and perceived barriers to the uptake of HPV vaccination among health professionals. BMC Womens Health. (2021) 21:65. doi: 10.1186/s12905-021-01205-8
28. Padmanabha, N, Kini, JR, Alwani, AA, and Sardesai, A. Acceptability of human papillomavirus vaccination among medical students in Mangalore, India. Vaccine. (2019) 37:1174–81. doi: 10.1016/j.vaccine.2019.01.032
29. Khan, M, Zafar, A, Muneer, R, Siddiqui, A, Khan, SA, and Zafar, A. Knowledge, attitude and practices regarding cervical Cancer and human papilloma virus (HPV) vaccination. Pak J Med Dentist. (2021) 10:94–100. doi: 10.36283/PJMD10-2/016
30. Shaikh, MY, Hussaini, MF, Narmeen, M, Effendi, R, Paryani, NS, Ahmed, A, et al. Knowledge, attitude, and barriers towards human papillomavirus (HPV) vaccination among youths of Karachi, Pakistan. Cureus. (2019) 11:e6134. doi: 10.7759/cureus.6134
31. Hirani, S, Khan, S, Akram, S, Virji, SN, Shaikh, PA, Naeem, E, et al. Knowledge, awareness, and practices of cervical cancer, its risk factors, screening, and prevention among women in Karachi, Pakistan. Eur J Cancer Prev. (2021) 30:97–102. doi: 10.1097/CEJ.0000000000000590
32. Shafiq, MH, Mansoor, M, Arshad, A, Mansoor, S, and Iftikhar, S. Frequency of human papilloma virus (HPV) vaccination among female health care providers and reasons for non-immunization at a public sector hospital. J Pak Med Assoc. (2023) 73:1150–63. doi: 10.47391/JPMA.6945
33. Shamsi, U, Zahid, F, Jabbar, ABA, Musharraf, MD, Gauhar, F, Akbar, I, et al. Human papillomavirus vaccine awareness and acceptability for primary prevention of cervical Cancer in Pakistan: a cross-sectional study. Asian Pac J Cancer Prev. (2024) 25:813–20. doi: 10.31557/APJCP.2024.25.3.813
34. Banik, R, Naher, S, Rahman, M, and Gozal, D. Investigating Bangladeshi rural Women’s awareness and knowledge of cervical Cancer and attitude towards HPV vaccination: a community-based cross-sectional analysis. J Cancer Educ. (2022) 37:449–60. doi: 10.1007/s13187-020-01835-w
35. Qayum, O, Billah, MM, Akhter, R, and Flora, MS. Women’s knowledge, attitude and practice on cervical Cancer and its screening in Dhaka, Bangladesh. Asian Pac J Cancer Prev. (2021) 22:3327–35. doi: 10.31557/APJCP.2021.22.10.3327
36. Qayum, MO, Hassan, MR, Henderson, A, Billah, MM, Nurunnahar, M, Afser, S, et al. Knowledge, attitude and practice of commercial sex workers regarding cervical Cancer and its screening, Daulatdia brothel, Rajbari District, Bangladesh, 2020-2021. Asian Pac J Cancer Prev. (2022) 23:4085–92. doi: 10.31557/APJCP.2022.23.12.4085
37. Baussano, I, Sayinzoga, F, Tshomo, U, Tenet, V, Vorsters, A, Heideman, DAM, et al. Impact of human papillomavirus vaccination, Rwanda and Bhutan. Emerg Infect Dis. (2021) 27:1–9. doi: 10.3201/eid2701.191364
38. Agimas, MC, Adugna, DG, Derseh, NM, Kassaw, A, Kassie, YT, Abate, HK, et al. Uptake of human papilloma virus vaccine and its determinants among females in East Africa: a systematic review and meta-analysis. BMC Public Health. (2024) 24:842–13. doi: 10.1186/s12889-024-18141-5
39. Addisu, D, Gebeyehu, NA, and Belachew, YY. Knowledge, attitude, and uptake of human papillomavirus vaccine among adolescent schoolgirls in Ethiopia: a systematic review and meta-analysis. BMC Womens Health. (2023) 23:279. doi: 10.1186/s12905-023-02412-1
40. Bruni, L, Diaz, M, Barrionuevo-Rosas, L, Herrero, R, Bray, F, Bosch, FX, et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. (2016) 4:e453–63. doi: 10.1016/S2214-109X(16)30099-7
41. Bruni, L, Saura-Lázaro, A, Montoliu, A, Brotons, M, Alemany, L, Diallo, MS, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev Med. (2021) 144:106399. doi: 10.1016/j.ypmed.2020.106399
42. Wilson, AR, Hashibe, M, Bodson, J, Gren, LH, Taylor, BA, Greenwood, J, et al. Factors related to HPV vaccine uptake and 3-dose completion among women in a low vaccination region of the USA: an observational study. BMC Womens Health. (2016) 16:1–9. doi: 10.1186/s12905-016-0323-5
43. Kutz, JM, Rausche, P, Gheit, T, Puradiredja, DI, and Fusco, D. Barriers and facilitators of HPV vaccination in sub-saharan Africa: a systematic review. BMC Public Health. (2023) 23:974–13. doi: 10.1186/s12889-023-15842-1
44. Cervical cancer. (2018). WHO Regional Office for Africa. Available at:. (https://www.afro.who.int/health-topics/cervical-cancer)
45. WHO. (2024). Global health observatory. Existence of national HPV vaccination programme in the national immunization schedule 2019. Available at:. (https://www.who.int/data/gho/data/indicators/indicator-details/GHO/existence-of-national-hpv-vaccination-programme)
46. Domgue, JF, Dille, I, Kapambwe, S, et al. HPV vaccination in Africa in the COVID-19 era: a cross-sectional survey of healthcare providers’ knowledge, training, and recommendation practices. Front Public Health. (2024) 12:1343064. doi: 10.3389/fpubh.2024.1343064
47. Senior, K. Africa needs to boost HPV vaccine uptake to stem rise in cervical cancer. Lancet Oncol. (2023) 24:955. doi: 10.1016/S1470-2045(23)00380-7
48. McGuire, JK, Kabagenyi, F, and Peer, S. Human papillomavirus vaccination in Africa: an airway perspective. Int J Pediatr Otorhinolaryngol. (2023) 165:111423. doi: 10.1016/j.ijporl.2022.111423
49. Zhang, Y, Wang, Y, Liu, L, Fan, Y, Liu, Z, Wang, Y, et al. Awareness and knowledge about human papillomavirus vaccination and its acceptance in China: a meta-analysis of 58 observational studies. BMC Public Health. (2016) 16:1–15. doi: 10.1186/s12889-016-2873-8
50. Chidobem, I, Tian, F, Ogbuokiri, E, Mgbodile, F, Mgbodile, C, Jokar, TO, et al. Trends in HPV and HPV vaccine awareness among gay and bisexual males in the U.S. Vaccine. (2022) 10:10040604. doi: 10.3390/vaccines10040604
51. Almehmadi, MM, Salih, MM, and Al-Hazmi, AS. Awareness of human papillomavirus infection complications, cervical cancer, and vaccine among the Saudi population: a cross-sectional survey. Saudi Med J. (2019) 40:555–9. doi: 10.15537/smj.2019.6.24208
52. Eva, FN, Khan, MAS, Islam, T, Monisha, UK, Meem, NES, Hossain, MA, et al. Awareness of HPV vaccine and its socio-demographic determinants among the parents of eligible daughters in Bangladesh: a nationwide study. Heliyon. (2024) 10:e30897. doi: 10.1016/j.heliyon.2024.e30897
53. Wheldon, CW, Krakow, M, Thompson, EL, and Moser, RP. National trends in human papillomavirus awareness and knowledge of human papillomavirus–related cancers. Am J Prev Med. (2019) 56:e117–23. doi: 10.1016/j.amepre.2018.11.005
54. Yam, PWA, Lam, PL, Chan, TK, Chau, KW, Hsu, ML, Lim, YM, et al. A cross sectional study on knowledge, attitude and practice related to human papillomavirus vaccination for cervical Cancer prevention between medical and non-medical students in Hong Kong. Asian Pac J Cancer Prev. (2017) 18:1689–95. doi: 10.22034/APJCP.2017.18.6.1689
55. Mahumud, RA, Gow, J, Alam, K, Keramat, SA, Hossain, MG, Sultana, M, et al. Cost-effectiveness of the introduction of two-dose bi-valent (Cervarix) and quadrivalent (Gardasil) HPV vaccination for adolescent girls in Bangladesh. Vaccine. (2020) 38:165–72. doi: 10.1016/j.vaccine.2019.10.037
56. Jiang, Y, Ni, W, and Wu, J. Cost-effectiveness and value-based prices of the 9-valent human papillomavirus vaccine for the prevention of cervical cancer in China: an economic modelling analysis. BMJ Open. (2019) 9:9. doi: 10.1136/bmjopen-2019-031186
57. Arora, S, and Tuffaha, H. Cost-effectiveness analysis of human papillomavirus vaccines for the prevention of cervical cancer in India. Asia Pac J Clin Oncol. (2024) 20:55–62. doi: 10.1111/ajco.13962
58. Kessels, SJM, Marshall, HS, Watson, M, Braunack-Mayer, AJ, Reuzel, R, and Tooher, RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine. (2012) 30:3546–56. doi: 10.1016/j.vaccine.2012.03.063
59. Holman, DM, Benard, V, Roland, KB, Watson, M, Liddon, N, and Stokley, S. Barriers to human papillomavirus vaccination among us adolescents a systematic review of the literature. JAMA Pediatr. (2014) 168:76–82. doi: 10.1001/jamapediatrics.2013.2752
60. Suk, R, Montealegre, JR, Nemutlu, GS, Nyitray, AG, Schmeler, KM, Sonawane, K, et al. Public knowledge of human papillomavirus and receipt of vaccination recommendations. JAMA Pediatr. (2019) 173:1099–102. doi: 10.1001/jamapediatrics.2019.3105
61. JTC, L, and Law, CK. Revisiting knowledge, attitudes and practice (KAP) on human papillomavirus (HPV) vaccination among female university students in Hong Kong. Hum Vaccin Immunother. (2018) 14:924–30. doi: 10.1080/21645515.2017.1415685
62. Groene, EA, Mohammed, I, Horvath, K, Basta, NE, Yared, N, and Kulasingam, S. Online media scans: applying systematic review techniques to assess statewide human papillomavirus vaccination activities. J Public Health Res. (2019) 8:1623. doi: 10.4081/jphr.2019.1623
63. Cartmell, KB, Mzik, CR, Sundstrom, BL, Luque, JS, White, A, and Young-Pierce, J. HPV vaccination communication messages, messengers, and messaging strategies. J Cancer Educ. (2019) 34:1014–23. doi: 10.1007/s13187-018-1405-x
64. Mohanty, S, Leader, AE, Gibeau, E, and Johnson, C. Using Facebook to reach adolescents for human papillomavirus (HPV) vaccination. Vaccine. (2018) 36:5955–61. doi: 10.1016/j.vaccine.2018.08.060
65. Blasi, PR, King, D, and Henrikson, NB. HPV vaccine public awareness campaigns: an environmental scan. Health Promot Pract. (2015) 16:897–905. doi: 10.1177/1524839915596133
66. Schülein, S, Taylor, KJ, König, J, Claus, M, Blettner, M, and Klug, SJ. Factors influencing uptake of HPV vaccination among girls in Germany. BMC Public Health. (2016) 16:995–8. doi: 10.1186/s12889-016-3663-z
67. Toor, J, Echeverria-Londono, S, Li, X, Abbas, K, Carter, ED, Clapham, HE, et al. Lives saved with vaccination for 10 pathogens across 112 countries in a pre-COVID-19 world. eLife. (2021) 10:10. doi: 10.7554/eLife.67635
68. Ochalek, J, Abbas, K, Claxton, K, Jit, M, and Lomas, J. Assessing the value of human papillomavirus vaccination in Gavi-eligible low-income and middle-income countries. BMJ Glob Health. (2020) 5:e003006. doi: 10.1136/bmjgh-2020-003006
69. Abbas, K, Yoo, KJ, Prem, K, and Jit, M. Equity impact of HPV vaccination on lifetime projections of cervical cancer burden among cohorts in 84 countries by global, regional, and income levels, 2010–22: a modelling study. EClinicalMedicine. (2024) 70:102524. doi: 10.1016/j.eclinm.2024.102524
70. Thanasa, E, Thanasa, A, Kamaretsos, E, Paraoulakis, I, Balafa, K, Gerokostas, EE, et al. Awareness regarding human papilloma virus among health professionals and will to accept vaccination: a systematic review. Cureus. (2022) 14:e30855. doi: 10.7759/cureus.30855
71. Coles, VAH, Patel, AS, Allen, FL, Keeping, ST, and Carroll, SM. The association of human papillomavirus vaccination with sexual behaviours and human papillomavirus knowledge: a systematic review. Int J STD AIDS. (2015) 26:777–88. doi: 10.1177/0956462414554629
72. Tusimin, M, Lo, YC, Razak, NZSA, Zainol, MI, Minhat, HS, and Rejali, Z. Sociodemographic determinants of knowledge and attitude in the primary prevention of cervical cancer among university Tunku Abdul Rahman (UTAR) students in Malaysia: preliminary study of HPV vaccination. BMC Public Health. (2019) 19:19. doi: 10.1186/s12889-019-7764-3
73. Badgujar, VB, Ahmad Fadzil, FS, Balbir Singh, HK, Sami, F, Badgujar, S, and Ansari, MT. Knowledge, understanding, attitude, perception and views on HPV infection and vaccination among health care students and professionals in Malaysia. Hum Vaccin Immunother. (2019) 15:156–62. doi: 10.1080/21645515.2018.1518843
74. Dubé, E, Gagnon, D, Clément, P, Bettinger, JA, Comeau, JL, Deeks, S, et al. Challenges and opportunities of school-based HPV vaccination in Canada. Hum Vaccin Immunother. (2019) 15:1650–5. doi: 10.1080/21645515.2018.1564440
75. Hofman, R, Van Empelen, P, Richardus, JH, De Kok, IMCM, De Koning, HJ, Van Ballegooijen, M, et al. Predictors of HPV vaccination uptake: a longitudinal study among parents. Health Educ Res. (2014) 29:83–96. doi: 10.1093/her/cyt092
76. Dorji, T, Tshomo, U, Gyamtsho, S, Tamang, ST, Wangmo, S, and Pongpirul, K. Gender-neutral HPV elimination, cervical cancer screening, and treatment: experience from Bhutan. Int J Gynaecol Obstet. (2022) 156:425–9. doi: 10.1002/ijgo.13728
Keywords: HPV vaccination, vaccination determinants, cervical cancer, South Asia, meta-analysis
Citation: Noreen K, Naeem Khalid S, Murad MA, Baig M and Khan SA (2024) Uptake and determinants of HPV vaccination in South Asia: a systematic review and meta-analysis. Front. Public Health. 12:1453704. doi: 10.3389/fpubh.2024.1453704
Edited by:
Ana Afonso, NOVA University of Lisbon, PortugalReviewed by:
Andrew Pavelyev, Merck, United StatesKarim A. Mohamed Al-Jashamy, SEGi University, Malaysia
Copyright © 2024 Noreen, Naeem Khalid, Murad, Baig and Khan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Khola Noreen, a2hhdWxhZHI2NkBnbWFpbC5jb20=
 Khola Noreen
Khola Noreen Samina Naeem Khalid2
Samina Naeem Khalid2 Mukhtiar Baig
Mukhtiar Baig Shahzad Ali Khan
Shahzad Ali Khan