- School of Physical Education, Southwest University, Chongqing, China
Background: Depression poses significant threats to adolescents’ health globally. Research has shown the potential of mind–body therapies to alleviate depression, but limited studies have directly compared the therapeutic effects of different types of mind–body therapies on adolescent depression and the optimal therapy remain unclear. Therefore, we conducted a systematic review and network meta-analysis of randomized controlled trials that met the inclusion criteria to explore the effectiveness of different types of mind–body therapies as interventions to improve depression among adolescents, and to identify the most effective interventions.
Methods: A comprehensive search of databases including PubMed, EMBASE, Cochrane Library, Web of Science, and Scopus up to January 2024 was conducted to assess the impact of mind–body therapies on depression among adolescents. The risk of bias of the included studies was evaluated using Cochrane Review Manager 5.4. STATA 18.0 was used for network meta-analysis. The node-splitting method was used to test the local inconsistency of the network meta-analysis. Funnel plots and the Egger’s test were utilized to assess the potential impact of bias in this study.
Result: This network meta-analysis included 9 randomized controlled trials involving a total of 955 subjects. The results indicated that yoga, dance therapy and Tai Chi were more effective than other mind–body therapies in reducing symptoms of depression among adolescents. Specifically, according to the SUCRA ranking, yoga was rated to be the optimal intervention for adolescents with depression (SCURA: 82.2%), followed by dance therapy (SCURA: 77.5%) and Tai Chi (SCURA: 64.9%).
Conclusion: This study revealed that mind–body therapies have positive effects on improving depression among adolescents. Yoga may be the most effective intervention among the different types of mind–body therapies. However, due to the small sample size of patients included, the certainty of the results was limited to some extent. Therefore, further investigation is necessary to strengthen the evidence base when more relevant studies become available.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42024508774.
1 Introduction
An estimated 3.8% of the population worldwide experience depression (1). Previous studies indicate that approximately 34% of adolescents worldwide are at risk of developing clinical depression, with the highest rates observed among adolescents living in the Middle East, Africa, and Asia (2). According to Report on National Mental Health Development in China (2021–2022), 24.1% adolescents were depressed, meaning that about one in four adolescents suffers from depression (3). Depression is a common, debilitating, burdensome, and chronic mental health problem that is prevalent during adolescence (4, 5). Stressors among adolescents, usually aged 10 to 19 (6), include physical and mental changes, academic pressure, and shifts in family and social relationships. At this time, due to the immature emotion regulation abilities of adolescents, long-term exposure to these stressors causes difficulty in coping with negative emotions, leading to malfunction of reward system (i.e., abnormal secretion of endorphins, dopamine, oxytocin, etc.) or the abnormalities in the hypothalamic–pituitary–adrenal (HPA) axis, which may provide the environment for the emergence of depression (7, 8). This mood disorder is broadly characterized by persistent feelings of sadness, loss of interest in activities, and impairment of daily functioning (1, 9). The damaging effects of depression also extend to adolescents’ social relationships to academic performance, and depression-induced suicide has become the second leading cause of death among adolescents (10–12). Moreover, adolescent depression has high comorbidity with other mental disorders such as anxiety, substance abuse, and conduct disorders, and is often associated with risky behaviors. Early onset of depression during adolescence presents a more severe depression in adulthood (i.e., longer episodes, higher recurrence rates, and more residual symptoms), and adverse psychosocial outcomes such as lower subsequent educational attainments, lower perceived social support (13–16). Rather than conceptualizing depression as qualitatively distinct “entities” (i.e., major depressive disorder, persistent depressive disorder, premenstrual dysphoric disorder, etc.) (9), current research proposed the dimensional model, which conceptualizes depression as a continuously process starting from subthreshold depression (17), with all individuals falling somewhere on the depressive symptom spectrum, distress and impairment occurring at the extremes of the continuum where the individual lies (4, 18–20). Since dimensional models have been proven to be more valid than traditional categorical models in examining the etiology and treatment of adolescent depression (19), we will also use the term “depression” in the rest of this review to broadly refer to various collections of depressive disorders and symptoms.
Medication and psychotherapy are the primary clinical interventions for depression among adolescents. However, despite the fact that these therapeutic approaches have been adequately implemented, they can only reduce the disease burden of depression by 30% (21). A significant number of patients received insufficient relief of their symptoms, while 50% suffered at least one recurrence of a depressive episode after 6–12 months of treatment (22). Previous studies denoted that antidepressant medication carried potential side effects and might increase the risk of suicidality among adolescents (23–25). For instance, Selective Serotonin Reuptake Inhibitors (SSRIs) in clinical trials have increased the intensity of suicidal predictors in depressed patients, such as dysphoria, anxiety, impulsiveness, aggressivity, agitation, etc. (26). Besides, although psychotherapy can be effective, many patients may refuse it due to the stigma related to their symptoms, and for some adolescent patients, especially in low-and middle-income countries, it is very expensive and unaffordable (1, 27). In this context, there is a paramount necessity to find cost-effective, side-effect-free, and easily accessible forms of treatment for depression in addition to options that already exist (28).
Due to its low cost, simplicity of implementation, varied forms and enjoyable nature, exercise therapy has become a prevalent adjunctive treatment for adolescent depression in recent years (29, 30). Research has demonstrated that the physiological mechanisms underlying the positive effects of exercise on depression are related to cytokines, monoamine neurotransmitters, inflammatory factors, neural systems and other factors in the body (31). However, mind–body therapies (MBTs), combining various forms of exercise, have been developed as an effective intervention for the treatment of depression by strengthening the mind’s capacity to interact dynamically with the body’s functions and symptoms, and to establish a strong connection between the brain, mind, body and behavior, in order to achieve overall health (32). To date, MBTs may include, but are not limited to, yoga, mindfulness-based meditation practices, Tai Chi, dance therapy, Qigong, and Buduanjin etc., and effects varied with different forms of exercise. For instance, yoga reducing stress and psychiatric symptoms, can be an effective treatment option for depression (33, 34). As it helps regulate negative emotions and attention, mindfulness training is essential for both preventing and treating depression (35). Traditional Chinese MBTs like Tai Chi, Qigong, and Buduanjin were proven to enhance patients’ neurocognition through mild movements combined with breathing relaxation techniques (36, 37). However, despite the growing variety of mind–body therapies from the East and West (32), there is a lack of evidence to support the efficacy of different MBTs for depression among adolescents, and the best non-pharmacological treatment strategy for depression in adolescents is unclear (38).
Therefore, the aim of this study is to assess the effects of different types of MBTs on depression among adolescents, and use a network meta-analysis to comprehensively compare and rank multiple different mind–body interventions, thus providing a basis for selecting the optimal treatment plan and informing clinicians when developing non-pharmacological treatment strategies.
2 Materials and methods
We have registered (CRD42024508774) this systematic review and network meta-analysis in the International Prospective Register of Systematic Reviews (PROSPERO), and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Network Meta-Analysis (PRISMA -NMA) statement for reporting. Ethical approval is not required as it is a systematic review.
2.1 Search strategy
We performed a systematic search following in the five electronic databases (PubMed, Embase, Cochrane Library, Web of Science, and Scopus) and used a snowball strategy to find relevant articles from their references and subsequent citations. The search was limited to English language literature and the period covered from the inception of each database until January 2024, and the search strategy followed the PICOS principle:
(P) population: adolescent patients with depression or depressive symptoms;
(I) intervention: mind–body therapies, including Yoga, Mindfulness, Tai Chi, Dance, etc.;
(C) control group: usual care including daily care, waitlist control conditions, routine exercise or other social activities;
(O) outcomes: The outcome measures included at least one of the following: the Patient Health Questionnaire (PHQ-9), the Beck Depression Inventory (BDI), the Symptom Checklist (SCL), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Hamilton Rating Scale for Depression (HAM-D);
(S) study type: randomized controlled trials (RCTs).
The search strategy is provided in the Supplementary material, as the PubMed interface.
2.2 Exclusion criteria
The current study excluded: (1) non- randomized controlled trials, such as quasi-randomized controlled trials, animal studies, protocols, conference abstracts, case reports, etc.; (2) studies with incomplete or unreported data; (3) purely descriptive studies.
2.3 Literature screening
We utilized Endnote X9 literature management software to detect and exclude the duplications. Subsequently, two authors (SLL and ZYM) independently evaluated the titles and abstracts of the retrieved articles to ensure their eligibility for inclusion in the study. No further review was conducted for studies that did not meet inclusion criteria. Then, the two authors reviewed the full texts of the remaining literature. During this process, any disagreements were discussed to reach a resolution, or addressed by consulting another author (SL).
2.4 Data extraction and quality assessment
Three authors (GSF, GGM, and XYZ) independently extracted the data from selected RCTs including (1) basic information such as the first author’s name, year of publication, and country; (2) characteristics of the subjects, including mean age and gender; (3) experimental settings, including sample size, exercise type, cycle, frequency, and time; (4) primary outcome measures and measurement tools.
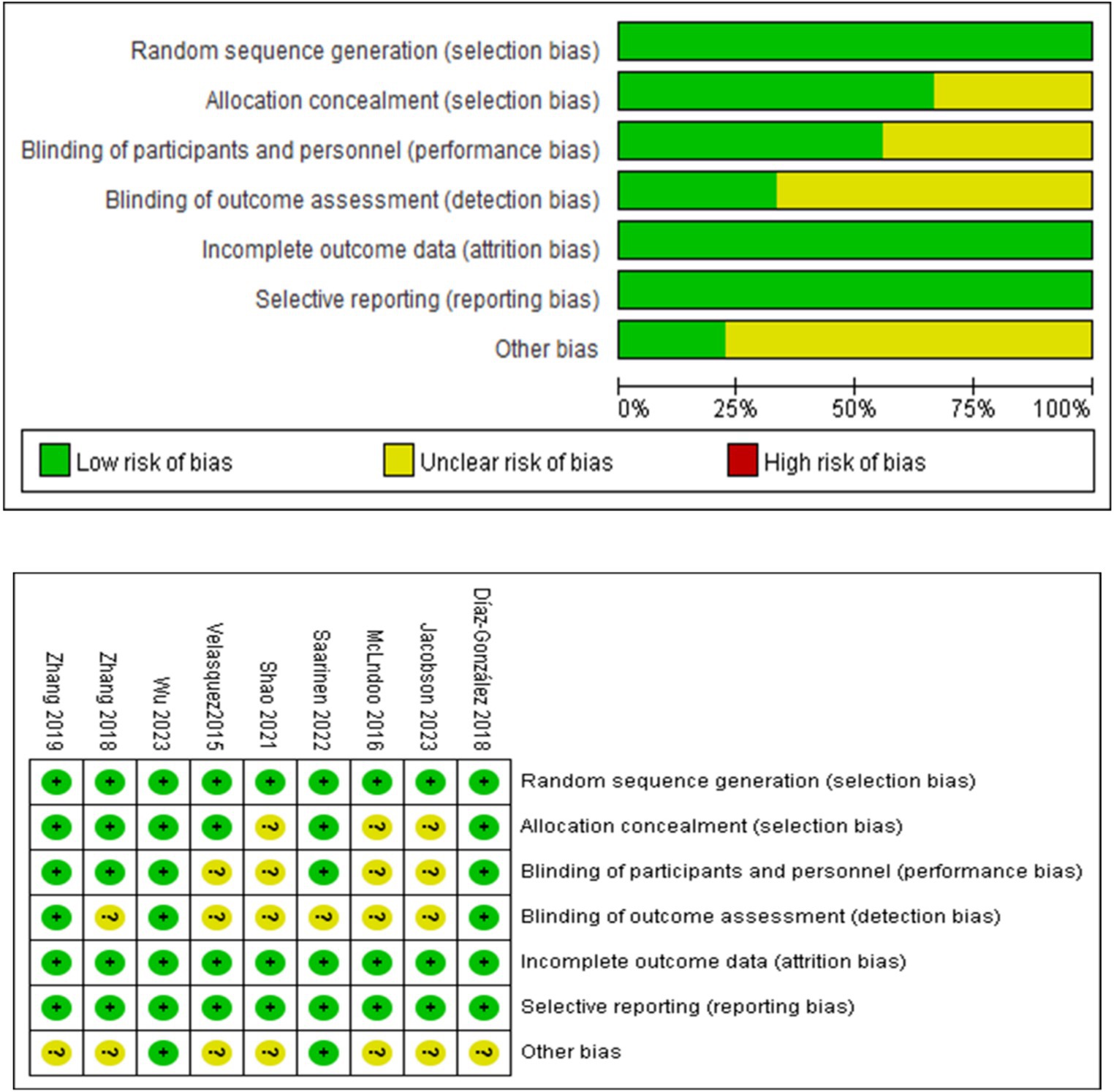
Risk of bias (ROB) assessment was conducted using Cochrane Review Manager 5.4 version, the assessment criteria included the following seven aspects: (1) Generation of the random sequence, (2) Hidden treatment allocation, (3) Blinding of study subjects or intervention personnel, (4) Blinding of result assessors, (5) Completeness of data results, (6) Selective reporting of results, and (7) Other bias. Each item was evaluated using “Low risk of bias,” “High risk of bias” and “Unclear risk of bias.” Trials were categorized into three levels of ROB by the number of components for which high ROB potentially existed: high risk (five or more), moderate risk (three or four) and low risk (two or less).
2.5 Statistical analysis
We utilized Stata 18.0 to perform a network meta-analysis and followed the PRISMA-NMA instruction manual. This method is particularly effective for data processing in multi-arm trials, providing comprehensive comparisons of multiple interventions while the statistical power and precision of the estimates are well-maintained (39). Considering that the outcome measures were continuous variables and the assessment scales were different across included articles, we used the standard mean difference (SMD) and 95% confidence interval (CI) as the effect size measure of the summarized results, with p < 0.05 indicating statistical significance. Statistical tests were used for evaluating heterogeneity, when p > 0.10 and I2 < 50%, indicating low heterogeneity, a common-effect model was used; while p < 0.10 and I2 > 50% indicated high heterogeneity and a random-effects model was used (40). A global consistency test was conducted to assess potential inconsistency between direct and indirect evidence, and node splitting was employed to ascertain local consistency (41). If the analysis showed p > 0.05, indicating that the direct and indirect comparisons did not have a significant difference, the effect sizes of multiple treatment comparisons could be analyzed using a consistency model. If not, an inconsistency model was applied. When there were closed loops present in the comparative studies, a test for inconsistency in the loops was conducted, with a 95% CI containing 0 denoting no significant loop inconsistency.
By comparing the surface under the cumulative ranking curve (SUCRA), rankings of different MBTs were established. A higher SUCRA value implies a higher probability of ranking (42). Network funnel plots were generated and visually monitored using symmetry criteria to assess if a small-scale study could result in publication bias in the network meta-analysis. In summary, the above methods for investigating the geometry of the treatment network and potential biases contributed to a more valid and reliable network meta-analysis result.
3 Results
3.1 Literature selection
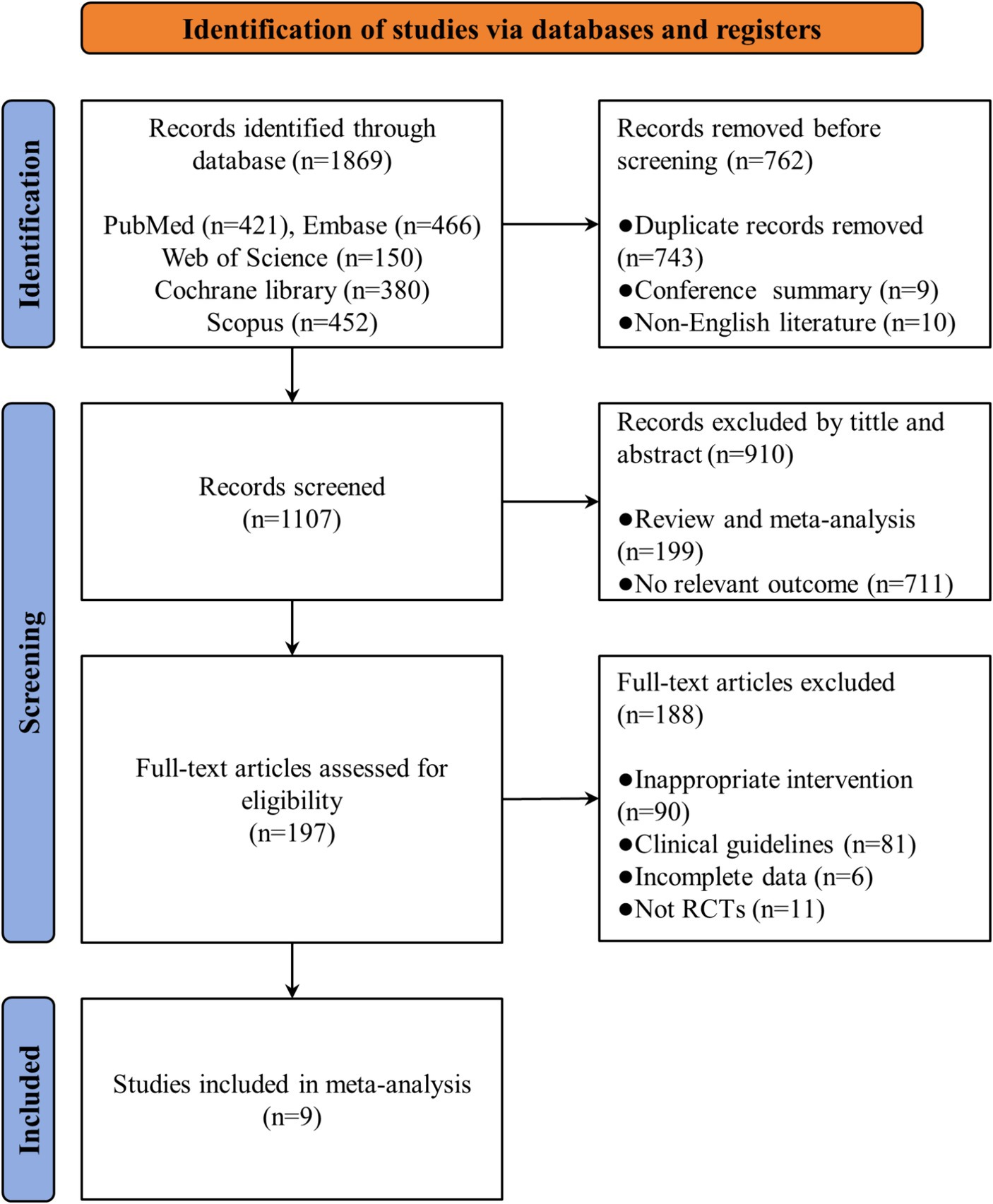
A total of 1869 articles were identified from five databases aforementioned. After excluding 743 duplicates, 10 non-English literature and 9 conference abstracts, we completed a preliminary review of titles and abstracts, excluding 910 irrelevant articles and meta-analyses. The remaining 197 articles were eligible for the full-text review, after a comprehensive and careful review, 188 articles were excluded for reasons such as being non-randomized controlled trials, containing incomplete data, being improper article types like meeting abstract, or inappropriate intervention type. Finally, we included 9 published randomized controlled trials in this systematic review and network meta-analysis. The whole selection process has been illustrated in Figure 1.
3.2 Quality assessment of the included studies
All 9 studies included in this review mentioned using methods like random number tables and computers to generate random sequences. Six studies allocation reported concealment methods such as opaque sealed envelopes. Five studies blinded patients, while only 3 blinded those who assessed the study results. The integrity of data in all 9 studies was generally good, and no signs of selective reporting were observed. Two studies showed no other biases, and for the remaining studies, other biases were unknown. The detailed quality assessment results are presented in Figure 2.
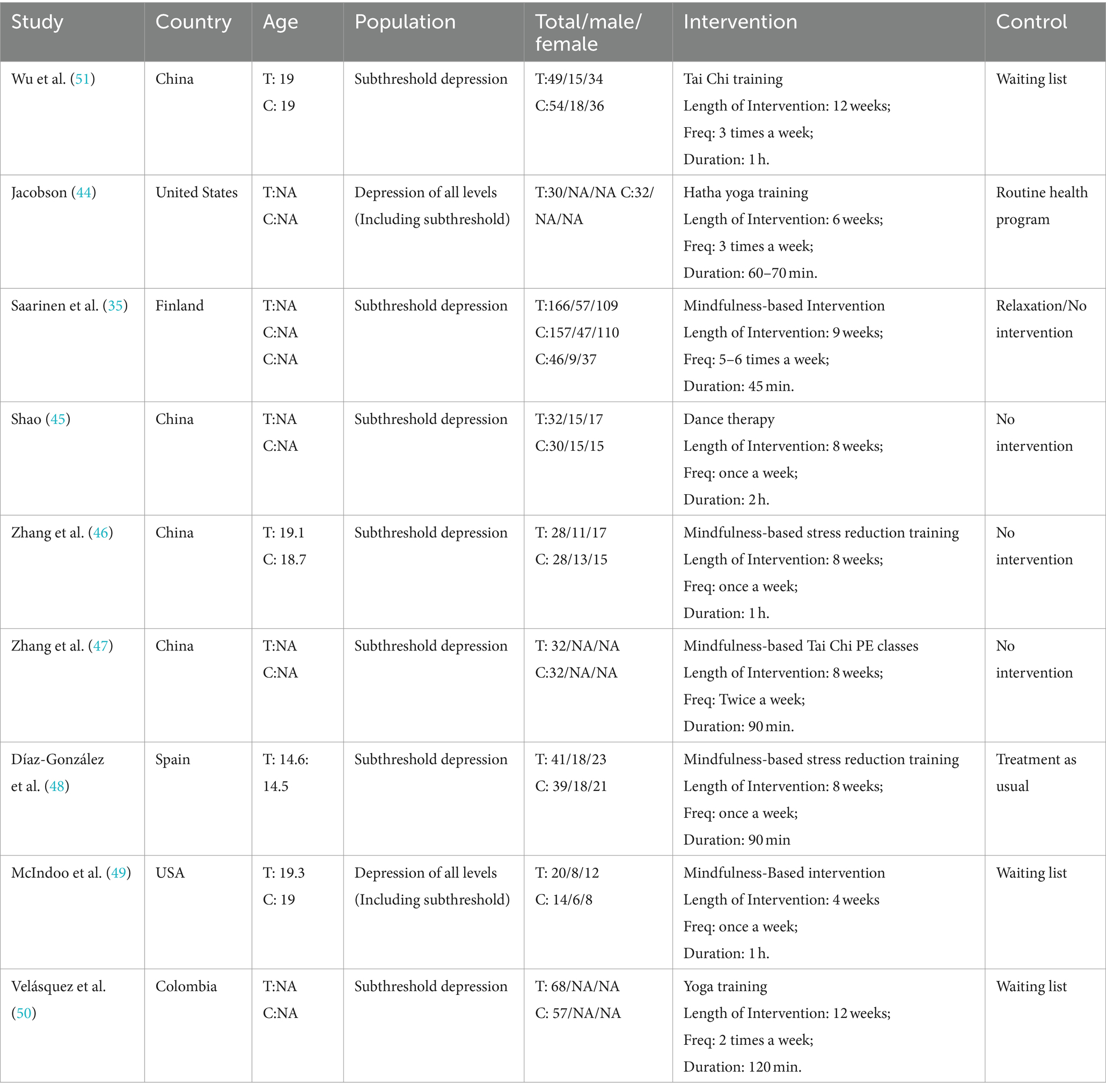
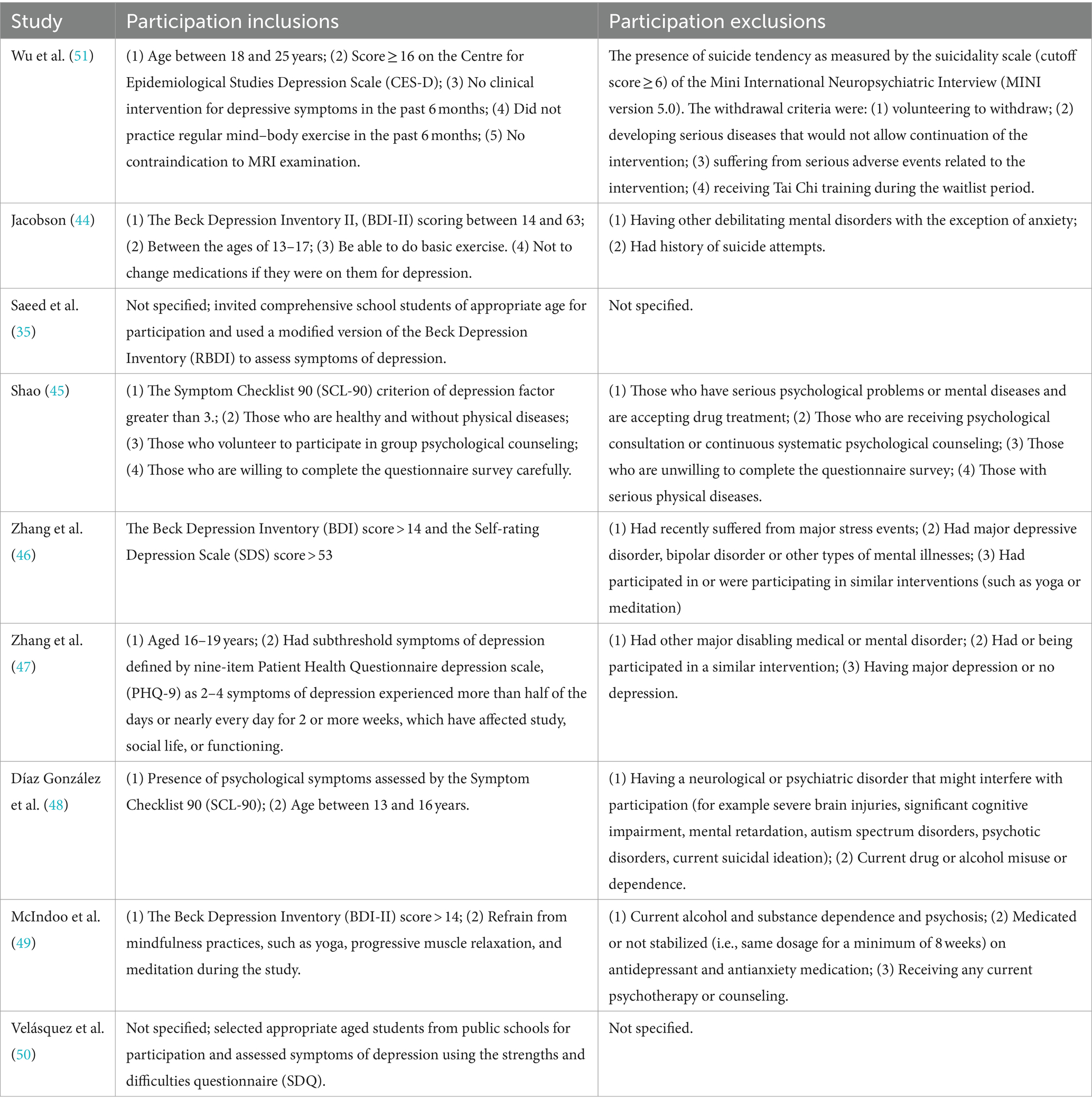
3.3 Basic characteristics of the selected studies
This study covers 9 randomized controlled trials, which involved a total of 955 adolescent patients with varying levels of depression. All participants were randomly assigned to the experimental group and control group. The experimental group was treated with a variety of interventions, including 4 involving mindfulness-based interventions, two involving yoga, two involving Tai Chi, and one involving dance therapy. Each intervention lasted 45 min–2 h, and the frequency varied from once a week to six times a week. The control group received interventions such as treatment as usual, physical exercises, and relaxation activities. The distribution of the included studies takes place in China (4), the United States (2), Spain (1), Finland (1), and Columbia (1), with the publication year mainly concentrated between 2015 and 2023. The outcome measurements varied across studies. Depression among adolescents were evaluated utilizing the Patient Health Questionnaire, Beck Depression Inventory, Revised Beck Depression Inventory, Symptom Checklist 90, and Strengths and Difficulties Questionnaire. The characteristics and details of the selected literature are summarized in Tables 1, 2.
3.4 Network meta-analysis
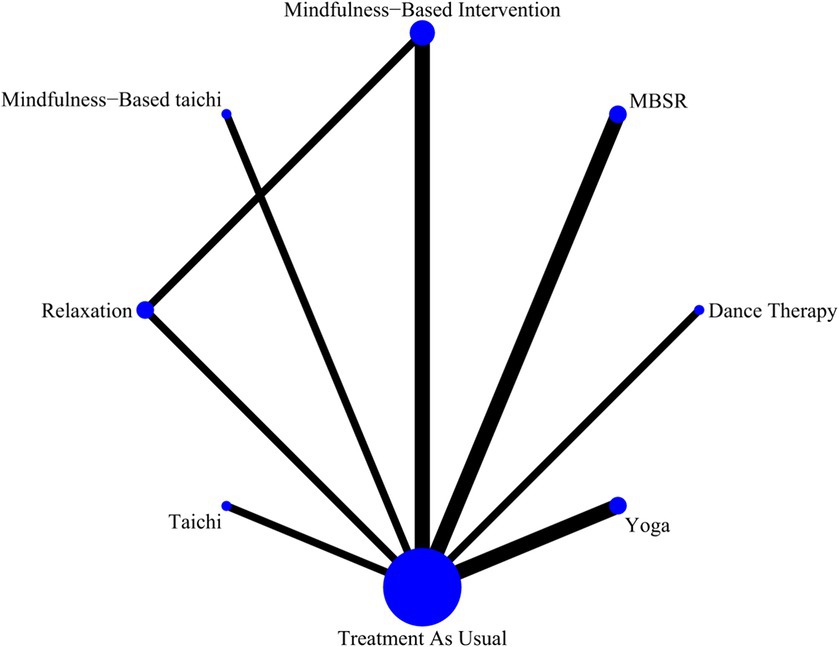
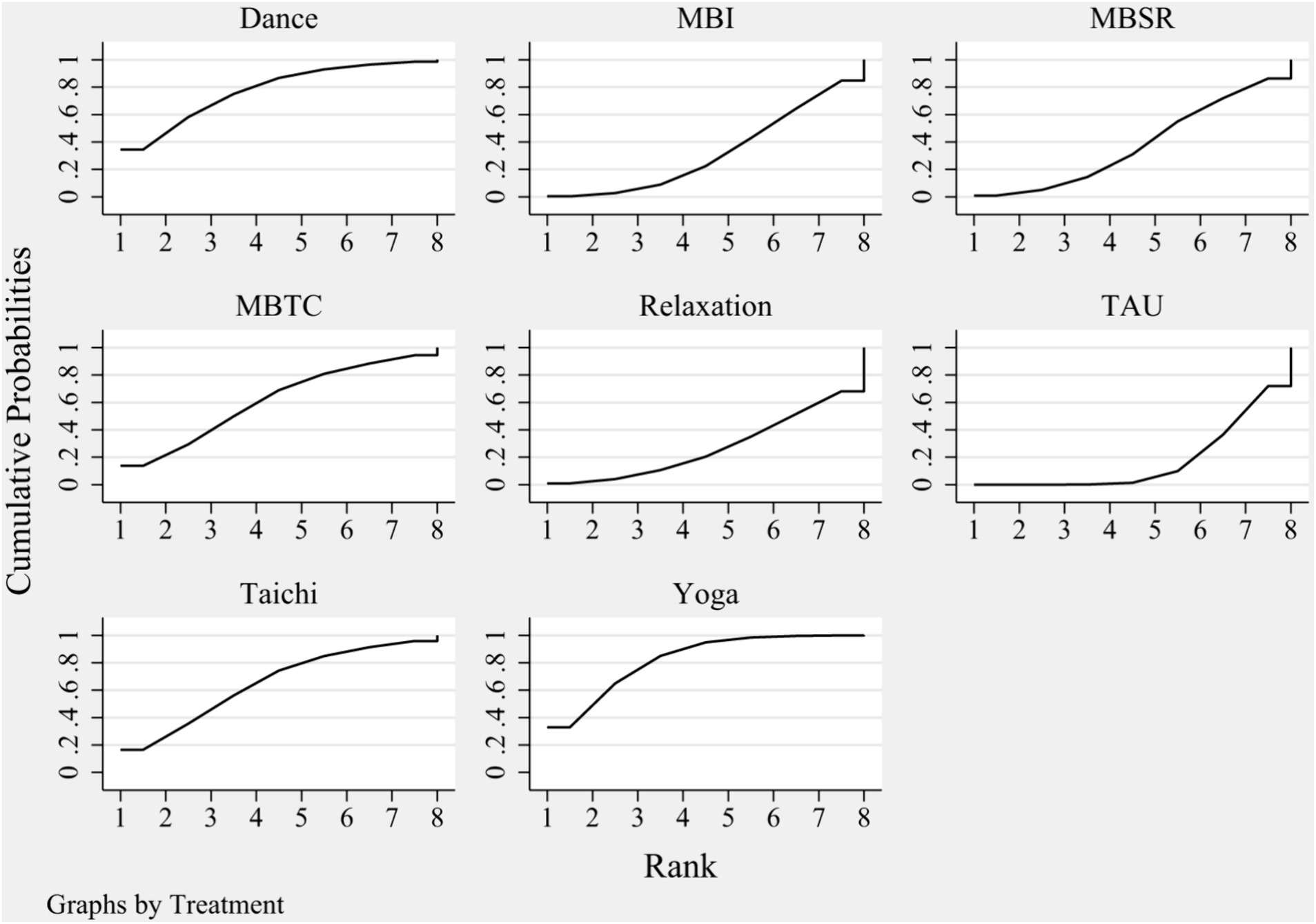
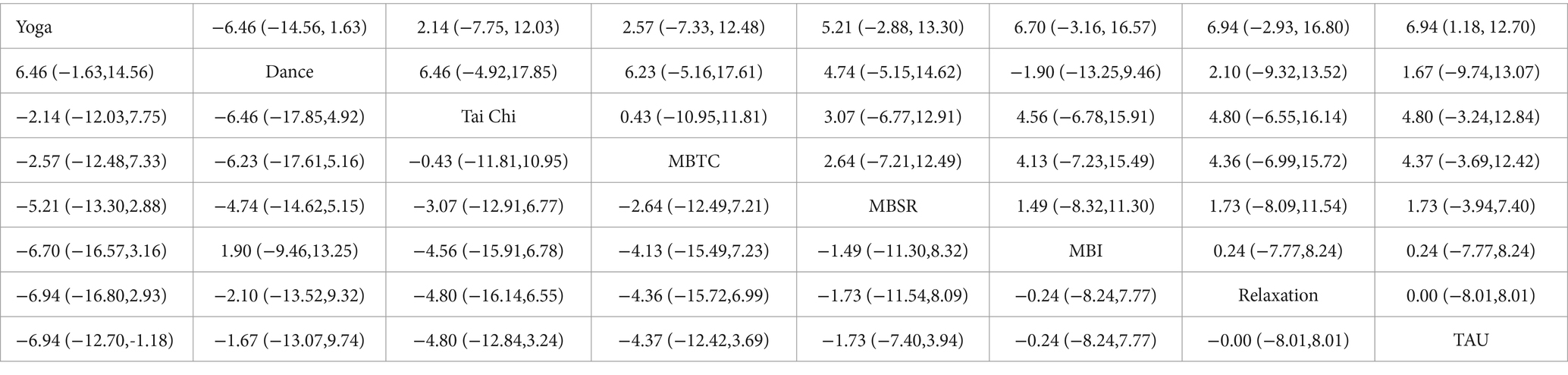
This study adheres to the principles of coherence, transferability, and consistency when conducting network meta-analysis. A network diagram (Figure 3) was established between different MBTs used to treat depression among participated adolescents. More specifically, the presence of the line between the two nodes in the diagram represents the direct comparison of studies, and vice versa. The thickness of the lines linking interventions reflects the number of studies comparing the two interventions. Figure 3 shows the comparisons among different interventions. Figure 4 demonstrates the rankings of interventions according to their potential to be the best choice for depression among adolescents (Table 3).
The p-values for indirect and direct comparisons between studies were examined for global inconsistency. The effect of consistency between studies was acceptable since all p-values were above 0.05. The network relationship was centered on treatment as usual and formed three closed loops (Figure 3) which were subjected to local inconsistency tests using the node-splitting method, and the results indicated no significant inconsistency in the closed loops.
The results of network meta-analysis showed that yoga and dance therapy were significantly effective in reducing depression when compared to treatment as usual received by the control group. In the SUCRA ranking table (Figure 4), yoga was rated to be the optimal intervention for adolescents with depression with a probability of 82.2%, followed by dance therapy (77.5%) and Tai Chi (64.9%). According to the results of ranking, the effects of decreasing adolescents’ depression of different MBTs are as follow: yoga> dance therapy> Tai Chi> mindfulness-based Tai Chi> mindfulness-based stress reduction> mindfulness-based intervention> relaxation> control group.
3.5 Publication bias test
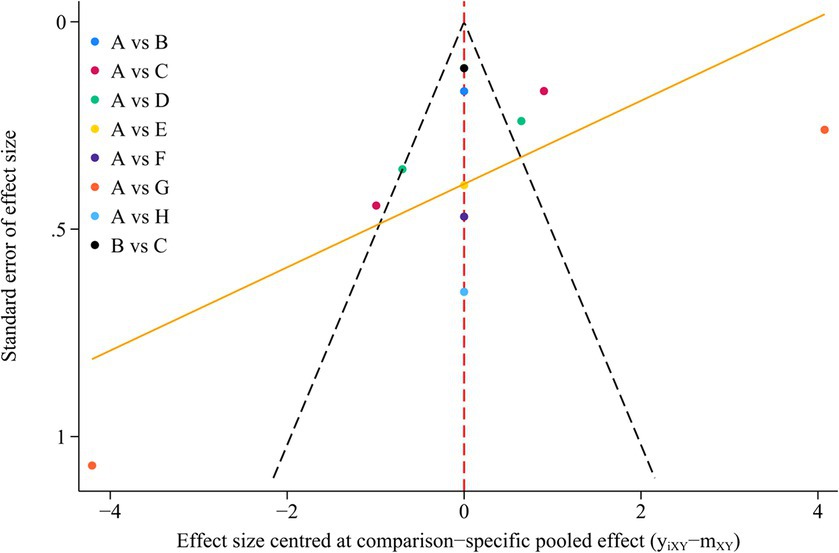
We generated funnel plot for outcomes using STATA software version 18 to asses potential publication bias. The results showed that the symmetrical distribution of all the studies in the funnel plot could not be well observed, so we further conducted the Egger’s test for quantitative analysis of the publication bias test. The p-value in the Egger’s test was 0.09, indicating that there was no significant publication bias for the outcome indicators. The funnel plot is shown in Figure 5.
3.6 Sensitivity analysis
We performed sensitivity analyses by excluding individual studies, and the results showed no significant change in the statistical significance of the outcomes in this study. This further validates the robustness of our results.
4 Discussion
This network meta-analysis aimed to evaluate the effectiveness of different mind–body interventions on depression among adolescents and compared it with the control group. The results showed that MBTs such as yoga, dance therapy, Tai Chi, significantly alleviated depression levels compared to the control group interventions. These findings are consistent with the previous reviews with respect to the effects of MBTs addressing the mental health issues among adolescents (32). Therefore, the current review findings may provide referenceable evidence to apply MBTs to the young population. Pairwise comparisons revealed that yoga and dance therapy showed stronger effects on depression than other interventions. Based on the size of the efficacy and the ranking probability of the SUCRA values, yoga proved to be the most effective for depression among adolescents (SUCRA: 82.2%), followed by dance therapy (SUCRA: 77.5%) and Tai Chi (SUCRA: 64.9%).
Yoga is an ancient spiritual discipline that includes physical postures, movement control, breathing exercises, and mindfulness meditation (52–54). These methods facilitate the integration of the body, breath, thought and affect, thereby relieving stress and psychiatric symptoms (34, 55). Our findings revealed that yoga ranks high in SUCRA values for addressing depression in adolescents, demonstrating its potential as an optimal complementary treatment option. The pathogenesis of depression has not been elucidated clearly and is currently thought to be related to biological, genetic, environmental and psychosocial factors. Initially, it was thought that depression was associated with abnormalities in monoamine neurotransmitters, with dopamine being one of them (43). Dopamine is related to emotion regulation and plays an important role in the reward circuitry (56). By affecting the neurochemicals released in the brain, yoga is considered one of the most beneficial coping strategies for reducing stress (57). Many studies have proven the effects of yoga on the regulation of the dopamine system. During yoga meditation, there was a 7.9% reduction in 11C-raclopride binding in the ventral striatum, indicating a 65% increase in endogenous dopamine release (56). In addition, yoga induces complete relaxation of the body through simple to advanced breathing exercises that bring one into a meditative state, which can enhance inhibitory neuronal function (58–60), thereby helping to adjust the overreactive state of the dopamine system (61). However, recent theories suggest that depression is also related to more complex neuromodulator systems and neural circuits (43). Typical examples such as HPA axis dysfunction and inflammatory cytokines induced by psychosocial stressors may trigger depression (62–64). Specifically, yoga’s mindfulness techniques assist in stress reduction, exert a positive influence on an individual’s ability to self-regulate (65, 66), and inhibit the overactive HPA axis function (67). In addition, the yoga components of slow breathing, relaxation practices, mindfulness of sensations in the body can activate the vagal anti-inflammatory pathways (68, 69), which could be an essential mechanism whereby yoga practice reduces depression (70).
Dance therapy is the psychotherapeutic use of movements to promote emotional, social, cognitive, and physical integration in the individual, for the purpose of improving health and well-being (71). Over the decades, dance therapy has become a typical MBTs intervention prevailing in many regions of the world and across all age groups (72). Our results indicated that dance therapy ranked second only to yoga. The antidepressant effect of dance therapy can be explained from an endocrine perspective. Firstly, endorphins are chemicals naturally produced by the nervous system to control pain or stress which are commonly labeled as “feel-good” chemicals (73). The movement, music and rhythm involved in dance therapy can affect endorphin release by significantly altering mood, stimulating intense feeling states and even strengthening prefrontal cortex function (74–79). Moreover, oxytocin is a hypothalamic neuropeptide associated with interpersonal functioning, stress coping, social memories formation and prosocial behavior in humans (80–83). Research previously found negative correlation between severity of depression and serum oxytocin concentrations in a clinical population (84). Deficits in oxytocin levels make it difficult for depressed people to cushion the negative emotions of loneliness, which is a significant predictor of depression, via the perception of social support (85, 86). Dance therapy augments the mirror neuron system when using mirroring techniques (87, 88) to produce synchronized movements, which affects oxytocin (89), thus helping to alleviate depression. Furthermore, contrary to yoga and Tai Chi, dance therapy movements may be more vigorous and rhythmic, making it more appealing to adolescents, especially young girls. Thus, the social potential of this intervention for antidepressant impact cannot be ignored. Depressed adolescents who gather to practice dance and get in touch with others struggling with similar symptoms can help them overcome loneliness and promote a positive antidepressant effect (90).
Tai Chi is a traditional Chinese fitness practice well known for its slow, fluid movements, deep breathing and meditative elements. It is particularly favored by a large group of older people as being composed of a series of gentle movements. Many studies have investigated the effects of Tai Chi on the physical and mental health of older adults (91, 92). However, the high SUCRA rankings of Tai Chi in our findings support its applicability to the adolescent population. As mentioned previously, the difficulty in regulating negative emotions caused by various stressors is an important contributor to depression among adolescents (7). However, Tai Chi’s emphasis on meditation and the connection between mind and body promotes superb emotional management (93). Besides, the deep breathing practices of Tai Chi enable individuals to cope with stressors in a more composed manner by stabilizing the autonomic nervous system, creating full relaxation of the body and mind, decreasing tension and anxiety (94). Additionally, when practicing Tai Chi, the focus on fluid body postures and combined with meditation can enhance concentration and self-harmony as well as reduce negative thoughts, which is a key factor in alleviating anxiety and depression and enables individuals to better cope with depressive emotions (37, 95).
Overall, this study bridges the research gap involving the adolescent population. The results of our network meta-analysis suggest that MBTs, particularly yoga, possess potential value in the treatment of depression among adolescents. However, it is worth noting that antidepressant medications remain the first-line therapies for the treatment of depression. Therefore, what needs to be clarified is that our findings should not be viewed as evidence that over-emphasizes such supplementary therapies. We would like to call for future research to devote more efforts to combining non-pharmacological treatments such as mind–body therapies with traditional medication and psychotherapeutic interventions, and to explore their interactions and strengths, so as to make up for the shortcomings of the existing treatment system.
5 Limitations and future directions
There are several limitations in this network meta-analysis. Firstly, we focused only on the overall effects of MBTs due to methodological limitations of the study without considering the influence of other exercise factors such as frequency, duration and intensity of exercise. Second, few studies have reported on the treatment of depression among adolescents after a longer follow-up period (no less than 6 months), even though one study showed that the intervention was still effective in reducing depression levels after 6 months, we do not suggest that it provides sufficient evidence of the long-term effectiveness for adolescent depression. Moreover, although the adoption of MBTs for the adolescent population is an emerging and promising practice, some MBTs remain underutilized, such as Qigong, Buduanjin, and Pilates, whose effects on adolescent depression have not been explored in depth. Consequently, the types of mind–body therapies covered in our current study are limited. Lastly, due to the limited number of eligible studies, we included a small sample size. The included studies were of relatively low quality and relied on self-reported outcomes measured by scales. There were a few studies that kept some depressed patients on stable medication for the duration of the trial to ensure stability due to patient health concerns, as well as a small number of studies that did not explicitly report participation exclusions, so there was a possibility that the effects of MBTs could have been slightly interfered with. Therefore, the results should be construed cautiously and might be reconsidered by researchers in the future when more quality studies are available.
In forthcoming research endeavors, it would be beneficial to discuss and investigate the dose effects related to MBTs, including the optimal frequency, duration, and intensity. Moreover, the long-term effects of MBTs on depression among adolescents deserve further investigation. Finally, it is absolutely imperative that more rigorous, standardized, high-quality randomized controlled trials be conducted to validate and enhance the reliability of the current findings. In particular, where feasible, a broader range of mind–body interventions, including but not limited to Qigong, Buduanjin, Pilates, etc., should be used to provide a more scientific and comprehensive exploration of the clinical outcomes of MBTs on adolescent depression.
6 Conclusion
Previous studies may have overlooked the application of MBTs in the adolescent population. This study is the first to explore the effectiveness of different types of MBTs for the treatment of depression among adolescents. Our findings revealed that yoga, dance therapy, and Tai Chi were effective in reducing depression level, with yoga producing the greatest effect. Considering the challenges of implementing effective interventions and the economic burden of treating adolescent depression, our findings are of significant value. However, the certainty of the evidence is limited by the small sample size of patients included and the low quality of the studies, and further investigation is necessary to strengthen the evidence base when more relevant studies become available.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
SUL: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. ZM: Supervision, Validation, Visualization, Writing – review & editing. GF: Data curation, Writing – review & editing. GM: Data curation, Writing – review & editing. XZ: Data curation, Writing – review & editing. SIL: Data curation, Formal analysis, Funding acquisition, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Education of Humanities and Social Science Research on Youth Fund (project 20YJC890016).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1431062/full#supplementary-material
References
1. World Health Organization . (2023). Depressive disorder (depression). Available at: https://www.who.int/zh/news-room/fact-sheets/detail/depression (Accessed February 25, 2024).
2. Shorey, S, Ng, ED, and Wong, CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: a systematic review and meta-analysis. Br J Clin Psychol. (2022) 61:287–305. doi: 10.1111/bjc.12333
3. Institute of Psychology, Chinese Academy of Sciences . (2023). Report on National Mental Health Development in China (2021–2022). Available at: https://cmhr.psych.ac.cn/NationalMentalHealthStatus.html
4. Griffith, JM, McCormick, KC, and Hankin, BL. Depression and depressive disorders. In: Reference module in neuroscience and biobehavioral psychology : Elsevier (2023). doi: 10.1016/B978-0-323-96023-6.00037-3
5. Hankin, BL . Depression from childhood through adolescence: risk mechanisms across multiple systems and levels of analysis. Curr Opin Psychol. (2015) 4:13–20. doi: 10.1016/j.copsyc.2015.01.003
6. World Health Organization . (2024). Setting standards for adolescent care. Available at: https://www.who.int/health-topics/adolescent-health/setting-standards-for-adolescent-care#tab=tab_1 (Accessed February 25, 2024).
7. Ahmed, SP, Bittencourt-Hewitt, A, and Sebastian, CL. Neurocognitive bases of emotion regulation development in adolescence. Dev Cogn Neurosci. (2015) 15:11–25. doi: 10.1016/j.dcn.2015.07.006
8. Casey, BJ, Duhoux, S, and Cohen, MM. Adolescence: what do transmission, transition, and translation have to do with it? Neuron. (2010) 67:749–60. doi: 10.1016/j.neuron.2010.08.033
9. American Psychiatric Association . (2022). Diagnostic and statistical manual of mental disorders Fifth Edition, Text Revision.
10. Lundy, SM, Silva, GE, Kaemingk, KL, Goodwin, JL, and Quan, SF. Cognitive functioning and academic performance in elementary school children with anxious/depressed and withdrawn symptoms. Open Pediatr Med J. (2010) 4:1–9. doi: 10.2174/1874309901004010001
11. Viduani, A, Arenas, DL, Benetti, S, Wahid, SS, Kohrt, BA, and Kieling, C. Systematic review and Meta-synthesis: how is depression experienced by adolescents? A synthesis of the qualitative literature. J Am Acad Child Adolesc Psychiatry. (2024). doi: 10.1016/j.jaac.2023.11.013
12. World Health Organization . (2021). Mental health of adolescents. Available at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (Accessed February 25, 2024).
13. Clayborne, ZM, Varin, M, and Colman, I. Systematic review and meta-analysis: adolescent depression and long-term psychosocial outcomes. J Am Acad Child Adolesc Psychiatry. (2019) 58:72–9. doi: 10.1016/j.jaac.2018.07.896
14. Fergusson, DM, Boden, JM, and Horwood, LJ. Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. Br J Psychiatry. (2007) 191:335–42. doi: 10.1192/bjp.bp.107.036079
15. Liu, Y-H, Chen, L, Su, Y-A, Fang, Y-R, Srisurapanont, M, Hong, JP, et al. Is early-onset in major depression a predictor of specific clinical features with more impaired social function? Chin Med J. (2015) 128:811–5. doi: 10.4103/0366-6999.152654
16. Wickersham, A, Sugg, HV, Epstein, S, Stewart, R, Ford, T, and Downs, J. Systematic review and meta-analysis: the association between child and adolescent depression and later educational attainment. J Am Acad Child Adolesc Psychiatry. (2021) 60:105–18. doi: 10.1016/j.jaac.2020.10.008
17. Zhan, Z, Wang, M, Suo, T, and Jiang, Y. “A continuous process” and “three stages”: an analysis of the etiology of emotional dysregulation in depressed adolescents. Adv Psychol Sci. (2024) 32:928–38. doi: 10.3724/SP.J.1042.2024.00928
18. Fried, E . Moving forward: how depression heterogeneity hinders progress in treatment and research. Expert Rev Neurother. (2017) 17:423–5. doi: 10.1080/14737175.2017.1307737
19. Hankin, BL . A choose your own adventure story: conceptualizing depression in children and adolescents from traditional DSM and alternative latent dimensional approaches. Behav Res Ther. (2019) 118:94–100. doi: 10.1016/j.brat.2019.04.006
20. Kotov, R, Krueger, RF, Watson, D, Achenbach, TM, Althoff, RR, Bagby, RM, et al. The hierarchical taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. (2017) 126:454–77. doi: 10.1037/abn0000258
21. Bellon, JA, Conejo-Ceron, S, Sanchez-Calderon, A, Rodriguez-Martin, B, Bellon, D, Rodriguez-Sanchez, E, et al. Effectiveness of exercise-based interventions in reducing depressive symptoms in people without clinical depression: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry. (2021) 219:578–87. doi: 10.1192/bjp.2021.5
22. Bahr, R. (2009). Aktivitetshåndboken: fysisk aktivitet i forebygging og behandling. Available at: http://hdl.handle.net/11250/2493895
23. Cipriani, A, Zhou, X, Del Giovane, C, Hetrick, SE, Qin, B, Whittington, C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. Lancet. (2016) 388:881–90. doi: 10.1016/S0140-6736(16)30385-3
24. Karkou, V, Aithal, S, Zubala, A, and Meekums, B. Effectiveness of dance movement therapy in the treatment of adults with depression: a systematic review with Meta-analyses. Front Psychol. (2019) 10:936. doi: 10.3389/fpsyg.2019.00936
25. Vitiello, B, and Davico, C. Twenty years of progress in paediatric psychopharmacology: accomplishments and unmet needs. BMJ Ment Health. (2018) 21:e10–12. doi: 10.1136/ebmental-2018-300040
26. Mihanović, M, Restek-Petrović, B, Bodor, D, Molnar, S, Orešković, A, and Presečki, P. Suicidality and side effects of antidepressants and antipsychotics. Psychiatr Danub. (2010) 22:79–84. https://hrcak.srce.hr/48623.
27. Walter, E, Traunfellner, M, Gleitsmann, M, Zalesak, M, and Helmenstein, C. The cost-of-illness and burden-of-disease of treatment-resistant depression in Austria. J Med Econ. (2023) 26:1432–44. doi: 10.1080/13696998.2023.2264718
28. Kella, K, Hyvönen, K, Pylvänäinen, P, and Muotka, J. Dance movement therapy for depressed clients: profiles of the level and changes in depression. Body Move Dance Psychother. (2022) 17:133–49. doi: 10.1080/17432979.2021.1927188
29. Cooney, G, Dwan, K, and Mead, G. Exercise for depression, Exercise for depression. JAMA. (2014) 2013:CD004366–2433. doi: 10.1002/14651858.CD004366.pub6
30. Wunram, HL, Hamacher, S, Hellmich, M, Volk, M, Jänicke, F, Reinhard, F, et al. Whole body vibration added to treatment as usual is effective in adolescents with depression: a partly randomized, three-armed clinical trial in inpatients. Eur Child Adolesc Psychiatry. (2018) 27:645–62. doi: 10.1007/s00787-017-1071-2
31. Zhang, J, and Hou, L. Study on the influence mechanism of sports on adolescent depression under the background of physical-medical integration. Front Sport Res. (2023) 5:1–6. doi: 10.25236/FSR.2023.050101
32. Grasser, LR, and Marusak, H. Strong mind, strong body: the promise of mind–body interventions to address growing mental health needs among youth. Ment Health Sci. (2023) 1:58–66. doi: 10.1002/mhs2.16
33. Cramer, H, Anheyer, D, Lauche, R, and Dobos, G. A systematic review of yoga for major depressive disorder. J Affect Disord. (2017) 213:70–7. doi: 10.1016/j.jad.2017.02.006
34. Cramer, H, Sellin, C, Schumann, D, and Dobos, G. Yoga in arterial hypertension: a three-armed, randomized controlled trial. Dtsch Arztebl Int. (2018) 115:833–9. doi: 10.3238/arztebl.2018.0833
35. Saarinen, A, Hintsanen, M, Vahlberg, T, Hankonen, N, and Volanen, SM. School-based mindfulness intervention for depressive symptoms in adolescence: for whom is it most effective? J Adolesc. (2022) 94:118–32. doi: 10.1002/jad.12011
36. Tao, J, Liu, J, Chen, X, Xia, R, Li, M, Huang, M, et al. Mind-body exercise improves cognitive function and modulates the function and structure of the hippocampus and anterior cingulate cortex in patients with mild cognitive impairment. NeuroImage. (2019) 23:101834. doi: 10.1016/j.nicl.2019.101834
37. Yeung, A, Lepoutre, V, Wayne, P, Yeh, G, Slipp, LE, Fava, M, et al. Tai Chi treatment for depression in Chinese Americans: a pilot study. Am J Phys Med Rehabil. (2012) 91:863–70. doi: 10.1097/PHM.0b013e31825f1a67
38. Dossett, ML, Fricchione, GL, and Benson, H. A new era for mind–body medicine. N Engl J Med. (2020) 382:1390–1. doi: 10.1056/NEJMp1917461
39. Zhang, T . A suite of network commands in Stata for network Meta-analysis. Chin J Evid Based Med. (2015) 15:1352–6. doi: 10.7507/1672-2531.20150221
40. Borenstein, M, Hedges, LV, Higgins, JP, and Rothstein, HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
41. Zhang, C, Yan, J, Sun, F, Liu, Q, Guo, Y, and Zeng, X. Identification and treatment methods for consistency of reticulated Meta-analysis. Chin J Evid Based Med. (2014) 14:884–8. doi: 10.7507/1672-2531.20140146
42. Salanti, G, Ades, A, and Ioannidis, JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
43. Wu, Y, Yan, D, and Yang, J. Effectiveness of yoga for major depressive disorder: a systematic review and meta-analysis. Front Psych. (2023) 14:1138205. doi: 10.3389/fpsyt.2023.1138205
44. Jacobson, J. (2023). Overcoming depression: A controlled randomized pre-post and follow-up test study on reducing depressive symptoms in teenagers using life-inspire yoga program [Palo Alto (CA):doctoral dissertation, Sofia university].
45. Shao, S . Intervention effect of dance therapy based on the Satir model on the mental health of adolescents during the COVID-19 epidemic. Psychiatr Danub. (2021) 33:411–7. doi: 10.24869/psyd.2021.411
46. Zhang, J-Y, Ji, X-Z, Meng, L-N, and Cai, Y-J. Effects of modified mindfulness-based stress reduction (MBSR) on the psychological health of adolescents with subthreshold depression: a randomized controlled trial. Neuropsychiatr Dis Treat. (2019) 15:2695–704. doi: 10.2147/NDT.S216401
47. Zhang, J, Qin, S, Zhou, Y, Meng, L, Su, H, and Zhao, S. A randomized controlled trial of mindfulness-based Tai Chi Chuan for subthreshold depression adolescents. Neuropsychiatr Dis Treat. (2018) 14:2313–21. doi: 10.2147/NDT.S173255
48. Díaz González, MDC, Pérez Dueñas, C, Sánchez Raya, MA, Moriana Elvira, JA, and Sánchez Vázquez, V. Mindfulness-based stress reduction in adolescents with mental disorders: a randomised clinical trial. Psicothema. (2018) 30:165–70. doi: 10.7334/psicothema2017.259
49. McIndoo, CC, File, A, Preddy, T, Clark, C, and Hopko, D. Mindfulness-based therapy and behavioral activation: a randomized controlled trial with depressed college students. Behav Res Ther. (2016) 77:118–28. doi: 10.1016/j.brat.2015.12.012
50. Velásquez, AM, López, MA, Quiñonez, N, and Paba, DP. Yoga for the prevention of depression, anxiety, and aggression and the promotion of socio-emotional competencies in school-aged children. Educ Res Eval. (2015) 21:407–21. doi: 10.1080/13803611.2015.1111804
51. Wu, J, Song, J, He, Y, Li, Z, Deng, H, Huang, Z, et al. Effect of Tai Chi on young adults with subthreshold depression via a stress–reward complex: a randomized controlled trial, Effect of Tai Chi on young adults with subthreshold depression via a stress-reward complex: a randomized controlled trial. Sports Med Open. (2023) 9:90. doi: 10.1186/s40798-023-00637-w
52. Mishra, N, and Garg, R. Yoga interventions in OCD and depression: a comprehensive review. Int J Ind Psychol. (2024) 12:1104–11. doi: 10.25215/1201.103
53. Rajkumar, RP . Biomarkers of response to adjunctive yoga-based interventions in depression: a scoping review (2024). doi: 10.20944/preprints202403.0181.v1,
54. Saeed, SA, Cunningham, K, and Bloch, RM. Depression and anxiety disorders: benefits of exercise, yoga, and meditation. Am Fam Physician. (2019) 99:620–7. https://www.aafp.org/pubs/afp/issues/2019/0515/p620.html.
55. Weinstein, R . North American yoga practitioners’ lived experiences of mind-body connection: a phenomenological study. Int J Yoga Ther. (2020) 31:043. doi: 10.17761/2020-D-19-00043
56. Singh, N . Neurobiological basis for the application of yoga in drug addiction. Front Psych. (2024) 15:1373866. doi: 10.3389/fpsyt.2024.1373866
57. Padmavathi, R, Kumar, APSDK, Venugopal, V, Silambanan, SKM, and Shah, P. Role of yoga in stress management and implications in major depression disorder. J Ayurveda Integ Med. (2023) 14:100767. doi: 10.1016/j.jaim.2023.100767
58. Chu, I-H, Wu, W-L, Lin, I-M, Chang, Y-K, Lin, Y-J, and Yang, P-C. Effects of yoga on heart rate variability and depressive symptoms in women: a randomized controlled trial. J Altern Complement Med. (2017) 23:310–6. doi: 10.1089/acm.2016.0135
59. Kuppusamy, M, Kamaldeen, D, Pitani, R, Amaldas, J, and Shanmugam, P. Effects of Bhramari pranayama on health – a systematic review. J Tradit Complement Med. (2018) 8:11–6. doi: 10.1016/j.jtcme.2017.02.003
60. Vidyashree, H, Maheshkumar, K, Sundareswaran, L, Sakthivel, G, Partheeban, P, and Rajan, R. Effect of yoga intervention on short-term heart rate variability in children with autism spectrum disorder. Int J Yoga. (2019) 12:73–7. doi: 10.4103/ijoy.IJOY_66_17
61. Grace, AA . Dysregulation of the dopamine system in the pathophysiology of schizophrenia and depression. Nat Rev Neurosci. (2016) 17:524–32. doi: 10.1038/nrn.2016.57
62. Mao, L, Ren, X, Wang, X, and Tian, F. Associations between autoimmunity and depression: serum IL-6 and IL-17 have directly impact on the HAMD scores in patients with first-episode depressive disorder. J Immunol Res. (2022) 2022:1–6. doi: 10.1155/2022/6724881
63. Morrens, M, Overloop, C, Coppens, V, Loots, E, Van Den Noortgate, M, Vandenameele, S, et al. The relationship between immune and cognitive dysfunction in mood and psychotic disorder: a systematic review and a meta-analysis. Mol Psychiatry. (2022) 27:3237–46. doi: 10.1038/s41380-022-01582-y
64. Shukla, R, Newton, DF, Sumitomo, A, Zare, H, Mccullumsmith, R, Lewis, DA, et al. Molecular characterization of depression trait and state. Mol Psychiatry. (2022) 27:1083–94. doi: 10.1038/s41380-021-01347-z
65. Friese, M, and Hofmann, W. State mindfulness, self-regulation, and emotional experience in everyday life. Motiv Sci. (2016) 2:1–14. doi: 10.1037/mot0000027
66. Keng, S-L, and Tong, EMW. Riding the tide of emotions with mindfulness: mindfulness, affect dynamics, and the mediating role of coping. Emotion. (2016) 16:706–18. doi: 10.1037/emo0000165
67. Gothe, NP, Keswani, RK, and McAuley, E. Yoga practice improves executive function by attenuating stress levels. Biol Psychol. (2016) 121:109–16. doi: 10.1016/j.biopsycho.2016.10.010
68. Brown, RP, and Gerbarg, PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: part I—neurophysiologic model. J Altern Complement Med. (2005) 11:189–201. doi: 10.1089/acm.2005.11.189
69. Oke, SL, and Tracey, KJ. The inflammatory reflex and the role of complementary and alternative medical therapies. Ann N Y Acad Sci. (2009) 1172:172–80. doi: 10.1196/annals.1393.013
70. Kinser, PA, Goehler, LE, and Taylor, AG. How might yoga help depression? A neurobiological perspective. Explore. (2012) 8:118–26. doi: 10.1016/j.explore.2011.12.005
71. American Dance Therapy Association . (2018). What is dance/movement therapy? Available at: https://adta.memberclicks.net/what-is-dancemovement-therapy
72. Dunphy, K, Federman, D, Fischman, D, Gray, A, Puxeddu, V, Zhou, TY, et al. Dance therapy today: an overview of the profession and its practice around the world. Creat Arts Educ Ther. (2021) 7:158–86. doi: 10.15212/CAET/2021/7/13
73. Ali, AH, Ahmed, HS, Jawad, AS, and Mustafa, MA. Endorphin: function and mechanism of action. Sci Arch. (2021) 2:09–13. doi: 10.47587/SA.2021.2102
74. Colcombe, SJ, Erickson, KI, Scalf, PE, Kim, JS, Prakash, R, McAuley, E, et al. Aerobic exercise training increases brain volume in aging humans. J Gerontol Ser A Biol Med Sci. (2006) 61:1166–70. doi: 10.1093/gerona/61.11.1166
75. Goldstein, A . Thrills in response to music and other stimuli. Physiol Psychol. (1980) 8:126–9. doi: 10.3758/BF03326460
76. Rodsaaad, N, Matyakhan, T, Kongyok, C, Buachuen, A, Phayakka, P, Chesa, PE, et al. Dance therapy for generation Y adolescents. Asian J Arts Cul. (2023) 23:259230. doi: 10.48048/ajac.2023.259230
77. Salerian, AJ . Endorphin agonists for severe depression. Pharmacy & Pharmacology. Int J. (2015) 2:00017. doi: 10.15406/ppij.2015.02.00017
78. Tarr, B, and Dunbar, RIM. The evolutionary role of dance: group bonding but not prosocial altruism. Evol Behav Sci. (2023). doi: 10.1037/ebs0000330
79. Tarr, B, Launay, J, Benson, C, and Dunbar, RI. Naltrexone blocks endorphins released when dancing in synchrony. Adapt Hum Behav Physiol. (2017) 3:241–54. doi: 10.1007/s40750-017-0067-y
80. Domes, G, Sibold, M, Schulze, L, Lischke, A, Herpertz, SC, and Heinrichs, M. Intranasal oxytocin increases covert attention to positive social cues. Psychol Med. (2013) 43:1747–53. doi: 10.1017/S0033291712002565
81. Eckstein, M, and Hurlemann, R. Oxytocin: evidence for a therapeutic potential of the social neuromodulator. Nervenarzt. (2013) 84:1321–8. doi: 10.1007/s00115-013-3832-6
82. Eckstein, M, Scheele, D, Weber, K, Stoffel-Wagner, B, Maier, W, and Hurlemann, R. Oxytocin facilitates the sensation of social stress. Hum Brain Mapp. (2014) 35:4741–50. doi: 10.1002/hbm.22508
83. Kosfeld, M, Heinrichs, M, Zak, PJ, Fischbacher, U, and Fehr, E. Oxytocin increases trust in humans. Nature. (2005) 435:673–6. doi: 10.1038/nature03701
84. Scantamburlo, G, Hansenne, M, Fuchs, S, Pitchot, W, Marechal, P, Pequeux, C, et al. Plasma oxytocin levels and anxiety in patients with major depression. Psychoneuroendocrinology. (2007) 32:407–10. doi: 10.1016/j.psyneuen.2007.01.009
85. Tsai, T-Y, Tseng, H-H, Chi, MH, Chang, HH, Wu, C-K, Yang, YK, et al. The interaction of oxytocin and social support, loneliness, and cortisol level in major depression. Clin Psychopharmacol Neurosci. (2019) 17:487–94. doi: 10.9758/cpn.2019.17.4.487
86. Wang, J, Mann, F, Lloyd-Evans, B, Ma, R, and Johnson, S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156–16. doi: 10.1186/s12888-018-1736-5
87. Koch, SC, Riege, RFF, Tisborn, K, Biondo, J, Martin, L, and Beelmann, A. Effects of dance movement therapy and dance on health-related psychological outcomes. A Meta-analysis update. Front Psychol. (2019) 10:1806. doi: 10.3389/fpsyg.2019.01806
88. Millman, LSM, Terhune, DB, Hunter, ECM, and Orgs, G. Towards a neurocognitive approach to dance movement therapy for mental health: a systematic review. Clin Psychol Psychother. (2021) 28:24–38. doi: 10.1002/cpp.2490
89. Feldman, R . Oxytocin and social affiliation in humans. Horm Behav. (2012) 61:380–91. doi: 10.1016/j.yhbeh.2012.01.008
90. Tao, D, Gao, Y, Cole, A, Baker, JS, Gu, Y, Supriya, R, et al. The physiological and psychological benefits of dance and its effects on children and adolescents: a systematic review. Front Physiol. (2022) 13:925–58. doi: 10.3389/fphys.2022.925958
91. Fakhari, M . Effects of Tai Chi exercise on depression in older adults: a randomized controlled trial. Bali Med J. (2017) 6:679. doi: 10.15562/bmj.v6i3.706
92. Manson, J, Rotondi, M, Jamnik, V, Ardern, C, and Tamim, H. Effect of Tai Chi on musculoskeletal health-related fitness and self-reported physical health changes in low income, multiple ethnicity mid to older adults. BMC Geriatr. (2013) 13:1–10. doi: 10.1186/1471-2318-13-114
93. Jiang, W, Liao, S, Chen, X, Lundborg, CS, Marrone, G, Wen, Z, et al. Taichi and Qigong for depressive symptoms in patients with chronic heart failure: a systematic review with meta-analysis. Evid Based Complement Alternat Med. (2021) 2021:5585239. doi: 10.1155/2021/5585239
94. Bonab, SB, and Parvaneh, M. The effect of twelve weeks of Tai Chi exercises on sleep quality, pain perception, and death anxiety in elderly women. Annales Médico-psychologiques revue psychiatrique. (2022) 180:905–11. doi: 10.1016/j.amp.2022.01.019
Keywords: mind–body therapies, adolescents, depression, network meta-analysis, yoga, dance therapy, Tai Chi
Citation: Luo S, Mei Z, Fang G, Mu G, Zhang X and Luo S (2024) Effects of mind–body therapies on depression among adolescents: a systematic review and network meta-analysis. Front. Public Health. 12:1431062. doi: 10.3389/fpubh.2024.1431062
Edited by:
Steffen Schulz, Charité University Medicine Berlin, GermanyReviewed by:
Octavian Vasiliu, Dr. Carol Davila University Emergency Military Central Hospital, RomaniaManuela Deodato, University of Trieste, Italy
Vijaya Kavuri, Svyasa, India
Copyright © 2024 Luo, Mei, Fang, Mu, Zhang and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shi Luo, bHVvc2hpMDYwNEAxMjYuY29t
 Shulai Luo
Shulai Luo Zhengyang Mei
Zhengyang Mei Guisong Fang
Guisong Fang Guogang Mu
Guogang Mu Xiuying Zhang
Xiuying Zhang Shi Luo
Shi Luo