- 1School of Health Economics and Management, Nanjing University of Chinese Medicine, Nanjing, China
- 2Jiangsu Research Center for Major Health Risk Management and TCM Control Policy, Nanjing University of Chinese Medicine, Nanjing, China
Objective: This study aims to elucidate the heterogeneous cognitive trajectories among older adults in China through a comprehensive, nationally representative longitudinal study. Furthermore, it seeks to investigate the impact of multidimensional social isolation on heterogeneous cognitive trajectories among older adults in China.
Methods: Utilizing data from three successive waves of the Chinese Longitudinal Aging Social Survey (CLASS) spanning 2016 to 2020, this investigation quantified baseline social isolation across three dimensions—family isolation, friend isolation, and subjective isolation—alongside cognitive function scores of older adults, measured across all three waves. Through latent class growth models, heterogeneous cognitive trajectories were delineated. The influence of family isolation, friend isolation, and subjective isolation on these cognitive trajectories was examined employing multinomial logistic regression analysis.
Results: The study included 6,378 participants aged 60 and above, revealing three primary cognitive trajectories: High baseline stable group (68.8%), High baseline but declining group (21.7%), and Low baseline deteriorating group (9.5%). Adjusting for variables such as personal physical characteristics, social networks, living and working conditions, and the surrounding policy environment, the findings indicated that family isolation did not significantly affect cognitive function’s high-level decline or low-level deterioration. Conversely, friend isolation markedly increased the risk of high-level cognitive decline (OR = 1.289) and low-level cognitive deterioration (OR = 1.592). Similarly, subjective isolation significantly heightened the risk for both high-level decline (OR = 1.254) and low-level deterioration (OR = 1.29) in cognitive function.
Conclusion: Mitigating friend and subjective isolation among older adults appears to be a more effective strategy in preventing or delaying cognitive decline, potentially reducing the strain on healthcare and social welfare systems.
1 Introduction
Cognitive function refers to the brain’s ability to retrieve, process, transform, and store information (1). A decline in cognitive function that exceeds what is typically observed as part of the normal aging process may result in cognitive impairments and ultimately lead to dementia (2). Severe cognitive impairment can significantly diminish the quality of life for older individuals (3, 4). These impairments are associated with an increased risk of long-term hospitalization (5) and elevated mortality rates among older adults (6). Currently, the global population of older adults with dementia is approximately 50 million, a figure projected to rise to 152 million by 2050 due to demographic aging (7). Notably, China accounts for about 25% of the global dementia population, posing a significant challenge for policymakers, healthcare professionals, and families (8, 9). The recent implementation of social distancing measures during the COVID-19 pandemic has intensified concerns regarding social isolation and its potential health consequences (10, 11). Despite increased interest, the relationship between social isolation and cognitive health in older adults remains unclear, with current literature presenting conflicting findings (12, 13). This underscores the necessity for further investigation into this complex relationship.
Social isolation can be categorized into objective and subjective dimensions. Objective isolation is measurable by the diminished size of social networks and reduced frequency of social interactions (14). In China, older adults significantly value personal and familial connections, necessitating the subdivision of objective isolation into two distinct categories: family isolation and friend isolation (15). Subjective isolation, on the other hand, pertains to an individual’s perception of the discrepancy between the desired and actual quantity and quality of social interactions (16). Examination of the interplay between the two facets of social isolation has highlighted a synergistic effect on health outcomes, affecting various health metrics differently (17, 18). Accordingly, this study aims to examine both the objective and subjective aspects of social isolation, with a specific focus on distinguishing between family and friend isolation. This approach endeavors to offer a more holistic understanding and deeper insight into the dynamics between social isolation and cognitive function among older adults.
Changes in cognitive function represent a long-term and dynamic process, which necessitates detailed examination through longitudinal studies. However, majority of existing longitudinal research on this topic is conducted in Western countries, often neglecting the intricate interplay between social structures and individual behaviors characteristic of Eastern collectivist cultures. Compared to Western contexts, there is a notable dearth of longitudinal studies in Eastern settings exploring the relationship between social isolation and cognitive function among older adults, with much of the research limited to cross-sectional studies at a single time point. Furthermore, from a life course perspective, the development of cognitive function is not only dynamic and heterogeneous but is also profoundly influenced by social interactions and relationships throughout an individual’s life. This perspective enables an exploration of how isolation from family and friends impacts cognitive trajectories among older adults (19). Nevertheless, most longitudinal studies rely on traditional regression or growth curve modeling techniques, which are limited to identifying average associations and fail to account for the variability in cognitive trajectories among different older adults (20, 21).
Hence, this research endeavors to conduct ongoing assessments of cognitive function within a nationally representative cohort of Chinese older adults, employing Latent Class Growth Modeling (LCGM) to delineate heterogeneous cognitive trajectories in this population. The primary aim is to scrutinize the associations between objective isolation (including both family and friend isolation), subjective isolation and heterogeneous cognitive trajectories, all within the unique milieu of an Eastern collectivist culture. Through these investigations, the study aspires to offer evidence-based insights for the formulation of precise cognitive health enhancement strategies tailored to older adults in Eastern collectivist societies, which can contribute significantly to the prevention of dementia and related conditions, decelerate cognitive aging processes, and thereby reduce the pressures on healthcare and social welfare systems.
2 Methods
2.1 Data source and sample selection
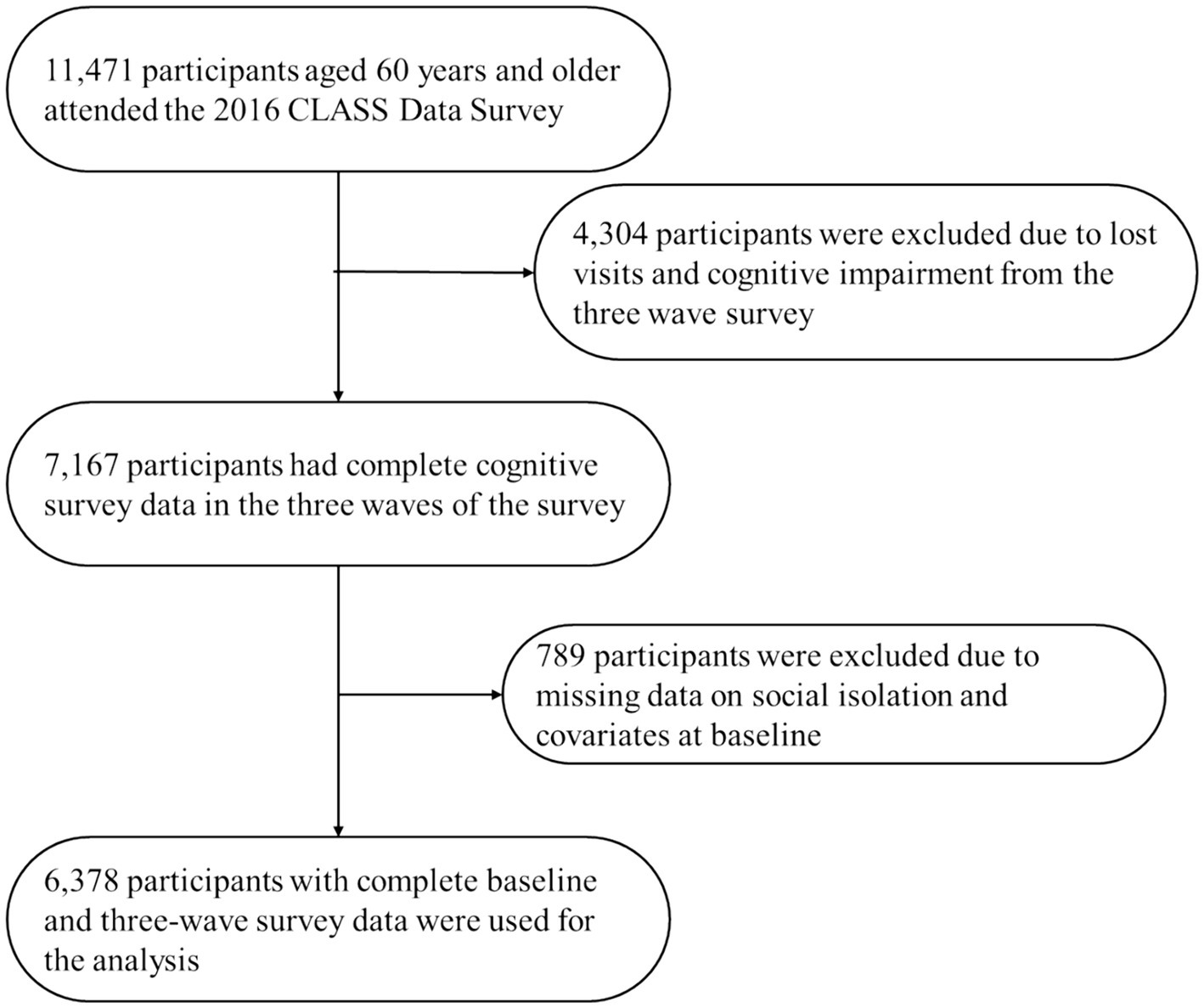
This investigation relies on data from the China Longitudinal Aging Social Survey (CLASS), employing a stratified multi-stage probability sampling design to select individuals aged 60 and above from 28 provincial units across the country. The CLASS dataset includes detailed records on personal demographics, physical and mental health, and social support systems pertinent to older adults. Initiated in 2014, this study included biennial follow-up surveys, with the most recent conducted in 2020. The study leverages data from the 2016, 2018, and 2020 waves. From 2016 onwards, a total of 11,471 older adults had contributed data to CLASS.
Given the inevitable attrition in longitudinal surveys, and recognizing that a prerequisite for completing the psychological assessment scale is that the participants do not exhibit signs of cognitive impairment—specifically, a cognitive score of no less than 5 points (22)—this study excludes 4,304 older adults who were either lost to follow-up or demonstrated cognitive impairment across the three waves of surveys conducted from 2016 to 2020. This research aims to analyze the influence of the baseline data from 2016 on the heterogeneous trajectories of cognitive development among older adults. To ensure data completeness and accuracy, cases with missing information on multidimensional social isolation and other essential covariates at the baseline stage were eliminated, resulting in a final sample size of 6,378 individuals. The flow chart of the CLASS follow-up and the sample selection of the current analysis is presented in Figure 1.
2.2 Measurements
2.2.1 Social isolation
To assess objective isolation, this study employed the Lubben Social Network Scale (LSNS) (23), as developed by Lubben and colleagues. This instrument evaluates the extent of social engagement among older adults by quantifying the number of family members and friends available for private discussions and support. It comprises two distinct components: family isolation (Cronbach’s alpha = 0.812) and friend isolation (Cronbach’s alpha = 0.856), incorporating a total of six questions. Response options range from 0 (none), 1 (one), 2 (two), 3 (three to four), 4 (five to eight), to 5 (nine or more). An aggregate score for family or friend networks below 6 points (23) signifies isolation in that domain, coded as 1 for isolated and 0 for not isolated.
Subjective isolation is quantified through the loneliness variable (24), which is evaluated using a single item from the Center for Epidemiologic Studies Depression Scale (CES-D): “How often did you feel lonely in the past week?” (25). Responses to this item are scored on a three-point scale: 1 (never), 2 (sometimes), and 3 (often). Participants who respond with “2” or “3” are classified as experiencing subjective isolation and are assigned a code of 1, while those who respond with “1” are coded as 0, indicating the absence of subjective isolation.
2.2.2 Cognitive function
The evaluation of cognitive function within this study utilizes the Mini-mental State Examination (MMSE) as provided by CLASS (26). This instrument measures the cognitive performance of older adults across various domains: orientation (5 items), memory (3 items), attention and calculation (5 items), and recall (3 items), including a total of 16 questions. Responses are scored on a binary scale: 1 point for each correct answer and 0 points for each incorrect answer, resulting in a possible score range of 0 to 16 points. A higher total score is indicative of superior cognitive functioning.
2.2.3 Covariates
In this study, covariates were selected based on the ecological model of health (27), examining determinants of cognitive function across various strata to underpin cognitive impairment prevention strategies among older adults. The specific covariates are as follows: The model’s innermost layer considers individual physical characteristics, including age (>60 years), gender (female, male), the presence of chronic diseases (yes or no), depression (assessed via the Center for Epidemiological Studies Depression Scale (CES-D) (25), with a total score of 24 points where higher scores denote more severe depression), and basic Activities of Daily Living (ADL) status (scored out of 33 points across 11 activities, with higher scores reflecting decreased basic activity capability). Notably, since subjective isolation is measured using an item from the CES-D, the depression variable in this analysis excludes this specific item to avoid overlap. The model’s second layer focuses on social networks, highlighting marital status (married, unmarried/divorced/widowed). The third layer explores living and working conditions, delineated by educational level (illiterate, primary school, junior high school, high school and above), employment status (employed, not employed), and household registration (rural, urban). The outermost layer assesses the policy environment, specifically the presence of pension insurance (having at least one type of pension insurance, none).
2.3 Statistical methods
LCGM is a comprehensive mixed model that combines the characteristics of Latent Growth Curve Modeling (LGCM) and Latent Class Analysis (20, 21, 28). First, it describes the trajectory of the growth curve using the latent growth curve model, and then further refines the analysis by determining the number of latent trajectory classes, categorizing individuals into distinct latent groups based on their growth trajectories. This method allows for a detailed examination of the variability in cognitive function among older adults, facilitating a deeper understanding of the heterogeneity within this demographic.
In determining the optimal number of latent trajectory classes, our approach involved incrementally increasing the number of classes until the improvement in model performance ceased to be significant. The evaluation and selection of the final model were guided by various statistical metrics: Sample-size Adjusted Bayesian Information Criterion (SABIC), Entropy, Bootstrap Likelihood Ratio Test (BLRT), and Vuong-Lo–Mendell–Rubin Likelihood Ratio Test (VLMR-LRT). An appreciable decrease in SABIC signals an enhanced fit of the model. Entropy values, which range from 0 to 1, reflect the clarity of class distinction, with higher scores indicating more distinct class separations. Both VLMR-LRT and BLRT compare models with varying numbers of classes, where a significant p-value supports the model with a greater number of classes as providing a superior fit. Additionally, it is essential for model validity that each identified class comprises at least 5% of the sample size. In the selection of the ultimate model, the interpretability and meaningfulness of each trajectory class also play a pivotal role.
Firstly, employing LCGM enables the precise differentiation of diverse cognitive trajectories among groups, enhancing the accuracy of identifying distinct cognitive patterns. Secondly, between-class differences were examined by Kruskal-Wallis rank sum test for continuous variables or χ2 test for categorical variables. Lastly, the application of multinomial logistic regression analysis aids in uncovering the impact of the baseline data from 2016 on the heterogeneous cognitive development trajectories among older adults. This approach provides empirical support for the detection and intervention of cognitive impairments in older adults. The analysis leverages Mplus8.3 software for identifying the heterogeneous cognitive trajectories among older adults, while Stata 17.0 is used for conducting χ2/t-tests and multinomial logistic regression analysis, with a significance level set at p < 0.05.
3 Results
3.1 Heterogeneous cognitive trajectories of older adults
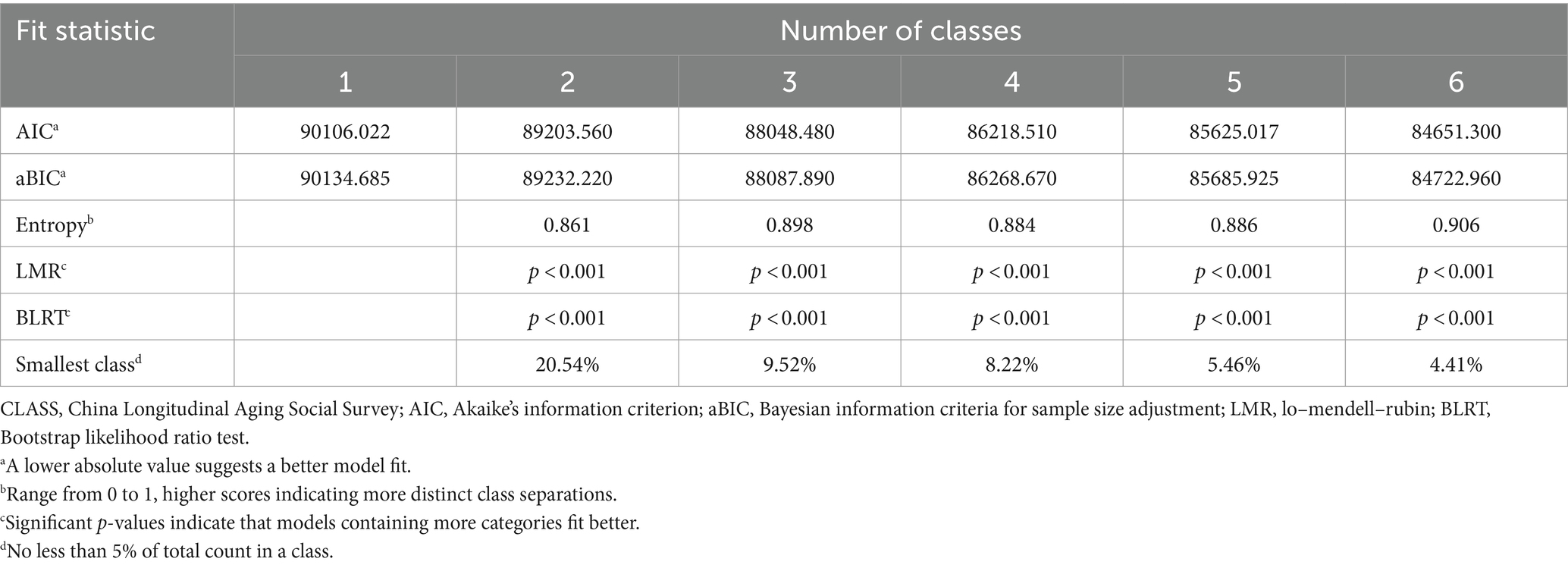
LCGM was employed to identify heterogeneous cognitive trajectories among older adults, with the analysis guided by key statistical metrics as detailed in Table 1. The investigation resulted in a 3-class LCGM model that balanced simplicity with adequate fit and clear classification (Entropy value = 0.898). Although a model with more classes showed some improvements in specific indicators, it was deemed potentially susceptible to overfitting. Therefore, the 3-class model was chosen for its statistical robustness, simplicity, and ability to effectively capture the underlying heterogeneity within the data.
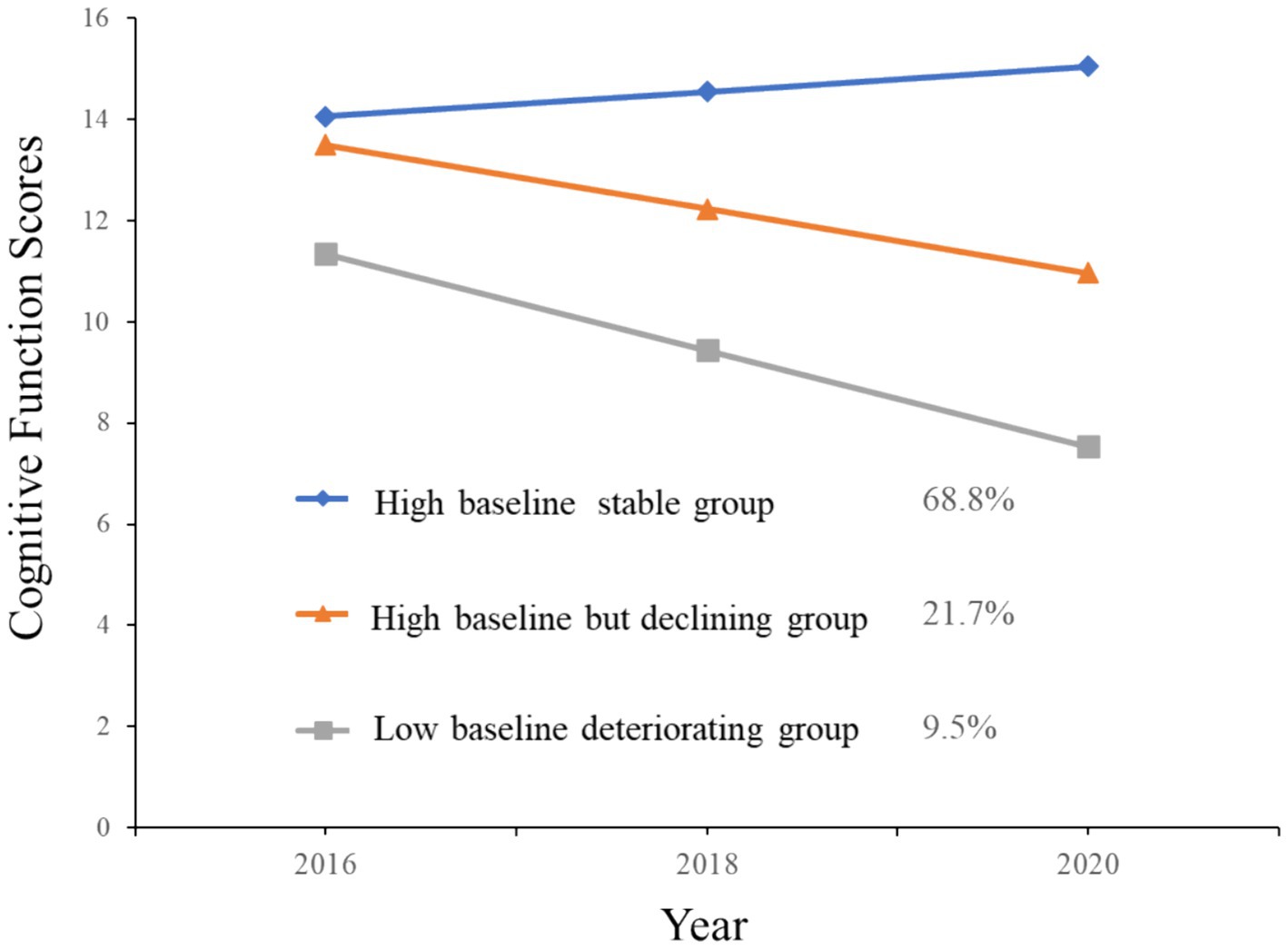
The analysis delineated three heterogeneous cognitive trajectories, with each class’s intercepts, slopes, and corresponding statistical tests summarized in Table 2 and illustrated in Figure 2. The first trajectory, including 68.8% of the sample (n = 4,388), displayed the highest average cognitive function at baseline (Intercept I = 14.055, p < 0.001) with a stable, albeit slight, upward trajectory (Slope S = 0.563, p < 0.001), and was thus classified as the “High baseline stable group.” The second trajectory, comprising 21.7% of the sample (n = 1,386), started with a relatively high baseline cognitive function (Intercept I = 13.499, p < 0.001) but experienced a significant decline over time (Slope S = −1.268, p < 0.001), leading to its classification as the “High baseline but declining group.” The third trajectory, accounting for 9.5% of participants (n = 604), began with the lowest average cognitive function (Intercept I = 11.341, p < 0.001) and underwent a more rapid decline (Slope S = −1.901, p < 0.001), identifying this group as the “Low baseline deteriorating group.”
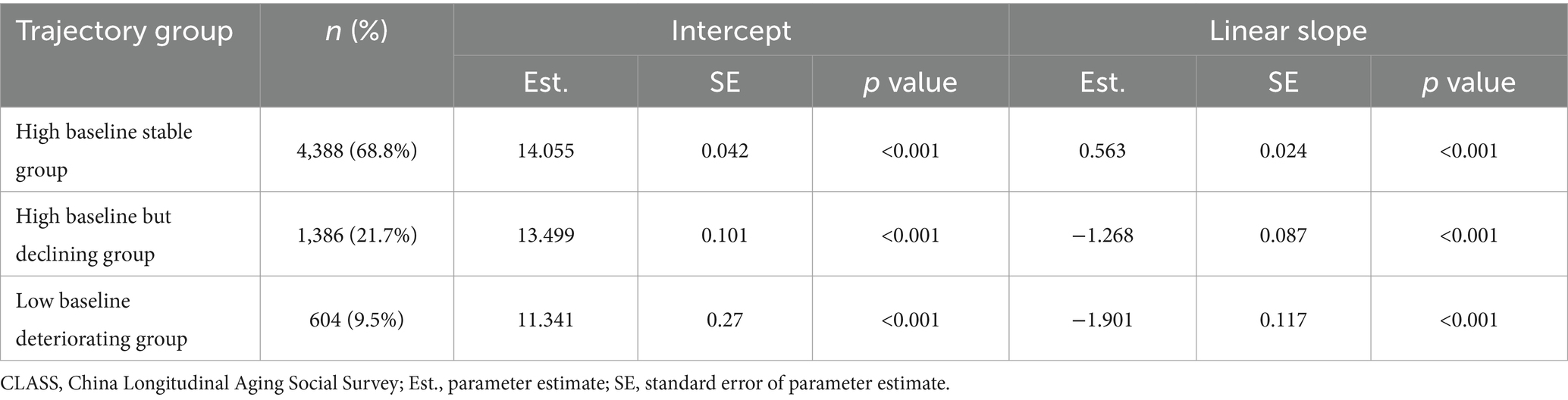
Table 2. The final three-group trajectory model of cognitive function of aged 60 years and older adults from CLASS.
3.2 Descriptive statistical analysis of study subjects
Table 3 presents the status of multidimensional social isolation among older adults. Out of 6,378 individuals, the prevalence rates of family isolation, friend isolation, and subjective isolation were 19.18, 28.77, and 42.79%, respectively. Additionally, it is important to note that 6.7% of the participants experienced both objective and subjective isolation concurrently. Comparative analyses across different cognitive trajectories highlighted that people in the “Low baseline deteriorating group” exhibited higher rates of family isolation, friend isolation, and subjective isolation than those in the “High baseline stable group,” with these differences reaching statistical significance (p < 0.01).

Table 3. Baseline characteristics of the participants according to trajectories of cognitive function aged 60 years and older adults from CLASS.
Demographically, males represented a slight majority (51.29%), and a significant portion of the sample fell within the 60–74 age range (84.45%). The presence of chronic diseases was common (55.74%), the average ADL score was 11.38 ± 1.40, and the average depression score stood at 13.81 ± 2.73, reflecting the health status of older adults. Our findings indicate that males are more likely to experience family and friend isolation, whereas females are more prone to subjective isolation. With increasing age, the proportion experiencing objective isolation gradually decreases, while the proportion experiencing subjective isolation increases. Higher ADL and depression scores are associated with a greater likelihood of subjective isolation. In terms of social networks, most of the sample were married individuals (77.00%), with a nearly equal distribution between rural (49.86%) and urban (50.14%) residences. The study showed that unmarried and rural older adults are more susceptible to subjective isolation. Regarding educational and occupational background, the majority of the sample had an education level of primary school or below (41.89%), with only 9.36% having attained high school education or higher. Most older adults were not employed (86.05%), with a significant portion being retired. The findings suggest that retired older adults are more likely to experience subjective isolation. In the policy environment, a large majority had some form of pension insurance (73.71%). However, older adults without pension insurance were found to be more vulnerable to both subjective and objective isolation.
Further Kruskal-Wallis rank sum test or χ2 test comparing characteristics among cognitive groups revealed that the “Low baseline deteriorating group” was more likely to include older females with more severe depression and diminished ADL capabilities. Social network analyses indicated higher proportions of unmarried individuals and those residing in rural areas within this group. Concerning living and working conditions, this group had lower educational levels and a higher percentage of non-working individuals. From a policy perspective, a lack of pension insurance was more prevalent among those in the “Low baseline deteriorating group” compared to the “High baseline stable group.”
3.3 Impact of multidimensional social isolation on heterogeneous cognitive trajectories among older adults
The analysis employed a multinomial logistic regression model, designating the identified cognitive trajectory groups (High baseline stable group, High baseline but declining group, Low baseline deteriorating group) as the dependent variable, with the High baseline stable group serving as the reference category. This model assessed the influence of multidimensional social isolation, alongside various covariates such as physical characteristics, social networks, living and working conditions, and policy environment, on cognitive trajectories among older adults. The findings, detailed in Table 4, primarily focused on the effects of different facets of social isolation.
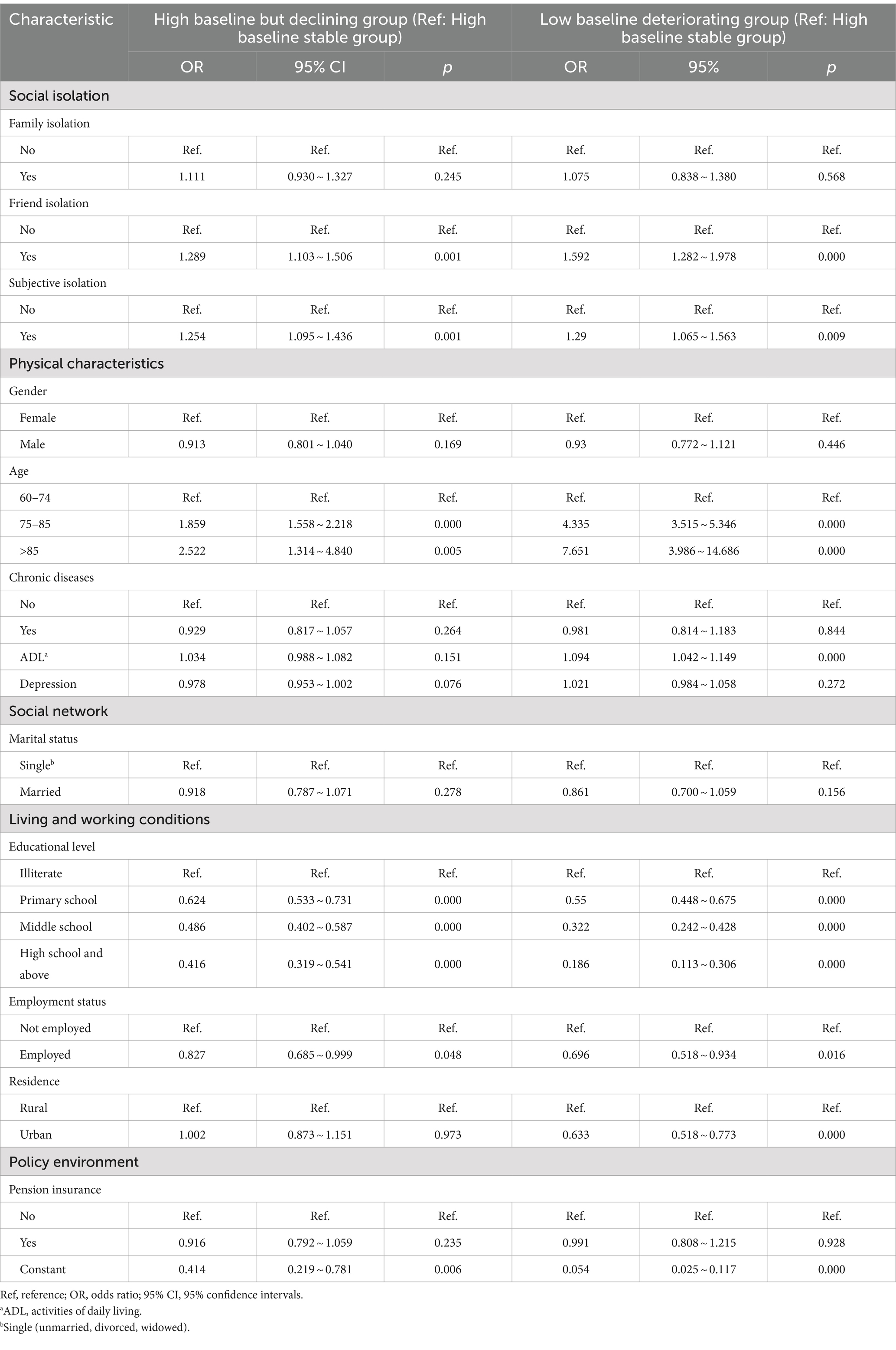
Table 4. Multinomial logistic regression analysis for the association between multidimensional social isolation and heterogeneous cognitive trajectories among older adults.
The analysis revealed that family isolation did not significantly influence the risk of transitioning to the High baseline but declining group or Low baseline deteriorating group cognitive groups. Conversely, friend isolation markedly heightened the risk of high-level cognitive declining (OR = 1.289) and low-level cognitive deteriorating (OR = 1.592). Similarly, subjective isolation significantly elevated the risks for high-level cognitive declining (OR = 1.254) and Low baseline deteriorating group (OR = 1.29). The inclusion of covariates such as individual physical characteristics, social networks, living and working conditions, and policy environment, resulted in only minimal alterations to the original findings regarding the influence of social isolation on cognitive trajectories, suggesting a strong independent effect of social isolation factors. The detailed outcomes of this extended analysis are visually presented in Figure 3.
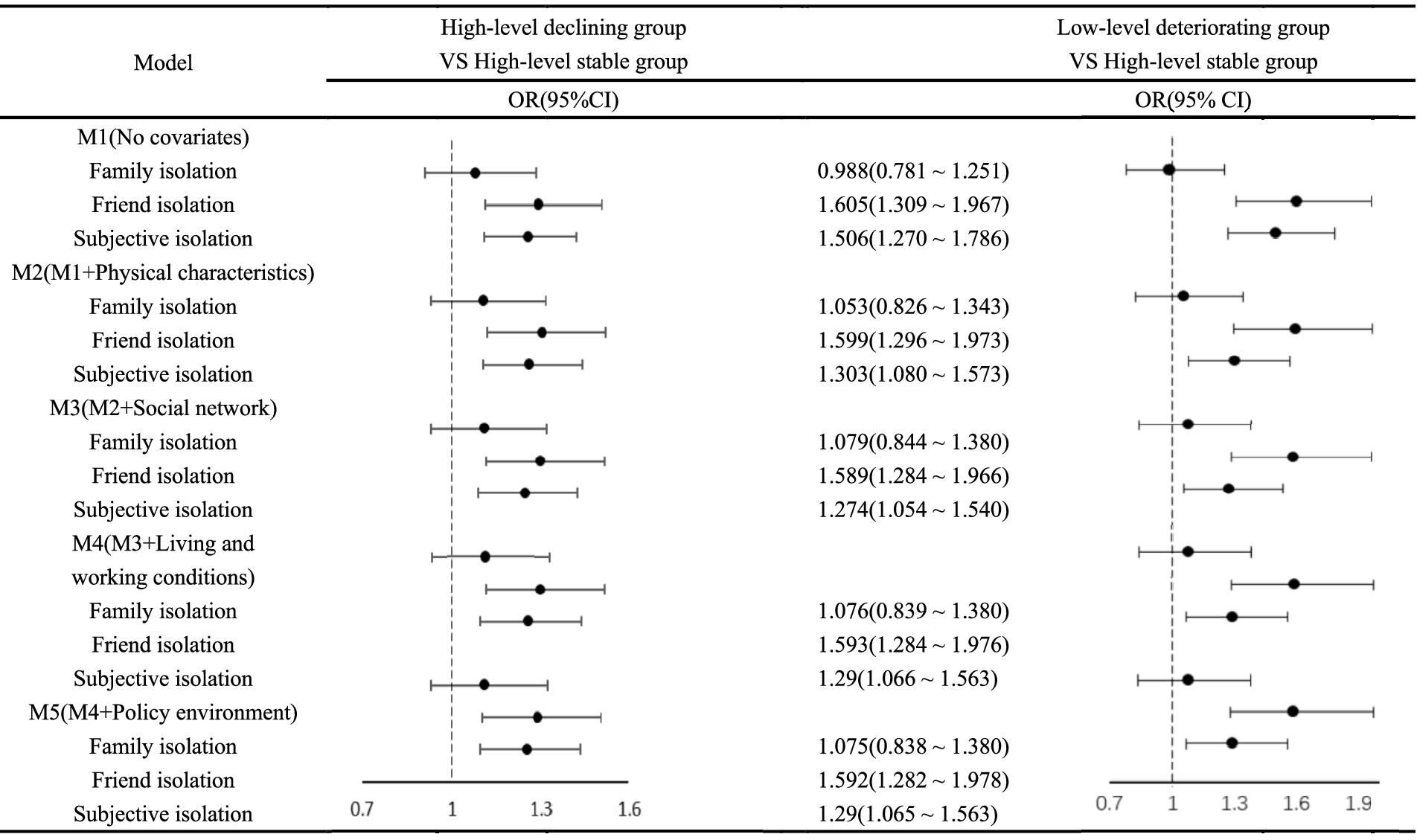
Figure 3. Stratified analysis for association between multidimensional social isolation and heterogeneous cognitive trajectories among older adults.
Examining the covariates, older age brackets (>85 years and 75–84 years) were significantly associated with increased risks of High baseline but declining group (OR = 2.522 and 1.859, respectively) and Low baseline deteriorating group (OR = 7.651 and 4.335, respectively) in cognitive function. Higher ADL scores were notably linked to an increased risk of cognitive function’s Low baseline deteriorating group (OR = 1.904). Urban household registration was associated with a reduced risk of cognitive function’s Low baseline deteriorating group (OR = 0.633). Higher educational levels and being employed were protective against the risk of high-level cognitive declining and Low baseline deteriorating group, with significant OR values indicating a reduced risk across these categories. These findings highlight the complex interplay of social isolation and other factors in influencing the cognitive aging process among older adults, underscoring the significance of multidimensional social support and engagement in maintaining cognitive health.
3.4 Sensitivity analysis
To verify the robustness of our research findings, we implemented two measures: First, we lowered the sample selection criteria to include older adults with cognitive impairments identified in 2018 and 2020, thereby comprehensively considering the cognitive trajectories of older adults with lower cognitive health levels. Figure 4 illustrates these results. After relaxing the sample selection criteria, the final sample size reached 6,499 older adults. The analysis results indicate that, despite the more inclusive sample criteria, the overall conclusions regarding the cognitive trajectories of older adults remained consistent with the original analysis. This consistency suggests strong support for the reliability of our classification of cognitive trajectories among older adults.
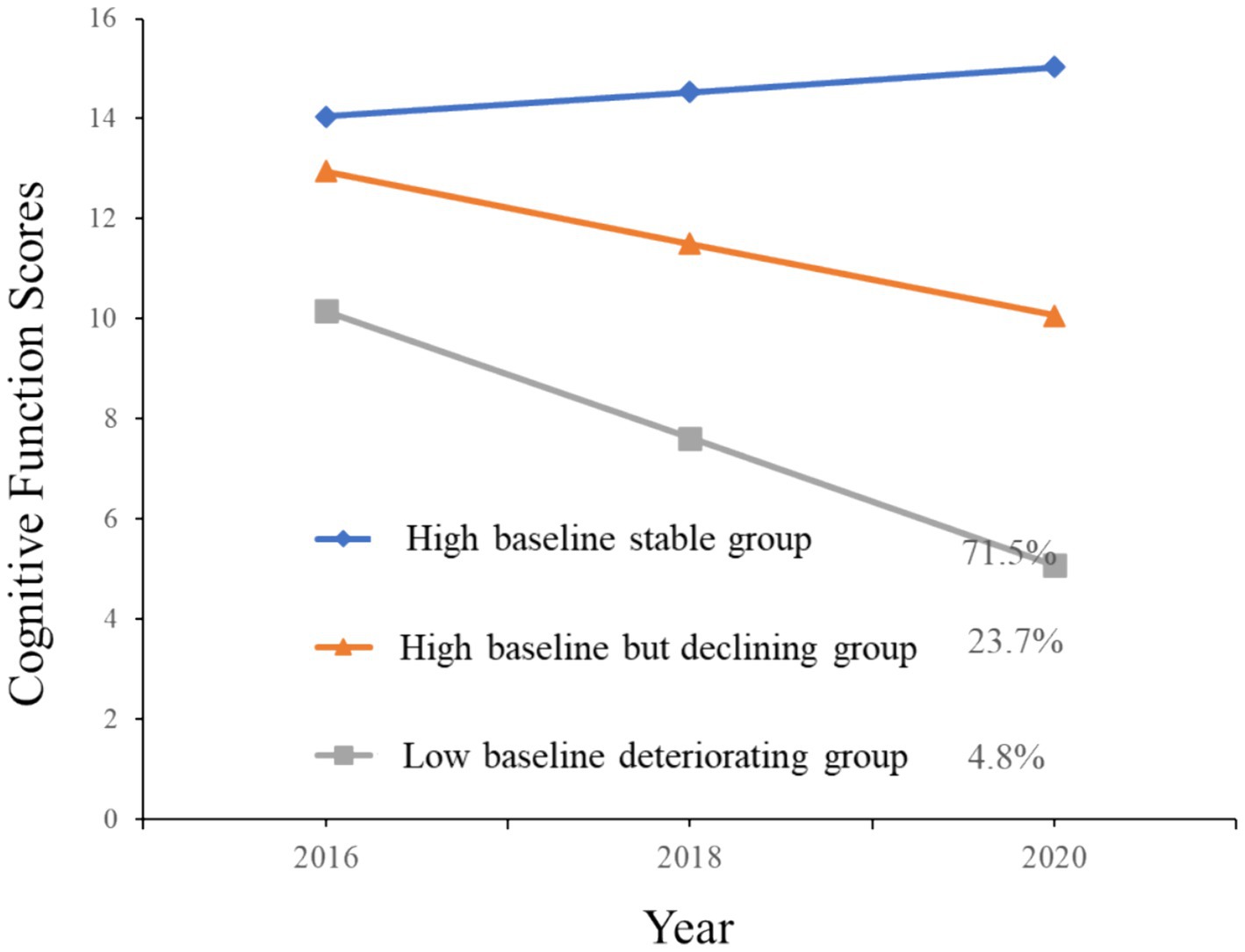
Figure 4. Trajectories of cognitive function scores by increasing year among older adults (including cognitively impaired groups in 2018 and 2020).
Secondly, we altered the treatment of the independent variables by analyzing social isolation as continuous variables rather than dichotomous ones. To avoid the potential information loss that occurs when continuous variables are converted to binary categories, we conducted an original treatment of the three dimensions of social isolation. Specifically, the dimensions of family isolation and friend isolation were converted into continuous variables of family networks and friend networks (where higher scores indicate a greater number of family members and friends the older adults can meet, contact, discuss private matters with, and seek help from). Subjective isolation retained the three-point scoring system of “1 (none), 2 (sometimes), 3 (often).” Table 5 presents these results. The findings show that a robust friend network significantly reduces the risk of both high-level cognitive decline and low-level cognitive deterioration, while subjective isolation significantly increases the risk of high-level cognitive decline. These results are consistent with our previous conclusions, further validating the relationship between social isolation and cognitive trajectories.
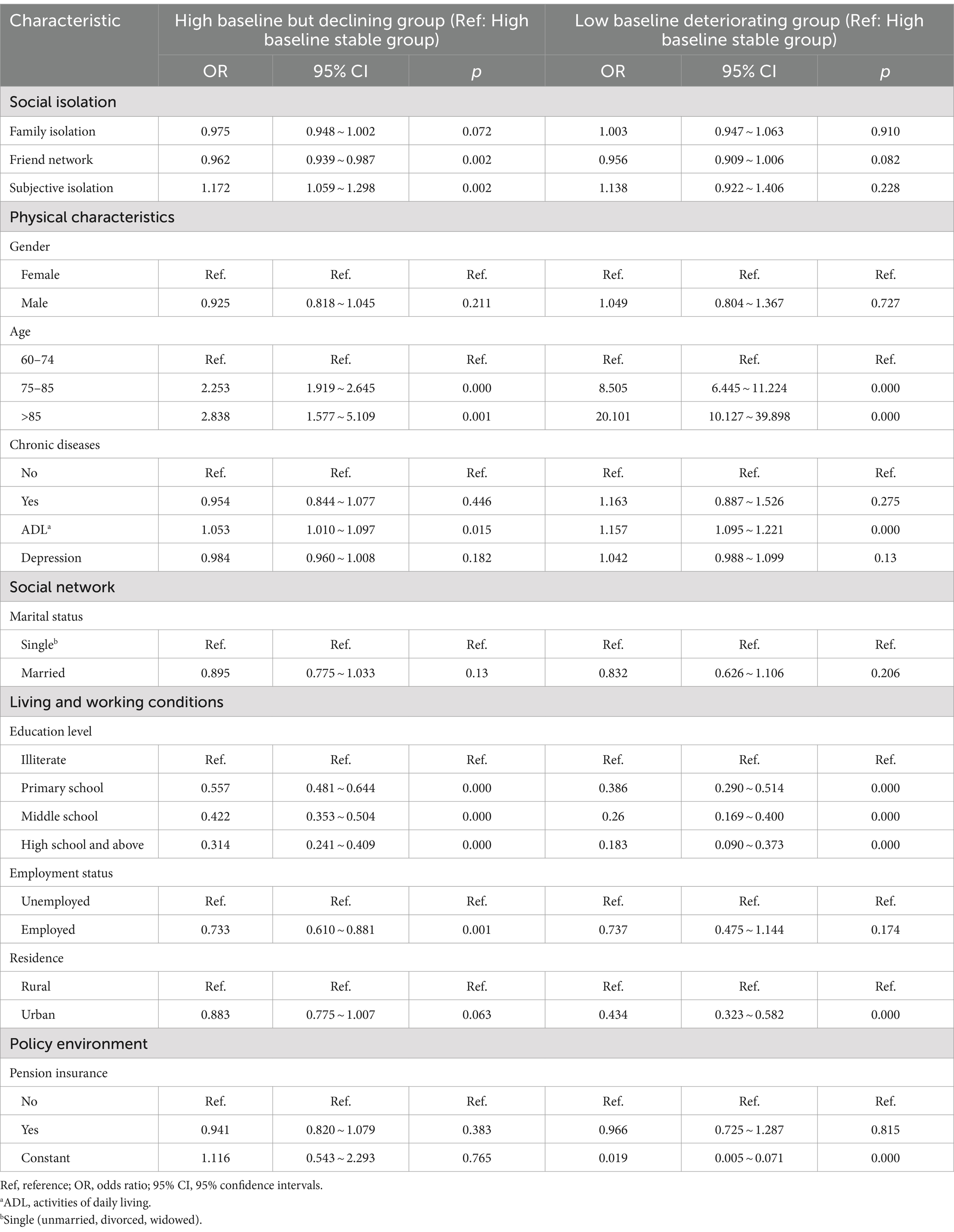
Table 5. Multinomial logistic regression analysis for the association between multidimensional social isolation and heterogeneous cognitive trajectories among older adults (analyzing the raw data for multidimensional social isolation as continuous variables).
4 Discussion
This investigation delves into the nuances of how family, friend, and subjective isolation uniquely influence cognitive trajectories among older adults in China. Utilizing latent class growth models on data from three successive waves of the Chinese Longitudinal Aging Social Survey (CLASS) spanning 2016 to 2020, with a sample of 6,378 participants aged 60 and above, we identified three cognitive trajectories: High baseline stable group, High baseline but declining group, and Low baseline deteriorating group. Our findings reveal that while family isolation has no significant impact, friend and subjective isolation markedly increase the risk of cognitive decline. By distinguishing between types of social isolation, this study enhances our understanding of their distinct effects on cognitive aging, informing more effective public health strategies for older adults.
This study reveals that 19.18% of older adults experience family isolation, 28.77% friend isolation, and 42.79% subjective isolation. These statistics align with prior research indicating objective isolation rates between 18.4 and 30.5% (29–31) and subjective isolation around 43% (24, 32). Given that a substantial portion of this study’s participants (84.45%) were aged 60–74 years, primarily younger older adults, the observed rates of social isolation were comparatively lower. Among these, older adults experience less isolation within families than with friends, which could be attributed to the strong caregiving culture in China, where familial support, especially from younger generations, plays a crucial role in older adult care (33).
Through the LCGM approach, three distinct cognitive trajectories among older adults were identified: High baseline stable group (68.8%), High baseline but declining group (21.7%), and Low baseline deteriorating group (9.5%). These categories correspond with findings from other studies (34, 35), although proportions vary, likely due to different study criteria and the inclusion of a younger senior population in our research. The significant representation of the High baseline stable group might be explained by the exclusion of individuals with cognitive impairments and the predominance of younger y older adults. Furthermore, variations in follow-up duration across studies might contribute to differing observations of cognitive decline (29, 36). Notably, while some research identifies diverse cognitive trajectories (29, 37), the number of trajectories detected often hinges on the interplay between subjective judgment and objective criteria in determining the optimal number of classes (28). This study’s findings underscore the complex dynamics of social isolation and cognitive health, highlighting the need for targeted interventions to mitigate cognitive decline among older adults.
Our findings reveal that while family isolation does not significantly affect cognitive decline at high levels or lead to low-level deterioration, both friend isolation and subjective isolation are notable risk factors for these adverse outcomes. This observation is consistent with existing literature, which has documented the detrimental effects of social isolation on cognitive functions (4, 24, 38, 39). Specifically, friend and subjective isolations are implicated in fostering adverse health behaviors (40, 41) that are linked to cognitive decline (36, 42), highlighting their potential roles in triggering these negative outcomes. However, friend isolation may predominantly affect cognitive abilities by reducing social stimulation, whereas subjective isolation could impact cognitive functions more through internal psychological stress. Frequent social interactions can bolster or maintain cognitive reserves, enhancing cognitive performance of older adults through the reallocation of brain networks or the adoption of alternative cognitive strategies (38, 43). Regular social engagement also stimulates cognitive activity, potentially increasing cortical synaptic density and, thereby, supporting the preservation of cognitive function in older age (4, 44). On the other hand, subjective isolation acts through psychological mechanisms, serving as a stressor that may lead to the overactivation of the hypothalamic–pituitary–adrenal (HPA) axis and increased expression of pro-inflammatory factors. These physiological responses can induce neurodegenerative changes in the hippocampus, a crucial area for memory and cognitive functions (45, 46). Moreover, subjective isolation can cause older adults to internalize their focus on social needs and negative emotions (40), which can consume substantial cognitive resources and negatively impact the execution of cognitive functions. This comprehensive understanding underscores the importance of addressing both friend and subjective isolations in efforts to mitigate cognitive decline among older adults.
Compared to friend isolation, this study found that family isolation does not significantly affect high-level cognitive decline and low-level deterioration in cognitive function, which aligns with some previous research findings (47, 48). This discrepancy can be attributed to several key factors. First, distinct functional roles. Family members predominantly fulfill economic and caregiving needs of older adults, while friends contribute to recreational and social developmental needs of older adults (44, 48). Friends provide diverse social stimuli, crucial for maintaining cognitive function, offering a range of social interactions that can stimulate cognitive processes in ways family relationships might not. Second, nature of interactions. Family interactions often carry obligatory undertones and may be more prone to negative exchanges, potentially causing greater psychological stress or harm to older adults (49, 50). Conversely, friendships, grounded in shared interests, tend to foster positive interactions, thereby enhancing sense of social identity and psychological well-being among older adults (47, 51). This positive dynamic with friends plays a crucial role in cognitive health maintenance. Third, mediation by friend networks. Functional support from family is pivotal for older adults to broaden their friend networks. The influence of family isolation on cognitive function is potentially fully mediated by friend isolation (48), indicating that the quality and extent of friendships are critical determinants of cognitive health. This mediation is particularly relevant in cultures where familial ties play a central role in social structures. Furthermore, some studies suggest no significant correlation between social isolation and cognitive trajectories, possibly due to difficulties in measuring and quantifying such complex social phenomena (13, 52, 53). The lack of a standardized tool for assessing social isolation contributes to these varying outcomes. Additionally, the hypothesis of a reverse causal relationship between social isolation and cognitive decline suggests that social isolation might be a consequence, rather than a cause, of cognitive deterioration (13, 36). This hypothesis underscores the importance of conducting longitudinal studies to better understand the directionalities and nuances of the relationship between social isolation and cognitive health in older adults.
Given the significant risk that friend isolation and subjective isolation pose to older adults in terms of high-level decline and low-level deterioration, it is crucial to implement measures to mitigate these impacts. A national strategy tailored to Chinese social and cultural norms, similar to the UK’s Anti-Social Isolation strategy (24), could boost social engagement using digital platforms, targeting those in remote areas. Additionally, enhancing public infrastructure and fostering family and community support can further facilitate social interactions among older adults. Early identification and personalized interventions for cognitive decline should also be considered to create a supportive ecosystem for older adults.
While this study provides valuable insights into the intricate dynamics between social isolation and cognitive trajectories among older adults, it is imperative to recognize certain limitations that could influence the generalizability of the findings. Firstly, the study relied on data from a broad social survey, employing relatively simplified tools for assessing complex constructs like subjective isolation, which was gauged with a single-item measure. This approach might not fully encapsulate the nuanced facets of loneliness. Moreover, cognitive function was assessed using the MMSE, which may have limitations in detecting subtle cognitive changes, particularly in early stages of impairment due to its ceiling effects. Secondly, the use of self-reported questionnaires, while practical for large-scale data collection, introduces potential biases related to participants’ memory accuracy, understanding of questions, and response tendencies, which might affect the data’s objectivity and precision. Thirdly, the longitudinal nature of the study led to exclusion of individuals who were less healthy, had lower education levels, or exhibited poorer cognitive function due to attrition or incomplete data. This could result in selection bias, possibly overlooking those with consistently low cognitive functioning. Finally, the relatively brief duration of follow-up might not be sufficient to capture the gradual progression of cognitive decline, limiting the ability to draw causal conclusions. It is also important to note that our results do not account for the potential influence of other mental health disorders, which may further restrict the generalizability of our findings.
5 Conclusion
This study utilizes data from the CLASS survey conducted between 2016 and 2020 to systematically chart the diverse cognitive trajectories of older adults in China, focusing on the impact of multidimensional social isolation on these trajectories. Three distinct cognitive groups were identified among older adults: the High Baseline Stable Group, the High Baseline Declining Group, and the Low Baseline Deteriorating Group. The findings indicate that friend isolation and subjective isolation significantly increase the risk of both high-level cognitive decline and low-level deterioration, while the impact of family isolation appears minimal. Consequently, addressing friend and subjective isolation among older adults emerges as a critical strategy for proactively safeguarding cognitive health, which could substantially alleviate pressures on healthcare and social welfare systems. These insights are vital for developing targeted interventions aimed at enhancing cognitive well-being and contribute to broader efforts to mitigate the onset and progression of dementia and related conditions within the older adult demographic. Future research should incorporate more comprehensive assessment tools, ensure broader and more diverse sample representation, and extend the duration of follow-up.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
Ethical approval was not required for the study involving human samples in accordance with the local legislation and institutional requirements because all procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The survey was conducted within the legal framework governed by articles 38, 39, and 40 of the Constitution of the People’s Republic of China and Chapter I, Article 9 from the statistics law of the People’s Republic of China. Therefore, the study was not reviewed by an ethics committee. Verbal informed consent was obtained from all individual participants included in the study. The design of this survey complied with the aforementioned articles and legal framework, where verbal informed consent was deemed acceptable and did not require review by an ethics committee. Furthermore, the interviewer documented detailed information on the process of obtaining informed consent, including agreement to participate, the time of consent, reasons for non-participation, among others. These details are stored by the Institute of Gerontology and National Survey Research Center at Renmin University of China.
Author contributions
XX: Writing – review & editing, Writing – original draft. YL: Writing – review & editing. FW: Writing – review & editing. AZ: Writing – review & editing. ZZ: Writing – review & editing. AX: Writing – review & editing, Writing – original draft, Resources, Methodology, Funding acquisition, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Social Science Foundations of China (2018VJX065).
Acknowledgments
The authors would like to thank all the participants of the China Longitudinal Aging Social Survey (CLASS) for contributing data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mayer, RE. Thinking and problem solving: an introduction to human cognition and learning. Scott, Foresman (1977).
2. Sanabria-Castro, A, Alvarado-Echeverría, I, and Monge-Bonilla, C. Molecular pathogenesis of Alzheimer’s disease: an update. Ann Neurosci. (2017) 24:46–54. doi: 10.1159/000464422
3. Hill, NL, McDermott, C, Mogle, J, Munoz, E, Depasquale, N, Wion, R, et al. Subjective cognitive impairment and quality of life: a systematic review. Int Psychogeriatr. (2017) 29:1965–77. doi: 10.1017/s1041610217001636
4. Kim, DE, and Yoon, JY. Trajectory classes of social activity and their effects on longitudinal changes in cognitive function among older adults. Arch Gerontol Geriatr. (2022) 98:104532. doi: 10.1016/j.archger.2021.104532
5. Fogg, C, Griffiths, P, Meredith, P, and Bridges, J. Hospital outcomes of older people with cognitive impairment: an integrative review. Int J Geriatr Psychiatry. (2018) 33:1177–97. doi: 10.1002/gps.4919
6. Lee, Y, Kim, J, Chon, D, Lee, K-E, Kim, J-H, Myeong, S, et al. The effects of frailty and cognitive impairment on 3-year mortality in older adults. Maturitas. (2018) 107:50–5. doi: 10.1016/j.maturitas.2017.10.006
7. Jia, L, Quan, M, Fu, Y, Zhao, T, Li, Y, Wei, C, et al. Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol. (2020) 19:81–92. doi: 10.1016/s1474-4422(19)30290-x
8. Nichols, E, Szoeke, CEI, Vollset, SE, Abbasi, N, Abd-Allah, F, Abdela, J, et al. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2019) 18:88–106. doi: 10.1016/s1474-4422(18)30403-4
9. Jia, L, Du, Y, Chu, L, Zhang, Z, Li, F, Lyu, D, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. (2020) 5:e661–71. doi: 10.1016/s2468-2667(20)30185-7
10. Cosco, TD, Fortuna, K, Wister, A, Riadi, I, Wagner, K, and Sixsmith, A. COVID-19, social isolation, and mental health among older adults: a digital catch-22. J Med Internet Res. (2021) 23:e21864. doi: 10.2196/21864
11. World Health Organization. Integrated care for older people (ICOPE) implementation framework: guidance for systems and services. Geneva, Switzerland: World Health Organization (2019). Available at: https://iris.who.int/handle/10665/325669
12. Kuiper, JS, Zuidersma, M, Zuidema, SU, Burgerhof, JG, Stolk, RP, Oude Voshaar, RC, et al. Social relationships and cognitive decline: a systematic review and meta-analysis of longitudinal cohort studies. Int J Epidemiol. (2016) 45:dyw089–206. doi: 10.1093/ije/dyw089
13. Evans, IEM, Martyr, A, Collins, R, Brayne, C, and Clare, L. Social isolation and cognitive function in later life: a systematic review and meta-analysis. J Alzheimers Dis. (2019) 70:S119–44. doi: 10.3233/jad-180501
14. Holt-Lunstad, J. Loneliness and social isolation as risk factors: the power of social connection in prevention. Am J Lifestyle Med. (2021) 15:567–73. doi: 10.1177/15598276211009454
15. Jang, Y, Park, NS, Chiriboga, DA, Yoon, H, Ko, J, Lee, J, et al. Risk factors for social isolation in older Korean Americans. J Aging Health. (2016) 28:3–18. doi: 10.1177/0898264315584578
16. VanderWeele, TJ, Hawkley, LC, and Cacioppo, JT. On the reciprocal association between loneliness and subjective well-being. Am J Epidemiol. (2012) 176:777–84. doi: 10.1093/aje/kws173
17. Beller, J, and Wagner, A. Disentangling loneliness: differential effects of subjective loneliness, network quality, network size, and living alone on physical, mental, and cognitive health. J Aging Health. (2018) 30:521–39. doi: 10.1177/0898264316685843
18. Holt-Lunstad, J, Robles, TF, and Sbarra, DA. Advancing social connection as a public health priority in the United States. Am Psychol. (2017) 72:517–30. doi: 10.1037/amp0000103
19. Fratiglioni, L, Wang, HX, Ericsson, K, Maytan, M, and Winblad, B. Influence of social network on occurrence of dementia: a community-based longitudinal study. Lancet. (2000) 355:1315–9. doi: 10.1016/s0140-6736(00)02113-9
20. Jung, T, and Wickrama, KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. (2008) 2:302–17. doi: 10.1111/j.1751-9004.2007.00054.x
21. Nagin, DS, and Odgers, CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. (2010) 6:109–38. doi: 10.1146/annurev.clinpsy.121208.131413
22. Petersen, RC, Smith, GE, Waring, SC, Ivnik, RJ, Tangalos, EG, and Kokmen, E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. (1999) 56:303–8. doi: 10.1001/archneur.56.3.303
23. Lubben, JE. Assessing social networks among elderly populations. Family Commun Health. (1988) 11:42–52. doi: 10.1097/00003727-198811000-00008
24. Luo, M, and Li, L. Social isolation trajectories in midlife and later-life: patterns and associations with health. Int J Geriatr Psychiatry. (2022) 37. doi: 10.1002/gps.5715
25. Radloff, LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
26. Folstein, MF, Folstein, SE, and Mchugh, PR. "Mini-mental state": a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98.
27. Ying, M, Bin, Z, Peng-Peng, J, and Rong-Xin, HE. Peculiarity, social environmental and in-patient service-based on the perspective of health ecology. J Northwest Univ. (2016) 46:146–58. doi: 10.16152/j.cnki.xdxbsk.2016-02-024
28. Ram, N, and Grimm, KJ. Growth mixture modeling: a method for identifying differences in longitudinal change among unobserved groups. Int J Behav Dev. (2009) 33:565–76. doi: 10.1177/0165025409343765
29. Cudjoe, TKM, Roth, DL, Szanton, SL, Wolff, JL, Boyd, CM, and Thorpe, RJ. The epidemiology of social isolation: National Health and aging trends study. J Gerontol B Psychol Sci Soc Sci. (2020) 75:107–13. doi: 10.1093/geronb/gby037
30. Poscia, A, Stojanovic, J, La Milia, DI, Duplaga, M, Grysztar, M, Moscato, U, et al. Interventions targeting loneliness and social isolation among the older people: an update systematic review. Exp Gerontol. (2018) 102:133–44. doi: 10.1016/j.exger.2017.11.017
31. Page-Reeves, J, Murray-Krezan, C, Regino, L, Perez, J, Bleecker, M, Perez, D, et al. A randomized control trial to test a peer support group approach for reducing social isolation and depression among female Mexican immigrants. BMC Public Health. (2021) 21:119. doi: 10.1186/s12889-020-09867-z
32. Perissinotto, CM, Stijacic Cenzer, I, and Covinsky, KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. (2012) 172:1078–83. doi: 10.1001/archinternmed.2012.1993
33. Su, Z, Hu, Z, and Peng, X. The impact of changes in China’s family patterns on family pension functions. Int J Health Plann Manag. (2017) 32:351–62. doi: 10.1002/hpm.2436
34. Elovainio, M, Sommerlad, A, Hakulinen, C, Pulkki-Råback, L, Virtanen, M, Kivimäki, M, et al. Structural social relations and cognitive ageing trajectories: evidence from the Whitehall II cohort study. Int J Epidemiol. (2018) 47:701–8. doi: 10.1093/ije/dyx209
35. Marioni, RE, Proust-Lima, C, Amieva, H, Brayne, C, Matthews, FE, Dartigues, JF, et al. Social activity, cognitive decline and dementia risk: a 20-year prospective cohort study. BMC Public Health. (2015) 15:1089. doi: 10.1186/s12889-015-2426-6
36. Lara, E, Caballero, FF, Rico-Uribe, LA, Olaya, B, Haro, JM, Ayuso-Mateos, JL, et al. Are loneliness and social isolation associated with cognitive decline? Int J Geriatr Psychiatry. (2019) 34:1613–22. doi: 10.1002/gps.5174
37. Liu, Z, Han, L, Gahbauer, EA, Allore, HG, and Gill, TM. Joint trajectories of cognition and frailty and associated burden of patient-reported outcomes. J Am Med Dir Assoc. (2018) 19:304–9.e2. doi: 10.1016/j.jamda.2017.10.010
38. Livingston, G, Huntley, J, Sommerlad, A, Ames, D, Ballard, C, Banerjee, S, et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet. (2020) 396:413–46. doi: 10.1016/s0140-6736(20)30367-6
39. Yang, R, Wang, H, Edelman, LS, Tracy, EL, Demiris, G, Sward, KA, et al. Loneliness as a mediator of the impact of social isolation on cognitive functioning of Chinese older adults. Age Ageing. (2020) 49:599–604. doi: 10.1093/ageing/afaa020
40. Hawkley, LC, and Cacioppo, JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. (2010) 40:218–27. doi: 10.1007/s12160-010-9210-8
41. Kent de Grey, RG, Uchino, BN, Trettevik, R, Cronan, S, and Hogan, JN. Social support and sleep: a meta-analysis. Health Psychol. (2018) 37:787–98. doi: 10.1037/hea0000628
42. Yuan, M, Chen, J, Han, Y, Wei, X, Ye, Z, Zhang, L, et al. Associations between modifiable lifestyle factors and multidimensional cognitive health among community-dwelling old adults: stratified by educational level. Int Psychogeriatr. (2018) 30:1465–76. doi: 10.1017/s1041610217003076
43. Stern, Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. (2002) 8:448–60. doi: 10.1017/S1355617702813248
44. Yates, LA, Ziser, S, Spector, A, and Orrell, M. Cognitive leisure activities and future risk of cognitive impairment and dementia: systematic review and meta-analysis. Int Psychogeriatr. (2016) 28:1791–806. doi: 10.1017/s1041610216001137
45. Friedler, B, Crapser, J, and McCullough, L. One is the deadliest number: the detrimental effects of social isolation on cerebrovascular diseases and cognition. Acta Neuropathol. (2015) 129:493–509. doi: 10.1007/s00401-014-1377-9
46. McEwen, BS. The neurobiology of stress: from serendipity to clinical relevance. Brain Res. (2000) 886:172, 172–89. doi: 10.1016/s0006-8993(00)02950-4
47. Balouch, S, Rifaat, E, Chen, HL, and Tabet, N. Social networks and loneliness in people with Alzheimer's dementia. Int J Geriatr Psychiatry. (2019) 34:666–73. doi: 10.1002/gps.5065
48. Shi, J, and Liu, X. Social isolation and cognitive function for Chinese older adults: a moderated chain mediation model. J Psychol Sci. (2022) 45:1182–9. doi: 10.16719/j.cnki.1671-6981.20220520
49. Fingerman, KL, and Birditt, HKS. The best of ties, the worst of ties: close, problematic, and ambivalent social relationships. J Marriage Fam. (2004) 66:792–808. doi: 10.1111/j.0022-2445.2004.00053.x
50. Schuster, TL, Kessler, RC, and Aseltine, RH Jr. Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol. (1990) 18:423–38. doi: 10.1007/bf00938116
51. Wang, N, Ji, H, and Song, F. Research progress on social isolation and loneliness of widowed elderly. Chin Nurs Res. (2022) 36:260–5.
52. Li, X, Zhang, J, Hou, R, Zheng, M, Singh, M, Li, H, et al. Bidirectional associations of intellectual and social activities with cognitive function among middle-aged and elderly adults in China. J Affect Disord. (2022) 319:83–9. doi: 10.1016/j.jad.2022.09.031
Keywords: family isolation, friend isolation, subjective isolation, heterogeneous cognitive trajectories, latent class growth models, Chinese older adults
Citation: Xie X, Lyu Y, Wu F, Zong A, Zhuang Z and Xu A (2024) Exploring the association between multidimensional social isolation and heterogeneous cognitive trajectories among older adults: evidence from China. Front. Public Health. 12:1426723. doi: 10.3389/fpubh.2024.1426723
Edited by:
Lenard Kaye, University of Maine, United StatesReviewed by:
Jo Wrigglesworth, Monash University, AustraliaKent Jason Go Cheng, The Pennsylvania State University, United States
Copyright © 2024 Xie, Lyu, Wu, Zong, Zhuang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aijun Xu, eHVhaWp1bjIwMDBAbmp1Y20uZWR1LmNu
 Xinlong Xie
Xinlong Xie Yanxia Lyu1,2
Yanxia Lyu1,2 Fanfan Wu
Fanfan Wu Anpeng Zong
Anpeng Zong Zhiruo Zhuang
Zhiruo Zhuang Aijun Xu
Aijun Xu