- 1Faculty of Medicine, Veterinary Medicine, and Life Sciences, University of Glasgow, Glasgow, United Kingdom
- 2College of Education Sciences, The Hong Kong University of Science and Technology, Guangzhou, Guangzhou, China
- 3School of Psychology, Shenzhen University, Shenzhen, China
- 4School of Physical Education and Sports Science, Soochow University, Suzhou, China
Background: 24-h movement guidelines (24-HMG) play an important role in various demographics such as early years, children, youth, and the older adult. Nevertheless, most existing research exploring the links between socioeconomic factors, dietary intake, and substance use with sleep patterns, physical activity (PA), and sedentary behavior (SB) has been conducted in high-income Western countries.
Purpose: Hence, this study seeks to investigate the relationship between adherence to the 24-HMG and smoking and alcohol use behaviors among children and adolescents in China.
Methods: A comprehensive survey, in collaboration with the Municipal Education Commission, was carried out across primary and middle schools in Shenzhen, China. Sleep duration was gauged using the Pittsburgh Sleep Quality Index (PSQI), screen time was assessed with items adapted from the Health Behavior of School-aged Children (HBSC) survey, and PA was measured using a single item adapted from the HBSC survey. Results were presented as odds ratios (ORs) with 95% confidence intervals (CIs), considering p-values below 0.05 as statistically significant.
Results: Among the sample, 51.9% were boys and 48% were girls. Those who did not meet any guidelines had a higher probability of smoking (OR = 1.62 [95% CI: 1.03, 2.56], p = 0.037) among children and adolescents. Conversely, meeting one (OR = 0.94 [95% CI: 0.61, 1.52], p = 0.874) or two guidelines (OR = 0.84 [95% CI: 0.52, 1.34], p = 0.459) showed no significant impact. The data displayed an inverse correlation between the number of guidelines adhered to and the likelihood of alcohol use among children and adolescents: none (OR = 2.07, p < 0.001), one guideline (OR = 1.40, p = 0.006), and two guidelines (OR = 1.22, p = 0.106).
Conclusion: Not meeting guidelines elevates smoking and alcohol use risks in children and adolescents, whereas following more guidelines lowers these risks, highlighting the importance of guideline adherence in reducing substance use.
1 Introduction
Regular participation in physical activity (PA) elicits a multitude of health benefits, encompassing enhanced muscular and cardiorespiratory fitness, facilitation of optimal bone mineralization (1–4), augmentation of subjective well-being (e.g., self-perception, self-esteem, and affective state), and mitigation of psychopathological symptoms (e.g., depression, anxiety, and stress) (5–8). Furthermore, PA is also correlated with heightened cognitive functioning and academic performance (2, 9–11). The World Health Organization (WHO) recommends that children and adolescents engage in at least 60 min of moderate to vigorous-intensity physical activity (MVPA) daily. (12, 13). PA during children and adolescence creates complete health for the youth (4, 14, 15), and also improves cardiovascular health, fitness levels, and the prevention of chronic illnesses (16–18). The positive effect is also extended to the mental realm, as PA serves to reduce symptoms of anxiety and depression. They are also psychologically beneficial, as they improve mood, self-esteem, and general emotional well-being (19). Additionally, sports and other PA are significant for the development of vital life skills such as teamwork, discipline, and perseverance (20, 21). These experiences are very formative and do not affect just health outcomes at that moment, but make a foundation for a healthy active lifestyle in the future (22). Hence, the importance of promoting and encouraging PA amongst youth in fostering their overall well-being cannot be underestimated.
Recent epidemiological studies in PA and related disciplines have increasingly acknowledged the significance of 24-h movement behaviors (2, 23–26). This encompasses PA, sedentary behavior (SB), and sleep, which are recognized as interdependent, wherein alterations in one behavior may impact the others (27, 28). Incorporating an integrated approach to these behaviors in health-related research is paramount. Such an approach facilitates a comprehensive analysis, yielding deeper insights into health outcomes and behavioral modifications. The growing emphasis on these behaviors in research is attributed to the myriad of health benefits associated with each behavior when adhered to at recommended levels.
Intervention experiments have been undertaken with the aim of augmenting PA, mitigating sedentary behavior (SB), and fostering adequate sleep (29–31). Researchers advocate for a minimum of 60 min of MVPA per day, limiting screen time to no more than 2 h daily, and ensuring adequate sleep across all age groups (26, 32). Since 2015, countries including Canada, Australia, New Zealand, and South Africa have released tailored (24-HMG) for various demographics such as early years, children, youth, and the older adult. The 24-HMG for children and adolescents provide a comprehensive framework that balances various behaviors over a 24-h period, recognizing that health is shaped by the cumulative effects of daily routines. These guidelines highlight the significance of incorporating movement behaviors consistently throughout the day to enhance health outcomes (27, 33, 34).
In addition to the association between the volume of PA and SB, research has unveiled the significance of considering a range of sociodemographic, dietary, and substance use factors that might be correlated with particular types of PA and SB (35). Undoubtedly, substance use has emerged as a prominent global public health concern, especially among adolescents, in industrialized and modernized societies for an extended period (36). Frequently misused substances include tobacco, alcohol, and cannabis (37). Studies consistently demonstrate that substance use tends to escalate during adolescence, with this pattern often initiating during this developmental stage and persisting into adulthood (38). In North America, substance use is prevalent among youths. Research by Joung et al. (39) highlights that in 2017, 56.8% of Canadian adolescents aged 15–19 consumed alcohol, compared to one-third of U.S. 12th graders. Additionally, 7.9% of Canadian adolescents smoked tobacco, while about 10% of U.S. 12th graders did the same (40). Drug consumption rates were 21.6% in Canada and 25% in the U.S. among youth (41). Similar trends are evident in other regions, including Australia (42), Thailand (43), and Spain (44). In China, substance use among youth is an increasing concern. Previous studies indicate that approximately 7.3% of Chinese children and adolescents aged 9 to 21 have reported drinking alcohol (45). A systematic review and meta-analysis found that the overall prevalence of smoking among Chinese youth is around 8.2% (46), with a significant increase in smoking rates observed among older adolescents (47).
Given that children and adolescents are in a crucial stage of growth and development, it is vital to prioritize their health behaviors during this time (48). Substance use during these formative years not only negatively affects health outcomes and lifestyle behaviors (49) but also predicts a variety of challenges for young people, including associations with delinquency and criminal behavior (50, 51). Given these significant risks, early prevention starting from primary school children is crucial, as this stage represents a formative period where foundational health behaviors are established, making it a critical time to intervene and mitigate future risks associated with smoking and alcohol use (52). While prior research has focused on adolescents, studies frequently highlight that the relationship between substance use and overall health is inversely related in this population (53). Additionally, sociodemographic factors combined with substance use can influence the 24-h movement behaviors of adolescents, such as increasing SB when alcohol and tobacco are used (54). Conversely, substance use is negatively associated with sleep quality, as demonstrated in a longitudinal study of U.S. adolescents from 1991 to 2014, where alcohol consumption was specifically linked to disrupted sleep patterns (55). Interestingly, previous research has suggested a potential correlation between alcohol use and higher levels of PA, possibly attributed to increased social interactions during sports events where alcohol is frequently consumed (56). Overall, the evidence suggests that while alcohol may encourage more PA, substance use generally promotes SB and impairs sleep, contributing to unhealthy 24-h movement behaviors in young people (57).
Nevertheless, most existing research exploring the links between socioeconomic factors, dietary intake, and substance use with sleep patterns, PA, and SB has been conducted in high-income Western countries (58, 59). This geographic concentration may limit the generalizability of findings, as socio-economic and cultural contexts vary significantly across different regions, potentially affecting sleep and activity patterns in diverse ways. This raises concerns about the applicability of these findings to low-and middle-income regions, particularly in less-developed countries in Asia, Africa, and South America, where cultural norms, legal frameworks, and social structures differ significantly. Recent empirical studies from China have broadened this research scope. Luo et al. (60) examined the relationship between adherence to the 24-HMG and health outcomes in older adult Chinese adults. Following this, Luo et al. (60) investigated how compliance with the 24-HMG affected depression and anxiety in Chinese adolescents. Furthering this line of inquiry, Luo (2024) (61) found that following the Sleep and Physical Activity recommendations of the 24-HMG significantly reduced the risk of visual impairments in non-obese adolescents. Despite these contributions, research in this area remains inadequate given the complexity of the issues involved. More studies are essential to deepen our understanding of how adherence to the 24-HMG affects health outcomes across diverse populations and age groups, especially in varied socioeconomic and cultural settings. Therefore, this study aims to explore the association between adherence to the 24-HMG (Combination of physical activity, screen time and sleep) and smoking and drinking behaviors among Chinese children and adolescents.
2 Methods
2.1 Participants and study design
In March 2021, a large-scale survey was conducted in collaboration with the Municipal Education Commission across primary and middle schools in Shenzhen, China. The survey encompassed students from all local public primary and secondary schools distributed throughout Shenzhen’s districts. Prior studies on PA among Chinese children and adolescents indicated that those aged 10 years and older possess adequate reading comprehension and can independently complete self-report questionnaires (62). Only students from grade 5 and higher were included as eligible participants due to developmental differences between younger and older students (63); those in grade 5 and above typically possess the cognitive and emotional maturity required to comprehend and accurately respond to the questionnaire. Therefore, the study population comprised students from upper primary (Mean ± SD: 11.5 ± 0.00), junior middle (Mean ± SD: 13.3 ± 0.00), and senior high schools (Mean ± SD: 16.0 ± 0.01).
Participants and their guardians received a written document detailing the study’s objectives. The survey aimed to gather data on physical and mental health outcomes, movement behaviors, and sociodemographic factors. Each student voluntarily completed the survey within approximately 20 min (Median: 18.27 min); all data were collected anonymously. Students who agreed to participate filled out the online questionnaire independently in the school’s computer room during a designated class period, under the supervision of a teacher who assisted as needed. The questionnaire was hosted on a widely used Chinese online platform1. An electronic informed consent form was displayed before participants could access the main survey questions. Only those who consented proceeded to the formal data collection stages. The survey protocol was approved by the Shenzhen University Research Committee (No. 2020005) and the participating schools.
A total of 78,428 participants initially completed the questionnaire. However, after excluding entries from participants who completed the questionnaire in less than 5 min or responded incorrectly to a key option item and considering the availability of variables required for the current analysis, the final sample size was reduced to 67,281 students.
2.2 Measures
Sleep duration was assessed using the Pittsburgh Sleep Quality Index (PSQI), which asks participants, “How many hours did you actually sleep at night in the past month?” The Chinese version of the PSQI has been validated for use among Chinese adolescents (64). Screen time was evaluated with items from the Health Behavior of School-aged Children (HBSC) survey, which includes various screen activities such as TV/movies, video games, and other leisure screen use over the past 7 days. Average daily screen time was calculated using the formula: ([total weekday screen time × 5] + [total weekend screen time × 2])/7. PA was measured with a single item adapted from the HBSC survey, asking, “How many days did you engage in MVPA for at least 60 min on weekdays over the past week?” with responses ranging from 0 (none) to 7 (every day). This measure has demonstrated satisfactory reliability among Chinese adolescents (65) and is extensively used in studies with Chinese children and adolescents (66, 67). According to the Canadian 24-Hour Movement Guidelines for Children and Youth (37), achieving 7 days of at least 60 min of MVPA is considered meeting the PA guidelines. Limiting screen time to no more than 2 ho per day meets the screen time (ST) guidelines. For sleep, 9–11 h per night for children (ages 5–12) and 8–10 h for adolescents (ages 13–17) are the benchmarks for guideline adherence. Compliance with these guidelines is assessed either by the total number of guidelines met (none, one, two, or three) or by specific combinations such as PA only, ST only, sleep only, combinations of two, or all three guidelines.
The survey collected comprehensive demographic and personal information, including sex (male/female), educational level by grade (primary school/junior middle school/senior middle school), self-reported height in centimeters, and weight in kilograms. Additional data included the number of siblings (only child or not), family structure (both parents or single parent), parental education level (ranging from junior middle school or below to master’s degree or above), ethnicity (Han or minority), and family socioeconomic status (SES). The geographic scope encompassed nine districts and 135 schools in total. Participants’ weight status was assessed using the body mass index (BMI), calculated from self-reported height and weight, and classified according to China’s normative reference data (68) into categories of normal weight, overweight, and obese. SES was evaluated using an adapted version of the MacArthur Scale of Subjective Social Status, which features a 10-rung ladder, with higher rungs indicating better socioeconomic status (69). To ensure robust statistical analysis, previous studies have controlled these variables to minimize confounding biases (70, 71).
Substance use behavior was assessed using items adapted from the Youth Risk Behavior Survey (72). The evaluation encompassed three distinct types of substance use behavior: whether participants had ever tried cigarette smoking, even if just one or two puffs; whether they had consumed at least one alcoholic drink beyond a few sips; and whether they had experienced drunkenness after consuming alcohol. Respondents were provided with the response options “Yes” or “No.” These items were chosen based partly on pilot feedback and our previous research endeavors (72, 73).
2.3 Statistical analysis
Statistical analyses were conducted using STATA BE 17.0 (College Station, Texas, USA), employing descriptive statistics to outline sample characteristics. Given the nested data structure across different layers—district (level 3), school (level 2), and individual (level 1), informed by the sampling strategy—a three-level mixed multilevel effect model was utilized to evaluate the associations between adherence to the 24-HMG and substance use. Substance use, the dependent variable, was treated as an ordinal variable for further analysis. A series of ordinal logistic regression models were then developed to examine these associations, controlling for all mentioned sociodemographic variables (e.g., SES, sex). Specifically, models 1 and 2 evaluated the number of guidelines met and specific combinations met, respectively, with “none” as the reference category, examining impacts on smoking and drinking. An interaction effect between grade group and adherence to the 24-HMG on substance use was detected, prompting stratified analyses by grade group, while controlling for other sociodemographic factors. Results were expressed as odds ratios (ORs) with 95% confidence intervals (CIs), considering p-values less than 0.05 as statistically significant.
3 Results
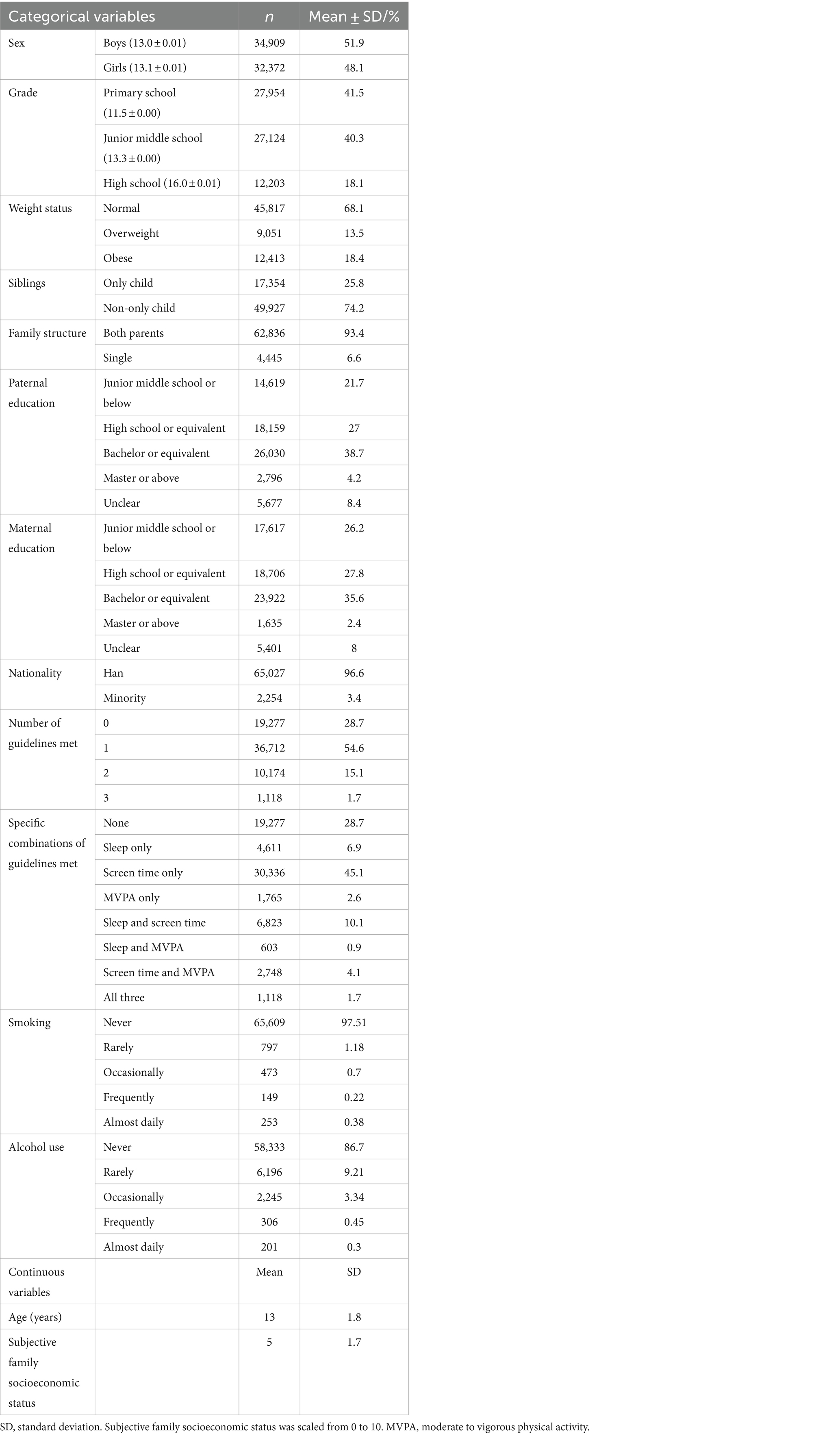
Table 1 presents the socio-demographic characteristics of the study participants. The sample was nearly evenly split between boys (51.9%) and girls (48%), with most participants from primary and junior middle schools. While 54.6% met two guidelines, only 1.7% met all three, and 28.7% met none. Compliance was highest for screen time (61.0%) but low for physical activity (9.3%) and sleep (19.6%). Smoking and alcohol use were rare, with 97.51% never smoking and 86.7% never alcohol use. The mean subjective family socioeconomic status was 5.0 (SD = 1.7).
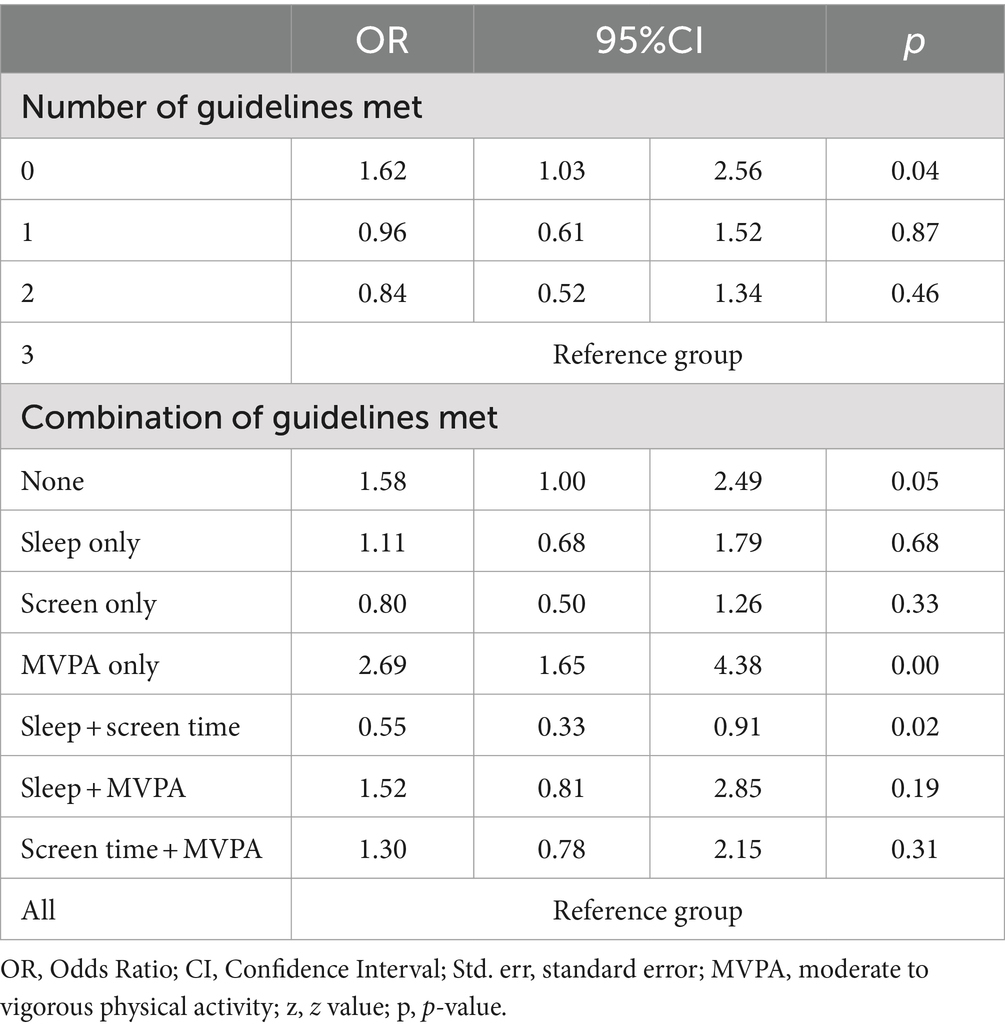
Table 2 highlights the associations between adherence to 24-HMG and smoking behavior. Participants who met none of the guidelines were more likely to smoke (OR = 1.62, p = 0.037). Adherence to one or two guidelines showed no significant effect on smoking likelihood.
Regarding specific combinations of guidelines, adherence to only the screen time recommendation was not associated with lower smoking rates (OR = 0.80 [95% CI: 0.50, 1.26], p = 0.68), nor was adherence to only the sleep recommendation (OR = 1.11 [95% CI: 0.68, 1.79], p = 0.68). However, adherence to only the MVPA guideline significantly increased the likelihood of smoking (OR = 2.69 [95% CI: 1.65, 4.38], p < 0.001). Combinations of sleep and screen time recommendations were associated with a lower likelihood of smoking (OR = 0.55 [95% CI: 0.33, 0.91], p = 0.02), while the combination of screen and MVPA guidelines did not reach statistical significance (OR = 1.30 [95% CI: 0.78, 2.15], p = 0.31). Participants meeting none of the guidelines also demonstrated an increased likelihood of smoking (OR = 1.58 [95% CI: 1.00, 2.49], p = 0.05).
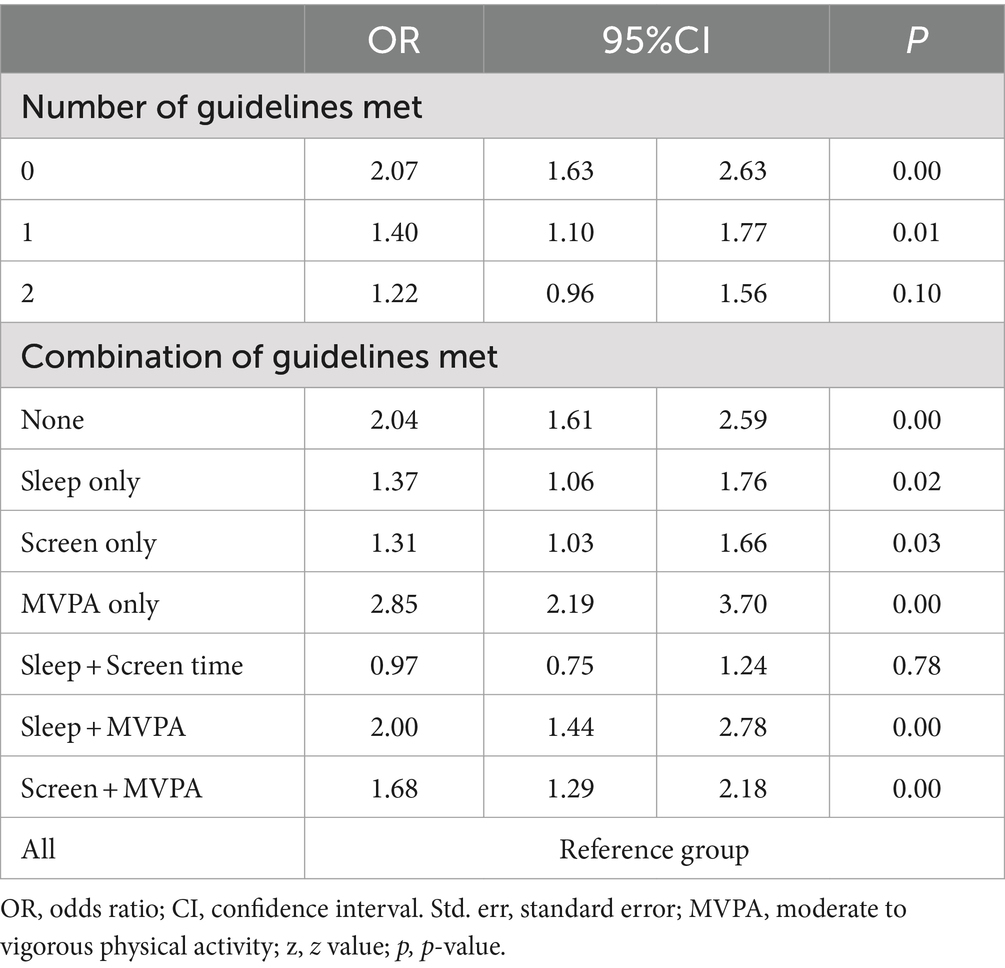
Table 3 illustrates an inverse relationship between adherence to 24-HMG and the likelihood of drinking. Participants who met none of the guidelines had the highest likelihood of alcohol use (OR = 2.07, p < 0.001), followed by those who met one guideline (OR = 1.40, p = 0.006), while meeting two guidelines showed a non-significant effect (OR = 1.22, p = 0.106).
Specific findings include adherence to only the screen time guideline (OR = 1.31, p = 0.028), only the MVPA guideline (OR = 2.85, p < 0.001), and only the sleep guideline (OR = 1.37, p = 0.015) all showing significant associations. Combinations of guidelines showed varied results: sleep and screen time (OR = 0.97, p = 0.783), screen time and MVPA (OR = 1.68, p < 0.001), and sleep and MVPA (OR = 2.0, p < 0.001) were also examined for their association with drinking behaviors.
4 Discussion
This study explored the relationship between adherence to the 24-HMG and the incidence of smoking and alcohol use among children and adolescents. The findings indicated that over half of the participants adhered to at least two of the movement guidelines, although adherence to the PA guidelines was particularly low. A significant association was found between adherence to these guidelines and a reduction in smoking and alcohol consumption. These results highlight a negative correlation between the extent of guideline adherence and the likelihood of engaging in harmful behaviors. This study emphasizes the potential role of routine adherence to movement guidelines in promoting healthier lifestyles among children and adolescents.
This study explored the complex relationship between adherence to the 24-HMG and smoking behavior among children and adolescents, highlighting the differential impacts of various components on smoking levels. Strikingly, only 1.7% of participants adhered to all three guidelines, reflecting the challenge of full compliance (OR = 0.84, p = 0.459). This low compliance rate suggests that comprehensive engagement with health behaviors may be associated with reduced smoking behaviors. Specifically, adherence to the MVPA guidelines showed a significant negative correlation with smoking (OR = 2.69, p < 0.001), consistent with the findings of Gismero-González et al. (74), who reported that vigorous exercise notably deters smoking, especially among beginners. Our findings reinforce this correlation, particularly in participants meeting both MVPA and sleep + MVPA guidelines, suggesting that the emotional benefits of physical exercise and its role in enhancing health consciousness could be key factors (75). These results align with previous research and underscore the importance of integrated health behaviors in reducing smoking prevalence among children and adolescents.
Conversely, adherence to screen time guidelines alone did not significantly impact smoking rates (OR = 0.8, p = 0.68), indicating that increased screen time may not directly influence smoking but could contribute to behaviors such as sedentariness, which are linked to smoking susceptibility (76). Similarly, adherence to sleep guidelines alone showed no significant reduction in smoking (OR = 1.11, p = 0.68), which contrasts with Wheaton’s (77) findings on the adverse effects of sleep deprivation on health behaviors. This study underscores the synergistic effects of adhering to multiple guidelines, illustrating that a holistic approach to health behaviors—such as combining adherence to sleep and screen time guidelines—can more effectively reduce smoking (OR = 0.55, p = 0.02). This finding supports the work of Barua et al. (78), who advocate for comprehensive health interventions rather than isolated behavioral changes to decrease youth smoking. An integrated strategy may help bridge the physical and mental aspects of health, guiding children and adolescents toward a healthier lifestyle and long-term avoidance of smoking.
This study highlights the complex relationship between lifestyle choices and adolescent health outcomes, particularly in relation to drinking behaviors. The findings reveal an inverse correlation between adherence to the 24-HMG and the prevalence of alcohol consumption among children and adolescents. Notably, adherence to MVPA guidelines alone showed the strongest deterrent effect on drinking behaviors (OR = 2.85, p < 0.001). However, not all 24-HMG components were associated with drinking. For instance, adherence to sleep and screen time guidelines combined was not linked to reduced drinking. In contrast, significant inverse correlations were found for PA alone, as well as for combinations like sleep + PA and screen time + PA, suggesting that physically active adolescents tend to focus on fitness, which correlates with lower engagement in harmful behaviors like alcohol consumption (79). PA is associated with promoting a healthier lifestyle and acts as a preventive measure against negative behaviors, including alcohol use, especially among infrequent drinkers (80). However, Liu et al. (2015) (81) highlighted that while PA can boost self-esteem and social connections, it might paradoxically increase alcohol consumption due to greater social opportunities (82), indicating that adolescent drinking behaviors are influenced by broader social contexts. Additionally, adherence to screen time guidelines also contributed to reduced drinking rates (OR = 1.31, p = 0.028), likely due to reduced exposure to alcohol-related advertising (83). Furthermore, sufficient sleep was linked to lower alcohol consumption (OR = 1.37, p = 0.015), as proper rest is associated with reduced stress and improved decision-making, which lowers the likelihood of drinking to alleviate stress (84). The combined adherence to sleep and PA guidelines significantly reinforced this inverse relationship (OR = 2.85, p < 0.001), supporting Bhochhibhoya and Branscum’s (85) assertion that an integrated behavioral strategy can effectively decrease the propensity for alcohol and drug use among children and adolescents. This study provides several implications for enhancing adherence to the 24-HMG among Chinese children and adolescents, with a particular focus on public health policies and educational strategies. A key takeaway is the pivotal role of school and family environments in fostering a healthy lifestyle (86–88). Schools can optimize their facilities to encourage PA, incorporate proper sleep schedules, and establish norms for screen use within their educational programs. These initiatives align with findings from previous studies that emphasize the importance of school-based interventions in fostering healthy behaviors among children and adolescents (89). Additionally, government policies could be instrumental in establishing and enforcing standards for physical education in school curricula. Such policies should not only prioritize PA as a fundamental component of quality education but also provide structured alternatives to minimize unsupervised screen time, supporting earlier research that links reduced screen time with better health outcomes (90). Moreover, regular family health awareness seminars could improve the effectiveness of guideline implementation, as family-based interventions are crucial for promoting children’s adherence to healthy behaviors (91). Given the cultural context of China, where the education system and family structures often emphasize academic performance, creating significant competitive pressure on teenagers (92, 93). It is essential to integrate mental health support with physical health measures and substance use management. Achieving these goals will require coordinated efforts among schools, families, and government entities to significantly enhance the public health status of China’s youth and reduce the prevalence of harmful behaviors such as smoking and drinking. While this study provides valuable insights into the relationship between adherence to lifestyle guidelines and youth behavior in China, future research should further explore broader environmental factors. Such research would help clarify the underlying influences on these behaviors and more effectively guide public health interventions.
This study demonstrates both strengths and limitations. One significant strength lies in its comprehensive approach, encompassing a wide array of lifestyle factors and utilizing diverse indicators to thoroughly evaluate the cumulative impact of health behaviors. Furthermore, the study benefits from a large sample size, which contributes to robust data sets, facilitating a more nuanced understanding of correlations between indicators and bolstering the generalizability of the findings within the Chinese context. However, a primary limitation stems from the reliance on self-reported data, which introduces the possibility of response bias. Participants may tend to underreport behaviors perceived as negative, such as smoking and drinking, potentially biasing the results. Additionally, the study does not delve deeply into the causal relationships between various external factors and health behaviors. For example, the influences of socioeconomic status and educational environments on adolescent behavior were not thoroughly explored.
5 Conclusion
This study investigates the influence of adhering to 24-HMG on smoking and drinking among children and adolescents. The results suggest that while more than half of the participants adhered to at least two of these guidelines, compliance with PA recommendations was notably lower. Importantly, the data unveiled a distinct correlation between adherence to these guidelines and a decrease in smoking and alcohol consumption. This underscores the inverse link between following the guidelines and participating in harmful behaviors, thereby emphasizing the study’s aim to demonstrate how daily habits can steer adolescents toward healthier lifestyles.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
The studies involving humans were approved by the survey protocol was approved by the Shenzhen University Research Committee (No. 2020005) and the participating schools. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
HS: Writing – original draft, Writing – review & editing, Data curation, Methodology, Supervision. DL: Writing – original draft, Writing – review & editing. KH: Writing – original draft, Writing – review & editing. JY: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by grants from the Reform and innovation of physical education courses in general education modules of science and technology universities under the background of discipline integration (No. 2024YBJG082); The practice of physical education curriculum reform in Sino-foreign cooperative schools in the Guangdong-Hong Kong-Macao Greater Bay Area: A case study of the Hong Kong University of Science and Technology (Guangzhou) (No. 2024110425).
Acknowledgments
The authors would like to appreciate the children who actively participate in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Cox, A, Fairclough, SJ, Kosteli, M-C, and Noonan, RJ. Efficacy of school-based interventions for improving muscular fitness outcomes in adolescent boys: a systematic review and meta-analysis. Sports Med. (2020) 50:543–60. doi: 10.1007/s40279-019-01215-5
2. Liu, S, Yu, Q, Hossain, M-M, Doig, S, Bao, R, Zhao, Y, et al. Meeting 24-h movement guidelines is related to better academic achievement: findings from the YRBS 2019 cycle. Int J Ment Health Promot. (2022) 24:13–24. doi: 10.32604/IJMHP.2021.017660
3. Li, H, Zhang, W, and Yan, J. Physical activity and sedentary behavior among school-going adolescents in low-and middle-income countries: insights from the global school-based health survey. PeerJ. (2024) 12:e17097. doi: 10.7717/peerj.17097
4. Zheng, W, Shen, H, Belhaidas, MB, Zhao, Y, Wang, L, and Yan, J. The relationship between physical fitness and perceived well-being, motivation, and enjoyment in Chinese adolescents during physical education: a preliminary cross-sectional study. Children. (2023) 10:111. doi: 10.3390/children10010111
5. Mavilidi, MF, Mason, C, Leahy, AA, Kennedy, SG, Eather, N, Hillman, CH, et al. Effect of a time-efficient physical activity intervention on senior school students’ on-task behaviour and subjective vitality: the ‘burn 2 Learn’cluster randomised controlled trial. Educ Psychol Rev. (2021) 33:299–323. doi: 10.1007/s10648-020-09537-x
6. Shi, J, Gao, M, Xu, X, Zhang, X, and Yan, J. Associations of muscle-strengthening exercise with overweight, obesity, and depressive symptoms in adolescents: findings from 2019 youth risk behavior surveillance system. Front Psychol. (2022) 13:980076. doi: 10.3389/fpsyg.2022.980076
7. Shi, C, Yan, J, Wang, L, and Shen, H. Exploring the self-reported physical fitness and self-rated health, mental health disorders, and body satisfaction among Chinese adolescents: a cross-sectional study. Front Psychol. (2022) 13:1003231. doi: 10.3389/fpsyg.2022.1003231
8. Liu, T, Li, D, Yang, H, Chi, X, and Yan, J. Associations of sport participation with subjective well-being: a study consisting of a sample of Chinese school-attending students. Front Public Health. (2023) 11:11. doi: 10.3389/fpubh.2023.1199782
9. Li, D, Wang, D, Zou, J, Li, C, Qian, H, Yan, J, et al. Effect of physical activity interventions on children's academic performance: a systematic review and meta-analysis. Eur J Pediatr. (2023) 182:3587–601. doi: 10.1007/s00431-023-05009-w
10. Zhang, Y, Yan, J, Jin, X, Yang, H, Zhang, Y, Ma, H, et al. Sports participation and academic performance in primary school: a cross-sectional study in Chinese children. Int J Environ Res Public Health. (2023) 20:3678. doi: 10.3390/ijerph20043678
11. Bao, R, Qin, H, Memon, AR, Chen, S, López-Gil, JF, Liu, S, et al. Is adherence to the 24-h movement guidelines associated with greater academic-related outcomes in children and adolescents? A systematic review and meta-analysis. Eur J Pediatr. (2024) 183:2003–14. doi: 10.1007/s00431-024-05461-2
12. Bull, FC, Al-Ansari, SS, Biddle, S, Borodulin, K, Buman, MP, Cardon, G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
13. Chaput, J-P, Willumsen, J, Bull, F, Chou, R, Ekelund, U, Firth, J, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Act. (2020) 17:1–9. doi: 10.1186/s12966-020-01037-z
14. Chen, P, Wang, D, Shen, H, Yu, L, Gao, Q, Mao, L, et al. Physical activity and health in Chinese children and adolescents: expert consensus statement (2020). Br J Sports Med. (2020) 54:1321–31. doi: 10.1136/bjsports-2020-102261
15. Shi, C, Chen, S, Wang, L, Yan, J, Liang, K, Hong, J, et al. Associations of sport participation, muscle-strengthening exercise and active commuting with self-reported physical fitness in school-aged children. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.873141
16. Durstine, JL, Gordon, B, Wang, Z, and Luo, X. Chronic disease and the link to physical activity. J Sport Health Sci. (2013) 2:3–11. doi: 10.1016/j.jshs.2012.07.009
17. Fan, H, Yan, J, Yang, Z, Liang, K, and Chen, S. Cross-sectional associations between screen time and the selected lifestyle behaviors in adolescents. Front Public Health. (2022) 10:932010. doi: 10.3389/fpubh.2022.932017
18. Huang, C, Memon, AR, Yan, J, Lin, Y, and Chen, S-T. The associations of active travel to school with physical activity and screen time among adolescents: do individual and parental characteristics matter? Front Public Health. (2021) 9:719742. doi: 10.3389/fpubh.2021.719742
19. Houben, M, Van Den Noortgate, W, and Kuppens, P. The relation between short-term emotion dynamics and psychological well-being: a meta-analysis. Psychol Bull. (2015) 141:901–30. doi: 10.1037/a0038822
20. Newman, TJ. Life skill development and transfer:“They’re not just meant for playing sports”. Res Soc Work Pract. (2020) 30:643–57. doi: 10.1177/1049731520903427
21. Kendellen, K, and Camiré, M. Applying in life the skills learned in sport: a grounded theory. Psychol Sport Exerc. (2019) 40:23–32. doi: 10.1016/j.psychsport.2018.09.002
22. Diener, E, Pressman, SD, Hunter, J, and Delgadillo-Chase, D. If, why, and when subjective well-being influences health, and future needed research. Appl Psychol Health Well Being. (2017) 9:133–67. doi: 10.1111/aphw.12090
23. Rosenberger, ME, Fulton, JE, Buman, MP, Troiano, RP, Grandner, MA, Buchner, DM, et al. The 24-hour activity cycle: a new paradigm for physical activity. Med Sci Sports Exerc. (2019) 51:454–64. doi: 10.1249/MSS.0000000000001811
24. You, Y, Mo, L, Tong, J, Chen, X, and You, Y. The role of education attainment on 24-hour movement behavior in emerging adults: evidence from a population-based study. Front Public Health. (2024) 12:1197150. doi: 10.3389/fpubh.2024.1197150
25. Chen, S, Brown, D, Parker, K, and Lee, E-Y. Trends in adherence to the 24-h movement guidelines among US adolescents from 2011 to 2019: evidence from repeated cross-sectional cycles of the youth risk behavior surveillance system. Scand J Med Sci Sports. (2024) 34:e14609. doi: 10.1111/sms.14609
26. Shi, G, Liang, C, Zang, W, Bao, R, Yan, J, Zhou, L, et al. 24-hour movement behaviours and self-rated health in Chinese adolescents: a questionnaire-based survey in eastern China. PeerJ. (2023) 11:e16174. doi: 10.7717/peerj.16174
27. Chen, Z, Chi, G, Wang, L, Chen, S, Yan, J, and Li, S. The combinations of physical activity, screen time, and sleep, and their associations with self-reported physical fitness in children and adolescents. Int J Environ Res Public Health. (2022) 19:5783. doi: 10.3390/ijerph19105783
28. Zhang, Y, Chi, X, Huang, L, Yang, X, and Chen, S. Cross-sectional association between 24-hour movement guidelines and depressive symptoms in Chinese university students. PeerJ. (2024) 12:e17217. doi: 10.7717/peerj.17217
29. Diamant, É, Perez, T, and Drouin, O. Nudging interventions to improve children's sleep, physical activity and sedentary behavior: a scoping review. Prev Med. (2023) 173:107572. doi: 10.1016/j.ypmed.2023.107572
30. Åslund, L, Arnberg, F, Kanstrup, M, and Lekander, M. Cognitive and behavioral interventions to improve sleep in school-age children and adolescents: a systematic review and Meta-analysis. J Clin Sleep Med. (2018) 14:1937–47. doi: 10.5664/jcsm.7498
31. Barbosa Filho, VC, Minatto, G, Mota, J, Silva, KS, de Campos, W, and da Silva Lopes, A. Promoting physical activity for children and adolescents in low-and middle-income countries: an umbrella systematic review: a review on promoting physical activity in LMIC. Prev Med. (2016) 88:115–26. doi: 10.1016/j.ypmed.2016.03.025
32. Kim, H, Ma, J, Harada, K, Lee, S, and Gu, Y. Associations between adherence to combinations of 24-h movement guidelines and overweight and obesity in Japanese preschool children. Int J Environ Res Public Health. (2020) 17:9320. doi: 10.3390/ijerph17249320
33. Ma, C, Yan, J, Hu, H, Shi, C, Li, F, and Zeng, X. Associations between 24-h movement behavior and internet addiction in adolescents: a cross-sectional study. Int J Environ Res Public Health. (2022) 19:16873. doi: 10.3390/ijerph192416873
34. Chen, S, Liang, K, López-Gil, JF, Drenowatz, C, and Tremblay, MS. Association between meeting 24-h movement guidelines and academic performance in a sample of 67,281 Chinese children and adolescents. Eur J Sport Sci. (2024) 24:487–98. doi: 10.1002/ejsc.12034
35. Ferrari, GLDM, Kovalskys, I, Fisberg, M, Gómez, G, Rigotti, A, Sanabria, LYC, et al. Socio-demographic patterning of objectively measured physical activity and sedentary behaviours in eight Latin American countries: findings from the ELANS study. Eur J Sport Sci. (2020) 20:670–81. doi: 10.1080/17461391.2019.1678671
36. Chiao, A, Hughes, ML, Premkumar, PK, and Zoucha, K. The effects of substance misuse on auditory and vestibular function: a systematic review. Ear Hear. (2024) 45:276–96. doi: 10.1097/AUD.0000000000001425
37. Schulte, MT, and Hser, Y-I. Substance use and associated health conditions throughout the lifespan. Public Health Rev. (2013) 35:1–27. doi: 10.1007/BF03391702
38. Sanchez, ZM, Prado, MCO, Sanudo, A, Carlini, EA, Nappo, SA, and Martins, SS. Trends in alcohol and tobacco use among Brazilian students: 1989 to 2010. Revista Saude Publica. (2015) 49:70.
39. Joung, KH, and Saewyc, EM. Factors related to heavy drinking between British Columbia Asian adolescents and south Korean adolescents. J Spec Pediatr Nurs. (2020) 25:e12296. doi: 10.1111/jspn.12296
40. Kaai, S., Manske, S., Leatherdale, S., Brown, K., and Murnaghan, D., Are experimental smokers different from their never-smoking classmates? A multilevel analysis of Canadian youth in grades 9 to 12. Health promotion and chronic disease prevention in Canada, (2014). 34.
41. Huỳnh, C, Morin, AJ, Fallu, J-S, Maguire-L, J, Descheneaux-Buffoni, A, and Janosz, M. Unpacking the longitudinal associations between the frequency of substance use, substance use related problems, and academic achievement among adolescents. J Youth Adolesc. (2019) 48:1327–41. doi: 10.1007/s10964-019-01038-7
42. Steele, ML, Meurk, C, Schess, J, Yap, L, Jones, J, Harden, S, et al. Substance use and help-seeking among justice-involved young people in Queensland and Western Australia: a cross-sectional survey of 14–17-year-olds. Drug Alcohol Rev. (2021) 40:617–26. doi: 10.1111/dar.13238
43. Ninkron, P, Yau, S, Khuntiterakul, P, and Nakamadee, B. Substance use and related risk behaviors among junior high school students in Nakhon Pathom province. Thailand J Health Res. (2022) 36:345–53. doi: 10.1108/JHR-05-2020-0137
44. Caravaca-Sánchez, F, Aizpurua, E, and Stephenson, A. Substance use, family functionality, and mental health among college students in Spain. Soc Work Public Health. (2021) 36:221–31. doi: 10.1080/19371918.2020.1869134
45. Guo, L, Deng, J, He, Y, Deng, X, Huang, J, Huang, G, et al. Alcohol use and alcohol-related problems among adolescents in China: a large-scale cross-sectional study. Medicine (Baltimore). (2016) 95:e4533. doi: 10.1097/MD.0000000000004533
46. Sheng Xiong, P, Juan Xiong, M, Xi Liu, Z, and Liu, Y. Prevalence of smoking among adolescents in China: an updated systematic review and meta-analysis. Public Health. (2020) 182:26–31. doi: 10.1016/j.puhe.2020.01.011
47. Lin, B, Liu, X, Lu, W, Wu, X, Li, Y, Zhang, Z, et al. Prevalence and associated factors of smoking among Chinese adolescents: a school-based cross-sectional study. BMC Public Health. (2023) 23:669. doi: 10.1186/s12889-023-15565-3
48. Patton, GC, Sawyer, SM, Santelli, JS, Ross, DA, Afifi, R, Allen, NB, et al. Our future: a lancet commission on adolescent health and wellbeing. Lancet. (2016) 387:2423–78. doi: 10.1016/S0140-6736(16)00579-1
49. Terry-McElrath, YM, Maslowsky, J, O'Malley, PM, Schulenberg, JE, and Johnston, LD. Sleep and substance use among US adolescents, 1991-2014. Am J Health Behav. (2016) 40:77–91. doi: 10.5993/AJHB.40.1.9
50. Chen, C-Y, and Lin, K-M. Health consequences of illegal drug use. Curr Opin Psychiatry. (2009) 22:287–92. doi: 10.1097/YCO.0b013e32832a2349
51. Ozgur, H, Koyuncu, O, Bikmazer, A, and Turan, S. Investigation of substance use, substance-related factors and delinquency in a nation-wide referred children sample. J Forensic Psychol Res Pract. (2024):1–15. doi: 10.1080/24732850.2024.2305219
52. Hawkins, JD, Catalano, RF, and Miller, JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. (1992) 112:64–105. doi: 10.1037/0033-2909.112.1.64
53. Paul, FA, Ganie, AUR, and Dar, DR. Substance use in university students: a comprehensive examination of its effects on academic achievement and psychological well-being. Soc Work Ment Health. (2024) 22:452–84. doi: 10.1080/15332985.2024.2306935
54. Pengpid, S, and Peltzer, K. Leisure-time sedentary behavior is associated with psychological distress and substance use among school-going adolescents in five southeast Asian countries: a cross-sectional study. Int J Environ Res Public Health. (2019) 16:2091. doi: 10.3390/ijerph16122091
55. Colrain, IM, Nicholas, CL, and Baker, FC. Alcohol and the sleeping brain. Handb Clin Neurol. (2014) 125:415–31. doi: 10.1016/B978-0-444-62619-6.00024-0
56. Moore, MJ, and Werch, C. Relationship between vigorous exercise frequency and substance use among first-year drinking college students. J Am Coll Heal. (2008) 56:686–90. doi: 10.3200/JACH.56.6.686-690
57. Liangruenrom, N, Dumuid, D, Craike, M, Biddle, SJ, and Pedisic, Z. Trends and correlates of meeting 24-hour movement guidelines: a 15-year study among 167,577 Thai adults. Int J Behav Nutr Phys Act. (2020) 17:1–17.
58. Mozaffarian, D, Afshin, A, Benowitz, NL, Bittner, V, Daniels, SR, Franch, HA, et al. Population approaches to improve diet, physical activity, and smoking habits. Circulation. (2012) 126:1514–63. doi: 10.1161/CIR.0b013e318260a20b
59. Etindele Sosso, FA, Holmes, SD, and Weinstein, AA. Influence of socioeconomic status on objective sleep measurement: a systematic review and meta-analysis of actigraphy studies. Sleep Health. (2021) 7:417–28. doi: 10.1016/j.sleh.2021.05.005
60. Luo, L, Cao, Y, Hu, Y, Wen, S, Tang, K, Ding, L, et al. The associations between meeting 24-hour movement guidelines (24-HMG) and self-rated physical and mental health in older adults—cross sectional evidence from China. Int J Environ Res Public Health. (2022) 19:13407. doi: 10.3390/ijerph192013407
61. Luo, L. 24-H movement behaviors and visual impairment among Chinese adolescents with and without obesity. Complement Ther Clin Pract. (2024) 54:101823. doi: 10.1016/j.ctcp.2023.101823
62. Chen, S-T, Liu, Y, Tremblay, MS, Hong, J-T, Tang, Y, Cao, Z-B, et al. Meeting 24-h movement guidelines: prevalence, correlates, and the relationships with overweight and obesity among Chinese children and adolescents. J Sport Health Sci. (2021) 10:349–59. doi: 10.1016/j.jshs.2020.07.002
63. Eccles, JS. The development of children ages 6 to 14. Futur Child. (1999) 9:30–44. doi: 10.2307/1602703
64. Ho, KY, Lam, KK, Xia, W, Chung, J, Cheung, AT, Ho, LL, et al. Psychometric properties of the Chinese version of the Pittsburgh sleep quality index (PSQI) among Hong Kong Chinese childhood cancer survivors. Health Qual Life Outcomes. (2021) 19:1–11. doi: 10.1186/s12955-021-01803-y
65. Liu, Y, Wang, M, Tynjälä, J, Lv, Y, Villberg, J, Zhang, Z, et al. Test-retest reliability of selected items of health behaviour in school-aged children (HBSC) survey questionnaire in Beijing. China BMC Med Res Methodol. (2010) 10:1–9.
66. Chen, S, Liang, K, Chen, S, Huang, L, and Chi, X. Association between 24-hour movement guideline and physical, verbal, and relational forms of bullying among Chinese adolescents. Asia Pacific J Public Health. (2023) 35:168–74. doi: 10.1177/10105395221148851
67. Liang, K, Chen, S, and Chi, X. Differential associations between meeting 24-hour movement guidelines with mental wellbeing and mental illness among Chinese adolescents. J Adolesc Health. (2023) 72:658–66. doi: 10.1016/j.jadohealth.2022.11.231
68. Zhu, Z, Tang, Y, Zhuang, J, Liu, Y, Wu, X, Cai, Y, et al. Physical activity, screen viewing time, and overweight/obesity among Chinese children and adolescents: an update from the 2017 physical activity and fitness in China—the youth study. BMC Public Health. (2019) 19:1–8. doi: 10.1186/s12889-019-6515-9
69. Cundiff, JM, Smith, TW, Uchino, BN, and Berg, CA. Subjective social status: construct validity and associations with psychosocial vulnerability and self-rated health. Int J Behav Med. (2013) 20:148–58. doi: 10.1007/s12529-011-9206-1
70. Marciano, L, and Camerini, A-L. Recommendations on screen time, sleep and physical activity: associations with academic achievement in Swiss adolescents. Public Health. (2021) 198:211–7. doi: 10.1016/j.puhe.2021.07.027
71. Lien, A, Sampasa-Kanyinga, H, Colman, I, Hamilton, H, and Chaput, J-P. Adherence to 24-hour movement guidelines and academic performance in adolescents. Public Health. (2020) 183:8–14. doi: 10.1016/j.puhe.2020.03.011
72. Wang, F, Lin, L, Lu, J, Cai, J, Xu, J, and Zhou, X. Mental health and substance use in urban left-behind children in China: a growing problem. Child Youth Serv Rev. (2020) 116:105135. doi: 10.1016/j.childyouth.2020.105135
73. Guo, L, Wang, W, Du, X, Guo, Y, Li, W, Zhao, M, et al. Associations of substance use behaviors with suicidal ideation and suicide attempts among US and Chinese adolescents. Front Psych. (2021) 11:611579. doi: 10.3389/fpsyt.2020.611579
74. Gismero-González, E, Bermejo-Toro, L, Cagigal, V, Roldán, A, Martínez-Beltrán, MJ, and Halty, L. Emotional impact of COVID-19 lockdown among the Spanish population. Front Psychol. (2020) 11:616978. doi: 10.3389/fpsyg.2020.616978
75. Mahumud, RA, Sahle, BW, Owusu-Addo, E, Chen, W, Morton, RL, and Renzaho, AM. Association of dietary intake, physical activity, and sedentary behaviours with overweight and obesity among 282,213 adolescents in 89 low and middle income to high-income countries. Int J Obes. (2021) 45:2404–18. doi: 10.1038/s41366-021-00908-0
76. Tremblay, MS, LeBlanc, AG, Kho, ME, Saunders, TJ, Larouche, R, Colley, RC, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. (2011) 8:98–22. doi: 10.1186/1479-5868-8-98
77. Wheaton, AG, Ferro, GA, and Croft, JB. School start times for middle school and high school students—United States, 2011–12 school year. Morb Mortal Wkly Rep. (2015) 64:809–13. doi: 10.15585/mmwr.mm6430a1
78. Barua, RS, Rigotti, NA, Benowitz, NL, Cummings, KM, Jazayeri, M-A, Morris, PB, et al. 2018 ACC expert consensus decision pathway on tobacco cessation treatment: a report of the American College of Cardiology Task Force on clinical expert consensus documents. J Am Coll Cardiol. (2018) 72:3332–65. doi: 10.1016/j.jacc.2018.10.027
79. West, AB, Bittel, KM, Russell, MA, Evans, MB, Mama, SK, and Conroy, DE. A systematic review of physical activity, sedentary behavior, and substance use in adolescents and emerging adults. Transl Behav Med. (2020) 10:1155–67. doi: 10.1093/tbm/ibaa008
80. Janssen, I, Katzmarzyk, PT, Boyce, WF, King, MA, and Pickett, W. Overweight and obesity in Canadian adolescents and their associations with dietary habits and physical activity patterns. J Adolesc Health. (2004) 35:360–7. doi: 10.1016/S1054-139X(04)00058-8
81. Liu, M, Wu, L, and Ming, Q. How does physical activity intervention improve self-esteem and self-concept in children and adolescents? Evidence from a meta-analysis. PLoS One. (2015) 10:e0134804. doi: 10.1371/journal.pone.0134804
82. Kelly, EV, Newton, NC, Stapinski, LA, and Teesson, M. Prospective associations between personality and bullying among Australian adolescents. Austrl N Z J Psychiatry. (2018) 52:173–80. doi: 10.1177/0004867417726583
83. McCreanor, T, Lyons, A, Griffin, C, Goodwin, I, Moewaka Barnes, H, and Hutton, F. Youth drinking cultures, social networking and alcohol marketing: implications for public health. Crit Public Health. (2013) 23:110–20. doi: 10.1080/09581596.2012.748883
84. Wang, X, Li, Y, and Fan, H. The associations between screen time-based sedentary behavior and depression: a systematic review and meta-analysis. BMC Public Health. (2019) 19:1–9. doi: 10.1186/s12889-019-7904-9
85. Bhochhibhoya, A, and Branscum, P. The application of the theory of planned behavior and the integrative behavioral model towards predicting and understanding alcohol-related behaviors. J Alcohol Drug Educ. (2018) 62:39–63.
86. Yan, J, Jones, B, Smith, JJ, Morgan, P, and Eather, N. A systematic review investigating the effects of implementing game-based approaches in school-based physical education among primary school children. J Teach Phys Educ. (2023) 42:573–86. doi: 10.1123/jtpe.2021-0279
87. Yan, J, Malkin, M, Smith, JJ, Morgan, P, and Eather, N. Current teachers’ perceptions and students' perspectives regarding activities modalities, instructional settings during primary school physical education classes in China: a cross-sectional observational study. Front Sports Active Living. (2024) 6:6. doi: 10.3389/fspor.2024.1378317
88. Yan, J, Morgan, PJ, Smith, JJ, Chen, S, Leahy, AA, and Eather, N. Pilot randomized controlled trial of a game-based intervention for teaching basketball in Chinese primary school physical education. J Sports Sci. (2024) 42:25–37. doi: 10.1080/02640414.2024.2319457
89. Chen, Y, Ma, L, Ma, Y, Wang, H, Luo, J, Zhang, X, et al. A national school-based health lifestyles interventions among Chinese children and adolescents against obesity: rationale, design and methodology of a randomized controlled trial in China. BMC Public Health. (2015) 15:210. doi: 10.1186/s12889-015-1516-9
90. Forte, C, O'Sullivan, D, McDowell, CP, Hallgren, M, Woods, CB, and Herring, MP. Associations between screen-time, physical activity and depressive symptoms differ based on gender and screen-time mode. Eur Child Adolesc Psychiatry. (2023) 32:2313–22. doi: 10.1007/s00787-022-02080-w
91. Brown, HE, Atkin, AJ, Panter, J, Corder, K, Wong, G, Chinapaw, MJ, et al. Family-based interventions to increase physical activity in children: a meta-analysis and realist synthesis protocol. BMJ Open. (2014) 4:e005439. doi: 10.1136/bmjopen-2014-005439
92. McBride-Chang, C, and Chang, L. Adolescent-parent relations in Hong Kong: parenting styles, emotional autonomy, and school achievement. J Genet Psychol. (1998) 159:421–36. doi: 10.1080/00221329809596162
Keywords: physical activity, screen time, sleep, substance use, China
Citation: Su H, Lyu D, Huang K and Yan J (2024) Association of physical activity, screen time and sleep with substance use in children and adolescents: a large sample cross-sectional study. Front. Public Health. 12:1432710. doi: 10.3389/fpubh.2024.1432710
Edited by:
Marco Branco, Polytechnic Institute of Santarém, PortugalReviewed by:
Adela Badau, Transilvania University of Brașov, RomaniaKell Grandjean Da Costa, Colby–Sawyer College, United States
Copyright © 2024 Su, Lyu, Huang and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ke Huang, aHVhbmdrZWluMTYzQDE2My5jb20=; Jin Yan, amlueWFuMTEyNkBzdWRhLmVkdS5jbg==
 Huadong Su1
Huadong Su1 Dongye Lyu
Dongye Lyu Ke Huang
Ke Huang Jin Yan
Jin Yan