
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 30 January 2025
Sec. Public Health and Nutrition
Volume 12 - 2024 | https://doi.org/10.3389/fpubh.2024.1417289
This article is part of the Research Topic Transforming Food Systems: Addressing Malnutrition and Inequality in Low- and Middle-Income Countries View all 18 articles
 Mahider Awoke Belay1*
Mahider Awoke Belay1* Eyob Ketema Bogale2
Eyob Ketema Bogale2 Mitiku Tefera Haile3
Mitiku Tefera Haile3 Solomon Ketema Bogale4
Solomon Ketema Bogale4 Eyob Getachew5
Eyob Getachew5 Getnet Alemu Andarge4
Getnet Alemu Andarge4 Kedir Seid6
Kedir Seid6 Gebeyehu Lakew5
Gebeyehu Lakew5 Amlaku Nigusie Yirsaw5
Amlaku Nigusie Yirsaw5 Zenebe Abebe Gebreegziabher7
Zenebe Abebe Gebreegziabher7 Birhan Ewunu Semagn8
Birhan Ewunu Semagn8 Ayenew Takele Alemu1
Ayenew Takele Alemu1Introduction: The double burden of malnutrition (DBM) at the household level has increased in sub-Saharan African countries as a result of rapid changes in global food systems and growing urbanization. The presence of overweight or obese mothers with undernourished (stunted, wasted, or underweight) children within the same household holds particular significance. However, no comprehensive study or meta-analysis has been conducted to summarize the national evidence of the double burden of malnutrition in mother–child pairs. Therefore, the purpose of this study was to determine the pooled prevalence of the double burden of malnutrition at the household level in Ethiopia in 2024.
Methods: This systematic review and meta-analysis was conducted on the prevalence of the double burden of malnutrition and associated factors among households in Ethiopia, using an advanced search of electronic databases and search engines. The standardized Joanna Briggs Institute (JBI) method was used to extract data from a Microsoft Excel spreadsheet and evaluate the quality of each article. The analysis was performed using STATA V.17. A random-effects model was used to conduct the meta-analysis. Heterogeneity was assessed using the I2 and Q tests.
Results: A total of seven publications met the inclusion criteria, including data from 56,877 and 43,770 mother–child pairs for the systematic review and meta-analysis, respectively. The pooled prevalence of the double burden of malnutrition among the mother–child pairs was 8.30% (95% confidence interval (CI): 1.51, 15.09). The heterogeneity test revealed extremely high heterogeneity (I2 = 99.91%; p = 0.00). In the subgroup analysis based on sample size, the pooled estimated prevalence of the double burden of malnutrition was high for a sample size of fewer than 1,000 mother–child pairs (11.69% (95% CI: 3.11, 20.28)). The pooled estimate from the subgroup analysis of the data collected 8 years ago was 8.61% (95% CI: 1.11, 22.33). Residence, household size, housing quality, wealth index, household food security status, mother’s age and educational status, and child’s age are some of the factors that influence the double burden of malnutrition among mother–child pairs.
Conclusion: In Ethiopia, the double burden of malnutrition among mother–child pairs is rapidly emerging. As a result, double-duty interventions should be implemented to address this issue, taking into account multiple factors at the household level.
Systematic review registration: The protocol for the systematic review and meta-analysis was registered under the registration ID CRD42024517778 with the PROSPERO (International Prospective Register of Systematic Review and Meta-analysis).
The global population is now experiencing the double burden of malnutrition (DBM). The DBM is defined as the simultaneous coexistence of malnutrition due to excess and deficiency in nutrition, including overweight, obesity, undernutrition, and nutrition-related chronic disorders (1). Multiple forms of malnutrition, ranging from undernutrition and micronutrient deficiencies to overnutrition and diet-related non-communicable diseases (NCDs), coexist in communities, families, and individuals due to rapid changes in global food systems and increased urbanization (2–4). The poorest low- and middle-income countries (LMICs) have seen a rise in the DBM, mostly as a result of increasing rates of obesity and overweight (5). One key indicator of the double burden of malnutrition at the household level is the coexistence of an overweight or obese mother and an underweight, stunted, and/or wasted child in the same household (5). Household-level DBM mainly occurs in pairs such as father–child and/or mother–child (6, 7).
Globally, the burden of undernutrition decreased from 900 million (14.7%) people in 2000 to 815 million (11%) in 2016 (3). According to recent estimates, 149.2 million children under the age of 5 were found to be stunted, 45.4 million were found to be wasted, and 38.9 million were found to be overweight (1). The pooled estimates of the DBM among children in 65 low- and middle-income countries (LMICs) were found to be 29.0, 7.5, 15.5, and 5.3% for stunting, wasting, underweight, and overweight/obesity, respectively (8). The pooled estimate of the DBM among mother–child pairs in South and Southeast Asia was reported to be 10.0% (9). In sub-Saharan African (SSA) countries, approximately 8 and 5% of households faced DBM and the triple burden of malnutrition (TBM) among mother–child pairs, respectively (10). The prevalence of the DBM among mother–child pairs was reported to be high in studies conducted in Malaysia (26%) (11), Indonesia (39%) (12), West Java (30.6%) (13), and Argentina (12%) (14). The overall weighted prevalence of the DBM was found to be 1.8% among mother–child pairs in Ethiopia, according to the Ethiopian Demographic and Health Survey (EDHS) report (15).
In addition to being caused by abnormal nutritional absorption, malnutrition (both undernutrition and overnutrition) is also characterized by persistent inflammation and recurrent infections, which may indicate an underlying immunological defect (16). The availability of inexpensive, highly processed foods and beverages, along with the introduction of activity-saving technologies, has led to significant decreases in physical activity at work, at home, and during leisure, primarily contributing to the rise in overweight and obesity (5, 17). The nutrition transition, demographic transition, and epidemiological transition of nations are the three global shifts linked to the causes of the DBM (4).
The DBM has been linked to both undernutrition and overnutrition, with the former leading to increased susceptibility to infectious diseases and impaired childhood development and the latter leading to the increased risk of non-communicable diseases and visceral fat. These health effects have resulted in financial costs for individuals and economies due to decreased productivity, lower wages, and increased medical expenses (18, 19).
Maternal, Infant and Young Child Nutrition (MIYCN) is a complementary strategy to the global action plan on NCDs, which includes targets to reduce obesity and other NCD risk factors, as well as to end all forms of malnutrition by 2030 (20–22). Ethiopia’s National Nutrition Program aims to meet the Millennium Development Goals and address the country’s high rate of malnutrition. National nutrition programs in developing countries should be proactive in addressing both overnutrition and undernutrition, taking into account all aspects of the food and nutrition environment (23). By addressing both issues, this comprehensive approach could prevent the rising issues of OW–OB and associated comorbidities before they become widespread (24). However, one of Ethiopia’s biggest public health concerns and a growing issue is the double burden of malnutrition (25–28). A scoping review was conducted in Ethiopia on the DBM; however, the study included only three publications involving mother–child pairs and did not identify the pooled components (28).
To the best of our knowledge, there are no nationally representative data on the DBM at the household level in Ethiopia. Therefore, this study aimed to determine the pooled prevalence of the DBM at the household level in Ethiopia. The findings contribute to the expanding body of literature on the pooled prevalence of the DBM and offer policymakers additional options for addressing it in Ethiopia to support efforts in achieving the Sustainable Development Goal (SDG), which aims to eliminate all forms of malnutrition by 2030.
The entire systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (29). The techniques and selection of eligible studies were presented using the PRISMA flow diagram (30). The protocol for the systematic review and meta-analysis was registered under the registration ID CRD42024517778 with PROSPERO (International Prospective Register of Systematic Review and Meta-analysis).
Studies conducted in Ethiopia on the double or dual burden of malnutrition and associated factors across all age groups within the household, studies conducted at any time, and studies published in the English language were included. These studies must have reported the prevalence of the DBM [overnutrition (overweight or obesity) or undernutrition (stunting, wasting, underweight, or thinness)] in households or mother–child or father–child pairs. Eligible study designs included cross-sectional (descriptive or analytical), case–control, and cohort studies. Original articles using either secondary data sources or original (primary) surveys, as well as articles that might be published or unpublished, were eligible for inclusion.
Studies without full texts, studies published in languages other than English, reviews, studies conducted outside of Ethiopia, and book reviews were excluded.
To prevent research duplication, PROSPERO registration was initially used to verify whether a prior, comparable study had been carried out. We developed search terms for the PubMed, Cochrane Library, and Health Inter-Network Access to Research Initiative (HINARI) databases. Gray literature was retrieved using the Google and Google Scholar search engines. From March 5 to 7, 2024, a literature search was conducted. The reference lists of the selected studies were examined by contacting experts and using communication addresses that could not be found through search engines and databases.
Article results were limited to human participants and the English language, thereby reducing the number of irrelevant studies found during preliminary searches. The following search keywords were used: “double burden of malnutrition,” “dual forms of malnutrition,” “dual burden of malnutrition,” “determinant*,” “associated factor*,” “mother–child pair*,” “father-child pair*,” “household*,” and “Ethiopia.” Boolean operators (“AND” and “OR”) and truncation (“*”) were applied during the advanced database searching.
Following a detailed search, each study was evaluated by two independent reviewers (MAB and EKB) using the abstracts and titles as a guide. The full text was also evaluated by two other independent reviewers (MTH and SKB). When Cohen’s kappa coefficient was greater than 0.6, the two reviewers’ agreement was accepted. When Cohen’s kappa coefficient was less than 0.6, the screening process was repeated (31). A dual consensus was reached, and a full-text review was conducted. Discussions resolved any disagreements during the review process.
A standardized data extraction format, derived from the Joanna Briggs Institute (JBI) data extraction format generated on a Microsoft Excel spreadsheet, was used by the two independent reviewers (EGD and GAA) to extract data from the selected studies (32, 33). A representative sample of the studies to be examined was used for a pilot test of all data extraction forms, and the results of the test were used to make corrections to the form. Finally, using the structured data extraction format, the two reviewers (KS and GL) independently extracted the following information from the full texts: author, year of publication, study design, region, residence, sample size, participants, prevalence of the DBM, and associated factors.
The quality of the studies was evaluated by the two independent reviewers (ANY and ZAG). The quality of each article, including analytical and descriptive cross-sectional research, was assessed using the standardized Joanna Briggs Institute (JBI) critical evaluation method, which included eight and nine question items, respectively, for each type of study (32, 33). The quality of the results was also evaluated by other two independent reviewers (BES and ATA) after being assessed by ANT and ZAG to check for consistency. The tools consisted of questions with a “Yes” or “No” choice, with a score of one for “Yes” answers and zero for “No” answers. The results were totaled and converted to percentages. For the meta-analysis and systematic review of the prevalence, only studies with a score of 50% or above were considered (32, 33). Low-quality studies were excluded from the review. Any discrepancies in the assessors’ scores were addressed by performing a comprehensive revision, and conflicts were settled through discussion. A funnel plot and Egger’s test were used to assess publication bias (p < 0.05 indicated statistically significant publication bias). Publication bias was addressed using the trim-and-fill method for imputation.
The studies found in the selected databases were imported into EndNote, and duplicate files were removed. The retrieved data were transferred to STATA V.17 for further analysis. Heterogeneity was evaluated using the I2 test and Q test. An I2 value above 75% and a p-value less than 0.05 for both the I2 test and Q test were considered indicative of significant heterogeneity. According to the interpretation, low, medium, and high heterogeneity were present at I2 values of 25, 50, and 75%, respectively (34). The meta-analysis was performed using a random-effects model with the restricted maximum likelihood (REML) method for the test results with heterogeneity. Subgroup and sensitivity analyses were conducted to investigate the potential causes of heterogeneity. A forest plot for proportion with a 95% confidence interval (CI) was used to present the findings of the meta-analysis. Tables and texts were used to display the results of the systematic review and meta-analysis.
During the database search, a total of 1,722 articles were retrieved from PubMed (776), the Cochrane Library (89), HINARI (35), Google Scholar (518), and Google (304). Of these, 122 duplicate results were removed and 1,574 articles were excluded after screening the titles and abstracts. Finally, we assessed the full texts of the 26 studies for eligibility, and 19 more were excluded based on the inclusion criteria. The remaining seven articles were considered for the systematic review (15, 26, 35–38). One study included two eligible outcome variables and was conducted in Addis Ababa and the rural area of Kersa district in the Oromia region (26). Of the seven studies, six were used to estimate the pooled prevalence of the DBM among households in Ethiopia. One study was excluded from the meta-analysis because it did not report the outcome variable (37) (Figure 1).
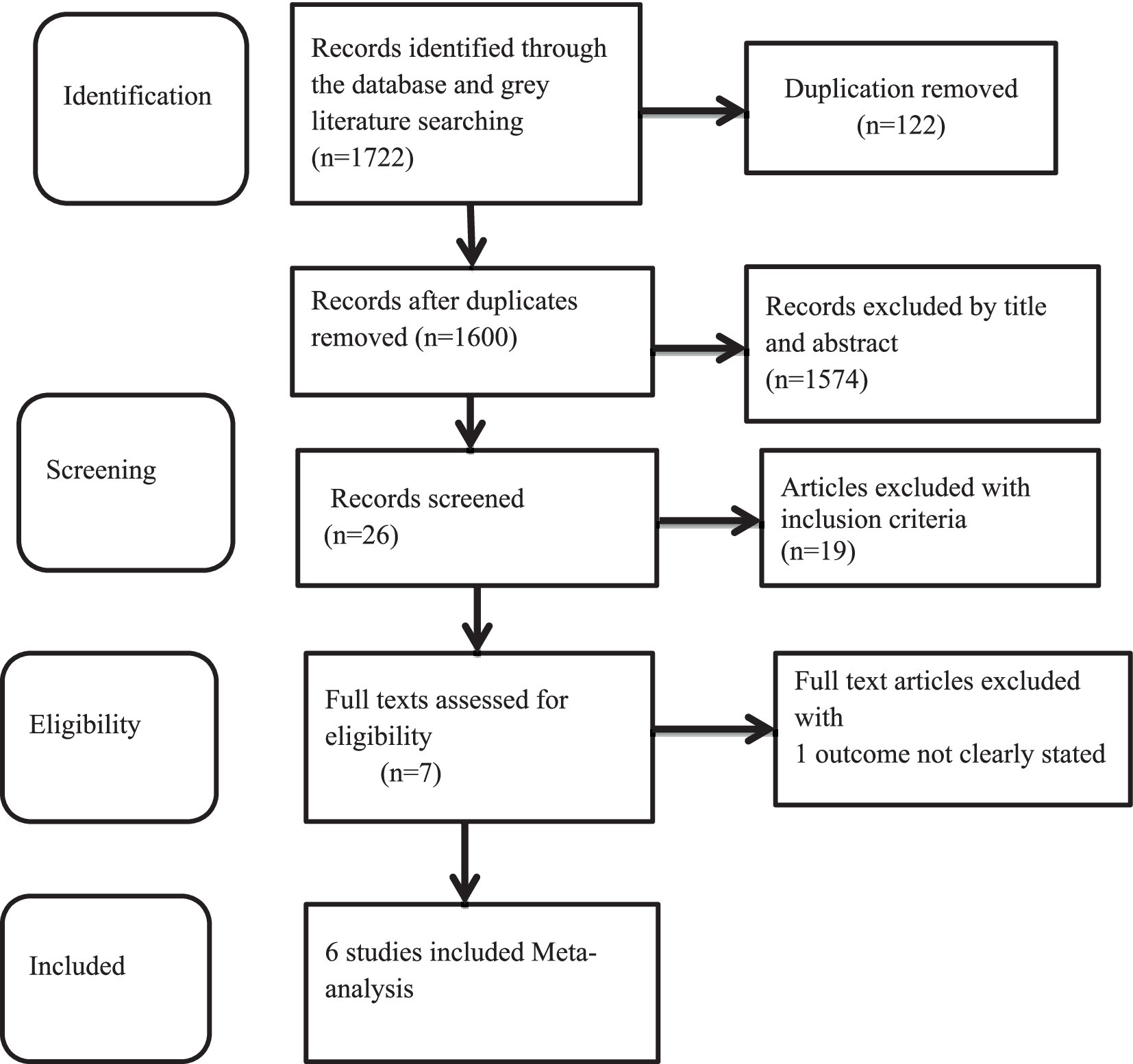
Figure 1. Flow diagram of the studies included in the review of the DBM among mother–child pairs in households in Ethiopia, 2024.
A total of 56,877 and 43,770 mother–child pairs were included in the analysis for the systematic review and meta-analysis, respectively. All studies were cross-sectional. The sample sizes ranged from 577 (35) to 33,454 (38). Three studies used secondary data that were further analyzed by the Ethiopian Demographic and Health Survey (EDHS), conducted in both urban and rural parts of the country (15, 35, 38). The other studies were conducted in Bahir Dar, the capital city of the Amhara region (36); Addis Ababa, the capital city of Ethiopia; and the rural area of Kersa district, Oromia region (26). The highest prevalence of the DBM was reported in the national data of the EDHS 2016, with 22.8% of mothers being overweight or obese with stunted children (35). Similarly, the lowest prevalence (1.52) of the DBM among the mother–child pairs was recorded in the national data of the EDHS 2000–2016 (38) (Table 1).
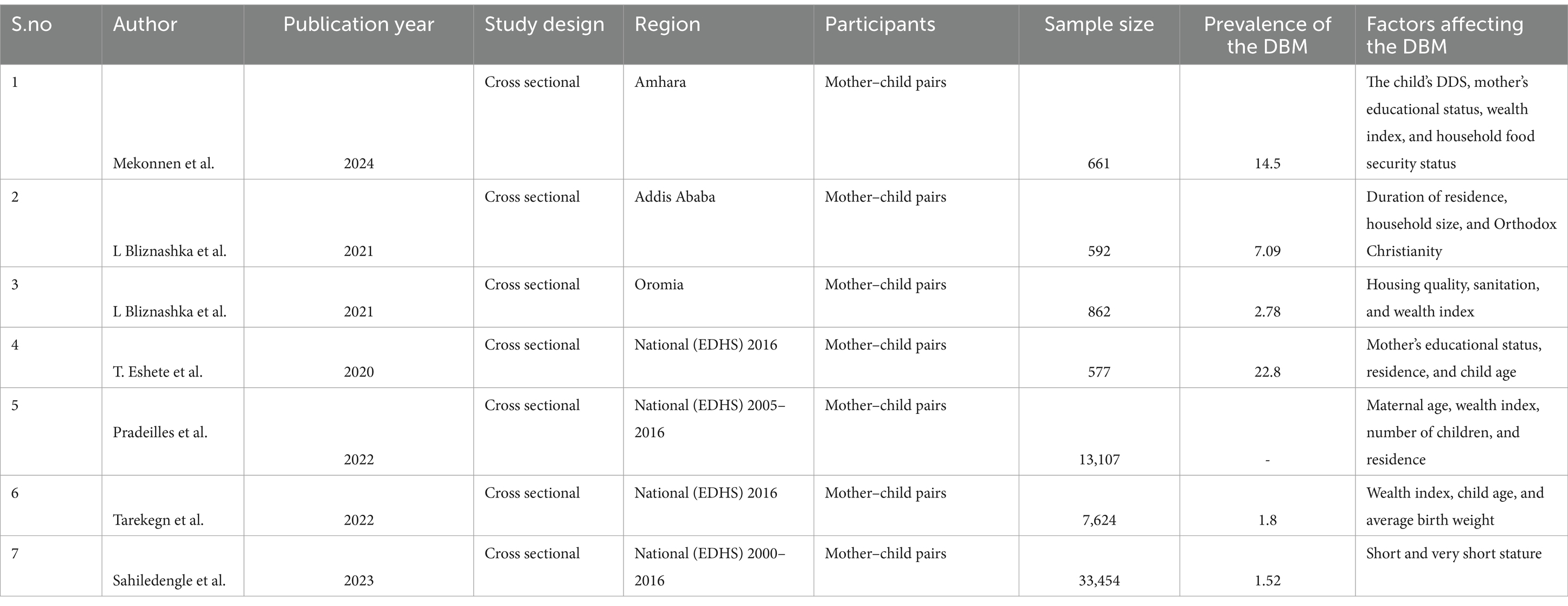
Table 1. Summary of the included studies on the DBM among mother–child pairs in households in Ethiopia, 2024.
A total of six studies were included to estimate the pooled prevalence of the DBM among mother–child pairs in households in Ethiopia. Due to the presence of heterogeneity, a random-effects model was employed, and the pooled prevalence of the DBM among the mother–child pairs was 8.30 (95% CI: 1.51, 15.09). Therefore, subgroup analyses were conducted to explain some of the possible causes of heterogeneity. The heterogeneity test for the pooled estimates of the DBM was very high (I2 = 99.91% and p = 0.00). Subgroup analysis was conducted using sample size and the data collection period. The pooled estimated prevalence of the DBM was high for a sample size of fewer than 1,000 mother–child pairs [11.69% (95% CI: 3.11, 2028)]. The heterogeneity test was also very high (I2 = 98.52%, p = 0.00). The pooled estimated prevalence of the DBM for the subgroup analysis with a sample size greater than 1,000 mother–child pairs was low [1.63 (95% CI: 1.36, 1.89)]. The heterogeneity test result for this subgroup analysis was categorized as moderate (I2 = 64.72%, p = 0.09). The pooled estimates of the DBM among the mother–child pairs for the subgroup analysis of the data collection period within 8 years and the data collected 8 years ago were relatively similar: 8.04 (95% CI: 1.35, 14.72) and 8.61 (1.11, 22.33), respectively. The heterogeneity test was very high for both time points (I2 = 97.36, p = 0.000 and I2 = 99.58, p = 0.00 for data collected within 8 years and 8 years ago, respectively) (Figures 2–4).
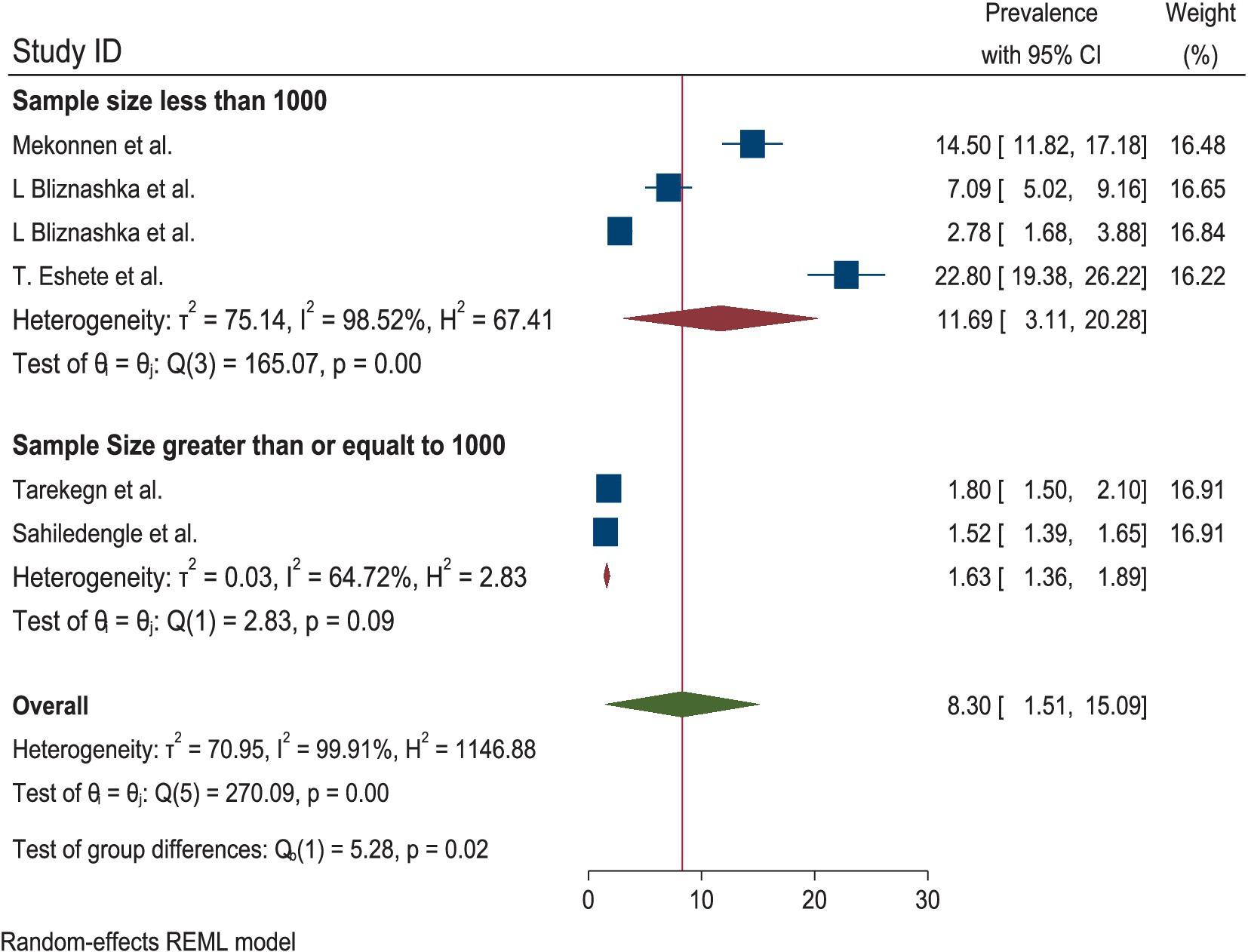
Figure 3. Subgroup analysis by sample size of the DBM among the mother–child pairs in households in Ethiopia, 2024.
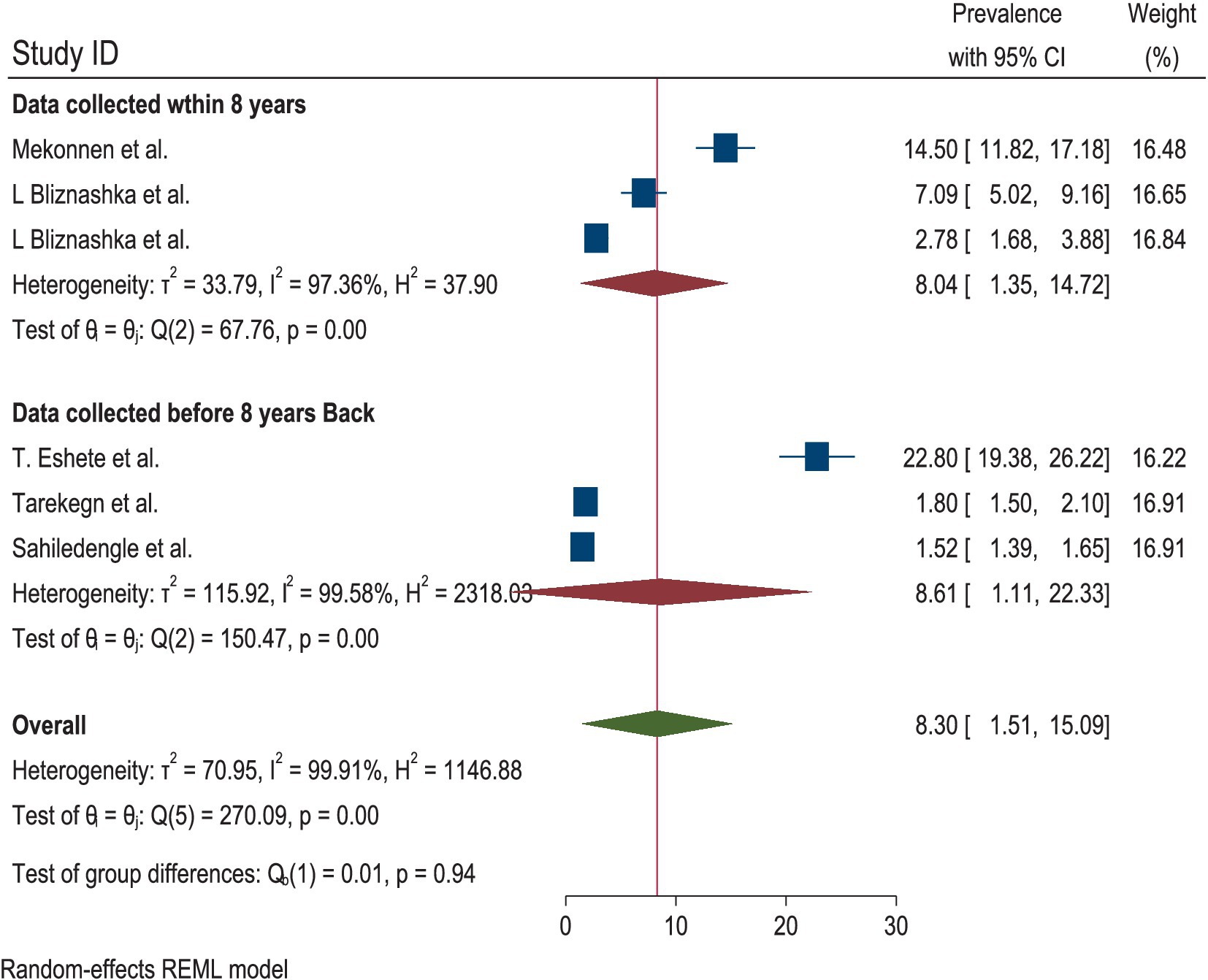
Figure 4. Subgroup analysis by the date of the data collection period for the DBM among the mother–child pairs in households in Ethiopia, 2024.
The quality score of all studies was above 80%. The funnel plot displayed an asymmetric distribution, and the Egger’s test yielded a significant result (Prob >|z| = 0.0000), suggesting the presence of publication bias (Figure 5; Table 2).
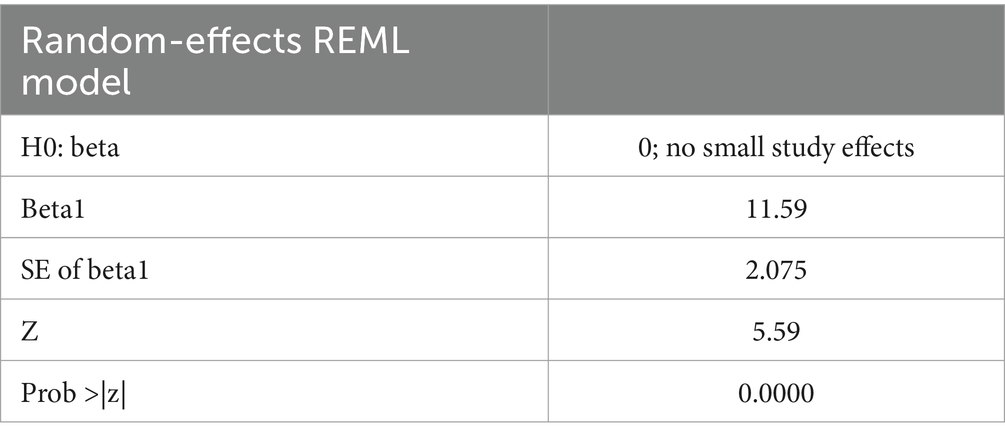
Table 2. Results of the regression-based Egger’s test for small study effects, objectively indicating the presence of publication bias.
Publication bias was reduced using the trim-and-fill method for analyzing publication bias, with the imputation of zero (0) studies. After imputation, the funnel plot appeared symmetric (Table 3; Figure 6). The sensitivity analysis of the studies showed that no findings affected the overall pooled prevalence, and the p-value remained significant (Figure 7).
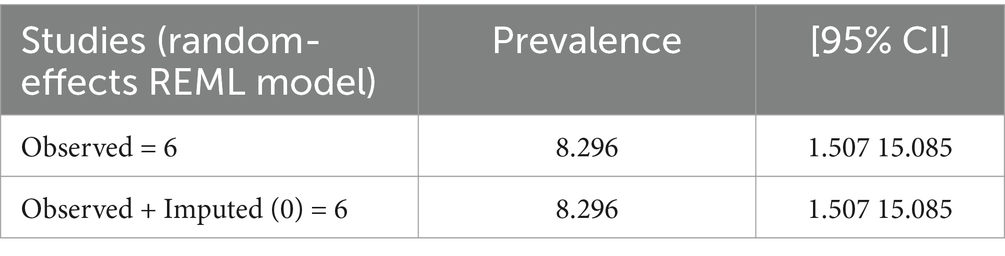
Table 3. Non-parametric trim-and-fill analysis of publication bias for the pooled estimates of the DBM among the mother–child pairs in households in Ethiopia, 2024.
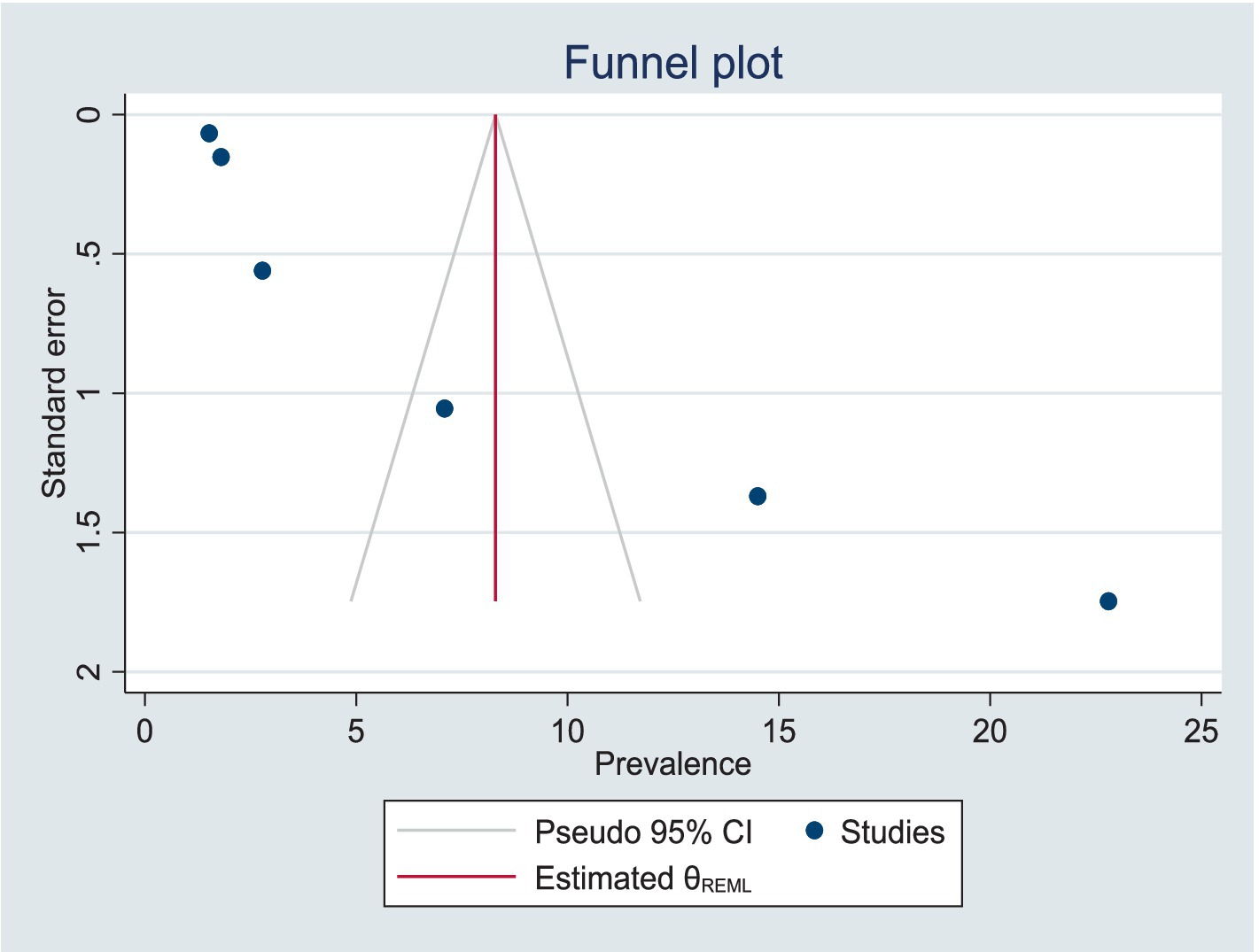
Figure 6. Symmetric presentation of the data after the trim-and-fill method for the analysis of publication bias.
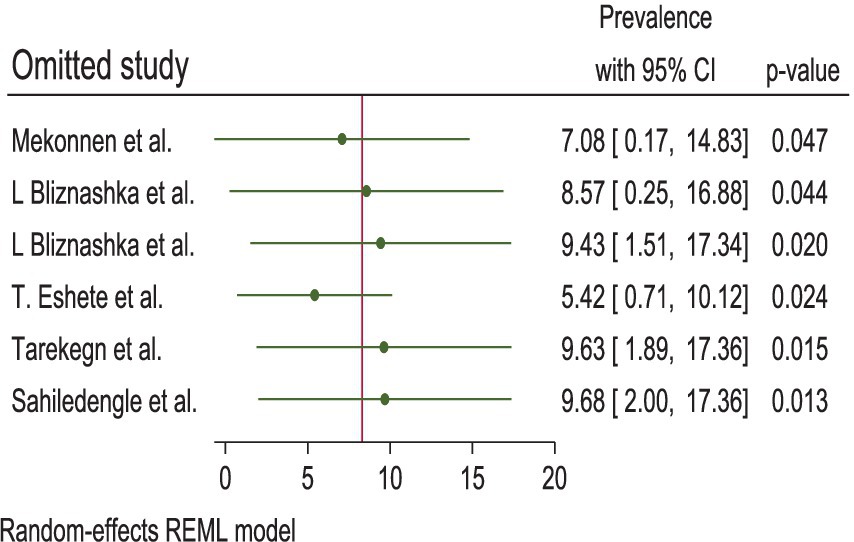
Figure 7. The sensitivity test of the pooled estimates of DBM among mother–child pairs at households in Ethiopia, 2024.
The factors affecting the DBM among mother–child pairs included the duration of residence, household size, Orthodox Christianity, housing quality, sanitation (26), child’s DDS, household food security status (36), mother’s educational status (35, 36), residence (35, 37), maternal age, number of children (37), child age (15, 35), average birth weight (15), wealth index (15, 35–37), and short and very short stature (38). We did not estimate the pooled factors for the DBM among the mother–child pairs in Ethiopia because of the absence of common factors and consistent categories across the retrieved studies.
According to the random-effects model, the pooled prevalence of the DBM among the mother–child pairs in households in Ethiopia was 8.30 (95% CI: 1.51, 15.09). The heterogeneity test for the pooled estimates was very high (I2 = 99.91% and p = 0.00). Regarding the subgroup analysis, the pooled prevalence of the DBM was higher in the studies with a sample size of fewer than 1,000 mother–child pairs (11.69% (95% CI: 3.11, 2028)). The heterogeneity test was also very high (I2 = 98.52%, p = 0.00). The pooled estimates from the subgroup analysis of the data collected within 8 years and 8 years ago were relatively similar: 8.04 (95% CI: 1.35, 14.72) and 8.61 (1.11, 22.33), respectively.
In line with the current study, research conducted in various countries has shown the coexistence of overweight or obese mothers with stunted, underweight, or wasted children in households. These studies include those from Ghana (14.2%) (39), sub-Saharan Africa (8%) (10), Bangladesh (6.4%) (40), South and Southeast Asia (12.0%) (9), Colombia (7.8%) (41), Argentina (12%) (14), India (6%) (42), Mexico (8.1%) (43), Philippines (4.3%) (7), Brazil (2.6%) (44), Tanzania (5.6%) (45), and Cameroon (7.7%) (46). Similarly, the DBM prevalence was 4.10, 1.54, 3.93, and 5.54% in Bangladesh, Nepal, Pakistan, and Myanmar (47), respectively. The similarity across these studies may reflect the phenomenon of nutrition transition; the DBM has increased in the poorest low- and middle-income countries. Overweight and obesity primarily increase due to rapid changes in the food system and the availability of cheap processed beverages and foods in LMIC, as well as an increase in leisure-related activities and a reduction in physical activities.
However, the findings of the current study were lower compared to those of studies conducted in Malaysia (26%) (11), Indonesia (39%) (12), West Java (30.6%) (13), Maharashtra (19.7%) (48), Cameroon (16.5%) (46), and Bangladesh (24.5 and 19.8%), where overweight mothers had stunted and underweight children (49). The difference in the result may be due to the current study’s pooled estimates from six different studies, whereas the other studies reported single instances of overweight or obese mothers concurrently with a stunted, wasted, or underweight child. In addition, the difference in the results may be due to variations in the study area, sociodemographic and socioeconomic characteristics, residence, sample size, and study time.
The factors affecting the DBM among the mother–child pairs were identified as the duration of residence, household size, Orthodox Christianity, housing quality, sanitation (26), child’s DDS, household food security status (36), mother’s educational status (35, 36), residence (35, 37), maternal age, number of children (37), child age (15, 35), average birth weight (15), wealth index (15, 35–37), and short and very short stature (38). Since the transition to energy-dense foods, soft drinks, and processed foods leads to increased overnutrition (overweight, obesity, and/or non-communicable diseases), the opposite—dietary inadequacy—aggravates micronutrient deficiencies and undernutrition (stunting, wasting, and underweight).
The findings of the current study reveal that the prevalence of the double burden of malnutrition among mother–child pairs in households in Ethiopia is emerging as a significant public health issue. Therefore, double-duty interventions should be implemented to address the double burden of malnutrition, taking into account various risk factors at the household level. Some of the factors affecting the double burden of malnutrition at the household level included residence, child DDS, wealth index, child and maternal age, educational status of the mother, mother’s stature, average birth weight of the child, household size, number of children, sanitation, and household food security status. Therefore, double-duty interventions, programs, and policies should be implemented to concurrently address the double burden of malnutrition—undernutrition (underweight, wasting, and stunting) and overnutrition (overweight, or obesity)—taking into account these various factors at the household level.
The policy aims to promote, protect, and encourage healthy food choices through legislative measures, communication, and capacity building. As the prevalence of households affected by the double burden of malnutrition continues to rise, the importance of investigating this issue will grow, driving further research in the future. Promoting affordable, well balanced, and healthy meals that align with cultural customs and local food production, along with encouraging the habit of physical exercise, appears to be one of the key strategies for preventing the double burden of malnutrition. The limitations of this study include the small number of studies conducted in Ethiopia, significant heterogeneity, publication bias, and the fact that the available studies for the systematic review and meta-analysis were all cross-sectional. These findings offer policymakers a strategy to support efforts toward achieving the Sustainable Development Goal (SDG) in Ethiopia, which aims to eliminate all forms of malnutrition by 2030.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
MB: Writing – original draft, Writing – review & editing. EB: Writing – original draft, Writing – review & editing. MH: Writing – original draft, Writing – review & editing. SB: Writing – original draft, Writing – review & editing. EG: Writing – original draft, Writing – review & editing. GA: Writing – original draft, Writing – review & editing. KS: Writing – original draft, Writing – review & editing. GL: Writing – original draft, Writing – review & editing. AY: Writing – original draft, Writing – review & editing. ZG: Writing – original draft, Writing – review & editing. BS: Writing – original draft, Writing – review & editing. AA: Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
DBM, Double Burden of Malnutrition; DDS, Dietary Diversity Score; EDHS, Ethiopian Demographic and Health Survey; HINARI, Health InterNetwork Access to Research Initiative; JBI, Joanna Briggs Institute; LMIC, Low and Middle-Income Countries; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-analysis.
1. Khan, Z, and Ali, A. Global food insecurity and its association with malnutrition. Emerg Chall Agric Food Sci. (2023) 2:3–4. doi: 10.9734/bpi/mono/978-81-19217-36-6/CH1
2. Davis, JN, Oaks, BM, and Engle-Stone, R. The double burden of malnutrition: A systematic review of operational definitions. Curr Dev Nutr. (2020) 4:nzaa127. doi: 10.1093/cdn/nzaa127
3. Prentice, AM. The double burden of malnutrition in countries passing through the economic transition. Ann Nutr Metab. (2018) 72:47–54. doi: 10.1159/000487383
4. Moh, MH, Mya, O, Sandar, T, Thidar, K, Wah Wah, W, and Su Su, H. The double burden of malnutrition. Food and Nutrition. (2012) 12.
5. Popkin, BM, Corvalan, C, and Grummer-Strawn, LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. (2020) 395:65–74. doi: 10.1016/S0140-6736(19)32497-3
6. Bose, A, Mondal, N, and Sen, J. Household levels of double burden of malnutrition in low–middle-income countries: a review. J Anthropol Surv India. (2022) 71:125–60. doi: 10.1177/2277436X211043628
7. Gaupholm, J, Dodd, W, Papadopoulos, A, and Little, M. Exploring the double burden of malnutrition at the household level in the Philippines: analysis of National Nutrition Survey data. PLoS One. (2023) 18:e0288402. doi: 10.1371/journal.pone.0288402
8. Akombi, BJ, Chitekwe, S, Sahle, BW, and Renzaho, AM. Estimating the double burden of malnutrition among 595,975 children in 65 low-and middle-income countries: a meta-analysis of demographic and health surveys. Int J Environ Res Public Health. (2019) 16:2886. doi: 10.3390/ijerph16162886
9. Biswas, T, Townsend, N, Magalhaes, RS, Hasan, M, and Mamun, A. Patterns and determinants of the double burden of malnutrition at the household level in south and Southeast Asia. Eur J Clin Nutr. (2021) 75:385–91. doi: 10.1038/s41430-020-00726-z
10. Christian, AK, and Dake, FA. Profiling household double and triple burden of malnutrition in sub-Saharan Africa: prevalence and influencing household factors. Public Health Nutr. (2022) 25:1563–76. doi: 10.1017/S1368980021001750
11. Wong, CY, Zalilah, MS, Chua, EY, Norhasmah, S, Chin, YS, and Siti Nur’Asyura, A. Double-burden of malnutrition among the indigenous peoples (orang Asli) of peninsular Malaysia. BMC Public Health. (2015) 15:680. doi: 10.1186/s12889-015-2058-x
12. Lowe, C, Kelly, M, Sarma, H, Richardson, A, Kurscheid, JM, Laksono, B, et al. The double burden of malnutrition and dietary patterns in rural Central Java, Indonesia. Lancet Reg Health West Pac. (2021) 14:100205. doi: 10.1016/j.lanwpc.2021.100205
13. Sekiyama, M, Jiang, HW, Gunawan, B, Dewanti, L, Honda, R, Shimizu-Furusawa, H, et al. Double burden of malnutrition in rural West Java: household-level analysis for father-child and mother-child pairs and the association with dietary intake. Nutrients. (2015) 7:8376–91. doi: 10.3390/nu7105399
14. Bassete, M, Romaguera, D, Giménez, M, Lobo, M, and Samman, N. Prevalence and determinants of the dual burden of malnutrition at the household level in Puna and Quebrada of Humahuaca, Jujuy, Argentina. Nutr Hosp. (2014) 29:322–30. doi: 10.3305/nh.2014.29.2.7075
15. Tarekegn, BT, Assimamaw, NT, Atalell, KA, Kassa, SF, Muhye, AB, Techane, MA, et al. Prevalence and associated factors of double and triple burden of malnutrition among child-mother pairs in Ethiopia: spatial and survey regression analysis. BMC Nutr. (2022) 8:34. doi: 10.1186/s40795-022-00528-5
16. Bourke, CD, Berkley, JA, and Prendergast, AJ. Immune dysfunction as a cause and consequence of malnutrition. Trends Immunol. (2016) 37:386–98. doi: 10.1016/j.it.2016.04.003
17. Batal, M, Deaconu, A, and Steinhouse, L. The nutrition transition and the double burden of malnutrition In: Nutritional health: strategies for disease prevention. Switzerland: Springer (2023). 33–44.
18. Nugent, R, Levin, C, Hale, J, and Hutchinson, B. Economic effects of the double burden of malnutrition. Lancet. (2020) 395:156–64. doi: 10.1016/S0140-6736(19)32473-0
19. Seifu, BL, Mare, KU, Legesse, BT, and Tebeje, TM. Double burden of malnutrition and associated factors among women of reproductive age in sub-Saharan Africa: a multilevel multinomial logistic regression analysis. BMJ Open. (2024) 14:e073447. doi: 10.1136/bmjopen-2023-073447
20. Ramanujam, N, and Richardson, SB. Ending child malnutrition under SDG 2: the moral imperative for global solidarity and local action. Soc Altern. (2018) 37:18–24.
21. Bennett, JE, Stevens, GA, Mathers, CD, Bonita, R, Rehm, J, Kruk, ME, et al. NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. (2018) 392:1072–88. doi: 10.1016/S0140-6736(18)31992-5
22. International Food Policy Research Institute (IFPRI). Series Name: Global Nutrition Report. Washington, D.C.: International Food Policy Research Institute (IFPRI) (2016).
23. Tekle, DY, Rosewarne, E, Santos, JA, Trieu, K, Buse, K, Palu, A, et al. Do food and nutrition policies in Ethiopia support the prevention of non-communicable diseases through population-level salt reduction measures? A policy content analysis. Nutrients. (2023) 15:1745. doi: 10.3390/nu15071745
24. Zello, GA. National nutrition programs in emerging countries: coping with the double burden of malnutrition and obesity in Ethiopia. Can J Diabetes. (2015) 39:S4. doi: 10.1016/j.jcjd.2015.01.023
25. Taklual, W, Baye, S, Mekie, M, and Andualem, T. Double burden of malnutrition among female adolescent students in Bahir Dar City, Amhara, Ethiopia. Biomed Res Int. (2020) 2020:6249524. doi: 10.1155/2020/6249524
26. Bliznashka, L, Blakstad, MM, Berhane, Y, Tadesse, AW, Assefa, N, Danaei, G, et al. Household-level double burden of malnutrition in Ethiopia: a comparison of Addis Ababa and the rural district of Kersa. Public Health Nutr. (2021) 24:6354–68. doi: 10.1017/S1368980021003700
27. Gezaw, A, Melese, W, Getachew, B, and Belachew, T. Double burden of malnutrition and associated factors among adolescent in Ethiopia: A systematic review and meta-analysis. PLoS One. (2023) 18:e0282240. doi: 10.1371/journal.pone.0282240
28. Getacher, L, Ademe, BW, and Belachew, T. Understanding the national evidence on the double burden of malnutrition in Ethiopia for the implications of research gap identifications: a scoping review. BMJ Open. (2023) 13:e075600. doi: 10.1136/bmjopen-2023-075600
29. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. (2021) 134:103–12. doi: 10.1016/j.jclinepi.2021.02.003
30. Park, HY, Suh, CH, Woo, S, Kim, PH, and Kim, KW. Quality reporting of systematic review and meta-analysis according to PRISMA 2020 guidelines: results from recently published papers in the Korean journal of radiology. Korean J Radiol. (2022) 23:355–69. doi: 10.3348/kjr.2021.0808
31. Jacobson, E, Conboy, L, Tsering, D, Shields, M, McKnight, P, Wayne, PM, et al. Experimental studies of inter-rater agreement in traditional Chinese medicine: a systematic review. J Altern Complement Med. (2019) 25:1085–96. doi: 10.1089/acm.2019.0197
32. Munn, Z, Tufanaru, C, and Aromataris, E. JBI's systematic reviews: data extraction and synthesis. AJN Am J Nurs. (2014) 114:49–54. doi: 10.1097/01.NAJ.0000451683.66447.89
33. Bui, DDA, Del Fiol, G, Hurdle, JF, and Jonnalagadda, S. Extractive text summarization system to aid data extraction from full text in systematic review development. J Biomed Inform. (2016) 64:265–72. doi: 10.1016/j.jbi.2016.10.014
34. Stogiannis, D, Siannis, F, and Androulakis, E. Heterogeneity in meta-analysis: a comprehensive overview. Int J Biostatist. (2024) 20:169–99. doi: 10.1515/ijb-2022-0070
35. Eshete, T, Kumera, G, Bazezew, Y, Marie, T, Alemu, S, and Shiferaw, K. The coexistence of maternal overweight or obesity and child stunting in low-income country: further data analysis of the 2016 Ethiopia demographic health survey (EDHS). Sci Afr. (2020) 9:e00524. doi: 10.1016/j.sciaf.2020.e00524
36. Mekonnen, S, Birhanu, D, Menber, Y, Gebreegziabher, ZA, and Belay, MA. Double burden of malnutrition and associated factors among mother–child pairs at household level in Bahir Dar City, Northwest Ethiopia: community based cross-sectional study design. Front Nutr. (2024) 11:1340382. doi: 10.3389/fnut.2024.1340382
37. Pradeilles, R, Irache, A, Norris, T, Chitekwe, S, Laillou, A, and Baye, K. Magnitude, trends and drivers of the coexistence of maternal overweight/obesity and childhood undernutrition in Ethiopia: evidence from demographic and health surveys (2005-2016). Mater Child Nutr. (2022) 20:e13372. doi: 10.1111/mcn.13372
38. Sahiledengle, B, Mwanri, L, and Agho, KE. Association between maternal stature and household-level double burden of malnutrition: findings from a comprehensive analysis of Ethiopian demographic and health survey. J Health Popul Nutr. (2023) 42:7. doi: 10.1186/s41043-023-00347-9
39. Kushitor, SB, Owusu, L, and Kushitor, MK. The prevalence and correlates of the double burden of malnutrition among women in Ghana. PLoS One. (2020) 15:e0244362. doi: 10.1371/journal.pone.0244362
40. Islam, MS, Mahfuz, M, Fahim, SM, Ahmed, T, and Biswas, T. Double burden of malnutrition among mother-child pairs of Bangladesh: prevalence and socio-demographic determinants. Vol. 10. London, UK: BMC Nutrition (2018).
41. Sansón-Rosas, AM, Bernal-Rivas, J, Kubow, S, Suarez-Molina, A, and Melgar-Quiñonez, H. Food insecurity and the double burden of malnutrition in Colombian rural households. Public Health Nutr. (2021) 24:4417–29. doi: 10.1017/S1368980021002895
42. Patel, R, Srivastava, S, Kumar, P, and Chauhan, S. Factors associated with double burden of malnutrition among mother-child pairs in India: a study based on National Family Health Survey 2015–16. Child Youth Serv Rev. (2020) 116:105256. doi: 10.1016/j.childyouth.2020.105256
43. Félix-Beltrán, L, Macinko, J, and Kuhn, R. Maternal height and double-burden of malnutrition households in Mexico: stunted children with overweight or obese mothers. Public Health Nutr. (2021) 24:106–16. doi: 10.1017/S136898002000292X
44. Gubert, MB, Spaniol, AM, Segall-Corrêa, AM, and Pérez-Escamilla, R. Understanding the double burden of malnutrition in food insecure households in Brazil. Matern Child Nutr. (2017) 13:e12347. doi: 10.1111/mcn.12347
45. Chen, S, Shimpuku, Y, Honda, T, Mwakawanga, DL, and Mwilike, B. Dietary diversity moderates household economic inequalities in the double burden of malnutrition in Tanzania. Public Health Nutr. (2024) 27:e141. doi: 10.1017/S136898002400106X
46. Wandji Nguedjo, M, Tchuente, BRT, Ngoumen, DJN, Mouafo, HT, Dibacto, REK, Fandio, GCDW, et al. The phenotypes of double burden of malnutrition in pairs of mothers and their children aged 0–59 months at a rural district in west region, Cameroon: a cross-sectional study. Clin Epidemiol Global Health. (2024) 29:101743. doi: 10.1016/j.cegh.2024.101743
47. Anik, AI, Rahman, MM, Rahman, MM, Tareque, MI, Khan, MN, and Alam, MM. Double burden of malnutrition at household level: A comparative study among Bangladesh, Nepal, Pakistan, and Myanmar. PLoS One. (2019) 14:e0221274. doi: 10.1371/journal.pone.0221274
48. Jeyakumar, A, Godbharle, S, Kesa, H, Shambharkar, P, Bhalekar, P, Chalwadi, S, et al. Comparison of household double burden of malnutrition among mother-child dyads in different settings in Maharashtra. Cities & Health. 8:1031–9. doi: 10.1080/23748834.2024.2333128
Keywords: double burden, malnutrition, mother–child pairs, households, systematic review, meta-analysis, Ethiopia
Citation: Belay MA, Bogale EK, Haile MT, Bogale SK, Getachew E, Andarge GA, Seid K, Lakew G, Yirsaw AN, Gebreegziabher ZA, Semagn BE and Alemu AT (2025) Double burden of malnutrition among households in Ethiopia: a systematic review and meta-analysis. Front. Public Health. 12:1417289. doi: 10.3389/fpubh.2024.1417289
Received: 14 April 2024; Accepted: 16 December 2024;
Published: 30 January 2025.
Edited by:
Richard Rosenkranz, University of Nevada, Las Vegas, United StatesReviewed by:
Akim Tafadzwa Lukwa, University of Cape Town, South AfricaCopyright © 2025 Belay, Bogale, Haile, Bogale, Getachew, Andarge, Seid, Lakew, Yirsaw, Gebreegziabher, Semagn and Alemu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mahider Awoke Belay, bWFoaWRlcnNlbGFtQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.