Abstract
Background:
With the acceleration of population aging, depressive symptoms in older adults have become an urgent global public health issue. It is critical to understand how to prevent and intervene the epidemic of depressive symptoms. Several studies have reported the prevalence of depressive symptoms among older adults in urban and rural China, but there is a lack of cross-sectional studies on the prevalence of depressive symptoms among older adults in Anhui Province after the COVID-19 pandemic.
Methods:
Between December 2023 and February 2024, we used convenience sampling to randomly recruit 1,175 older people over 60 years old in Anhui Province, China. The PHQ-9 depressive symptom scale, frailty scale, and social frailty scale were used in the study. Logistic regression was used to analyze the association between frailty, social frailty, family health and depressive symptoms in older adults.
Result:
Of the 1,175 participants, 406 (34.6%) had depressive symptoms. Binary logistic regression results showed that Status of body pain (p < 0.001), Number of hospitalizations in the past year (p < 0.001), Status of social frailty (p < 0.001) and Status of frailty (p < 0.001) were highly correlated with depressive symptoms in older adults. While family health (OR = 0.53, 95% CI = 0.26–1.11, p = 0.092) was a protective factor for depressive symptoms in older adults.
Conclusion:
The prevalence of depressive symptoms among older adults is high in Anhui Province, China. Frailty, social frailty, and poor family health are associated with higher prevalence of depressive symptoms in older adults. Public health departments should pay more attention to the construction of mental health protection in the three environmental contexts of individual, family and society to promote healthy aging.
Introduction
As the proportion of older adults in the population increases rapidly, countries around the world are facing the challenge of population aging. According to the seventh national census of China by the end of 2020, the number of older adults aged 60+ in China mainland had reached 264 million, accounting for 18.7% percent of the mainland’s total population (1). It is expected that by 2050, China’s older adult population will reach 400 million, accounting for one-third of the total population, meaning that China will enter the deep aging society by 2050 (2). According to data from the World Health Organization, due to the increase in life expectancy and the decline in the general fertility rate, the proportion of China’s population over 60 years old is expected to reach 28% by 2040 (3). Inevitably, China will soon face the tremendous pressure that diseases related to older adults put on the national healthcare system and families (4).
Older adults are a key group whose health problems need to be solved in the “Healthy China 2030,” which is related to the implementation of the national health strategy and the advancement of the healthy aging process (5). Depressive symptoms are a common mental health problem among older adults, which not only seriously reduces the quality of life and social participation, but also brings additional economic burden to medical and health institutions (6). In 2019, the Chinese government implemented the Healthy China Action Plan (2019–2030), an essential goal of which is to mitigate the rising trend of depression by 2030 (7).
Depressive symptoms are a major global public health problem that not only affects an individuals’ quality of life, but also imposes a high economic burden on society and families as a whole. Depressive symptoms are associated with physical health and cognitive function problems, shortage labor, and greater health care utilization (8). Depression is a common mental disorder affecting approximately 3.5 billion people worldwide (9). In China, the prevalence of depression among Chinese adults is approximately 6.9% (10), and about 40% of people aged more than 60 have suffered from depressive symptoms (11). According to research, approximately 30% of men and 40% of women aged 45 and above experience depressive symptoms (12). Depressive symptoms are considered the second leading cause of disability in China, and their prevalence is increasing rapidly with China’s GDP growth and population aging (13). Depression is the most common psychiatric disorder among older adults, with 8 to 16% of community-dwelling older adults experiencing clinically significant depressive symptoms (14). A meta-analysis showed that the prevalence of depressive symptoms among Chinese older adults was as high as 20.0% (15). The harm of depression in older adults is multifaceted. It may not only increase the risk of stroke but also cause immune system disorders and inflammation (16), unhealthy behaviors (17), reduced medication compliance (18), and the occurrence of hypertension and diabetes (19). The high prevalence of depressive symptoms in older adults has dramatically increased medical expenditures in China (20). Therefore, exploring the influencing factors of depressive symptoms in older adults and reducing their prevalence is crucial for the physical and mental health of older adults and the development of social public health.
As China’s aging population intensifies, the prevalence of frailty among older adults is on the rise. Frailty is defined by as a clinical geriatric syndrome, characterized by diminished strength, endurance and decreased physiological function, which is associated with increased risks of adverse clinical outcomes including falls, disability, hospitalization, mortality, and their prevalence is aggravated by age (21). Mounting prospective cohort studies indicates that frailty is associated with depressive symptoms. For example, the results of a prospective cohort study by Makizako et al. showed that frailty was an independent predictor of depressive symptoms among community-dwelling older people (22). In view of there was a paucity of large-sample cross-sectional studies demonstrating the relationship between frailty and depressive symptoms in older adults. Therefore, we conducted a cross-sectional study to investigate the association between frailty and depressive symptoms in older adults.
In recent years, the concept of “social frailty” has received increasing attention from academic circles. As an important dimension of frailty, social frailty was classically defined as the risk of individuals facing a decline in social functioning, which was characterized by a lack of social resource support sources, weak social networks, and low levels of social participation (23). Social frailty not only affects the process of healthy aging in China, but also poses serious threats to individuals, families, society and healthcare services systems. Studies have found that the prevalence of social frailty among community-dwelling older adults is estimated to be about 20% (24), which was significantly higher than the prevalence of physical frailty of about 10% (25), indicating that social frailty is a more serious social problem. Social frailty could negatively impact physical functioning in older adults (26) and, at the same time, could also lead to depression and disability in older adults (27). A four-year follow-up study found that social frailty was more closely related to depressive symptoms in community-dwelling older adults than physical frailty and cognitive frailty among the components of frailty (28). However, there is insufficient research on the relationship between depressive symptoms and social frailty among older adults in China. Therefore, exploring the association between social frailty and depressive symptoms in older adults could help accelerate the process of active aging and reduce the prevalence of depressive symptoms among older adults in China.
Family health has recently become a prominent focus in the field of modern geriatric medicine. In recent years, “family health” as a relatively new concept, has received more and more attention from scholars (29). On January 2, 2024, the Chinese National Health Commission issued the “Notice on Comprehensively Carrying out the Construction of Healthy Families,” which proposed to improve family health literacy and create a healthy family environment (30). Family systems theory underscores that the family is an organized system in which family members influence each other through their commitment to each other, exchange of information, emotions, and interests (31). Family health is “family-level resources that develop based on each member’s health, communication, abilities, and their interaction with the family’s physical, social, emotional, economic, and medical resources” (32). Family health covers a wide range of health-related social support and family interactions and resources (33), which helps improve individual health literacy and increase the level of healthy behaviors, thereby reducing the risk of disease. A healthy family can promote a sense of belonging among family members (34) and cultivate the ability of family members to take care of each other and assume life responsibilities (35). Family health research can enhance the cohesion and sense of belonging among family members, cultivate the ability of family members to care for each other and fulfill family life responsibilities, and ultimately contribute to the overall development of society (36). We therefore hypothesized that depressive symptoms in older adults would be significantly reduced as the intensity of support from spouses, children, or other family members increases. Therefore, family health can serve as an essential target for health intervention. However, there have been few studies on family health in older adults, and there are no previous studies on the relationship between family health and depressive symptoms in older adults.
As China is about to enter a profoundly aging society, special attention should be paid to the depressive symptoms of older adults. Old age is a more emotionally vulnerable time in a person’ s life. Physical aging in old age inevitably brings about many major losses, which have a significant impact on an individual’ s physical condition, emotions, and social status. Previous findings suggest that older adults are at increased risk for depressive symptoms. Depressive symptoms can take a toll on older adults’ physical and mental health, and the damage can last long or even get worse. There is an urgent need to explore the prevalence of depressive symptoms and related influencing factors in older adults to provide a reference for formulating effective intervention measures. However, to our knowledge, the effects of frailty, social frailty, and family health on depressive symptoms in older adults have not been previously studied. We hypothesize that frailty and social frailty may trigger depressive symptoms, leading to adverse health outcomes. Therefore, the purposes of this study are (1) to investigate the prevalence of depressive symptoms among older adults and (2) to explore the influencing factors of depressive symptoms in older adults.
In this study, we first analyzed the prevalence and sociodemographic characteristics of depressive symptoms among older adults in China. In the second step, we investigated the risk factors and protective factors associated with depressive symptoms in older adults and advocated promoting family health activities as “protective factors.” This study meets the needs of an aging society for the prevention and management of depressive symptoms in older adults. It can further help the government, society, and families develop effective psychological intervention measures to reduce the impact of depressive symptoms on the physical and mental health of older adults. Our findings identify critical elements for preventing and treating depressive symptoms in older adults, which are essential for reducing depressive symptoms and improving mental health in older adults.
Materials and methods
Study design and setting
This was a large-scale cross-sectional study that strictly followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Participants and data collection
Participants were recruited using convenience sampling in Anhui Province, China, between December 2023 and February 2024. Convenience sampling, also known as random sampling and chance sampling, is a non-probability sampling method in which the investigator randomly selects respondents at a specific time and in a particular location in a specific community to match the research topic. In this study, trained medical students from Wannan Medical College in Anhui Province administered a face-to-face questionnaire to each participant using a standardized questionnaire. The training for investigators included the purpose and significance of the investigation, the unified investigation terms, and related precautions that needed to be mastered. Based on this cross-sectional study design, participants aged 60 years and above, without deafness or dementia/neurological or mental illness, and who voluntarily participated in our survey met the criteria for filling out the questionnaire. Participants were completely voluntary, and the participants were informed in detail about the purpose, methods, procedures and confidentiality of the survey data before participating in the cross-sectional survey, and finally signed an electronic informed consent form. If participants no longer wish to cooperate in completing the survey, they may withdraw from the study at any time without any conditions. Participants carefully filled out the questionnaire, and data submission was conducted via a smartphone or tablet by a survey team member. Research team members strictly supervised the online data collection to achieve the desired research objectives. A total of 1,200 subjects were included in this study. After excluding invalid questionnaires, 1,175 valid subjects were finally included for data analysis, with an effective recovery rate of 97.9% (details are shown in Figure 1).
Figure 1
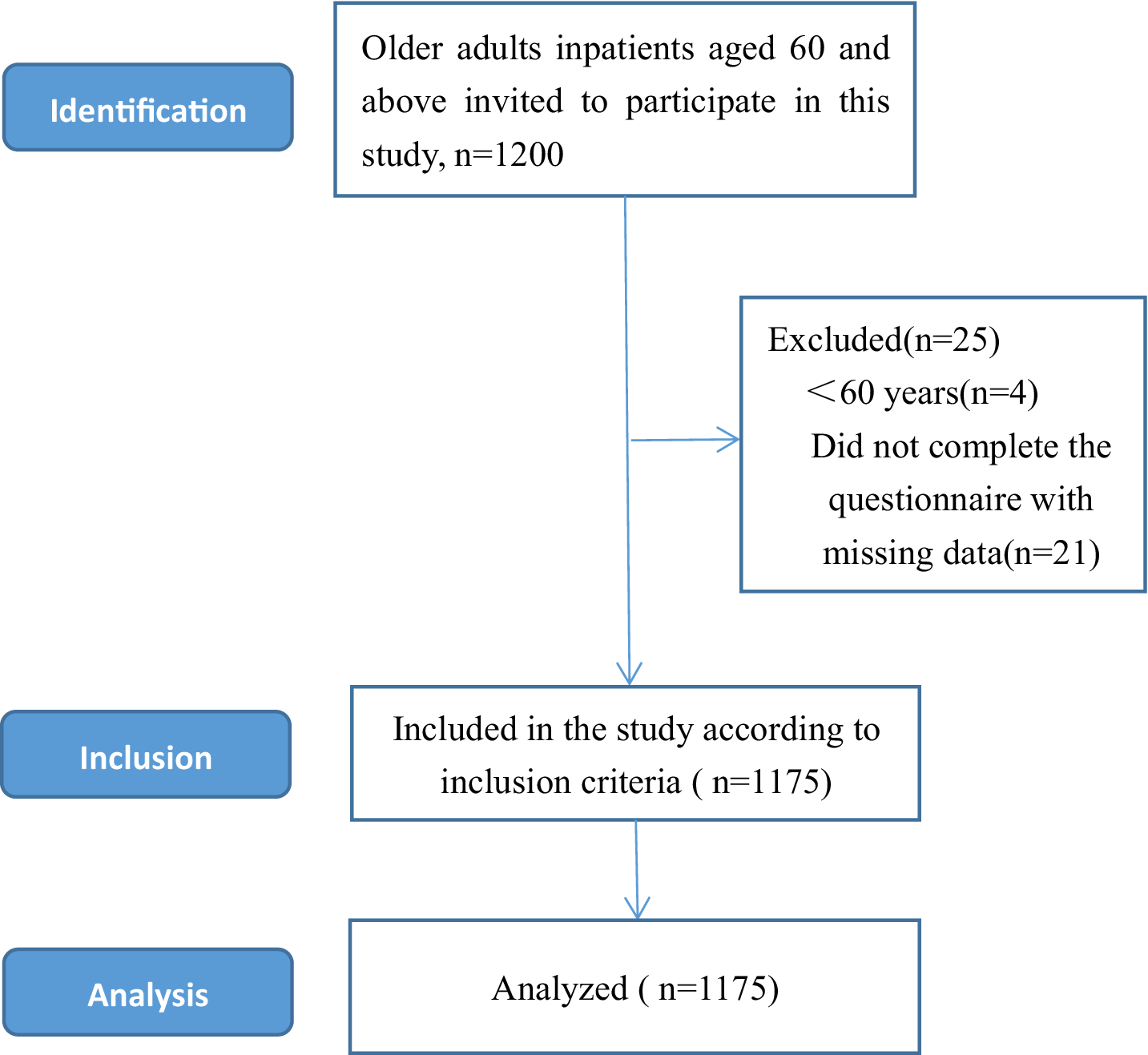
Sample selection process for this cross-sectional study.
Measurements
Demographic questionnaire
We developed the demographic questionnaire based on an extensive literature review and research purposes. The general sociodemographic information of this study includes age, gender, place of residence, education level, marital status, current chronic disease status, current work status, and self-evaluated physical pain status.
Assessment of depression symptoms
Depressive symptoms in older adults were assessed with the Patient Health Questionnaire (PHQ-9) (37). The PHQ-9 is a 9-item depression symptoms self-report instrument that evaluates the frequency of symptoms of depression symptoms in the past 2 weeks. Each of the 9 items was divided into a four-point degrees of the scale (0 = not at all; 1 = several days; 2 = more than half the time; 3 = nearly every day); the PHQ-9 total score range from 0 to 27, with higher scores indicated greater depression symptoms. All items of the PHQ-9 screening scale are consistent with the nine diagnostic criteria for depression in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (37). In our study, a score of <10 was considered as no depressive symptoms, and a score of ≥10 was considered as depressive symptoms (38). In the current study, Cronbach’s alpha was 0.85.
Frailty
Frailty was indicated by fatigue sensation, resistance, free movement descent, coexistence of multiple diseases, weight loss (39). FRAIL scale consists of 5 items, each with “yes” and “no” options. The frailty final score was calculated cumulatively, with a total score of 0–5. Participants were considered “frail” if their total score was 3 or above. With a total score of less than 3 points was obtained, and participants were classified as “non-frail” (40). In the current study, Cronbach’s alpha was 0.83.
Social frailty
Social frailty was defined using the social frailty scale (41) (Help, Participation, Loneliness, Financial, Talk Scale, HALFT)comprising five components: (1) Have you been able to help a friend or family member in the past year? (2)Have you engaged in any social or recreational activities in the past year? (3) Have you felt lonely in the past week? (4) Is the income in the past year sufficient to survive for 1 year? (5) Are there people you chat with every day? Respondents answered each question with “yes” or “no,” the total score was 5 points, and respondents who answered three or more were considered to be in a state of social frailty. In the current study, Cronbach’s alpha was 0.82.
Family health
Participants’ family health was measured utilizing the Family Health Scale-Short Form (FHS-SF) (42). Each item was rated on a Likert scale with scores ranging from1 (strongly disagree) to 5 (strongly agree), with questions 6, 9 and 10 reverse-scored. Points were accumulated and the total score ranges from 1 to 50 points. The higher the score, the higher the levels of healthy family. In this study, participants who scored greater than or equal to 20 on the family health scale were classified as having a healthy family, while those who scored lower than 20 were classified as without healthy family. In the current study, Cronbach’s alpha was 0.82.
Statistical analyses
Data analyses were performed using IBM Statistical Package for Social Science version 26.0 (SPSS Inc., Chicago, IL, United States). Demographic characteristics, depressive symptom scores, family health, frailty, and social frailty were presented as means, standard deviations (SD), numbers, and percentages. Chi-square tests were used to compare differences in categorical variables between depressive symptom groups and non-depressive symptom groups. In addition, logistic regression analysis was used to explore the relationship between depressive symptoms in older adults and general demographic characteristics, family health, and social weakness. The correlation among family health, social weakness and depressive symptoms was evaluated by Pearson’s correlation analysis. The Cronbach’s α coefficient of the scale in this study was 0.892.
Results
Demographic characteristic
A total of 1,175 participants were included in this study. The age of the participants ranged from 60 to 93 years old, with an average age of 71.73 ± 6.4 years old. These1175 participants were divided into four age groups: (1) 60–70 years old, 705 participants; (2) 71–80 years old, 367 participants; (3) 81–90 years old, 87 participants; and (4) >90 years old, 16 participants. 530 (45.1%) were male, and 645 (54.9%) were female. Place of residence had three categories: rural was 513 (43.7%), town was 432 (43.7%) and city was 230(19.6%). Detailed sociodemographic characteristics of participants are presented in Table 1.
Table 1
| Item | Categories | N(%) | Depressive symptoms | No depressive symptoms | χ2/Z-values | p-values |
|---|---|---|---|---|---|---|
| Sex | Men | 530(45.1%) | 188(35.5%) | 342(64.5%) | 0.360 | 0.548 |
| Women | 645(54.9%) | 218(33.8%) | 427(66.2%) | |||
| Place of residence | Rural | 513(43.7%) | 169(32.9%) | 344(67.1%) | 1.056 | 0.590 |
| Town | 432(36.8%) | 154(35.6%) | 278(64.4%) | |||
| City | 230(19.6%) | 83(36.1%) | 147(63.9%) | |||
| Age group | 60-70 years old | 705(60.0%) | 205(29.1%) | 500(70.9%) | 30.026 | <0.001 |
| 71–80 years old | 367(31.2%) | 146(39.8%) | 221(60.2%) | |||
| 81–90 years old | 87(7.4%) | 46(52.9%) | 41(47.1%) | |||
| >90 years old | 16(1.4%) | 9(56.2%) | 7(43.8%) | |||
| Suffering from chronic diseases | No | 667(57.6%) | 205(30.3%) | 472(69.7%) | 12.894 | <0.001 |
| Yes | 498(42.4%) | 201(40.4%) | 297(59.6%) | |||
| Education level | Below elementary school | 409(34.8%) | 147(35.9%) | 262(64.1) | 7.640 | 0.177 |
| Elementary school | 388(33%) | 143(36.9%) | 245(63.1%) | |||
| Junior high school | 170(14.5%) | 46(27.1%) | 124(72.9%) | |||
| High school | 105(8.9%) | 40(38.1%) | 65(61.9%) | |||
| Junior college | 24(2.0%) | 6(25.0%) | 18(75.0%) | |||
| Bachelor and above | 79(6.7%) | 24(30.4%) | 55(69.6%) | |||
| Profession | Worker | 155(13.2%) | 64(41.3%) | 91(58.7%) | 15.014 | 0.091 |
| Farmer | 541(46.0%) | 183(33.8%) | 358(66.2%) | |||
| Employees | 80(6.8%) | 36(45.0%) | 44(55.0%) | |||
| Public employees | 61(5.2%) | 20(32.8%) | 41(67.2%) | |||
| Medical staff | 20(1.7%) | 9(45.0%) | 11(55.0%) | |||
| Self-employed | 56(4.8%) | 17(30.4%) | 39(69.6%) | |||
| Freelancer | 54(4.6%) | 11(20.4%) | 43(79.6%) | |||
| Teacher | 46(3.9%) | 13(28.3%) | 33(71.7%) | |||
| Professional and technical | 9(0.8%) | 4(44.4%) | 5(55.6%) | |||
| Other | 153(13.0%) | 49(32.0) | 104(68.0%) | |||
| Number of hospitalizations in the past year | 0 | 470(40.0%) | 87(18.5%) | 383(81.5%) | 134.505 | <0.001 |
| 1 | 321(27.3%) | 104(32.4%) | 217(67.6%) | |||
| 2 | 202(17.2%) | 106(52.5%) | 96(47.5%) | |||
| ≥3 | 182(15.5%) | 109(59.9%) | 73(40.1%) | |||
| Marital Status | Single | 50(4.3%) | 19(38.0%) | 31(62.0%) | 44.599 | <0.001 |
| Married | 849(72.3%) | 252(29.7%) | 597(70.3%) | |||
| Divorced | 36(3.1%) | 25(69.4%) | 11(30.6%) | |||
| Widowed | 217(18.5%) | 96(44.2%) | 121(55.8%) | |||
| Other | 23(2.0%) | 14(60.9%) | 9(39.1%) | |||
| Status of physical pain | No physical pain | 410(34.9%) | 77(18.8%) | 333(81.2%) | 129.620 | <0.001 |
| Mild physical pain | 577(49.1%) | 207(35.9%) | 370(64.1%) | |||
| Moderate physical pain | 147(12.5%) | 88(59.9%) | 59(40.1%) | |||
| Severe pain | 41(3.5%) | 34(82.9%) | 7(17.1%) | |||
| Type of employment | Manual workers | 725(61.7%) | 249(34.3%) | 476(65.7%) | 0.553 | 0.758 |
| Both manual and mental workers | 333(28.3%) | 113(33.9%) | 220(66.1%) | |||
| Mental workers | 117(10%) | 44(37.6%) | 73(62.4%) | |||
| Frailty | No | 947(80.6%) | 240(25.3%) | 707(74.7%) | 183.061 | <0.001 |
| Yes | 288(19.4%) | 166(72.8%) | 62(27.2%) | |||
| Social frailty | No | 991(84.3%) | 280(28.3%) | 711(71.7%) | 111.032 | <0.001 |
| Yes | 184(15.7%) | 126(68.5%) | 58(31.5%) |
Sociodemographic characteristics of the participants (N = 1,175).
Factors associated with depressive symptoms in univariate analyses
In this study, the prevalence of depressive symptoms among older adults was 34.6% (406/1175). There were significant differences between age groups, chronic disease status, number of hospitalizations in the last 1 years, physical pain status, marital status, and medical insurance type (p < 0.01; Table 1).
Correlations between frailty, social frailty, family health, and depressive symptoms
As shown in Figure 1, there was a significant positive correlation between frailty in older adults, social frailty and depressive symptoms (p < 0.01). In contrast, family health was significantly negatively correlated with depressive symptoms (p < 0.01).
Binary analysis factors associated with depressive symptoms
The influencing factors of depressive symptoms in older adults are shown in Table 2 and Figure 2. Depressive symptoms were more severe in older adults with mild body pain, moderate body pain, and severe body pain (OR = 1.589, 95% CI 1.125–2.243; OR = 2.335, 95% CI 1.437–3.794; OR = 4.020, 95% CI 1.564–10.337). The number of hospitalizations in the past year is a risk factor for depressive symptoms in older adults; older people who have been hospitalized once, twice and more than three times have a significantly increased risk of depressive symptoms, which was 1.885, 2.887 and 3.627 times higher than healthy people, respectively. The more severe the frailty in older adults, the higher the depressive symptom score (OR = 4.231, 95% CI 2.946–6.076). Social frailty in older adults increased the risk of depressive symptoms (OR = 2.874, 95% CI 1.942–4.253). Family health was a protective factor for depressive symptoms in older adults (OR = 2.867, 95% CI 2.134–3.851; Figure 3).
Table 2
| Characteristics | B | S.E. | Wald | p | OR | (95%CI) |
|---|---|---|---|---|---|---|
| Sociodemographic | ||||||
| Status of body pain | 17.079 | 0.001 | ||||
| Mild pain | 0.463 | 0.176 | 6.911 | 0.009 | 1.589 | 1.125–2.243 |
| Moderate pain | 0.848 | 0.248 | 11.717 | 0.001 | 2.335 | 1.437–3.794 |
| Severe physical pain | 1.391 | 0.482 | 8.338 | 0.004 | 4.020 | 1.564–10.337 |
| Number of hospitalizations in the past year | 40.969 | <0.001 | ||||
| 1 | 0.634 | 0.192 | 10.931 | 0.001 | 1.885 | 1.295–2.746 |
| 2 | 1.060 | 0.215 | 24.300 | <0.001 | 2.887 | 1.894–4.400 |
| ≥3 | 1.289 | 0.225 | 32.887 | <0.001 | 3.627 | 2.335–5.634 |
| Status of family health | −1.053 | 0.151 | 48.942 | <0.001 | 0.349 | 0.260–0.469 |
| Status of frailty | 1.442 | 0.185 | 60.992 | <0.001 | 4.231 | 2.946–6.076 |
| Status of social frailty | 1.056 | 0.200 | 27.851 | <0.001 | 2.874 | 1.942–4.253 |
| Constant | −2.665 | 0.190 | 197.349 | <0.001 | 0.070 | |
Binary logistic regression analysis of factors associated with depressive symptoms.
Figure 2
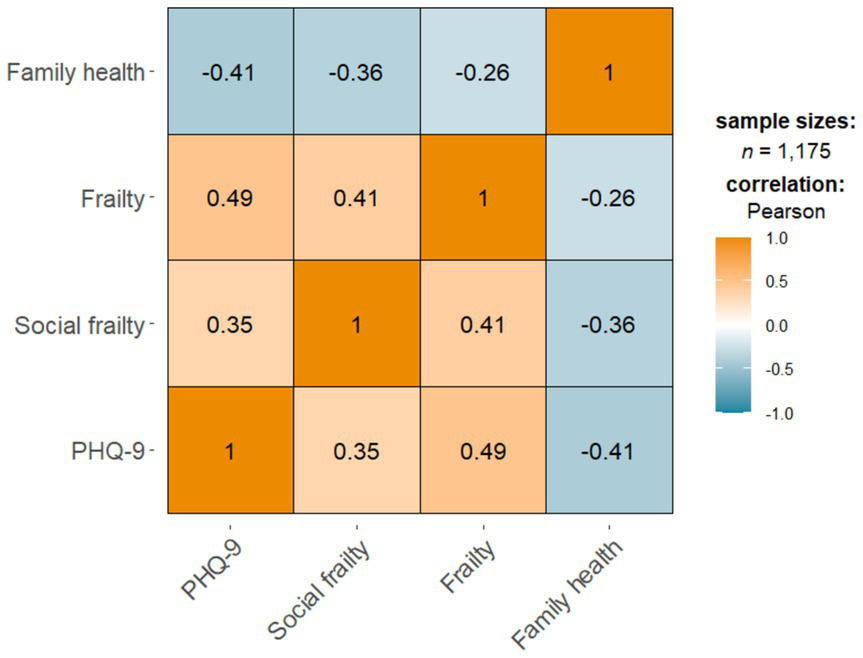
Correlations between frailty, social frailty, family health, and depressive symptoms.
Figure 3
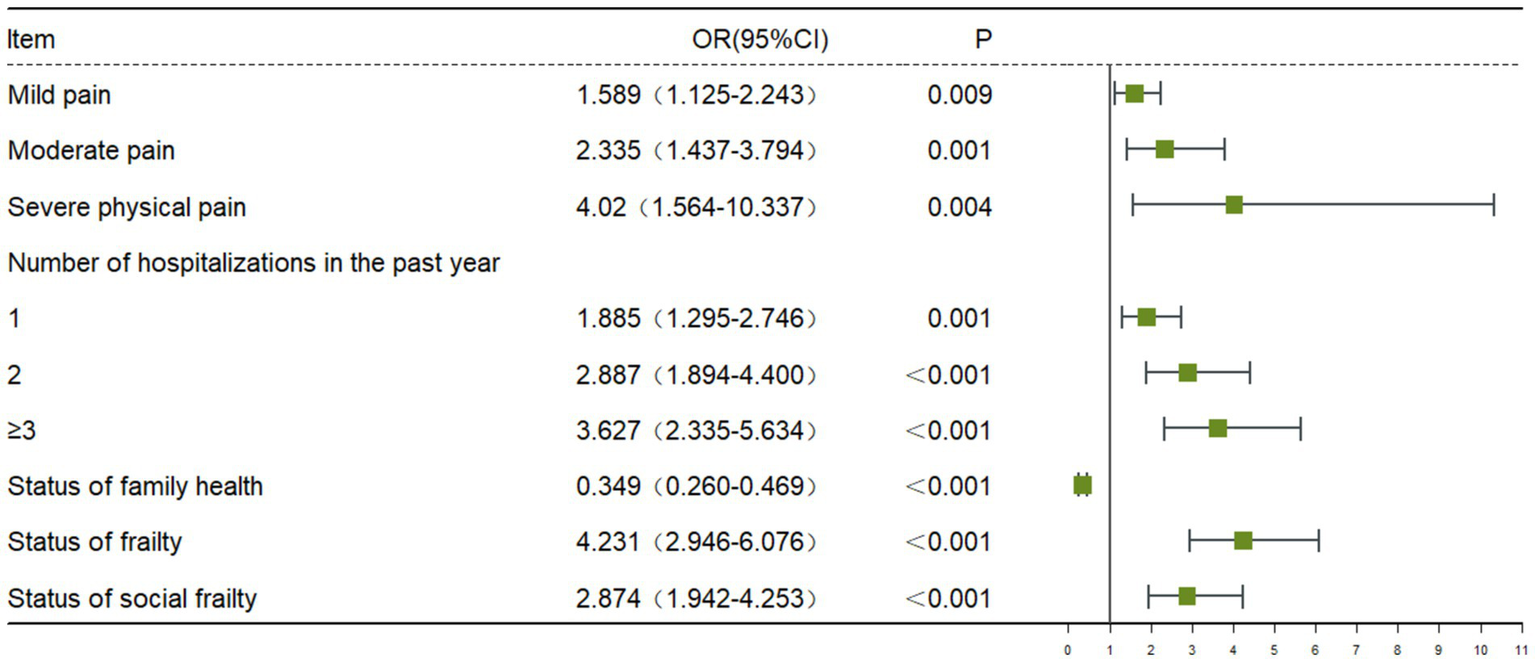
Binary logistic regression analysis of factors associated with depressive symptoms.
Discussion
In recent years, with the acceleration of population aging in China, the prevalence of depressive symptoms in older adults has continued to increase, which has attracted widespread attention from more and more scholars. The purpose of this study was to explore the prevalence and influencing factors of depressive symptoms among older adults in China. In this cross-sectional study, we explored the prevalence of depressive symptoms and risk factors for depressive symptoms in 1175 older adults. The results showed that physical pain, hospitalizations in the past year, frailty, social frailty and poor family health were more likely to cause depressive symptoms in older adults than other factors. The research results provide a certain theoretical basis for the screening, prevention and psychological intervention of depressive symptoms in older adults.
In this cross-sectional study, we found that the prevalence of depressive symptoms with PHQ-9 total score ≥ 10 among Chinese older adults was 34.6%. The findings are consistent with some previous studies, including Zhou L et al. (43), who reported a prevalence of depressive symptoms of 35.19% among 4,771 older people in China. The prevalence of depressive symptoms among the older adults in this study was higher than the 20.36% prevalence rate of depressive symptoms among the community-dwelling older adults in Hainan, China (44), and the 16.2% prevalence rate of depressive symptoms among a Longitudinal Cohort Study (45), but lower than the reported 53% prevalence rate of depressive symptoms among the rural older adults in Anhui, China (46). The results of this study, like previous similar studies, suggesting that the depressive symptoms in older adults in China are serious, and the burden of depressive symptoms had been and would be gradually increase, placing a heavy burden on medical and health institutions. In addition, Yan Yu meng et al. used CHARLS data in 2015 and 2018 to study the prevalence of depressive symptoms among older adults in China. The results showed that the prevalence of depressive symptoms among older adults in China increased from 33.8% in 2015 to 50.6% in 2018 (47). Our results show that the prevalence of depressive symptoms among older adults in Anhui Province was different from that reported in other studies, which may be due to different assessment tools and survey times among the populations involved in studies conducted in different regions. It is worth mentioning that the PHQ-9 has been proven to be a reliable and valid screening tool for depressive symptoms, and it has been widely used in relevant cross-sectional studies on depressive symptoms among older adults in China. Therefore, the prevalence of depressive symptoms in older adults measured by the PHQ-9 still has a certain degree of reliability in this study.
Consistent with previous studies, our present study results demonstrated that frailty was significantly positively associated with the occurrence of depressive symptoms among older adults in China (48, 49). Previous a Mendelian randomization studyhave shown that a strong bidirectional relationship between depressive symptoms and frailty among older adults (48). Several potential reasons could explain the positive association between frailty and depressive symptoms in older adults. ① In epidemiological studies, frail older adults are often affected by higher levels of chronic, mild inflammatory markers, especially interleukin-6 (IL-6), which serves as a biomarker of depressive symptoms in older adults substances are thought to be more susceptible to geriatric depression (50). ② Frailty is a clinical syndrome in older adults characterized by weakness, slow gait, inactivity, exhaustion, and weight loss. As time goes on, older adults may have a sense of despair, worthlessness, and emptiness due to limited physiological functions, and may no longer be interested in things they were originally interested in, which may lead to symptoms of depression to a certain extent (51). We concluded that participants with frailty was at higher risk for depressive symptoms. Therefore, it is necessary to conduct regular frailty screening for older adults, and provide timely psychological comfort and psychological counseling to the frail older adults.
In our study, social frailty scores were positively correlated with depressive symptom scores, and these data suggest that social frailty might be a risk factor for depressive symptoms. The results of binary logistic regression analysis showed that participants social frailty were 2.874 times more likely to experience depressive symptoms than non-socially frailty participants. When older adults entered the second half of their lives, they tend to reduce their social participation activities to varying degrees due to age, chronic illness and other reasons. The dramatic change in social roles may result in less interaction with people, which may further cause some degree of mental health problems in older adults (52). According to the stress-buffering hypothesis, social activities may significantly reduce adverse psychological effects on individuals’ mental health through their buffering effect on stress levels (53). In addition, research have shown that group psychological support, friend-making activities, and social support interventions could have a positive impact on the mental health of older adults and help improve their social frailty of older adults (23). Therefore, it is recommended that mental health staff pay more attention to and dynamically assess the social frailty and depressive symptoms of older adults, enrich the social activities of older adults, and play an active role in social participation.
Interestingly, our findings showed that older adults with healthy families were 0.677 times less likely to experience depressive symptoms. In this study, family health was found to be a protective factor for depressive symptoms in older adults, indicating that family health plays an important role in improving mental health in older adults, this means that poor family health may lead to significant increases in depressive symptoms in older adults. Family is the essential environment for individual life. In traditional Chinese culture, family means “shelter” and is the primary basis for solving psychological problems (54). Therefore, family health is considered a health unit involving each family member and the entire family system (55). According to family systems theory, families provide a strong emotional foundation for maintaining supportive relationships among members, which helps promote psychological well-being (56). The family is both a resource and a priority group that plays a very critical preventive and therapeutic role throughout the life course of its members’ life course (57). Family health emphasizes health-related elements and closely links personal health with social health, which can enhance the family’s ability to obtain external resources. The study found that family health was significantly negatively correlated with frailty among Chinese older adults. Improving family health can increase individual health literacy and reverse frailty (29). Previous research has shown that the role of family is critical in predicting better health-related quality of life in older adults (58). The existence of family is an essential source of social support for older adults as they accept the aging process, and family health helps motivate older adults to participate in daily activities and improve self-esteem (59).
This study’s results revealed that physical pain is a risk factor for depressive symptoms in older adults, which is consistent with Lu L’s previous study (60). Possible explanations for this finding include: First, physical pain directly contributes to negative emotions and negative experiences in older adults. Secondly, chronic pain generally accompanies the occurrence of chronic diseases, which can lead to adverse consequences such as limited physical activity and high disability rates. The worry about adverse consequences can lead to an increase in depressive symptoms in older adults (61).
The results of this study indicate that the prevalence of depressive symptoms in older adults increases with the number of hospitalizations. One possible explanation for this research result may be related to chronic disease and its complications. Older adults who are hospitalized more often are more likely to have more and more severe chronic conditions, and these chronic conditions often carry serious associated complications with age. Increased hospitalizations may lead to increased frailty. In addition, older adult’s excessive worries about their physical health and the pressure of medical expenses would have a more profound negative impact on their mental health status, which may further induce depressive symptoms in older adults (62). Therefore, for older people with acute and chronic diseases, physical health status is one of the risk factors for depressive symptoms. The prevalence of depression in older adults might be further reduced by improving their health.
This study provides a specific scientific basis for the improvement of the theoretical framework related to depression in the older adults, the optimization of intervention strategies, and the formulation of public policies. This not only promotes cutting-edge research on older adult’s mental health but also provides specific guidance for achieving healthy aging.
Strengths and limitations
Our study has strengths to this study. The PHQ-9 scale is well-known for being a simple and effective test for measuring depressive symptoms. However, some limitations of the current study cannot be ignored. First, cross-sectional designs cannot infer causal relationships among factors influencing depressive symptoms in older adults. Future large-sample multicenter prospective cohort studies are necessary to validate causal associations. Second, the PHQ-9 was designed to measure depressive symptoms and was not a diagnostic tool for depression. Third, self-reported scales may introduce information bias from participants and investigators, and subsequent cross-sectional studies need to introduce more objective measurement tools.
Conclusion
Our data showed a high prevalence of depressive symptoms among Chinese older adults. Physical pain, number of hospitalizations in the past year, frailty, and social frailty were found to be significant predictors of depressive symptoms. At the same time, family health was a protective factor for depressive symptoms. These results indicate that it is critical to proactively and effectively identify mental health conditions in older adults. Our study contributes to the early identification and management of depressive symptoms in older adults, which may help prevent the possible harmful effects of depressive symptoms on the physical and mental health of older adults. Promote the health and well-being of the older adults and actively respond to the country’s strategic requirements for dealing with population aging.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Nursing Department of the First Affiliated Hospital (Yijishan Hospital) of Wannan Medical College (WNYXYYJSYYHLB 2024-02-01). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XH: Funding acquisition, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. HL: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. QL: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. TY: Investigation, Writing – original draft, Writing – review & editing. MD: Investigation, Writing – original draft, Writing – review & editing. YL: Investigation, Writing – original draft, Writing – review & editing. JM: Investigation, Writing – original draft, Writing – review & editing. GM: Project administration, Writing – original draft, Writing – review & editing. XT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Writing – original draft, Writing – review & editing. BX: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. MZ: Conceptualization, Formal Analysis, Funding acquisition, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by Anhui Provincial University Scientific Research Key Project (2023AH051733, 2023AH051730), the National Natural Science Fund of China (32371112), Anhui Province Educational Science Research Project (JK23173), the Key Laboratory of Philosophy and Social Science of Anhui Province on Adolescent Mental Health and Crisis Intelligence Intervention(SYS2023B09), the Industry-University Cooperation Collaborative Education Project of the Ministry of Education (220905875062412), the Anhui Provincial College Outstanding Young Talents Support Program(gxyq2022045), the Teaching Quality and teaching reform project of Wannan Medical College (2020jyxm58), the School project of the University Student Mental Health Education Research Center of Wannan Medical College (SJD202110), the Key Project Research Fund of Wannan Medical College (WK2023SZD03), and the Teaching Reform Project of Wannan Medical College (2021zybz06).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
National Bureau of Statistics (2021). Main data of the seventh national census EB/OL. Available at: http://www.stats.gov.cn/tjsj/zxfb/202105/t20210510_1817176.html (Accessed on 2024-01-11)
2.
Qiu QW Li J Li JY Xu Y . Built form and depression among the Chinese rural elderly: a cross-sectional study. BMJ Open. (2020) 10:e038572. doi: 10.1136/bmjopen-2020-038572
3.
Bao J Zhou L Liu G Tang J Lu X Cheng C et al . Current state of care for the elderly in China in the context of an aging population. Biosci Trends. (2022) 16:107–18. doi: 10.5582/bst.2022.01068
4.
Chen X Giles J Yao Y Yip W Meng Q Berkman L et al . The path to healthy ageing in China: a Peking University-lancet commission. Lancet. (2022) 400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X
5.
Tan X Zhang Y Shao H . Healthy China 2030, a breakthrough for improving health. Glob Health Promot. (2019) 26:96–9. doi: 10.1177/1757975917743533
6.
Wu J Qiu L Xiong W Shen Y Li J Wu J et al . COVID-19 anxiety and related factors amid adjusted epidemic prevention policies: a cross-sectional study on patients with late-life depression in China. BMJ Open. (2023) 13:e072725. doi: 10.1136/bmjopen-2023-072725
7.
NHC China . The healthy China action plan (2019–2030). Plan dev div. (2019). Available at:http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm (accessed June 26, 2022).
8.
Segel-Karpas D Shrira A Cohn-Schwartz E Bodner E . Daily fluctuations in subjective age and depressive symptoms: the roles of attitudes to ageing and chronological age. Eur J Ageing. (2022) 19:741–51. doi: 10.1007/s10433-021-00681-z
9.
Zhao X Ma J Wu S Chi I Bai Z . Light therapy for older patients with non-seasonal depression: a systematic review and meta-analysis. J Affect Disord. (2018) 232:291–9. doi: 10.1016/j.jad.2018.02.041
10.
Huang Y Wang Y Wang H Liu Z Yu X Yan J et al . Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. (2019) 6:211–24. doi: 10.1016/S2215-0366(18)30511-X
11.
Ni Y Tein JY Zhang M Yang Y Wu G . Changes in depression among older adults in China: a latent transition analysis. J Affect Disord. (2017) 209:3–9. doi: 10.1016/j.jad.2016.11.004
12.
Lei X Sun X Strauss J Zhang P Zhao Y . Depressive symptoms and SES among the mid-aged and elderly in China: evidence from the China health and retirement longitudinal study national baseline. Soc Sci Med. (1982) 120:224–32. doi: 10.1016/j.socscimed.2014.09.028
13.
Zhang X Li G Shi C Sun Y . Associations of sleep duration, daytime napping, and snoring with depression in rural China: a cross-sectional study. BMC Public Health. (2023) 23:1530. doi: 10.1186/s12889-023-16479-w
14.
Taylor WD . Clinical practice. Depression in the elderly. N Engl J Med. (2014) 371:1228–36. doi: 10.1056/NEJMcp1402180
15.
Tang T Jiang J Tang X . Prevalence of depressive symptoms among older adults in mainland China: a systematic review and meta-analysis. J Affect Disord. (2021) 293:379–90. doi: 10.1016/j.jad.2021.06.050
16.
Miller AH Raison CL . The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. (2016) 16:22–34. doi: 10.1038/nri.2015.5
17.
Holma IA Holma KM Melartin TK Ketokivi M Isometsä ET . Depression and smoking: a 5-year prospective study of patients with major depressive disorder. Depress Anxiety. (2013) 30:580–8. doi: 10.1002/da.22108
18.
Srivastava P Butler J Shroyer AL Lacey M Parikh PB . Impact of depressive disorder on access and quality of Care in Veterans with Prevalent Cardiovascular Disease. Am J Cardiol. (2018) 121:1629–33. doi: 10.1016/j.amjcard.2018.02.048
19.
Herrmann-Lingen C Meyer T Bosbach A Chavanon ML Hassoun L Edelmann F et al . Cross-sectional and longitudinal associations of systolic blood pressure with quality of life and depressive mood in older adults with cardiovascular risk factors: results from the observational DIAST-CHF study. Psychosom Med. (2018) 80:468–74. doi: 10.1097/PSY.0000000000000591
20.
Sun X Zhou M Huang L Nuse B . Depressive costs: medical expenditures on depression and depressive symptoms among rural elderly in China. Public Health. (2020) 181:141–50. doi: 10.1016/j.puhe.2019.12.011
21.
Rosko AE Wall S Baiocchi R Benson DM Brammer JE Byrd JC et al . Aging phenotypes and restoring functional deficits in older adults with hematologic malignancy. J Natl Compr Cancer Netw. (2021) 19:1027–36. doi: 10.6004/jnccn.2020.7686
22.
Makizako H Shimada H Doi T Yoshida D Anan Y Tsutsumimoto K et al . Physical frailty predicts incident depressive symptoms in elderly people: prospective findings from the Obu study of health promotion for the elderly. J Am Med Dir Assoc. (2015) 16:194–9. doi: 10.1016/j.jamda.2014.08.017
23.
Li Z Gu J Li P Hu J Wang S Wang P et al . The relationship between social frailty and loneliness in community-dwelling older adults: a cross-sectional study. BMC Geriatr. (2024) 24:73. doi: 10.1186/s12877-024-04666-2
24.
Yu S Wang J Zeng L Yang P Tang P Su S . The prevalence of social frailty among older adults: a systematic review and meta-analysis. Geriatr Nurs. (2023) 49:101–8. doi: 10.1016/j.gerinurse.2022.11.009
25.
Yamada M Arai H . Understanding social frailty. Arch Gerontol Geriatr. (2023) 115:105123. doi: 10.1016/j.archger.2023.105123
26.
Tsutsumimoto K Doi T Makizako H Hotta R Nakakubo S Makino K et al . Association of social frailty with both cognitive and physical deficits among older people. J Am Med Dir Assoc. (2017) 18:603–7. doi: 10.1016/j.jamda.2017.02.004
27.
Kume Y Kodama A Takahashi T Lee S Makizako H Ono T et al . Social frailty is independently associated with geriatric depression among older adults living in northern Japan: a cross-sectional study of ORANGE registry. Geriatr Gerontol Int. (2022) 22:145–51. doi: 10.1111/ggi.14330
28.
Tsutsumimoto K Doi T Makizako H Hotta R Nakakubo S Kim M et al . Social frailty has a stronger impact on the onset of depressive symptoms than physical frailty or cognitive impairment: a 4-year follow-up longitudinal cohort study. J Am Med Dir Assoc. (2018) 19:504–10. doi: 10.1016/j.jamda.2018.02.008
29.
Li H Wu Y Bai Z Xu X Su D Chen J et al . The association between family health and frailty with the mediation role of health literacy and health behavior among older adults in China: Nationwide cross-sectional study. JMIR Public Health Surveill. (2023) 9:e44486. doi: 10.2196/44486
30.
State Council of the People’s Republic of China . Notice on comprehensively carrying out the construction of healthy families[EB/OL]. (2024). Available at: https://www.gov.cn/zhengce/zhengceku/202401/content_6927249.htm (Accessed November 03, 2024).
31.
Rothbaum F Rosen K Ujiie T Uchida N . Family systems theory, attachment theory, and culture. Fam Process. (2002) 41:328–50. doi: 10.1111/j.1545-5300.2002.41305.x
32.
Weiss-Laxer NS Crandall A Okano L Riley AW . Building a Foundation for Family Health Measurement in National Surveys: a modified Delphi expert process. Matern Child Health J. (2020) 24:259–66. doi: 10.1007/s10995-019-02870-w
33.
Güney E Karataş Okyay E Uçar T . Families’ health behavior: validity and reliability of the Turkish version of the family health climate scale. Soc Work Public Health. (2021) 36:707–22. doi: 10.1080/19371918.2021.1948484
34.
Kim W Kreps GL Shin CN . The role of social support and social networks in health information-seeking behavior among Korean Americans: a qualitative study. Int J Equity Health. (2015) 14:40. doi: 10.1186/s12939-015-0169-8
35.
Hansen L Rosenkranz SJ Mularski RA Leo MC . Family perspectives on overall Care in the Intensive Care Unit. Nurs Res. (2016) 65:446–54. doi: 10.1097/NNR.0000000000000179
36.
Aslanturk H Mavili A . The sense of family belonging in university students from a single parent family compared with those from a two-biological-parent family. Curr Psychol. (2020) 39:2026–39. doi: 10.1007/s12144-020-00725-0
37.
Kroenke K Spitzer RL Williams JB . The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
38.
Manea L Gilbody S McMillan D . A diagnostic meta-analysis of the patient health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry. (2015) 37:67–75. doi: 10.1016/j.genhosppsych.2014.09.009
39.
Chen X Liu M Ma Q Liu X Peng X He C . Mediating effects of depression on sleep disturbance and frailty in older adult type 2 diabetes patients in the community. Front Public Health. (2023) 11:1237470. doi: 10.3389/fpubh.2023.1237470
40.
Dong L Qiao X Tian X Liu N Jin Y Si H et al . Cross-cultural adaptation and validation of the FRAIL scale in Chinese community-dwelling older adults. J Am Med Dir Assoc. (2018) 19:12–7. doi: 10.1016/j.jamda.2017.06.011
41.
Ma L Sun F Tang Z . Social frailty is associated with physical functioning, cognition, and depression, and predicts mortality. J Nutr Health Aging. (2018) 22:989–95. doi: 10.1007/s12603-018-1054-0
42.
Wang F Wu Y Sun X Wang D Ming WK Sun X et al . Reliability and validity of the Chinese version of a short form of the family health scale. BMC Prim Care. (2022) 23:108. doi: 10.1186/s12875-022-01702-1
43.
Zhou L Ma X Wang W . Relationship between cognitive performance and depressive symptoms in Chinese older adults: the China health and retirement longitudinal study (CHARLS). J Affect Disord. (2021) 281:454–8. doi: 10.1016/j.jad.2020.12.059
44.
Sun Z Lin J Zhang Y Yao Y Huang Z Zhao Y et al . Association between immunoglobulin a and depression in Chinese older adults: findings from a cross-sectional study. Immun Ageing. (2022) 19:21. doi: 10.1186/s12979-022-00283-y
45.
Han T Zhang L Jiang W Wang L . Persistent depressive symptoms and the changes in serum cystatin C levels in the elderly: a longitudinal cohort study. Front Psychol. (2022) 13:917082. doi: 10.3389/fpsyt.2022.917082
46.
Rong J Chen G Wang X Ge Y Meng N Xie T et al . Correlation between depressive symptoms and quality of life, and associated factors for depressive symptoms among rural elderly in Anhui. China Clin Interv Aging. (2019) 14:1901–10. doi: 10.2147/CIA.S225141
47.
Frontiers Production Office . Erratum: physical function, ADL, and depressive symptoms in Chinese elderly: evidence from the CHARLS. Front Public Health. (2023) 11:1241226. doi: 10.3389/fpubh.2023.1241226
48.
Zhu J Zhou D Nie Y Wang J Yang Y Chen D et al . Assessment of the bidirectional causal association between frailty and depression: a Mendelian randomization study. J Cachexia Sarcopenia Muscle. (2023) 14:2327–34. doi: 10.1002/jcsm.13319
49.
Yuan Y Peng C Burr JA Lapane KL . Frailty, cognitive impairment, and depressive symptoms in Chinese older adults: an eight-year multi-trajectory analysis. BMC Geriatr. (2023) 23:843. doi: 10.1186/s12877-023-04554-1
50.
Xu Y Wang M Chen D Jiang X Xiong Z . Inflammatory biomarkers in older adults with frailty: a systematic review and meta-analysis of cross-sectional studies. Aging Clin Exp Res. (2022) 34:971–87. doi: 10.1007/s40520-021-02022-7
51.
Sang N Liu RC Zhang MH Lu ZX Wu ZG Zhang MY et al . Changes in frailty and depressive symptoms among middle-aged and older Chinese people: a nationwide cohort study. BMC Public Health. (2024) 24:301. doi: 10.1186/s12889-024-17824-3
52.
McGinty EE Presskreischer R Han H Barry CL . Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. (2020) 324:93–4. doi: 10.1001/jama.2020.9740
53.
Cohen S Wills TA . Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
54.
Fangmin G Pei Y Yibo W . The impact of media use behavior on adolescent depression—the chain mediating role of family health and self-efficacy. J J Jishou University (Soc Sci Edition). (2023) 44:124–36. doi: 10.13438/j.cnki.jdxb.2023.06.011
55.
Denham SA . Familial research reveals new practice model. Holist Nurs Pract. (2003) 17:143–51. doi: 10.1097/00004650-200305000-00005
56.
Nabayinda J Kizito S Ssentumbwe V Namatovu P Sensoy Bahar O Damulira C et al . The relationship between family cohesion and depression among school-going children with elevated symptoms of behavioral challenges in southern Uganda. J Adolesc Health. (2023) 72:S11–7. doi: 10.1016/j.jadohealth.2022.12.016
57.
Barnes MD Hanson CL Novilla LB Magnusson BM Crandall AC Bradford G . Family-centered health promotion: perspectives for engaging families and achieving better health outcomes. Inquiry. (2020) 57:46958020923537. doi: 10.1177/0046958020923537
58.
Abdala GA Kimura M Duarte YA Lebrão ML dos Santos B . Religiosidade e qualidade de vidarelacionada à saúde do idoso religiousness and health-related quality of life of older adults. Rev Saude Publica. (2015) 49:55. doi: 10.1590/s0034-8910.2015049005416
59.
Andrade JM Drumond Andrade FC de Oliveira Duarte YA Bof de Andrade F . Association between frailty and family functionality on health-related quality of life in older adults. Qual Life Res. (2020) 29:1665–74. doi: 10.1007/s11136-020-02433-5
60.
Lu L Shen H Tan L Huang Q Chen Q Liang M et al . Prevalence and factors associated with anxiety and depression among community-dwelling older adults in Hunan, China: a cross-sectional study. BMC Psychiatry. (2023) 23:107. doi: 10.1186/s12888-023-04583-5
61.
Bai J Cheng C . Anxiety, depression, chronic pain, and quality of life among older adults in rural China: an observational, cross-sectional, multi-center study. J Community Health Nurs. (2022) 39:202–12. doi: 10.1080/07370016.2022.2077072
62.
Wang Q Song D Lin Q Tao A Zhang Y Li X et al . The critical role of physical frailty and function on depressive symptoms among community-dwelling older adults in China: a cross-sectional study. Front Psychol. (2023) 14:1134427. doi: 10.3389/fpsyt.2023.1134427
Summary
Keywords
depressive symptoms, prevalence, risk factors, older adults, China
Citation
Hu X, Liu H, Liu Q, Yuan T, Duan M, Luo Y, Min J, Mei G, Tao X, Xuan B and Zhang M (2024) Depressive symptoms and their influencing factors among older adults in China: a cross-sectional study. Front. Public Health 12:1423391. doi: 10.3389/fpubh.2024.1423391
Received
25 April 2024
Accepted
29 October 2024
Published
15 November 2024
Volume
12 - 2024
Edited by
Mika Venojärvi, University of Eastern Finland, Finland
Reviewed by
María Antonia Parra Rizo, Miguel Hernández University of Elche, Spain
Gabriel Obukohwo Ivbijaro, NOVA University of Lisbon, Portugal
Updates
Copyright
© 2024 Hu, Liu, Liu, Yuan, Duan, Luo, Min, Mei, Tao, Xuan and Zhang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiubin Tao, 1325609568@qq.comBin Xuan, xuanbin@ahnu.edu.cnMing Zhang, wnyxyzhangming@foxmail.com
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.