- 1Ageing and Health Research Group, The Faculty of Medicine and Health, The University of Sydney, Sydney, NSW, Australia
- 2Sydney Medical School, The Faculty of Medicine and Health, The University of Sydney, Sydney, NSW, Australia
- 3School of Population Health, The Faculty of Medicine & Health, University of New South Wales, Sydney, NSW, Australia
- 4Sydney School of Public Health, The University of Sydney, Sydney, NSW, Australia
- 5Discipline of General Practice, The Faculty of Health, University of Newcastle, Newcastle, NSW, Australia
- 6University Centre for Rural Health, The University of Sydney, Lismore, NSW, Australia
- 7School of Medicine, Western Sydney University, Lismore, NSW, Australia
- 8Clinical Excellence Commission NSW, Sydney, NSW, Australia
- 9Kolling Institute, Northern Sydney Local Health District and the University of Sydney, Sydney, NSW, Australia
The iSOLVE implementation project established and evaluated integrated processes and pathways, including a decision-making tool and educational interventions for general medical practitioners (GPs) and the upskilling of allied health professionals (AHPs). The study used a mixed-methods (parallel) design comprising surveys, qualitative methodologies, and an embedded cluster randomized controlled trial (RCT). Sampling was conducted within a Primary Health Network (PHN) geographic area in Sydney, Australia. AHP workshops (n = 367 attendees) covered six evidence-based interventions, resulting in increased confidence (p < 0.001) and numerous enhancements in fall prevention delivery. Among GPs, 75 were recruited from 27 practices. GPs in the experimental group were more likely to engage in fall prevention activities, including risk assessments, medication reviews, and providing advice, compared to the control group (p = 0.002). They were also more likely to refer patients to AHPs at 3 months (p = 0.002); however, this effect was not significant at 12 months (p = 0.13), as referral behaviors increased in the control group over time. Responses to free-text questions of practice change highlighted differences, with the experimental group reporting a more proactive and comprehensive approach to fall prevention. In a subset of GP patients (n = 560), no significant effect was observed in reducing the rate of falls (IRR = 0.96). The pragmatic nature of the project and potential contamination across multiple elements likely influenced this outcome. However, an area-wide survey of GPs (n = 562) revealed an increase in fall prevention referrals to AHPs over 5 years, from 70 to 82% (p = 0.028). Our findings highlight the importance of equipping GPs with tools and strategies to adopt a proactive approach to fall prevention among older patients. AHPs play a crucial role in this effort, and fostering relationships and connectivity across primary care networks is essential to maximizing the impact of fall prevention initiatives.
Clinical trial registration: Australian New Zealand Clinial Trials Registry, ACTRN12615000401550, https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=368286.
1 Introduction
It is estimated approximately a third of people over 65 years will have at least one fall per year (1), with more falls experienced by people over 75 years and some falling multiple times in a year. Primary care, which can include general medical practice, allied health services, community health, and community pharmacy, is generally the first point of contact people have with a health system. General medical practitioners (GPs) (family practice physicians), in particular, are relied on to manage the needs of older patients who experience falls (2, 3). This leaves many older people dealing with the aftermath of a fall in the community who could benefit from primary care interventions to prevent further falls. Falls are serious events with consequences of injury affecting mobility and independence, as well as psychological consequences such as loss of autonomy, loss of self-efficacy, and fear of falling (4), all of which would benefit from interventions through primary care (3).
Several Cochrane reviews have confirmed that exercise (5), reducing environmental fall hazards at home (6), and multi-component fall prevention (7) reduce the rate of falls in older people. Studies have also suggested that community fall prevention programs can reduce fall-related health service use (8, 9). A systematic review and meta-analysis of fall prevention by GPs did not demonstrate an effect on fall reduction, though it demonstrated an effect on injury prevention (10). The authors noted that the fidelity of interventions was limited by independent GP decisions and a reliance on patients to initiate intervention.
Despite strong evidence to guide effective fall prevention interventions in community-residing older people, there are few models (10, 11) and no clear model in Australia for engaging GPs in fall prevention. Additionally, routine use of allied health professionals (AHPs) in fall prevention has been slow, limiting widespread dissemination. To address these gaps, we developed the Integrated Solutions for Sustainable Fall Prevention (iSOLVE) implementation project (12) to establish and evaluate processes and pathways to identify at-risk older people and engage a whole primary care approach to fall prevention. We sought to engage GPs and AHPs in fall prevention, increase awareness, improve access to evidence-based fall prevention interventions, and enable ongoing knowledge acquisition and sustainable action. This study aims to describe how a multifaceted fall prevention process, implemented through upskilling in evidence-based practice and supporting workflow practices, can impact GPs’ and AHPs’ engagement in fall prevention for older adults in the community.
Our implementation objectives and related study design characteristics were to:
• Develop a process for implementing fall prevention in GP practice (Development).
• Upskill AHPs within the Primary Health Network (PHN) geographic area in evidence-based fall prevention (complementary upskilling).
• Recruit, upskill, and engage recruited GPs in fall prevention management as a routine practice and evaluate the degree of practice change over 1 year [sampling-cluster randomized controlled trial (RCT)].
• Evaluate a subsample of GP patients’ engagement in fall prevention and effectiveness on the rate of falls over 1 year (sampling-cluster RCT).
• Explore GP and AHP experiences in iSOLVE (published elsewhere) (13–15) (Convergence).
• Evaluate engagement in fall prevention by GPs across the PHN geographic area over 5 years to explore flow-on effects from project activities (Diffusion).
• Review drivers of practice change and develop online resources enabling education and support for sustained implementation of iSOLVE into primary practice (Reflection and Expansion).
2 Materials and methods
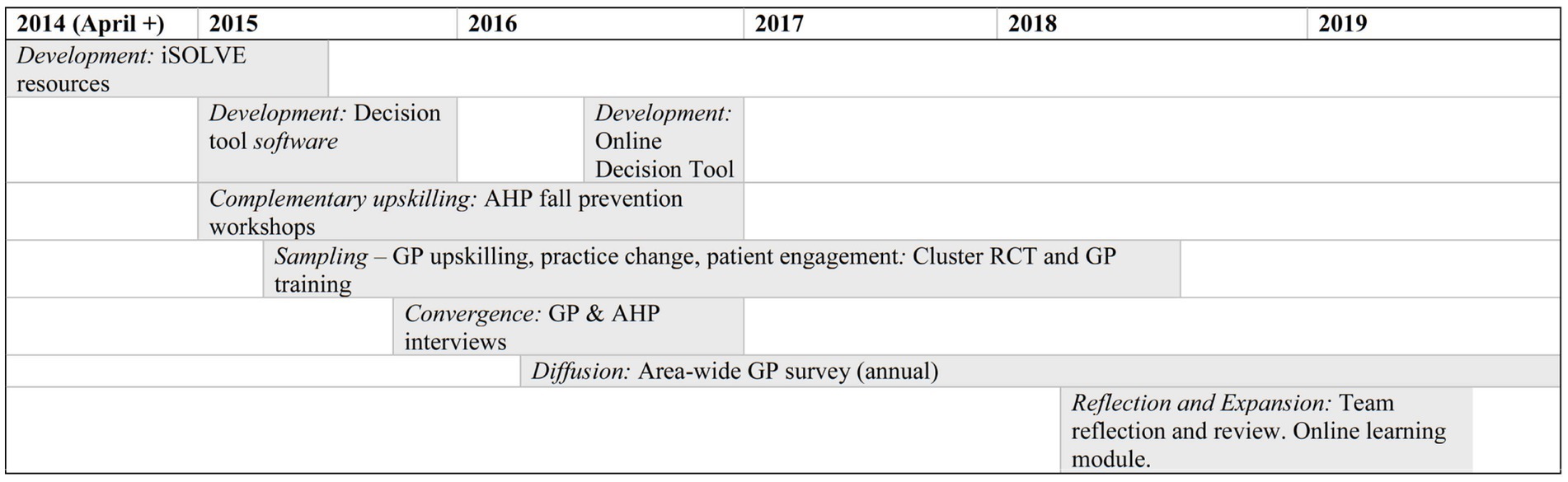
Table 1 outlines the objectives and descriptors of this pragmatic hybrid-type-2 effectiveness and mixed-methods (parallel) study (16, 17) to implement iSOLVE. Methods and results are presented for each objective.
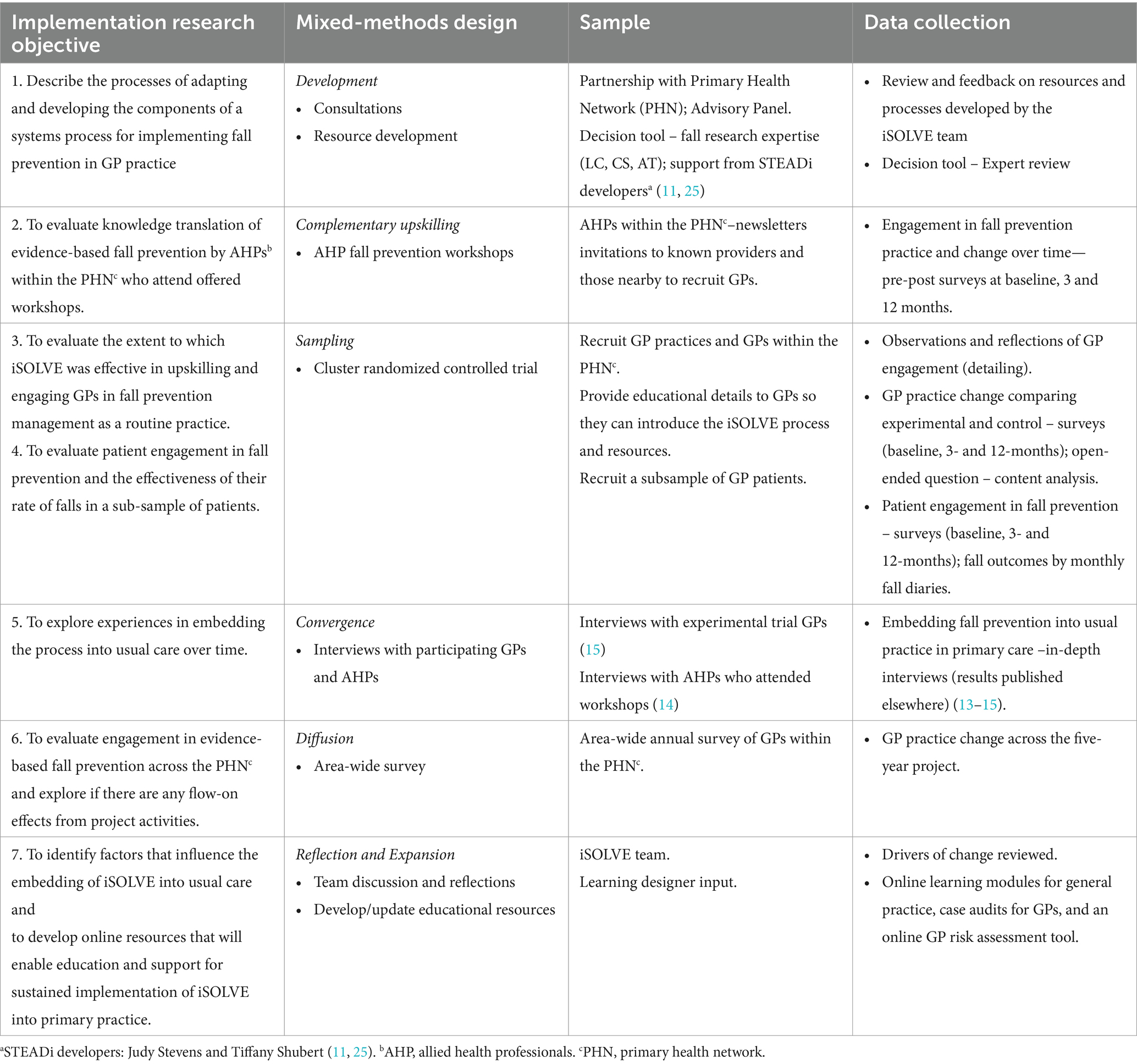
Table 1. Objectives of the pragmatic iSOLVE project and descriptors of the (parallel) mixed-methods design.
A parallel relationship denotes that the samples for the qualitative and quantitative components are different but are drawn from the same underlying population. Integrating complementary multiple methods allowed us to provide a more nuanced understanding of the implemented iSOLVE’s strengths, weaknesses, and real-world implications (17, 18). We drew on Palinkas et al. (19) and Gilmer et al. (20) in describing the characteristics of the mixed-methods design. These studies provided a structure for how the implementation questions and corresponding methods related to and built on each other.
In conceiving and designing the project, we partnered with a primary care network, the Northern Sydney Medicare Local (NSML), which, within the 1st year, was restructured into Sydney North Primary Health Network (the PHN). PHNs were established by the Australian Government to localize and improve the provision, coordination, and navigation of the complex healthcare system. They have a role in increasing the efficiency of medical services and in providing education and networking opportunities for health professionals. The major restructuring of the PHN resulted in a larger study recruitment area, a change of leadership, and the loss of our initial network partner. The new leadership supported the project, and while initially focused on their restructuring, their engagement evolved over time.
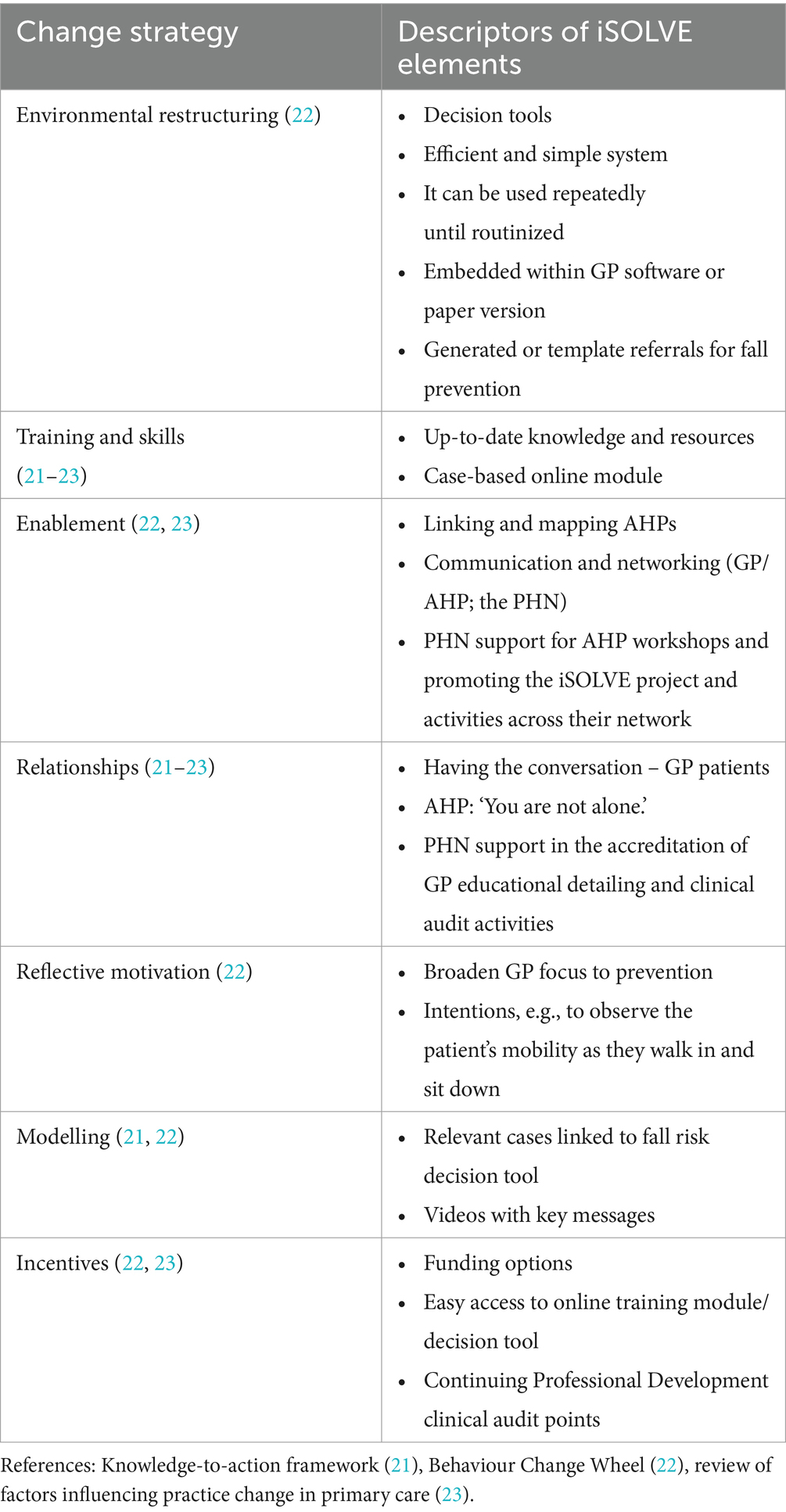
The final reflection and expansion phase reviewed drivers of change and emergent findings to produce final resources and a GP online learning module. Expected drivers of change were initially theorized in our protocol paper (12) using elements of the knowledge-to-action framework (KAT) (21), Michie et al.’s Behavior Change Wheel (22), and supported by Lau et al.’s review (23). Reporting of our implementation outcomes has been guided by Lengnick-Hall et al. (24) and Curren et al. (16).
Ethical approval was obtained from the Human Research Ethics Committee of the University of Sydney (2014/316, 2014/848). All GPs, patients, and allied health professionals recruited in the cluster RCT and in-depth interviews were given the Participant Information Statement and provided written informed consent. Survey participants were given their information statement at the start of the survey, and the submitted survey indicated consent.
2.1 Development phase
We consulted widely in developing the iSOLVE systems and resources during the project roll-out. We worked with service coordinators and management at the primary care network (NSML and the PHN) and our advisory group (GP, consumer, physiotherapist, exercise physiologist, occupational therapist, pharmacist, podiatrist, nurse, and fall prevention champions). We further consulted with local GPs, geriatricians, a geriatrician-clinical pharmacologist, and an ambulatory care specialist. The developers (11, 25) of the STEADi primary care resources in the US shared their resources and their experience with the team.
The development phase focused on developing resources and tools (12) to provide a simple workflow system for identifying people at risk of falls and to initiate fall prevention in GP practice. The resources adapted or developed for iSOLVE are summarized below.
• Decision Support Tool to provide a simple workflow system for GP Practice, with the GP first asking the questions, ‘Have you had a fall?’ and “Are you worried about falling?.” The iSOLVE Decision Tool (Figure 1) was developed by a team of fall research experts (LC, CS, ATi) drawing on current evidence and based on the US STEADi algorithm (11, 26). The tool includes the patient Stay Independent checklist (Supplementary Appendix 1) and the GP Fall Risk Assessment (Supplementary Appendix 2). Along with a new element, we added ‘Tailoring Interventions to Fall Risk Factors’ (Supplementary Appendix 3) to map patient risk factors to appropriate interventions. Referral lists to local fall prevention service providers were also developed.
• GP manual (27) included summaries of fall prevention evidence, a series of case studies providing examples of using the Decision Tool and tailoring management options (Supplementary Appendix 4–example case study), Australian Government Medicare Benefits Schedule (MBS) funding options, and examples of ‘how to talk to your patients about falls’.
• GP software. We offered paper and electronic versions of the Decision Tool. The Decision Tool was developed within a commercial GP software (PenCS third-party software Topbar) that was used by some GPs in the area. A tablet, intended for practice nurses or reception staff use, was set up with a patient Stay Independent checklist to automatically send preliminary risk information to the GP software.
• GP face-to-face educational detailing sessions (2.3.1.1).
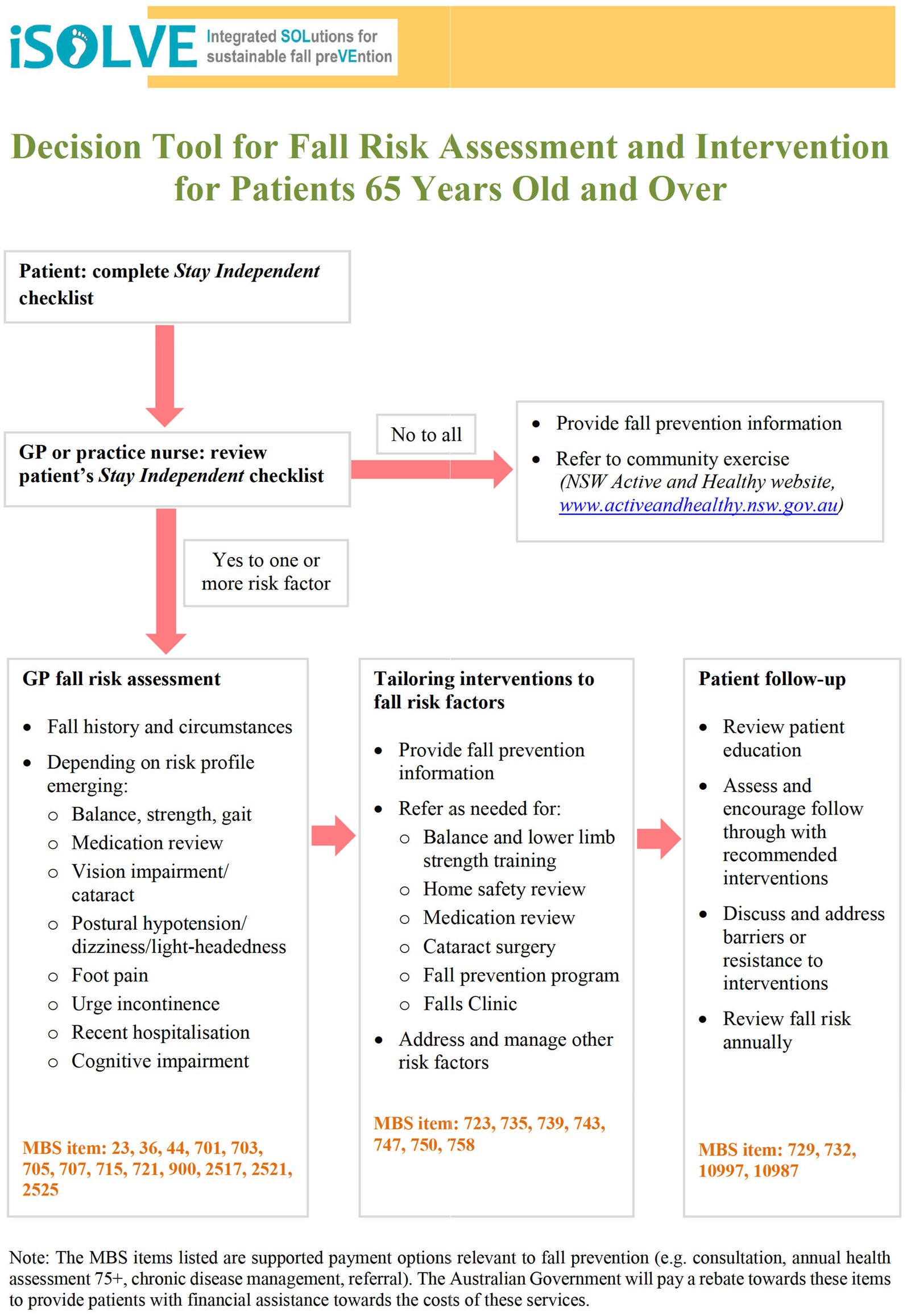
Figure 1. iSOLVE decision support tool for GPs (development reported in Clemson et al. (12) – see Table 1, column “Active ingredients”, section 1.2 in (12)). Decision tool and relevant resources are downloadable from Clemson et al. (27).
2.2 Complementary upskilling—AHP workshops
During the project, interactive workshops were delivered to educate and upskill AHPs in evidence-based fall prevention interventions. AHPs working within the PHN geographical area and providing services to older adults in the community were invited. Workshops were advertised by the PHN and to providers who advertised their services using publicly available databases. We also invited AHPs known to or located nearby to recruit general practices.
Participant AHPs were asked to complete an online survey pre-workshop and post-workshop at three and 12 months. Using mostly four-point Likert scales, the items related to the frequency of fall prevention screening, assessment, intervention and referrals, funding sources, beliefs about fall prevention, and confidence in fall prevention delivery. Changes in fall prevention knowledge were measured using a second survey related to each topic pre- and post-workshop. At follow-up surveys, questions included whether their fall prevention practice had changed and provided examples of changes and why change had not occurred. Frequencies and percentages were used to describe survey responses. The chi-square test was used to compare statistically. A content analysis (28) was conducted for the free-text practice change question. Similar responses were grouped into categories to analyze text data and then refined into subcategories.
Five workshop topics were offered (Table 2). The workshops comprised presentations of current evidence, case studies, and group discussions. Printed materials were provided, and workshops were recorded as webinars for future educational purposes (29). After each workshop, participants discussed strategies to implement and sustain fall prevention strategies in their workplace. All workshop leaders were academic and experienced researchers in their fall prevention specialty.
Workshop participants also provided contact details if they wished to be linked to GPs for fall prevention referrals. A mapping exercise was undertaken, and an online database hosted by the PHN was created containing a list of fall prevention-trained AHPs by profession and area of service (30). This enabled local information to be provided for experimental GPs.
2.3 Sampling—cluster RCT
The cluster RCT (12) was conducted according to CONSORT guidelines for cluster randomized trials (31). Primary outcomes were GP fall prevention management practices and the effect of the rate of falls in a sub-sample of GP patients. Implementation outcomes included patient engagement in fall prevention. The sample size estimate of 560 patients from 28 GP practices, as reported in our protocol paper (12), was designed to have 80% power to detect a 15% between-group difference of falls based on previous meta-analysis (32) and expected loss of practices and patients. Recruitment strategies to engage general practices and GPs are described elsewhere (33).
2.3.1 Engaging and upskilling GPs
GPs from the PHN were invited to participate and were expected to routinely assess and implement fall prevention with all their patients aged 65 and over. We aimed to recruit 28 GP practices. The general practice was the unit of randomization stratified by practice size (<80 eligible patients 65 years or older for low, ≥80 for high). Practices were randomized individually after completing GP recruitment within each practice [computer-generated block randomization at a distant site by a researcher (JS) not involved with allocation or data collection] (12). The research coordinator was blinded during GP recruitment but unblinded after randomization to recruit patients and implement interventions with GPs.
GP engagement in fall prevention management, including referral practices, measured the primary outcome of GP practice change. The unblinded research coordinator collected data by surveys at baseline, 3 months, and 12 months. The research team developed the GP survey (Supplementary Appendix 5) (academic GP, fall prevention, population health expertise; CR, CDP, LC, RP, SP) and piloted it with five GP colleagues.
2.3.1.1 Educational detailing
Participating GPs from practices randomized to the experimental group were offered an educational detailing session (34, 35) conducted by ATa (pharmacist), who was trained in fall prevention. She was also involved in the development of the resources and participated in all AHP workshops. If randomized to the control group, the GP practice was offered the same educational detailing and resources after their 12-month follow-up. Observations and reflections of GPs’ engagement were reported in field notes following each session. Reflective analysis (36) included ‘thinking aloud’ and reflective recall by the facilitator (ATa) along with regular meetings with lead investigators (LC, LM).
A face-to-face format was chosen to train GPs on how to implement the iSOLVE Decision Tool in practice. A single one-hour session—either 1:1 or in a group session—was selected to recognize GP time constraints and supported in a Cochrane review (37). Sessions were also offered to practice nurses (if available) and other staff (if requested) to encourage a whole-practice approach.
Content covered instructions and background using the GP Provider Resource (27) and the iSOLVE Decision Tool, utilizing the iSOLVE case studies as illustrative examples and, if using, demonstrating the Topbar software; local referral options; discussion of overcoming challenges and implementation ideas; and opportunity to ask questions. The practice was provided with hard copy resources for GPs/practice nurses and the Stay Independent checklists (hard copy and tablet for those with Topbar) in the waiting room. A follow-up phone call was conducted with the GP or practice manager/nominated nurse 2–4 weeks after the session to allow for further questions. GPs interested in using the clinical audit activity for Continuing Professional Development points were followed up to assist with completing the activity based on their own patient consultations.
2.3.1.2 GP trial survey: practice change and engagement
2.3.1.2.1 GP practice change
At three and 12 months, GPs were asked a dichotomous (yes/no) question about changing how they managed their older patients who had fallen in the past 3 months. The data were first analyzed using logistic regression, considering clustering by general practice using a random effect and stratification by the practice size (note that this gives the p-value for comparing groups). The clustering by practice was small (ICC = 0.10) and not significantly different from 0 (p = 0.27) at 3 months, and ICC was 0 at 12 months. Modified Poisson regression with robust standard errors, allowing for stratification, was used to estimate the rate ratio for experimental participants compared with controls.
Those who responded yes to changing practice were asked for example(s) of how their practice had changed. We asked all GPs about challenges in doing fall prevention in their practice and to provide an example(s). Responses to open-ended questions were analyzed by content analysis and grouped thematically (38).
2.3.1.2.2 GP engagement in assessing fall risk, reviewing medications, and providing advice
Engagement was determined by the survey questions: How many of your older patients (aged 65 years and over) do you (i) assess for fall risk factors, (ii) review medications likely to contribute to fall risk, and (iii) give verbal or written advice on ways to reduce fall risks? Responses were none, very few, some, or most; they scored 0 to 3, with the three questions summed to give a total out of 9. The total score at each follow-up was compared between groups using linear regression analysis with baseline score as a covariate and adjusting for clustering by GP practice and for stratification.
2.3.1.2.3 GP engagement in referring for managing falls
GP referral behavior for managing falls was evaluated by asking to whom you refer your older patients because they are at risk of falling (never, rarely, sometimes, or often). A referral score was created by counting the number of types of practitioners (out of 13 possible professions) to whom a GP sometimes or often referred older patients at risk of falling. Because the distribution of referral scores was approximately normal at each time point, linear regression was used instead of the planned Poisson regression. The referral score for each GP at each follow-up was compared between groups using linear regression analysis with baseline referral score as a covariate and adjusting for clustering by GP practice and for stratification.
2.3.2 Recruitment of subsample of patients
To recruit a sample of patients, the practice staff of participating GPs was asked to generate a list of patients 65 years and older. GPs were allowed to vet the list and exclude ineligible patients (unstable medical condition, moderate–severe dementia, receiving palliative services). The letter, signed by the GP, invited participation in the trial if they had had a fall in the past year or were concerned about falling. It included the study team’s contact details. We aimed to recruit 20 patients from each practice, for a total of 560. A research assistant (RA) blinded to GP practice allocation explained the study, obtained written consent, and conducted baseline assessments during a home visit. The participating patients from practices randomized to the experimental group were asked to make an appointment to see their GP to talk about preventing falls. They were given the patient Stay Independent checklist to complete before the visit and a copy of a fall prevention book (39). Patients from practices randomized to control were asked not to disclose study participation to their GP. GPs were not informed which patients were recruited to support the intended practice-wide adoption of the fall prevention process.
Baseline data included fall history, comorbidity, and number and type of medications. During the 12-month follow-up, patient participants were asked to self-report any falls in a monthly diary that was mailed to the blinded RA. After 12 months, a survey was mailed asking about their engagement in fall prevention and administered by phone if not returned. Control patients were provided with resources after 12 months (and after their GP received educational details) and asked to consult with their GP.
2.3.2.1 Patient–participant interaction with GP, engagement in fall prevention, fall outcomes, and medication changes at 12 months
Patient-participant engagement in fall prevention was determined by asking, “Did you do any of the following in the past year to help you prevent falls?” with a list of possible actions. They were also asked, “In the past year, have you changed the way you do things to prevent falls?.” To determine interactions between them and their GP, they were asked if “In the past year, (i) has your GP asked you about your fall history?, (ii) have you talked to your GP about what you can do to prevent fall(s)?, (iii) did your GP provide any fall prevention advice?, and, (iv) did your GP refer you to anyone else for fall prevention?” The percent of patients responding yes was analyzed using mixed-effects logistic regression, taking into account clustering by both GP and general practice using random effects and stratifying by practice size.
To analyze total falls per patient-participant, we used negative binomial regression with days in the trial as the exposure, adjusting for stratification by practice size (low/high) and allowing for clustering by GP using the generalized estimating equations (GEE) approach with an exchangeable covariance matrix and robust standard errors. To examine clustering, a mixed-effects negative binomial model was fitted, allowing for clustering by both practice and GP within practice. This analysis showed that, after accounting for clustering by GP, there was no additional clustering by practice. To analyze medication changes, based on self-reported data, we evaluated changes in the prevalence of fall risk-increasing drugs (40) from baseline to 12 months.
2.4 Convergence—GPs and AHPs in-depth interviews
Cluster RCT experimental GPs were invited to participate in audiotaped interviews lasting 10–45 min about their experience of the iSOLVE process. Data were coded, and a thematic analysis of interview transcripts was conducted (41). AHPs who had attended iSOLVE workshops were invited to participate in audiotaped interviews to explore how fall prevention was being incorporated into their routine practice. Again, thematic analysis was used to analyze transcripts (41). These studies have been published elsewhere (13–15).
2.5 Diffusion—area-wide annual GP survey
The GP area-wide survey, replicating the trial survey (2.3.1) and piloted with 31 GPs in 2015, examined referral patterns and practices as markers of uptake and implementation across the PHN geographic region. Using the PHN GP database, the survey was mailed to a random sample of GPs each year for the first 3 years (25% in 2016; 50% in 2017 and 2018), and in the final year (2019), it was sent to all GPs. Chi-square tests were used to compare responses to questions about GP engagement in fall management and referral behavior over time. The last survey included an open-ended question related to change in practice, which was explored using content analysis (38).
2.6 Reflection and expansion
In the project’s final phase, the research team undertook a reflective review of the processes and the findings against the theoretical frameworks underpinning the planned active ingredients of the iSOLVE components (12). This enabled the mapping of elements to effective implementation of change strategies. This review was important as it brought together the team’s collective understanding of the mixed methodologies and helped make meaning of the findings (42). From this process, we determined what drivers of change should be replicated and how the resources developed during the project should be accessible in the future. As part of this process, the team worked with a learning designer experienced in developing teaching and learning products in higher education to translate the iSOLVE process and resources into an online format.
3 Results
The results are presented by the project implementation objectives as in Table 1. Figure 2 provides a timeline of the project over the 5 years.
3.1 Complementary skills—upskilling AHPs
3.1.1 AHP workshops
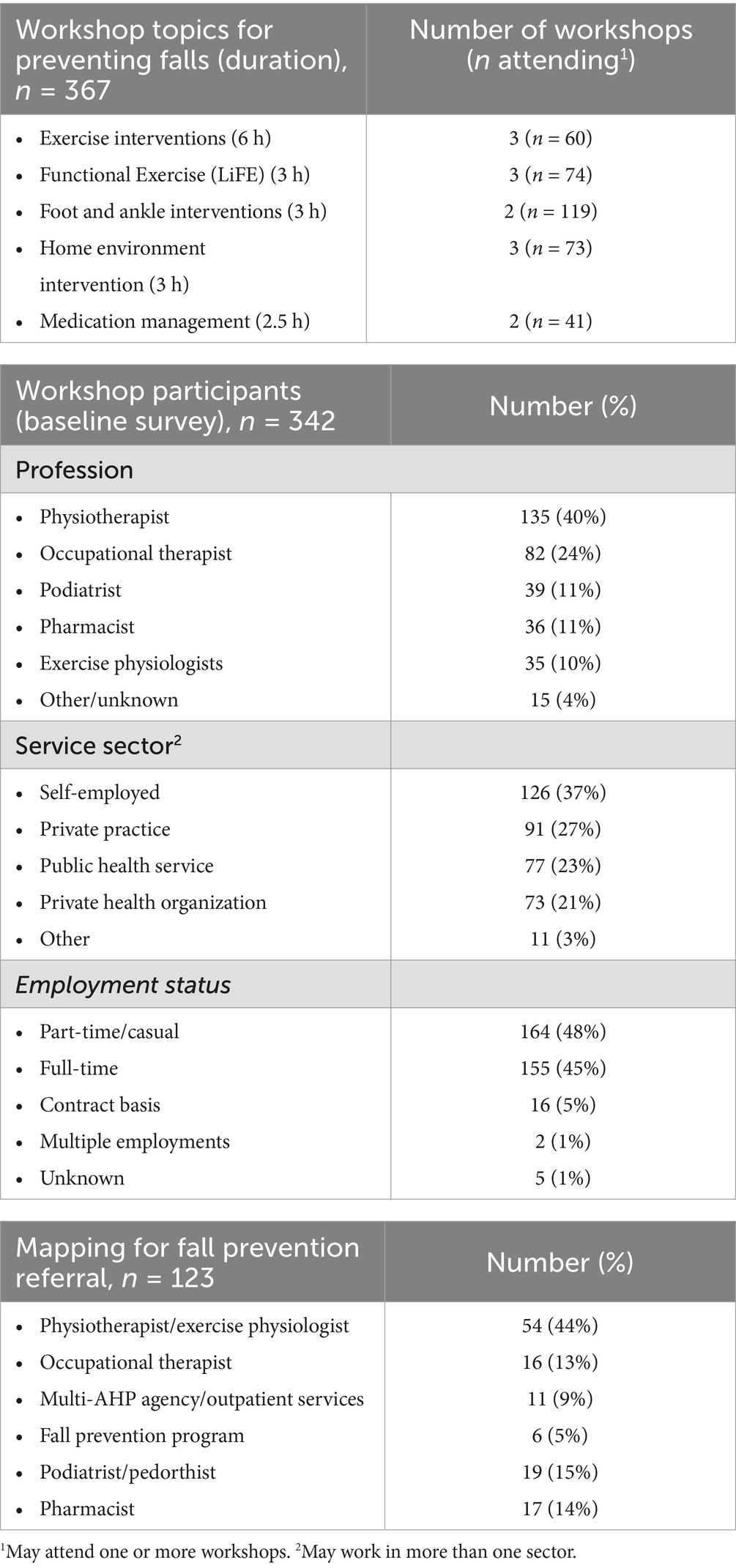
Table 2 summarizes workshop topics, AHP-participant characteristics, and mapping for GP referral. The results from the pre-workshop and post-workshop knowledge questions are presented in Supplementary Appendix 6.
Of the 367 workshop participants, 342 of them submitted the baseline surveys (administered pre-workshop). Baseline survey responses showed that most were physiotherapists (n = 135, 40%), followed by occupational therapists (n = 82, 24%). The majority of the participants were self-employed (n = 126, 37%), with almost half (n = 164, 48%) working part-time or casually. At baseline, AHPs (n = 255) reported the number of referrals they received from GPs varied: 27% never or rarely, 43% sometimes, and 29% often. There was a large and diverse range of referral sources that included other AHPs (percent of sometimes/often: physiotherapists 59%, occupational therapists 53%, exercise physiologists 16%, podiatrists 9%, pharmacists 6%), fall prevention program (Stepping On) leaders (13%), falls clinic (25%), nurses (46%), and geriatricians (44%). They also frequently received self-referrals (67% sometimes/often).
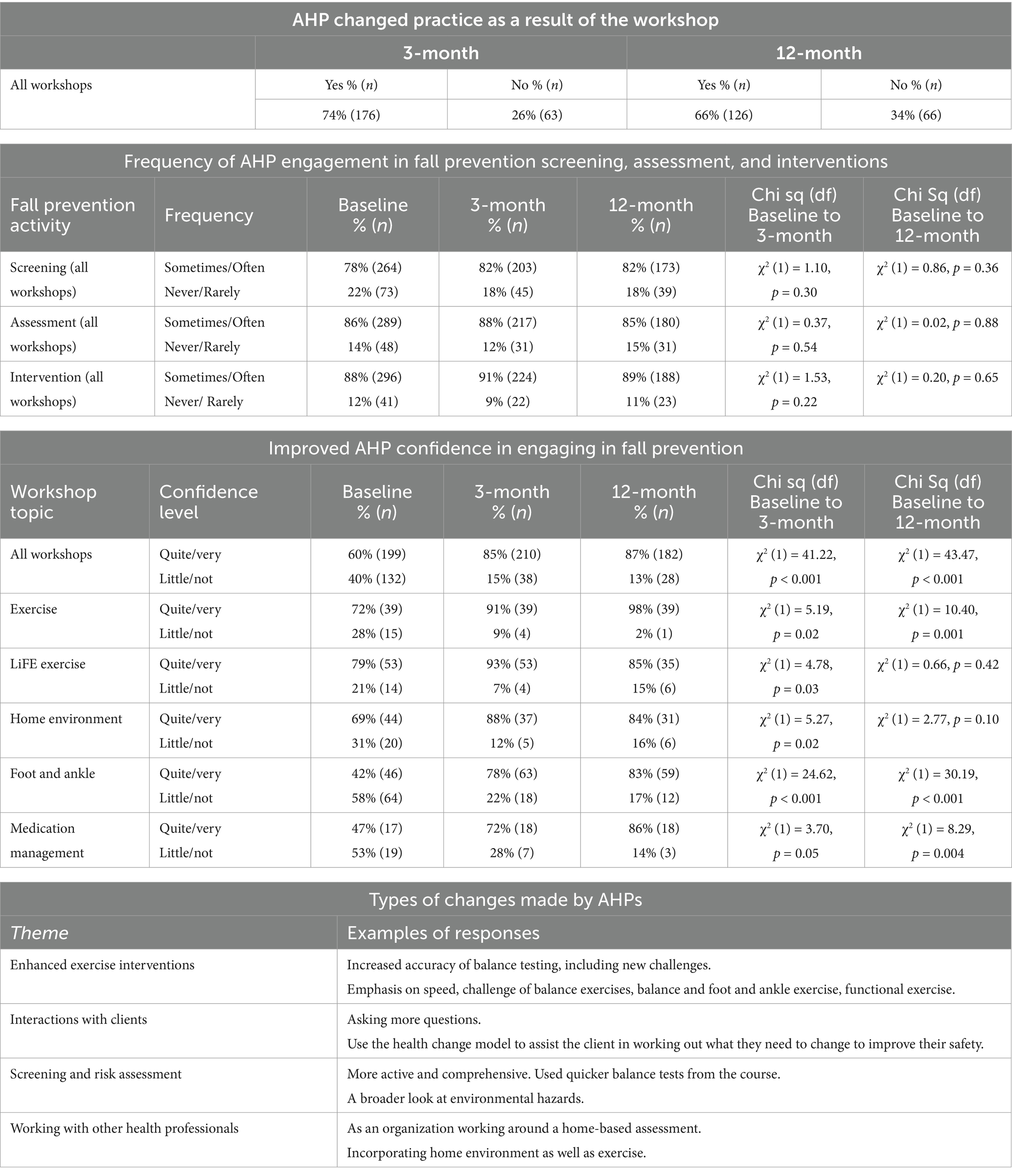
3.1.2 AHP-participant surveys at follow-up
Survey findings are presented in Table 3. Follow-up surveys were returned by 250 (73%) AHP participants at 3 months and 214 (63%) at 12 months. There was a statistically significant increase in self-confidence compared to baseline across all workshops. There was high engagement of AHPs in the frequency of fall prevention practices at baseline, with little change over the follow-up period in the frequency of fall prevention screening, assessment, and interventions. However, at 3 months, 74% of AHPs reported change in practice, and 66% reported change since baseline at 12 months.
Responses to the practice change question demonstrated evidence of change in the nuances and nature of how the AHPs delivered their fall prevention. For example, they broadened their awareness of fall prevention, added practice enhancements with new ideas, and referred to others to more fully meet clients’ needs, as illustrated below and in Table 3.
“Included more information in the assessment and have tried making the client more involved in finding solutions to the risks/issues/behaviors—asking more open-ended questions to guide the client in coming up with solutions him/herself (taking more responsibility in the process) and in setting goals.” (H3).
AHPs who did not change their practice cited issues such as implementing the interventions already or lack of time and opportunity (e.g., no referrals, inability to provide multiple visits, difficulty in providing a thorough service within funded appointment time, no older clients).
3.2 Sampling—cluster RCT
3.2.1 Recruiting and training GP practices and GPs
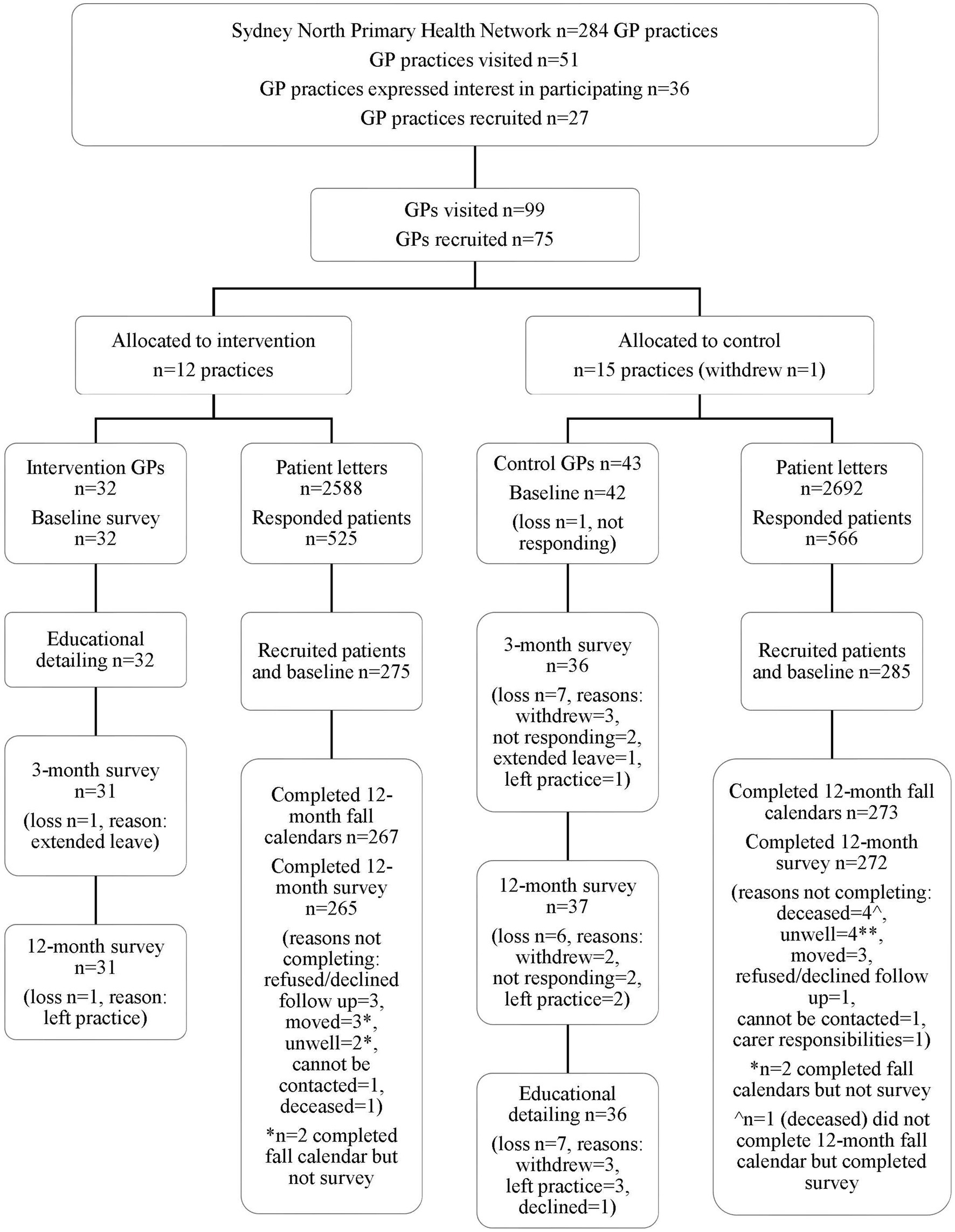
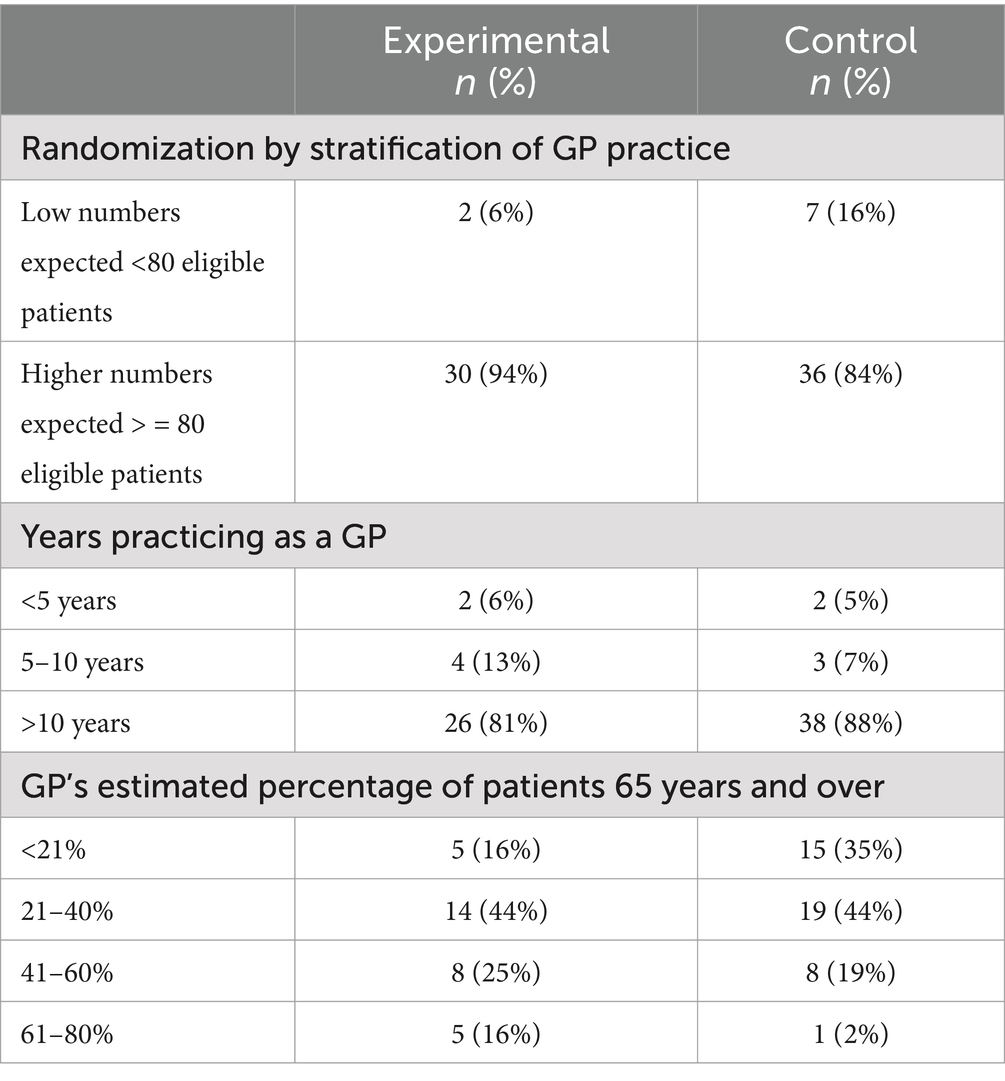
Twenty-six practices were randomized into two groups: 12 to experimental (32 GPs) and 15 to control (43 GPs). One practice (3 GPs) withdrew post-randomization. Figure 3 shows the cluster RCT flowchart and baseline characteristics of GPs, which are reported in Table 4 [Supplementary Appendix 7 reports the GP sample per GP practice and stratum (high/low)].
3.2.1.1 Educational detailing
A total of 27 face-to-face sessions were conducted with 12 experimental GP practices. The 27 educational detailing sessions were attended by 32 GPs, two GP registrars, one medical student, and 13 practice nurses. There were 16 individual sessions, six with two participants and five with 3–5 participants. Of the 27 sessions, 17 were with GPs, seven were with practice nurses, and three were mixed staff sessions. The mean session duration was 51 min (range 30–90). The two sessions, which were 90 min long, were large practices with all recruited GPs in attendance. Eleven GPs chose to additionally undertake the case audits during the trial, with the PHN facilitating their professional education points.
A major part of the educational detailing was an emphasis on the GP’s role in routinizing fall prevention into everyday practice with every patient 65 years and over (i.e., asking if they have had a fall or worried about falling) and working through several iSOLVE case studies (27) (Supplementary Appendix 4), which demonstrate how the Decision Tool is used and how to tailor fall prevention interventions. As an alternative to prepared cases, some GPs reflected on their own patient(s). A common theme raised by GPs was their referral practices and familiarity with local fall prevention providers; local referral lists to AHPs were well-received. Another common theme was patient resistance or systemic difficulties in accessing services; counterpoints (e.g., how to encourage patients, transport options) were offered to assist GPs with their patient consultation.
The majority of the recruited GPs appeared keen to learn and felt it aligned with their vision of wellbeing for their older patients. Some GPs could not believe that their patients were interested, particularly those they perceived as low or no risk. Peer influences were evident during discussions when some recruited GPs shared resources with others in practice, and six practices requested additional education be organized for new GPs or staff.
Six practices had ‘top-up’ sessions to demonstrate the GP software, which was delayed in development. Some GPs opted to stay with paper versions; others experienced some software function and practice computer issues. During the trial, the team developed an external web-based decision tool as an alternative that provided easier access for GPs to practice the decision tool.
3.2.2 GP practice change: RCT survey
3.2.2.1 Changed practice in managing older patients who have had a fall
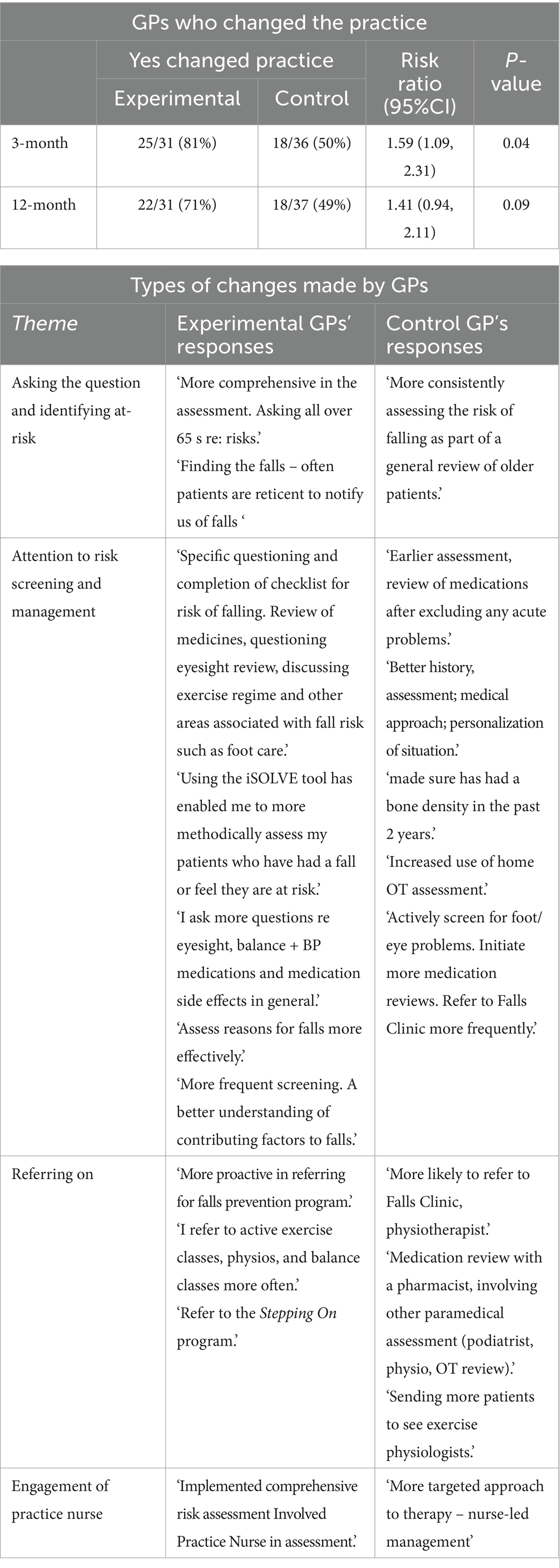
Both groups reported change in practice. Experimental GPs were significantly (p = 0.04) more likely to have changed the way they managed their older patients who had had a fall and were 1.6 times more likely to have changed than those in the control group (Table 5). At 12 months, the risk ratio was smaller, though this may be due to the question only asking about changes in the past 3 months.
For those who answered ‘yes,’ content analysis of their comments about how they changed practice revealed change across four themes: ‘Asking the question and identifying at-risk,’ ‘Attention to risk screening and management, ‘Referring on,’ and ‘Engagement of practice nurse’ (examples in Table 5). While more experimental GPs reported change, both groups demonstrated change. Overall, those in the experimental group reported change across more preventive dimensions, often reporting a more ‘proactive’ and comprehensive approach involving discussion with their patients. The control GPs were most likely to focus on medical risk factors and predominantly on referral, which reflected their knowledge of fall prevention and increased knowledge of local referral options, particularly those listed in the survey. A few practices in both groups (six experimental, five control) involved their practice nurse implementing iSOLVE.
3.2.2.2 Challenges to doing fall prevention
Content analysis of GP responses to challenges in doing fall prevention in their practice was explored in the context of ‘yes’ or ‘no’ answers to items indicating change in practice. In the experimental group, responses to challenges at each follow-up were provided by 17 who reported practice change and two who reported no change. There were an additional 12 GPs who reported practice change in one survey and no change in the other. In the control group, responses to challenges at each follow-up were provided by 13 GPs who reported practice change and 8 GPs who reported no change. An additional 16 GPs reported practice change in one survey and no change in the other.
The most common challenge theme for the experimental group that reported change in practice was patient factors (such as patient reluctance), which were closely followed by time. Other themes were service issues, and several GPs reported the complexity/frailty of their fall patients. For those experimental GPs who did not report a change in practice, the most common theme was time. The most common issues for the control group who reported change in practice were patient factors, followed by comorbidity/frailty, service issues, and time. These findings were similar for the control GPs, who reported no change in practice.
There were further differences, similar to the challenges between the experimental and control groups. It appeared that many experimental GPs practicing fall prevention at 12 months also recognized challenges that can make it difficult to be thorough. For example, one GP whose practice change was expressed as ‘Assess reasons for falls more effectively’ also noted challenges of ‘Patients are often resistant to change (SIC) their behavior. Often not enough time to do a thorough job.’ Control GPs tended to see multiple problems and more often associated falls with a person who, as one GP expressed, ‘tends to be frail, older adult, has difficulty, and (therefore) is disinterested in participating in (fall) management.’ Another responded, ‘It is a multifactorial problem, often part of the complex clinical setting, and there are so many things to consider.’ The experimental group tended to be more succinct and often focused on convincing their patients of the importance of fall prevention, as one GP stated, ‘Convincing patients that they are a fall risk. Older adult men are not convinced until they have a fall’. Time constraints for the experimental group were often mentioned as the ‘time it takes’ or the time to conduct a ‘full fall prevention.’ The control group saw more complexities around accessing service providers and were unsure of services, issues that were much less evident in the experimental group. The control group GPs more often listed practical issues of transport, home environment hazards, and mobility aids.
3.2.2.3 Engagement in fall prevention: assessing fall risk, reviewing medications, and providing advice
A total of 66 participating GPs answered the three questions about assessing risk, reviewing medications, and providing advice at both baseline and 3 months. The model estimate of the engagement score was significantly higher (0.98 units, 95%CI 0.36 to 1.60) (p = 0.002) in the experimental group than the controls at 3 months, after adjusting for baseline score and stratification (see Table 6).
The estimated intra-cluster correlation (ICC) was 0, indicating no clustering by practice. Among the 68 GPs who responded to all three questions at both baseline and 12 months, the engagement score in the experimental group was significantly higher by 0.90 units (95%CI 0.33 to 1.46; p = 0.002) compared to the experimental group at 12 months. This result accounts for adjustments based on baseline scores and stratification, confirming the effectiveness of the intervention in improving engagement.
3.2.2.4 Engagement in fall prevention: referral behavior
More than half of the GPs in the experimental group (55%) used the Active and Healthy Website to find local exercise and fall prevention classes at 3 months, an increase from 6% at baseline, and this was largely maintained at 12 months (42%). Usage by control GPs remained at only 2–3% over 3 months and increased to 14% at 12 months.
Table 7 outlines the practitioners and programs to which the GPs referred their older patients at risk of falls (% sometimes/often). Among the GPs who answered at both baseline and 3 months (Table 6), the model estimate of the referral score, out of a possible 13, was significantly higher (1.10 units, 95%CI 0.02 to 2.18) in the experimental group than the controls (p = 0.045) at 3-months, after adjusting for baseline score, clustering, and stratification. The estimated intra-cluster correlation was ICC = 0. Among the GPs who answered the question at both baseline and 12 months, the model estimate of the referral score was higher but not significant (1.29 units, 95%CI −0.38 to 2.97) (p = 0.13) in the experimental group than control at 12 months, after adjusting for baseline score, clustering, and stratification. In this case, there was clustering by practice, with an estimated ICC = 0.39.
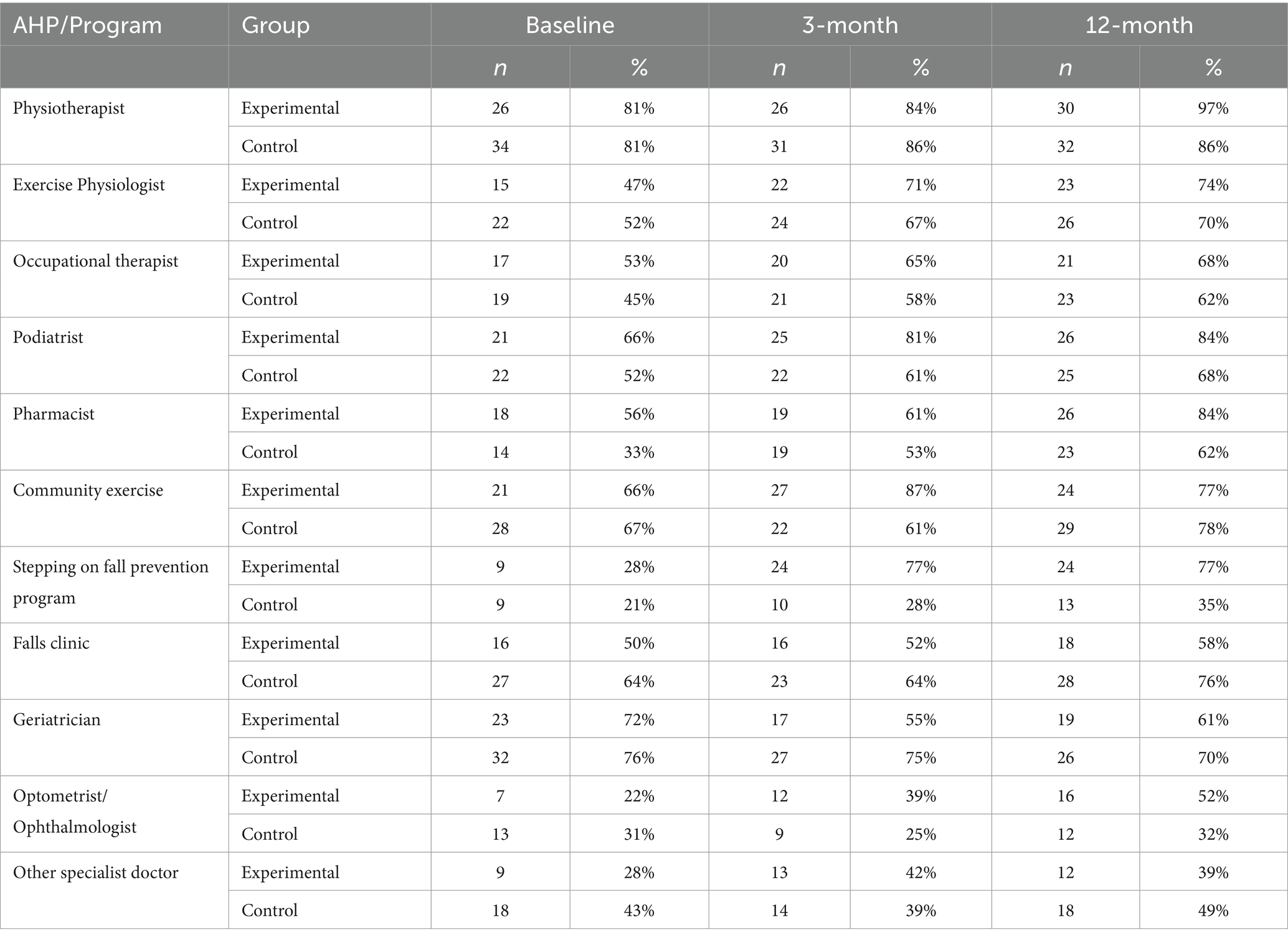
Table 7. Referral by trial GP to practitioner/program: ‘Sometimes or often’ refer older patients at risk of falling.
Physiotherapists were the most common practitioners with high referrals at all time points. The three-month referral difference appears to be driven by a very large increase in referrals to the Stepping On fall prevention program and larger increases than controls in referrals to exercise physiologists, podiatrists, community exercise, and optometrists/ophthalmologists. At 12 months referrals across services were more balanced between the two groups, though for the experimental group still remained a higher proportion for Stepping On programs and for the control group a higher proportion to Fall Clinics, geriatricians, and other specialist doctors.
3.2.3 Patient engagement in fall prevention, interaction with GP, fall and medication outcomes
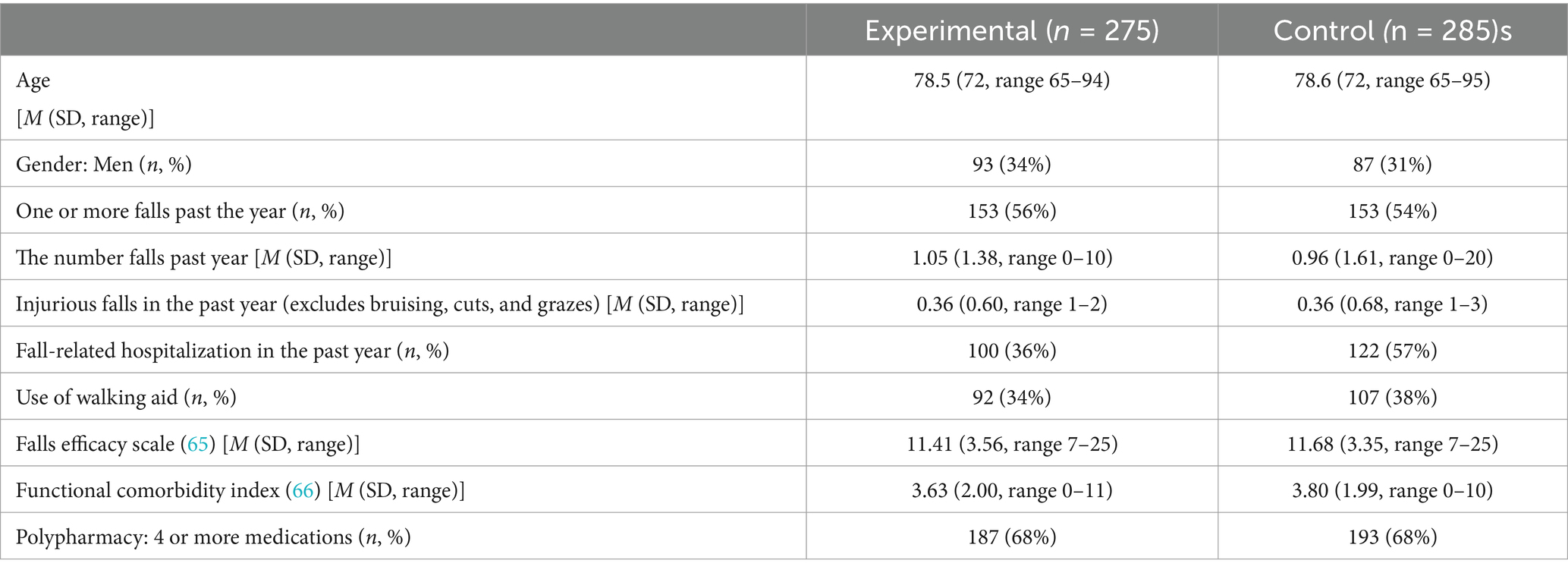
In the experimental group, 275 patients were recruited from 30 enrolled GPs (mean 9.2 patients per GP, range 4–35). In the control group, 285 patients were recruited from 37 enrolled GPs (mean 7.7 patients per GP, range 3–35) (Supplementary Appendix 7—patient sample per practice).
Figure 3 shows a flowchart of patients in the cluster RCT, and Table 8 outlines the patient’s characteristics at baseline. There was a high percentage of patients (over 50%) who had a history of one or more falls in the past year, with half of these reporting multiple falls (50% experimental, 41% control), reflecting the subgroup of recruited patients who were at high risk of falling.
At 12 months, patients were asked what they had done in the past year to help them prevent falls (Table 9). Seventy-nine percent of experimental (n = 216, mean = 2.4, SD 1.5) and 69% of control patients (n = 196, mean = 1.6, SD 1.5) reported one or more fall prevention activities, the median of both being two and maximum six. Three types of activities indicated significantly higher engagement by experimental patients: prescribed home exercise, fall prevention program, and medication review. There was also a significant difference, with the experimental group being 1.9 times more likely to ‘change their ways’ to prevent falls.

Table 9. Participating patient engagement in fall prevention and fall-related interactions with GP, including referrals from GP.
Table 9 also shows the percentage of patients reporting interactions with their GP related to fall prevention, with the experimental group more likely to interact with their GP. Patient recall of referral by GP for fall prevention for both groups was low (10–21%), though significantly different between groups.
3.2.3.1 Patient fall outcomes
There was a mean of 1.52 (SD 2.68) falls (range 0–27) in the experimental group and 1.67 (SD 3.70) falls (range 0–49) in the control group. There were 60% (n = 164) of patients in the experimental group who fell one or more times in the 12-month follow-up period, compared with 57% (n = 161) in the control group (Supplementary Appendix 8—total falls and time in a trial). The analysis showed no effect of the iSOLVE intervention in reducing the number of falls, with an estimated incidence rate ratio of 0.96 (95% CI: 0.77 to 1.20; n = 570). This means little or no difference in the rate of falls (4% reduction), with a wide confidence interval from 23% fewer falls to 20% more falls.
3.2.3.2 Patient medication outcomes
The mean number of fall risk-increasing drugs at baseline was 2.1 ± 2.0 (control group) and 1.8 ± 1.6 (experimental group, p < 0.05). The mean change in the number of fall-risk-increasing drugs from baseline to 12 months was an increase of 0.11 ± 0.05 in the control group and 0.14 ± 0.04 in the intervention group (n.s.). The fall risk-increasing drug classes that were ceased most commonly were diuretics, calcium channel blockers, ACE inhibitors/angiotensin, and two receptor antagonists in both the experimental and control groups.
3.3 Convergence—in-depth interviews with GPs (experimental group) and AHPs
Interviews with the GPs in the experimental group (n = 24, 75%) enabled an in-depth perspective on their experience of embedding fall prevention in their everyday practice over time and reported elsewhere (15). Six themes were identified: (i) making it easy to ask the iSOLVE questions, (ii) internalizing the process, (iii) integrating the iSOLVE into routine practice, (iv) addressing assumptions about patients and fall prevention, (v) the degree of change in practice, and (vi) contextual issues influencing uptake.
In interviews with AHPs (n = 15) who attended the upskilling workshops, four major themes emerged and were reported elsewhere (14). These were (i) AHPs valued fall prevention in practice as they recognized benefits for themselves and their clients, (ii) AHPs recognized the complexity of fall prevention work, such as complex clients, relationships with other health professionals, and changing funding environments, (iii) AHPs worked through complexities according to client demographics and issues with running a business, and (iv) strategies adopted for integrating fall prevention into routine practice included asking every client about falls, being aware of falls as relevant to many clients, having processes in place to assess clients for risk of falls, and having a structured program for fall prevention.
3.4 Diffusion—area-wide annual survey 2016–2019
Response rates to the area-wide GP survey averaged 20–28% [2016 (n = 81), 2017 (n = 155), 2018 (n = 124)] for the first 3 years of sampling, and in the final year (2019) were 15% (n = 202) when sent to all GPs in the area. Surveys totaled 562 (overall response rate 20%) from 2,847 invitations. Across all surveys, 7% had <5 years practicing as a GP, 10% had between 5 and 10 years, and 83% had >10 years’ experience. Across all surveys, 20% of GPs estimated they saw less than 20% of patients 65 years and over, 53% estimated 20–40, 18% estimated 40–60, 8% estimated 60–80, and 1% of GPs had higher than 80% of patients 65 years and over.
3.4.1 GP engagement in fall prevention, including referral behavior
GP engagement in assessing fall risk, reviewing medications, and providing advice did not significantly change from 2016 to 2019. Overall referrals for fall prevention to AHPs increased significantly from 70% in 2016 to 82% in 2019 (χ2 = 4.85, df = 1, p = 0.028). Type of referrals showed that referrals to Falls Clinics (χ2 = 6.02, p = 0.014, df = 1) and the Stepping On Fall Prevention Program (χ2 = 9.37, p = 0.002, df = 1) increased significantly, but others (physiotherapist, exercise physiologist, occupational therapist, community exercise class, and pharmacist) were unchanged. Reported familiarity with fall prevention services in the local area significantly increased from just over half (51%) in 2016 to almost three-quarters (72%) in 2019 (χ2 = 10.41, p = 0.001, df = 1), though the use of the NSW Health Department Active and Healthy website to refer to local exercise classes remained low (4–7%) (see Supplementary Appendix 9 for a full description).
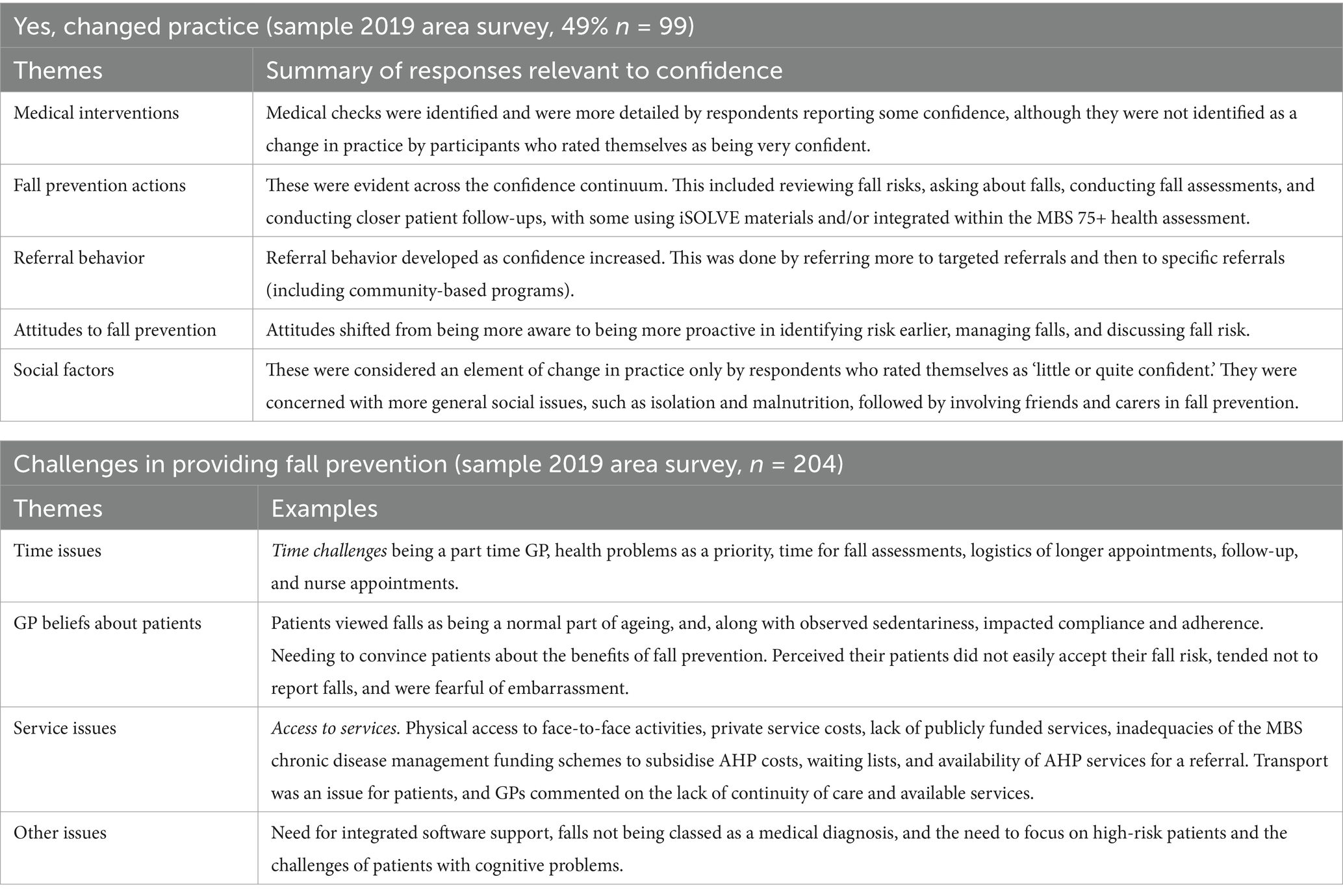
3.4.2 Changes in practice
In the final 2019 annual survey, a free-text question asked how GPs changed practice and the challenges they encountered. Changes in practice were analyzed in the context of the GPs’ confidence level in fall prevention. Half the GP respondents (n = 99, 49%) indicated changes had been made to practice, and all of them indicated some level of confidence: 29% rated themselves as having a little confidence, 62% quite confident, and 9% as very confident.
Five key themes emerged in the free-text responses relating to changes in practice: medical interventions, fall prevention actions, referral behavior, attitudes to fall prevention, and social factors. Responses varied markedly in those who reported increased confidence and are summarized in Table 10.
All 204 respondents commented on challenges to providing fall prevention, with themes of time issues, GP beliefs about patients, service issues, and other issues such as patient characteristics (Table 10). Those who were very confident and had made changes to their practice described being intentional about providing fall prevention for their patients, whereas less confident respondents who made changes tended to be less proactive and more often externalized the challenges (e.g., the patient being negative, lacking insight; no practice nurse support). Regardless of GP confidence levels or change in practice, dominant challenges were aspects of limited time to undertake fall prevention activities and beliefs about perceived patient acceptance of risk or reluctance to change. However, more confident people were proactive despite these and other challenges. Those who did not change practice for each level of confidence reported a much larger list of challenges than those who did make changes. A very small number of GPs who rated themselves as not confident (n = 4) made no changes to their practice in fall prevention. This group tended to be less positive about fall prevention and were not convinced it was beneficial.
3.5 Reflection and expansion
A reflective review by the research team of the iSOLVE process and findings enabled the mapping of iSOLVE elements to effective implementation change strategies (21–23), as presented in Table 11. This provides a better understanding of key elements driving change in practice. These learnings from the project were used to frame the approach in translating the iSOLVE resources online so they continue to be efficient, available, and accessible. Working with the PHN, the process was also embedded in their Health Pathways (43), a local online resource for general practice, and ongoing access to the AHP mapping (30).
As it was found overall that it was not workable to embed the Decision Tool in the commercial software (Topbar), the final product was an online website managed by the New South Wales State Falls Network. Thus, the planned dissemination document as per our protocol (12) was replaced by online resources for general practice, which include an interactive GP fall risk assessment (44) and downloadable paper versions of the patient Stay Independent checklist, GP fall risk assessment, and Tailoring interventions to fall risk factors (27). We also developed GP learning modules that provide an alternative to face-to-face educational detailing and a clinical audit activity eligible for GP Continuing Professional Development points (45). Online learning modules for AHPs are in development (45), and recorded workshops are available online (29).
4 Discussion
4.1 Our findings
This project was designed to influence clinical practice and address gaps in fall prevention across primary care, and our results were equally complex. Overall, our data provides insight into a number of mechanisms within a pragmatically implemented, multifaceted fall prevention process, which can improve GPs’ and AHPs’ engagement in fall prevention for older adults in the community.
The PHN area had a strong level of engagement by AHPs, particularly by physiotherapists, occupational therapists, exercise physiologists, pharmacists, and those delivering fall prevention group programs. This engagement was reflected by interest in both the workshops and mapping exercise, along with AHPs’ survey responses, demonstrating a high knowledge base. Post-workshop changes reflected increased confidence in fall prevention overall, and responses showed multiple enhancements in how they delivered fall prevention. The AHPs worked across sectors in the community, and referrals were from multiple sources, including GPs and between AHP disciplines. Our interviews with AHPs who attended the workshops (14) provide complementary evidence of how they valued fall prevention in their practice, recognized challenges in working alongside other health professionals, and appreciated a better understanding of others’ roles through the iSOLVE workshops. They reported concerns about complicated and changing funding systems impacting sustainable fall prevention. GPs value ‘reliable and good’ AHPs, with trust developing over time, though the patient more often delivers the feedback they receive than by the AHP (13).
We found GPs could change practice and engage in fall prevention. While both control and experimental GPs engaged in fall prevention, the experimental group was significantly higher at both time points for assessing fall risk, reviewing medications, and providing advice. Referral behavior was significantly higher for the experimental group at 3 months but not at 12 months, when the control group had increased their rate of referrals. Responses to free-text questions about practice change highlighted nuanced differences, with the experimental group reporting a more proactive and comprehensive approach compared to the control group, who were more likely to focus on medical risk factors and predominately on referral to specialists and Falls Clinics, reflecting their understanding of fall prevention. The GP software to support the GP management of patients at risk of falls did not work for all GP practices due to technical problems, but they could effectively use the paper alternatives (15).
Both experimental and control GPs reported challenges, in particular patient-related factors and time constraints. However, there were differences in the frequency and nature of how these challenges were perceived. Despite the challenges, more experimental GPs reported change in practice, and more often, they reported challenges centered around the thoroughness needed to identify and manage falls for their older patients. The control GPs focused on frailer patients with multiple problems, the complexities of accessing service providers, and practical issues such as transport. It appeared that their perceived role in the management of falls differed. A minority expressed that fall prevention was not worthwhile.
Interviews with experimental GPs (15) support and extend the findings of the GP trial survey. Groups that changed practice talked about how they engaged in the process as a simple’ system’ and provided ‘fall scripts’ to follow in what can be done and said. Over time, the process was internalized, where they asked their patients more in-depth questions. The opportunity to ‘practice’ with their at-risk patients was a process that appeared important in moving fall management to routine practice.
The outcome for the subgroup of GP patients did not translate to a significant increase or decrease in falls. The higher engagement of both control and experimental patient groups may reflect the area’s AHP activity, and contamination may occur when running an embedded trial in a broader implementation study. Engagement in fall prevention activities was moderate for both participating patient groups. However, the experimental group significantly engaged more often in interventions supported by robust evidence, that is, medication reviews by a GP or pharmacist (46), prescribed home exercises (5), and in a multicomponent fall prevention program (7). Our project provided extensive upskilling of AHPs in the study area who also reported multiple sources of referrals to them, including self-referrals. Our fall outcome was similar to the previous systematic review, (4) in which change in participant falls relied on GP referrals to others. While our experimental GPs engaged in broader fall management than referrals alone, the cluster RCT still relied on the small sample of participating patients initiating a referral with their GP. Recall of being referred for fall prevention by their GP was low (10–20%) in both groups. The Mackenzie et al. systematic review demonstrated a significant reduction in fall-related injury (10), which our trial was not powered to test.
The GP annual survey showed trends for change within the broad geographic area of the PHN. Familiarity with fall services significantly increased from 50% to over 70%, and the use of evidence-based fall prevention also increased, such as the Stepping On Fall Prevention program, community exercise, and Falls Clinic. While this finding is promising, more work is needed to understand and enable implementation more widely. In addition to iSOLVE activities, strong relationships with PHN staff enabled the iSOLVE resources to be included in their fall prevention Health Pathways (a guiding online resource for GP practice) (43), and they continued their commitment to GP and AHP education beyond the trial.
4.2 Relevance to current practice
Numerous studies have evaluated the implementation of the STEADi algorithm and workflow practices in the US (47–49), which we drew on as a basis for the iSOLVE Decision Tool. Our findings are novel in that GPs, through supported workflow practice, can change practice and engage in fall prevention, not just in screening for fall risk. The US study outcomes have focused largely on increased screening (49–52), with one study demonstrating a reduction in fall-related hospitalizations (52). In the US, some organizations have been able to embed the STEADi algorithm into electronic medical records, whereas we relied on external software, websites, or paper versions. However, a consistent finding is the importance of GPs in familiarizing themselves with the workflow (48, 50), supporting our findings of internalizing the process (15). As we found, the patient Stay Independent checklist was critical in simplifying the screening process, particularly focusing on the three key questions (fall in the past year, worried about falling, feeling unsteady) (51).
There are competing interests for GPs, and there is a shift from traditional medical approaches to a belief that a GP’s role can be to engage in fall management and prevention. Barriers related to the complexity of patient care time demands and other practical issues, such as transport, were supported in our interviews (14) and others (48, 53, 54). Yet our study, like those in the US (STEADi) (48–50), has demonstrated workflow support’s importance in mediating these challenges. Our GPs who were more confident and changed practice more often reported a more ‘proactive’ and comprehensive approach, involving discussion with their patients and less on the practical restraints.
GPs were surprised when ‘asking the question’ about a fall identified younger, less frail older adults who fall. Fall prevention actions need to address the needs of diverse groups of older people at lower, intermediate, and high risk of falls (1, 55, 56). Capturing those at intermediate risk who do not have multiple risk factors but have had a fall could have a greater longer-term preventive impact.
We articulated and reflected on what we observed as key drivers of change. These provide important lessons for wider implementation. A central part was a relevant and simple system, training, documentation, and resources. Vandervelde et al. (57), in their review of implementation strategies in fall prevention, found such technical assistance a key strategy. More work is needed for longer-term sustainability and maintenance, such as establishing partnerships, continuing commitment to fall prevention, improving communication and collaboration between multiple professionals, and ongoing attention to drivers of change (47). The barriers and facilitators of implementing fall prevention in primary care in the iSOLVE project aligned closely with those identified in the STEADI initiative (48). Since fall prevention has proven to be cost-effective (6, 58, 59) and can reduce hospitalization and mediate fall-related health services (8, 9), widespread dissemination of the iSOLVE Decision Tool and resources is warranted. The PHN is important in educating and supporting general practice and AHPs in fall prevention.
In Australia, a financial incentive for chronic disease management in general practice is available in the form of five MBS-subsidized allied health services annually. However, this scheme is underutilized for fall prevention for various reasons (3). Despite the indication of these items being effective for fall prevention in primary care (60), professionals providing services using this scheme reported inadequate reimbursement and needing to charge patients for additional expenses, insufficient numbers of items per year to provide high-quality care, and the administrative burden on the professionals to use the system (61). Sustainable reimbursement mechanisms are needed to support integrated care in the future.
Our intervention targeted changes in general practice and increased referrals to AHPs, a crucial part of fall prevention management. A novel aspect of our approach was the emphasis on upskilling AHPs, training them comprehensively, and enhancing GP awareness of the roles, range of expertise, and contact pathways for AHPs. The PHN area demonstrated high AHP engagement; however, expanding these services to meet rising demand in this and other regions will depend on fostering cross-sectorial partnerships. Further research is needed to cultivate and embed these relationships within healthcare systems (48, 57).
Referral systems for fall prevention have previously been described as fragmented (47). The reality is that fall prevention requires cross-sectorial collaboration, operating within a matrix of referral patterns and funding coalitions. Each sector plays a critical role in developing fall prevention pathways. For example, fall-related ambulance callouts could incorporate the iSOLVE patient Stay Independent checklist, facilitating referrals to GPs or directly them to AHPs, such as occupational therapy therapists, for home visits. Our findings showed active cross-referrals between AHPs to address patient needs (13).
In our project, the PHN acknowledged the importance of and actively participated in providing educational support for GPs and AHPs. Leadership and engagement in public health and primary care remain vital (48, 62), aligning with increasing calls for policy action to strengthen these systems (55).
4.3 Strengths and weaknesses
The strength of this project in exploring practice change lies in the opportunity to triangulate findings using multiple methods. Rigorous investigation of key questions was achieved through a combination of quantitative and qualitative data, supported by interviews with study participants (13–15). While surveys and interviews may be subject to social desirability bias, the primary objective was to examine the personal experiences of health professionals in their engagement with the iSOLVE program.
The inclusion of qualitative data in a pragmatic trial is a well-established approach to assessing the real-world application of an intervention (16, 17). Additionally, response rates to the annual area-wide surveys are considered reasonable (63, 64), given that the total population comprised GPs within the PHN area.
This implementation project enabled shared resources and the development of knowledge over time. It is likely that, given the pragmatic nature of the project, multiple elements of introduced bias and potential contamination occurred that influenced the embedded trial results. For example, parallel work in upskilling AHPs, trial surveys, and area-wide surveys may have raised awareness of fall prevention options. The study focused on a specific geographic area, and the findings might not be generalizable to all GP populations without further research.
5 Conclusion
This project has shown that GPs can successfully change practice and engage in fall prevention by equipping them with resources and strategies to become more proactive in preventing falls among their older patients. Our emphasis on facilitating evidence-based approaches, partnerships, and referral processes was crucial to this project. The project’s intent was implementation, and the goal for GPs was to implement the process routinely with all their older patients. The experimental GPs were more likely to be comprehensive in their approach, and they perceived their role in fall prevention differently. Previously, their focus might have been primarily on diagnosing and treating specific diseases. We recognized the competing demands on GPs’ time, so fall prevention processes must be relevant and easy to use in busy GP practices.
From this project, we produced a range of useful and accessible resources and a decision tool that is now freely available to general practice. By empowering GPs to proactively address fall prevention, the iSOLVE process has the potential to significantly reduce fall-related injuries. AHPs are vital in fall prevention and facilitating relationships and connectedness across primary care networks. Further, the PHN can be crucial in promoting and supporting fall prevention and facilitating referral pathways. Work is needed to implement what is learned from this and other implementation studies across primary care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material. Further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving humans were approved by the Human Research Ethics Committee of the University of Sydney (2014/316, 2014/848). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ML: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CR: Conceptualization, Funding acquisition, Investigation, Methodology, Software, Validation, Writing – review & editing. RP: Conceptualization, Funding acquisition, Investigation, Methodology, Validation, Writing – review & editing. CS: Conceptualization, Funding acquisition, Investigation, Methodology, Validation, Writing – review & editing. ACWT: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. CP: Conceptualization, Investigation, Methodology, Software, Validation, Writing – review & editing. SP: Conceptualization, Funding acquisition, Investigation, Methodology, Software, Validation, Writing – review & editing. AT: Conceptualization, Investigation, Methodology, Validation, Writing – review & editing. LL: Conceptualization, Investigation, Methodology, Validation, Writing – review & editing. SH: Formal analysis, Methodology, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The project was supported by a National Health and Medical Research Council (NHMRC) Partnership grant 1072790.
Acknowledgments
The iSOLVE team would like to acknowledge the following for their assistance with the project. Di Sfiligoi from the former Northern Sydney Medicare Local and Cynthia Stanton, Deborah Pallavicini, Brooke Jay, and Alexandra Jaksetic from Sydney North Health Network for their partnership and assistance with developing and supporting iSOLVE within their network. The iSOLVE advisory group for their advice and feedback during the course of the project: consumer representative Mary Potter; GPs from the network John Renju and Alexandra Fletcher; Northern Sydney Local Health District Falls Prevention Coordinator Margaret Armstrong, physiotherapists Amanda Cooke and Sharon Butler, exercise physiologist Michael Kline, Stepping On coordinator Nadia Williams, occupational therapist Liz Irwin, clinical consultant pharmacist Elizabeth Sabolch, registered nurse Jan Eaton, and podiatrists Andrew Scown and Shawn Tomkins. We thank Lisa Kouladjian O’Donnell, consultant pharmacist, for assistance with the design, data collection and education for the medication review intervention. We also wish to thank James Tracy (Senior Learning Designer) for his assistance in web design and coding structure for the GP learning module and clinical audit courses and Marguerite Tracy (Senior Lecturer in General Practice, The University of Sydney) for her assistance and advice in setting the modules as Continuing Professional Development.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1446525/full#supplementary-material
References
1. Australian Commission on Safety and Quality in Healthcare. Preventing falls and harm from falls in older people - best practice guidelines for Australian community care. (2009). Available at: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/preventing-falls-and-harm-falls-older-people-best-practice-guidelines-australian-community-care (Accessed November 23, 2024).
2. Grant, A, Mackenzie, L, and Clemson, L. How do general practitioners engage with allied health practitioners to prevent falls in older people? An exploratory qualitative study. Australas J Ageing. (2015) 34:149–54. doi: 10.1111/ajag.12157
3. Mackenzie, L, Clemson, L, and Irving, D. Fall prevention in primary care using chronic disease management plans: a process evaluation of provider and consumer perspectives. Aust Occup Ther J. (2020) 67:22–30. doi: 10.1111/1440-1630.12618
4. Lord, SR, Sherrington, C, and Naganathan, V. Falls in older people: Risk factors, strategies for prevention and implications for practice. 3rd ed. Cambridge: Cambridge University Press (2021).
5. Sherrington, C, Fairhall, NJ, Wallbank, GK, Tiedemann, A, Michaleff, ZA, Howard, K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. (2019) 1:Cd012424.
6. Clemson, L, Stark, S, Pighills, AC, Fairhall, NJ, Lamb, SE, Ali, J, et al. Environmental interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. (2023) 3:Cd013258.
7. Hopewell, S, Adedire, O, Copsey, BJ, Boniface, GJ, Sherrington, C, Clemson, L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. (2018) 7:Cd012221.
8. Paul, SS, Khalatbari-Soltani, S, Dolja-Gore, X, Clemson, L, Lord, SR, Harvey, L, et al. Fall-related health service use in stepping on programme participants and matched controls: a non-randomised observational trial within the 45 and up study. Age Ageing. (2022) 51:afac272. doi: 10.1093/ageing/afac272
9. Ford, JH 2nd, Abramson, B, Wise, M, Dattalo, M, and Mahoney, JE. Bringing healthy aging to scale: a randomized trial of a quality improvement intervention to increase adoption of evidence-based health promotion programs by community partners. J Public Health Manag Pract. (2017) 23:e17–24. doi: 10.1097/PHH.0000000000000503
10. Mackenzie, L, Beavis, AM, Tan, ACW, and Clemson, L. Systematic review and Meta-analysis of intervention studies with general practitioner involvement focused on falls prevention for community-dwelling older people. J Aging Health. (2020) 32:1562–78. doi: 10.1177/0898264320945168
11. Stevens, JA, and Phelan, EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract. (2013) 14:706–14. doi: 10.1177/1524839912463576
12. Clemson, L, Mackenzie, L, Roberts, C, Poulos, R, Tan, A, Lovarini, M, et al. Integrated solutions for sustainable fall prevention in primary care, the iSOLVE project: a type 2 hybrid effectiveness-implementation design. Implement Sci. (2017) 12:12. doi: 10.1186/s13012-016-0529-9
13. Liddle, J, Clemson, L, Mackenzie, L, Lovarini, M, Tan, A, Pit, SW, et al. Influences on general practitioner referral to allied health professionals for fall prevention in primary care. Australas J Ageing. (2020) 39:e32–9. doi: 10.1111/ajag.12680
14. Liddle, J, Lovarini, M, Clemson, L, Mackenzie, L, Tan, A, Pit, SW, et al. Making fall prevention routine in primary care practice: perspectives of allied health professionals. BMC Health Serv Res. (2018) 18:598.
15. Mackenzie, L, Liddle, J, Clemson, LM, Tan, ACW, Lovarini, M, Pit, SW, et al. Perspectives of Australian GPs on tailoring fall risk management: a qualitative study. Aust J Prim Health. (2021) 27:409–15. doi: 10.1071/PY21022
16. Curran, GM, Bauer, M, Mittman, B, Pyne, JM, and Stetler, C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. (2012) 50:217–26. doi: 10.1097/MLR.0b013e3182408812
17. Collins, KMT, Onwuegbuzie, AJ, and Jiao, QG. A mixed methods investigation of mixed methods sampling designs in social and health science research. J Mixed Methods Res. (2007) 1:267–94. doi: 10.1177/1558689807299526
18. Edmunds, JA, Gicheva, D, Thrift, B, and Hull, M. Using mixed methods to explore variations in impact within RCTs: the case of project COMPASS. J Mixed Methods Res. (2022) 16:478–99. doi: 10.1177/15586898211033144
19. Palinkas, LA, Horwitz, SM, Chamberlain, P, Hurlburt, MS, and Landsverk, J. Mixed-methods designs in mental health services research: a review. Psychiatr Serv. (2011) 62:255–63. doi: 10.1176/ps.62.3.pss6203_0255
20. Gilmer, TP, Katz, ML, Stefancic, A, and Palinkas, LA. Variation in the implementation of California’s full service partnerships for persons with serious mental illness. Health Serv Res. (2013) 48:2245–67. doi: 10.1111/1475-6773.12119
21. Graham, ID, Logan, J, Harrison, MB, Straus, SE, Tetroe, J, Caswell, W, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. (2006) 26:13–24. doi: 10.1002/chp.47
22. Michie, S, van Stralen, MM, and West, R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42.
23. Lau, R, Stevenson, F, Ong, BN, Dziedzic, K, Treweek, S, Eldridge, S, et al. Achieving change in primary care--causes of the evidence to practice gap: systematic reviews of reviews. Implement Sci. (2016) 11:40. doi: 10.1186/s13012-016-0396-4
24. Lengnick-Hall, R, Gerke, DR, Proctor, EK, Bunger, AC, Phillips, RJ, Martin, JK, et al. Six practical recommendations for improved implementation outcomes reporting. Implement Sci. (2022) 17:16.
25. Shubert, TE, Smith, ML, Prizer, LP, and Ory, MG. Complexities of fall prevention in clinical settings: a commentary. Gerontologist. (2014) 54:550–8. doi: 10.1093/geront/gnt079
26. Rubenstein, LZ, Vivrette, R, Harker, JO, Stevens, JA, and Kramer, BJ. Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. J Saf Res. (2011) 42:493–9. doi: 10.1016/j.jsr.2011.08.006
27. Clemson, L, Mackenzie, L, Roberts, C, Pond, D, Tan, A, Liddle, J, et al. Preventing falls in older patients in the community – Provider resource: NSW fall prevention and healthy ageing network (2019). Available at: https://fallspreventiononlineworkshops.com.au/wp-content/uploads/2018/07/Complete_Provider_Resource.pdf or https://fallspreventiononlineworkshops.com.au/resources/#gp (Accessed February 20, 2024)
28. Bengtsson, M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. (2016) 2:8–14. doi: 10.1016/j.npls.2016.01.001
29. ArmchairMedical. Fall prevention. (2017). Available at: https://conferences.armchairmedical.tv/falls-prevention (Accessed November 9, 2023)
30. Sydney North Health Network. iSOLVE - northern Sydney fall prevention referral options. Available at: https://services.chillidb.com/WebControls/Organisations/?Guid=b0171cbb-816b-4c22-bef8-5331ced403eb&InstanceID=37 (Accessed 12 March, 2024).
31. Campbell, MK, Piaggio, G, Elbourne, DR, and Altman, DG. Consort 2010 statement: extension to cluster randomised trials. BMJ. (2012) 345:e5661. doi: 10.1136/bmj.e5661
32. Robertson, MC, Campbell, AJ, Gardner, MM, and Devlin, N. Preventing injuries in older people by preventing falls: a meta-analysis of individual-level data. J Am Geriatr Soc. (2002) 50:905–11. doi: 10.1046/j.1532-5415.2002.50218.x
33. Tan, ACW, Clemson, L, Mackenzie, L, Sherrington, C, Roberts, C, Tiedemann, A, et al. Strategies for recruitment in general practice settings: the iSOLVE fall prevention pragmatic cluster randomised controlled trial. BMC Med Res Methodol. (2019) 19:236.
34. Yee, M, Simpson-Young, V, Paton, R, and Zuo, Y. How do GPs want to learn in the digital era? Aust Fam Physician. (2014) 43:399–402.
35. Van Hoof, TJ, Harrison, LG, Miller, NE, Pappas, MS, and Fischer, MA. Characteristics of academic detailing: results of a literature review. Am Health Drug Benefits. (2015) 8:414–22.
36. Osmond, J, and Darlington, Y. Reflective analysis: techniques for facilitating reflection. Aust Soc Work. (2005) 58:3–14. doi: 10.1111/j.0312-407X.2005.00179.x
37. Carson, KV, Verbiest, ME, Crone, MR, Brinn, MP, Esterman, AJ, Assendelft, WJ, et al. Training health professionals in smoking cessation. Cochrane Database Syst Rev. (2012) 2012:Cd000214.
38. Vaismoradi, M, Turunen, H, and Bondas, T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci. (2013) 15:398–405. doi: 10.1111/nhs.12048
40. Seppala, LJ, Petrovic, M, Ryg, J, Bahat, G, Topinkova, E, Szczerbińska, K, et al. STOPPFall (screening tool of older persons prescriptions in older adults with high fall risk): a Delphi study by the EuGMS task and finish group on fall-risk-increasing drugs. Age Ageing. (2021) 50:1189–99. doi: 10.1093/ageing/afaa249
41. Braun, V, and Clarke, V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. (2021) 18:328–52. doi: 10.1080/14780887.2020.1769238
42. Scammon, DL, Tomoaia-Cotisel, A, Day, RL, Day, J, Kim, J, Waitzman, NJ, et al. Connecting the dots and merging meaning: using mixed methods to study primary care delivery transformation. Health Serv Res. (2013) 48:2181–207. doi: 10.1111/1475-6773.12114
43. Sydney north HealthPathways: Sydney north health network (2024). Available at: https://sydneynorth.communityhealthpathways.org/28919.htm (Accessed May 6, 2024)
44. Clemson, L, Mackenzie, L, Roberts, C, Pond, D, Tan, A, Liddle, J, et al. iSOLVE GP fall risk assessment tool: NSW fall prevention and healthy ageing network (2019) Available at: https://fallspreventiononlineworkshops.com.au/tool/ (Accessed March 12, 2024).
45. Clemson, L, Mackenzie, L, Roberts, C, Pond, D, Tan, A, Liddle, J, et al. Fall prevention courses: NSW fall prevention and healthy ageing network (2019) Available at: https://fallspreventiononlineworkshops.com.au/courses/ (Accessed November 9, 2023)
46. Pit, SW, Byles, JE, Henry, DA, Holt, L, Hansen, V, and Bowman, DA. A quality use of medicines program for general practitioners and older people: a cluster randomised controlled trial. Med J Aust. (2007) 187:23–30. doi: 10.5694/j.1326-5377.2007.tb01110.x
47. Shubert, TE, Smith, ML, Schneider, EC, Wilson, AD, and Ory, MG. Commentary: public health system perspective on implementation of evidence-based fall-prevention strategies for older adults. Front Public Health. (2016) 4:252. doi: 10.3389/fpubh.2016.00252
48. Johnston, YA, Reome-Nedlik, C, Parker, EM, Bergen, G, Wentworth, L, and Bauer, M. Preventing falls among older adults in primary care: a mixed methods process evaluation using the RE-AIM framework. Gerontologist. (2023) 63:511–22. doi: 10.1093/geront/gnac111
49. Stevens, JA, Smith, ML, Parker, EM, Jiang, L, and Floyd, FD. Implementing a clinically based fall prevention program. Am J Lifestyle Med. (2020) 14:71–7. doi: 10.1177/1559827617716085
50. Casey, CM, Parker, EM, Winkler, G, Liu, X, Lambert, GH, and Eckstrom, E. Lessons learned from implementing CDC’s STEADI falls prevention algorithm in primary care. Gerontologist. (2017) 57:787–96. doi: 10.1093/geront/gnw074
51. Eckstrom, E, Parker, EM, Lambert, GH, Winkler, G, Dowler, D, and Casey, CM. Implementing STEADI in academic primary care to address older adult fall risk. Innov. Aging. (2017) 1:igx028. doi: 10.1093/geroni/igx028
52. Johnston, YA, Bergen, G, Bauer, M, Parker, EM, Wentworth, L, McFadden, M, et al. Implementation of the stopping elderly accidents, deaths, and injuries initiative in primary care: an outcome evaluation. Gerontologist. (2019) 59:1182–91. doi: 10.1093/geront/gny101
53. Meekes, WMA, Leemrijse, CJ, Weesie, YM, van de Goor, IAM, Donker, GA, and Korevaar, JC. Falls prevention at GP practices: a description of daily practice. BMC Fam Pract. (2021) 22:190. doi: 10.1186/s12875-021-01540-7
54. Landis, SE, and Galvin, SL. Implementation and assessment of a fall screening program in primary care practices. J Am Geriatr Soc. (2014) 62:2408–14. doi: 10.1111/jgs.13137
55. Lovitt, L, Clemson, L, Delbaere, K, Sherrington, C, Elkington, J, and Sturnieks, D. Fall prevention in NSW: White paper 2023. Sydney: NSW Government Clinical Excellence Commission (2023).
56. Montero-Odasso, M, van der Velde, N, Martin, FC, Petrovic, M, Tan, MP, Ryg, J, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. (2022) 51. doi: 10.1093/ageing/afac205
57. Vandervelde, S, Vlaeyen, E, de Casterlé, BD, Flamaing, J, Valy, S, Meurrens, J, et al. Strategies to implement multifactorial falls prevention interventions in community-dwelling older persons: a systematic review. Implement Sci. (2023) 18:4. doi: 10.1186/s13012-022-01257-w
58. Pinheiro, MB, Sherrington, C, Howard, K, Caldwell, P, Tiedemann, A, Wang, B, et al. Economic evaluations of fall prevention exercise programs: a systematic review. Br J Sports Med. (2022) 56:1353–65. doi: 10.1136/bjsports-2022-105747
59. Carande-Kulis, V, Stevens, JA, Florence, CS, Beattie, BL, and Arias, I. A cost-benefit analysis of three older adult fall prevention interventions. J Saf Res. (2015) 52:65–70. doi: 10.1016/j.jsr.2014.12.007
60. Mackenzie, L, and Clemson, L. Can chronic disease management plans including occupational therapy and physiotherapy services contribute to reducing falls risk in older people? Aust Fam Physician. (2014) 43:211–5.
61. Middlebrook, S, and Mackenzie, L. The enhanced primary care program and falls prevention: perceptions of private occupational therapists and physiotherapists. Australas J Ageing. (2012) 31:72–7. doi: 10.1111/j.1741-6612.2011.00527.x
62. Smith, ML, Schneider, EC, Byers, IN, Shubert, TE, Wilson, AD, Towne, SD Jr, et al. Reported systems changes and sustainability perceptions of three state departments of health implementing multi-faceted evidence-based fall prevention efforts. Front Public Health. (2017) 5:120. doi: 10.3389/fpubh.2017.00120
63. Alreck, PL, and Settle, RB. The survey research handbook. 3rd ed. New York: McGraw-Hill Education (2003).
65. Yardley, L, Beyer, N, Hauer, K, Kempen, G, Piot-Ziegler, C, and Todd, C. Development and initial validation of the falls efficacy scale-international (FES-I). Age Ageing. (2005) 34:614–9. doi: 10.1093/ageing/afi196
Keywords: general medical practice, family practice physicians, allied health, cluster randomized controlled trial, surveys, mixed-methods, parallel study design, fall prevention
Citation: Clemson L, Mackenzie L, Lovarini M, Roberts C, Poulos R, Sherrington C, Tan ACW, Simpson J, Pond CD, Pit S, Tiedemann A, Lovitt L and Hilmer SN (2024) Integrated solutions for sustainable fall prevention in primary care: a pragmatic hybrid-type 2 mixed methods implementation and effectiveness study. Front. Public Health. 12:1446525. doi: 10.3389/fpubh.2024.1446525
Edited by:
Nattawan Utoomprurkporn, Chulalongkorn University, ThailandReviewed by:
Tony Kuo, University of California, Los Angeles, United StatesSusan Patton, University of Arkansas, United States
Copyright © 2024 Clemson, Mackenzie, Lovarini, Roberts, Poulos, Sherrington, Tan, Simpson, Pond, Pit, Tiedemann, Lovitt and Hilmer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lindy Clemson, bGluZHkuY2xlbXNvbkBzeWRuZXkuZWR1LmF1
 Lindy Clemson
Lindy Clemson Lynette Mackenzie
Lynette Mackenzie Meryl Lovarini
Meryl Lovarini Christopher Roberts2
Christopher Roberts2 Roslyn Poulos
Roslyn Poulos Catherine Sherrington
Catherine Sherrington Amy C. W. Tan
Amy C. W. Tan Constance Dimity Pond
Constance Dimity Pond Anne Tiedemann
Anne Tiedemann Sarah N. Hilmer
Sarah N. Hilmer