- 1Department of Gastroenterology, Nanjing First Hospital, Nanjing Medical University, Nanjing, Jiangsu, China
- 2Department of Emergency, Nanjing First Hospital, Nanjing Medical University, Nanjing, Jiangsu, China
Background and objective: The Maastricht VI/Florence Consensus and Chinese National Consensus Report provide comprehensive guidelines for treating Helicobacter pylori infection. This study aimed to assess physicians' understanding of and adherence to this consensus in different hospitals.
Methods: Chinese medical staff attending gastrointestinal conferences across various regions were selected for this study. The questionnaire included: 1. the number of patients with peptic ulcer bleeding in hospitals of different levels annually and the diagnostic methods used for H. pylori; 2. whether routine H. pylori examination was conducted and the specific methods employed; and 3. Treatment plans for H. pylori eradication; 4. The mean follow-up duration after treatment 5. Plans for re-eradication in cases of H. pylori treatment failure.
Results: Across all levels of Chinese hospitals, the urea breath test was the most commonly used method for detecting H. pylori infection. Most primary (81.53%), secondary (89.49%), and tertiary (91.42%) centers opted for a 14-day quadruple regimen. The preferred antibiotic regimen at all hospital levels was amoxicillin+clarithromycin, with rates of 63.69, 58.08, and 59.27% in the primary, secondary, and tertiary hospitals, respectively. The rates of H. pylori re-examination were 68.15, 87.07, and 87.46% in the primary, secondary, and tertiary hospitals. If H. pylori eradication failed, hospitals at different levels choose to replace the initial plan.
Conclusion: There is a need for an enhanced understanding of and adherence to guidelines for H. pylori among physicians in hospitals at all levels.
Introduction
Upper gastrointestinal bleeding refers to bleeding occurring in the gastrointestinal tract proximal to the ligament of Treitz. Failure to promptly treat upper gastrointestinal bleeding results in 2–10% of annual deaths globally (1). Peptic ulcer disease is a common cause of upper GI bleeding, accounting for 30–60% of cases (2). Peptic ulcers are ulcerative conditions that primarily affect the stomach and duodenum and typically present with symptoms including abdominal distension, belching, and nausea. Severe disease can lead to gastrointestinal bleeding and even malignancy (3). The incidence of peptic ulcers ranges from 6 to 15% in Europe and America and ~10–12% in China (4). The development of peptic ulcers is closely associated with factors such as glucocorticoid use, thinning of the gastrointestinal mucosa, genetic susceptibility, excessive gastric acid production, and infection with H. pylori (5–7). H. pylori infection significantly contributes to developing peptic ulcers because the toxins this bacterium produces trigger immune responses that lead to mucosal damage.
H. pylori infection affects approximately half of the global population, with an infection rate of about 46.7% among the Chinese population (8, 9). The current status of H. pylori diagnosis and treatment can be summarized as having “three highs and one low”: high infection rate, high drug resistance rate, high pathogenicity, and low eradication rate. Antibiotic resistance in H. pylori is the primary factor contributing to the decline in the eradication rate (10). Globally, H. pylori antibiotic resistance is increasing, particularly in China. The Maastricht VI/Florence consensus was published in Gut in 2022 to address this concern. Following this consensus, the Helicobacter pylori Group of the Gastroenterology Branch of the Chinese Medical Association released the sixth national consensus report on the management of H. pylori infection in 2022. However, whether physicians from different hospitals across the country are well-acquainted with the content and application of these guidelines remains uncertain. A questionnaire was distributed in June 2023 to investigate the current diagnosis and treatment practices for H. pylori-related peptic ulcer bleeding among physicians in hospitals of varying levels. This study aimed to assess physicians' understanding of the consensus guidelines, particularly among gastroenterologists from hospitals of different levels.
Methods
Study participants
The study participants were Chinese medical staff who attended digestion conferences held in various regions of the country from June 2023 to November 2023. Medical staff were categorized into primary, secondary, and tertiary hospitals. Primary hospitals are healthcare institutions that directly provide the community with comprehensive services, such as medical treatment, prevention, rehabilitation, and healthcare. Secondary hospitals are regional hospitals that provide medical and health services across several communities and are technical centers for regional medical prevention. Tertiary hospitals provide medical and health services across regions, provinces, cities, and nationwide. These are medical prevention technology centers with comprehensive medical, teaching, and research capabilities. This study was approved by the Medical Ethics Committee of the Nanjing First Hospital.
Research methods
The research was conducted using a questionnaire distributed through a WeChat mini program, which allowed for convenient distribution of the questionnaire and data collection. The questionnaire included the following topics.
1. Annual number of patients with peptic ulcer bleeding in hospitals of different levels and H. pylori diagnostic methods employed.
2. Determining whether patients with peptic ulcer bleeding undergo routine H. pylori examination and the specific methods used for H. pylori testing.
3. Assessing the timing of H. pylori eradication, treatment plan and choice of antibiotics for H. pylori eradication.
4. Investigating the duration of follow-up after treatment.
5. Examination of the timing and plan for re-eradication in cases of H. pylori treatment failure.
Statistical analysis
The collected data were analyzed using SPSS 22.0. Descriptive statistics were used to present count data as percentages. Intergroup comparisons were performed using the chi-square test or Fisher's exact probability method. Statistical significance was set at p < 0.05.
Results
Demographic characteristics of participants
The WeChat mini program received 3,422 survey questionnaires, as depicted in Figure 1A, illustrating the distribution of Chinese medical staff and the provinces where they worked. Among the Chinese medical staff participating in the questionnaire survey, men accounted for 48.77% (1,669/3,422), and women accounted for 51.23% (1,753/3,422) (Figure 1B). Gastroenterologists, general practitioners, nurses, and other department physicians constituted 81.82% (2,800/3,422), 5.58% (191/3,422), 8.91% (305/3,422), and 3.68% (126/3,422) of the sample, respectively (Figure 1C). Among the Chinese medical staff, Chief Physicians, Attending Doctors, and Resident Doctors represented 54.44% (1,863/3,422), 31.33% (1,072/3,422), and 14.23% (487/3,422), respectively (Figure 1D). The results indicated that 10.23% (350/3,422) had ≤ 5 years' experience, 51.40% (1,759/3,422) had 520 years, 23.96% (820/3,422) had worked 21–30 years, and 14.41% (493/3,422) had been working ≥30 years (Figure 1E). Questionnaire respondents worked in primary hospitals, 4.59% (157/3,422), secondary hospitals, 25.31% (866/3,422), and tertiary hospitals, 70.11% (2,399/3,422) (Figure 1F).
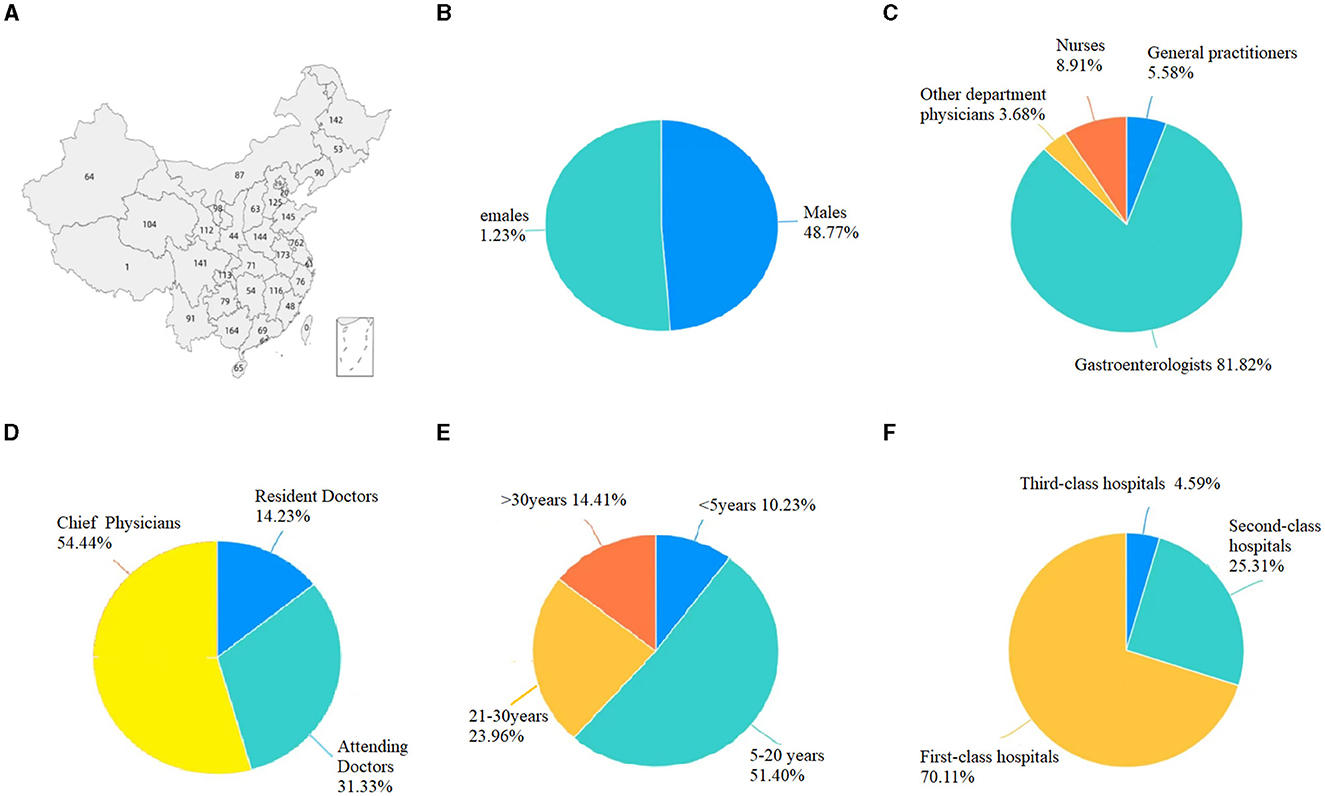
Figure 1. Demographic characteristics of participants. (A) The distribution of Chinese medical staff and the provinces where they worked. (B) Gender distribution of medical staff. (C) Composition of medical staff. (D) Levels of the surveyed physicians. (E) Years of service of the surveyed physicians. (F) The levels of the hospital where the surveyed physicians are located.
The annual number of patients with peptic ulcer bleeding in hospitals of different levels and the H. pylori diagnostic methods applied
Among primary hospitals, 127 had fewer than 50 individuals requiring hospitalization for peptic ulcer bleeding annually, 21 admit 50–100 patients annually, and nine admit over 100 patients annually. In secondary hospitals, 280 admitted ≤ 50 patients per year because of peptic ulcer bleeding, 351 admit 50–100 patients per year, and 235 admitted >100 patients annually. Among the tertiary hospitals, 172 admitted no more than 50 patients per year, 636 admit between 50–100 patients per year, and 1,591 admit more than 100 patients per year (Table 1).

Table 1. Annual number of patients with peptic ulcer bleeding in hospitals of different levels, and the H. pylori diagnostic methods applied.
We found that 16.56% (26/157) of primary hospitals do not perform diagnostic testing for H. pylori, secondary hospitals accounted for 1.73% (15/866), and tertiary hospitals for 0.1% (4/2,399). The top five methods were the rapid urease test, 13C urea breath test, 14C urea breath test, the serological antibody test, and the pathological tissue test, with the urea breath test being the most commonly used (Table 1).
H. pylori examination in hospitals of different levels
In primary hospitals, 68.79% (108/157) of the patients underwent H. pylori examination during hospitalization, 16.56% (26/157) underwent outpatient examination after discharge, and 14.65% (23/157) did not undergo examination. During hospitalization in secondary hospitals, 80.72% (698/866) of the patients underwent H. pylori examination, 17.09% (148/866) underwent outpatient examination after discharge, and 2.19% (19/866) did not undergo examination. In tertiary hospitals, 76.01% (1,824/2,399) of the patients underwent H. pylori examination during hospitalization, 22.45% (539/2,399) underwent outpatient examination after discharge, and 1.54% (37/2,399) did not undergo examination (Table 2).
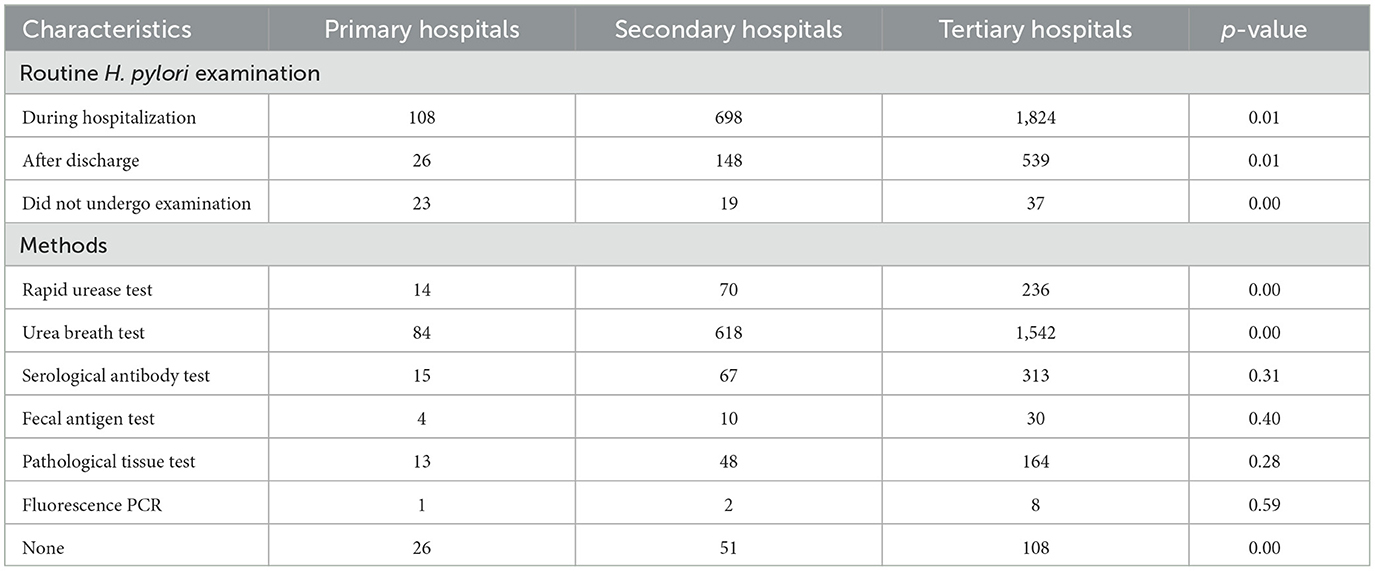
Table 2. Routine H. pylori examination and examination methods for patients with peptic ulcers and bleeding in hospitals of different levels.
The methods used for H. pylori examination in primary hospitals included rapid urease test (8.92%, 14/157), urea breath test (53.5%, 84/157), serological antibody test (9.55%, 15/157), fecal antigen test (2.55%, 4/157), histopathological test (8.28%, 13/157), and polymerase chain reaction (PCR) testing (0.64%, 1/157). In secondary hospitals, the methods included rapid urease test in 8.08% (70/866), urea breath test in 71.36% (618/866), serological antibody test in 7.74% (67/866), fecal antigen test in 1.15% (10/866), histopathological test in 5.54% (48/866), and PCR testing in 0.23% (2/866). In the tertiary hospitals, the methods used were as follows: rapid urease test, 9.83% (236/2,399); urea breath test, 64.22% (1,542/2,399); serological antibody test, 13.04% (313/2,399); fecal antigen test, 1.25% (30/2,399); histopathological test, 6.83% (164/2,399); and PCR test, 0.33% (8/2,399) (Table 2).
Timing and regimen of H. pylori eradication
In primary hospitals, H. pylori eradication was achieved in 21.02% (33/157) of patients during hospitalization; 50.31% (79/157) were cured after discharge, 17.83% (28/157) were cured after ulcer healing, and 10.83% (17/157) did not achieve eradication. During hospitalization in secondary hospitals, 31.99% (277/866) of the patients underwent H. pylori eradication, 51.96% (450/866) underwent post-discharge diagnosis and eradication, 13.05% (113/866) underwent ulcer healing eradication, and 3% (26/866) underwent non-eradication. In tertiary hospitals, H. pylori eradication was achieved in 22.87% (548/2,399) of patients; 58.90% (1,413/2,399) were cured after discharge, 17.41% (418/2,399) were cured after ulcer healing, and 0.83% (20/2,399) did not achieve eradication (Table 3).
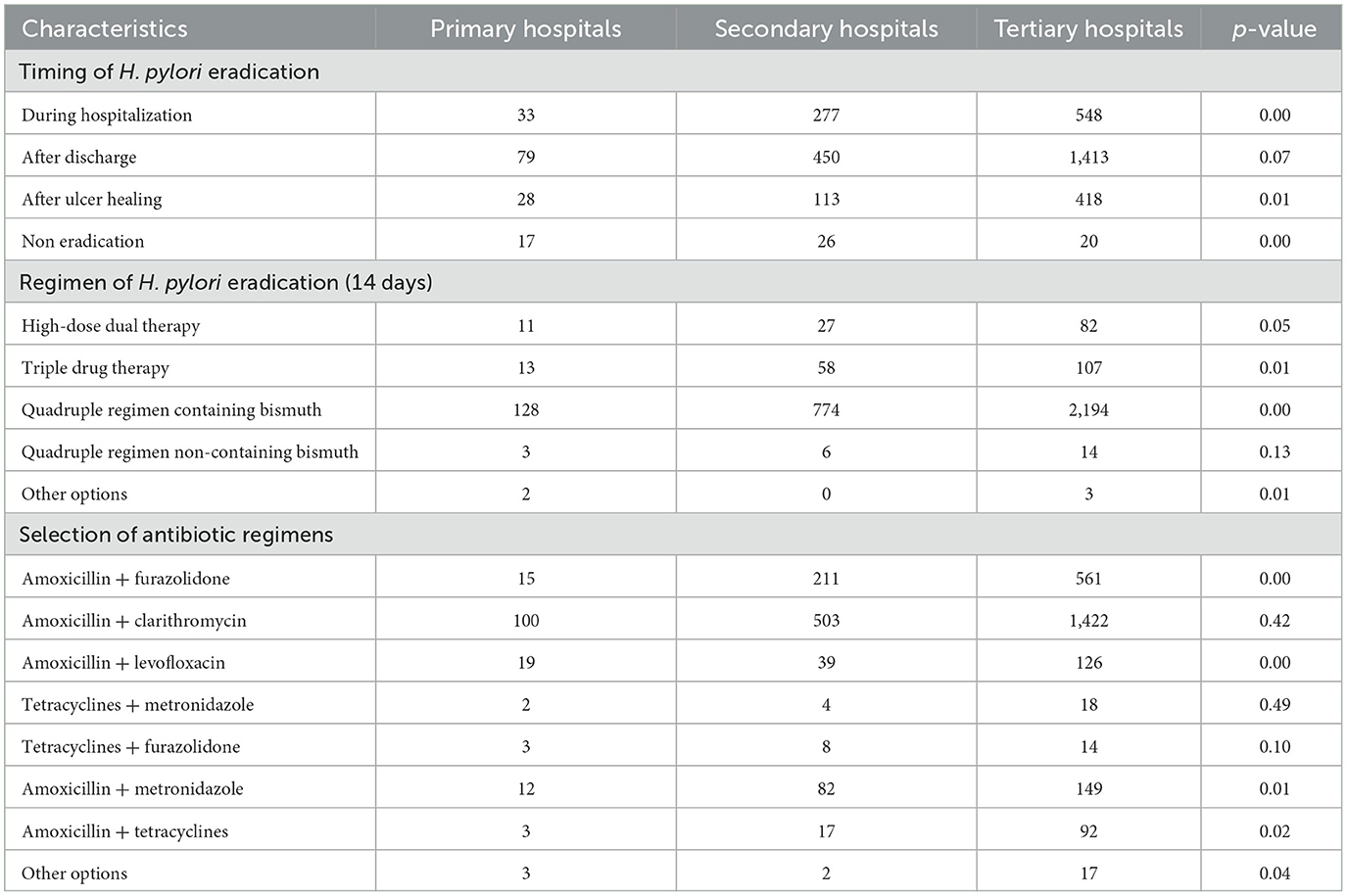
Table 3. Timing and regimen of H. pylori eradication and selection of antibiotics for patients with peptic ulcers and bleeding in hospitals of different levels.
Most primary, secondary, and tertiary hospitals selected a quadruple 14-day bismuth regimen, accounting for 81.53, 89.49, and 91.42%, respectively). The high-dose dual therapy 14-day regimen ranked third, accounting for 7.01, 3.12, and 3.42%, respectively (Table 3).
Amoxicillin and clarithromycin were the most commonly chosen options at all levels of hospitals, accounting for 63.69% (100/157) of primary hospitals, 58.08% (503/866) of secondary hospitals, and 59.27% (1,422/2,399) of tertiary hospitals. In primary hospitals, amoxicillin + levofloxacin accounted for 12.10% (19/157), amoxicillin + furazolidone 9.55% (15/157), and amoxicillin + metronidazole 7.64% (12/157). In secondary and tertiary hospitals, the follow-up plans included amoxicillin + furazolidone at 24.36 and 23.41% (211/866, 561/2,399), amoxicillin + metronidazole at 9.47 and 6.21% (82/866, 149/2,399), and amoxicillin + levofloxacin at 4.50 and 5.25% (39/866, 126/2,399), respectively (Table 3).
Timing of re-examination for H. pylori in patients with peptic ulcers and bleeding after eradication
The results indicated that after the eradication of H. pylori, the rates of H. pylori re-examination after stopping medication for 2 weeks, 4 weeks, 6 months, and no re-examination after stopping medication in primary hospitals were 20.38% (32/157), 68.15% (107/157), 7.01% (11/157), and 4.46% (7/157), respectively. In the secondary hospitals, the rates were 8.78% (76/866), 87.07% (753/866), 3.35% (29/866), and 0.81% (7/866), respectively. Tertiary hospitals had rates of 8.54% (205/2,399), 87.46% (2,099/2,399), 3.79% (91/2,399), and 0.21% (5/2,399), respectively (Table 4).
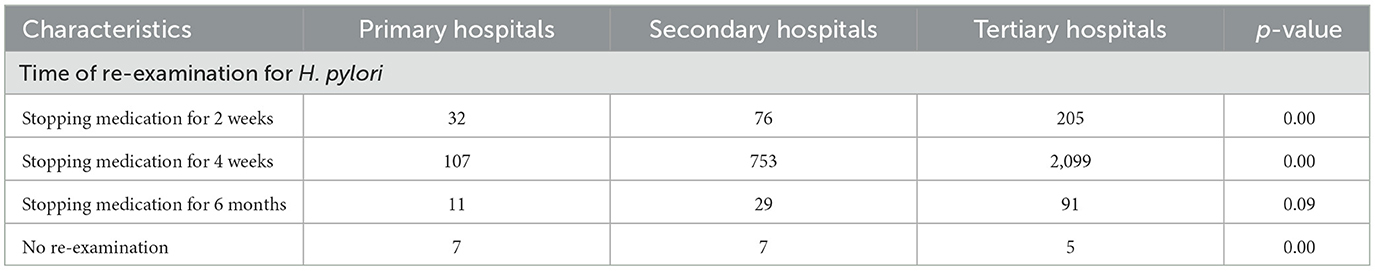
Table 4. Time for re-examination of H. pylori in patients with peptic ulcers and bleeding in hospitals of different levels after eradication of H. pylori.
The time and plan selection for re-eradication of H. pylori in patients with treatment failure
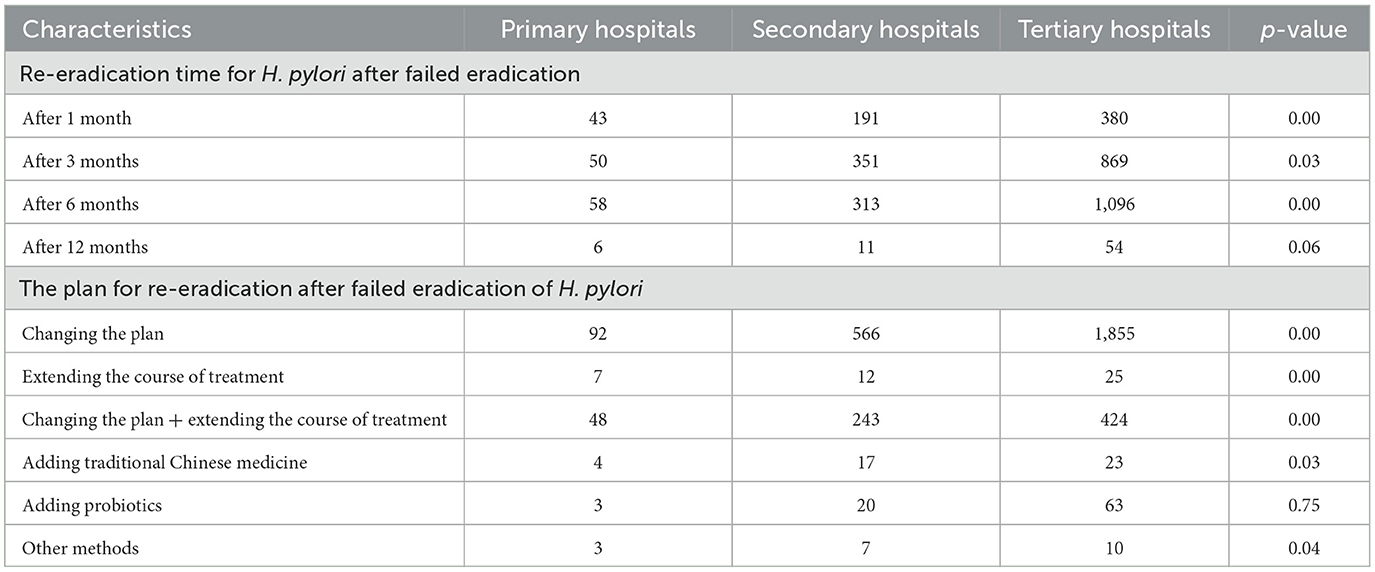
The re-eradication times for H. pylori after failed eradication were 27.39% (43/157), 31.85% (50/157), 36.94% (58/157), and 3.82% (6/157) in primary hospitals after 1, 3, 6, and 12 months, respectively. In secondary hospitals, the rates were 22.06% (191/866), 40.53% (351/866), 36.14% (313/866), and 1.27% (11/866). Tertiary hospitals had rates of 15.83% (380/2,399), 36.23% (869/2,399), 45.69% (1,096/2,399), and 2.25% (54/2,399), respectively (Table 5).
The selection of a plan for re-eradication after the failed eradication of H. pylori included changing the plan, extending the course of treatment, changing the plan and extending the course of treatment, adding traditional Chinese medicine, adding probiotics, and other methods. Choices in primary hospitals were 58.60% (92/157), 4.46% (7/157), 30.57% (48/157), 2.25% (4/157), 1.91% (3/157), and 1.91% (3/157), respectively. Secondary hospitals had choices of 65.47% (566/866), 1.39% (12/866), 28.06% (243/866), 1.96% (17/866), 2.31% (20/866), and 0.81% (7/866), respectively. Tertiary hospitals showed choices of 77.30% (1,855/2,399), 1.04% (25/2,399), 17.66% (424/2,399), 0.96% (23/2,399), 2.62% (63/2,399), and 0.42% (10/2,399), respectively (Table 5).
Discussion
Peptic ulcers are a prevalent disease worldwide, and their most significant complication is bleeding, which can be life-threatening in severe cases. Extensive domestic and international research has confirmed that H. pylori is the primary causative factor of peptic ulcers. The detection rate of H. pylori in gastric mucosal biopsy samples from peptic ulcer patients is reported to exceed 80% in gastric ulcer patients and 90–100% in duodenal ulcer patients. The risk of peptic ulcer development is significantly increased in individuals infected with H. pylori. Eradicating H. pylori has been shown to reduce the annual recurrence rate of gastric and duodenal ulcers to < 20%, whereas patients who have not undergone eradication treatment can experience an annual recurrence rate of >60% (11). Therefore, consensus guidelines recommend H. pylori eradication as an effective measure for preventing and treating peptic ulcers.
This survey included practitioners in hospitals in provinces country-wide except Taiwan. The participants consisted mainly of gastroenterologists, accounting for 81.82%, and 89.77% had more than 5 years of experience. Most (85.77%) held positions as professors or attending doctors, primarily working in tertiary hospitals. Therefore, this survey provided valuable insights into the awareness and application of Consensus Guidelines among doctors at different hospital levels.
The survey revealed that hospitals at different levels had patients admitted for peptic ulcer bleeding. As the hospital level increased, the number of patients also increased, potentially indicating a higher trust of patients in tertiary hospitals. Various methods have been employed to diagnose H. pylori, with the urea breath test being the most commonly used across hospital levels. Other frequently employed methods included serological antibody testing, histopathological testing, and rapid urease testing, fulfilling the basic requirements for diagnosing and re-examining H. pylori patients. The proportion of bacterial cultures and drug sensitivity testing exceeded that of fecal antigen testing. Monoclonal fecal antigen testing has similar accuracy to the urea breath test but has limitations regarding adult acceptance due to the need for stool collection. Monoclonal fecal antigen testing has advantages over the urea breath test in cases where patients are unwilling or unable to undergo the breath test or have poor breath coordination (12, 13). Additionally, many hospitals have initiated genetic testing for antibiotic resistance, a crucial technical foundation for guiding personalized treatment in the fight against H. pylori.
This survey investigated routine H. pylori testing and examination methods for patients with peptic ulcers and bleeding at different hospital levels. During hospitalization, 68.79% of primary, 80.72% of secondary, and 76.01% of tertiary hospitals conducted H. pylori examinations. After discharge, 16.56, 17.09, and 22.45% of primary, secondary, and tertiary hospitals, respectively, performed outpatient H. pylori examinations. However, a relatively high proportion of primary hospitals (14.65%) did not perform H. pylori testing, indicating a need for improvement. Primary hospitals should strengthen their education on the etiology of peptic ulcers with bleeding and implement routine H. pylori testing.
Regarding diagnostic methods, the urea breath test is the most commonly used across hospitals at different levels, with a usage rate exceeding 50%. The rates of the rapid urease test, serological antibody test, and histopathological test ranged from 5 to 10%. However, in tertiary hospitals, the usage rate of serological antibody tests is only 13.04%, primarily for epidemiological investigations. Current infections can be considered in specific circumstances, such as peptic ulcer bleeding, patients with atrophic gastritis, and gastric mucosa-associated lymphoid tissue lymphoma who are positive for H. pylori antibodies and have not received eradication treatment (14). The development of rapid urease and pathological tests is relatively limited and requires further investigation.
In terms of treatment, the timing and protocol of H. pylori eradication and the selection of antibiotics were investigated in patients with peptic ulcers and bleeding at different levels of hospitals. Most hospitals at various levels chose to eradicate ulcers immediately after discharge. The percentages of immediate eradication during hospitalization and after discharge were 71.34, 83.95, and 81.74% in primary, secondary, and tertiary hospitals, respectively. After ulcer healing, the eradication rates were 17.83, 13.05, and 17.41% in the primary, secondary, and tertiary hospitals, respectively. The proportions of non-eradication of H. pylori in primary, secondary, and tertiary hospitals were 10.83, 3, and 0.83%, respectively, indicating that treatment in primary hospitals was highly non-standard. The H. pylori study group should enhance the learning of the consensus guidelines among physicians at primary hospitals.
Regarding eradication options, using bismuth-containing quadruple 14-day regimens accounted for 81.53, 89.49, and 91.42% in primary, secondary, and tertiary hospitals, respectively. This aligns with the sixth National Consensus Report on the Management of H. pylori Infections in China, which recommends using bismuth-containing quadruple regimens for primary and secondary eradication. The survey also revealed that the rates of choosing high-dose combination therapy for 14 days in primary, secondary, and tertiary hospitals were 7.01, 3.12, and 3.42%, respectively. A significant proportion of physicians still choose triple therapy, with an average eradication rate of 71.3% in China. Triple therapy is no longer recommended, and its continued use may be attributed to the slow updating of physician knowledge and insufficient familiarity with the latest consensus guidelines.
Regarding the choice of antibiotic regimens, the investigation found that in primary hospitals, amoxicillin + clarithromycin had the highest proportion, followed by amoxicillin + levofloxacin and amoxicillin + furazolidone. In secondary and tertiary hospitals, the most common regimens were amoxicillin + furazolidone and amoxicillin + metronidazole, respectively.
The survey results highlighted several important findings regarding H. pylori eradication treatments. First, physicians' preference for amoxicillin and clarithromycin regimens indicates the need for increased awareness of antibiotic resistance and the importance of conducting antibiotic sensitivity testing. The Maastricht VI/Florence Consensus recommends resistance testing before using clarithromycin-containing prescriptions (15). In China, PCR-based clarithromycin-resistance gene detection kits are available and have been used during the COVID-19 pandemic. Personalized treatments based on resistance gene testing have shown promise in improving eradication rates.
The survey also revealed high resistance rates to antibiotics commonly used for H. pylori eradication, such as clarithromycin, levofloxacin, and metronidazole. Furazolidone and tetracycline are relatively sensitive, but their availability is limited. Furazolidone is no longer used in many countries owing to safety concerns. Metronidazole is widely available but has a high resistance rate (16). The availability of clarithromycin and amoxicillin is high, making personalized treatment guided by clarithromycin resistance genes the preferred option.
Regarding the timing of re-examination after H. pylori eradication, a significant proportion of hospitals chose not to conduct follow-up examinations or scheduled them too early. Re-examination after 4 weeks of discontinuation was common, but some physicians opted for a 6-month interval to ensure accurate determination of eradication success. The lack of adherence to recommended guidelines suggests the need for further education and awareness among physicians.
In cases where H. pylori eradication failed, the survey explored the timing and protocol selection for re-eradication. European guidelines (17) suggest allowing H. pylori to regain activity after a 3–6-month interval before initiating re-eradication treatment. Hospitals have chosen various approaches, with the majority replacing eradication plans. It is crucial to consider local clinical characteristics such as drug resistance and accessibility and avoid reusing previously ineffective antibiotics.
Resistance to clarithromycin and levofloxacin is also associated with eradication failure (18). Therefore, a thorough investigation of a patient's history of antibiotic use is necessary to guide treatment decisions. Primary resistance to amoxicillin, tetracycline, and furazolidone is rare in China. The treatment duration is also an important consideration, with a 14-day course showing higher eradication rates in refractory cases.
Non-antibiotic adjunctive drugs, such as traditional Chinese medicines and probiotics, have shown the potential to reduce adverse reactions and improve patient tolerance to H. pylori eradication treatment (19, 20). However, further research is needed to establish their efficacy and role in improving eradication rates.
Conclusion
It is important for physicians at all hospital levels, particularly primary hospitals, to enhance their understanding of H. pylori infection, eradication, follow-up, and re-eradication. The Maastricht VI/Florence and Chinese National Consensus reports provide valuable guidelines for H. pylori management and should be incorporated into clinical practice.
It should be noted that this survey was conducted after the publication of the Maastricht VI/Florence Consensus and the Chinese National Consensus Report, indicating the need for continued education and implementation of the latest guidelines. This study had some limitations, including the relatively small proportion of primary hospitals, which should be addressed in future research.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of the Nanjing First Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZJ: Conceptualization, Data curation, Funding acquisition, Project administration, Writing – original draft. YD: Formal analysis, Investigation, Methodology, Resources, Writing – original draft. CL: Data curation, Investigation, Validation, Visualization, Writing – original draft. ZZ: Conceptualization, Project administration, Resources, Supervision, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Nanjing Medical Science and Technique Development Foundation (grant number YKK20108).
Acknowledgments
We thank everyone who helped us during this investigation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Moledina SM, Komba E. Risk factors for mortality among patients admitted with upper gastrointestinal bleeding at a tertiary hospital: a prospective cohort study. BMC Gastroenterol. (2017) 17:165. doi: 10.1186/s12876-017-0712-8
2. Gralnek IM, Dumonceau JM, Kuipers EJ, Lanas A, Sanders DS, Kurien M, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. (2015) 47:a1–46. doi: 10.1055/s-0034-1393172
3. Serafim C, Araruna ME, Júnior EA, Diniz M, Hiruma-Lima C, Batista L, et al. Review of the role of flavonoids in peptic ulcer (2010-2020). Molecules. (2020) 25:5431. doi: 10.3390/molecules25225431
4. Yeo SH, Yang CH. Peptic ulcer disease associated with Helicobacter pylori infection. Korean J Gastroenterol. (2016) 67:289–99. doi: 10.4166/kjg.2016.67.6.289
5. den Hollander WJ, Sostres C, Kuipers EJ, Lanas A. Helicobacter pylori and nonmalignant diseases. Helicobacter. (2013) 18(Suppl. 1):24–7. doi: 10.1111/hel.12074
6. Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. (2014) 19(Suppl. 1):1–5. doi: 10.1111/hel.12165
7. Pan W, Zhang H, Wang L, Zhu T, Chen B, Fan J. Association between Helicobacter pylori infection and kidney damage in patients with peptic ulcer. Ren Fail. (2019) 41:1028–34. doi: 10.1080/0886022X.2019.1683029
8. Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. (2017) 153:420–9. doi: 10.1053/j.gastro.2017.04.022
9. Li M, Sun Y, Yang J, de Martel C, Charvat H, Clifford GM, et al. Time trends and other sources of variation in Helicobacter pylori infection in mainland China: a systematic review and meta-analysis. Helicobacter. (2020) 25:e12729. doi: 10.1111/hel.12729
10. Katelaris P, Hunt R, Bazzoli F, Cohen H, Fock KM, Gemilyan M, et al. Helicobacter pylori world gastroenterology organization global guideline. J Clin Gastroenterol. (2023) 57:111–26. doi: 10.1097/MCG.0000000000001719
11. Silverstein FE. Improving the gastrointestinal safety of NSAIDs: the development of misoprostol–from hypothesis to clinical practice. Dig Dis Sci. (1998) 43:447–58.
12. Konstantopoulos N, Rüssmann H, Tasch C, Sauerwald T, Demmelmair H, Autenrieth I, et al. Evaluation of the Helicobacter pylori stool antigen test (HpSA) for detection of Helicobacter pylori infection in children. Am J Gastroenterol. (2001) 96:677–83. doi: 10.1111/j.1572-0241.2001.03603.x
13. Alzoubi H, Al-Mnayyis A, Al Rfoa I, Aqel A, Abu-Lubad M, Hamdan O, et al. The use of 13C-urea breath test for non-invasive diagnosis of Helicobacter pylori infection in comparison to endoscopy and stool antigen test. Diagnostics. (2020) 10:448. doi: 10.3390/diagnostics10070448
14. Lerang F, Haug JB, Moum B, Mowinckel P, Berge T, Ragnhildstveit E, et al. Accuracy of IgG serology and other tests in confirming Helicobacter pylori eradication. Scand J Gastroenterol. (1998) 33:710–5. doi: 10.1080/00365529850171648
15. Malfertheiner P, Megraud F, Rokkas T, Gisbert JP, Liou JM, Schulz C, et al. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. (2022) gutjnl-2022-327745. doi: 10.1136/gutjnl-2022-327745
16. Zhong Z, Zhang Z, Wang J, Hu Y, Mi Y, He B, et al. A retrospective study of the antibiotic-resistant phenotypes and genotypes of Helicobacter pylori strains in China. Am J Cancer Res. (2021) 11:5027–37.
17. Megraud F, Bruyndonckx R, Coenen S, Wittkop L, Huang TD, Hoebeke M, et al. Helicobacter pylori resistance to antibiotics in Europe in 2018 and its relationship to antibiotic consumption in the community. Gut. (2021) 70:1815–22. doi: 10.1136/gutjnl-2021-324032
18. Graham DY. Implications of the paradigm shift in management of Helicobacter pylori infections. Therap Adv Gastroenterol. (2023) 16:17562848231160858. doi: 10.1177/17562848231160858
19. Feng JR, Wang F, Qiu X, McFarland LV, Chen PF, Zhou R, et al. Efficacy and safety of probiotic-supplemented triple therapy for eradication of Helicobacter pylori in children: a systematic review and network meta-analysis. Eur J Clin Pharmacol. (2017) 73:1199–208. doi: 10.1007/s00228-017-2291-6
Keywords: peptic ulcer bleeding, Helicobacter pylori, questionnaire, consensus, different level hospitals
Citation: Jiang Z, Ding Y, Li C and Zhang Z (2024) National survey questionnaire on the diagnosis and treatment status of Helicobacter pylori in peptic ulcer bleeding disease. Front. Public Health 12:1433139. doi: 10.3389/fpubh.2024.1433139
Received: 15 May 2024; Accepted: 28 August 2024;
Published: 11 September 2024.
Edited by:
Ponsiano Ocama, Makerere University, UgandaReviewed by:
Amit Ranjan, Columbia University, United StatesPaweł Krzyżek, Wroclaw Medical University, Poland
Copyright © 2024 Jiang, Ding, Li and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenyu Zhang, YWh6aGFuZ3poZW55dUBzaW5hLmNvbQ==
†These authors have contributed equally to this work
 Zongdan Jiang
Zongdan Jiang Yaokun Ding
Yaokun Ding Chao Li
Chao Li Zhenyu Zhang
Zhenyu Zhang