- 1Department of Environmental Health, Beijing Center for Disease Prevention and Control, Beijing, China
- 2Department of Environmental Health, Beijing Fengtai District Center for Disease Prevention and Control, Beijing, China
- 3Department of Environmental Health, Beijing Dongcheng District Center for Disease Prevention and Control, Beijing, China
- 4Department of Environmental Health, Beijing Huairou District Center for Disease Prevention and Control, Beijing, China
The risk of Legionella transmission in built environments remains a significant concern. Legionella can spread within buildings through aerosol transmission, prompting the exploration of airborne transmission pathways and proposing corresponding prevention and control measures based on building characteristics. To this end, a comprehensive literature review on the transmission risk of Legionella in built environments was performed. Four electronic databases (PubMed, Web of Science, Google Scholar, and CNKI) were searched from inception to March 2024 for publications reporting the risk of Legionella transmission in built environments. Relevant articles and gray literature reports were hand-searched, and 96 studies were finally included. Legionella pollution comes from various sources, mainly originates in a variety of built environments in which human beings remain for extended periods. The sources, outbreaks, national standards, regulations, and monitoring techniques for Legionella in buildings are reviewed, in addition to increases in Legionella transmission risk due to poor maintenance of water systems and long-distance transmission events caused by aerosol characteristics. Air and water sampling using various analytical methods helps identify Legionella in the environment, recognize sources in the built environments, and control outbreaks. By comparing the standard regulations of national organizations globally, the authors further highlight gaps and deficiencies in Legionella surveillance in China. Such advancements offer essential insights and references for understanding and addressing Legionella transmission risk in the built environment, with the potential to contribute to safeguarding public health and building environment safety.
1 Introduction
Legionella is a pathogenic gram-negative bacterium and the pathogen associated with Legionellosis. Legionellosis represents two types of illnesses: one is a mild flue like illness known as Pontiac fever (1), and the second is a fatal pneumonia known as Legionnaires' disease, with a mortality rate between 3 and 33% (2, 3). Legionella can affect anyone but it principally affects individuals who are susceptible due to age, illness, immunosuppression, or other risk factors, such as smoking (3). From 2000 to 2018, the reported incidence of Legionnaires' disease increased more than 6-fold. Risk environments and susceptible populations are found globally, but most currently available epidemiologic data focus on Legionellosis in large metropolitan areas in developed regions. The problem of Legionella is potentially underappreciated and underestimated by a factor of eight to ten (3). The spread of Legionella is mainly related to the aerosol atomization of bacteria from water to air. Therefore, the transmission risk is higher in built environments with aerosol production characteristics (4, 5). The built environment mainly refers to residential, multi-purpose commercial, and mixed-use buildings, including apartments, offices, hotels, hospitals, and schools (6). A variety of familiar water sources in the built environment, including showers, faucets, hot tubs, swimming pools, cooling towers, and fountains, can produce large amounts of aerosols from heated water sources contaminated with Legionella that can spread over long distances (7). Although many sources are associated with Legionnaires' disease, water systems often have conditions conducive for Legionella growth, including suitable water temperature, water retention, the presence of scale, sediments, and biofilms in pipes and fixtures, and the absence of disinfectants (8). A common route of transmission is inhaling water droplets or aerosols in a contaminated environment, resulting in infection with Legionnaires' disease. Because humans are accidental hosts of Legionella, Legionnaires' disease is generally not considered to spread from person to person.
Despite increased global awareness of Legionnaires' disease and efforts to control Legionella spread, outbreaks continue to occur, the sources of pathogens are expanding, and the number of reported cases shows no sign of decreasing (9). In 2023, Poland experienced an outbreak of Legionnaires' disease, with a total of 166 confirmed cases and 23 deaths, resulting in a mortality rate of 14% (10). Due to its high morbidity and mortality, Legionnaires' disease has become a significant public health concern. Epidemiological data show that most reported Legionella cases occur in large built environments (3), and tourism-related Legionnaires' disease outbreaks may occur in cruise ships, hotels, or resorts. A common feature of such environments is the existence of a large complex water supply system and lack of adequate maintenance (11). Legionella is ubiquitous in freshwater resources globally; however, the number of Legionella in such environments is insufficient to cause the disease, and the conditions for the proliferation of Legionella are not as conducive as those in the built environment (11). Therefore, the spread of Legionella in built environments requires attention due to its significance. We should implement intervention measures to reduce the spread of Legionella and prevent outbreaks of Legionella infections.
Legionnaires' disease occurs worldwide. The incidence of Legionellosis varies greatly based on the level of surveillance and reporting across countries. The lack of robust surveillance systems may lead to underreporting and poor control measures for Legionella in developing countries, posing a significant public health challenge. The current status of Legionella management in China, as in developing countries such as India, is an area that requires further attention and research, as well as robust surveillance systems, guidelines, and regulations (12). This review focuses on research related to the risk of Legionella transmission in the built environments, which could improve building safety, facilitate development of prevention and control strategies, enhance surveillance capacity, and facilitate the effective management of Legionella infection.
2 Materials and methods
A comprehensive search of the academic databases PubMed, Web of Science, Google Scholar, and CNKI was conducted. Specific terms, such as “Legionella and built environment,” “Legionella and aerosols,” “Legionella and transmission risk,” “Legionella aerosol and sampling,” and “Legionella aerosol and detection” were searched. The titles and abstracts of the articles were screened and assessed for inclusion in the review. Articles were cross-checked, and duplicated and irrelevant articles were excluded. A list of 747 papers was discussed extensively to resolve any discrepancies and reach consensus. Finally, 96 references were included in the present, out of which 79% were published from 2010 onward.
3 Built environment and Legionnaires' disease
In recent years, with an increase in urbanization, equipment for aerosol production has been introduced into buildings in large numbers. Improper design and poor operational management have resulted in areas becoming breeding grounds and dissemination sites for Legionella. Therefore, the risk of outbreaks and epidemics is increasing gradually.
3.1 Cooling towers
Cooling towers are essential components of centralized air-conditioning systems. Their structures and operating temperatures are highly suitable for the growth and reproduction of Legionella, making them crucial sources for Legionnaires' disease outbreaks in public buildings. If cooling towers are not cleaned and disinfected promptly, protozoa multiply, providing conditions for the growth of Legionella. A study conducted in 44 hospitalized medical institutions in Spain from 2005 to 2006 found that Legionella accounted for nearly 24% of the 470 cooling tower samples collected (13). Similarly, testing 96 cooling towers in public buildings in Greece showed that almost 49% of those towers were infested by Legionella (14).
3.2 Water supply system
Building water supply systems, including hot water showers, hot springs, and swimming pools, are common in modern cities, and is an ideal breeding environment for Legionella. Large buildings with centralized hot water systems often have complex pipelines, in which certain conditions, including low residual disinfectants, favorable water temperature, high water age, sediment accumulation, and free-living amoebae, support the growth of bacteria in biofilms. Legionella is often found in stagnant or unused pipe sections, intermittently used water tanks, and other places, which can amplify ideal living environments (15). The optimal growth temperature for Legionella is between 25 and 45°C, which is common in hot water pipes of building water supply systems. Samples of hot water systems in 40 hotels in five different regions of Italy revealed the presence of Legionella in 75% of the buildings (16). Changes in water flow or flushing can disrupt biofilms and release Legionella downstream (17). A research report stated that compared with that in high-usage faucets, the number of Legionella pneumophila in low-usage faucets was increased 125 times, with more stagnant water and more significant water flow variations (18). Hospital-acquired Legionnaires' disease is also associated with Legionella in water-supply systems (19). A recent study in Hungary found Legionella in hot water systems of 92% of the investigated healthcare facilities (N = 24), with a median exceeding 1,000 CFU/L in seven hospitals (20).
3.3 Medical equipment
The occurrence of Legionnaires' disease in hospitals that use tap water is related to aerosol-generating equipment (21). Hamilton et al. (22) found that the surface-area-to-volume ratio of water pipes in dental clinics is high, which is conducive to biofilm growth. Combined with high-pressure water equipment, fine aerosols can be generated in the breathing zone, posing a potential risk of L. pneumophila inhalation. Built environment exposure to aerosol-producing water fixing devices, including medical and dental equipment, will atomize water containing Legionella into easily-inhaled aerosols during work (23, 24). These devices are an essential part of modern urban building environments, in which conditions are conducive to the growth and proliferation of Legionella, posing a high risk of transmission.
3.4 Green building
At present, green building is promoted vigorously, and its essential goal is the conservation of energy, water, and materials. Water-saving characteristics are due to the need to reduce unsustainable water intake, especially in response to drought and other consequences of climate change. Energy conservation involves reducing dependence on fossil fuels and limiting greenhouse gas emissions; however, such measures often also have effects on water supply systems and increase Legionella breeding risk in building water supply systems (25).
The extremes of green buildings are off-grid or “net zero” buildings that do not rely on external water networks to provide drinking water or wastewater services (26). The primary goal of certification, such as the “Living Building Challenge,” is for this building to be independent of water facilities. It is characterized by using water-saving equipment to reduce water consumption, in addition to rainwater collection, reservoirs, etc. However, such design configurations pose unique challenges and corresponding public health problems. Leadership in Energy and Environmental Design (LEED) certified green buildings typically save 20–50% of drinking water. Water-saving measures inherently increase stagnation and overall water age, both at the municipal level (i.e., primary water distribution system) and at the building level (i.e., water age of house pipes) (27). One survey found that in a typical LEED-certified healthcare suite, the water age was 8 days old, while in an off-grid office suite, it was more than 6 months old (27). In addition, excessively high water age can also aggravate corrosion, taste, and odor problems and cause loss of disinfectant residues and regrowth of microorganisms, damaging to the primary water distribution systems (28). In a previous study, gene copies of Legionella were not detectable in the incoming water supply in LEED-certified healthcare suites. Still, they ranged between 10,000 and 100,000 GC/mL in three out the five housing pipeline sampling locations (27).
Green buildings can also save energy by lowering the temperature and creating conditions conducive to Legionella growth (29). Lowering the temperature of water heater outlets could increase the possibility of Legionella detection and the degree of contamination of faucets significantly. Moreover, turning off the recirculation system at night causes stagnation for up to 8 h or longer. Even in thermal insulation systems, water reaches the desired temperature for Legionella growth during such a long arrest period (30). Darelid et al. conducted a 10-year Legionella surveillance program; according to the results, maintaining the circulating hot water temperature > 55°C could limit bacterial growth and thus control the disease outbreak (31). As part of the water management plan, green buildings should pay close attention to maintenance of the temperature of hot water at 55–60°C and cold water at <25°C (3). In addition, use of heat pumps or solar water heaters may lead to water temperatures beneficial for Legionella growth. Rhoads et al. observed that the added storage incurred by a solar water heater in a net zero energy home increased the hot-water age from <1 day to between 2 and 3 days (27). Moreover, the solar preheated tank may be within the optimal temperature range for Legionella growth on cloudy days. The copy number measured by qPCR in the hot water manifold receiving hot water and delivering it to the faucet was significantly higher (>106 GC/mL) (27).
3.5 Transmission risk
The literature indicates that aerosol transmission can occur over a wide range, from a few to several thousands of meters (32, 33), with records showing that aerosols containing L. pneumophila are capable of infecting persons residing at a distance of >6 km from the contaminated source (34).
Most outbreaks are associated with healthcare and hotel buildings, as well as buildings supplied by large (>10,000 people) water systems (35). In 1994, 50 passengers on a cruise ship were infected with Legionella due to exposure to contaminated hot springs. Research has found that for every additional hour spent in hot springs, the risk of contracting Legionnaires' disease increases by 64% (36). In 2005, the lack of proper maintenance of a decorative fountain in a restaurant in South Dakota led to 18 people being infected with Legionella (37). In contrast to retrospective investigations of Legionella outbreaks abroad, domestic studies in China have mainly focused on the current status of Legionella contamination in public environments. For example, Zhang et al. (38) studied the hot water supply system of a hotel building in East China and reported an L. pneumophila detection rate of 50%. The highest contamination of L. pneumophila was found in the heat exchanger, which was attributed to the low hot-water temperature and high turbidity of the hotel. Zhang et al. (39) investigated L. pneumophila contamination in the centralized air-conditioned cooling water of public transport buildings, with an average detection rate of 47.70%. Therefore, the risk of Legionella transmission in building environments is high. It is vital to monitor and manage Legionella incidents and improve Legionnaires' disease risk alerts and prevention measures.
4 Major Legionella outbreaks
An outbreak of Legionella is usually associated with buildings or structures with complex water supply systems, such as hotels, long-term care facilities, hospitals, and cruise ships. Since its discovery, Legionnaires' disease has occurred in several countries, including the United States (40), Sweden (41), Netherlands (42), Italy (43, 44), Spain (7, 45), and Japan (46). China has also reported Legionella detection multiple times, with numerous outbreaks of Legionnaires' disease in Beijing alone (47, 48). In comparison, areas with relatively high medical standards have a better understanding and detection of Legionella. Modern equipment, such as fountains, showers, and air conditioning, are more commonly used in these areas, increasing the likelihood of Legionella infection. Outbreaks often occur in developed cities. The specific events are shown in Table 1.
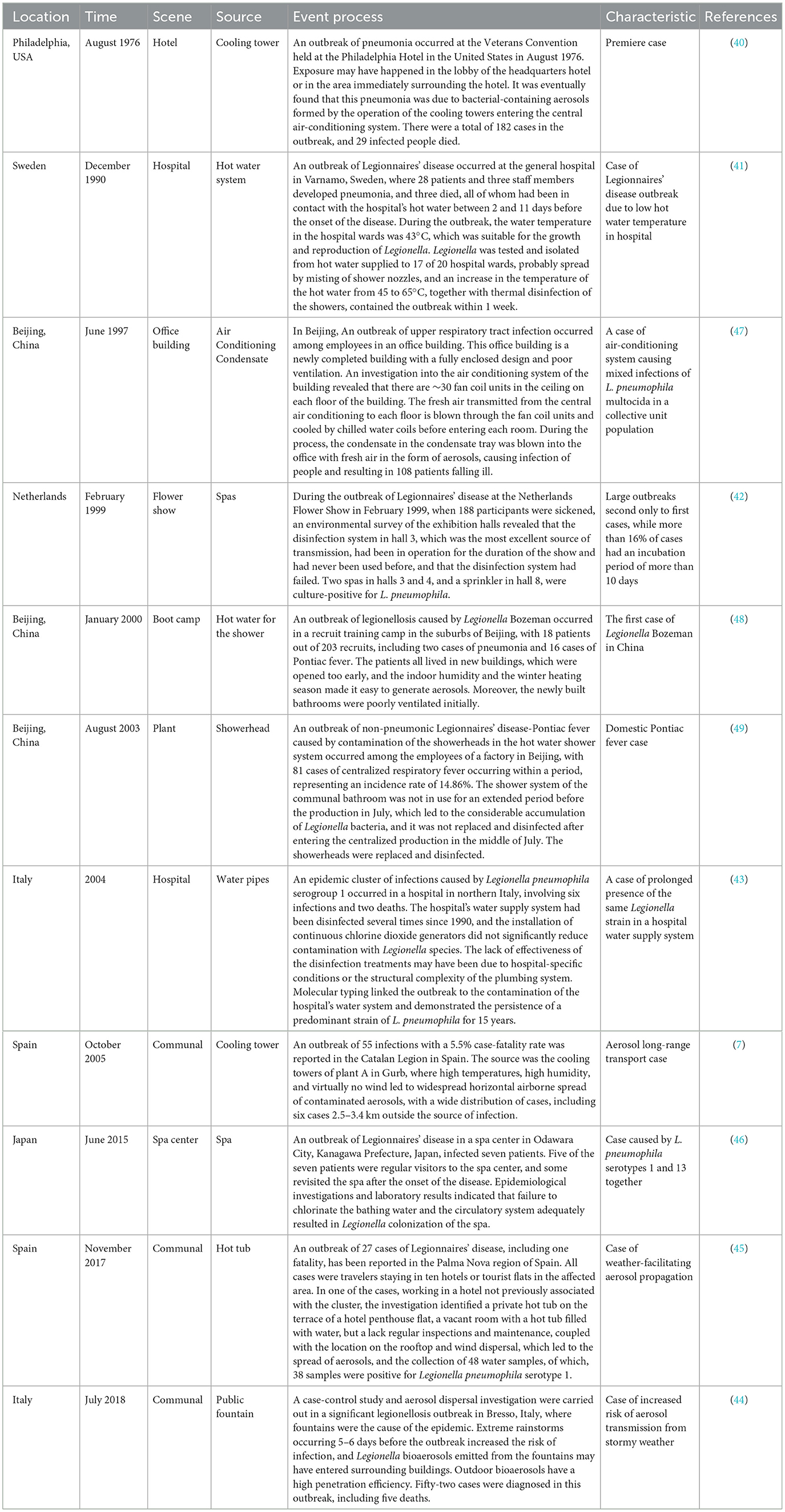
Table 1. Typical events of Legionella outbreak in built environment water systems in different countries from 1976 to 2018: sources, process and characteristics.
Outbreaks have continued since Legionella was first detected, resulting in multiple infections and even death and posing a severe threat to public health and safety. These incidents have aroused public concern about Legionella infections and heightened awareness and vigilance against Legionnaires' disease, prompting the government and relevant departments to introduce stricter regulations and standards to regulate the management of cooling towers and water systems in public places and to strengthen monitoring and preventive and control measures to reduce the likelihood of recurrence of similar incidents. Aerosols play an important role in significant events and can spread over long distances under the influence of weather. At the same time, in areas with well-established routine surveillance systems, it is easy to detect trends in legionellosis outbreaks at an early stage and trace the source of environmental contamination, so that effective measures can be taken to control the further evolution of legionellosis outbreaks.
5 Legionella monitoring regulations
Incidents of Legionella morbidity in buildings occur nationwide, and the risk of the disease and difficulty in treating it is of great concern to Governments and the World Health Organization (WHO). Around the world, regulatory agencies and health organizations have issued and developed recommendations and regulations aimed at controlling and preventing the risk of contracting Legionellosis, including the sanitation of water supplies, maintenance through regular cleaning, and disinfection of facilities and equipment to reduce the presence of the pathogen.
5.1 World Health Organization
In 1987, the WHO issued guidelines for controlling Legionella in water sources and supply systems, emphasizing the management of water quality and supply facilities to reduce the risk of Legionella infections. In 1993, the WHO formally declared Legionella infection a global problem, advocating for broader guidance on prevention, diagnosis, and treatment. In 2007, the WHO published “Legionella and the prevention of legionellosis,” guiding the assessment and management of risks associated with potential hazardous environments such as cooling towers, swimming pools, and hot springs. The document also identifies necessary measures to prevent or adequately control Legionella exposure risk in specific environments (50). In 2009, the WHO issued the WHO guidelines for indoor air quality: dampness and mold, which guides public health and other authorities in planning or formulating regulations, action plans, and policies to increase safety and ensure healthy building conditions (51). In 2017, the WHO made suggestions regarding water system construction, design, routine operational monitoring, and management incorporation in water safety plans developed by building owners or managers (52). The WHO recommends implementing water safety plans, based on Hazard Analysis and Critical Control Points (HACCP) principles, to proactively identify, assess, and manage risks related to water quality. This can be an effective method for actively managing Legionella contamination risks in various environments such as hospitals, long-term care facilities, spas, and hotels. Continuous research and implementation of effective control measures are essential for ensuring water safety and minimization of the spread of Legionella in water systems. For example, Salah et al. (53) discussed the successfully implementation of a water safety plan at UAB Medical Center, highlighting the importance of water system management plans in guiding risk assessment and mitigation strategies. Marino et al. (54) also highlighted the importance of comprehensive water safety plans in dental clinic complexes in identifying new risk factors associated with Legionella and Pseudomonas aeruginosa contamination.
5.2 European Union
Legionella-related research in Europe has been continuing for a significant period of time. In 1986, Europe established the European Working Group for Legionella Infections (EWGLI), which promoted the standardization of guidelines for Legionella disease prevention and control in member countries and travel-related settings (55). In 2010, the EWGLI was merged into the European Center for Disease Control and Prevention (ECDC). The primary goal of the current European Legionnaires' disease surveillance network is to detect, control, and prevent the dispersion, occurrence, clustering, and outbreak of the disease within the EU or European Economic Area members, with all data being shared fully with member countries (56). In 2011 and 2012, ECDC issued the Travel-Associated Legionnaires' Disease (TALD) survey, Control and Prevention Technical Guidelines, and the European Legionella Surveillance Network Operation Manual, providing guidelines on the diagnosis and reporting of Legionnaires' disease, in addition to the tracing and environmental treatment of cases (57, 58). In 2014, the EU revised the Water Framework Directive (WFD), which required member states to monitor and manage water in public places.1 With an increase in the occurrences of Legionnaires' disease in recent years, the EU has integrated the regulation of Legionella bacteria into EU Directive 2020/2184. The directive includes the assessment of Legionella concentrations among the parameters to be evaluated when determining the quality of drinking water intended for human consumption. The directive has also been extended to monitoring of Legionella bacteria in all drinking water distribution systems, including ample domestic water and industrial distribution systems. The limit for Legionella species was established at 1,000 CFU/L. Notably, the EU directive requires testing for Legionella spp. and not just L. pneumophila.2
5.3 United States
Legionellosis is required to be reported to the US Centers for Disease Control and Prevention (CDC) as a nationally notifiable disease, monitored using both the National Notifiable Diseases Surveillance System (NNDSS) and Supplemental Legionnaires Disease Surveillance System (SLDSS).3 (59). Legionella regulations were adopted in the U.S. immediately after the 1976 Legionella outbreak in Philadelphia (40). The U.S. Environmental Protection Agency (EPA) revised the Safe Drinking Water Act (SDWA) in 1986, explicitly adding Legionella-related regulations for public water systems and specifying that the number of Legionella detected in residential drinking water should be zero (60). The 2021 American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) Standard 188 establishes the minimum number of Legionella bacteria in building water supply systems.4 In 2021, the CDC published the Legionella Control Toolkit, which provides control measures for familiar sources of Legionella as well as recommendations for the design and testing of methods for Legionella, and recommendations for new methods in the future (61). In 2024, the U.S. CDC released a CDC Yellow Book Legionnaires' Disease & Pontiac Fever, providing an overview of the current research on Legionella bacteria (11).
5.4 Japan
In 1993, Japan adopted an amendment to the Drinking Water Sanitation Law that required water treatment facilities to control Legionella in drinking water (62). The Ministry of Health, Labour and Welfare has issued a series of guidelines for the prevention and control of Legionella infections, such as the “Guidelines for Water Quality Standards, for Public Baths,” which stipulates that the abundance of Legionella bacteria in bathing water must be <10 CFU/100 mL, and the “New Version of the Outline of Prevention of Legionella Bacteria,” which stipulates that when Legionella bacteria counts of 2 CFU/mL or more are found in non-inhalable water for human beings, disinfecting measures should be taken until the detected bacterial counts are <10 CFU/100 mL. Legionella counts in human inhalable water (e.g., bathtub water and shower water) should be <10 CFU/100 mL. If Legionella is detected, measures such as cleaning and disinfection should be taken immediately.
5.5 Australia
Australia has not established a dedicated monitoring system for Legionella; however, as Legionella is a nationally recognized contagious disease in Australia, all cases need to be reported to NNDSS, and infectious disease outbreaks are reported on a quarterly basis. The relevant standards for controlling and preventing Legionella in cooling systems include the Australian/New Zealand standard AS/NZS 3666: 2011, “Air Treatment of Buildings and Microbial Control in Water Systems,” which specifies the minimum requirements for operating and maintaining air and water supply systems in buildings for microbial control purposes (63). Further guidance can be found in other relevant Australian and Australian/New Zealand Standards and State and Territory guidelines (64). In 2016, the Environmental Health Standing Committee (enHealth) released Guidelines for Legionella control, which assists facility managers to assess the risk from Legionella in health and aged care facilities (65).
5.6 Poland
In Polish law, Legionellosis has been classified as an infectious disease and is regulated in the revised bill on the prevention and control of human infections and infectious diseases in 2008. In March 2007, in the revised law on drinking water quality, “the Minister of Health Regulations” pointed out that four points in the hot water system need to be tested for the presence of Legionella. The regulatory annex specifies the microbiological requirements that hot water should meet, and the number of Legionella colony forming units in 100 ml of hot water should not exceed 100. However, in closed medical facilities for patients with immunodeficiency (including those receiving immunosuppressive treatment), a 1,000 ml of water sample should not contain Legionella. The revised Regulations of “the Minister of Infrastructure”, revised on March 12, 2009, stipulate the technical conditions that buildings should meet, and require the maintenance of hot water temperatures within the 55–60°C during network construction (66). In recent years, due to Legionella outbreak in Poland, Legionella management has been of great concern, and the country lacks national guidelines for risk management. Sporadic outbreaks of Legionella have been reported before, and between 2017 and 2021, Poland reported 38 and 74 cases of Legionnaires' disease annually to the European Surveillance System (TESSy) (67).
5.7 India
Water safety regulations for Legionella monitoring and decontamination are absent in India, and there have been sporadic reports of Legionella in specific locations. However, so far, no outbreaks of the disease have been detected. As a developing country with limited resources, more research is required to understand the disease burden caused by Legionella to improve Legionella testing accuracy (68, 69).
5.8 China
China has a different approach to the monitoring and managing Legionellosis than other countries, such as the United States and Europe; there is no monitoring system for Legionellosis, and it has not yet been classified as a legally reportable infectious disease. In 2003, the Ministry of Health promulgated the “Hygienic specification of central air conditioning ventilation system in public places” (WS 394-2012), which is an essential basis for the prevention and treatment of Legionella in China. The Norms stipulate that Legionella bacteria should not be detected in centralized air-conditioning cooling water and condensate. In 2023, the Ministry of Health formulated “Measures for the hygienic management of concentrated air conditioning ventilation system in Public Places”, “Hygienic specification of central air conditioning ventilation system in public places” (WS 10013–2023), “Hygienic evaluation specification of central air conditioning ventilation system in public places” (WS/T 10004–2023), and “Specification of cleaning and disinfecting for central air conditioning ventilation system in public places” (WS/T 10005–2023).5−7 These standards were officially implemented on May 1, 2024 to clarify the monitoring and prevention of Legionella infections.
Beijing took the lead in 2007 by introducing the local standard “Hygienic Management Specification for Central Air Conditioning and Ventilation Systems in Public Places” (DB11/485-2007),8 providing norms and guidance for the cleaning and disinfection of central air conditioning and ventilation systems throughout the city. In subsequent revisions, public and residential buildings were included under the jurisdiction, gradually incorporating Legionella detection methods for central air conditioning and ventilation systems to provide a basis for effective Legionella prevention. In 2016, Beijing established a Legionnaires' disease early warning technology for cooling towers in public buildings, comprehensively analyzing the reproduction, transmission, and population infection risks of cooling towers from the perspective of airborne diseases, expressing their risk levels intuitively with an index that is of great significance for the early warning and prevention of Legionnaires' disease outbreaks in public buildings (70). This technology has been piloted in the Beijing Public Health Hazard Factor Active Monitoring System since 2016, received project funding for promotion in 2017, and its promotion and application in the disease control centers of 16 districts in Beijing was completed in 2018, being officially included in the city's Public Health Hazard Factor Active Monitoring System. In 2020, the focus of the technology in the annual health and population health status report of Beijing was on conducting risk classification assessments for cooling towers in theaters, hospitals, offices, shopping places, or accommodation places.9 Owing to its high timeliness, the technology has been widely utilized to ensure various large-scale events. Hong Kong has issued the “Guidelines for the Prevention of Legionnaires' Disease” and the “Guidelines for Cleaning Drinking Water Tanks.” In contrast, the Macau Water Supply Department issued Decrees No. 2 and No. 33, stipulating control indicators and risk control measures for Legionella in cooling water systems and domestic water.
Currently, no vaccine is available for the prevention of Legionnaire's disease. Prevention measures mainly focus on controlling and regularly monitoring water quality. Mandatory measurement indicators related to facility hygiene conditions are utilized to minimize or avoid conditions for bacterial reproduction and survival, such as biofilm formation, including maintenance, cleaning, and disinfection, and to ensure the regular operation of water facilities and related devices to reduce or prevent the spread of aerosols.
6 Legionella monitoring technology
To better monitor and prevent the spread of Legionnaires' disease, relevant personnel have conducted in-depth research on environmental monitoring of Legionella. Collecting and testing samples from water sources and air enable measures to be taken against infection sources, and accurate and efficient detection of Legionella is crucial for its prevention and control.
6.1 Sampling techniques
Water sampling typically refers to collecting samples from water sources. This can be done by sampling contaminated building environments, such as hot water pipes or cooling towers, to help identify the source of infection and infection risks. Water sampling needs to be adjusted according to the specific environment. The detection of Legionella is easier in sampling water that has been stagnant for a long time, such as cooling towers or shower water. Collins et al. (71) collected water samples from household showerheads, with the showerhead being unused for several hours before sampling. The water temperature was set to the usual temperature, and the first liter of water was collected in a sterile bottle containing sodium thiosulfate. Legionella was detected in 8% of the water samples.
Aerosol sampling equipment should have a high collection efficiency over a wide range of particle sizes to avoid underestimating the infection risk of airborne transmission. Additionally, structural and biological damage may occur during the sampling process, which could lead to inappropriate results in subsequent quantitative analyses. The Coriolis cyclonic sampler can effectively collect Legionella spp. Nocker et al. (72) used a Coriolis sampler to collect exhaust gas samples below the exhaust plane of a cooling tower or above the water distribution level of a naturally ventilated cooling tower (system C) in the upwind direction, with only the aerosol detection of cooling tower system B being positive. Niculita-Hirzel et al. (73) used a Coriolis air sampler to sample Legionella aerosols from two types of showerheads that emitted similar levels of biological aerosols, accounting for only 0.02% of the total bacteria in the water. Montagna et al. (74) collected Legionella samples from medical facilities using a Coriolis sampler. The collection efficiency of the Coriolis sampler does not exceed 50%, and the bacterial concentration often falls below the actual results. Therefore, future considerations should include calibration or correction factors.
6.2 Detection techniques
There are multiple methods of detection and quantification of Legionella, and we need to better understand their limitations and the relationships among them. The International Organization for Standardization (ISO) provides two options for the detection and quantitation of Legionella contamination in water systems. ISO11731: 2017-05 is a culture-based method for detecting only culturable Legionella (75), and it is considered the gold standard. However, it is time-consuming and takes 10–14 days, but displays errors in detecting viable but non-culturable (VBNC) Legionella, resulting in underestimated and false negatives of Legionella numbers (76). Chen et al. (77) and Pan et al. (78) used culture isolations to detect Legionella. However, this method has a sensitivity ranging from 50 to 70%, has a long detection period, and is not suitable for rapid testing in emergencies. In addition, ISO/TS12869:2019 is a quantitative PCR (qPCR) based assay, which estimates bacterial genomic load (79). In contrast, the qPCR method is more rapid; however, it quantifies live, VBNC and dead Legionella, resulting in overestimations and false positive. Sánchez-Parra et al. (80) employed a dual PCR detection method targeting the V3 and V5 hypervariable regions of the 16S rRNA gene to precisely to identify pathogenic L. pneumophila in low-concentration outdoor DNA samples precisely.
Colloidal gold immunochromatography is commonly used for early rapid diagnosis in on-site monitoring to prevent outbreaks and the spread of Legionella. Ren et al. (81) prepared colloidal gold immunochromatographic test strips for rapid Legionella detection and conducted performance tests. The test strips did not cross-react with other pathogens, enabling fast detection; however, they may not be suitable for environments requiring high accuracy. Strain-typing methods can differentiate between different isolates of the same bacterial species and determine the cause of an outbreak. Currently, DNA sequence-based typing (SBT) serves as the reference standard for strain typing L. pneumophila isolates (82). Due to a disproportionate representation of some sequence types among the over 2,000 types in clinical cases, SBT may neither differentiate between outbreak-related and non-outbreak-related Legionella isolates nor assess changes over time within sequence types (STs) (83). Whole genome sequencing (WGS) is an essential tool for elucidating the epidemiology of these pathogens. WGS has been used in real-time to determine the sources of Legionella in individual and outbreak patients and to study the epidemiology of Legionella in facilities over time (84–86).
Currently, efforts are being made to improve Legionella detection, particularly in the identification of VBNC bacteria that may pose a risk to in clinical setting. As the ISO sample processing protocol has been adopted for detecting and quantifing VBNC Legionella, the number of VBNC Legionella observed in mixed bacterial cultures has increased significantly (87). Furthermore, a Chip-based duplex real-time PCR has been developed for water quality monitoring that can detect VBNC Legionella (88). Innovative techniques such as the PVT VIABLE™ method, have also been introduced for detection of Legionella that cannot form colonies using the traditional spread plate method (such as those in the ISO protocol) (89). Exposure to environmental stress and disinfection treatments promotes the formation of resistant and potentially infectious VBNC Legionella, and the presence of VBNC Legionella hinders the management of engineered water systems to prevent Legionella disease (87, 90). Advancing Legionella detection methods could improve our understanding of the role that VBNC cells play in the spread of Legionellosis and is critical to improving the control and risk management strategies for Legionnaires' disease prevention.
7 Summary and outlook
The COVID-19 outbreak has brought to the forefront the issue of indoor airborne pathogens into the spotlight, with the level of risk of aerosolized pathogens being exceptionally high in enclosed buildings. Increasing urbanization has led to increased population densities and the widespread use of modern equipment, which increases the exposure of the population to Legionella and leads to a continued rise in disease incidences. Legionella is transmitted from various sources and can be spread over long distances via aerosols. The possibility of aerosols being discharged from outdoor sources, transported over long distances, and entering the built environment is thus realistic, especially considering the efficient penetration of outdoor bioaerosols into the indoor environment (91). Despite significant progress in our understanding of the sources and spread of Legionella in the built environment, many issues are remain overlooked.
This review provides insights into Legionella transmission risk in the built environments for improved surveillance of Legionella in such environments, targeted development of preventive control strategies, and further systematic and exploratory research. There is a wide range of sources of Legionella in the built environment, and further research is necessary to determine whether neglected sources pose a risk of disease transmission. Legionella regulations and standards in developed countries have been established early and include well-established surveillance systems. However, in developing countries, such as China, where Legionnaires' disease has not yet been listed as a national statutory infectious disease, there is a deficiency in surveillance and a need to raise awareness of the severity of the problem, as effective regulations can reduce risk of transmission. Multiple approaches are available to detect and quantify Legionella. Non-culture-based methods can complement culture-based methods, and WGS development has paved the way for an improved analysis of the sources of Legionella infections and the emergence of new causative organisms, which are still relatively unexplored. Moreover, there is considerable uncertainty concerning quantitative microbiological risk assessment of Legionella infections. Frameworks should prioritize appropriate aerosol exposure modeling approaches, consider trade-offs between model validity and complexity, and incorporate research that strengthens confidence in quantitative microbial risk assessment (QMRA) results.
Green buildings have exacerbated many of the problems with Legionella species by extending the duration of water residence (leading to the loss of disinfectant residues) and lowering the hot water temperature in the house pipe. While vigorously promoting “green” building functions, focus should be directed at such emerging problems and more forward-looking Legionella control strategies. The certification standards for green building, energy saving functions, and water saving functions should be adapted to account for the risk factors for the growth of Legionella and other water-based pathogens in the building water supply system. While protecting public health, significant water conservation can still be achieved through more open water age management, for example, by regularly flushing the water to be consumed. In conclusion, the persistence of Legionella in green or zero-energy buildings is a complex problem requiring a multidisciplinary approach to address the challenges posed by energy conservation, water saving, and microbial contamination. Efforts to balance such factors while ensuring the safety and health of building users are essential for the design and maintenance of sustainable buildings.
The contribution of climate change to the spread of infectious diseases such as Legionella is increasingly being recognized. Advanced studies have been conducted to longitudinally examine Legionellosis case data about hydrometeorological factors to understand the impact of weather and climate on increased morbidity (92–96). China joined the Paris Climate Change Agreement in 2016, and research on climate change and health-related topics has been expanding. However, there is still a gap in research related to Legionellosis. Future research should also further investigate the exposure pathways between changes in hydrometeorological factors and Legionella infections in the built environment, and find simple interventions around water-to-air transmission to reduce the spread of Legionella and protect populations from infection. An in-depth understanding of the risk of Legionellosis transmission in buildings could provide the theoretical basis, technical methods, and practical applications for the prevention and control of the next airborne disease pandemic.
Author contributions
XHY: Resources, Conceptualization, Writing – review & editing, Writing – original draft. FS: Writing – review & editing, Supervision, Resources, Project administration, Funding acquisition, Conceptualization. JH: Writing – review & editing, Resources, Investigation. LH: Writing – review & editing, Resources, Investigation. BK: Writing – review & editing, Resources, Investigation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported and funded by the “Technology Winter Olympics” Key Project (No. 2021YFF0307400).
Acknowledgments
The authors thank the editor and reviewers for taking the time to assess the manuscript and giving valuable and professional comments.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^Commission Directive 2014/101/EU of 30 October 2014 amending Directive 2000/60/EC of the European Parliament and of the Council Establishing a Framework for Community Action in the Field of Water Policy Text with EEA Relevance. (2014). Available online at: https://eur-lex.europa.eu/eli/dir/2014/101/oj.
2. ^European Parliament and of the Council. Directive (EU) 2020/2184 of the European Parliament and of the Council of 16 December 2020 on the Quality of Water Intended for Human Consumption. Official Journal of the European Union (2020). p. 435.
3. ^US CDC (2012-12-07). National Notifiable Diseases Surveillance Saystem (EB/OL). Available online at: http://wwwn.cdc.gov/nndss.
4. ^ANSI-ASHRAE 188-2018. Legionellosis: Risk Management for Building Water Systems.
5. ^WS 10013–2023. Hygienic Specification of Central Air Conditioning Ventilation System in Public Places.
6. ^WS/T 10004–2023. Hygienic Evaluation Specification of Central Air Conditioning Ventilation System in Public Places.
7. ^WS/T 10005–2023. Specification of Cleaning and Disinfecting for Central Air Conditioning Ventilation System in Public Places.
8. ^DB11/485-2007. Hygienic Management Specification for Central Air Conditioning and Ventilation Systems in Public Places.
9. ^Beijing Municipal Government. Annual Report on Health and Population Health in Beijing. People's Medical Publishing House.
References
1. Glick TH, Gregg MB, Berman B, Mallison G, Rhodes WW Jr, Kassanoff I. Pontiac fever. An epidemic of unknown etiology in a health department I Clinical and epidemiological aspects. Am J Epid. (1978) 107:149–60. doi: 10.1093/oxfordjournals.aje.a112517
2. World Health Organization. Legionella and the Prevention of Legionellosis. Geneva: WHO (2007). p. 1–10.
3. National National Academies of Sciences Engineering and Medicine Health Health and Medicine Division; Division on Earth and Life Studies Board Board on Population Health and Public Health Practice Board Board on Life Sciences Water Science and Technology Board Committee Committee on Management of Legionella in Water Systems. Management of Legionella in Water Systems. Washington, DC: National Academies Press (US) (2019).
4. Prussin AJ, Schwake DO, Marr LC. Ten questions concerning the aerosolization and transmission of Legionella in the built environment. Build Environ. (2017) 123:684–95. doi: 10.1016/j.buildenv
5. Donohue MJ, Mistry JH, Tucker N, Vesper SJ. Hot water plumbing in residences and office buildings have distinctive risk of Legionella pneumophila contamination. Int J Hyg Environ Health. (2022) 245:114023. doi: 10.1016/j.ijheh.2022.114023
6. National National Academies of Sciences Engineering and Medicine. Microbiomes of the Built Environment: A Research Agenda for Indoor Microbiology, Human Health, and Buildings. Washington, DC: The National Academies Press (2017).
7. Sala Ferré MR, Arias C, Oliva JM, Pedrol A, García M, Pellicer T, et al. A community outbreak of Legionnaires' disease associated with a cooling tower in VIC and Gurb, Catalonia (Spain) in 2005. Euro J Clin Microbiol Infect Dis. (2009) 28:153–9. doi: 10.1007/s10096-008-0603-6
8. Falkinham JO. Living with Legionella and other waterborne pathogens. Microorganisms. (2020) 8:2026. doi: 10.3390/microorganisms8122026
9. Carratalà J, Garcia-Vidal C. An update on Legionella. Curr Opin Infect Dis. (2010) 23:152–7. doi: 10.1097/QCO.0b013e328336835b
10. Jain N, Krygowska AM. Legionnaire's looms: Europe's wake-up call to enhance vigilance in detection and reporting. New Microb New Infect. (2023) 55:101194. doi: 10.1016/j.nmni.2023.101194
11. William CE. Legionnaires' Disease & Pontiac Fever. CDC Yellow Book (2024). Available online at: https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/legionnaires-disease-and-pontiac-fever (accessed March 28, 2024).
12. World Health Organization. Legionellosis. (2022). Available online at: https://www.who.int/news-room/fact-sheets/detail/legionellosis (accessed March 28, 2024).
13. Rivera JM, Aguilar L, Granizo JJ, Vos-Arenilla A, Giménez MJ, Aguiar JM, et al. Isolation of Legionella species/serogroups from water cooling systems compared with potable water systems in Spanish healthcare facilities. J Hosp Infect. (2007) 67:360–6. doi: 10.1016/j.jhin.2007.07.022
14. Mouchtouri VA, Goutziana G, Kremastinou J, Hadjichristodoulou C. Legionella species colonization in cooling towers: risk factors and assessment of control measures. Am J Infect Control. (2010) 38:50–5. doi: 10.1016/j.ajic.2009.04.285
15. Springston JP, Yocavitch L. Existence and control of Legionella bacteria in building water systems: a review. J Occup Environ Hyg. (2017) 14:124–34. doi: 10.1080/15459624.2016
16. Borella P, Montagna MT, Stampi S, Stancanelli G, Romano-Spica V, Triassi M, et al. Legionella contamination in hot water of Italian hotels. Appl Environ Microbiol. (2005) 71:5805–13. doi: 10.1128/AEM.71.10.5805-5813.2005
17. Schofield GM, Wright AE. Survival of Legionella pneumophila in a model hot water distribution system. J Gen Microbiol. (1984) 130:1751–6. doi: 10.1099/00221287-130-7-1751
18. Rhoads WJ Ji P, Pruden A, Edwards MA. Water heater temperature set point and water use patterns influence Legionella pneumophila and associated microorganisms at the tap. Microbiome. (2015) 3:67. doi: 10.1186/s40168-015-0134-1
19. Allen JG, Myatt TA, Macintosh DL, Ludwig JF, Minegishi T, Stewart JH, et al. Assessing risk of health care-acquired Legionnaires' disease from environmental sampling: the limits of using a strict percent positivity approach. Am J Infect Control. (2012) 40:917–21. doi: 10.1016/j.ajic.2012.01.013
20. Barna Z, Kádár M, Kálmán E, Scheirich Szax A, Vargha M. Prevalence of Legionella in premise plumbing in Hungary. Water Res. (2016) 90:71–8. doi: 10.1016/j.watres.2015.12.004
21. Sabria M, Yu VL. Hospital-acquired legionellosis: solutions for a preventable infection. Lancet Infect Dis. (2002) 2:368–73. doi: 10.1016/s1473-3099(02)00291-8
22. Hamilton KA, Kuppravalli A, Heida A, Joshi S, Haas CN, Verhougstraete M, et al. Legionnaires' disease in dental offices: quantifying aerosol risks to dental workers and patients. J Occup Environ Hyg. (2021) 18:378–93. doi: 10.1080/15459624.2021.1939878
23. Hamilton KA, Prussin AJ 2nd, Ahmed W, Haas CN. Outbreaks of legionnaires' disease and Pontiac fever 2006–2017. Curr Environ Health Rep. (2018) 5:263–71. doi: 10.1007/s40572-018-0201-4
24. Optenhövel M, Mellmann A, Kuczius T. Occurrence and prevalence of Legionella species in dental chair units in Germany with a focus on risk factors. Eur J Clin Microbiol Infect Dis. (2023) 42:1235–44. doi: 10.1007/s10096-023-04659-w
25. Rhoads WJ, Pearce A, Pruden A, Edwards MA. Anticipating the effects of green buildings on water quality and infrastructure. J Am Water Works Assoc. (2015) 107:50–61. doi: 10.5942/jawwa.2015.107.0058
26. EPA. Sustainable Design and Green Building Toolkit for Local Governments. Washington, DC: EPA (2013).
27. Rhoads WJ, Pruden A, Edwards MA. Survey of green building water systems reveals elevated water age and water quality concerns. Environ Sci Water Res Technol. (2016) 2:164–73. doi: 10.1039/C5EW00221D
28. EPA. Effects of Water Age on Distribution System Water Quality. Cincinnati, OH: EPA Office of Water, Office of Ground Water and Drinking Water (2002).
29. Brazeau RH, Edwards MA. Role of hot water system design on factors influential to pathogen regrowth: temperature, chlorine residual, hydrogen evolution, and sediment. Environ Eng Sci. (2013) 30:617–27. doi: 10.1089/ees.2012.0514
30. Bédard E, Lévesque S, Martin P, Pinsonneault L, Paranjape K, Lalancette C, et al. Energy conservation and the promotion of Legionella pneumophila growth: the probable role of heat exchangers in a nosocomial outbreak. Infect Control Hosp Epidemiol. (2016) 37:1475–80. doi: 10.1017/ice.2016.205
31. Darelid J, Löfgren S, Malmvall BE. Control of nosocomial Legionnaires' disease by kee** the circulating hot water temperature above 55 C: experience from a 10-year surveillance programme in a district general hospital. J Hospital Infect. (2002) 50:213–9. doi: 10.1053/jhin.2002.1185
32. Li QL. Identification of Aerosol Generation and Transmission of Escherichia coli and Novel Influenza A (H1N1) Virus Aerosols (dissertation/master's thesis). Shandong Agricultural University, Shandong, China (2011).
33. Phares CR, Russell E, Thigpen MC, Service W, Crist MB, Salyers M, et al. Legionnaires' disease among residents of a long-term care facility: the sentinel event in a community outbreak. Am J Infect Control. (2007) 35:319–23. doi: 10.1016/j.ajic.2006.09.014
34. Nhu Nguyen TM, Ilef D, Jarraud S, Rouil L, Campese C, Che D, et al. A community-wide outbreak of legionnaires disease linked to industrial cooling towers–how far can contaminated aerosols spread? J Infect Dis. (2006) 193:102–11. doi: 10.1086/498575
35. Holsinger H, Tucker N, Regli S, Studer K, Roberts VA, Collier S, et al. Characterization of reported legionellosis outbreaks associated with buildings served by public drinking water systems: United States, 2001–2017. J Water Health. (2022) 20:702–11. doi: 10.2166/wh.2022.002
36. Benkel DH, McClure EM, Woolard D, Rullan JV, Miller GB Jr, Jenkins SR, et al. Outbreak of Legionnaires' disease associated with a display whirlpool spa. Int J Epidemiol. (2000) 29:1092–8. doi: 10.1093/ije/29.6.1092
37. O'Loughlin RE, Kightlinger L, Werpy MC, Brown E, Stevens V, Hepper C, et al. Restaurant outbreak of Legionnaires' disease associated with a decorative fountain: an environmental and case-control study. BMC Infect Dis. (2007) 7:93. doi: 10.1186/1471-2334-7-93
38. Zhang YM, Dai XL, Yang WC, Li WY. Legionella levels and influencing factors in building hot water systems. Water Purif Technol. (2022) 41:118–24. doi: 10.15890/j.cnki.jsjs.2022.06.016
39. Zhang X, Chen M, Hou XB, Zhang JM, Fu C, Zhang L, et al. Current status and influencing factors of Legionella contamination in cooling water of central air conditioning systems in public transportation buildings in a city. J Environ Occup Med. (2021) 38:402–4077. doi: 10.13213/j.cnki.jeom.2021.20499
40. Fraser DW, Tsai TR, Orenstein W, Parkin WE, Beecham HJ, Sharrar RG, et al. Legionnaires' disease: description of an epidemic of pneumonia. N Engl J Med. (1977) 297:1189–97. doi: 10.1056/NEJM197712012972201
41. Darelid J, Bengtsson L, Gästrin B, Hallander H, Löfgren S, Malmvall BE, et al. An outbreak of Legionnaires' disease in a Swedish hospital. Scand J Infect Dis. (1994) 26:417–25. doi: 10.3109/00365549409008615
42. Den Boer JW, Yzerman EP, Schellekens J, Lettinga KD, Boshuizen HC, Van Steenbergen JE, et al. A large outbreak of Legionnaires' disease at a flower show, the Netherlands, 1999. Emerg Infect Dis. (2002) 8:37–43. doi: 10.3201/eid0801.010176
43. Scaturro M, Dell'eva I, Helfer F, Ricci ML. Persistence of the same strain of Legionella pneumophila in the water system of an Italian Hospital for 15 years. Infect Control Hosp Epidemiol. (2007) 28:1089–92. doi: 10.1086/519869
44. Faccini M, Russo AG, Bonini M, Tunesi S, Murtas R, Sandrini M, et al. Large community-acquired Legionnaires' disease outbreak caused by Legionella pneumophila serogroup 1, Italy, July to August 2018. Euro Surveill. (2020) 25:1900523. doi: 10.2807/1560-7917.ES.2020.25.20.1900523
45. Gumá M, Drasar V, Santandreu B, Cano R, Afshar B, Nicolau A, et al. A community outbreak of Legionnaires' disease caused by outdoor hot tubs for private use in a hotel. Front Microbiol. (2023) 14:1137470. doi: 10.3389/fmicb.2023.1137470
46. Kuroki T, Amemura-Maekawa J, Ohya H, Furukawa I, Suzuki M, Masaoka T, et al. Outbreak of legionnaire's disease caused by Legionella pneumophila serogroups 1 and 13. Emerg Infect Dis. (2017) 23:349–51. doi: 10.3201/eid2302.161012
47. Ma XY, Wang YQ. Investigation of an outbreak of legionnaires' disease caused by an air conditioning system leading to upper respiratory tract infections. Chin J Epidemiol. (1998) 19:5.
48. Deng CY, Fang XS, Wan CQ, Ren HY, Qiu Q, Yang XP, et al. An outbreak of Bergerman's legionnaires' disease occurred at a recruit training camp on the outskirts of Beijing. Chin J Epidemiol. (2001) 03:26–7. doi: 10.3760/j.issn:0254-6450.2001.03.008
49. Peng XM, Wu J, Li XY, Wang XM, Teng RM, He X, et al. Investigation of an outbreak of Pontiac fever legionellosis caused by a hot water shower system. Chin J Epidemiol. (2004) 25:1. doi: 10.3760/j.issn:0254-6450.2004.12.024
50. Bartram J, Chartier Y, Lee JV, Pond K, Surman-Lee S. Legionella and the Prevention of Legionellosis. Genava: World Health Organization (2007).
51. World Health Organization. WHO Guidelines for Indoor Air Quality Dampness & Mould. (2009). Available online at: http://www.euro.who.int/en/publications/abstracts/who-guidelines (accessed June 10, 2024).
52. World Health Organization. Guidelines for Drinking-Water Quality. Incorporating the 1st Addendum. 4th ed. Available online at: https://www.who.int/publications-detail-redirect/9789241549950 (accessed June 10, 2024).
53. Salah S, Lee RA, Camins B, Sidari F. From outbreak to compliance and beyond: UAB Medicine's successful implementation of a water safety program. Infect Control Hosp Epidemiol. (2020) 41:S479. doi: 10.1017/ICE.2020.1155
54. Marino F, Mazzotta M, Pascale MR, Derelitto C, Girolamini L, Cristino S. First water safety plan approach applied to a dental clinic complex: Identification of new risk factors associated with Legionella and P. aeruginosa contamination, using a novel sampling, maintenance and management program. J Oral Microbiol. (2023) 15:2223477. doi: 10.1080/20002297.2023.2223477
55. European Working Group for Legionella Infections. European Guidelines for Control and Prevention of Travel Associated legionnaires' Disease (R). Stockholm (2005). p. 5–79.
56. European Centre for Disease Prevention and Control. European Legionnaires'Disease Surveillance Setwork (ELDSNet), Operating Procedures. Stockholm (2012). p. 2–3.
57. European Working Group for Legionella Infections. EWGLI Technical Guidelines for the Investigation Control and Prevention of Travel Associated Legionnaires' Disease. Stockholm: European Commission Funding (2011). p. 16–30.
58. European Agency for Safety and Health at Work. Legionella and Legionnaires' Disease: A policy Overview. Stockholm: Publications Office of the European Union (2012). p. 19–23.
59. Hunter B, Wilbur L. Legionellosis- United States, 2000-2009. Am J Transplant. (2011) 60:1083–6. doi: 10.1016/j.annemergmed.2012.04.015
60. EPA. National Primary Drinking Water Regulations. Environmental Protection Agency (2024). Available online at: https://www.epa.gov/ground-water-and-drinking-water/national-primary-drinking-water-regulations (accessed June 10, 2024).
61. US CDC. Toolkit: Controlling Legionella in Common Sources of Exposure. Available online at: https://www.cdc.gov/control-Legionella/php/toolkit/control-toolkit.html (accessed June 11, 2024).
62. Li WY Li FS, Gao NY. Japan's latest drinking water quality standards and related management. China Water Supply Drainage. (2004) 5:104–6. doi: 10.3321/j.issn:1000-4602.2004.05.035
63. Standards Australia. AS/NZS 3666.1 Air-Handling and Water Systems of Buildings - Microbial Control (2012).
64. Queensland Health. Review of the Prevention and Control of Legionella pneumophila infection in Queensland. Brisbane, QLD: Chief Health Officer Branch, Queensland Health (2013).
65. enHealth. Guidelines for Legionella control in the Operation and Maintenance of Water Distribution Systems in Health and Aged Care Facilities. Canberra, ACT (2015).
66. Chaudhry R, Sreenath K, Agrawal SK, Valavane A. Legionella and Legionnaires' disease: time to explore in India. Indian J Med Microbiol. (2018) 36:324–33. doi: 10.4103/ijmm.IJMM_18_298
67. Sreenath K, Chaudhry R, Vinayaraj EV, Dey AB, Kabra SK, Thakur B, et al. Distribution of virulence genes and sequence-based types among Legionella pneumophila isolated from the water systems of a tertiary care hospital in India. Front Public Health. (2020) 8:596463. doi: 10.3389/fpubh.2020.596463
68. Żak M, Zaborowski P. Legionella: Law and Recommendations in Poland and in the World. Medycyna Rodzinna (2011).
69. World Health Organization. Disease Outbreak News; Legionellosis in Poland. Available online at: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON487 (accessed June 22, 2024).
70. Shen F, Jia Y, Zhang Y, Zhao R, Pan X. Construction of hegionellosis health risk assessment index system for cooling towers in public buildings. J Environ Health. (2017) 34:142–5. doi: 10.16241/j.cnki.1001-5914.2017.02.012
71. Collins S, Stevenson D, Bennett A, Walker J. Occurrence of Legionella in UK household showers. Int J Hyg Environ Health. (2017) 220:401–6. doi: 10.1016/j.ijheh.2016.12.001
72. Nocker A, Schulte-Illingheim L, Frösler J, Welp L, Sperber O, Hugo A. Microbiological examination of water and aerosols from four industrial evaporative cooling systems in regard to risk of Legionella emissions and methodological suggestions for surveillance. Int J Hyg Environ Health. (2020) 229:113591. doi: 10.1016/j.ijheh.2020.113591
73. Niculita-Hirzel H, Vanhove AS, Leclerc L, Girardot F, Pourchez J, Allegra S. Risk exposure to Legionella pneumophila during showering: the difference between a classical and a water saving shower system. Int J Environ Res Public Health. (2022) 19:3285. doi: 10.3390/ijerph19063285
74. Montagna MT, De Giglio O, Cristina ML, Napoli C, Pacifico C, Agodi A, et al. Evaluation of Legionella air contamination in healthcare facilities by different sampling methods: an Italian multicenter study. Int J Environ Res Public Health. (2017) 14:670. doi: 10.3390/ijerph14070670
75. International Organization for Standardization. ISO11731:2017-05 Water Quality-Enumeration of Legionella. Geneva: ISO (2017).
76. Whiley H, Taylor M. Legionella detection by culture and qPCR: comparing apples and oranges. Crit Rev Microbiol. (2016) 42:65–74. doi: 10.3109/1040841X.2014.885930
77. Chen MC, Liu JZ, Chen ZY, Chen XL. Contamination status and virulence gene carriage of Legionella in cooling tower water of public places in Quanzhou City, Fujian Province, 2008-2019. Dis Surveill. (2020) 35:1115–9. doi: 10.3784/j.issn.1003-9961.2020.12.012
78. Pan LJ, Zhang BY, Chen XD, Zhou TS, Wang JQ. Research on Legionella bioaerosol monitoring method in central air conditioning ventilation system. J Environ Health. (2010) 3:2. doi: 10.16241/j.cnki.1001-5914.2010.03.029
79. International Organization for Standardization. ISO/TS12869:2019 Water Quality – Detection and Quantification of Legionella spp. and/or Legionella pneumophila by Concentration and Genic Amplification by Quantitative Polymerase Chain Reaction (qPCR). Geneva: ISO (2019).
80. Sánchez-Parra B, Núñez A, Moreno DA. Preventing legionellosis outbreaks by a quick detection of airborne Legionella pneumophila. Environ Res. (2019) 171:546–9. doi: 10.1016/j.envres.2019.01.032
81. Ren M, Zhang SK, Yang B, Wang Y, Hu Z. Performance evaluation of Legionella pneumophila colloidal gold test paper. Chin J Biol Prod. (2023) 36:306–14. doi: 10.13200/j.cnki.cjb.003835
82. Mentasti M, Cassier P, David S, Ginevra C, Gomez-Valero L, Underwood A, et al. Rapid detection and evolutionary analysis of Legionella pneumophila serogroup 1 sequence type 47. Clin Microbiol Infect. (2017) 23:264.e1–9. doi: 10.1016/j.cmi.2016.11.019
83. David S, Rusniok C, Mentasti M, Gomez-Valero L, Harris SR, Lechat P, et al. Multiple major disease-associated clones of Legionella pneumophila have emerged recently and independently. Genome Res. (2016) 26:1555–64. doi: 10.1101/gr.209536.116
84. Weiss D, Boyd C, Rakeman JL, Greene SK, Fitzhenry R, McProud T, et al. A large community outbreak of Legionnaires' disease associated with a cooling tower in New York City, 2015. Public Health Rep. (2017) 132:241–50. doi: 10.1177/0033354916689620
85. Bartley PB, Ben Zakour NL, Stanton-Cook M, Muguli R, Prado L, Garnys V, et al. Hospital-wide eradication of a nosocomial Legionella pneumophila serogroup 1 outbreak. Clin Infect Dis. (2016) 62:273–9. doi: 10.1093/cid/civ870
86. Graham RM, Doyle CJ, Jennison AV. Real-time investigation of a Legionella pneumophila outbreak using whole genome sequencing. Epidemiol Infect. (2014) 142:2347–51. doi: 10.1017/S0950268814000375
87. Nisar MA, Ross KE, Brown MH, Bentham R, Best G, Whiley H. Detection and quantification of viable but non-culturable Legionella pneumophila from water samples using flow cytometry-cell sorting and quantitative PCR. Front Microbiol. (2023) 14:1094877. doi: 10.3389/fmicb.2023.1094877
88. Reuter C, Hentschel S, Breitenstein A, Heinrich E, Aehlig O, Henkel T, et al. Chip—based duplex real—time PCR for water quality monitoring concerning Legionella pneumophila and Legionella spp. Water Environ J. (2021) 35:371–80. doi: 10.1111/wej.12635
89. Wickenberg L, Gabrie K, McCarthy P, Cain M. Validation of PVT VIABLE® for detection of Legionella in potable and non-potable water: AOAC performance tested method SM 082303. J AOAC Int. (2024) 107:120–8. doi: 10.1093/jaoacint/qsad112
90. Allegra S, Grattard F, Girardot F, Riffard S, Pozzetto B, Berthelot P. Longitudinal evaluation of the efficacy of heat treatment procedures against Legionella spp. in hospital water systems by using a flow cytometric assay. Appl Environ Microbiol. (2011) 77:1268–75. doi: 10.1128/AEM.02225-10
92. Han XY. Effects of climate changes and road exposure on the rapidly rising Legionellosis incidence rates in the United States. PLoS ONE. (2021) 16:e0250364. doi: 10.1371/journal.pone.0250364
93. Gleason JA, Kratz NR, Greeley RD, Fagliano JA. Under the weather: Legionellosis and meteorological factors. Ecohealth. (2016) 13:293–302. doi: 10.1007/s10393-016-1115-y
94. Han XY. Solar and climate effects explain the wide variation in Legionellosis incidence rates in the United States. Appl Environ Microbiol. (2019) 85:e01776–19. doi: 10.1128/AEM.01776-19
95. Passer JK, Danila RN, Laine ES, Como-Sabetti KJ, Tang W, Searle KM. The association between sporadic Legionnaires' disease and weather and environmental factors, Minnesota, 2011-2018. Epidemiol Infect. (2020) 148:e156. doi: 10.1017/S0950268820001417
96. Beauté J, Sandin S, Uldum SA, Rota MC, Brandsema P, Giesecke J, et al. Short-term effects of atmospheric pressure, temperature, and rainfall on notification rate of community-acquired Legionnaires' disease in four European countries. Epidemiol Infect. (2016) 144:3483–93. doi: 10.1017/S0950268816001874
Keywords: Legionella, built environment, aerosol, transmission risk, monitoring
Citation: Yao XH, Shen F, Hao J, Huang L and Keng B (2024) A review of Legionella transmission risk in built environments: sources, regulations, sampling, and detection. Front. Public Health 12:1415157. doi: 10.3389/fpubh.2024.1415157
Received: 10 April 2024; Accepted: 08 July 2024;
Published: 26 July 2024.
Edited by:
Mohiuddin Md. Taimur Khan, Washington State University Tri-Cities, United StatesReviewed by:
Tarikuwa Natnael, Wollo University, EthiopiaMuhammad Atif Nisar, Flinders University, Australia
Copyright © 2024 Yao, Shen, Hao, Huang and Keng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fan Shen, ZmVpc2hlcnNoZW5AMTI2LmNvbQ==
 Xiao Hui Yao
Xiao Hui Yao Fan Shen
Fan Shen Jing Hao2
Jing Hao2