- 1Emergency Department, The Affiliated Brain Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
- 2Nursing Department, The Affiliated Brain Hospital of Nanjing Medical University, Nanjing, Jiangsu, China
Background: Adolescents are vulnerable to mental disorders due to physiological, psychosocial, and cognitive changes during this critical developmental stage. Depression, in particular, can lead to high-risk behaviors such as self-injury (SI) and suicide. This study aims to estimate the pooled prevalence of SI behaviors among adolescents with depression.
Materials and methods: We systematically searched databases including EMBASE, Scopus, PubMed, and Web of Sciences for relevant articles published on adolescents with depression from January 1, 2000, to January 1, 2024. The quality assessment of the studies was conducted using the Joanna Briggs Institute (JBI) criteria. The global prevalence of SI was calculated based on a random effects model using Stata software version 17.
Results: Our analysis included 29 studies involving 12,934 adolescents. The lifetime prevalence of SI was 52% (95% Confidence Interval [CI]: 41–64), while the period prevalence was 57% (95% CI: 49–64). Notably, a significant relationship was observed between the prevalence of SI and the year of publication of articles (p = 0.002). Furthermore, publication bias was not significant for both lifetime prevalence (p = 0.281) and period prevalence (0.358).
Conclusion: The prevalence of self-injurious behaviors in adolescents with depression is alarmingly high, with more than half of adolescents having engaged in these high-risk behaviors during their lifetime or within the last year. Given the associated risk of suicide, it is crucial to identify individuals at risk and provide timely interventions.
Introduction
Self-injury (SI) or non-suicidal self-injury (NSSI) refers to the direct and intentional destruction of body tissues without suicidal intent (1). Common forms of SI include cutting, burning, scratching and hitting oneself (2). The concept of these behaviors was first discussed in the book “Man Against Himself,” where self-injury was described as a form of “partial suicide” by the author (3). Despite continuous research efforts, there is still no generally accepted definition for this behavior. Various terms, such as “syndrome of delicate self-cutting,” “deliberate self-harm,” “self-wounding,” and “moderate self-mutilation” have been proposed, which has made it difficult to understand these behaviors due to the diversity and lack of consensus (4–7).
Adolescence refers to the transitional stage between the ages of 10 and 19. Although this stage is typically considered problem-free, nearly 20% of young people experience a mental health problem (8). The prevalence of SI in the general population is 4% (9), while 15% of teenagers and young adults have had a history of SI (10). Additionally, 46% of ninth and tenth grade students have engaged in at least one SI behavior during the past year (11).
SI results from dysregulation of emotions, internalizing behaviors, and inability to cope effectively. The results of studies conducted on different populations show that people who harm themselves have higher levels of depression and anxiety (12–15). Individuals with depressive symptoms often use SI as a coping mechanism for negative emotions, providing temporary relief followed by subsequent feelings of sadness and guilt (16). If SI is performed repeatedly, it fails to alleviate depressive symptoms and instead exacerbates negative emotions over time, increasing the risk of depression (17).
SI is distinct from suicide, but they can be connected. Suicidal behavior involves any action with the intention of ending one’s own life. Self-injury behaviors do not aim to cause death but serve as coping mechanisms for emotional pain, stress, or trauma and occur more frequently than suicide attempts (18). The primary risk of SI is its potential to become chronic and progress into other types of self-injurious acts, such as suicide attempts (19). Despite the distinction between these behaviors and suicide attempts, which typically do not require immediate medical attention or result in death, such dangerous behaviors may serve as a precursor to suicidal behaviors in the future (20, 21). Experts argue that despite differences in intent, epidemiology, and lethality between SI and suicide, these two behaviors often co-occur (21–23).
Numerous studies have been undertaken to investigate the prevalence of SI among depressed individuals, yielding mixed results. Additionally, only a limited portion of these studies have focused on adolescents. This study aims to answer the question: what is the period prevalence (the proportion with the characteristic at any point during a specified time period) and lifetime prevalence (the proportion who have ever had the characteristic at some point in their lives) of self-injury among depressed adolescents? Thus, this study was conducted with the objective of estimating the period and lifetime prevalence of SI among depressed adolescents.
Materials and methods
This meta-analysis was conducted with the aim of estimating the pooled prevalence of SI among depressed adolescents on published articles from 2000 to 2024 based on the Preferred Reporting Items for Systematic Review and Meta-analyses PRISMA checklist (24).
Search strategy
In this review, Medline, Web of Science, Scopus, and EMBASE electronic databases were searched from January 2000 to January 2024 with the keywords “self-injurious behavior,” “self-mutilation,” “self-harm,” “depression,” “depressive disorder,” “adolescent,” and their combinations. Google Scholar and ResearchGate were searched to access other related studies. Searching and screening of articles were conducted from January to March 2024. Initially, abstracts and titles of retrieved articles were screened to determine eligibility. Irrelevant papers were removed, and the full text of the remaining articles was reviewed by two authors independently. The references of the articles were manually searched to access additional relevant studies.
Eligibility criteria
The inclusion criteria were: Publication in English between 2000 and 2024, observational studies involving depressed adolescents (people aged 10 to 19), and reporting necessary data such as frequency or prevalence of SI. Studies conducted on other age groups, reviews, qualitative articles, editorials, and intervention were excluded from the analysis.
Data extraction
Data were extracted by a member of the research team based on a pre-prepared form and then double-checked by a second reviewer. Any disagreements were resolved through discussion with a third author. The extracted information included the first author, year of publication, sample size, country, and frequency or prevalence of SI.
Risk of bias assessment
The quality of the selected articles was evaluated independently by two authors. The Joanna Briggs Institute (JBI) critical appraisal checklist for prevalence studies was used to evaluate bias in selected articles. The JBI appraisal checklist comprises nine items, with answers of yes (score 1) and no, unclear and not applicable (score zero). The overall score ranges from 0 to 9, where a higher score indicates higher quality (25).
Statistical analysis
The data was analyzed with Stata version 17 software. Due to the expected heterogeneity caused by differences in methodological approaches and geographic locations, the cumulative prevalence of SI was calculated using a random effects model (26). Heterogeneity was assessed using Cochran’s Q test (X2) and I2. I2 was evaluated with thresholds greater than or equal to 25%, greater than or equal to 50%, and greater than or equal to 75%, indicated low, medium, and high heterogeneity, respectively (27). A forest plot was used to display the estimated cumulative prevalence of SI (with 95% confidence interval [CI]). Sensitivity analysis was conducted to evaluate the robustness of the results, and meta-regression was performed to examine the relationship between the prevalence of SI and sample size, year of publication and mean age of participants. Subgroup analysis was performed to estimate the lifetime and period prevalence by the study countries (China and other countries). Publication bias was assessed using a funnel plot and Egger’s test.
Results
Selection results and study characteristics
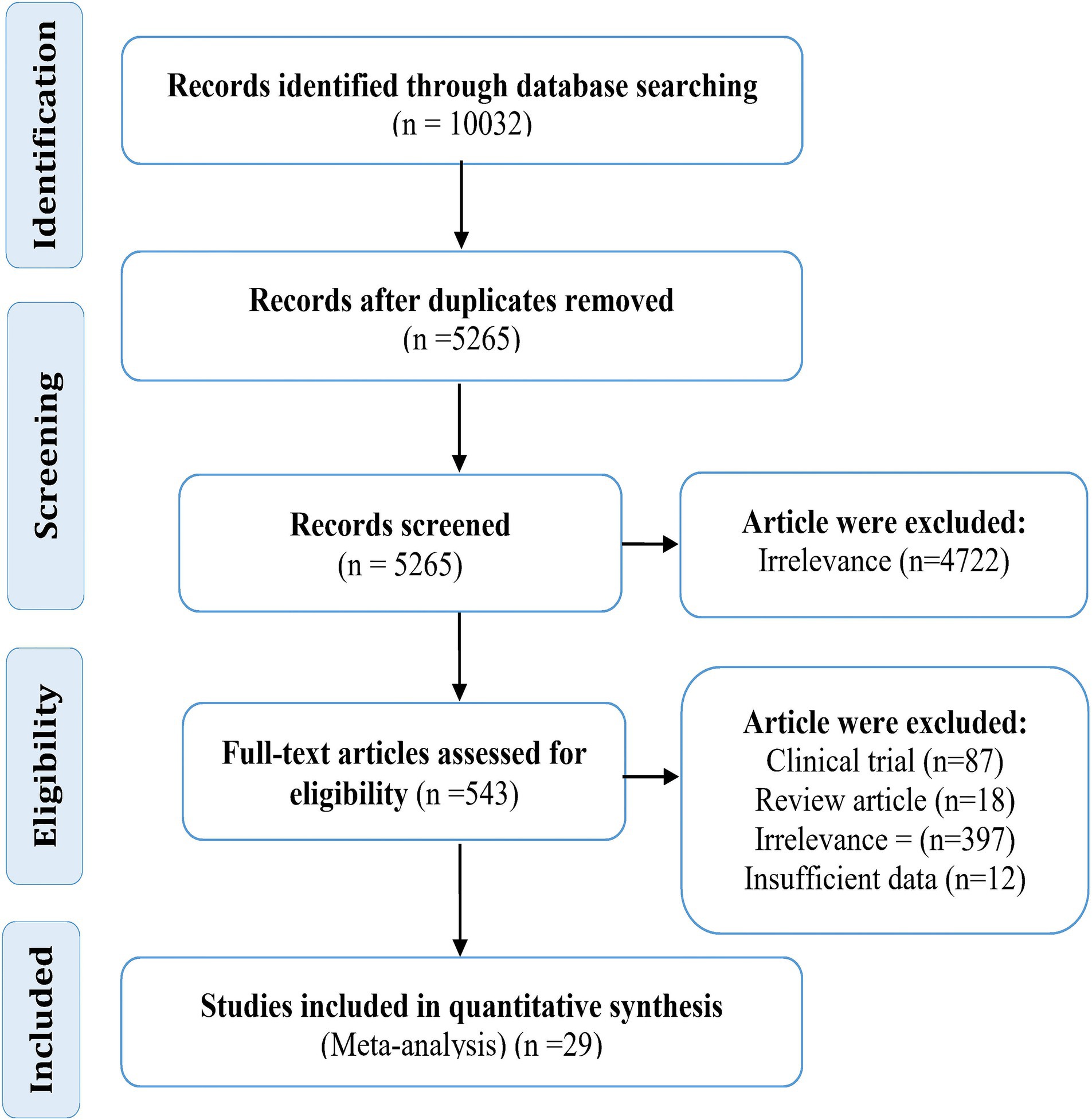
In the initial search, 10,032 articles were retrieved. Of these, 4,767 were duplicate articles. After reviewing the title and abstract of the remaining articles, 4,722 were removed. The full text of 543 articles was then reviewed. At this stage, 18 review articles, 87 clinical trials, 12 articles with insufficient data, and 397 irrelevant articles were excluded. Finally, 29 studies published in English, with a sample size of 12,934 subjects, were analyzed.
The smallest and largest sample sizes were 44 (28) and 2,343 (29), respectively. Most studies were published in 2023 (n = 11) and 2022 (n = 8). Also, 76% of selected studies were conducted in China. The rest of the studies were related to the countries of Colombia (n = 1), Turkey (n = 1), United States (n = 1), England (n = 1), and South Korea (n = 3). In terms of quality, 24 studies had good quality and five studies had moderate quality. The mean age of participants was reported in 14 studies (Table 1).
Lifetime and period prevalence
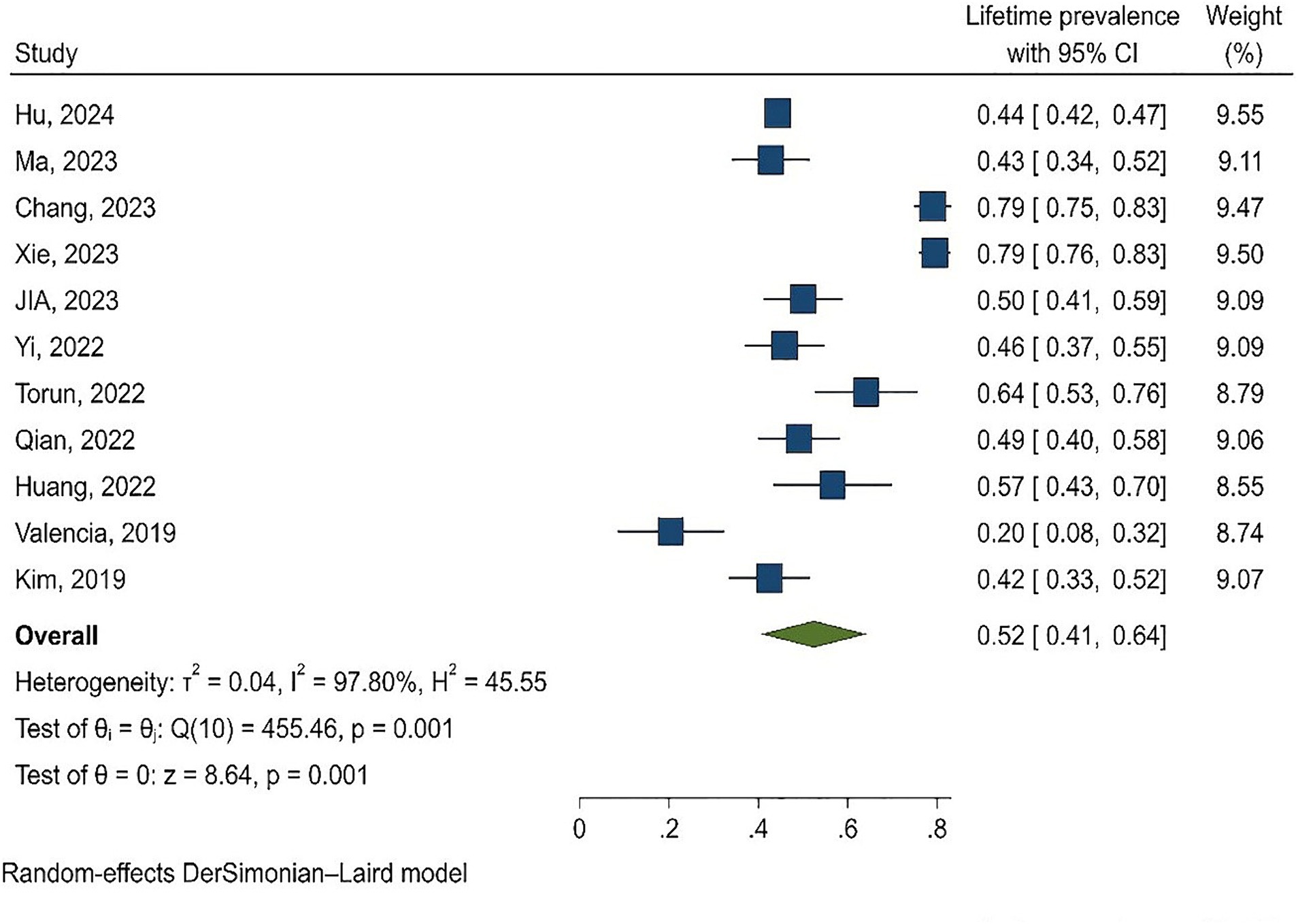
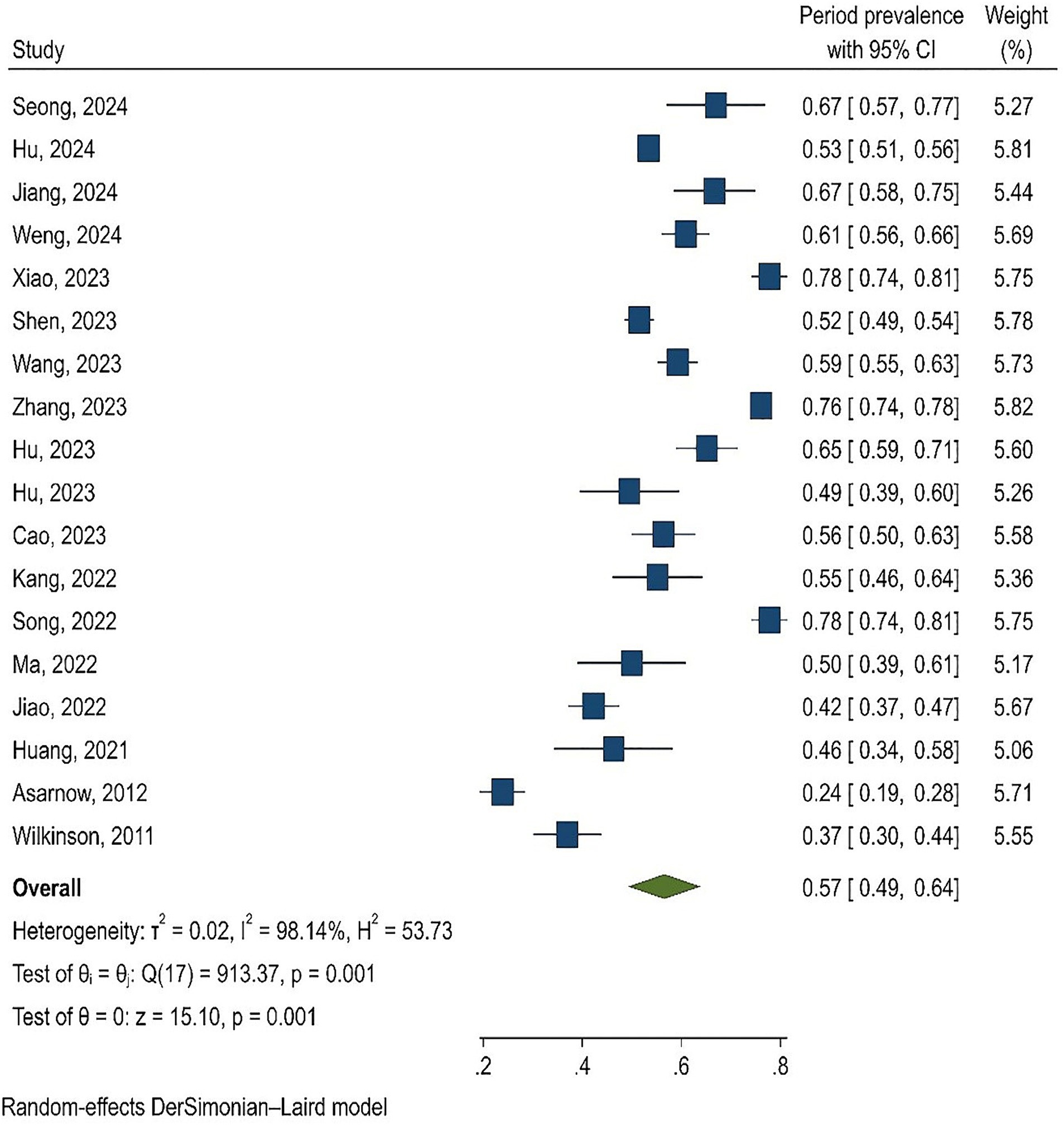
Of the 29 analyzed studies, 10 reported lifetime prevalence (28, 36, 38, 39, 43, 46, 49–51, 53), and 18 (29–35, 37, 40–42, 44, 45, 47, 48, 52, 54, 55) reported period prevalence. In one study, both lifetime and period prevalence were reported (31). In this study, ‘period prevalence’ referred to the prevalence in the last 6 to 12 months. Specifically, six studies reported prevalence in the last 6 months (31, 33, 42, 44, 52, 54), while 12 studies reported prevalence in the last year (29, 30, 32, 34, 35, 37, 40, 41, 45, 47, 48, 55). The lowest and highest lifetime prevalence rates were 20.4% (28) and 78.9% (38), respectively. Similarly, the lowest and highest period prevalence rates were 23.9% (54) and 77.8% (45), respectively (Figure 1).
The results of the meta-analysis showed that the lifetime prevalence and period prevalence of SI were 52% (95% CI: 41–64, I2 = 97.80%) and 57% (95% CI: 49–64, I2 = 98.14%), respectively (Figures 2, 3). Since most of the analyzed studies were related to China, subgroup analysis was performed and lifetime and period prevalence were assessed separately by region (China and other countries). The findings revealed that lifetime prevalence in China was 56% (95% CI: 45–67) compared to 42% (95% CI: 18–67) in other countries. Similarly, period prevalence in China was 60% (95% CI: 54–66) versus 45% (95% CI: 27–64) in other countries. The period and lifetime prevalence of suicide in China and other countries were not significantly different.
The results of subgroup analysis by year showed that the lifetime prevalence of SI was 59% (95% CI: 43–76, I2 = 98.66%) in 2023 and 2024, and 46% (95% CI: 35–58, I2 = 86.51%) in previous years (Q = 1.60, p = 0.206). Additionally, the prevalence of SI in the years 2023 and 2024 was 62% (95% CI: 57–68, I2 = 95.95%), which was significantly higher than in previous years (47% with 95% CI: 35–60, I2 = 96.73; Q = 4.25, p = 0.039).
Meta-regression analysis
Meta-regression was employed to investigate the relationship between lifetime and period prevalence with the year of publication of articles, mean age of participants and sample size. The results indicated a relationship between the period prevalence of SI and the year of publication of the articles (p = 0.002); such that between 2011 and 2024, the period prevalence of SI increased. In other words, from the publication of the oldest to the newest selected article, the period prevalence of SI has increased significantly.
Publication bias
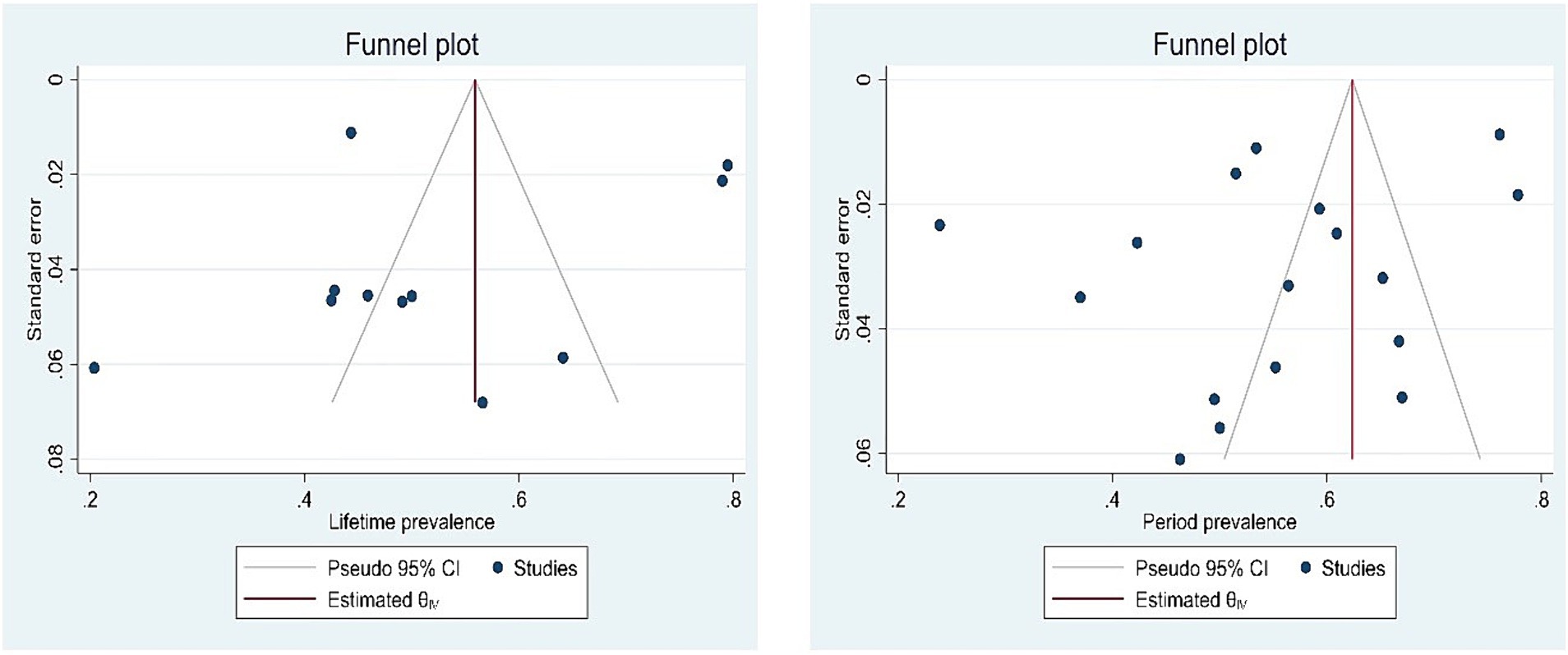
Publication bias was evaluated using Egger’s test and funnel plot. Publication bias was not significant in lifetime prevalence (p = 0.281) and period prevalence (0.358; Figure 4).
Discussion
In this study, the lifetime and period prevalence of self-injurious behavior among adolescents with depression was systematically reviewed. The results of this study showed that the lifetime and period prevalence of SI among adolescents with depression were 52 and 57%, respectively. In other words, more than half of adolescents with depression have a history of self-injurious behaviors. Self-injury, in which a person overtly harms themselves, is important because of the difficulties in determining whether an adolescent is attempting to die (56). Research on adolescents who intentionally hurt themselves and seek treatment at hospitals shows that their actions are often impulsive. These incidents are usually triggered by family or friend issues, school difficulties, or disciplinary problems. Additionally, some cases are related to depression, anxiety, or behavioral disorders (57). The results of our study showed that the lifetime and period prevalence of SI among adolescents with depression were 52 and 57%, respectively. In other words, more than half of adolescents with depression have a history of self-injurious behaviors. Adolescence is a sensitive and vulnerable age in which a person learns the methods of internalizing and externalizing emotions, and if they learn and use unhealthy coping mechanisms, a wide range of problematic behaviors can appear (58).
Xiao et al.’s meta-analysis revealed that the prevalence of lifetime and period SI in non-clinical adolescents was 22 and 23.2%, respectively. However, our present study found a higher prevalence. One possible explanation for this discrepancy is the coexistence of depression with these behaviors, which may intensify the desire to engage in self-injury and suicidal thoughts (59). Based on the comparison of these studies, it can be concluded that although the prevalence of self-injury behaviors is high among adolescents, these behaviors are much higher among those who also suffer from depression.
People with depression may perceive life in a negative and distorted way through the activation of negative events. They think based on the “cognitive triad” that they are worthless, the world is unfair, and their future is hopeless. Triggered by this negative triad, adolescents with depressive disorder may self-harm to end their symptoms (60). The results of Zhang et al.’s study (2023) the prevalence of SI in the last year among 2,343 adults with depression was 76.06% (29). In another study that was conducted on 1,095 students, the frequency of self-injury among depressed students was 35.14% (61). It appears that the prevalence of self-injurious behaviors among depressed youth is lower than among adults who suffer from depression. The presence of depression can heighten the prevalence of suicidal ideation (SI) behaviors and increase the likelihood of suicide (62). Therefore, the most basic method of suicide prevention is the screening of suicidal behaviors. The results of Park et al.’s study showed that the prevalence of SI among depressed people was higher than non-depressed people (63). According to the Third Variable theory, a third variable must exist to connect SI to suicide. This variable can include psychological issues such as depression, suicidal thoughts, personality disorders, low self-esteem, and lack of family support (21, 64). The relationship between depression and SI is rarely linear, and a combination of predisposing factors such as genetics and previous experiences and acceleration of stressful events is involved in its occurrence (65). In another study, teenagers with SI behaviors had less suicidal thoughts and depression symptoms, more self-esteem, and more parental support compared to teenagers who attempted suicide (66). The results of a systematic review showed that SI behaviors with the following characteristics are associated with a significant rate of suicide attempts: duration of more than 1 year, use of multiple methods, self-cutting, frequent SI episodes, absence of physical pain during self-injury, severe physical harm, strong conscious intent to die, and concealment of the act (64).
Meta-regression results showed that from 2011 to 2024, the period prevalence of SI has increased significantly. The reason for this rising prevalence of SI may be the escalating level of daily stress and serious crises in recent years. The reason behind this finding may be that self-harm is associated with less stigma than many other inappropriate behaviors. Consequently, teenagers engage in self-harm more readily and even share their experiences with their peers. Further exploration of this issue necessitates qualitative studies.
Subgroup analysis revealed that while the lifetime and period prevalence of SI was higher in studies conducted in China compared to studies in other countries, this difference did not reach statistical significance. The prevalence of deliberate self-injury in 2023 and 2024 was significantly higher than in previous years. This increase may be attributed to heightened mental health concerns related to the onset of World War III and conflicts in the Middle East.
To the best of our knowledge, this meta-analysis is the first to examine the prevalence of self-injurious behaviors among depressed adolescents. SI behaviors are known as one of the predictors of suicide, so knowing the prevalence of SI in this age group provides new insights for researchers and policy makers to make decisions and adopt appropriate policies. This meta-analysis had several limitations: (1) only articles published in English were analyzed, (2) there were no other systematic review and meta-analysis studies conducted on adolescents, to which the findings of the present study could be compared, (3) Due to the small number of selected studies, studies with a small sample size were also included in the analysis, which may affect the reported estimated pooled prevalence.
Conclusion
The prevalence of self-injurious behaviors among adolescents with depression is high, so that 57% of adolescents have committed these behaviors during the last year and 52% of adolescents have committed these behaviors during their lifetime. Considering that these behaviors can increase the chance of suicide, it seems necessary to identify people at risk.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YW: Data curation, Methodology, Software, Writing – original draft, Writing – review & editing. YZ: Data curation, Formal analysis, Resources, Writing – original draft, Writing – review & editing. CW: Data curation, Methodology, Software, Writing – original draft, Writing – review & editing. BH: Investigation, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nock, MK . Self-injury. Annu Rev Clin Psychol. (2010) 6:339–63. doi: 10.1146/annurev.clinpsy.121208.131258
2. Cipriano, A, Cella, S, and Cotrufo, P. Nonsuicidal self-injury: a systematic review. Front Psychol. (2017) 8:282818. doi: 10.3389/fpsyg.2017.01946
4. Favazza, AR, and Rosenthal, RJ. Diagnostic issues in self-mutilation. Psychiatr Serv. (1993) 44:134–40. doi: 10.1176/ps.44.2.134
5. Pao, PN . The syndrome of delicate self-cutting. Br J Med Psychol. (1969) 42:195–206. doi: 10.1111/j.2044-8341.1969.tb02071.x
6. Pattison, EM, and Kahan, J. The deliberate self-harm syndrome. Am J Psychiatry. (1983) 140:867–72. doi: 10.1176/ajp.140.7.867
7. Tantam, D, and Whittaker, J. Personality disorder and self-wounding. Br J Psychiatry. (1992) 161:451–64. doi: 10.1192/bjp.161.4.451
8. Silva, SA, Silva, SU, Ronca, DB, Gonçalves, VSS, Dutra, ES, and Carvalho, KMB. Common mental disorders prevalence in adolescents: a systematic review and meta-analyses. PLoS One. (2020) 15:e0232007. doi: 10.1371/journal.pone.0232007
9. Briere, J, and Gil, E. Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. Am J Orthop. (1998) 68:609–20. doi: 10.1037/h0080369
10. Laye-Gindhu, A, and Schonert-Reichl, KA. Nonsuicidal self-harm among community adolescents: understanding the “whats” and “whys” of self-harm. J youth Adolescence. (2005) 34:447–57. doi: 10.1007/s10964-005-7262-z
11. Lloyd-Richardson, EE, Perrine, N, Dierker, L, and Kelley, ML. Characteristics and functions of non-suicidal self-injury in a community sample of adolescents. Psychol Med. (2007) 37:1183–92. doi: 10.1017/S003329170700027X
12. Brown, SA, Williams, K, and Collins, A. Past and recent deliberate self-harm: emotion and coping strategy differences. J Clin Psychol. (2007) 63:791–803. doi: 10.1002/jclp.20380
13. Glenn, CR, and Klonsky, ED. Social context during non-suicidal self-injury indicates suicide risk. Personal Individ Differ. (2009) 46:25–9. doi: 10.1016/j.paid.2008.08.020
14. Selby, EA, Bender, TW, Gordon, KH, Nock, MK, and Joiner, TE Jr. Non-suicidal self-injury (NSSI) disorder: a preliminary study. Personality Disorders: Theory, Research, Treatment. (2012) 3:167–75. doi: 10.1037/a0024405
15. Wester, KL, and Trepal, HC. Nonsuicidal self-injury: exploring the connection among race, ethnic identity, and ethnic belonging. J Coll Stud Dev. (2015) 56:127–39. doi: 10.1353/csd.2015.0013
16. Kaniuka, AR, Kelliher-Rabon, J, Chang, EC, Sirois, FM, and Hirsch, JK. Symptoms of anxiety and depression and suicidal behavior in college students: conditional indirect effects of non-suicidal self-injury and self-compassion. J Coll Stud Psychother. (2020) 34:316–38. doi: 10.1080/87568225.2019.1601048
17. Whitlock, J, Muehlenkamp, J, Eckenrode, J, Purington, A, Abrams, GB, Barreira, P, et al. Nonsuicidal self-injury as a gateway to suicide in young adults. J Adolesc Health. (2013) 52:486–92. doi: 10.1016/j.jadohealth.2012.09.010
18. Predescu, E, and Sipos, R. Self-harm behaviors, suicide attempts, and suicidal ideation in a clinical sample of children and adolescents with psychiatric disorders. Child Aust. (2023) 10:725. doi: 10.3390/children10040725
19. Hawton, K, Helen, B, Navneet, K, Jayne, C, Sarah, S, Jennifer, N, et al. “Repetition of self‐harm and suicide following self‐harm in children and adolescents: Findings from the Multicentre Study of Self‐harm in England.” J. Child Psychol. Psychiatry. (2012) 53:1212–1219. doi: 10.1111/j.1469-7610.2012.02559.x
20. Bryan, CJ, Bryan, AO, Ray-Sannerud, BN, Etienne, N, and Morrow, CE. Suicide attempts before joining the military increase risk for suicide attempts and severity of suicidal ideation among military personnel and veterans. Compr Psychiatry. (2014) 55:534–41. doi: 10.1016/j.comppsych.2013.10.006
21. Hamza, CA, Stewart, SL, and Willoughby, T. Examining the link between nonsuicidal self-injury and suicidal behavior: a review of the literature and an integrated model. Clin Psychol Rev. (2012) 32:482–95. doi: 10.1016/j.cpr.2012.05.003
22. Benjet, C, González-Herrera, I, Castro-Silva, E, Méndez, E, Borges, G, Casanova, L, et al. Non-suicidal self-injury in Mexican young adults: prevalence, associations with suicidal behavior and psychiatric disorders, and DSM-5 proposed diagnostic criteria. J Affect Disord. (2017) 215:1–8. doi: 10.1016/j.jad.2017.03.025
23. Glenn, CR, Lanzillo, EC, Esposito, EC, Santee, AC, Nock, MK, and Auerbach, RP. Examining the course of suicidal and nonsuicidal self-injurious thoughts and behaviors in outpatient and inpatient adolescents. J Abnorm Child Psychol. (2017) 45:971–83. doi: 10.1007/s10802-016-0214-0
24. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. PRISMA group* t. preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
25. Munn, Z, Moola, S, Lisy, K, Riitano, D, and Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. JBI Evidence Implementation. (2015) 13:147–53. doi: 10.1097/XEB.0000000000000054
26. DerSimonian, R, and Laird, N. Meta-analysis in clinical trials. Control Clin Trials. (1986) 7:177–88. doi: 10.1016/0197-2456(86)90046-2
27. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
28. Valencia, LFF, Maya, JF, Cubillos, GVI, Suárez, LFG, and Moreno, MJV. Relationship between self-injurious behavior with non-suicidal purposes and depression in a schooled adolescent population. Cuad Hispanoam. (2019) 19:1–25. doi: 10.18270/chps..v19i2.3145
29. Zhang, B, Zhang, W, Sun, L, Jiang, C, Zhou, Y, and He, K. Relationship between alexithymia, loneliness, resilience and non-suicidal self-injury in adolescents with depression: a multi-center study. BMC Psychiatry. (2023) 23:445. doi: 10.1186/s12888-023-04938-y
30. Seong, E, Lee, KH, Lee, J-S, Kim, S, Seo, DG, Yoo, JH, et al. Depression and posttraumatic stress disorder in adolescents with nonsuicidal self-injury: comparisons of the psychological correlates and suicidal presentations across diagnostic subgroups. BMC Psychiatry. (2024) 24:138. doi: 10.1186/s12888-024-05533-5
31. Hu, R, Peng, L-L, Du, Y, Feng, Y-W, Xie, L-S, Shi, W, et al. Reciprocal effect between non-suicidal self-injury and depressive symptoms in adolescence. Front Public Health. (2024) 11:1243885. doi: 10.3389/fpubh.2023.1243885
32. Jiang, Y, Yu, H, Zheng, Q, Zhu, Y, Qin, Q, Zhang, J, et al. Effects of decision making and impulsivity on the addictive characteristics of non-suicidal self-injurious behavior in adolescents with depressive disorders. [Preprint] (2024). doi: 10.21203/rs.3.rs-3856456/v1
33. Weng, X, Tang, R, Chen, L, Weng, X, Wang, D, Wu, Z, et al. Pathway from childhood trauma to nonsuicidal self-injury in adolescents with major depressive disorder: the chain-mediated role of psychological resilience and depressive severity. Eur Arch Psychiatry Clin Neurosci. (2024):1–9. doi: 10.1007/s00406-023-01746-z
34. Xiao, Q, Song, X, Huang, L, Hou, D, and Huang, X. Association between life events, anxiety, depression and non-suicidal self-injury behavior in Chinese psychiatric adolescent inpatients: a cross-sectional study. Front Psychol. (2023) 14:1140597. doi: 10.3389/fpsyt.2023.1140597
35. Shen, Y, Hu, Y, Zhou, Y, and Fan, X. Non-suicidal self-injury function: prevalence in adolescents with depression and its associations with non-suicidal self-injury severity, duration and suicide. Front Psychol. (2023) 14:1188327. doi: 10.3389/fpsyt.2023.1188327
36. Ma, L, Zhou, D-D, Zhao, L, Hu, J, Peng, X, Jiang, Z, et al. Impaired behavioral inhibitory control of self-injury cues between adolescents with depression with self-injury behavior and those without during a two-choice oddball task: an event-related potential study. Front Psychol. (2023) 14:1165210. doi: 10.3389/fpsyt.2023.1165210
37. Wang, L, Zou, HO, Liu, J, and Hong, JF. Prevalence of adverse childhood experiences and their associations with non-suicidal self-injury among Chinese adolescents with depression. Child Psychiatry Hum Dev. (2023):1–11. doi: 10.1007/s10578-023-01508-x
38. Chang, L, and Zhang, Y. Establishment and verification of a diagnostic prediction model for non-suicidal self-injury behaviors in adolescents with depressive disorder. Sichuan Mental Health. (2023) 6:12–8.
39. Xie, X, Liu, J, Gong, X, Sun, T, Li, Y, Liu, Z, et al. Relationship between childhood trauma and nonsuicidal self-injury among adolescents with depressive disorder: mediated by negative life events and coping style. Neuropsychiatr Dis Treat. (2023) 19:2271–81. doi: 10.2147/NDT.S431647
40. Hua, C, Huang, J, Shang, Y, Huang, T, Jiang, W, and Yuan, Y. Child maltreatment exposure and adolescent nonsuicidal self-injury: the mediating roles of difficulty in emotion regulation and depressive symptoms. Child Adolesc Psychiatry Ment Health. (2023) 17:16. doi: 10.1186/s13034-023-00557-3
41. Hub, C, Jiang, W, Wu, Y, Wang, M, Lin, J, Chen, S, et al. Microstructural abnormalities of white matter in the cingulum bundle of adolescents with major depression and non-suicidal self-injury. Psychol Med. (2023) 54:1–9.
42. Cao, P, Peng, R, Yuan, Q, Zhou, R, Ye, M, and Zhou, X. Predictors of non-suicidal self-injury in adolescents with depressive disorder: the role of alexithymia, childhood trauma and body investment. Front Psychol. (2023) 15:1336631. doi: 10.3389/fpsyg.2024.1336631
43. Jia, X, Wang, T, Han, H, Liu, J, Wang, L, Tian, B, et al. Correlation of cognitive function and clinical characteristics in adolescent depressive disorder patients with self-injury behavior. Chinese journal of behavioral medicine and brain. Science. (2023) 12:707–13.
44. Kang, B, Hwang, J, Woo, S-i, Hahn, S-W, Kim, M, Kim, Y, et al. The mediating role of depression severity on the relationship between suicidal ideation and self-injury in adolescents with major depressive disorder. J Korean Acad Child and Adoles Psychiatry. (2022) 33:99–105. doi: 10.5765/jkacap.220014
45. Song, X, Huang, L, Hou, D, Ran, M, Huang, X, and Xiao, Q. Influencing factors of non-suicidal self-injury according to DSM-5 in adolescents admitted to the psychiatric department: a cross-sectional study. Translational pediatrics. (2022) 11:1972–84. doi: 10.21037/tp-22-588
46. Yi, P-c, Qin, Y-h, Zheng, C-m, Ren, K-m, Huang, L, and Chen, W. Tumor markers and depression scores are predictive of non-suicidal self-injury behaviors among adolescents with depressive disorder: a retrospective study. Front Neurosci. (2022) 16:953842. doi: 10.3389/fnins.2022.953842
47. Ma, J, Zhao, M, Niu, G, Wang, Z, Jiang, S, and Liu, Z. Relationship between thyroid hormone and sex hormone levels and non-suicidal self-injury in male adolescents with depression. Front Psychol. (2022) 13:13. doi: 10.3389/fpsyt.2022.1071563
48. Jiao, T, Guo, S, Zhang, Y, Li, Y, Xie, X, Ma, Y, et al. Associations of depressive and anxiety symptoms with non-suicidal self-injury and suicidal attempt among Chinese adolescents: the mediation role of sleep quality. Front Psychol. (2022) 13:1018525. doi: 10.3389/fpsyt.2022.1018525
49. Taş Torun, Y, Gul, H, Yaylali, FH, and Gul, A. Intra/interpersonal functions of non-suicidal self-injury in adolescents with major depressive disorder: the role of emotion regulation, alexithymia, and childhood traumas. Psychiatry. (2022) 85:86–99. doi: 10.1080/00332747.2021.1989854
50. Qian, H, Shu, C, Feng, L, Xiang, J, Guo, Y, and Wang, G. Childhood maltreatment, stressful life events, cognitive emotion regulation strategies, and non-suicidal self-injury in adolescents and young adults with first-episode depressive disorder: direct and indirect pathways. Front Psychol. (2022) 13:838693. doi: 10.3389/fpsyt.2022.838693
51. Huang, F, and Liu, T. Association between non-suicidal self-injury behavior and impulsivity in adolescent patients with depressive disorder in the first hospitalization. Sichuan mental. Health. (2022) 6:132–6.
52. Huang, Q, Xiao, M, Ai, M, Chen, J, Wang, W, Hu, L, et al. Disruption of neural activity and functional connectivity in adolescents with major depressive disorder who engage in non-suicidal self-injury: a resting-state fMRI study. Front Psychol. (2021) 12:571532. doi: 10.3389/fpsyt.2021.571532
53. Kim, G-M . 3.53 the association between NonSuicidal self-injury (NSSI) and suicide attempts in korean adolescents with clinical depression. J Am Acad Child Adolesc Psychiatry. (2019) 58:S212. doi: 10.1016/j.jaac.2019.08.216
54. Asarnow, JR, Porta, G, Spirito, A, Emslie, G, Clarke, G, Wagner, KD, et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: findings from the TORDIA study. Focus. (2012) 10:380–8. doi: 10.1176/appi.focus.10.3.380
55. Wilkinson, P, Kelvin, R, Roberts, C, Dubicka, B, and Goodyer, I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the adolescent depression antidepressants and psychotherapy trial (ADAPT). Am J Psychiatry. (2011) 168:495–501. doi: 10.1176/appi.ajp.2010.10050718
56. Peterson, J, Freedenthal, S, Sheldon, C, and Andersen, R. Nonsuicidal self injury in adolescents. Psychiatry (Edgmont). (2008) 5:20–6.
57. Rodham, K, Hawton, K, and Evans, E. Reasons for deliberate self-harm: comparison of self-poisoners and self-cutters in a community sample of adolescents. J Am Acad Child Adolesc Psychiatry. (2004) 43:80–7. doi: 10.1097/00004583-200401000-00017
58. Lanfredi, M, Macis, A, Ferrari, C, Meloni, S, Pedrini, L, Ridolfi, ME, et al. Maladaptive behaviours in adolescence and their associations with personality traits, emotion dysregulation and other clinical features in a sample of Italian students: a cross-sectional study. Borderline personality disorder and emotion dysregulation. (2021) 8:14. doi: 10.1186/s40479-021-00154-w
59. Xiao, Q, Song, X, Huang, L, Hou, D, and Huang, X. Global prevalence and characteristics of non-suicidal self-injury between 2010 and 2021 among a non-clinical sample of adolescents: a meta-analysis. Front Psychol. (2022) 13:912441. doi: 10.3389/fpsyt.2022.912441
60. Hendrick, MT . Depression’s connection to self-harming behavior in adolescents. Fisher Digital Publications. (2016).
61. Yuan, Q . The association between depression and non-suicidal self-injury among college students. MEDS Public Health Preven Med. (2023) 3:1–8.
62. Erskine, HE, Maravilla, JC, Wado, YD, Wahdi, AE, Loi, VM, Fine, SL, et al. Prevalence of adolescent mental disorders in Kenya, Indonesia, and Viet Nam measured by the National Adolescent Mental Health Surveys (NAMHS): a multi-national cross-sectional study. Lancet. (2024) 403:1671–80. doi: 10.1016/S0140-6736(23)02641-7
63. Park, Y-H, Jeong, Y-W, Kang, Y-H, Kim, S-W, Park, S-Y, Kim, K-J, et al. Mediating the effects of depression in the relationship between university students' attitude toward suicide, frustrated interpersonal needs, and non-suicidal self-injury during the COVID-19 pandemic. Arch Psychiatr Nurs. (2022) 37:25–32. doi: 10.1016/j.apnu.2021.11.005
64. Grandclerc, S, De Labrouhe, D, Spodenkiewicz, M, Lachal, J, and Moro, MR. Relations between nonsuicidal self-injury and suicidal behavior in adolescence: a systematic review. PLoS One. (2016) 11:e0153760. doi: 10.1371/journal.pone.0153760
65. Harrington, R . Depression, suicide and deliberate self-harm in adolescence. Br Med Bull. (2001) 57:47–60. doi: 10.1093/bmb/57.1.47
Keywords: adolescent, non-suicidal self-injury, self-injury, depression, meta-analysis
Citation: Wu Y, Zhang Y, Wang C and Huang B (2024) A meta-analysis on the lifetime and period prevalence of self-injury among adolescents with depression. Front. Public Health. 12:1434958. doi: 10.3389/fpubh.2024.1434958
Edited by:
Joemer Calderon Maravilla, The University of Queensland, AustraliaReviewed by:
Amirah Wahdi, Gadjah Mada University, IndonesiaDaisy Huelva Alberto, De La Salle Health Sciences Institute, Philippines
Copyright © 2024 Wu, Zhang, Wang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beibei Huang, aHVhbmdiYl9uYmhAb3V0bG9vay5jb20=
 Yanli Wu1
Yanli Wu1 Beibei Huang
Beibei Huang