- 1Department of Health Education and Health Promotion, School of Health, Social Development and Health Promotion Research Center, Gonabad University of Medical Sciences, Gonabad, Iran
- 2Student Research Committee, Gonabad University of Medical Sciences, Gonabad, Iran
- 3Neonatal and Children's Research Center, Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran
- 4Social Development and Health Promotion Research Center, Gonabad University of Medical Sciences, Gonabad, Iran
- 5Department of Clinical Psychology, Islamic Azad University, Birjand, Iran
- 6Social Determinants of Health Research Center, Gonabad University of Medical Sciences, Gonabad, Iran
Background: This study was conducted to measure depression literacy (D-Lit) and mental health literacy (MHL) and to investigate their relationship with psychological status and quality of life among Iranian patients with type 2 diabetes mellitus (T2DM).
Methods: This cross-sectional study was conducted in 2021 among 400 patients with T2DM in Iran. Samples were selected using proportional stratified sampling. Data collection tools comprised a demographic questionnaire, measures of MHL and D-Lit, the diabetes quality of life (DQOL) scale, and the DASS-21. After confirming the normality of the data using the Kolmogorov-Smirnov test, parametric statistical tests (such as one-way ANOVA, independent samples t-test, and Chi-Square) were used to investigate the relationship between the variables using SPSS v22 software. The results of continuous quantitative data are reported in the form of means and standard deviations, and qualitative data are reported in the form of absolute and relative frequencies.
Results: In this study, 10.25% of the participants (n = 41) had severe depression, while 36.75% (n = 147) experienced severe anxiety. The mean (standard deviation) of MHL was 80.92 (9.16) from 130 points. Of the participants, only 1.7% (n = 7) did not answer any questions correctly on the D-lit scale, and only 5.8% (n = 23) were able to answer 15 questions or more correctly on the D-lit. MHL had a significant negative correlation with depression (r = −0.236), anxiety (r = −0.243), and stress (r = −0.155) (P < 0.001). There was a positive and significant correlation between MHL and D-Lit (r = 0.186) (P < 0.001). D-Lit had a significant negative correlation with depression (r = −0.192), anxiety (r = −0.238), and stress (r = −0.156) (P < 0.001). There was a positive and significant correlation between the ability to recognize disorders (r = 0.163), knowledge of self-treatment (r = 0.154), and DQOL (P < 0.001). Depression (r = −0.251), anxiety (r = −0.257), and stress (r = −0.203) had a significant negative correlation with DQOL (P < 0.001).
Conclusion: MHL and D-Lit levels were found to be inadequate in patients with T2DM. These low levels of MHL and D-Lit among patients with T2DM were associated with higher levels of anxiety, depression, and stress, as well as a lower quality of life. Therefore, designing and implementing preventive programs to improve the mental health of patients with T2DM can help prevent mental disorders and ultimately improve their quality of life.
Background
Type 2 diabetes mellitus (T2DM) is a common chronic and serious disease that threatens life, causes complications and disabilities, increases the cost of living, and reduces life expectancy (1, 2). The prevalence of global diabetes in adults is approximately 10.5% (536.6 million) and is estimated to increase in 2045 to 12.2% (783.2 million) (1). In addition, according to the report of the IDF (International Diabetes Federation) in 2019, the areas of the Middle East and North Africa had the highest prevalence of diabetes (12.2%) (3, 4). In Iran, approximately five million adults developed diabetes in 2017, and it is estimated that by 2030, 9.2 million people will have the disease (3, 5).
Diabetes and psychiatric disorders have a bidirectional association that influences one another in multiple ways and in different patterns (6). Studies have shown that anxiety, depression, stress, and distress are key psychological factors affecting diabetes, which may directly affect the development of the disease and the effectiveness of treatment (7–11). Depression is the most common psychiatric disorder in individuals with diabetes, and it worsens glycemic control and increases the risk of developing secondary complications (12, 13). Along with depression, anxiety is also common among patients with diabetes, and many studies have reported it (14–16). During psychological stress, counter-regulatory hormones such as catecholamine, a neurotransmitter, glucocorticoids, growth hormones, and glucagon are activated, which may cause poor glycemic control and functional impairment (17). Psychological stress, as a chief causative factor for psychosomatic disorders, has important effects on the development of diabetes through different pathways via behavioral and physiological mechanisms. Stress is associated with unhealthy lifestyle behaviors, such as inadequate eating in terms of food quality and quantity, low exercise levels, smoking, and alcohol abuse (18).
Health literacy (HL), including mental health literacy (MHL), is an important health predictor (19). MHL refers to the ability to obtain and maintain mental health information, understand mental disorders, treat them, reduce the stigma associated with mental disorders, and increase efficiency (20). A type of MHL is depression literacy (D-Lit), which includes personal and general knowledge of depression and belief in its treatment (21). Studies have shown that most people have inadequate MHL (22, 23). Most people do not know about psychological disorders, and they have a negative attitude toward their treatment or the effectiveness of treatment (24). However, the mental health of individuals in the community requires increased knowledge regarding mental illnesses to facilitate early diagnosis and intervention programs for mental disorders (24).
MHL has a negative correlation with depression and anxiety (25). D-Lit is a variable that can lead to increased professional help-seeking and improved mental health (26). Results: a study showed that MHL played a mediating role between psychological distress and mental help-seeking intentions (27). A study in Portugal reported that with improved MHL, stigma was reduced (28). A previous study mentioned that D-Lit had a negative correlation with depression stigma (29). MHL and D-Lit had a positive correlation with quality of life, and improving MHL could improve quality of life (30).
T2DM has a major impact on QOL in various domains, such as social, physical, and psychological wellbeing (31, 32). In Iran, some studies have been conducted in the field of HL and QOL among patients with T2DM (33, 34). According to the findings of a previous study, the QOL of patients with T2DM was predictable based on HL and self-care behaviors, and improved HL and self-care behaviors increased the QOL of patients with T2DM (35). In another study, MHL for psychiatric disorders associated with T2DM improved compatibility, thereby improving the quality of life and lifestyle of people with T2DM (36). However, no study has been conducted that surveys the D-Lit and MHL with regard to psychological status and quality of life in patients with T2DM. Therefore, the purpose of this study was to determine the status of MHL and depression literacy and their relationship with psychological status and quality of life among Iranian patients with T2DM.
Method
This cross-sectional survey study was conducted in 2021 among 400 patients with T2DM in Gonabad city, Iran.
Sample size
According to a previous study (37) and based on the following formula (the test power of 80%, the confidence level of 0.95%, the accuracy/d = 0.09, and the standard deviation of QOL= 0.62), the sample size required was calculated as 372. In addition, with a 10% drop rate, the sample size increased to 413 participants.
Sampling method
We used proportional stratified sampling to select the required sample. In the first stage, we considered Gonabad health centers to be strata. Then, from each center, patients with T2DM who met the inclusion criteria were selected via the simple random sampling method. After selecting the samples, we provided questionnaires to the eligible participants, who completed the questionnaires in a self-reporting manner. In this study, the researcher completed a questionnaire for illiterate people using an interview method. In this study, the inclusion criteria were as follows: patients had at least 1 year of residence in Gonabad city, had T2DM, had more than a year since the diagnosis of their diabetes, and were satisfied to participate in the study. People who did not answer more than 20% of the questions were excluded during the analysis phase.
Data collection instruments
Data were collected using a demographic questionnaire and four additional scales: the MHL scale, the D-Lit scale, the diabetes quality of life (DQOL) scale, and the DASS-21 scale (depression, anxiety, and stress).
1. Demographic questionnaire: In this section, we describe the demographic details of T2D patients (marital status, sex, age, inhabitant, education level, job status, age at the onset of diabetes, and duration of diabetes).
2. DASS-21: Lovibond designed the scale to measure depression, stress, and anxiety. This scale has 21 questions and three subscales of anxiety, depression, and stress, with seven questions (38). The questions were measured on a 4-point Likert scale (did not apply to me at all, applied to me to some degree or some of the time, applied to me to a considerable degree or a good part of the time, and applied to me very much or most of the time). A lower score in each subscale indicates better depression, stress, and anxiety. In the Iranian population, the validity and reliability of this scale were assessed by Samani and Joukar, and Cronbach's alpha coefficients of depression, stress, and anxiety were 0.85, 0.87, and 0.75, respectively (39). In addition, the r value of the depression subscale of the DASS was 0.74 compared with the Beck depression inventory, and the anxiety subscale was 0.81 compared with the Beck anxiety inventory (38).
3. MHL scale: O'Connor created and evaluated the MHL scale in 2015 (40). The validity and reliability of this questionnaire in the Iranian population were assessed by Nejatian et al. in 2021 (41). The questionnaire was confirmed with 29 questions and six subscales: the ability to recognize disorders with eight questions, knowledge of self-treatment with two questions, attitudes that promote recognition or appropriate help-seeking behavior with 10 questions, knowledge of the professional help available with three questions, knowledge of risk factors and causes with two questions, and knowledge of where to seek information with four questions. The questions are measured with 5-point Likert scale and 4-point Likert scale, with the scoring range of this questionnaire being 29–130, with a higher score indicating a better MHL status. In addition, the omega-McDonald's and Cronbach's alpha coefficients for the entire questionnaire were 0.797 and 0.789 (41). The results of the MHL test-retest in the O'Connor study showed good stability (r = 0.797) (40).
4. D-Lit scale: This scale was created and evaluated by Griffiths et al. (42, 43), and Cronbach's alpha calculated as 0.70 (42). The validity and reliability of the D-Lit were assessed by Tehrani et al. in the Iranian population, and the Cronbach's alpha coefficient of the D-Lit was 0.890 (44). This scale has 21 questions and five subscales of knowledge about the effectiveness of available treatment methods (four questions); knowledge of psychological symptoms (five questions); knowledge about taking medications and their side effects (four questions); knowledge about cognitive-behavioral symptoms (six questions); and knowledge of disease severity with two questions. The questions were measured using a 3-point Likert scale ranging from “I don't know,” “True,” and “False.” Each correct answer received a score of 3, the incorrect answer received a score of 1, and I do not know if it received a score of 2. The questionnaire's scoring range is 21–63, with higher scores indicating better D-Lit status (44). The results of D-Lit's test-retest indicated good stability and reliability (r = 071) (42).
5. DQOL Brief Clinical Inventory scale: Burroughs and Partners designed this scale for people with T2DM (45). The questionnaire contains 15 questions and evaluates the QOL of patients with type 2 diabetes. The eight questions were measured using a 5-point Likert scale (completely unhappy to completely satisfied), and seven questions were measured by a 5-point Likert scale (never to always). The questionnaire's scoring range is 15–75, and a higher score indicates an appropriate DQOL status. The validity and reliability of this tool were evaluated by Mirfeizi in Iran, and the Persian version had a CVR >0.99, a CVI >0.75, and acceptable Cronbach's alpha coefficient (a = 0.75) and test-retest reliability (intraclass correlation coefficient = 0.81) (46).
Statistical analysis
SPSS v22 software was used for data analysis. Before the data analysis, the normality of the data was verified using the Kolmogorov–Smirnov test, which was found to be normal. Therefore, parametric statistical tests consisting of one-way ANOVA (relationship between a quantitative variable and a qualitative variable with three or more states), an independent t-test (relationship between a quantitative variable and a qualitative variable with two states), and a chi-square test (relationship between qualitative variables) were used to investigate the relationship between variables. Pearson's correlation coefficient was used to evaluate the correlation between quantitative variables. Continuous parametric data are presented as mean and standard deviation, while dichotomous data are presented as absolute and relative frequencies. All tests were analyzed at a significance level of 0.05.
Results
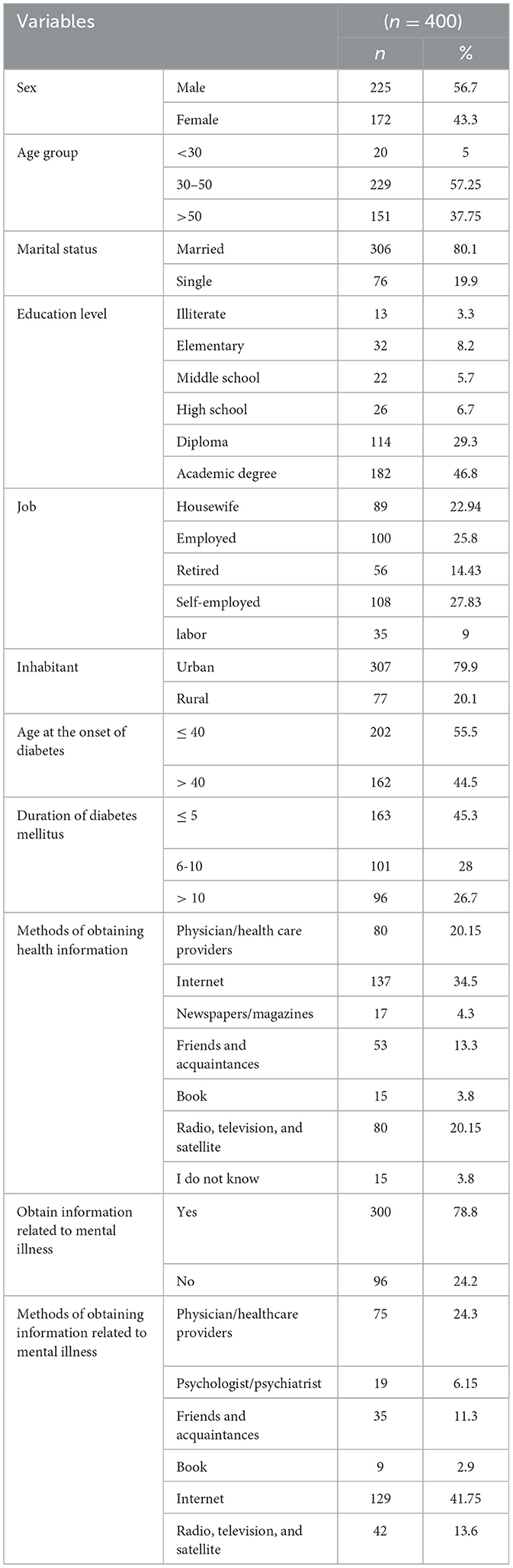
In this study, the response rate was 96.85%. Table 1 presents the demographic information about the participants. The mean (standard deviation) age of the patients, the age at the onset of diabetes, and the duration of the disease were 48.18 (11.69), 40.79 (9.60), and 8.38 (6.80), respectively. Most participants were men (n = 225) and married (n = 306). Other information is provided in Table 1.
Education level had a significant relationship with anxiety, and the level of anxiety was higher among those with elementary education, whereas those with academic education had a lower level of anxiety (P = 0.002). There was a significant relationship between receiving mental health information and depression levels, with those who received mental health information having lower depression levels (P = 0.014). There was a significant relationship between methods of obtaining information about mental health and anxiety, and those who received information from their friends and acquaintances had lower anxiety levels (P = 0.001). There was a significant relationship between the method of obtaining information about mental health and stress, and those who received their information from physicians/health care providers had lower stress levels (P = 0.042).
Age had a significant relationship with depression (P = 0.046), stress (P = 0.001), and anxiety (P < 0.001), whereas people younger than 30 years had lower levels of depression, stress, and anxiety. Job status had a significant relationship with anxiety, and self-employed individuals had low levels of anxiety (P = 0.023). Job status had a significant relationship with stress, and individuals with employed jobs experienced low levels of stress (P = 0.021). The age at the onset of diabetes had a significant relationship with stress (P = 0.009) and anxiety (P = 0.026), and people who had diabetes at the age of 40 years or less experienced low levels of stress and anxiety. The duration of diabetes had a significant relationship with depression, stress, and anxiety, and individuals with a duration of diabetes of 5 years had low levels of depression (P = 0.036), stress (P = 0.004), and anxiety (P < 0.001) (Table 2).
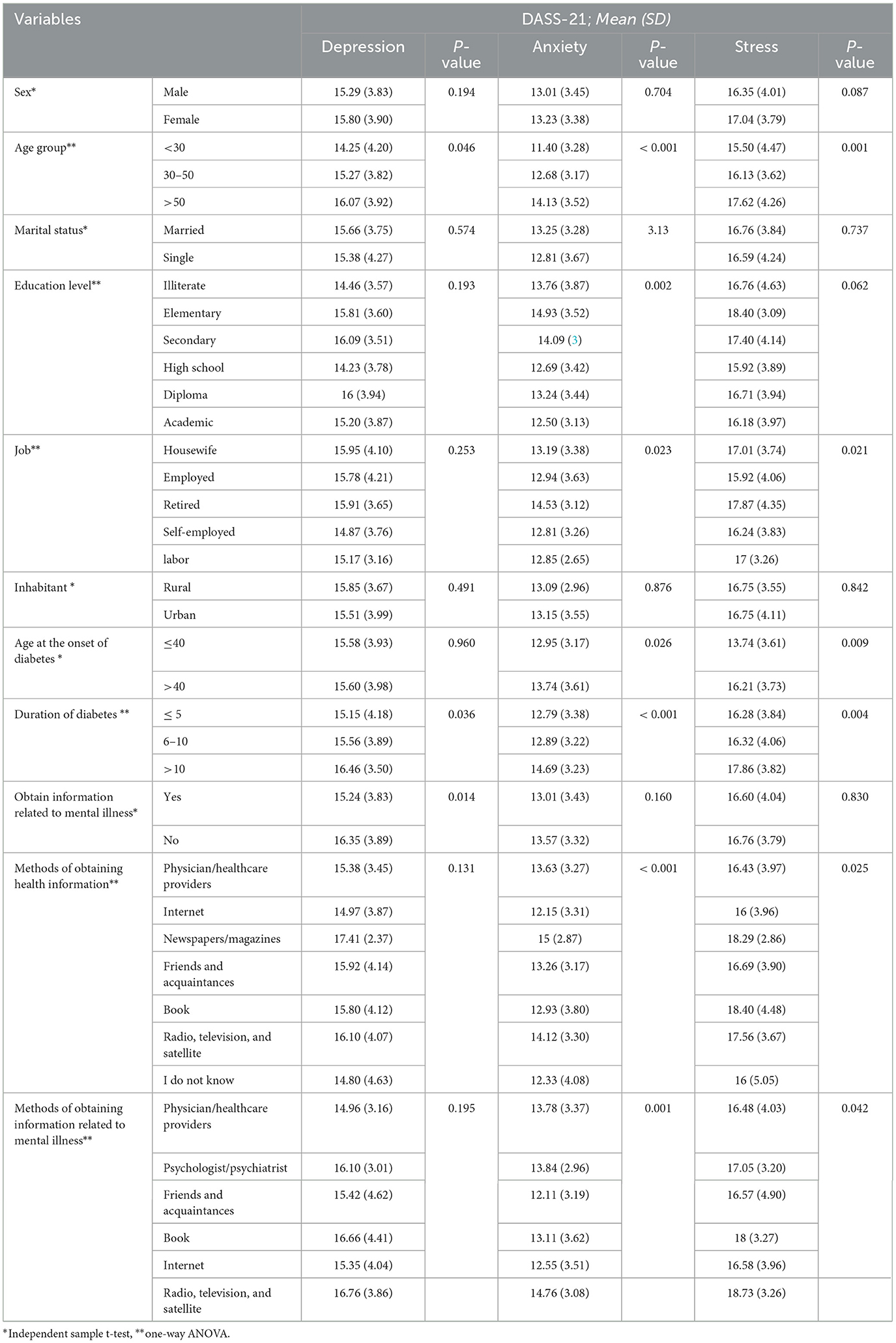
Table 2. Relationship between demographic variables and psychological status (depression, anxiety, and stress).
The mean (standard deviation) of MHL was 80.92 (9.16). Marital status had a significant relationship with MHL, and single individuals had a higher MHL (P = 0.009). The level of education had a significant relationship with knowledge of where to seek information, and those with higher education levels had a higher HL on this subscale (P < 0.001). The economic situation had a significant relationship with MHL, and patients with better economic conditions had higher MHL (P < 0.001). The economic situation had a significant relationship with knowledge of where to seek information, and those with better economic conditions had higher HL scores in this subscale (P < 0.001) (Table 3).
There was a significant relationship between receiving mental health information and the level of MHL, with those who received mental health information having higher levels of MHL (P = 0.001). There was a significant relationship between receiving mental health information and the ability to recognize disorders (P = 0.001), knowledge of self-treatment (P = 0.001), and knowledge of the professional help available (P = 0.015), and those who received mental health information in these subscales had higher levels of MHL. Similarly, patients who received health information online had a higher MHL (P < 0.001). Patients who received mental health information from a psychologist/psychiatrist had higher levels of MHL (P = 0.014) (Table 3).
Age was significantly associated with MHL, and patients younger than 30 years had higher levels of MHL (P < 0.001). Job status had a significant relationship with MHL, and self-employed individuals had higher levels of MHL (P = 0.010). Age at the onset of diabetes had a significant relationship with MHL, and patients who had diabetes at the age of 40 years or less had higher levels of MHL (P = 0.040). The duration of diabetes was significantly associated with MHL, and patients with a duration of diabetes of ≤ 5 years had higher levels of MHL (P = 0.026) (Table 3).
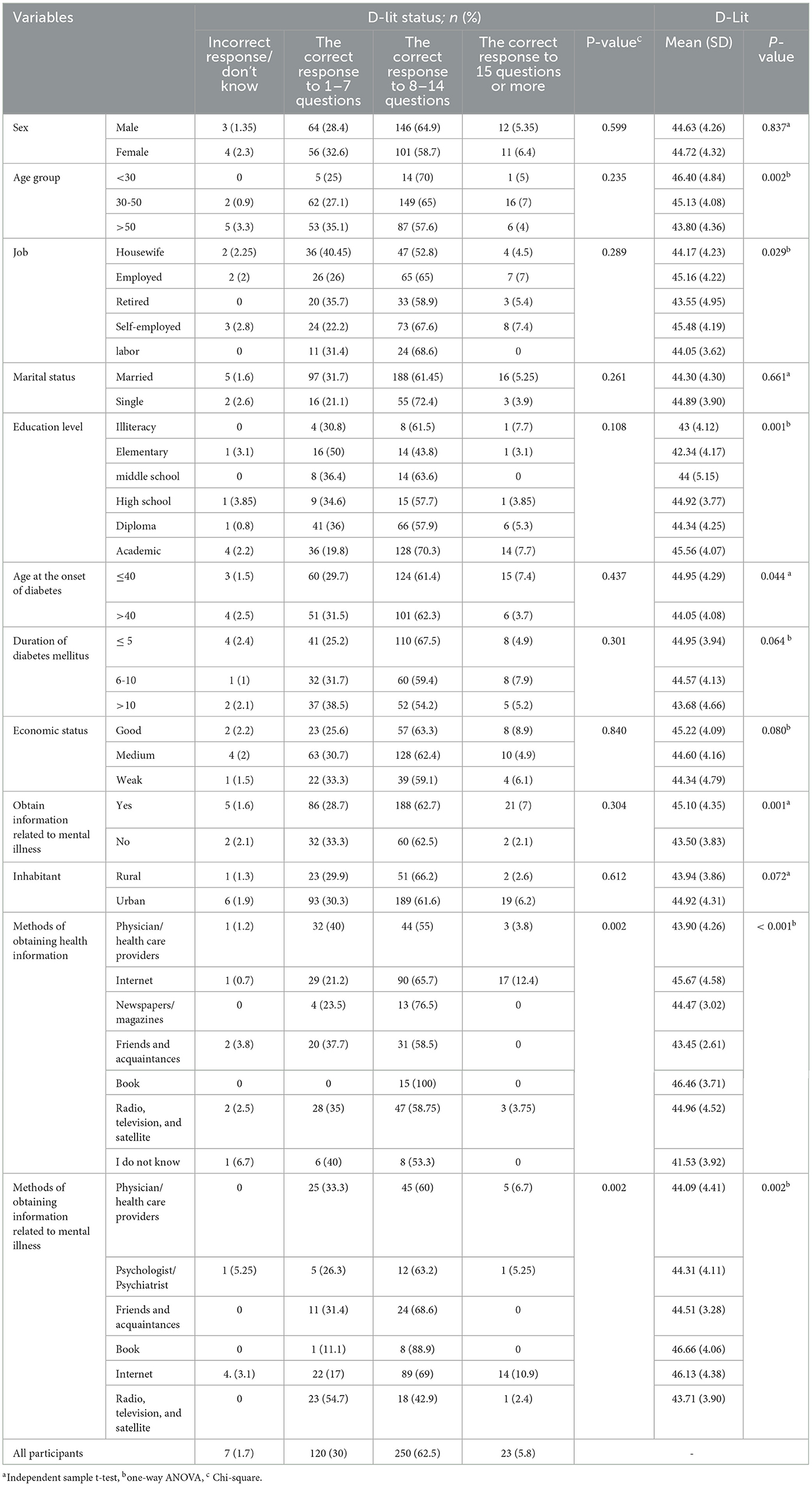
Age had a significant relationship with D-Lit, and people younger than 30 years had a higher D-Lit (P = 0.002). Job status had a significant relationship with D-Lit, and self-employed individuals had higher levels of D-Lit (P = 0.029). Age at the onset of diabetes had a significant relationship with D-Lit, and individuals who had a disease at the age of ≤ 40 years had higher levels of D-Lit (P = 0.044). There was a significant relationship between receiving mental health information and D-Lit levels, with those who received mental health information having higher levels of D-Lit (P = 0.001). Patients who received health information from the book had higher levels of D-Lit (P < 0.001). Patients who received mental health information from the book had higher D-Lit scores (P = 0.002) (Table 4).
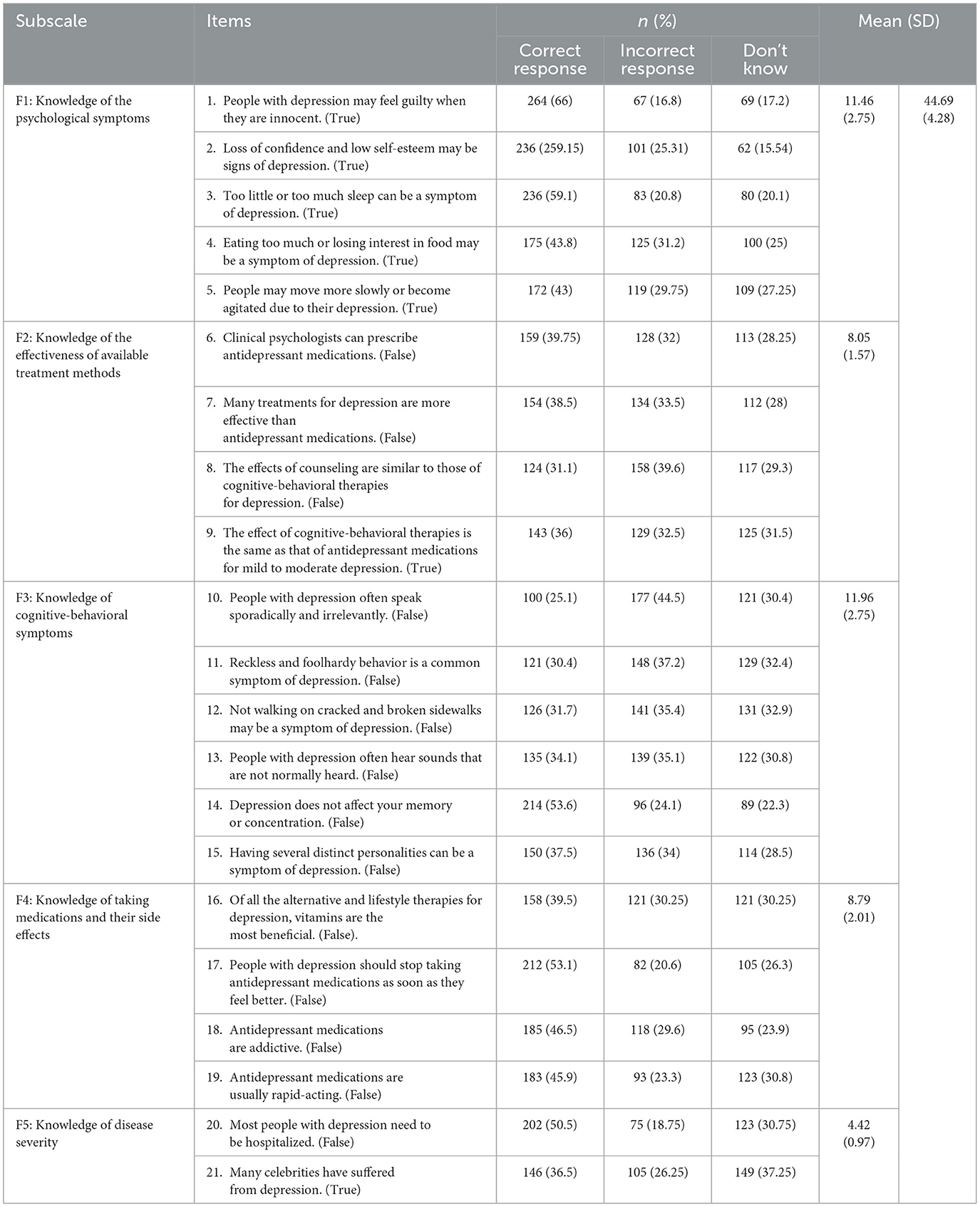
In response to the D-Lit questions, only 1.7% (n = 7) of the participants failed to answer any questions correctly, and 5.8% (n = 23) were able to answer 15 questions or more correctly (Table 4). The participants' responses to the questions and subscales of the D-Lit are listed in Table 5. The mean (SD) D-Lit of the participants was 44.69 (4.28). The mean (SD) of the subscales of the D-Lit are presented in Table 5.
Regarding the subscales of the D-Lit questionnaire, the responses revealed varied levels of knowledge among the participants. Specifically, only 21.5% (n = 86) could correctly answer all items related to knowledge of psychological symptoms. Only 2% (n = 8) correctly answered all questions about the effectiveness of available treatment methods. A slightly higher percentage, 4.5% (n = 18), correctly answered all questions pertaining to cognitive-behavioral symptoms. The participants' knowledge about taking medications and their side effects was accurately known by 13% (n = 52). Furthermore, 19.3% (n = 77) were able to correctly answer all questions regarding knowledge about disease severity.
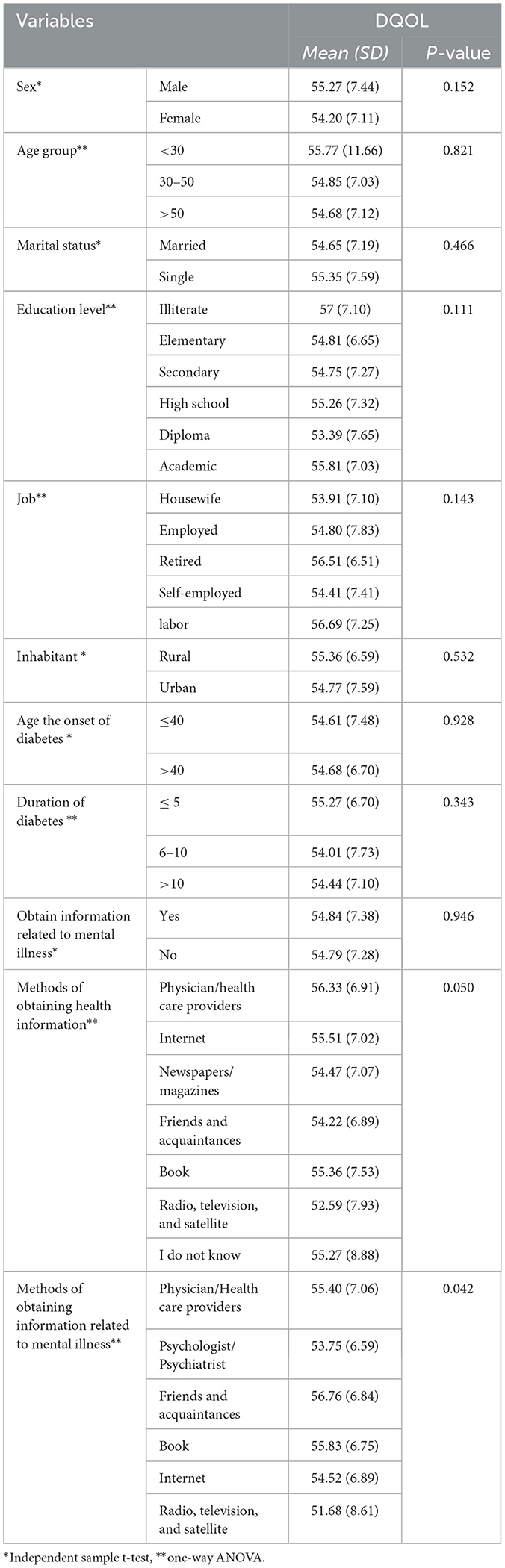
There was a significant relationship between the sources of mental health information and the DQOL. Specifically, those who received information from their friends and acquaintances reported a higher DQOL (P = 0.042) (Table 6). Additionally, the results of Tukey's post hoc tests exploring the relationships between demographic factors and variables such as depression, anxiety, stress, MHL, D-Lit, and DQOL are presented in Supplementary Files S1–S6.
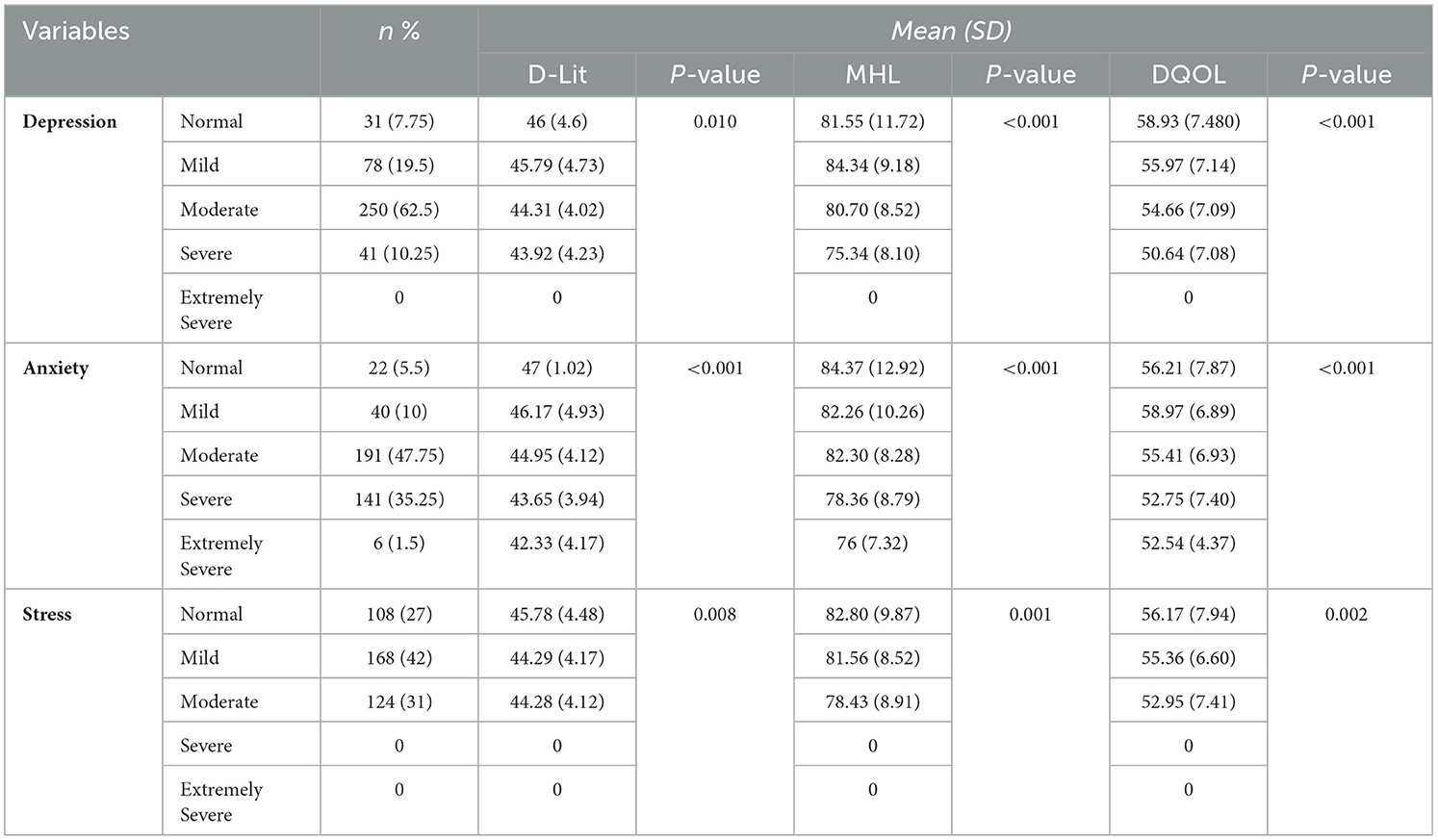
As can be observed from Table 7, only 10.3% (n = 41) had severe depression, 36.8% (n = 147) had severe anxiety and extremely severe anxiety, and 31% (n = 124) had moderate stress. Depression (P = 0.010), anxiety (P < 0.001), and stress (P = 0.008) were significantly associated with D-Lit, whereas patients with severe depression, extremely severe anxiety, and moderate stress had lower levels of D-Lit. Depression (P < 0.001), anxiety (P < 0.001), and stress (P = 0.001) were significantly associated with MHL, and patients with severe depression, extremely severe anxiety, and moderate stress had lower levels of MHL. In addition, depression (P < 0.001), anxiety (P < 0.001), and stress (P = 0.002) were significantly associated with DQOL, and patients with severe depression, extremely severe anxiety, and moderate stress had lower levels of DQOL (Table 7).
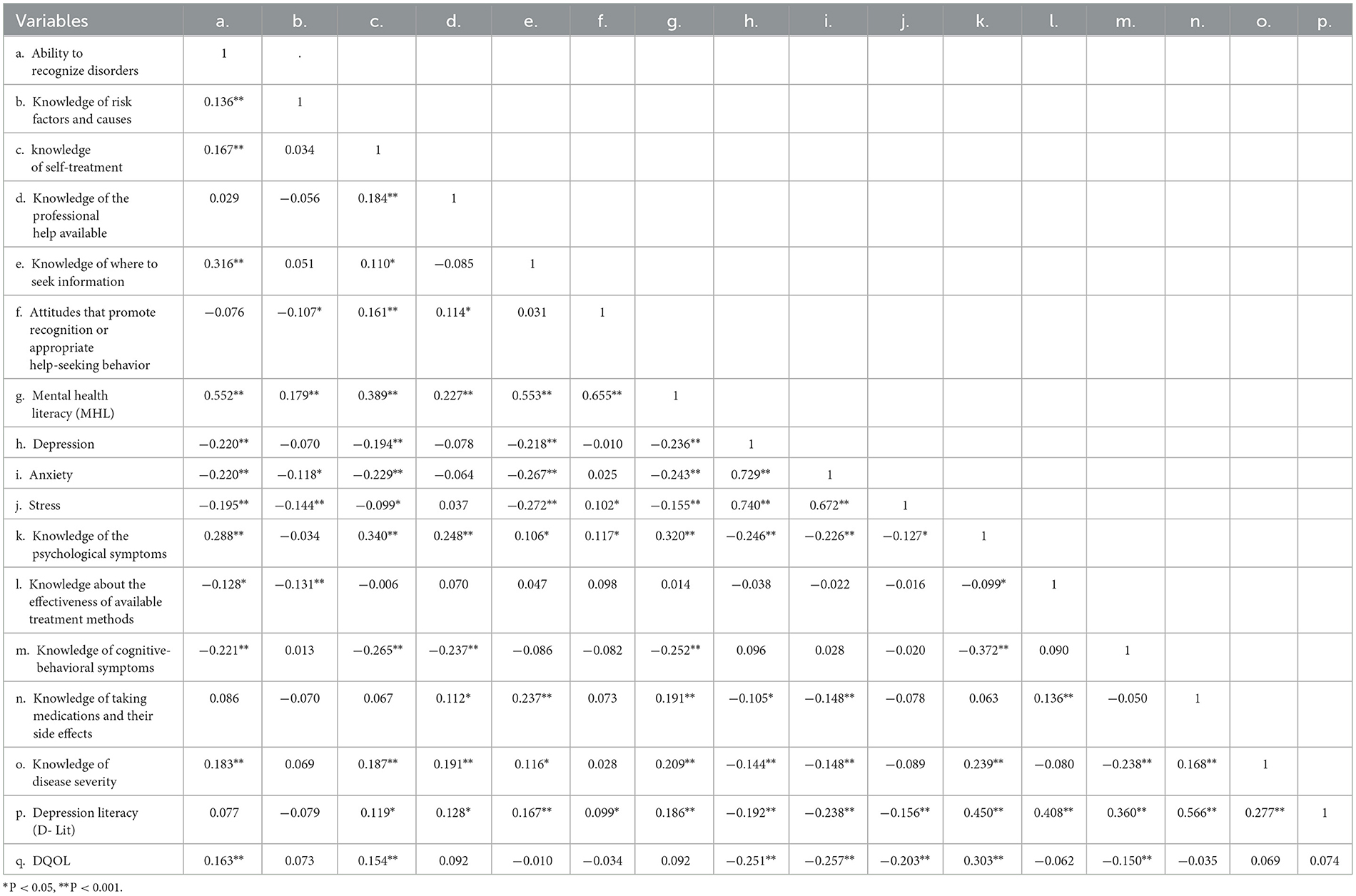
The results in Table 8 show the correlation between variables. According to the results, there was a negative and significant correlation between MHL and depression (r = −0.236), anxiety (r = −0.243), and stress (r = −0.155) (P < 0.001). There was a positive and significant correlation between MHL and D-Lit (r = 0.186) (P < 0.001). There was a negative and significant correlation between D-Lit and depression (r = −0.192), anxiety (r = −0.238), and stress (r = −0.156) (P < 0.001). There was a positive and significant correlation between the ability to recognize disorders (r = 0.163) and knowledge of self-treatment (r = 0.154) with DQOL (P <0.001). There was a negative and significant correlation between the state of depression (r = −0.251), anxiety (r = −0.257), stress (r = −0.203), and DQOL (P < 0.001) (Table 8).
Discussion
This research showed that MHL was not high and that only 5.8% of patients had high D-Lit scores and were able to answer 15 or more questions correctly. However, in this study, only 7.8% of the patients were free of depression, 5.5% had no anxiety, and 27% were not stressed. In a previous study, the results showed that these patients had insufficient health literacy regarding their illness, and the provision of simple and understandable educational resources for the diabetic population was effective in increasing their health literacy (47). HL assessment is an important prerequisite for reinforcing the proper management of DT2, following treatment, and adopting more flexible health policies (48).
In this study, there was a significant and negative correlation between D-Lit and MHL and the levels of depression, anxiety, and stress. Additionally, there was a significant and negative correlation between levels of depression, anxiety, stress, and the QOL. These results indicate that increasing MHL and D-Lit can decrease the prevalence of anxiety, depression, and stress while improving QOL. These results can be useful for designing educational programs aimed at preventing mental illness and improving T2DM patients' quality of life. Other research indicates that people with low HL are more likely to exhibit depressive symptoms or be considered depressed (49, 50). A previous study found that depressive symptoms affect self-care management and quality of care, negatively affecting health outcomes in people with diabetes (51–53). A previous study also showed that COVID-19 profoundly affects anxiety levels, impacting patients' psychological wellbeing (54). A study from China observed that enhancing D-Lit during the pandemic reduced depression, (55) while another study noted that MHL was negatively correlated with stress and positively correlated with psychological health during the COVID-19 pandemic (56). Therefore, adequate MHL can not only support individuals in critical situations but also play a crucial role in preventing mental disorders.
In this study, there was a positive and significant correlation between knowledge of psychological symptoms, the ability to recognize disorders, and QOL. It appears that people's ability to recognize mental disorder symptoms in the early stages helps them take prompt actions, while awareness of available treatment options facilitates their use of appropriate interventions. As a result, these proactive measures can reduce the risk of various complications, thereby enhancing QOL. The findings of several studies have reported a significant relationship between the ability to diagnose mental disorders and the seeking of mental health services (57–59). People who are adept at diagnosing various types of mental disorders are more likely to seek mental health services, allowing for the early diagnosis and appropriate treatment of their conditions (57–59).
This research revealed a statistically significant relationship between age and lower levels of stress and anxiety among people aged 30 years. One study found that early-onset T2DM is associated with mood disorders, anxiety, and stress (60). The findings of another study indicated that younger people exhibit higher levels of depression and anxiety than older people, which is likely due to their low levels of experience in managing the stresses related to treatment and diabetes challenges (61). Additionally, the effect of the disease on physical and mental performance and QOL contribute to higher rates of depression and anxiety among younger patients (61). The findings of our study contrast those reported in the Palizgir study, which indicated different age-related impacts on psychological wellbeing (61). More research is needed to determine whether there is a relationship between age, stress, and anxiety in T2DM. Other factors, such as the stress associated with managing chronic illnesses, may also contribute to stress and anxiety in patients with T2DM.
There was a statistically significant relationship between education level and anxiety, with patients with elementary education exhibiting higher levels of anxiety compared to those with higher academic education, who displayed lower levels of anxiety. The level of education has another protective effect against anxiety, as people with higher education levels tend to use health and treatment services and have no problem finding places that provide such services (62). In addition, higher education levels are associated with a decreased likelihood of engaging in unhealthy behaviors (63, 64). The findings of a previous study showed that a high education level is a protective factor against anxiety and depression (63). Another study found that patients with T2DM who had low education levels were more likely to experience anxiety (65).
There was also a significant relationship between education levels and knowledge of where to find information, with those with higher education levels having higher knowledge. In line with this result, a relationship between education and HL has already been reported (66). We found a positive relationship between education levels and HL scores, as in other studies (66–68). More educated people have fewer problems finding valid health care and understanding health information.
There was a significant relationship between economic status and MHL; patients with better economic conditions had higher levels of MHL. These results are similar to those of a previous study (69), suggesting that socioeconomic status may be an independent variable that can affect HL directly through education and indirectly through access to digital medical content using tablets and smartphones. In addition, this study found a significant relationship between receiving mental health information and the levels of MHL and D-Lit, and those who received mental health information had higher MHL.
The results of this study can be combined and explained with the mind sponge theory, which was first presented by Vuong and Napier (70). According to the mind-sponge model, the human mind acts like a sponge, absorbing values and information that are compatible with one's mindset and discarding those that are not. This metaphorical sponge consists of several layers, with the mindset encompassing an individual's core values positioned at the center. Information, values, cultural norms, and environmental beliefs are evaluated based on their alignment with these core values, determining their acceptance or rejection (71–74).
According to Jorm's definition of MHL, correct knowledge, beliefs, and attitudes about identifying mental illnesses, their causes, risk factors, and avenues for seeking help are the fundamental components of MHL (75). As a result, by implementing strategies and policies to promote MHL, it can be expected that societal mindsets will evolve over time, leading to the adoption of more correct values, beliefs, and attitudes toward mental issues, replacing erroneous ones. Once the core values concerning mental health issues are corrected. people will be better equipped to judge and use the information around them. More correct information will be absorbed by the “mind sponge,” while incorrect information will be rejected. This shift lays the groundwork for adopting correct behaviors, such as seeking professional help when in need. For example, a person experiencing symptoms of depression but possessing a high level of MHL due to correct knowledge, attitudes, and values, is likely to make more accurate cost-benefit analyses. Consequently, while absorbing more accurate information from the environment, such people are more inclined to seek professional help and adopt self-help measures. Conversely, in individuals with low MHL and incorrect values, the absorption of incorrect information, such as methods for suicide attempts or the avoidance of psychological help due to stigmatizing attitudes, can be expected.
As a result, improving MHL, specifically depression health literacy, can facilitate the restructuring of the knowledge, beliefs, values, and attitudes in the mind-sponge mindset of people with diabetes, leading to more correct judgments and, ultimately, more correct help-seeking behaviors. Consequently, the occurrence of mental disorders, such as depression and anxiety, is expected to be prevented. If these disorders occur, the patient is more likely to receive timely treatment and ultimately experience a better quality of life.
Quality of life plays a fundamental role in achieving treatment goals and the early diagnosis of diabetes (76). The significant prevalence of depression, stress, and anxiety among people with diabetes and their potential negative impact on quality of life are concerning. The findings of this study suggest that screening and initial assessment of individuals with diabetes at the community-based care level are necessary to address their mental health problems. As a result, it is advisable for primary healthcare providers to regularly evaluate patients' mental health while implementing routine interventions, such as monitoring patients' glycemic status, dietary compliance, and activity levels and referring patients to mental health specialists when necessary. Improving mental health and depression health literacy can form the cornerstone of mental health education for all people with diabetes. Educators, armed with a thorough understanding of the main components of MHL and depression literacy, can provide more targeted, coherent, and useful education, ultimately leading to transformative changes in the values and mindsets of patients. Depression is also associated with an increased risk of hospitalization (for any reason) in patients with diabetes (77). Therefore, nurses and practitioners should not neglect to take the mental history of patients with diabetes into account in addition to initial clinical evaluations. Finally, depression and anxiety contribute to increased healthcare system costs (78), highlighting the need for policymakers to invest in preventive interventions, especially in improving MHL and depression literacy.
This study has limitations that should be considered when interpreting the findings. The cross-sectional nature of this study restricts our ability to establish causal relationships among the variables. Although we observed associations between MHL, psychological status (anxiety, depression, and stress), and quality of life, we cannot definitively conclude that one variable causes the other. Longitudinal studies are required to further investigate the temporal relationships between these variables. In addition, the sample of 400 patients with DT2 from Gonabad, Iran, may not be representative of the entire diabetic population. Consequently, these findings may not be generalizable to patients in other geographic areas or those with different demographic characteristics. Participants' recall accuracy and the potential for socially desirable responses could also skew results. Objective measures, such as clinical assessments, can help address these concerns. The DASS-21 questionnaire, while useful, is used to assess depression, anxiety, and stress; a more comprehensive assessment using in-depth clinical interviews or specialized mental health questionnaires can provide a more accurate understanding of the participants' mental health status.
Conclusion
Our study revealed that lower MHL and D-Lit scores among patients with T2DM were associated with higher levels of anxiety, depression, and stress, as well as a lower quality of life. These findings demonstrate the important role of MHL and D-Lit in promoting psychological wellbeing and overall quality of life in this population. The findings showed that the MHL and D-Lit levels in patients with T2DM were inadequate. Considering the high risk of various mental disorders in patients with T2DM, it is necessary to improve their MHL to detect such disorders in the early stages, seek mental health services, and receive available treatments. In addition, designing preventive programs to improve the mental health of patients with T2DM can prevent the occurrence of mental disorders and improve their QOL. For example, the PATIENT strategy (P: patient's perception; A: assessment; T: tailored approach; I: iterative evaluation; E: education; N: non-pharmacological approach; T: team) used in the previous study can be applied (79).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of Gonabad University of Medical Sciences with the code of ethics IR.GMU.REC.1401.017. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AJ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. MM: Conceptualization, Investigation, Project administration, Supervision, Writing – original draft, Writing – review & editing. FN: Conceptualization, Investigation, Project administration, Writing – original draft, Writing – review & editing. MG-G: Conceptualization, Investigation, Software, Writing – original draft, Writing – review & editing. VA: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. KK: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. MN: Conceptualization, Investigation, Methodology, Project administration, Software, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank the Social Development and Health Promotion Research Center at Gonabad University of Medical Sciences. We would also like to thank everyone who assisted us in running this research project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1421053/full#supplementary-material
Abbreviations
MHL, Mental health literacy; HL, health literacy; D-Lit, depression literacy; DQOL, diabetes quality of life; T2DM, Type 2 diabetes mellitus; QOL, quality of life.
References
1. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
2. Heald AH, Stedman M, Davies M, Livingston M, Alshames R, Lunt M, et al. Estimating life years lost to diabetes: outcomes from analysis of National Diabetes Audit and Office of National Statistics data. Cardiovas Endocrinol Metabol. (2020) 9:183. doi: 10.1097/XCE.0000000000000210
3. Taheri H, Rafaiee R, Rafaiee R. Prevalence of complications of diabetes and risk factors among patients with diabetes in the diabetes clinic in Southeast of Iran. Iran J Diab Obesity. (2021). doi: 10.18502/ijdo.v13i1.5745
4. Haghdoost A, Rezazadeh Kermani M, Sadghirad B, Baradaran H. Prevalence of type 2 diabetes in the Islamic Republic of Iran: systematic review and meta-analysis. EMHJ. 15:591–99. doi: 10.26719/2009.15.3.591
5. Care D. 6. Glycemic targets: standards of medical care in diabetes-−2019. Diabet Care. (2019) 42:S61–70. doi: 10.2337/dc19-S006
6. Balhara YPS. Diabetes and psychiatric disorders. Indian J Endocrinol Metab. (2011) 15:274–83. doi: 10.4103/2230-8210.85579
7. Smith KJ, Béland M, Clyde M, Gariépy G, Pagé V, Badawi G, et al. Association of diabetes with anxiety: a systematic review and meta-analysis. J Psychosom Res. (2013) 74:89–99. doi: 10.1016/j.jpsychores.2012.11.013
8. Graham EA, Deschenes SS, Khalil MN, Danna S, Filion KB, Schmitz NJJ. Measures of depression and risk of type 2 diabetes: A systematic review and meta-analysis. J Affect Disord. (2020) 265:224–32. doi: 10.1016/j.jad.2020.01.053
9. Sunena, Mishra DN. Stress etiology of type 2 diabetes. Curr Diabetes Rev. (2022) 18:50–6. doi: 10.2174/1573399818666220224140934
10. Parsa S, Aghamohammadi M, Abazari M. Diabetes distress and its clinical determinants in patients with type II diabetes. Diabetes Metab Syndr. (2019) 13:1275–9. doi: 10.1016/j.dsx.2019.02.007
11. Liu X. Metabolic syndrome, obesity. advances in psychological and social aetiology of patients with diabetes. Diabetes Metab Syndr Obes. (2024) 16:4187–94. doi: 10.2147/DMSO.S439767
12. Kalra S, Jena BN, Yeravdekar R. Emotional and psychological needs of people with diabetes. Indian J Endocrinol Metab. (2018) 22:696–704. doi: 10.4103/ijem.IJEM_579_17
13. Nouwen A, Adriaanse M, van Dam K, Iversen MM, Viechtbauer W, Peyrot M, et al. Longitudinal associations between depression and diabetes complications: a systematic review and meta-analysis. Diabet Med. (2019) 36:1562–72. doi: 10.1111/dme.14054
14. Sharma K, Dhungana G, Adhikari S, Pandey AB, Sharma M. Practice. Depression and anxiety among patients with type II diabetes mellitus in Chitwan Medical College Teaching Hospital, Nepal. Nurs Res Pract. (2021) 2021:8846915. doi: 10.1155/2021/8846915
15. Alzahrani A, Alghamdi A, Alqarni T, Alshareef R, Alzahrani A. Prevalence and predictors of depression, anxiety, and stress symptoms among patients with type II diabetes attending primary healthcare centers in the western region of Saudi Arabia: a cross-sectional study. Int J Ment Health Syst. (2019) 13:1–7. doi: 10.1186/s13033-019-0307-6
16. Khan P, Qayyum N, Malik F, Khan T, Khan M, Tahir A. Incidence of anxiety and depression among patients with type 2 diabetes and the predicting factors. Cureus. (2019) 11:e4254. doi: 10.7759/cureus.4254
17. Grisel JE, Rasmussen PR, Sperry L. Anxiety and depression: physiological and pharmacological considerations. J Occup Psychol. (2006) 62:4.
18. Rod NH, Grønbaek M, Schnohr P, Prescott E. Kristensen T. Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J Intern Med. (2009) 266:467–75. doi: 10.1111/j.1365-2796.2009.02124.x
19. Wei Y, McGrath PJ, Hayden J, Kutcher S. Measurement properties of mental health literacy tools measuring help-seeking: a systematic review. J Ment Health. (2017) 26:543–55. doi: 10.1080/09638237.2016.1276532
20. Kutcher S, Wei Y, Coniglio C. Mental health literacy: past, present, and future. Can J Psychiat. (2016) 61:154–8. doi: 10.1177/0706743715616609
21. Deen TL, Bridges AJ. Depression literacy: rates and relation to perceived need and mental health service utilization in a rural American sample. Rural Remote Health. (2011) 11:83–95. doi: 10.22605/RRH1803
22. Mahmoodi SMH, Ahmadzad-Asl M, Eslami M, Abdi M, Hosseini Kahnamoui Y, Rasoulian M. Mental Health literacy and mental health information-seeking behavior in Iranian University Students. Front Psychiatry. (2022) 13:893534. doi: 10.3389/fpsyt.2022.893534
23. Abesinghe A, Katuwawela K, Lakmali K, Jayanetti N, Munidasa P, De Silva BS, et al. Mental health literacy: a survey of the public's ability to recognize mental disorders and their knowledge about the effectiveness of helpful interventions to help the victims. J Evid-Based Psychotherap. (2023) 23:173–202. doi: 10.24193/jebp.2023.2.16
24. Reavley NJ, Morgan AJ, Jorm AF. Development of scales to assess mental health literacy relating to recognition of and interventions for depression, anxiety disorders and schizophrenia/psychosis. Aust New Zeal J Psychiat. (2014) 48:61–9. doi: 10.1177/0004867413491157
25. Yao Z-Y, Wang T, Yu Y-K, Li R, Sang X, Fu Y-N, et al. Mental health literacy and suicidal ideation among Chinese college students: the mediating role of depressive symptoms and anxiety symptoms. J Affect Disord. (2023) 339:293–301. doi: 10.1016/j.jad.2023.07.050
26. Lee YJ. Depression literacy, associated factors, and correlation of related variables in middle-aged korean adults: a cross-sectional study. Int J Environ Res Public Health. (2023) 20:6021. doi: 10.3390/ijerph20116021
27. Zeng F, John WCM, Qiao D, Sun X. Association between psychological distress and mental help-seeking intentions in international students of national university of Singapore: a mediation analysis of mental health literacy. BMC Public Health. (2023) 23:2358. doi: 10.1186/s12889-023-17346-4
28. Simões de Almeida R, Trigueiro MJ, Portugal P, de Sousa S, Simões-Silva V, Campos F, et al. Mental health literacy and stigma in a municipality in the north of Portugal: a cross-sectional study. Int J Environ Res Public Health. (2023) 20:3318. doi: 10.3390/ijerph20043318
29. Al-Shannaq Y, Jaradat D, Ta'an WF, Jaradat D. Depression stigma, depression literacy, and psychological help seeking attitudes among school and university students Archives of psychiatric nursing. Arch Psychiatr Nurs. (2023) 46:98–106. doi: 10.1016/j.apnu.2023.08.010
30. Tehrani H, Vali M, Nejatian M, Moshki M, Charoghchian Khorasani E, Jafari A. The status of depression literacy and its relationship with quality of life among Iranian public population: a cross sectional study. BMC Psychiatry. (2022) 22:1–9. doi: 10.1186/s12888-022-04251-0
31. John R, Pise S, Chaudhari L. Deshpande PR. Evaluation of quality of life in type 2 diabetes mellitus patients using quality of life instrument for indian diabetic patients: a cross-sectional study. J Midlife Health. (2019) 10:81–8. doi: 10.4103/jmh.JMH_32_18
32. Abualhamael SA, Baig M, Alghamdi W, Gazzaz ZJ, Al-Hayani M. Bazi A. Quality of life, stress, anxiety and depression and associated factors among people with type 2 diabetes mellitus in Western region Saudi Arabia. Front Psychiatry. (2024) 14:1282249. doi: 10.3389/fpsyt.2023.1282249
33. Jafari A, Zadehahmad Z, Armanmehr V, Talebi M, Tehrani H. The evaluation of the role of diabetes health literacy and health locus of control on quality of life among type 2 diabetes using the Path analysis. Sci Rep. (2023) 13:5447. doi: 10.1038/s41598-023-32348-3
34. Shafiei H. Nasiri S. The role of health literacy, psychological wellbeing and self–efficacy in prediction the quality of life of patients with type 2 diabetes. J Health Psychol. (2020) 9:7–22. doi: 10.30473/hpj.2020.47749.4497
35. Ghorbani Nohouji M, Kooshki SH, Kazemi AS, Khajevand Khoshli A. Evaluation of health-related quality of life in patients with type 2 diabetes based on health-related literacy and self-efficacy: mediating role of self-care activity. J Health Care. (2020) 22:25766. doi: 10.52547/jhc.22.3.257
36. Vazifehkhorani AK, Karimzadeh M, Poursadeghiyan M. Rahmati-Najarkolaei F. Psychoeducation on improving mental health literacy and adjustment to illness in patients with type 2 diabetes: an experimental study. Iran Rehabil J. (2018) 16:395–404. doi: 10.32598/irj.16.4.395
37. Solimani Z, Barati H, Mozafari Join A, Ershadi Moqadam H, Mohammadi M. The quality of life of patients with diabetes from the City of Sabzevar during year 2016. Milit Caring SciJ. (2017) 3:264–71. doi: 10.18869/acadpub.mcs.3.4.264
38. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
39. Samani S, Joukar B, A. study on the reliability and validity of the short form of the depression anxiety stress scale (DASS-21). J Soc Sci Humant. (2007) 26:65–77.
40. O'Connor M, Casey L. The Mental Health Literacy Scale (MHLS): a new scale-based measure of mental health literacy. Psychiatry Res. (2015) 229:511–6. doi: 10.1016/j.psychres.2015.05.064
41. Nejatian M, Tehrani H, Momeniyan V, Jafari A. A modified version of the mental health literacy scale (MHLS) in Iranian people. BMC Psychiatry. (2021) 21:1–11. doi: 10.1186/s12888-021-03050-3
42. Griffiths KM, Christensen H, Jorm AF, Evans K, Groves C. Effect of web-based depression literacy and cognitive–behavioural therapy interventions on stigmatising attitudes to depression: randomised controlled trial. Br J Psychiatry. (2004) 185:342–9. doi: 10.1192/bjp.185.4.342
43. Gulliver A, Griffiths KM, Christensen H, Mackinnon A, Calear AL, Parsons A, et al. Internet-based interventions to promote mental health help-seeking in elite athletes: an exploratory randomized controlled trial. J Med Internet Res. (2012) 14:e69. doi: 10.2196/jmir.1864
44. Tehrani H, Nejatian M, Moshki M, Jafari A. Psychometric properties of Persian version of depression literacy (D-Lit) questionnaire among general population. Int J Ment Health Syst. (2022) 16:1–11. doi: 10.1186/s13033-022-00550-x
45. Burroughs TE, Desikan R, Waterman BM, Gilin D, McGill J. Development and validation of the diabetes quality of life brief clinical inventory. Diab Spect. (2004) 17:41–9. doi: 10.2337/diaspect.17.1.41
46. Mirfeizi M, Jafarabadi MA, Toorzani ZM, Mohammadi SM, Azad MD, Mohammadi AV, et al. Feasibility, reliability and validity of the Iranian version of the Diabetes Quality of Life Brief Clinical Inventory (IDQOL-BCI). Diabetes Res Clin Pract. (2012) 96:237–47. doi: 10.1016/j.diabres.2011.12.030
47. Khosravi A, Ahmadzadeh K, Arastoopoor S, Tahmasbi R. Health literacy levels of diabetic patients referred to Shiraz health centers and its effective factors. Health Inf Manage. (2015) 12:205.
48. Marathe J, Ogden K, Woodroffe J. Health literacy, genetic literacy and outcomes in patients with genetic cardiac disease: a review of the literature. Heart, Lung Circu. (2014) 23:e12. doi: 10.1016/j.hlc.2014.07.032
49. Coffman MJ, Norton CK. Demands of immigration, health literacy, and depression in recent Latino immigrants. Home Health Care Manag Pract. (2010) 22:116–22. doi: 10.1177/1084822309347343
50. Sudore RL, Mehta KM, Simonsick EM, Harris TB, Newman AB, Satterfield S, et al. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. (2006) 54:770–6. doi: 10.1111/j.1532-5415.2006.00691.x
51. Ali S, Stone M, Peters J, Davies M, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diab Med. (2006) 23:1165–73. doi: 10.1111/j.1464-5491.2006.01943.x
52. Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. Gen Hosp Psychiat. (2003) 25:246–52. doi: 10.1016/S0163-8343(03)00055-0
53. Katon W, Von Korff M, Ciechanowski P, Russo J, Lin E, Simon G, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diab Care. (2004) 27:914–20. doi: 10.2337/diacare.27.4.914
54. Buonanno P, Marra A, Iacovazzo C, Vargas M, Nappi S, de Siena AU, et al. Preoperative anxiety during COVID-19 pandemic: a single-center observational study and comparison with a historical cohort. Front Med. (2022) 9:1062381. doi: 10.3389/fmed.2022.1062381
55. Shan D, Li S, Xu R, Huang J, Wang Y, Zheng Y, et al. Low depression literacy exacerbates the development and progression of depressive mood in Chinese adult social media users during COVID-19: A 3-month observational online questionnaire-based study with multiple cross-sectional analyses. Front Public Health. (2023) 11:1096903. doi: 10.3389/fpubh.2023.1096903
56. Fakhari A, Shalchi B, Rahimi VA, Naghdi Sadeh R, Lak E, Najafi A, et al. Mental health literacy and COVID-19 related stress: the mediating role of healthy lifestyle in Tabriz. Heliyon. (2023) 9:e18152. doi: 10.1016/j.heliyon.2023.e18152
57. Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. (2010) 10:1–9. doi: 10.1186/1471-244X-10-113
58. Rüsch N, Müller M, Ajdacic-Gross V, Rodgers S, Corrigan PW, Rössler W, et al. Shame, perceived knowledge and satisfaction associated with mental health as predictors of attitude patterns towards help-seeking. Epidemiol Psychiatr Sci. (2014) 23:177–87. doi: 10.1017/S204579601300036X
59. Yu Y, Liu Z-w, Hu M, Liu H-m, Yang JP, Zhou L, et al. Mental health help-seeking intentions and preferences of rural Chinese adults. PLoS ONE. (2015) 10:e0141889. doi: 10.1371/journal.pone.0141889
60. Mersha AG, Tollosa DN, Bagade T, Eftekhari P. A bidirectional relationship between diabetes mellitus and anxiety: a systematic review and meta-analysis. J Psychosom Res. (2022) 2022:110991. doi: 10.1016/j.jpsychores.2022.110991
61. Palizgir M, Bakhtiari M, Esteghamati A. Association of depression and anxiety with diabetes mellitus type 2 concerning some sociological factors. Iran Red Crescent Med J. (2013) 15:644. doi: 10.5812/ircmj.12107
62. World Health Organization. Type 2 Diabetes: Practical Targets and Treatments. Geneva: World Health Organization (2005).
63. Bjelland I, Krokstad S, Mykletun A, Dahl AA, Tell GS, Tambs K. Does a higher educational level protect against anxiety and depression? The HUNT study Social science & medicine. Soc Sci Med. (2008) 66:1334–45. doi: 10.1016/j.socscimed.2007.12.019
64. Steele LS, Dewa CS, Lin E, Lee KL. Education level, income level and mental health services use in Canada: associations and policy implications. Healthc Policy. (2007) 3:96. doi: 10.12927/hcpol.2007.19177
65. Fidan Ö, Takmak S, Zeyrek AS, Kartal A. Patients with type 2 diabetes mellitus: Obstacles in coping. J Nurs Res. (2020) 28:e105. doi: 10.1097/jnr.0000000000000379
66. Van Der Heide I, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, Uiters E. The relationship between health, education, and health literacy: results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun. (2013) 18:172–84. doi: 10.1080/10810730.2013.825668
67. Marimwe C, Dowse R. Health literacy test for limited literacy populations (HELT-LL): Validation in South Africa. Cogent Med. (2019) 6:1650417. doi: 10.1080/2331205X.2019.1650417
68. Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. (2006) 21:806–12. doi: 10.1111/j.1525-1497.2006.00539.x
69. Saeed H, Saleem Z, Naeem R, Shahzadi I, Islam M. Impact of health literacy on diabetes outcomes: a cross-sectional study from Lahore, Pakistan. Public Health. (2018) 156:8–14. doi: 10.1016/j.puhe.2017.12.005
70. Vuong QH, Napier NK. Acculturation and global mindsponge: an emerging market perspective. Int J Intercult Relat. (2015) 49:354–67. doi: 10.1016/j.ijintrel.2015.06.003
72. Vuong Q-H, Le T-T, Nguyen M-H. Mindsponge mechanism: an information processing conceptual framework. In: The Mindsponge and BMF Analytics for Innovative Thinking in Social Sciences and Humanities. Berlin: De Gruyter. (2022). p. 21–46.
73. Jin R, Wang X. “Somewhere I belong?” A study on transnational identity shifts caused by “double stigmatization” among Chinese international student returnees during COVID-19 through the lens of mindsponge mechanism. Front. Psychol. (2022) 13:1018843. doi: 10.3389/fpsyg.2022.1018843
75. Jorm AF. Mental health literacy: public knowledge and beliefs about mental disorders. Br J Psychiat. (2000) 177:396–401. doi: 10.1192/bjp.177.5.396
76. Trikkalinou A, Papazafiropoulou AK, Melidonis A. Type 2 diabetes and quality of life. World J Diab. (2017) 8:120–9. doi: 10.4239/wjd.v8.i4.120
77. Tardif I, Guénette L, Zongo A, Demers É, Lunghi C. Depression and the risk of hospitalization in type 2 diabetes patients: a nested case-control study accounting for non-persistence to antidiabetic treatment. Diabet Metab. (2022) 48:101334. doi: 10.1016/j.diabet.2022.101334
78. AlBekairy A, AbuRuz S, Alsabani B, Alshehri A, Aldebasi T, Alkatheri A, et al. Exploring factors associated with depression and anxiety among hospitalized patients with type 2 diabetes mellitus. Med Princ Pract. (2017) 26:547–53. doi: 10.1159/000484929
Keywords: mental literacy, stress, psychological status, depression, anxiety
Citation: Jafari A, Moshki M, Naddafi F, Ghelichi-Ghojogh M, Armanmehr V, Kazemi K and Nejatian M (2024) Depression literacy, mental health literacy, and their relationship with psychological status and quality of life in patients with type 2 diabetes mellitus. Front. Public Health 12:1421053. doi: 10.3389/fpubh.2024.1421053
Received: 21 April 2024; Accepted: 24 June 2024;
Published: 11 July 2024.
Edited by:
Steffen Schulz, Charité University Medicine Berlin, GermanyReviewed by:
Ni Putu Wulan Purnama Sari, Widya Mandala Catholic University Surabaya, IndonesiaAndrea Uriel De Siena, University of Naples Federico II, Italy
Copyright © 2024 Jafari, Moshki, Naddafi, Ghelichi-Ghojogh, Armanmehr, Kazemi and Nejatian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mahbobeh Nejatian, bWFoYnViZWhuZWphdGlhbkBnbWFpbC5jb20=
 Alireza Jafari
Alireza Jafari Mahdi Moshki
Mahdi Moshki Fatemehzahra Naddafi
Fatemehzahra Naddafi Mousa Ghelichi-Ghojogh3
Mousa Ghelichi-Ghojogh3 Mahbobeh Nejatian
Mahbobeh Nejatian