- School of Public Policy and Administration, Xi’an Jiaotong University, Xi’an, China
Objectives: To better understand the outcome benefits of community health services for the aged (CHSA) and provide bottom-up identity for development, this study examined the impact of using CHSA on well-being of older adults from both objective and subjective dimensions.
Methods: Data from 1,411 people aged 60+ in Shaanxi, China was used in this study. The OLS estimate was used to analyze the impact of using CHSA on well-being of older adults. Then, the instrumental variable estimate was further hired to examine associations among variables to address the potential endogeneity concerns. The heterogeneity among disabled and non-disabled group was also estimated.
Results: For objective well-being, the mental health (β = 0.44) and financial well-being (β = 0.59) of older people using CHSA were significantly higher than those not using any service. The impact on objective well-being were more significant in non-disabled group. For subjective well-being, life meaning (β = 0.54) and security (β = 0.72) were positively associated with CHSA utilization, while independence index (β = −0.33) was negatively related with CHSA utilization. The subjective well-being of disabled group using services increased more than non-disabled group.
Conclusion: Findings underscore the positive, albeit group-selective, role of CHSA in improving well-being of older people in China and imply the necessity of high-quality development of CHSA and the targeted differentiation strategy.
Introduction
In 2016, ‘Outline of the Healthy China 2030 Plan’ had highlighted the healthcare concerns of focus groups like older people, which matters a lot to the well-being of an individual and the society (1). As the country with the largest aged population in the world, China is facing great care services burden for the aged, especially health services. The poor accessibility to institutional medical resources is a national concern in China, no exception for older people (2). Whilst older adults are more likely to obtain quality health services in nursing homes, only a minority of them afford the nursing home resources to solve their care demands, even it does not match their living preference (3, 4). As most Asian countries, families are the basic part of Chinese care services system for the aged, but most of them are incapable of meeting the multi-leveled health demands, which is a potential barrier for older people, especially those having special difficulties like chronic diseases, disabilities or frailty, to aging in place (5, 6).
Under this circumstance, the superiority of the community in supplying health services for the aged has aroused widely concern. Since the 1990s, the Chinese government has promoted the development of the community as an important carrier for connecting and integrating multiple public resources, and seized the momentum to develop community care service for the aged (CCSA) (7, 8). CCSA provides in local communities are aimed to satisfy various care service needs in terms of daily care support, healthcare, recreational and spiritual needs of the community-dwelling older people and share the pressure of family care. Thereinto, health services have been embedded in the development of CCSA. It is believed that the development of community health services for the aged (CHSA) has strong rationality, as it supports older adults to age in place with more accessible and professional health services (9). CHSA have diverse service modes and providers. For instance, the primary health care agencies like community health care centers or stations in urban area or village clinics in rural area are one of the main medical service providers of CHSA. With the support of the government, the CCSA centers could connect and integrate social healthcare resources and provide services like free medical examination and health documentation, as well as door-to-door medical services, escorting to hospital and emergency assistance with low price. Also, the senior or health associations, voluntary organizations and universities are included with services like free health lecture and local pharmacies are encouraged to offer free medication guidance. Based on the rationality of this system, the Chinese government has put great emphasis on development of CHSA to improve the accessibility of health resources and respond to the rapid growth of healthcare demands of older people (10, 11). While CHSA have obtained great system rationality and top-down policy support, the service utilization rate is surprisingly low (12). One of the key reasons is that benefits of using these services are still unclear and older people have not built confidence in them yet. That is, the bottom-up identity from older people for the development of CHSA is deficient. Evaluations on benefits of public interventions on individuals is the important basis for shaping public identity and decisions making on the allocation of limited public resources (13), thus calling for further empirical evidence on the outcome benefits of CHSA.
Previous studies on this issue were mainly focus on CCSA, and the health-related outcomes dominate the research on benefits of CCSA. It is reported that for older adults in western countries or in China, the provision or utilization of CCSA is effective in reducing hospitalization risks and in delaying institutionalization (14), decreasing health vulnerability and contributing to health (15, 16). For the frail and disabled older adults, using CCSA also has protective effect on their physical and mental health (17, 18). Few studies had focused on outcome benefits of CHSA on older people, even it is a more rigid and irreplaceable service compared with other CCSA categories like daily care services (19).
With increasing awareness that for evaluations conducted in the aged care sector, effectiveness is best determined through the measurement of outcomes with broad scopes (20), health that reduces outcome benefits into a single dimension seem to be no longer appropriate as they may underestimate the effect of healthcare resources on overall well-being of older people (21, 22). Thus, well-being, referring to the set of individuals’ welfares (23), is highly recommended and widely accepted for evaluations on the outcomes of health and social care interventions for the aged. Well-being can be divided into objective well-being and subjective well-being, by distinguishing between functional dimensions and subjective perception dimensions (23). In general, objective well-being refers to functions or capabilities independent of individual preferences (i.e., health condition and finance capability), while subjective well-being refers to subjective feeling or evaluation on life based on individual standards. Previous studies on well-being measurement mainly focuses on subjective well-being (24, 25).
Till now, no empirical evidence on the impact of using CHSA on well-being of older adults from both objective and subjective dimensions has been provided. Additionally, CHSA is developed for all community-dwelling older people and is required to incline to older people with special difficulties. In particular, disability is a prominent problem in older people, which decreases a person’s ability to carry out activities of daily living, and further places a strain on family members and calls for healthcare support urgently (26). So far, effect of CHSA utilization on the disabled older adults has not been fully studied in China. Therefore, the aim of this study is to examine the impact of CHSA utilization on objective and subjective well-being of older adults and further test the heterogeneity between disabled and non-disabled group. To address this potential endogeneity issue, the instrumental variable model is applied in this study. The current study will provide further empirical evidence on the bottom-up identity for CHSA development, forming pulling force for older people to use these services and supporting policy makers to implement more optimal allocate strategy with limited healthcare resources.
Methods
Participants and sampling
The data used in this study were obtained through the survey organized by Xi’an Jiaotong University from October 2019 to January 2020. This survey was conducted in China’s Shaanxi Province, which is ideal for our study, as it is characterized by rapid population aging and ranked as moderate in economic development. Also, Shaanxi is one of the CCSA reform pilot provinces in China and was awarded the outstanding case. A stratified sampling method was employed to yield the sample in this study. We conducted a pre-research in three representative cities first, namely, Baoji, Yan’an, and Hanzhong. Then, the survey was fully conducted in all 10 cities in Shaanxi. In each city, the isometric random sampling method was used to select two or three counties (districts). Three communities equipped with integrated service centers of CCSA were selected according to their administrative divisions. Finally, we randomly selected about 20 participants in each community if they (1) were aged ≥60 years, (2) were able to communicate easily or communicate with investigators’ assistance, and (3) volunteered to participate in the study.
Data collection
Data were collected through face-to-face interviews conducted by well-trained investigators from the research team. In this process, our investigators asked the participants and completed questionnaires based on their answers. Three categories of indicators were included in this survey: (a) utilization of CCSA (including CHSA); (b) objective and subjective well-being of older adults; and (c) socio-demographic questions. A total of 1,479 older people took part in this survey and 1,411 older people were included in final sample after filtering questionnaires with amounts of indicators data missing. Informed consent was obtained from all participants prior to the survey. Study protocols and consent forms were approved by the medical ethics committee of Health Science Center of Xi’an Jiaotong University (approval number 2016-416). All participants provided informed consent to participate in the study.
Measures
Outcome variable
The dependent (outcome) variable, well-being of older adults, was divided into objective well-being and subjective well-being in this study. Objective well-being was assessed by constructing physical health well-being index (PHW index), mental health well-being index (MHW index), social health well-being index (SHW index) and financial well-being index (FW index). The detailed measurement of objective well-being indexes was shown in Appendix Table 1.
Based on dimensions and indicators of previous subjective well-being scales for older people (13, 21, 23), eight subjective well-being indicators, including life satisfaction, feeling hopeful, personal safety, independence, achievement in life, feeling useful, feeling respected and future safety, were selected from our questionnaire. Life meaning index, security index and independence index were extracted by principal component analysis (PCA) from eight indicators (see Appendix Table 2) and the three indexes were measured by calculating the average value of common indicator(s). All the three subjective well-being indexes were standardized in regression. To all indexes, the higher the score, the higher the degree of well-being.
Independent variable
CHSA utilization was the dependent variable in this study. Five CHSA items, including health management (i.e., health lecture and medical examination), door-to-door medical services (i.e., therapy and traditional Chinese medicine health care), medical services in community health center, escorting to hospital and emergency assistance, were listed in the questionnaire and participants were asked if they had used each of them. Once a respondent said that he/she had used one or more service items, CHSA utilization was defined as Yes and a value of 1 was assigned. If a respondent did not use any service, it was defined as No and a value of 0 was assigned.
Control variables
Age, gender, educational level, marital status, living with children, Hukou location, family care and weekly exercise were included as control variables based on prior researches and expectation that they would affect well-being of older adults. These control variables also strengthen the instruments’ exogeneity as they reduce the effect of the error term on the instrument.
Instrumental variable
While using CHSA may have a significant impact on well-being of older adults, the decision on services use of older people is also influenced by their well-being status. For instance, older people with better physical health status may be less likely to use health services (27, 28). To address the potential endogenous issue and accurately estimate the impact of CHSA utilization on well-being, the prevalence of using services in a community (PUSC) was chosen as the instrument in this study to solve the potential endogeneity bias. PUSC is measured by calculating the proportion of older people (not including the participant) in the community who have used services. It was expected to positively drive or inhibit the CHSA utilization of the participant (relevance), but not to affect well-being of the participant and error term directly (exogeneity).
Statistical analysis
Simple descriptive statistics were estimated to illustrate the characteristics of our participants. To estimate the impact of CHSA utilization on well-being of older adults, the ordinary least square (OLS) estimate was first conducted. Given the potential bias caused by endogeneity, instrumental variable (IV) estimate was further used. The two-stage least square (2SLS) approach is one of the most common IV approaches. In this study, our initial stage is to test the exclusion restrictions of instrument and it is presented by the equation as follows:
Where is our endogenous regressor (CHSA utilization), is the estimated parameter coefficients, is the instrument (PUSC), is a vector of all control variables and is the error term. CD Wald F statistic was conducted in the first stage to avoid weak instrument (29).
In the second stage, the regression between predicted CHSA utilization obtained from Equation 1 and well-being of older adults is estimated by the Equation 2 as follows:
Where is the unbiased estimation of our dependent variable (well-being of older adults), is the estimated parameter coefficients, is the “purged” endogenous variable, is a vector of all other control variables and is the error term.
To further analyze the well-being outcomes differences of using CHSA between disabled and non-disabled older people, heterogeneity test on the impact of CHSA utilization on well-being of disabled and non-disabled groups was further conducted in this study. All statistical analyses were conducted in Stata version 15 (StataCorp, College Station, TX, USA).
Results
Characteristics of participants
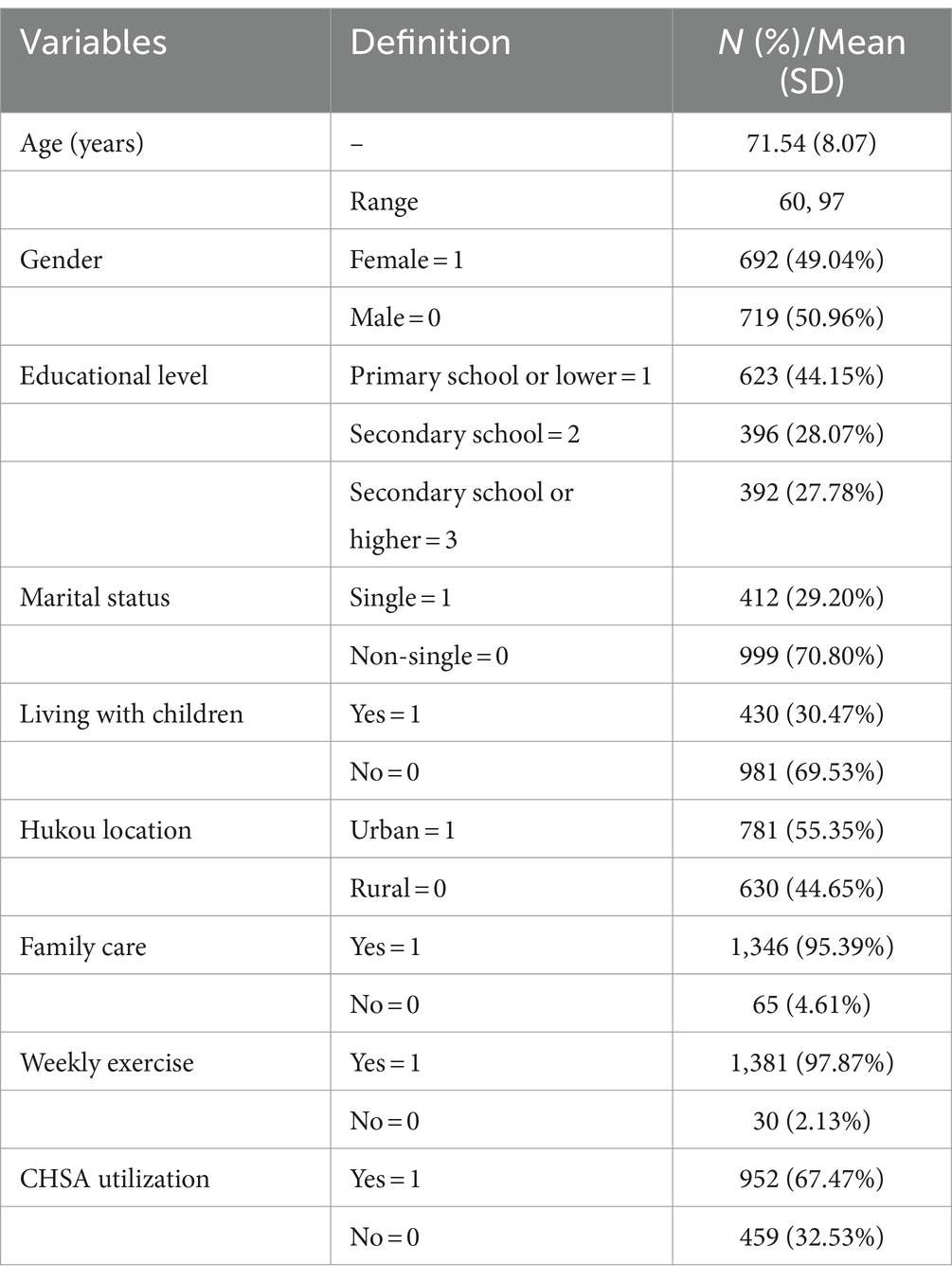
A total of 1,411 older people fully completed the survey. The baseline characteristics of participants are reported in Table 1. The age of participants ranged from 60 to 97, with 71.54 on average. 49.04% of older people were female and 44.15% of them had the educational level of primary school or lower. Most participants (70.80%) were non-single. 30.47% of them lived with children and 55.35% were urban residents. Most participants had pension insurance (95.39%) and health insurance (97.87%). Nine hundred and fifty two participants reported receiving family care and 35.65% had regular exercise weekly. 16.16%of participants reported that they had used CHSA.
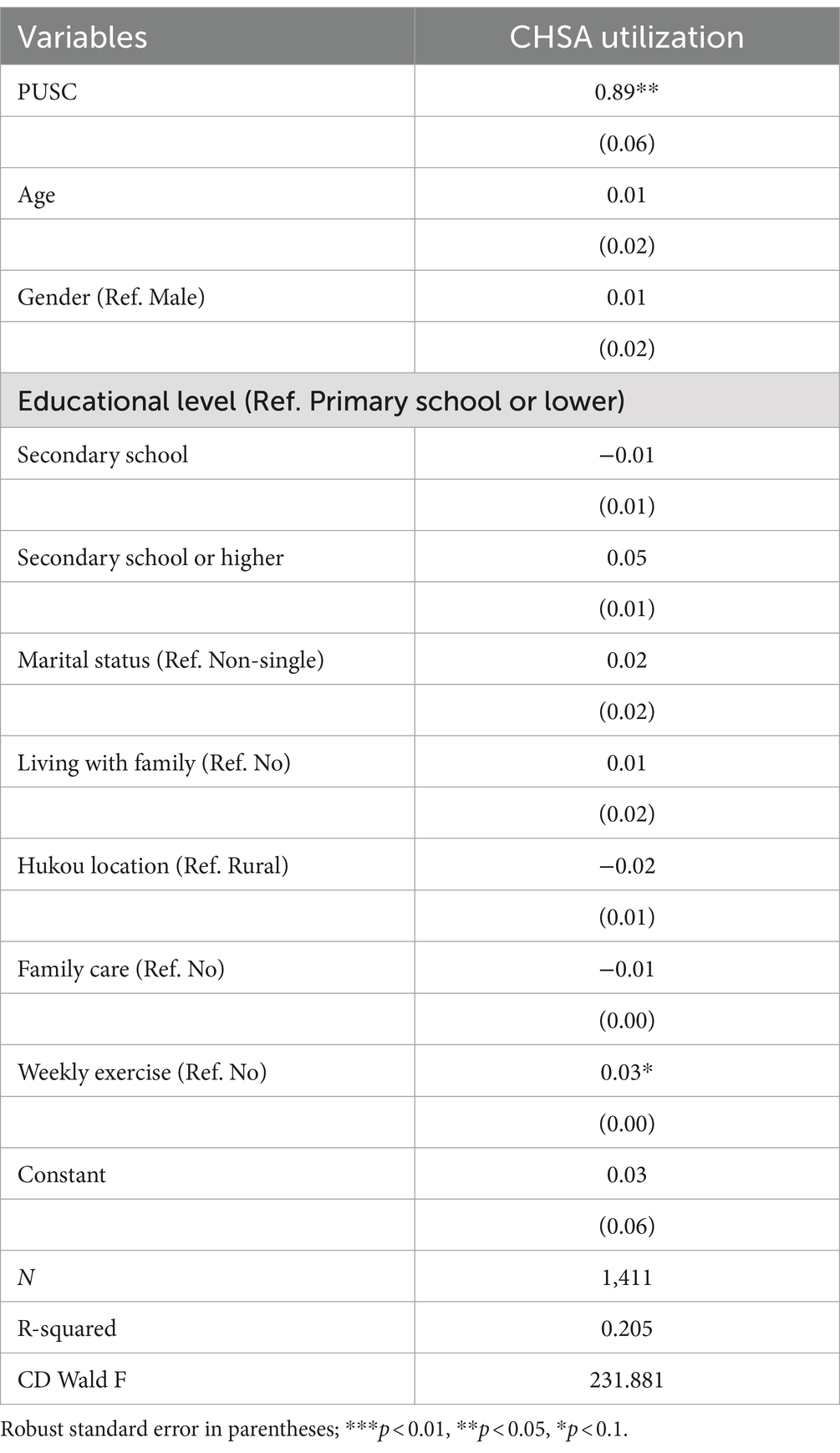
IV estimate results—first stage results
To overcome potential endogeneity problems, 2SLS model was estimated in this study. First of all, the first stage of the 2SLS process was estimated to confirm the relevance of the instruments on CHSA utilization. According to the results of first stage of 2SLS model (Table 2), PUSC is a positive explanatory factor to CHSA utilization, showing a significant relationship between the instrument and the endogenous regressor. The results indicated the rationality of the instrument choice. The CD Wald F was 231.881 in this study, easily exceeding the threshold value 10 and we can conclude that PUSC is not an invalid or weak instrument.
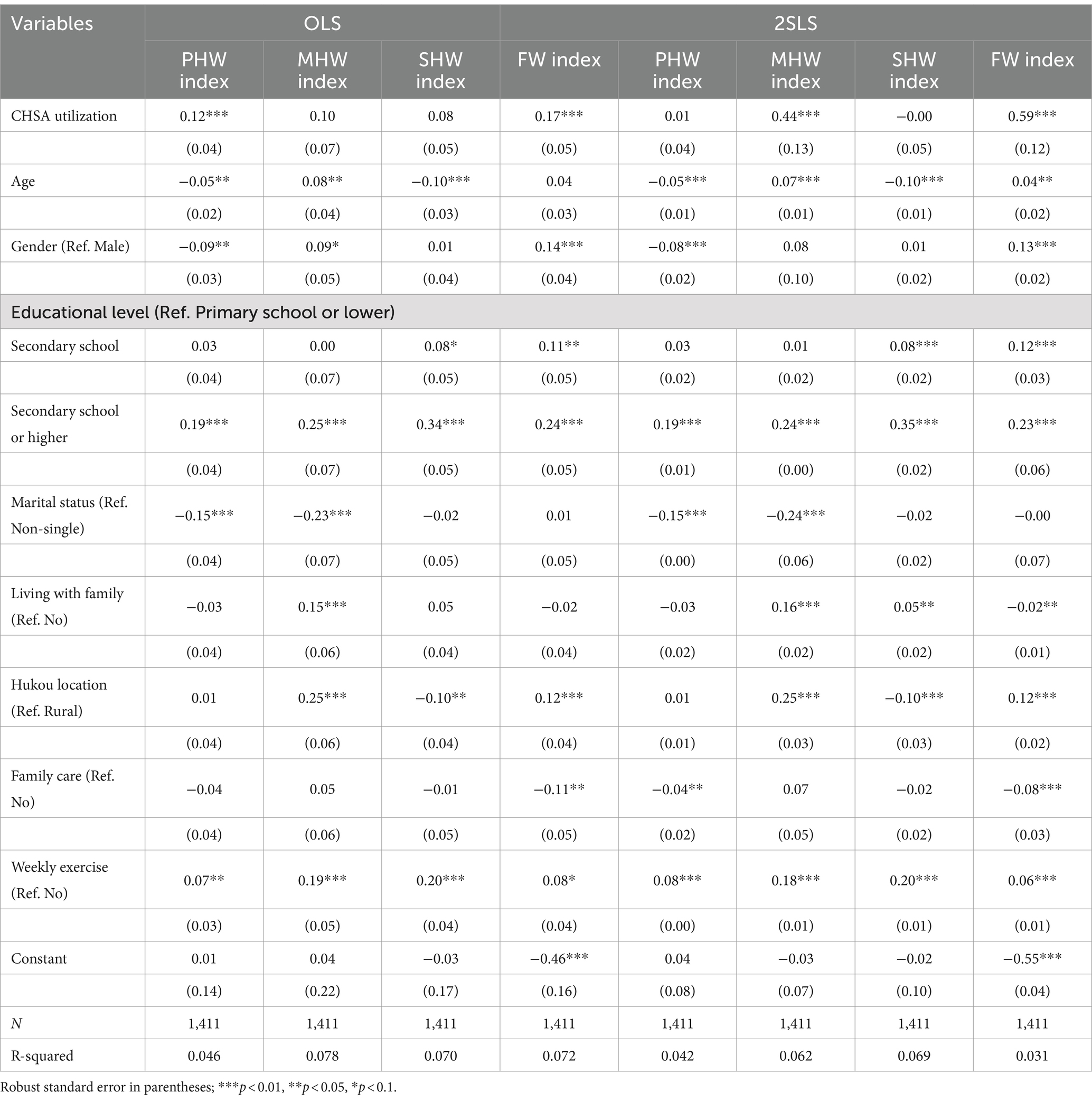
Effect of CHSA utilization on objective well-being
Table 3 shows the results of 2SLS estimate of CHSA utilization on objective well-being. The OLS estimate is also reported for comparison. The OLS results indicated a significant positive relationship between using CHSA and PHW index and FW index. Everything else being equal, a 1% increase in CHSA utilization is associated with a 12% increase in the PHW index, and a 17% increase in the FW index. After addressing the endogeneity, the 2SLS estimate showed different results, indicating that using CHSA has a significantly positive impact on MHW index and FW index. The results of 2SLS models showed that, everything else being equal, a 1% increase in CHSA utilization was correlated with a 44 and 59% increase in MHW index and FW index of older people.
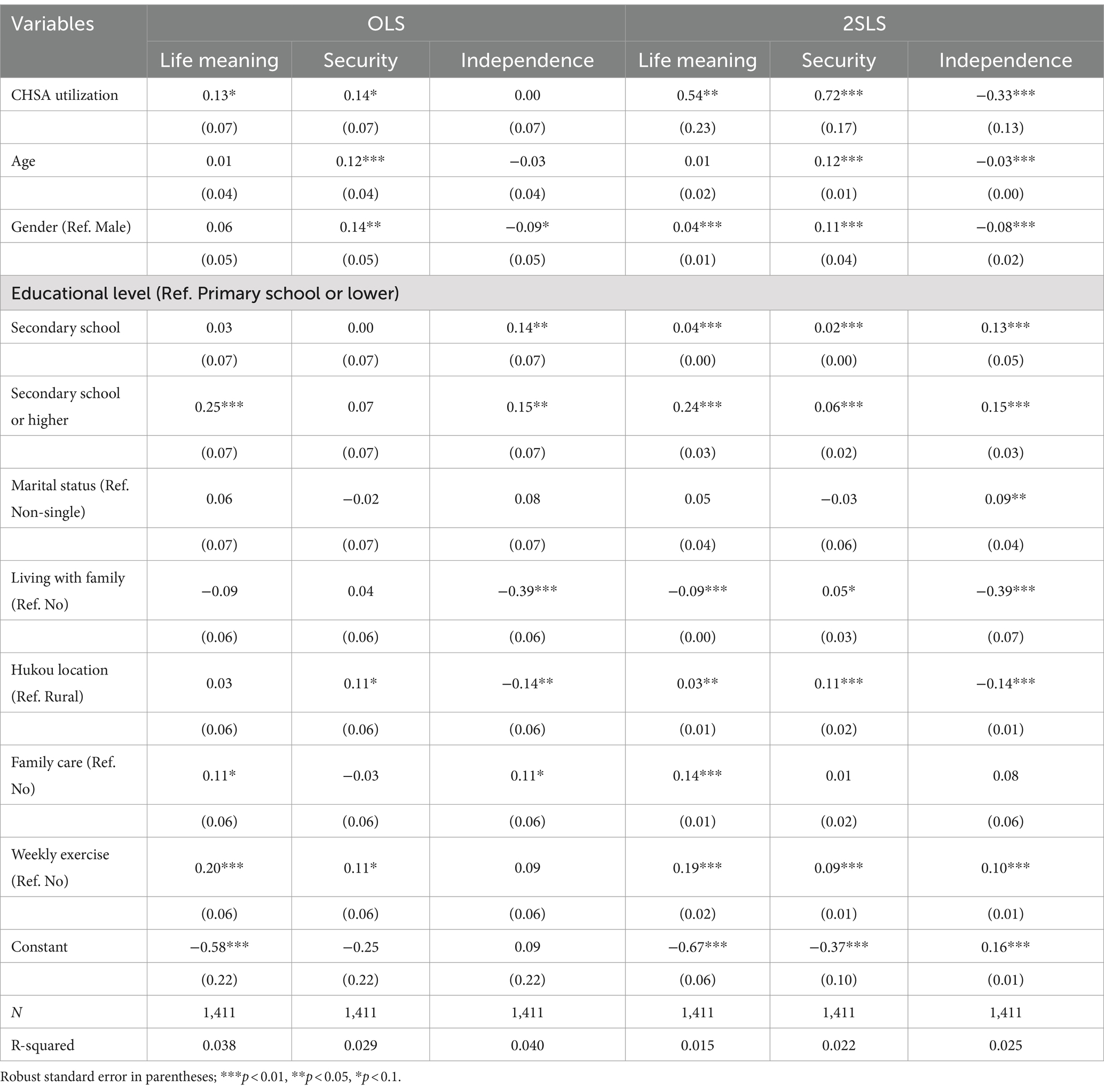
Effect of CHSA utilization on subjective well-being
Table 4 presents the results of IV estimate of CHSA utilization on subjective well-being. The OLS results indicated significantly positive impact of using CHSA on life meaning index (β = 0.13) and security index (β = 0.14), while the significant relationship between using CHSA and independence index was not observed. With the endogeneity problem considered, the 2SLS results also indicated a positive impact of using CHSA on life meaning index and security index. Everything else being equal, a 1% increase in CHSA utilization is associated with a 54% increase in the life meaning index, and a 72% increase in the security index, showing a larger impact than the estimation results of OLS models. Unlike the results of OLS models, 2SLS models also showed a negative impact on independence index (β = −0.33). It is likely that the OLS models may underestimate the impact of CHSA utilization on subjective well-being of older adults and the endogeneity bias should not be ignored.
Heterogeneity test
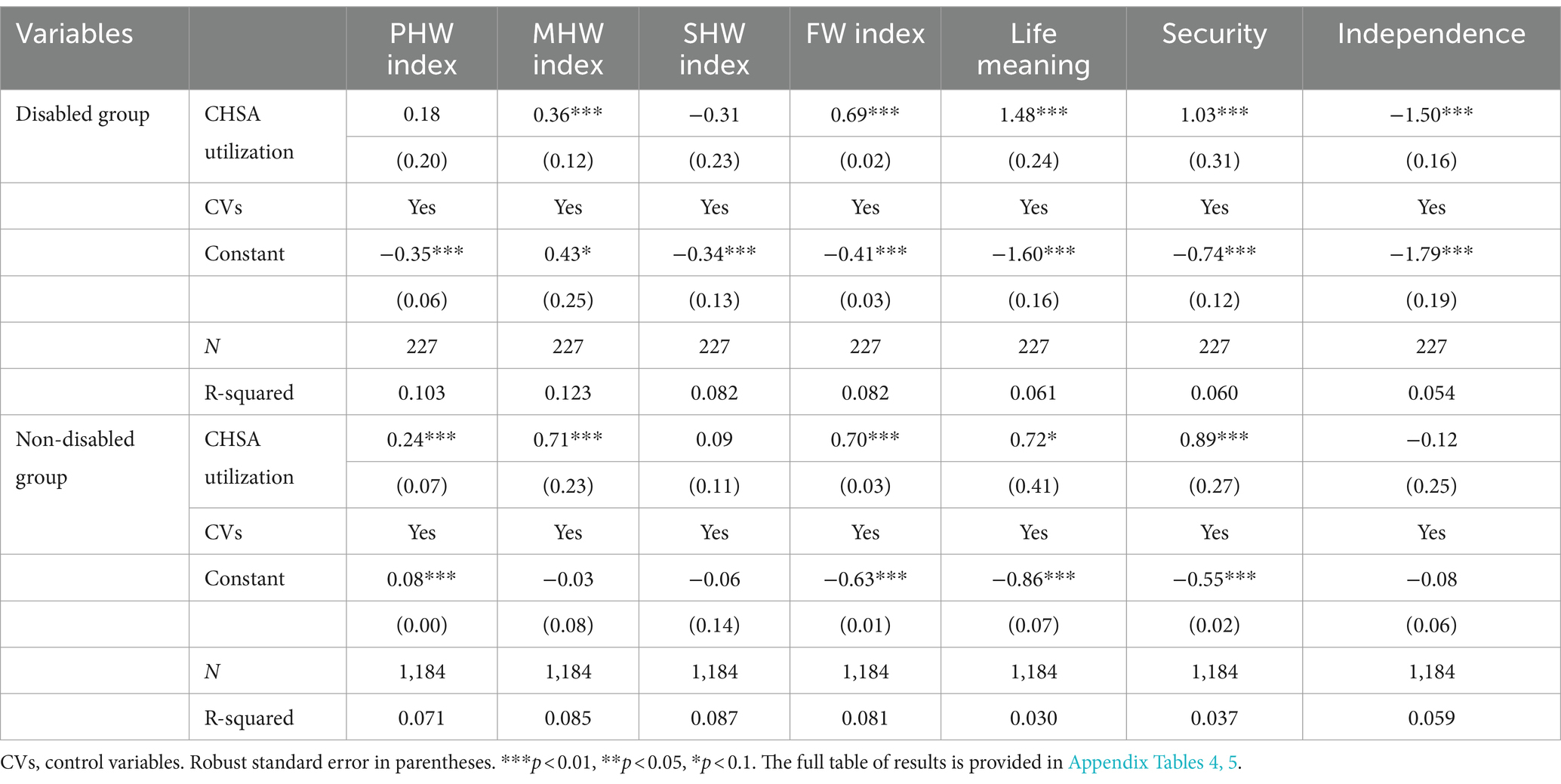
To better understand the well-being outcomes differences of using CHSA between disabled and non-disabled older people, heterogeneity test on the impact of CHSA utilization on well-being of disabled and non-disabled groups was further analyzed by using 2SLS estimate. In this study, disabled older people are defined as those reporting as needing any assistance(s) on one or more items of activities of daily living (ADL) (including bathing, dressing, using the toilet, indoor transferring, controlling urination and defecation, and eating) (30).
The results of the first stage of the 2SLS estimate are presented in Appendix Table 3. It shows that there is a significant relationship between the instrument and the endogenous regressor among both disabled and non-disabled group, with the instrument (PUSC) are significant at the 10% level. Besides, the CD Wald F was 31.864 among the disabled group and 96.810 among the non-disabled group, exceeding the threshold value 10 and passing the weak instrument test.
According to results of the second stage of the 2SLS estimate, for the 227 disabled older people, CHSA utilization had significantly positive impact on MHW index (β = 0.36), SHW index (β = 0.31), FW index (β = 0.69), life meaning index (β = 1.48) and security index (β = 1.03) of older people, while the impact of CHSA utilization on independence index (β = −1.50) was significantly negative and no significant relationship between CHSA utilization and PHW index was observed.
For the 1,184 non-disabled older people, CHSA utilization had significantly positive impact on all well-being indexes, except for SHW index (β = 0.09) and independence index (β = −0.12). Comparatively, the impact of CHSA utilization on objective well-being, particularly the physical and mental health well-being in non-disabled group were stronger than in disabled group. Conversely, the result indicated a 0.72 and 0.89 increase in life meaning index and security index of non-disabled older people using CHSA, significantly weaker than disabled older people (Table 5).
Discussion
To our knowledge, this is the first study to examine the impact of CHSA utilization on well-being of older adults from both objective and subjective dimensions. Also, IV estimate was first hired in this issue to address endogeneity concerns, which were obviously neglected in previous studies (31). With PUSC as the instrumental variable, the 2SLS estimate offered a more accurate prediction. It was evidenced that except for PHW index and SHW index, CHSA utilization had a significant impact on all objective well-being and subjective well-being of older adults.
In terms of objective well-being, older people using CHSA had significant increase on their MHW index and FW index, but not on PHW index and SHW index. Previous studies indicated that CHSA could help older adults increase health knowledge and health awareness, thus preventing the onset of disability, chronic diseases and depressive symptoms (32, 33). Our findings were only partly consistent with previous studies, with no significant association between CHSA and physical health observed. There is no denying that the implement of community-based health services policy is effective on promoting accessibility of professional health interventions for community-dwelling older people in China (34). However, China is still suffering from insufficient medical resources, especially the primary medical care in the community level. So far, CHSA in China mainly focuses on basic service items like free medical examination and medication guidance, which are hard to improve physical function of older people in a short time. For social health well-being of older adults, numerous studies had proved that social engagement is an important predictor of physical and mental health of older people (35) and conversely, better physical function is related with higher social integration and less social isolation (36). However, as mentioned above, CHSA utilization was not effective on improving physical health and it may consequently lead to the ineffective impact of CHSA utilization on social health well-being. For financial well-being, using CHSA is unlikely to boost income directly though, it works on reducing expenditures on health as a low-cost substitution for basic medical services in large hospital (37).
In terms of subjective well-being, there were significantly positive correlations between CHSA utilization and life meaning and security, while the correlation between CHSA utilization and independence was negative. Life meaning reflects the satisfaction or recognition on life or individual value of older people. As discussed above, CHSA utilization could potentially improve older people’s health and financial well-being, thus increasing their perceived life satisfaction and value (38). For the positive effect of CHSA utilization on security index, CHSA could facilitate older people’s access to healthcare interventions, shortening the time and distance between medical resources and community-dwelling older people greatly and relieving their anxiety and insecurity about health (39). Also, using CHSA works on decreasing older people’s health worries and financial pressure, and further enhances their confidence on later life. Independence index reflects whether older people feel free to do what they want to do or make their decision, which is influenced by their physical function and autonomy (23). For the negative relationship between CHSA utilization and independence index, older adults using CHSA may have some health problems that impede them to live their life independently. Another possible explanation is that even using CHSA works on functional improvement of older people, they may still be restrained by factors like family life or money to live life freely.
As expected, the impact of CHSA utilization on well-being of older adults was different between disabled and non-disabled older people. Comparatively, impact of CHSA utilization on objective well-being in non-disabled group seemed to be stronger. Specifically, using CHSA was significantly and positively correlated with physical and mental health well-being among the non-disabled older adults, while no significant correlation between CHSA utilization and physical health well-being was observed among disabled older people. A possible explanation is that, for older people without serious health problems, CHSA may be benefit on their health promotion and improve their physical condition. While owning to the unbalanced and inadequate medical resources allocation in China, the existing CHSA are far from meeting the high-level professional healthcare demands of disabled older people and making essential improvement on their physical health (33). Furthermore, the positive impact on subjective well-being were relatively stronger in disabled group. With impaired self-care ability, disabled older people are suffering from multiple life difficulties and their baseline level of subjective well-being is inevitably lower than non-disabled people, thus they may be more sensitive to the benefits from using CHSA and obtain higher life satisfaction or life security. In particular, given the limited services quality, it is unlikely for older adults with ADL limitations to recover to a good functional condition for living independently, thus the negative relationship between CHSA utilization and independence index of disabled older people is not surprising.
Policy implications
This study extends upon earlier findings and has important implications for policy and practice. For a long time, CHSA has been viewed as an important coping strategy for the increasing healthcare demands of older people and obtained great top-down policy support in China based on its system rationality. However, the evaluation of outcome benefits of these services has been overlooked. The current study provides empirical evidences on the positive impact of CHSA utilization on well-being of older adults and these findings are unbiased, implying that the role of CHSA as a policy tool in China is effective and providing the important bottom-up identity basis for further development. With these findings, policy advocacy about the benefits of using CHSA should be more widely promoted among older adults to encourage engagement and utilization. Meanwhile, more efforts should be taken to increase the accessibility and quality of health services for community-dwelling older people. For example, the government could take the lead to input more public investments and attract more social funds to support the establishment and upgrade of community healthcare facilities. More focus should be shifted to the professional training of healthcare personnel and offering high-quality professional treatments on diseases of old age (40). Also, the quality evaluation on CHSA from public perspective could be taken as an important indicator in community performance assessment. Moreover, the results revealed the difference between disabled and non-disabled group. It indicated the unmet needs for health services of disabled older people and implied the differentiation strategy on CHSA in China. A more targeted and high-quality provision system of CHSA that meet more accurate demands and incentivizes deeper engagement may be valuable.
Limitations
Our study has some limitations that must be considered in the interpretation of the findings. First, this study was a cross-sectional study with a focus on one province. While Shaanxi Province is an ideal representative area for this study, it might not be able to reflect the longitudinal perspectives and capture all regional characteristics of the impact of CHSA utilization on well-being of older adults in China. Secondly, CHSA have diverse contents while they were viewed as a whole in this study, which may obscure the specific benefits of different CHSA contents. Thirdly, this study focused on the heterogeneity between disabled and non-disabled group, while the sample size of disabled older people was only 227, which may lead to some statistical bias and weak stability of the results. Also, more specific groups like different age groups, frailty groups or urban–rural groups should be further studied to support the diverse development and targeted provision of CHSA.
Conclusion
Our findings indicated that CHSA utilization had a positive impact on objective well-being like mental health and financial well-being, and on subjective well-being like life meaning and security of community-dwelling older people, while the relationship between CHSA utilization and independence was negative. Comparatively, the positive impact on objective well-being was stronger in non-disabled group, while the positive impact on subjective well-being relatively higher in non-disabled group. These findings recognized the effective role of CHSA as a policy tool in China by evaluating its benefits on promoting well-being of older adults, forming the bottom-up identity basis for further development.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of Health Science Center of Xi’an Jiaotong University (approval number 2016-416). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LY: Conceptualization, Investigation, Methodology, Writing – original draft, Writing – review & editing. LW: Investigation, Methodology, Writing – review & editing, Data curation, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Chinese Postdoctoral Science Foundation (GZC20232082), The Research Funds of Xi’an Jiaotong University (SK2024030), Philosophy and Social Science Research Federation of Shaanxi Province (2024QN002), and Project of Humanities and Social Sciences of Ministry of Education in China (24C10698049).
Acknowledgments
We express our gratitude to all the individuals who voluntarily took part in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1447217/full#supplementary-material
Abbreviations
CHSA, community health services for the aged; CCSA, community care services for the aged; OLS, ordinary least square estimate; 2SLS, two-stage least square estimate; IV, instrumental variable estimate; PHW index, physical health well-being index; MHW index, mental health well-being index; SHW index, social health well-being index; FW index, financial well-being index; PUSC, prevalence of using services in a community.
References
1. State Council. Outline of the healthy China 2030 plan. Available at: https://www.gov.cn/zhengce/2016-10/25/content_5124174.htm (Accessed June 07, 2024).
2. Lu, C, Zhang, ZX, and Lan, XT. Impact of China’s referral reform on the equity and spatial accessibility of healthcare resources: a case study of Beijing. Soc Sci Med. (2019) 235:112386. doi: 10.1016/j.socscimed.2019.112386
3. Zhang, HM. Sending parents to nursing homes is unfilial? An exploratory study on institutional elder care in China. Int Soc Work. (2019) 62:351–62. doi: 10.1177/0020872817725137
4. Song, S, Wang, D, Zhu, W, and Wang, C. Study on the spatial configuration of nursing homes for the elderly people in Shanghai: based on their choice preference. Technol Forecast Soc Chang. (2020) 152:119859. doi: 10.1016/j.techfore.2019.119859
5. Baumbusch, J, Moody, E, Hole, R, Jokinen, N, and Stainton, T. Using healthcare services: perspectives of community-dwelling aging adults with intellectual disabilities and family members. J Policy Pract Intell Disab. (2019) 16:4–12. doi: 10.1111/jppi.12264
6. Allen, JC, Rickards, TS, Roberts, CLH, and Baird, ES. Aging in place and ‘the little things’: prioritizing mobile health and social care in rural communities. J Aging Soc Policy. (2024) 1–7. doi: 10.1080/08959420.2024.2323880
7. Jiang, N, Lou, VWQ, and Lu, N. Does social capital influence preferences for aging in place? Evidence from urban China. Aging Ment Health. (2018) 22:405–11. doi: 10.1080/13607863.2016.1249455
8. Wang, D, Zhang, HL, Ren, H, and Luo, Y. Qualitative analyses of lived experience for residents in the elderly care departments at the community health service centres in southwestern China. Health Soc Care Community. (2018) 26:E164–72. doi: 10.1111/hsc.12490
9. Zhou, J, and Walker, A. The impact of community care services on the preference for ageing in place in urban China. Health Soc Care Community. (2020) 29:1041–50. doi: 10.1111/hsc.13138
10. Tu, J, and Liao, J. Primary care providers’ perceptions and experiences of family-centered care for older adults: a qualitative study of community-based diabetes management in China. BMC Geriatr. (2021) 21:438. doi: 10.1186/s12877-021-02380-x
11. Zhou, WS, Jiang, BY, Yu, LJ, and Dai, WD. Measuring demand and supply of community care services for older people healthy ageing in rural Zhejiang Province. BMC Geriatr. (2022) 22:286. doi: 10.1186/s12877-022-02906-x
12. Gong, N, Meng, Y, Hu, Q, Du, QQ, Wu, XY, Zou, WJ, et al. Obstacles to access to community care in urban senior-only households: a qualitative study. BMC Geriatr. (2022) 22:122. doi: 10.1186/s12877-022-02816-y
13. Hackert, MQN, van Exel, J, and Brouwer, WBF. Content validation of the well-being of older people measure (WOOP). Health Qual Life Outcomes. (2021) 19:200. doi: 10.1186/s12955-021-01834-5
14. Van Cleve, R, Cole, E, and Degenholtz, HB. Risk of hospitalization associated with different constellations of home & community based services. BMC Geriatr. (2023) 23:36. doi: 10.1186/s12877-022-03676-2
15. Ormsby, J, Stanley, M, and Jaworski, K. Older men’s participation in community-based men’s sheds programs. Health Soc Care Community. (2010) 18:607–13. doi: 10.1111/j.1365-2524.2010.00932.x
16. Yang, L, Wang, LJ, Di, XD, and Dai, XL. Utilisation of community care services and self-rated health among elderly population in China: a survey-based analysis with propensity score matching method. BMC Public Health. (2021) 21:1936. doi: 10.1186/s12889-021-11989-x
17. Nyman, SR, and Victor, CR. Use of personal call alarms among community-dwelling older people. Aging Soc. (2014) 34:67–89. doi: 10.1017/S0144686X12000803
18. Makizako, H, Shimada, H, Doi, T, Tsutumimoto, K, Yoshida, D, and Suzuki, T. Effects of a community disability prevention program for frail older adults at 48-month follow up. Geriatr Gerontol Int. (2017) 17:2347-2353. doi: 10.1111/ggi.13072
19. Li, X, Lu, J, Hu, S, Cheng, K, De Maeseneer, J, Meng, QY, et al. The primary health-care system in China. Lancet. (2017) 390:2584–94. doi: 10.1016/S0140-6736(17)33109-4
20. Ratcliffe, J, Laver, K, Couzner, L, Cameron, ID, Gray, L, and Crotty, M. Not just about costs: the role of health economics in facilitating decision making in aged care. Age Ageing. (2010) 39:426–9. doi: 10.1093/ageing/afq041
21. Coast, J, Peters, TJ, Natarajan, L, Sproston, K, and Flynn, T. An assessment of the construct validity of the descriptive system for the ICECAP capability measure for older people. Qual Life Res. (2008) 17:967–76. doi: 10.1007/s11136-008-9372-z
22. Makai, P, Koopmanschap, MA, Brouwer, WB, and Nieboer, AAP. A validation of the ICECAP-O in a population of post-hospitalized older people in the Netherlands. Health Qual Life Outcomes. (2013) 11:57. doi: 10.1186/1477-7525-11-57
23. Makai, P, Brouwer, WBF, Koopmanschap, MA, Stolk, EA, and Nieboer, AP. Quality of life instruments for economic evaluations in health and social care for older people: a systematic review. Soc Sci Med. (2014) 102:83–93. doi: 10.1016/j.socscimed.2013.11.050
24. Landau, R, and Litwin, H. Subjective well-being among the old-old: the role of health, personality and social support. Int J Aging Hum Dev. (2001) 52:265–80. doi: 10.2190/RUMT-YCDX-X5HP-P2VH
25. de Albornoz, SC, and Chen, G. Relationship between health-related quality of life and subjective wellbeing in asthma. J Psychosom Res. (2021) 142:110356. doi: 10.1016/j.jpsychores.2021.110356
26. Lei, P, Feng, ZX, and Wu, ZC. The availability and affordability of long-term care for disabled older people in China: the issues related to inequalities in social security benefits. Arch Gerontol Geriatr. (2016) 67:21–7. doi: 10.1016/j.archger.2016.06.018
27. Yoon, S, Jun, DB, and Park, S. The effect of general health checks on healthcare utilization: accounting for self-selection bias. J R Stat Soc Ser A Stat Soc. (2020) 183:3–36. doi: 10.1111/rssa.12482
28. Sari, N. Physical inactivity and its impact on healthcare utilization. Health Econ. (2009) 18:885–901. doi: 10.1002/hec.1408
29. Stock, JH, Wright, JH, and Yogo, M. A survey of weak instruments and weak identification in generalized method of moments. J Bus Econ Stat. (2002) 20:518–29. doi: 10.1198/073500102288618658
30. Cawley, A, O'Donoghue, C, Heanue, K, Hilliard, R, and Sheehan, M. The impact of extension services on farm-level income: an instrumental variable approach to combat endogeneity concerns. Appl Econ Perspect Policy. (2018) 40:585–612. doi: 10.1093/aepp/ppx062
31. Yang, W, and Tang, SY. Is informal care sufficient to meet the long-term care needs of older people with disabilities in China? Evidence from the China health and retirement longitudinal survey. Ageing Soc. (2021) 41:980–99. doi: 10.1017/S0144686X1900148X
32. Hikichi, H, Kondo, N, Kondo, K, Aida, J, Takeda, T, and Kawachi, I. Effect of a community intervention programme promoting social interactions on functional disability prevention for older adults: propensity score matching and instrumental variable analyses, JAGES Taketoyo study. J Epidemiol Community Health. (2015) 69:905–10. doi: 10.1136/jech-2014-205345
33. Huang, LP, Huang, RY, Fei, Y, Liu, TS, Mellor, D, Xu, WY, et al. Lower health literacy of mania than depression among older people: a random survey of a community healthcare service center. Front Psych. (2021) 12:512689. doi: 10.3389/fpsyt.2021.512689
34. Liu, HJ, Hai, L, Zhao, M, and Wang, H. Does maintaining high accessibility to medical care services increase psychological well-being of Chinese older adults? Health Soc Care Commun. (2024) 2024:1–11. doi: 10.1155/2024/3011392
35. Liu, Y, Hu, YQ, and Nan, Y. Impact of social cognition on the self-rated health of the elderly and its mechanisms: evidence from China's comprehensive social survey. Front Psychol. (2022) 12:737081. doi: 10.3389/fpsyg.2021.737081
36. Arcury, TA, Chen, HY, Savoca, MR, Anderson, AM, Leng, XY, Bell, RA, et al. Ethnic variation in oral health and social integration among older rural adults. J Appl Gerontol. (2013) 32:302–23. doi: 10.1177/0733464811420428
37. Gu, TT, Yuan, JF, Li, LZ, Shao, QH, and Zheng, CJ. Demand for community-based care services and its influencing factors among the elderly in affordable housing communities: a case study in Nanjing City. BMC Health Serv Res. (2020) 20:241. doi: 10.1186/s12913-020-5067-0
38. Zhang, YK, Yeager, VA, and Hou, ST. The impact of community-based supports and services on quality of life among the elderly in China: a longitudinal study. J Appl Gerontol. (2018) 37:1244–69. doi: 10.1177/0733464816661945
39. Levasseur, M, Routhier, S, Clapperton, I, Doré, C, and Gallagher, F. Social participation needs of older adults living in a rural regional county municipality: toward reducing situations of isolation and vulnerability. BMC Geriatr. (2020) 20:456. doi: 10.1186/s12877-020-01849-5
Keywords: community health services for the aged, objective well-being, subjective well-being, older people, instrumental variable
Citation: Yang L and Wang L (2024) From rationality to identity: the impact of using community health services for the aged on the well-being of older adults in China. Front. Public Health. 12:1447217. doi: 10.3389/fpubh.2024.1447217
Edited by:
Andreas Koch, University of Salzburg, AustriaCopyright © 2024 Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lijian Wang, d2FuZ2xpamlhbjJAbWFpbC54anR1LmVkdS5jbg==
 Liu Yang
Liu Yang Lijian Wang
Lijian Wang