
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 01 October 2024
Sec. Life-Course Epidemiology and Social Inequalities in Health
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1434106
 Shengxuan Jin1,2†
Shengxuan Jin1,2† Ruobing Fa1†
Ruobing Fa1† Jiaqi Wu1
Jiaqi Wu1 Jiawei Lin1
Jiawei Lin1 Shuyuan Zhang1
Shuyuan Zhang1 Majid Ali1
Majid Ali1 Shaofan Chen1*
‡
Shaofan Chen1*
‡ Dongfu Qian1,3*
‡
Dongfu Qian1,3*
‡Background: Multiple intersections, including socioeconomic inequalities, influence health equity for disabled people and sub-populations. However, this association has not been sufficiently analyzed among Chinese-impaired persons. This study aimed to investigate the health services utilization and inequalities in middle and older adult persons with disabilities and subgroups.
Methods: The China Health and Retirement Longitudinal Study (CHARLS) database in 2011, 2013, 2015, and 2018 were used. Health services utilization was measured by outpatient, inpatient, and self-treatment service utilization. Types of disabilities were classified into six categories. The pooled cross-section regression, concentration index, horizontal inequity index, and concentration index decomposition were used to evaluate inequalities and explore their main contributing factor.
Results: The utilization and non-utilization of healthcare services showed variations across years (p < 0.05). The CIs and HIs for inpatient health service utilization were positive for all years and disability types. The total CIs of inpatient utilization were the highest (0.248). The highest disparities in utilization of inpatient services were for physical disabilities (0.4515 for CI in 2011), and the highest in self-treatment services were for intellectual disability (0.1538 for CI in 2011). The expenditure factor was the main contributor to inequalities. Chronic disease, educational level, and health insurance factors also contribute to the utilization inequalities.
Conclusion: Policies should promote medical insurance and assistance for disabled people with serious impairment and poor. It is crucial to improve the provision of basic medical services, including meeting the demand for varied disabilities and the accessibility of facilities and equipment to enhance the access and well-being of people with disabilities.
People with disabilities are among the most disadvantaged and marginalized populations, frequently facing prejudice and challenges in terms of social, economic, and health disparities (1). Around 1.3 billion people, or 16% of the world’s population, were estimated to be disabled (2). China currently has the largest number of persons with disabilities in the world, with over 85 million individuals affected (6% of the country’s total population) (3). The general trend toward an increase in human life expectancy is leading to an aging population, which will inevitably lead to a significant increase in the number of older people with disabilities and semi-disabilities. Healthcare is crucial for people with disabilities as it provides equal opportunities by sustaining fundamental function and health promotion (4). A person with disabilities is more likely to report being in poor health and to have a higher incidence of chronic diseases such as diabetes, cardiac disease, overweight, and asthma (5–7). Compared to younger adults with disabilities, older adults with disabilities are more likely to have functional limitations and co-morbid conditions (8). Thus the demands for the use of healthcare services among those with disabilities are rising. However, the increased expenditures on health care, personal care, equipment, or other modifications connected to disabilities may cause families to fall into poverty or return to poverty due to their disabilities (9, 10). Equality in health service utilization is the basis of achieving health equality (11). A recent report demonstrated that health inequalities for persons with disabilities are influenced by multiple intersections, especially social determinants of health and broad barriers in the health system (2). Different disability types suffer various environmental and self-dysfunctional issues, which may result in more pronounced inequalities in specific subgroups (12). Research have pointed out that China currently at a medium-high level of social disability risk, suggesting that the Government urgently needs to take measures to meet the needs of the aging population and the older adult population with disabilities and semi-disabilities (13). As a result, understanding the use of health services and its inequalities for people with disabilities to support their access to health services and avoid significant complications and secondary diseases becomes an urgent issue in China.
The international policy and guidance framework for disability health inequalities has evolved over time (2). Many programs proposed in recent years, such as the WHO Global Disability Action Plan 2014–2021 (2014), the Sustainable Development Goal (SDG) target 3.8 (2015) explicitly refers to “access to health services for all persons with disabilities,” and the political declaration of “Universal health coverage” (2019) includes a specific reference for persons with disabilities. At the 74th World Health Assembly in 2021, Resolution 74.8 sets out “The highest attainable standard of health for persons with disabilities.” Furthermore, many countries have established policy promises to improve the health of people with disabilities. The Disability Strategy 2021–2031 has been formed in Australia, which includes the health and well-being of people with disabilities as one of seven outcome areas (14). To facilitate people with disabilities access to comprehensive health care, the Brazilian Ministry of Health adopted the National Health Policy for Persons with Disabilities (PNSPD) in 2002 and has recently made clear commitments to increase the availability of assistive technologies and rehabilitative services (15, 16). Due to the enormous number of disabled persons in China, the Law on the Protection of Persons with Disabilities was first implemented in 1991, which signaled the start of China’s legalization of disability protection. A unique welfare subsidy system for persons with disabilities, including living allowances for persons with difficulties and care subsidies for severely disabled persons, was established in 2015 (17). Guidance on the Expansion of the Pilot Long-term Care Insurance System (2020) proposed to focus on fullfill the fundamental care protection needs of older adults, the older adult who are disabled, and those with severe impairments (18). Medical rehabilitation projects are covered by medical insurance and expanded to 29 services. Although many nations have achieved significant progress, it is still far from ensuring people with disabilities get access to the highest attainable standard of health.
Previous studies have been carried out worldwide on the inequalities in health services utilization for persons with disabilities. According to Jeon B’s (4) analysis of the characteristics of persons with disabilities and the relationship between disability severity and health care utilization, people with disabilities have less access to preventative and outpatient health services. Julie Maltais (19) compared the healthcare utilization of intellectual disabilities to that of the general population, discovering inequalities for intellectual disabilities, particularly those more likely to develop secondary health issues. In Afghanistan, Trani Jean-Francois’s (20) analysis of health care utilization and inequalities for persons with disabilities shows inequalities in health care utilization in favor of low-income people. Several studies on health inequalities for people with disabilities have been conducted in China, some of which are based on functional disability measurements such as activities of daily living (ADL) and instrumental activities of daily living (IADL) to analyze the socioeconomic characteristics of disability in older adults in China (21, 22), and to determine the inequalities in functional disability of older populations (23). Scholars such as Xiao Jian (8) discovered disparities in health service utilization across disability trajectory categories, including progressive, late-onset, and normal categories. Guo Chao (24) investigated socioeconomic disparities in mental health service utilization among older adults with intellectual disabilities in China, finding that urban residence, higher education, marital status, health insurance coverage, and higher household income were associated with higher mental health service utilization. Their research teams also analyzed the utilization rate of auxiliary aids and healthcare services between 1987 and 2006 (25). Xintong Zhao (26) analyzed the unmet healthcare needs of people with disabilities across different residence and disability types in China and found that the rural–urban factor were significantly associated with unmet needs with rural types experiencing a significant increase in unmet healthcare needs of 13–40%. However, the older adult, people with chronic illnesses, and other demographics are primarily the focus of studies on health service utilization inequalities in China. Such as Jing Guo (27) explored socioeconomic inequalities among chronic disease populations, revealing significant differences in inequalities related to living areas, education level, economic status, and social participation. Xiaojing Fan (28) studied the inpatient health services utilization among urban and rural residents and found that the inpatient health services utilization was more concentrated among low economic groups. As a result, we reveal that inequalities exist in middle-aged and older adult persons with disabilities and may eventually worsen due to the aging population, making health service utilization inequalities for the disabled a critical public health issue.
Present research on the disabled population is insufficient since there lacks a comprehensive analysis of the utilization of health services and the inequalities in services utilization of the disabled population in Chinese. Firstly, the majority of these studies were cross-sectional in design, assessing health services inequalities at a single point in time, which fails to capture the trajectory over time. Secondly, these studies were limited to a particular type of disability or within the overall type of disability and were not subdivided into more types of disability. Thirdly, these studies have primarily examined a certain type of health services utilization. It is therefore possible to provide comprehensive evidence based on the Chinese population by analyzing each type of disability and each type of health service utilization and exploring changes over time. This study aims to analyze the utilization and the inequality of health services among middle-aged and older adult persons with disabilities and sub-types in Chinese population, and explore changes over time. Targeted references and strategies for promoting health equality and protecting the fundamental medical rights and interests of persons with disabilities were provided.
China Health and Retirement Longitudinal Survey (CHARLS) was used in the current study. It is a longitudinal survey designed to represent the population aged 45 years and older in mainland China. The baseline survey was conducted in 2011–12, followed by wave 2 in 2013, wave 3 in 2015, and wave 4 in 2018. To ensure a representative sample, the CHARLS baseline survey covered 150 counties/districts and 450 villages/urban communities across China, involving 17,708 individuals in 10,257 households, covering the Chinese middle-aged and older adult population (29).
This study focused on middle-aged and older persons with disabilities, and the inclusion criteria were: (1) aged 45 and over. (2) had one or more disabilities. The situation of disability was extracted from the question “Do you have one of the following disabilities” in the CHARLS, which included five options: physical disabilities, intellectual disabilities, vision problems, hearing problems, and speech impediments. Participants with two or more disability problems were defined as “Multiple disabilities.”
The current utilization of health services were analyzed firstly, then the inequalities were measured and the main influences affecting service utilization and its inequalities were explored. A longitudinal comparative analysis was conducted using the four waves in CHARLS: 2011, 2013, 2015, and 2018. The data were first selected by age and type of disability inclusion criteria, obtaining 3,088, 2,388, 2,634, and 2,425 individuals, respectively. Secondly, the variable of annual per capita household expenditure, is an important socioeconomic status variable for this study. The distribution of the data was observed by plotting a histogram, which revealed a small number of extreme values at both ends, which may adversely affect our analyses. By referring to the literature’s treatment of the annual per capita household expenditure variable and combining it with the distribution of the data in this study, we chose 2 per cent as the threshold to exclude the outliers of the annual per capita household expenditure variable, which could effectively removes these extreme values while retaining most of the observations within the normal range. Ultimately, 2,910, 2,123, 2,442, and 2,320 persons with disabilities were chosen for the study.
Three binary outcome variables of health services utilization by the disabled were adopted, outpatient service utilization, inpatient service utilization, and self-treatment service utilization. The three variables were extracted from the following questions in the CHARLS database: “In the last month have you visited a public hospital, private hospital, public health center, clinic, or health worker’s or doctor’s practice, or been visited by a health worker or doctor for outpatient care?,” “Have you received inpatient care in the past year?” and “Did you use any of the following self-treatment methods during the past month? (circle all that apply).” The answers to the questions were either “yes” or “no” and assign a value of “1” to the “yes” option and “0” to the “No” option.
In order to measure the horizontal inequity in healthcare utilization, it is essential to standardize health care needs of individuals. Actual services use is a factual depiction of the extent of equality (or inequality) in the distribution of health services. Need-expected services use represents predicted services use based on the needs-based variables. Need-standardized services use means the actual distribution of services use that is determined by non-need factors in the absence of differences in the distribution of health needs (30, 31). Therefore, study defined the health services utilization is associated not only with responses to need variables, but also with non-need variables (32). Needs-based variables are those related to the characteristics and health status that impact their medical service needs. The non-needs variables refer to the socioeconomic related factors that affect the demand for health services utilization, beyond the own health problems variable (31–33). Ideally, the needs-based variables would be the determinants of health service utilization. In this study, the Needs-based variables were defined as gender, age, self-rated health, chronic disease, activities of daily living (ADL), and instrumental activity of daily living (IADL). The non-needs variables were defined as household expenditure level, smoking, alcohol drinking, marital status, educational level, social activity, child financial support, region, and basic medical insurance.
In this study, the socioeconomic status was measured by the annual per capita household expenditure level, which represents household expenditure in the year preceding the survey and is the average of the permanent household population, excluding productive expenditure (31, 34). This measurement avoids the possible impact of household income outliers in the CHARLS database (35). At the same time, in order to minimize the effect of the variance in household expenditure caused by the state of the national economy in each year, the annual per capita household expenditures variable was divided into five levels of “Low level,” “Low-middle level,” “Average level,” “High-middle level,” and “High level” by calculating the 20 per cent, 40 per cent, 60 per cent, and 80 per cent quartiles for each of the four waves. The specific definitions of the variables are shown in Table 1.
Descriptive analysis was shown by frequency and percentage. Chi-squared test was used to analyze the differences in sample characteristics, health services utilization across waves and disability types. The wave factors were included in the pooled cross-section regression to evaluate the associated factors with health services utilization. The p-values, odd ratio (OR) and 95% confidence interval were reported. The health services utilization inequalities were measured by the Concentration index (CI), Horizontal inequity index (HI) and decomposition of concentration index (36). The STATA 14.0 was used for data analysis.
The Concentration index (CI) was used to measure the inequities in health services utilization, which was introduced by Wagstaff (36) to measure income-related health service use and health inequities and is widely accepted. CI ranges from −1 to 1, with the positive value indicating that income-related inequality concentrates on the rich, whereas the negative value indicates pro-poor inequality. A zero value represents that the distribution of healthcare utilization is equal. The equation of CI is as follows (37):
Where C was defined in terms of the covariance between the outcome variable (h) for whether health service utilization occurs and the fractional ranks of annual per capita household consumption expenditure (r). μ is the mean value of health service utilization (h).
The Horizontal inequity index (HI) measured the utilization of necessary standardized health services. It reveals inequalities in health service utilization by controlling for the influence of need-based variables on health service use. It is interpreted as the impact on health service utilization due to different socioeconomic status when the health condition is given the same demand for health services (38). Similar to CI, the positive value suggests the health service is more concentrated on the wealthier groups and vice versa. The equation of HI is as follows:
Where is the needs-based variables, is the marginal effects (dy/dx) of , is the means of , is the concentration index of .
The method of decomposition of the Concentration index, proposed by Wagstaff et al., was used to analyze the contribution of independent variables to the inequalities (39). A Probit regressions model was employed to calculate the effects. A positive concentration index indicates that the factor exacerbates inequality in the use of health services, and a negative concentration index indicates that it reduces inequality. The percentage contribution rate represents the factor’s contribution extent to inequity. The equation is as follows:
is the non-need variable, is the marginal effects (dy/dx) of , is the means of , , and are the concentration indexes of and , is the concentration index of the error term ε.
Ethical approval was obtained from the Institutional Review Board of Peking University (protocol code IRB00001052-11015) for the collection of human subjects data. All participants provided informed consent before data collection.
Table 1 shows the basic information about middle-aged and older persons with disabilities. A total of 9,795 individuals were included in the study. The majority of people had hearing problems, followed by vision problems and multiple disabled. The age increased during the 4 years, predominantly aged 60–74, accounting for 41.2, 48.8, 47.9, and 50.6%, respectively. Health status is predominantly poor, with more than 60% of the population suffering from chronic diseases. Age, IADL, education, child financial support, and basic medical insurance were statistically significant (p < 0.05) in the comparison of 4 year.
The utilization of health services for persons with disabilities was demonstrated in Table 2. There were statistically significant differences in outpatient, inpatient, and self-treatment service utilization between years (p < 0.05). Over the 4 years, outpatient service utilization was 23.4, 28.1, 25.4, and 20.7%, with non-utilization decreasing year on year from 87.9% (2011) to 79.0% (2015). Persons with multiple disabilities used outpatient services the most (27.1%), whereas speech impediments had the greatest non-utilization rate (87.5%). The hospitalization rate grew from 12.1% in 2011 to 27% in 2018, although the no-hospitalization rate increased from 7.9% in 2011 to 27.0% in 2018. Persons with speech impediments had the highest rates of hospitalization and no-hospitalization, followed by people with multiple disabilities. There has been a decrease in the rate of outpatient services that should have been seen but not seen, from 88.7 to 79%. The proportion of should have been hospitalized but were not has shown an increase and then decrease. Self-treatment utilization increased from 55.6% (2011) to 68.3% (2018), with intellectual disability (64.6%) having the highest prevalence, followed by multiple disabilities (63.8%).
The results of the pooled cross-section regressions were shown in Table 3, where there was an increase in the utilization of inpatient and self-treatment services from 2013 to 2018 compared to 2011 (p < 0.05). Older people utilized more inpatient and self-treatment than middle-aged people with disabilities. The inpatient service utilization was higher for male, and the self-treatment service utilization was higher for female. In the health-related factors, those with poorer self-rated health and with chronic diseases had higher utilization of the three health services, while those with ADL (OR = 1.365) and IADL (OR = 1.733) had higher utilization of inpatient services. Household expenditure level contributes to outpatient and inpatient service utilization. High levels of education facilitated inpatient and self-treatment services utilization (p < 0.05). Socially active people had 1.362 times higher utilization of outpatient services and 1.18 times higher self-treatment than non-socially active people. Having medical insurance promoted the utilization of inpatient services (OR = 2.115). After adding the disability types variable to the three types of service use, the results showed that factors have a stable effect on the utilization. With regard to the category of disability, only the results in outpatient services utilization indicated that individuals with multiple disabilities exhibited a higher utilization rate than those with physical disability (OR = 1.436). The other results had no significant effect (p > 0.05).
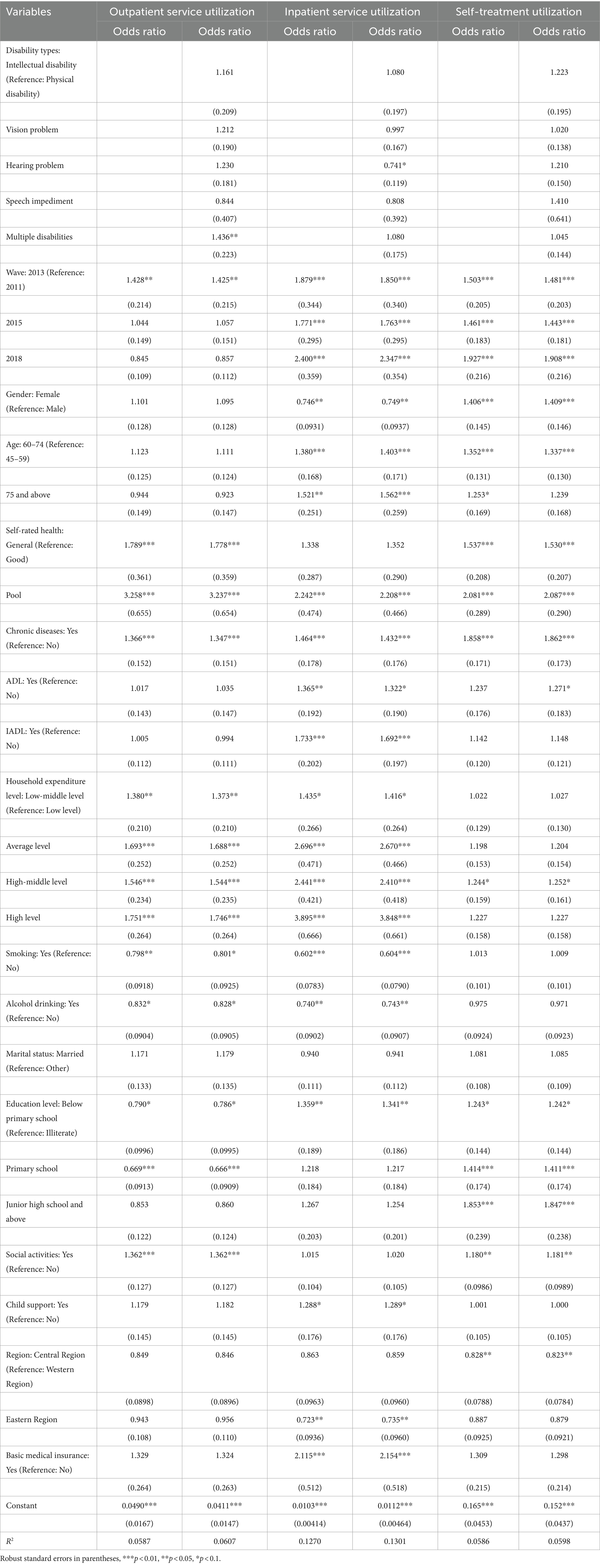
Table 3. Pooled cross-section regression of the health services utilization for persons with disabilities.
Figure 1 illustrated the CIs and the HIs for health services utilization from 2011 to 2018, with all positive results for inpatient services (p < 0.01), indicating that there were pro-rich inequalities in the services use caused by socioeconomic related characteristics. Among the three types of health service utilization, inpatient service utilization had the highest degree of inequality (0.2480 for CI in all groups), followed by outpatient service utilization (0.0882 for CI in all groups) and self-treatment (0.0487 for CI in all groups) (Figure 2). Among the annual differences, as a whole, the inpatient service utilization decreased while the use of self-treatment service utilization essentially constant. The biggest disparities of utilization of inpatient services were for physical disabilities (0.4515 for CI in 2011), and the highest disparities of utilization of self-treatment services were for intellectual disability (0.1538 for CI in 2011).
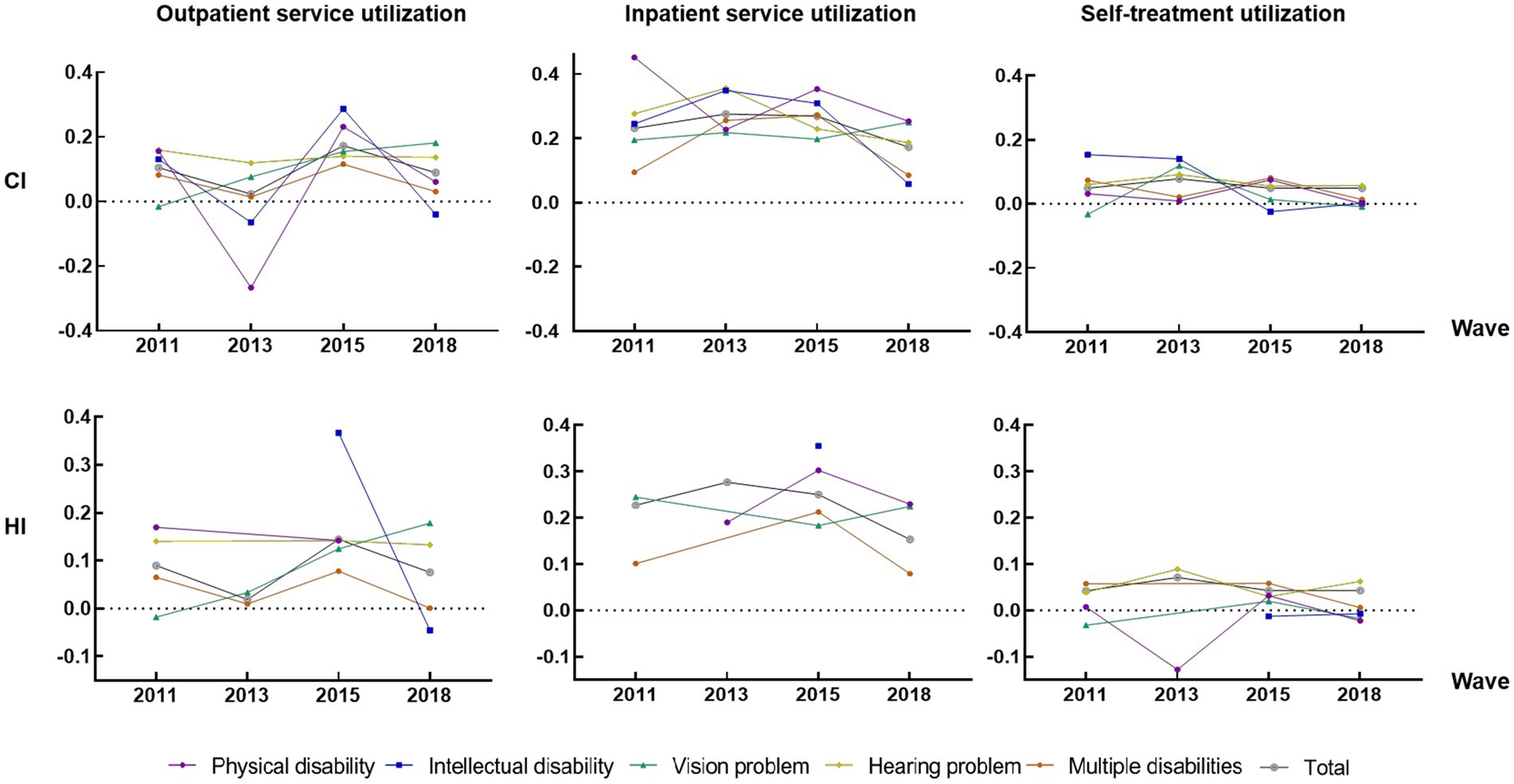
Figure 1. Inequality analysis for health service utilization by different waves and disabilities groups. HI results have some missing values due to insufficient data quantity.
Table 4 analyzed the decomposition of inequality in health service utilization for 2011 and 2018, revealing that expenditure is the most significant contribution to inequalities in health services utilization, followed by self-rated health status, contributing to pro-rich inequalities. The annual trend showed a gradual decrease in expenditure contribution, from 112.87 to 65.06% in outpatient utilization and from 74.82 to 47.73% in self-treatment service utilization. The inequalities were also influenced by chronic disease, educational level and health insurance factors.
Reducing health inequalities in health services utilization for persons with disabilities is necessary for promoting health equalities and social equality. Using data from four waves of CHARLS 2011, 2013, 2015 and 2018, this longitudinal comparative study focused on disability types to carry out comparisons of health service utilization and the socioeconomic related disparities in health service utilization among persons with disabilities and the sub-populations. This study provides a comprehensive analysis of health service utilization among the disabled population in China, including the utilization of health services for different periods and types of disabilities and measures the inequalities of service utilization. The national database is also used to reflect the utilization of health services in China, making the study more representative.
The utilization of health services by people with disabilities revealed poor initiative. The decrease in outpatient services utilization and the increase in self-treatment services utilization for the four-year comparison can be assumed that middle-aged and older adults with disabilities may passively avoid medical treatment and wait for self-healing facing minor illnesses due to financial and medical access difficulties. The proportion of people who “should have been hospitalized but were not” grew and is higher than the 10.2% reported in the 6th China Health Services Statistical Survey (CHSSS) in 2018 (40). It may indicate that there are still many disabled people in China who require hospitalization but the accessibility is inadequate. The World Report on Disability stated that the affordability of health services and transportation are two main barriers for people with disabilities to access health services (41). Related research found that telemedicine has the potential to be used to improve the health of the impaired population while being efficient and affordable (42). The advantages of telemedicine should therefore be fully exploited by enhancing the accessibility that considers the disabled special usability needs (43). At the same time, family carers (i.e., relatives or friends) play a key role in supporting people with disabilities to ensure that their basic needs are met while their rights are respected and protected, so the supportive role of the family can be fully realized (44).
Our finding revealed a pro-rich inequalities in health services utilization for persons with disabilities, meaning that persons with higher socioeconomic related status is more accessible to health services, consistent with the findings of Bin Guo et al. (45) on equality in urban and rural health service utilization and Sun et al. (46) on inequality in inpatient service utilization. The CIs and HIs in outpatient and inpatient services showed declines over the four waves comparisons and the pooled cross-section regression concluded that inpatient service utilization had increased in all years compared to 2011. This result is probably due to several effective measures implemented in recent years to ensure the use of health services for persons with disabilities, such as increasing the participation rate of basic medical insurance and fully covering the nursing care subsidy for key groups of persons with disabilities (47). Inpatient health service utilization inequality was the greatest of the three types of utilization, consistent with the findings of Sun et al. (46) that inpatient service utilization inequality was higher than outpatient service utilization. The severity of inpatient service utilization inequality has been highlighted in other studies (48, 49). Persons with disabilities face more health and socioeconomic risks than non-disabled people. Since the inpatient costs are much higher than outpatient and self-treatment, low-income residents are more likely to be forced into poverty (49). To ensure that patients with serious impaired and the dirt-poor have access to essential medical services, medical assistance for persons with disabilities should be upgraded and made available to key populations.
Disparities in different disability groups should also be considered. Severe inequalities were found in outpatient and self-treatment among people with intellectual disabilities. On the one hand, patients with intellectual impairments may only interact with clinicians using simple phrases, leading to misdiagnosis and delays in receiving the best care. On the other hand, there are issues with prejudice and unfavorable attitudes of doctors toward the disabled (1). Physical disabilities experience access disparities in inpatient service, which may be related to the significant demand for rehabilitation during hospitalization because of the patients’ restricted physical function and activity (50). The lengthy rehabilitation process and high rehabilitation expense considerably raise the financial burden on families of people with disabilities. Therefore, it is crucial to refine the provision of basic medical services for the individual demands of varied disabilities. Furthermore, the provision of disability-friendly health facilities and equipment would contribute to inclusive and accessible health care for all (51). However, as mentioned in the Disability Rights and Protection Act 2013 (52), using audio, braille and sign language interpreters when necessary is not implemented in many hospitals. Therefore, hospitals should improve basic infrastructure (e.g., toilets and ramps) and information and services (e.g., provision of sign language interpreters) (53) to enhance the access and well-being of people with disabilities in the health services utilization.
The economic factors were shown to be the dominant factor contributing to disparities for persons with disabilities. This may be because of the direct relationship between economic situations and health service affordability, which is a crucial element of equal access to health services (54). Consistent with the results in the utilization of preventive health services and outpatient inpatient services (46, 55). Health-related variables such as self-rated health and chronic disease also contribute to service utilization inequality, showing that service demand is the fundamental factor for service utilization. Disabled people are likely to have overlapping functional limitations or complex health conditions that increase their healthcare needs and costs (56). Attention should be paid to the chronic diseases of the middle-aged and older adult disabled population to prevent the significant financial burden of multiple co-morbidities on disabled people. Furthermore, the educational level and basic health insurance were the following factors to promote service utilization and contributed to pro-rich inequalities in socioeconomic variables. The education variable may be because persons with higher educational levels are more health-conscious and have advantages in health information access, which increases the use of health services (57, 58). In order to increase the health literacy of the disabled population and inhabitants, health education for those with low educational attainment should be a priority. Efforts to assimilate e-health literacy are important to improve the capacity for adaptation to a digital society. On this basis, the digital tools in the healthcare system need to be ensured to be suitable for persons with disabilities (59). The results of the basic health insurance factor are consistent with prior studies (60), which demonstrated that the increase in medical insurance coverage for hospitalization service expenditure promotes the utilization of health services. Consequently, a multi-level medical security system for disabled people should be established through the triple system of basic medical insurance, critical diseases insurance and medical assistance so as to improve the medical security capacity for persons with disabilities (61).
Our study also has several limitations. Firstly, reporting bias is unavoidable in the open databases used in this study based on questionnaires. Secondly, the method of concentrated index decomposition is descriptive analysis. The causal analysis and results should be interpreted with caution. Thirdly, the selection of variables was limited by the open databases. Therefore some variables that are theoretically more relevant to the utilization of services for persons with disabilities were not included. Despite the above limitations, facing the population aging with disabilities and the high social disability risk in China, attention should be paid to research on the health economics evaluation related to the utilization of services for the disabled and its subgroups.
Our results indicated that the persons with disabilities are less likely to take the initiative to use health services. The pro-rich inequalities existed in health services utilization from 2011 to 2018 waves, with the disparities in inpatient services being the largest, although the inequalities decreased over time. The decomposition analysis revealed that the economy was the dominant factor exacerbating inequalities. Policies should promote medical assistance for key disabled people, improve the capacity of the primary hospital to provide medical and rehabilitation services to people with disabilities and support accessible facilities and services for different disability groups.
Publicly available datasets were analyzed in this study. Data were obtained from the China Health and Retirement Longitudinal Study and are available at https://charls.pku.edu.cn/, with the permission of Peking University of China. The data underlying this article will be shared on reasonable request to the corresponding author.
The studies involving humans were approved by the Institutional Review Board of Peking University (protocol code IRB00001052-11015). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
SJ: Writing – review & editing, Writing – original draft. RF: Writing – review & editing, Writing – original draft. JW: Writing – review & editing. JL: Writing – review & editing. SZ: Writing – review & editing. MA: Writing – review & editing. SC: Writing – review & editing. DQ: Writing – review & editing, Writing – original draft, Supervision, Funding acquisition, Conceptualization.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China (Grant number: 71874085).
The authors thank all participants of the National School of Development workshop in Peking University for their support and free access to the China Health and Retirement Longitudinal Study (CHARLS).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CHARLS, China Health and Retirement Longitudinal Study; ADL, Activities of daily living; IADL, Instrumental activities of daily living; CI, Concentration index; HI, Horizontal inequity index; OR, Odds ratio.
1. Magnusson, L, Kebbie, I, and Jerwanska, V. Access to health and rehabilitation services for persons with disabilities in Sierra Leone – focus group discussions with stakeholders. BMC Health Serv Res. (2022) 22:1003–3. doi: 10.1186/s12913-022-08366-8
2. World Health Organization . Global report on health equity for persons with disabilities. (2022). Available at: https://www.who.int/publications/i/item/9789240063600.
3. Youran, S, Kang, L, and Xianchun, B. Of blue book for the handicapped: the developmental report for the status of Chinese handicapped 2019. Modern Special Educ. (2020) 02:55–9. doi: 10.18356/9789210564991c009
4. Jeon, B, Kwon, S, and Kim, H. Health care utilization by people with disabilities: a longitudinal analysis of the Korea welfare panel study (KoWePS). Disabil Health J. (2015) 8:353–62. doi: 10.1016/j.dhjo.2015.01.001
5. Reichard, APD, Stolzle, HMPH, and Fox, MHSD. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disabil Health J. (2011) 4:59–67. doi: 10.1016/j.dhjo.2010.05.003
6. Havercamp, SM, and Scott, HM. National health surveillance of adults with disabilities, adults with intellectual and developmental disabilities, and adults with no disabilities. Disabil Health J. (2015) 8:165–72. doi: 10.1016/j.dhjo.2014.11.002
7. Mitra, M, Long-Bellil, L, Moura, I, Miles, A, and Kaye, HS. Advancing health equity and reducing health disparities for people with disabilities in the United States. Health Affair. (2022) 41:1379–86. doi: 10.1377/hlthaff.2022.00499
8. Xiao, J, Shi, Z, and Fang, Y. Association between disability trajectory and health care service utilization among older adults in China. J Am Med Dir Assoc. (2021) 22:2169–2176.e4. doi: 10.1016/j.jamda.2020.12.041
9. Nguyen, L, Lee, JT, Hulse, ESG, Hoang, MV, and Le, DB. Health service utilization and out-of-pocket expenditure associated with the continuum of disability in Vietnam. Env Res Pub He. (2021) 18:5657. doi: 10.3390/ijerph18115657
10. Pumkam, CPD, Probst, JCPD, Bennett, KJPD, Hardin, JPD, and Xirasagar, SPD. Health care expenditures among working-age adults with physical disabilities: variations by disability spans. Disabil Health J. (2013) 6:287–96. doi: 10.1016/j.dhjo.2013.03.002
11. Zhu, L, Peng, M, Jiang, L, and Wang, Z. Inequality of opportunity in health service utilization among middle-aged and elderly community-dwelling adults in China. Arch Public Health. (2023) 81:13. doi: 10.1186/s13690-022-01010-1
12. Drum, CE, Horner-Johnson, W, and Walsh, ES. Construction and validation of the outpatient health care usability profile (OHCUP). Disabil Health J. (2012) 5:292–7. doi: 10.1016/j.dhjo.2012.08.001
13. Guo, Q, Sun, Y, Fan, M, and Li, Z. What is the degree of social disability risk in China under the background of the aging population? Social disability risk measurement index system design and evaluation research based on China. Front Public Health. (2023) 11:1087276–6. doi: 10.3389/fpubh.2023.1087276
14. Australian Government Department of Social Services . Australia’s Disability Strategy 2021–2031. (2022). Available at: https://www.disabilitygateway.gov.au/document/3106.
15. Brazil . Portaria Ministerial N° 1060; Ministério da Saúde: Brasília, Brazil, 2002. (2002). Available at: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2002/prt1060_05_06_2002.html.
16. Santos, CC, Pedde, V, Kuhn Junior, N, and Renner, JS. Política pública, deficiência física, concessão de órteses, próteses e meios de locomoção no rio grande do sul: período pré/pós plano viver sem limites. Interfaces Científicas Saúde E Ambiente. (2017) 5:17–26. doi: 10.17564/2316-3798.2017v5n3p17-26
17. The Opinions on Establishing a Comprehensive System of Living Subsidies for Disabled Persons with Difficulties and Nursing Subsidies for Severe Disabled Persons . (2023). Available at: https://www.gov.cn/zhengce/content/2015-09/25/content_10181.htm.
18. Guidance of the National Medical Insurance Administration and the Ministry of Finance on expanding the pilot of long-term care insurance system . (2023). Available at: http://www.nhsa.gov.cn/art/2020/9/16/art_37_3586.html.
19. Maltais, J, Morin, D, and Tassé, MJ. Healthcare services utilization among people with intellectual disability and comparison with the general population. J Appl Res Intellect. (2020) 33:552–64. doi: 10.1111/jar.12698
20. Jean-Francois, T, and Cecile, B. Measuring equity in disability and healthcare utilization in Afghanistan. Med Confl Surviv. (2012) 28:219–46. doi: 10.1080/13623699.2012.714651
21. Ma, L, Li, Z, Tang, Z, Sun, F, Diao, L, Li, J, et al. Prevalence and socio-demographic characteristics of disability in older adults in China: findings from China comprehensive geriatric assessment study. Arch Gerontol Geriat. (2017) 73:199–203. doi: 10.1016/j.archger.2017.07.029
22. Qiao, R, Jia, S, Zhao, W, Xia, X, Su, Q, Hou, L, et al. Prevalence and correlates of disability among urban–rural older adults in Southwest China: a large, population-based study. BMC Geriatr. (2022) 22:10.1186/s12877-022-03193-2. doi: 10.1186/s12877-022-03193-2
23. Zhang, T, Liu, C, Lu, B, and Wang, X. Changes of inequality in functional disability of older populations in China from 2008 to 2018: a decomposition analysis. BMC Geriatr. (2022) 22:308. doi: 10.1186/s12877-022-02987-8
24. Guo, C, Li, N, Chen, G, and Zheng, X. Mental health service utilization and its associated social factors among elderly people with a mental disability in China: a national population-based survey. Scand J Public Healt. (2019) 47:215–20. doi: 10.1177/1403494817722705
25. Guo, C, Chang, J, Zheng, X, and Wang, L. Utilization rate of healthcare Service of the Elderly with disabilities - China, 1987-2014. China Cdc Weekly. (2020) 2:516–9. doi: 10.46234/ccdcw2020.140
26. Zhao, X, and Wang, H. Disparities in unmet health service needs among people with disabilities in China. Int J Qual Health C. (2021) 33:mzab136. doi: 10.1093/intqhc/mzab136
27. Guo, J, Li, J, Huang, K, Huang, N, and Feng, XL. Socio-economic inequalities in the chronic diseases management among Chinese adults aged 45 years and above: a cross sectional study. Arch Public Health. (2021) 79:157. doi: 10.1186/s13690-021-00678-1
28. Fan, X, Su, M, Zhao, Y, Si, Y, and Zhou, Z. Trends in equity of inpatient health service utilization for the middle-aged and elderly in China: based on longitudinal data from 2011 to 2018. BMC Public Health. (2021) 21:1162. doi: 10.1186/s12889-021-11203-y
29. Zhao, Y, Hu, Y, Smith, JP, Strauss, J, and Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
30. The World Bank . Measuring and Explaining Inequity in Health Service Delivery. (2006). Available at: https://www.worldbank.org/en/search?q=Measuring+inequity+in+health+service+delivery¤tTab=1.
31. Xu, J, Tian, G, Sun, J, Liu, J, Chen, F, Shi, Q, et al. Horizontal inequity trends of health care utilization in rural China after the medicine and healthcare system reform: based on longitudinal data from 2010 to 2018. Int J Equity Health. (2023) 22:90. doi: 10.1186/s12939-023-01908-4
32. Zhang, X, Ning, N, Zhou, H, Shan, L, Hao, Y, Jiao, M, et al. Inequity in health services utilization in economically underdeveloped regions of Northeast China. Front Public Health. (2022) 10:850157. doi: 10.3389/fpubh.2022.850157
33. Pan, ZLT. Health differentiation, health inequality and its influencing factors: an empirical analysis based on the difference of health care expenditure level of the disabled in Hunan Province. Study Practice. (2015) 4:125–34. doi: 10.19624/j.cnki.cn42-1005/c.2015.04.015
34. Zhang, H, Fu, Y, Chen, M, and Si, L. Socioeconomic inequality in health care use among cancer patients in China: evidence from the China health and retirement longitudinal study. Front Public Health. (2022) 10:942911. doi: 10.3389/fpubh.2022.942911
35. Tu, S. Socioeconomic differences in the prevalence and control of hypertension in the rural elderly population in Shandong Province: [dissertation]. China: Shandong University (2009).
36. Wagstaff, A, Paci, P, and van Doorslaer, E. On the measurement of inequalities in health. Soc Sci Med. (1991) 33:545–57. doi: 10.1016/0277-9536(91)90212-U
37. Lai, S, Shen, C, Yang, X, Zhang, X, Xu, Y, Li, Q, et al. Socioeconomic inequalities in the prevalence of chronic diseases and preventive care among adults aged 45 and older in Shaanxi Province, China. BMC Public Health. (2019) 19:1460. doi: 10.1186/s12889-019-7835-5
38. Lera, J, Pascual-Sáez, M, and Cantarero-Prieto, D. Socioeconomic inequality in the use of long-term care among European older adults: an empirical approach using the SHARE survey. Env Res Pub He. (2020) 18:20. doi: 10.3390/ijerph18010020
39. Wagstaff, A, van Doorslaer, E, and Watanabe, N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J Econ. (2003) 112:207–23. doi: 10.1016/S0304-4076(02)00161-6
40. Yao, C. Improving the accessibility of the medical and health services for the residents. Health Rep. (2021). doi: 10.28415/n.cnki.njika.2021.000428
41. World Health Organization . World report on disability. (2011). Available at: https://www.who.int/publications/i/item/9789241564182
42. van Kessel, R, Hrzic, R, O'Nuallain, E, Weir, E, Wong, B, Anderson, M, et al. Digital health paradox: international policy perspectives to address increased health inequalities for people living with disabilities. J Med Internet Res. (2022) 24:e33819. doi: 10.2196/33819
43. Valdez, RS, Rogers, CC, Claypool, H, Trieshmann, L, Frye, O, Wellbeloved-Stone, C, et al. Ensuring full participation of people with disabilities in an era of telehealth. J Am Med Inform Assoc. (2021) 28:389–92. doi: 10.1093/jamia/ocaa297
44. Flood, B. Safety of people with intellectual disabilities in hospital. What can the hospital pharmacist do to improve quality of care? Pharmacy. (2017) 5:44. doi: 10.3390/pharmacy5030044
45. Guo, B, Xie, X, Wu, Q, Zhang, X, Cheng, H, Tao, S, et al. Inequality in the health services utilization in rural and urban China. Medicine. (2020) 99:e18625. doi: 10.1097/MD.0000000000018625
46. Sun, X, Zhang, H, Hu, X, Gu, S, Zhen, X, Gu, Y, et al. Measurement and analysis of equity in health: a case study conducted in Zhejiang Province, China. Int J Equity Health. (2018) 17:36. doi: 10.1186/s12939-018-0746-8
47. Chen, G, Tan, W, Liu, S, Kang, N, and Jin, X. Mid-term assessment of the implementation of the 13th five-year plan - third-party assessment. Chinese J Rehabil Med. (2020) 35:1025–31. doi: 10.3969/j.issn.1001-1242.2020.09.001
48. Li, C, Dou, L, Wang, H, Jing, S, and Yin, A. Horizontal inequity in health care utilization among the middle-aged and elderly in China. Int J Env Res Pub He. (2017) 14:10.3390/ijerph14080842. doi: 10.3390/ijerph14080842
49. Fu, X, Wang, L, Sun, C, Wang, D, He, J, Tang, Q, et al. Inequity in inpatient services utilization: a longitudinal comparative analysis of middle-aged and elderly patients with the chronic non-communicable diseases in China. Int J Equity Health. (2020) 19:6. doi: 10.1186/s12939-019-1117-9
50. Tian, H, Qiu, Z, Li, X, Ma, H, Sheng, W, Du, R, et al. A logistic regression analysis of rehabilitation needs and development of rehabilitation services. Rehabil Theory Practice China. (2020) 26:508–12. doi: 10.3969/j.issn.1006-9771.2020.05.003
51. Dassah, E, Aldersey, HM, McColl, MA, and Davison, C. Health care providers’ and persons with disabilities’ recommendations for improving access to primary health care services in rural northern Ghana: a qualitative study. PLoS One. (2022) 17:e0274163. doi: 10.1371/journal.pone.0274163
52. Torsha, N, Rahman, FN, Hossain, MS, Chowdhury, HA, Kim, M, Rahman, S, et al. Disability-friendly healthcare at public health facilities in Bangladesh: a mixed-method study to explore the existing situation. BMC Health Serv Res. (2022) 22:1178. doi: 10.1186/s12913-022-08538-6
53. Mac-Seing, M, Zinszer, K, Eryong, B, Ajok, E, Ferlatte, O, and Zarowsky, C. The intersectional jeopardy of disability, gender and sexual and reproductive health: experiences and recommendations of women and men with disabilities in northern Uganda. Sex Reprod Hlth Matt. (2020) 28:1772654. doi: 10.1080/26410397.2020.1772654
54. Kruk, ME, and Freedman, LP. Assessing health system performance in developing countries: a review of the literature. Health Policy. (2007) 85:263–76. doi: 10.1016/j.healthpol.2007.09.003
55. Xu, Y, Zhang, T, and Wang, D. Changes in inequality in utilization of preventive care services: evidence on China’s 2009 and 2015 health system reform. Int J Equity Health. (2019) 18:172–2. doi: 10.1186/s12939-019-1078-z
56. Dejong, G, Palsbo, SE, and Beatty, PW. The organization and financing of health services for persons with disabilities. Milbank Q. (2002) 80:261–301. doi: 10.1111/1468-0009.t01-1-00004
57. Costa, C, and Santana, P. Trends of amenable deaths due to healthcare within the European Union countries. Exploring the association with the economic crisis and education. SSM Popul Hlth. (2021) 16:100982. doi: 10.1016/j.ssmph.2021.100982
58. Rotarou, ES, and Sakellariou, D. Determinants of utilisation rates of preventive health services: evidence from Chile. BMC Public Health. (2018) 18:839. doi: 10.1186/s12889-018-5763-4
59. Paige, SR, Stellefson, M, Krieger, JL, Anderson-Lewis, C, Cheong, J, and Stopka, C. Proposing a transactional model of eHealth literacy: concept analysis. J Med Internet Res. (2018) 20:e10175. doi: 10.2196/10175
60. Fan, X, Su, M, Si, Y, Zhao, Y, and Zhou, Z. The benefits of an integrated social medical insurance for health services utilization in rural China: evidence from the China health and retirement longitudinal study. Int J Equity Health. (2021) 20:126. doi: 10.1186/s12939-021-01457-8
Keywords: persons with disabilities, health service utilization, inequality, concentration index, longitudinal comparative study
Citation: Jin S, Fa R, Wu J, Lin J, Zhang S, Ali M, Chen S and Qian D (2024) Inequalities changes in health services utilization among middle-aged and older adult disabled people in China: based on CHARLS 2011–2018. Front. Public Health. 12:1434106. doi: 10.3389/fpubh.2024.1434106
Received: 17 May 2024; Accepted: 16 September 2024;
Published: 01 October 2024.
Edited by:
Victor Adekanmbi, University of Texas Medical Branch at Galveston, United StatesReviewed by:
Jiefei Wang, University of Texas Medical Branch at Galveston, United StatesCopyright © 2024 Jin, Fa, Wu, Lin, Zhang, Ali, Chen and Qian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongfu Qian, ZHFpYW5AbmptdS5lZHUuY24=; Shaofan Chen, c2hhb2Zhbi5jaGVuQG5qbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.