- 1Department of Psychiatry, Faculty of Medicine, Dalhousie University, Halifax, NS, Canada
- 2Department of Psychiatry, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, AB, Canada
- 3Mental Health and Addictions Program, IWK Health, Halifax, NS, Canada
Background: Individuals exposed to wildfires are at risk of developing adverse mental health conditions in the months following the event. Receiving supportive text interventions during and after a wildfire event can have a significant impact on reducing mental health conditions over time.
Objectives: The study aimed to assess the effectiveness of a supportive text message intervention service in reducing the severity and prevalence of psychological conditions 3 months following the 2023 wildfires in Alberta and Nova Scotia, two regions heavily affected by these natural disasters.
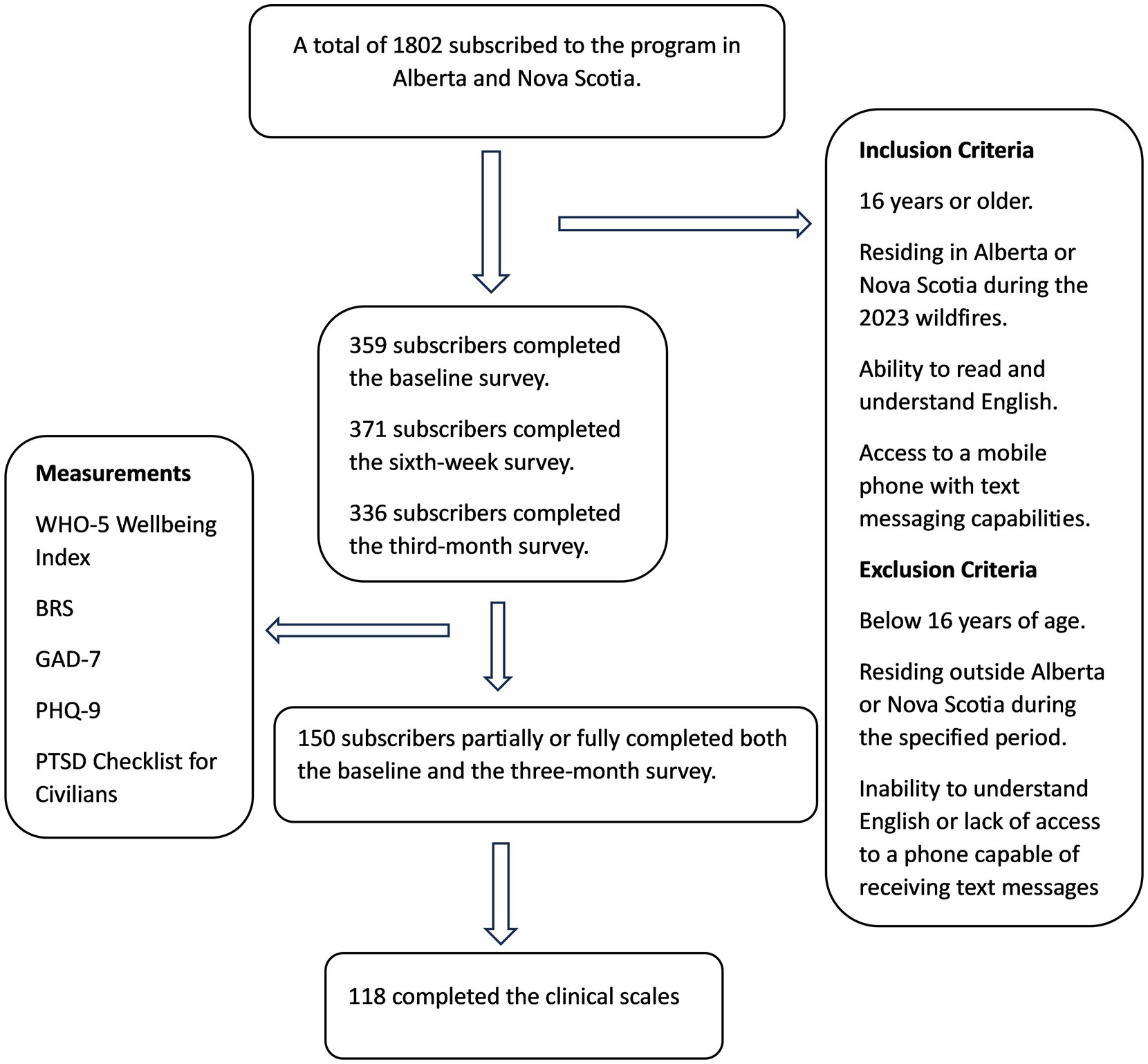
Methods: In this longitudinal study, participants voluntarily subscribed to the Text4Hope-AB and Text4Hope-NS services, receiving supportive text interventions for 3 months. On enrolment and at 3 months post-enrolment, participants completed online surveys. The severity and prevalence of mental wellbeing, resilience, depression, anxiety, and post-traumatic stress were measured using the World Health Organization- Five Well-Being Index (WHO-5), Brief Resilience Scale (BRS), Patient Health Questionnaire 9 (PHQ-9), Generalized Anxiety Disorder - 7 scale (GAD-7), and Post-Traumatic Stress Disorder Checklist for Civilians (PCL-C) respectively. Data analysis involved using McNemar’s chi-square test and paired sample t-tests.
Results: A total of 150 subscribers partially or fully completed both the baseline and 3-month assessments. The results show a statistically significant change in the mean scores on the WHO-5 Wellbeing Index (+ 24.6%), PHQ-9 (−17.0%), GAD-7 scale (−17.6%), PCL-C (−6.0%), and BRS (+3.2%) from baseline to 3 months. Similarly, there was a reduction, although not statistically significant, in the prevalence of low resilience (55.1 vs. 53.4%), poor mental well-being (71.6 vs. 48.3%), likely MDD (71.4 vs. 40.7%), likely GAD (42.1 vs. 33.3%), and likely PTSD (42.0 vs. 38.4%).
Conclusion: The study’s findings underscore the potential of the supportive text intervention program in effectively aiding individuals who have endured natural disasters such as wildfires. Providing supportive text messages during wildfire events is a promising strategy for mitigating mental health conditions over time.
Introduction
In recent years, mental health challenges arising from natural disasters, such as wildfires, have garnered increased attention due to their profound and enduring impacts on affected individuals and communities (1, 2). Wildfires happening naturally, especially in determined seasons, exacerbated by climate change and human activities, not only pose immediate threats to physical safety and property but also inflict significant psychological distress on those exposed to them (3, 4). The 2023 wildfire season in Canada was not exceptional; millions of hectares of vegetation were burnt (5–7), and residents had to evacuate their homes (8). The severity of the wildfire necessitated Alberta province to declare a state of emergency (8), and Nova Scotia experienced the most devastating wildfire on record (6). The combined severity of the wildfires in 2023 led to it being declared the worst in Canada’s history, surpassing all fire seasons since 2014 (9). Understanding the intricate relationship between wildfire exposure and its impact on mental well-being is crucial for efficiently devising and delivering robust interventions and support systems. This understanding is pivotal in crafting effective strategies to alleviate the enduring effects of these occurrences.
One-third of individuals exposed to wildfires experience a myriad of mental health challenges, including heightened measures of low resilience, anxiety, depression, and post-traumatic stress disorder (PTSD) (10–12). Literature has recorded a high prevalence of psychological conditions following natural disasters, with 5.8 to 54% of adult victims reporting depressive symptoms, which may last for 10 years following wildfires (9, 13, 14). Similarly, a one-month prevalence recorded in a study conducted in Fort McMurray shows 24.8, 18.0, and 13.6% in depression, anxiety, and PTSD, respectively (14). Survivors of the wildfire in Victoria exhibited increased rates of psychological incidents 3 to 4 years later (15). Psychological symptoms remained consistent throughout follow-up periods among the high-impact group (12, 15).
Regarding the escalating mental health crisis following wildfires, studies have increasingly focused on evaluating the efficacy of interventions and examining the longitudinal trajectories of mental health outcomes in affected populations (16). Given the intricate nature of mental health, understanding the evolution of mental health status over time is key for tailoring interventions to the particular needs of wildfire-affected individuals (1).
Supportive interventions, such as text message-based interventions, have shown promise in mitigating mental health symptoms and promoting resilience among disaster-affected populations (1, 4). Text-based interventions provide convenient and accessible support, allowing individuals to seek help at their own pace and convenience while reaching a more significant number of individuals simultaneously, making them particularly effective for supporting communities affected by natural disasters. The effectiveness of text-based interventions in post-disaster contexts has been demonstrated in several studies (17, 18). For example, Ruzek et al. (17) found that text-based interventions reduced symptoms of post-traumatic stress disorder (PTSD) and related issues after war and disasters (17). By providing timely and accessible support, these interventions can help people cope with the psychological challenges associated with wildfire exposure, reduce hospitalization, and facilitate recovery (19, 20).
Supportive text message intervention improves one’s resilience during a disaster (21). Resilience, a key outcome measure in this study, is conceptualized as the ability to adapt and bounce back in the face of adversity (22, 23). This involves the ability to maintain mental and emotional well-being amidst significant stress and trauma (21, 24). The study examines changes in resilience over time as a measure of the effectiveness of the Text4Hope intervention in promoting psychological well-being and coping strategies among wildfire-affected populations.
The findings will contribute to developing evidence-based strategies focusing on psychological conditions. The objective of this study is to assess the longitudinal changes in mental health status among individuals affected by wildfires over 3 months and to examine the impacts of a texting mental health service (Text4Hope-AB and Text4Hope-NS) on the severity and prevalence of psychological conditions 3 months following the wildfires.
Methods
Study design and setting
The study employed a longitudinal study design centered on subscribers of the Text4Hope service. It was conducted across two Canadian provinces, Alberta and Nova Scotia, which encountered wildfire. Alberta is Canada’s fourth largest province, occupying 661,848 square kilometers, while Nova Scotia covers 55,284 square kilometers. The wildfire in Alberta started late April 2023 to early November 2023, with Alberta recording approximately 2.2 million hectares burned between March 1 and October 31, 2023 (7). On May 27, 2023, Nova Scotia experienced its largest recorded wildfire in history (6). Alberta and Nova Scotia were selected as research locations because of collaboration with the regional health authorities to implement the Text4Hope program as an emergency psychological response during the wildfire season.
Institutional review board approval
The study adhered to the guidelines in the Declaration of Helsinki and obtained approval from the Alberta Health Research Ethics Committee (Pro00086163) and the Research Ethics Board at Nova Scotia Health (REB file #1028254). Participants’ consent was obtained upon completing the online survey and submitting responses.
Program intervention
The supportive text messages were crafted by Cognitive behavioral therapists, psychiatrists, and psychologists in collaboration with a diverse group of end users. These messages were uploaded onto a web-based platform, which automatically sent the messages daily at 9 am Mountain Time. Participants self-subscribed to the service by texting the word “HopeNS” (Nova Scotia) or HopeAB” (Alberta) to a short code and received unidirectional supportive SMS text messages for 3 months. Participants could also opt out by texting ‘STOP’ to the same shortcode. These daily supportive messages are based on cognitive behavioral therapy principles and are delivered to subscribers’ mobile phones. The messages focus on promoting resilience, coping strategies, and overall well-being. The initial message welcomed subscribers to the service. It encouraged them to voluntarily fill out a web-based baseline survey aimed at gathering demographic and clinical information primarily related to resilience, well-being, anxiety, depression, and PTSD. Participants received another text message link 6 weeks and 3 months later, inviting them to complete a follow-up web-based survey. The survey required a maximum of 10 min to complete, and participants were not incentivized to complete the surveys. Text4Hope was implemented in previous disaster contexts, including the COVID-19 pandemic (25). It is a scalable and cost-effective intervention that can reach many individuals simultaneously, making it well-suited for supporting communities affected by natural disasters. An example of the message is:
“No matter what setbacks you have faced or challenges that lie ahead, you can succeed if you have inner strength and stay focused. Have faith in yourself, and success will be yours no matter what problems the wildfire throws at you.” (1).
Enrollment, inclusion/exclusion criteria
Participants self-subscribed to the program through various channels, including social media, community outreach, and referrals from mental health service providers. Eligibility criteria for participation included:
1. Age 16 years or older.
2. Residing in Alberta or Nova Scotia during the 2023 wildfires.
3. Ability to read and understand English.
4. Access to a mobile phone with text messaging capabilities.
Participant will be ineligible if they do not meet the inclusion criteria.
Data collection
An internet-based questionnaire was utilized in data collection and powered by Research Electronic Data Capture (REDCap 13.7.1) software (26). The study commenced in May 2023. Longitudinal data collection occurred between August 2023 and December 2023, representing 3 months post-enrollment into the program and receipt of supportive text message intervention. The survey questionnaire encompassed a range of sociodemographic factors, including gender, age, ethnicity, marital status, employment status, educational attainment, and housing situation. Additionally, self-reported clinical information on mental health symptoms was collected at baseline and 3 follow-ups.
Outcome measure
The study’s primary outcome measures were the change in mean scores of the clinical scales from baseline to 3 months. The change in mean scores of well-being, resilience, anxiety, depression, and PTSD symptoms measured on the World Health Organization- 5 Wellbeing Index (WHO-5) (27), the Brief Resilience Scale (BRS) (28), Generalized Anxiety Disorder 7-item (GAD-7) (29), Patient Health Questionnaire-9 (PHQ-9) (30) and the PTSD Checklist – Civilian Version (PCL-C) (31) respectively. Secondary outcomes were the differences in prevalence between baseline and 3 months of mental well-being, resilience, likely MDD, GAD, and PTSD.
The criteria for low resilience were an average BRS score of less than three (28) and a cut-off WHO-5 score below 13 as a criterion for poor mental well-being (27, 32). The presence of a score of 10 or higher on the GAD-7 and PHQ-9 indicated likely GAD (29) or MDD (30), while a PCL-C score of 44 or higher indicates likely PTSD (31). These measures have been shown to have strong reliability and validity (33).
Hypothesis
Participants who subscribe to the program will have at least 20% reduced mean scores on PHQ-9, GAD-7, and PCL-C and a 20% increase in the mean scores on the BRS and WHO-5 at 3 months compared with their enrolment scores. We also hypothesized that the prevalence of poor mental well-being, low resilience, likely GAD, MDD, and PTSD will achieve a 20% lower rate at 3 months than their baseline score. The stated hypothesis is based on the findings of the literature, which recorded those participants who received supportive text intervention reduced their psychological symptoms by 20 to 50% (20, 33–38).
Sample size considerations
To achieve a power of 80% (β = 0.2), a two-sided significance level of 5% (α < 0.05), and detecting an effect size of 0.3 between pairs, a sample size of 90 would be needed (39).
Statistical analysis
Data from the study were analyzed using SPSS for Windows, version 28 (IBM Corporation, Armonk, NY, USA) (40). Demographic and clinical variables were examined against participants who completed the baseline and those who completed both the baseline and follow-up survey employing the chi-square or Fisher exact test. Chi-square analysis adopted a two-tailed criterion with a significance level of less than 0.05 (α < 0.05). The Chi-square test was adopted to assess generalizability and determine whether there are differences in the clinical and demographic characteristics between participants who completed both the baseline and follow-up surveys and participants who completed the baseline survey. Similarly, to examine the differences in the mean scores of the clinical scales at baseline and 3 months, McNemar’s chi-square test and a paired sample 2-tailed t-test were performed. Paired sample t-tests were used to assess changes in continuous variables between baseline and follow-up, while McNemar’s chi-square test was employed for categorical data. Before applying the paired sample t-tests, the normality assumption was assessed using the Shapiro–Wilk test, suitable for smaller sample sizes. We also conducted Levene’s test to check for homogeneity of variances. In addition, we examined the prevalence of poor mental health, low resilience, likely GAD, MDD, and PTSD at each time point, and the results were summarized as numbers and percentages. Participants with missing responses at a 3-month had their missing data imputed, employing the last observations carried forward, precisely their responses at the 6-week responses (41).
Results
Figure 1 illustrates the flow chart of study participants in Alberta and Nova Scotia. Three hundred fifty-nine (359) participants completed the baseline survey, 371 completed the 6-week survey, and 336 completed the 3-month survey. One hundred fifty (150) participants partially or fully completed both the baseline and 3-month surveys, yielding a 41.7% response rate of participants who completed the baseline assessment, and 118 participants completed the clinical scales.
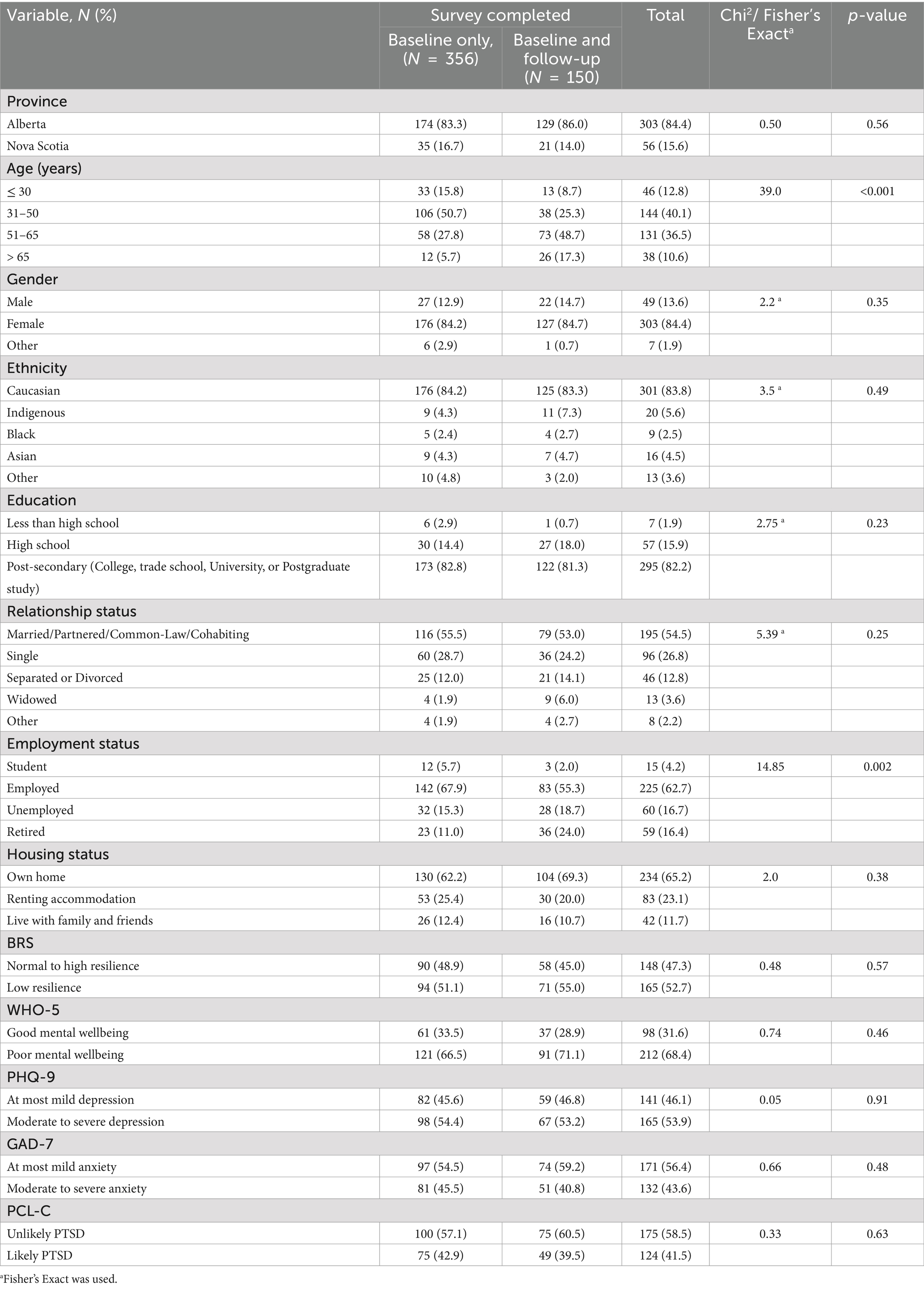
Table 1 demonstrates the distribution of the baseline demographic characteristics of study participants across the survey completion status. Out of the participants who completed their demographic information, three hundred and three were from Alberta, and fifty-six were from Nova Scotia. The result shows that the majority of the participants, 144 (40.1%), were between the ages of 31 and 50 years, 303 (84.4%) were females, 301 (83.8%) were Caucasian, and 295 (82.2%) completed postsecondary education, while 195 (54.5%) were either married, partnered, cohabiting or in a common-law. In addition, 225 (62.7%) were employed, and 234 (65.2%) owned their home. The chi-square analysis shown in Table 1 reported no significant differences in the participants’ demographic characteristics and clinical characteristics between those who completed their demographic information at baseline and those who completed follow-up surveys except for their age and employment status. Employed participants may have varying levels of availability or motivation to complete surveys. Older participants, particularly those aged 31–50, reported higher rates of completing baseline and follow-up surveys.
Among the study participants, more than half experienced low resilience (165, 52.7%), poor mental wellbeing (212, 68.4%), moderate to severe depression (165, 53.9%), and moderate to severe anxiety (132, 43.6%). Fewer reported likely PTSD symptoms (124, 41.5%).
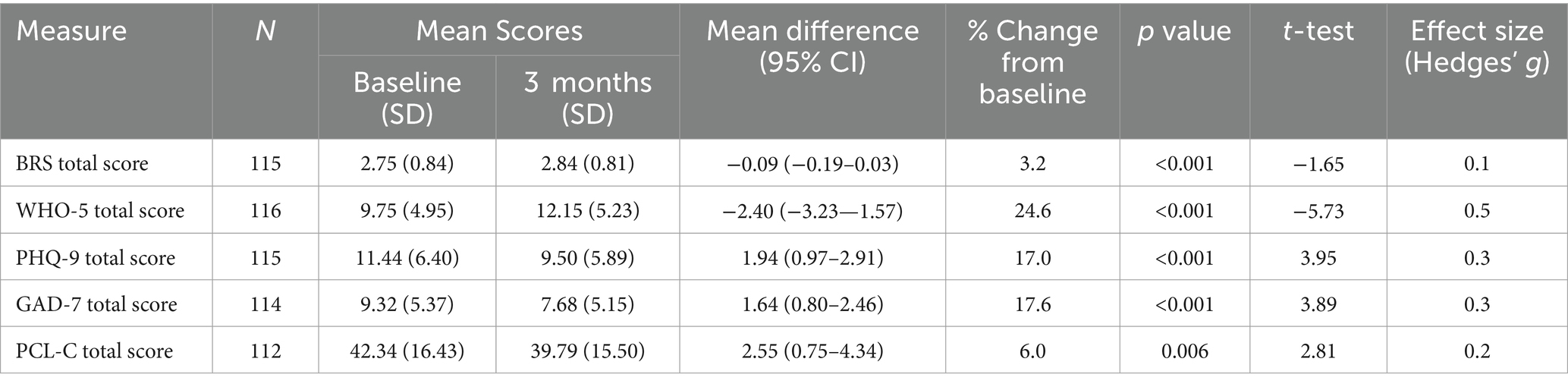
Table 2 shows the mean scores for the BRS, WHO-5, PHQ-9, GAD-7, and PCL-C scores between participants’ baseline and 3-month time points. McNemar’s chi-square test and a paired sample 2-tailed t-test were employed to achieve these results. Significant improvements were found for all measures (p < 0.001), indicating changes in mental health status over the 3 months, with percentage changes ranging from 3.2 to 24.6%. Table 3 showed that scores on the WHO recorded the highest change from baseline with a medium effect size (Hedges’ g = 0.5).
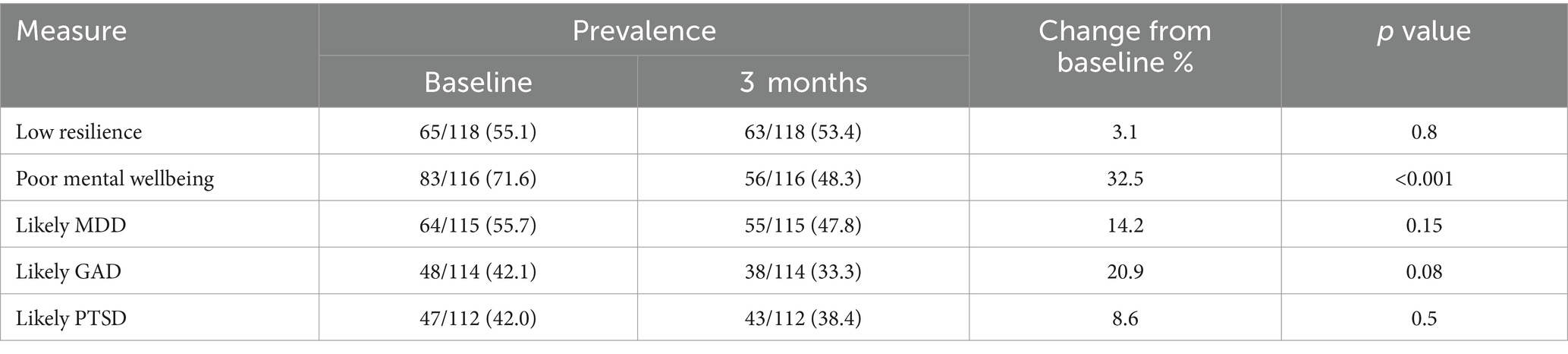
Table 3. Changes in the prevalence of clinical parameters from baseline to 3 months (McNemar’s chi-square test).
Table 3 displays the prevalence of low resilience, poor mental well-being, likely MDD, GAD, and PTSD at baseline and 3-month follow-up time points. Overall, there was an apparent reduction in the prevalence of all the measures. However, the prevalence of poor mental well-being was the only condition that significantly decreased from baseline to the 3-month follow-up (χ2 = 24.1, p < 0.001). Conversely, the prevalence of low resilience, likely MDD, likely GAD, and likely PTSD did not exhibit statistically significant changes over the same period (p > 0.05).
Discussion
This longitudinal study examined the effectiveness of Text4Hope among subscribers 3 months after the wildfire in Alberta and Nova Scotia. Our findings revealed that the mean scores on the PHQ-9, GAD-7, and PCL-C were reduced from baseline compared to the 3-month follow-up by 17.0, 17.6, and 6.0%, respectively, while mean scores on the WHO-5 and BRS increased by 24.6 and 3.2%, respectively. Our study findings partially met our hypothesis of at least a 20% reduction in prevalence and mean scores of the psychological symptoms. Notwithstanding, poor mental well-being recorded a statistically significant decrease in the prevalence (32.5%) from baseline to 3 months and an improvement in the mean scores by 24.6%, which exceeded our hypothesis of attaining at least a 20% reduction in psychological symptoms. Although the prevalence of low resilience, likely MDD, GAD, and PTSD, recorded a reduction, they were not statistically significant.
Although changes in the prevalence of depression, anxiety, PTSD, and low resilience were not statistically significant in our study, their mean scores were statistically significant. The reduction in the prevalence of psychological symptoms among wildfire victims aligns with findings from previous research (42–44). A study conducted in the aftermath of disasters recorded a similar decrease in the prevalence of mental health symptoms among affected individuals after receiving an intervention (42, 43, 45). This consistency across studies underscores the potential effectiveness of interventions in mitigating the psychological impact of wildfires on affected communities. The prevalence of psychological symptoms was higher at baseline compared to participants’ 3-month scores. The high prevalence of mental health conditions at baseline in this study also aligns with other studies that reported a high prevalence of PTSD, depression, and anxiety among affected individuals following wildfires (45–47). Individuals exposed to disasters may be at risk of developing adverse mental health conditions that worsen when intervention is not provided (48). However, participants were in significant distress at baseline, and a randomized control trial that evaluated the long-term impacts of those who did/did not receive an intervention would be beneficial. Various research has assessed the effects of a psychological intervention on mental health outcomes among disaster survivors (36, 37). These studies highlight the potential of targeted interventions to alleviate psychological distress and promote resilience in the aftermath of natural disasters.
Our study examined the demographic characteristics of study participants, mental health outcomes, and interventions during wildfires. Literature has identified significant differences in mental health status and the quest for treatment across different age groups and employment statuses among wildfire survivors (49). Wildfires can have profound and lasting impacts on the mental health of individuals, including those aged 31 to 50, females of Caucasian ethnicity with post-secondary education, married or in a committed relationship, employed, and homeowners. Research has shown that individuals in these demographics may encounter distinct challenges in coping with the aftermath of such disasters (14). Similar programs, such as Text4PTSI and Text4Wellbeing, have effectively improved mental well-being during traumatic conditions, as shown in this current study (38). Our study results showed that most of the participants own their homes; this may provide comfort and their willingness for participants to subscribe and receive supportive text messages (50). Moreover, the adaptability of text message interventions to individuals’ schedules and preferences is a key factor in their effectiveness. Subscribers can engage with the intervention at their own pace and in the privacy of their own homes, reducing potential barriers to participation (50).
Scalable and effective interventions to reduce psychological symptoms among wildfire survivors are crucial in emergency preparedness (51, 52) and appealing to health policymakers (37). The text intervention approach helps reach individuals who may otherwise face barriers to accessing traditional mental health services during disasters like wildfires (53). This implies that supportive text messages provided during wildfires could reduce the mean scores of psychological symptoms and the prevalence of poor mental well-being of wildfire victims. The results of our study provide valuable insights into the trajectories of mental health outcomes over 3 months, particularly with interventions targeting various facets of mental well-being. This finding agrees with the literature highlighting the efficacy of interventions to enhance mental wellness during crises (54–56). Such interventions have been shown to contribute positively to individuals’ overall mental health and quality of life, underscoring their importance in promoting psychological resilience and well-being.
In addition, a study conducted during the pandemic concluded that the text message intervention reduced the psychological burden of victims by approximately 25% during a 3-month follow-up (25). A focus group conducted 3 months after an intensive intervention showed positive experiences with text messaging to support behavior change maintenance (57). This suggests that the continued support provided through text messages can have lasting effects on individuals’ well-being. The baseline prevalence of mental health conditions in our study was higher than the 3-month prevalence, which may be due to the intervention received at baseline to reduce further psychological symptoms among participants. This consistency across studies underscores the potential effectiveness of interventions in mitigating the psychological impact of wildfires on affected communities. Furthermore, the importance of early detection and treatment of mental health conditions has been highlighted in various studies (58). Detecting and addressing mental health issues promptly can not only improve individual outcomes but also reduce the overall burden on healthcare services. Furthermore, the integration of physical and mental health care has been advocated to address the pervasive nature of mental health conditions globally (59).
However, while our study demonstrates positive changes in mental health outcomes, like mental well-being, resilience, depression, anxiety, and PTSD symptoms, other studies have reported contrasting findings. For instance, a longitudinal study found that mental health symptoms persisted or worsened over time among wildfire survivors (46), highlighting the variability in mental health trajectories following such disasters. These discrepancies may stem from differences in sample characteristics, intervention strategies, or follow-up periods across studies (60).
Limitation
Considering the limitations of our study and the broader literature, these findings need to be interpreted cautiously. Firstly, the relatively limited number of participants who completed the baseline and 3-month follow-up surveys (150) suggests that this study may have been underpowered in detecting significant differences from baseline to 3 months post-intervention, further compounded by the low response rate, possibly influenced by the surveys’ online format, which could affect the generalizability of our study. Moreover, research indicates that surveys delivered via text messages have approximately 15% lower retention rates for follow-up assessments than paper-based surveys (61, 62). Secondly, all the validated scales were self-rated instead of formal diagnosis, which may cause response bias and inaccuracies due to the subjective nature of self-reporting. Again, the study was conducted in a non-randomized manner and did not include a control group. The absence of a control group restricts the ability to attribute observed changes directly to the intervention. Lastly, missing survey responses for outcome measures at the 3-month time point were imputed from the 6-week survey responses. Consequently, it is likely that the 6-week outcome data, particularly for those with imputed data, may not precisely reflect their clinical outcomes at the 3-month assessment, and much about the specific impacts of the wildfires on these participants are unknown Despite the study’s limitations, it adds to the growing body of research examining mental health outcomes and the experience of being impacted by wildfires, shedding light on the efficacy of interventions targeted at alleviating the psychological distress associated with wildfires.
Conclusion
Results from the study show an improvement in the psychological symptoms of the study participants 3 months after the wildfires. This highlighted the importance of ongoing research to understand better the nuances of changes in mental health outcomes over time after wildfires and to develop tailored interventions that effectively address the various needs of individuals experiencing mental health challenges. Addressing the needs and challenges encountered by this population, text messaging interventions have the potential to offer valuable support and resources to promote mental well-being in the aftermath of wildfires. The Text4Hope-AB and Text4Hope-NS programs have the prospect of reducing individuals’ mental health burden 3 months after experiencing wildfires. Moreover, ongoing interventions play essential roles in promoting mental well-being and reducing the prevalence of adverse mental health conditions in the aftermath of wildfires. Continued research efforts are needed to refine intervention strategies, address disparities in mental health outcomes, and ultimately support the psychological well-being of individuals and communities affected by wildfires and other disasters.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Alberta Health Research Ethics Committee (Pro00086163) and the Research Ethics Board at Nova Scotia Health (REB file #1028254). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GO-D: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. RS: Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. BA: Writing – original draft, Writing – review & editing. RD: Writing – original draft, Writing – review & editing. EE: Writing – original draft, Writing – review & editing. LW: Writing – review & editing. VA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study received funding from the Queen Elizabeth II Foundation, the Mental Health Foundation, the Royal Alexandra Hospital Foundation, the Calgary Health Trust, the Alberta Children’s Hospital Foundation, the Alberta Cancer Foundation, the University Hospital Foundation, and the Canadian Red Cross with support from the Global Psychological eHealth Foundation, the Department of Psychiatry at Dalhousie University, and the University of Alberta. The funders were not involved in any aspect of the study, including its design, execution, data collection, management, analysis, interpretation, manuscript preparation, review, approval, or the decision to submit the findings for publication.
Acknowledgments
Marianne Hrabok assisted in the drafting of the program messages.
Conflict of interest
VA is the founder and Principal Investigator of the ResilienceNHope messaging programs and volunteers as the Board Chair of the Global Psychological eHealth Foundation, a not-for-profit organization. BA volunteers as the President and Chief Executive Officer of the Global Psychological eHealth Foundation. RS volunteers as the Program Director of the Global Psychological eHealth Foundation. RD volunteers as the Director of Communications of the Global Psychological eHealth Foundation. VA, BA, RS, and RD receive no financial or other compensation from the Global Psychological eHealth Foundation and have no financial conflicts of interest about this article. GO-D has no commercial or financial conflict of interest.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Obuobi-Donkor, G, Shalaby, R, Agyapong, B, Dias, RL, and Agyapong, VIO. Mitigating psychological problems associated with the 2023 wildfires in Alberta and Nova Scotia: six-week outcomes from the Text4Hope program. J Clin Med. (2024) 13:865. doi: 10.3390/jcm13030865
2. To, P, Eboreime, E, and Agyapong, VIO. The impact of wildfires on mental health: a scoping review. Behav Sci. (2021) 11:126. doi: 10.3390/bs11090126
3. Eriksson, CB, Kemp, HV, Gorsuch, R, Hoke, S, and Foy, DW. Trauma exposure and PTSD symptoms in international relief and development personnel. J Trauma Stress. (2001) 14:205–12. doi: 10.1023/A:1007804119319
4. McFarlane, AC, Williamson, P, and Barton, CA. The impact of traumatic stressors in civilian occupational settings. J Public Health Policy. (2009) 30:311–27. doi: 10.1057/jphp.2009.21
5. Parisien, MA, Barber, QE, Flannigan, MD, and Jain, P. Broadleaf tree phenology and springtime wildfire occurrence in boreal Canada. Glob Chang Biol. (2023) 29:6106–19. doi: 10.1111/gcb.16820
6. Press, A. (2023). Nova Scotia wildfires grow, prompt air quality warnings as far south as Virginia. Available at: (https://apnews.com/article/canada-wildfires-halifax-firefighters-us-south-africa-20f340036282d892aaa5528f1e48e618).
7. Tran, C. (2024). 'Learning to live with fire': New study details impact of 2023 wildfire season. Available at: (https://edmontonjournal.com/news/local-news/learning-to-live-with-fire-wildfire-alberta-canada-report).
8. Meilleur, D. (2023). Alberta declares state of emergency as wildfires rage. Available at: (https://globalnews.ca/news/9679627/alberta-premier-adresses-wildfire-state-of-emergency/).
9. Mao, W, Shalaby, R, Agyapong, B, Obuobi-Donkor, G, da Luz Dias, R, and Agyapong, VIO. Devastating wildfires and mental health: major depressive disorder prevalence and associated factors among residents in Alberta and Nova Scotia, Canada. Behav Sci. (2024) 14:209. doi: 10.3390/bs14030209
10. Bryant, RA, Waters, E, Gibbs, L, Gallagher, HC, Pattison, P, Lusher, D, et al. Psychological outcomes following the Victorian black Saturday bushfires. Aust N Z J Psychiatry. (2014) 48:634–43. doi: 10.1177/0004867414534476
11. Agyapong, B, Shalaby, R, Eboreime, E, Obuobi-Donkor, G, Owusu, E, Adu, MK, et al. Cumulative trauma from multiple natural disasters increases mental health burden on residents of Fort McMurray. Eur J Psychotraumatol. (2022) 13:2059999. doi: 10.1080/20008198.2022.2059999
12. Bryant, RA, Gibbs, L, Gallagher, HC, Pattison, P, Lusher, D, MacDougall, C, et al. Longitudinal study of changing psychological outcomes following the Victorian black Saturday bushfires. Aust N Z J Psychiatry. (2018) 52:542–51. doi: 10.1177/0004867417714337
13. Tang, B, Liu, X, Liu, Y, Xue, C, and Zhang, L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health. (2014) 14:623. doi: 10.1186/1471-2458-14-623
14. Agyapong, VIO, Ritchie, A, Brown, MRG, Noble, S, Mankowsi, M, Denga, E, et al. Long-term mental health effects of a devastating wildfire are amplified by socio-demographic and clinical antecedents in elementary and high school staff. Front Psych. (2020) 11:448. doi: 10.3389/fpsyt.2020.00448
15. Bryant, RA, Gibbs, L, Colin Gallagher, H, Pattison, P, Lusher, D, MacDougall, C, et al. The dynamic course of psychological outcomes following the Victorian black Saturday bushfires. Aust N Z J Psychiatry. (2021) 55:666–77. doi: 10.1177/0004867420969815
16. Norris, FH, Friedman, MJ, and Watson, PJ. 60,000 disaster victims speak: part II. Summary and implications of the disaster mental health research. Psychiatry. (2002) 65:240–60. doi: 10.1521/psyc.65.3.240.20169
17. Ruzek, JI, Kuhn, E, Jaworski, BK, Owen, JE, and Ramsey, KM. Mobile mental health interventions following war and disaster. Mhealth. (2016) 2:37. doi: 10.21037/mhealth.2016.08.06
18. Ruzek, JI, and Yeager, CM. Internet and mobile technologies: addressing the mental health of trauma survivors in less resourced communities. Glob Ment Health. (2017) 4:e16. doi: 10.1017/gmh.2017.11
19. Cohen, O, Shapira, S, and Furman, E. Long-term health impacts of wildfire exposure: a retrospective study exploring hospitalization dynamics following the 2016 wave of fires in Israel. Int J Environ Res Public Health. (2022) 19:5012. doi: 10.3390/ijerph19095012
20. Obuobi-Donkor, G, Shalaby, R, Vuong, W, Agyapong, B, Hrabok, M, Gusnowski, A, et al. Effects of Text4Hope-addiction support program on cravings and mental health symptoms: results of a longitudinal cross-sectional study. JMIR Form Res. (2023) 7:e40440. doi: 10.2196/40440
21. Obuobi-Donkor, G, Eboreime, E, Shalaby, R, Agyapong, B, Adu, MK, Owusu, E, et al. Evaluating community resilience and associated factors one year after the catastrophic Fort McMurray flood. Int J Environ Res Public Health. (2022) 19:16153. doi: 10.3390/ijerph192316153
22. Fletcher, D, and Sarkar, M. Psychological resilience. Eur Psychol. (2013) 18:12–23. doi: 10.1027/1016-9040/a000124
23. American Psychological Association. (2012). Building your resilience. What is resilience? Available at: (https://www.apa.org/topics/resilience)
24. Masten, AS. Ordinary magic: resilience processes in development. Am Psychol. (2001) 56:227–38. doi: 10.1037/0003-066X.56.3.227
25. Agyapong, VIO, Hrabok, M, Shalaby, R, Vuong, W, Noble, JM, Gusnowski, A, et al. Text4Hope: receiving daily supportive text messages for 3 months during the COVID-19 pandemic reduces stress, anxiety, and depression. Disaster Med Public Health Prep. (2021) 16:1326–30. doi: 10.1017/dmp.2021.27
26. Harris, PA, Taylor, R, Thielke, R, Payne, J, Gonzalez, N, and Conde, JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
27. Topp, CW, Østergaard, SD, Søndergaard, S, and Bech, P. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. (2015) 84:167–76. doi: 10.1159/000376585
28. Smith, BW, Dalen, J, Wiggins, K, Tooley, E, Christopher, P, and Bernard, J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) 15:194–200. doi: 10.1080/10705500802222972
29. Spitzer, RL, Kroenke, K, Williams, JBW, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
30. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
31. Weathers, FW, Litz, BT, Herman, DS, Huska, JA, and Keane, TM. The PTSD checklist (PCL): reliability, validity, and diagnostic utility. San Antonio, TX: Annual convention of the international society for traumatic stress studies (1993).
32. World Health Organization., Wellbeing measures in primary health care/the DepCare project: report on a WHO meeting, 12–13. (1998), World Health Organization. Stockholm, Sweden.
33. Shalaby, R, Agyapong, B, Vuong, W, Hrabok, M, Gusnowski, A, Surood, S, et al. Naturalistic randomized controlled trial demonstrating effectiveness of Text4Hope in supporting male population mental health during the COVID-19 pandemic. Front Public Health. (2022) 10:1002288. doi: 10.3389/fpubh.2022.1002288
34. Agyapong, VIO, Juhás, M, Ohinmaa, A, Omeje, J, Mrklas, K, Suen, VYM, et al. Randomized controlled pilot trial of supportive text messages for patients with depression. BMC Psychiatry. (2017) 17:286. doi: 10.1186/s12888-017-1448-2
35. Agyapong, VIO, Juhás, M, Mrklas, K, Hrabok, M, Omeje, J, Gladue, I, et al. Randomized controlled pilot trial of supportive text messaging for alcohol use disorder patients. J Subst Abus Treat. (2018) 94:74–80. doi: 10.1016/j.jsat.2018.08.014
36. Dias, RDL, Shalaby, R, Agyapong, B, Vuong, W, Gusnowski, A, Surood, S, et al. The effectiveness of CBT-based daily supportive text messages in improving female mental health during COVID-19 pandemic: results from the Text4Hope program. Front Glob Womens Health. (2023) 4:1182267. doi: 10.3389/fgwh.2023.1182267
37. Agyapong, B, Shalaby, R, Vuong, W, Gusnowski, A, Surood, S, Greenshaw, AJ, et al. Text4Hope effectiveness in reducing psychological symptoms among young adults in Canada: longitudinal and naturalistic controlled program evaluation. J Clin Med. (2023) 12:1942. doi: 10.3390/jcm12051942
38. Obuobi-Donkor, G, Shalaby, R, Eboreime, E, Agyapong, B, Phung, N, Eyben, S, et al. Text4PTSI: a promising supportive text messaging program to mitigate psychological symptoms in public safety personnel. Int J Environ Res Public Health. (2023) 20:4215. doi: 10.3390/ijerph20054215
39. Dhand, N., and Khatkar, M., (2023). Sample size calculator for comparing paired differences. Available at: https://statulator.com/SampleSize/ss2PM.html (Accessed December 24, 2023).
41. Xu, H, and Biogenidec, I. LOCF method and application in clinical data analysis. Burlington VT: National SAS Users Group (2009).
42. Lowe, SR, Joshi, S, Pietrzak, RH, Galea, S, and Cerdá, M. Mental health and general wellness in the aftermath of hurricane Ike. Soc Sci Med. (1982) 124:162–70. doi: 10.1016/j.socscimed.2014.11.032
43. Lowe, SR, Bonumwezi, JL, Valdespino-Hayden, Z, and Galea, S. Posttraumatic stress and depression in the aftermath of environmental disasters: a review of quantitative studies published in 2018. Curr Environ Health Rep. (2019) 6:344–60. doi: 10.1007/s40572-019-00245-5
44. Eisenman, D, McCaffrey, S, Donatello, I, and Marshal, G. An ecosystems and vulnerable populations perspective on Solastalgia and psychological distress after a wildfire. EcoHealth. (2015) 12:602–10. doi: 10.1007/s10393-015-1052-1
45. Eisenman, DP, and Galway, LP. The mental health and well-being effects of wildfire smoke: a scoping review. BMC Public Health. (2022) 22:2274. doi: 10.1186/s12889-022-14662-z
46. MRG, B, Pazderka, H, VIO, A, Greenshaw, AJ, Cribben, I, et al. Mental health symptoms unexpectedly increased in students aged 11-19 years during the 3.5 years after the 2016 Fort McMurray wildfire: findings from 9,376 survey responses. Front Psych. (2021) 12:676256. doi: 10.3389/fpsyt.2021.676256
47. Rosenthal, A, Stover, E, and Haar, RJ. Health and social impacts of California wildfires and the deficiencies in current recovery resources: an exploratory qualitative study of systems-level issues. PLoS One. (2021) 16:e0248617. doi: 10.1371/journal.pone.0248617
48. Salazar de Pablo, G, Guinart, D, and Correll, CU. What are the physical and mental health implications of duration of untreated psychosis? Eur Psychiatry. (2021) 64:e46. doi: 10.1192/j.eurpsy.2021.22
49. Stain, HJ, Kelly, B, Carr, VJ, Lewin, TJ, Fitzgerald, M, and Fragar, L. The psychological impact of chronic environmental adversity: responding to prolonged drought. Soc Sci Med. (2011) 73:1593–9. doi: 10.1016/j.socscimed.2011.09.016
50. Berrouiguet, S, Baca-García, E, Brandt, S, Walter, M, and Courtet, P. Fundamentals for future Mobile-health (mHealth): a systematic review of Mobile phone and web-based text messaging in mental health. J Med Internet Res. (2016) 18:e135. doi: 10.2196/jmir.5066
51. Goldmann, E, and Galea, S. Mental health consequences of disasters. Annu Rev Public Health. (2014) 35:169–83. doi: 10.1146/annurev-publhealth-032013-182435
52. Mao, W, and Agyapong, VI. The role of social determinants in mental health and resilience after disasters: implications for public health policy and practice. Front Public Health. (2021) 9:8528. doi: 10.3389/fpubh.2021.658528
53. Huguet, A, Rao, S, McGrath, PJ, Wozney, L, Wheaton, M, Conrod, J, et al. A systematic review of cognitive behavioral therapy and behavioral activation apps for depression. PLoS One. (2016) 11:e0154248. doi: 10.1371/journal.pone.0154248
54. Agyapong, VIO, Shalaby, R, Hrabok, M, Vuong, W, Noble, JM, Gusnowski, A, et al. Mental health outreach via supportive text messages during the COVID-19 pandemic: improved mental health and reduced suicidal ideation after six weeks in subscribers of Text4Hope compared to a control population. Int J Environ Res Public Health. (2021) 18:2157. doi: 10.3390/ijerph18042157
55. Keyes, CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. (2002) 43:207–22. doi: 10.2307/3090197
56. Wood, AM, and Joseph, S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten year cohort study. J Affect Disord. (2010) 122:213–7. doi: 10.1016/j.jad.2009.06.032
57. Smith, KL, Kerr, DA, Fenner, AA, and Straker, LM. Adolescents just do not know what they want: a qualitative study to describe obese adolescents' experiences of text messaging to support behavior change maintenance post intervention. J Med Internet Res. (2014) 16:e103. doi: 10.2196/jmir.3113
58. Khushalani, JS, Qin, J, Cyrus, J, Buchanan Lunsford, N, Rim, SH, Han, X, et al. Systematic review of healthcare costs related to mental health conditions among cancer survivors. Expert Rev Pharmacoecon Outcomes Res. (2018) 18:505–17. doi: 10.1080/14737167.2018.1485097
59. Nowels, MA, and VanderWielen, LM. Comorbidity indices: a call for the integration of physical and mental health. Prim Health Care Res Dev. (2018) 19:96–8. doi: 10.1017/S146342361700041X
60. Nsagha, DS, Siysi, VV, Ekobo, S, Egbe, TO, and Kibu, OD. One-way and two-way Mobile phone text messages for treatment adherence among patients with HIV: protocol for a randomized controlled trial. JMIR Res Protoc. (2020) 9:e16127. doi: 10.2196/16127
61. Bendtsen, M, and Bendtsen, P. Feasibility and user perception of a fully automated push-based multiple-session alcohol intervention for university students: randomized controlled trial. JMIR Mhealth Uhealth. (2014) 2:e30. doi: 10.2196/mhealth.3233
Keywords: wildfires, mental health, supportive text intervention, Alberta, Nova Scotia
Citation: Obuobi-Donkor G, Shalaby R, Agyapong B, Dias RdL, Eboreime E, Wozney L and Agyapong VIO (2024) Evaluating the 3-month post-intervention impact of a supportive text message program on mental health outcomes during the 2023 wildfires in Alberta and Nova Scotia, Canada. Front. Public Health. 12:1452872. doi: 10.3389/fpubh.2024.1452872
Edited by:
Xiao Zhang, Peking University Sixth Hospital, ChinaReviewed by:
Assis Kamu, Universiti Malaysia Sabah, MalaysiaShanling Ji, Jining Medical University, China
Copyright © 2024 Obuobi-Donkor, Shalaby, Agyapong, Dias, Eboreime, Wozney and Agyapong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vincent Israel Opoku Agyapong, dm42MDIzNjdAZGFsLmNh
 Gloria Obuobi-Donkor
Gloria Obuobi-Donkor Reham Shalaby
Reham Shalaby Belinda Agyapong
Belinda Agyapong Raquel da Luz Dias
Raquel da Luz Dias Ejemai Eboreime
Ejemai Eboreime Lori Wozney
Lori Wozney Vincent Israel Opoku Agyapong1,2*
Vincent Israel Opoku Agyapong1,2*