- 1Outpatient Department, First Vienna Pediatric Medical Center, Vienna, Austria
- 2Department of Pediatrics and Adolescent Medicine, Medical University of Vienna, Vienna, Austria
Background: Vaccine hesitancy is considered a primary cause of outbreaks of vaccine-preventable infectious diseases. The Austrian vaccination plan includes 24 vaccinations in the first 2 years of life, 12 for free and 12 subject to a fee. Since preterm babies are more susceptible to severe infections, immunization is a vital protection strategy. This study examines the routine immunization schedule recommended for children in Austria, the number of timely vaccinations, and the number of delayed and rejected vaccinations. Possible reasons for vaccination delays and rejection and potential influencing factors (preterm birth, COVID-19 pandemic, information sources) are also analyzed.
Methods: We included children aged 2 to 5 years who presented to Vienna's largest pediatric center with an Austrian mother-child pass and spent the first 2 years of their lives in Austria. Data was collected using questionnaires about the vaccination status, parents' reasons for any rejections or delays in the recommended vaccination regimen, the impact of the COVID-19 pandemic on individuals' vaccination behavior, and child-specific influencing factors such as preterm birth and socioeconomic factors.
Results: 90% of the 150 study subjects follow the recommendations on routine vaccinations, while 40–62% accept vaccinations subject to a fee. Preterm infants received less fee-based (53%) as well as gratuitous (88%) vaccinations. While free vaccinations tend to be delayed, more fee based vaccinations are rejected. With free vaccinations, delays and refusals occur due to illness or missed appointments. In the case of fee- required vaccinations, however, fears of side effects are also one of the main reasons. Due to the COVID-19 pandemic, about a quarter of parents have become more skeptical about vaccines. However, the vaccination rate of premature babies is usually just below that of full-term babies. Physicians remain the most trustworthy source of information about vaccinations.
Conclusion: Free vaccinations are more accepted by parents than fee based vaccinations. Preterm babies, which are a high risk group for vaccination preventable diseases, show a lower or delayed vaccination rate, which must be prevented through intensive doctor education. In addition, vaccination hesitancy changed during the COVID-19 pandemic, which needs to be addressed during the medical consultation.
Introduction
Child mortality has fallen sharply worldwide in recent decades thanks to vaccination campaigns (1, 2). Since the introduction of the WHO Expanded Program on Immunization (EPI) in 1974, vaccination was estimated to be directly responsible for 40% of reduced global infant mortality (3). However, increased negative attitudes toward vaccinations lead to a recurrence of vaccine-preventable diseases (4, 5). The 2023 Austrian vaccination plan recommends 22 vaccinations for children in the first 24 months of life. The state fully covers twelve of these; the others are subject to a fee. The free vaccinations include up to three partial vaccinations against rotavirus, three against diphtheria-tetanus-pertussis-poliomyelitis-Haemophilus influenzae B-hepatitis B (hexavalent), three against pneumococci (PCV), and two against measles-mumps-rubella (MMR). The following are part of the pay-for vaccination program: three vaccinations against meningococcal B, one against meningococcal ACW135Y, three against tick-borne encephalitis (TBE), two against varicella, and two against hepatitis A, the latter being only a travel immunization for high risk countries (6). According to the Austrian Ministry of Social Affairs, vaccination rates of those fully immunized against MMR and the hexavalent vaccine reached 87% in 2022, which is well below the recommended 95% limit recommended by the world health organization (WHO) (7, 8). Some population groups are at particular risk to develop infections and should preferably be immunized quickly. Premature babies have an above-average mortality rate due to their naive immune system and reduced diaplacental antibody transfer, making them more exposed to life-threatening infectious diseases (9, 10). According to the WHO, 15 million children are born before the 37th week of pregnancy every year (11). In 2022, the premature birth rate in Austria was 6.9% (12). Refusal of vaccination is primarily motivated by skepticism among parents and medical staff who fear side effects in such a vulnerable cohort, but delays might also be caused by hospital stays or scheduling conflicts (13). The COVID-19 pandemic has strongly impacted almost all areas of human life. The hard-fought progress in improving vaccination adherence over the last few decades has faced considerable setbacks, indicated by increasing numbers of measles or pertussis worldwide (14–16). According to WHO and UNICEF data this was the largest decline in childhood vaccinations in 30 years. In specific, diphtheria, tetanus and pertussis vaccine coverage dropped 5% points in 2021; the first dose of measles coverage has fallen more than 7% worldwide to 81% during the pandemic, being the lowest levels since 2008 (17, 18), which means that children are at higher risk for vaccine-preventable diseases.
The aim of this study was to assess parents' adherence to the Austrian vaccination recommendations of their children within the first 2 years of life.
Therefore, the number of timely vaccinations, those booked slightly late (1–3 months), the number of appointments booked with a significant delay (>3 months), and the number of refused vaccinations were investigated. Furthermore, possible reasons for vaccination delays and rejections are explored, as well as their connection to preterm birth, the COVID-19 pandemic, and sources of information about vaccinations.
Material and methods
Study design
This retrospective cross-sectional study was conducted at the “First Vienna Pediatric Medical Center” from January to February, 2023. Over 57,000 patients are seen at this center annually, or 16% of all outpatient care in Vienna. It is, therefore, the largest primary care facility in Austria (as of 2015) (19).
Study population
Children aged 2 to 5 years who had an Austrian mother-child pass and spent the first 2 years of life in Austria were included. For better comparability, children who did not undergo the routine mother child pass examinations at the study center were excluded.
The Ethics Committee of the Medical University of Vienna (EK No. 1964/2023) approved this study. The legal guardians were informed about the study and had to give written consent.
The study involved a questionnaire (Supplementary Table 1) with general information about the participant (age, gender, preterm birth) and socioeconomic factors (father's/mother's age at birth, current father's/mother's age, highest educational qualification, number of siblings). Further information was collected regarding the accuracy, timeliness, and completeness of the vaccinations according to the Austrian vaccination recommendations in the first 2 years of life and information about the effects of the COVID-19 pandemic on vaccination behavior. To increase data accuracy, the study team checked the vaccination times from the vaccination certificate, calculated the age in months and compared them with the recommended vaccination time intervals. The vaccination appointments and intervals based on the recommendations of the Austrian vaccination schedule were examined and compared to determine minor (one to 3 months) or significant (>3 months) delays, as well as rejections. Respondents were asked to provide their motivations for delayed or rejected vaccinations. The vaccinations against rotavirus, pneumococcus, MMR, the hexavalent vaccine, and the first two doses against meningococcal B were considered delayed if administered at least 1 month later than the recommended schedule, which then was further divided into minor delays (1–3 months late) and significant delays (>3 months late). The vaccinations against meningococcal ACW135Y, TBE, hepatitis A, varicella, and the third meningococcal B dose were considered delayed if administered after the age of two (second birthday).
Data regarding the source of information about vaccinations and the impact of the COVID-19 pandemic on vaccination behavior were then analyzed.
Statistics
The data collected in this study was entered as raw data in an Excel file and analyzed using IBM SPSS Statistics Version 29.0 software. The statistical significance level was set at p < 0.05. As this study was conducted over a fixed period of time (2 months), it was the aim to include at least 150 children (N). This number was set in consultation with a statistician in order to be able to represent a representative collective in this descriptive study over a fixed observation time. For this reason, a power analysis was not performed.
The nominal variable timing of vaccinations was divided into four groups: on time, 1–3 months late, more than 3 months late (summarized as vaccinated) and not vaccinated, which also resulted in the vaccination coverage rates. Other nominal variables were gender, preterm birth, reasons for vaccination delays/refusals, source of information regarding vaccinations, changes in vaccination behavior due to the Covid-19 pandemic and reasons for changes in vaccination behavior due to the Covid-19 pandemic. The nominal as well as the ordinal variable highest educational qualification were each given in absolute and relative frequencies (in %). For most metric data (father's age at birth, mother's age at birth, father's current age, mother's current age and number of siblings), the mean value and the 1st and 3rd quartiles were given for the number of valid values (n). The data for the metric variable age of the child, on the other hand, was determined with minimum and maximum. The descriptive statistics of the patient collective were presented using absolute and relative frequencies, the arithmetic mean and the interquartile range. Furthermore, the vaccination coverage rates (fully and partially immunized) as well as the timing of all vaccinations (total of all vaccinations, individual vaccines, free and paid vaccinations) were presented with absolute and relative frequencies. All reasons for vaccination delays and refusals (total of all vaccination delays and refusals, individual vaccines, free and paid vaccines) were also presented, as well as the data on the impact of the Covid-19 pandemic on vaccination behavior and the reasons for the change in vaccination behavior during the Covid-19 pandemic.
A chi-square test (χ2) was used to examine the categorical variables premature birth and vaccination delays or refusals (on time, 1–3 months late, >3 months late and not vaccinated) in total and in subdivision of the individual vaccinations as well as the paid and free vaccinations. The connection between the source of information regarding vaccinations and vaccination delays or refusals was analyzed. To check the effect size of the chi-square tests, Cramer's V was used on the basis of the classification according to Rea and Parker (r = 0.10–0.20 weak correlation, r = 0.20–0.40 moderate correlation and r = 0.40–0.60 relatively strong correlation) (20). The Bonferroni correction was applied to avoid errors due to multiple testing (21).
Results
One hundred fifty children between the ages of two (after 2nd birthday) and five (before 5th birthday) who spent their first 2 years in Austria and had an Austrian mother child pass issued by the “First Vienna Pediatric Medical Center” were included in this study during the observation period from January to February, 2023. Among our study cohort, 48.7% were male, and 51.3% were female; 17.3% were born before the 37th week of pregnancy (Supplementary Table 2).
General clinical data
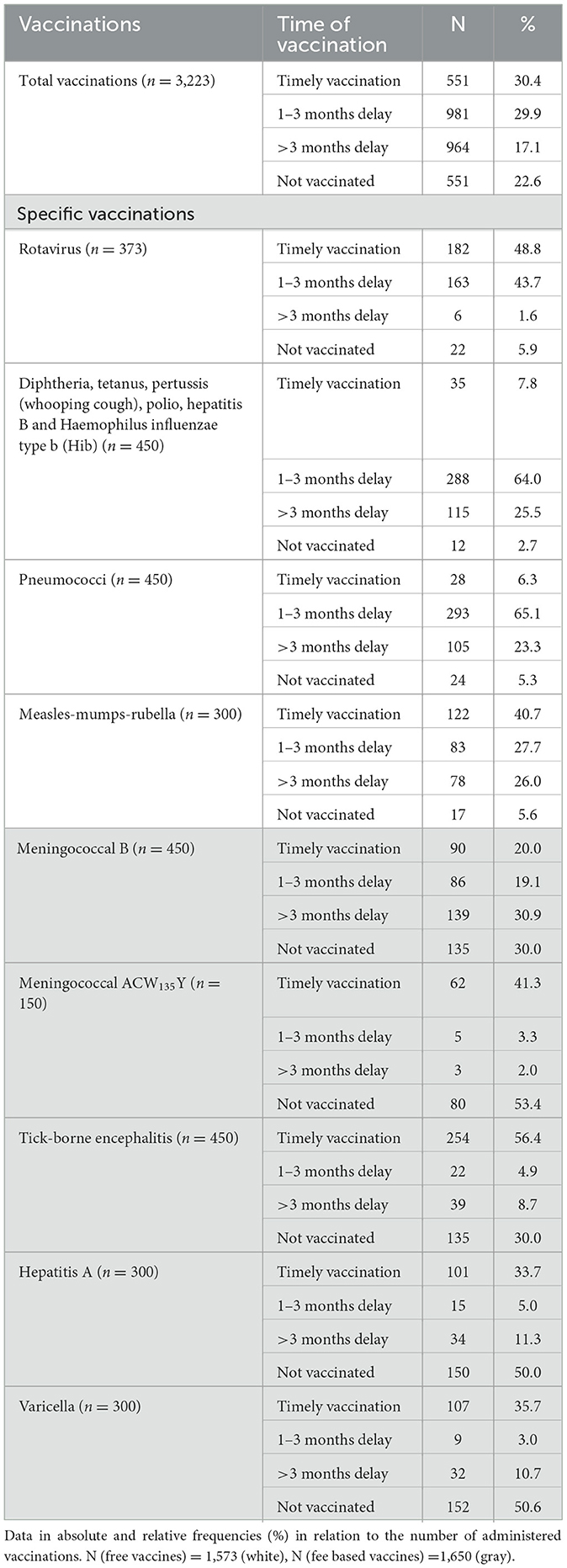
According to the Austrian vaccination plan, timely vaccinations are administered within the recommended month. Minor delays refer to “up to 3 months,” and significant delays indicate “>3 months”. In total, 22.6% of the recommended vaccinations were not administered (Table 1), while 77.4% (n = 2,496) vaccines were administered either on time or delayed. Overall, vaccinations against rotavirus (48.8%) and against TBE (56.4%) and MMR (40.7%) were most often administered on time. The hexavalent vaccination (64.0%), and the pneumococcus (PCV) (65.1%) were most frequently performed with a delay of one to three months.
In contrast, patients received vaccinations against meningococcal B (30.9%) with >3 months delay. Vaccinations against meningococcal ACW135Y (53.4%), hepatitis A (50.0%), and varicella (50.6%) were the most refused (Table 1).
Vaccination rate for the entire patient population
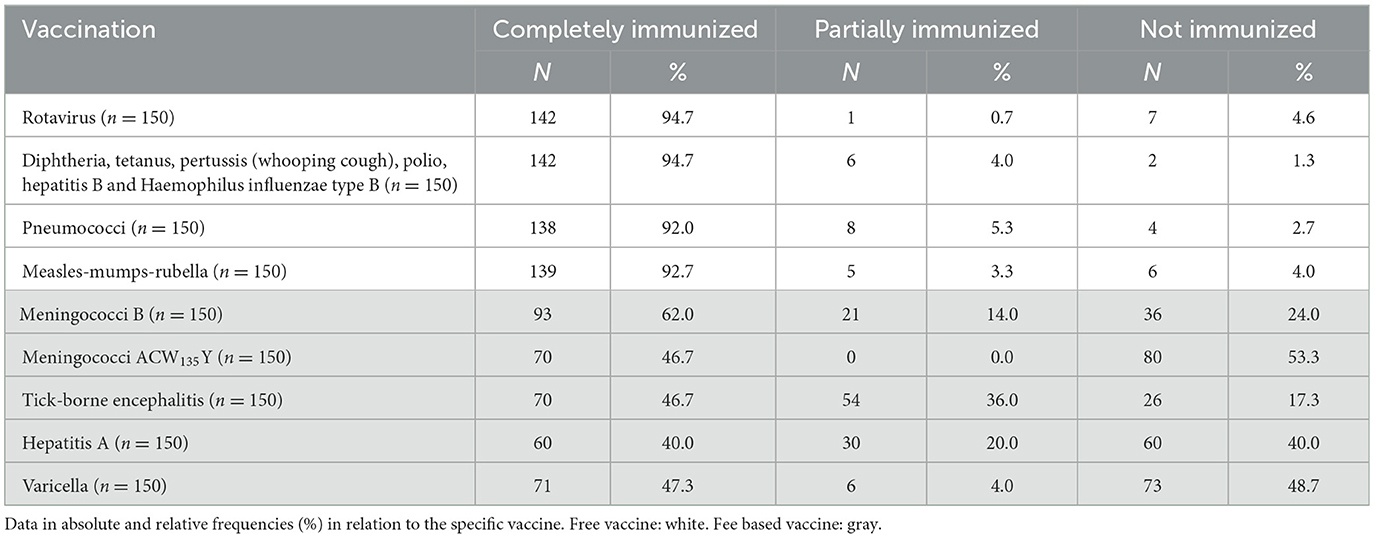
Complete vaccination coverage means all doses were administered; partial signifies one or more doses were not administered. The patient is considered not immunized in case of failure to administer even a single dose. We observed high complete vaccination rates (above 90%) for the cost-free vaccinations (rotavirus, hexavalent, PCV and MMR). In the case of more fee based vaccinations, however, the vaccination rates of those who are fully immunized ranged between 40% and 62% (Table 2).
Effect of preterm birth on vaccination adherence
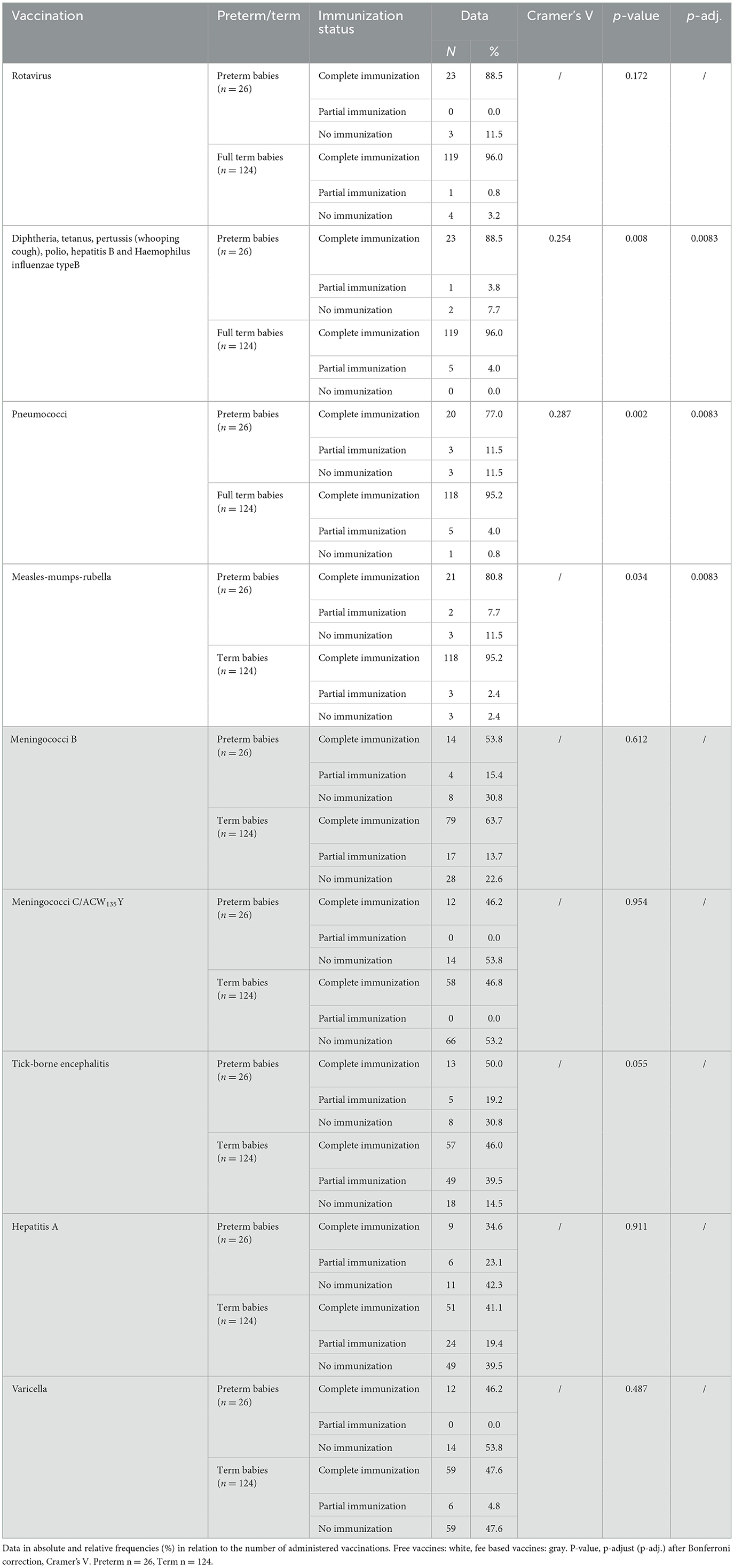
A connection between premature births and rejected vaccinations was observed, with 29.3% of all vaccinations being rejected for premature babies and only 21.1% in full-term babies (Cramer's V 0.075/p < 0.001/p-adj. = 0.006) (Supplementary Table 3).
Vaccinations against rotavirus (41.5%) and TBE (48.7%) were most frequently administered on time to premature babies. The hexavalent vaccination (48.7%), the one against PCV (52.6%), and MMR vaccines (34.6%) were administered 1–3 months late in most cases. Vaccinations against meningococcal B (30.8%) were most frequently delayed by >3 months. In contrast, vaccinations against meningococcal ACW135Y (53.8%), hepatitis A (53.8%), and varicella (53.8%) were mostly rejected (Supplementary Table 3).
Among the fully immunized pre-term children, the vaccination coverage is between 77.0% and 88.5% (free vaccinations), while the fee based vaccinations rate falls between 34.6% and 53.8%. 96.0% of the full-term babies, but only 88.5% of the premature babies, received all hexavalent vaccinations (Cramer's V 0.254/p = 0.008/p-adj. 0 0083). 95.2% of full-term infants are completely immunized against PCV, while only 4.0% remain partially immunized. In comparison, 77.0% of premature infants receive total immunization and 11.5% partial immunization against PCV (Cramer's V 0.287/p = 0.002/p-adj. 0 0083) (Table 3).
Timely administration of vaccinations
As for the free vaccines, 21 children (14.0%) of the entire cohort (n = 150) received all shots against rotavirus, one child received all partial vaccinations against PCV (0.7%), and 29 children (19.3%) were both times vaccinated against MMR on time. No child (0.0%) received all hexavalent vaccinations on time. In contrast, as for the fee based vaccinations, four children (2.7%) received all vaccinations against meningococcal B, 62 children (42.3%) were completely vaccinated against meningococcal ACW135Y, 23 children (15.3%) received all partial vaccinations against TBE, 29 Children (19.3%) got both vaccinations against hepatitis A, and 49 children (32.7%) were administered both partial vaccinations against varicella on time.
Reasons for vaccination delays and refusal
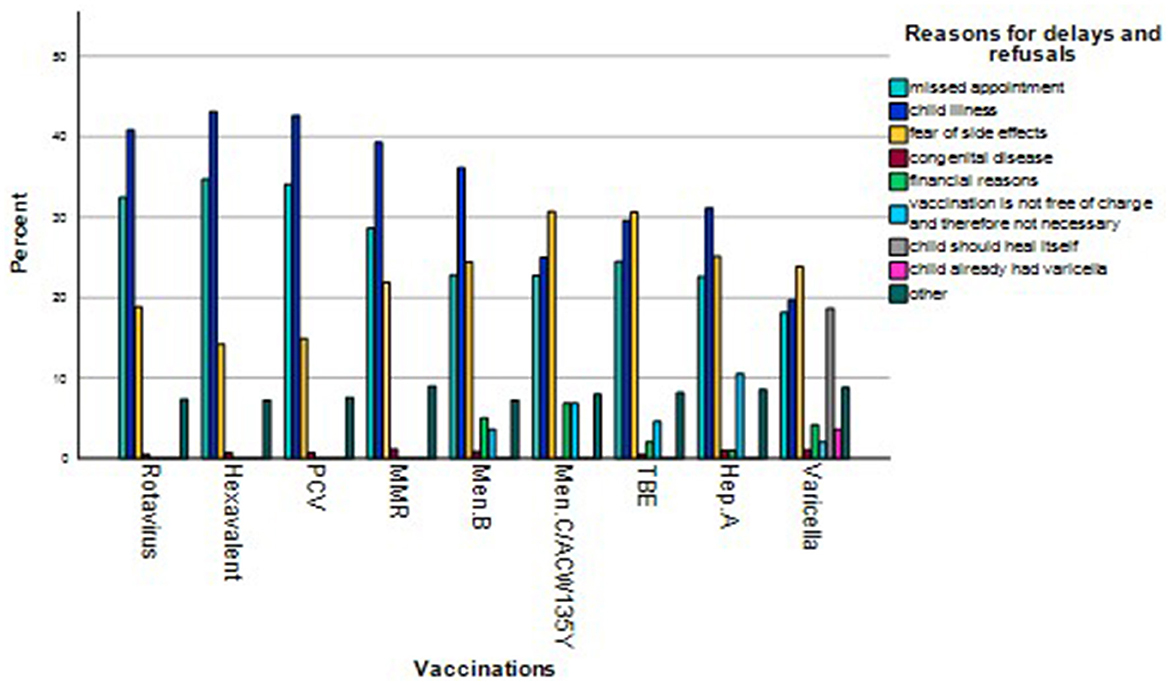
The main reasons for vaccination delays and refusal include “missed appointment” (28.1%) and “child illness” (36.4%). However, other factors, such as “fear of side effects” (20.9%), “financial reasons” (1.7%), or “vaccination is not free and therefore not essential” (2.4%), also play a role (Table 4).
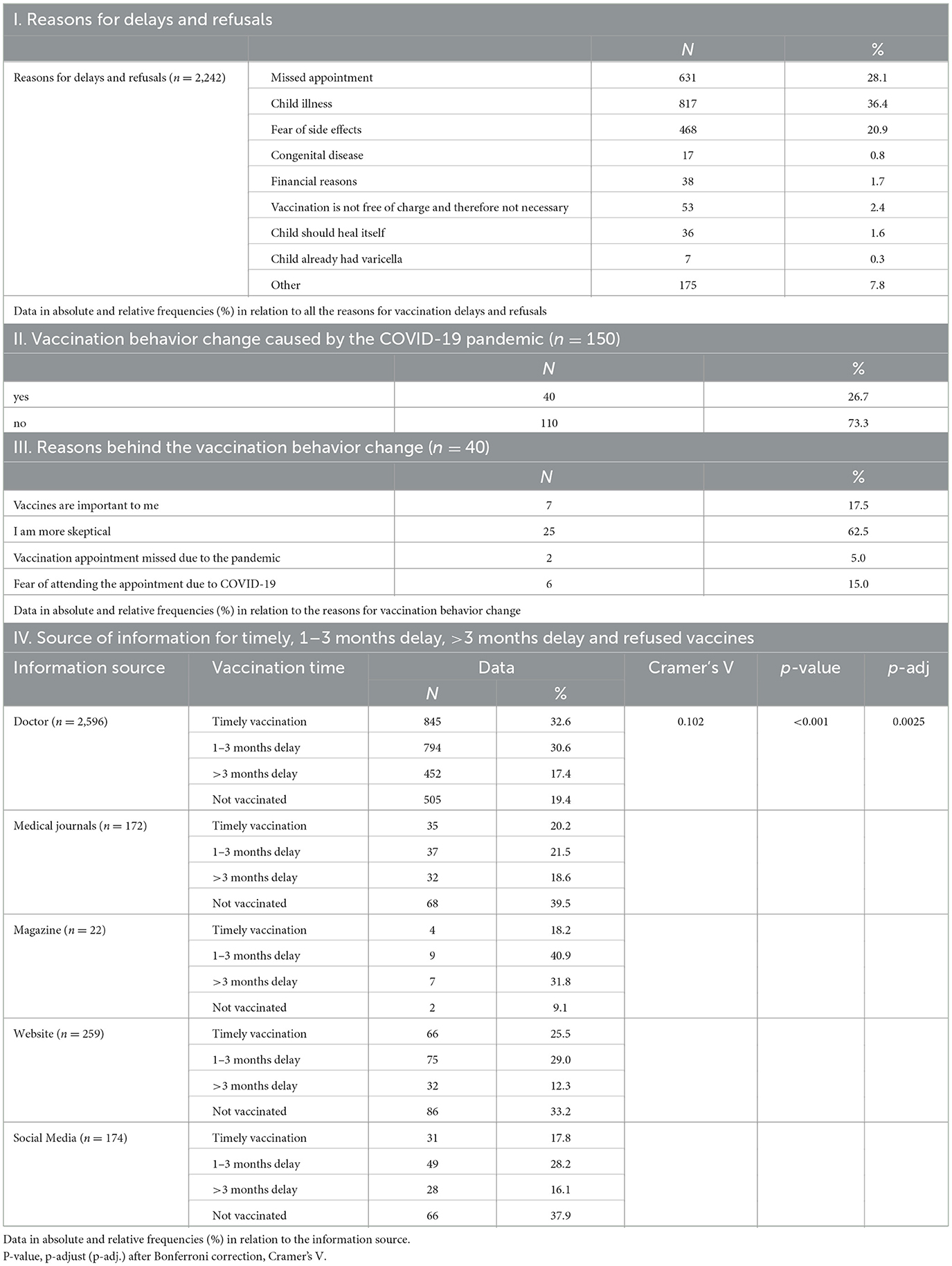
Table 4. Reasons for delays/Vaccination behavior change caused by the COVID-19 pandemic/Source of information.
While “missed appointment” and “child illness” were the most frequent reasons for vaccination delays and refusals for free vaccinations, “fear of side effects” is the prevailing answer for fee based vaccinations. However, in some cases, “financial reasons” and “vaccination is not free and therefore not essential” were also cited as reasons for delayed and refused vaccinations (Figure 1).
There is a strong correlation in the entire cohort between free or fee based vaccinations and timely, but also delayed or not carried out vaccinations, with 95.0% of the free vaccines but only 60.5% of the fee based ones being administered (Cramer's V 0.562/p < 0.001/p-adj. = 0.00625) (Table 5). While free vaccinations are more likely to be carried out late, fee based vaccinations are more likely to be refused. This finding also indicates a moderate correlation between free or fee based vaccinations and vaccinations carried out or refused in premature babies, with 97.5% of the free vaccinations and only 63.2% of fee based vaccinations administered to premature infants (Cramer's V 0.4/p < 0.001/p-adj. = 0.0083) (Table 5).
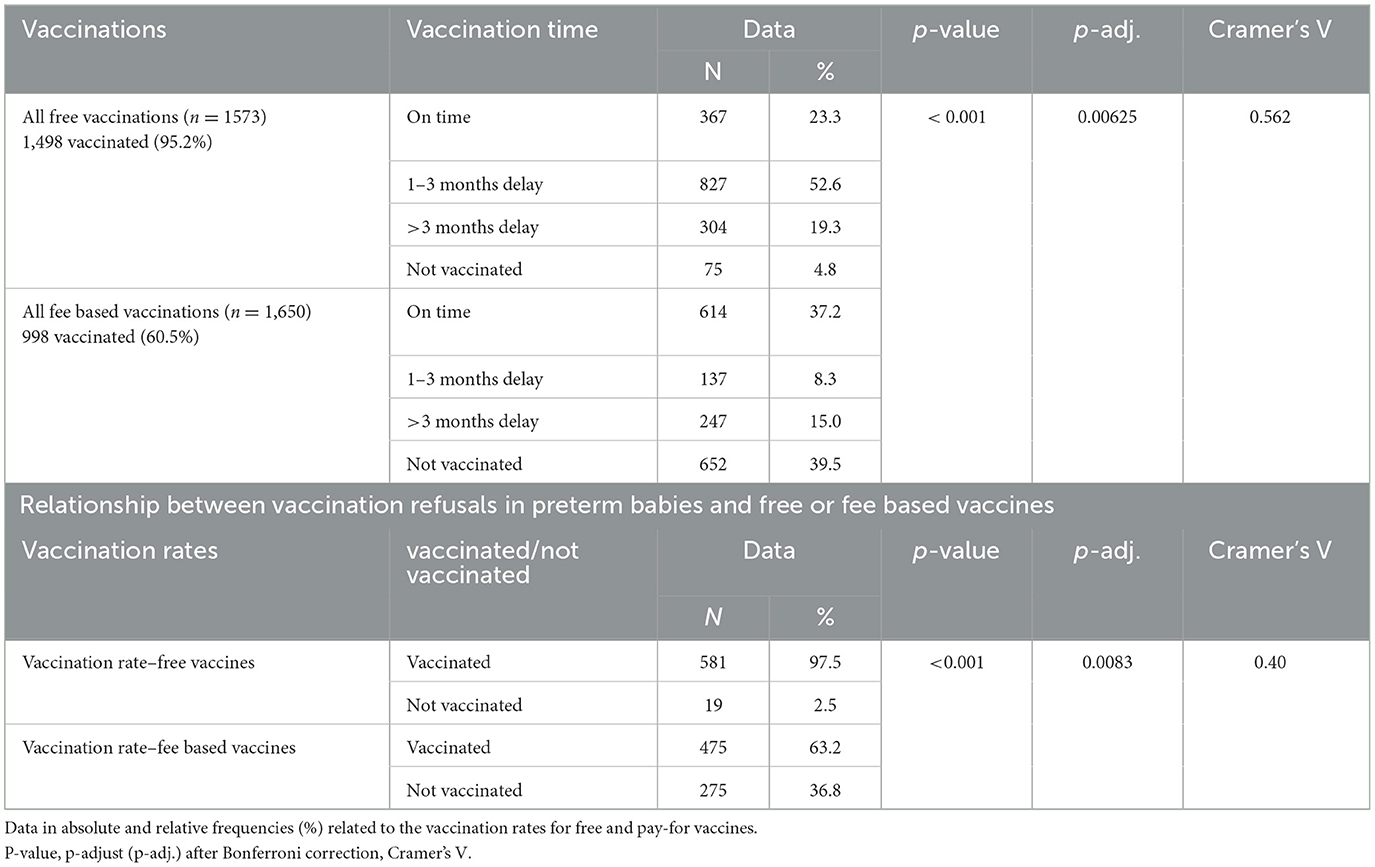
Table 5. Vaccination time for free and fee based vaccinations of the entire cohort/Relationship between refusals in preterm babies and free or fee based vaccinations.
Impact of the COVID-19 pandemic
Of the legal guardians who reported that the COVID-19 pandemic changed their vaccination attitude, over 26% became more hesitant. For some, however, the pandemic has strengthened their pro-vaccination stance (Table 4).
Source of information
Physicians are the most reliable advisors regarding vaccinations. Therefore, consultations appear connected to the percentage of timely and refused vaccinations, with 32.6% of timely vaccinations and only 19.4% rejected appointments.
The role of social media in conveying information regarding vaccinations is also fundamental (Cramer's V 0.102/p < 0.001/p-adj. = 0.0025) (Table 4).
Discussion
While the vaccination rate among fully immunized children is over 90% when it comes to free vaccinations, that of fee based vaccinations fluctuates between 40% and 62%. While free vaccinations tend to be performed late, fee based vaccinations are more likely to be refused, which results in a moderate correlation between free or fee based vaccinations and administered or refused ones. Furthermore, a strong correlation emerges between free or fee based vaccinations and vaccinations administered on time, with a delay, or not at all. A comparison between the vaccination rates among premature and full-term infants proves that the first group is typically less likely to be vaccinated than the second one. Vaccines against meningococcal ACW135Y, hepatitis A, and varicella are most frequently refused, both among premature babies and the entire patient population. There is a slight correlation between preterm birth and lack of immunization when it comes to free vaccinations. In the case of fee based vaccinations, however, there is no connection between prematurity and vaccination delays/rejections. The main reasons behind delays and refusals include child illness and missed appointments. However, the fear of side effects is also common for fee based vaccinations, followed by financial reasons and the assumption that the vaccines that come for a cost are negligible. For around a quarter of legal guardians, vaccination behavior has changed so considerably due to the COVID-19 pandemic that some have become highly skeptical.
Doctors are the most influential information providers when it comes to vaccines. There is a slight connection between information providers and timely and rejected vaccinations.
We categorized delayed vaccinations for those vaccines being recommended in the first year of life into minor delays (1–3 months) and significant delays (>3 months). Other studies have also defined 1 month late as a delay in vaccination schedules (22). It is believed that this delay should not put the child at any significant risk. Prior to this study, we have observed that short delays of a few weeks might mainly be due to infections or problems making an appointment. However, longer delays seem to be associated with skepticism, which is why we wanted to analyze differences with this classification. For the vaccines recommended after the first birthday a delay was defined as vaccination after the age of two. This is because in Austria a number of vaccinations are recommended in the second year of life without any clear ranking. A ranking is then also based on seasonality, e.g. tick vaccination in spring and summer.
This hypothesis was in line with our results, as delays < 3 months are often due to financial reasons or increased infection rates in the winter months, also among premature babies. In this case, scheduling conflicts seem to play a significant role. Delays >3 months are primarily motivated by skepticism.
In this study, the vaccination rate of those fully immunized against rotavirus was 94.7%, against 80% reported in international studies (23, 24). For vaccinations against MMR, the percentage was 92.7%, compared to 78.3% in Germany and Austria (25), 78% in the Netherlands (26), and 94.3% in the USA (27). The vaccination rates against meningococcal B and TBE in this study reached 62.0% and 46.7%, respectively, higher than those observed abroad (28.9%, 10%) (28–30). The vaccination rate of the fully immunized against varicella in this study is 47.3%. Research efforts in Poland and Sweden document that varicella vaccinations are not part of the national routine vaccination schedule, and vaccination rates only reach 4.2% and 15%, respectively (31). In general, in Austria, vaccinations are not mandatory (6).
Since premature babies are immunologically immature, they are at exceptionally high risk for infectious diseases (13), and their need for increased medical attention may increase the risk of infections (32); early and complete immunization is essential in this patient group (33). The vaccination rate of fully immunized premature infants observed in this study is 88.5% for hexavalent vaccinations and 76.9% against PCV. A German study, however, describes that only 47% of premature babies received all vaccines against pneumococci, while 71% had received all hexavalent doses. However, premature babies were vaccinated according to the 3+1 vaccination schedule (34). Contrarily, our cohort's immunization routine followed the 2+1 system.
Austria is in part critical toward vaccination recommendations. Especially during the COVID-19 pandemic, the population and parents were confronted with false information in social media by so-called self-proclaimed experts. In a recent Austrian study, vaccine hesitancy was motivated by concerns about “personal freedom restriction”, “lack of trust in the pharmaceutical industry” and “lack of trust in the government” which were not receptive to discussion. However, concerns such as “side effects”, “long-term side effects” and “questionable benefit of vaccination” could be ruled out by evidence-based information. Parental vaccination hesitancy and social characteristics such as gender, educational level, economic status or political opinion are associated (35).
As mentioned, the COVID-19 pandemic sparked the vaccination debate worldwide. According to the WHO, the PCV vaccination rate plunged from 86% in 2019 to 83% the following year, or 22.7 million children who did not receive their vaccine doses (36), meaning preventive measures reduced vaccination rates. In contrast, our findings show a vaccination rate of 92% for those fully immunized against PCV. The correlation between timely vaccinations, refused vaccination, and legal guardians who receive information about vaccination from their physicians indicates that doctors' recommendations contribute greatly to both timely administration and refusals. A Danish study shows that positive attitudes toward MMR vaccination among general practitioners led to average vaccination rates of 85%, compared to 69% in practices with stronger hesitancy toward vaccination (37).
Limitations
The data of children whose parents refused to participate could not be recorded. Additionally, children whose parents are totally against vaccines also refused to take part in the study, which indeed leads to a data bias. Another limiting factor is the monocentric study design. However, the “First Vienna Pediatric Medical Center” is the largest group practice in Austria, meaning our study population can be considered reasonably representative. In addition, “child illness” and “missed appointment” were mentioned frequently as reasons for vaccination delays and refusals, which may indicate a participant bias.
Conclusion
In summary, vaccination coverage rates are quite remarkable in our study. These are over 90% for the free vaccinations and between 40% (hepatitis A) and 62.0% (meningococcal B) for the fee based vaccinations. There is a strong connection between free and administered vaccinations and between fee based and refused vaccinations, with 95.2% of the free vaccinations being accepted as opposed to only 60.5% of the fee based vaccinations. Except for TBE, the vaccination coverage of premature babies is below that of full-term babies. Approximately the same percentage of free and fee based vaccinations were administered on time. While free-of-charge vaccinations are more likely delayed in the entire patient population and in premature babies, fee based vaccinations are more likely rejected.
As for free vaccinations, we noticed a mild correlation between premature births and rejected vaccinations. While “child illness” and “missed appointment” are the most frequent reasons for vaccination delays and refusals for free vaccinations, “fear of side effects” is the most common for vaccinations that are not free of charge. In addition, the COVID-19 pandemic influenced legal guardians' vaccination behavior and increased their hesitancy. The importance attached to the role of the doctor can significantly influence the vaccination behavior of many. Considering these findings, information about vaccines could be more efficiently delivered, especially in relation to premature babies and specific fee based vaccinations.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Medical University of Vienna (EK No. 1964/2023). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
RM: Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. PV: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JV: Data curation, Formal analysis, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SD-T: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1438737/full#supplementary-material
References
1. Benn CS, Fisker AB, Rieckmann A, Sørup S, Aaby P. Vaccinology: time to change the paradigm? Lancet Infect Dis. (2020) 20:e274–83. doi: 10.1016/S1473-3099(19)30742-X
2. Campagne G, Garba A, Schuchat A, Boulanger D, Plikaytis BD, Ousseini M, et al. Response to conjugate Haemophilus influenzae B vaccine among infants in Niamey, Niger. Am J Trop Med Hyg. (1998) 59:837–42. doi: 10.4269/ajtmh.1998.59.837
3. Shattock AJ, Johnson HC, Sim SY, Carter A, Lambach P, Hutubessy RCW, et al. Contribution of vaccination to improved survival and health: modelling 50 years of the Expanded Programme on Immunization. Lancet. (2024) 403:2307–16. doi: 10.1016/S0140-6736(24)00850-X
4. Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. (2013) 9:1763–73. doi: 10.4161/hv.24657
5. Ryan J, Malinga T. Interventions for vaccine hesitancy. Curr Opin Immunol. (2021) 71:89–91. doi: 10.1016/j.coi.2021.05.003
6. Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz. Impfplan Österreich 2023/2024 (2023). Available at: https://www.sozialministerium.at/dam/jcr:32a90bf4-6728-432e-ae5b-f52bd07c25c0/Impfplan_%C3%96sterreich_2023_2024_Version_2.0_vom_14.5.2024_pdfUA.pdf (accessed September 2, 2024).
7. Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz. Kurzbericht Masern (2023). Available at: https://www.sozialministerium.at/dam/jcr:04d0e207-6564-4bef-add1-c6d3b03f66f4/Kurzbericht_Masern_2022_Version%201.0.pdf (accessed December 10, 2023).
8. Bundesministerium für Soziales, Gesundheit, Pflege und Konsumentenschutz. Kurzbericht Polio (2023). Available at: https://www.sozialministerium.at/dam/jcr:0fe489fa-d919-4b08-ae64-37000415022c/Kurzbericht_Polio_2022_Version%201.0.pdf (accessed December 10, 2023).
9. Howson CP, Kinney MV, McDougall L, Lawn JE. The born too soon preterm birth action group. Born too soon: preterm birth matters. Reprod Health. (2013) 10:S1. doi: 10.1186/1742-4755-10-S1-S1
10. Riise ØR, Laake I, Vestrheim D, Flem E, Moster D, Riise Bergsaker MA, et al. Risk of pertussis in relation to degree of prematurity in children less than 2 years of age. Pediatr Infect Dis J. (2017) 36:e1516. doi: 10.1097/INF.0000000000001545
11. Locke A, Kanekar S. Imaging of premature infants. Clin Perinatol September. (2022) 49:641–55. doi: 10.1016/j.clp.2022.06.001
12. Statista Austria. Anteil der Frühgeborenen in Österreich (2023). Available at: https://de.statista.com/statistik/daten/studie/1018502/umfrage/anteil-der-fruehgeborenenin-oesterreich/ (accessed November 15, 2023).
13. Laurenz M, von Eiff C, Borchert K, Jacob C, Seidel K, Schley K. Vaccination rates and adherence in premature infants before and after pneumococcal conjugate vaccine schedule change for term infants - a claims database analysis in Germany. Vaccine. (2021) 39:7387–93. doi: 10.1016/j.vaccine.2021.11.002
14. Habas K, Nganwuchu C, Shahzad F, Gopalan R, Haque M, Rahman S, et al. Resolution of coronavirus disease 2019 (COVID-19). Expert Rev Anti Infect Ther. (2020) 18:1201–11. doi: 10.1080/14787210.2020.1797487
15. Olusanya OA, Bednarczyk RA, Davis RL, Shaban-Nejad A. Addressing parental vaccine hesitancy and other barriers to childhood/adolescent vaccination uptake during the Coronavirus (COVID-19) pandemic. Front Immunol. (2021) 12:663074. doi: 10.3389/fimmu.2021.663074
16. Elam-Evans LD, Yankey D, Singleton JA, Sterrett N, Markowitz LE, Williams CL, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years — United States, 2019. MMWR Morb Mortal Wkly Rep. (2020) 69:1109–16. doi: 10.15585/mmwr.mm6933a1
17. UNICEF. Immunization (2024). Available at: https://data.unicef.org/topic/child-health/immunization/ (accessed August 1, 2024).
18. Locke J, Marinkovic A, Hamdy K, Balendra V, Sanyaolu A. Routine pediatric vaccinations during the COVID-19 pandemic: a review of the global impact. World J Virol. (2023) 12:256–61. doi: 10.5501/wjv.v12.i5.256
19. Schwab E, Voitl P, Loeffler-Stastka H. Primary Healthcare Center: Möglichkeiten, Strukturen und Grenzen von Primärversorgungseinheiten. Psychopraxis Neuropraxis. (2018) 21:276–8. doi: 10.1007/s00739-018-0494-y
20. Kotrlik J, Williams H, Jabor K. Reporting and interpreting effect size in quantitative agricultural education research. JAE. (2011) 52:132–42. doi: 10.5032/jae.2011.01132
21. Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. (2014) 34:502–8. doi: 10.1111/opo.12131
22. Choudhary TS, Reddy NS, Apte A, Sinha B, Roy S, Nair NP, et al. Delayed vaccination and its predictors among children under 2 years in India: insights from the national family health survey−4. Vaccine. (2019) 37:2331–9. doi: 10.1016/j.vaccine.2019.03.039
23. Marquis A, Koch J. Impact of routine rotavirus vaccination in Germany: evaluation five years after its introduction. Pediat Infect Dis J. (2020) 39:e109. doi: 10.1097/INF.0000000000002656
24. Kempe A, O'Leary ST, Cortese MM, Crane LA, Cataldi JR, Brtnikova M, et al. Why aren't we achieving high vaccination rates for rotavirus vaccine in the U. S? Acad Pediatr. (2022) 22:542–50. doi: 10.1016/j.acap.2021.07.003
25. Kohler S, Koinig I. The effect of science-related populism on vaccination attitudes and decisions. J Behav Med. (2023) 46:229–38. doi: 10.1007/s10865-022-00333-2
26. Klomp JHE, van Lier A, Ruijs WLM. Vaccination coverage for measles, mumps and rubella in anthroposophical schools in Gelderland, The Netherlands. Eur J Public Health. (2015) 25:501–5. doi: 10.1093/eurpub/cku178
27. Mellerson JL, Maxwell CB, Knighton CL, Kriss JL, Seither R, Black CL. Vaccination coverage for selected vaccines and exemption rates among children in kindergarten — United States, 2017–18 School Year. MMWR Morb Mortal Wkly Rep. (2018) 67:1115–22. doi: 10.15585/mmwr.mm6740a3
28. Souliotis K, Golna C, Kotsopoulos N, Kapaki V, Dalucas C. Meningitis B vaccination: knowledge and attitudes of pediatricians and parents in Greece. Heliyon. (2018) 4:e00902. doi: 10.1016/j.heliyon.2018.e00902
29. Erber W, Schmitt HJ. Self-reported tick-borne encephalitis (TBE) vaccination coverage in Europe: results from a cross-sectional study. Ticks Tick-borne Dis. (2018) 9:768–77. doi: 10.1016/j.ttbdis.2018.02.007
30. Zens KD. Tick-borne encephalitis - viral transmission and considerations for vaccination. Ther Umsch. (2022) 79:471–81. doi: 10.1024/0040-5930/a001390
31. Arnheim-Dahlström L, Zarabi N, Hagen K, Bencina G. Parental acceptance and knowledge of varicella vaccination in relation to socioeconomics in Sweden: a cross-sectional study. PLoS ONE. (2021) 16:e0256642. doi: 10.1371/journal.pone.0256642
32. Steiner L, Diesner SC, Voitl P. Risk of infection in the first year of life in preterm children: an Austrian observational study. PLoS ONE. (2019) 14:e0224766. doi: 10.1371/journal.pone.0224766
33. Omeñaca F, Vázquez L, Garcia-Corbeira P, Mesaros N, Hanssens L, Dolhain J, et al. Immunization of preterm infants with GSK's hexavalent combined diphtheria-tetanus-acellular pertussis-hepatitis B-inactivated poliovirus-Haemophilus influenzae type b conjugate vaccine: a review of safety and immunogenicity. Vaccine. (2018) 36:986–96. doi: 10.1016/j.vaccine.2018.01.005
34. Schley K, Borchert K, Seidel K, Jacob C, von Eiff C, Laurenz M. Did the change of the vaccination schedule effect pneumococcal conjugate vaccination compliance and adherence of premature and mature born infants in Germany? Answers from a claims database analysis. Vaccine. (2023) 41:4081–91. doi: 10.1016/j.vaccine.2023.05.045
35. Lenart C, Prager M, Sachs M, Steininger C, Fernandes C, Thannesberger J. Tackling vaccine hesitancy and increasing vaccine willingness among parents of unvaccinated children in Austria. Int J Public Health. (2023) 68:1606042. doi: 10.3389/ijph.2023.1606042
36. Jiang BS, Feng LZ. [Understanding the behavioural and social drivers of vaccine uptake: introduction and implications of World Health Organization Position Paper, 2022]. Zhonghua Yu Fang Yi Xue Za Zhi. (2022) 56:1494–8. doi: 10.3760/cma.j.cn112150-20220706-00686 (Chinese).
Keywords: adherence, vaccination, children, COVID-19, Austria, preterm birth
Citation: Magyar R, Voitl PK, Voitl JJM and Diesner-Treiber SC (2024) Vaccine hesitancy among parents of children in their first two years of life. Front. Public Health 12:1438737. doi: 10.3389/fpubh.2024.1438737
Received: 26 May 2024; Accepted: 19 August 2024;
Published: 19 September 2024.
Edited by:
Deep Shikha, Swami Rama Himalayan University, IndiaReviewed by:
Richa Sinha, Government Doon Medical College Dehradun, IndiaSai Chandan Das, Institute of Medical Sciences and Sum Hospital, India
Copyright © 2024 Magyar, Voitl, Voitl and Diesner-Treiber. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susanne C. Diesner-Treiber, U3VzYW5uZS5kaWVzbmVyLXRyZWliZXJAa2luZGVyYXJ6dC5hdA==
†These authors have contributed equally to this work
 Ruth Magyar1†
Ruth Magyar1† Peter K. Voitl
Peter K. Voitl Julian J. M. Voitl
Julian J. M. Voitl Susanne C. Diesner-Treiber
Susanne C. Diesner-Treiber