- 1Faculty of Medicine and Health, Black Dog Institute, UNSW Sydney, Randwick, NSW, Australia
- 2Faculty of Medicine and Health, Central Clinical School, University of Sydney, Camperdown, NSW, Australia
- 3Australian Research Council (ARC) Centre of Excellence for Children and Families Over the Life Course, Sydney, NSW, Australia
- 4Faculty of Medicine and Health, University of New South Wales, Sydney, NSW, Australia
- 5Department of Psychology and Behavioral Sciences, School of Business and Social Sciences, Aarhus University, Aarhus, Denmark
- 6Institute for Health Transformation, School of Health and Social Development, Deakin University, Geelong, VIC, Australia
Mental health problems among the working population represent a growing concern with huge impacts on individuals, organizations, compensation authorities, and social welfare systems. The workplace presents both psychosocial risks and unique opportunities for intervention. Although there has been rapid expansion of workplace mental health interventions over recent decades, clear direction around appropriate, evidence-based action remains limited. While numerous workplace mental health models have been proposed to guide intervention, general models often fail to adequately consider both the evidence base and where best-practice principles alone inform action. Further, recommendations need to be updated as new discoveries occur. We seek to update the Framework for Mentally Healthy Workplaces based on new evidence of intervention effectiveness while also incorporating evidence-based principles. The updated model also integrates concepts from existing alternate models to present a comprehensive overview of strategies designed to enhance wellbeing, minimize harm, and facilitate recovery. Examples of available evidence and obstacles to implementation are discussed. The Framework is designed to support employers and managers in determining which strategies to apply and to guide future avenues of research.
Background
Employee mental health and wellbeing is arguably the most significant public health issue facing modern workplaces (1), affecting both high- and low-income countries (2). Leaders needing to think about employee mental health is no longer extraneous to business considerations or only the realm of select industries or organizations. Apart from the personal consequences of psychological injury, the costs associated with productivity loss, turnover, absenteeism, and healthcare (e.g., compensation, early retirement payouts) make this issue not only a social, but a financial imperative for businesses (3). Workplace safety is often defined around hazards (aspects that have the potential to cause harm) and risk (encompasses the probability of exposure and the extent of damage). Increasing focus on these areas in terms of mental health is occurring with major focus on psychosocial risk in the workplace.
Psychosocial risk at work
There is strong evidence linking specific workplace factors with poor mental health outcomes. These factors relate to: (i) the design and content of the work being conducted (job factors), (ii) the environment in which this occurs (operational and team factors), and/or (iii) the wider context and culture of an organization (systems and policy factors; Figure 1). Specifically these include job demands (e.g., monotony, workload, hours) (4–7), role factors (e.g., role clarity, role conflict) (8), job control (e.g., flexibility, autonomy) (4, 5, 9), routine exposure to high-risk situations (e.g., trauma, shift work) (10–13), recognition and job stability (e.g., insecurity, effort-reward imbalance) (14, 15), interpersonal relationships (e.g., lack of support, conflict, bullying and harassment) (16, 17), and organizational justice and culture (5, 16, 18, 19). In addition to an increased understanding of workplace risk factors, research efforts have produced a growing evidence-base for workplace interventions that can either modify or mitigate these risk factors (20).
Previous workplace mental health frameworks, models, and guidelines
Greater understanding of the role workplaces can play in improving population mental health has led to specific evidence-based framing and guidance in the management of risk and response to distress, illness, and incapacity. Some noteworthy examples include the Integrated Intervention Approach (21), the World Health Organisation’s (WHO) Guidelines on Mental Health at Work (2), and Thrive at Work Integrative Framework (22, 23).
Our own model, the Framework to Create Mentally Healthy Workplaces (18, 24) was based on a significant review of the available evidence base (20) and outlined the role of workplace interventions in addressing worker mental health according to five broad areas: (1) Designing work to minimize harm, (2) Building organizational resilience through good management, (3) Enhancing personal resilience, (4) Promoting and facilitating early help-seeking, and (5) Supporting recovery and return to work. Three major developments have since occurred to suggest that an update to this framework is required. Firstly, in 2022, the WHO produced their first ever evaluation and guidance for mental health at work (2). This, together with our own updated meta-review of the evidence base (25), highlights important new knowledge [(e.g., 26)] that should be translated into guidance for employers and policy makers. Secondly, national and international regulatory and legislative changes (27) have led to shifts in employer responsibilities regarding mental health at work. Thirdly, there is an opportunity to bring together some of the concepts and perspectives captured in the various workplace mental health frameworks into one unifying model.
This paper aims to provide an update of this prior framework that can be applied by organizations, guide managers and policy makers, and highlight important areas for further research. The updated Framework presents a synthesis of the major workplace models, illustrating which strategies and interventions are indicated for employees with different mental health and wellbeing support needs and the different levels of an organization where interventions can be conducted.
Updated framework to create mentally healthy workplaces
We considered two sources of evidence for the Framework update (Figure 2). Firstly, we sighted primary, secondary, and tertiary level evidence from specific programs or interventions which are rolled out to reduce risk, mental ill health, or to improve wellbeing. Secondly, we sighted evidence-informed principles underpinning mental health and wellbeing strategies within organizations. This more complete approach expands on the original Framework (24) in order to enhance recommendations for action where the most rigorous of evaluations are complex, and thus, lacking.
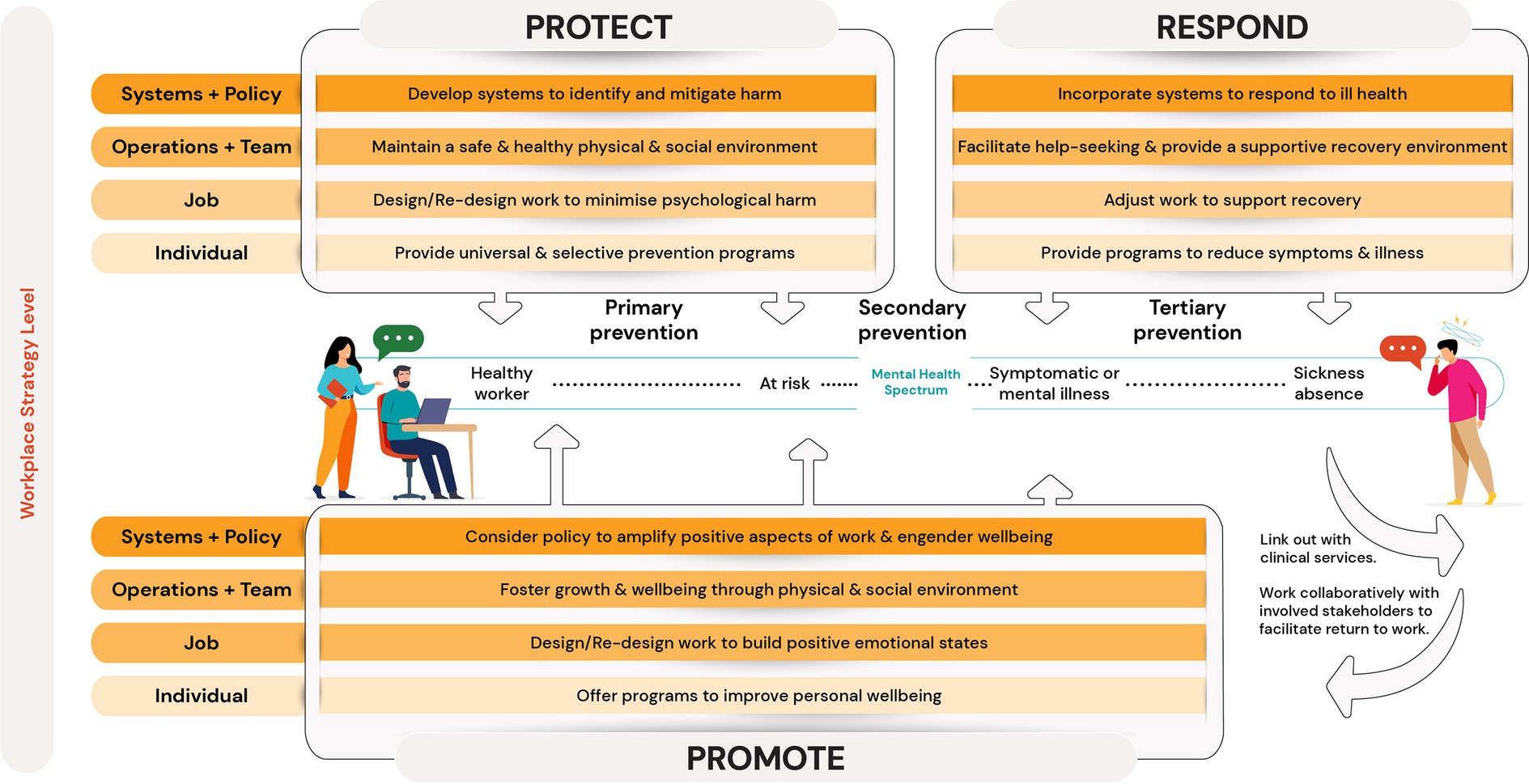
The updated Framework looks to highlight where strategies aim to deliver benefit on an individual worker’s mental health spectrum (i.e., during periods of healthy working life, in the early stages of injury or illness, or once an injury or illness is present). To this end, we adopted the Protect, Respond, and Promote pillar classifications (21, 28). Protect strategies are those primary or universal prevention interventions or initiatives in order to mitigate hazards and minimize harm or psychosocial injury. Promote strategies go beyond harm minimization and hazard mitigation and toward enhanced wellbeing and thriving. Respond strategies are those interventions that are delivered in response to a worker experiencing distress, and tertiary interventions aimed at workers who are unwell (either at-work or on leave) or returning from sick-leave. Where Protect and Respond operate at distinct ends of the mental health spectrum, promote strategies are likely to hold benefit to all workers regardless of where on the spectrum they lie, however, primary emphasis is on the early stages in the mental health spectrum.
Four workplace strategy levels provide guidance around where, within an organization, engagement is directed. These workplace strategy levels were designed to align with categories of workplace risk factors (Figure 1). The Systems and Policy level comprises of the policies or procedural arrangements operating within an organization. The Operations and Team level encompasses initiatives aimed at optimizing the interpersonal, team, and general environment in which work occurs. The Job level refers to initiatives to alter the design, delivery, or content of the work tasks being performed. The Individual level encapsulates those programs delivered to employees in order to modify perceptions and responses to conditions/experiences rather than via workplace changes. This 4-level conceptualization expands on the previous structure of organization, team, and individual levels.
In contrast to the original framework, the major changes are as follows: (i) incorporation of promotional pillar; (ii) finer delineation of the four strategy levels of intervention; (iii) richer consideration of evidence-informed principles underpinning strategies within organizations; (iv) update based on new evidence. The updated Framework was developed and is described in a way that intends to allow for variation depending on industry or size, while providing a unifying model and an evidence-based to integrate workplace mental health considerations, strategies, and interventions. The following sections synthesize the available evidence under each of these three pillars (Protect, Respond, Promote) across the four levels (Systems and Policy, Operations and Team, Job, and Individual).
Summary of the evidence base
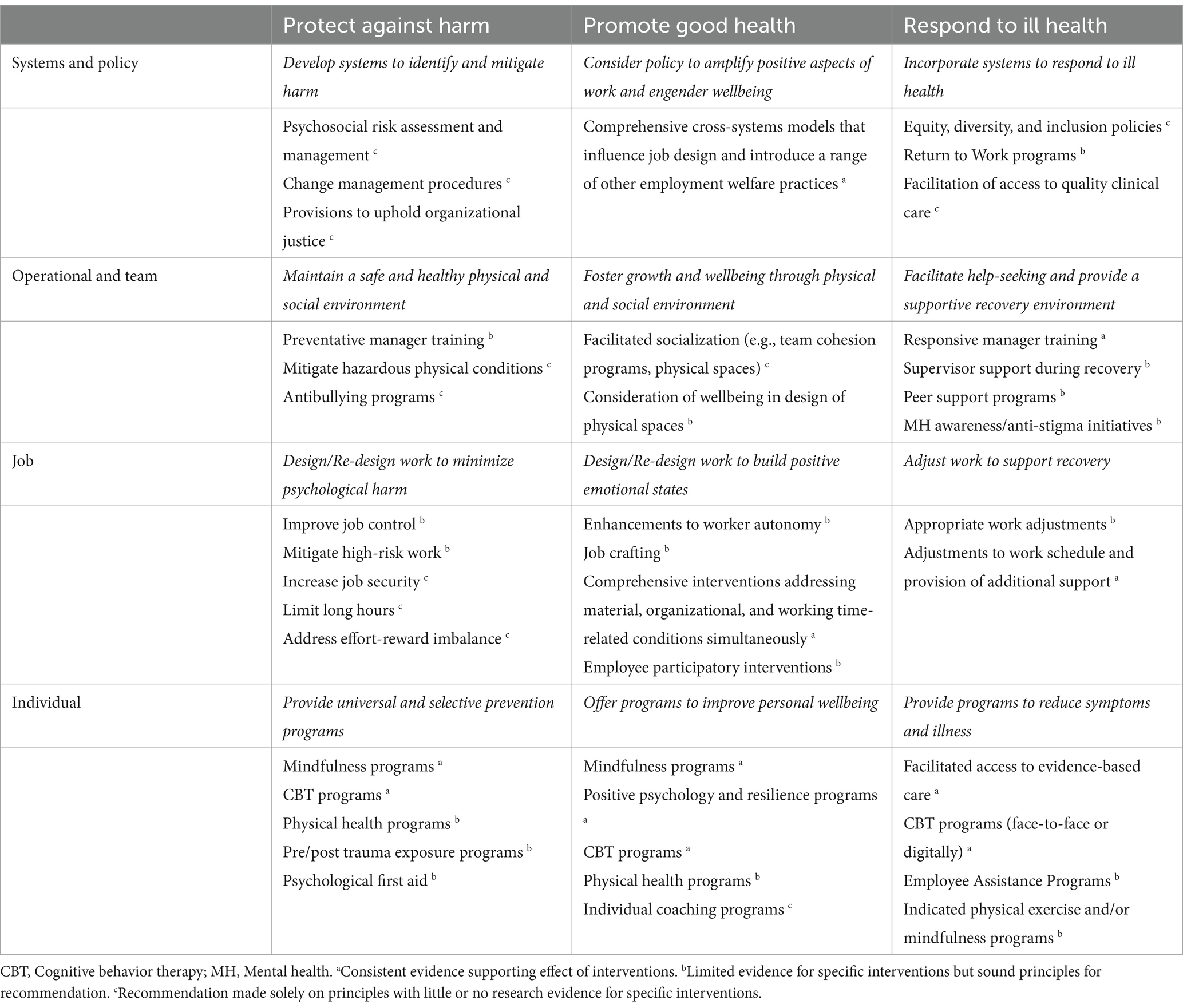
While this framework attempts to summarize the available evidence (25), it is important to highlight a disconnect that can occur between mentally healthy workplaces as defined in academic literature, and the reality of what employers are able to achieve (18). We have attempted to accommodate this research evidence gap by including some recommendations based on evidence-informed principles even if intervention trial data is lacking. In some cases, rigorous evaluation via traditional means is difficult, this is particularly true for many systems and operational interventions, we discuss this in turn. Table 1 summarizes some notable examples of workplace mental health strategies and the current level of evidence available for each of them.
Protect
“Protect” strategies involve the identification and management of work-related hazards to reduce risks to mental health to prevent and minimize harm or injury. Employers are obligated to take reasonable steps to identify and manage psychosocial hazards (along with physical, chemical, biological, radiological, ergonomic ones). Thus, compliance with legal obligations related to work health and safety, workers’ compensation, workplace relations, privacy and discrimination laws are fundamental. Relevant strategies and interventions are recommended across workplaces to meet these obligations.
Systems and policy level: develop systems to identify and mitigate harm
This category includes the systems and policies built into an organization which reflect the investment in protecting worker mental health. Where these policies aim to optimize the salutogenic aspects of the job, they are discussed in the Promote pillar, while risk management would fall under Protect and Respond. This level subsumes the broader regulatory framework within which most organizations operate. In many jurisdictions, legislative amendments and codes of practice oblige employers to implement psychosocial work factors into occupational health and safety risk assessments [(e.g., 29)]. This is exemplified by the International Labor Organization’s guidance for businesses (30) suggesting prevention of psychosocial workplace risk requires:
• Implementation of collective risk assessment and management/control measures;
• Increasing the coping ability of workers via job control increases;
• Improving organizational communication;
• Allowing workers’ participation in decision-making;
• Building social support systems within the workplace;
• Consideration of working and living conditions;
• Optimize safety and health culture within the organization.
A typical risk assessment captures what could cause harm (hazard analysis), the impact of this harm along with current precautions implemented (risk evaluation), and the implementation, monitoring and reviewing of elimination/mitigation strategies (31). This method, however, has been criticized as inadequate for psychosocial risks (32), particularly due to difficulty determining critical exposure levels. Due to this complexity, several tools for psychosocial risk assessment have been developed in recent years. A recent review identified 10 different tools of this kind (33). A lack of usage of observational methods (e.g., worker surveys) and a lack of guidance around corrective actions for employers constituted the most significant limitations of the reviewed tools.
In addition to the way organizations respond to the regulatory requirements, systems/policies should also reflect the cultural beliefs and values held regarding employee wellbeing and the prioritization of psychological health within that organization. In many cases these systems/policies provide the means for implementation of practices at various other levels (e.g., flexible working policies, procedural fairness standards). In other cases, these systems/policies are processes to better engage or communicate with workers (e.g., improving change management procedures, avenues for worker feedback/participation).
Operational and team level: maintain a safe and healthy physical and social environment
The operational and team level incorporates initiatives to prevent illness, injury, and minimize hazards and associated risks of psychological harm through improving the interpersonal or physical environment in which work occurs. To mitigate interpersonal harms of bullying and harassment, anti-bullying interventions have been developed. Unfortunately, there is currently little evidence of the effectiveness of any program of this nature despite the significant negative impact of this psychosocial hazard (34).
It is well-established that managers have considerable influence on employee mental health (35), and as such the potential benefits of effective manager mental health training has attracted increased attention. Evidence suggests that skill-based training for managers can improve knowledge, attitudes, and self-reported behavior in supporting employees experiencing mental health problems (36). Evaluation of preventative programs and employee-level outcomes are limited, however, preliminary findings are encouraging.
Physically unsafe environmental factors (e.g., faulty machinery, chemical exposure, presence of spills) have direct and indirect consequences for employee mental health (37). Recommendations focus on risk management and mitigation of such hazards, however, research in this space is limited. Relevant physical work environment factors include ambient elements (e.g., noise, temperature, air quality), spatial arrangements (e.g., layout, level of enclosure), architectural design (e.g., lighting, natural light, lack of privacy and comfort) and equipment (e.g., ergonomics, safety equipment) (38, 39). Interventions to modify the physical environment include furniture or structural barriers, break-out room space, noise canceling headphones, and lighting systems that alert staff to high noise volume in shared spaces (40). Overall, rigorous evaluation of these interventions in improving mental health outcomes is lacking.
Job level: design and re-design jobs to minimize psychological harm
Job design is an ongoing process of review and redesign where jobs are continually reshaped in response to internal and external considerations. One of the most widely researched aspects of job design is job strain, which describes high work demands combined with low decision latitude. There is strong evidence that workers who report job strain will experience poorer mental health over time compared to those who do not (41). A range of strategies have been developed to enhance employees’ decision latitude, such as problem-solving committees, health promotion and training workshops, facilitated employee control over job tasks, and stress management committees (42). While several studies demonstrate that improving worker autonomy can be protective and result in reduced psychological distress, the evidence for any specific type of participatory intervention is weak (42). Increased employee discretion may lead to negative consequences in some circumstances, for example, when increased autonomy leads to task overload and role ambiguity (43). There is evidence to suggest certain flexible working arrangements (including, worktime control, working from home) may increase employees’ control, but the direct mental health consequences are less clear (44). There is some preliminary evidence around the use of capacity-building workshops and action plans to reduce work and organizational stressors to improve morale and absenteeism, but broader effects on organization-wide improvements are lacking (45).
Emerging evidence holds promise for multidimensional job design interventions to help improve physical and psychological demands, emotional exhaustion, and social support (46, 47). The SMART work design model aims to prevent harm by increasing job resources and reducing adverse job demands (48). The model first looks to assess—both from the perspective of workers and the organizational practices—an organization’s job design and provide guidance for restructuring of roles, activities, and responsibilities. Recommendations for workplace adjustments consider the need and the readiness of the organization to make certain changes (23). Trial level evaluation of the model is limited but there is considerable evidence around the principles upon which the model is based (49) and there is substantial application of the model in practice.
Individual level: provide universal and selective prevention programs
Within the Protect pillar, individual-level interventions incorporate initiatives delivered to employees to prevent illness at a universal or selective level. There is considerable overlap with programs to enhance wellbeing and improve resilience (Promote pillar). Equally, many of these programs utilize theoretical underpinnings that also underlie indicated prevention and treatment programs (Respond pillar).
Universal prevention programs
Primary prevention programs are those offered to all individuals (regardless of health status) to better withstand the adverse impacts of stressors, preventing mental illness symptom development. In the workplace context, the most widely evaluated interventions are based on cognitive behavior therapy (CBT), stress management, or mindfulness principles. There is evidence to show that universal CBT-based programs prevent depressive symptoms in workers, albeit with small effect sizes (50, 51). In many cases, these programs are delivered digitally and have been associated with mild to moderate improvements of experiences of stress, depression, and anxiety (52–54). A metareview of a range of preventative workplace programs found good evidence for universal prevention interventions focused on CBT, mindfulness, or stress management strategies (55). These programs yielded moderate and large effects on mental health and quality of life outcomes. Mindfulness and contemplative interventions specifically yielded moderate effects on general distress. Mindfulness- and Acceptance and Commitment Therapy (ACT)-based programs have been found to be efficacious in reducing employee stress, psychological distress, burnout, poor sleep, and anxiety symptoms (56, 57), and when delivered digitally (53, 54). Programs between 1 and 4 sessions, or short-term engagement with longer programs, appear to have little effect (58).
Physical activity programs remain popular initiatives to protect against mental illness and improve mental health outcomes within organizations despite inconsistent evidence for their effectiveness, especially for workplace exercise programs (59). A related body of research has focused on the benefits of yoga or tai chi for stress or anxiety. These programs have most reliable effect where participants commit to at least 12 h of practice (60).
Selective prevention programs
Selective prevention interventions are aimed at employees at specific risk, with much work focused on high-stress, high-hazard, and high-risk occupations (e.g., first responders, military personnel, healthcare workers). Most programs have utilized CBT or mindfulness techniques (46, 61–63), with some evidence supporting physical activity programs to improve mental health outcomes (64). A recent umbrella review of 16 meta-analyses found that psychosocial selective prevention interventions were associated with small and moderate effects on depression, anxiety, and stress outcomes (55). Mindfulness-based interventions were associated with small effects for general distress and burnout, and with moderate and large effects on depression and stress and anxiety (55).
Many selective prevention interventions target the effects of work-related exposure to traumatic events (65). Post-incident interventions show the strongest support for the utility of trauma-focused CBT for individuals with a diagnosis of acute stress disorder (65). Team-based skills training has also been shown to reduce poor mental health symptoms after major incidents (66). Emerging evidence suggests the potential of mind–body exercise programs for trauma-exposed workers (67). Pre-incident interventions include pre-stress inoculation training (68) and attention bias modification training for the prevention of posttraumatic stress disorder (PTSD) (69, 70). Stress inoculation training is a form of CBT aimed at shifting negative bodily and mental reactions to stressors, helping the person cope with and manage difficult emotions (via direct [e.g., problem solving], and indirect [e.g., self-talk, breathing exercises] strategies). Attention bias modification training is a process to modify attention to attend to specific target stimuli and ignore others, attempting to correct attentional biases inherent in certain disorders. For pre-incident interventions, however, strong evidence is lacking. It should be noted that most trauma-focused selective prevention intervention studies engage military personnel, which limits the generalizability of findings to other occupational groups.
The importance of a strong evidence-base for initiatives to mitigate risk and protect trauma-exposed workers from harm has been underscored by the practice of psychological debriefing (following critical incident exposure). Importantly, research has consistently found such practices to be of minimal benefit and potential harm (71). Current guidelines discourage this form of debriefing, with a focus instead on watchful waiting (71) and practical support (72). Psychological first aid (PFA) has also become a popular intervention following exposure to conflict or disaster, emphasizing reduction of initial distress, addressing of basic needs, and promoting adaptive coping. Early studies have suggested PFA is a helpful and safe alternative to debriefing (73). As much as possible, workplaces should seek to increase social support and reduce work pressures in the period following exposure to traumatic events.
Promote
While most emphasis is placed on harm prevention and response (due in part to regulatory considerations), there is growing interest in how positive aspects of work and strengths-based approaches can facilitate sustained and enhanced wellbeing outcomes (43). Traditionally, attention within workplace to mental health (where it exists) has been driven by an illness ideology (identifying risk factors for mental illness, underlying mechanisms, and appropriate intervention), with little attention given mental health and wellbeing and means to promote it (74). This is driven by the common conflation of the absence of mental illness with true mental health (74, 75), and further compounded by the regulatory and liability considerations of illness and injury. The Promote pillar captures initiatives that enhance the positive aspects of work as well as worker strengths and capacities in pursuit of positive outcomes (e.g., joy, engagement, job satisfaction). Wellbeing is a central concept in the Promote pillar with social, psychological, spiritual, and physical dimensions are all relevant (76). Traditionally, definitions of wellbeing tended to focus on psychological wellbeing as a composition of autonomy, positive relations with others, purpose in life, self-acceptance, environmental mastery and personal growth (77). In recent years, there has been a shift on PERMA theory of wellbeing encompassing aspects of both subjective wellbeing (positive emotion, meaning) and psychological wellbeing (engagement, relationships, accomplishment) (78). Thompson and Marks (79) suggest the wellbeing can be conceptualized as a dynamic process which asserts that individuals can flourish and experience subjective wellbeing through personal resources (e.g., optimism, self-esteem), appropriate external conditions (e.g., safe, secure, suitable environments), and psychosocial engagement (e.g., social connection, autonomy, respect). Organizations have capacity to influence these domains through policies, practices, design, and intervention. Workplace research in this space often centers on the concept of “thriving,” which is positively associated with affect, work engagement, and a range of social and health-related outcomes (80).
Systems and policy level: consider policy to amplify positive aspects of work and engender wellbeing
To reflect the shift in mental health conceptualizations toward a more holistic regard for a person’s overall wellbeing (81), this category encapsulates policies and practices that strive to enhance positive wellbeing, optimize the benefits of work, or promote working within a strengths-based approach. Comprehensive programs that integrate both organizational and individual approaches such as Total Worker Health (TWH) have demonstrated positive impact on wellbeing outcomes (82, 83). The TWH approach incorporates programs in line with a hierarchy of controls around elimination/control of hazards, substitution of practices, work redesign, education, and individual change. Similarly, a review of 33 studies utilizing system-wide approaches that simultaneously enhance job design and introduce a range of other employment welfare practices concluded that such programs were associated with improvements in employee wellbeing and performance (84).
Central to employee wellbeing are cultural aspects inherent to workplaces including how organizations are designed and managed. Perceptions of support are a critical factor, while the development of psychologically safe environments are a means to engender such perceptions (85). A psychologically safe environment is one based on mutual trust in which employees feel confident to raise ideas, questions, concerns and make mistakes without fear of punishment, rejection, or humiliation (86) which relates positively to employee wellbeing (87, 88). Although theoretically appealing little is known on the impact of specific interventions in this space.
Operational and team level: foster growth and wellbeing through a physical and social environment
Social wellbeing focusses on the extent to which individuals have meaningful relationships with others. Social integration, sense of belonging, interdependence, collective consciousness, and collective fate have been identified as key determinants of social wellbeing (89). The kinds of workplace initiatives often employed to target relational enhancements include team cohesion programs (e.g., social events, retreats) and the creation of communal spaces to increase social connection (90, 91). Generally, these programs are delivered as components of broader programs, thus, determining the specific role of singular components is difficult (92). Despite consistent evidence for the importance of co-worker relationships for employee job and life satisfaction (93–95), there is an absence of evidence around how to best improve such relationships (96). A recent review found only six studies of interventions in this space and while there is some evidence that interventions increasing the frequency of shared activities could improve worker performance and social environment, findings were inconsistent, and the overall impact on wellbeing remains unclear (90).
Spatial considerations (e.g., natural light, outdoor space) have also been linked with employee wellbeing particularly when employees are involved in the development of such design and placement considerations (38, 97). Open outdoor spaces have been linked with enhanced socialization, active relaxation, and stress reduction (98). Interventions incorporating natural and green spaces have been found to increase positive emotions in the workplace and can lead to long term improvements in functioning and wellbeing (99). Evaluations on the use of indoor plant installations suggest that plants can improve air quality, employees’ perceived comfort, psychological wellbeing, and reduce fatigue (100). Overall, however, physical environmental evaluations tend to be of low quality and meta-analyses are lacking. Furthermore, studies that do exist tend to focus exclusively on office environments.
Job level: design and re-design jobs to build positive emotional states
There is considerable overlap between strategies to protect and those to promote at a job level, that is, practices which eliminate or successfully mitigate psychological hazards can often also promote positive wellbeing (101, 102). For instance, the SMART work design model aims to enhance workplace wellbeing and thriving within workers beyond simply minimizing hazards to reduce risks (48).
A review of interventions aimed at promoting employee health more broadly through altering working conditions (e.g., work time, intensity, job demands/control) reported significant positive effects in approximately half the studies included (103). Success rates were greater for comprehensive interventions addressing material, organizational, and working time-related conditions simultaneously. A review of healthcare-based interventions to facilitate “sustainable jobs” found that critical components included the enforcement of health and safety obligations, improvements in the workers’ compensation process, the provision of flexible work arrangements, and the integration of employee participation in decision-making (104).
Autonomy at work is strongly related to subjective wellbeing, specifically satisfaction with life and positive affect and is associated with a reduced negative affect (105). Autonomy is closely linked to job control and flexible working conditions, which also contribute to a range of positive health effects (106–108). Similarly, initiatives to improve self-efficacy, mastery (109) and reward/recognition systems (110, 111) are likely to have beneficial effects on employee wellbeing. Few available interventions have been evaluated from a targeted wellbeing perspective, with most instead focused on occupational outcomes (e.g., job performance, turnover intentions).
Job crafting is a means to build autonomy that can circumvent impracticalities of designing jobs to fit all employees (112). Through job crafting, employees can modify tasks and roles to suit their optimal ways of working (113–116). This form of job design is distinctive in that it takes a “bottom-up,” employee-initiated approach, rather than the traditional “top-down” approach in which managers/employers create jobs and roles (117, 118). Job crafting has been linked to increased employee health, job satisfaction, and engagement (119–121). A recent review highlighted the mediating role that job crafting may play in relation to transforming social resources into improved work outcomes (122). However, as this intervention is less prescriptive, there can be unintended consequences stemming from particular decisions employees make in the crafting process (119, 123).
Individual level: offer programs to improve employee wellbeing
Individual wellbeing interventions usually have a dual function, both increasing positive psychological states and contentment, and reducing negative outcomes such as burnout and absenteeism (124). There is evidence that, in addition, to enhancing mental health directly, such programs can moderate the impact of job stressors (125).
Most individual employee wellbeing interventions utilize physical activity, mindfulness or meditation, positive psychology, or resilience training principles. A recent review found that psychological interventions (e.g., mindfulness and CBT-based approaches) were among the most consistently high-performing interventions to improve worker wellbeing (126). Mindfulness-based programs are among the most widely implemented and evaluated in the workplace. Such programs have been shown to increase positive affect, improve overall wellbeing, life satisfaction, and resilience (126–130). Further findings reported additional benefits to stress and mental health (131). A review of meta-analyses found universally-delivered mindfulness and contemplative interventions yielded a large effect on subjective wellbeing (55). Mindfulness-based interventions also showed a moderate improvement in self-compassion. Compared to mindfulness interventions, CBT-based interventions showed slightly smaller but significant positive effects on wellbeing. Among selectively-delivered programs, psychosocial interventions of this kind had small-to-moderate effects on optimism, self-efficacy, and resilience, and a large effect on positive emotions.
Positive psychology interventions tend to be gratitude- or mindfulness-focused and have also been associated with small-to-moderate effects on work engagement, job performance, and perceived job stress (132). Evidence suggests further positive associations with wellbeing, job and life satisfaction, self-compassion, relaxation, and resilience as well as negative associations with symptoms of depression, anxiety, burnout, and general distress (133). Meyers and colleagues (134) found strong evidence for workplace positive psychology interventions in enhancing employee wellbeing. Resilience interventions based on a combination of CBT and/or mindfulness techniques have also been recommended to both improve wellbeing and reduce the risk of mental ill health (135). Reviews of such resilience trainings indicate positive effects on subjective wellbeing and mental health (136, 137), at least in the short-term (138). Similarly, there is some evidence for the usefulness of CBT solution-focused coaching (and goal setting) (139). There is also emerging evidence exploring the use of spiritual interventions (particularly in healthcare settings) for improving quality of life and wellbeing (140). However, largely these studies are predominantly yoga or mindfulness/meditation based (141).
Several reviews exploring the efficacy of physical health or exercise programs at work focus on productivity outcomes (142–144). Although there is also promising evidence that these interventions (e.g., yoga, walking) can be effective in improving wellbeing, inconsistent findings and low study quality limit conclusions (143, 145). There is also some support for music and art-based interventions on psychological wellbeing among healthcare workers (146). However, evidence tends to be of lower quality.
Respond
Workplaces have in important role in responding to psychological distress and mental illness of employees. Organizations can support workers who experience mental health problems by building appropriate systems, facilitating care, and offering appropriate adjustments and programs to staff. As with the Protect pillar, in most jurisdictions there are legislated requirements such as workers compensation, discrimination, privacy, and workplace relations laws that direct some aspects within this pillar.
Systems and policy level: incorporate systems to respond to ill health
How an organization responds to employees showing signs of distress or mental ill-health is in part directed by the broader regulatory framework within which it operates. Relatedly, equity, diversity and inclusion practices are pertinent (e.g., destigmatization). A systematic review of international guidelines found implementation of workplace mental health strategies was often impacted by inconsistent language and a lack of consultation with diverse populations (147). To help comply with legal and ethical requirements, organizations should recognize and address the unique mental health needs related to diversity (e.g., cultural, gender, sexual orientation, ability). While anti-discrimination policies, inclusive hiring practices, and the provision of diversity training is also critical.
Early identification of mental health problems to facilitate care is essential. Wellbeing checks or mental health screening tools are regularly used by organizations to identify those in need of follow-up and intervention. While some early studies indicated that mental health screening in the workplace hold value in improved employee health (148), others have not been able to replicate such findings (149, 150). Further, ineffective screening has the potential to cause harm (151). Most recent findings suggest this kind of screening to only have benefit when linked to enhanced access to treatment (26). As such, currently mental health screening programs have not been recommended in international guidelines for workplaces (2). Although education around care options is important to empower and deliver care, universal approaches followed by advice or provision of referral options is likely to be ineffective in facilitating help-seeking. This is distinct from assessment in the course provision of care or where facilitated access to care occurs which is a necessary component of treatment.
Return-to-work (RTW) planning is generally considered central to recovery and successful reintegration of employees experiencing psychological injury (2). Planning should consider clarity of roles, alignment of worker-employer expectations, advocacy provided by the RTW coordinator, support for the worker’s psychological wellbeing, and the literacy of supervisors and colleagues (152). A recent UK-based review explored evidence for frequently used workplace adjustments related to psychological injury recovery (153). These included adjustments to work schedules, roles and responsibilities, work environment, policy changes, support and assistance, and redeployment. Out of these adjustments, only the work schedule and support and assistance recommendations had evidence of associated health outcomes. Furthermore, despite many workplace adjustments consistently being perceived as effective by staff and stakeholders, adequate testing is lacking and significant barriers to accessing and implementing workplace modifications exist (153).
An Australian rapid review (154) highlighted key themes among programs designed to enable recovery at work or RTW. Themes included the importance of destigmatization, mental health policy, recognition of early warning signs, addressing harms, collaboratively planning (with individual/employer/healthcare provider/case manager), and sustained communication during absence and upon return. While acknowledging a lack of clear evidence for the effectiveness of identified themes, the review recommended that flexible working arrangements, workplace modifications, setting of realistic goals and job expectations, identification of RTW barriers and facilitators, and maintaining trust and confidentiality between the employee and organization should be included in recovery at work or RTW plans.
Operational and team level: facilitate help-seeking and provide a supportive recovery environment
Operational or team strategies to respond to mental ill health tend to focus on worker- and illness-directed interventions and initiatives to facilitate help-seeking and support recovery. Some of the best evidence for tools to support this process is associated with skill-based training for managers (2). Supervisor support is consistently associated with a range of positive outcomes after a psychological injury at work, including reduced symptoms of poor mental health (155). Evidence indicates that training which focuses on enhancing manager confidence and teaching them new skills in having mental health focused conversations generates improved rates of supportive managerial behaviors (36). There is also evidence from controlled trials that such training also results in reduced rates of work-related sick leave for employees experiencing mental health problems improvements in mental health symptoms at the level of employees have not yet been clearly established (36).
Mental health awareness and anti-stigma programs are also commonly used tools that aim to improve knowledge about mental ill-health and reduce stigmatizing attitudes and discrimination. Evidence suggests that such interventions can have a small positive effect on mental-health knowledge, attitudes, and self-reported supportive behavior, confidence, and readiness-to-help (156–158). There is, however, only limited evidence of sustained improvements of behavior change are mostly derived from subjective self-reports rather than objective observations. Furthermore, how such changes may improve individual symptoms is seldom examined. Relatedly, Mental Health First Aid (MHFA), attempts to teach recognition and response to mental health problems/crises to facilitate help-seeking. This type of training has been associated with improvements in knowledge, attitudes, symptom/sign recognition, and confidence in management of distressed workers (156). MHFA training has also been associated with improvements in reported intentions and provision of support, however, changes in observed behaviors and quality of provided support as well the magnitude of MHFA training impact on any mental health outcomes remain unclear (159).
Peer support programs—in which a small group of specially trained employees provide wellbeing support to other employees—are an emerging form of intervention, especially in high-risk occupations (160, 161). Such programs, which are primarily aimed at improving rates of early help-seeking, have been associated de-stigmatization and fewer perceived barriers to care, with emerging evidence that these shifts may result in reduced sickness absence (162).
Job level: adjust work to support recovery
RTW policy, supportive environment, active management, RTW plans, and collaborative consultation are considered critical aspects in supporting recovery (163). Labor market integration initiatives including different countries’ laws against discrimination on the basis of disability [(e.g., 164)] require employers to provide reasonable adjustments to ensure that employees with disabilities are not discriminated against in the workplace. Job-level adjustments (including, working hour adjustments, staggered return, review of tasks/goals/expectations, private areas, recording of meetings) also apply where recovery takes place in conjunction with work. In addition to adjustments and RTW planning Clayton and colleagues (165) also recommend training and education for staff and managers.
Individual level: provision of programs to reduce symptoms and illness
Unlike universal or selective approaches, these interventions are aimed at employees who already have symptoms of mental health conditions, with the aim of limiting the progression of illness (“indicated prevention”) and treating those with clinical conditions.
Evidence for indicated prevention for depression supports CBT approaches (55), with some evidence for indicated physical exercise, mindfulness, and resilience training interventions for employees identified as being at-risk of or with early symptoms of a mental illness (166). Digital CBT-based interventions also have been shown to have small effects on depression and anxiety symptoms, while digital stress management interventions have shown promise, but with limited evidence for reducing depressive symptoms and stress (54).
One of the more common interventions offered by organizations to respond to employees experiencing psychological distress at work is workplace counseling, usually facilitated by externally contracted employee assistance programs (EAPs). Workplace counseling can be effective in improving anxiety, stress, and depressive symptoms, but the effectiveness is dependent on the type and quality of psychological intervention provided, which can be very broad and ill-defined (167, 168). More recent reviews on EAPs specifically support the effectiveness of such programs to improve levels of presenteeism and functioning (169). Generally, studies in the area have been of lower quality, with methodological limitations and there is also a lack of meta-analyses to determine overall strength of evidence (170).
Discussion
This updated Framework seeks to better coordinate strategies and interventions for improving mental health and wellbeing in the workplace and provide recommendations for best practice. There remains a very large gap in knowledge around key aspects of what would constitute effective evidence-based workplace interventions. Some have argued this is in part due to a lack of integration of interdisciplinary expertise and prevention strategies (147), while the complexities of conducting high-quality trials of multifaceted interventions within workplaces are undoubtably also an issue (18). The intricacy of developing tailored interventions for specific workplaces is a further barrier to research practice and scalability. However, recent high-quality studies testing specific workplace interventions suggests that these challenges are not insurmountable and that further research on popular or promising workplace practices must occur.
The evidence base for interventions is clearest at an individual level (as opposed to job, team, or system level) where evaluation studies are least onerous to conduct, involve fewer uncontrollable confounders, investment costs, and demands on organizations. This also highlights a tendency of workplaces to favor changes at the level of an individual worker rather than changes to the work or organization (103). This risk of this approach is twofold. Firstly, it places the onus to remain mentally well on employees and risks overlooking mental health-averse operational or systemic factors that may be present. Secondly, there is a real possibility that the most effective workplace interventions will be at the level of organization-wide or systems-level changes. However, if a robust evidence-base for these is not developed, then best practice cannot be ascertained. It is for these reasons that this new Framework incorporates advice based on both intervention studies and robust, evidence-based theory. Difficulties in conducting trial-based research may require reassessment of the value of traditionally less methodologically rigorous means of evaluation, including high quality observational evidence (e.g., triangulation, natural experiments) (171–173).
In light of an increasing appreciation for the role and benefits of maintaining mentally healthy workplaces (2), these efforts can no longer be considered tokenistic or relegated to individualized, disconnected programs. Although it is important to evaluate specific components to determine the key elements of success, at the level of implementation, holistic multi-level approaches are required that support all workers no matter where they fall on the mental health spectrum, involving all levels of an organization.
It should also be acknowledged that a multitude of external aspects, including broader regulatory and policy frameworks, health and community services, welfare systems, individual lifestyle factors, social networks, and socioeconomic and biological antecedents, influence employee mental health and wellbeing and can impact what workplaces can do to support workers. It is also important to consider both individual disorders and the impacts of comorbidities, both with other mental health conditions, substance use, and physical health conditions and the additional complexities such comorbidities can present. It must therefore be stressed that employers are not solely responsible for employee mental health but are responsible for providing a workplace as free from recognized hazards to mental health and wellbeing as feasible, and for providing a non-discriminatory work environment that promotes wellbeing and recovery from any mental health symptoms that arise. Furthermore, there are important considerations relating to external systems that can inhibit or facilitate action in this space. Compensatory pathways, for instance may provide significant barriers to the recovery process (174). For instance, the definitions around “injury events” and explicit requirements relating to workplace factors and disease causation/contribution differ in different regions, which will impact recovery and return-to-work. The implementation of certain comprehensive programs may also face barriers and challenges during where these external factors are involved (175). In addition, mandatory reporting frameworks and potential career harms of reporting in different roles and industries may impact capacity to provide resources or care options to those in need. It is critical that policy makers and organizations consider the potential stigma and consequences of these factors and appropriately balance worker safety with confidential care options promoting early intervention.
One of the most difficult aspects in providing strong business level recommendations is the heterogenous nature of—not only industry sectors—but individual businesses within a sector. Employers must therefore consider their individual business circumstances, current practices, and risk factors specific to their workplace. The updated Framework looks to categorize specific strategies on different levels of an organization to aid identification of appropriate measures. It should be reiterated that many interventions do not discretely incorporate just one element, address just one pillar or level, or target a single outcome. This segmentation is meant to aid in the identification of appropriate strategies and gaps in an organization’s existing approach. In some cases, particularly at the individual level, there is significant overlap of strategies. Segmentation is useful to highlight where these approaches have differential impact but there tends—unsurprisingly—to be expansive benefit not limited to protect, promote, or respond in isolation. Best evidence presented here, suggests mindfulness and physical health programs may form useful universal protective programs, which also promote wellbeing, while most evidence for CBT programs focuses on symptom reduction (i.e., indicated care). Peer support, similarly, is an example of an intervention which can hold protective, responsive, promotional benefit and future research is needed to explore specific benefits of such programs.
A critical gap in the scientific literature is a lack of information surrounding comparative (cost-)effectiveness, uptake, and acceptability of interventions. This gap is especially pronounced for smaller non-sedentary workforces or workforces in resource-poor settings that do not reflect the generally large white-collar organizations in high-income countries where the evidence base has typically been developed. As the costs of managing workplace mental health issues exceed the costs of prevention measures (176), action in this regard is essential. Generalized OECD advice recommends that employers establish clear policies and conduct organizational psychosocial risk assessments, upskill line managers to increase awareness and competence of mental health-related matters, and support RTW for those on mental health-related sick leave (177). Implementation services can be employed to aid with taking necessary steps, for example, employers could consider liaising with evidence-based consulting services to design and implement initiatives appropriate to circumstances specific to their organization (178). Where organizational resources are not substantial, for example, in smaller businesses, strengthening interpersonal support through relationship building between managers and staff may be critical to aid employee health and wellbeing (28).
Conclusion
Workplaces have great potential as a facilitator of improving population mental health. While traditionally studies of the links between work and mental health have focused on the role work/workplaces can have in precipitating mental ill health, there is increasing evidence that well-designed and well-managed work can enhance mental health. Ideally, workplaces should be able to promote positive wellbeing, mitigate risk, and to address symptoms of poor mental health at all stages of symptom severity. This goal, however, can only be realized if employers are equipped with the knowledge and access to the resources they need to make positive changes that are appropriate for their specific business and workforce. To this end we have revisited our earlier Framework to Create Mentally Healthy Workplaces (18). The updated Framework provides an overview of different interventions and evidence-based principles to support the wellbeing and mental health of employees. This model clearly defines the types of interventions that are required to create a mentally healthy workplace at the level of systems, operations, job, and individual employee. While the updated Framework presents strategies and initiatives based existing literature or evidence-informed principles of how to protect, respond to, and promote mental health in the workplace, it will need to be applied on a case-by-case basis, by considering what is achievable or relevant for each individual business. A systematic, coordinated, and considered approach to mental health and wellbeing that looks to prevent psychological harm, reduce psychological hazards, support individual recovery, and value employee wellbeing is critical to creating workplaces where employees are healthy and can thrive.
Author contributions
MD: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. SS: Project administration, Conceptualization, Visualization, Writing – original draft, Writing – review & editing. LT: Writing – original draft, Writing – review & editing. NG: Methodology, Supervision, Writing – original draft, Writing – review & editing. AG: Visualization, Writing – original draft, Writing – review & editing. KP: Writing – original draft, Writing – review & editing. VD: Writing – original draft, Writing – review & editing. ES: Investigation, Methodology, Writing – original draft, Writing – review & editing. AL: Supervision, Writing – original draft, Writing – review & editing. SH: Conceptualization, Funding acquisition, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. MD and AG were supported by funding from icare NSW. SH was supported by the National Health and Medical Research Council (NHMRC) investigator grant (grant no. 1178666). SS was supported by a fellowship from NSW State Insurance Regulatory Authority (SIRA). The funding sources had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
At the time of writing MD, SS, AG, SH, and KP were all employed by the Black Dog Institute (BDI). The BDI offers clinical services and fee-for-service training for individuals and workplaces in mental health and wellbeing areas.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ACT, Acceptance and Commitment Therapy; CBT, Cognitive behavior therapy; EAP, Employee assistance program; MH, Mental health; MHFA, Mental Health First Aid; PTSD, Posttraumatic stress disorder; RTW, Return-to-work; WHO, World Health Organisation
References
1. Hassard, J, Teoh, KRH, Visockaite, G, Dewe, P, and Cox, T. The cost of work-related stress to society: a systematic review. J Occup Health Psychol. (2018) 23:1–17. doi: 10.1037/ocp0000069
2. WHO . WHO guidelines on mental health at work. Geneva: World Health Organization (2022) Available at: https://apps.who.int/iris/rest/bitstreams/1469640/retrieve.
3. Hassard, J, Teoh, KRH, Visockaite, G, Dewe, P, and Cox, T. The financial burden of psychosocial workplace aggression: a systematic review of cost-of-illness studies. Work Stress. (2017) 32:6–32. doi: 10.1080/02678373.2017.1380726
4. Madsen, IEH, Nyberg, ST, Magnusson Hanson, LL, Ferrie, JE, Ahola, K, Alfredsson, L, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med. (2017) 47:1342–56. doi: 10.1017/S003329171600355X
5. Niedhammer, I, Bertrais, S, and Witt, K. Psychosocial work exposures and health outcomes: a meta-review of 72 literature reviews with meta-analysis. Scand J Work Environ Health. (2021) 47:489–508. doi: 10.5271/sjweh.3968
6. Virtanen, M, Jokela, M, Madsen, IEH, Magnusson Hanson, LL, Lallukka, T, Nyberg, ST, et al. Long working hours and depressive symptoms: systematic review and meta-analysis of published studies and unpublished individual participant data. Scand J Work Environ Health. (2018) 44:239–50. doi: 10.5271/sjweh.3712
7. Wong, K, Chan, AHS, and Ngan, SC. The effect of long working hours and overtime on occupational health: a Meta-analysis of evidence from 1998 to 2018. Int J Environ Res Public Health. (2019) 16:2102. doi: 10.3390/ijerph16122102
8. Sun, C, Hon, CKH, Way, KA, Jimmieson, NL, and Xia, B. The relationship between psychosocial hazards and mental health in the construction industry: a meta-analysis. Saf Sci. (2022) 145:105485. doi: 10.1016/j.ssci.2021.105485
9. Harvey, SB, Modini, M, Joyce, S, Milligan-Saville, JS, Tan, L, Mykletun, A, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. (2017) 74:301–10. doi: 10.1136/oemed-2016-104015
10. Berger, W, Coutinho, ESF, Figueira, I, Marques-Portella, C, Luz, MP, Neylan, TC, et al. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1001–11. doi: 10.1007/s00127-011-0408-2
11. Brown, JP, Martin, D, Nagaria, Z, Verceles, AC, Jobe, SL, and Wickwire, EM. Mental health consequences of shift work: an updated review. Curr Psychiatry Rep. (2020) 22:7. doi: 10.1007/s11920-020-1131-z
12. Torquati, L, Mielke, GI, Brown, WJ, Burton, NW, and Kolbe-Alexander, TL. Shift work and poor mental health: a meta-analysis of longitudinal studies. Am J Public Health. (2019) 109:e13–20. doi: 10.2105/AJPH.2019.305278
13. Zhao, Y, Richardson, A, Poyser, C, Butterworth, P, Strazdins, L, and Leach, LS. Shift work and mental health: a systematic review and meta-analysis. Int Arch Occup Environ Health. (2019) 92:763–93. doi: 10.1007/s00420-019-01434-3
14. De Witte, H . Job insecurity: review of the international literature on definitions, prevalence, antecedents and consequences. SA J Ind Psychol. (2005) 31:1–6. doi: 10.4102/sajip.v31i4.200
15. Rugulies, R, Aust, B, and Madsen, IEH. Effort–reward imbalance at work and risk of depressive disorders. A systematic review and meta-analysis of prospective cohort studies. Scand J Work Environ Health. (2017) 43:294–306. doi: 10.5271/sjweh.3632
16. Milner, A, Witt, K, LaMontagne, AD, and Niedhammer, I. Psychosocial job stressors and suicidality: a meta-analysis and systematic review. Occup Environ Med. (2017) 75:245–53. doi: 10.1136/oemed-2017-104531
17. Nielsen, MB, and Einarsen, S. Outcomes of exposure to workplace bullying: a meta-analytic review. Work Stress. (2012) 26:309–32. doi: 10.1080/02678373.2012.734709
18. Harvey, SB, Joyce, S, Tan, L, Johnson, A, Nguyen, H, and Modini, M. Developing a mentally healthy workplace: a review of the literature. (2014). Available at: http://www.headsup.org.au/docs/default-source/resources/developing-a-mentally-healthy-workplace_literature-review.pdf?sfvrsn=2.
19. Lesener, T, Gusy, B, and Wolter, C. The job demands-resources model: a meta-analytic review of longitudinal studies. Work Stress. (2018) 33:76–103. doi: 10.1080/02678373.2018.1529065
20. Joyce, S, Modini, M, Christensen, H, Mykletun, A, Bryant, R, Mitchell, PB, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med. (2015) 46:683–97. doi: 10.1017/S0033291715002408
21. LaMontagne, AD, Martin, A, Page, KM, Reavley, NJ, Noblet, AJ, Milner, AJ, et al. Workplace mental health: developing an integrated intervention approach. BMC Psychiatry. (2014) 14:131. doi: 10.1186/1471-244X-14-131
22. Parker, SK, and Jorritsma, K. Good work design for all: multiple pathways to making a difference. Eur J Work Organ Psy. (2020) 30:456–68. doi: 10.1080/1359432X.2020.1860121
23. Parker, SK, Jorritsma, K, and Griffin, MA. Shifting the mental health conversation: present and future applications of the “thrive at work” framework In: Brough P, Gardiner E, and Daniels K, editors. Handbook on management and employment practices. Switzerland: Springer International Publishing (2022). 727–47.
24. Petrie, K, Joyce, S, Tan, L, Henderson, M, Johnson, A, Nguyen, H, et al. A framework to create more mentally healthy workplaces: a viewpoint. Aust N Z J Psychiatry. (2017) 52:15–23. doi: 10.1177/0004867417726174
25. Stratton, E, Johnson, A, and Glozier, N. Psychosocial risks and interventions for mental ill-health in the workplace – a meta-review of the evidence workplace psychosocial risks and interventions. Sydney: Safework (2021).
26. Strudwick, J, Gayed, A, Deady, M, Haffar, S, Mobbs, S, Malik, A, et al. Workplace mental health screening: a systematic review and meta-analysis. Occup Environ Med. (2023) 80:469–84. doi: 10.1136/oemed-2022-108608
27. Technical Committee ISO/TC 283. ISO 45003: 2021 . Occupational health and safety management—psychological health and safety at work—guidelines for managing psychosocial risks. Geneva: ISO (2021).
28. National Mental Health Commission . Blueprint for mentally healthy workplaces. Sydney: National Mental Health Commission (2021).
29. Safe Work Australia . Managing psychosocial hazards at work code of practice. Sydney: Safe Work Australia (2022).
30. International Labour Organization . Psychosocial risks and work-related stress. (2022). Available at: https://www.ilo.org/global/topics/safety-and-health-at-work/areasofwork/workplace-health-promotion-and-well-being/WCMS_108557/lang--en/index.htm.
31. Clarke, SG, and Cooper, CL. The risk management of occupational stress. Health Risk Soc. (2000) 2:173–87. doi: 10.1080/713670158
32. Metzler, YA, von Groeling-Müller, G, and Bellingrath, S. Better safe than sorry: methods for risk assessment of psychosocial hazards. Saf Sci. (2019) 114:122–39. doi: 10.1016/j.ssci.2019.01.003
33. Oakman, J, Weale, V, Kinsman, N, Nguyen, H, and Stuckey, R. Workplace physical and psychosocial hazards: a systematic review of evidence informed hazard identification tools. Appl Ergon. (2022) 100:103614. doi: 10.1016/j.apergo.2021.103614
34. Gillen, PA, Sinclair, M, Kernohan, WG, Begley, CM, and Luyben, AG. Interventions for prevention of bullying in the workplace. Cochrane Database Syst Rev. (2017) 1:CD009778. doi: 10.1002/14651858.CD009778.pub2
35. Petrie, K, Gayed, A, Bryan, BT, Deady, M, Madan, I, Savic, A, et al. The importance of manager support for the mental health and well-being of ambulance personnel. PLoS One. (2018) 13:e0197802-e. doi: 10.1371/journal.pone.0197802
36. Gayed, A, Milligan-Saville, JS, Nicholas, J, Bryan, BT, LaMontagne, AD, Milner, A, et al. Effectiveness of training workplace managers to understand and support the mental health needs of employees: a systematic review and meta-analysis. Occup Environ Med. (2018) 75:462–70. doi: 10.1136/oemed-2017-104789
37. Russo, M, Lucifora, C, Pucciarelli, F, and Piccoli, B. Work hazards and workers’ mental health: an investigation based on the fifth European working conditions survey. Med Lav. (2019) 110:115–29. doi: 10.23749/mdl.v110i2.7640
38. Colenberg, S, Jylhä, T, and Arkesteijn, M. The relationship between interior office space and employee health and well-being—a literature review. Build Res Inform. (2020) 49:352–66. doi: 10.1080/09613218.2019.1710098
39. Kouvonen, A, Mänty, M, Lallukka, T, Lahelma, E, and Rahkonen, O. Changes in psychosocial and physical working conditions and common mental disorders. Eur J Public Health. (2016) 26:458–63. doi: 10.1093/eurpub/ckw019
40. Minutillo, S, Cleary, M, and Visentin, D. Employee well-being in open-plan office spaces. Issues Ment Health Nurs. (2021) 42:103–5. doi: 10.1080/01612840.2020.1865072
41. Theorell, T, Hammarström, A, Aronsson, G, Träskman Bendz, L, Grape, T, Hogstedt, C, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health. (2015) 15:738. doi: 10.1186/s12889-015-1954-4
42. Egan, M, Bambra, C, Thomas, S, Petticrew, M, Whitehead, M, and Thomson, H. The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that aim to increase employee control. J Epidemiol Community Health. (2007) 61:945–54. doi: 10.1136/jech.2006.054965
43. Martin, A, Shann, C, and LaMontagne, AD. Promoting workplace mental wellbeing In: Bültmann U, Siegrist J, editors. Handbook of disability, work and health. Switzerland: Springer International Publishing (2019). 1–19.
44. Shiri, R, Turunen, J, Kausto, J, Leino-Arjas, P, Varje, P, Väänänen, A, et al. The effect of employee-oriented flexible work on mental health: a systematic review. Healthcare. (2022) 10:883. doi: 10.3390/healthcare10050883
45. Dollard, MF, and Gordon, JA. Evaluation of a participatory risk management work stress intervention. Int J Stress Manag. (2014) 21:27–42. doi: 10.1037/a0035795
46. Duhoux, A, Menear, M, Charron, M, Lavoie-Tremblay, M, and Alderson, M. Interventions to promote or improve the mental health of primary care nurses: a systematic review. J Nurs Manag. (2017) 25:597–607. doi: 10.1111/jonm.12511
47. Rickard, G, Lenthall, S, Dollard, M, Opie, T, Knight, S, Dunn, S, et al. Organisational intervention to reduce occupational stress and turnover in hospital nurses in the Northern Territory, Australia. Collegian. (2012) 19:211–21. doi: 10.1016/j.colegn.2012.07.001
48. Parker, SK, and Knight, C. The SMART model of work design: a higher order structure to help see the wood from the trees. Hum Resour Manag. (2023) 63:265–91. doi: 10.1002/hrm.22200
49. Parker, SK, Morgeson, FP, and Johns, G. One hundred years of work design research: looking back and looking forward. J Appl Psychol. (2017) 102:403–20. doi: 10.1037/apl0000106
50. Tan, L, Wang, M-J, Modini, M, Joyce, S, Mykletun, A, Christensen, H, et al. Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med. (2014) 12:74. doi: 10.1186/1741-7015-12-74
51. Wan Mohd Yunus, WMA, Musiat, P, and Brown, JSL. Systematic review of universal and targeted workplace interventions for depression. Occup Environ Med. (2017) 75:66–75. doi: 10.1136/oemed-2017-104532
52. Carolan, S, Harris, PR, and Cavanagh, K. Improving employee well-being and effectiveness: systematic review and meta-analysis of web-based psychological interventions delivered in the workplace. J Med Internet Res. (2017) 19:e271. doi: 10.2196/jmir.7583
53. Phillips, EA, Gordeev, VS, and Schreyögg, J. Effectiveness of occupational e-mental health interventions: a systematic review and meta-analysis of randomized controlled trials. Scand J Work Environ Health. (2019) 45:560–76. doi: 10.5271/sjweh.3839
54. Stratton, E, Lampit, A, Choi, I, Calvo, RA, Harvey, SB, and Glozier, N. Effectiveness of eHealth interventions for reducing mental health conditions in employees: a systematic review and meta-analysis. PLoS One. (2017) 12:e0189904. doi: 10.1371/journal.pone.0189904
55. Miguel, C, Amarnath, A, Akhtar, A, Malik, A, Baranyi, G, Barbui, C, et al. Universal, selective and indicated interventions for supporting mental health at the workplace: an umbrella review of meta-analyses. Occup Environ Med. (2023) 80:225–36. doi: 10.1136/oemed-2022-108698
56. Luken, M, and Sammons, A. Systematic review of mindfulness practice for reducing job burnout. Am J Occup Ther. (2016) 70:7002250020p1–7002250020p10. doi: 10.5014/ajot.2016.016956
57. Slemp, GR, Jach, HK, Chia, A, Loton, DJ, and Kern, ML. Contemplative interventions and employee distress: a meta-analysis. Stress Health. (2019) 35:227–55. doi: 10.1002/smi.2857
58. Ivandic, I, Freeman, A, Birner, U, Nowak, D, and Sabariego, CÂ. A systematic review of brief mental health and well-being interventions in organizational settings. Scand J Work Environ Health. (2017) 43:99–108. doi: 10.5271/sjweh.3616
59. Chu, AHY, Koh, D, Moy, FM, and Muller-Riemenschneider, F. Do workplace physical activity interventions improve mental health outcomes? Occup Med. (2014) 64:235–45. doi: 10.1093/occmed/kqu045
60. Bischoff, LL, Otto, A-K, Hold, C, and Wollesen, B. The effect of physical activity interventions on occupational stress for health personnel: a systematic review. Int J Nurs Stud. (2019) 97:94–104. doi: 10.1016/j.ijnurstu.2019.06.002
61. Clough, BA, March, S, Chan, RJ, Casey, LM, Phillips, R, and Ireland, MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev. (2017) 6:144. doi: 10.1186/s13643-017-0526-3
62. Kunzler, AM, Helmreich, I, Chmitorz, A, König, J, Binder, H, Wessa, M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst Rev. (2020) 7:CD012527. doi: 10.1002/14651858.CD012527.pub2
63. Petrie, K, Crawford, J, Baker, STE, Dean, K, Robinson, J, Veness, BG, et al. Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta-analysis. Lancet Psychiatry. (2019) 6:225–34. doi: 10.1016/S2215-0366(18)30509-1
64. Brown, HE, Gilson, ND, Burton, NW, and Brown, WJ. Does physical activity impact on presenteeism and other indicators of workplace well-being? Sports Med. (2011) 41:249–62. doi: 10.2165/11539180-000000000-00000
65. Bisson, JI, Wright, LA, Jones, KA, Lewis, C, Phelps, AJ, Sijbrandij, M, et al. Preventing the onset of post-traumatic stress disorder. Clin Psychol Rev. (2021) 86:102004. doi: 10.1016/j.cpr.2021.102004
66. Tan, L, Petrie, K, Deady, M, Bryant, RA, and Harvey, SB. Systematic review of first responder post-deployment or post-incident psychosocial interventions. Occup Med. (2022) 72:160–9. doi: 10.1093/occmed/kqab182
67. Tan, L, Strudwick, J, Deady, M, Bryant, R, and Harvey, SB. Mind-body exercise interventions for prevention of post-traumatic stress disorder in trauma-exposed populations: a systematic review and meta-analysis. BMJ Open. (2023) 13:e064758. doi: 10.1136/bmjopen-2022-064758
68. Hourani, L, Tueller, S, Kizakevich, P, Lewis, G, Strange, L, Weimer, B, et al. Toward preventing post-traumatic stress disorder: development and testing of a pilot predeployment stress inoculation training program. Mil Med. (2016) 181:1151–60. doi: 10.7205/MILMED-D-15-00192
69. Wald, I, Bitton, S, Levi, O, Zusmanovich, S, Fruchter, E, Ginat, K, et al. Acute delivery of attention bias modification training (ABMT) moderates the association between combat exposure and posttraumatic symptoms: a feasibility study. Biol Psychol. (2017) 122:93–7. doi: 10.1016/j.biopsycho.2016.01.005
70. Wald, I, Fruchter, E, Ginat, K, Stolin, E, Dagan, D, Bliese, PD, et al. Selective prevention of combat-related post-traumatic stress disorder using attention bias modification training: a randomized controlled trial. Psychol Med. (2016) 46:2627–36. doi: 10.1017/S0033291716000945
71. National Institute for Health and Care Excellence . Post-traumatic stress disorder: evidence reviews for psychological, psychosocial and other non-pharmacological interventions for the prevention of PTSD in adults. London, UK: National Institute for Health and Care Excellence (2018).
72. Phoenix Australia . Australian guidelines for the prevention and treatment of acute stress disorder, posttraumatic stress disorder and complex PTSD. Melbourne: Phoenix Australia (2023) Available at: https://www.phoenixaustralia.org/australian-guidelines-for-ptsd/.
73. Hermosilla, S, Forthal, S, Sadowska, K, Magill, EB, Watson, P, and Pike, KM. We need to build the evidence: a systematic review of psychological first aid on mental health and well-being. J Trauma Stress. (2022) 36:5–16. doi: 10.1002/jts.22888
74. Gatt, JM, Burton, KLO, Schofield, PR, Bryant, RA, and Williams, LM. The heritability of mental health and wellbeing defined using COMPAS-W, a new composite measure of wellbeing. Psychiatry Res. (2014) 219:204–13. doi: 10.1016/j.psychres.2014.04.033
75. Slade, M . Mental illness and well-being: the central importance of positive psychology and recovery approaches. BMC Health Serv Res. (2010) 10:6. doi: 10.1186/1472-6963-10-26
76. Alagaraja, M . Wellbeing in the workplace: a new conceptual model and implications for practice In: Dhiman SK, editor. The Palgrave handbook of workplace well-being. Palgrave Macmillan, Cham (2020). 1–22.
77. Ryff, CD, and Keyes, CLM. The structure of psychological well-being revisited. J Pers Soc Psychol. (1995) 69:719–27. doi: 10.1037//0022-3514.69.4.719
78. Seligman, MEP . Flourish: a new understanding of happiness and well-being and how to achieve them. London: Free Press (2011).
79. Thompson, S, and Marks, N. Measuring well-being in policy: issues and applications. New Economics Foundation (2008). Available at: https://neweconomics.org/uploads/files/575659b4f333001669_ohm6iiogp.pdf.
80. Kleine, AK, Rudolph, CW, and Zacher, H. Thriving at work: a meta-analysis. J Organ Behav. (2019) 40:973–99. doi: 10.1002/job.2375
81. Diener, E . Guidelines for national indicators of subjective well-being and ill-being. J Happiness Stud. (2006) 7:397–404. doi: 10.1007/s10902-006-9000-y
82. Anger, WK, Elliot, DL, Bodner, T, Olson, R, Rohlman, DS, Truxillo, DM, et al. Effectiveness of total worker health interventions. J Occup Health Psychol. (2015) 20:226–47. doi: 10.1037/a0038340
83. LaMontagne, AD, Martin, A, Page, KM, Reavley, NJ, Noblet, AJ, Milner, AJ, et al. Developing an integrated approach to workplace mental health: total worker health. Am Psychol Assoc. (2019):211–27. doi: 10.1037/0000149-013
84. Daniels, K, Gedikli, C, Watson, D, Semkina, A, and Vaughn, O. Job design, employment practices and well-being: a systematic review of intervention studies. Ergonomics. (2017) 60:1177–96. doi: 10.1080/00140139.2017.1303085
85. Nielsen, K, Taris, T, and Cox, T. The future of organizational interventions: addressing the challenges of today’s organizations. Work Stress. (2010) 24:219–33. doi: 10.1080/02678373.2010.519176
86. Edmondson, A . The fearless organization: creating psychological safety in the workplace for learning, innovation, and growth. New York, NY: John Wiley and Sons (2019).
87. Duan, J, Wang, X, Brinsfield, C, and Liu, S. How enhancing employee well-being can encourage voice behavior: a desire fulfillment perspective. Hum Perform. (2020) 33:425–46. doi: 10.1080/08959285.2020.1811708
88. Hasan, F, and Kashif, M. Psychological safety, meaningfulness and empowerment as predictors of employee well-being: a mediating role of promotive voice. Asia Pacif J Bus Admin. (2020) 13:40–59. doi: 10.1108/APJBA-11-2019-0236
90. Daniels, K, Watson, D, and Gedikli, C. Well-being and the social environment of work: a systematic review of intervention studies. Int J Environ Res Public Health. (2017) 14:918. doi: 10.3390/ijerph14080918
91. Khazanchi, S, Sprinkle, TA, Masterson, SS, and Tong, N. A spatial model of work relationships: the relationship-building and relationship-straining effects of workspace design. Acad Manag Rev. (2018) 43:590–609. doi: 10.5465/amr.2016.0240
92. Hardman Smith, L, Hviid, K, Frydendall, KB, and Flyvholm, M-A. Improving the psychosocial work environment at multi-ethnic workplaces: a multi-component intervention strategy in the cleaning industry. Int J Environ Res Public Health. (2013) 10:4996–5010. doi: 10.3390/ijerph10104996
93. Brunetto, Y, Xerri, M, Shriberg, A, Farr-Wharton, R, Shacklock, K, Newman, S, et al. The impact of workplace relationships on engagement, well-being, commitment and turnover for nurses in Australia and the USA. J Adv Nurs. (2013) 69:2786–99. doi: 10.1111/jan.12165
94. Dutton, JE . Energize your workplace: how to create and sustain high-quality connections at work. San Francisco: Jossey-Bass (2003).
95. Shakespeare-Finch, J, and Daley, E. Workplace belongingness, distress, and resilience in emergency service workers. Psychol Trauma Theory Res Pract Policy. (2017) 9:32–5. doi: 10.1037/tra0000108
96. Jessiman-Perreault, G, Smith, PM, and Gignac, MAM. Why are workplace social support programs not improving the mental health of Canadian correctional officers? An examination of the theoretical concepts underpinning support. Int J Environ Res Public Health. (2021) 18:2665. doi: 10.3390/ijerph18052665
97. Bergefurt, L, Appel-Meulenbroek, R, Maris, C, Arentze, T, Weijs-Perrée, M, and de Kort, Y. The influence of distractions of the home-work environment on mental health during the COVID-19 pandemic. Ergonomics. (2022) 66:16–33. doi: 10.1080/00140139.2022.2053590
98. Schweitzer, M, Gilpin, L, and Frampton, S. Healing spaces: elements of environmental design that make an impact on health. J Altern Complement Med. (2004) 10:S71–83. doi: 10.1089/1075553042245953
99. Gritzka, S, MacIntyre, TE, Dörfel, D, Baker-Blanc, JL, and Calogiuri, G. The effects of workplace nature-based interventions on the mental health and well-being of employees: a systematic review. Front Psych. (2020) 11:323. doi: 10.3389/fpsyt.2020.00323
100. Genjo, K, Matsumoto, H, Ogata, N, and Nakano, T. Feasibility study on mental health-care effects of plant installations in office spaces. Jpn Archit Rev. (2019) 2:376–88. doi: 10.1002/2475-8876.12098
101. Eatough, EM, and Spector, PE. The role of workplace control in positive health and wellbeing In: C. L. Cooper (Ed.), Wellbeing : Wiley (2014). 1–19.
102. Thompson, CA, and Prottas, DJ. Relationships among organizational family support, job autonomy, perceived control, and employee well-being. J Occup Health Psychol. (2006) 11:100–18. doi: 10.1037/1076-8998.10.4.100
103. Montano, D, Hoven, H, and Siegrist, J. Effects of organisational-level interventions at work on employees' health: a systematic review. BMC Public Health. (2014) 14:135. doi: 10.1186/1471-2458-14-135
104. Haby, M, Chapman, E, Clark, R, and Galvão, L. Interventions that facilitate sustainable jobs and have a positive impact on workers’ health: an overview of systematic reviews. Pan Am J Public Health. (2016) 40:332–40.
105. Yu, S, Levesque-Bristol, C, and Maeda, Y. General need for autonomy and subjective well-being: a meta-analysis of studies in the US and East Asia. J Happiness Stud. (2017) 19:1863–82. doi: 10.1007/s10902-017-9898-2
106. Abendroth, A-K, and den Dulk, L. Support for the work-life balance in Europe: the impact of state, workplace and family support on work-life balance satisfaction. Work Employ Soc. (2011) 25:234–56. doi: 10.1177/0950017011398892
107. Joyce, K, Pabayo, R, Critchley, JA, and Bambra, C. Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev. (2010) 2010:CD008009. doi: 10.1002/14651858.CD008009.pub2
108. Nijp, HH, Beckers, DGJ, Geurts, SAE, Tucker, P, and Kompier, MAJ. Systematic review on the association between employee worktime control and work–non-work balance, health and well-being, and job-related outcomes. Scand J Work Environ Health. (2012) 38:299–313. doi: 10.5271/sjweh.3307
109. Watson, D, Tregaskis, O, Gedikli, C, Vaughn, O, and Semkina, A. Well-being through learning: a systematic review of learning interventions in the workplace and their impact on well-being. Eur J Work Organ Psy. (2018) 27:247–68. doi: 10.1080/1359432X.2018.1435529
110. Parent-Lamarche, A, Marchand, A, and Saade, S. How do work organization conditions affect job performance? The mediating role of workers’ well-being. J Work Behav Health. (2021) 36:48–76. doi: 10.1080/15555240.2021.1872382
111. Langove, N, and Isha, A. Impact of rewards and recognition on Malaysian IT executives well-being and turnover intention: a conceptual framework. Glob Bus Manag Res. (2017) 9:153–61.
112. Grant, AM, and Parker, SK. Redesigning work design theories: the rise of relational and proactive perspectives. Acad Manag Ann. (2009) 3:317–75. doi: 10.5465/19416520903047327
113. Tims, M, and Bakker, AB. Job crafting: towards a new model of individual job redesign. SA J Ind Psychol. (2010) 36:1–9. doi: 10.4102/sajip.v36i2.841
114. Tims, M, Bakker, AB, and Derks, D. The impact of job crafting on job demands, job resources, and well-being. J Occup Health Psychol. (2013) 18:230–40. doi: 10.1037/a0032141
115. Tims, M, Bakker, AB, and Derks, D. Job crafting and job performance: a longitudinal study. Eur J Work Organ Psy. (2014) 24:914–28. doi: 10.1080/1359432X.2014.969245
116. Tims, M, Bakker, AB, and Derks, D. Examining job crafting from an interpersonal perspective: is employee job crafting related to the well-being of colleagues? Appl Psychol. (2015) 64:727–53. doi: 10.1111/apps.12043
117. Grant, AM, Fried, Y, Parker, SK, and Frese, M. Putting job design in context: introduction to the special issue. J Organ Behav. (2010) 31:145–57. doi: 10.1002/job.679
118. Hornung, S, Rousseau, DM, Glaser, J, Angerer, P, and Weigl, M. Beyond top-down and bottom-up work redesign: customizing job content through idiosyncratic deals. J Organ Behav. (2010) 31:187–215. doi: 10.1002/job.625
119. Lichtenthaler, PW, and Fischbach, A. A meta-analysis on promotion- and prevention-focused job crafting. Eur J Work Organ Psy. (2018) 28:30–50. doi: 10.1080/1359432X.2018.1527767
120. Rudolph, CW, Katz, IM, Lavigne, KN, and Zacher, H. Job crafting: a meta-analysis of relationships with individual differences, job characteristics, and work outcomes. J Vocat Behav. (2017) 102:112–38. doi: 10.1016/j.jvb.2017.05.008
121. Vogt, K, Hakanen, JJ, Brauchli, R, Jenny, GJ, and Bauer, GF. The consequences of job crafting: a three-wave study. Eur J Work Organ Psy. (2015) 25:353–62. doi: 10.1080/1359432X.2015.1072170
122. Wang, H, Li, P, and Chen, S. The impact of social factors on job crafting: a meta-analysis and review. Int J Environ Res Public Health. (2020) 17:8016. doi: 10.3390/ijerph17218016
123. Wang, H, Demerouti, E, and Bakker, AB. A review of job crafting research: the role of leader behaviors in cultivating successful job crafters In: SKBU Parker , editor. Proactivity at work: making things happen in organizations. London: Routledge (2016). 77–104.
124. Wagner, SL, White, MI, Schultz, IZ, Williams-Whitt, K, Koehn, C, Dionne, CE, et al. Social support and supervisory quality interventions in the workplace: a stakeholder-centered best-evidence synthesis of systematic reviews on work outcomes. Int J Occup Environ Med. (2015) 6:189–204. doi: 10.15171/ijoem.2015.608
125. Page, KM, Milner, AJ, Martin, A, Turrell, G, Giles-Corti, B, and LaMontagne, AD. Workplace stress. J Occup Environ Med. (2014) 56:814–9. doi: 10.1097/JOM.0000000000000230
126. Sakuraya, A, Imamura, K, Watanabe, K, Asai, Y, Ando, E, Eguchi, H, et al. What kind of intervention is effective for improving subjective well-being among workers? A systematic review and meta-analysis of randomized controlled trials. Front Psychol. (2020) 11:528656. doi: 10.3389/fpsyg.2020.528656
127. Bartlett, L, Martin, A, Neil, AL, Memish, K, Otahal, P, Kilpatrick, M, et al. A systematic review and meta-analysis of workplace mindfulness training randomized controlled trials. J Occup Health Psychol. (2019) 24:108–26. doi: 10.1037/ocp0000146
128. Johnson, KR, Park, S, and Chaudhuri, S. Mindfulness training in the workplace: exploring its scope and outcomes. Eur J Train Dev. (2020) 44:341–54. doi: 10.1108/EJTD-09-2019-0156
129. Lomas, T, Medina, JC, Ivtzan, I, Rupprecht, S, and Eiroa-Orosa, FJ. Mindfulness-based interventions in the workplace: an inclusive systematic review and meta-analysis of their impact upon wellbeing. J Posit Psychol. (2018) 14:625–40. doi: 10.1080/17439760.2018.1519588
130. Lomas, T, Medina, JC, Ivtzan, I, Rupprecht, S, Hart, R, and Eiroa-Orosa, FJ. The impact of mindfulness on well-being and performance in the workplace: an inclusive systematic review of the empirical literature. Eur J Work Organ Psy. (2017) 26:492–513. doi: 10.1080/1359432X.2017.1308924
131. Jamieson, SD, and Tuckey, MR. Mindfulness interventions in the workplace: a critique of the current state of the literature. J Occup Health Psychol. (2017) 22:180–93. doi: 10.1037/ocp0000048
132. Donaldson, SI, Lee, JY, and Donaldson, SI. Evaluating positive psychology interventions at work: a systematic review and meta-analysis. Int J Appl Posit Psychol. (2019) 4:113–34. doi: 10.1007/s41042-019-00021-8
133. Townsley, AP, Li-Wang, J, and Katta, R. Healthcare workers' well-being: a systematic review of positive psychology interventions. Cureus. (2023) 15:e34102. doi: 10.7759/cureus.34102
134. Meyers, MC, van Woerkom, M, and Bakker, AB. The added value of the positive: a literature review of positive psychology interventions in organizations. Eur J Work Organ Psy. (2013) 22:618–32. doi: 10.1080/1359432X.2012.694689
135. Joyce, S, Shand, F, Tighe, J, Laurent, SJ, Bryant, RA, and Harvey, SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. (2018) 8:e017858. doi: 10.1136/bmjopen-2017-017858
136. Hartmann, S, Weiss, M, Newman, A, and Hoegl, M. Resilience in the workplace: a multilevel review and synthesis. Appl Psychol. (2019) 69:913–59. doi: 10.1111/apps.12191
137. Robertson, IT, Cooper, CL, Sarkar, M, and Curran, T. Resilience training in the workplace from 2003 to 2014: a systematic review. J Occup Organ Psychol. (2015) 88:533–62. doi: 10.1111/joop.12120
138. Vanhove, AJ, Herian, MN, Perez, ALU, Harms, PD, and Lester, PB. Can resilience be developed at work? A meta-analytic review of resilience-building programme effectiveness. J Occup Organ Psychol. (2015) 89:278–307. doi: 10.1111/joop.12123
139. Theeboom, T, Beersma, B, and van Vianen, AEM. Does coaching work? A meta-analysis on the effects of coaching on individual level outcomes in an organizational context. J Posit Psychol. (2014) 9:1–18. doi: 10.1080/17439760.2013.837499
140. Pirkola, H, Rantakokko, P, and Suhonen, M. Workplace spirituality in health care: an integrated review of the literature. J Nurs Manag. (2016) 24:859–68. doi: 10.1111/jonm.12398
141. de Diego-Cordero, R, Zurrón Pérez, MP, Vargas-Martínez, AM, Lucchetti, G, and Vega-Escaño, J. The effectiveness of spiritual interventions in the workplace for work-related health outcomes: a systematic review and meta-analysis. J Nurs Manag. (2021) 29:1703–12. doi: 10.1111/jonm.13315
142. Grimani, A, Aboagye, E, and Kwak, L. The effectiveness of workplace nutrition and physical activity interventions in improving productivity, work performance and workability: a systematic review. BMC Public Health. (2019) 19:1676. doi: 10.1186/s12889-019-8033-1
143. Pereira, MJ, Coombes, BK, Comans, TA, and Johnston, V. The impact of onsite workplace health-enhancing physical activity interventions on worker productivity: a systematic review. Occup Environ Med. (2015) 72:401–12. doi: 10.1136/oemed-2014-102678
144. Rongen, A, Robroek, SJW, van Lenthe, FJ, and Burdorf, A. Workplace health promotion. Am J Prev Med. (2013) 44:406–15. doi: 10.1016/j.amepre.2012.12.007
145. Abdin, S, Welch, RK, Byron-Daniel, J, and Meyrick, J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: a systematic review. Public Health. (2018) 160:70–6. doi: 10.1016/j.puhe.2018.03.029
146. Phillips, CS, and Becker, H. Systematic review: expressive arts interventions to address psychosocial stress in healthcare workers. J Adv Nurs. (2019) 75:2285–98. doi: 10.1111/jan.14043
147. Memish, K, Martin, A, Bartlett, L, Dawkins, S, and Sanderson, K. Workplace mental health: an international review of guidelines. Prev Med. (2017) 101:213–22. doi: 10.1016/j.ypmed.2017.03.017
148. Evans-Lacko, S, Koeser, L, Knapp, M, Longhitano, C, Zohar, J, and Kuhn, K. Evaluating the economic impact of screening and treatment for depression in the workplace. Eur Neuropsychopharmacol. (2016) 26:1004–13. doi: 10.1016/j.euroneuro.2016.03.005
149. Marshall, RE, Milligan-Saville, JS, Steel, Z, Bryant, RA, Mitchell, PB, and Harvey, SB. A prospective study of pre-employment psychological testing amongst police recruits. Occup Med. (2020) 70:162–8. doi: 10.1093/occmed/kqaa008
150. Rona, RJ, Burdett, H, Khondoker, M, Chesnokov, M, Green, K, Pernet, D, et al. Post-deployment screening for mental disorders and tailored advice about help-seeking in the UK military: a cluster randomised controlled trial. Lancet. (2017) 389:1410–23. doi: 10.1016/S0140-6736(16)32398-4
151. Greenberg, PE, Fournier, A-A, Sisitsky, T, Simes, M, Berman, R, Koenigsberg, SH, et al. The economic burden of adults with major depressive disorder in the United States (2010 and 2018). PharmacoEconomics. (2021) 39:653–65. doi: 10.1007/s40273-021-01019-4
152. Woods, M, and Matthewson, ML. Managing and mitigating suffering in the return-to-work process. Front Psychol. (2021) 12:805855. doi: 10.3389/fpsyg.2021.805855
153. Yarker, J, Sinclair, A, Donaldson-Feilder, E, and Lewis, R. Work adjustments for mental health: a review of the evidence and guidance. (2019). Available at: https://www.acas.org.uk/work-adjustments-for-mental-health-a-review-of-the-evidence-and-guidance-html#4.-summary-and-recommendations.
154. Gray, S, Osborne, R, Di Donato, M, and Collie, A. Recovery at work support tools: rapid review. Melbourne: SIRA (2019).
155. Smith, P, LaMontagne, AD, Lilley, R, Hogg-Johnson, S, and Sim, M. Are there differences in the return to work process for work-related psychological and musculoskeletal injuries? A longitudinal path analysis. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:1041–51. doi: 10.1007/s00127-020-01839-3
156. Anderson, M, Werner-Seidler, A, King, C, Gayed, A, Harvey, SB, and O’Dea, B. Mental health training programs for secondary school teachers: a systematic review. Sch Ment Heal. (2019) 11:489–508. doi: 10.1007/s12310-018-9291-2
157. Tóth, MD, Ihionvien, S, Leduc, C, Aust, B, Amann, BL, Cresswell-Smith, J, et al. Evidence for the effectiveness of interventions to reduce mental health related stigma in the workplace: a systematic review. BMJ Open. (2023) 13:e067126. doi: 10.1136/bmjopen-2022-067126
158. Hanisch, SE, Twomey, CD, Szeto, ACH, Birner, UW, Nowak, D, and Sabariego, C. The effectiveness of interventions targeting the stigma of mental illness at the workplace: a systematic review. BMC Psychiatry. (2016) 16:1. doi: 10.1186/s12888-015-0706-4
159. Morgan, AJ, Ross, A, and Reavley, NJ. Systematic review and meta-analysis of mental health first aid training: effects on knowledge, stigma, and helping behaviour. PLoS One. (2018) 13:e0197102. doi: 10.1371/journal.pone.0197102
160. Agarwal, B, Brooks, SK, and Greenberg, N. The role of peer support in managing occupational stress: a qualitative study of the sustaining resilience at work intervention. Workplace Health Saf. (2019) 68:57–64. doi: 10.1177/2165079919873934
161. Watson, L, and Andrews, L. The effect of a trauma risk management (TRiM) program on stigma and barriers to help-seeking in the police. Int J Stress Manag. (2018) 25:348–56. doi: 10.1037/str0000071
162. Whybrow, D, Jones, N, and Greenberg, N. Promoting organizational well-being: a comprehensive review of trauma risk management. Occup Med. (2015) 65:331–6. doi: 10.1093/occmed/kqv024
163. Reavley, NJ, Ross, A, Killackey, EJ, and Jorm, AF. Development of guidelines to assist organisations to support employees returning to work after an episode of anxiety, depression or a related disorder: a Delphi consensus study with Australian professionals and consumers. BMC Psychiatry. (2012) 12:135. doi: 10.1186/1471-244X-12-135
164. Disability Discrimination Act 1992 (Cth) (2018). Available at https://www.legislation.gov.au/C2004A04426/latest/text
165. Clayton, S, Barr, B, Nylen, L, Burström, B, Thielen, K, Diderichsen, F, et al. Effectiveness of return-to-work interventions for disabled people: a systematic review of government initiatives focused on changing the behaviour of employers. Eur J Pub Health. (2011) 22:434–9. doi: 10.1093/eurpub/ckr101
166. Nigatu, YT, Huang, J, Rao, S, Gillis, K, Merali, Z, and Wang, J. Indicated prevention interventions in the workplace for depressive symptoms: a systematic review and meta-analysis. Am J Prev Med. (2019) 56:e23–33. doi: 10.1016/j.amepre.2018.08.027
167. Csiernik, R . The glass is filling: an examination of employee assistance program evaluations in the first decade of the new millennium. J Work Behav Health. (2011) 26:334–55. doi: 10.1080/15555240.2011.618438
168. McLeod, J . The effectiveness of workplace counselling: a systematic review. Couns Psychother Res. (2010) 10:238–48. doi: 10.1080/14733145.2010.485688
169. Joseph, B, Walker, A, and Fuller-Tyszkiewicz, M. Evaluating the effectiveness of employee assistance programmes: a systematic review. Eur J Work Organ Psy. (2017) 27:1–15. doi: 10.1080/1359432X.2017.1374245
170. Chen, YC, Chu, HC, and Wang, PT. Employee assistance programs: a meta-analysis. J Employ Couns. (2021) 58:144–66. doi: 10.1002/joec.12170
171. Bothwell, LE, Greene, JA, Podolsky, SH, and Jones, DS. Assessing the gold standard—lessons from the history of RCTs. N Engl J Med. (2016) 374:2175–81. doi: 10.1056/NEJMms1604593
172. de Vocht, F, Katikireddi, SV, McQuire, C, Tilling, K, Hickman, M, and Craig, P. Conceptualising natural and quasi experiments in public health. BMC Med Res Methodol. (2021) 21:32. doi: 10.1186/s12874-021-01224-x
173. Munafò, MR, and Davey, SG. Robust research needs many lines of evidence. Nature. (2018) 553:399–401. doi: 10.1038/d41586-018-01023-3
174. Deady, M, Arena, A, Sanatkar, S, Gayed, A, Manohar, N, Petrie, K, et al. Psychological workplace injury and incapacity: a call for action. J Ind Relat. [ePub ahead of print] (2024). doi: 10.1177/00221856241258561
175. Hudson, HL, Schill, AL, and Richards, R. An exploratory, qualitative study of how organizations implement the hierarchy of controls applied to Total worker health(®). Int J Environ Res Public Health. (2021) 18:10032. doi: 10.3390/ijerph181910032
176. Australian Human Rights Commission . Workers with mental illness: a practical guide for managers. Canberra: Australian Human Rights Commission (2010) Available at: https://humanrights.gov.au/sites/default/files/document/publication/workers_mental_illness_guide_0.pdf.
177. OECD . Fitter Minds, Fitter Jobs: From Awareness to Change in Integrated Mental Health, Skills and Work Policies, Mental Health and Work, OECD Publishing, Paris (2021).
Keywords: work stress, occupational mental health, return to work, psychological hazards, employee wellbeing, intervention, mental health, workplace
Citation: Deady M, Sanatkar S, Tan L, Glozier N, Gayed A, Petrie K, Dalgaard VL, Stratton E, LaMontagne AD and Harvey SB (2024) A mentally healthy framework to guide employers and policy makers. Front. Public Health. 12:1430540. doi: 10.3389/fpubh.2024.1430540
Edited by:
Adam Hege, Appalachian State University, United StatesReviewed by:
Mansoor Malik, Johns Hopkins Medicine, United StatesDavid Paige Gilkey, Montana Technological University, United States
Copyright © 2024 Deady, Sanatkar, Tan, Glozier, Gayed, Petrie, Dalgaard, Stratton, LaMontagne and Harvey. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark Deady, bS5kZWFkeUB1bnN3LmVkdS5hdQ==
†These authors share first authorship
 Mark Deady
Mark Deady Samineh Sanatkar1†
Samineh Sanatkar1† Aimee Gayed
Aimee Gayed Vita Ligaya Dalgaard
Vita Ligaya Dalgaard Elizabeth Stratton
Elizabeth Stratton