- 1Faculty of Pharmacy, Jinnah University for Women, Karachi, Pakistan
- 2Faculty of Pharmacy, Karachi University, Karachi, Pakistan
- 3Faculty of Pharmacy, Jinnah Sindh Medical University, Karachi, Pakistan
- 4Department of Oncology, National Institute of Blood Diseases and Bone Marrow Transplant, Karachi, Pakistan
- 5Department of Clinical Oncology, Jinnah Postgraduate Medical Centre, Karachi, Pakistan
Introduction: Cancer, particularly breast cancer, is a major contributor to mortality and a significant impediment to life expectancy. In 2020, breast cancer accounted for 11.7% of all cancer cases and caused approximately 685,000 deaths worldwide, surpassing lung cancer in prevalence. The study aims to evaluate the impact of an educational intervention on breast cancer awareness among pharmacy students by comparing their understanding before and after the program.
Method: A pre-post quasi-experimental study was designed to assess knowledge and awareness of breast cancer, breast self-examination (BSE) practices, and attitudes toward breast cancer among female university students in Karachi, Pakistan. Participants completed a pre-session questionnaire, attended an awareness workshop and video tutorial, and then completed a post-session questionnaire 2 weeks later.
Results: Of 1,200 participants, 1,015 of them completed both the pre- and post-intervention questionnaires. Key demographic features included 83.9% of the participants being in the 18–24 age group, 26.8% being married, and only 14.2% having a family history of breast cancer. Before the intervention, 60.7% of the participants were not involved in regular breast self-exams due to a lack of awareness. Post-intervention results showed a significant increase in awareness, with 35.9% rising to 94.9%. The use of screening methods increased from 46.7 to 94.8%. Knowledge of breast cancer improved from 51.2 to 96.7%, and the general perception rose from 48.2 to 93.4%. Attitudes toward self-examination also shifted positively, indicating a significant change in perception.
Interpretation and conclusion: The study concludes the baseline knowledge of breast cancer among female students was inadequate but improved significantly from over 40% to over 90% following the educational intervention. The intervention positively influenced the general perception and attitudes toward breast cancer. These findings highlight the need for regular educational sessions to enhance awareness, improve healthcare outcomes, and reduce mortality rates, particularly in developing countries.
Introduction
Cancer remains a major contributor to global mortality, significantly impacting not only life expectancy but also the quality of life. While a notable decline in the mortality rates from coronary heart diseases and strokes has been observed, cancer continues to pose a significant threat. Among various cancer types, female breast cancer has emerged as a leading concern. In 2020, breast cancer surpassed lung cancer, accounting for 11.7% of all cancer cases globally. It also ranked as the ninth most common cause of death worldwide, with official reports documenting 685,000 deaths. Breast cancer is the most prevalent among women, affecting approximately 1 in 6 cancer-related deaths (159/185) and in 1 in 4 cancer cases globally (1).
In low-income countries, several factors contribute to the delayed diagnosis of breast cancer. These factors include limited resources, low awareness due to illiteracy, insufficient screening and inadequate treatment facilities, financial constraints, and cultural myths and hindrances. These obstacles prevent women from fully accessing available treatment options. Additionally, mobility restrictions further restrict their ability to seek appropriate healthcare services (2).
The most critical barrier to increasing awareness is the need for education. Adequate awareness of screening techniques, the importance of timely diagnosis, and proper clinical examinations can help women overcome structural and individual challenges, leading to more effective and cost-effective treatments.
Frequent breast cancer programs implemented in various local areas can significantly improve the alignment of clinically detectable diseases with timely and accurate diagnostic services, especially for women who show clear signs and symptoms of breast cancer. In developing countries, delayed diagnoses at advanced stages are common, with rates ranging from 30 to 50% in Latin America to 75% in Sub-Saharan Africa. These advanced stages are often self-detected by patients through symptoms such as lumps, watery discharge, nipple inversion, or other noticeable changes in their breasts (3).
A well-managed social security system is vital for providing effective healthcare to the lower class and alleviating economic and social constraints. Unfortunately, Pakistan lacks such a system, resulting in negative health outcomes for impoverished populations (4, 5). Despite growing awareness about breast cancer and an increasing demand for diagnostic and treatment services, several factors prevent Pakistani women from seeking breast examinations and treatment. These factors include the inaccessibility of tertiary care hospitals in rural areas, cultural norms, and a lack of awareness. Together, these issues discourage open discussions about breast and reproductive health. Research indicates that Muslim women often prefer female physicians for examinations of private body parts and pregnancy checkups, as this helps them avoid the hesitation and discomfort they might experience when dealing with male physicians (6, 7).
Additional factors such as age, marital status, dependency, social restrictions, and varying codes of honor further limit women’s access to timely healthcare and optimal treatment. Younger women, in particular, face greater challenges in accessing healthcare compared to older women (8). Social and family support plays a critical role in patients’ psychosocial and physical wellbeing. Unfortunately, in countries like Pakistan, these aspects are often undervalued, which leads to social isolation and depression, ultimately hindering the psychosocial and physical recovery of women (5).
The World Health Organization (WHO) recommends early diagnosis as the most effective approach to controlling breast cancer (3). Early diagnosis can be achieved through awareness of screening methods such as breast self-examinations (BSE), clinical breast examinations (CBE), and mammography. Assessing women’s awareness of these methods can help health decision-makers identify information gaps and improve timely diagnosis and treatment, ultimately reducing mortality rates (9).
Mammography is the leading screening method for breast cancer globally and has been associated with a reported 25% reduction in mortality rate among those aged between 50 and 69 years. However, it is less beneficial for women aged 40 to 49 years (10), especially in developing countries where population-based mammography is often unavailable due to funding and infrastructure limitations (11–13). Consequently, clinical breast examination and BSE are emphasized as alternative methods in regions lacking national mammography programs.
Bi-monthly BSE, as recommended by Haagensen, can help detect tumors early and reduce the incidence of advanced malignancies. CBE, which involves the palpitation and inspection of both breasts by medical professionals, has shown varying effectiveness in low- and middle-income countries. Given the diverse sociocultural norms and contextual factors, breast cancer screening strategies should be tailored to each country’s specific needs through customized workshops (14).
Study objectives
The purpose of this research is to examine the attitudes, perspectives, and knowledge of future Pakistani female pharmacy students concerning BSE through their participation in screening programs and breast control measures. The study also aims to evaluate changes in their knowledge level, attitudes, and views regarding BSE and breast cancer following a specifically designed educational intervention. This project seeks to bridge the knowledge gap and empower medical professionals, policymakers, and the community at large to make well-informed decisions and collaborate to improve women’s breast health outcomes.
Materials and methods
Study site and study design
A pre-post quasi-experimental study was conducted from October to December 2023 with the aim of evaluating and improving knowledge, perceptions, and attitudes toward breast cancer among female pharmacy university students in Karachi, Pakistan. The participants were from the pharmacy departments of two different universities, one a private female university with morning and evening shifts and the other a co-educational public university.
Inclusion and exclusion criteria
The study included women aged 18 years and above. Excluded from the study were women under 18, men, and individuals who declined to participate.
Ethical considerations
The Jinnah University for Women Institutional Review Board granted ethical approval for the study (JUW/IERB/PHARM-ARA-007/2023), and permission to conduct the sessions was obtained from the deans of both universities. All students who participated in the study did so voluntarily, and their signed consent was obtained. The study’s objectives were thoroughly explained to each participant, and they were assured that their participation would remain anonymous, with no personal data collected. All information gathered was kept confidential and used exclusively for research purposes.
Questionnaire validation
The content validity of both questionnaires was evaluated using Lawshe’s test and quantitative face validity through impact scores. Reliability and necessity were measured using the Content Validity Index (CVI) and Content Validity Ratio (CVR), with items rated by 10 experts. Items with a CVR value greater than 0.62 were deemed acceptable according to the Lawshe Table (15). Questionnaire relevance was evaluated using the CVI, where 10 experts rated items on a scale from 1 to 4.
The S-CVI/Ave scores were 0.914 for the pre-session and 0.9375 for the post-session questionnaires, with I-CVI values exceeding the minimum threshold of 0.78. The CVR values were 0.905 and 0.913, respectively, indicating good validity for the instruments (16, 17). Quantitative face validity was conducted with 20 participants using the item impact method, where values greater than 1.5 indicated the appropriateness of items (18). The results for face validity showed that all items in the pre- and post-survey achieved impact scores higher than 1.5, indicating the appropriateness of all items.
Data collection and procedure
Baseline questionnaire administration
The study was conducted on 1,200 female pharmacy students recruited from two different universities. The consented participants were provided with a baseline questionnaire that had been previously validated, pilot-tested, and self-administered. The questionnaires were adapted from previously published studies and expert opinions (19–22).
The baseline questionnaire was divided into three sections:
Section 1: This section includes information regarding the participant’s socio-demographic information, including age, marital status, history of breast cancer in family/relatives and friends, their past breast cancer practices, and attendance at breast cancer sessions. Their names and academic years were also obtained to ensure follow-up for the post-session survey.
Section 2: This section consists of two main parts. Part one evaluated participants’ general perceptions and knowledge regarding breast cancer through six questions. Part two focused on attitudes toward breast cancer, which was assessed through four questions.
Section 3: This section was divided into three parts. Part one included 10 risk variables, part two included eight variables regarding symptoms, and part three comprised four questions to evaluate the participants’ understanding of BSE techniques. This included their familiarity with screening methods for identifying breast cancer, the frequency (e.g., “weekly,” “monthly”), and timing of BSE (e.g., “before menstruation,” “any time”), as well as the accurate age for each screening method.
Educational intervention
Awareness workshops were conducted over a period of 6 months, consisting of a 45-min awareness session, followed by a 7 min short video tutorial. At the end of each session, an information leaflet was provided to each participant. Then, 2 weeks after the session, the target population was provided with post-session questionnaires to assess the impact of the educational training. The pre- and post-session surveys used in this research were based on those utilized in related earlier investigations (19, 20, 23–25).
Post-session survey
The post-session form included only section two and three to assess changes in knowledge and perceptions following the educational intervention, as section one covered participants’ demographics and their past knowledge and practices.
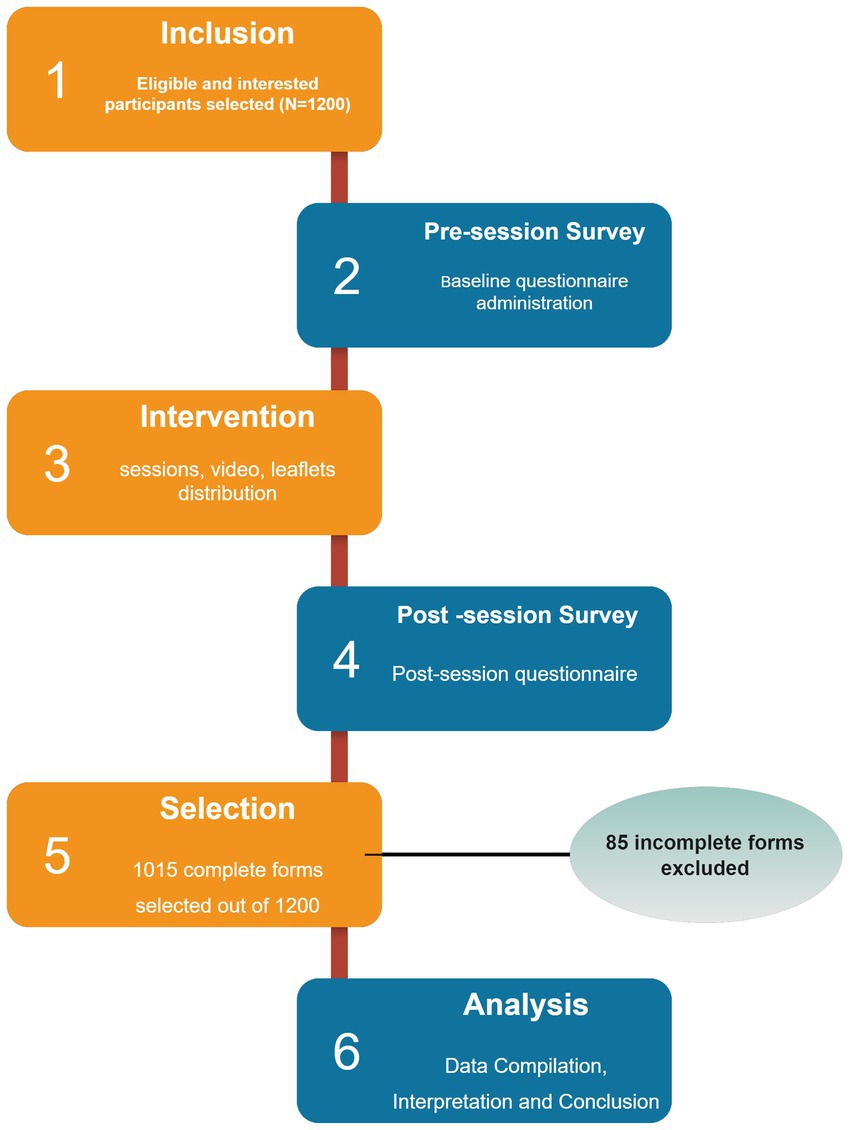
Each participant was assigned a specific number during the pre-session, which was linked to their post-session form to ensure the correct pairing of both the pre- and post-questionnaires (Figure 1).
Statistical workout
Following data collection, IBM SPSS statistics version 21 and Microsoft Office Excel were used to organize, code, and tabulate the data. Participants’ knowledge was categorized based on their scores in different domains: those scoring above 50% were classified as having adequate knowledge, while those scoring below 50% were classified as having inadequate knowledge. For instance, the participants who answered three or more questions correctly out of six in section two were considered knowledgeable. Pearson’s Chi-square test, dependent sample t-test, and ANCOVA (analysis of co-variance) were utilized to examine differences in knowledge before and after the session. Analysis was conducted using counts and percentages for categorical variables. SPSS version 21 was used for statistical analysis, and a p-value < 0.05 was considered statistically significant (20, 26).
Results
Participants demographics and past practices
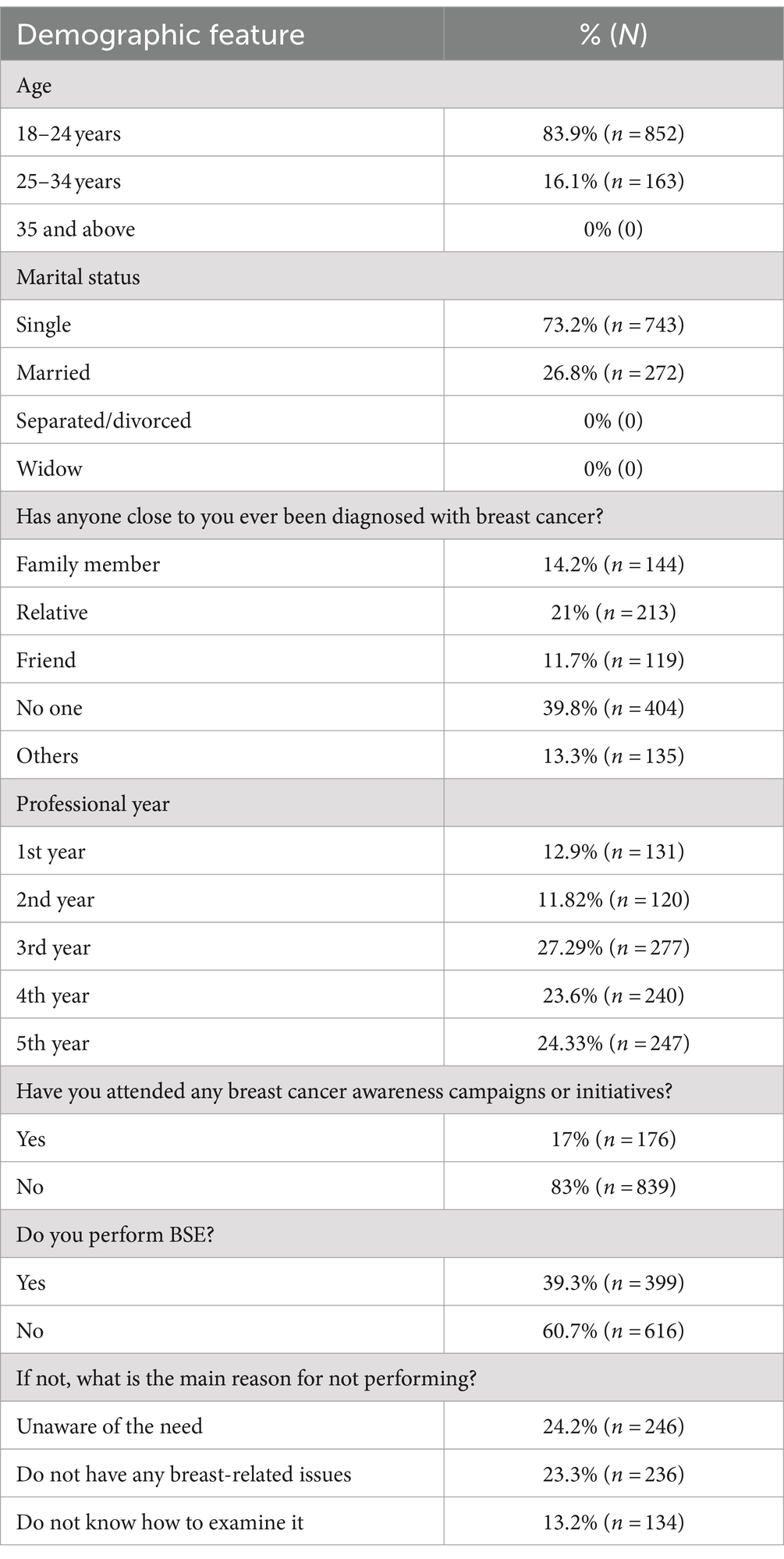
After a thorough evaluation and the exclusion of incomplete questionnaires, out of 1,200 participants, 1,015 of them completed pre- and post-session questionnaires were selected for analysis. Table 1 shows that 83.9% (n = 852) of the students were aged 18–24 years, while 16.1% (n = 163) were aged 25–34 years. Among these students, 26.8% (n = 272) were married, and 73.2% (n = 743) were single. The participants were distributed across different academic years: 12.9% (n = 131) were first-year students, 11.8% (n = 120) were second-year students, with the majority being third-year students at 27.3% (n = 277), followed by final-year students at 24.3% (n = 247), and fourth-year students at 23.6% (n = 240).
Regarding breast cancer history, 39.8% (n = 404) of the participants reported that no one in their social circle or family had been diagnosed with breast cancer, while 21% of the participants (n = 213) reported a history of breast cancer in their relatives, followed by 14.2% (n = 144) in their immediate family, 13.3% (n = 135) in others, and 11.7% (n = 119) in their friends. Only 17% of participants (n = 176) had attended breast cancer awareness campaigns or initiatives, while 83% of them (n = 839) had not. Among all participants, 39.3% of participants (n = 399) reported practicing breast self-exams regularly. However, 60.7% of participants (n = 616) did not practice breast self-exams regularly, with 24.2% of them (n = 246) stating they were unaware of the need, 23.3% of them (n = 236) believing they had no breast-related issues, and 13.2% of them (n = 134) indicating they were not familiar with breast self-exam techniques.
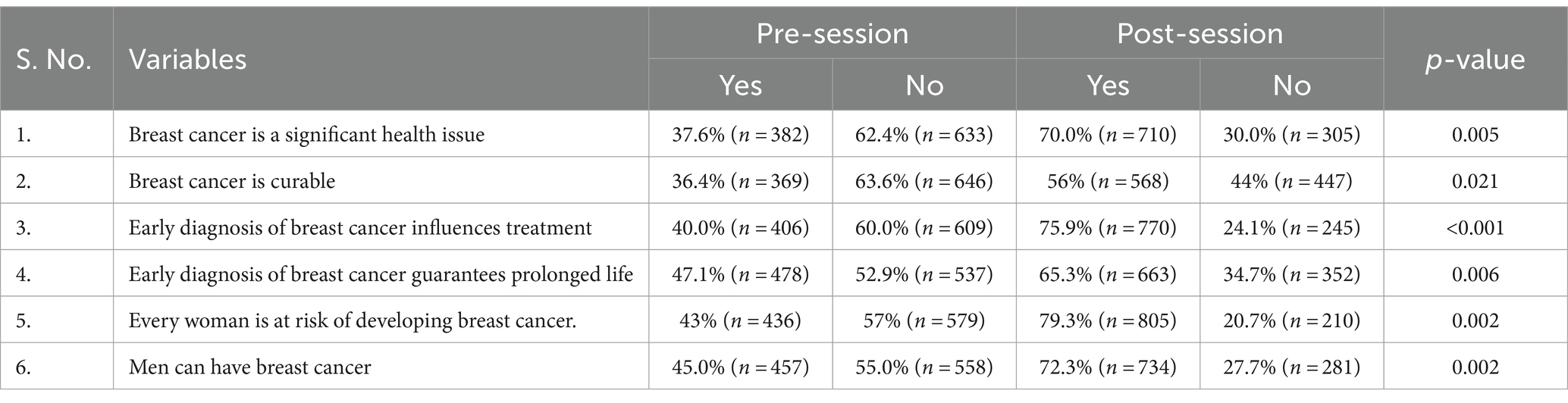
Impact on knowledge against general perceptions towards breast cancer
As shown in Table 2, the initial perception of breast cancer revealed that less than 50% of the participants considered breast cancer a significant health issue and or believed that it was curable. After the educational intervention, these perceptions improved significantly, with 70 and 56% of participants acknowledging breast cancer as a significant health issue and curable, respectively. Similarly, the belief that early diagnosis influences treatment and prolongs life increased from 40 and 47.1% before the session to 75.9 and 65.3% afterward. The percentage of participants who recognized that every woman is at risk of developing breast cancer rose significantly from 43 to 79.3% post-session. Additionally, awareness that men can also develop breast cancer improved from 45% before the session to 72.3% afterward.
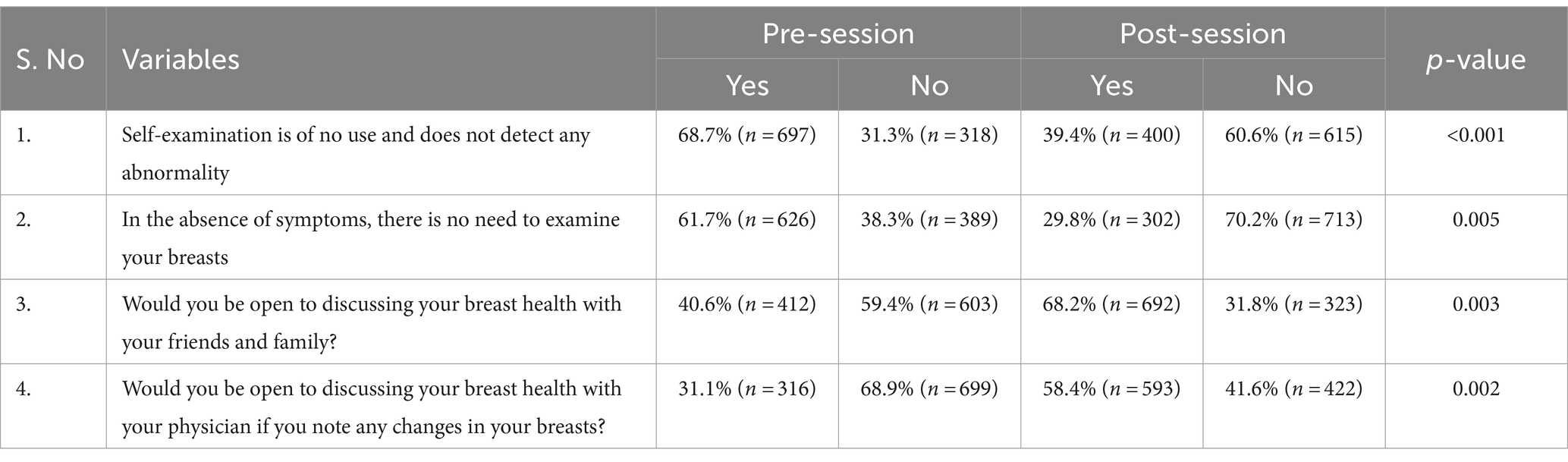
Impact on attitudes toward breast cancer
Table 3 summarizes the changes in attitudes toward breast cancer as a result of this session. Initially, 68.7 and 61.7% of participants believed that self-examination was unnecessary and that there was no need for breast examination in the absence of symptoms. After the session, these views shifted significantly, with only 39.4 and 29.8% holding these beliefs (p < 0.001 and p = 0.005, respectively). Additionally, 40.6 and 31.1% of participants initially expressed reluctance to discuss their breast health with family/friends and physicians, respectively. This reluctance decreased significantly after the session, with 68.2 and 58.4% of participants becoming more open to these discussions (p-value = 0.003 and 0.002, respectively).
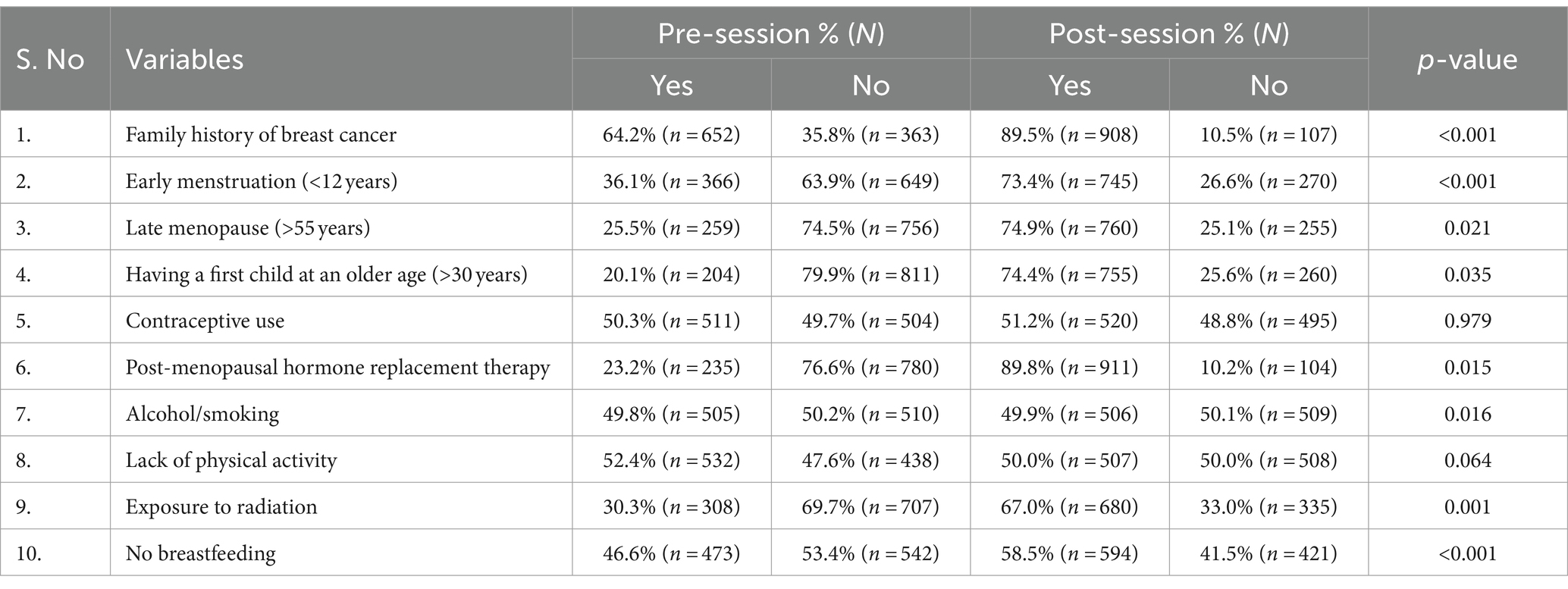
Impact on knowledge of breast cancer risk factors
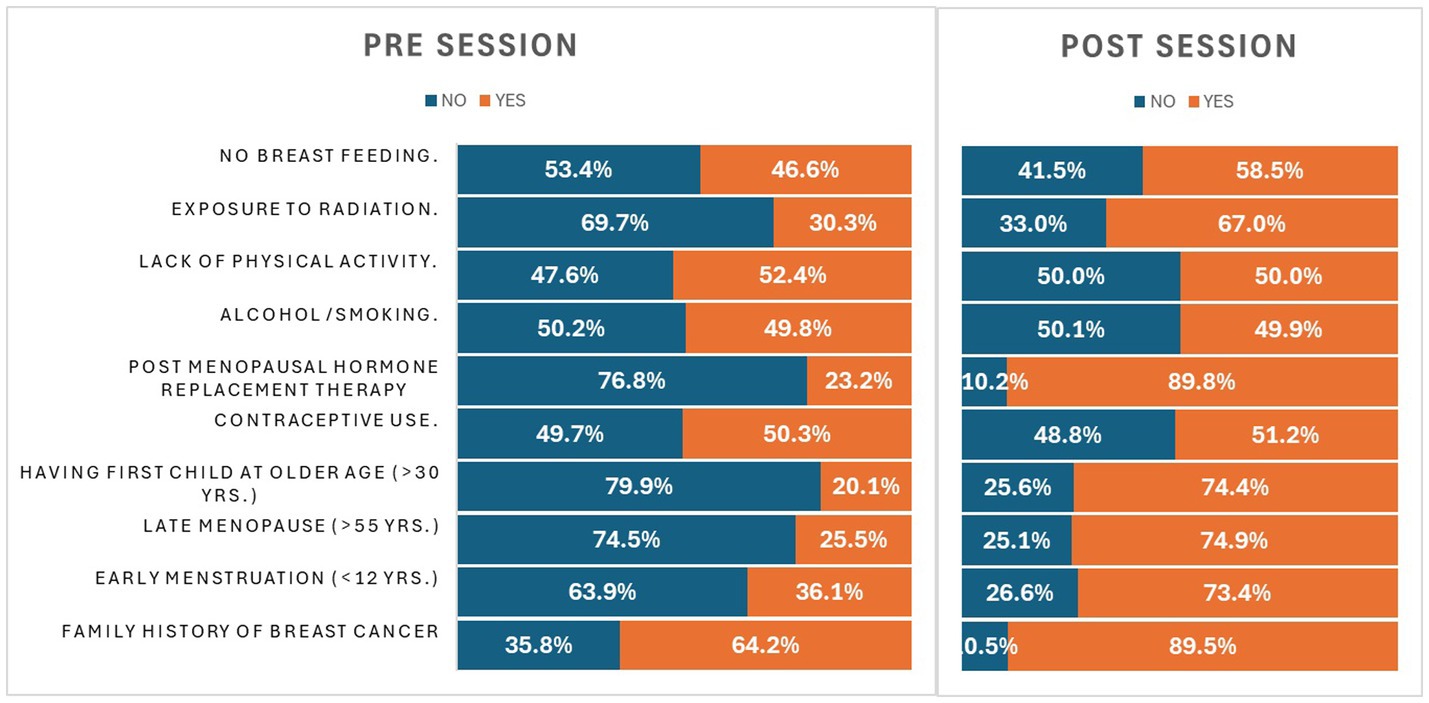
Table 4 shows the participants’ knowledge of breast cancer risk factors before and after the intervention. Initially, less than 50% of the participants were aware of risk factors such as early menstruation (36.1%), late menopause (25.5%), having a first child at an older age (20.1%), post-menopausal hormone replacement therapy (23.2%), radiation exposure (30.3%), and no breastfeeding (46.6%). After the session, there was significant progress (p < 0.05), with knowledge increasing to 73.4, 74.9, 74.4, 89.8, and 67.0%, respectively. The smallest increase was observed in awareness of the no breastfeeding factor, which rose to 58.5% post-session.
More than 50% of the participants already had knowledge of risk factors such as family history (64.2%) and lack of physical activity (52.4%). After the session, there was a significant increase in awareness of family history (89.5%), while a slight decline was noted in awareness of the lack of physical activity (50.0%). Regarding factors such as contraceptive use and alcohol/smoking, nearly 50% of the participants (50.3 and 49.8%) were well aware of these factors, and there was no significant change in their awareness levels after the session (51.2 and 49.9%). Figure 2 provides a graphical elucidation of this section.
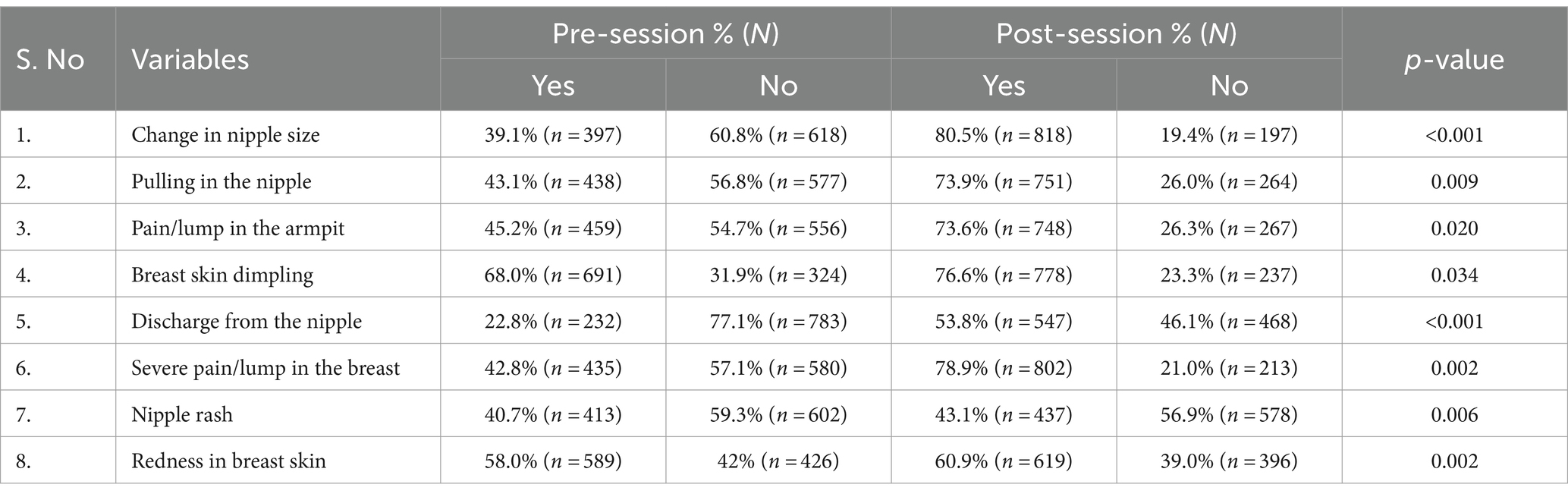
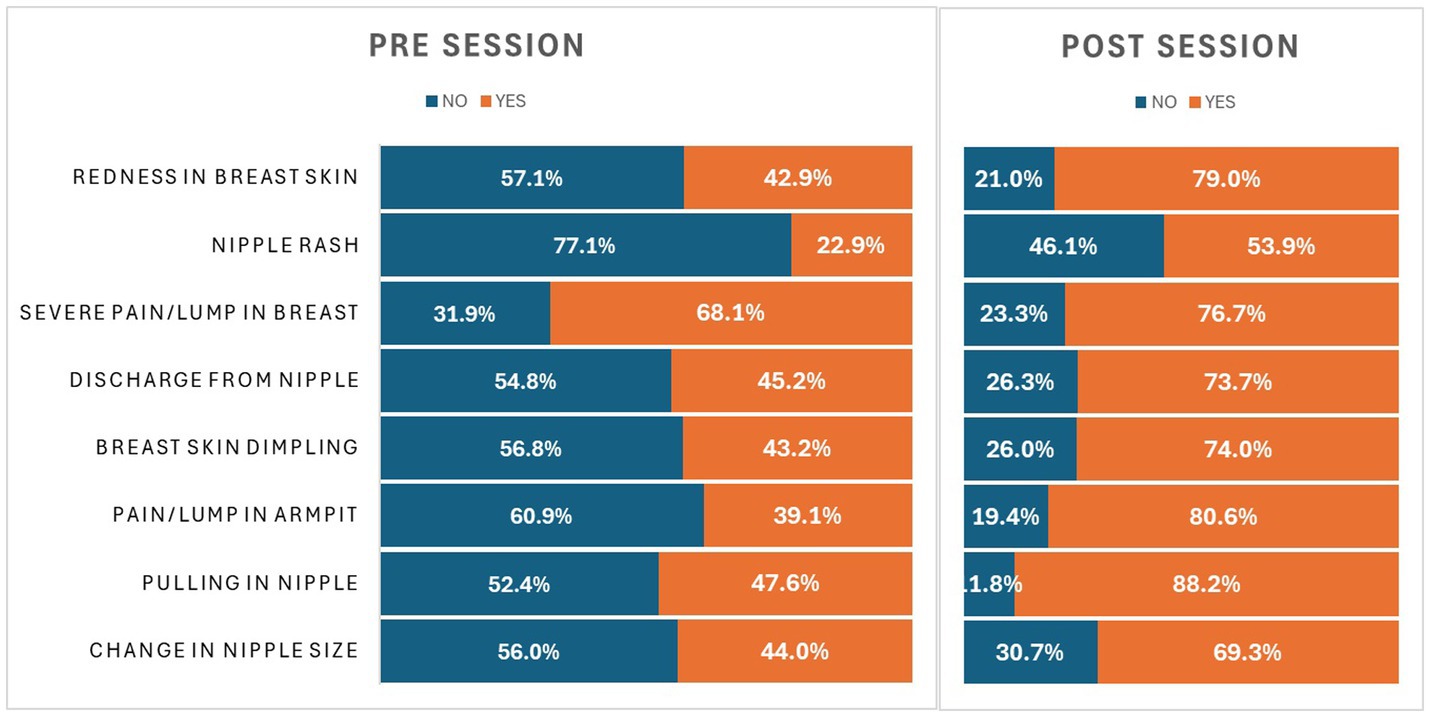
Impact on knowledge of breast cancer features
Table 5 reflects the impact on knowledge related to breast cancer signs/symptoms after the session. Our findings demonstrated that knowledge regarding changes in nipple size and nipple discharge was inadequate before the session (39.1 and 22.8%, respectively) but significantly improved post-session to 80.5 and 53.8% (i.e., <0.001). Knowledge of other variables such as pulling in nipples, pain/lump in the armpit, severe pain/lump in the breast, and nipple rash was also below 50% before the session (43.1, 45.2, 42.8, and 40.7%, respectively). After the session, knowledge increased to 73.9, 73.6, and 78.9% for these variables, except for nipple rash, which remained inadequate at 43.1% post-session. These improvements were statistically significant (p = 0.009, 0.020, 0.002, and 0.006, respectively). Knowledge regarding breast skin dimpling and redness was already adequate before the session (68.0 and 58.0%, respectively) but still showed a minor significant increase after the session (76.6 and 60.9%) with p-values of 0.034 and 0.002 (see Figure 3).
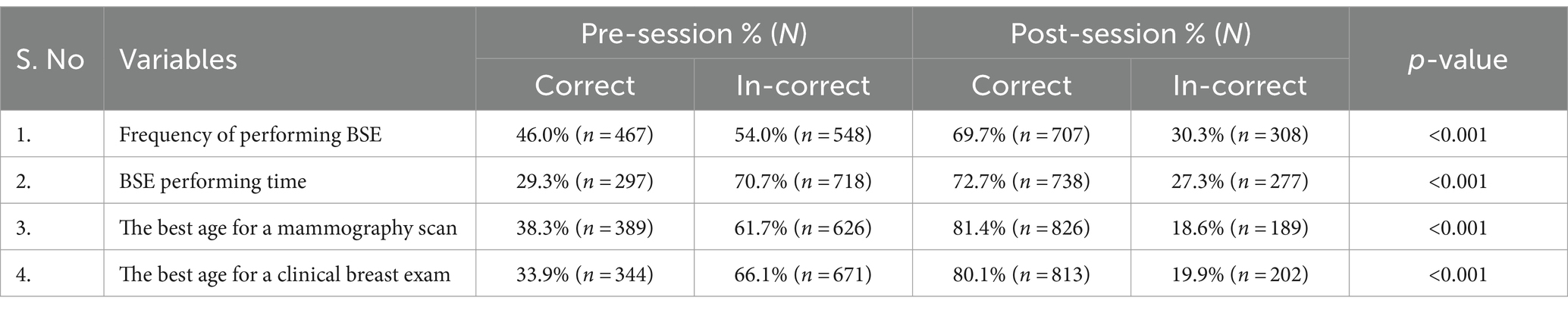
Impact on breast cancer screening technique knowledge
Table 6 shows the impact on knowledge related to breast cancer screening routines, which was found to have a significant effect (p < 0.001) on almost all domains after the session. Before the session, less than 50% of the participants had knowledge regarding the frequency of BSE (46.0%), the correct time to perform them (29.3%), or the appropriate ages for mammography (38.3%), and CBE (33.9%). After the intervention, there was a significant improvement in awareness, with knowledge levels rising to 69.7, 72.7, 81.4, and 80.1%, respectively.
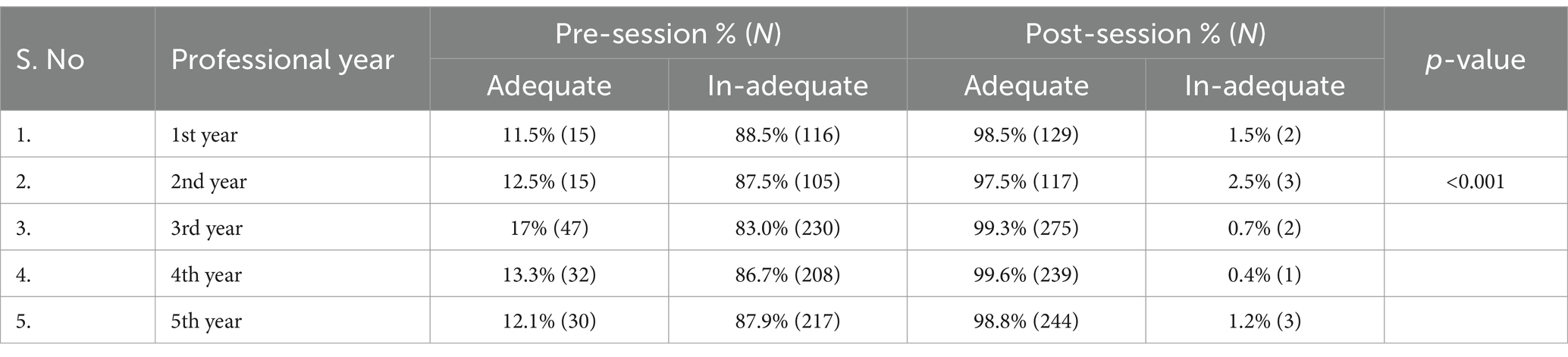
Impact on knowledge of professional years
Table 7 shows the impact of the educational intervention on knowledge across different professional years. Before the session, students from each year displayed overall inadequate knowledge about breast cancer, with 11.5% of first-year students, 12.5% of second-year students, 17% of third-year students, 13.3% of fourth-year students, and 12.1% of final-year students having sufficient knowledge. After the session, knowledge significantly improved across all years, with over 90% of students demonstrating adequate understanding, reflecting the success of the intervention.
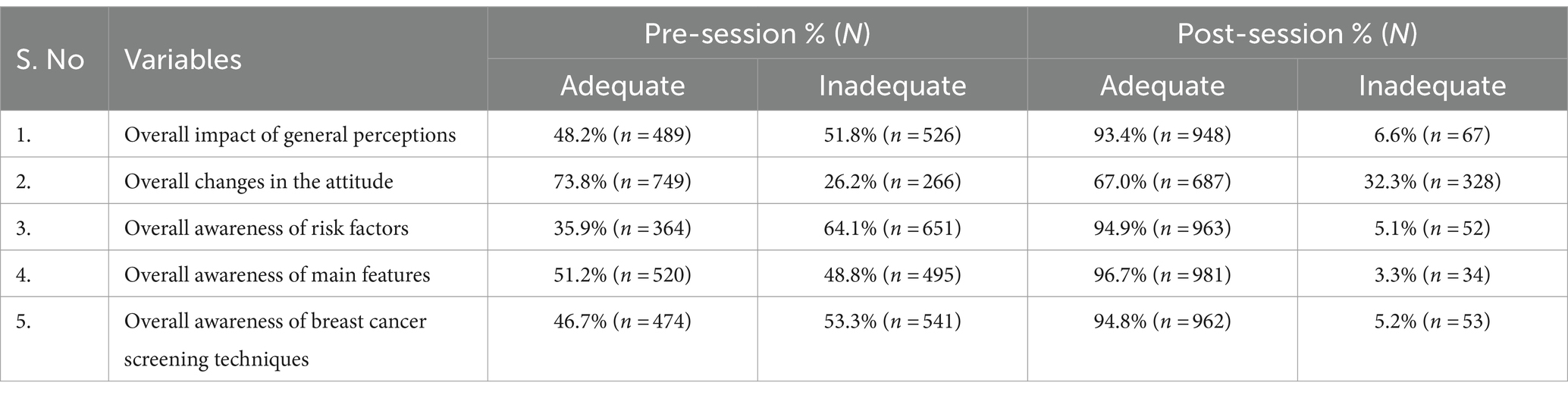
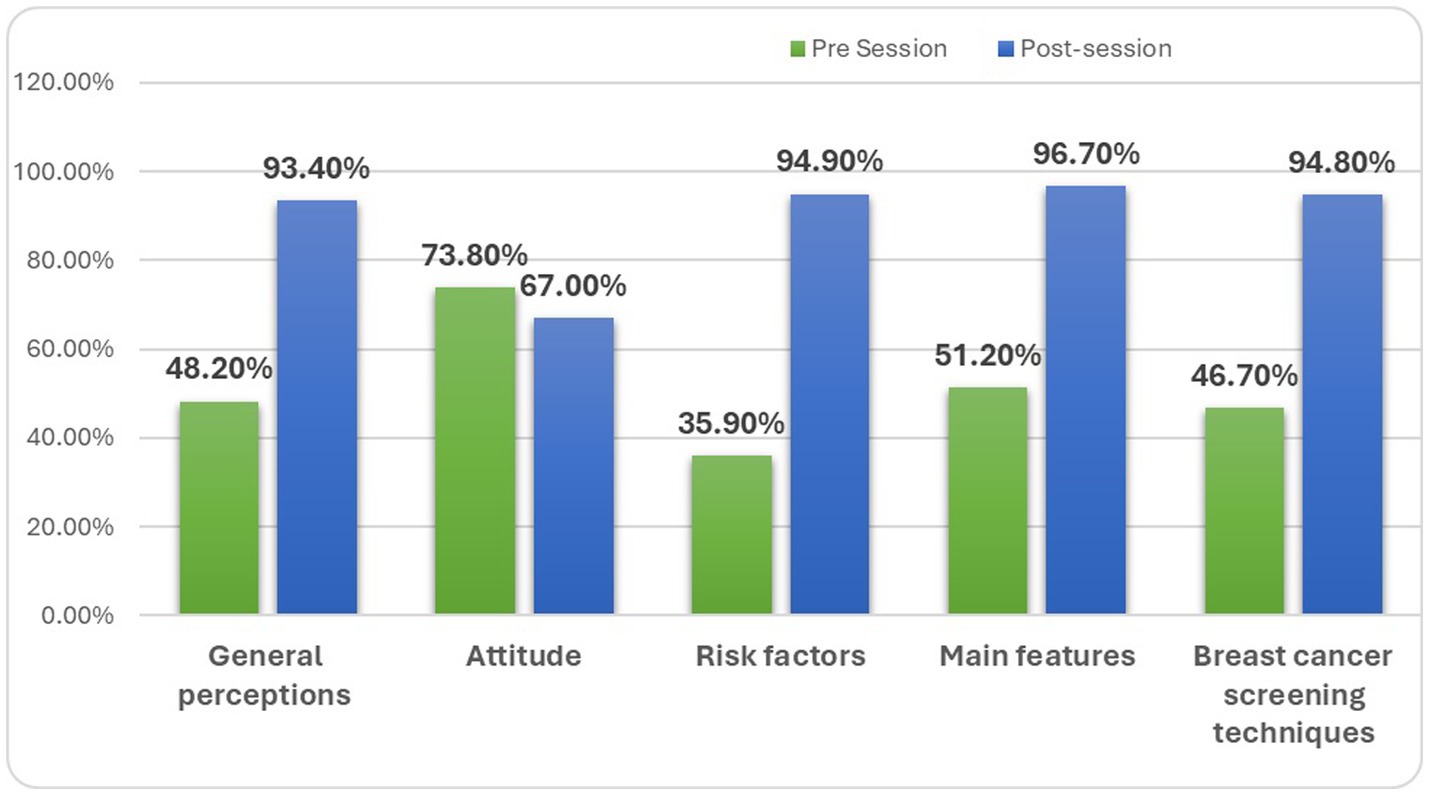
Complete case analysis of pre-post interventional studies
The designed awareness session was effective in significantly increasing overall awareness of breast cancer, altering public perceptions, and improving knowledge and attitudes. Table 8 and Figure 4 illustrate the overall increase in awareness across various domains, expressed in percentages. Knowledge of risk factors and screening methods showed a significant increase, rising from 35.9 and 46.7% and from 94.9 and 94.8%, respectively, with p-values of 0.010 for risk factors and < 0.001 for screening techniques. The most substantial impact was observed in the knowledge of breast cancer features, which increased from 51.2 to 96.7%, with a significant p-value of 0.022.
General perceptions of breast cancer improved from 48.2 to 93.4%, with a significant relationship (p-value 0.019). However, there was a significant decline in certain attitudes, with the percentage changing from 73.8 to 67.0% (p-value 0.009).
This decline aligns with the findings discussed earlier in Table 3, where 68.7 and 61.7% of the participants initially considered self-examination unnecessary or believed that there was no need for breast examination in the absence of symptoms. After the session, these views shifted to 39.4 and 29.8%, respectively. Table 9 presents the overall interventional effect, showing a significant shift in mean scores from 13.5 ± 2.68 to 21.92 ± 2.49, with an overall effect size of 8.42.
Discussion
Given the increasing prevalence of breast cancer in recent years in Pakistan (27), this study was designed as an effort to assess the basic level of education regarding breast cancer among pharmacy students and to enhance their awareness to better guide future generations. The study was implemented in three phases. Initially, a pre-session questionnaire was administered to evaluate the participants’ basic knowledge of breast cancer, including its features, risk factors, screening techniques, and general perceptions and attitudes toward breast cancer. Following this, an educational intervention was conducted, consisting of a 45-min session, a 7-min brief video, and precise educational leaflets. After 2 weeks, the same students were asked to complete a post-session questionnaire. The pre-test and educational intervention were conducted on the same day.
After analysis, it was determined that the overall knowledge of these students increased as a result of the planned educational intervention. Awareness improved across all aspects of breast cancer, including knowledge of its symptoms, risk factors, screening methods, and general perceptions, with positive changes in attitudes as well. The purpose of involving medical students in this session was to assess their baseline knowledge levels and to enhance their understanding of medical terms. The results of this study confirm that baseline knowledge regarding breast cancer was inadequate but could be significantly improved through the introduction of such educational sessions on a yearly basis.
Overall awareness of risk factors and screening methods increased significantly, reaching approximately 94.9 and 94.8%, respectively. The most significant impact was seen in the increase in knowledge of breast cancer features, which rose from 51.2 to 96.7%. General perceptions also improved, shifting from 48.2 to 93.4%, with a significant relationship. A closer examination of the results revealed that overall knowledge improved to over 90%, with a significant shift in the overall interventional effect, as indicated by the mean scores increasing from 13.5 ± 2.68 to 21.92 ± 2.49. This confirms the success of the study.
Available literature confirms that studies like this, conducted in different schools, universities, and other settings to promote breast cancer awareness, have a positive impact on increasing awareness (28, 29). For instance, a study conducted on a group of Nigerian adolescents used peer education in a pre-post interventional study to raise breast cancer awareness. This study found a significant improvement in baseline education after the educational intervention and demonstrated that such an approach could be cost-effective and easily implemented with limited resources (21). Similarly, a study conducted at a female university in Bangladesh successfully enhanced knowledge and awareness about breast cancer and BSE practices (28).
In Malaysia, a randomized controlled trial was conducted among Yemeni female school teachers, involving both control and intervention groups. The intervention group received a 1-day educational session, including a 90-min presentation on breast cancer screening, while the control group was only provided with similar educational material. The study aimed to assess the effectiveness of the educational intervention at different time intervals, with the goal of educating teachers so that they could, in turn, educate younger generations about breast cancer awareness (30).
In another study conducted in Bangladesh, a hospital-based survey among women revealed that a lack of knowledge and awareness programs, sociocultural norms, disease-related fear, and shyness were major barriers that prevented women from consulting or communicating their condition to anyone, including physicians (31).
However, further research showed a rise in the recognition of early-stage breast cancer among nurses and other healthcare professionals who had received CBE training. Additionally, CBE was shown to reduce the percentage of late-stage breast cancer recurrence by 50% (32).
In previous years, the American Cancer Society recommended that women begin performing BSE in their 20s and continue them regularly throughout their lives. However, these recommendations have evolved over time. The most recent guidelines, updated in 2015, emphasize the importance of breast awareness rather than adhering to a strict regimen or schedule for formal BSE (33). These discussions about breast health and its significance must continue throughout a woman’s life, beginning in adolescence and continuing into adulthood.
This study has several strengths. First, the questionnaire was validated by experts and oncologists. Every session and the completion of both questionnaires were conducted under supervision. Confidentiality was a top priority and was maintained throughout all stages of the intervention. However, there are also some limitations to this study. The results can be generalized to female pharmacy students but may not apply to all women or represent all healthcare professionals. Additionally, a follow-up session regarding breast self-exam practices could not be conducted due to time constraints.
Conclusion
Organizing breast cancer awareness sessions is particularly important in lower-middle-income countries, where access to healthcare and knowledge about the disease may be limited. These sessions serve as critical platforms for educating individuals about the warning signs and risk factors of breast cancer. By providing education on self-examinations, the importance of routine screenings, and the need for prompt medical attention, these workshops empower women to take an active role in managing their health. Raising awareness facilitates early detection, which can be life-saving by ensuring that those affected receive appropriate care and treatment in a timely manner. Such awareness initiatives have the potential to significantly improve healthcare outcomes, reduce mortality rates, and enhance the overall wellbeing of communities in lower-middle-income countries by fostering a culture of education and proactive health management.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Ethical Review Board (Jinnah University for Women). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NM: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. SN: Conceptualization, Resources, Supervision, Validation, Writing – review & editing. HA: Conceptualization, Investigation, Project administration, Supervision, Visualization, Writing – review & editing. AM: Conceptualization, Project administration, Resources, Validation, Writing – review & editing. SZ: Resources, Validation, Writing – review & editing. JS: Data curation, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
Dean faculty of pharmacy of both universities for granting approval, and all volunteers who participated are highly appreciated for their cooperation in the smooth conduction of this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CBE, Clinical breast exam; BSE, Breast self-exam; CVI, Content validity index; CVR, Content validity ratio; S-CVI/Ave, Scale content validity index/average; I-CVI, Item Content validity index
References
1. Sung, H, Ferlay, J, Siegel, RL, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Francies, FZ, Hull, R, Khanyile, R, and Dlamini, Z. Breast cancer in low-middle income countries: abnormality in splicing and lack of targeted treatment options. Am J Cancer Res. (2020) 10:1568–91.
3. Ginsburg, O, Yip, CH, Brooks, A, Cabanes, A, Caleffi, M, Dunstan Yataco, JA, et al. Breast cancer early detection: a phased approach to implementation. Cancer. (2020) 126:2379–93. doi: 10.1002/cncr.32887
4. Manzoor, I . Evolution of telehealth and its future in Pakistan. J Fatima Jinnah Med Univ. (2021) 15:148–9.
5. Agha, N, and Tarar, MG. Battling breast cancer: Women's narratives of struggle, family support and survival from rural Sindh, Pakistan. Pakistan J Women's Stud. (2019) 26:21–40. doi: 10.46521/pjws.026.01.0015
6. Khan, NH, Duan, S-F, Wu, D-D, and Ji, X-Y. Better reporting and awareness campaigns are needed for breast cancer in Pakistani women. Cancer Manag Res. (2021) 13:2125–9. doi: 10.2147/CMAR.S270671
7. Talib, Z, Amersi, F, Harit, A, and Saleh, M. Promoting breast cancer awareness and clinical breast examination in the LMIC: experiences from Tajikistan, Pakistan, and Kenya. Curr Breast Cancer Rep. (2019) 11:152–7. doi: 10.1007/s12609-019-00321-7
8. Woof, VG, Ruane, H, Ulph, F, French, DP, Qureshi, N, Khan, N, et al. Engagement barriers and service inequities in the NHS breast screening Programme: views from British-Pakistani women. J Med Screen. (2020) 27:130–7. doi: 10.1177/0969141319887405
9. Smith, RA, Andrews, KS, Brooks, D, Fedewa, SA, Manassaram-Baptiste, D, Saslow, D, et al. Cancer screening in the United States, 2019: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J Clin. (2019) 69:184–210. doi: 10.3322/caac.21557
10. Wu, T-Y, and Lee, J. Promoting breast cancer awareness and screening practices for early detection in low-resource settings. Eur J Breast Health. (2019) 15:18–25. doi: 10.5152/ejbh.2018.4305
11. Lim, YX, Lim, ZL, Ho, PJ, and Li, J. Breast cancer in Asia: incidence, mortality, early detection, mammography programs, and risk-based screening initiatives. Cancers. (2022) 14:4218. doi: 10.3390/cancers14174218
12. Manson, EN, and Achel, DG. Fighting breast cancer in low-and-middle-income countries – what must we do to get every woman screened on regular basis? Scient. African. (2023) 21:e01848. doi: 10.1016/j.sciaf.2023.e01848
13. Dan, Q, Zheng, T, Liu, L, Sun, D, and Chen, Y. Ultrasound for breast Cancer screening in resource-limited settings: current practice and future directions. Cancers. (2023) 15:2112. doi: 10.1200/JGO.18.10510
14. Albeshan, SM, Hossain, SZ, Mackey, MG, and Brennan, PC. Can breast self-examination and clinical breast examination along with increasing breast awareness facilitate earlier detection of breast cancer in populations with advanced stages at diagnosis? Clin Breast Cancer. (2020) 20:194–200. doi: 10.1016/j.clbc.2020.02.001
15. Wahab, YA, Nordin, N, Yip, NM, Mohd Lud, AF, Bariyyah, K, and Wan Hamedi, WH. Development of instruments on the impact of university towards sustainable socio-economic. European Proceedings of Multidisciplinary Sciences (2022).
16. L'Ecuyer, KM, Subramaniam, DS, and Reangsing, C. Development of the preceptor self-assessment tool and use of the content validity index. J. Contin. Educ. Nurs. (2020) 51:469–76. doi: 10.3928/00220124-20200914-09
17. Bobos, P, MacDermid, JC, Boutsikari, EC, Lalone, EA, Ferreira, L, and Grewal, R. Evaluation of the content validity index of the Australian/Canadian osteoarthritis hand index, the patient-rated wrist/hand evaluation and the thumb disability exam in people with hand arthritis. Health Qual Life Outcomes. (2020) 18:302. doi: 10.1186/s12955-020-01556-0
18. Sadeghi, N, Akbarfahimi, M, and Taghizadeh, HG. The Persian version of “meaningful activity participation assessment” questionnaire: evaluation of its face and content validity in elderly. Func Disabil J. (2021) 4:E44. doi: 10.32598/fdj.4.44
19. Abo Al-Shiekh, SS, Ibrahim, MA, and Alajerami, YS. Breast cancer knowledge and practice of breast self-examination among female university students, Gaza. Sci World J. (2021) 2021:1–7. doi: 10.1155/2021/6640324
20. Nsaful, J, Dedey, F, Nartey, E, Labi, J, Adu-Aryee, NA, and Clegg-Lamptey, JN. The impact of a breast cancer educational intervention in Ghanaian high schools. BMC Cancer. (2022) 22:1–10. doi: 10.1186/s12885-022-09991-6
21. Sadoh, AE, Osime, C, Nwaneri, DU, Ogboghodo, BC, Eregie, CO, and Oviawe, O. Improving knowledge about breast cancer and breast self examination in female Nigerian adolescents using peer education: a pre-post interventional study. BMC Womens Health. (2021) 21:1–9. doi: 10.1186/s12905-021-01466-3
22. Alrashid, FF, Idris, SA, Elamin, AA, Alnajib, AM, Elmisbah, HO, and Hussien, TM. Perspicacity of medical students towards breast self-examination. Med Sci. (2021) 25:440–6.
23. Hussain, I, Majeed, A, Masood, I, Ashraf, W, Imran, I, Saeed, H, et al. A national survey to assess breast cancer awareness among the female university students of Pakistan. PLoS One. (2022) 17:e0262030. doi: 10.1371/journal.pone.0262030
24. Rahman, SA, Al -Marzouki, A, Otim, M, Nehk, K, Yousef, R, and Rahman, P. Awareness about breast cancer and breast self-examination among female students at the University of Sharjah: a cross-sectional study. Asian Pac J Cancer Prev. (2019) 20:1901–8. doi: 10.31557/APJCP.2019.20.6.1901
25. Koc, G, Gulen-Savas, H, Ergol, S, Yildirim-Cetinkaya, M, and Aydin, N. Female university students' knowledge and practice of breast self-examination in Turkey. Niger J Clin Pract. (2019) 22:410–5. doi: 10.4103/njcp.njcp_341_18
26. Rehman, HT, Jawaid, H, Tahir, A, Imtiaz, M, Zulfiqar, T, and Aziz, T. Breast cancer knowledge among health professionals: a pre–post-knowledge-based intervention study. J Family Med Prim Care. (2022) 11:5649–55. doi: 10.4103/jfmpc.jfmpc_1226_22
27. Tufail, M, and Wu, C. Cancer statistics in Pakistan from 1994 to 2021: data from cancer registry. JCO Clin. Cancer Inform. (2023) 7:e2200142. doi: 10.1200/CCI.22.00142
28. Sarker, R, Islam, MS, Moonajilin, MS, Rahman, M, Gesesew, HA, and Ward, PR. Effectiveness of educational intervention on breast cancer knowledge and breast self-examination among female university students in Bangladesh: a pre-post quasi-experimental study. BMC Cancer. (2022) 22:199. doi: 10.1186/s12885-022-09311-y
29. Noman, S, Shahar, HK, Abdul Rahman, H, Ismail, S, Abdulwahid Al-Jaberi, M, and Azzani, M. The effectiveness of educational interventions on breast cancer screening uptake, knowledge, and beliefs among women: a systematic review. Int J Environ Res Public Health. (2021) 18:263. doi: 10.3390/ijerph18010263
30. Noman, S, Shahar, HK, Abdul Rahman, H, and Ismail, S. Effectiveness of an educational intervention of breast cancer screening practices uptake, knowledge, and beliefs among Yemeni female school teachers in Klang Valley, Malaysia: a study protocol for a cluster-randomized controlled trial. Int J Environ Res Public Health. (2020) 17:1167. doi: 10.3390/ijerph17041167
31. Amin, MN, Uddin, MG, Uddin, MN, Rahaman, MZ, Siddiqui, SA, Hossain, MS, et al. A hospital-based survey to evaluate knowledge, awareness and perceived barriers regarding breast cancer screening among females in Bangladesh. Heliyon. (2020) 6:e03753. doi: 10.1016/j.heliyon.2020.e03753
32. O'Neil, DS, Nxumalo, S, Ngcamphalala, C, Tharp, G, Jacobson, JS, Nuwagaba-Biribonwoha, H, et al. Breast Cancer early detection in Eswatini: evaluation of a training curriculum and patient receipt of recommended follow-up care. JCO Glob. Oncol. (2021) 7:1349–57. doi: 10.1200/GO.21.00124
Keywords: breast cancer awareness, educational intervention, pre- and post-study, quasi-experimental trials, breast self examination
Citation: Mansoor NuS, Naveed S, Ali H, Manzoor A, Zahoor S and Sheikh J (2024) Evaluation of a pre-post quasi-experimental educational intervention on breast cancer awareness among pharmacy professionals in Karachi, Pakistan. Front. Public Health. 12:1443249. doi: 10.3389/fpubh.2024.1443249
Edited by:
Muhammad Fawad Rasool, Bahauddin Zakariya University, PakistanReviewed by:
Zikria Saleem, Bahauddin Zakariya University, PakistanIltaf Hussain, Xian Jiaotong University, China
Copyright © 2024 Mansoor, Naveed, Ali, Manzoor, Zahoor and Sheikh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Noor us Saba Mansoor, bm9vcl9zYWJAbGl2ZS5jb20=
 Noor us Saba Mansoor
Noor us Saba Mansoor Safila Naveed
Safila Naveed Huma Ali
Huma Ali Ammara Manzoor
Ammara Manzoor Saima Zahoor
Saima Zahoor Javeria Sheikh
Javeria Sheikh