- 1Department of Occupational Health and Safety, Faculty of Public Health, Mahidol University, Bangkok, Thailand
- 2Center of Excellence on Environmental Health and Toxicology (EHT), OPS, MHESI, Bangkok, Thailand
- 3School of Health Science, Sukhothai Thammathirat Open University, Nonthaburi, Thailand
- 4Department of Occupational Health and Safety, Faculty of Public Health and Environment, Huachiew Chalermprakiet University, Samut Prakan, Thailand
- 5Department of Medical Humanities, School of Medicine, University of Occupational and Environmental Health, Japan, Kitakyushu, Japan
Background: This study aimed to develop a mental health action checklist for high school students that emphasized the importance of readiness, safety, and good hygiene at work to enhance their mental health and prepare them for the workforce.
Methods: In total, 949 students from public high schools in Bangkok, Thailand voluntarily participated in this study. The 15-item High School Mental Health Action Checklist was developed based on a literature review and a pilot study. We used the index of item-objective congruence (IOC) to verify the content validity of the Checklist and exploratory factor analysis (EFA) to establish its construct validity. The tool’s internal consistency was estimated using Cronbach’s alpha coefficient.
Results: The High School Mental Health Action Checklist had good content (IOC = 0.867) and construct validity. EFA revealed four factors that accounted for 46.5% of the variance. The overall reliability coefficient for the High School Mental Health Action Checklist was 0.788, and the reliability coefficients of the subdomains were 0.783–0.797.
Conclusion: The Checklist will allow schools to develop an annual action plan for student mental health promotion activities, in accordance with public health guidelines. Our results indicate the High School Student Mental Health Action Checklist has good psychometric properties.
1 Introduction
Adolescence, a critical developmental stage between 10 and 24 years, is marked by heightened sensitivity to social situations and a strong need for peer interaction (1). The Coronavirus Disease 2019 (COVID-19) pandemic has sharply increased psychological distress among adolescents. This distress was partly attributable to reduced face-to-face social interactions and an increased reliance on digital communication. Importantly, this shift had lasting impacts on students’ mental health. In addition, economic challenges faced by families and the hybrid onsite/online learning model continue to influence students’ well-being in the post-pandemic environment (2, 3).
It is essential to consider theories of perception and communication, including behaviorist learning theories and cognitive approaches, to fully understand adolescents’ behaviors during this period. These theories can help explain how adolescents process information and develop mental skills. Understanding these aspects is crucial for addressing selective attention, which reflects how adolescents focus on specific stimuli in their complex social environments while ignoring others (4).
Existing mental health screening tools for secondary school students, though available (5–10), are not fully adequate under current circumstances for a thorough and consistent assessment of high school students’ mental health (11). Therefore, there is a need to develop a specialized tool that include problem-focused and emotion-focused coping strategies, considered effective in psychotherapy (12). It should allow students to express their individual mental health concerns through open-ended questions, facilitating genuine self-expression, which is vital during adolescence (13).
Action checklists, widely utilized as practical training tools in various workplaces, play a crucial role in helping participants identify areas for improvement. These checklists are designed to leverage the experiences and knowledge of participants, fostering the creation of viable solutions, lists of potential actions, or practical steps for progress (14). Participants are asked to learn from existing good examples identified in the discussion setting (15, 16).
Over the past two decades, the development of action checklists has been an ongoing process, with numerous studies affirming their effectiveness across different sectors (13–15, 17–19). The International Labour Organization (ILO) has contributed significantly to this field by creating various effective action checklists applicable in diverse areas (17). However, the application of mental health action checklists specifically tailored to certain age groups, such as high school-aged adolescents, remains relatively unexplored. Addressing the mental health needs of high school students is of paramount importance, considering their transitional phase into the workforce. In Thailand, most mental health assessments in educational settings are quantitative, and there is a lack of qualitative approaches that can offer deep insights and inform improvements. This means the development of a qualitative mental health action checklist is essential.
Therefore, this study aims to develop a mental health action checklist for high school students. Particularly, the objective is to provide high school students with a structured tool that enhances their understanding and awareness of mental health issues. This checklist is intended to serve as a practical training intervention, assisting in the improvement of mental health among adolescents preparing for the challenges of the workforce.
2 Methods
2.1 Sample size calculation
The Office of the Education Council reported that Thailand’s public schools accommodate 1,543,041 high school students aged 14–20 years (20). Of these, 116,430 high school students are enrolled in Bangkok (21). We focused on Bangkok because it is Thailand’s capital city and these students face high educational competition and have diverse economic, family, social, and intellectual backgrounds. The required sample size for this study was determined using the finite population correction for proportions. With a 99% confidence interval (CI), 5% margin of error, and maximum variability for the estimated proportion (p = 0.5), the target sample size was calculated as 662 students. We received voluntary registrations from interested students that exceeded this number meaning our sample included 949 high school students.
2.2 Participants
We conducted a cross-sectional study among high school students in Bangkok, Thailand. Participants were recruited using purposive sampling. After development, the High School Mental Health Action Checklist was distributed in schools in Bangkok (total population of 116,430 students aged 14–20 years). This study enrolled 949 high school students as volunteer participants from May to August 2022. Thailand implemented various restrictions in response to the COVID-19 pandemic that caused significant financial strain for many families. Students were previously accustomed to engaging in group activities with their families, schools, and communities, but experienced a sharp decline in these interactions following the implementation of these restrictions. The increased reliance on online activities created challenges in adapting to reduced face-to-face communication, which adversely affected students’ mental health (22). We first sought permission from four identified schools and asked them to promote participation in the research project and seek students’ consent to participate. Next, we emailed a link to the High School Mental Health Action Checklist to students that were interested in participating.
2.3 Developing the High School Mental Health Action Checklist
The High School Mental Health Action Checklist was developed based on a review of the literature relevant to mental health and stress screening and assessment by the Participatory Action-Oriented Training framework (16) and coping (1, 3), from which we created a list of semi-structured in-depth questions (7, 16, 23–26). In the next phase of development, we held comprehensive focus-group interviews with 11 experts and stakeholders, including mental health specialists, educational assessment and administration specialists, and teachers. These discussions were instrumental in drafting an initial version of the checklist, comprising 16 items specifically tailored for high school students’ mental health needs. To assess the reliability of this checklist (overall reliability coefficient of 0.661), we conducted a pilot test with 36 students. Concurrently, three experts evaluated the content validity of our draft, resulting in the refinement of the checklist to 15 items. Finally, the quality of these 15 items was rigorously assessed using the item-objective congruence (IOC) method (average 0.788).
2.4 Statistical analysis
In this study, we developed the Mental Health Action Checklist, focusing on how high school students cope with issues that impact their mental health. Descriptive statistics were used to examine participants’ characteristics, including sex, age, and grade. The IOC was used to verify the content validity of the questionnaire, and Cronbach’s alpha coefficient was used to estimate its reliability/internal consistency (theoretical range 0.00–1.00). The factor solution was determined based on the number of eigenvalues greater than 1. We conducted exploratory factor analysis (EFA) using 0.50 as the factor loading criterion to distinguish components of the High School Mental Health Action Checklist. All statistical analyses were performed with SPSS version 23.
3 Results
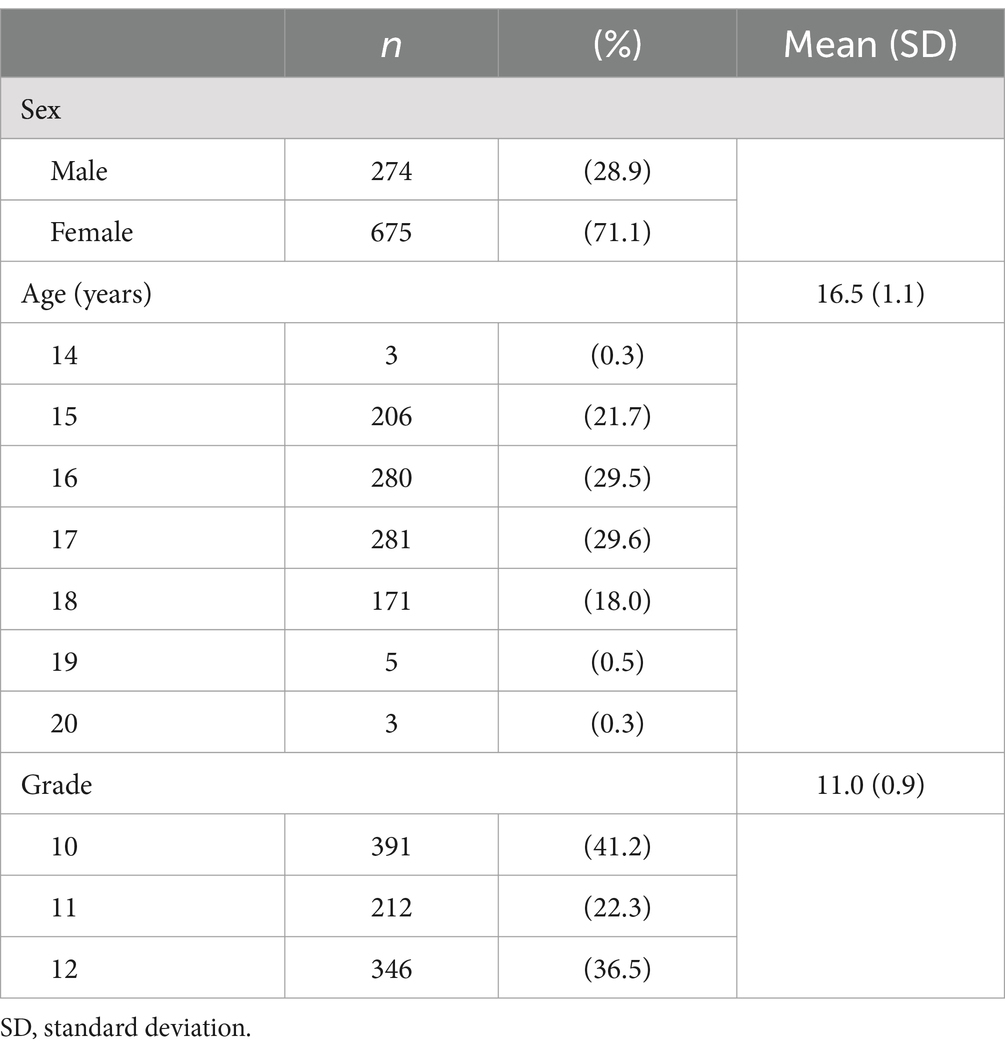
Participants’ (N = 949) demographic details are shown in Table 1. The majority of participating high school students were female (71.1%), 29.6% were aged 17 years (mean = 16.5 years, standard deviation [SD] = 1.1 years), and 41.2% were in Grade 10 (mean = 11.0, SD = 0.9).
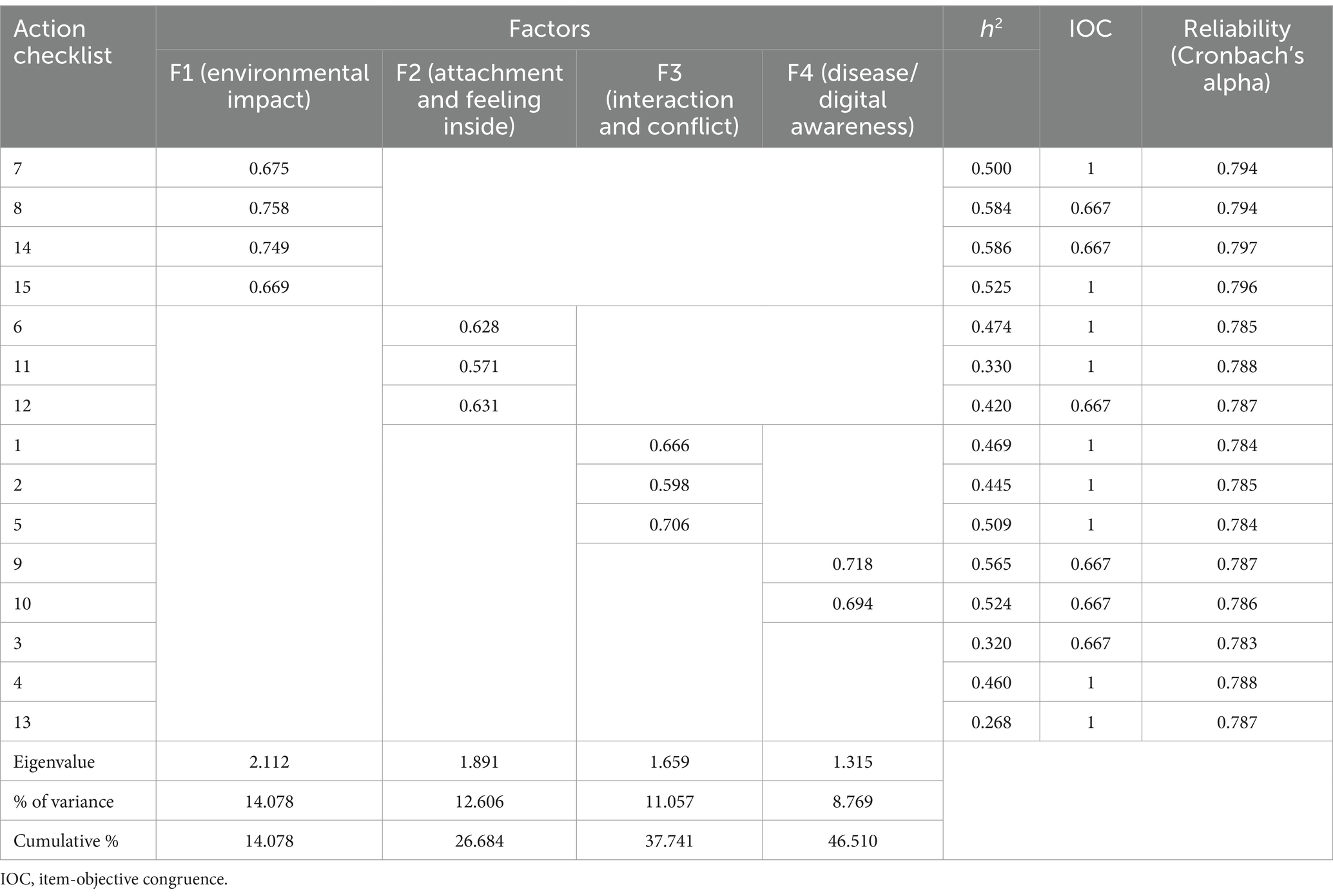
The factor structure of the High School Mental Health Action Checklist is shown in Table 2. The IOC for the checklist was 0.867, with 15 items defined as requiring revision (IOC > 0.05). Reliability coefficients ranged from 0.783 to 0.797, with an overall score of 0.788. The EFA included data for all 949 participants, and used varimax rotation because the underlying constructs were conceptualized as independent of each other. The Kaiser–Meyer–Olkin measure of sampling adequacy was 0.749, and Bartlett’s test of sphericity was statistically significant, which suggested that the correlation matrix was suitable for factor analysis. Four meaningful constructs/factors emerged: (1) environmental impact (four items), (2) attachment and feeling inside (three items), (3) interaction and conflict (three items), and (4) disease/digital awareness (two items). These factors accounted for 46.51% of the cumulative variance. Three items did not load on any of the factors.
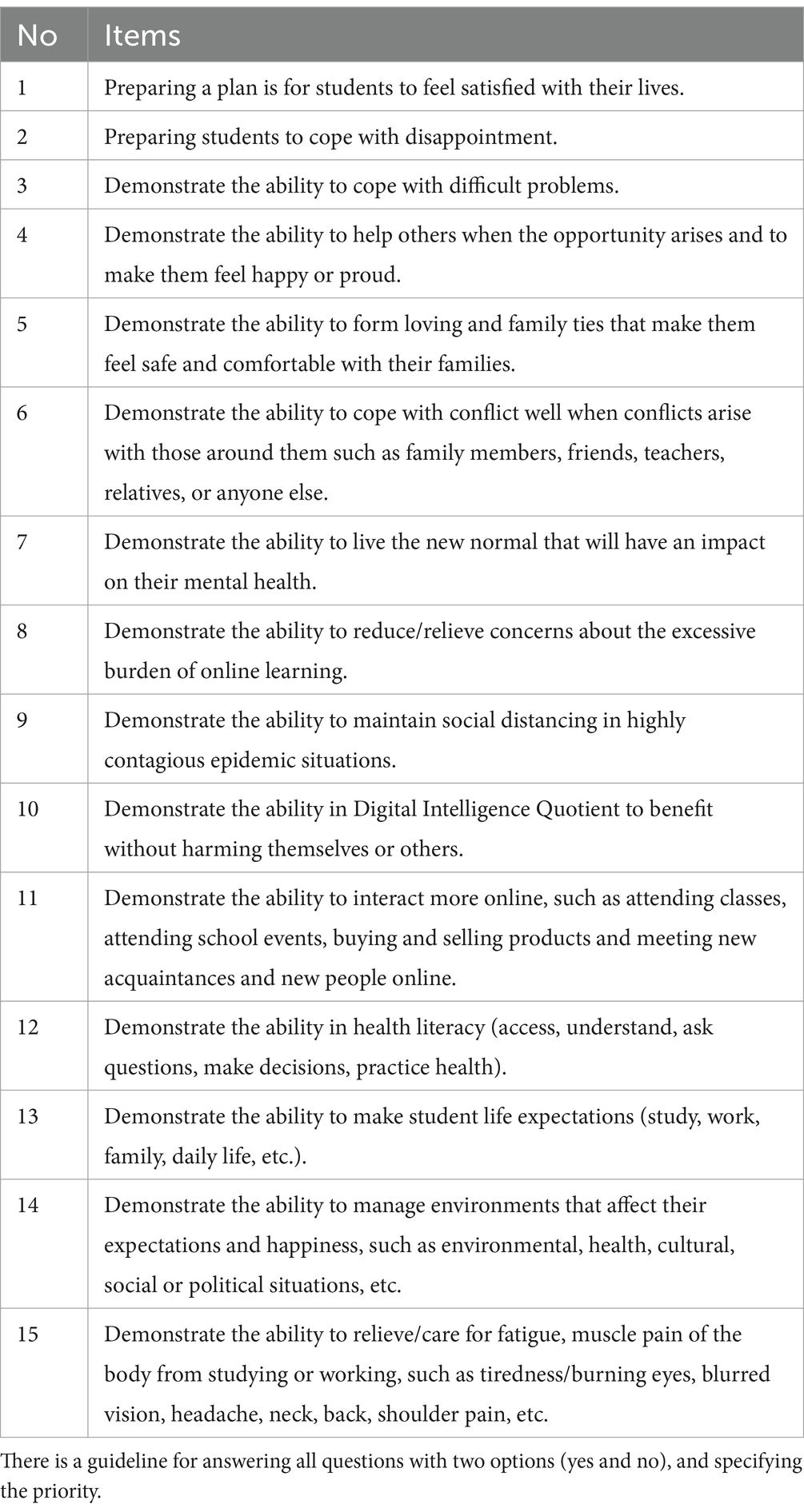
Table 3 presents the items included in the High School Mental Health Action Checklist. The Checklist asked students whether they were competent in relation to each item, and reliability coefficient testing resulted in 15-item summaries. Participants responded to this checklist without any empirical issues. All items were answered with “yes” or “no.” For higher-priority items, participants were also asked to write down their reasons or suggestions. A variety of responses were gathered regarding issues affecting participants’ mental health and their coping strategies. These insights were shared with the responsible teachers and used in further mental health promotion efforts at each school.
4 Discussion
The High School Mental Health Action Checklist was developed using the basic concepts of the ILO action checklist and demonstrated good content validity, construct validity, and reliability. Therefore, it is possible for individual students, schools, or those involved in remedial action to use the tool as a guide and method to promote mental health in schools (17).
Our study aligns with previous research indicating that EFA of similar tools typically reveals multiple factors. For instance, a recent relevant study identified five factors across 30 of 35 items, accounting for 42% of the variance. These factors included skills in seeking mental health information (27), consistent with another study focusing on the mediating role of COVID-19 coping strategies in anxiety and general health relationships (28). Our EFA distinguished three COVID-19-specific dimensions: perceived mental health impact (nine items: Cronbach’s α = 0.85), fear of COVID-19 (six items: α = 0.73), and positive coping (five items: α = 0.61). One item concerning the pandemic’s financial impact was excluded due to low factor loadings (29). This approach mirrors the structure of another action checklist encompassing 30 items across six technical areas, ranging from collaboration planning to workplace supervision (17). The High School Mental Health Action Checklist was designed to remain relevant and adaptable beyond the COVID-19 pandemic. Given that online and hybrid learning environments continue to be part of the educational landscape, this checklist will help address the ongoing mental health challenges associated with such settings. Moreover, the checklist is intended to be a dynamic tool, and items can be continually refined and updated on the basis of practical feedback following implementation in schools. This will ensure the long-term applicability and effectiveness of the instrument.
The High School Mental Health Action Checklist is expected to facilitate communication between students and teachers regarding mental health issues. Past studies have shown that action checklists can transform workplace environments, suggesting practical actions for environmental screening (18). They also facilitate rapid workplace-level discussions for effective screening (19). In our trials, some cases led to counseling or hospital treatment. For example, students who showed signs of depression or suicidal ideation received immediate support through counseling, with hospital referrals in severe cases. Later, as schools recognized the importance of mental health, they began planning training, assigning school counselors, and meeting with parents. It is noteworthy that the High School Mental Health Action Checklist that was developed in this study is used in these schools for regular mental health monitoring. Further research is necessary to confirm our checklist’s effectiveness in enhancing the school environment to improve high school students’ mental health and investigate the long-term impact on students’ decisions and well-being.
The present study had some limitations. First, this article focused on describing the development of the High School Mental Health Action Checklist, which was found to be easy to use, convenient, and accessible for student participants. It offers a questionnaire that can be used to screen students’ ability to cope with problems when encountering situations that affect their mental health. The results of the Checklist assessment were used to improve and promote the mental health of participating students. However, we cannot show that effect in this paper because the evaluation of the outcomes related to improving and promoting mental health using our Checklist has not yet been finalized. Second, this study was conducted in high schools located in and around Bangkok, Thailand. Therefore, caution should be exercised in generalizing the findings to other regions. Further research is necessary to evaluate the applicability of the High School Mental Health Action Checklist in different contexts, such as in other countries and different age groups, to ensure its effectiveness and adaptability across various settings. Third, the survey was conducted during the period of transition from online to on-site classes following the lifting of COVID-19 lockdown restrictions, and the timing of the survey could have influenced the results obtained. Therefore, further surveys are recommended to examine the universal reliability and validity of the checklist.
5 Conclusion
This study focused on the development of the High School Mental Health Action Checklist. This 15-item tool assists in screening coping mechanisms used to address students’ mental health challenges. Our findings showed that the tool had good validity and reliability. Students independently responded to the questionnaire, and the insights derived from their responses offered invaluable information for educators. Schools can therefore use these findings as a foundation or guideline for devising initiatives to promote students’ mental well-being. Regular and frequent use of the checklist to screen students’ mental health and plan interventions will allow schools to ensure that timely and effective interventions are offered. Encouraging a dynamic exchange of knowledge between teachers and students is crucial for enhancing the mental health of high school students.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethical Review Committee for Human Research, Faculty of Public Health, Mahidol University, Thailand. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SP: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation. SA: Writing – review & editing, Supervision, Funding acquisition, Conceptualization. CTh: Writing – review & editing, Supervision, Project administration, Methodology, Investigation. GB: Resources, Writing – review & editing, Methodology. CTa: Writing – review & editing, Validation, Methodology. SM: Validation, Writing – review & editing, Methodology. NC: Investigation, Writing – review & editing, Methodology. DY: Resources, Methodology, Writing – review & editing, Supervision. TI: Writing – review & editing, Validation, Supervision, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the National Health Security Fund, Region 13, project to promote mental health of school students in Bangkok. This study was partially supported by JSPS KAKENHI (Grant Number 22K17379).
Acknowledgments
We would like to acknowledge the cooperation of the school staff.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Orben, A, Tomova, L, and Blakemore, SJ. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc Health. (2020) 4:634–40. doi: 10.1016/s2352-4642(20)30186-3
2. Mukherjee, M. Challenges of mental wellbeing of digital native adolescent: promotion of mental health. BL College J. (2020) 2:28–46.
3. Guthold, R, Carvajal-Velez, L, Adebayo, E, Azzopardi, P, Baltag, V, Dastgiri, S, et al. The importance of mental health measurement to improve global adolescent health. J Adolesc Health. (2023) 72:S3–s6. doi: 10.1016/j.jadohealth.2021.03.030
4. Collin, C, Benson, N, Ginsburg, J, Grand, V, Layzan, M, and Weeks, M. The psychology book. London, UK: Dorling Kindersley Ltd (2012).
5. Eriksson, C, Arnarsson, ÁM, Damsgaard, MT, Löfstedt, P, Potrebny, T, Suominen, S, et al. Towards enhancing research on adolescent positive mental health. Nordic Welfare Res. (2019) 4:113–28. doi: 10.18261/issn.2464-4161-2019-02-08
6. Guo, C, Tomson, G, Keller, C, and Söderqvist, F. Prevalence and correlates of positive mental health in Chinese adolescents. BMC Public Health. (2018) 18:263. doi: 10.1186/s12889-018-5133-2
7. Sae-Koew, J In: A Lewis and S Yau, editors. Prevention in adolescent mental health: The development and evaluation of school-based interventions in disadvantaged communities. Perth, Australia: Murdoch University (2021)
8. Wong, MD, Dosanjh, KK, Jackson, NJ, Rünger, D, and Dudovitz, RN. The longitudinal relationship of school climate with adolescent social and emotional health. BMC Public Health. (2021) 21:207. doi: 10.1186/s12889-021-10245-6
9. Sellers, R, Warne, N, Pickles, A, Maughan, B, Thapar, A, and Collishaw, S. Cross-cohort change in adolescent outcomes for children with mental health problems. J Child Psychol Psychiatry. (2019) 60:813–21. doi: 10.1111/jcpp.13029
10. Siriratrekha, T. Mental health screening of school-age children. Bangkok, Thailand: Department of Mental Health, Ministry of Public Health, Thailand (2017).
11. Connors, EH, Moffa, K, Carter, T, Crocker, J, Bohnenkamp, JH, Lever, NA, et al. Advancing mental health screening in schools: innovative, field-tested practices and observed trends during a 15-month learning collaborative. Psychol Sch. (2022) 59:1135–57. doi: 10.1002/pits.22670
12. Boonsathirakul, J, and Boonsupa, C. Crisis and stress coping of senior high school students. Srinakharinwirot Acad J Educ. (2023) 17:268–80. doi: 10.14456/chulamedbull.2019.531
13. International Ergonomics Association. Ergonomic checkpoints: Practical and easy-to-implement solutions for improving safety, health and working conditions. Geneva, Switzerland: International Labour Organization (1996).
14. International Labour Office. Stress prevention at work checkpoints: Practical improvements for stress prevention in the workplace. Geneva, Switzerland: International Labour Organization (2012).
15. International Labour Organization. COVID-19 action checklist for the construction industry. Geneva, Switzerland: International Labour Organization (2020).
16. Khai, T, Kawakami, T, and Kogi, K. Participatory action-oriented training. ILO DWT for east and South-East Asia and the pacific. Hanoi, Vietnam. Hanoi, Vietnam: International Labour Organization (2011).
17. International Labour Office. Prevention and mitigation of COVID-19 at work action checklist. Geneva, Switzerland: International Labour Organization (2020).
18. Kogi, K, Sano, Y, Yoshikawa, T, and Yoshikawa, E. Extending participatory ergonomics to work stress prevention adapted to local situations. Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018). (2019):373–381.
19. Kogi, K, Sano, Y, Yoshikawa, T, and Yoshikawa, S. The design and use of ergonomic checkpoints for health care work. Proceedings of the 20th Congress of the International Ergonomics Association (IEA 2018). (2019):520–527.
20. Office of the Education Council, Ministry of Education, Thailand. Government education policy. (2021). Available at: https://www.onec.go.th/index.php/page/category/CAT0000019.
21. Office of the Permanent Secretary, Ministry of Education, Thailand. Educational statistics for the year 2021. (2022). Available at: https://edustatistics.moe.go.th/.
22. Thanachoksawang, C, Arphorn, S, Maruo, SJ, Punneng, S, Ishimaru, T, and Bangkadanara, G. Psychological distress among high school students in Bangkok Thailand. Health Psychol Res. (2024) 12:12. doi: 10.52965/001c.120045
23. Dray, J. Child and adolescent mental health and resilience-Focussed interventions: a conceptual analysis to inform future research. Int J Environ Res Public Health. (2021) 18:7315. doi: 10.3390/ijerph18147315
24. Magson, NR, Freeman, JYA, Rapee, RM, Richardson, CE, Oar, EL, and Fardouly, J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. (2021) 50:44–57. doi: 10.1007/s10964-020-01332-9
25. Tan, F, and Kawakami, T. The ASEAN occupational safety and health network good occupational safety and health practices 2008/2009. Vientiane, Laos: ASEAN Occupational Safety and Health Network (2009).
26. Singh, S, Roy, D, Sinha, K, Parveen, S, Sharma, G, and Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. (2020) 293:113429. doi: 10.1016/j.psychres.2020.113429
27. Heizomi, H, Kouzekanani, K, Asghari Jafarabadi, M, and Allahverdipour, H. Psychometric properties of the Persian version of mental health literacy scale. Int J Women's Health. (2020) 12:513–20. doi: 10.2147/ijwh.s252348
28. Yıldırım, M, Akgül, Ö, and Geçer, E. The effect of COVID-19 anxiety on general health: the role of COVID-19 coping. Int J Ment Heal Addict. (2022) 20:1110–21. doi: 10.1007/s11469-020-00429-3
29. Pan, KY, Kok, AAL, Eikelenboom, M, Horsfall, M, Jörg, F, Luteijn, RA, et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. (2021) 8:121–9. doi: 10.1016/s2215-0366(20)30491-0
Keywords: action checklist, coping, high school students, mental health, new normal
Citation: Punneng S, Arphorn S, Thanachoksawang C, Bangkadanara G, Tangtong C, Maruo SJ, Chantra N, Yogyorn D and Ishimaru T (2024) Developing a High School Mental Health Action Checklist in Thailand: insights on perception and communication. Front. Public Health. 12:1437957. doi: 10.3389/fpubh.2024.1437957
Edited by:
Padmavati Ramachandran, Schizophrenia Research Foundation, IndiaReviewed by:
Mark Vicars, Victoria University, AustraliaRhiannon Packer, Cardiff Metropolitan University, United Kingdom
Copyright © 2024 Punneng, Arphorn, Thanachoksawang, Bangkadanara, Tangtong, Maruo, Chantra, Yogyorn and Ishimaru. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara Arphorn, c2FyYS5hcnBAbWFoaWRvbC5hYy50aA==
 Suwatsa Punneng1,2
Suwatsa Punneng1,2 Chatchai Thanachoksawang
Chatchai Thanachoksawang Goontalee Bangkadanara
Goontalee Bangkadanara Niranyakarn Chantra
Niranyakarn Chantra Tomohiro Ishimaru
Tomohiro Ishimaru