- 1Student Research Committee, Nursing Care Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran
- 2Nursing Care Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran
- 3Department of Statistics and Mathematics, Shahid Beheshti University, Tehran, Iran
- 4Student Research Committee, Mazandaran University of Medical Sciences, Ramsar, Iran
- 5Department of Medicine, Islamic Azad University Tonekabon Branch, Tonekabon, Iran
Background: Identifying the hidden and pervasive phenomenon of burnout among family caregivers of older adults with chronic disease requires the use of a valid and reliable tool tailored to the cultural structure of the target community. Therefore, the present study aimed to design and psychometrically evaluate the family caregivers burnout inventory (FCBI) of older adults with chronic disease.
Methods: This research is a sequential exploratory mixed-methods study focused on instrument design, conducted in Iran in 2024. The study employed classical theory, involving three stages to create a valid instrument: item design using inductive (semi-structured face-to-face interviews with 13 caregivers) and deductive (literature review) methods, tool design, and tool evaluation using face validity, content validity, construct validity [exploratory factor analysis (EFA) (N = 297) and confirmatory factor analysis (297 participants)], convergent validity, and reliability (internal consistency and stability). Data were analyzed using AMOS version 24 and SPSS version 26.
Results: Based on qualitative findings, participant quotes, and item adoption from other studies, a pool of 228 items was designed using a 5-point Likert scale (always to never). After several stages of review by the research team, 102 items remained. Following face validity (2 items), content validity (46 items), and construct validity (23 items due to factor loadings less than 0.4 and cross-loadings), 71 items were eliminated, leaving 31 items. EFA results indicated that the family caregiver’s burnout construct of older adults with chronic diseases comprises six factors include; “neurosis,” “feeling victimized,” “extreme fatigue and helplessness,” “neglect or abuse of self and others,” “adaptation deficiency” and “emotional separation” explaining 52.93% of the total variance. The fit indices showed acceptable model fit with the data. In this study, composite reliability and average variance extracted (AVE) for the six factors were greater than 0.7 and 0.5, respectively, and the (AVE) for each factor was higher than the composite reliability. Cronbach’s alpha coefficient for the entire scale was 0.975, and there was a significant correlation between test and retest scores (p < 0.001).
Conclusion: FCBI demonstrates suitable validity and reliability and can be used in various settings by health service providers to identify symptoms of burnout in family caregivers.
Background
Older adults, due to their life conditions and the aging process, are susceptible to various chronic diseases, including high blood pressure, diabetes, heart diseases, and numerous psychological disorders, which significantly impact economic, social, and cultural aspects (1). Most of them face multiple chronic conditions, meaning they suffer from two or more chronic diseases, a phenomenon that has increased among adults worldwide over the past 20 years (2). Between 55 to 98% of the older adults are dealing with such conditions (3). This group of older adults, due to their multiple chronic conditions, must frequently visit health service providers for diagnostic services or follow-up treatments. Many of them have a low quality of life or are hospitalized due to medical needs. Older adults with chronic diseases, due to the development of care needs in various health dimensions, may face challenges in self-care interventions across different aspects of their personal and social lives. These individuals often suffer from physical and psychological problems, leading to further complexity in self-care (3, 4). Therefore, many of them require assistance from formal and informal caregivers to meet their growing needs in various health dimensions (5). Existing research evidence shows that the older adults generally prefer to receive home care, which aligns with government programs to delegate caregiving responsibilities to families at home (6, 7).
The complexity of care required for older adults with chronic diseases necessitates a shift beyond acute care to long-term home care (8). Nowadays, the formal medical role has shifted from healthcare professionals such as nurses and doctors to family caregivers. Family caregivers are responsible for providing most caregiving tasks, ranging from personal care to medical care, for older adults with chronic diseases (6). These caregivers face a wide range of demands over a prolonged caregiving period, indicative of chronic stress (9). They encounter various pressures, such as assisting patients with daily living activities, managing multiple appointments with healthcare specialists in different locations, helping the older adults adhere to multiple and complex medication regimens, and dealing with changes in their roles and responsibilities (10). Consequently, these individuals experience caregiving-related burden and live under stressful conditions, which has become a growing concern (7). Research indicates that caregivers experience an excessive prevalence of stress-related emotional burdens, limitations in social/recreational activities, decreased appetite and sleep, and an increased risk of mortality and psychological disorders compared to non-caregivers (11, 12). Cohen and colleagues note that such caregivers may no longer be able to continue their caregiving role, and if other family members or friends cannot assume the caregiving responsibility or if there is no support from formal or informal care systems, they may face burnout syndrome (13).
Burnout syndrome can manifest in two forms: psychological (low self-esteem, fatigue, anxiety, hopelessness, lack of concentration, and clinical manifestations such as headaches, insomnia, pain, and gastrointestinal issues) and behavioral (caffeine consumption) (14). The emergence of some burnout symptoms may interfere with the quality of care and lead to early or repeated hospitalization of the older adults. It may also result in social isolation, living under prolonged stressful conditions, increased biological vulnerability, a higher risk of developing psychological disorders, and an increased incidence of physical problems in caregivers (such as high blood pressure, increased stress-related hormones, immune system suppression, severe depression, and fatigue) (15, 16). Therefore, developing and implementing programs for caregivers can lead to high-quality care and reduce caregiving outcomes such as caregiving burden and burnout (17), thereby facilitating continuous care. Achieving this goal can be obtained through evidence-based data (18).
Since caregivers accompany the older adults to appointments with healthcare providers, including geriatric nurses, nurses play a key role in identifying caregiver burnout and can help prevent this phenomenon by evaluating and providing sufficient support to caregivers. Using valid and reliable tools to identify the symptoms and signs of burnout syndrome in informal caregivers of patients with chronic diseases can facilitate timely interventions by nurses and other healthcare providers to assist informal caregivers (19). Existing tools primarily focus on caregiver burden and do not specifically address the various aspects of caregiver burnout. These tools may be insufficient for accurately and comprehensively identifying burnout symptoms in family caregivers. Informal (family) caregivers work in environments and conditions that differ from formal work settings. Currently, screening for burnout syndrome is conducted using several tools, some of which are widely used in research. These tools include the Maslach Burnout Inventory (MBI) (20), Pines’ Burnout Measure (BM) (21), Psychologist Burnout Inventory (PBI) (22), Oldenburg Burnout Inventory (OLBI) (23), burnout potential inventory (24), Granada Burnout Questionnaire (25), Copenhagen Burnout Inventory (CBI) (26), Informal Caregiver Burnout Inventory (ICBI) (27), and the Informal Caregiver Burnout Scale (ICBS) (28).
The results of a systematic review (2021) that examined the psychometric indicators of burnout tools across 6,541 studies showed that 15 studies used the MBI to measure burnout. In contrast, BM, PBI, OLBI, and CBI were each used in only one study. The findings indicated that the OLBI had the most comprehensive validity, followed by the CBI, MBI, BM, and PBI. When examining the precision of these tools in interpreting results, the greatest discrepancies were observed for the MBI (27%), BM (25%), and CBI (17%). No discrepancies were found for the PBI and OLBI. The quality of evidence for content validity and psychometric properties was moderate for the OLBI and CBI. However, for the MBI, BM, and PBI, these indices were reported as very low (29).
Additionally, it should be noted that all these tools, except for the ICBI (27) and the ICBS (28), were designed to measure occupational burnout among formal caregivers or health team members. These tools primarily focus on occupational and workplace aspects within healthcare service delivery systems, and none of the mentioned tools specifically measure the burnout construct in family caregivers. Although these tools, especially the MBI, have been used in numerous studies to measure burnout among family caregivers of the older adults (15, 30–32), their results do not seem to have the necessary validity. Perhaps the most prominent difference between informal and formal caregiving lies in the environment and organizational structure. Formal employment involves workplace factors such as colleagues, supervisors, support units, corporate guidelines, agreed working hours, contracts, holidays, and even days off or sick leave. These factors do not directly impact the structure of caregiver burnout. Therefore, a specialized tool is necessary to measure burnout among informal caregivers (27). Although the ICBI and the ICBS are designed to measure the burnout construct among family caregivers, both are unidimensional and cannot comprehensively measure the dimensions of family caregiver burnout. Moreover, attention to the health of family caregivers has become one of the priorities of research projects worldwide to achieve this goal (33). To this end, designing culturally appropriate tools based on standard instrument development protocols to measure various health dimensions by researchers has seen significant growth (34). They usually do not benefit from organizational supports such as vacations, insurance, and colleague support, which can lead to increased stress and burnout.
Objectives
Therefore, designing an appropriate tool to identify and manage caregiver burnout can help improve the quality of life for both caregivers and patients. To develop and implement supportive and intervention programs to reduce caregiver burnout, accurate and reliable data is needed. Existing tools may not fully and accurately provide the necessary information. Designing a new and specific tool can help collect better and more precise data. Existing tools may not fully align with the culture and social conditions of the target country. Designing a localized tool can help better and more accurately identify caregiver burnout in family caregivers. Due to the lack of access to a comprehensive and specific tool for measuring the burnout construct among family caregivers, the researchers in this study aimed to design and psychometrically evaluate the family caregivers burnout inventory (FCBI) of older adults with chronic disease.
Materials and methods
Study design, participants, and procedure
The present research is a sequential exploratory mixed-methods study focused on instrument design, where the researchers collect and analyze data using both qualitative and quantitative approaches (35). In this study, the researchers first collected and analyzed qualitative data and then used the information obtained to determine how to collect the quantitative data in the subsequent stage. The study population consisted of all family caregivers of older adults with chronic diseases. Sampling was conducted in two stages: qualitative sampling using purposive sampling and quantitative sampling using convenience sampling.
The researcher visited the health information management units of hospitals affiliated with Babol University of Medical Sciences, Iran, and compiled a list of older adults with chronic diseases admitted to various departments, including CCU, internal medicine, gastroenterology, cardiology, infectious diseases, orthopedics, kidney transplantation, dialysis, neurology, hematology, and rheumatology. Additionally, the researcher obtained a list of older adults attending the associated clinics. The researcher then explained the research objectives to the caregivers who were present as patient companions in the hospitals and clinics. After assessing the inclusion criteria and obtaining consent, the researcher collected their phone numbers and provided them with the research tools via social media for completion. The inclusion criteria were: being the primary caregiver for the patient for at least 1 year, being 18 years or older, being a first-time caregiver, having access to the internet and a smartphone, and being a relative of the patient by blood or marriage. The exclusion criteria were the unwillingness to continue participating in the research or failure to complete the online questionnaire.
Steps in designing and psychometric evaluation of the FCBI of older adults with chronic disease
Most tools used in nursing research are developed based on classical test theory; hence, this study also utilized this theory. There are three stages in creating a valid instrument: item design, tool design, and tool evaluation (36).
Item design
This stage involves the creation of unique items. Two approaches exist for item creation: inductive and deductive. Instrument designers must decide which of these two methods is more appropriate for their study (37). In this study, to design the FCBI of older adults with chronic Disease, both themes identified from the qualitative study and reviews of existing literature and tools were used to ensure the designed tool comprehensively covers the dimensions of family caregiver burnout.
Qualitative stage/inductive method
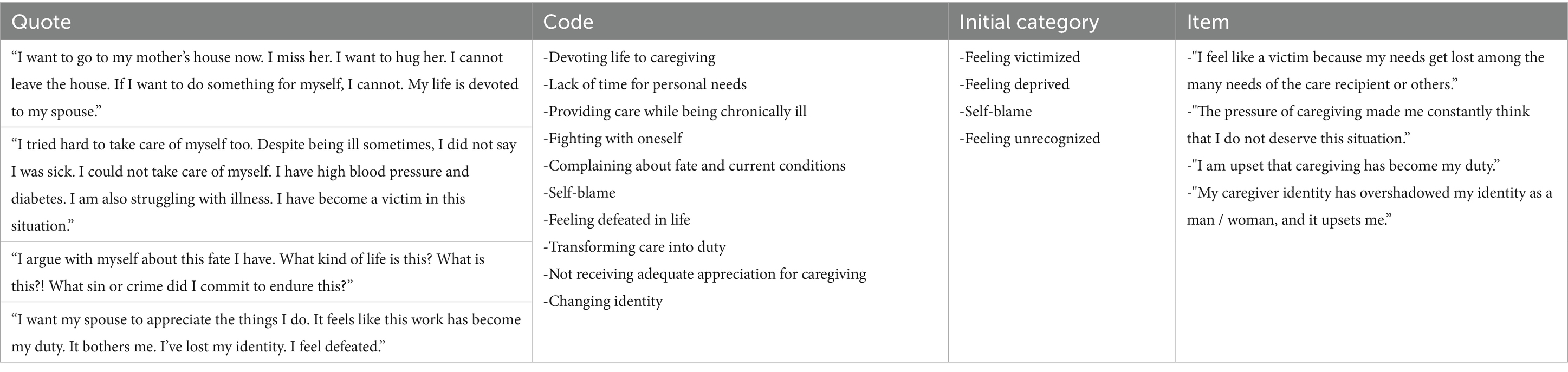
The interviews were coded by the research team. The analyses were conducted manually, and used conventional content analysis for data analysis. In this stage, a qualitative content analysis with a conventional approach was used. Qualitative content analysis allows researchers to interpret the authenticity and truthfulness of data subjectively but scientifically (38, 39). Data collection in this study was conducted through individual, semi-structured, and in-depth interviews. The interview questions were developed based on a review of the literature and the initial experiences and feedback from the caregivers. The number of 13 caregivers was chosen due to data saturation. The interviews were conducted by an expert (the corresponding author) using in-depth, face-to-face interviews to collect data until saturation was reached. Before starting the interview, the interviwer introduced themselves and explained the study’s objectives to the participant. Then, the interview began by establishing rapport and gaining the participant’s trust. At the beginning of each interview, questions such as “Please introduce yourself” and “How are you?” were asked to create interaction between the researcher and the participant, aiding in trust-building and starting the interview. Subsequent questions were asked based on the interview guide, including questions like “Please tell me about your experience in caring for a patient with a chronic disease,” “What challenges did you face while providing care?” and “What were the physical, mental, emotional, and social outcomes for you as a caregiver of a patient with a chronic disease?” Additionally, as needed, exploratory questions such as “What do you mean?” and “Could you please explain to me more?” or “How did you feel about this?” were used during the interviews. At the end of each interview, participants were asked if they had any additional comments and were informed about the possibility of future interviews. All participants provided their phone numbers so follow-up interviews could be scheduled if necessary or for verifying their statements after transcription. A total of 13 in-depth individual interviews were conducted with 13 participants, with each session lasting between 35 to 72 min. For qualitative data analysis, a conventional qualitative content analysis method was used. The interviews were coded by the research team. The analyses were conducted manually, and used conventional content analysis for data analysis. To achieve accurate and reliable information, a systematic and transparent seven-step process suggested by Graneheim and Lundman (40) was employed for data processing. The qualitative content analysis process included, the preparing the data, coding the text, reviewing codes against the text,categorizing and developing categories based on similarities and appropriateness, reviewing categories and comparing them again with the data to ensure the robustness of the codes, identifying themes through careful and thorough reflection and comparing them with each other and reporting the findings. An example of the item design process is presented in Table 1.
Ensuring validity and accuracy of qualitative findings
In this study, Lincoln and Guba’s parallel criteria were used to ensure the validity and accuracy of the qualitative findings: credibility, dependability, transferability, and confirmability (41). Several measures were taken to enhance credibility, including purposeful sampling with maximum diversity (selecting participants with varying occupations, genders, ages, number of children, durations of caregiving and relationships with the older adult), collecting sufficient data, selecting appropriate meaning units, explaining how categories and themes were formed, allocating sufficient time for data collection, and continuous and iterative engagement with the data. Additionally, the findings were checked with the participants. For this purpose, the transcriptions of some participants’ interviews were returned to them after coding to verify whether the codes assigned by the researcher matched their intended meanings. In some cases, participants indicated that their intended meaning differed from the researcher’s interpretation, and the codes were revised accordingly. Seeking consensus within the research team and conducting external audit reviews were also employed to control the credibility of the data. The researcher (first author) made an effort to ask all participants questions within the same domains during the interviews. All individual interviews were recorded and transcribed verbatim. The researcher’s decisions and activities regarding data collection and analysis were fully and continuously documented. Additionally, initial codes derived from participants’ experiences, examples of how themes were extracted, and excerpts from interviews for each theme were provided. An audit trail was also employed to ensure dependability. The researcher endeavored to minimize the influence of their assumptions in the data collection and analysis process.
Literature review/deductive method
For the design of the items in this study, relevant articles were reviewed using various databases and scientific search engines, including Scopus, PubMed, Proquest, Iranmedex, Elsevier, and Medlib. The search was conducted using the burnout in informal caregivers, burnout in family caregivers, caregivers burnout questionnaire, caregivers burnout scale, caregivers burnout list, caregiver burnout tool, older adults with chronic diseases, informal caregivers burnout inventory and informal caregivers burden experience keywords without time restrictions.
Instrument design
In this stage, the researcher needs to employ a set of items determined for the construct or constructs of the instrument and evaluate how well these items meet the expectations of the instrument’s structure (36). When designing an instrument, items are generated for respondents to answer. These responses are then converted into numerical form and statistically analyzed (42). Hence, the number of items in each scale and the length of the scale affect the quality of the responses (36). When designing a new measurement instrument, it is essential to determine the type of scale and response format to be used (42). In social sciences, the Likert format is the most common scale used for designing attitudinal scales (43). In the instrument designed for the present study, a five-point Likert scale ranging from “always” to “never” was used. The pilot study indicated that this number of options increased respondent accuracy and the receipt of genuine responses. In this tool, the option “always” was scored five, and “never” was scored one. The pilot testing of the instrument involved multiple readings of the items by the researcher, asking family caregivers to read the items in the presence of the researcher to identify any unclear items or words (10 participants in the face validity stage), and requesting feedback from the experts participating in the psychometric panel (10 participants). Throughout the psychometric process, the researcher consistently revised and improved the items. The initial instrument, along with questions related to demographic information, consisted of 16 and 54 items, respectively. Efforts were made to ensure that the items were as straightforward and clear as possible, with an estimated completion time of 10 to 15 min.
Instrument evaluation
To determine the psychometric properties of the FCBI of older adults with Chronic Disease, face validity, content validity, construct validity, and reliability were assessed.
Face validity
In this study, both qualitative and quantitative methods were used to determine face validity. In the qualitative method, the items were initially presented to 10 experts (faculty members in nursing, clinical psychology, and psychiatry), who were asked to comment on the difficulty level, relevance, and ambiguity of the items. Subsequently, quantitative face validity was evaluated using the item impact method. For this purpose, 10 experts (the same individuals invited for qualitative face validity assessment) were asked to rate the importance of each item based on their experiences using a five-point Likert scale (from “very important” to “not important at all”) (44).
Content validity
Content validity in this study was assessed using both qualitative and quantitative methods. For qualitative content validity, the same 10 experts (who were also involved in the face validity assessment) were asked to provide feedback on the grammar, appropriateness of wording, and placement of items. The research team reviewed their feedback and made the necessary revisions. For quantitative content validity, the content validity ratio (CVR) and content validity index (CVI) were calculated (44).
Content validity ratio (CVR)
To calculate the CVR, 10 experts were asked to rate each item on a three-point scale (not necessary to necessary) in terms of its necessity. According to Lawshe’s table, a score of 0.62 or higher was considered the criterion for retaining an item (45). The result obtained was compared with the criterion value in Lawshe’s table (0.62) (46) based on the number of the experts (47). If the obtained value was greater than the table value, it indicated that the item was statistically significantly necessary for the questionnaire (p < 0.05) (45). In this study, the CVRstrict method was used, meaning that only items deemed necessary were included in the CVR calculation formula (48). The CVR was calculated using the following formula:
Where ne is the number of experts who rated the item as essential, and N is the total number of experts. The CVR value ranges from −1 to +1. A CVR < 0 indicates that fewer than half of the experts believe the item is essential. A CVR of 0 means exactly 50% of the experts consider the item essential, and a CVR > 0 means more than 50% of the experts find the item essential (49).
Content validity index (CVI)
To evaluate the content validity index, experts were asked to assess each item on a four-point Likert scale for relevance, clarity, and simplicity. Experts rated the relevance of each item from 1 “not relevant,” 2 “somewhat relevant,” 3 “relevant,” and 4 “completely relevant.” Simplicity was rated as 1 “not simple,” 2 “somewhat simple,” 3 “simple,” and 4 “completely simple.” Clarity was rated similarly: 1 “not clear,” 2 “somewhat clear,” 3 “clear,” and 4 “completely clear” (50). An item was accepted if it achieved a CVI score higher than 0.79 (51).
Construct validity
In this study, construct validity was assessed using both exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). A sample of 596 participants were used for constant validity (297 participants for EFA and 297 other participants for CFA).
Exploratory factor analysis (EFA)
To explore the internal relationship between variables and identify clusters of variables with the highest correlations, EFA was conducted using the maximum likelihood (ML) method (52). Before extracting the factors, the Kaiser-Meyer-Olkin (KMO) test for sample adequacy and Bartlett’s test of sphericity were used to ensure that the items were suitable for principal component analysis (53). A sample of 297 participants was used for EFA.
Confirmatory factor analysis (CFA)
In CFA, the researcher specifies the number of factors, the variables that reflect these factors, and whether the factors are related (54). A descriptive cross-sectional study was conducted on a sample of 297 participants to perform CFA.
After examining the correlations between factors and identifying the factors in the first-order CFA, second-order CFA was conducted using structural equation modeling to confirm whether the identified factors constituted the construct of family caregiver burnout and to determine the contribution of these factors to the construct.
Data distribution, outliers, and missing data
Univariate and multivariate data distributions were examined separately to check for normal distribution and outliers. Multivariate outliers were identified using Mahalanobis distance (p < 0.001) and multivariate skewness was examined using Mardia’s coefficient (above 20) (55). The percentage of missing data was assessed using multiple imputation and then replaced with the mean response of participants.
Reliability
In this study, internal consistency and test–retest reliability were used:
Internal consistency
To evaluate the internal consistency of the family caregiver burnout construct, Cronbach’s alpha coefficients, McDonald’s omega, and composite reliability were used (56). Construct reliability or internal consistency of factors serves as an alternative to Cronbach’s alpha coefficient in structural equation modeling analysis (55).
Test–retest reliability
To determine the stability of the instrument, 28 family caregivers were asked to complete the final instrument twice, with a two-week interval between each completion. The intraclass correlation coefficient was calculated for all dimensions and for the entire instrument. An intraclass correlation coefficient of at least 0.4 was considered acceptable (57).
Convergent validity
After fitting the structural model, convergent validity of the family caregiver burnout construct was evaluated using Fornell and Larcker’s (58) criteria, composite reliability (CR), and average variance extracted (AVE). Convergent validity is achieved when the items of a construct correlate highly with each other and represent their respective construct. For convergent validity to be established, AVE > 0.5, CR > 0.7, and CR > AVE must be met (58).
Invariance testing
In this study, to test the invariance (equivalence) of the factor structure of family caregiver burnout by gender, a series of confirmatory factor analysis methods were used. First, the six-factor model was fitted separately for each gender group (male and female), and then a baseline measurement model without equality constraints was created for both groups. Invariance was tested using the chi-square difference test (Δχ2) and the comparative fit index (ΔCFI) (59). Measurement invariance was then assessed to determine the gender invariance of the six-factor structure of family caregiver burnout (60).
Standard error of measurement
The standard error of measurement is an indicator of the precision and reliability of the instrument. Due to the presence of error in repeated measurements, there is always some degree of variation (61). In this study, the standard error of measurement was also evaluated as a crucial psychometric property of the instrument. A lower standard error of measurement is important because clinically significant changes should be above the standard error of measurement (62). Additionally, the agreement parameter of the instrument was assessed by considering the smallest detectable change (SDC) and the minimal clinically important difference (MCID). The agreement parameter is positive if the SDC is greater than the MCID, indicating that the change is real and not due to measurement error (62).
Ceiling and floor effects
Ceiling and floor effects occur when more than 15% of respondents achieve the highest or lowest possible score, respectively. The presence of ceiling and floor effects indicates that the instrument may not include items representing the maximum and minimum intensity of the phenomenon, suggesting inadequate content validity (63).
Validity of the mixed-methods study
To ensure the validity of the mixed-methods study, the researcher addressed threats during data collection by using different participants in the qualitative and quantitative stages, ensuring that none of the qualitative study participants participated in the secondary quantitative study. Additionally, an adequate sample size was used in the qualitative phase, and a larger sample size was employed in the quantitative phase. To mitigate threats during data analysis, the instrument was designed based on themes and major categories extracted, and all processes during both the design and validation phases were meticulously conducted by the researcher and reviewed by advisors. To address potential threats during data interpretation, the researcher avoided comparing qualitative results with quantitative results directly but rather linked them. Following typical exploratory design procedures, the quantitative study was built on the qualitative study, and during data interpretation, qualitative data were interpreted first, followed by the interpretation of quantitative data.
Statistical analysis
To examine EFA and perform statistical tests related to the research hypotheses, SPSS version 26 was used. For validating the construct of family caregiver burnout, CFA using first and second-order maximum likelihood estimation was conducted using AMOS version 24. Multiple fit indices were employed to assess the model fit, including the chi-square to degrees of freedom ratio (χ2/df), the Parsimonious Normed Fit Index (PNFI), the Comparative Fit Index (CFI), the Parsimonious Comparative Fit Index (PCFI), the Incremental Fit Index (IFI), the Goodness of Fit Index (GFI), and the Root Mean Square Error of Approximation (RMSEA) (59). Convergent validity was evaluated using Fornell and Larcker’s criteria (1981) (58). To confirm the number of factors extracted in the EFA, parallel analysis was used. Additionally, to validate the six-factor structure of this scale, a novel network analysis approach using the R software was employed.
Ethics approval and consent to participate
Ethical considerations in this study included obtaining approval from the Ethics Committee of Babol University of Medical Sciences (Code: IR.MUBABOL.HRI.REC.1400.115), obtaining permission for audio recording, explaining the objectives and methodology to participants, securing written informed consent, informing participants of their right to withdraw at any stage of the research, adhering to the principle of non-maleficence, maintaining confidentiality and anonymity of participant information, and offering to share the research results with participants if they wished.
Results
Descriptive statistics
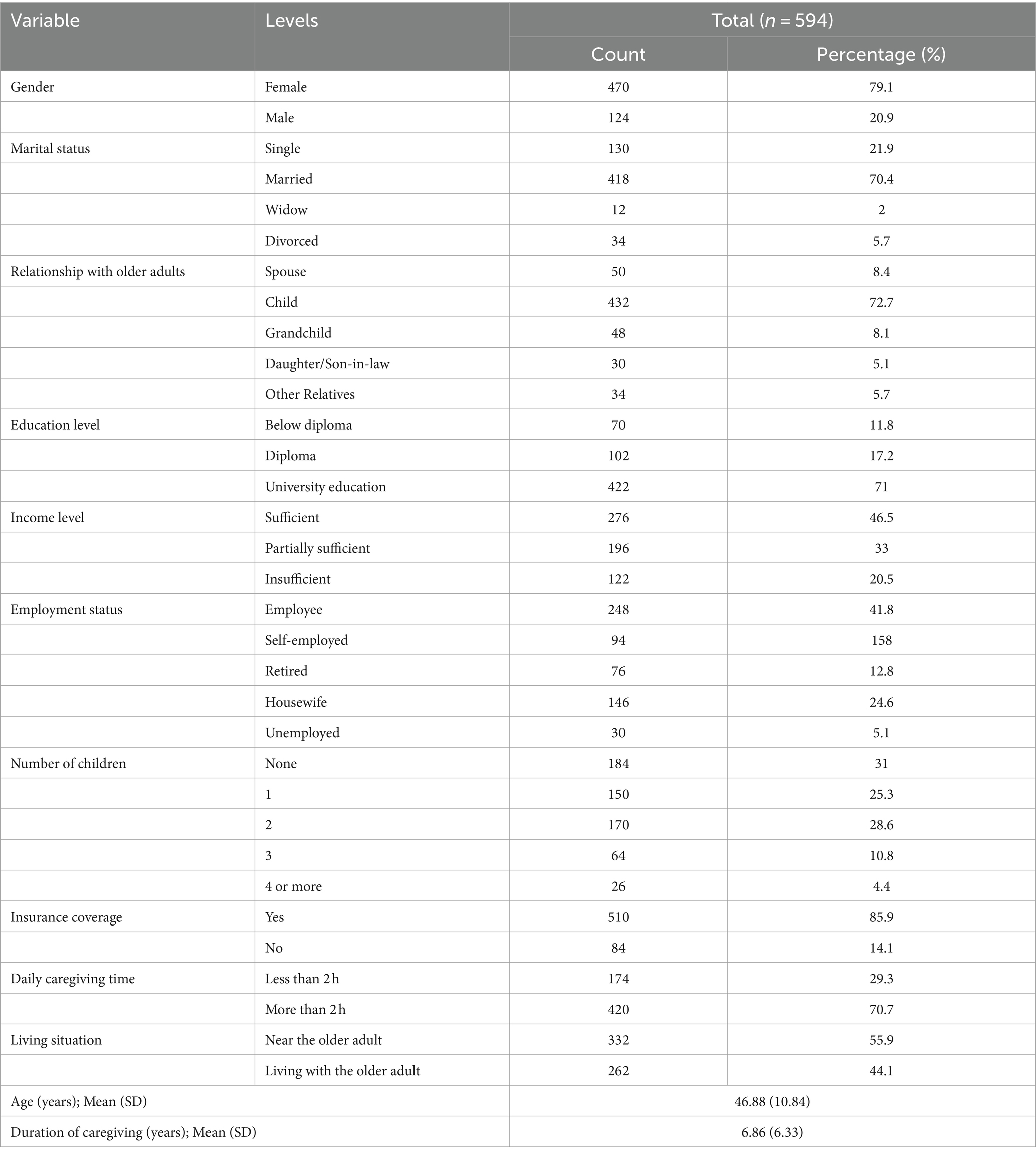
In this study, 594 caregivers of the older adults, with a mean age of 46.88 ± 10.84 years (age range: 21–80 years), were examined. Additionally, the mean duration of caregiving was 6.86 ± 6.33 years (range: 1–40 years). Other demographic variables of the participants are presented in Table 2.
Results of designing items for the FCBI of older adults with chronic disease
Qualitative results
The qualitative analysis resulted in 199 codes, 17 initial categories, and six final categories. Based on findings from interviews with family caregivers, literature reviews, and tools related to occupational burnout, a pool of 228 items (29 items derived from the literature review and 199 from the qualitative analysis) was developed using a 5-point Likert scale (always, often, sometimes, rarely, and never). After several rounds of review by the research team, 126 items were deleted or merged, and the remaining 102 items proceeded to the psychometric evaluation stage.
Quantitative results
Face and content validity
At this stage, all participant feedback on the appearance of the items was considered. In the quantitative face validity assessment, two items, “Life has dealt me a bad hand” and “My marital life has collapsed” were deleted due to scores below 1.5, resulting in a 100-item tool for the next phase. During the qualitative content validity review, some items were merged, and proposed changes to the appearance of items were made. Ultimately, the tool was reduced to 60 items. During the content validity ratio assessment, four items, “I’m stuck in the ‘if only’ and ‘maybe’“, “I blame myself,” “I’m upset with myself and look for my weaknesses,” and “I’m ashamed and embarrassed by the care recipient’s behavior” were removed due to scores below 0.62 and numerical judgments below 1.5, reducing the tool to 56 items. In the content validity index assessment, two items, “I’m on alert” and “I’m embarrassed by others’ disgusted looks” were removed due to scores below 0.7. Finally, the FCBI of older adults with chronic disease, consisting of 54 items, proceeded to the construct validity assessment stage.
Ease of use of the FCBI of older adults with chronic disease
The average time to complete the FCBI of older adults with chronic disease was 8 min (range 6–12 min). The non-response rate for all items was 0 %.
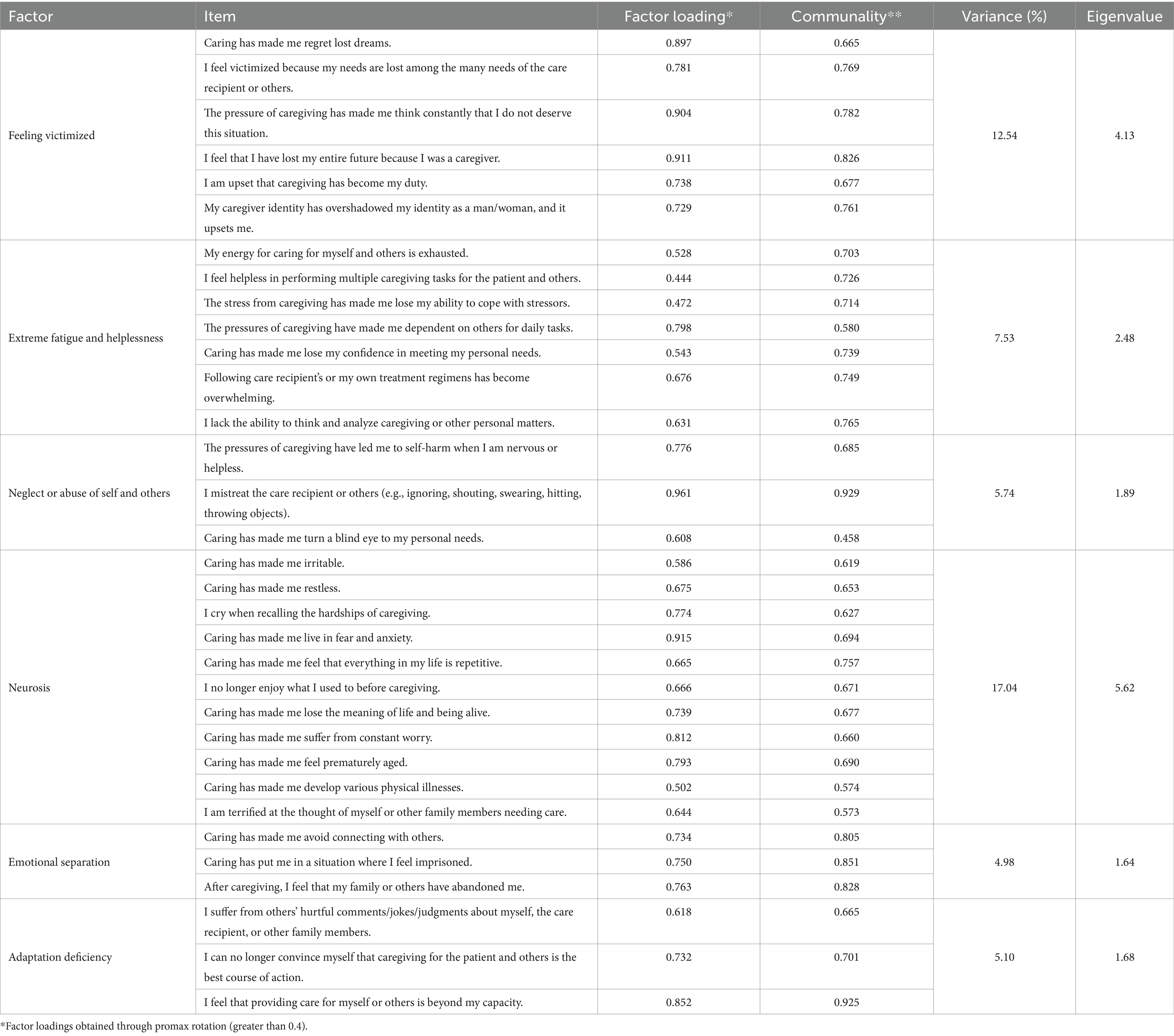
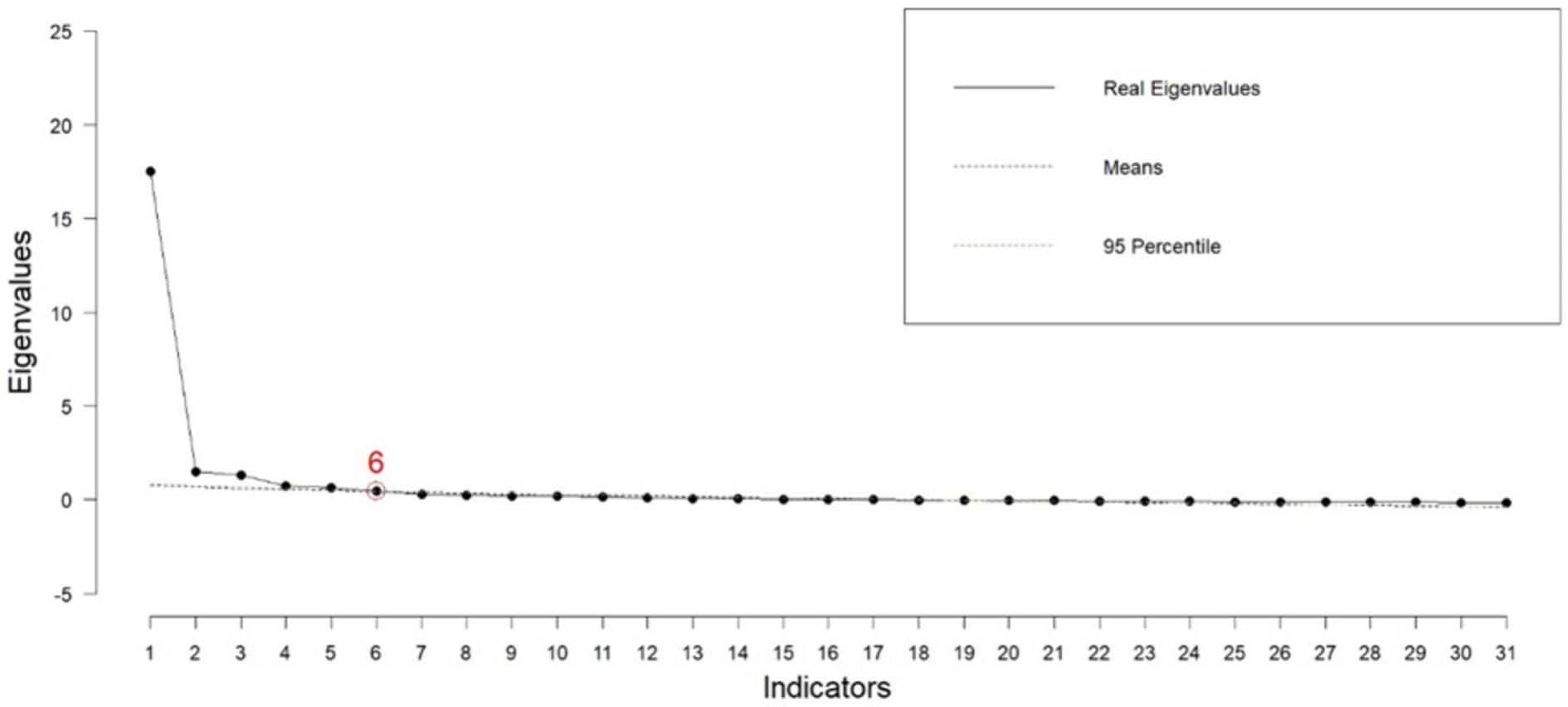
Construct validity
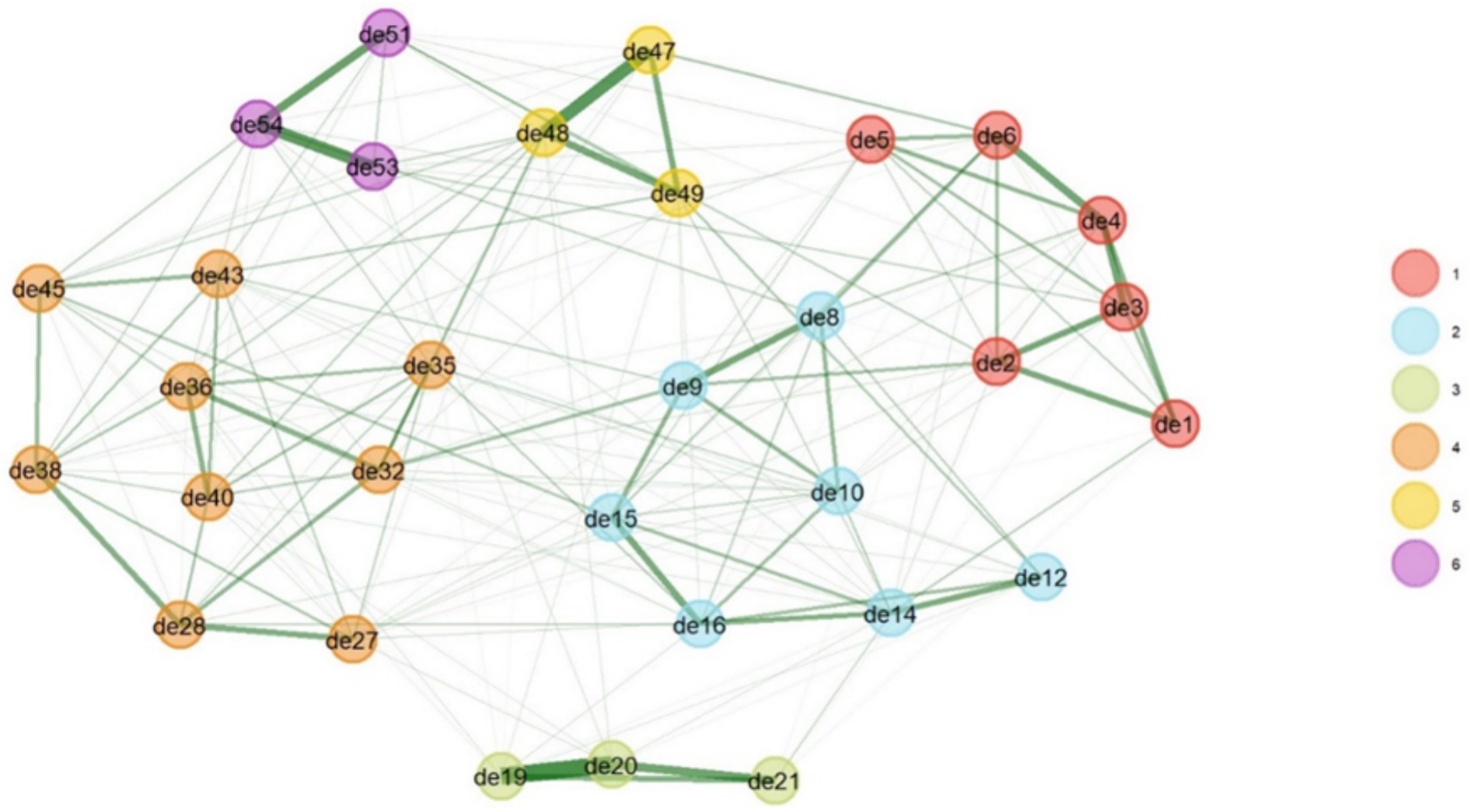
The results of the exploratory factor analysis indicated that the sample size for factor analysis was adequate, with a KMO value of 0.965, suggesting the data were sufficient for analysis. The Bartlett’s test result (p < 0.001, x2 = 9440.56) was significant, indicating sufficient correlations between items to justify factor analysis. The exploratory factor analysis of the FCBI revealed six factors: neurosis, feeling victimized, extreme fatigue and helplessness, neglect or abuse of self and others, adaptation deficiency, and emotional separation. These six latent factors explained 17.04, 12.54, 7.53, 5.74, 5.10, and 4.98% of the variance, respectively, accounting for a total of 52.93% of the variance in the FCBI. Twenty-three items were excluded from the analysis due to factor loadings below 0.4 and cross-loadings (see Table 3 and Figure 1).
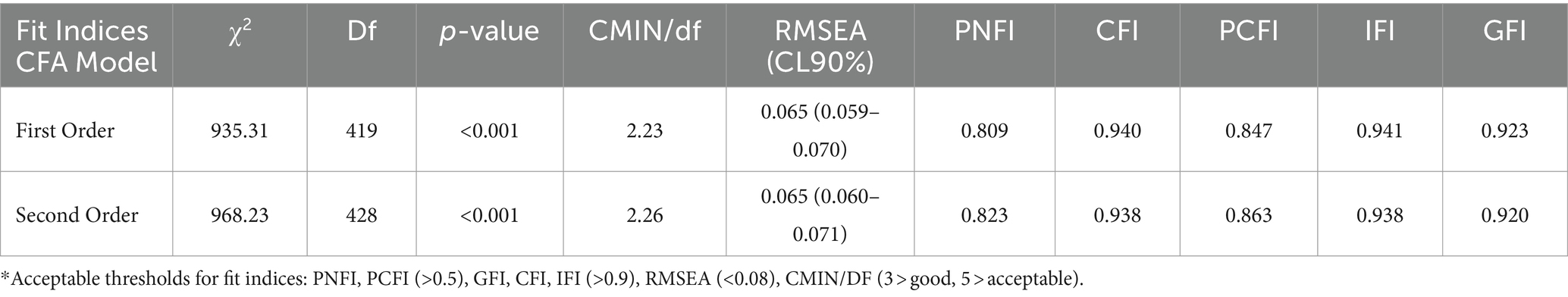
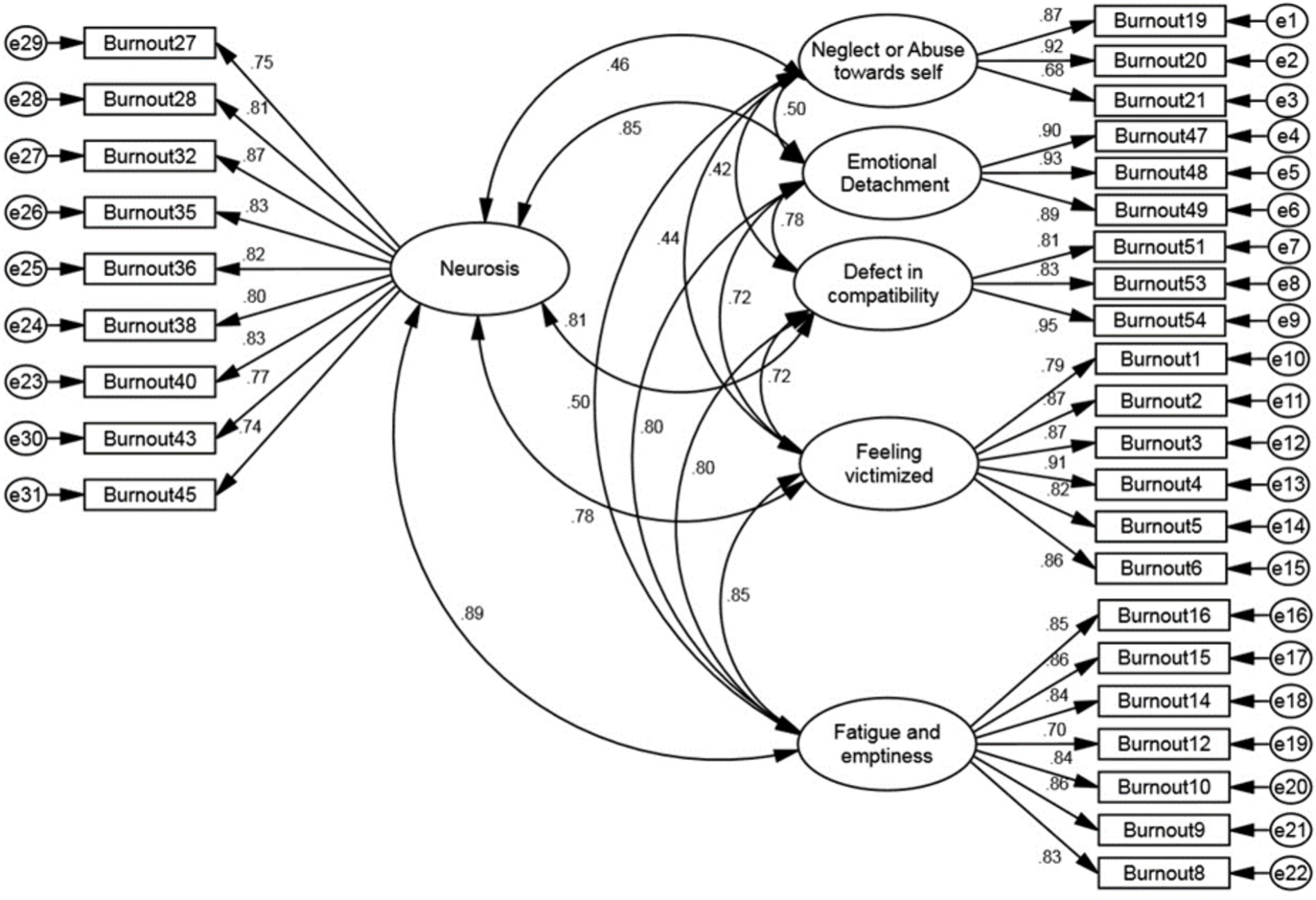
The results of the CFA indicated that all fit indices—PCFI = 0.847, PNFI = 0.809, CMIN/DF = 2.23, RMSEA = 0.065, IFI = 0.941, CFI = 0.940, and GFI = 0.923—confirmed the model’s good fit. Therefore, the six-factor model of the FCBI was validated (Table 4). The standardized factor loadings between items and factors in the first-order factor analysis showed that all factor loadings in the model were above 0.4 (Figure 2).
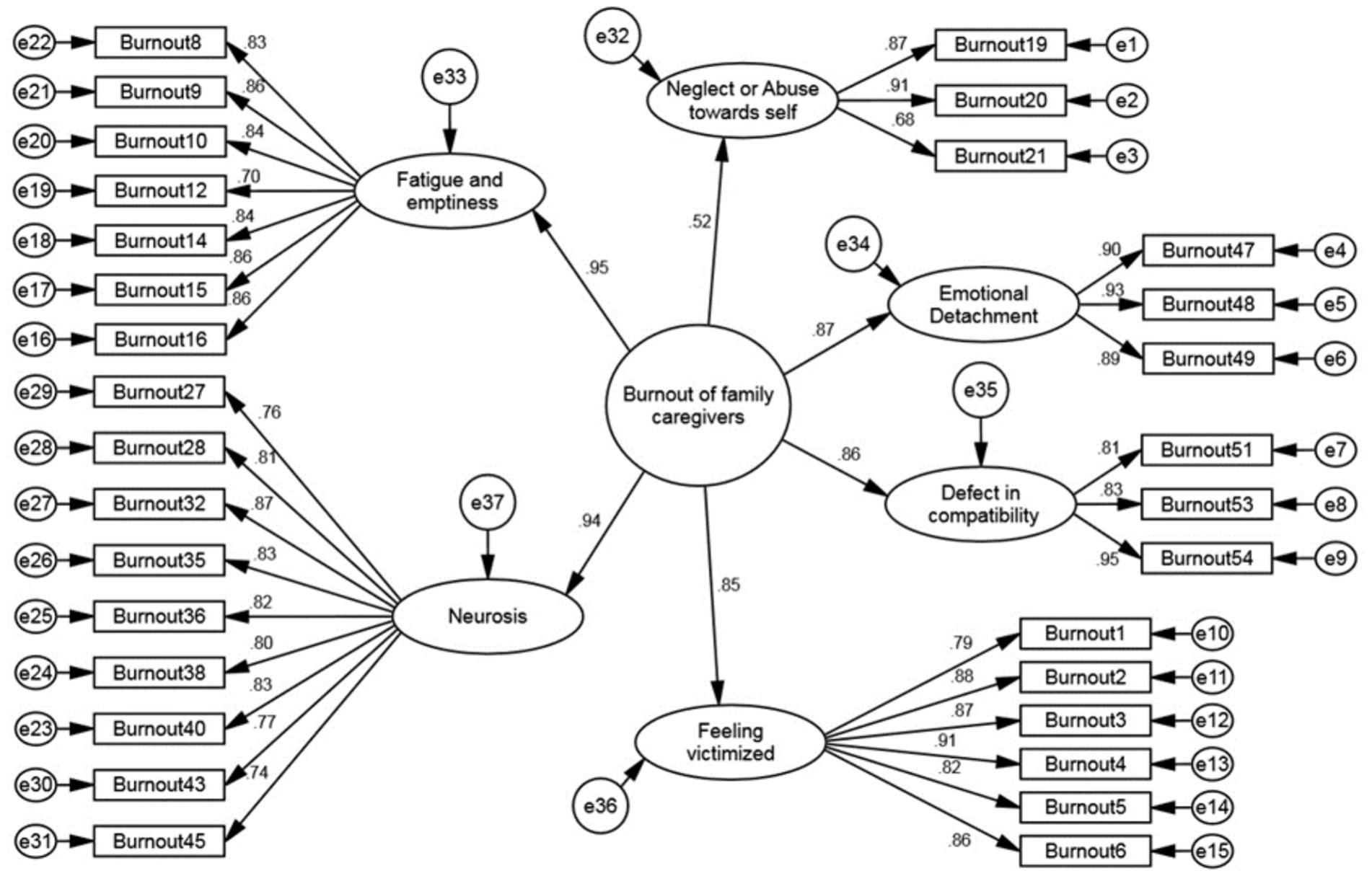
In the second-order confirmatory factor analysis, the fit indices indicated an acceptable fit of the proposed model with the data (Table 4). The correlation values between the factors of the FCBI indicated weak to moderate correlations between the factors, suggesting that the factors are divergent from one another (Figure 3).
The results of the first-order confirmatory factor analysis showed that the AVE values for the six factors of the FCBI were all greater than 0.5 and at an acceptable level. Additionally, the CR values for each factor were greater than their respective AVE values. These results indicate that the FCBI has good convergent validity (Table 5).
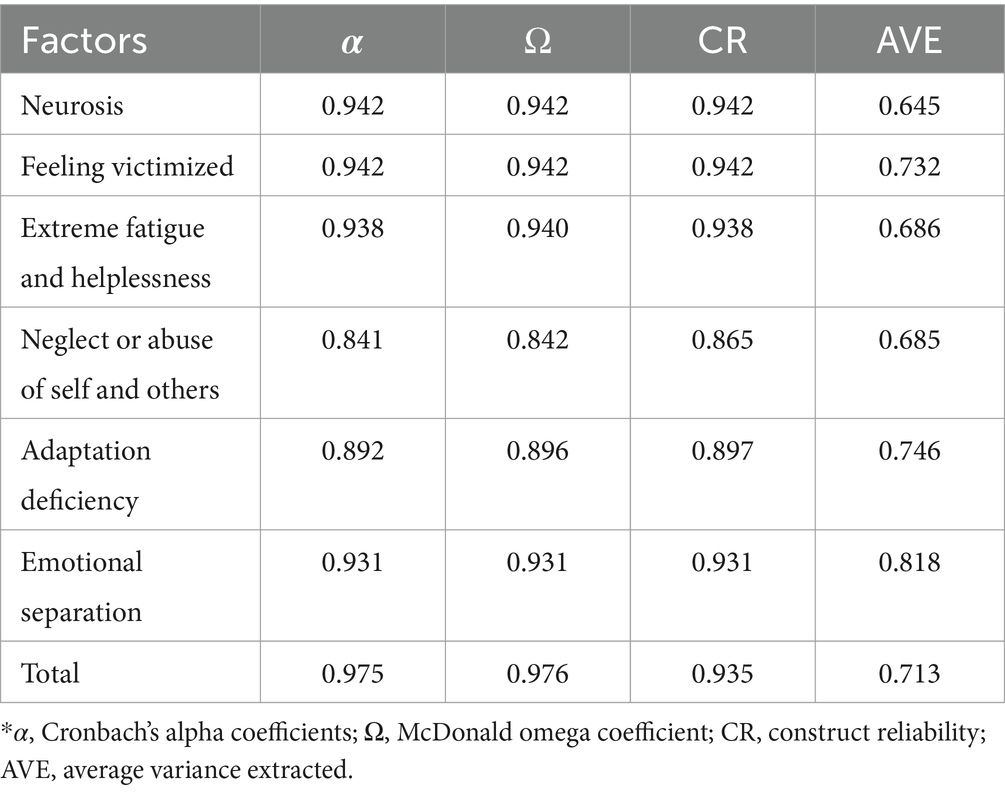
Table 5. Convergent validity, internal consistency, and stability of the family caregiver burnout construct.
Reliability
The results of internal consistency for the family caregiver burnout construct showed that the internal stability of the factors was greater than 0.7 (Table 5).
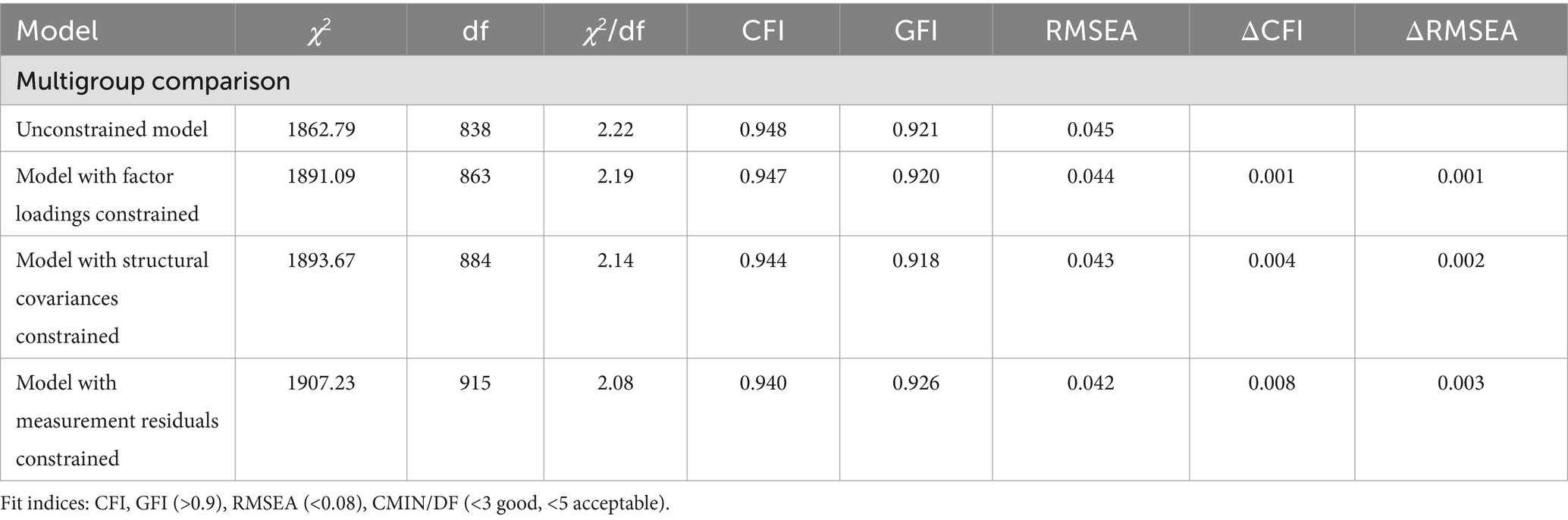
Invariance testing
The fit indices for the model separated by gender indicated that the six-factor model had an acceptable fit in each gender group (Table 6).
Network analysis
Network analysis estimated the six-factor structure of the family caregiver burnout construct. All item dimensions were similar to the findings of the exploratory factor analysis, as shown in Figure 1. Based on the bootstrap test and 95% confidence interval with a standard error of 0.063, the median of the six dimensions was obtained (Figure 4).
Scoring the FCBI of older adults with chronic disease
The FCBI uses a Likert scale ranging from one to five (Always = 5, Often = 4, Sometimes = 3, Rarely = 2, Never = 1). The score range is from 31 to 155. A score of 1 to 31 indicates no burnout, 32 to 73 indicates mild burnout, 74 to 114 indicates moderate burnout, and 115 to 155 indicates severe burnout.
Discussion
This exploratory mixed-methods research aimed to design and psychometrically evaluate the FCBI of patients with chronic disease and consisted of two sequential qualitative and quantitative phases. In sequential mixed-methods approaches, qualitative and quantitative data are interconnected (64). In the present study, a Likert scale ranging from one to five was used to score the FCBI of patients with chronic disease. The frequency-based Likert scale was deemed the most suitable for assessing family caregiver burnout, as the intensity may vary across different items (65). The nature of Likert scales is generally considered ordinal (66). Items based on the Likert scale can be three, four, five, six, or seven options, with the five-point scale being the most optimal (66).
In the quantitative face validity assessment, the impact score of each item was calculated. This method involves using respondents’ feedback to reduce and eliminate unsuitable items and to determine the importance of each item (67). Qualitative content validity was evaluated with the assistance of 10 experts familiar with the instrument’s constructs through the calculation of the CVR and CVI. Many researchers recommend using 10 or more experts for content validity assessment (68, 69). Subsequently, quantitative content validity was assessed using both the CVR and CVI methods with the same experts. Although many studies only mention qualitative content validity assessment (45), it is important to note that this approach is not methodologically flawless. Therefore, it is recommended that content validity be calculated quantitatively based on experts’ opinions using both CVR and CVI indices (70, 71).
In this study, construct validity was assessed using exploratory and confirmatory factor analysis. Factor analysis, which identifies the dimensions of an instrument, is part of construct validity, referred to as structural validity by Mokkink and colleagues (72). Before conducting the EFA, the correlations between items were examined to determine whether the instrument was unidimensional or multidimensional. This dimensionality was then confirmed through CFA (63). Once the subscales were identified, internal consistency for each subscale was calculated. An internal consistency between 0.7 and 0.9 is considered appropriate (73). Before extracting factors, the KMO test and Bartlett’s test of sphericity were performed to ensure sample adequacy and verify that the items were suitable for principal component analysis (74). The results indicated that the sample size for factor analysis was excellent, and Bartlett’s test was significant, confirming sufficient correlations between items for factor analysis. KMO values between 0.7 and 0.8 are considered good, and values between 0.8 and 1 are considered excellent (75).
In this study, EFA and CFA were each conducted with a sample of 297 participants (total 594 participants). Sample size is crucial in factor analysis, with a minimum of 100 participants generally recommended (59). Hatcher and O’Rourke (76) recommend at least five samples per item. According to some researchers, a sample size of 200 to 300 is sufficient for factor analysis (77, 78). Costello and colleagues suggest the best approach to determine sample size is the sample-to-item ratio, recommending 10 to 20 samples per item (79). EFA was performed using principal component analysis and varimax rotation. Collecting data online minimized missing data, which were then addressed using multiple imputation and replaced with the mean response of participants. Another important consideration during factor analysis is the acceptable level of communalities and the variance explained by each factor and the total variance explained (80). The type of rotation used should also be specified, as rotation simplifies and clarifies the structure (79). In this study, after confirming sample adequacy, the number of factors was determined using scree plot and eigenvalue methods. The results showed that the family caregiver burnout construct comprised six factors: “neurosis,” “feeling victimized,” “extreme fatigue and helplessness,” “neglect or abuse of self and others,” “adaptation deficiency” and “emotional separation” which together explained 52.93% of the total variance in the family caregiver burnout construct. At this stage, 23 items were excluded due to factor loadings below 0.4 and cross-loadings, resulting in a final 31-item instrument.
First factor: feeling victimized
This factor comprises six items that measure the caregiver’s feelings about the outcomes of caregiving, such as regret, feeling victimized, having no future, and losing identity. This factor accounts for the largest percentage of variance. In the MBI, the item “At the end of a workday, I feel like I’ve been used up” also measures feeling victimized (81). To explain this finding, it can be stated that many family caregivers claim they face two primary responsibilities: their personal lives and caregiving for the older adults. Consequently, caregiving can disrupt their personal and professional plans. Often, they prioritize the needs of the care recipient over their own, leading to disruptions in their daily routines and loss of personal goals. This issue is more prevalent when caring for older adults with Alzheimer’s, dementia, or stroke, which require more demanding and time-consuming care (82). Peacock et al. (10) described this situation as “life on hold” for caregivers, as they have to take leave, request job transfers, or even leave their jobs. Faronbi et al. (83) stated that caregiving prevents caregivers from attending daily or family events and fulfilling other personal responsibilities. Additionally, they are in a state of compulsion, often lacking enough time to spend with their families or to pursue career advancements. This state of compulsion fosters feelings of victimization. Feeling victimized reduces acceptance and adjustment to the caregiver role. Caregivers, in fact, become hidden patients who, due to their caregiving responsibilities, may be unable or unwilling to take care of their own health needs (84). Goodman and Punoos refer to long-term family caregivers as the “second victim” and the families of individuals with chronic disease as the “potential patient” (85).
Second factor: extreme fatigue and helplessness
This factor includes seven items and measures feelings of instability, feelings of helplessness, excessive fatigue, and dependency on others for making caregiving decisions and performing daily life activities. One of the items in the Tamarana et al. (28) ICBS is “I feel tired when I spend time caring for the recipient”. In the 10-item ICBI by James Nicholas, this factor ranked third in terms of factor loading (0.809), with six items measuring fatigue in informal caregivers: “I always feel tired,” “I feel emotionally drained,” “I feel physically drained,” “Caregiving is physically exhausting,” “Caregiving is emotionally exhausting” and “I feel burned out from caregiving” (27). The 17-item OLBI also includes an eight-item dimension that measures fatigue (86). The MBI identifies this factor as one of the critical dimensions for measuring burnout (81).
Third factor: neglect or abuse of self and others
This factor includes three items and measures neglect and abuse toward oneself and the care recipient. One of the items in the Tamarana et al. (28) ICBS is “I get angry at the care recipient’s demands” which is used to measure symptoms of burnout. Abuse by caregivers can be physical, financial, sexual, emotional, or psychological. In older adults, psychological abuse is more prevalent and includes emotional mistreatment, verbal abuse, deprivation of contact, humiliation, blaming, and controlling behavior by the caregiver. It also includes intentional or unintentional neglect, financial exploitation, and abandonment (87). The study by Ashrafzadeh et al. (88) found that burnout is associated with symptoms such as failure to follow the treatment regimen carefully, leaving the patient alone at home, verbal aggression in response to repeated questions, neglecting personal hygiene protocols, abandoning the patient, and not paying adequate attention to the needs of the patient under their care.
Fourth factor: neurosis
This factor includes 11 items and measures the psychological and physical consequences of caregiving. One of the items in the James Nicholas ICBI is “I often feel hopeless” (27). Two items in the Tamarana et al. (28) ICBS include “My physical health has deteriorated because of caregiving responsibilities” and “My sleep is affected by my caregiving responsibilities” which also measure symptoms of neurosis in caregiver burnout. To explain this finding, it can be said that the majority of older adults with chronic diseases, especially those with Alzheimer’s, are cared for at home. The burden of caring for such patients particularly falls on relatives who try to support and care for them (89). This is why these caregivers are often referred to as “hidden patients” (90), as providing care for an older adult, vulnerable person can expose the caregiver to negative physical, emotional, and social consequences (89). Caregivers frequently struggle with a world of worries, fears, and anxieties, along with their internal turmoil, which may inadvertently affect the health of the care recipient as well (91–93).
Fifth factor: emotional separation
This factor includes three items and measures aspects such as ineffective communication and feelings of social isolation. According to numerous studies, burnout is associated with symptoms such as feelings of loneliness, isolation, boredom, and frustration among caregivers (94–98). Caregivers often suffer from emotional loneliness (e.g., lack of intimacy) and social loneliness (e.g., absence of an extensive social network) (99). Generally, social isolation in these individuals occurs in two main dimensions: structural (e.g., infrequent or rare social contacts, limited social interactions, and poor participation in social activities) and functional (e.g., lack of a sense of belonging or dissatisfaction with social relationships), where functional isolation is closely linked with social loneliness (100–102). Social isolation and feelings of loneliness and abandonment have been identified as risk factors for both physical and mental health (103).
Sixth factor: adaptation deficiency
This factor includes three items and measures the consequences of the inability to adapt to caregiving situations, such as addiction, dissatisfaction with life and current conditions, and the inability to care for oneself and others. One of the items in the Tamarana et al. (28) ICBS is “I compromise my responsibilities regarding self-care”. A critical aspect of caregiving often overlooked by caregivers is their coping strategies. These coping strategies, ranging from resilience and optimism to despair and withdrawal from providing care, play a vital role in determining how caregivers adapt to their multiple roles as caregivers. Coping strategies can significantly modulate the level of caregiving burden, either amplifying or mitigating it (104, 105). Notably, the nature and extent of the burden caregivers feel and its consequences, such as burnout, depend on their unique coping strategies, belief systems, and attitudes (91).
After conducting EFA, CFA was performed in this study. The results of the model fit evaluation for the six-factor model of family caregiver burnout showed that all indices confirmed a good fit for the model (59). Among burnout instruments, the MBI and its various versions have been used extensively by researchers for structure, development, and measurement of burnout (26, 106). The MBI is considered the gold standard for measuring occupational burnout (107) and is used in over 90% of studies in the field of burnout syndrome (106). However, this has led to a close link between theory and measurement, ultimately “neglecting other conceptual approaches to burnout” (106). Additionally, the scoring of the three dimensions of this scale in both positive and negative ways has led to artificial clustering of sub factors (108). On the other hand, results from extensive factor analysis on 45 studies using the MBI showed that in addition to the three-factor model by Maslach, empirical data also support alternative models, including two-, four-, or five-factor models or models with higher factors (109).
Although the CBI (26) and the Shirom-Melamed Burnout Measure (SMBM) were developed to address this issue, reducing the burnout tool to a unidimensional structure has been strongly discouraged by several researchers (107, 110, 111). The OLBI was proposed as an alternative to address the content and methodological drawbacks of the aforementioned occupational burnout tools (112, 113). However, the items in these tools are specifically related to work and education and cannot cover burnout caused by caregiving by informal caregivers. Therefore, the ICBI (27) and the ICBS (28) were designed for family caregivers, but both have a unidimensional structure. Hence, there is still a need for a valid and multidimensional tool to measure burnout, especially in different target groups (114).
Given the aforementioned points, the tool designed in the present study (using both deductive and inductive methods) specifically measures the symptoms of burnout among family caregivers of older adults with chronic diseases and comprises six factors, covering the deficiencies present in available tools. The tool designed in this study also has acceptable reliability. The most common method for examining internal consistency is the calculation of Cronbach’s alpha. For multi-option Likert scales, Cronbach’s alpha is used to determine internal consistency (61, 72). In this study, Cronbach’s alpha coefficients, McDonald’s omega, and composite reliability were used to evaluate the internal stability of the family caregiver burnout factors. The results showed that the internal consistency of the burnout construct for family caregivers of older adults with chronic diseases was acceptable. Reliability greater than 0.7 was considered appropriate (60).
The results also showed that the convergent validity of the six factors of the family caregiver burnout construct was at an acceptable level, with high correlations among items within a factor, indicating that they represented their respective constructs well. Thus, this tool has acceptable convergent validity, which is a part of construct validity and helps establish the tool’s credibility (61).
The final tool in this study includes 31 items, with at least three items per factor. There is no specific rule for the number of items that should be extracted. Instruments with fewer items have lower response errors (due to less fatigue among respondents), and the items should represent the intended content. To achieve the desired internal consistency, having at least three items per construct is necessary (37).
This research is the first study to design a domain-specific tool for measuring burnout among family caregivers of older adults with chronic diseases. As such, it provides a foundation for conducting similar studies in different cultures with adequate sample sizes. Although the label of this tool includes the term “older adult” due to the researcher’s focus as a geriatric nursing student, the items are not specific to the older adult group. Therefore, this tool can be used to assess burnout among family caregivers of adult patients with chronic diseases. This study offers a stronger theoretical foundation for research on family caregiver burnout. The use of both inductive and deductive approaches for item design is another strength of the present study. Most designed tools have only focused on assessing the validity of the tool. They have mainly relied on internal consistency and, occasionally, stability, while other aspects of reliability, such as standard error and reproducibility, have been overlooked. In this study, we evaluated most reliability indices. This study also had limitations. For instance, due to limited access to male caregivers in the research environment, we could not include more male caregivers in our study. Divergent validity was not assessed in this study. Completing the tool through self-reporting and the potential impact of the physical, emotional, and psychological state of the participants on their responses to the items is another limitation of the present study. Another limitation relates to the nature of the convenience sampling method used in the construct validity section. The descriptive-cross-sectional study conducted to assess construct validity was performed in a specific geographic area, which may limit the generalizability of the results. The use of online data collection methods might affect the validity of the data, as those with access to the internet may not be representative of the general population of family caregivers of older adults with chronic diseases.
Conclusion
The results showed that the FCBI has acceptable validity and reliability. It consists of 31 items for assessing burnout among family caregivers and includes 16 demographic items, totaling 47 items. Consequently, it takes approximately 6 to 12 min to complete. In designing this tool, efforts were made to ensure both appropriate content validity and a manageable number of items so that its use would not be time-consuming or exhausting for nurses and other healthcare providers. The items of this tool have been revised at various stages based on the feedback from experts and users, resulting in items that are understandable and acceptable to healthcare providers and users. Therefore, this tool can be used as an easy-to-respond, straightforward, and appropriately itemized instrument for measuring burnout among family caregivers. It is recommended to use this tool during follow-up visits in clinical centers or home visits in the community by healthcare providers, especially nurses.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical considerations in this study included obtaining approval from the Ethics Committee of Babol University of Medical Sciences (Code: IR.MUBABOL.HRI.REC.1400.115), obtaining permission for audio recording, explaining the objectives and methodology to participants, securing written informed consent, informing participants of their right to withdraw at any stage of the research, adhering to the principle of nonmaleficence, maintaining confidentiality and anonymity of participant information, and offering to share the research results with participants if they wished.
Author contributions
KF: Conceptualization, Writing – original draft, Writing – review & editing, Data curation. AS: Investigation, Validation, Writing – review & editing. MK: Formal analysis, Software, Writing – review & editing, Methodology. KS: Investigation, Validation, Writing – review & editing. RE: Investigation, Validation, Writing – review & editing. FG: Conceptualization, Data curation, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Babol University of Medical Sciences.
Acknowledgments
We are grateful to all the family caregivers who shared their experiences with us and collaborated as participants in the quantitative phase of our study. We also thank the experts for their cooperation and assistance in enhancing the quality of our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
FCBI, Family caregivers burnout inventory; EFA, Exploratory factor analysis; AVE, Average variance extracted; MBI, Maslach Burnout Inventory; BM, Pines' Burnout Measure; PBI, Psychologist Burnout Inventory; OLBI, Oldenburg Burnout Inventory; CBI, Copenhagen Burnout Inventory; ICBI, Informal Caregiver Burnout Inventory; ICBS, Informal Caregiver Burnout Scale; CVR, Content validity ratio; CVI, Content validity index; EFA, Exploratory factor analysis; CFA, Confirmatory factor analysis; ML, Maximum likelihood; KMO, Kaiser-Meyer-Olkin; AVE, Average variance extracted; Δχ2, Chi-square difference test; ΔCFI, Comparative fit index; SDC, Smallest detectable change; MCID, Minimal clinically important difference; χ2/df, Chi-square to degrees of freedom ratio; PNFI, Parsimonious Normed Fit Index; CFI, Comparative Fit Index; PCFI, Parsimonious Comparative Fit Index; IFI, Incremental Fit Index; GFI, Goodness of Fit Index; RMSEA, Root Mean Square Error of Approximation.
References
1. Maresova, P, Javanmardi, E, Barakovic, S, Barakovic Husic, J, Tomsone, S, Krejcar, O, et al. Consequences of chronic diseases and other limitations associated with old age -a scoping review. BMC public health. (2019). 19: 1–7. Available at: https://doi.org/10.1186/s12889-019-7762-5
2. Ploeg, J, Matthew-Maich, N, Fraser, K, Dufour, S, McAiney, C, Kaasalainen, S, et al. Managing multiple chronic conditions in the community: a Canadian qualitative study of the experiences of older adults, family caregivers and healthcare providers. BMC Geriatr. (2017) 17:1–15. doi: 10.1186/s12877-017-0431-6
3. Poduri, K, and Vanushkina, M. Epidemiology of aging, disability, frailty and overall role of physiatry. Geriatric rehabilitation (1st Edn.). Elsevier. (2018). 1–17.
4. Ploeg, J, Canesi, M, Fraser, KD, McAiney, C, Kaasalainen, S, Markle-Reid, M, et al. Experiences of community-dwelling older adults living with multiple chronic conditions: a qualitative study. BMJ Open. (2019) 9:e023345. doi: 10.1136/bmjopen-2018-023345
5. Malmir, S, Navipour, H, and Negarandeh, R. Exploring challenges among Iranian family caregivers of seniors with multiple chronic conditions: a qualitative research study. BMC Geriatr. (2022) 22:1–12. doi: 10.1186/s12877-022-02881-3
6. Panagioti, M, Stokes, J, Esmail, A, Coventry, P, Cheraghi-Sohi, S, Alam, R, et al. Multimorbidity and patient safety incidents in primary care: a systematic review and meta-analysis. PLoS One. (2015) 10:e0135947. doi: 10.1371/journal.pone.0135947
7. Williams, A, Sethi, B, Duggleby, W, Ploeg, J, Markle-Reid, M, Peacock, S, et al. A Canadian qualitative study exploring the diversity of the experience of family caregivers of older adults with multiple chronic conditions using a social location perspective. Int J Equity Health. (2016) 15:1–16. doi: 10.1186/s12939-016-0328-6
8. Kogan, AC, Wilber, K, and Mosqueda, L. Person-centered care for older adults with chronic conditions and functional impairment: a systematic literature review. JAGS. (2016) 64:e1–7. doi: 10.1111/jgs.13873
9. Vitaliano, PP, Strachan, E, Dansie, E, Goldberg, J, and Buchwald, D. Does caregiving cause psychological distress? The case for familial and genetic vulnerabilities in female twins. Ann Behav Med. (2014) 47:198–207. doi: 10.1007/s12160-013-9538-y
10. Peacock, S, Sethi, B, Williams, A, Duggleby, W, Bayly, M, Swindle, J, et al. Older adult spouses with multiple chronic conditions: challenges, rewards, and coping strategies. CJA/RCV. (2017) 36:209–22. doi: 10.1017/S0714980817000095
11. Morris, SM, King, C, Turner, M, and Payne, S. Family carers providing support to a person dying in the home setting: a narrative literature review. Palliat Med. (2015) 29:487–95. doi: 10.1177/0269216314565706
12. Cheng, S-T . Dementia caregiver burden: a research update and critical analysis. Curr Psychiatry Rep. (2017) 19:1–8 doi: 10.1007/s11920-017-0818-2
13. Cohen-Mansfield, J, and Wirtz, PW. The reasons for nursing home entry in an adult day care population: caregiver reports versus regression results. J Geriatr Psychiatry Neurol. (2009) 22:274–81. doi: 10.1177/0891988709335799
14. Valente, L, Truzzi, A, Souza, WF, Alves, GS, Sudo, FK, Alves, CEO, et al. Autopercepção de saúde em cuidadores familiares e o tipo de demência: resultados preliminares de uma amostra ambulatorial. Rev Bras Neurol. (2013) 49:13–9.
15. Alves, LCS, Monteiro, DQ, Bento, SR, Hayashi, VD, Pelegrini, LNC, and Vale, FAC. Burnout syndrome in informal caregivers of older adults with dementia: a systematic review. Dement Neuropsychol. (2019) 13:415–21. doi: 10.1590/1980-57642018dn13-040008
16. Otero, LMR . Burnout syndrome in family caregivers of dependentes. Int J Asian Soc Sci. (2016) 6:12–20. doi: 10.18488/journal.1/2016.6.1/1.1.12.20
17. Kaymaz, TT, and Ozdemir, L. Effects of aromatherapy on agitation and related caregiver burden in patients with moderate to severe dementia: a pilot study. Geriatr Nurs. (2017) 38:231–7.
18. Nichols, E, Steinmetz, JD, Vollset, SE, Fukutaki, K, Chalek, J, Abd-Allah, F, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the global burden of disease study 2019. Lancet Public Health. (2022) 7:e105–25. doi: 10.1002/alz.051496
19. Cooper, E . Staff education on identifying burden and burnout in family caregivers. [dissertation/master’s thesis]. Minneapolis, MN, USA: Walden University (2021).
20. Maslach, C, and Jackson, SE. The measurement of experienced burnout. J Organ Behav. (1981) 2:99–113.
21. Malach-Pines, A . The burnout measure, short version. Int J Stress Manag. (2005) 12:78. doi: 10.1037/1072-5245.12.1.78
22. Ackerley, GD, Burnell, J, Holder, DC, and Kurdek, LA. Burnout among licensed psychologists. Psychol: Res Pract. (1988) 19:624
23. Demerouti, E, Bakker, AB, Nachreiner, F, and Schaufeli, WB. The job demands-resources model of burnout. J Appl Psychol. (2001) 86:499. doi: 10.1037//0021-9010.86.3.499
24. Potter, BA . Overcoming job burnout: How to renew enthusiasm for work. Springer Nature, Switzerland, AG: Ronin Publishing (2009). doi: 10.1007/978-3-031-25233-4
25. de la Fuente, EI, Lozano, LM, García-Cueto, E, San Luis, C, Vargas, C, Cañadas, GR, et al. Development and validation of the Granada burnout questionnaire in Spanish police. IJCHP. (2013) 13:216–25. doi: 10.1016/s1697-2600(13)70026-7
26. Kristensen, TS, Borritz, M, Villadsen, E, and Christensen, KB. The Copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. (2005) 19:192–207. doi: 10.1080/02678370500297720
27. James, N. Rethinking burnout in informal caregivers: Development and validation of the informal caregiver burnout Inventory-10 item form (2020).
28. Tamarana, R, Jain, E, Sinha, S, Manjunatha, S, Amissah, AA, and Balaji, B. Development and initial evaluation of informal caregiver burnout scale. IJCNE. (2023) 24:87–91. doi: 10.4103/ijcn.ijcn_83_22
29. Shoman, Y, Marca, S, Bianchi, R, Godderis, L, Van der Molen, H, and Canu, IG. Psychometric properties of burnout measures: a systematic review. Epidemiol Psychiatr Sci. (2021) 30:e8. doi: 10.1017/s2045796020001134
30. El-Nady, MT . Relationship between caregivers' burnout and elderly emotional abuse. Sci Res Essays. (2012) 7:3535–41. doi: 10.5897/SRE11.1256
31. Khalaila, R . Does emotional empathy moderate the association between caregiver burden and burnout among Arab family caregivers of older relatives? Health Soc Care Community. (2022) 30:e2478–88. doi: 10.1111/hsc.13689
32. Valle-Alonso, D, Hernández-López, I, Zúñiga-Vargas, M, and Martínez-Aguilera, P. Overload and burnout among aged informal caregivers. Enferm Univ. (2015) 12:19–27. doi: 10.1016/j.reu.2015.05.004
33. Caputo, J, Pavalko, EK, and Hardy, MA. The long-term effects of caregiving on women's health and mortality. JMF. (2016) 78:1382–98. doi: 10.1111/jomf.12332
34. Boateng, GO, Neilands, TB, Frongillo, EA, Melgar-Quiñonez, HR, and Young, SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. (2018) 6:149. doi: 10.3389/fpubh.2018.00149
35. Creswell, JW, and Clark, VLP. Designing and conducting mixed methods research. Thousand Oaks, California: Sage Publications (2017).
36. Hinklin, TR . A review of scale development practices in the study of organizations. J Manag. (1995) 21:967–88.
37. Hinkin, TR . A brief tutorial on the development of measures for use in survey questionnaires. Organ Res Methods. (1998) 1:104–21.
38. Hsieh, H-F, and Shannon, SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15:1277–88. doi: 10.1177/1049732305276687
40. Graneheim, UH, and Lundman, B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. (2004) 24:105–12. doi: 10.1016/j.nedt.2003.10.001
41. Lincoln, YS, and Guba, EG. Naturalistic inquiry. Newbury Park, California: SAGE Publications (1985).
42. Rattray, J, and Jones, MC. Essential elements of questionnaire design and development. J Clin Nurs. (2007) 16:234–43. doi: 10.1111/j.1365-2702.2006.01573.x
43. Benson, J, and Clark, F. A guide for instrument development and validation. AJOT. (1982) 36:789–800.
44. Ayre, C, and Scally, AJ. Critical values for Lawshe’s content validity ratio: revisiting the original methods of calculation. JMEEP. (2014) 47:79–86. doi: 10.1177/0748175613513808
45. Mohammadbeigi, A, Mohammadsalehi, N, and Aligol, M. Validity and reliability of the instruments and types of measurments in health applied researches. JRUMS. (2015) 13:1153–70. doi: 10.18502/aoh.v3i3.1281
46. Zeraati, M, and Alavi, NM. Designing and validity evaluation of Quality of Nursing Care Scale in Intensive Care Units. J Nurs Meas. (2014) 22:461–71. doi: 10.1891/1061-3749.22.3.461
47. Vakili, MM, and Jahangiri, N. Content validity and reliability of the measurement tools in educational, behavioral, and health sciences research. Med Educ Dev. (2018) 10:106–18. doi: 10.29252/edcj.10.28.106
48. Ghaffari, F, Alipour, A, and Fotokian, Z. The effects of education on nurses' ability to recognize elder abuse induced by family members. NMS. (2020) 9:1–8. doi: 10.4103/nms.nms_29_19
49. Brinkman, W-P. Design of a questionnaire instrument. Handbook of mobile technology research methods: Nova Publishers; (2009). p. 31–57.
50. Polit, DF, Beck, CT, and Owen, SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. RINAH. (2007) 30:459–67. doi: 10.1002/nur.20199
51. Polit, DF, and Beck, CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. RINAH. (2006) 29:489–97. doi: 10.1002/nur.20147
52. Fabrigar, LRWD, MacCallum, RC, and Strahan, EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods. (1999) 4:272.
53. Sullivan, JJ, Pett, MA, and Lackey, NR. Making sense of factor analysis, the use of factor analysis for instrument development in health care research. California: Sage (2003).
54. Thompson, B . Exploratory and confirmatory factor analysis: Understanding concepts and applications. United Kingdom: American Psychological Association (2004).
55. Vinzi, VE, Chin, WW, Henseler, J, and Wang, H. Handbook of partial least squares. Verlag Berlin: Springer (2010).
56. Javali, SB, Gudaganavar, NV, and Raj, SM. Effect of varying sample size in estimation of coefficients of internal consistency. Webmedcentral. (2011) 2
57. Baumgartner, TA, and Chung, H. Confidence limits for intraclass reliability coefficients. MPEES. (2001) 5:179–88. doi: 10.1207/s15327841mpee0503_4
58. Fornell, CL, and David, F. Evaluating structural equation models with unobservable variables and measurement error. JMR. (1981) 18:39–50.
59. Kline, R . Data preparation and psychometrics review. Principles and practice of structural equation modeling. 4th ed. New York, NY: Guilford (2023).
60. Hair, JF Jr, Sarstedt, M, Hopkins, L, and Kuppelwieser, VG. Partial least squares structural equation modeling (PLS-SEM): an emerging tool in business research. Eur Bus Rev. (2014) 26:106–21. doi: 10.1108/ebr-10-2013-0128
61. Lenz, ER . Measurement in nursing and health research. Germany: Springer Publishing Company (2010).
62. Creswell, JW, and Creswell, JD. Research design: Qualitative, quantitative, and mixed methods approaches. 3rd ed. New York: Sage Publications (2017).
63. Terwee, CB, Bot, SD, de Boer, MR, van der Windt, DA, Knol, DL, Dekker, J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. (2007) 60:34–42. doi: 10.1016/j.jclinepi.2006.03.012
64. Creswell, JW, Klassen, AC, Plano Clark, VL, and Smith, KC. Best practices for mixed methods research in the health sciences. Bethesda, MD: The Office of Behavioral and Social Sciences Research (2011).
65. Bayen, E, Papeix, C, Pradat-Diehl, P, Lubetzki, C, and Joël, M. Patterns of objective and subjective burden of informal caregivers in multiple sclerosis. Behav Neurol. (2015) 2015:648415. doi: 10.1155/2015/648415
67. Ebadi, A, Zarshenas, L, Rakhshan, M, Zareiyan, A, Sharifnia, S, and Mojahedi, M. Principles of scale development in health science. Tehran: Jame-e-negar (2017). 6 p.
68. Hyrkäs, K, Appelqvist-Schmidlechner, K, and Oksa, L. Validating an instrument for clinical supervision using an expert panel. Int J Nurs Stud. (2003) 40:619–25. doi: 10.1016/s0020-7489(03)00036-1
69. Juarez-Hernandez, LG, and Tobón, S. Análisis de los elementos implícitos en la validación de contenido de un instrumento de investigación. Revista espacios. (2018) 39:23–29.
70. DeVon, HA, Block, ME, Moyle-Wright, P, Ernst, DM, Hayden, SJ, Lazzara, DJ, et al. A psychometric toolbox for testing validity and reliability. J Nurs. (2007) 39:155–64. doi: 10.1111/j.1547-5069.2007.00161.x
72. Mokkink, LB, Terwee, CB, Patrick, DL, Alonso, J, Stratford, PW, Knol, DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. (2010) 63:737–45. doi: 10.1016/j.jclinepi.2010.02.006
73. Nunnally, JC, and Bernstein, IH. Psychometric theory. New York: McGraw-Hill Companies, Incorporated (1994).
74. Pett, MA, Lackey, NR, and Sullivan, JJ. Making sense of factor analysis: The use of factor analysis for instrument development in health care researche. Thousand Oaks, California: Sage (2003).
75. Chan, LLIN . Validity and reliability of the instrument using exploratory factor analysis and Cronbach’s alpha. IJ-ARBSS. (2017) 7:400–10. doi: 10.6007/ijarbss/v7-i10/3387
76. Hatcher, L, and O'Rourke, N. A step-by-step approach to using SAS for factor analysis and structural equation modeling. North Carolina, USA: SAS Institute (2013).
77. Plichta, SB, and Kelvin, EA. Munro’s statistical methods for health care research. 6th ed. Philadelphia: Wolters Kluwer, Lippincott Williams & Wilkins, (2013).
78. Munro, BH . Statistical methods for health care research. Philadelphia, USA: Lippincott Williams & Wilkins (2005).
79. Costello, AB, and Osborne, J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. PARE. (2019) 10:7.
80. Henson, RK, and Roberts, JK. Use of exploratory factor analysis in published research: common errors and some comment on improved practice. Educ Psychol Meas. (2006) 66:393–416. doi: 10.1177/0013164405282485
81. Maslach, C, Jackson, SE, and Leiter, MP. Maslach burnout inventory 3rd ed. Palo Alto, California: Consulting Psychologists Press (1997). doi: 10.1177/2235042X20981190
82. Ploeg, J, Garnett, A, Fraser, KD, Baird, LG, Kaasalainen, S, McAiney, C, et al. The complexity of caregiving for community-living older adults with multiple chronic conditions: a qualitative study. J Comorb. (2020) 10:1190.
83. Faronbi, JO, Faronbi, GO, Ayamolowo, SJ, and Olaogun, AA. Caring for the seniors with chronic illness: the lived experience of caregivers of older adults. Arch Gerontol Geriatr. (2019) 82:8–14. doi: 10.1016/j.archger.2019.01.013
84. Mourad, GM, Zaki, RA, and Ali, RA. Improving coping abilities among caregivers of patients with cerebrovascular stroke. J Educ Pract. (2014) 5:8–20.
85. Goodman, CC, and Pynoos, J. A model telephone information and support program for caregivers of Alzheimer's patients. Gerontol. (1990) 30:399–404.
86. Demerouti, E, Mostert, K, and Bakker, AB. Burnout and work engagement: a thorough investigation of the independency of both constructs. J Occup Health Psychol. (2010) 15:209–22. doi: 10.1037/a0019408
87. Mohamed, SEA . Relation between Caregivers' burnout and psychological and verbal abuse for elderly living in geriatric institutions. Egypt J Health Care. (2017) 8:300–14. doi: 10.21608/ejhc.2017.47174
88. Ashrafizadeh, H, Gheibizadeh, M, Rassouli, M, Hajibabaee, F, and Rostami, S. Explain the experience of family caregivers regarding care of Alzheimer's patients: a qualitative study. Front Psychol. (2021) 12:699959. doi: 10.3389/fpsyg.2021.699959
89. Yılmaz, A, Turan, E, and Gundogar, D. Predictors of burnout in the family caregivers of Alzheimer's disease: evidence from Turkey. AJA. (2009) 28:16–21. doi: 10.1111/j.1741-6612.2008.00319.x
90. Fengler, AP, and Goodrich, N. Wives of elderly disabled men: the hidden patients. Gerontologist. (1979) 19:175–83.
91. Özönder Ünal, I, and Ordu, C. Decoding Caregiver Burden in Cancer: Role of Emotional Health, Rumination, and Coping Mechanisms. Healthcare. (2023) 11:2300. Available at: https://www.mdpi.com/2227-9032/11/19/2700/pdf?version=1696852884
92. del-Pino-Casado, R, Priego-Cubero, E, López-Martínez, C, and Orgeta, V. Subjective caregiver burden and anxiety in informal caregivers: a systematic review and meta-analysis. PLoS One. (2021) 16:e0247143. doi: 10.1371/journal.pone.0247143
93. Kaminishi, KS, Safavi, R, and Hirsch, CH. Caregiver burnout. In: CHH Ana Hategan and Caroline Giroux, James A. Bourgeois, editor. Geriatric psychiatry: A case-based textbook. Cham, Switzerland: Springer International Publishing; (2018). p. 691–708.
94. Czekanski, K . CE: original research: the experience of transitioning to a caregiving role for a family member with Alzheimer's disease or related dementia. Am J Nurs. (2017) 117:24–32. doi: 10.1097/01.NAJ.0000524517.60352.84
95. Greenwood, N, Pound, C, Brearley, S, and Smith, R. A qualitative study of older informal carers’ experiences and perceptions of their caring role. Maturitas. (2019) 124:1–7. doi: 10.1016/j.maturitas.2019.03.006
96. Greenwood, N, Pound, C, Smith, R, and Brearley, S. Experiences and support needs of older carers: a focus group study of perceptions from the voluntary and statutory sectors. Maturitas. (2019) 123:40–4. doi: 10.1016/j.maturitas.2019.02.003
97. Vasileiou, K, Barnett, J, Barreto, M, Vines, J, Atkinson, M, Lawson, S, et al. Experiences of loneliness associated with being an informal caregiver: a qualitative investigation. Front Psychol. (2017) 8:585. doi: 10.3389/fpsyg.2017.00585
98. Daly, L, McCarron, M, Higgins, A, and McCallion, P. ‘Sustaining P lace’–a grounded theory of how informal carers of people with dementia manage alterations to relationships within their social worlds. J Clin Nurs. (2013) 22:501–12. doi: 10.1111/jocn.12003
99. Guan, Z, Poon, AWC, and Zwi, A. Social isolation and loneliness in family caregivers of people with severe mental illness: a scoping review. Am J Community Psychol. (2023) 72:443–63. doi: 10.1002/ajcp.12698
100. Leigh-Hunt, N, Bagguley, D, Bash, K, Turner, V, Turnbull, S, Valtorta, N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. (2017) 152:157–71. doi: 10.1016/j.puhe.2017.07.035
101. Johnson, S, Bacsu, J, McIntosh, T, Jeffery, B, and Novik, N. Social isolation and loneliness among immigrant and refugee seniors in Canada: a scoping review. IJMHSC. (2019) 15:177–90. doi: 10.1108/ijmhsc-10-2018-0067
102. Holt-Lunstad, J . The potential public health relevance of social isolation and loneliness: prevalence, epidemiology, and risk factors. Public Policy Aging Rep. (2017) 27:127–30. doi: 10.1093/ppar/prx030
103. Holt-Lunstad, J . Loneliness and social isolation as risk factors: the power of social connection in prevention. AJLM. (2021) 15:567–73. doi: 10.1177/15598276211009454
104. Lovell, B . Predicting potentially harmful psychological and physical behaviours by parental caregivers toward children with autism Spectrum disorder. J Child Fam Stud. (2018) 27:2422–9. doi: 10.1007/s10826-018-1087-3
105. Lyons, AM, Leon, SC, Roecker Phelps, CE, and Dunleavy, AM. The impact of child symptom severity on stress among parents of children with ASD: the moderating role of coping styles. J Child Fam Stud. (2010) 19:516–24. doi: 10.1007/s10826-009-9323-5
106. Shirom, A, and Melamed, S. A comparison of the construct validity of two burnout measures in two groups of professionals. Int J Stress Manag. (2006) 13:176. doi: 10.1037/1072-5245.13.2.176
107. Schaufeli, WB, and Taris, TW. The conceptualization and measurement of burnout: common ground and worlds apart. Work Stress. (2005) 19:256–62. doi: 10.1080/02678370500385913
108. Halbesleben, JR, and Demerouti, E. The construct validity of an alternative measure of burnout: investigating the English translation of the Oldenburg burnout inventory. Work Stress. (2005) 19:208–20. doi: 10.1080/02678370500340728
109. Worley, JA, Vassar, M, Wheeler, DL, and Barnes, LL. Factor structure of scores from the Maslach burnout inventory: a review and meta-analysis of 45 exploratory and confirmatory factor-analytic studies. Educ Psychol Meas. (2008) 68:797–823. doi: 10.1177/0013164408315268
110. Maslach, C, Schaufeli, WB, and Leiter, MP. Job burnout. Annu Rev Psychol. (2001) 52:397–422. doi: 10.1146/annurev.psych.52.1.397
111. Maslach, C, Leiter, M, and Schaufeli, W. Measuring burnout. The Oxford handbook of organizational well-being. New York: Oxford University Press (2008).
112. Demerouti, E, and Nachreiner, F. Zur Spezifität von burnout für dienstleistungsberufe: fakt oder artefakt. Zeitschrift fur Arbeitswissenschaft. (1998) 52:82–9.
113. Demerouti, E, Bakker, AB, Vardakou, I, and Kantas, A. The convergent validity of two burnout instruments: a multitrait-multimethod analysis. EJPA. (2003) 19:12. doi: 10.1027//1015-5759.19.1.12
Keywords: chronic disease, older adults, family caregivers, burnout measurement, psychometric evaluation, informal caregiving
Citation: Farokhmanesh K, Shamsalinia A, Kordbageri MR, Saadati K, Ebrahimi Rad R and Ghaffari F (2024) Design and psychometrics of the family caregivers burnout inventory of older adults with chronic disease. Front. Public Health. 12:1449273. doi: 10.3389/fpubh.2024.1449273
Edited by:
Ivy Yan Zhao, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Gema Pérez-Rojo, CEU San Pablo University, SpainLuis Manuel Mota de Sousa, Universidade Atlântica, Portugal
Copyright © 2024 Farokhmanesh, Shamsalinia, Kordbageri, Saadati, Ebrahimi Rad and Ghaffari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fatemeh Ghaffari, Z2hhZmFyaWZhdGVtZUB5YWhvby5jb20=
†ORCID: Kataneh Farokhmanesh, orcid.org/0000-0002-3010-8667
Abbas Shamsalinia, orcid.org/0000-0003-0731-0215
Mohammad Reza Kordbageri, orcid.org/0000-0002-9901-4423
Kiyana Saadati, orcid.org/0000-0003-2299-6016
Reza Ebrahimi Rad, orcid.org/0000-0002-0269-2683
Fatemeh Ghaffari, orcid.org/0000-0003-1940-1579
 Kataneh Farokhmanesh
Kataneh Farokhmanesh Abbas Shamsalinia
Abbas Shamsalinia Mohammad Reza Kordbageri3†
Mohammad Reza Kordbageri3† Fatemeh Ghaffari
Fatemeh Ghaffari