- Faculty of Public Health, Al-Quds University, Jerusalem, Palestine
Background: Death anxiety and maladaptive coping accompany breast cancer diagnoses. The coping mechanisms and death anxiety among Palestinian patients with breast cancer have not been studied.
Aim: To assess the prevalence of death anxiety and its relationship with coping strategies among Palestinian women with breast cancer who are treated in Beit Jala Governmental Hospital in Bethlehem.
Method: A cross-sectional design was used, and 214 breast cancer patients who visited the Beit Jala Governmental Hospital in Bethlehem were recruited. Templer's Death Anxiety Scale and the Brief COPE Scale were used. To investigate the relationship between coping strategies and death anxiety, frequency, percentages, chi-square tests, and Pearson's correlation tests were utilized.
Results: The results indicated that 58.40% of the patients experienced death anxiety. The participants who used positive reframing (adjusted odds ratio (AOR) = 1.487, p = < 0.026), self-blame (AOR = 1.309, p = < 0.023), and religion (AOR = 1.260, p = < 0.031) as coping mechanisms were more likely to experience death anxiety. Conversely, the participants who adopted substance use (AOR = 0.657, p < 0.005) and active coping (AOR = 0.629, p < 0.007) as coping strategies had a lower likelihood of experiencing death anxiety.
Conclusion: The study revealed that breast cancer patients tended to use a combination of functional and emotional coping strategies and that a significant proportion of these patients (58.4%) experienced symptoms of death anxiety. This study emphasizes the significance of screening for death anxiety and understanding the coping strategies utilized by the patients. Gaining this understanding will assist in identifying patients who need more guidance and support.
1 Introduction
Breast cancer is the most frequently diagnosed cancer in women. According to the WHO, the global breast cancer incidence in 2022 was 2.3 million, with 670,000 deaths (1). Cancer typically elicits psychological reactions characterized by traumatic stress (2) and requires treatment with extreme caution due to the negative connotation associated with the term “cancer” (2, 3). Patients who are diagnosed with cancer experience profoundly intense psychological reactions, including a sense of impending death. As a result, death anxiety is widely regarded as the most important psychological factor affecting cancer management. Death anxiety is the emotional reaction that individuals exhibit when they encounter negative thoughts associated with death (4). It can harm cancer patients' psychological wellbeing, potentially leading to mental disorders and reduced overall quality of life (5, 6). Furthermore, death anxiety has a significant effect on cancer treatment and eradication (7). Cancer patients reported moderate levels of death anxiety, with women diagnosed with breast cancer reporting higher levels (8). According to Masror Roudsary et al.'s (9) study in Iran, 79% of patients with breast cancer have a fear of death. Furthermore, a cross-sectional study conducted in Pakistan on 80 patients with breast cancer revealed that 13.8%, 51.2%, 27.5%, and 7.5% of the patients had low, medium, high, and very high levels of death anxiety, respectively (10).
A fear of death among people arises from various reasons, including identity loss, anxiety about life after death, pain and distress, and loved ones' wellbeing. Fear of death affects patients' prognoses, leading to treatment skepticism or discontinuation (11). Many studies have explored cancer patients and their families' fear of death (3, 12–15). However, it is unclear what early-stage patients experience in terms of fear of death because most published research focuses on the terminally ill (16). Shakeri et al. (3) found that death anxiety scores in patients with breast cancer was 67.5%. Women harbored apprehensions about mortality, exacerbation of their illness, loss of their future, and dependence on other people (3).
Women diagnosed with breast cancer adopt coping strategies to navigate the complex and multifaceted challenges that arise from the psychological, social, and spiritual aspects of their new life circumstances (17). They must adjust to the changes that happen every day to lessen their pain and improve their quality of life (18). Coping is the mindset and actions adopted to maintain emotional health during cancer complications (19). Researchers found that patients with critical and terminal illnesses who use coping mechanisms live longer and increase life satisfaction (20). Emotion-focused coping manages strong emotions, while problem-focused coping addresses the source of distress (21). Patients with cancer often resort to denial, alcohol or drugs, venting, self-distraction, and behavioral disengagement; these strategies make them less adaptive (17). When cancer is diagnosed, these coping strategies increase the risk of depression and a decline in self-esteem (22). Religion-based problem-solving and coping methods are more adaptive and reduce depressive symptoms (23). However, there is a lack of quantitative studies that assess coping strategies among Palestinian women diagnosed with breast cancer. According to a qualitative study, Palestinian women with breast cancer most commonly rely on social support and religion as coping strategies (24). Pre-existing coping styles, as well as supportive relationships with others, have an impact on an individual's ability to effectively cope with illness. In addition, the perception of cancer as a threat appears to promote active coping behavior (2). Conversely, cancer patients who perceive their illness as long-term, emotionally burdensome, and with more negative consequences are more likely to employ passive coping strategies (25).
Throughout their cancer treatment, many breast cancer patients suffer from various mental health issues, including but not limited to anxiety, depression, cognitive impairment, distress, poor body image, and sexual dysfunction (26). In addition, stressful events such as accepting a diagnosis, beginning treatment, learning about the prognosis, addressing side effects, preparing for a relapse, and facing an unknown future can lead to mental instability and mood disorders such as depression and anxiety (27). Studies revealed that cognitive behavioral therapy, an intervention to improve coping and communication, mindfulness-based stress reduction, and supportive psychotherapy are all potential treatments that can effectively address the psychosocial problems faced by cancer patients (27).
In Palestine, breast cancer has perpetually been highly prevalent. Breast cancer incidence was 934 in 2022, with 18.5 cases per 100,000 people and 37.4 per 100,000 women. Cancer deaths among women were 45% (28). Palestinian cancer patients may struggle with infertility, changing social roles, body image, sexual issues, and strained relationships (29, 30). Many studies have found that Arab women may hide breast cancer from friends, family, and neighbors due to social stigma (29, 30). Moreover, Arab women perceive cancer as a punishment or a divine test. The concerns center on the stigma associated with breast examination, the potential reaction of the spouse upon discovering a lump, and the impact of cultural and religious modesty (30). This may exacerbate their psychological distress and anxiety about mortality, influencing breast cancer detection and prognosis (29, 30). According to Madkhali et al. (31), Arab women with breast cancer frequently seek medical attention only at the advanced stage of the disease, with large breast lumps that are difficult to manage at home and cause intense pain.
Despite the high prevalence of breast cancer among Arab and Palestinian women, there has been little research into the relationship between specific medical conditions such as breast cancer and death anxiety. Furthermore, most previous research on this topic has focused on students (32–34).
To our knowledge, no study has examined coping mechanisms and death anxiety in Palestinian or Arab breast cancer patients. In addition, Palestinian general hospitals lack qualified mental health professionals, which may increase death anxiety among breast cancer patients due to misdiagnosis and inadequate treatment. Therefore, this study aimed to assess the prevalence of death anxiety in Palestinian women diagnosed with breast cancer. Furthermore, it sought to assess the relationship between death anxiety and sociodemographic and psychological factors along with coping strategies. Finally, it explored the factors that predict the development of death anxiety among women with breast cancer. The results of the study may help healthcare practitioners in providing effective treatment for women with breast cancer.
2 Materials and methods
This study examined death anxiety and coping strategies among Palestinian breast cancer patients at Beit Jala Governmental Hospital in Bethlehem, Palestine. A cross-sectional study was conducted using self-reported questionnaires. Participants included Palestinian women with breast cancer treated at the Beit Jala Governmental Hospital, the only government hospital in Bethlehem and a referral center for Palestinian cancer patients requiring chemotherapy. The study focused on women aged 18 and above with breast cancer, typically in stage three or four, treated in the daycare center and outpatient clinics of the hospital. Women hospitalized for breast cancer, lung cancer, or colon cancer were excluded from the study. Due to the unavailability of official statistics on the number of breast cancer patients treated at the hospital, patients with breast cancer treated from April 2016 to January 2017 were recruited using a convenience sampling method. A total of 214 women agreed to participate. The researchers distributed questionnaires to participants in the daycare center and outpatient clinics during their hospital visits.
2.1 Measures
The data were collected using a questionnaire comprising three sections and a total of 53 questions. The first section included sociodemographic factors (i.e., age, place of residence, marital status, educational level, and economic status) and psychological variables (i.e., onset of breast cancer, whether seeking psychological treatment, psychological treatment obstacles, whether receiving psychological support, and source of psychological support).
The second section used Templer's Death Anxiety Scale (Templer DAS) to assess death anxiety (35). The scale comprises 15 questions that assess absolute death anxiety, fear of patience and pain, death-related thoughts, passing of time and short life, and fear of future. Each item has two possible answers, yes or no, with 1 and 0 values, respectively, and the true response indicates participants' anxiety. The Templer DAS scores range from 0 (no death anxiety) to 15 (highest death anxiety), with a cutoff score of 6. A class interval of 0–6 indicates no death anxiety, 7–8 indicates an average level of death anxiety, and 9–15 indicates a high level of death anxiety. Studies categorize death anxiety as low (0–6) or high (7–15) (36).
The third section had the Brief COPE scale, developed by Carver and comprising 28 questions (37). It is one of the most frequently used self-reporting tools for measuring coping responses. Both cognitive and behavioral strategies of coping are included. For each category, respondents indicate whether they have used a coping response on a four-point Likert scale, where 1 indicates “I have not been doing this at all,” 2 indicates “I have been doing this a little bit,” 3 indicates “I have been doing this an average amount,” and 4 indicates “I have been doing this a lot.” The higher the score, the greater are the coping strategies used by the respondents. In addition, the coping dimensions are divided into two major categories: problem-focused strategies (i.e., active coping, planning, and use of instrumental support) and emotion-focused strategies (i.e., positive reframing, acceptance, religion, use of emotional support, and denial).
As the scale was not previously evaluated among Palestinian cancer patients, a committee of three mental health specialists evaluated it for cultural appropriateness; no changes were required. A certified medical translator reverse-translated the scale from Arabic to English after the research team translated it. The accuracy of the translation was verified by comparing the original English questionnaire with the back-translated version. A pilot test was conducted by administering the tool to 15 patients with breast cancer for verifying language clarity. Cronbach's alpha values of 0.753 for the Templer DAS and 0.73 for the Brief COPE scale indicate good reliability.
2.2 Statistical analysis
The data were analyzed using the statistical package for social sciences (SPSS) version 18.0. The relationships of sociodemographic variables and psychological factors with the Templer DAS were analyzed using frequency, percentages, and the chi-square test. Pearson's correlation coefficient (r) was employed to examine the relationships between coping strategies and death anxiety. In addition, a multivariate regression analysis was performed, and the results were obtained as an adjusted odds ratio (AOR) with a 95% confidence interval (CI). A p < 0.05 was considered a significant association.
2.3 Ethical approval and consent to participate
This study followed the Helsinki Declaration for all methods and was ethically approved by the Faculty of Public Health/ Community Mental Health Ethical Research Committee at Al Quds University (Ref No. FPH: 1-4-2016). Subsequently, a formal letter explaining the study's purpose and the questionnaire were sent to the Palestinian Ministry of Health and Beit-Jala Governmental Hospital administration for permission. Participants received an information sheet about the study's purpose and were informed about the option to not participate in the study. All participants gave written informed consent and were assured confidentiality and privacy.
3 Results
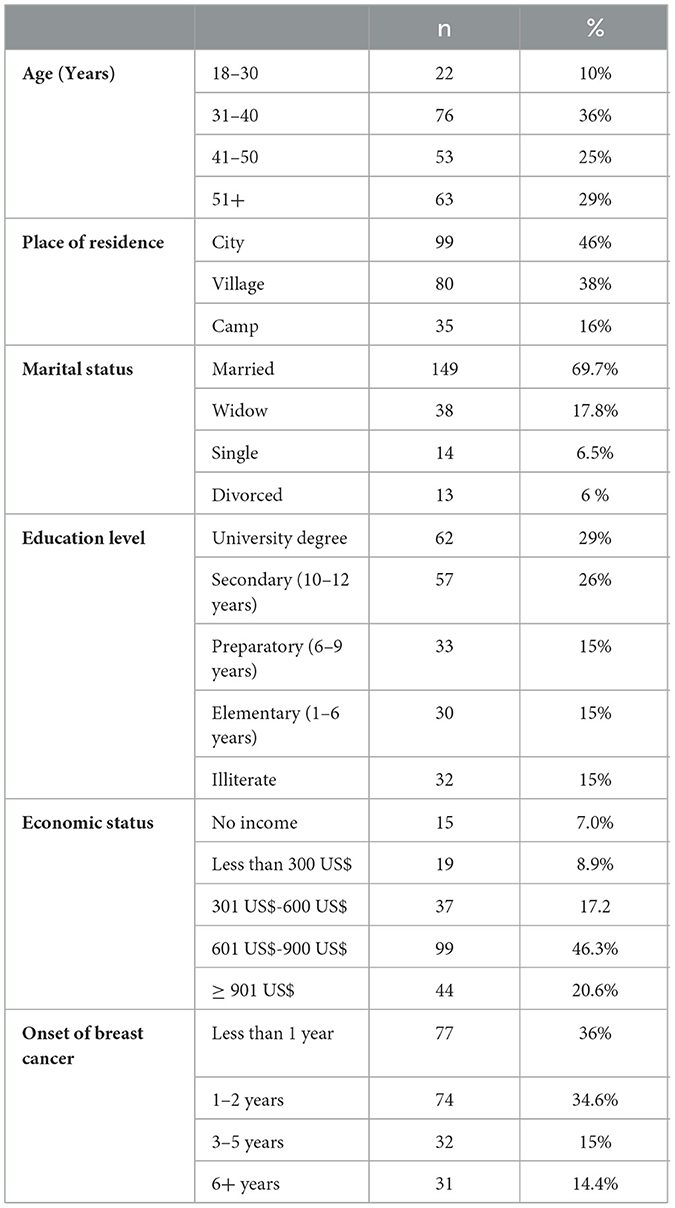
A total of 214 participants agreed to participate in the study. According to Table 1, 36% (n = 76) of the participants were aged between 31 and 40 years, while 46% (n = 99) lived in cities. Furthermore, 69.7% of the participants (n = 149) were married, and 46.3% (n = 99) earned 601–900 US$ per month. In addition, 36% (n = 77) of the participants reported that their cancer began less than a year ago.
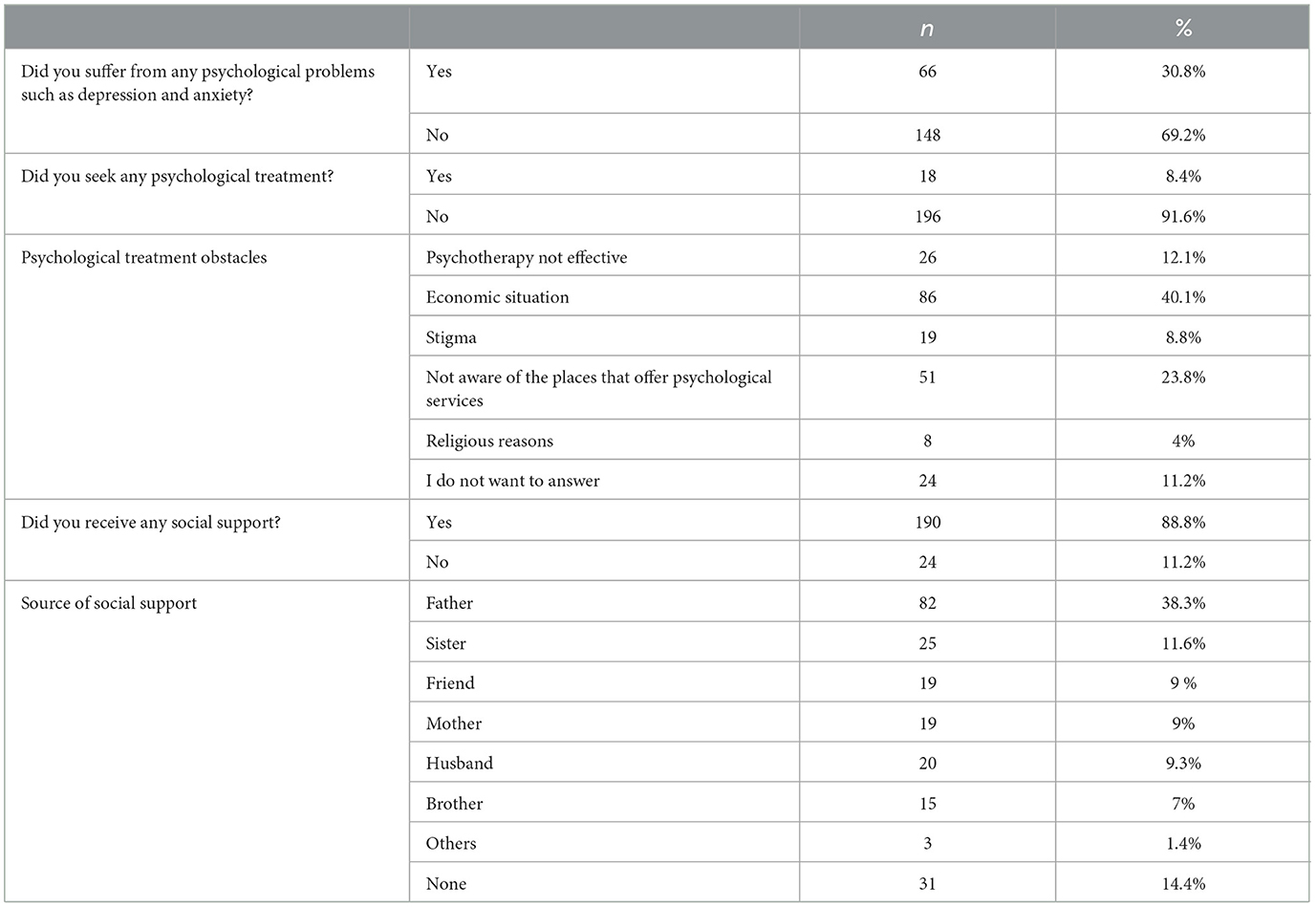
As shown in Table 2, 30.8% (n = 66) of the participants reported that they suffered from psychological problems such as depression and anxiety. The participants were discouraged from seeking therapy because 12.1% (n = 26) thought it was ineffective, 40.1% (n = 86) cited their family's financial situation, and 8.8% (n = 19) were concerned about the stigma associated with seeking therapy. When asked if they had received any social support, 11.2% (n = 24) answered no and only 9.3% (n = 20) said that they received support from their husbands.
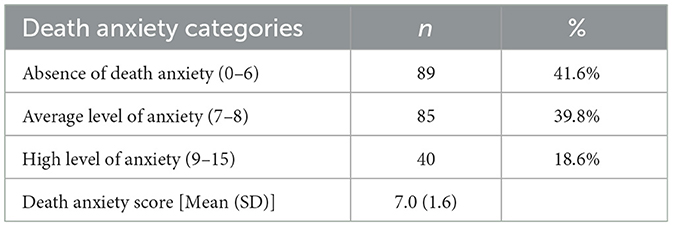
As shown in Table 3, the mean Templer DAS scores for death anxiety among breast cancer patients were moderate (mean = 7.0, standard deviation (SD) = 1.6). Furthermore, 39.8% of the participants had an average level of death anxiety, 41.6% had an absence of death anxiety, and 18.6% had high levels of death anxiety.
Moreover, as shown in Table 4, no statistically significant relationship was observed between death anxiety and sociodemographic variables, except monthly income. The participants who had no income had a higher likelihood of developing death anxiety (80%, p = 0.016), as shown in Table 4.
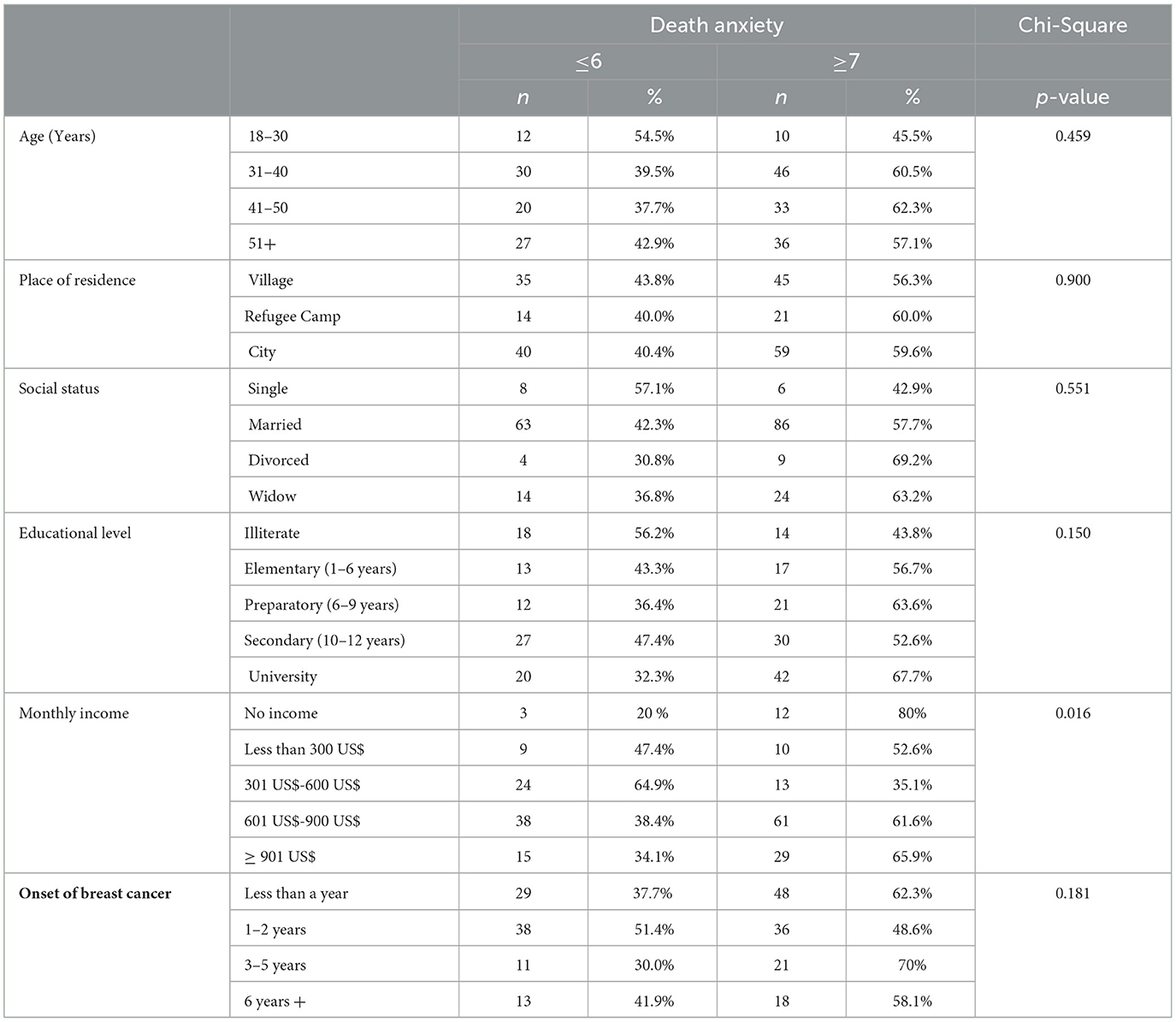
Table 4. Association between death anxiety and study sociodemographic variables as well as onset of breast cancer.
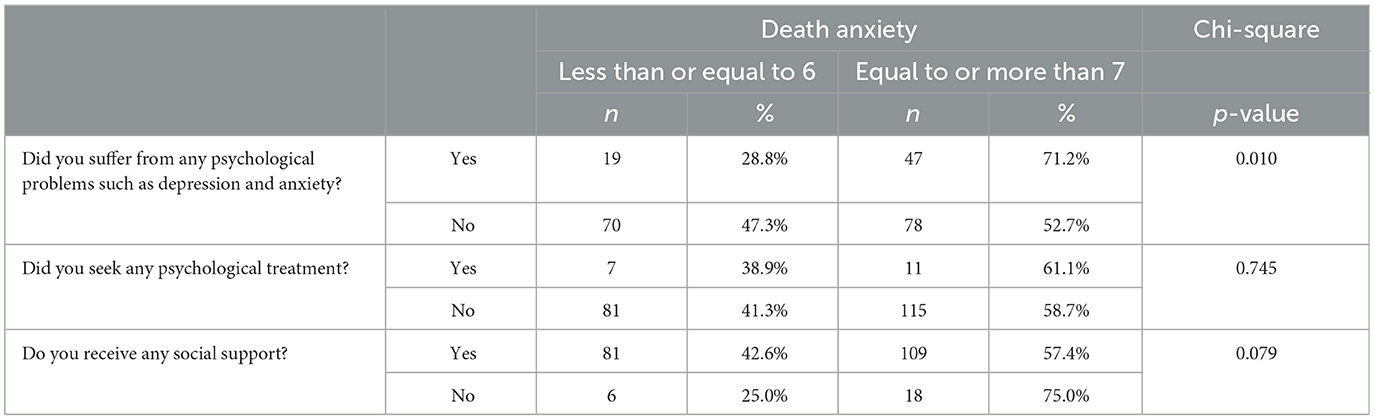
Table 5 presents a significant relationship between death anxiety and the presence of psychological problems such as depression and anxiety (71.2%, p = 0.010).
3.1 Relationship between the brief COPE scale and templer DAS
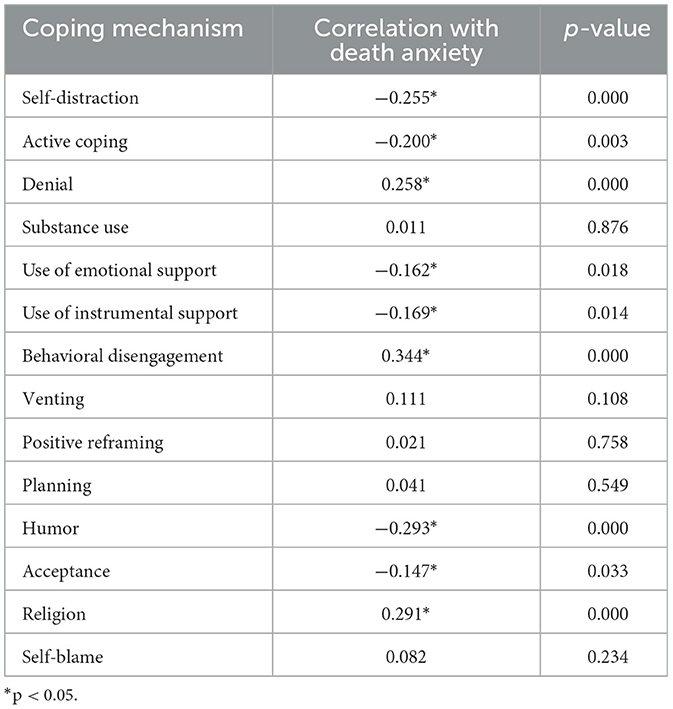
Finally, the results of Pearson's correlation test employed to examine the relationships between the application of coping mechanisms and death anxiety are presented in Table 6. The results indicate significant weak and negative correlations between death anxiety and self-distraction (r = −0.255, p < 0.000), active coping (r = −0.200, p < 0.003), use of instrumental support (r = −0.169, p < 0.014), use of emotional support (r = −0.162, p < 0.018), humor (r = −0.293, p < 0.000), and acceptance (r = −0.147, p < 0.033). Furthermore, statistically significant weak and positive correlations were observed between death anxiety and behavioral disengagement (r = 0.344, p < 0.000), religion (r = 0.291, p < 0.000), and denial (r = 0.258, p < 0.000).
3.2 multivariate logistic regression for determinants of death anxiety
Table 7 shows the factors that may contribute to the development of death anxiety. Individuals who used positive reframing (AOR = 1.487, CI: 1.049–2.107, p < 0.026), self-blame (AOR = 1.309, CI: 1.039–1.650, p < 0.023), and religion (AOR = 1.260, CI: 1.021–1.556, p < 0.031) as coping mechanisms were more likely to experience death anxiety than those who did not use these strategies. Conversely, individuals who used substances (AOR = 0.657, CI: 0.490–0.879; p < 0.005) and active coping (AOR = 0.629, CI: 0.450–0.880, p < 0.007) as coping strategies had lower likelihood of experiencing death anxiety.
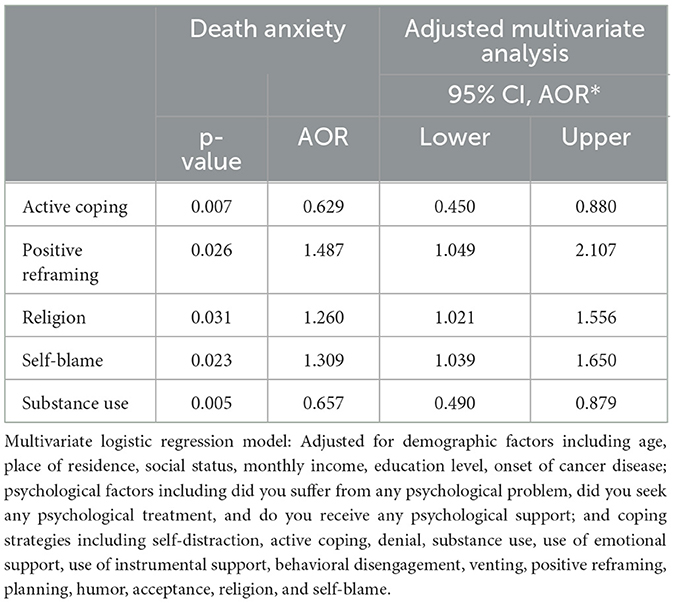
Table 7. Multivariate logistic regression model for the associations between death anxiety and demographic factors, psychological factors, and coping strategies.
4 Discussion
This study aimed to assess the prevalence of death anxiety and its relationship with coping strategies in Palestinian patients with breast cancer. The findings of this study revealed that the majority of participants (58.4%) had symptoms of death anxiety (exhibiting average to high levels of anxiety about death), with a moderate overall mean score for death anxiety of 7.0. In China, Gong et al. (38) found that women with breast cancer had an average death anxiety score of 7.72, while Salehi et al. (39) found that patients had an average death anxiety score of 9.71 ± 3.58, which was higher than the average DAS score for the general population (2.77) (7). In addition, 72.9% of patients with breast cancer reported high levels of death anxiety. According to Shakeri et al. (3), 67.5% of patients with breast cancer experienced death anxiety =. Another study conducted in Iran by Masror Roudsary et al. (9) revealed that 79% of patients with breast cancer experienced death anxiety. Furthermore, a cross-sectional study conducted on 80 breast cancer patients in Pakistan revealed that 51.2% had a medium level of anxiety about death, 27.5% had a high level of anxiety, and 7.5% had an extremely high level of anxiety (10). However, in contrast to the current study, Shakeri et al. (3) reported a prevalence of death anxiety in 67.5% of the breast cancer patients. Furthermore, Soleimani et al.'s (8) systematic review and meta-analysis revealed that death anxiety was only mild in cancer patients (6.84).
Palestinian breast cancer patients may experience high levels of death anxiety related to factors including disease progression, apprehension about their future, and becoming dependent and unable to perform daily tasks (3). Okaye et al. (40) found that oncology patients were concerned about treatment uncertainty. Death anxiety can exacerbate fatigue, sleep disturbances, anxiety, depression, and maladaptation. Individuals who suffer from death anxiety may experience distressing thoughts and difficulties in recovering. Thus, patients require psychological support to cope with death and overcome their fear (8). Palestinian cancer patients do not have access to death anxiety-relieving interventions due to a lack of medical resources and awareness. A robust death education program in Palestinian oncology hospitals and clinics can help breast cancer patients live in the present moment and meaningfully. Effective psychotherapies can help patients deal with death and fear (8).
There have been a few studies that examine the relationship between death anxiety and coping strategies in women with breast cancer (8, 41).
The current study found that participants who used positive reframing, self-blame, or religion as coping strategies were more likely to have death anxiety. By contrast, Bovero et al. (42) found that cancer patients who used coping strategies such as religion and positive reframing were more resilient in the face of death (42). These strategies helped them relieve emotional distress or alter their perception of their medical condition (43). In addition, Guo et al. (44) found that cancer patients who engaged in self-blame experienced higher levels of anxiety.
Self-blame is a maladaptive self-esteem response that involves assigning negative events to one's stable aspects, such as low ability and personal deficiencies. For individuals with a perceived incurable and life-threatening illness, avoiding self-blame as a coping mechanism is crucial. If a person believes they are responsible for their serious illness and attributes it to internal factors, they are likely to feel increased distress, guilt, and low self-esteem. This mindset can make coping with the illness even more difficult because minimizing the psychological impact of the disease is critical for long-term survival (45, 46).
In the current study, using religion as a coping mechanism increased the likelihood of experiencing death anxiety, which was unexpected. Zarzycka and Zietek (47) found that religious people were more distressed and dissatisfied with life. The lack of presence of God in their coping mechanisms resulted in cognitive dissonance (48). Furthermore, distressed cancer patients frequently blame God, causing intense rage toward God and potentially increasing their death anxiety (45). Other studies, however, found a negative correlation between religion and death anxiety (49). Many other studies in the literature review (17, 50) focused on religion's role in reducing death anxiety in breast cancer patients. Elsheshtawy et al. (41) showed that “leaving it in God's hands” helped women cope with uncertainty, illness, and death. The participants believed that God had predestined their path. One possible explanation for Palestinian women with breast cancer having higher levels of death anxiety is that they seek relief through religion but are not intrinsically religious. It has been reported that individuals with an intrinsic religious motivation (who practice their religion) have significantly lower levels of fear of death than those with an external religious motivation (who use religion for social benefits) (51). As a result, hospital and palliative counselors who work with breast cancer patients are recommended to conduct spiritual assessments that include questions about God, the afterlife, and death, as well as offer religious services to these women, to reduce death anxiety.
Furthermore, the current study found that patients who used substances and engaged in active coping strategies were less likely to experience death anxiety. Problem-focused coping involves actions aimed at resolving a problem or situation to improve adaptive adjustment, such as active coping (52). Sharma et al. (53) found that positive problem-solving is the most common coping strategy among breast cancer patients (54). Active coping strategies and problem-solving have been linked to higher moods and enhanced psychological wellbeing. In addition, avoidant coping strategies such as substance use are not always maladaptive and can have varying effects depending on the severity of a patient's symptoms and stress levels (55). Furthermore, research indicates that certain substances, such as psychedelics, may reduce death anxiety (56). However, Krasne et al. (57) reported that cancer patients who relied moderately or heavily on alcohol or drug use as a coping mechanism were more likely to experience anxiety. One explanation for this finding is that women diagnosed with breast cancer often utilize medications such as morphine, codeine, benzodiazepines, Xanax, and Valium to alleviate the side effects associated with cancer or its treatment, including pain, anxiety, and insomnia. These medications can enhance their comfort and alleviate anxiety symptoms, including death anxiety (58).
This study has certain limitations. The cross-sectional designs and convenience sampling make it difficult to establish causality. In addition, the prevalence of death anxiety was assessed using the self-reported DAS, which is not a diagnostic tool. Moreover, various cancer-related variables such as recurrence or metastasis were not evaluated. The study's focus on only Beit Jala Governmental Hospital in Bethlehem implies that the results may not be generalizable to other public or private oncology clinics and centers. Furthermore, almost seven years have passed since data collection; therefore, updated studies on death anxiety among Palestinian women with breast cancer are required. Despite these limitations, this study is the first to assess death anxiety in Palestinian breast cancer patients, making a significant contribution to the literature.
5 Conclusion
To address death anxiety among patients diagnosed with breast cancer in Palestinian hospitals, it is crucial to establish and improve mental health services. This should include psychological interventions and counseling provided by mental health professionals in oncology departments. The timely identification of patients facing difficulty in coping is critical for improving distress management and treatment adherence. A psychiatric evaluation should be performed to assess death anxiety in breast cancer patients. This assessment tool enables healthcare professionals to gain a more comprehensive understanding of the coping mechanisms required to meet the psychosocial needs of women with breast cancer.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Faculty of Public Health/Mental Health Research Ethics Committee/Al Quds University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MA: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. FS: Conceptualization, Data curation, Investigation, Methodology, Validation, Formal analysis, Writing – review & editing. IA: Formal analysis, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank all participants for their participation in the study and the Palestinian Ministry of Health teams for facilitating the study implementation. The authors also thank Mr. Mohammad Zawahra for his assistance in conducting the statistical analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Breast Cancer. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=Key%20facts,out%20of%20185%20in%202022.
2. Güner P, Sar V, Pehlivan T. Three phases of cancer in the process of mental trauma: diagnosis, treatment, survival. J Psychiatric Nurs. (2018) 9:45–54. doi: 10.14744/phd.2017.79663J
3. Shakeri B, Abdi K, Bagi M, Dalvand S, Shahriari H, Sadeghi S, et al. Systematic review and meta-analysis of death anxiety among iranian patients with cancer. Omega. (2024) 89:247–58. doi: 10.1177/00302228211070400
4. Waite S, Hyland P, Bennett K, Bentall R, Shevlin M. Testing alternative models and predictive utility of the death anxiety inventory-revised: a COVID-19 related longitudinal population based study. Acta Psychologica. (2022) 225:103539. doi: 10.1016/j.actpsy.2022.103539
5. Maraqa BN, Ahmead M. Quality of life and post-traumatic stress disorder among adult females with cancer in Palestine: a cross-sectional study. Eur J Psychotraumatol. (2021) 12:1904699. doi: 10.1080/20008198.2021.1904699
6. Su Z, Zhou Y, Han X, Pang Y, He S, Tang L. Symptom burden in advanced breast cancer patients and its association between death anxiety and psychological distress. Chin J Cancer Res. (2022) 34:298–308. doi: 10.21147/j.issn.1000-9604.2022.03.09
7. Sharif Nia H, Pahlevan Sharif S, Koocher GP, Yaghoobzadeh A, Haghdoost AA, Mar Win MT. Psychometric properties of the death anxiety scale-extended among patients with end-stage renal disease. Omega J. Death Dying. (2020) 80:380–96. doi: 10.1177/0030222817733220
8. Soleimani MA, Bahrami N, Allen KA, Alimoradi Z. Death anxiety in patients with cancer: a systematic review and meta-analysis. Eur J Oncol Nurs. (2020) 48:101803. doi: 10.1016/j.ejon.2020.101803
9. Masror Roudsary D, Lehto RH, Sharif Nia H, Kohestani D. the relationship between religious orientation and death anxiety in iranian muslim patients with cancer: the mediating role of hope. J Relig Health. (2022) 61:1437–50. doi: 10.1007/s10943-021-01487-0
10. Bibi A, Khalid MA. Death anxiety, perceived social support, and demographic correlates of patients with breast cancer in Pakistan. Death Stud. (2020) 44:787–92. doi: 10.1080/07481187.2019.1614108
11. Hong Y, Yuhan L, Youhui G. Death anxiety among advanced cancer patients: a cross-sectional survey. Support Care Cancer. (2022) 30:3531–9. doi: 10.1007/s00520-022-06795-z
12. Liu H, Liu X, Liu Z, Wang Y, Feng R, Zheng R, et al. Death anxiety and its relationship with family function and meaning in life in patients with advanced cancer-A cross-sectional survey in China. Asia Pac J Oncol Nurs. (2022) 9:100134. doi: 10.1016/j.apjon.2022.100134
13. Eggen AC, Reyners AKL, Shen G, Bosma I, Jalving M, Leighl NB, et al. Death anxiety in patients with metastatic non-small cell lung cancer with and without brain metastases. J Pain Symptom Manage. (2020) 60:422–9. doi: 10.1016/j.jpainsymman.2020.02.023
14. Yang K, Ren Y, Peng W, Wang X, Du X, Wang J, et al. Subjective well-being among Chinese breast cancer patients: the unique contributions of death anxiety, self-esteem, and social support. J Health Psychol. (2024) 29:213–24. doi: 10.1177/13591053231195391
15. Uslu-Sahan F, Terzioglu F, Koc G. Hopelessness, death anxiety, and social support of hospitalized patients with gynecologic cancer and their caregivers. Cancer Nurs. (2019) 42:373–80. doi: 10.1097/NCC.0000000000000622
16. van der Padt-Pruijsten A, Oostergo T, Leys MBL, van der Rijt CCD, van der Heide A. Hospitalisations of patients with cancer in the last stage of life. Reason to improve advance care planning? Eur J Cancer Care. (2022) 31:e13720. doi: 10.1111/ecc.13720
17. Boatemaa Benson R, Cobbold B, Opoku Boamah E, Akuoko CP, Boateng D. Challenges, coping strategies, and social support among breast cancer patients in Ghana. Adv Pub Health. (2020) 2020:1–11. doi: 10.1155/2020/4817932
18. Nipp RD, El-Jawahri A, Fishbein JN, Eusebio J, Stagl JM, Gallagher ER, et al. The relationship between coping strategies, quality of life, and mood in patients with incurable cancer. Cancer. (2016) 122:2110–6. doi: 10.1002/cncr.30025
19. Barre PV, Padmaja G, Rana S. Stress and quality of life in cancer patients: medical and psychological intervention Indian J Psychol Med. (2018) 40:232–8. doi: 10.4103/IJPSYM.IJPSYM_512_17
20. Garg R, Chauhan V, Sabreen B. Coping styles and life satisfaction in palliative care. Indian J Palliat Care. (2018) 24:491–5. doi: 10.4103/IJPC.IJPC_63_18
22. Teo I, Fingeret MC, Liu J, Chang DW. Coping and quality of life of patients following microsurgical treatment for breast cancerrelated lymphedema. J Health Psychol. (2016) 21:2983–93. doi: 10.1177/1359105315589801
23. Cieslak K, Golusinski W. Coping with loss of ability vs. emotional control and self-esteem in women after mastectomy. Rep Prac Oncol Radiotherapy. (2018) 23:168–74. doi: 10.1016/j.rpor.2018.02.002
24. Hammoudeh W, Hogan D, Giacaman R. From a death sentence to a disrupted life: palestinian women's experiences and coping with breast cancer. Qual Health Res. (2017) 27:487–96. doi: 10.1177/1049732316628833
25. Hopman P, Rijken M. Illness perceptions of cancer patients: relationships with illness characteristics and coping. Psychooncology. (2015) 2411–8. doi: 10.1002/pon.3591
26. Guimond AJ, Ivers H, Savard J. Clusters of psychological symptoms in breast cancer: is there a common psychological mechanism? Cancer Nurs. (2019) 43:343–53. doi: 10.1097/NCC.0000000000000705
27. Dinapoli L, Colloca G, Di Capua B, Valentini V. Psychological aspects to consider in breast cancer diagnosis and treatment. Curr Oncol Rep. (2021) 23:38. doi: 10.1007/s11912-021-01049-3
28. Palestinian Ministry of Health, Health Annual Report Palestine. (2022) Available online at: https://site.moh.ps/Content/Books/qEbwa3OkFYRzxTPkZMgjNqwMUHxyrrY2NPBl5lui4Fu5kUPtNtDIva_jdAtJuL53McCo1cwhdKheWcMLNwVMRo2a7EJhCs7LE5jQklgULmBUj.pdf
29. Moey SF, Sowtali SN, Mohamad Ismail MF, Hashi AA, Mohd Azharuddin NS, Che Mohamed N. Cultural, religious and socio-ethical misconceptions among muslim women towards breast cancer screening: a systematic review. Asian Pac J Cancer Prev. (2022) 23:3971–82. doi: 10.31557/APJCP.2022.23.12.3971
30. Azaiza F, Cohen M. Between traditional and modern perceptions of breast and cervical cancer screenings: a qualitative study of Arab women in Israel. Psycho- Oncology. (2008) 17:34–41. doi: 10.1002/pon.1180
31. Madkhali NA, Santin O, Noble H, Reid J. Breast health awareness in an Arabic culture: a qualitative exploration. J Adv Nurs. (2019) 75:1713–22. doi: 10.1111/jan.14003
32. Abdel-Khalek AM. Death, anxiety, and depression in Lebanese undergraduates. Omega: Journal of Death and Dying. (1998) 37:289–302. doi: 10.2190/CN5K-XF4C-2NPG-17E0
33. Abdel-Khalek AM. Death, anxiety, and depression in Kuwaiti undergraduates. Omega: J Death Dying. (2001) 42:309–20. doi: 10.2190/NJJN-FHHU-3WWQ-928V
34. Al-Sabwah MN, Abdel-Khalek AM. Religiosity and death distress in Arabic college students. Death Stud. (2006) 30:365–75. doi: 10.1080/07481180600553435
35. Templer DI. The construction and validation of a death anxiety scale. J Gen Psychol. (1970) 82:165–77. doi: 10.1080/00221309.1970.9920634
36. Moudi S, Bijani A, Tayebi M, Habibi S. Relationship between death anxiety and mental health status among nurses in hospitals affiliated to Babol University of Medical Sciences. J Babol Univ Med Sci. (2017) 19:47–53.
37. Carver CS. You want to measure coping but your protocol is too long: consider the brief cope. Int J Behav Med. (1997) 4:92–100. doi: 10.1207/s15327558ijbm0401_6
38. Gong Y, Yan Y, Yang R, Cheng Q, Zheng H, Chen Y, et al. Factors influencing death anxiety among Chinese patients with cancer: a cross-sectional study. BMJ Open. (2022) 12:e064104. doi: 10.1136/bmjopen-2022-064104
39. Salehi F, Salehi Zahabi S, Salehi Zahabi S, Mahmoudi Sh. The relationship between religious orientation and death anxiety in patients with breast cancer. Health Spiritual Med Ethics. (2017) 4:22–7.
40. Okyere Asante PG, Owusu AY, Oppong JR, Amegah KE, Nketiah-Amponsah E. The psychosocial burden of women seeking treatment for breast and cervical cancers in Ghana's major cancer hospitals. PLoS ONE. (2023) 18:e0289055. doi: 10.1371/journal.pone.0289055
41. Elsheshtawy EA, Abo-Elez WF, Ashour HS, Farouk O, El Zaafarany MI. Coping strategies in egyptian ladies with breast cancer. Breast Cancer. (2014) 8:97–102. doi: 10.4137/BCBCR.S14755
42. Bovero A, Tosi C, Botto R, Opezzo M, Giono-Calvetto F, Torta R. The spirituality in end-of-life cancer patients, in relation to anxiety, depression, coping strategies and the daily spiritual experiences: a cross-sectional study. J Relig Health. (2019) 58:2144–60 doi: 10.1007/s10943-019-00849-z
43. Sen HE, Colucci L, Browne DT. Keeping the faith: religion, positive coping, and mental health of caregivers during COVID-19. Front Psychol. (2022) 12:805019. doi: 10.3389/fpsyg.2021.805019
44. Guo YQ, Ju QM, You M, Liu Y, Yusuf A, Soon LK. Depression, anxiety and stress among metastatic breast cancer patients on chemotherapy in China. BMC Nurs. (2023) 22:33. doi: 10.1186/s12912-023-01184-1
45. Jannati Y, Nia HS, Froelicher ES, Goudarzian AH, Yaghoobzadeh A. Self-blame attributions of patients: a systematic review study. Cent Asian J Glob Health. (2020) 9:e419. doi: 10.5195/cajgh.2020.419
46. Jong J, Ross R, Philip T, Chang SH, Simons N, Halberstadt J. The religious correlates of death anxiety: a systematic review and meta-analysis. Relig Brain Behav. (2018) 8:4–20. doi: 10.1080/2153599X.2016.1238844
47. Zarzycka B, Zietek P. Spiritual growth or decline and meaning-making as mediators of anxiety and satisfaction with life during religious struggle. J Relig Health. (2019) 58:1072–86. doi: 10.1007/s10943-018-0598-y
48. Rybarski R, Bartczuk RP, Sliwak J, Zarzycka B. Religiosity and death anxiety among cancer patients: the mediating role of religious comfort and struggle. Int J Occup Med Environ Health. (2023) 36:450–64. doi: 10.13075/ijomeh.1896.02094
49. Secinti E, Wu W, Krueger EF, Hirsh AT, Torke AM, Hanna NH, et al. Relations of perceived injustice to psycho-spiritual outcomes in advanced lung and prostate cancer: examining the role of acceptance and meaning making. Psychooncology. (2022) 31:2177–84. doi: 10.1002/pon.6065
50. Salmanian K, Marashian FS. Association of coping strategies with death anxiety through mediating role of disease perception in patients with breast cancer. Archives of Breast Cancer. (2021) 8:226–32. doi: 10.32768/abc.202183226-232
51. Flannelly KJ. Religion and death anxiety. Religious Beliefs, Evol Psychiatr Mental Health in Am Religion Spirituality Health Soc Sci Approach. (2017) 1:153–64. doi: 10.1007/978-3-319-52488-7_16
52. Wu Y, Yu W, Wu X, Wan H, Wang Y, Lu G. Psychological resilience and positive coping styles among Chinese undergraduate students: a cross-sectional study. BMC Psychol. (2020) 8:79. doi: 10.1186/s40359-020-00444-y
53. Fischer R, Scheunemann J, Moritz S. Coping strategies and subjective well-being: context matters. J Happ Studies Interdisciplinary Forum Subj Well-Being. (2021) 22:3413–34. doi: 10.1007/s10902-021-00372-7
54. Sharma D, Dutta M, Kaur S, Yadav BS, Kumar K, Dahiya D. Coping strategies being practiced by the breast cancer survivors before receiving first cycle of chemotherapy. Asian Pacific J Cancer Care. (2021) 6:167–73. doi: 10.31557/apjcc.2021.6.2.167-173
55. Hofmann SG, Hay AC. Rethinking avoidance: Toward a balanced approach to avoidance in treating anxiety disorders. J Anxiety Disord. (2018) 55:14–21. doi: 10.1016/j.janxdis.2018.03.004
56. Moreton SG, Szalla L, Menzies RE, Arena AF. Embedding existential psychology within psychedelic science: reduced death anxiety as a mediator of the therapeutic effects of psychedelics. Psychopharmacology. (2019) 237:21–32. doi: 10.1007/s00213-019-05391-0
57. Krasne M, Ruddy KJ, Poorvu PD, Gelber SI, Tamimi RM, Schapira L, et al. Coping strategies and anxiety in young breast cancer survivors. Support Care Cancer. (2022) 30:9109–16. doi: 10.1007/s00520-022-07325-7
Keywords: breast cancer, fear, death anxiety, women, coping strategies, Palestine
Citation: Ahmead M, Shehadah F and Abuiram I (2024) Correlation of death anxiety with coping strategies among Palestinian women with breast cancer: a cross-sectional study. Front. Public Health 12:1420306. doi: 10.3389/fpubh.2024.1420306
Received: 19 April 2024; Accepted: 27 May 2024;
Published: 10 June 2024.
Edited by:
İsmail Toygar, Mugla University, TürkiyeReviewed by:
Aristea Ilias Ladas, University of York Europe Campus, GreeceDeniz Kacmaz, Izmir Bakircay University, Türkiye
Copyright © 2024 Ahmead, Shehadah and Abuiram. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Muna Ahmead, bXVuYWFobWVhZEB5YWhvby5jb20=
†These authors share first authorship
‡Deceased
 Muna Ahmead
Muna Ahmead Feda Shehadah†‡
Feda Shehadah†‡ Issa Abuiram
Issa Abuiram