- 1Department of Health Care Sciences, Palliative Care Research Center, Marie Cederschiöld University, Stockholm, Sweden
- 2Department of Community Health Nursing, School of Nursing & Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Nursing Care Research Center in Chronic Diseases, Medical and Surgical Nursing Department, School of Nursing and Midwifery, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 4Department of Biostatistics and Epidemiology, School of Public Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
- 5Medical and Surgical Nursing Department, Taleghani Hospital, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Background: During the spread of COVID-19, nurses on the front line of fighting the disease experienced severe psychological pressures. The ability to adapt to difficult situations is an essential requirement for maintaining individuals’ endurance during a crisis. This study was designed to explore the relationship between three outcome variables of resilience, sense of coherence (SOC), and perceived social support in a sample of Iranian nurses during the spread of the COVID-19 pandemic.
Methods: A cross-sectional study with a correlational design was conducted on 360 registered nurses from six university hospitals during the seventh wave of COVID-19 in our society. Data collection was conducted by the demographic information questionnaire, the Connor–Davidson Resilience Scale (CD-RISC), the Sense of Coherence Scale (SOC-13), and the Multidimensional Scale of Perceived Social Support (MSPSS).
Results: The results of the structural equation modeling (SEM) showed that social support had a direct positive effect on the SOC (β = 0.498, p < 0.001), and the SOC had a direct positive effect on the resilience (β = 0.688, p < 0.001). Furthermore, we found an indirect effect of social support on resilience through the complete mediating role of the SOC.
Conclusion: The full mediating role of SOC in the relationship between social support and resilience showed that nurses with a higher level of SOC had a better understanding of social support, and this can influence their resilience in the COVID-19 crisis. This is theoretical support for the application of the salutogenic approach to health intervention plans to promote a healthy orientation in nurses toward mobilizing resources.
Introduction
Now more than 4 years have passed since the beginning of the COVID-19 pandemic worldwide, but its harmful psychological effects on the general health of individuals have remained (1). Nurses, as the first group on the front line of facing the COVID-19 pandemic, experienced different severe psychological pressures (2). Continuous stress experienced by nurses—stemming from high workloads, the fear of transmitting the coronavirus to family and friends, feelings of loneliness, low perceived social support, and decreased life expectancy—has resulted in numerous physical, mental, social, and spiritual challenges for them (1–3). The results of a study conducted to examine nurses’ perceptions and experiences during the COVID-19 outbreak in Iran revealed that Iranian nurses experienced high levels of psychological distress. This distress was attributed to several factors, including the unexpected nature of the situation, insufficient knowledge and skills to manage it, and concerns about the health of their families, as well as social stigma (4). Furthermore, they brought consequences such as weakness in decision-making and prioritization of care and ultimately a decrease in the quality of patient care (5).
Evidence indicates that the ability to adapt to challenging situations, known as resilience, has been a crucial factor in maintaining individuals’ endurance during crises such as COVID-19 (6, 7). Resilience is regarded as a personality trait that enhances one’s capacity to explain and predict issues and increase the capacity to cope with stressful events (8). Individuals with high resilience possess the ability to strategize, make sound decisions, and try to solve problems by operational and communication skills. They have a positive attitude toward themselves and their activities (9). The results of earlier studies indicate that higher resilience among nurses during the COVID-19 pandemic was strongly associated with increased job satisfaction, improved quality of patient care, reduced burnout, and lower levels of psychological distress (6, 10–12). Various factors influence the resilience of nurses, among them sense of coherence (SOC) as an inner strength can be a useful factor in dealing with unavoidable stressors. Previous literature shows that higher SOC was related to higher resilience (13). In other words, SOC appeared to be beneficial for mental health and mental well-being strengthening the individual’s resilience (14, 15).
SOC is an individual’s overall orientation to his life, and it guides him to find and use appropriate resources to maintain his health and manage his stress (16). It has been raised in Antonovsky’s Salutogenic model. Antonovsky defined the SOC as a stable and dynamic sense in humans that makes life events comprehensible, manageable, and meaningful (17). SOC is an inner strength that moderates the effects of stress on health (16). Nurses who have high levels of SOC are more task-oriented and are more capable of dealing with tensions in their work environments (18). Studies conducted during the COVID-19 pandemic have indicated that nurses confronted many challenges, and the SOC is indicated to be a strong predictor of psychological components and mental health (19). Thus, nurses with a low SOC experienced more psychological distress (2).
In addition to the SOC, another factor that plays a predictor of mental health and leads to the improvement of the level of resilience in individuals is social support (3, 20). Perceived social support (PSS) includes love, empathy, care, self-esteem, attention, and receiving help from others and refers to people’s cognitive evaluation of relationships and support systems (20). It is one of the components that plays a significant role in nurses’ performance in critical situations and plays a significant role in overcoming stress and tensions in the nursing work environment (12, 21). Low levels of social support in nurses have been associated with job burnout, depression, stress, anxiety, and reduced performance in the care of their patients (3, 22). The results of studies during the COVID-19 pandemic have also indicated the positive effects of social support on reducing psychological pressures caused by the pandemic (3).
Considering the psychological needs and problems of nurses during the COVID-19 pandemic and the importance of paying attention to this category of issues, healthcare sector employees, especially nurses, need to be equipped with the necessary psychological skills (23). For this purpose, the correct understanding of the psychological needs and problems of individuals is very important. It is also necessary to identify strategies that can protect the mental health of nurses after the COVID-19 pandemic and/or other crises. These strategies enable them to have an appropriate response to crises in the future (24). It is important to know that the COVID-19 pandemic is not over yet and it will not be the last pandemic in our lives. Thus, it is always important to deal with crises and be aware of practical solutions.
Although there are various studies in the field of resilience and its relationship with the variables of social support and SOC, and also some studies have been published recently that have investigated these three variables simultaneously (25, 26), the aims of these studies are different from ours, and the effect of these three variables on each other has not been investigated. We tried to explore the relationship between resilience, SOC, and social support in a sample of Iranian nurses during the spread of the COVID-19 pandemic. By identifying the direct, indirect, and general effects of these variables on each other, the mechanisms of how the variables affect each other would be clarified (27).
Methods
Design
This is a cross-sectional study with a correlational design which was conducted from the first of September 2021 to the end of January 2022, simultaneously with the seventh wave of COVID-19 in our society (28).
Hypotheses
To better understand the relationships between resilience, SOC, and PSS, we propose the following hypotheses:
1. The level of PSS has a direct positive effect on the level of resilience.
2. The level of PSS has a direct positive effect on the level of SOC.
3. The level of SOC has a direct positive effect on the level of resilience.
4. The level of PSS has an indirect effect on the level of resilience through the level of SOC (the mediating role of the SOC).
Sampling and data collection
Registered nurses were selected by quota sampling from six major university hospitals in Ahvaz, the capital of Khuzestan province, Southwestern Iran. Nurses who worked at least 6 months in COVID-19 time at university hospitals with a minimum of 1 year of nursing experience were employed to participate in the study. According to the nurses’ population at university hospitals (n = 1900), 320 nurses were enrolled in the study. Calculation of the sample size was conducted by the Cochrane formula (95% confidence interval and 80% power of the study). We accessed the list of nurses’ names through the nursing departments of the university hospitals and selected eligible nurses. One and a half times the calculated quota in each university hospital, an online invitation letter to participate in the study together with an online informed consent form and a link to the website to access the questionnaires was sent to eligible nurses through social networks and/or SMS. They were asked to answer the questionnaires for four working days. In this way, 540 registered nurses in six university hospitals got these invitations, but only 366 registered nurses answered positively to participate in the study (67.8%).
Measurements
Data were collected through a demographic information questionnaire and a Persian version of the three self-reported scales.
Demographic information questionnaire
The questionnaire included variables such as age, sex, education level, work experience, and history of caring for COVID-19 patients.
Connor–Davidson resilience scale
The resilience of nurses was measured using the CD-RISC. The CD-RISC consists of 25 items and 5 subscales: personal competence, high standards and tenacity (8 items), trust in one’s instincts, tolerance of negative affect and strengthening effects of stress (7 items), positive acceptance of change and secure relationships (5 items), self-control (3 items), and spiritual influences (2 items). The responses are rated on a 5-point Likert scale ranging from completely incorrect (score: 0) to completely correct (score: 4). The values on the scale range from 0 to 100, with higher values, indicating greater resilience (29). A Persian version of the CD-RISC has been validated in Iran (30). The reliability of the scale was calculated at 0.83 using Cronbach’s alpha coefficient in the present study.
Sense of coherence scale
Nurses’ SOC was measured by the SOC scale with 13 items and three subscales of comprehensibility (5 items), manageability (4 items), and meaningfulness (4 items). The scale has a semantic differential format with two anchoring responses (1 to 7). The scoring range is 13–91; the higher the score, the stronger the SOC (17). This scale has been previously validated in the Iranian population (31). In the current study, the reliability of the scale was calculated at 0.74 using Cronbach’s alpha coefficient.
Multidimensional scale of perceived social support
The MSPSS includes 12 items with three subscales: family (4 items), friends (4 items), and significant others (4 items) (32). The participants’ responses were rated on a 7-point Likert scale ranging from very strongly disagree to very strongly agree (1 to 7). The total score of the scale varies from 12 to 84, with a higher score, indicating better PSS. The scale has been validated in Iran (33). In the current study, the reliability of the scale was calculated at 0.96 using Cronbach’s alpha coefficient.
Statistical analysis
Data analysis was performed by SPSS version 20 (IBM Corporation, Armonk, NY, United States). All variables met the normality assumptions by P–P plots. An independent t-test was used to compare the mean score of resilience, the SOC, and the PSS in terms of dichotomous demographic variables. At first, relationships between three outcome variables (resilience, SOC, and PSS) were evaluated in a correlation matrix using Pearson’s correlation coefficients. Structural equation modeling (SEM) analysis was conducted by AMOS version 20.0 (34). All independent variables were included in the model, regardless of their significance, to understand the role of all variables. The effects of independent variables are adjusted in the model (coefficients in Figure 1). No paths have been excluded from the model. In the SEM analysis, maximum likelihood estimation (MLE) was applied as the most commonly used estimation method (35). Several specific indices and cutoff points were selected for SEM analysis. The indices were chi-square to the degrees of freedom ratio (criteria: ratio < 6), goodness-of-fit index (GFI) (criteria: ≥ 0.90), normed fit index (NFI) (criteria: ≥ 0.90), comparative fit index (CFI) (criteria: ≥ 0.90), Tucker–Lewis index (TLI) (criteria: ≥ 0.90), and incremental fit index (IFI) (criteria: ≥ 0.90), root mean square error of approximation (RMSEA) (criteria: less than 0.05 are good, between 0.05 and 0.08 are acceptable) (36). As a rule of thumb (37), the degree of SOC is considered a total mediator if the correlation between the independent (PSS) and dependent (resilience) variables would be non-significant in the SEM analysis, while their relationship was significant earlier in a two-by-two matrix.
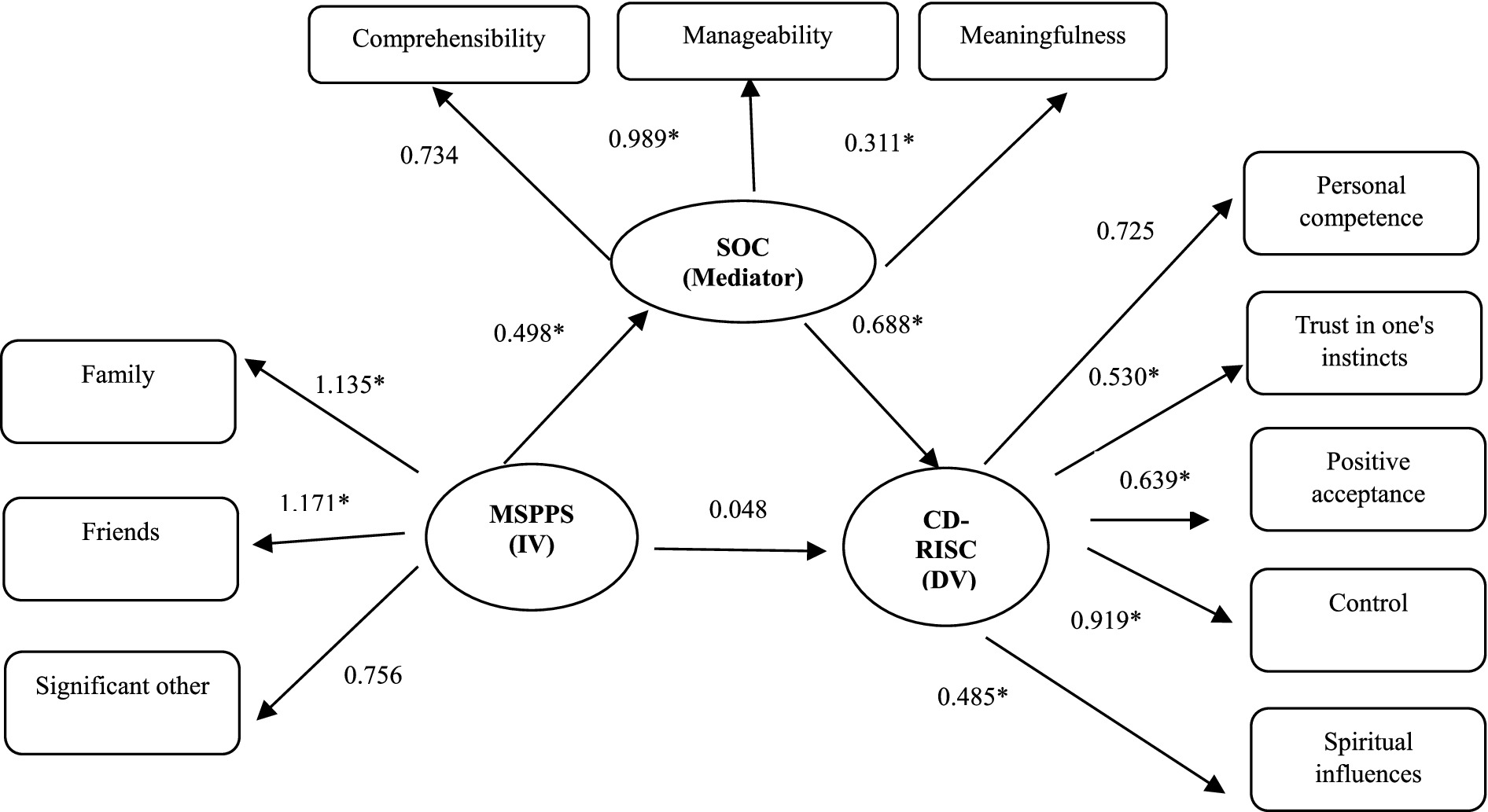
Figure 1. Structural equation modeling with dependent (DV) and independent (IV) variables. The numbers are standardized regression weights (β); SOC, sense of coherence; CD-RISC, Connor–Davidson resilience scale; MSPSS, multidimensional scale of perceived social support; *p < 0.001.
Results
Descriptive results
The mean age of registered nurses was 33.6 ± 6.03 years old. Most of the nurses were females (74.1%) and 63.5% of them had a history of caring for COVID-19 patients in ICUs (30.5%) or general wards of university hospitals (33%). The history of caring for COVID-19 patients was significant in registered nurses based on the mean scores of three outcome variables. Nurses who had experience caring for COVID-19 patients had significantly higher resilience (p = 0.001), SOC (p < 0.001), and PSS (p = 0.001). The rest of the demographic characteristics of registered nurses is presented in Table 1 based on the mean levels of resilience, SOC, and PSS.
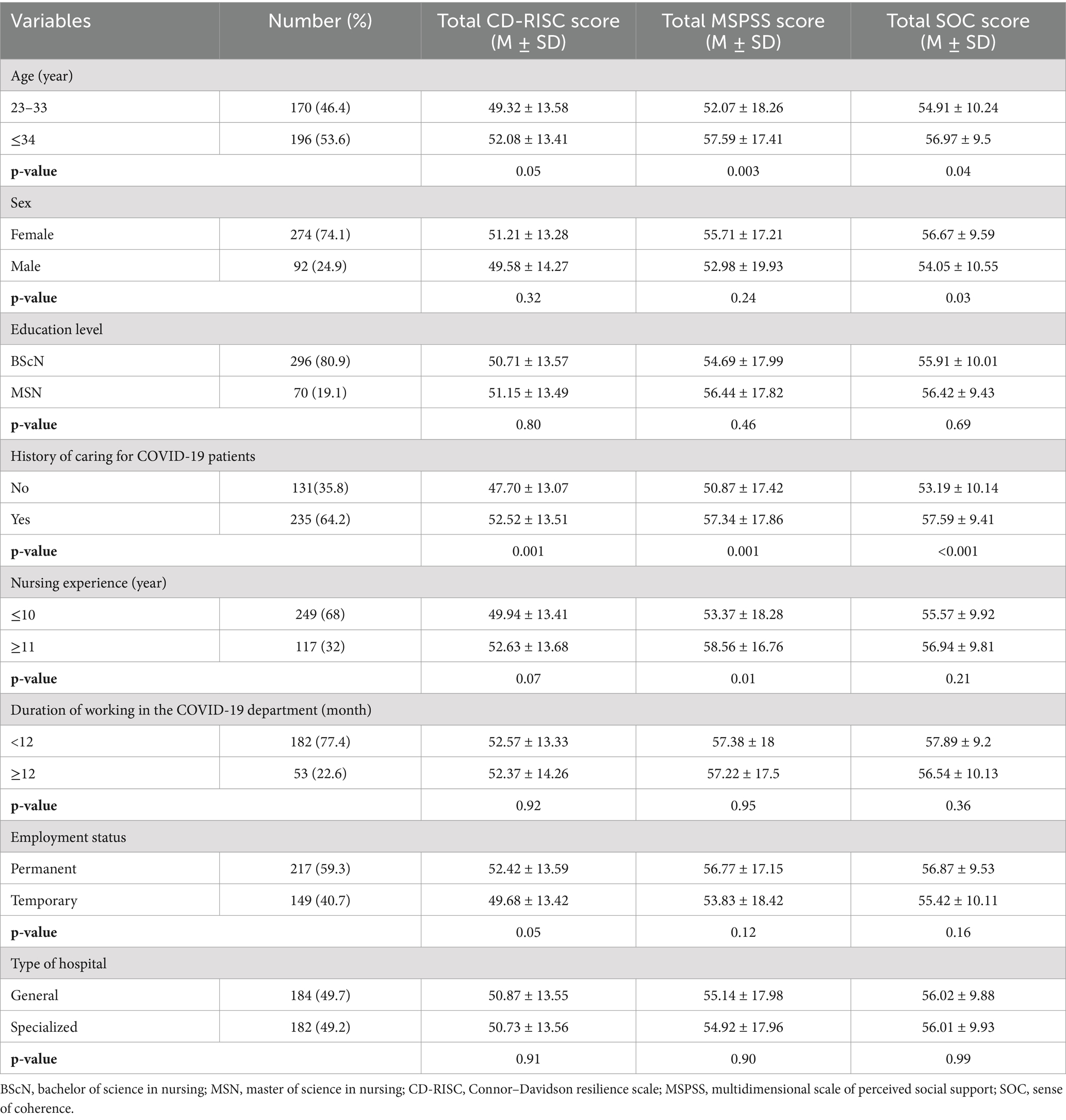
Table 1. Demographic characteristics of registered nurses based on the three outcome variables; the CD-RISC, the MSPSS, and the SOC (n = 366).
Nurses’ mean scores of resilience with five subscales, the PSS with three subscales, and the SOC scale with three subscales are presented in Table 2. The mean scores of three outcome variables of resilience, PSS, and SOC were reported as 50.80 ± 13.54 (range: 0–100), 55.03 ± 17.95 (range: 12–84), and 56.01 ± 9.89 (range: 13–91), respectively (Table 2).
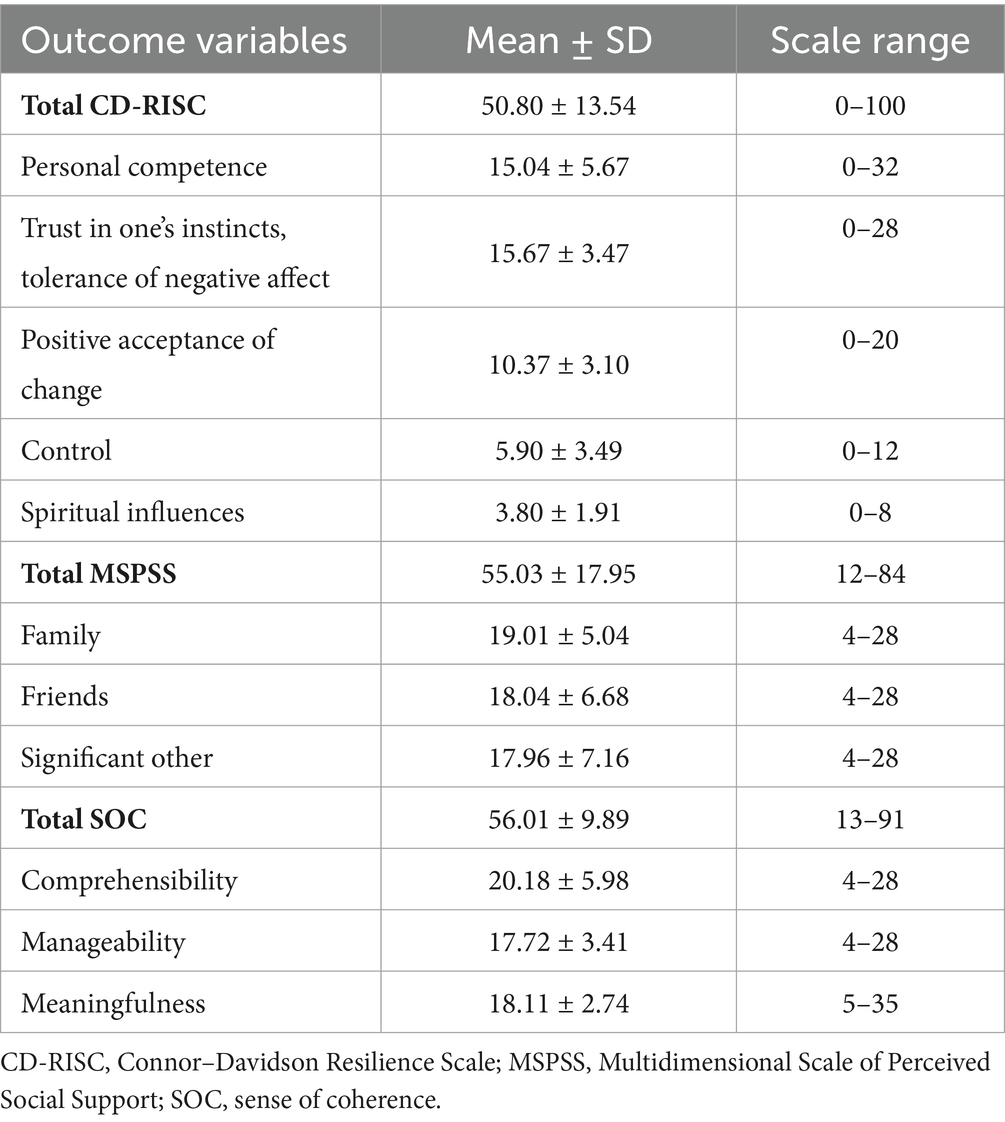
Table 2. Descriptive data for outcome variables, including the CD-RISC, the MSPSS, and the SOC in nurses (n = 366).
Results of the two-by-two relationships between variables
Analyses started with the calculation of Pearson correlation coefficients between SOC, PSS, and resilience scale scores in a correlation matrix (Table 3). The results showed that there is a significant positive correlation between the PSS and the resilience (r = 0.51, p < 0.001) as well as between the SOC and the resilience (r = 0.61, p < 0.001). Furthermore, a significant positive correlation was found between the SOC and the PSS (r = 0.51, p < 0.001).
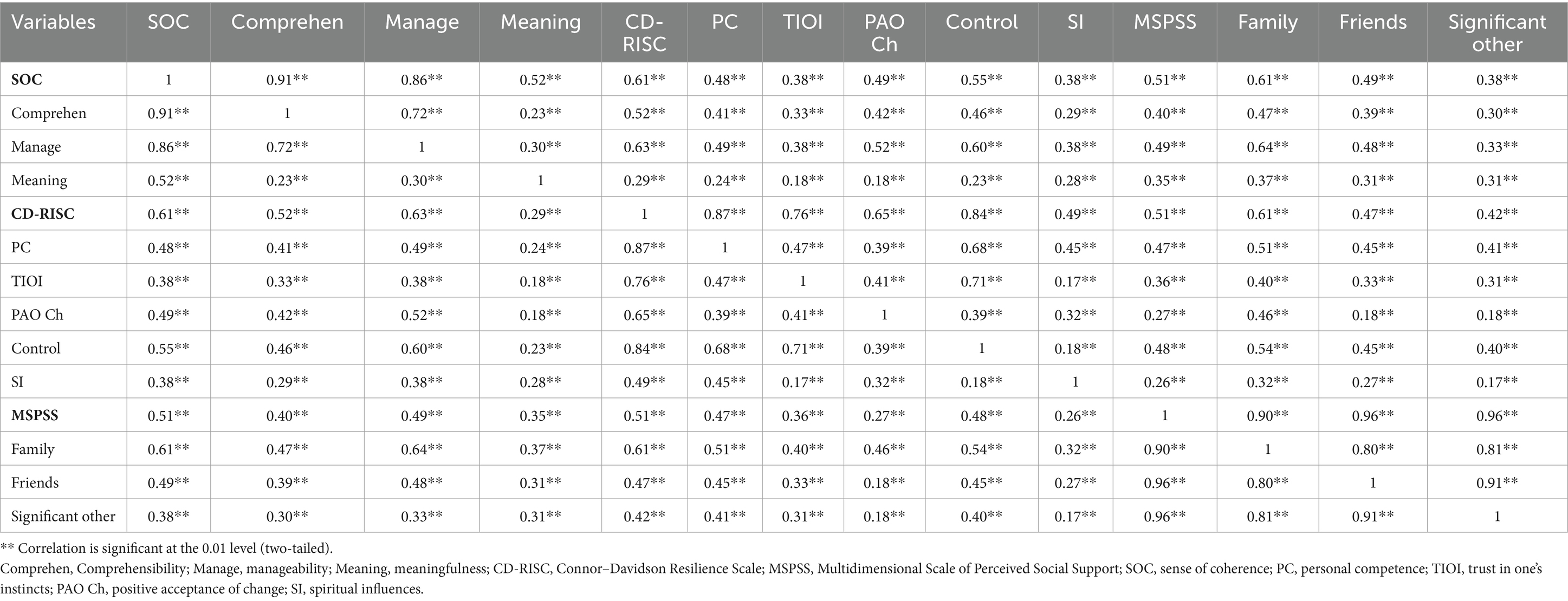
Table 3. Correlation matrix between variables of the CD-RISC, the MSPSS, and the SOC in a sample of Iranian nurses (n = 366).
Results of the role of the variables in the relationships
According to the results of the correlation matrix, the mediating role of the SOC was tested on the relationship between variables of PSS (independent variable) and resilience (dependent variable) by SEM analysis. After controlling for demographic variables of age (continuous variable), sex (dichotomous variable), education level (two categories), years of nursing experience (continuous variable), duration of working in the COVID-19 department (continuous variable), employment status (two categories), history of caring for COVID-19 patients (dichotomous variable), and type of university hospital (two categories), the level of SOC showed a fully mediating effect in the relationships between the PSS and the resilience. For clarity, independent variables have been omitted from Figure 1.
The fit indices of the model were not ideal before the modifications; however, after adjusting the relationships between covariances, the indices in the final modified model showed significant improvement (Table 4).
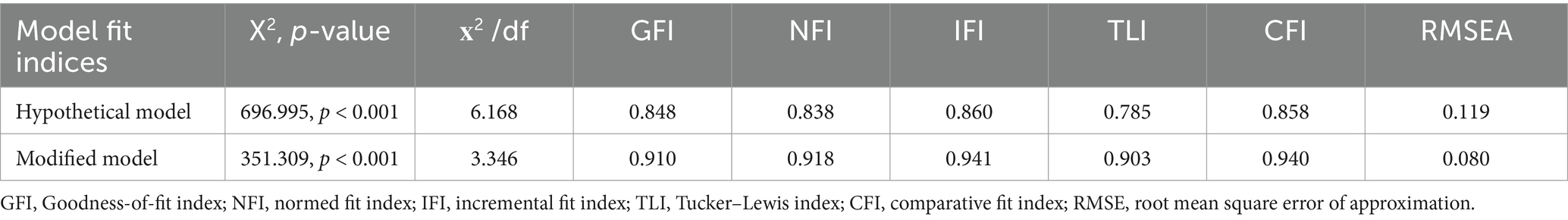
Table 4. Goodness of fit indices in hypothetical and modified models by SEM analyses in a sample of Iranian nurses (n = 366).
Therefore, in response to the hypotheses of the study, the first hypothesis was rejected (the direct positive effect of the PSS on resilience), but the rest of them were accepted (the direct positive effect of the PSS on the SOC and the direct positive effect of the SOC on the resilience). Moreover, the indirect effect of PSS on resilience through the level of SOC was confirmed.
The paths and standardized regression coefficients (the standardized regression weights represent the amount of change in the dependent variable that is attributable to a single standard deviation unit’s worth of change in the predictor variable) and the mediating effect of the SOC have been shown in the modified model in Figure 1. As shown, the PSS has a significant direct effect on the SOC (β = 0.498, p < 0.001), and the SOC has a significant direct effect on the resilience (β = 0.688, p < 0.001), but the direct effect between the PSS and the resilience (r = 0.51, p = 0.01 in Table 3) disappeared through the mediating role of the SOC (β = 0.048, p = 0.055) (Figure 1).
Discussion
The present study is designed to test the relationships between three outcome variables of resilience, SOC, and PSS in a sample of registered nurses at university hospitals during the seventh wave of COVID-19 in Iran. Our results showed that the hypothetical model of the study had a good fit after adjustment and that all the hypotheses of this model were accepted except the first hypothesis (the level of PSS has a direct positive effect on the level of resilience). Thus, the complete mediating role of SOC in the relationship between PSS and resilience was confirmed in this model.
Previous studies showed that there is a bidirectional relationship between PSS and resilience. PSS refers to people’s subjective assessment of supportive relationships and behaviors (20) and is known as one of the most important external factors affecting people’s capacity to overcome stressful situations and their resilience level in difficult situations (38, 39). On the other hand, the level of resilience is also a person’s confidence in their coping abilities, self-esteem, and personal characteristics, which increases the reception of PSS from others (40). Because resilience emphasizes the use of coping strategies in difficult situations (8), it leads individuals to receive more PSS. In fact, due to their positive thinking, high sense of empathy, and cooperative problem-solving in unfavorable and tense situations, people who have high resilience will rush to help family members, friends, and others and enjoy a wide circle of support and social relations (3). Furthermore, studies have shown that nurses who received support from friends, family members, relatives, managers, and colleagues during the critical situation of COVID-19 reported higher resilience (41, 42).
According to our results, it can be argued that there was not a simple relationship between PSS and resilience among Iranian nurses during the conditions of the COVID-19 crisis. This relationship was influenced by an important salutogenic factor, i.e., nurses’ level of SOC. It seems that nurses’ salutogenic view of life in the form of the SOC promoted their healthy attitudes toward the use of available resources such as social support, and it can influence their resilience in their lives, probably caring for COVID-19 and non-COVID-19 patients and managing their stressors during the COVID-19 crisis. Focusing on the role and power of the nurses’ SOC on the relationship between their PSS and resilience is one of the great lessons learned during the COVID-19 epidemic. Planning for salutogenic interventions based on the level of SOC as an internal resource and its development can assist the nurses in overcoming daily stressors during the crisis. Although Antonovsky believed that SOC is developed until the age of 30 and then remains stable and only decreases slightly during crises (16), later studies showed that an individual’s SOC can be improved by health interventions (43). People probably develop and enhance their use of SOC strategies as they accumulate experiences in managing life over time and in different circumstances (44). Antonovsky (17), in his model, explained that the level of SOC is a salutogenic factor that creates positive health. Furthermore, the level of SOC is dependent on two types of resistance resources: generalized (GRRs) and specific (SRR). GRRs have a “wide-ranging” benefit to stress management, but SRRs have a “situation-specific” benefit on special occasions of stress management (16). PSS is a GRR that can assist in developing a stronger SOC (45). Interestingly, evidence shows that PSS, in comparison to the received social support, is linked to health outcomes (46). Thus, individuals’ perception of available social support can change their perspective on their lives and even lead them to have a higher SOC, more resilience, and health. In the impact of social support in stressful situations, two models were reported in the literature: “buffering social support” and “main social support.” In the first model, the people who perceive more social support experience less stress in stressful situations compared to those who have less PSS. In the second model, there is a perception of social support even without stressful conditions (47). It is a complicated process; however, it is more likely nurses experienced the buffering effect of social support during the COVID-19 pandemic in the present study. Findings from a qualitative study conducted during the COVID-19 pandemic to determine nurses’ perceptions of social support indicated that nurses engaged with the crisis to assess their social support requirements and the feasibility of meeting those needs. They concentrated on the support that was accessible or believed to be accessible while setting aside certain needs that could not realistically be met at that time. Support from colleagues and the organization played a critical role in this process (48).
In any case, the effect of PSS on resilience is activated in the presence of SOC. In other words, the way nurses look at their life events is important; how much they understand them is meaningful, manageable, and comprehensible, influencing the relationship between their perception of social support and resilience. In a review of the literature, we could not find the mediating effect of SOC in the relationships between variables of social support and resilience. However, the results of a similar study showed that SOC and social support were simultaneously predictors of resilience in nurses during the COVID-19 era, although SOC was introduced as the strongest predictor of resilience (25). Furthermore, previous studies showed that the level of SOC was shown to have a mediating effect on relationships between stress management and individuals’ perception of health and well-being in different samples (47, 49).
Jiang and Luo (49) studied the mediating role of SOC in the relationship between PSS and social anxiety and found that in addition to having a direct effect on reducing students’ social anxiety, the perception of PSS exerted an indirect effect through the mediation of SOC. This relationship shows that by strengthening SOC in people, it is possible to help resolve existing tensions and create greater effects on improving people’s mental health and resilience. SOC has three characteristics, namely perceptibility, controllability, and meaningfulness, which means that people with higher SOC perceive life experiences as more perceivable, controllable, and meaningful (17). The high level of these components in SOC reflects the fact that people have a higher ability to mobilize resources and facilities in critical situations and can use useful resources to reduce pressure in external environments to maintain their internal stability in social interactions. This leads to optimism and adaptability in behavioral domains and can cause more PSS from people around the individual. Therefore, individuals with higher SOC also receive higher perceived PSS (49).
PSS, SOC, and resilience are individuals’ ways of handling stressors and maintaining health and well-being (2, 21, 50). From the complex relationships between them, it can be concluded that the application of a salutogenic approach to health-targeted intervention (e.g., training programs or workshops) plans may promote a healthy orientation in nurses toward mobilizing resources and experiencing more social support to manage daily stressors and benefit more resilience during the COVID-19 pandemic.
Strengths and limitations of the study
One of the strengths of the study is the investigation of relationships among three variables; such as resilience, SOC, and social support together. However, these relationships were evaluated in this study by a cross-sectional design. Therefore, for a deeper understanding of the causal relationships between these variables, it is suggested to evaluate them in longitudinal studies. In addition, the use of validated scales and the diversity of the sample from multiple hospitals can be as other strengths of this study.
Conclusion
The relationships between the three outcome variables of resilience, SOC, and PSS in a sample of registered nurses during the seventh wave of COVID-19 in Iran showed that the level of SOC completely mediates the relationship between PSS and resilience. In other words, nurses with higher levels of SOC experienced better perceptions of social support, which in turn helped promote nurses’ resilience during the COVID-19 pandemic. Our results provide theoretical support to reveal the mechanism between these three variables during the COVID-19 crisis. It can serve as a hypothesis for future research to design studies based on salutogenic interventions to promote the level of SOC as well as PSS and implement longitudinal studies to show broader dimensions of the complex mechanism between these variables.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (code number: IR.AJUMS.REC.1400.320). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. No potentially identifiable images or data are presented in this study.
Author contributions
CR: Writing – original draft, Writing – review & editing, Methodology, Conceptualization. MA: Writing – original draft, Writing – review & editing, Methodology, Data curation, Conceptualization, Investigation, Formal analysis, Resources, Project administration, Supervision, Validation. MST: Writing – review & editing, Data curation, Methodology, Formal analysis, Software. LM: Writing – review & editing, Visualization, Investigation, Data curation.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The project of this study (U-00148) was financially supported by the Ahvaz Jundishapur University of Medical Sciences, Ahvaz-Iran.
Acknowledgments
This study was extracted from a research proposal approved by the Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran (NO: U-00148). The researchers appreciate all staff in “Research & Technology Chancellor” at Ahvaz Jundishapur University of Medical Sciences for their financial support and all the nurses who participated in this study. We acknowledge the use of WORDVICE.AI (https://wordvice.ai/proofreading/6c21e242-4286-4ed0-93c7-ea479dd98f86) to proofread some sentences of our work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Brown, R, Da Rosa, P, Pravecek, B, and Carson, P. Factors associated with changes in nurses' emotional distress during the COVID-19 pandemic. Appl Nurs Res. (2023) 69:151659. doi: 10.1016/j.apnr.2022.151659
2. Gómez-Salgado, J, Domínguez-Salas, S, Romero-Martín, M, Ortega-Moreno, M, García-Iglesias, JJ, and Ruiz-Frutos, C. Sense of coherence and psychological distress among healthcare workers during the COVID-19 pandemic in Spain. Sustain For. (2020) 12:6855. doi: 10.3390/su12176855
3. Schierberl Scherr, AE, Ayotte, BJ, and Kellogg, MB. Moderating roles of resilience and social support on psychiatric and practice outcomes in nurses working during the COVID-19 pandemic. SAGE Open Nurs. (2021) 7:23779608211024213. doi: 10.1177/23779608211024213
4. Kalateh Sadati, A, Zarei, L, Shahabi, S, Heydari, ST, Taheri, V, Jiriaei, R, et al. Nursing experiences of COVID-19 outbreak in Iran: a qualitative study. Nurs Open. (2021) 8:72–9. doi: 10.1002/nop2.604
5. Yu, F, Raphael, D, Mackay, L, Smith, M, and King, A. Personal and work-related factors associated with nurse resilience: a systematic review. Int J Nurs Stud. (2019) 93:129–40. doi: 10.1016/j.ijnurstu.2019.02.014
6. Shahrbabaki, PM, Abolghaseminejad, P, lari, L, Zeidabadinejad, S, and Dehghan, M. The relationship between nurses’ psychological resilience and job satisfaction during the COVID-19 pandemic: a descriptive-analytical cross-sectional study in Iran. BMC Nurs. (2023) 22:1–8. doi: 10.1186/s12912-023-01310-z
7. Piras, I, Piazza, MF, Piccolo, C, Azara, A, Piana, A, Finco, G, et al. Experiences, emotions, and health consequences among COVID-19 survivors after intensive care unit hospitalization. Int J Environ Res Public Health. (2022) 19:6263. doi: 10.3390/ijerph19106263
8. Southwick, SM, Bonanno, GA, Masten, AS, Panter-Brick, C, and Yehuda, R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol. (2014) 5:25338. doi: 10.3402/ejpt.v5.25338
9. Manomenidis, G, Panagopoulou, E, and Montgomery, A. Resilience in nursing: the role of internal and external factors. J Nurs Manag. (2019) 27:172–8. doi: 10.1111/jonm.12662
10. Polizzi, C, Lynn, SJ, and Perry, A. Stress and coping in the time of COVID-19: pathways to resilience and recovery. Clin Neuropsychiatry. (2020) 17:59–62. doi: 10.36131/CN20200204
11. Afshari, D, Nourollahi-darabad, M, and Chinisaz, N. Psychosocial factors associated with resilience among Iranian nurses during COVID-19 outbreak. Front Public Health. (2021) 9:1092. doi: 10.3389/fpubh.2021.714971
12. Moisoglou, I, Katsiroumpa, A, Malliarou, M, Papathanasiou, IV, Gallos, P, and Galanis, P. Social support and resilience are protective factors against COVID-19 pandemic burnout and job burnout among nurses in the post-COVID-19 era. Healthcare. (2024) 12:710. doi: 10.3390/healthcare12070710
13. Konaszewski, K, Kolemba, M, and Niesiobędzka, M. Resilience, sense of coherence and self-efficacy as predictors of stress coping style among university students. Curr Psychol. (2021) 40:4052–62. doi: 10.1007/s12144-019-00363-1
14. Izydorczyk, B, Sitnik-Warchulska, K, Kühn-Dymecka, A, and Lizińczyk, S. Resilience, sense of coherence, and coping with stress as predictors of psychological well-being in the course of schizophrenia. The study design. Int J Environ Res Public Health. (2019) 16:1266. doi: 10.3390/ijerph16071266
15. Kase, T, Ueno, Y, and Endo, S. Association of sense of coherence and resilience with distress and infection prevention behaviors during the coronavirus disease pandemic. Curr Psychol. (2024) 43:707–16. doi: 10.1007/s12144-023-04359-w
16. Mosknes, U.K. Sense of coherence. In G. Haugan and M. Eriksson (Eds), Health promotion in health care – Vital theories and research. (2021). pp. 35–46. Springer Nature. Available at: https://link.springer.com/content/pdf/10.1007/978-3-030-63135-2_4?pdf=chapter%20toc (accessed August 8, 2023).
17. Antonovsky, A. Unraveling the mystery of health: how people manage stress and stay well. San Francisco, CA: Jossey-Bass (1987).
18. Michele Masanotti, G, Paolucci, S, Abbafati, E, Serratore, C, and Caricato, M. Sense of coherence in nurses: a systematic review. Int J Environ Res Public Health. (2020) 17:1861. doi: 10.3390/ijerph17061861
19. Schmuck, J, Hiebel, N, Rabe, M, Schneider, J, Erim, Y, Morawa, E, et al. Sense of coherence, social support and religiosity as resources for medical personnel during the COVID-19 pandemic: a web-based survey among 4324 health care workers within the German network university medicine. PLoS One. (2021) 16:e0255211. doi: 10.1371/journal.pone.0255211
20. Yang, C, Xia, M, Han, M, and Liang, Y. Social support and resilience as mediators between stress and life satisfaction among people with substance use disorder in China. Front Psych. (2018) 9:436. doi: 10.3389/fpsyt.2018.00436
21. Gholi, S, Jafari, S, Asgari, MR, and Kheirkhah, F. Role of perceived social support and job satisfaction on psychological distress of clinical nurses. Koomesh. (2020) 22:633–43. doi: 10.29252/koomesh.22.4.633
22. Chang, HE, and Cho, S-H. The influence of social support on the relationship between emotional demands and health of hospital nurses: a cross-sectional study. Healthcare. (2021) 9:1–13. doi: 10.3390/healthcare9020115
23. Fathi, E, Malekshahi Beiranvand, F, Hatami Varzaneh, A, and Nobahari, A. Health care workers challenges during coronavirus outbreak: the qualitative study. J Res Behav Sci. (2020) 18:237–48. doi: 10.52547/rbs.18.2.237
24. Aloweni, F, Ayre, TC, Teo, I, Tan, HK, and Lim, SH. A year after COVID-19: its impact on nurses' psychological well-being. J Nurs Manag. (2022) 30:2585–96. doi: 10.1111/jonm.13814
25. Kondo, A, Oki, T, and Eckhardt, AL. Factors related to resilience and attitudes towards care of the dying among critical care nurses. Nurs Crit Care. (2024) doi: 10.1111/nicc.13146 [Epub ahead of print].
26. Kagee, A, Padmabhanunni, A, Coetzee, B, Booysen, D, and Kidd, M. Sense of coherence, social support, satisfaction with life and resilience as mediators between fear of COVID-19, perceived vulnerability to disease and depression. S Afr J Psychol. (2024) 54:300–13. doi: 10.1177/00812463241259123
27. Buis, ML. Direct and indirect effects in a logit model. Stata J. (2010) 10:11–29. doi: 10.1177/1536867X1001000104
28. Ghotbi, N. The COVID-19 pandemic response and its impact on post-Corona health emergency and disaster risk Management in Iran. Sustain For. (2022) 14:14858. doi: 10.3390/su142214858
29. Connor, KM, and Davidson, JR. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
30. Derakhshanrad, SA, Piven, E, Rassafiani, M, Hosseini, SA, and Mohammadi Shahboulaghi, F. Standardization of connor-Davidson resilience scale in iranian subjects with cerebrovascular accident. J Rehabil Sci Res. (2014) 1:73–7. doi: 10.30476/jrsr.2014.41059
31. Rohani, C, Khanjari, S, Abedi, HA, Oskouie, F, and Langius-Eklöf, A. Health index, sense of coherence scale, brief religious coping scale and spiritual perspective scale: psychometric properties. J Adv Nurs. (2010) 66:2796–806. doi: 10.1111/j.1365-2648.2010.05409.x
32. Zimet, GD, Dahlem, NW, Zimet, SG, and Farley, GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
33. Bagherian-Sararoudi, R, Hajian, A, Ehsan, HB, Sarafraz, MR, and Zimet, GD. Psychometric properties of the Persian version of the multidimensional scale of perceived social support in Iran. Int J Prev Med. (2013) 4:1277–81.
34. Arbuckle, JL, and Wothke, W. IBM SPSS Amos 20 user’s guide. Amos Development Corporation, SPSS Inc. Chicago, IL, USA (1999).
36. Chen, FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Model Multidiscip J. (2007) 14:464–504. doi: 10.1080/10705510701301834
37. Chen, F, Curran, PJ, Bollen, KA, Kirby, J, and Paxton, P. An empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociol Methods Res. (2008) 36:462–94. doi: 10.1177/0049124108314720
38. Zhao, Y, Wang, H, Sun, D, Ma, D, Li, H, Li, Y, et al. Job satisfaction, resilience and social support in relation to nurses' turnover intention based on the theory of planned behaviour: a structural equation modelling approach. Int J Nurs Pract. (2021) 27:e12941. doi: 10.1111/ijn.12941
39. Ozsaban, A, Turan, N, and Kaya, H. Resilience in nursing students: the effect of academic stress and social support. Clin Exp Health Sci. (2019) 9:69–76. doi: 10.33808/marusbed.546903
40. Huang, Y, Wu, R, Wu, J, Yang, Q, Zheng, S, and Wu, K. Psychological resilience, self-acceptance, perceived social support and their associations with mental health of incarcerated offenders in China. Asian J Psychiatr. (2020) 52:102166. doi: 10.1016/j.ajp.2020.102166
41. Wang, L, Tao, H, Bowers, BJ, Brown, R, and Zhang, Y. Influence of social support and self-efficacy on resilience of early career registered nurses. West J Nurs Res. (2018) 40:648–64. doi: 10.1177/0193945916685712
42. Kılınç, T, and Sis, ÇA. Relationship between the social support and psychological resilience levels perceived by nurses during the COVID-19 pandemic: a study from Turkey. Perspect Psychiatr Care. (2021) 57:1000–8. doi: 10.1111/ppc.12648
43. Vastamäki, J, Moser, K, and Paul, KI. How stable is sense of coherence? Changes following an intervention for unemployed individuals. Scand J Psychol. (2009) 50:161–71. doi: 10.1111/j.1467-9450.2008.00695.x
44. Moghimi, D, Scheibe, S, and Freund, AM. The Model of Selection, Optimization, Compensation. In B Baltes, C Rudolph, & H Zacher (Eds.). Work Across the Lifespan (1 ed.). Elsevier (2019), 81–110.
45. Vinje, HF, Langeland, E, and Bull, T. Aaron Antonovsky’s Development of Salutogenesis, 1979 to 1994. 2016 Sep 3. In: Mittelmark MB, Sagy S, Eriksson M, Bauer GF, Pelikan JM, Lindström B, Espnes GA, editors. The Handbook of Salutogenesis [Internet]. Cham (CH): Springer (2017):25–40.
46. Drageset, J. Social support. In G. Haugan and M. Eriksson (Eds), Health promotion in health care – Vital theories and research. (2021): 137–144. Springer Nature. Available at: https://link.springer.com/chapter/10.1007/978-3-030-63135-2_11 (accessed August 8, 2023).
47. Kulcar, V, Kreh, A, Juen, B, and Siller, H. The role of sense of coherence during the COVID-19 crisis: does it exercise a moderating or a mediating effect on university students’ well-being? SAGE Open. (2023) 13:21582440231160123. doi: 10.1177/21582440231160123
48. Sahay, S, and Wei, W. “Everything is changing, but I am not alone”: nurses’ perceptions of social support during COVID-19. Sustain For. (2022) 14:3262. doi: 10.3390/su14063262
49. Jiang, J, and Luo, D. The Relationship between Perceived Social Support and Social in College Students: The Mediation of Sense of Coherence. SHS web of conferences (2021) 123:01006. doi: 10.1051/shsconf/202112301006
Keywords: resilience, sense of coherence, social support, nurse, COVID-19, Iran
Citation: Rohani C, Ahmadi M, Seyedtabib M and Mehdipoorkorani L (2025) Exploring the relationship between resilience, sense of coherence, and social support in a sample of nurses during the spread of COVID-19: a mediation analysis study. Front. Public Health. 12:1451236. doi: 10.3389/fpubh.2024.1451236
Edited by:
Christine Rummel-Kluge, Leipzig University, GermanyReviewed by:
Luigi Isaia Lecca, University of Cagliari, ItalyAkiko Kondo, Tokyo Medical and Dental University, Japan
Yunier Broche-Pérez, Universidad Central Marta Abreu de Las Villas, Cuba
Copyright © 2025 Rohani, Ahmadi, Seyedtabib and Mehdipoorkorani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mehrnaz Ahmadi, TWVyLmFobWFkaUBnbWFpbC5jb20=
 Camelia Rohani
Camelia Rohani Mehrnaz Ahmadi
Mehrnaz Ahmadi Maryam Seyedtabib
Maryam Seyedtabib Ladan Mehdipoorkorani5
Ladan Mehdipoorkorani5