- 1Department of Gynecology, The Eastern Area of Dongzhimen Hospital of Beijing University of Chinese Medicine, Beijing, China
- 2Department of TCM Gynecology, China-Japan Friendship Hospital, Beijing, China
- 3Department of Gynecology, Beijing Shijingshan District Hospital of Traditional Chinese Medicine, Beijing, China
- 4Department of Gynecology, Beijing Xicheng Guangwai Hospital, Beijing, China
Background: This study aimed to examine the knowledge, attitude, and practice (KAP) of women in Beijing regarding cervical precancerous lesions.
Methods: This web-based, cross-sectional study included women at Dongzhimen Hospital of Beijing University of Chinese Medicine between March 13, 2024 and April 9, 2024. A self-administered questionnaire was developed to collect participants’ demographic information and KAP scores toward cervical precancerous lesions.
Results: The study included 951 valid questionnaires, with a mean age of 40.0 years. The mean knowledge, attitude, and practice scores were 12.55 ± 6.23 (possible range: 0–26), 50.66 ± 7.48 (possible range: 13–65), and 26.13 ± 4.98 (possible range: 7–35), respectively. The knowledge score (OR = 1.071, 95%CI: 1.040–1.103, p < 0.001), currently married (OR = 0.548, 95%CI: 0.304–0.985, p = 0.045), and with a history of HPV infection (OR = 2.302, 95%CI: 1.062–4.990, p = 0.035) were independently associated with the attitude score. The knowledge score (OR = 1.155, 95%CI: 1.119–1.192, p < 0.001), monthly income >20,000 (OR = 2.793, 95%CI: 1.249–6.248, p = 0.012), a history of HPV infection (OR = 0.380, 95%CI: 0.222–0.650, p < 0.001), unknown HPV infection status (OR = 0.289, OR = 0.177–0.473, p < 0.001), vaccinated against HPV (OR = 1.752, 95%CI: 1.221–2.514, p = 0.002), giving birth to one child (OR = 1.991, 95%CI: 1.186–3.341, p = 0.009), and giving birth to two or more children (OR = 2.160, 95%CI: 1.240–3.763, p = 0.007) were independently associated with the practice score. The structured equation model showed that knowledge directly influenced attitude (β = 0.237, p = 0.004) and practice (β = 0.490, p = 0.010). Attitude directly influenced practice (β = 0.193, p = 0.009).
Conclusion: This study revealed inadequate knowledge, moderate attitude, and practice toward cervical precancerous lesions among women in Beijing. Educational interventions should be developed to enhance knowledge in this regard.
Background
Cervical cancer (CC) is a malignancy originating in the transformation zone of the cervix, most commonly in squamous cells (1). CC is the second most common cancer in women worldwide (estimated 661,021 new cases in 2022, or 3.3% of all cancers) and the third most common cause of cancer-related mortality in women (estimated 348,189 related deaths in 2022, or 3.6% of all cancer-related deaths) (49). Notably, CC is largely preventable. Over the last 30 years, the incidence and mortality of CC in high-income countries have decreased by more than 50%, a trend attributed to the implementation of formal screening programs (2, 3). CC is mainly prevented by screening for and treating cervical precancerous lesions (4). Cervical precancerous lesions are abnormal cells that can progress to CC without intervention and include cervical intraepithelial neoplasia grade 2–3 (CIN2-3) and adenocarcinoma in situ (AIS) (4).
Since CIN constitutes a continuum of progression, detecting and managing the lesions as soon as possible is conducive to improving prognosis (5–7). Although radical surgery can be necessary for advanced CC, early CC can be treated using fertility-sparing options (8, 9), such as laparoscopic-assisted vaginal trachelectomy. The collaboration of the women is essential for screening and managing cervical lesions. Indeed, sexually active women should undergo cervical screening regularly, request HPV vaccination, and follow their physicians’ advice (10, 11). Hence, proper knowledge and attitude of the women are prerequisites for the proper practice of CC prevention, including regarding precancerous lesions.
Knowledge, attitude, and practice (KAP) survey is a tool that provides quantitative and qualitative data about the gaps, misconceptions, and misunderstandings regarding a specific subject in a specific population (12, 13). Previous studies revealed highly variable KAP levels regarding cervical lesions and CC screening among different woman populations around the globe (14–20). A previous study examined the KAP toward CC screening among an ethnic minority in China (21), but no study examined the KAP toward cervical precancerous lesions in Beijing (China). In particular, the Beijing Municipal Health Commission issued the “Implementation Plan for Accelerating the Elimination of Cervical Cancer in Beijing (2023–2030)” in September 2023, stating that free cervical cancer screenings will progressively extend coverage to the entire permanent population of the whole city (22). Against this backdrop, there is an urgent need to investigate the current awareness among women in Beijing regarding cervical precancerous lesions.
Therefore, the objective of this study was to explore the KAP of Chinese women in Beijing regarding cervical precancerous lesions, with the aim of identifying critical areas where educational interventions are urgently required to improve awareness and preventive behaviors within the target population.
Methods
Study design and participants
This cross-sectional study included female inpatients, outpatients, and medical workers at the Dongzhimen Hospital of Beijing University of Chinese Medicine between March 13, 2024, and April 9, 2024. Women aged over 18 years, with clear consciousness, and capable of independently responding to the questionnaire were included in the study. No exclusion criteria were applied in this research. The research protocol was approved by the Ethics Committee of Dongzhimen Hospital Affiliated with the Beijing University of Chinese, under the approval number 2024DZMEC-093-02. All participants provided written informed consent before completing the questionnaire.
Questionnaire
The design of the questionnaire was based on the 2021 WHO Guidelines: Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention (Second Edition) (23) and the related literature (6, 11, 24). Two gynecology experts, each with over 20 years of experience, rigorously reviewed the questionnaire items to ensure their accuracy and relevance, leading to the removal of any items deemed incorrect or inappropriate, thereby enhancing content validity. A total of 46 valid questionnaires were collected during the pre-survey, revealing a Cronbach’s α coefficient of 0.868, with values of 0.906, 0.700, and 0.761 for the knowledge, attitude, and practice sections, respectively, suggesting good internal consistency. During the pilot study, participants were encouraged to provide feedback on any items they found confusing or unclear, and no items were reported, thus confirming face validity. Finally, a confirmatory factor analysis was conducted, which demonstrated good model fit with the following indices: CFI (Comparative Fit Index) = 0.896, IFI (Incremental Fit Index) = 0.897, TLI (Tucker-Lewis Index) = 0.885, RMSEA (Root Mean Square Error of Approximation) = 0.060, and CMIN/DF (Chi-square value/degrees of freedom) = 4.285.
The final questionnaire was in Chinese and comprised four sections: (1) demographic information, including age, height, body weight, education level, HPV vaccination history, and sexual activity history, (2) knowledge dimension, (3) attitude dimension, and (4) practice dimension. The Body Mass Index (BMI) is calculated as the weight in kilograms divided by the square of the height in meters, with classifications of <18.5 kg/m2 as underweight, 18.5–23.9 kg/m2 as normal weight, 24–27.9 kg/m2 as overweight, and ≥ 28 kg/m2 as obesity (25). The knowledge (K) dimension included 13 questions, with scores ranging from 0 to 26, where 2 points were assigned for a “very familiar” response, 1 point for “heard about,” and 0 points for “unclear.” The knowledge dimension of this study encompassed a comprehensive understanding of cervical cancer, including its definition (items 1), risk factors (items 2–3), early detection and screening (items 4–7), treatment options (items 8–10), and HPV vaccination (items 11–13). The attitude (A) dimension consisted of 13 questions using a 5-point Likert scale, ranging from “strongly agree” (5 points) to “strongly disagree” (1 point), with total scores ranging from 13 to 65 points. The practice dimension included nine questions about practice frequency, rated from “never” to “always” and assigned values from 1 to 5. Items P8 and P9 did not show positive or negative attitude tendencies, and hence, a descriptive analysis of this question was performed, and the possible score range of practice dimension was 7–35 points.
Questionnaire distribution and quality control
An online questionnaire was created using the Sojump website,1 and a QR code was generated for data collection via WeChat. The participants scanned the QR code to log in and complete the questionnaire. To ensure the quality and completeness of the questionnaire, all items were mandatory. If participants encountered any problem in answering, members of the research group were responsible for interpreting and solving the problem. After questionnaire collection, data quality checks were conducted, and questionnaires with logical errors or repeated pattern choices were considered invalid and excluded.
Statistical analysis
The minimal sample size was estimated based on 10 times the number of demographic information and KAP items based on the sample size estimation methods for surveys (26). Hence, the minimal sample size was 550. When accounting for a 20% invalid questionnaire rate, the minimal sample size was 660.
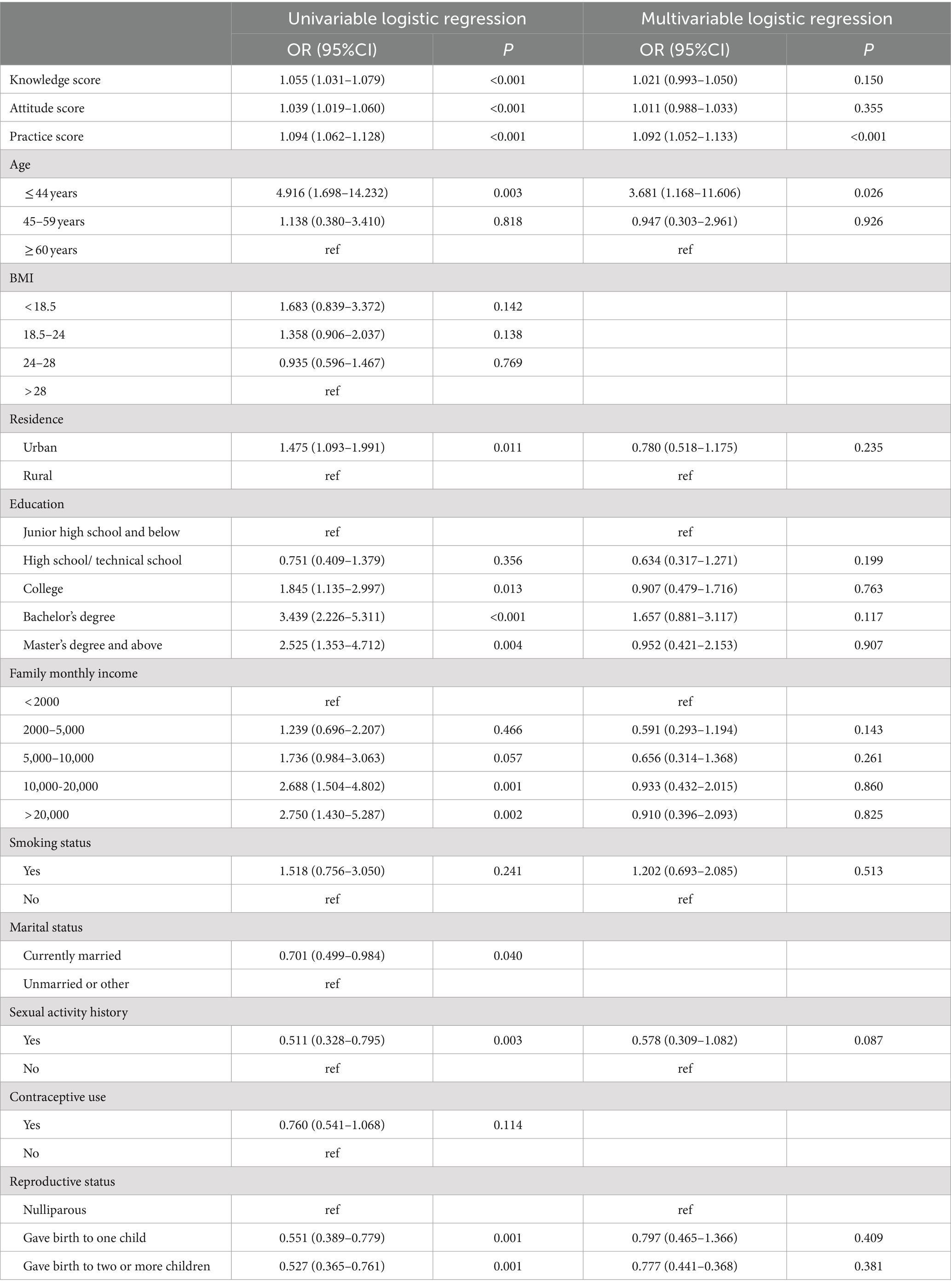
SPSS 26.0 (IBM, Armonk, NY, United States) and AMOS 24.0 (IBM, Armonk, NY, USA) were used for the analysis. The continuous variables were described as means ± standard deviations and analyzed using Student’s t-test or ANOVA. The categorical variables were described as n (%) and analyzed using the chi-square test. Pearson correlation was used to analyze the correlation among the KAP scores. Univariable and multivariable logistic regression analyses were used to analyze the attitude and practice scores using 70% of the total score as the cutoff value. Univariable and multivariable logistic regression analyses were also used to analyze the factors influencing HPV vaccination. The variables with p < 0.05 in the univariable analyses were included in the multivariable analyses. A structural equation modeling (SEM) analysis was conducted to test the hypotheses that (H1) knowledge directly affects attitude, (H2) knowledge directly affects practice, and (H3) knowledge indirectly affects practice through attitude. Two-sided p-values <0.05 were considered statistically significant.
Results
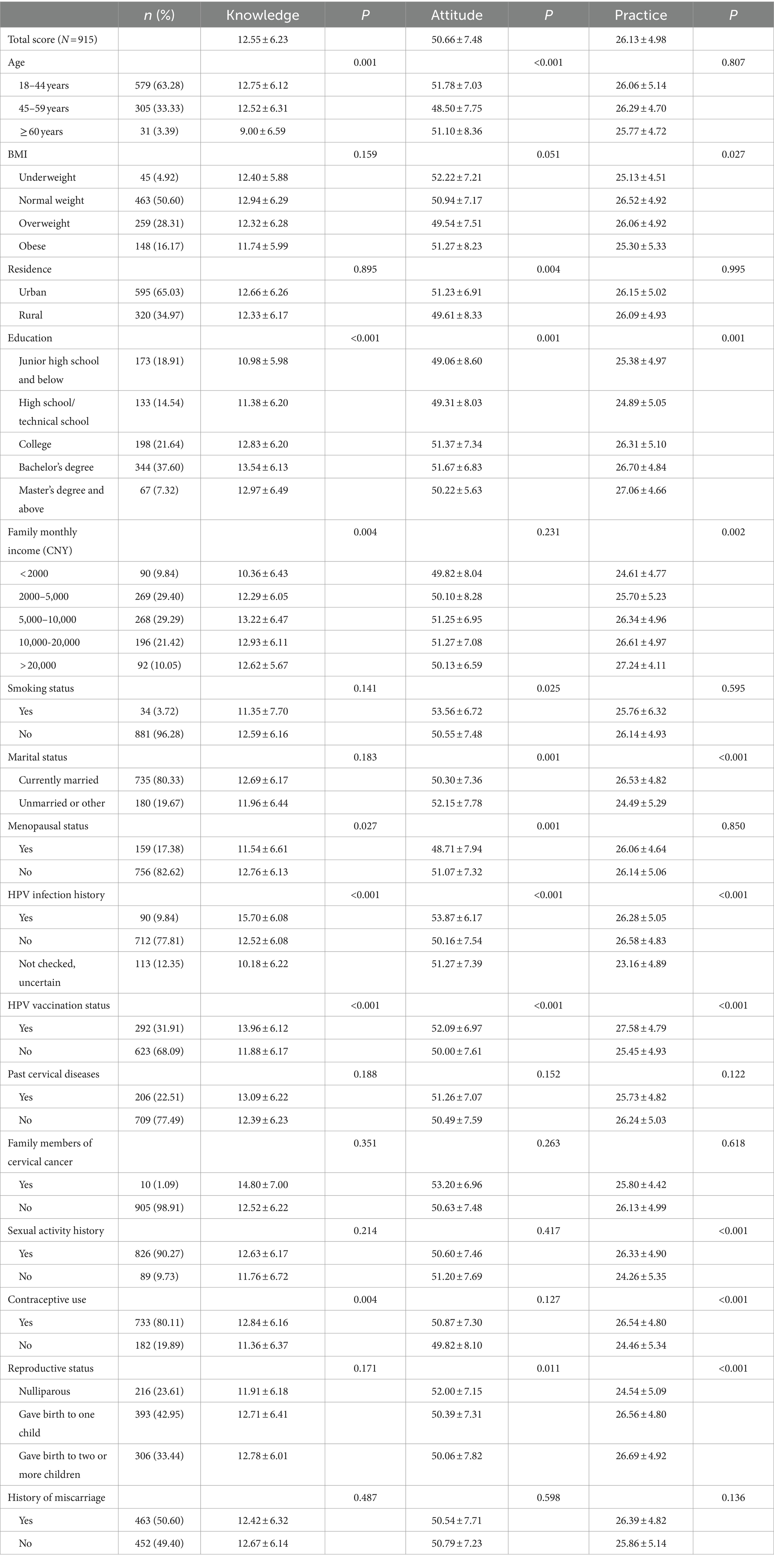
A total of 951 questionnaires were collected; 3 were missing informed consent, 1 participant reported <18 years of age, 13 had incomplete data or logical errors, and 19 where the participants chose “uncertain” for all knowledge-related questions. After the exclusions, 915 valid questionnaires were included for analysis. 18–44 age range (63.28%), maintained a normal BMI (50.60%), resided in urban areas (65.03%), were non-smokers (96.28%), currently married (80.33%), premenopausal (82.62%), not vaccinated against HPV (68.09%), and had no personal history of cervical lesions (77.49%), as outlined in Table 1.
The mean knowledge score was 12.55 ± 6.23 (possible range: 0–26). Higher knowledge scores were observed in younger women (p = 0.001), with higher education (p < 0.001), with a higher income (p = 0.004), premenopausal (p = 0.027), with a history of HPV infection (p < 0.001), vaccinated against HPV (p < 0.001), and using contraceptives (p = 0.004) (Table 1). Among all the items, the item with the largest proportion choosing “very familiar” was K7 (30.16% very familiar; Free regular cervical cancer screening was organized annually in Beijing) and K12 (34.86% very familiar; There are three types of HPV vaccines available in China—bivalent, quadrivalent, and nonavalent—all of which are approved and can be received at the individual’s expense). On the contrary, the item with the largest proportion choosing “unclear” was K4 (36.28% unclear; Patients with cervical precancerous lesions generally do not exhibit obvious symptoms.) and K9 (43.39% unclear, Low-grade cervical precancerous lesions may naturally regress, requiring only regular follow-up without the need for treatment) (Supplementary Table S1).
The mean attitude score was 50.66 ± 7.48 (possible range: 13–65). Higher attitude scores were observed in the 18–44 age group (p < 0.001), urban residents (p = 0.004), with higher education (p = 0.001), smoking (p = 0.025), unmarried (p = 0.001), premenopausal (p = 0.001), with a history of HPV infection (p < 0.001), vaccinated against HPV (p < 0.001), and nulliparous (p = 0.011) (Table 1). Supplementary Table S2 shows the distribution of the responses to the attitude items.
The mean practice score was 26.13 ± 4.98 (possible range: 7–35). Higher practice scores were observed in women with normal BMI (p = 0.027), with higher education (p = 0.001), with higher income (p = 0.002), currently married (p < 0.001), without known status of HPV infection (p < 0.001), vaccinated against HPV (p < 0.001), history of sexual activity (p < 0.001), using contraceptives (p < 0.001), and with children (p < 0.001) (Table 1). Supplementary Table S3 shows the distribution of the responses to the practice items. Notably, 41.31% of participants indicated that they “always” or “often” undergo regular screening for cervical precancerous lesions. Besides, the most common means of obtaining information about cervical precancerous lesions were social media (41.31%), hospital lectures, and physicians (19.02%), while the predominant channels of obtaining information about HPV vaccination were social media (38.36%) and advice from relatives and friends (21.64%).
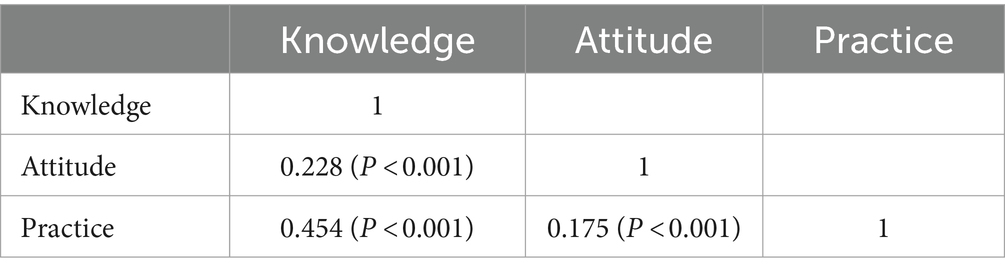
As shown in Table 2, the knowledge score was correlated to the attitude (r = 0.228, p < 0.001) and practice (r = 0.454, p < 0.001) scores. The attitude score was correlated to the practice score (r = 0.175, p < 0.001).
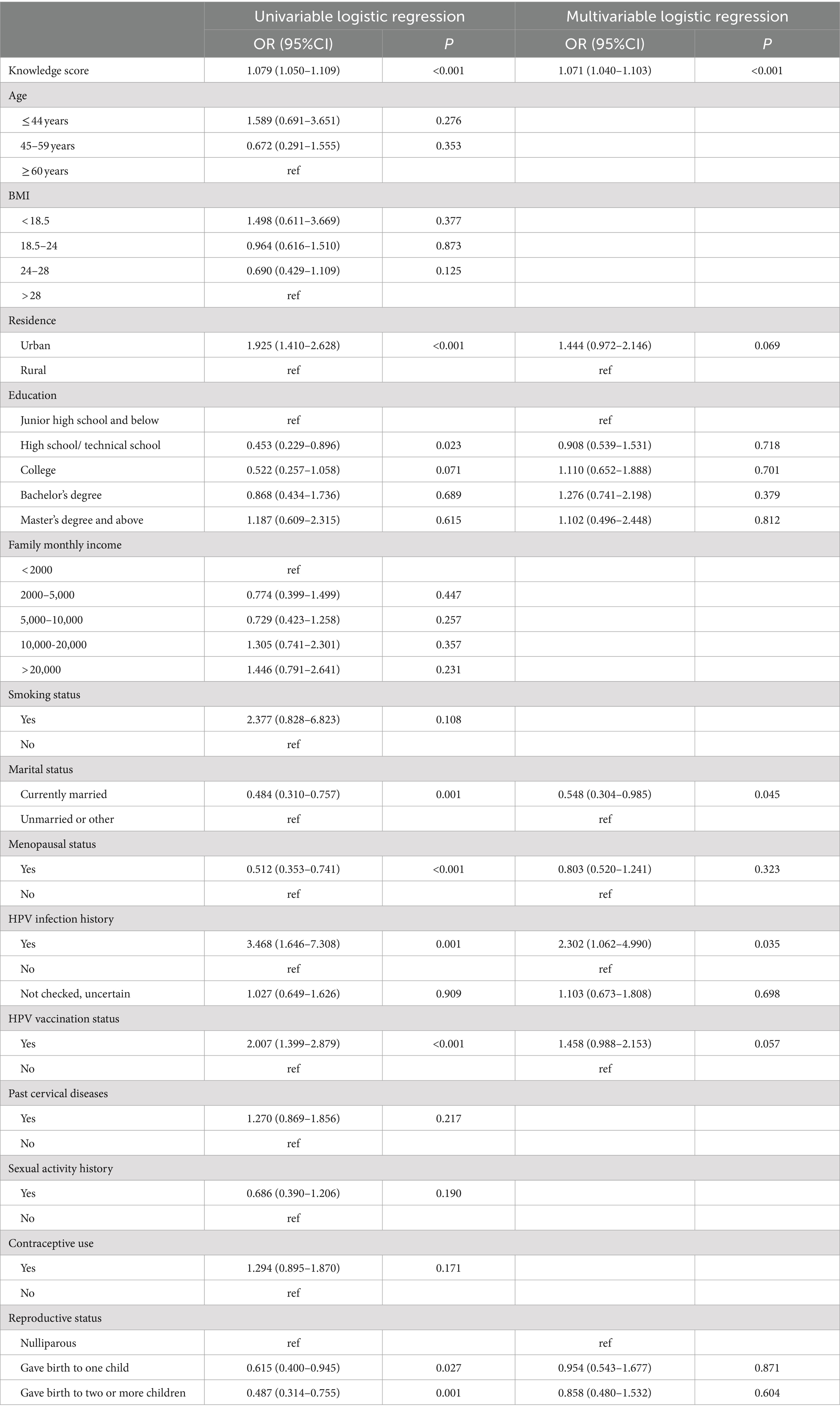
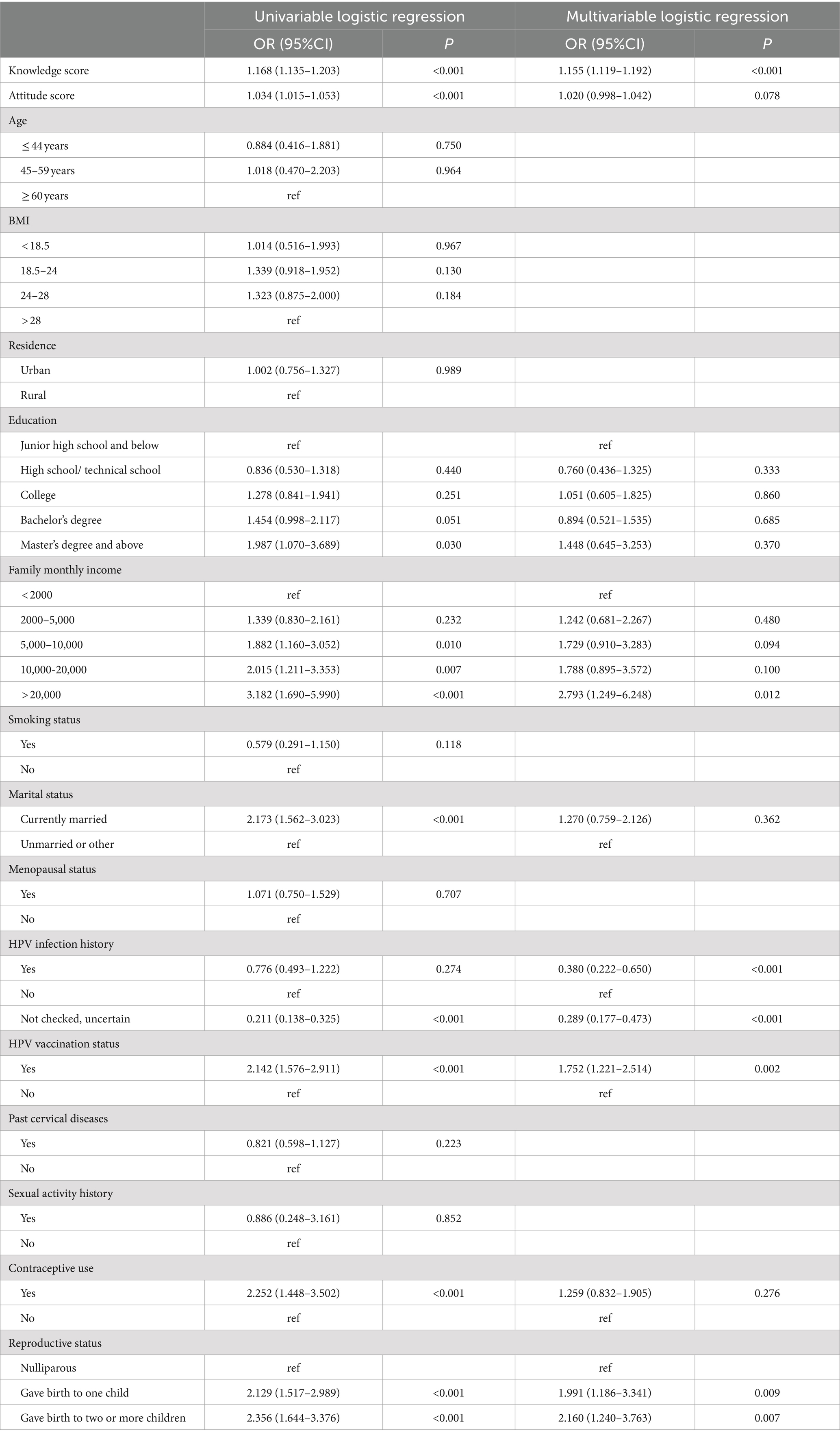
The results of multivariate regression revealed that knowledge score (OR = 1.071, 95%CI: 1.040–1.103, p < 0.001), marital status (OR = 0.548, 95%CI: 0.304–0.985, p = 0.045), and a history of HPV infection (OR = 2.302, 95%CI: 1.062–4.990, p = 0.035) were independently associated with the attitude score (Table 3). The knowledge score (OR = 1.155, 95%CI: 1.119–1.192, p < 0.001), monthly income >20,000 (OR = 2.793, 95%CI: 1.249–6.248, p = 0.012), a history of HPV infection (OR = 0.380, 95%CI: 0.222–0.650, p < 0.001), unknown HPV infection status (OR = 0.289, OR = 0.177–0.473, p < 0.001), HPV vaccination status (OR = 1.752, 95%CI: 1.221–2.514, p = 0.002), giving birth to one child (OR = 1.991, 95%CI: 1.186–3.341, p = 0.009), and giving birth to two or more children (OR = 2.160, 95%CI: 1.240–3.763, p = 0.007) were independently associated with the practice score (Table 4). The practice score (OR = 1.092, 95%CI: 1.052–1.133, p < 0.001) and age ≤ 44 years (OR = 3.681, 95%CI: 1.168–11.606, p = 0.026) were independently associated with receiving vaccination against HPV (Table 5).
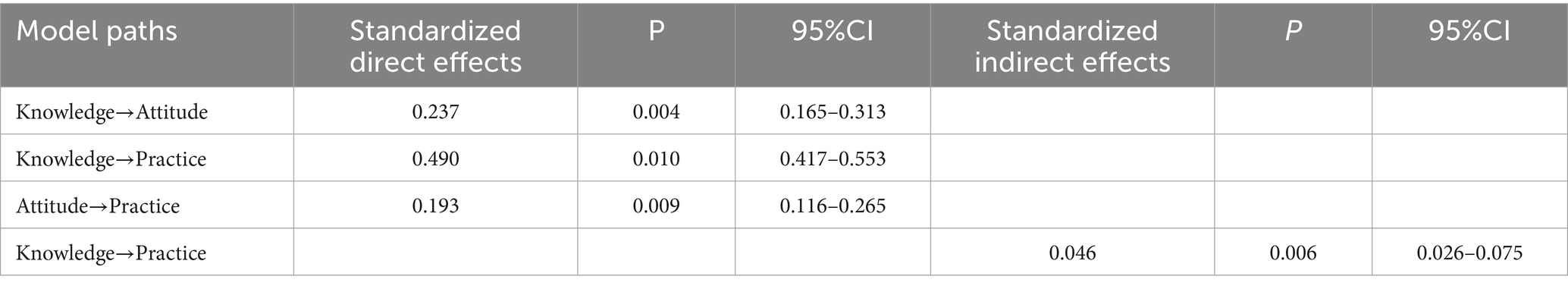
The SEM showed that knowledge directly influenced attitude (β = 0.237, p = 0.004) and practice (β = 0.490, p = 0.010). Attitude directly influenced practice (β = 0.193, p = 0.009). And knowledge indirectly influenced practice (β = 0.046, p = 0.006) (Table 6, Figure 1). Supplementary Table S4 shows that all fit indexes were good.
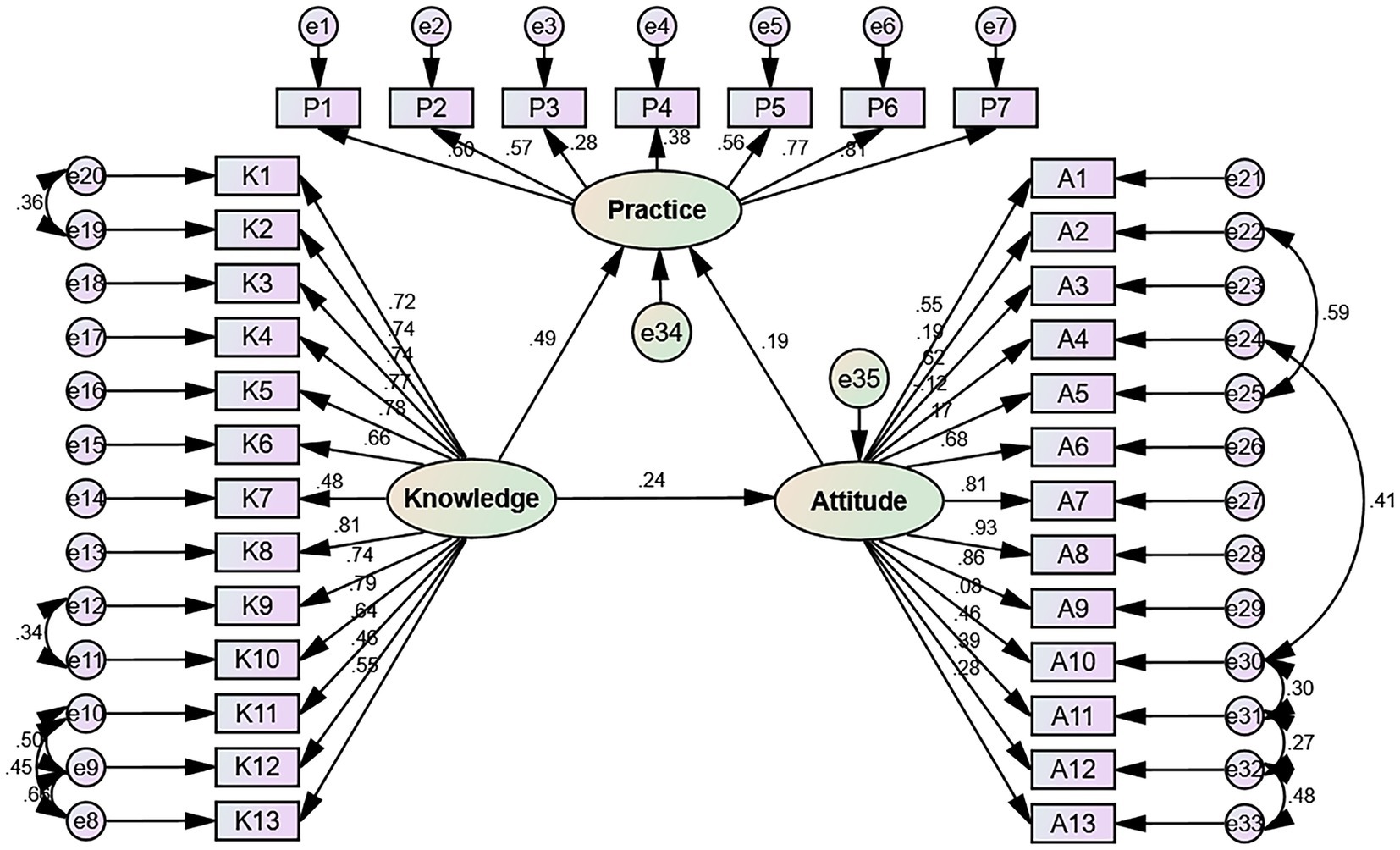
Figure 1. Structural equation model showing the associations among KAP scores. The direction of causality is indicated by single-headed arrows. The standardized path coefficients are presented alongside the arrows.
Discussion
The results of this cross-sectional study revealed women in Beijing displayed poor knowledge, moderate attitude, and moderate practice toward cervical precancerous lesions. The current rate of vaccination against HPV is low. Educational interventions should be designed to improve knowledge of cervical precancerous lesions and HPV vaccination rates.
The responsibility for being screened for cervical lesions belongs to each woman, but proper knowledge of the advantages and risks of being screened or not must be well-understood to cultivate the proper attitudes that would lead to optimal practice. Previous studies generally reported relatively poor to moderate KAP toward cervical lesions in different countries. Indeed, a study in Ethiopia reported that 61% of the participants had heard of CC, and 72% were willing to be screened, but only 2% did (14). Similar results were reported in Uganda (16), India (17, 20), and Peru (18). In another study from Ethiopia, in a study population with a 27% rate of cervical precancerous lesions, 63 and 67% of the women had good knowledge and favorable attitudes, respectively (15). On the other hand, an Italian study reported good knowledge about the Pap test, CC, and HPV infection (19). A study on the Uyghur population in China showed that women had a poor knowledge of CC, and only 6% had heard of the HPV vaccine (21). Similarly, poor knowledge of CC prevention was also observed in Shenzhen (27) and Guizhou (28). The present study was performed in the general population of women in Beijing and not specifically in minorities, but the knowledge of CC and its prevention would nevertheless require improvements. Of course, the level of economic development and education the government provides can influence the women’s KAP. The present study reported poor knowledge but moderate attitude and practice toward cervical precancerous lesions among women in Beijing. Still, the standard deviations on the mean scores were high, indicating high variability among the participants. This disparity may stem from women’s inclination to heed advice from the local community or healthcare professionals, yet there is a lack of channels or interest in deeply understanding the underlying reasons behind these recommendations. The low knowledge scores identified in this study may also originate from traditional beliefs and misconceptions about HPV infection. Indeed, many Chinese women are influenced by traditional views prevalent in the East Asian culture and tend to associate cervical lesions and HPV infection with immorality, sexual shame, and sexually transmitted diseases (29, 30). This association often leads to reluctance among these women to learn more about this condition. In addition, a significant proportion of postmenopausal women and rural women hold the erroneous belief that menopause or the absence of sexual activity precludes the risk of developing cervical lesions. This misconception leads to the refusal to acquire relevant knowledge, consequently impacting their attitudes and practices toward the disease. It is recommended that efforts to disseminate knowledge about the progression of precancerous lesions be expanded within communities, health check-up centers, and medical institutions, alongside strengthened follow-up management for high-risk groups.
The present study suggests a complex interplay of factors influencing attitudes and practices regarding cervical precancerous lesions. Indeed, the results indicated that marriage was associated with a decreased concern regarding cervical precancerous lesions, possibly due to misconceptions about sexual risk factors (31). Indeed, it is true that the risk of cervical lesions increases with the number of sexual partners, but it is crucial to acknowledge that having a single sexual partner can also be associated with an increased risk of cervical lesions if the partner carries HPV (31–33). A history of HPV infection correlated with a more positive outlook, likely due to heightened awareness of medical explanations (15). Indeed, such women are more susceptible to having received detailed explanations about HPV infections and precancerous cervical lesions. Having an unchecked HPV status and having a history of HPV infection was also associated with poor practice. Having children was also associated with a better practice toward cervical lesions. It could be related to the higher risk of cervical lesions with parity and a closer follow-up by gynecologists (15). A high income was associated with more proactive practice toward cervical lesion screening, possibly related to better access to healthcare resources (15). This study found an association between lower educational levels and unsatisfactory KAP regarding cervical precancerous lesions, aligning with findings from prior research (34, 35). Given that women with lower socioeconomic status are at higher risk and represent the most affected demographic for cervical cancer (36–38), emphasizing screening promotion for these groups is crucial. This discrepancy requires the development of more customized health communication strategies that cater to the different backgrounds and needs of various demographic groups.
HPV vaccination is an important preventive measure against cervical lesions and CC (39). In the present study, the rate of HPV vaccination was relatively low, at 32%. In China, HPV vaccines are presently purchased privately, and the pilot program for HPV vaccine immunization among girls of eligible age in Beijing is scheduled to commence in 2023 (22). Therefore, the women must decide to be vaccinated. Being ≤44 years old was independently associated with being vaccinated against HPV, probably mainly because the approved age for HPV vaccines is under 45 years old (40). Besides, it is the period of higher sexual activity. In addition, HPV vaccines and their importance are relatively novel (39), and it is more likely that younger women were targeted by their physicians for advice on the vaccine. It is supported by a study that showed that age > 41 years was associated with a more unfavorable attitude toward HPV vaccination in China (28). A previous study in China showed that mothers of daughters were more willing to be vaccinated themselves and have their daughters vaccinated (27), but it was not observed in the present study, possibly because the sex of the participants’ offspring was not collected. Furthermore, novel technologies such as mRNA testing are being made available for the rapid and effective screening of HPV (41). Fertility-sparing options are increasingly available (9, 42), but considering the risk of preterm birth in women with cervical precancerous lesions treated with conization (43), the prevention of HPV infection with vaccination makes more sense.
The SEM analysis revealed that knowledge positively influenced attitude and practice and that attitude positively influenced practice. Hence, improving knowledge should also improve the attitude and practice of the women toward cervical precancerous lesions. The results showed poor knowledge about the nature of the lesions, the role of HPV, the risk factors for cervical lesions, symptoms, cervical testing methods, CC screening, treatments, the possibility of CIN regression, and the continuum from CIN to CC. Hence, future educational interventions should target those points in particular. Educational programs on the progression of precancerous lesions in communities, health check-up centers, and medical institutions should be performed, and the follow-up management of high-risk groups should be strengthened. A study in China showed that exposing young women to information about HPV-related diseases increased their intention of getting vaccinated (44).
This study had several limitations. The study was performed at a single hospital, limiting the patients to a given geographical area and generalizability of the results. In addition, the participants were selected based on predefined criteria, possibly introducing bias. The study was cross-sectional, preventing the analysis of causality, for which longitudinal studies are necessary. Nevertheless, an SEM analysis was performed to estimate causality among KAP dimensions, but SEM analyses are statistical surrogates based on predefined hypotheses, and the results must be taken cautiously (45, 46). The questionnaire was designed by the investigators according to local practice, culture, and policies, limiting the exportability of the questionnaire to other centers or geographical areas and the generalizability of the results. All KAP studies are at risk of social desirability bias, in which the participants can answer what they know they should think or do instead of what they are actually doing (47, 48). Nevertheless, the questionnaire was self-reported, possibly introducing bias due to understanding the questions and response choices. In addition, the questionnaire was web-based, introducing a selection bias due to the access to technology. This study focused solely on cervical precancerous lesions without accounting for broader factors influencing women’s health behaviors. Finally, although qualitative analyses would have enriched the results and conclusion, they were not performed.
Future research could focus on several key areas to address the identified limitations and unanswered questions. First, longitudinal studies would be valuable for establishing causal relationships between KAP related to cervical precancerous lesions and HPV vaccination. Additionally, research could explore the impact of targeted educational interventions on improving KAP scores, particularly to address the significant variability observed in this study, with a focus on increasing HPV vaccination rates among young, sexually active women. Furthermore, qualitative research could provide deeper insights into the underlying reasons for knowledge gaps and attitudes, thereby refining public health strategies.
Conclusion
In conclusion, women in Beijing displayed poor knowledge and moderate attitude and practice toward cervical precancerous lesions. This underscores the urgent need for comprehensive educational strategies specifically tailored to the identified needs and challenges of the target population, aiming to enhance awareness and promote preventive behaviors among women in Beijing to reduce the incidence of cervical precancerous conditions.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Dongzhimen Hospital Affiliated with the Beijing University of Chinese. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LW: Data curation, Investigation, Project administration, Resources, Writing – original draft, Writing – review & editing. QW: Formal analysis, Methodology, Resources, Software, Writing – original draft, Writing – review & editing. XZ: Methodology, Resources, Software, Validation, Writing – original draft, Writing – review & editing. HL: Data curation, Resources, Software, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1433718/full#supplementary-material
Footnotes
References
1. Burmeister, CA, Khan, SF, Schafer, G, Mbatani, N, Adams, T, Moodley, J, et al. Cervical cancer therapies: current challenges and future perspectives. Tumour Virus Res. (2022) 13:200238. doi: 10.1016/j.tvr.2022.200238
2. Cohen, PA, Jhingran, A, Oaknin, A, and Denny, L. Cervical cancer. Lancet. (2019) 393:169–82. doi: 10.1016/s0140-6736(18)32470-x
3. Zhang, M, Chen, J, Cui, M, Jia, J, Zhao, M, Zhou, D, et al. Analysis of the global burden of cervical cancer in young women aged 15-44 years old. Eur J Pub Health. (2024) 34:839–46. doi: 10.1093/eurpub/ckae084
4. Perkins, RB, Wentzensen, N, Guido, RS, and Schiffman, M. Cervical Cancer screening: a review. JAMA. (2023) 330:547–58. doi: 10.1001/jama.2023.13174
5. Small, W Jr, Bacon, MA, Bajaj, A, Chuang, LT, Fisher, BJ, Harkenrider, MM, et al. Cervical cancer: a global health crisis. Cancer. (2017) 123:2404–12. doi: 10.1002/cncr.30667
6. Perkins, RB, Guido, RS, Castle, PE, Chelmow, D, Einstein, MH, Garcia, F, et al. 2019 ASCCP risk-based management consensus guidelines for abnormal cervical Cancer screening tests and Cancer precursors. J Low Genit Tract Dis. (2020) 24:102–31. doi: 10.1097/LGT.0000000000000525
7. Basu, P, Taghavi, K, Hu, SY, Mogri, S, and Joshi, S. Management of cervical premalignant lesions. Curr Probl Cancer. (2018) 42:129–36. doi: 10.1016/j.currproblcancer.2018.01.010
8. Pavone, M, Goglia, M, Scambia, G, Querleu, D, Akladios, C, and Lecointre, L. Laparoscopic-assisted vaginal Trachelectomy with prophylactic Cerclage: a safe fertility-sparing treatment for early stage cervical Cancer. Ann Surg Oncol. (2024) 31:1804–5. doi: 10.1245/s10434-023-14737-0
9. NCCN. NCCN clinical practice guidelines in oncology (NCCN guidelines). Cervical Cancer. Version 3.2024. Fort Washington: National Comprehensive Cancer Network (2024).
10. Rayner, M, Welp, A, Stoler, MH, and Cantrell, LA. Cervical Cancer screening recommendations: now and for the future. Healthcare. (2023) 11:11. doi: 10.3390/healthcare11162273
11. Wang, W, Arcà, E, Sinha, A, Hartl, K, Houwing, N, and Kothari, S. Cervical cancer screening guidelines and screening practices in 11 countries: a systematic literature review. Prev Med Rep. (2022) 28:101813. doi: 10.1016/j.pmedr.2022.101813
12. Andrade, C, Menon, V, Ameen, S, and Kumar, PS. Designing and conducting knowledge, attitude, and practice surveys in psychiatry: practical guidance. Indian J Psychol Med. (2020) 42:478–81. doi: 10.1177/0253717620946111
13. World Health Organization. Advocacy, communication and social mobilization for TB control: a guide to developing knowledge, attitude and practice surveys. (2008) Available at: http://whqlibdoc.who.int/publications/2008/9789241596176_eng.pdf (Accessed November 22, 2022).
14. Tadesse, A, Tafa Segni, M, and Demissie, HF. Knowledge, attitude, and practice (KAP) toward cervical Cancer screening among Adama science and technology university female students. Ethiopia Int J Breast Cancer. (2022) 2022:1–9. doi: 10.1155/2022/2490327
15. Ephrem Dibisa, K, Tamiru Dinka, M, Mekonen Moti, L, and Fetensa, G. Precancerous lesion of the cervix and associated factors among women of west Wollega, West Ethiopia, 2022. Cancer Control. (2022) 29:107327482211179. doi: 10.1177/10732748221117900
16. Usman, IM, Chama, N, Aigbogun Jr, EO, Kabanyoro, A, Kasozi, KI, Usman, CO, et al. Knowledge, attitude, and practice toward cervical Cancer screening among female university students in Ishaka Western Uganda. Int J Women’s Health. (2023) 15:611–20. doi: 10.2147/IJWH.S404845
17. Sakrawal, K, Meena, G, Gupta, A, Malav, K, and Grover, S. Knowledge, attitude, and practice about cervical cancer among adult women in rural Jaipur: an observational analysis. J Family Med Prim Care. (2023) 12:2379–84. doi: 10.4103/jfmpc.jfmpc_933_23
18. Pieters, MM, Proeschold-Bell, RJ, Coffey, E, Huchko, MJ, and Vasudevan, L. Knowledge, attitudes, and practices regarding cervical cancer screening among women in metropolitan Lima, Peru: a cross-sectional study. BMC Womens Health. (2021) 21:304. doi: 10.1186/s12905-021-01431-0
19. Donati, S, Giambi, C, Declich, S, Salmaso, S, Filia, A, Ciofi degli Atti, M, et al. Knowledge, attitude and practice in primary and secondary cervical cancer prevention among young adult Italian women. Vaccine. (2012) 30:2075–82. doi: 10.1016/j.vaccine.2012.01.057
20. Khanna, D, Khargekar, N, and Budukh, A. Knowledge, attitude, and practice about cervical cancer and its screening among community healthcare workers of Varanasi district, Uttar Pradesh. India J Family Med Prim Care. (2019) 8:1715–9. doi: 10.4103/jfmpc.jfmpc_143_19
21. Abudukadeer, A, Azam, S, Mutailipu, AZ, Qun, L, Guilin, G, and Mijiti, S. Knowledge and attitude of Uyghur women in Xinjiang province of China related to the prevention and early detection of cervical cancer. World J Surg Oncol. (2015) 13:110. doi: 10.1186/s12957-015-0531-8
22. Commission B M H. Notice on the issuance of the implementation plan for accelerating the elimination of cervical Cancer in Beijing (2023-2030). (2023) Available at: https://wjw.beijing.gov.cn/zwgk_20040/zcwj2022/gfxwj/202310/t20231018_3281123.html (Accessed April 16, 2024).
23. World Health Organization. WHO guidelines: Screening and treatment of precancerous lesions for cervical Cancer prevention. Geneva: World Health Organization (2021).
24. Marth, C, Landoni, F, Mahner, S, McCormack, M, Gonzalez-Martin, A, Colombo, N, et al. Cervical cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. (2017) 28:iv72–83. doi: 10.1093/annonc/mdx220
25. Pan, XF, Wang, L, and Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. (2021) 9:373–92. doi: 10.1016/s2213-8587(21)00045-0
26. Ni, P, Chen, JL, and Liu, N. Sample size estimation for quantitative studies in nursing research (2010) 45:378–80. doi: 10.3761/j.issn.0254-1769.2010.04.037
27. Lin, W, Wang, Y, Liu, Z, Chen, B, Yuan, S, Wu, B, et al. Awareness and attitude towards human papillomavirus and its vaccine among females with and without daughter(s) who participated in cervical cancer screening in Shenzhen. China Trop Med Int Health. (2019) 24:1054–63. doi: 10.1111/tmi.13283
28. Xie, L, Ren, J, Min, S, Zhu, X, Xu, D, Qiao, K, et al. Knowledge, attitude, and perception regarding HPV-related diseases and vaccination among the general public in Guizhou Province of China. Vaccine. (2023) 41:1119–31. doi: 10.1016/j.vaccine.2022.12.027
29. Wijayanti, KE, Schutze, H, MacPhail, C, and Braunack-Mayer, A. Parents’ knowledge, beliefs, acceptance and uptake of the HPV vaccine in members of the Association of Southeast Asian Nations (ASEAN): a systematic review of quantitative and qualitative studies. Vaccine. (2021) 39:2335–43. doi: 10.1016/j.vaccine.2021.03.049
30. Lee, PW, Kwan, TT, Tam, KF, Chan, KK, Young, PM, Lo, SS, et al. Beliefs about cervical cancer and human papillomavirus (HPV) and acceptability of HPV vaccination among Chinese women in Hong Kong. Prev Med. (2007) 45:130–4. doi: 10.1016/j.ypmed.2007.07.013
31. Ganesan, S, Subbiah, VN, and Michael, JC. Associated factors with cervical pre-malignant lesions among the married fisher women community at Sadras, Tamil Nadu. Asia Pac J Oncol Nurs. (2015) 2:42–50. doi: 10.4103/2347-5625.146223
32. Zhang, S, Xu, H, Zhang, L, and Qiao, Y. Cervical cancer: epidemiology, risk factors and screening. Chin J Cancer Res. (2020) 32:720–8. doi: 10.21147/j.issn.1000-9604.2020.06.05
33. Wencel-Wawrzenczyk, A, Lewitowicz, P, Lewandowska, A, and Saluga, A. Sexual behavior and the awareness level of common risk factors for the development of cervical, Anogenital and oropharyngeal Cancer among women subjected to HR HPV DNA-testing. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19159580
34. Huang, HY, Tsai, WC, Chou, WY, Hung, YC, Liu, LC, Huang, KF, et al. Quality of life of breast and cervical cancer survivors. BMC Womens Health. (2017) 17:30. doi: 10.1186/s12905-017-0387-x
35. Thapa, N, Maharjan, M, Xiong, Y, Jiang, D, Nguyen, TP, Petrini, MA, et al. Impact of cervical cancer on quality of life of women in Hubei. China Sci Rep. (2018) 8:11993. doi: 10.1038/s41598-018-30506-6
36. Weaver, KE, Geiger, AM, Lu, L, and Case, LD. Rural-urban disparities in health status among US cancer survivors. Cancer. (2013) 119:1050–7. doi: 10.1002/cncr.27840
37. Long, ME, Lee, YS, and Vegunta, S. Cervical cancer screening in menopause: when is it safe to exit? Menopause. (2023) 30:972–9. doi: 10.1097/gme.0000000000002222
38. Devesa, SS, and Diamond, EL. Association of breast cancer and cervical cancer incidence with income and education among whites and blacks. J Natl Cancer Inst. (1980) 65:515–28.
39. Pathak, P, Pajai, S, and Kesharwani, H. A review on the use of the HPV vaccine in the prevention of cervical Cancer. Cureus. (2022) 14:e28710. doi: 10.7759/cureus.28710
40. Meites, E, Szilagyi, PG, Chesson, HW, Unger, ER, Romero, JR, and Markowitz, LE. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. (2019) 68:698–702. doi: 10.15585/mmwr.mm6832a3
41. Frega, A, Pavone, M, Sesti, F, Leone, C, Bianchi, P, Cozza, G, et al. Sensitivity and specificity values of high-risk HPV DNA, p16/ki-67 and HPV mRNA in young women with atypical squamous cells of undetermined significance (ASCUS) or low-grade squamous intraepithelial lesion (LSIL). Eur Rev Med Pharmacol Sci. (2019) 23:10672–7. doi: 10.26355/eurrev_201912_19765
42. Taliento, C, Scutiero, G, Arcieri, M, Pellecchia, G, Tius, V, Bogani, G, et al. Simple hysterectomy versus radical hysterectomy in early-stage cervical cancer: a systematic review and meta-analysis. Eur J Surg Oncol. (2024) 50:108252. doi: 10.1016/j.ejso.2024.108252
43. Frega, A, Santomauro, M, Sesti, F, Di Giuseppe, J, Colombrino, C, Marziani, R, et al. Preterm birth after loop electrosurgical excision procedure (LEEP): how cone features and microbiota could influence the pregnancy outcome. Eur Rev Med Pharmacol Sci. (2018) 22:7039–44. doi: 10.26355/eurrev_201810_16176
44. Wang, Y, Chen, Y, and Bao, S. The impact of exposure to HPV related information and injunctive norms on young women’s intentions to receive the HPV vaccine in China: a structural equation model based on KAP theory. Front Public Health. (2022) 10:1102590. doi: 10.3389/fpubh.2022.1102590
45. Beran, TN, and Violato, C. Structural equation modeling in medical research: a primer. BMC Res Notes. (2010) 3:267. doi: 10.1186/1756-0500-3-267
46. Fan, Y, Chen, J, and Shirkey, G. Applications of structural equation modeling (SEM) in ecological studies: an updated review. Ecol Process. (2016) 5:19. doi: 10.1186/s13717-016-0063-3
47. Bergen, N, and Labonte, R. “everything is perfect, and we have no problems”: detecting and limiting social desirability Bias in qualitative research. Qual Health Res. (2020) 30:783–92. doi: 10.1177/1049732319889354
48. Latkin, CA, Edwards, C, Davey-Rothwell, MA, and Tobin, KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore. Maryland Addict Behav. (2017) 73:133–6. doi: 10.1016/j.addbeh.2017.05.005
Keywords: knowledge, attitude, practice, women, cervical precancerous lesions, China, cross-sectional study
Citation: Wang L, Wang Q, Zhou X and Liu H (2024) Women’s knowledge, attitude, and practice regarding cervical precancerous lesions: a cross-sectional study in Beijing, China. Front. Public Health. 12:1433718. doi: 10.3389/fpubh.2024.1433718
Edited by:
Matteo Pavone, Agostino Gemelli University Polyclinic (IRCCS), ItalyReviewed by:
Baroni Alessandro, Agostino Gemelli University Polyclinic (IRCCS), ItalyMari Kannan Maharajan, University of Nottingham Malaysia Campus, Malaysia
Copyright © 2024 Wang, Wang, Zhou and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lingyan Wang, bGluZ3lhbl8xMUAxNjMuY29t
†These authors share first authorship
 Lingyan Wang
Lingyan Wang Qianping Wang2†
Qianping Wang2†