- Mental Health Center of Jiangnan University, Wuxi Central Rehabilitation Hospital, Wuxi, Jiangsu, China
Objective: To understand the physical health condition and its influencing factors among the low-income population.
Method: Low-income residents who visited or consulted at our Hospital during 2022 were selected for this study. Through telephone or face-to-face interviews, a self-made basic information questionnaire was used for data collection. The physical health level of the low-income population was analyzed, and a logistic regression model was applied to study its influencing factors.
Results: A total of 2,307 people were included in this study, of which 2,069 had various types of diseases, indicating a disease rate of 89.68%. Multivariate logistic regression analysis showed that age ≥ 60 years old (OR = 1.567, 95%CI: 1.122–2.188), poor mental health status (OR = 2.450, 95%CI: 1.203–3.678), smoking (OR = 1.752, 95%CI: 1.269–2.206), pulse pressure difference ≥ 60 (OR = 1.485, 95%CI: 1.164–1.787), and poor hearing (OR = 1.268, 95%CI: 1.026–1.324) were risk factors for disease, whereas being female (OR = 0.729, 95%CI: 0.540–0.984) was a protective factor for physical health.
Conclusion: As a developing country with a large population, we should particularly focus on the physical health issues of the low-income population, take targeted measures for disease situations, and improve the quality of life of the low-income population.
1 Introduction
In recent years, with the rapid economic and urbanization development in China, the health issues of the public have gradually received government attention, especially the quality of life and disease conditions of specific groups such as low-income populations. The Chinese government has carried out a series of support and policy support work (1). However, it should also be noted that due to economic reasons, low-income populations often have untreated chronic diseases and are in relatively poor physical health (2). The direct link between low-income and poor health outcomes has been widely documented. Low-income individuals face adverse social factors such as malnutrition, poor living conditions, and discrimination, which contribute to the deterioration of physical and mental health across generations and persistent long-term poverty (3).
This study was conducted in Wuxi City, Jiangsu Province. Wuxi is located between 31°07′ and 32°02′ north latitude and 119°33′ and 120°38′ east longitude, situated in the southeastern part of Jiangsu Province, within the Yangtze River Delta corridor. It borders Suzhou to the east and is 128 km from Shanghai; it faces Huzhou in Zhejiang Province across Taihu Lake to the south. The total area of Wuxi is 4,627.47 sq. km, with the urban area covering 1,643.88 sq. km. In terms of population, by the end of 2023, Wuxi had a registered population of 5.2095 million, with an annual population growth rate of 3.73‰. The urbanization rate of the registered population was 87.56%. The city’s permanent resident population was 7.495 million at the end of the year. Economically, Wuxi’s GDP was 1.55 trillion yuan, with a GDP growth rate of 6%, and a per capita GDP of 206,300 yuan, ranking first among prefecture-level cities nationwide. Although Wuxi’s economic level ranks high nationally and per capita income has increased, it is important to note that the large population and uneven distribution of health and economic resources mean that a portion of the population remains at a low-income level. Therefore, the low-income population should not be overlooked in the pursuit of common prosperity. Currently, China’s low-income groups mainly include manual laborers, lower-tier workers, and other low-income earners. According to data from the second quarter of 2024 regular press conference held by the Ministry of Civil Affairs, the national dynamic monitoring platform for low-income populations covers 80.15 million people, accounting for about 5.7% of the total population. These low-income individuals mainly include nearly 40 million people on subsistence allowances, over 4.6 million people in extreme poverty, and other low-income individuals such as members of families on the edge of subsistence allowances and those being monitored to prevent them from falling back into poverty. To further improve the living conditions of low-income groups, the government and various sectors of society are taking a series of measures. These include strengthening the social security system, raising subsistence allowance standards, and helping low-income groups mitigate disease risks through charitable medical assistance, among other methods.
The health status of China’s low-income groups is influenced by various factors, including working conditions, lifestyle, and dietary habits, which may increase health risks and affect income and medical expenses (4). The health risks faced by low-income groups are becoming an increasing focus of social concern. Moreover, the health status of low-income groups is also affected by other factors. For example, the living conditions of low-income populations in remote areas and the risks they face are complexly intertwined. The vulnerability of their livelihoods and the worsening risk environment can lead to difficulties in living and even poverty. Therefore, conducting surveys on the health status of low-income populations in this region and understanding the related influencing factors to improve their health and living standards remains a top priority for government departments at all levels. Comprehensive measures to improve the health status of this group include strengthening health education and promotion, raising public awareness of health risks, and alleviating their economic pressure and living burdens through policies and social support. This will provide a scientific basis for formulating assistance policies for other gradually developing regions in China.
2 Subjects and methods
2.1 Subjects
Data were collected from low-income residents who visited or called for consultation at the Wuxi City Central Rehabilitation Hospital. A total of 2,307 cases were collected as research subjects, and the subjects’ basic personal information and disease-related information were collected. Inclusion criteria for research subjects: Age ≥ 18 years old; Able to communicate normally. Researchers with a lot of missing basic information and those who disagreed to participate in the survey were excluded.
2.2 Methods and related definitions
Cross-sectional research methods were applied. To ensure the validity and reliability of the self-made questionnaire, it was designed based on the research theme and objectives of this survey. The questionnaire was created to be user-friendly and easy for respondents to complete, thereby improving the completion rate. Additionally, interviews with two senior clinical doctors were conducted, which ultimately led to the finalization of the questionnaire, including gender, age, education level, marital status, smoking, drinking, disease conditions, self-rated mental health status, family care status, height, weight, blood pressure, hearing conditions, etc. Disease condition refers to diseases diagnosed by medical institutions, mainly including history of mental illness, substance dependence, heart attack, hepatitis, cirrhosis, tuberculosis, kidney disease, chronic bronchitis, stroke, hypertension, diabetes, tumor history, coronary heart disease, etc. BMI = weight (kg)/height (m)2. Pulse pressure difference is the average value of systolic pressure—diastolic pressure measured three times under resting conditions. Self-rated mental health status refers to whether one feels psychologically healthy. Low-income residents are defined as four types of people: those registered in the civil affairs system as minimum living allowance recipients, extremely poor individuals, families on the brink of minimum living allowance, and families with expenditure difficulties. By testing the reliability and validity of the questionnaire, it was found that the Cronbach’s α coefficient was 0.78 and the average content validity index (S-CVI/Ave) was 0.82, indicating good reliability and validity.
2.3 Statistical analysis
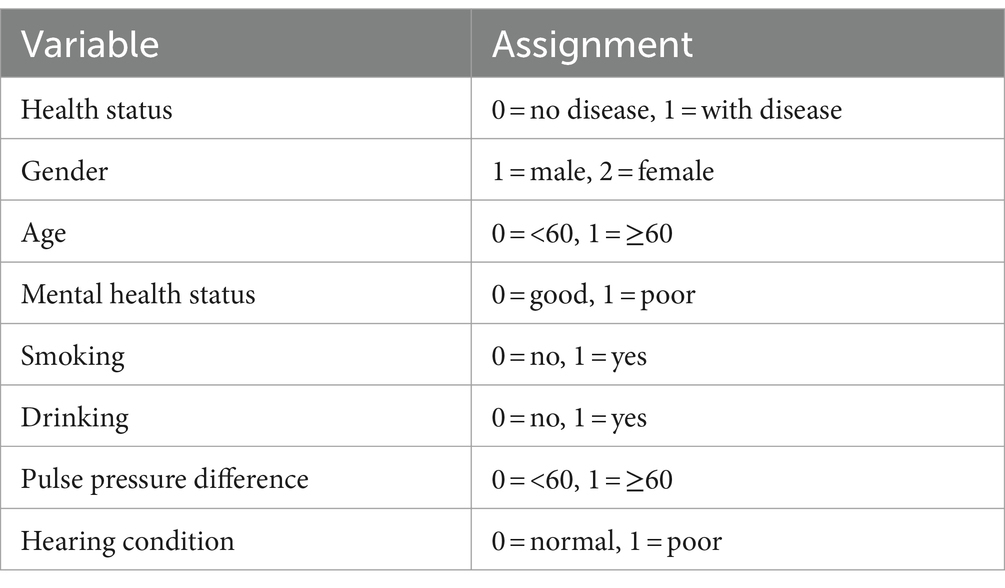
A multivariate logistic regression analysis model was constructed using SPSS 20.0 statistical software. Count data were expressed as rates or proportions. Quantitative data that followed a normal distribution were expressed as . Univariate analysis used the χ2 test. Variables with statistically significant differences were included in the logistic regression model. The assignment of independent variables was shown in Table 1. Differences were considered statistically significant at p < 0.05.
3 Results
3.1 Basic situation
A total of 2,307 people were included in the study, 1,568 were males (67.97%) and 739 were females (32.03%). The average age was 47.26 ± 17.64, and the majority had a junior high school education level (52.97%). A total of 2,069 people (89.68%) had illnesses, with the top three diseases being hypertension (50.20%), diabetes (18.25%), and infectious diseases (12.27%).
3.2 Univariate analysis of disease status
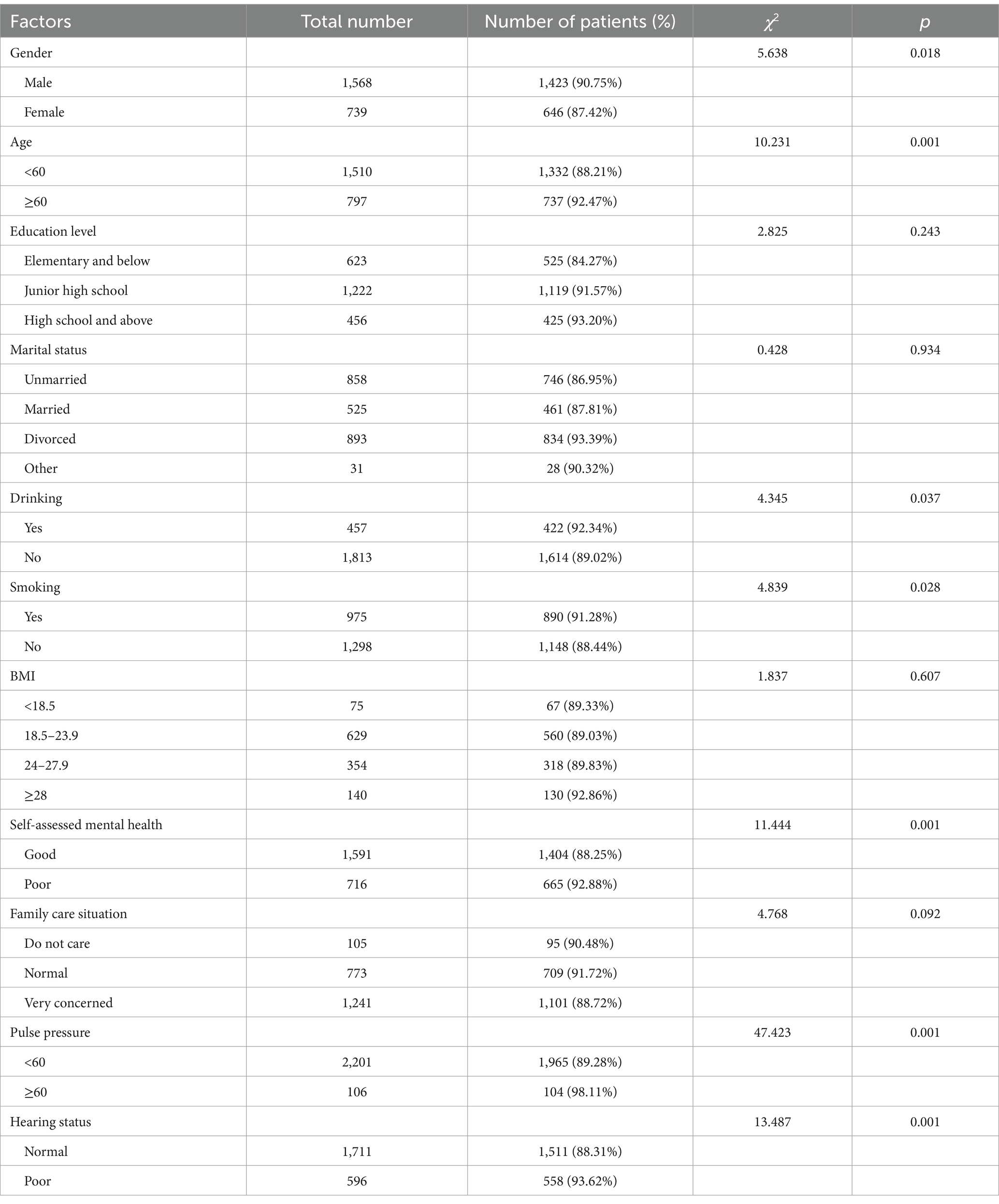
The disease rate in males was higher than in females, higher in people aged ≥60 years old than in those <60 years old, higher in smokers than in non-smokers, higher in alcohol consumers than in non-alcohol consumers, higher in those with poor mental health than in those with good mental health, higher in those with a pulse pressure difference ≥60 than in those with a pulse pressure difference <60, and higher in those with poor hearing than in those with normal hearing. The differences within each group were statistically significant (p < 0.05) (Table 2).
3.3 Analysis of influencing factors
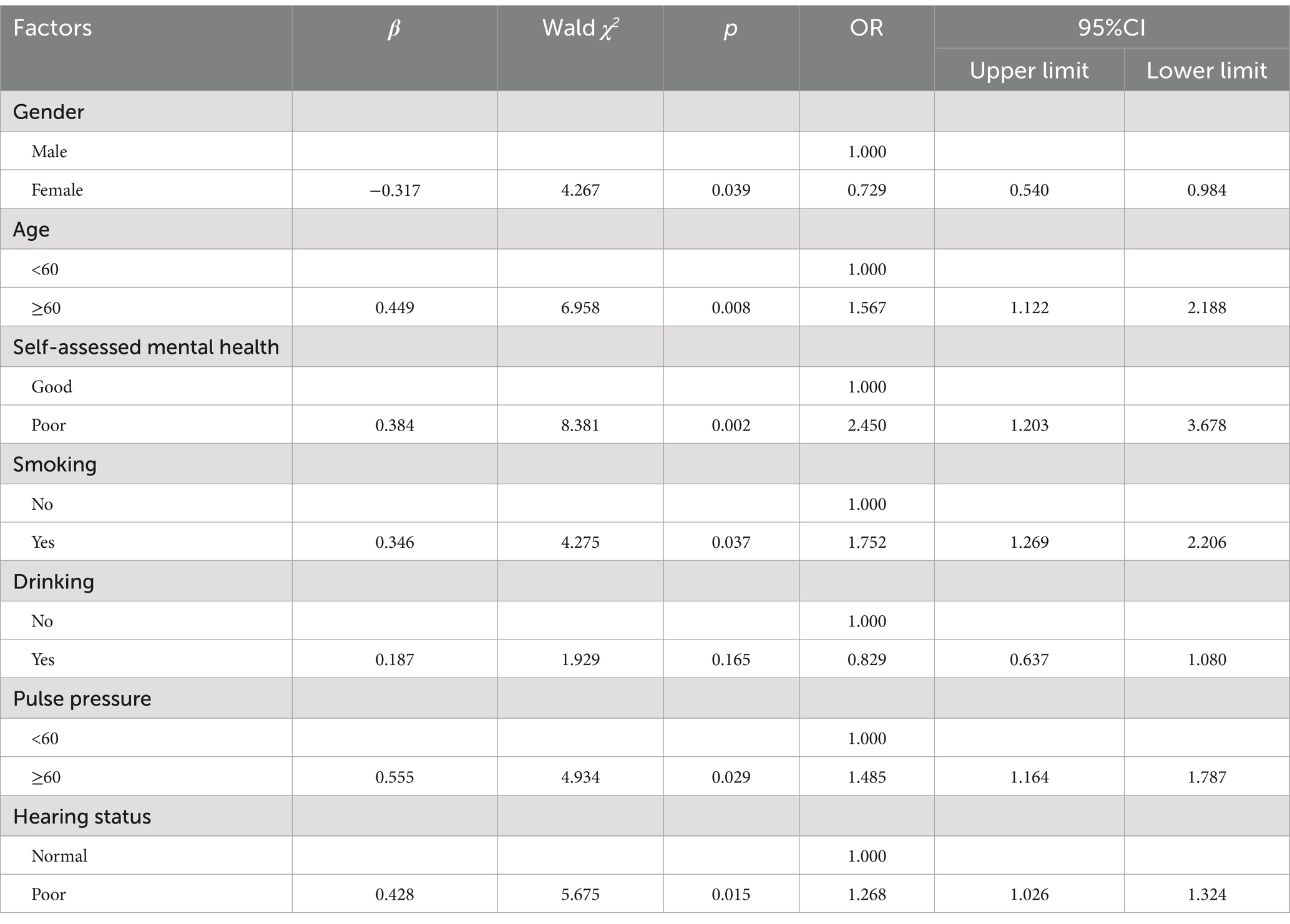
The variables that were statistically significant in the univariate analysis were included in the multivariate logistic regression model. The results suggest that the main influencing factors for disease in the low-income population are gender, age, self-rated mental health status, smoking status, pulse pressure difference, and hearing status. Specifically, compared to those under 60 years old, the risk of disease in low-income individual’s ≥60 years old is 1.567 times higher. Those with poor self-rated mental health have a disease risk 2.450 times higher than those with good mental health. Low-income residents who smoke have a disease risk 1.752 times higher than non-smokers. Those with a pulse pressure difference ≥60 have a disease risk 1.485 times higher than those with a pulse pressure difference <60. Low-income individuals with poor hearing have a disease risk 1.268 times higher than those with normal hearing. Being female appears to be a protective factor in the low-income population, with women being less likely to get sick compared to men (Table 3).
4 Discussion
Low-income or impoverished populations often experience health damage or loss. The influence of disease impacts a patient’s personal work capacity and can even affect their sources of income (5), intensifying the progression of the disease (6). Through this study, we found that in the Wuxi region, the incidence of various diseases among low-income populations reached 89.68%, a relatively high level and higher than the incidence found in other domestic studies (7, 8). This includes common chronic diseases such as hypertension and diabetes, as well as infectious diseases such as hepatitis B, hepatitis C, and tuberculosis. Therefore, individuals with chronic diseases are more likely to be impoverished due to the disease, creating not only a burden of disease but also significant economic costs (9). Therefore, it is necessary to conduct research investigations based on the health status of the low-income population and its influencing factors, providing further intervention measures.
This study found that women in the low-income population are less likely to suffer from various types of diseases compared to men, possibly because men are more susceptible to disease than women (10, 11). Compared with the low-age group of the low-income population, people aged 60 and older are more likely to develop various chronic or infectious diseases. Research reports that increasing age is a risk factor for chronic diseases (12). As age increases, the body’s immune and physiological recovery abilities gradually decline. Coupled with the impact of economic status, the older adult are more susceptible to various diseases (13). Other research has reported that more older adult people’s households are impoverished (4). We evaluated the mental health status of our study subjects and found that low-income populations who perceive their mental health as poor are more likely to fall ill. This may be because their self-awareness and satisfaction about their mental state are in a poor condition. Poor mental emotions can promote the occurrence and development of diseases, so attention to the mental health status of this population is particularly important (14). Smokers are more likely to develop chronic diseases than non-smokers. Smoking itself produces harmful chemicals like nicotine and tar, which have been proven to be carcinogenic and can also cause chronic lung diseases such as emphysema and bronchitis (15). Research also shows that smoking can exacerbate symptoms of anxiety and depression (16), all of which contribute to the reason why smokers are more prone to chronic diseases. We also found that residents with a pulse pressure difference of ≥60 are more likely to fall ill, it is very likely that an increase in pulse pressure difference will gradually shift from a sub-healthy state to a state of disease, leading to illness (17). We conducted a survey on the hearing status of the low-income population and found that those with poorer hearing are more likely to fall ill. It’s possible that impaired hearing is affected by brain or nerve, mental system abnormalities, which in turn leads to decreased hearing.
Based on this study and Weimer and Vining’s generic policies and policy-related studies (18), combined with the current stage of social development in China, the policy recommendations to improve the health levels of low-income groups mainly include expanding medical insurance coverage, improving the quality of medical services, strengthening health education and disease prevention, and increasing the income of low-income groups. To expand medical insurance coverage, gradually extend the scope of major disease treatment for low-income populations in rural and remote areas, covering major and severe diseases. Further expand the coverage of special treatment programs, incorporating diseases that impose significant local burdens into the local major disease treatment programs, and increase medical assistance efforts for low-income groups (19). This includes improving the medical insurance system, reducing their medical expenses, providing better medical services, and improving the accessibility and affordability of healthcare to benefit more impoverished people. Additionally, encourage social forces to participate and form a diversified health service model. Guide social capital into the medical field to invest in constructing medical institutions or providing medical services. At the same time, leverage the roles of non-governmental organizations and volunteers to provide public health services such as health consultations and check-ups for low-income groups.
Furthermore, strengthen inter-departmental collaboration to form a joint force. Government departments should enhance communication and cooperation to jointly develop and implement health policies for low-income groups. Strengthen cooperation and exchange with international organizations and other countries, learning from their successful experiences and practices to contribute to improving the health levels of low-income groups. Additionally, promote the development of the health industry and encourage the research and production of health products suitable for low-income groups, such as low-cost medicines and medical devices (20). This can not only meet the health needs of low-income groups but also promote innovation and development in the health industry.
In terms of improving medical service quality, all regions should continue to carry out special treatment programs for major diseases among low-income groups, enhance diagnosis and treatment capabilities, and improve medical quality so that most major disease patients can receive better medical services nearby (21, 22). Implement detailed family doctor contracting services for low-income groups, focusing on the standardized management of chronic disease patients such as those with hypertension and diabetes (23). Continuously strengthen health education and disease prevention efforts, advancing the three-year action plan for health promotion in poverty-stricken areas under the guidance of national policies. Conduct health education activities in villages, families, and schools to improve the health levels of residents in impoverished areas (24). Increase support for early diagnosis and treatment projects for major chronic diseases such as cancer in impoverished areas, promoting chronic disease screening, intervention, and early diagnosis and treatment.
To increase the income of low-income groups, increase their wage and business income. Encourage low-income individuals to work in cities or county towns to increase wage income, while developing local specialty industries to provide farmers with more employment opportunities and income sources. Strengthen the construction of the social security system: establishing a sound social security system is fundamental to increasing the income of low-income individuals. The government should increase investment to expand the coverage and level of social security projects such as social assistance, subsistence allowances, medical insurance, and pension insurance. Finally, in terms of education and employment, greater support for low-income groups is also needed. Education is an important means to enhance personal abilities and social status, so investment in the education of children from low-income families should be increased to ensure they receive a good education. Provide vocational training and employment guidance services to help low-income groups improve their employment skills and increase employment opportunities (25), thereby fundamentally improving their economic status and quality of life (26). By seriously implementing these policy recommendations, the government can effectively address the health and economic challenges faced by low-income groups, improve their health levels and quality of life, and promote social equity and harmony.
The advantage of this study is the large sample survey of the health status and influencing factors of low-income groups. However, the study has limitations due to the cross-sectional nature, which restricts causal inference; there are recall and information biases in the survey of selected subjects. Additionally, the lack of relevant data on genetic, psychological, and behavioral factors affects the survey results. Finally, due to the absence of specific income data for low-income groups, it is not possible to conduct a stratified analysis of their economic status, which impacts the stability of the results.
5 Conclusion
In summary, in the context of implementing poverty alleviation policies in China, the number of impoverished people is gradually decreasing. However, the health conditions of the impoverished population remain our primary concern. We need to pay attention to the impact of chronic diseases on low-income populations to prevent the reoccurrence of poverty due to illness. Disease health monitoring and economic policy support should be launched for this special population. We should encourage low-income individuals to participate in social labor and provide corresponding policies (27) to help them completely escape poverty. Enhancing the economic income and health knowledge literacy of the impoverished population will ultimately improve their quality of life.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Wuxi Mental Health Centre. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YJ: Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft. YW: Data curation, Investigation, Methodology, Project administration, Resources, Writing – original draft. YYJ: Formal analysis, Investigation, Methodology, Project administration, Writing – original draft. LT: Investigation, Methodology, Project administration, Writing – original draft. QY: Formal analysis, Investigation, Methodology, Project administration, Writing – original draft. HZ: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The work is supported by the National Natural Science Foundation of China (82104244), Wuxi Municipal Science and Technology Bureau (K20231039 and K20231049), Top Talent Support Program for young and middle-aged people of Wuxi Health Committee (HB2023088), Scientific Research Program of Wuxi Health Commission (Q202101 and ZH202110), Wuxi Taihu Talent Project (WXTTP2021), Medical Key Discipline Program of Wuxi Health Commission (FZXK2021012).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhao, D, and Fang, Q. Hierarchical structure and historical changes of rural anti-poverty policies since the founding of new China. J Huazhong Agric Univ (Soc Sci Ed). (2019) 3:1–10+158. doi: 10.13300/j.cnki.hnwkxb.2019.03.001
2. Oates, GR, Jackson, BE, Partridge, EE, Singh, KP, Fouad, MN, and Bae, S. Sociodemographic patterns of chronic disease: how the mid-south region compares to the rest of the country. Am J Prev Med. (2017) 52:S31–9. doi: 10.1016/j.amepre.2016.09.004
3. Price, JH, Khubchandani, J, and Webb, FJ. Poverty and health disparities: what can public health professionals do? Health Promot Pract. (2018) 19:170–4. doi: 10.1177/1524839918755143
4. Ai, X, Xu, A, Qiao, X, and Song, Y. Study on health shocks and influencing factors of low-income population. J Nanjing Med Univ (Soc Sci Ed). (2021) 21:572–8.
5. Lan, X, Zhou, Z, Si, Y, Shen, C, Fan, X, Chen, G, et al. Assessing the effects of the percentage of chronic disease in households on health payment-induced poverty in Shaanxi Province, China. BMC Health Serv Res. (2018) 18:871. doi: 10.1186/s12939-014-0107-1
6. Ren, T, Ju, J, Huang, M, Pan, M, and Zhang, M. Poverty, disease and precise health poverty alleviation policy: based on the quality of life evaluation of the poor residents. Chinese Health Policy Res. (2018) 11:61–4.
7. Long, Y, Xie, Q, Chen, X, Wu, J, Qin, Y, Xiong, W, et al. Investigation on the health status of the poor population in Ezhou City. Public Health Prevent Med. (2019) 30:116–9.
8. Wang, X, Zhu, G, Sun, N, Feng, J, Xiao, Y, Shi, F, et al. Analysis of the health status and influencing factors of the poor population in Sanchunjie town, Dongming County. J Shandong Univ (Med Ed). (2021) 59:108–14.
9. Ciarambino, T, Crispino, P, Leto, G, Mastrolorenzo, E, Para, O, and Giordano, M. Influence of gender in diabetes mellitus and its complication. Int J Mol Sci. (2022) 23:8850. doi: 10.3390/ijms23168850
10. Goryakin, Y, and Suhrcke, M. The prevalence and determinants of catastrophic health expenditures attributable to non-communicable diseases in low- and middle-income countries: a methodological commentary. Int J Equity Health. (2014) 7:107.
11. Connelly, PJ, Azizi, Z, Alipour, P, Delles, C, Pilote, L, and Raparelli, V. The importance of gender to understand sex differences in cardiovascular disease. Can J Cardiol. (2021) 37:699–710. doi: 10.1016/j.cjca.2021.02.005
12. Li, J, Liu, J, Wu, E, Guo, X, Wang, Y, and Qi, H. Analysis of the prevalence and risk factors of hypertension among adult residents in Zhengzhou. Modern Prevent Med. (2020) 47:2263–2266+2286.
13. Guo, X, Zhao, B, Chen, T, Hao, B, Yang, T, and Xu, H. Multimorbidity in the elderly in China based on the China health and retirement longitudinal study. PLoS One. (2021) 16:e0255908. doi: 10.1371/journal.pone.0255908
14. Zhang, YL, Wu, BJ, Chen, P, and Guo, Y. The self-rated health status and key influencing factors in middle-aged and elderly: evidence from the CHARLS. Medicine (Baltimore). (2021) 100:e27772. doi: 10.1097/MD.0000000000027772
15. Christenson, SA, Smith, BM, Bafadhel, M, and Putcha, N. Chronic obstructive pulmonary disease. Lancet. (2022) 399:2227–42. doi: 10.1016/S0140-6736(22)00470-6
16. Melamed, OC, Walsh, SD, and Shulman, S. Smoking behavior and symptoms of depression and anxiety among young adult backpackers: results from a short longitudinal study. Scand J Psychol. (2021) 62:211–6. doi: 10.1111/sjop.12699
17. Lacey, B, Lewington, S, Clarke, R, Kong, XL, Chen, Y, Guo, Y, et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0·5 million adults in China: a prospective cohort study. Lancet Glob Health. (2018) 6:e641–9. doi: 10.1016/S2214-109X(18)30217-1
19. Desai, SM, Padmanabhan, P, Chen, AZ, Lewis, A, and Glied, SA. Hospital concentration and low-income populations: evidence from New York state Medicaid. J Health Econ. (2023) 90:102770. doi: 10.1016/j.jhealeco.2023.102770
20. Tan, Z, and Liu, Y. The connotation, characteristics, and development path of new productivity in the health sector. Health Econ Res. (2024) 41:1–4. doi: 10.14055/j.cnki.33-1056/f.2024.06.001
21. Chen, M, and Chen, C. A study on the equity of health service utilization in Jiangsu Province from the perspective of universal health coverage. Chinese Health Serv Manag. (2018) 35:177–81.
22. Sun, J, Li, L, Liu, C, Wang, Q, Hou, X, Shi, F, et al. Analysis of the impact of socioeconomic status on health service utilization among migrant elderly. Chinese J Prevent Med. (2024) 25:526–31. doi: 10.16506/j.1009-6639.2024.05.003
23. Song, Z, Gao, L, Mou, S, Chen, H, and Lu, X. Research Progress on the role of family doctors in chronic disease management. Occup Health. (2019) 35:1869–72. doi: 10.13329/j.cnki.zyyjk.2019.0489
24. National Health Commission, Development and Reform Commission, Ministry of Finance, Medical Insurance Bureau, State Council Poverty Alleviation Office . Notice on issuing the implementation plan for the three-year action plan for health poverty alleviation. Gazette State Council People's Republic of China. (2019) 5:73–8.
25. Fan, Y, and Cong, S. Financial support and continuous income growth of low-income groups. Econ Theory Bus Manag. (2024) 44:65–82.
26. Luo, C, and Liang, X. Income growth and common prosperity of rural low-income groups. J Financ Econ. (2022) 37:61–72.
Keywords: low-income population, physical health condition, influencing factors, Wuxi, China
Citation: Li S, Jiang Y, Wu Y, Ji Y, Tian L, Yang Q and Zhu H (2024) Analysis of the health status and its influencing factors of the low-income populations in Wuxi, China. Front. Public Health. 12:1424448. doi: 10.3389/fpubh.2024.1424448
Edited by:
Yawen Jiang, Sun Yat-sen University, ChinaReviewed by:
Srirath Gohwong, Kasetsart University, ThailandOlusanya Olubusoye, University of Ibadan, Nigeria
Copyright © 2024 Li, Jiang, Wu, Ji, Tian, Yang and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Queping Yang, d3V4aXFwX3lhbmdAMTYzLmNvbQ==; Haohao Zhu, emh1aGhAamlhbmduYW4uZWR1LmNu
†These authors have contributed equally to this work
 Shiming Li
Shiming Li Ying Jiang
Ying Jiang Yue Wu
Yue Wu Haohao Zhu
Haohao Zhu