- 1Faculty of Medicine, Institute of Pharmacology, Clinical Pharmacology and Toxicology, University of Belgrade, Belgrade, Serbia
- 2Faculty of Medicine, Institute of Medical Statistics and Informatics, University of Belgrade, Belgrade, Serbia
- 3Faculty of Medicine, Institute of Social Medicine, University of Belgrade, Belgrade, Serbia
- 4Faculty of Medicine, Laboratory for Strengthening the Capacity and Performance of Health Systems and Health Workforce for Health Equity, University of Belgrade, Belgrade, Serbia
Introduction: Monitoring the pharmacotherapy adherence in society is crucial for identifying occurance and causes of potential inadequate use of drugs and inform providers about the need for better customer counceling. It is necessary component of the strategic planning of the quality of healthcare services. This population- based study aimed to assess the medication intake adherence in the Republic of Serbia and the individual factors and health system variables influencing its pattern.
Methods: We applied a cross-sectional approach to study medication intake adherence using a secondary analysis of the latest 2019 Serbian National Health Survey data. The statistical modeling of the pharmacotherapy adherence incorporated sociodemographic data, self-reported disease, and lifestyle behavior.
Results: In 2019, in the representative sample of 12,066 adults in Serbia, requiring prescribed medicine, 49.8% did comply with the prescribed drugs, and 50.2% do not. Participants who adhered to prescribed medication were significantly (p < 0.001) older (62.4 ± 14 years), predominantly female (55.3%), had secondary education (48.5%), resided in southern and eastern parts of Serbia (55.5%), and belonged to the lowest income quintile (21.4%). The participants most often take prescribed drugs for hypertension (64.1%) and lower back pain (30.5%), while around 20% take medication for coronary disease, diabetes mellitus, and high blood cholesterol. About 85–92% of participants with financial or general difficulties using prescribed medication.
Conclusion: There is poor medication intake adherence to prescribed medication in Serbia. Gender, age, and region determine the adherence. Also, health-related and healthcare system-related factors impact the use of prescribed medication. Study findings can inform planning the counceling interventions in the target groups where improving medication adherence is necessary, as well as to enhance training of healthcare providers about pharmacotherapy adherence.
Introduction
Pharmacotherapy adherence refers to the extent to which a patient’s behavior in taking medication aligns with a doctor’s advice regarding timing, dosage, and frequency of use (1, 2). According to the International Society for Pharmacoeconomics and Outcome Research (ISPOR) Medication Compliance and Persistence Working Group, adherence is a synonym for compliance (2). Full adherence is when a patient follows a doctor’s instructions completely. Although opinions vary, non-adherence is generally defined as taking medications less than 80% of the time (3, 4). Consequently, the incidence of suboptimal adherence may vary based on different definitions. In our study, the prevalence with 95% CI of medication intake adherence was studied not among the patients but at the population level.
Healthcare providers may have difficulties in routine control of adherence with prescribed therapy due to various reasons including of patients’ absenteism on sheduled follow-ups, loss of memory among older adult, multimorbidity induced polypharmacy, etc. Non-adherence to the medication can be intentional or unintentional. In unintentional non-adherence, patients typically forget to take their medication, or were unaware of its relevance. With regard to adherence of prescribed generic drugs, which are often less expensive then branded drugs, many authors found out that among demographic, social, psychological and clinical factors a lower income of patients is significant for optimal adherence, regardless of their gender or age (5). There are many reasons for intentional non-adherence, including experiencing or anticipating side effects, disagreement with the pharmacological treatment, and an inability to pay for the medications (6). According to data from the World Health Organization, about 50% of patients with chronic diseases do not consistently follow the treatment recommendations of pharmacists and doctors, resulting in a lack of the expected response to proven effective medications (7). It is estimated that up to 30% of prescribed drugs never reach the pharmacist for dispensation (3). As a result of insufficient patient adherence, treatment success is questioned, leading to unwanted quality of life and clinical outcomes, unnecessary healthcare utilization and treatment costs, which ultimately may additionally strain the healthcare budget (8–10). It has been estimated that in the US, of all medication-related hospital admissions, about 33–70% result from poor adherence, which represents an annual cost of US$ 100 billion (11).
Adherence can be measured by subjective (patient self-reports, family interviews, and questionnaires) and objective methods (prescription refill rates, residual pill counting, and electronic measurement devices), and there is no specific measure of medication adherence. In our study focus was on self-reports of pharmacotherapy adherence, which allowed us also exploring the respondents’ awareness and reasons of the applied adherence patterns.
Many studies explore medication adherence for specific disease (12–14), factors (15), or drugs (16), and most of these investigations are within specific healthcare institutions or regions (13, 15). In Serbia, patients with Parkinson’s disease and depression compared to Parkinson’s disease patients without depression have a three times higher risk for lower adherence to pharmacotherapy (12). A recently published study conducted in one of the larger cities in Serbia showed that adherence to hypertension medications is poor and that non-adherence is more common when taking more medications and a more complicated dosing regimen, and among residents of the urban settlements (13). Additionally, in Serbia, one study has investigated self-medication (the use of medicine without a doctor’s prescription) at the population level (17). The prevalence of self-medication was 27.1%, and was associated with sociodemographic and health-related factors, as well as unmet healthcare needs (17). To the best of our knowledge, no studies have assessed nationwide medication intake adherence to prescribed medication within the Serbian population.
This study aimed to assess the prevalence of medication intake adherence to prescribed medication among adults in Serbia and identify factors that might affect adherence. We focused on examining the impact of social and demographic factors, disease-related factors, and barriers within the healthcare system.
Methods
Study design
This is a population-based, cross-sectional study. The study is a secondary analysis of the Serbian National Health Survey data conducted between October and December 2019 by the Institute of Statistics of the Republic of Serbia in cooperation with the Institute of Public Health of Serbia “Dr. Milan Jovanovic Batut” and the Ministry of Health of the Republic of Serbia.
The study followed the Declaration of Helsinki (1964 and 2013) and was approved by the Ethics Committee of Faculty of Medicine University of Belgrade, Belgrade, Serbia (permit number 1322/IX-9). To safeguard the privacy of survey participants and collected data, all procedures were in accordance with the General Data Protection Regulation and the National Personal Data Protection Act.
Sample
Subject sampling and the study protocol were implemented in accordance with the guidelines of the European Health Interview Survey-third wave (EHIS wave 3) (18). In brief, a two-stage stratified sample was used based on the type of settlement (urban or other) and geographical areas (four statistical regions: Vojvodina, Belgrade, Šumadija, and western Serbia, southern and eastern Serbia). The survey included a representative sample size of the population, based on Eurostat recommendations for conducting population health surveys. From 13,589 participants, based to the focus of this research and after adjust for age (18 years and older) and answers from the use of drugs prescribed by a doctor (yes/no) the total number of participants was 12,066.
Research instrument and variables and setting
For data collection, a face-to-face self-reported questionnaire was used. The questionnaire was standardized and based on Eurostat (19). Trained interviewers gave the participants a printed document with information about the survey.
The sociodemographic characteristics, health status (disease and chronic conditions), use of prescribed medicines by participants, and information regarding the healthcare system were extracted from the National Health Survey 2019 database. The following specific questions about regular use of the medication were used: ``During the past two weeks, have you used any drugs prescribed by your doctor?`` (yes or no), ``Do you have difficulty performing certain activities - taking medication?`` (yes or no) and ``In the past 12 months, have you needed prescribed medication but could not afford it due to financial reasons?`` (yes or no).
The variable ``During the past two weeks, have you used any drugs prescribed by your doctor?`` was dichotomized into a variable with two modalities, “no” and “yes,” where “yes” was the reference category and represented the dependent variable. That variable (medication intake adherence) is related to the use of drugs prescribed by a doctor (relevant to study the adherence, as proposed by EHIS wave 3 Methodological Manual instructions) served as the basis for creating the database in this study. The analysis included pharmaceutical drugs, while vitamins, minerals, herbal medicines, and herbal teas (unless classified as medicines) were excluded. The analysis included the following independent variables: (1) sociodemographic (age years as continuous variable 18+), gender (male/female), level of education (no formal education/primary school/secondary school/ undergraduate studies/postgraduate studies), socioeconomic status (income quintile, five categories from lowest to highest); (2) health-related including the presence of a chronic disease from a list of most common diseases in the population (yes/no). The following question was used:``Have you had any of the above diseases or conditions in the past 12 months?`` with answers yes or no; (3) healthcare system-related, such as unmet healthcare needs (medication intake) in the past 12 months due to either inability to afford prescribed medication for financial reasons, or difficulty in taking medication. The following questions were used: ``In the past 12 months, have you needed prescribed medication but could not afford it due to financial reasons?`` with answers yes or no and ``Do you have difficulty performing certain activities - taking medication?`` with answers yes or no.
The outcome of interest was medication intake adherence to prescribed medication. In most studies, adherence is defined as taking 80% or more of the prescribed medication doses (3, 4). However, depending on the outcome, that threshold of 80% can be different and cannot be confirmed or rejected (20). It is estimated that adherence to chronic medications is around 50%. Based on the literature data, adherence to medication is considered low or suboptimal if greater than 20–50% of participants are non-adherent to prescribed medications (12, 21–25).
Statistical analysis
The data are presented with descriptive statistics as n (%), arithmetic mean ± standard deviation or median (min-max), depending on the type of variables and the normality of the distribution. The t- and chi-square tests were used to test statistical hypotheses. Logistic regression was used to model the relationship between the dependent variable (medication intake adherence with prescribed pharmacotherapy) and potential predictors. Variables significantly associated with the prescribed drugs in the univariate analysis were included in the multivariate logistic regression models. Statistical significance in all analyses was considered if the computed probability value was ≤0.05. The results are presented in tabular and graphic form. All data were processed in the IBM SPSS Statistics 24 (SPSS Inc., Chicago, IL, United States) software package or the R programming environment.
Results
Adherence with prescribed pharmacotherapy
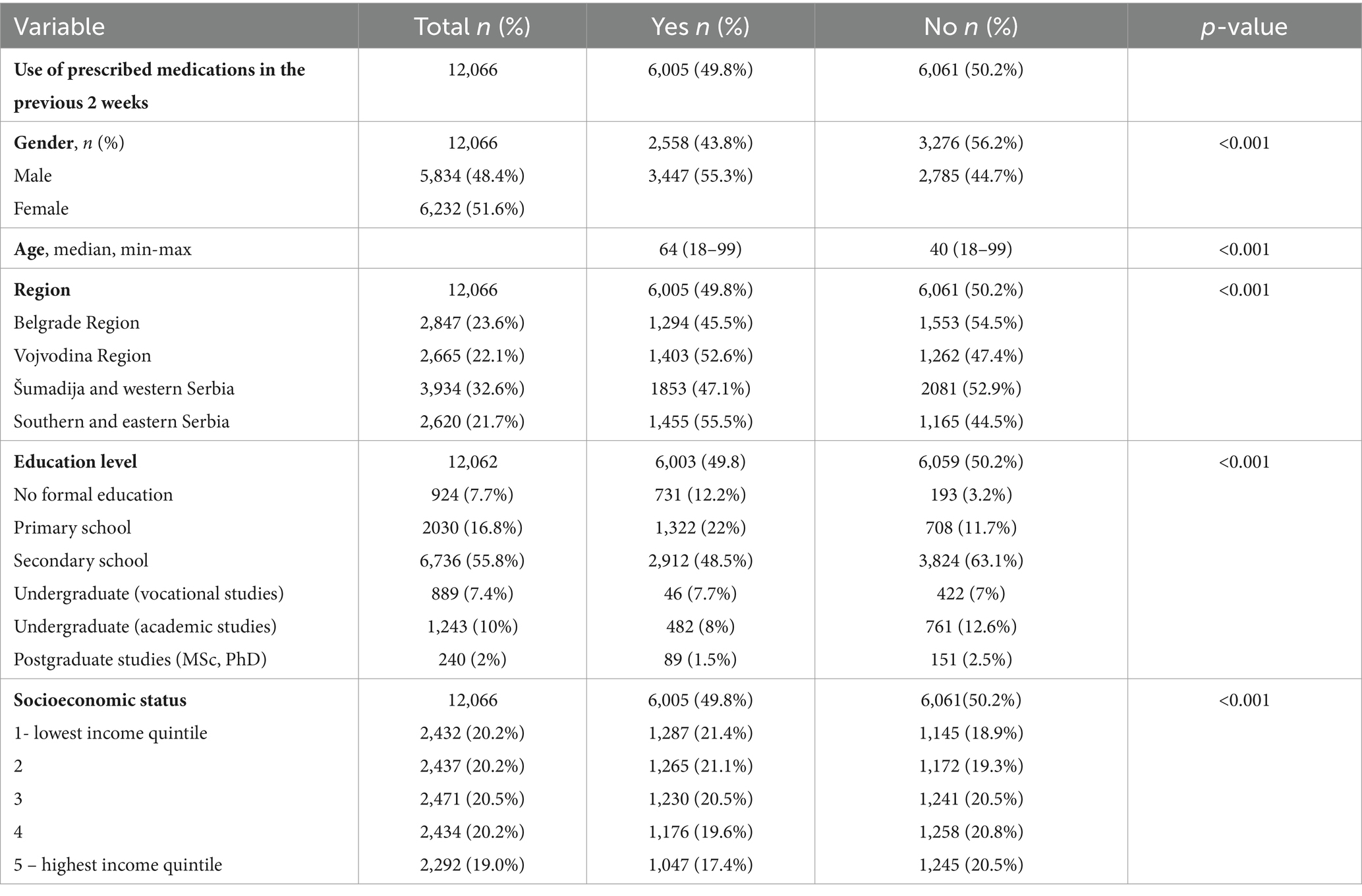
The final total sample included 12,066 adult participants requiring medicine 2 weeks before survey. The prevalence of prescribed medicine use is 49.8% (95% CI 48.9–50.1). Participants who used and did not use prescribed medications in the previous 2 weeks were almost equally distributed in the study sample, 6,005 (49.8%), and 6,061 (50.2%), respectively (Table 1).
Adherence and association with sociodemographic characteristics
Participants who adhered, take prescribed medication in the last 2 weeks, were statistically significant (p < 0.001), predominantly female (55.3%), had secondary education (48.5%), resided in southern and eastern Serbia (55.5%), and belonged to the lowest income quintile (21.4%). Older participants (average age 62.4 ± 14) used prescribed drugs more often than younger participants (average age 41.8 ± 15.5). Participants who not take the prescribed medication were predominantly men, participants with secondary school and higher income quintile, resided in Belgrade region. Detailed sociodemographic characteristics of the study sample are shown in Table 1.
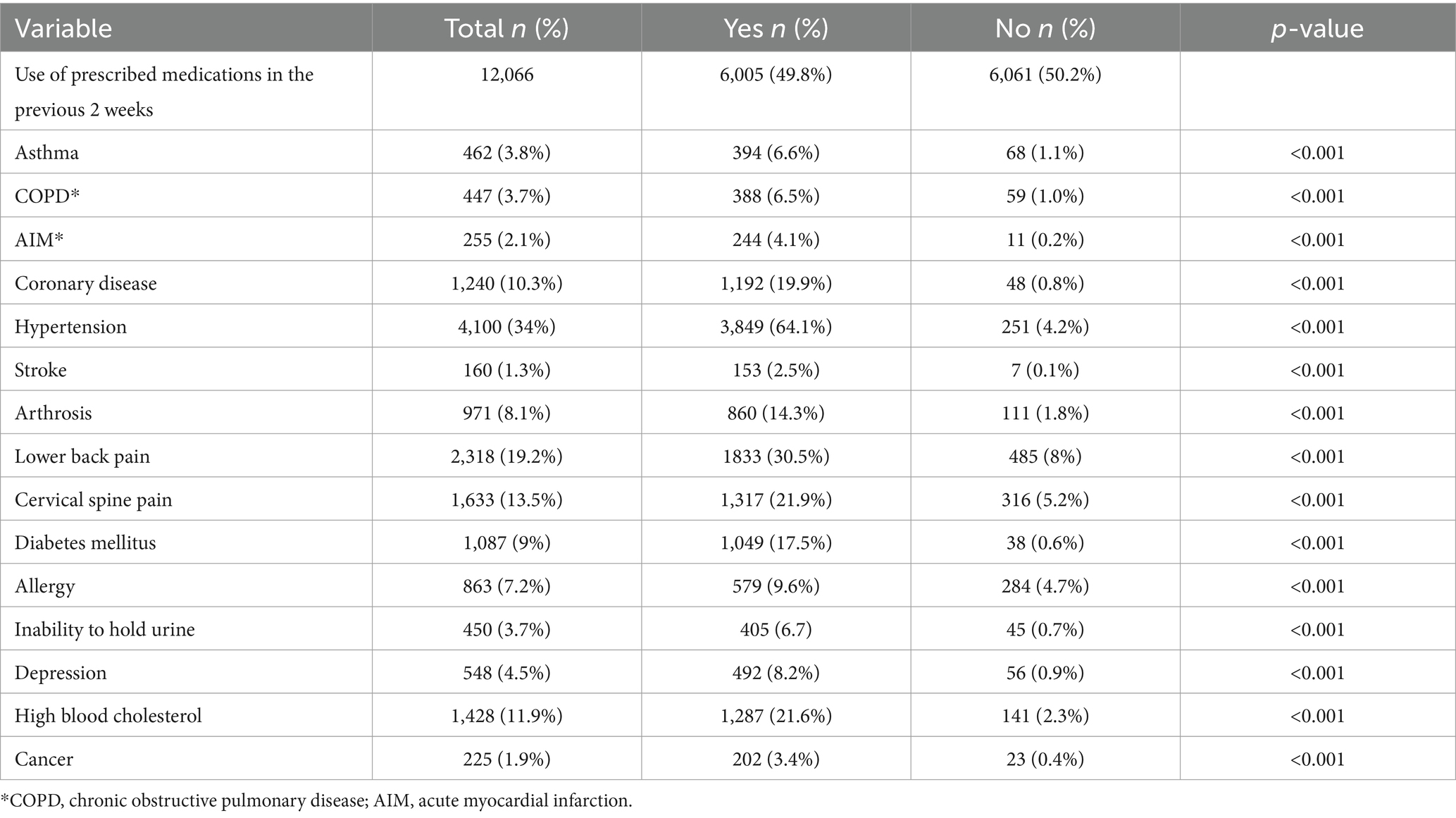
Use of prescribed medications associated with disease
The use of prescribed medicines for certain diseases is significantly (p < 0.001) higher than non-use. Participants who reported taking prescribed medicines significantly (p < 0.001) suffered from hypertension (64.1%) and lower back pain (30.5%), while about 20% of the respondents had coronary disease, cervical spine pain, diabetes mellitus and high blood cholesterol (Table 2). Our results indicated that there are probably respondents with more than one specific disease, since that the total number of respondents who have specific disease (16.187) is higher than total number of participants (12.066) (Table 2).
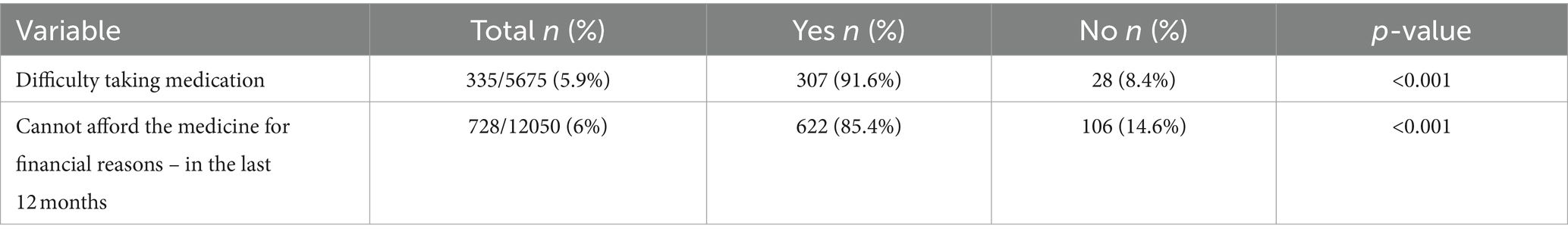
Adherence with prescribed pharmacotherapy associated with the healthcare system
Analysis showed that prescribed medication use was significantly (p < 0.001) associated with unmet healthcare needs in the past 12 months (Table 3). There is a statistically significant (p < 0.001) difference in the frequency of respondents who have financial difficulties in obtaining medication (728/12050) in relation to whether or not the respondents take prescribed medicine (Table 3). However, the respondents with financial difficult to afford medications still in a high extent (85%) intake prescribed medications. The respondents with financial difficulties were more prevalent in the Belgrade region, as well as eastern and southern Serbia. There is a statistically significant difference (p < 0.001) in the frequency of difficulty taking medication in relation to whether or not the respondents are taking the prescribed medication. About 91% of respondents who used medication typically had difficulty (minor, major difficulties or total incapacity) in taking prescribed medication (Table 3). Difficulties in performing daily activities, particularly in adhering to therapy (medicines), are significantly (p < 0.001) higher in older people (78 ± 8–9 years old), women compared to men (62% vs. 37.7%), and in the regions of Šumadija, western, southern, and eastern Serbia.
Predictors of adherence with prescribed pharmacotherapy
In a multivariate logistic regression model, medication intake adherence with prescribed pharmacotherapy was the dependent variable, while social and demographic independent variables were included as adjusted for the existence of a disease or condition in the last 12 months. There was no significant multicollinearity between the social and demographic variables.
In the multivariate logistic regression model, statistically significant potential predictors of medication intake adherence with prescribed pharmacotherapy were female gender (B = 0.460; p < 0.001), older age (B = 0.060; p < 0.001), and the region [Belgrade (B = -0.344; p < 0.001)], with southern and eastern Serbia as a reference category (Figure 1).
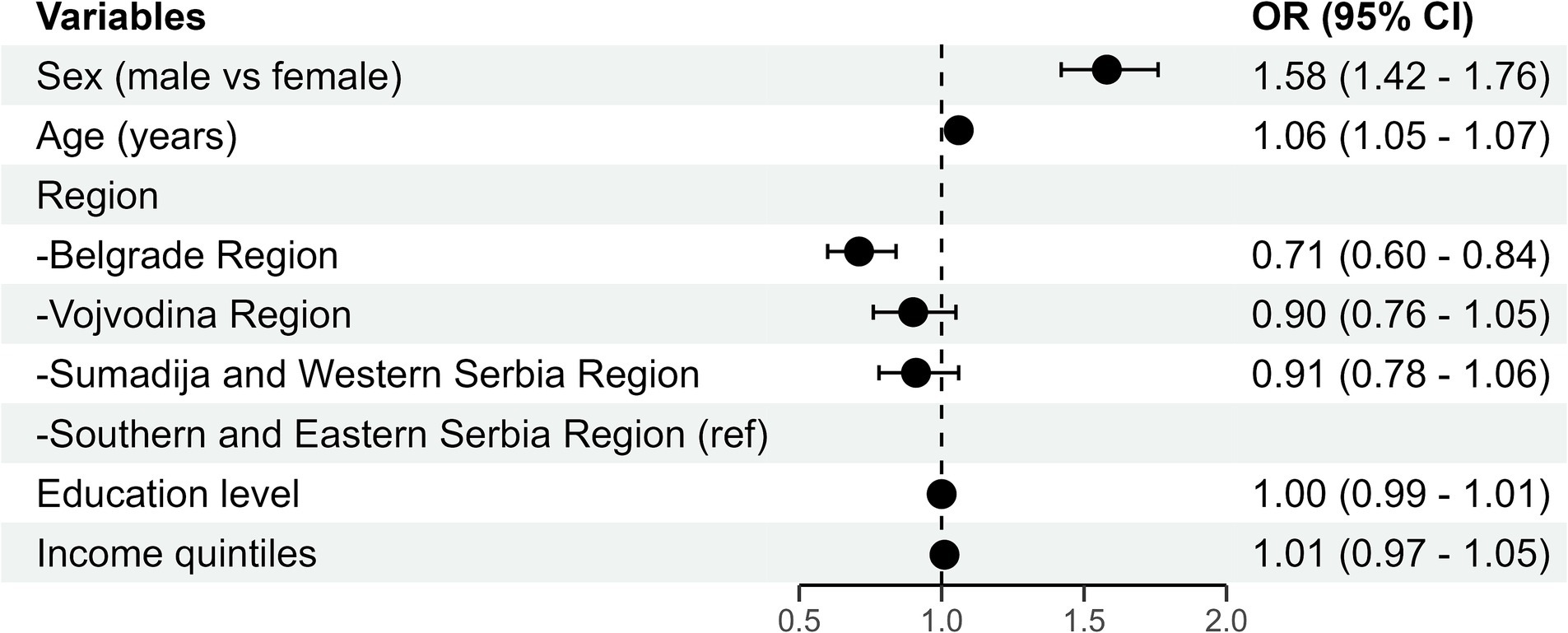
Figure 1. Forest plots with odds ratios (ORs) and associated confidence intervals (CIs) (95%) of the statistically significant results of multivariate analysis.
Discussion
This was the first study to investigate the characteristics and predictors of prescribed medication usage at the national level in Serbia, allowing to understand the frequency and reasons for non- adherence with prescribed pharmacotherapy. The prevalence of prescribed medicine use is 49.8% (95% CI 48.9–50.1). The study revealed a significantly high frequency (about 50%) of non-use of prescribed medicines in the population and poor adherence. Significant associations between the sociodemographic factors and prescribed medication use among adults in Serbia were observed, as well as the impact of health- and healthcare system-related factors and prescribed medication use. Based on these findings, gender, age, and region are factors determining the use of prescribed medication in Serbia. Among the adult population, female gender, older age, and residence in the regions of southern and eastern Serbia are significantly associated with higher use of prescribed medicines. Also, individuals with secondary school education and belonging to the lowest income quintile were not associated with medication intake adherence to the prescribed medication. In Serbia, the population primarily takes prescribed drugs to treat conditions such as hypertension, lower back pain, coronary disease, cervical spine pain, diabetes mellitus, and high blood cholesterol. Our results indicate that the population have unmet healthcare needs due to financial constraints or difficulties in adhering to medication therapy which significantly affect the use of medicines, but on the other hand people have high prevalence (85–92%) of medication intake adherence to prescribed medications.
Between the two national surveys, a slight increase in the frequency of prescribed drug use in the population was observed. In 2013, about 44% of the population reported using medicines prescribed by a doctor within the 2 weeks before the survey (26); results of this study show that this frequency was 49% in 2019. However, our results indicate that around 50% of the participants did not use prescribed medicines, which points a high prevalence of nonintake of medication and to poor adherence. Since 98% of the population has obligatory social health insurance, in the Serbian predominant Bismarck social model (income-based and financed jointly by employers) of health system, a burden of costs for prescribed pharmacotherapy is shared between the Health Insurance Fund (27) and out-of-pocket copayment. In 2013, female gender, middle age, and chronic disease were sociodemographic factors associated with self-medication in Serbia (17). Similarly, in our study conducted in 2019, these same factors were found to be associated with the adherence with prescribed pharmacotherapy. As this is about the use of prescribed and non-prescribed drugs, it is possible that a certain degree of self-medication is also present in our respondents.
Our results are in the accordance with the results from population-based study in Germany (21). In Germany at least 33% of population does not use prescribed medication and nonadherence to medication occurs more often in younger populations with higher socioeconomic status than in older populations with chronic conditions (21). Results of the National Health Survey in Spain showed that about 92% of participants take some medication prescribed by a doctor, but unlike Serbia, they included only respondents aged 65+ which does not allow the comparisons (28). For instance, in our research, the age was important from two distinct perspectives. Middle aged individuals (about 40 years and older) were more prone to be non-adherent, and older individuals (about 78 years and above) had difficulties in medicine use. The majority of participants use prescribed medicines for specific diseases, a factor that positively influences treatment outcomes and health preservation Similar to our results, in Spain women take prescribed drugs significantly more often than men, and these drugs are mostly used for the treatment of hypertension, diabetes, and other chronic diseases (28). Our results agree with data obtained from the adult population in Austria, indicating that individuals from less educated and lower socioeconomic groups were more likely to use prescribed medicines (29). One of the most important predictor of nonadherence may be out-of-pocket costs for medication (30). Our results suggest that although participants have difficulties in taking and buying medications, there is still a high prevalence (85–92%) of the intake of prescribed medication and good adherence in relation to the general intake medication adherence. In some patients (both low-income and high-income, depression and asthma), it is possible that cost associated nonadherence with may be influenced by patient beliefs, about the perceived value of prescription medication (31). In general, it is difficult to directly compare our results to results of other studies due to methodological differences in sample selection, assessment of adherence, type of drugs and disease and differences between countries.
Study about medication intake adherence was performing in Albania in similar period. As in Serbia and in Albania, there is a high incidence of nonintake of prescribed medication (about 20%) in adult population (23). Factors associated with nonintake of medication in Albania included rural residence, low educational level and low economic level, while in Serbia were residence in capital region, lower educational and higher economic level. In both countries, financial difficulties have a significant impact on the use of prescribed medication, however, in Serbia the frequency of medication intake is still high (85%) compared to Albania (9%). As Albania is a country in transition in Southeast Europe, just like Serbia, the results are interesting to compare because both studies included intake medication adherence and associated factors. However, the results cannot be fully compared, given that the study was in Albania included primary users health care, not general population.
The descriptive data on the extent of medication intake (non-)adherence in the Serbian population are highly informative. The present real-world analysis included 12,066 adults (18+ years) who need prescribed medicine and was not limited by selection bias. The study findings can inform stakeholders efforts toward improving medication adherence in the population and enhancing implementation of national healthcare programs in specific population groups. Moreover, a recommendation is to add more specific questions for polipharmacy into the questionnaire for the next National Health Survey. Pharmacoepidemiologic data from the Health Surveys may be limited due to self-reporting if understanding of the adherence with prescribed pharmacotherapy differs among respondents. The suboptimal level of pharmacotherapy adherences indicates a necessity for rising awareness and counseling of its relevance among people as well as its control among pharmacotherapy prescribers.
This study has some limitations. For monitoring the medication adherence we used subjective method - patient interview and self-report assessments. This is simple to use and less expensive method for measure of medication adherence, but respondents may be biased and give expected answers. However, this is a one of the most common tool for measure of medication adherence, especially useful for nationwide study. As the study was conducted in the population and as a part of a national investigation, the results are useful in the future investigations of medication adherence and in acting on critical factors for a patient’s non-adherence and in developing policy to improve adherence in improving treatment outcomes and reducing overall health costs. Next, this survey include medication intake adherence but not determine adherence using another tools. It would be more appropriate, if the survey determine taking medication with more questions and only for specific disease and determine which number taking medication for more than one disease etc. Furthermore, in this study we controlled only the use of prescribed drugs, while the use of drugs on its own was not included. Also, self-medication in these patients can affect the adherence in prescribed pharmacotherapy. In addition language barriers in some regions (e.g., Vojvodina) should be assessed.
Conclusion
This study gives evidence about the extent and sociodemographic determinants of medication intake adherence among adult population in a transitional South Eastern European region. Our research shows that lower adherence to prescribed medicines is common in the adult population in Serbia. Gender, age and geographic region are the main social and demographic predictors for prescription medicine use. In Serbia, the population most often takes prescribed drugs for the treatment of chronic disease such as hypertension, coronary disease, diabetes mellitus and high blood cholesterol. Although population has difficulties in taking and buying medicines, there is still a high prevalence of the use of prescribed medicines and good adherence in relation to the general intake medication adherence. The priority population groups for improving adherence with prescribed pharmacotherapy includes men, young adults, individuals with higher levels of education and income, and the population residing in the Belgrade region. Study findings can inform for planning health politics because there are determinants that can be influenced by improving health regulations and training health service providers on the necessity of monitoring and advising patients on pharmacotherapy adherence. Decision-makers and policy-makers in Serbia should consider these findings because the costs of noncompliance may be higher.
Data availability statement
The data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the [patients/ participants OR patients/participants legal guardian/next of kin] was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
DS: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing. ZB: Software, Visualization, Writing – review & editing. MŠM: Data curation, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The study is a part of the 2019 National Health Survey for the population of Serbia (excluding Kosovo) that was carried out by the Ministry of Health of the Republic of Serbia and professional support of the Institute of Public Health of Serbia “Dr Milan Jovanovic Batut.” The authors were supported by the Ministry of Science, Technological Development and Innovation of the Republic of Serbia (contract 451-03-66/2024-03/200110).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor AB declared a shared affiliation with the authors at the time of review.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO . Adherence to long-term therapies: evidence for action. WHO. World Health Organization. Available at: https://apps.who.int/iris/handle/10665/42682
2. Cramer, JA, Roy, A, Burrell, A, Fairchild, CJ, Fuldeore, MJ, Ollendorf, DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. (2008) 11:44–7. doi: 10.1111/j.1524-4733.2007.00213.x
3. Nieuwlaat, R, Wilczynski, N, Navarro, T, Hobson, N, Jeffery, R, Keepanasseril, A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. (2014) 2014:CD000011. doi: 10.1002/14651858.CD000011.pub4
4. Tilea, I, Petra, D, Voidazan, S, Ardeleanu, E, and Varga, A. Treatment adherence among adult hypertensive patients: a cross-sectional retrospective study in primary care in Romania. Patient Prefer Adherence. (2018) 12:625–35. doi: 10.2147/PPA.S162965
5. Mishuk, AU, Qian, J, Howard, JN, Harris, I, Frank, G, Kiptanui, Z, et al. The association between patient sociodemographic characteristics and generic drug use: a systematic review and Meta-analysis. J Manag Care Spec Pharm. (2018) 24:252–64. doi: 10.18553/jmcp.2018.24.3.252
6. Garcia Popa-Lisseanu, MG, Greisinger, A, Richardson, M, O’Malley, KJ, Janssen, NM, Marcus, DM, et al. Determinants of treatment adherence in ethnically diverse, economically disadvantaged patients with rheumatic disease. J Rheumatol. (2005) 32:913–9.
7. Sabate, E . Adherence to long-term therapies: Evidence for action. Geneva: World Health Organization (2003).
8. Ágh, T, Dömötör, P, Bártfai, Z, Inotai, A, Fujsz, E, and Mészáros, Á. Relationship between medication adherence and health-related quality of life in subjects with COPD: a systematic review. Respir Care. (2015) 60:297–303. doi: 10.4187/respcare.03123
9. Eakin, MN, Bilderback, A, Boyle, MP, Mogayzel, PJ, and Riekert, KA. Longitudinal association between medication adherence and lung health in people with cystic fibrosis. J Cyst Fibros. (2011) 10:258–64. doi: 10.1016/j.jcf.2011.03.005
10. Milgrom, H, Bender, B, Ackerson, L, Bowry, P, Smith, B, and Rand, C. Noncompliance and treatment failure in children with asthma. J Allergy Clin Immunol. (1996) 98:1051–7. doi: 10.1016/s0091-6749(96)80190-4
11. Berg, JS, Dischler, J, Wagner, DJ, Raia, JJ, and Palmer-Shevlin, N. Medication compliance: a healthcare problem. Ann Pharmacother. (1993) 27:S5–S19. doi: 10.1177/10600280930270S902
12. Radojević, B, Dragašević-Mišković, NT, Milovanović, A, Svetel, M, Petrović, I, Pešić, M, et al. Adherence to medication among Parkinson’s disease patients using the adherence to refills and medications scale. Int J Clin Pract. (2022) 2022:6741280–7. doi: 10.1155/2022/6741280
13. Nikolic, A, Djuric, S, Biocanin, V, Djordjevic, K, Ravic, M, Stojanovic, A, et al. Predictors of non-adherence to medications in hypertensive patients. Iran J Public Health. (2023) 52:1181–9. doi: 10.18502/ijph.v52i6.12960
14. Emamikia, S, Gomez, A, Ådahl, T, von Perner, G, Enman, Y, Chatzidionysiou, K, et al. Factors associated with non-adherence to medications in systemic lupus erythematosus: results from a Swedish survey. Lupus. (2024) 33:615–28. doi: 10.1177/09612033241242692
15. Krajnović, D, Ubavić, S, and Bogavac-Stanojević, N. Pharmacotherapy literacy of parents in the rural and urban areas of Serbia-are there any differences? Medicina (Kaunas). (2019) 55:590. doi: 10.3390/medicina55090590
16. Masi, S, Kobalava, Z, Veronesi, C, Giacomini, E, Degli Esposti, L, and Tsioufis, K. A retrospective observational real-word analysis of the adherence, healthcare resource consumption and costs in patients treated with Bisoprolol/perindopril as single-pill or free combination. Adv Ther. (2024) 41:182–97. doi: 10.1007/s12325-023-02707-7
17. Tripković, K, Nešković, A, Janković, J, and Odalović, M. Predictors of self-medication in Serbian adult population: cross-sectional study. Int J Clin Pharm. (2018) 40:627–34. doi: 10.1007/s11096-018-0624-x
18. Insitute of Public Health of Serbia . Results of the national health survey of the republic of Serbia 2019. Belgrade: Insitute of Public Health of Serbia, Omnia Bgd (2021).
19. Eurostat . European health interview survey (EHIS wave 3)—methodological manual. Eur Secur. (2018).
20. Baumgartner, PC, Haynes, RB, Hersberger, KE, and Arnet, I. A systematic review of medication adherence thresholds dependent of clinical outcomes. Front Pharmacol. (2018) 9:1290. doi: 10.3389/fphar.2018.01290
21. Glombiewski, JA, Nestoriuc, Y, Rief, W, Glaesmer, H, and Braehler, E. Medication adherence in the general population. PLoS One. (2012) 7:e50537. doi: 10.1371/journal.pone.0050537
22. Menditto, E, Cahir, C, Aza-Pascual-Salcedo, M, Bruzzese, D, Poblador-Plou, B, Malo, S, et al. Adherence to chronic medication in older populations: application of a common protocol among three European cohorts. Patient Prefer Adherence. (2018) 12:1975–87. doi: 10.2147/PPA.S164819
23. Roshi, D, Burazeri, G, Italia, S, Schröder-Bäck, P, Ylli, A, and Brand, H. Prevalence and sociodemographic correlates of medication intake adherence among primary health-care users in Albania. East Mediterr Health J. (2021) 27:516–23. doi: 10.26719/emhj.21.008
24. Ge, L, Heng, BH, and Yap, CW. Understanding reasons and determinants of medication non-adherence in community-dwelling adults: a cross-sectional study comparing young and older age groups. BMC Health Serv Res. (2023) 23:905. doi: 10.1186/s12913-023-09904-8
25. Menditto, E, Guerriero, F, Orlando, V, Crola, C, Di Somma, C, Illario, M, et al. Self-assessment of adherence to medication: a case study in Campania region community-dwelling population. J Aging Res. (2015) 2015:682503:1–6. doi: 10.1155/2015/682503
26. “Research on the health of the population of Serbia, 2013” Institute for Public Health of the republic of Serbia “Dr. Milan Jovanović Batut”. Belgrade, Serbia: Sluzbeni glasnik (2014).
27. National Health Insurance Fund . Number of insured persons. (2014). Available at: http://www.rfzo.rs/index.php/broj-osiguranika-stat.
28. Gutiérrez-Valencia, M, Aldaz Herce, P, Lacalle-Fabo, E, Contreras Escámez, B, Cedeno-Veloz, B, and Martínez-Velilla, N. Prevalence of polypharmacy and associated factors in older adults in Spain: data from the National Health Survey 2017. Med Clin. (2019) 153:141–50. doi: 10.1016/j.medcli.2018.12.013
29. Mayer, S, and Österle, A. Socioeconomic determinants of prescribed and non-prescribed medicine consumption in Austria. Eur J Pub Health. (2015) 25:597–603. doi: 10.1093/eurpub/cku179
30. Frankenfield, DL, Wei, II, Anderson, KK, Howell, BL, Waldo, D, and Sekscenski, E. Prescription medication cost-related non-adherence among Medicare CAHPS respondents: disparity by Hispanic ethnicity. J Health Care Poor Underserved. (2010) 21:518–43. doi: 10.1353/hpu.0.0314
Keywords: compliance, adults, population study, chronic disease, pharmacotherapy, medication intake
Citation: Srebro D, Bukumirić Z and Šantrić Milićević M (2024) A real-world analysis of pharmacotherapy adherence and the factors influencing it in Serbia: a nationwide, population-based, cross-sectional study. Front. Public Health. 12:1437796. doi: 10.3389/fpubh.2024.1437796
Edited by:
Aleksandra Barac, University Clinical Center of Serbia, SerbiaReviewed by:
Svetlana Ranko Radevic, University of Kragujevac, SerbiaSasa Vukmirovic, University of Novi Sad, Serbia
Copyright © 2024 Srebro, Bukumirić and Šantrić Milićević. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dragana Srebro, c3JlYnJvZHJhZ2FuYTFAZ21haWwuY29t
 Dragana Srebro
Dragana Srebro Zoran Bukumirić2
Zoran Bukumirić2 Milena Šantrić Milićević
Milena Šantrić Milićević