- 1Department of Environmental Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
- 2Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 3Department of Occupational Health and Safety, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Background: In resource-limited areas, especially in conflict-affected settings, managing the risk of hospital-acquired infections is difficult due to the destruction of essential facilities in healthcare settings. The study aimed to assess adherence to Infection prevention practices and associated factors among healthcare workers in Northeastern Ethiopia following the Northern Ethiopia conflict.
Methods and materials: A facility-based cross-sectional study was done with 408 healthcare workers. The survey data was collected using a structured questionnaire based on published articles. Data entry and analysis was done using Epi-Data version 4.6 and SPSS version 25.0, respectively. Binary logistic regression was used to determine the association between dependent and outcome variables, with a cut-off p value 0.05 at 95% confidence interval with a p-value less than 0.05 and a 95% confidence interval for determining factors associated with adherence to infection prevention practices among study participants.
Results: The study included 408 healthcare workers with a response rate of 96.7%. The majority of participants were women 206 (50.5%), married 250 (61.3%), Orthodox followers 211 (51.7%), and educational status of master holder and above with a master’s degree or higher 177 (43.4%). Slightly more than half, 53.7% (219) of the respondents demonstrated safe infection prevention practices. Respondents who received training on infection prevention practices (AOR = 2.662, 95% CI: 1.361, 5.120) had an active infection prevention committee (AOR = 2.203, 95% CI: 1.359, 3.572), use infection prevention guidelines in working departments (AOR = 2.090, 95% CI: 1.013, 4.312), and access to adequate personal protective equipment (AOR = 2.773, 95% CI: 1.560, 4.929) were factors significantly associated with adherence to infection prevention practices.
Conclusion: Overall, only half of the respondents practiced safe infection prevention practices. Receive training on infection prevention guidelines, presence of active infection prevention committee and working guidelines, and the availability of personal protective equipment were factors of infection prevention. Hence, essential facilities like Personal protective equipment, working guidelines should be supplied by donors.
Introduction
The conflict in Northern Ethiopia began on November 3, 2020, between the Tigray People Liberation Front (TPLF) and the Federal government of Ethiopia. Since then, it has extended to the nearby Amhara and Afar regions (1, 2). Armed conflict has profound public health implications, leading to both direct and indirect consequences. Direct effects include immediate injuries and deaths caused by utilization of firearms and explosives during conflict (1) and may cause for the death of an estimated 133,750 people every year, excluding indirectly attributable mortality (3). Moreover the indirect effects may cause for decline of the public health through the collapsing of the overall health systems, shortage of medical supplies, displacement of healthcare workers, and disruption of food and clean water supplies. Hence, preventive and curative services of the healthcare facilities become collapsed (1, 3).
Experiences from countries like Syria, South Sudan, Angola, and Nepal showed that healthcare facilities became the targets of armed fighters. For instance, in Syria, 185 health facilities were damaged either knowingly or unknowingly (4). Armed conflicts damage health systems, resulting in a resurgence of preventable infectious diseases. Globally, over three-quarters of the deaths are non-communicable, especially in low and middle-income countries (LMIC), where armed conflict exacerbate long term health issues (5). In LMIC, healthcare facilities face various challenges, including infrastructure, unbalancing of high patient load and low staffs, may complicate the efforts of infection prevention and control measures (6). Armed conflicts further damage the public health infrastructure and hindering healthcare delivery due to destruction of health facilities, shortage of ambulances, medical supplies and equipment’s. (7). Areas affected by conflict usually operate with insufficient staffs which limits the capacity of IPC (8). Hence, implementation of effective IPC programs could potentially reduce the burden of IPC by up to one-third (9).
HAIs are the global public health problem, particularly occur worldwide, particularly prevalent in LMIC. Approximately 10% of hospitalized patients in developed countries and 25% in developing countries experiences HAIs leading to a negative health consequences, including an increased hospital stay, economic burden, morbidity, and mortality (9–11). In Africa, HAIs may affect 3 and 15% in hospitalized patients (12). Adherences to IPC may be hindered by a high workload, insufficient time, and in balanced patient-to-health practitioner ratio. Therefore, implementing various strategies of IPC improvement intervention tactics has been proven to lower HAIs and increase HCWs adherence (13). A systematic review and meta-analysis in Ethiopia revealed that the prevalence of HAI was 16.96% (14). The use of effective and low-cost IPC measures reduces the burden of HCAIs by at least one-third. Despite these strategies are implemented, adherence with standard IPC practices remains very low, especially in LMIC, in which Ethiopia is not exceptional due to the existences of continuous conflict in the region (15).
The Ethiopian Federal Ministry of Health has launched various initiatives to safeguard patients and healthcare workers by establishing standards and guidelines. However, in resource-limited areas, especially in conflict-affected settings, controlling the risk of HCAIs is challenging due to the destruction of essential facilities in healthcare settings. The lack of knowledge and motivation to implement standard infection prevention practices contribute to this challenge (16). In the Northern Ethiopia conflict, there have been numerous reports of destruction and atrocities against health systems and civilians despite, most of the reports have relied on press reports of eyewitness accounts, journalists, humanitarian agencies and official announcements of combatants (1). To the best of our knowledge, there is scanty information on IPC following conflict-affected areas in Ethiopia. Hence, this study aimed to assess adherence with infection prevention practices and associated factors among HCWs in Northeastern Ethiopia, following the Northern Ethiopia conflict.
Methods and materials
Study setting and period
The study was carried out in Northeastern Ethiopia. The study catchment has 22 districts. Based on the 2014 population projection report, the total population of the study area was 2,925,559, of which 1,448,174 were males and 1,477,385 were females (17). In terms of healthcare facilities, there were 14 public hospitals, 3 private hospitals, 135 health centers, 496 clinics, and 175 pharmacies (18). The study was conducted from June 1 to June 30, 2022.
Study design
A facility-based cross-sectional study was carried out using a structured standardized questionnaire based on published articles to assess the adherence to infection prevention practices among healthcare professionals in government healthcare facilities in the South Wollo zone of Northeastern Ethiopia, following the Northern Ethiopia conflict.
Population (source and study populations)
The source population of the study consisted of all healthcare workers (such as general practitioners, public health officers, nurses, midwives, laboratory technicians and technologists, dentists, anesthetists, ophthalmologists, and cataract surgeons) who were working in governmental healthcare facilities in the South Wollo Zone, Northeastern Ethiopia. On the other hand, the study includes healthcare workers working in the selected governmental healthcare facilities during the study period.
Inclusion criteria
The study included healthcare workers with direct contact with at least one of four potential sources, namely patients, medical equipment, linens, and high-risk waste.
Exclusion criteria
Healthcare workers with less than six months of working experience, on annual leave, maternity leave, or experiencing illness during the study period were excluded from participating in the study. Additionally, administrative staff and cleaners were also excluded from the study.
Sample size determination and sampling procedures
The sample size for this study was determined using a single population proportion formula with the following assumptions. Half (50%) of the HCWs were assumed to have good infection prevention practices due to the lack of previous studies following conflicts, a margin of error of 5% and, a 95% confidence interval (CI) were taken into account during the calculation.
Where: n represents the required sample size, Z is the z-score corresponding to the desired level of confidence (for a 95% confidence level, Z would be 1.96), p is the estimated proportion of the population (50% of the HCWs had good infection prevention practices), d is the desired margin of error (the maximum difference allowed between the sample estimate and the true population proportion).
Applying these values, the calculated sample size is 384. Finally, considering for the potential non-response rate of 10%, the final sample size is adjusted to 422.
Sampling procedures
Regarding the sampling procedures, the initial step involved the selection of 22 governmental healthcare facilities including, health centers, and hospitals by a simple random technique using a lottery method. The number of healthcare providers in each selected facility was obtained from their respective human resource offices. Then, proportional allocation was carried out based on the number of healthcare providers present during the data collection period. Finally, participants were selected using a simple random sampling technique utilizing a sampling frame list provided by their respective human resources offices.
Study variables
The outcome variable of the study was IPCs which were measured either good or poor. The assessment of healthcare provides infection prevention practices encompassed various measures, including hand hygiene practices, waste management and handling practices, use of PPEs, and vaccination history of the participants against hepatitis immunization. On the other hand, the independent variables of the study were socio-demographic factors of the respondents (age, sex, marital status, working experience, etc.), behavioral and organizational factors (such as training of IPC, Presence of IPC committee, health and safety supervision, availability of infection prevention guidelines in their working departments, availability of PPE, etc.), knowledge, and attitude of IPCs.
Data collection tools and techniques
Data collection was performed using a structured questionnaire that was pre-tested and adapted from existing published articles and contextualized based on the study setting (16, 19–21). The questionnaire was initially created in English, then translated into Amharic, and subsequently back-translated into English to ensure consistency. The questionnaire included questions on respondents’ socio-demographic characteristics, as well as behavioral and institutional factors, knowledge, attitudes, and infection prevention and control (IPC) measures. Data were collected through face-to-face interviews and observations, carried out by four environmental health professionals under the supervision of two public health experts.
Data measurements
To assess the IPC of the healthcare providers, a set of 12 IPC-related questions were used with the option of either yes or no options. A score of 1 point was given to respondents who reported performing the specific IPC, while a score of 0 was given to those who did not perform it. Therefore, the overall score for IPC ranges from 0 to 12 and respondents who scored 80% or above were declared as having good infection prevention practices. On the contrary, respondents who scored below 80% were considered to have poor adherences infection prevention practices (22, 23).
Knowledge of IPC was measured using 10 questions with either “correct” or “incorrect” responses. For each knowledge-based question, respondents were given 1 point was given for correct response and 0 for an incorrect response. The overall knowledge score of the respondents were in the range of 0 to 10. Respondents who scored 80% or above were considered as having a good knowledge on adherence of infection prevention practices. On the contrary, HCWs who scored below 80% were considered as poor knowledge of IPC (22, 23).
Attitude HCWs on IPC was assessed using 10 items using a Likert scale with three options: disagree, agree, and neutral. For positive statements, those who responded “agree” were given three points, “neutral” responses were given two points, and “disagree” responses were given one point and vice versa for negative statements. Generally, respondents’ attitude scores ranged from 10 to 30 and those who scored 80% or higher were considered to have a favorable attitude whereas scored less than 80% were considered as having unfavorable attitude (23).
Data quality assurance
Before starting the final data collection, a two-day training was given for both data collectors and supervisors. The contents of the training includes study objectives, clarity of the questionnaire, data collection procedures, and other related points. The content validity of the questionnaire was assessed using a pre-test with 5% of healthcare workers (21 HCWs) at Woldia General Hospital. Feedback from this pre-test was taken into account for final questionnaire, leading to necessary amendment of the questionnaire. During the process, close supervision was implemented to intervene any issues, with prompt corrections made for any incomplete or missing data to ensure data quality. Additionally, a random sample of 10% was selected for an extra data entry check to reduce potential errors.
Data management and analysis
Data were entered into Epi-Data version 4.6 and exported to the Statistical Package for Social Sciences (SPSS) version 25 for data cleaning and analysis. The study findings were presented using descriptive statistics based on the nature of the data. The association between independent and dependent variables was assessed through binary logistic regression analysis, utilizing a 95% confidence interval. The strength of the association was expressed as odds ratios (OR) along with their corresponding 95% confidence intervals (CI). In bi-variable logistic regression analysis, independent variables with p-values less than 0.25 were retained for multivariable logistic regression analysis to account for potential confounders. The adjusted odds ratio (AOR) with 95% confidence intervals and a p-value under 0.05 were used to determine the significance of associations in the multivariable model. Model fitness was tested using the Hosmer and Lemeshow test; a p-value greater than 0.05 indicated a good fit. Reliability coefficients were assessed using Cronbach’s alpha, with values for knowledge, attitude, and practices related to infection prevention being 0.875, 0.756, and 0.821, respectively, all exceeding 0.7, which indicates acceptable reliability.
Results
Socio-demographic, behavioral, and organization-related characteristics of the HCWs
This study included 408 healthcare workers with a response rate of 96.7%. The mean age of the respondents was 33.03 ± 6 years. The majority, 50.5% (206), were female, and 45.8% (187) belonged to the age group of 31 to 40 years old. The majority of the respondents’ married 61.3% (250), and 43.4% (177) had an educational qualification of master’s degree and above. One-third 32.8% (134) of the HCWs have received training on infection prevention practices and 58.8% (240) had functional infection prevention committees while 74.5% (304) did not have infection prevention guidelines in their working healthcare facilities. Finally, more than two-thirds 68.9% (281) of the healthcare workers reported the lack of personal protective equipment in their working departments of healthcare facilities (Table 1).
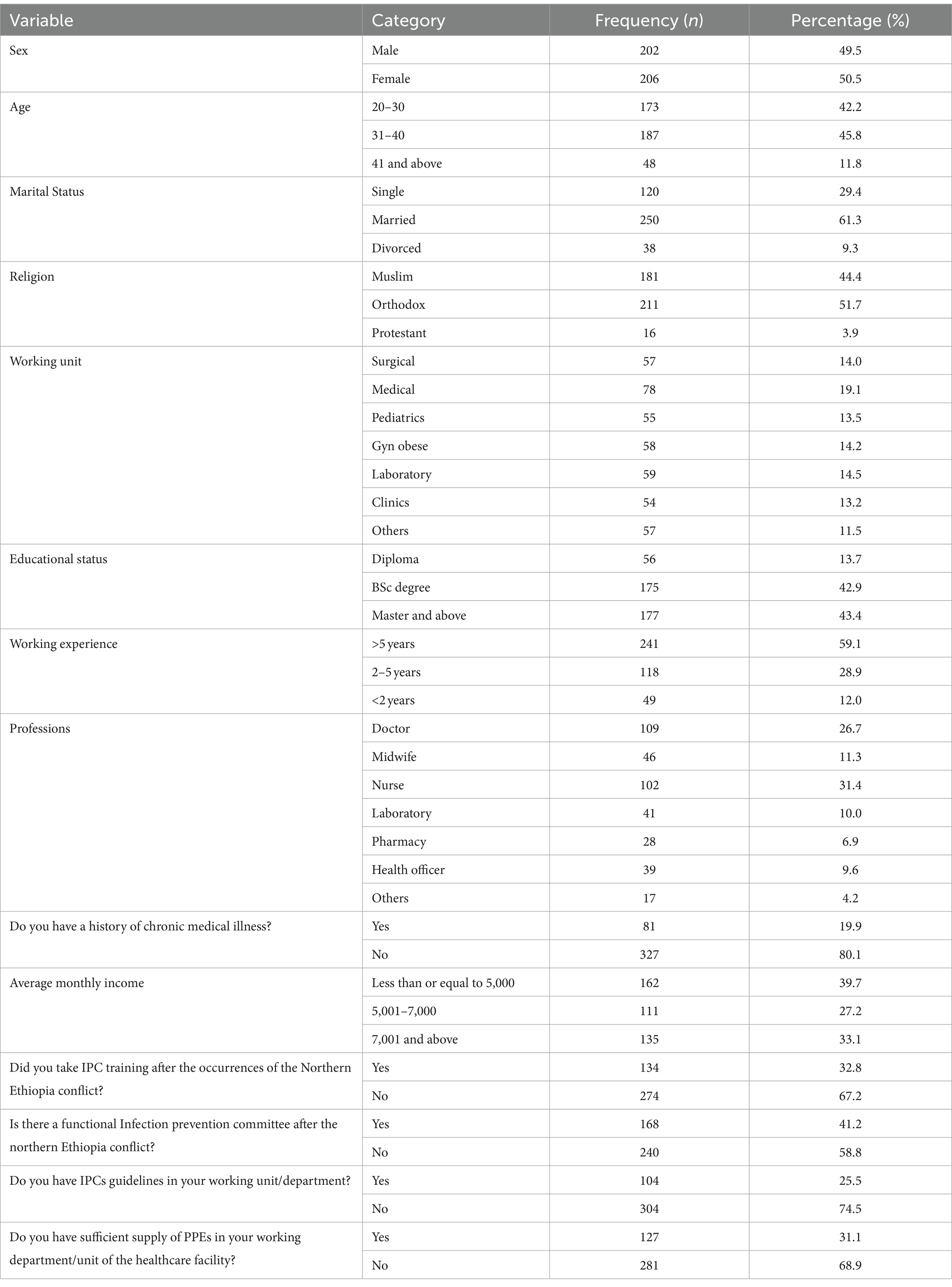
Table 1. Socio-demographic, behavioral, and organizational characteristics of the healthcare workers in South Wollo Zone, Northeastern Ethiopia, following the Northern Ethiopia conflict from June 1 to 30, 2022 (n = 408).
Knowledge of the HCWs on infection prevention practices
In this study, a substantial most of the participants, 96.1% (392) of participants had good knowledge of IPC. The average knowledge score of the respondents was 8.8 ± 1.0, with scores ranging from 7 to 10. Additionally, nearly one-third, 36.0% of the respondents knew that wearing gloves cannot replace the use of hand washing. It was found that only two-thirds of the participants, 273 (66.9%), recognized the need for administering post-exposure prophylaxis within 72 h to prevent the transmission of HCAIs. Moreover, less than half of the respondents, 165 (40.4%), were knowledgeable about the increased risk of nosocomial infections associated with an extended healthcare stay (Table 2).
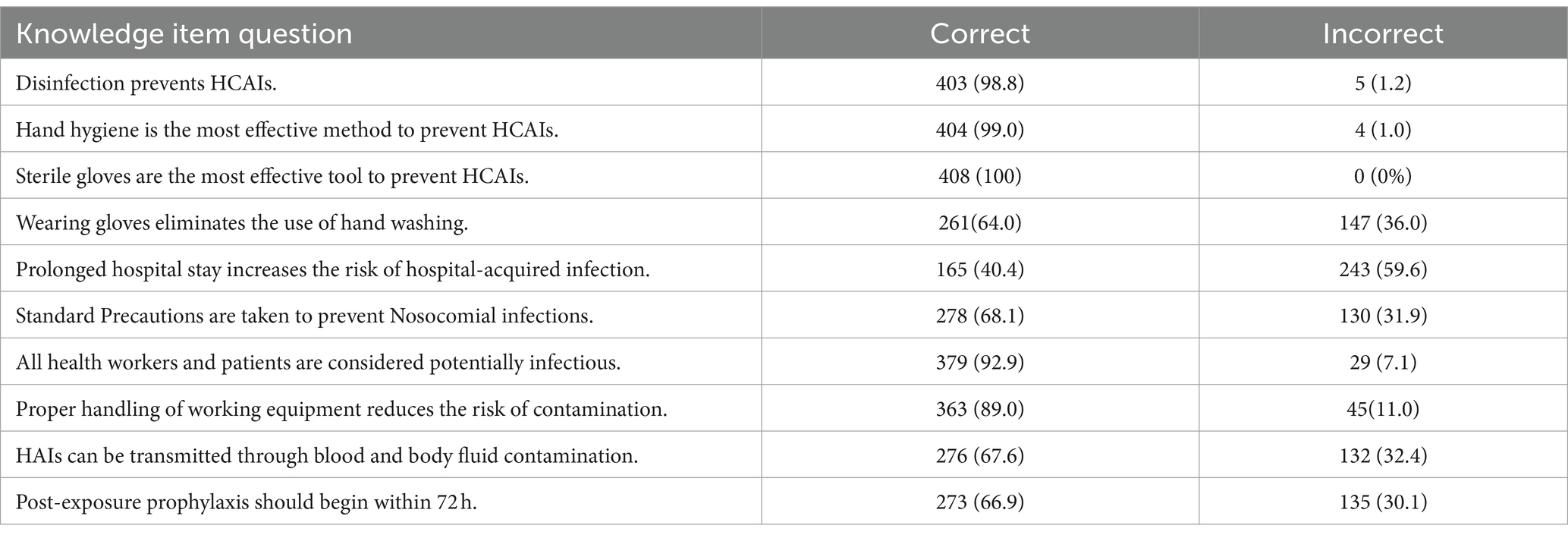
Table 2. Healthcare worker’s knowledge of infection prevention practices in South Wollo Zone, Northeastern Ethiopia, following the northern Ethiopia conflict from June 1 to 30, 2022.
Attitude of HCWs on infection prevention practices
This study revealed that slightly more than three-quarters, 315 (77.2%) of the respondents showed a favorable attitude toward infection prevention practices. The mean score of attitude was 24.7 ± 1.6, out of a total score of 30. Approximately, one-third 127 (31.1%) of the respondents agreed that implementing standard operating procedures in healthcare settings reduces the risk of HCAIs. Moreover, slightly more than three-quarters of 79.9% (326) of the respondents agreed that proper ventilation through the opening of doors and windows can minimize the risk of HAIs. Finally, slightly more than one-third, 39.0% (159) of the participants acknowledged that nosocomial infections have serious consequences for healthcare providers (HCPs) (Table 3).
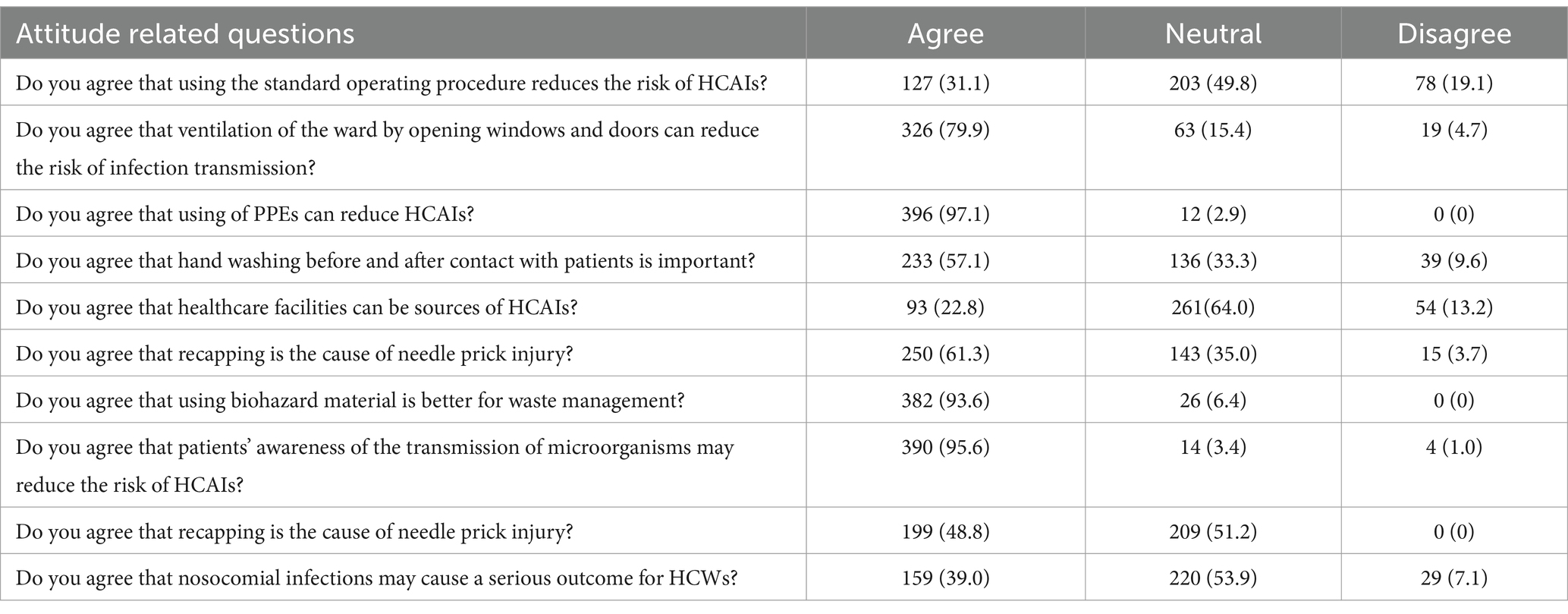
Table 3. Attitude of HCWs on infection prevention practices in South Wollo Zone, Northeastern Ethiopia, following the Northern Ethiopia conflict from June 1 to 30, 2022.
Infection prevention practice on HCWs
This study revealed that slightly more than half, 53.7% (219) of the respondents demonstrated safe infection prevention practices. The average score for infection prevention practices was 19.5 ± 1.4 (SD). Among all participants, 75.5% (308) reported washing their hands before providing patient care, 81.4% (334) used soap and water for hand washing, and 96.8% (395) washed their hands after coming into contact with body fluids. However, less than three-quarters of the participants, 72.8% (297), practiced segregation of healthcare waste at the point of generation based on its characteristics. Additionally, half of the respondents 49.5% (202), disposed of needles or sharps wastes in safety boxes and discarded these boxes when they were three-quarters full. Finally, less than two-thirds of the respondents, 60.3% (246), had received vaccination against the Hepatitis B virus (Table 4).
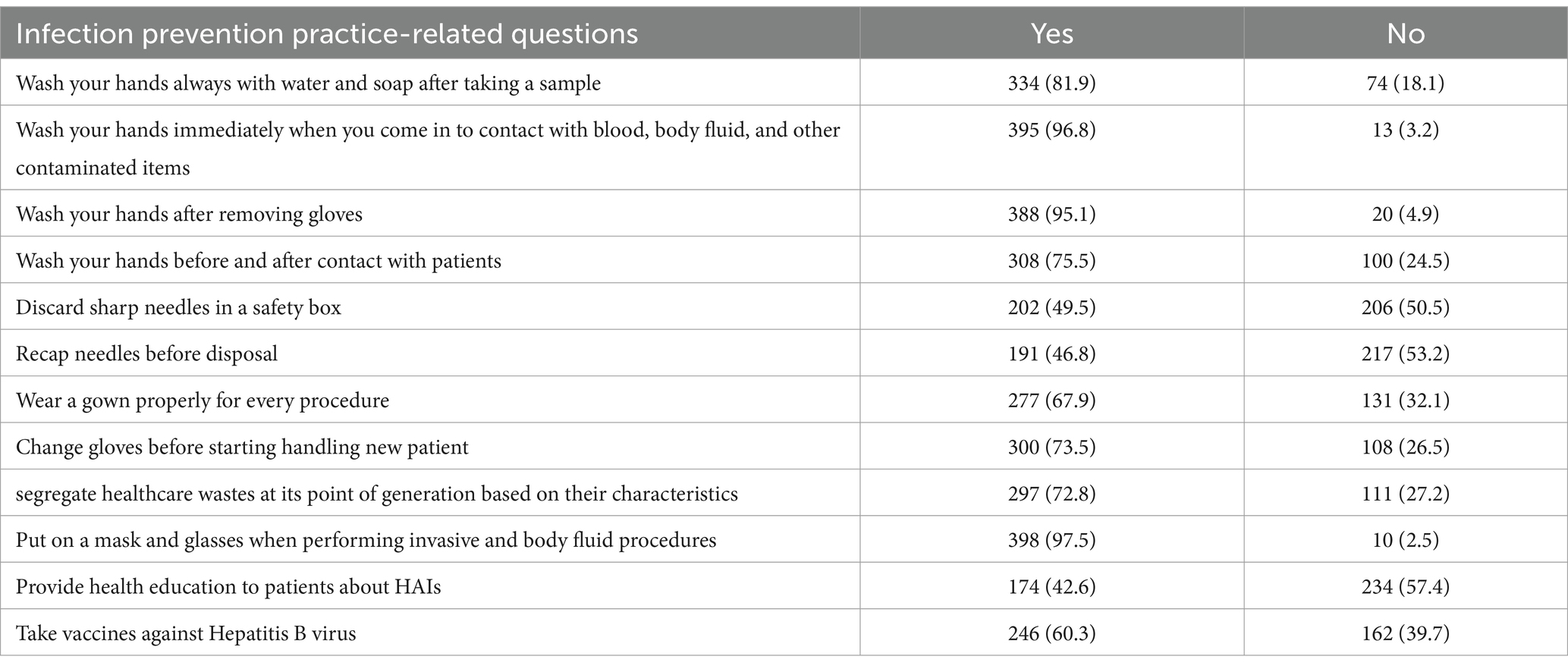
Table 4. Infection prevention practice among HCWs in South Wollo Zone, Northeastern Ethiopia, following the Northern Ethiopia conflict from June 1 to 30, 2022.
Factors associated with infection prevention practices among HCPs
In the multivariable logistic regression analysis, receiving training on IPC, the presence of a functional infection prevention committee, and the availability of infection prevention guidelines and personal protective equipment in the working departments of their healthcare settings were factors significantly associated with IPC of Healthcare workers.
HCWs who had received training on IPC had 2.662 times better IPCs compared to those who had not received the training (adjusted odds ratio [AOR] = 2.662, 95% confidence interval [CI]: 1.361, 5.120). Similarly, respondents with a functional infection prevention committee in their working departments had 2.203 times better IPCs compared to those who did not have such a committee (AOR = 2.203, 95% CI: 1.359, 3.572). Additionally, HCWs with infection prevention guidelines in their working departments had 2.090 times better infection prevention practices compared to those who did not have access to these guidelines (AOR = 2.090, 95% CI: 1.013, 4.312). Finally, respondents who had sufficient supplies of PPE in their working departments were 2.773 times more likely to implement safe IPC compared to those who did not have an adequate supply of these essential PPEs (AOR = 2.773, 95% CI: 1.560–4.929) (Table 5).
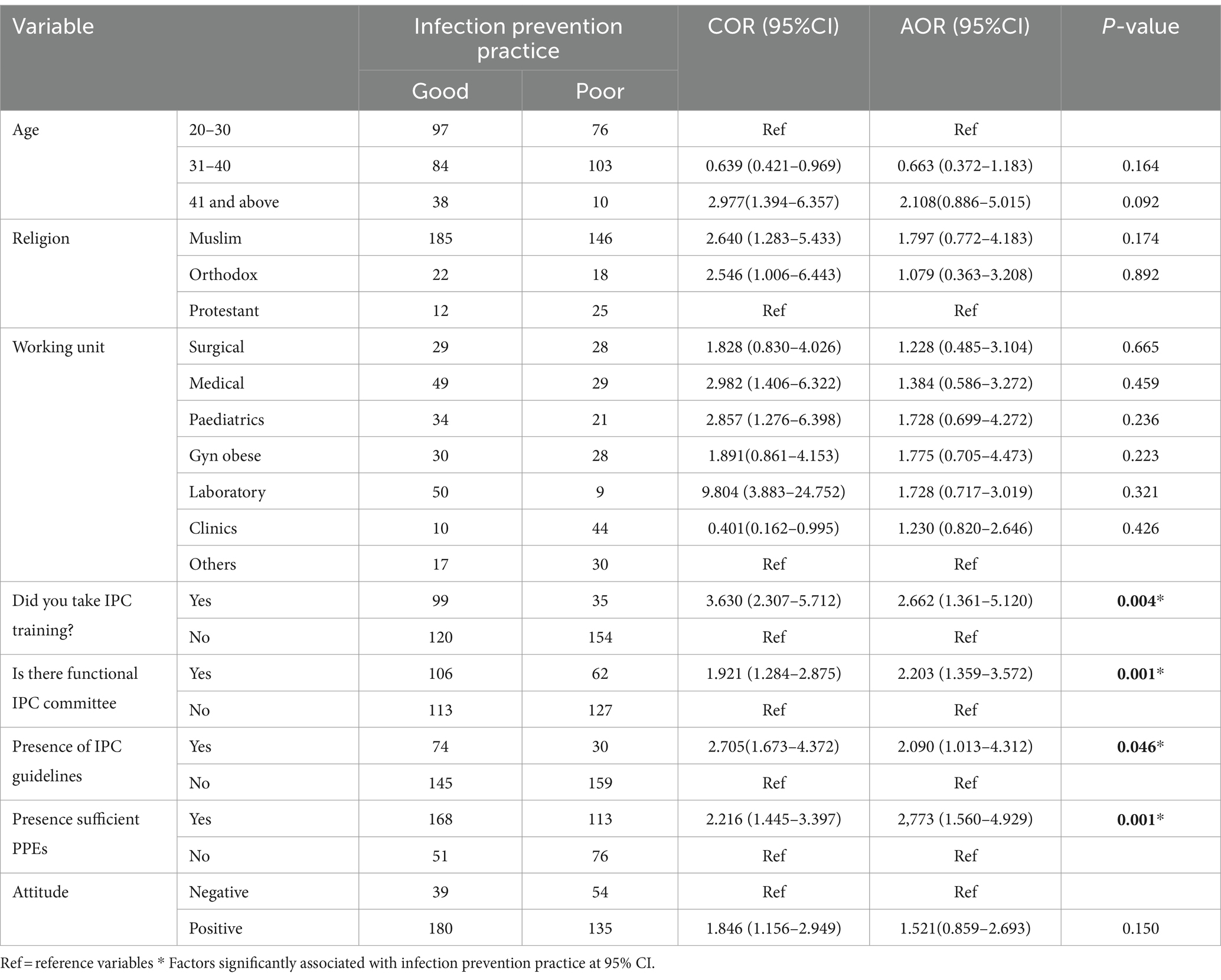
Table 5. Factors associated with infection prevention practice among healthcare workers in South Wollo Zone, Northeastern Ethiopia, following the Northern Ethiopia conflict, June 1–30, 2022.
Discussion
In Africa, the combination of endemic poverty and fragile health systems magnifies the adverse impacts of armed conflicts in the region. Conflict-prone areas are highly vulnerable to the re-emergence of infectious diseases caused by a shortage of healthcare personnel, inadequately equipped facilities, disrupted medical supply chains, limited access to health services, including preventive and curative interventions, and inadequate water and sanitation facilities (5, 24). The impact of these diseases has been further intensified by the presence of armed conflicts, resulting in severe and long-lasting consequences (5).
Globally, HCAIs continue to be a significant contributor to patient illness and death. Therefore, Implementation of a good IPC plays a crucial in ensuring the quality of care and safeguarding healthcare workers, patients, and communities from substantial risks (15, 25). The results of this study indicated that the respondents’ overall knowledge score regarding infection prevention practices was 88%, which is in line with studies done in Ethiopia (84.6%) (10). However, this score was higher compared to studies conducted in Ethiopia (76%) (26), (53.7%) (27), and Nigeria (16.6%) (28). More than three-quarters (86.1%) of the participating healthcare workers (HCWs) showed good knowledge, which aligns with studies conducted in Saudi Arabia (81%) (29), and Ethiopia (86% (30), 84.7% (10)). Conversely, it was lower compared to studies conducted in Bangladesh (37.5%) (31), Trinidad and Tobago (20.3%) (32), Palestine (53.9%) (22), Saudi Arabia (67.6%) (23), and Ethiopia (53.7% (27), 55.4% (33), and 60.4%) (34). However, it should be noted that this finding was higher than studies conducted in Ethiopia (90%) (11), (95.19%) (35). The variations observed in these findings may be attributed to differences in sample size, study context, composition of study participants, and the availability of ongoing awareness programs on infection prevention practices conducted by healthcare workers.
This finding also disclosed that approximately three-quarters of the participants showed a positive attitude towards infection prevention, which aligns with a study conducted in Ethiopia (76.4%) (30). However, this finding was slightly lower compared to studies conducted in Saudi Arabia (82%) (29) and Ethiopia (83.3%) (33). On the contrary, this finding was it was higher than studies conducted in Trinidad and Tobago (46.7%) (32), Saudi Arabia (61.5%) (23), and Ethiopia (57.2%) (11).These differences may be attributed due to variations in the study setting, duration, and the socio-demographic characteristics of the study populations.
More than half (53.7%) of the respondents reported safe infection prevention practices which was lower than studies done in Riyadh, Saudi Arabia (59%) (29), Palestinian (91.1%) (22), Saudi Arabia (61.5%) (23), and Ethiopia (60.4%) (34), (87.5%) (35), and (66.1%) (33). On the contrary, this result was higher than studies conducted in Bangladesh (39.1%) (31), Trinidad and Tobago (44.0%) (32), and Ethiopia (36.5%) (27), (36%) (11), (36.7%) (19). These variations could be attributed to variations in the composition of the study participants, the level of healthcare settings (being health centers, hospitals, and others) the location and timing of the study, the availability of essential PPEs, and the method of data collection.
Lack of resources in healthcare settings emerged as a significant challenge to implement safe IPCs, particularly in conflict-affected settings due to the destruction of essential healthcare facilities. These facilities include a lack of hospital furniture, limited availability of medicines, essential supplies for IPCs, including (PPEs), hand hygiene products, and cleaning equipment. Therefore, the lack of PPEs in healthcare settings plays a crucial role in the spread of healthcare-associated infections (9, 36).
The current finding revealed that lack of PPEs was one of the factors in implementing a safe IPC among healthcare workers which was supported by previous studies conducted in Ethiopia (10, 19, 32), Bangladesh (31), and India (36). Despite the responses to the ongoing coronavirus pandemic providing important lessors for IPC programs in resource-limited and conflict-affected settings, implementing safe infection prevention practices is still in a backward position due to the lack of essential facilities and services due to the ongoing destruction in the conflict process (9). Therefore, both parties of the combatants should ensure the safety of these essential facilities to provide better healthcare services for both parties of the conflict and the communities as a whole. Therefore, concerned governmental and non-governmental organizations should closely follow the process and facilitate and design a timely intervention (9).
The provision of continuous awareness creation sessions on infection prevention practices among healthcare providers plays a vital role in implementing safe infection prevention practices to reduce the burden of HCAIs (36). In conflict-affected regions, regular in-service training, including hands-on practical sessions and consistent monitoring and supervision of staff, is acknowledged as an effective strategy to enhance IPC practices (9). The finding of this study also supports that the implementation of updated training on infection prevention practices was another factor which affected in implementation of safe infection prevention practices which was supported by other previous findings done in Ethiopia (10, 26, 27), India (36), and Saudi Arabia (23). Training programs based on updated guidelines have the potential to enhance the knowledge, skills, and confidence of healthcare workers, enabling them to effectively implement better infection prevention practices, particularly in resource-limited settings due to the damage of essential facilities (9).
WHO released guidelines regarding IPC at national and facility levels which are designed to be applicable in all countries and healthcare settings. Nevertheless, its implementation universally can significantly vary based on the unique circumstances and conditions of each situation (9). The results of this study demonstrate that the utilization of infection prevention guidelines in working departments served as an additional contributing factor in the successful implementation of effective infection prevention practices. This finding aligns with previous research conducted in Ethiopia, (10, 27, 33), Riyadh, Saudi Arabia (29), and India (36) highlighting the importance of following established guidelines to ensure the safety of infection prevention measures. However, during periods of critical circumstances such as armed conflicts, the implementation of these guidelines becomes challenging due to the destruction of vital facilities. In such situations, the presence of a functional IPC committee becomes crucial as it offers a platform for interdisciplinary involvement, cooperation, and the exchange of information. These facilitates are fundamental for the successful implementation of safe infection prevention practices despite the difficult circumstances (22, 34). The availability of an infection prevention and control (IPC) committee is a fundamental initial action in establishing an IPC program, especially in settings impacted by conflict (9). The results of this study indicate that the presence of a functional IPC committee is a significant influencing factor in ensuring the safe implementation of infection prevention measures. This finding is consistent with previous research conducted in various conflict-affected countries, further supporting the importance of having a well-functioning IPC committee in such contexts (9). The findings of this study will provide insight into humanitarian interventions and serve as input for government and other stakeholders in designing evidence-based health interventions for conflict-affected areas. It will also serve as baseline evidence for further investigation in the area.
Limitations of the study
This study has certain limitations. Initially, the use of a cross-sectional design makes it challenging to establish a definitive cause-and-effect relationship between the dependent and independent variables under investigation. Secondly, the measurement of infection prevention practices relied on self-reported responses from the participants, which may introduce the possibility of social desirability bias influencing the accuracy of the data.
Conclusion
In conclusion, slightly more than half of the healthcare workers exhibited good adherence to infection prevention practices. Regarding to factors, existence of a functioning infection prevention committee, utilizing of infection prevention guidelines in their working department, availability of personal protective equipment (PPE) in their departments, and received training on infection prevention and control were factors significantly associated with adherences of infection prevention among healthcare workers. Therefore, it is recommended that ongoing awareness program should be implemented to enhance their knowledge and practices. Additionally, donor organizations in collaboration with government organization should ensure a sufficient supply of PPE to support healthcare workers in improving their infection prevention efforts during this critical period. For a more comprehensive understanding, future research should adopt a mixed-methods approach that integrates both qualitative and quantitative methods to gather in-depth information.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study received approval from the Ethical Review Committee of Wollo University, College of Medicine and Health Sciences, with the reference number RCSPG-156/14. Permission was obtained from the South Wollo Zone Health Department. Prior starting the data collection, informed consent was obtained from all participants after explaining the purpose of the study. Confidentiality was strictly maintained by avoiding the use of any potential identifiers, such as participants' names. All information provided by the participants was treated as confidential. Participants were informed of their rights, including the option to decline participation, withdraw from the study, or withhold information. The study was conducted in accordance with the principles outlined in the Helsinki Declaration.
Author contributions
GB: Formal analysis, Methodology, Writing – original draft, Supervision. AG: Formal analysis, Software, Supervision, Validation, Writing – review & editing. LB: Conceptualization, Data curation, Supervision, Visualization, Writing – review & editing. BS: Conceptualization, Data curation, Supervision, Writing – review & editing. BA: Software, Supervision, Writing – review & editing. ZW: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. MA: Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. KG: Formal analysis, Methodology, Writing – review & editing, Conceptualization, Funding acquisition, Investigation, Resources, Software, Validation, Visualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The fund of this research was covered by Wollo University.
Acknowledgments
First of all, we would like to convey our sincerest appreciation to Wollo University for providing the necessary funding for this research project. Additionally, we would like to express our gratitude to the data collectors, supervisors, and study participants for their dedicated efforts, which were instrumental in the completion of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AOR, adjusted odd ration; CI, confidence interval; COR, crude odd ratio; HCAIs, Healthcare Acquired infections; HCFS, Health care facilities; HCPS, Healthcare workers; IPC, Infection prevention and control; UNICEF, United Nations Child Fund; WASH, Water Sanitation and Hygiene; WHO, World Health Organization.
References
1. Arage, MW, Kumsa, H, Asfaw, MS, Kassaw, AT, Dagnaw, EM, Tunta, A, et al. Exploring the health consequences of armed conflict: the perspective of Northeast Ethiopia, 2022: a qualitative study. BMC Public Health. (2023) 23:2078. doi: 10.1186/s12889-023-16983-z
2. Arage, MW, Kumsa, H, Asfaw, MS, Kassaw, AT, Dagnaw, EM, Tunta, A, et al. Assessing the health consequences of northern Ethiopian armed confict, 2022. J Public Health Policy. (2024) 45:43–57. doi: 10.1057/s41271-023-00464-z
3. Ekzayez, A, Ahmad, YA, Alhaleb, H, and Checchi, F. The impact of armed confict on utilisation of health services in north-West Syria: an observational study. Confl Heal. (2021) 15:91. doi: 10.1186/s13031-021-00429-7
4. Awojobi, ON. The impact of conflict on health outcomes: a systematic evidence from sub-Saharan Africa. Mgbakoigba J Afr Stud. (2019) 8:88–100.
5. Tekulu, F.B., Gebre, H.T., Hailu, H.G., Asgedom, D.B., Desta, G.M., Shifare, T.H., et al.et.al. The effect of war on health institutions of eastern Tigray zone, Tigray state, Ethiopia. Ethiopia J Health Commun. (2023). [Preprint].
6. Bardossy, AC, Zervos, J, and Zervos, M. Preventing Hospitalacquired infections in low-income and middle-income countries: impact, gaps, and opportunities. Infect Dis Clin N Am. (2016) 30:805–18. doi: 10.1016/j.idc.2016.04.006
7. Kodo, TK, Kidie, AB, Merecho, TH, Tiruneh, MG, Yayeh, BM, and Getaneh, BA. The impact of armed conflict on services and outcomes related to maternal and reproductive health in north Wollo, Amhara, Ethiopia: a qualitative study. Int J Women's Health. (2024) 16:1055. doi: 10.2147/IJWH.S457529
8. World Health Organization. Global strategy on infection prevention and control. Geneva: World Health Organization (2023).
9. Lowe, H, Woodd, S, Lange, IS, Janjanin, S, Barnet, J, and Graham, W. Challenges and opportunities for infection prevention and control in hospitals in confict-afected settings: a qualitative study. Confict Health. (2021) 15:94. doi: 10.1186/s13031-021-00428-8
10. Desta, M, Ayenew, T, Sitotaw, N, Tegegne, N, Dires, M, and Getie, M. Knowledge, practice and associated factors of infection prevention among healthcare workers in Debre Markos referral hospital, Northwest Ethiopia. BMC Health Serv Res. (2018) 18:465. doi: 10.1186/s12913-018-3277-5
11. Bayleyegn, B, Mehari, A, Damtie, D, and Negash, M. Knowledge, attitude and practice on hospital-acquired infection prevention and associated factors among healthcare Workers at University of Gondar comprehensive specialized hospital, Northwest Ethiopia. Infect Drug Resist. (2021) 14:259. doi: 10.2147/IDR.S290992
12. Tirivanhu, C., Estele, M., Elizabeth, T., and Chipo, C.. Knowledge and practices of healthcare workers in prevention and control of hospital-acquired infections in the maternity Department at Bindura Provincial Hospital, (Zimbabwe: International Journal of Infection Control). (2023).
13. Abalkhail, A, and Alslamah, T. Institutional factors associated with infection prevention and control practices globally during the infectious pandemics in resource-limited settings. Vaccine. (1811) 10:10. doi: 10.3390/vaccines10111811
14. Alemu, AY, Endalew, A, and Bayih, WA. The burden of healthcare-associated infection in Ethiopia: a systematic review and meta-analysis. Tropical. Med Health. (2020) 48:77. doi: 10.1186/s41182-020-00263-2
15. Tesfaye, AH, Mekonnen, TH, Desye, B, and Yenealem, DG. Infection prevention and control practices and associated factors among healthcare cleaners in Gondar City: an analysis of a cross-sectional survey in Ethiopia. Risk Manag Healthc Policy. (2023) 16:1317–30. doi: 10.2147/RMHP.S419110
16. Murray, CJL, King, G, Lopez, AD, and TomijimaN, KEG. Armed conflict as a public health problem education and debate. BMJ. (2002) 324:346–9. doi: 10.1136/bmj.324.7333.346
17. Hassen, SL, Astatkie, A, Mekonnen, TC, and Bogale, GG. Survival status and its determinants among under-five children with severe acute malnutrition admitted to inpatient therapeutic feeding centers in south Wollo zone, Amhara region, Ethiopia. J Nutr Metab. (2019) 2019:1–9. doi: 10.1155/2019/2643531
18. Abebe, A Federal Democratic Republic of Ethiopia central statistical agency population projection of Ethiopia for all regions at Wereda level from 2014–2017. Federal Demographic Republic of Ethiopia Central Statistical Agency: Population Projection of Ethiopia for All Regions At Wereda Level from 2014 – 2017. (2013).
19. Zenbaba, D, Sahiledengle, B, and Bogale, D. Practices of healthcare workers regarding infection prevention in bale zone hospitals, Southeast Ethiopia. Hindawi Adv Public Health. 2020:4198081. doi: 10.1155/2020/4198081
20. Jiménez, A, Livsey, J, Åhlén, I, Scharp, C, and Takane, M. Global assessment of accountability in water and sanitation services using GLAAS data. Water Alternat. (2018) 11:238–59.
21. Assefa, J, Diress, G, and Adane, S. Infection prevention knowledge, practice, and its associated factors among healthcare providers in primary healthcare unit of Wogdie District, Northeast Ethiopia, 2019: a cross-sectional study. Antimicrob Resist Infect Control. (2020) 9:136. doi: 10.1186/s13756-020-00802-w
22. Fashafsheh, I, Ayed, A, Eqtait, F, and Harazneh, L. Knowledge and practice of nursing staff towards infection control measures in the Palestinian hospitals. J Educ Pract. (2015) 6:79–90.
23. Abalkhail, A, Al Imam, MH, Elmosaad, YM, Jaber, MF, Hosis, KA, Alhumaydhi, FA, et al. Knowledge, attitude, and practice of standard infection control precautions among health-Care Workers in a University Hospital in Qassim, Saudi Arabia: a cross-sectional survey. Int J Environ Res Public Health. (2021) 18:11831. doi: 10.3390/ijerph182211831
24. Haddison, EC, Chia, E, Julius, CE, and Kagina, BM. Health services utilisation before and during an armed conflict; experiences from the southwest region of Cameroon. Open Public Health J. (2020) 13:547–54. doi: 10.2174/1874944502013010547
25. Sifir, CK. Infection prevention practices and associated factors among healthcare Workers in Governmental Hospitals in Addis Ababa, Ethiopia. Adv Sex Reprod Health Res. (2022) 2:190–6.
26. Amsalu, A, and Kassaye, H. Healthcare workers’ compliance and factors for infection prevention and control precautions at Debre Tabor referral hospital, Ethiopia. PAMJ One Health. [research square]. (2022) 7:32202. doi: 10.11604/pamj-oh.2022.7.35.32202
27. Geberemariyam, BS, Donka, GM, and Wordofa, B. Assessment of knowledge and practices of healthcare workers towards infection prevention and associated factors in healthcare facilities of west Arsi District, Southeast Ethiopia: a facility-based cross-sectional study. Arch Public Health. 76:69. doi: 10.1186/s13690-018-0314-0
28. Oluwagbemiga, AO, Akinsete, SJ, Ana, GR, and Gunseye, OO. Knowledge, attitude and self-reported practice of healthcare workers on infection control in a health facility in Akure, Nigeria. Int J Infect Control. (2021) 17:20818. doi: 10.3396/ijic.v17.20818
29. Alshathri, N. Knowledge, attitude and practice regarding infection control measures among healthcare Workers at King Khaled eye Specialist Hospital (KKESH) in Riyadh, KSA. Res Squ. (2021). doi: 10.21203/rs.3.rs-958840/v1
30. Gezie, H, Leta, E, Admasu, F, Gedamu, S, and Dires, A. Health care workers' knowledge, attitude, and practice towards hospital-acquired infection prevention at Dessie referral hospital, Northeast Ethiopia. Clin J Nurs Care Pract. (2019) 3:059–63. doi: 10.29328/journal.cjncp.1001019
31. Hsan, K, Islam, MS, Islam, MZ, Awal, N, Gozal, D, MMM, K, et al. Healthcare providers infection prevention practices and associated factors in community clinics in Bangladesh: a cross-sectional study. PLoS Glob Public Health. (2022) 2:e0000574. doi: 10.1371/journal.pgph.0000574
32. Unakal, CG, Nathaniel, A, Keagan, B, Alexandria, B, Lauralee, B, Chatoo, VC, et al. Assessment of knowledge, attitudes, and practices towards infection prevention among healthcare workers in Trinidad and Tobago. International journal of community medicine and public health Unakal CG et al. Int J Community Med Public Health. (2017) 4:2240–7. doi: 10.18203/2394-6040.ijcmph20172813
33. Sahiledengle, B, Gebresilassie, A, Hiko, D, and Getahun, T. Infection prevention practices and associated factors among healthcare Workers in Governmental Healthcare Facilities in Addis Ababa, Ethiopia. Ethiop J Sci. (2018) 28:177–86. doi: 10.4314/ejhs.v28i2.9
34. Sado, MH, Fasil, N, and Bekere, A. Assessment of infection prevention practice and associated factors among healthcare providers in the case of Bishoftu referral hospital. Clin Med Res. (2021) 10:212–24. doi: 10.11648/j.cmr.20211006.17
35. Alemayehu, R, Ahmed, K, and Sada, O. Assessment of knowledge and practice on infection prevention among health Care Workers at Dessie Referral Hospital, Amhara region, south Wollo zone, North East Ethiopia. J Community Med Health Educ. (2016) 6:487. doi: 10.4172/2161-0711.1000487
Keywords: healthcare workers, infection prevention practices, healthcare facilities, conflict, Northern Ethiopia
Citation: Berihun G, Gizeyiatu A, Berhanu L, Sewunet B, Ambaw B, Walle Z, Abebe M and Gasheya KA (2024) Adherence to infection prevention practices and associated factors among healthcare workers in Northeastern Ethiopia, following the Northern Ethiopia conflict. Front. Public Health. 12:1433115. doi: 10.3389/fpubh.2024.1433115
Edited by:
Kun-Shan Wu, Tamkang University, TaiwanReviewed by:
David Brett-Major, University of Nebraska Medical Center, United StatesPatrizia Laurenti, Catholic University of the Sacred Heart, Italy
Copyright © 2024 Berihun, Gizeyiatu, Berhanu, Sewunet, Ambaw, Walle, Abebe and Gasheya. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kassahun Ayele Gasheya, YXN0ZWRla2Fzc2FodW5AZ21haWwuY29t
†ORCID: Gete Berihun, orcid.org/0000-0002-5511-2072
 Gete Berihun
Gete Berihun Adinew Gizeyiatu
Adinew Gizeyiatu Leykun Berhanu
Leykun Berhanu Birhanu Sewunet1
Birhanu Sewunet1 Zebader Walle
Zebader Walle Kassahun Ayele Gasheya
Kassahun Ayele Gasheya