- 1Department of Public Health Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 2Department of Obstetrics & Gynaecology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 3Department of Psychiatry, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Fear of childbirth (FOC) or tokophobia adversely affects women during pregnancy, delivery, and postpartum. Childbirth fear may differ across regions and cultures. We aimed to identify factors influencing the fear of childbirth among the Asian population. A systematic literature search was performed using the PubMed, Scopus, and Web of Science databases in November 2023. Original articles in English with research conducted in Asian countries were included. The independent factors associated with childbirth fear, from the relevant studies were identified and discussed. Forty-six papers met the eligibility criteria but only 26 studies were discussed in this review. The significant factors were categorized into (1) demographics, (2) clinical, (3) healthcare service, (4) childbirth education & information, and (5) COVID-19 pandemic. The prevalence of childbirth fear among Asians ranged between 56.6 and 84.8%. Significant demographic factors included age, education, marital status, economic status, and area of residence. Greater levels of tokophobia were linked to nulliparity, unplanned pregnancy, infertility, miscarriage, and pregnancies at risk. Effective doctor-patient communication and more frequent antenatal visits were shown to alleviate maternal childbirth fear. There was consistent evidence of prenatal childbirth education’s benefit in reducing FOC. The usage of smartphone apps and prolonged exposure to electronic devices were linked to a higher degree of tokophobia. Nulliparas who received too much pregnancy-related information also reported increased childbirth fear. There was a positive correlation between maternal fear of COVID-19 infection and FOC. Keeping updated with COVID-19 information increased the maternal childbirth fear by two-fold. In conclusion, a stable economy and relationship contribute to lesser childbirth fear among Asian women. Poor maternal health and pregnancy complications were positive predictors of FOC. Health practitioners may reduce maternal childbirth through women’s education, clear communication as well as accurate information and guidance to expectant mothers. Further study is required into the content of childbirth fear among Asian women. These research findings hopefully will lead to the development of culturally adapted screening tools and interventions that reduce the burden of FOC among expectant mothers.
1 Introduction
Pregnancy and childbirth are among the most important events in a woman’s life. Fear of childbirth (FOC) or Tokophobia has been defined as “an unreasoning dread of childbirth,” and further classified into primary (affecting nullipara) and secondary (involving parous women who have experienced birth) (1, 2). A systematic review by O’Connell et al. in 2016 showed that the tokophobia prevalence ranged between 3.7 and 43% with a pooled prevalence of 14% (95%CI 12–16%) (3). Factors including anxious personality, traumatic delivery, previous miscarriages, low social support, and poor partner relationships have been associated with tokophobia (4, 5).
Childbirth fear has been associated with greater use of epidural, prolonged labor, and increased risks of labor dystocia as well as emergency cesarean section (6, 7). Previous studies demonstrated a link between tokophobia with negative birth experiences and post-traumatic stress disorder (PTSD) (4, 5). A negative childbirth experience can lead to dysfunctional maternal–infant bonding and reduced exclusive breastfeeding (8). Negative experiences also carry a greater risk of postpartum depression and negatively impact individual’s attitudes toward future birth, resulting in a maternal request for cesarean delivery (9, 10). Post-partum PTSD adversely affects not only maternal psychological well-being but also the child’s socioemotional and cognitive development (11). Women with low economic status are at greater risk of PTSD and those from developing countries are particularly vulnerable due to healthcare limitations and stigma surrounding mental health (12).
Fear of childbirth is multi-dimensional. Qualitative studies demonstrated that women report various childbirth concerns including maternal and child risk, loss of control, uncertainty, pain, and isolation (13). Understanding FOC in a local cultural context is paramount as women’s perception of childbirth is also strongly influenced by their culture (13).
There has been increasing interest in tokophobia in empirical research and clinical practice over the last 30 years (3). However, the lack of international consensus on the definition and gold standard measurement of tokophobia resulted in significant heterogeneity among the published studies (3). A review by Richens et al. found that a majority of research was conducted in Scandinavia and utilized a range of assessment tools to measure childbirth fear. The authors concluded that the inconsistent instruments used by the various studies were a reflection of the challenges in defining FOC (14).
Standardized tools to assess maternal childbirth fear may be restrictive due to a wide range of cultural backgrounds, alongside different perceptions and beliefs regarding birth (14). The Wijma Delivery Expectancy Questionnaire Part A (WDEQ-A) is the most commonly used diagnostic tool (15). WDEQ-A consists of a 33-item self-assessment questionnaire with a six-point Likert scale response per item, and a score ranging from 0 to 165. WDEQ-A score of ≥85 is indicative of severe fear of childbirth (16). It is a valid and reliable instrument in a variety of populations, while some concerns have been raised about the items’ cross-cultural applicability (17). Previous research demonstrated significant differences in the exploratory factor analyses of the WDEQ-A in European cohorts, suggesting that the content of FOC may differ between countries (18). Lukasse et al. demonstrated that FOC consisted of six factors, i.e., Lack of self-efficacy, Loneliness, Negative appraisal, Lack of positive anticipation, Fear, and Concern for the child. The prominence of each component varied across nations. For example, Icelandic women expressed the least lack of self-efficacy and recorded the lowest score for the fear component. Danish women had the least expectations of being lonely, while Belgian mothers scored the highest for the factor (18).
The majority of studies on tokophobia are conducted in developed countries from Europe, Scandinavia, and North America (19). As birth is a multifaceted experience, it is natural for childbirth fear to differ across regions or cultures (17). Recognizing the factors associated with tokophobia is essential in planning and providing an effective intervention to lessen its burden on expectant mothers. Our study aims to identify the factors which influence maternal childbirth fear among pregnant women in Asia. We hope that the findings will improve the understanding of FOC among Asian women and encourage more culturally adapted research on tokophobia.
2 Materials and methods
2.1 Literature search
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for scoping review (20). We performed a literature search on electronic databases (PubMed, Scopus, and Web of Science) using the following search string; (childbirth fear OR “tokophobia” OR “prenatal fear”) AND (risk OR pred* or “risk factor”). The search frame was from the inception of the databases until September 2023.
Original articles in English and from Asian countries, with the following features, were included: (1) studies assessing childbirth fear as the main outcome; (2) childbirth fear assessment during the antepartum period or labor; (3) FOC was measured using a validated scale, and not as a subdomain of a larger assessment tool. We also included all cross-sectional and cohort studies alongside meta-analysis and systematic reviews to identify relevant studies. Articles with the following characteristics were excluded: (1) conference abstracts, letters or commentary, editorial and book chapters; (2) studies involving Asian immigrants in non-Asian countries or Asian-Americans; (3) studies conducted in the postpartum period; (4) qualitative or intervention study.
Endnote (version 20.6, Clarivate, United States) was utilized to organize the literature and detect duplicates. The article titles and abstracts were screened by two authors, A.K. and I.K.A. Subsequently, full texts were obtained for in-depth analysis following the inclusion and exclusion criteria. The third author (S.S) would be consulted to resolve any discrepancies in the study inclusion. The data extracted include authors (years), study design including assessment tools, subject characteristics (gestation, parity, pregnancy risk), and study findings (associated factors and correlations).
3 Results
The literature search using three electronic databases discovered 2,232 items (Pubmed = 541, Scopus = 732 and Web of Science = 959). After the removal of duplicates (930), we screened the title and abstract of 1,302 items. A total of 1,218 papers were excluded for various reasons resulting in 84 remaining items that were subjected to full-text screening. Finally, we identified 46 eligible papers for this review. Upon detailed assessment of the data, we found that the factors contributing to childbirth fear can be classified into several categories including (1) demographics, (2) clinical, (3) psycho-social, (4) healthcare service, (5) childbirth education & information, and (6) spiritualism. Due to the vast amount of data collected, we have decided to limit our discussion to the maternal demographic and clinical characteristics, health service provision, childbirth education, and COVID-19 pandemic; which involved 26 articles (Figure 1). The remaining findings related to the psycho-social and spiritual components were reported in a separate journal article.
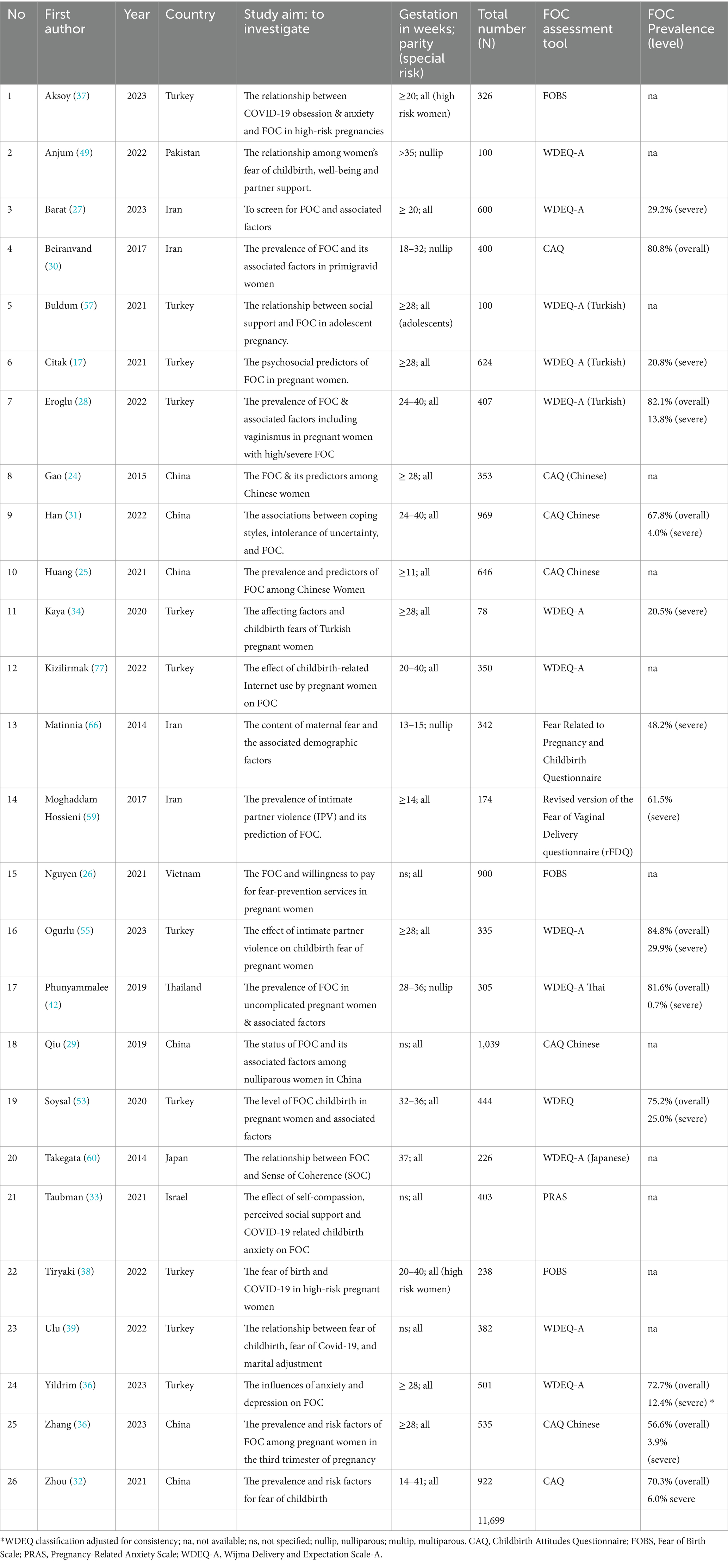
Table 1 depicts the studies included in our review. Most of the research, which were published between 2014 and 2023, were conducted in Turkey. Our review included six studies from China and four from Iran. The remaining studies were from Japan, Vietnam, Thailand, Pakistan and Israel. A total number of 11,699 women were involved in all of the studies, which were of cross-sectional design. Majority of the studies used WDEQ-A or Childbirth Attitudes Questionnaire (CAQ) (21) as the assessment tool for childbirth fear. Four studies focused on nulliparous subjects, two on high-risk women and one study involved pregnant adolescents.
The overall prevalence of childbirth fear in our review ranged between 56.6 and 84.8%. This finding could be attributed to the different FOC assessment tools, with varying cut-off scores to define severity levels. Some authors quoted the overall FOC prevalence while some focused on severe tokophobia. Studies with WDEQ-A used a score of ≥38 as indicative of FOC and ≥ 85 as severe fear (22), while CAQ scoring to detect tokophobia and the severe level was ≥28 and ≥ 52, respectively (23). Research from Iran and Turkey in West Asia used four types of questionnaires (WDEQ-A, CAQ, Fear Related to Pregnancy and Childbirth Questionnaire, and the revised version of the Fear of Vaginal Delivery questionnaire). Data from East Asian countries like Thailand and China were based on WDEQ-A and CAQ.
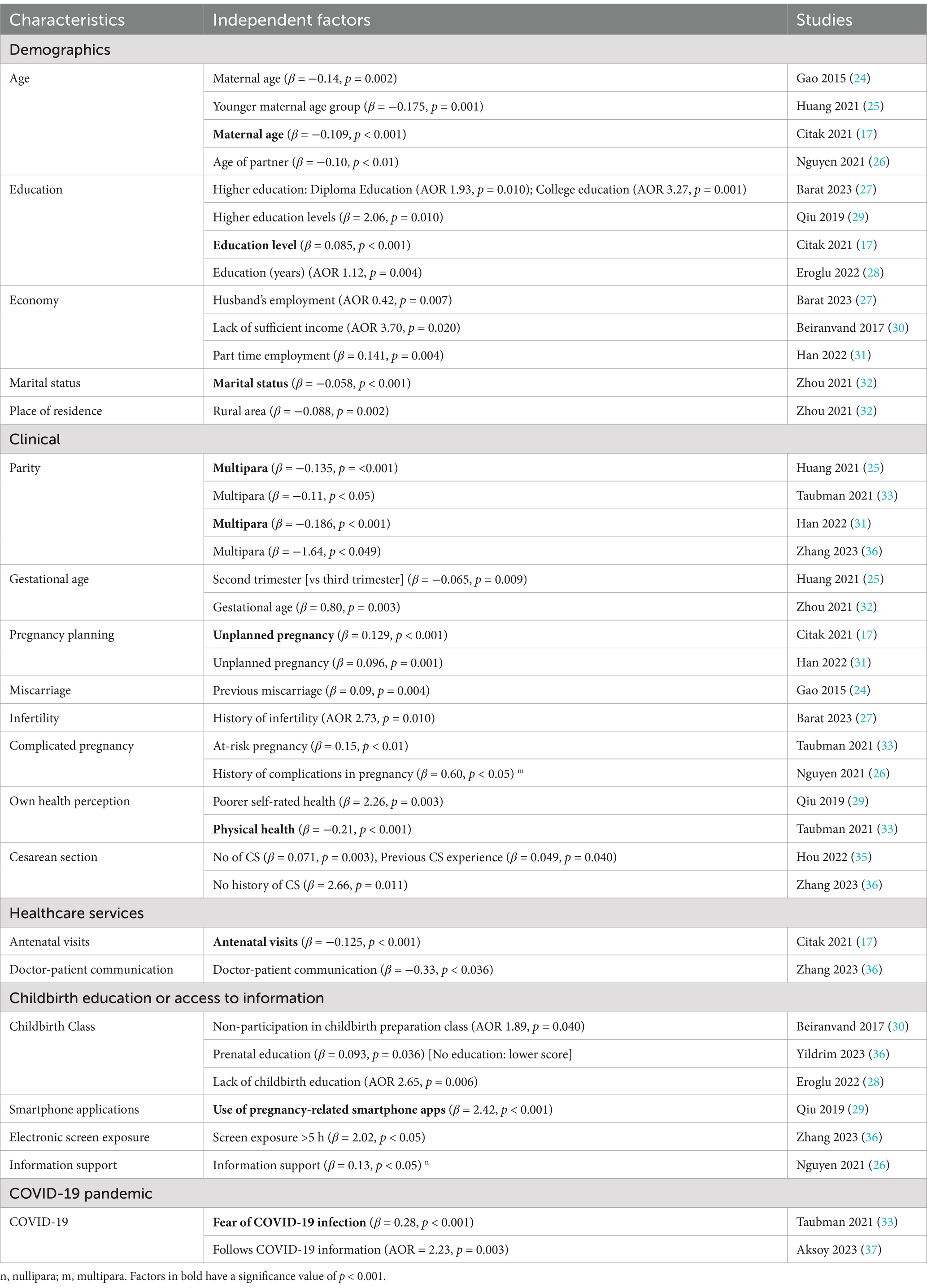
We identified independent factors associated with fear of childbirth, based on multivariable logistic or regression analysis, as demonstrated in Table 2. The factors with a significance value of p < 0.001 are highlighted in bold. Factors that significantly correlated to FOC were also discussed in this review.
3.1 Maternal demographics
Three studies found that maternal age was an independent factor associated with childbirth fear (17, 24, 25). Two studies demonstrated a negative association, i.e., advanced maternal age is linked with a lower level of fear (17, 24). In contrast, Huang et al. observed reduced childbirth fear among women in the younger age group (25). A study from Vietnam found that increasing age of the partner was linked to a decrease in childbirth fear (26).
Maternal education level was shown to be independently associated with FOC in four studies (17, 27–29); with three of them demonstrating an increased level of childbirth fear with higher education (27–29). Economy status posed a significant influence on maternal childbirth fear. Husband’s employment was associated with reduced odds of FOC (adjusted odd ratio, AOR 0.42, 95% CI 0.22–0.79) (27), while lack of sufficient income increased the likelihood by almost four-fold (AOR 3.70, 95% CI 1.23–11.14) (30). Study from China observed that being a part-time worker is a risk factor of FOC among multiparous (β = 0.141, p = 0.004) (31). Marital status was also an independent factor for childbirth fear, with married women reported lower level of FOC (32). Zhou et al. also reported strong association between place of residence and FOC; in which greater level of fear was found among women living in the rural area compared to the urban dwelling (32).
3.2 Clinical factors
Being a multipara was independently associated with reduced level of tokophobia (23, 25, 31, 33). Gestational age was also an independent predictor (25, 32), with a significant positive correlation to FOC (34). Unplanned pregnancy (17, 31), previous miscarriage (24) and history of infertility (27), were all associated with an increased risk of tokophobia. Complications in pregnancy; either in the past or present was positively associated with childbirth fear (26, 33). Pregnant women who perceived themselves in poor health also reported greater level of tokophobia (29, 33).
Hou et al. showed that the number of cesarean sections (CS) was positively associated with childbirth fear, i.e., women with two or more CS reported an increased level of FOC (β = 0.071, 95%CI 0.450–2.217) (35). The authors also found that the experience of previous cesarean section (moderate or severe fear) was positively related to tokophobia among Chinese women (β = 0.049, 95%CI 0.029–1.217) (35). In contrast, Zhang et al. observed an increased level of fear among pregnant women with no history of CS compared to individuals with previous cesarean birth (β = 2.66, 95% CI 0.61–4.71) (23).
3.3 Healthcare services
The number of antenatal visits was independently associated with reduced childbirth fear. Citak et al. observed increasing number of antenatal follow-ups was linked to a lesser degree of FOC (β = −0.125, p < 0.001) (17). Doctor-patient communication was also a significant contributor of childbirth fear with good communication was linked to lower level of tokophobia (23).
3.4 Childbirth education and access to information
Childbirth education was an independent predictor of FOC. Results from three studies consistently showed deficiency in prenatal preparation class was associated with an increased risk of childbirth fear (28, 30, 36).
Studies from China found positive association between the use of pregnancy related smartphone apps and prolonged screen exposure (>5 h) with greater risk of FOC (23, 29). Nguyen et al. observed a higher level of information support was linked to an increase in childbirth fear among nulliparous women in Vietnam (β = 0.13, p < 0.05) (26).
3.5 COVID-19 pandemic
Four studies on maternal childbirth fear were conducted during the background of COVID-19 pandemic (33, 37–39). Taubman et al. observed that women who reported fear of COVID-19 infection were more likely suffer from tokophobia (β = 0.28, p < 0.001) (33). Pregnant women who followed the COVID-19 information were twice more likely to report fear of childbirth (adjusted odd ratio, AOR 2.65, 95%CI 1.32–3.77) (37).
4 Discussion
The prevalence of childbirth fear differs across nations, despite similar measurement (15). Different evaluation instruments and cultural differences could explain some of the variations, albeit the exact reasons remain unknown (14, 15). More recent data demonstrated the global prevalence of severe FOC of 16% (95%CI 14–16%) with an increasing trend since 2015 (40). The prevalences of severe tokophobia in our review were higher; in the range of 0.7 to 61.5%. The variations could be attributed to the different socio-economic, political, and weaker health systems in the developing countries, compared to the more affluent Western countries (40). Developed countries like Sweden have an established multidisciplinary approach to care for women with severe FOC through the specialized clinic that is supported by experienced midwives, obstetrician, psychologist, social worker and psychiatrist (41). Continuity of care through midwifery-led models or single obstetrician follow-up throughout pregnancy which are available in Western health system (18), may partly explained the lower prevalence of tokophobia among non-Asians. Factors that characterized a population such as ethnicity, religion, beliefs, social structures, and social norms, will also influence maternal childbirth fear (42).
We found that independent association between maternal age and FOC. Studies from China and Turkey demonstrated that older mother reported lesser childbirth fear (17, 24). Other studies in this review also showed lower WDEQ-A scores among pregnant women above the age of 32, compared to the younger women (39, 43). Only one study demonstrated higher FOC among expectant in the older age group (25). Evidence from Scandinavian countries supported the link between advanced maternal age and greater childbirth fear (44, 45). Eriksson et al. reported intense FOC among primiparous women above the age of 32 (RR 2.3, 95% CI 1.6–3.5) (44). Age-related differences in the causes of childbirth fear include high-risk pregnancies in older women, and the concerns about loss of sexual enjoyment and attractiveness among younger mothers (45, 46). Lesser knowledge and experience in childbirth may also contribute toward higher FOC in young pregnant women (39).
A Vietnamese study found a significant association between the partner’s age and maternal childbirth fear. Nguyen et al. observed that a higher age of partner was associated with a lower score of FOC in mothers (β = −0.10, 95%CI = −0.16; −0.05) (26). This could be a reflection of tokophobia experienced by men; as evidence showed a significant positive relationship between the childbirth fear of women and their partners (r = 0.602, p < 0.001) (47). Studies from Turkey and Sweden found an increased FOC among men aged 25–35 compared to older individuals (47, 48). These men were more likely to be first-time fathers; who were at higher risk of experiencing tokophobia (AOR 1.8, 95% CI 1.2–2.6) (48). As partner support is positively correlated to maternal psychological wellbeing (r = 0.48, p < 0.001) (49), and is a mediator in the relationship between self-efficacy and childbirth fear in pregnant women (17), it is therefore important to consider the presence of tokophobia among men. Recent evidence showed that childbirth preparation for expectant fathers was associated with a more positive childbirth experience. A Swedish trial found that a psychoprophylaxis training model that focuses on the man’s role as a coach during labor, decreased the risk of frightening childbirth experiences among men with tokophobia (AOR 0.30;95% CI 0.10–0.95) (50). Bergström et al. also found that the training model which includes instruction on coaching, breathing, relaxation, and massage techniques, reduced the likelihood of feeling unprepared among expectant fathers (AOR 0.20, 95%CI 0.05–0.86) (50).
Our review showed that higher education level was an independent predictor of maternal childbirth fear. Storksen et al. made similar observation in their Norwegian study that reported increased risk of FOC among women with higher levels of education (AOR 2.1, 95% CI 1.3–3.3) (51). A large cohort study from Finland also demonstrated that higher educational level was more common among women with childbirth fear (45). Melender et al. reported that women with university level education tended to be more critical and have more negative experiences related to childbirth than controls with lower education levels (52). Individuals with higher education may seek birth-related information more actively than less educated women (51). Greater access to internet and social media among educated women lead to increased knowledge of birth complications and trauma that may exacerbate tokophobia (53). Qiu et al. suggested that educated women preferred a well-planned and structured lives. The uncontrollable aspects of childbirth that include length of labor, degree of pain and change in body shape will inevitably result in greater fear (29).
Our review demonstrated that stable and sufficient household income leads to a lesser fear of childbirth. Similarly, a study on the Danish National Birth Cohort reported a significant association between unemployment and tokophobia (AOR 1.62, 95% CI 1.35–1.93) (54). Low income and unstable finances may exacerbate the life stress among pregnant women. In contrast, a population-based study from Finland observed an increased prevalence of FOC among pregnant women of high socio-economic status (SES) regardless of parity. Raisanen et al. attributed this finding to the fact that high-risk pregnancies were common among these women, due to advanced maternal age (45).
Our observation confirmed the increased level of childbirth fear among women living in the rural area. Ogurlu et al. found that Turkish women who lived in the villages reported higher WDEQ-A scores than those living in the district areas (p = 0.026) (55). In urban areas, hospitalization for childbirth is advocated and the health facilities are well-resourced to deliver maternal and child healthcare. Conversely, rural health services may be deficient in professional staff and maternal care practices such as home visit, which result in greater tokophobia among expectant mothers (32, 40).
A study from Turkey demonstrated the impact of migration on FOC. Soysal et al. observed a lower level of childbirth fear among immigrants, compared to the pregnant Turkish women (p < 0.001). The authors also found a larger proportion of local women displaying severe form of childbirth fear than the migrant women (26.8% vs. 4.1%, p < 0.001) (54). In contrast, Ternström et al. reported that foreign-born women were more likely to have FOC compared to Swedish-born women (OR 2.7, 95% CI 1.7–4.0). Living in a foreign country with a different culture and language, alongside the lack of knowledge of the adopted country including civil rights and social system would probably contribute to women’s fear (56). In contrast, the migrant women in the Turkish study were mostly Syrian war refugees. Their worries would probably be lessened by the knowledge that they would give birth in a country free from conflict and with superior medical resources (53).
Our review found that being married reduced the likelihood of childbirth fear. Comparably, a recent meta-analysis of research from non-Asian countries revealed a higher prevalence of FOC among single or divorced women than those who were married or cohabited (21% vs. 15%) (40). Furthermore, data from six European countries supported the protective role of a stable civil relationship against tokophobia (AOR 0.64, 95% CI 0.45–0.87) (18). Women who received spousal support had consistently reported reduced level of FOC (25, 31, 49, 57). Spousal support during pregnancy reduces the anxiety and stress of the pregnant woman, and as that support increases, so does the expectant mother’s capacity to handle the problems she experienced during pregnancy (58). Spousal support had also been shown to be the mediator between childbirth self-efficacy (women’s confidence and ability to cope with childbirth) and FOC (17).
We found consistent evidence of reduced risk of tokophobia with multiparity. Studies from Iran and Japan also confirmed the negative correlation between childbirth fear and the number of deliveries (59, 60). A systematic review of 27 observational studies demonstrated the pooled prevalence of severe FOC in nulliparous women was higher than multiparous women (17% vs. 14%) (61). Greater tokophobia observed among the nullipara can be attributed to childbirth inexperience and fear of the unknown which include labor pain and support (62, 63). FOC among these women is also influenced by frightening information and negative birth stories from others (52). A contrast observation was made by Kaya et al. in which FOC increased significantly with the increasing number of pregnancies and parity (34). Increased tokophobia among multipara is usually related to a previous traumatic or negative birth experience (15); in parallel with the study by Hou et al. that observed greater FOC among women who experienced moderate to severe fear during their previous cesarean section (35). European data also reported a five-fold increase in the risk of childbirth fear in women with negative birth experiences (AOR 5.11, 95%CI 4.07–6.42) (18). Conversely, our review demonstrated a protective effect of multiparity against tokophobia. A mother’s prior delivery experience can boost her confidence and ability to handle challenging situations like labor and delivery (64), which will lessen her worry about the next pregnancy. Culturally, motherhood confers social value and this may encourage women to disregard their negative experiences and welcome their future pregnancy with joy and gratefulness (65).
Studies from Thailand, Turkey, and Iran demonstrated that women with unplanned pregnancy consistently reported greater WDEQ-A scores compared to individuals who planned their pregnancies (34, 42, 66). In line with our findings, a systematic review by Dencker et al. also found that unplanned pregnancy was a significant risk factor for FOC (19), which can be related to a lack of social support. Women in a stable relationship are probably more equipped to both prevent and cope with unintended pregnancies (19). Conversely, women with unplanned pregnancies reported higher FOC due to perceived inadequacy or unpreparedness for motherhood (67).
Our review found that poor maternal health is significantly associated with FOC. A similar observation was also made by Ulu et al. during the COVID-19 pandemic (39). Pregnant women are more susceptible to severe COVID-19 complications due to pregnancy-related physiological and immunity changes (68), and individuals with co-existing medical conditions are particularly vulnerable. Unsurprisingly, there was a significant positive correlation between COVID-19 fear and FOC (38, 39) and women who reported fear of COVID-19 infection were more likely to suffer from tokophobia (33).
Effective doctor-patient is important to alleviate maternal childbirth fear as evidenced by our finding. Previous research demonstrated that good communication between a physician and patient improves compliance and patient satisfaction (69). Regular antenatal care allows health professionals to offer adequate support to pregnant women including that to address fear and concerns about childbirth (34) with a positive impact on FOC reduction. A study from Iceland demonstrated that Enhanced Antenatal Care (EAC), which consists of a midwifery-led care model that combines one-to-one and group antenatal care is more effective in reducing tokophobia than standard care (Cohen’s d = −0.21) (70). The EAC model provides the usual antenatal appointments focusing on screening and physical assessment, alongside group sessions that allow extensive discussion about pregnancy, birth, and parenthood with midwives and other expecting parents. The authors concluded that the high satisfaction among women in the EAC group was likely due to increased social support, education, continuity of care, and personal relationship with midwives which women value in antenatal care services (70).
Insufficient knowledge of labor has been associated with increased childbirth fear (34, 71). Prenatal education had been shown not only to improve maternal knowledge, but also reduce anxiety regarding delivery (72) and fear of childbirth (73). Learning about childbirth brought comfort to some women as it helped them prepare for labor (74) and recognize how uncommon certain birth complications were (75). However, having too much information especially contradicting ones might elevate the fear of childbirth (74–76). This may explain the positive correlation between FOC and the level of information support among nullipara.
The internet has allowed women to access and share various information on delivery process, coping with labor pain alongside experience on pregnancy, birth and infant care (29, 77). Poor quality resources such as false or conflicting information, and unfavorable stories are more likely to have a negative impact on women’s perception of childbirth, resulting in increased FOC (29, 52). Unsurprisingly, prolonged screen exposure and the use of smartphone apps predisposed expectant mothers to greater childbirth fear. Women with extended internet use were more likely to access the forum web pages with a high amount of traumatic birth stories that could produce unrealistic picture of childbirth (78). Recent evidence indicated that exposure to electronic screens for more than 5 h per day in pregnant women was a risk factor for depressive symptoms (79) that in turn were associated with childbirth fear (32).
Healthcare professionals therefore play a vital role in providing the relevant advice and guidance to expectant mothers on trustworthy information sources, and timely emotional support to diminish their anxiety during the pregnancy period (80).
4.1 Strengths and limitations
Our paper is the first to systematically review studies that were exclusive to the Asian population. This review discussed the independent factors associated with maternal childbirth fear, that were derived from multivariable regression analysis. This review provided more insight into Asian women’s fear of childbirth, which is different from that of the more commonly researched European and Scandinavian populations.
Our review has several limitations. First off, the results may not accurately reflect the Asian nations as data from other countries in Southeast Asia, the Middle East, and the Indian subcontinent is lacking. Secondly, the cross-sectional design of the studies in our review prevents the establishment of causal relationship between the variables. Thirdly, due to differing assessment tools and cutoffs, we were unable to conduct a meta-analysis. The fourth point, qualitative studies that may provide deeper cultural insights into childbirth fear among Asian women, were not included in our review as we focused on quantitative research. The fifth point, as we excluded studies on Asian immigrants in non-Asian countries, we might have missed the factors influenced by the diasporic experiences of childbirth fear. Lastly, given the heterogeneity of the population in terms of ethnicity, religion, economic development, and social structure; results interpretation should be done with particular caution.
5 Conclusion
The greater FOC prevalence among Asian women is attributed to various factors including the country’s resources, socio-demographics, and cultural beliefs. Financial and relationship stability are important to reduce maternal childbirth fear. Medical conditions affecting maternal health or pregnancy will lead to increased FOC. Prenatal education is vital to impart the necessary knowledge to expectant mothers. However, conflicting information and facts overload may result in higher FOC, especially among first-time mothers. Health professionals play vital roles in addressing childbirth fear through adequate health provision, effective communication, childbirth education, and guidance on trustworthy information. Therefore, initiatives to address tokophobia among Asian women should include culturally appropriate communication training among healthcare providers, alongside locally adapted antenatal programs and mental health support for expectant mothers.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
AK: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. IKA: Investigation, Supervision, Writing – review & editing. SS: Investigation, Supervision, Writing – review & editing. NS: Conceptualization, Supervision, Writing – review & editing. SAS: Conceptualization, Formal analysis, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study received funding from the Faculty of Medicine Fundamental Grant (Project Code: FF-2023-316).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hofberg, K, and Brockington, I. Tokophobia: an unreasoning dread of childbirth. A series of 26 cases. Br J Psychiatry. (2000) 176:83–5. doi: 10.1192/bjp.176.1.83
2. Hofberg, K, and Ward, MR. Fear of childbirth, Tocophobia, and mental health in mothers: the obstetric-psychiatric Interface. Clin Obstet Gynecol. (2004) 47:527–34. doi: 10.1097/01.grf.0000132527.62504.ca
3. O'Connell, MA, Leahy-Warren, P, Khashan, AS, Kenny, LC, and O'Neill, SM. Worldwide prevalence of Tocophobia in pregnant women: systematic review and Meta-analysis. Acta Obstet Gynecol Scand. (2017) 96:907–20. doi: 10.1111/aogs.13138
4. Ayers, S. Fear of childbirth, postnatal post-traumatic stress disorder and midwifery care. Midwifery. (2014) 30:145–8. doi: 10.1016/j.midw.2013.12.001
5. Çapik, A, and Durmaz, H. Fear of childbirth, postpartum depression, and birth-related variables as predictors of posttraumatic stress disorder after childbirth. Worldviews Evid-Based Nurs. (2018) 15:455–63. doi: 10.1111/wvn.12326
6. Haines, HM, Pallant, JF, Fenwick, J, Gamble, J, Creedy, DK, Toohill, J, et al. Identifying women who are afraid of giving birth: a comparison of the fear of birth scale with the Wdeq-a in a large Australian cohort. Sex Reprod Healthc. (2015) 6:204–10. doi: 10.1016/j.srhc.2015.05.002
7. Ortega-Cejas, CM, Roldán-Merino, J, Lluch-Canut, T, Castrillo-Pérez, MI, Vicente-Hernández, MM, Jimenez-Barragan, M, et al. Reliability and validity study of the Spanish adaptation of the "Wijma delivery expectancy/experience questionnaire" (W-Deq-a). PLoS One. (2021) 16:e0248595. doi: 10.1371/journal.pone.0248595
8. Taheri, M, Takian, A, Taghizadeh, Z, Jafari, N, and Sarafraz, N. Creating a positive perception of childbirth experience: systematic review and Meta-analysis of prenatal and intrapartum interventions. Reprod Health. (2018) 15:73. doi: 10.1186/s12978-018-0511-x
9. Pang, MW, Leung, TN, Lau, TK, and Hang Chung, TK. Impact of first childbirth on changes in Women's preference for mode of delivery: follow-up of a longitudinal observational study. Birth. (2008) 35:121–8. doi: 10.1111/j.1523-536X.2008.00225.x
10. Demšar, K, Svetina, M, Verdenik, I, Tul, N, Blickstein, I, and Globevnik, VV. Tokophobia (fear of childbirth): prevalence and risk factors. J Perinat Med. (2018) 46:151–4. doi: 10.1515/jpm-2016-0282
11. Suarez, A, and Yakupova, V. Effects of postpartum Ptsd on maternal mental health and child socioemotional development - a two-year follow-up study. BMC Pediatr. (2024) 24:789. doi: 10.1186/s12887-024-05282-0
12. Ahsan, A, Nadeem, A, Habib, A, Basaria, AAA, Tariq, R, and Raufi, N. Post-traumatic stress disorder following childbirth: a neglected cause. Front Glob Womens Health. (2023) 4:1273519. doi: 10.3389/fgwh.2023.1273519
13. Takegata, M, Haruna, M, Morikawa, M, Yonezawa, K, Komada, M, and Severinsson, E. Qualitative exploration of fear of childbirth and preferences for mode of birth among Japanese Primiparas. Nurs Health Sci. (2018) 20:338–45. doi: 10.1111/nhs.12571
14. Richens, Y, Smith, DM, and Lavender, DT. Fear of birth in clinical practice: a structured review of current measurement tools. Sex Reprod Healthc. (2018) 16:98–112. doi: 10.1016/j.srhc.2018.02.010
15. Nilsson, C, Hessman, E, Sjöblom, H, Dencker, A, Jangsten, E, Mollberg, M, et al. Definitions, measurements and prevalence of fear of childbirth: a systematic review. BMC Pregnancy Childbirth. (2018) 18:28. doi: 10.1186/s12884-018-1659-7
16. Ryding, EL, Wijma, B, Wijma, K, and Rydhström, H. Fear of childbirth during pregnancy may increase the risk of emergency cesarean section. Acta Obstet Gynecol Scand. (1998) 77:542–7. doi: 10.1034/j.1600-0412.1998.770512.x
17. Çıtak Bilgin, N, Coşkun, H, Coşkuner Potur, D, İbar Aydın, E, and Uca, E. Psychosocial predictors of the fear of childbirth in Turkish pregnant women. J Psychosom Obstet Gynaecol. (2021) 42:123–31. doi: 10.1080/0167482x.2020.1734791
18. Lukasse, M, Schei, B, and Ryding, EL. Prevalence and associated factors of fear of childbirth in six European countries. Sex Reprod Healthc. (2014) 5:99–106. doi: 10.1016/j.srhc.2014.06.007
19. Dencker, A, Nilsson, C, Begley, C, Jangsten, E, Mollberg, M, Patel, H, et al. Causes and outcomes in studies of fear of childbirth: a systematic review. Women Birth. (2019) 32:99–111. doi: 10.1016/j.wombi.2018.07.004
20. Tricco, AC, Lillie, E, Zarin, W, Jangsten, E, Mollberg, M, Patel, H, et al. Prisma extension for scoping reviews (Prisma-Scr): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/m18-0850
21. Lowe, NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women. J Psychosom Obstet Gynaecol. (2000) 21:219–24. doi: 10.3109/01674820009085591
22. Toohill, J, Fenwick, J, Gamble, J, and Creedy, DK. Prevalence of childbirth fear in an Australian sample of pregnant women. BMC Pregnancy Childbirth. (2014) 14:275. doi: 10.1186/1471-2393-14-275
23. Zhang, T, Liu, M, Min, F, Wei, W, Liu, Y, Tong, J, et al. Fear of childbirth and its determinants in pregnant women in the third trimester: a cross-sectional study. BMC Psychiatry. (2023) 23:574. doi: 10.1186/s12888-023-05070-7
24. Gao, LL, Liu, XJ, Fu, BL, and Xie, W. Predictors of childbirth fear among pregnant Chinese women: a cross-sectional questionnaire survey. Midwifery. (2015) 31:865–70. doi: 10.1016/j.midw.2015.05.003
25. Huang, J, Huang, J, Li, Y, and Liao, B. The prevalence and predictors of fear of childbirth among pregnant Chinese women: a hierarchical regression analysis. BMC Pregnancy Childbirth. (2021) 21:643. doi: 10.1186/s12884-021-04123-7
26. Nguyen, LD, Nguyen, LH, Ninh, LT, Nguyen, HTT, Nguyen, AD, Vu, LG, et al. Fear of childbirth and preferences for prevention services among urban pregnant women in a developing country: a multicenter, cross-sectional study. Int J Environ Res Public Health. (2021) 18:382. doi: 10.3390/ijerph18105382
27. Barat, S, Kordinejad, B, Faramarzi, M, Khafri, S, Bouzari, Z, and Ebrahim, E. Prevalence of fear of childbirth and its effective factors in pregnant women in Babol, Iran (2019-2020): a cross-sectional study. Int J Women's Health and Reproduction Sci. (2023) 11:25–32. doi: 10.15296/ijwhr.2023.05
28. Eroglu, EO, Yildiz, MI, Turkoglu, O, Tanriover, E, Evran, A, Karahan, S, et al. High/severe fear of childbirth and related risk factors among pregnant women: is vaginismus a risk factor? J Obstet Gynaecol. (2022) 42:2860–6. doi: 10.1080/01443615.2022.2110459
29. Qiu, L, Sun, N, Shi, X, Zhao, Y, Feng, L, Gong, Y, et al. Fear of childbirth in nulliparous women: a cross-sectional multicentre study in China. Women Birth. (2020) 33:e136–41. doi: 10.1016/j.wombi.2019.04.005
30. Beiranvand, SP, Moghadam, ZB, Salsali, M, Majd, HA, Birjandi, M, and Khalesi, ZB. Prevalence of fear of childbirth and its associated factors in Primigravidwomen: a cross- sectional study. Shiraz E Medical J. (2017) 18:896. doi: 10.5812/semj.61896
31. Han, L, Bai, H, Lun, B, Li, Y, Wang, Y, and Ni, Q. The prevalence of fear of childbirth and its association with intolerance of uncertainty and coping styles among pregnant Chinese women during the Covid-19 pandemic. Front Psychol. (2022) 13:935760. doi: 10.3389/fpsyt.2022.935760
32. Zhou, X, Liu, H, Li, X, and Zhang, S. Fear of childbirth and associated risk factors in healthy pregnant women in northwest of China: a cross-sectional study. Psychol Res Behav Manag. (2021) 14:731–41. doi: 10.2147/prbm.S309889
33. Taubman-Ben-Ari, O, Chasson, M, and Abu-Sharkia, S. Childbirth anxieties in the shadow of Covid-19: self-compassion and social support among Jewish and Arab pregnant women in Israel. Health Soc Care Community. (2021) 29:1409–19. doi: 10.1111/hsc.13196
34. Kaya, D, and Evcili, F. The affecting factors of childbirth fear for pregnant women admitted to a health center and University Hospital in Turkey. J Health Res. (2020) 34:389–97. doi: 10.1108/JHR-07-2019-0147
35. Hou, Y, Zhou, X, Yao, M, and Liu, S. Fear of childbirth and its predictors in re-pregnant women after cesarean section: a cross-sectional multicenter study in China. BMC Pregnancy Childbirth. (2022) 22:393. doi: 10.1186/s12884-022-04721-z
36. Yıldırım, A, and Alp, YF. Effects of depression and anxiety on the fear of childbirth. Curr Psychol. (2023) 43:7691–6. doi: 10.1007/s12144-023-04975-6
37. Aksoy, SD, Ozdemir, S, and Akbal, E. Effects of Covid-19 anxiety and obsession on fear of childbirth in high-risk pregnancy during the pandemic in Turkey. Int J Psychiatry Med. (2023) 58:476–92. doi: 10.1177/00912174231183925
38. Tiryaki, O, Zengin, H, Gok, K, Bostanci, MS, and Ozden, S. Concerns of high-risk pregnancies during pandemic: Covid-19 and fear of birth. Florence Nightingale J Nurs. (2022) 30:274–80. doi: 10.5152/fnjn.2022.21251
39. Ulu, E, and Ertunç, T. Being pregnant in Covid-19: fear of giving birth, fear of Covid-19, and marital adjustment. Cyprus Turkish J Psychiatry Psychol. (2022) 4:222–30. doi: 10.35365/ctjpp.22.3.02
40. Sanjari, S, Chaman, R, Salehin, S, Goli, S, and Keramat, A. Update on the global prevalence of severe fear of childbirth in low-risk pregnant women: a systematic review and Meta-analysis. Int J Women's Health and Reproduction Sci. (2022) 10:3–10. doi: 10.15296/ijwhr.2022.02
41. Waldenström, U, Hildingsson, I, and Ryding, EL. Antenatal fear of childbirth and its association with subsequent caesarean section and experience of childbirth. BJOG. (2006) 113:638–46. doi: 10.1111/j.1471-0528.2006.00950.x
42. Phunyammalee, M, Buayaem, T, and Boriboonhirunsarn, D. Fear of childbirth and associated factors among low-risk pregnant women. J Obstet Gynaecol. (2019) 39:763–7. doi: 10.1080/01443615.2019.1584885
43. Uludağ, E, Cerit, E, and Karatepe, Y. Gender roles and personality traits as predictive factors for fear of childbirth. Women Health. (2022) 62:315–24. doi: 10.1080/03630242.2022.2068735
44. Eriksson, C, Westman, G, and Hamberg, K. Experiential factors associated with childbirth-related fear in Swedish women and men: a population based study. J Psychosom Obstet Gynaecol. (2005) 26:63–72. doi: 10.1080/01674820400023275
45. Räisänen, S, Lehto, SM, Nielsen, HS, Gissler, M, Kramer, MR, and Heinonen, S. Fear of childbirth in nulliparous and multiparous women: a population-based analysis of all singleton births in Finland in 1997-2010. BJOG. (2014) 121:965–70. doi: 10.1111/1471-0528.12599
46. Fairbrother, N, Thordarson, DS, and Stoll, K. Fine tuning fear of childbirth: the relationship between childbirth fear questionnaire subscales and demographic and reproductive variables. J Reprod Infant Psychol. (2018) 36:15–29. doi: 10.1080/02646838.2017.1396300
47. Serçekuş, P, Vardar, O, and Özkan, S. Fear of childbirth among pregnant women and their Partners in Turkey. Sex Reprod Healthc. (2020) 24:100501. doi: 10.1016/j.srhc.2020.100501
48. Hildingsson, I, Johansson, M, Fenwick, J, Haines, H, and Rubertsson, C. Childbirth fear in expectant fathers: findings from a regional Swedish cohort study. Midwifery. (2014) 30:242–7. doi: 10.1016/j.midw.2013.01.001
49. Anjum, A, Mushtaq, M, Anwar, T, and Ali, M. Fear of childbirth: wellbeing and partner support in first-time pregnant women. J Liaquat University of Med Health Sci. (2023) 22:55–8. doi: 10.22442/jlumhs.2022.00941
50. Bergström, M, Rudman, A, Waldenström, U, and Kieler, H. Fear of childbirth in expectant fathers, subsequent childbirth experience and impact of antenatal education: subanalysis of results from a randomized controlled trial. Acta Obstet Gynecol Scand. (2013) 92:967–73. doi: 10.1111/aogs.12147
51. Størksen, HT, Garthus-Niegel, S, Adams, SS, Vangen, S, and Eberhard-Gran, M. Fear of childbirth and elective caesarean section: a population-based study. BMC Pregnancy Childbirth. (2015) 15:221. doi: 10.1186/s12884-015-0655-4
52. Melender, HL. Experiences of fears associated with pregnancy and childbirth: a study of 329 pregnant women. Birth. (2002) 29:101–11. doi: 10.1046/j.1523-536x.2002.00170.x
53. Soysal, C, and Isikalan, MM. Determination of risk factors affecting fear of childbirth during pregnancy. Cukurova Medical J. (2020) 45:1340–5. doi: 10.17826/cumj.723669
54. Laursen, M, Hedegaard, M, and Johansen, C. Fear of childbirth: predictors and temporal changes among nulliparous women in the Danish National Birth Cohort. BJOG. (2008) 115:354–60. doi: 10.1111/j.1471-0528.2007.01583.x
55. Ogurlu, M, and Erbil, N. The effect of intimate partner violence on fear of childbirth among pregnant women. J Interpers Violence. (2023) 38:3737–55. doi: 10.1177/08862605221109915
56. Ternström, E, Hildingsson, I, Haines, H, and Rubertsson, C. Higher prevalence of childbirth related fear in foreign born pregnant women--findings from a community sample in Sweden. Midwifery. (2015) 31:445–50. doi: 10.1016/j.midw.2014.11.011
57. Buldum, A, and Guner, ET. The fear of childbirth and social support in adolescent pregnancy. J Pediatr Adolesc Gynecol. (2021) 34:839–46. doi: 10.1016/j.jpag.2021.06.005
58. Kucukkaya, B, and Basgol, S. The effect of perceived spousal support on childbirth self-efficacy on pregnant women in Turkey. BMC Pregnancy Childbirth. (2023) 23:173. doi: 10.1186/s12884-023-05508-6
59. Moghaddam Hossieni, V, Toohill, J, Akaberi, A, and HashemiAsl, B. Influence of intimate partner violence during pregnancy on fear of childbirth. Sex Reprod Healthc. (2017) 14:17–23. doi: 10.1016/j.srhc.2017.09.001
60. Takegata, M, Haruna, M, Matsuzaki, M, Shiraishi, M, Okano, T, and Severinsson, E. Antenatal fear of childbirth and sense of coherence among healthy pregnant women in Japan: a cross-sectional study. Arch Womens Ment Health. (2014) 17:403–9. doi: 10.1007/s00737-014-0415-x
61. Sanjari, S, Fakhraei, AA, Soleimani, MRM, and Alidousti, K. Validation of the Slade fear of childbirth scale for pregnancy in a sample of Iranian women: a Crosssectional study. Crescent J Med Biolog Sci. (2022) 9:138–46. doi: 10.34172/cjmb.2022.24
62. Kjærgaard, H, Wijma, K, Dykes, AK, and Alehagen, S. Fear of childbirth in obstetrically low-risk nulliparous women in Sweden and Denmark. J Reprod Infant Psychol. (2008) 26:340–50. doi: 10.1080/02646830802408498
63. Mohamamdirizi, S, Mohamadirizi, M, and Mohamadirizi, S. The comparison of fear of childbirth and sense of coherence among low-risk and high-risk pregnancy women. J Educ Health Promot. (2018) 7:143. doi: 10.4103/jehp.jehp_179_17
64. Korukcu, O, Bulut, O, and Kukulu, K. Psychometric evaluation of the Wijma delivery expectancy/experience questionnaire version B. Health Care Women Int. (2016) 37:550–67. doi: 10.1080/07399332.2014.943838
65. Korukcu, O, Bulut, O, and Kukulu, K. From experiences to expectations: a quantitative study on the fear of childbirth among multigravida women. Arch Psychiatr Nurs. (2019) 33:248–53. doi: 10.1016/j.apnu.2018.11.002
66. Matinnia, N, Faisal, I, Hanafiah Juni, M, Herjar, AR, Moeini, B, and Osman, ZJ. Fears related to pregnancy and childbirth among Primigravidae who requested caesarean versus vaginal delivery in Iran. Matern Child Health J. (2015) 19:1121–30. doi: 10.1007/s10995-014-1610-0
67. Ilska, M, Brandt-Salmeri, A, Kołodziej-Zaleska, A, Banaś, E, Gelner, H, and Cnota, W. Factors associated with fear of childbirth among polish pregnant women. Sci Rep. (2021) 11:4397. doi: 10.1038/s41598-021-83915-5
68. Wastnedge, EAN, Reynolds, RM, van Boeckel, SR, Stock, SJ, Denison, FC, Maybin, JA, et al. Pregnancy and Covid-19. Physiol Rev. (2021) 101:303–18. doi: 10.1152/physrev.00024.2020
69. Barrier, PA, Li, JT, and Jensen, NM. Two words to improve physician-patient communication: what Else? Mayo Clin Proc. (2003) 78:211–4. doi: 10.4065/78.2.211
70. Swift, EM, Zoega, H, Stoll, K, Avery, M, and Gottfreðsdóttir, H. Enhanced antenatal care: combining one-to-one and group antenatal care models to increase childbirth education and address childbirth fear. Women Birth. (2021) 34:381–8. doi: 10.1016/j.wombi.2020.06.008
71. Soltani, F, Eskandari, Z, Khodakarami, B, Parsa, P, and Roshanaei, G. Factors contributing to fear of childbirth among pregnant women in Hamadan (Iran) in 2016. Electron Physician. (2017) 9:4725–31. doi: 10.19082/4725
72. Hassanzadeh, R, Abbas-Alizadeh, F, Meedya, S, Mohammad-Alizadeh-Charandabi, S, and Mirghafourvand, M. Primiparous Women's knowledge and satisfaction based on their attendance at childbirth preparation classes. Nurs Open. (2021) 8:2558–66. doi: 10.1002/nop2.787
73. Hassanzadeh, R, Abbas-Alizadeh, F, Meedya, S, Mohammad-Alizadeh-Charandabi, S, and Mirghafourvand, M. Fear of childbirth, anxiety and depression in three groups of Primiparous pregnant women not attending, irregularly attending and regularly attending childbirth preparation classes. BMC Womens Health. (2020) 20:180. doi: 10.1186/s12905-020-01048-9
74. Melender, HL. Fears and coping strategies associated with pregnancy and childbirth in Finland. J Midwifery Womens Health. (2002) 47:256–63. doi: 10.1016/s1526-9523(02)00263-5
75. Fenwick, J, Toohill, J, Creedy, DK, Smith, J, and Gamble, J. Sources, responses and moderators of childbirth fear in Australian women: a qualitative investigation. Midwifery. (2015) 31:239–46. doi: 10.1016/j.midw.2014.09.003
76. Serçekuş, P, and Okumuş, H. Fears associated with childbirth among nulliparous women in Turkey. Midwifery. (2009) 25:155–62. doi: 10.1016/j.midw.2007.02.005
77. Kizilirmak, A, and Calpbinici, P. Investigation of the effect of pregnant Women's childbirth-related internet use on fear of childbirth. J Obstet Gynaecol. (2022) 42:3007–13. doi: 10.1080/01443615.2022.2125297
78. Bjelke, M, Martinsson, AK, Lendahls, L, and Oscarsson, M. Using the internet as a source of information during pregnancy - a descriptive cross-sectional study in Sweden. Midwifery. (2016) 40:187–91. doi: 10.1016/j.midw.2016.06.020
79. Wang, L, Yang, N, Zhou, H, Mao, X, and Zhou, Y. Pregnant Women's anxiety and depression symptoms and influence factors in the Covid-19 pandemic in Changzhou. China Front Psychol. (2022) 13:855545. doi: 10.3389/fpsyg.2022.855545
Keywords: Asia, childbirth, fear, pregnancy, tokophobia
Citation: Kalok A, Kamisan Atan I, Sharip S, Safian N and Shah SA (2025) Factors influencing childbirth fear among Asian women: a scoping review. Front. Public Health. 12:1448940. doi: 10.3389/fpubh.2024.1448940
Edited by:
Zahir Vally, United Arab Emirates University, United Arab EmiratesReviewed by:
Vera Mateus, University of Coimbra, PortugalMadhuri H. Nanjundaswamy, National Institute of Mental Health and Neurosciences (NIMHANS), India
Copyright © 2025 Kalok, Kamisan Atan, Sharip, Safian and Shah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shamsul Azhar Shah, ZHJzaGFtQGhjdG0udWttLmVkdS5teQ==
 Aida Kalok
Aida Kalok Ixora Kamisan Atan
Ixora Kamisan Atan Shalisah Sharip3
Shalisah Sharip3 Nazarudin Safian
Nazarudin Safian