- 1Department of Parasitology and Medical Entomology, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
- 2Gua Musang District Health Office, Kelantan, Malaysia
- 3Department of Community Health, Faculty of Public Health, Kasetsart University, Sakon Nakhon, Thailand
Introduction: Anaemia remains a primary concern of public health in developing countries. Indigenous populations are a significant and frequently underreported group at risk for anaemia. This study aimed to assess the prevalence of anaemia and identify its determinants in the Temiar sub-ethnic indigenous Orang Asli (OA) community in Peninsular Malaysia.
Methodology: A community-based cross-sectional study was conducted among 640 indigenous Temiar OA participants from a remote settlement in Gua Musang, Kelantan, Malaysia. Data was collected using face-to-face interviews with a standardised pretested questionnaire and through blood samples collected for haemoglobin (Hb) testing. Anaemia status was determined using the Hb level cut-off established by the World Health Organization (WHO). Descriptive analysis was used to determine the prevalence of anaemia, while multiple logistic regression was used to determine factors associated with anaemia.
Results: The overall anaemia prevalence was 44.7% (286/640), and the prevalence rates of mild, moderate and severe anaemia were 42.7, 50.7 and 6.6%, respectively. Anaemia-specific prevalence varied significantly by age group (p < 0.001) and was highest in the ≤5 group for both moderate anaemia (43.4%) and severe (42.1%), followed by the 6–17 age group for mild anaemia (39.3%). The prevalence of anaemia was also highest among students (53.9%), with a significant difference observed between the three anaemia severity classifications (p = 0.002). In the multivariate logistic regression, only age groups of 6–17 (adjusted odds ratio [aOR] 0.38, p < 0.001), 18–40 (aOR 0.18, p < 0.001) and > 40 (aOR 0.25, p < 0.001) were significantly associated with the lower odds of anaemia in the population.
Conclusion: This study has highlighted the high prevalence of anaemia among indigenous OA in Peninsular Malaysia and revealed that younger children were positively associated with childhood anaemia. Effective interventions and special attention to this indigenous population need to be implemented to reduce the risk of anaemia.
1 Introduction
Anaemia has been identified as a major worldwide public health issue as it affects more than two billion people or represents 24.8% of the world’s population (1). Anaemia is a condition in which the number of red blood cells or the haemoglobin (Hb) concentration within the human body is lower than normal (2, 3). Haemoglobin is required to carry oxygen, and the blood’s capacity to deliver oxygen to the body’s tissues will be reduced if the individual has extremely low or abnormal amounts of red blood cells or insufficient Hb. This condition will lead to general symptoms, including recurrent vagueness, exhaustion, shortness of breath and poor focus (4).
Anaemia has multiple precipitating factors and may result from a multifactorial deficiency of micronutrients (e.g., iron, folic acid, vitamin A and B12), infectious diseases (e.g., malaria and helminth) and inherited disorders (e.g., sickle cell disease and thalassemia) (5, 6). Anaemia affects almost all age groups, from infants to the older adult. However, blood loss from menstruation in women of childbearing age are at a higher risk of acquiring a disease (7). Infants between the ages of 1 and 2 are also at risk for anaemia if they do not consume enough iron in their meals (8). According to the World Health Organization (WHO), 42% of children under five years old and 40% of pregnant women worldwide are estimated to be anaemic (9). Furthermore, people who live in the less developed areas of the country and among hard-to-reach populations are more susceptible to anaemia because of poor quality diet, social–emotional and exposure to parasitic infections (10).
The indigenous population is an important and often unreported group at risk of anaemia (11). Anaemia is a mild concern among indigenous people living in developed countries, but it has become a significant concern in the world’s poorest regions (11). Indigenous communities who are minorities often experience substantial and persistent differences in the socioeconomic determinants of health, such as access to healthcare services, education, work, housing and food security (12). This is related to the causes of anaemia, which include a lack of exercise, unfavourable environmental conditions and an association with infectious diseases like malaria and intestinal parasites (5, 6).
In Malaysia, the indigenous communities known as Orang Asli (OA) represent 0.6% of the total population of Malaysians (13). The OA in Peninsular Malaysia is divided into three main lines (i.e., Negrito, Senoi and Proto-Malay). The Senoi lineage is the largest ethnical group, constituting 55% of the total OA population, with a large majority from the Temiar sub-ethnic (Malaysia Department of Orang Asli). Roughly 37% of 869 OA villages throughout the country are still located in remote and forested areas (14). Poverty and remote settlements have previously been reported to contribute to numerous health problems related to malnourishment and the high prevalence of infectious diseases in these communities (15–26). Although several studies have assessed the nutritional status and metabolic syndrome among the OA in Malaysia, there is a lack of information on anaemia status among this population, especially among the Temiar sub-ethnic indigenous OA communities. A recent study conducted among the Negrito OA from inland jungle villages and resettlement at town peripheries reported an overall prevalence of anaemia among children and adolescents was 68.4% (23). Previous studies have also shown that the contributing factors of anaemia among the indigenous OA population in Malaysia are largely due to poor dietary intake of iron, recurrent infections and low socioeconomic status (27, 28).
This study aimed to determine the prevalence and associated risk factors of anaemia among Temiar sub-ethnic indigenous OA communities in Peninsular Malaysia. Results from this study would be useful for informing national prevention strategies and could be used by several already existing national agencies dedicated to improving morbidity and mortality among indigenous peoples.
2 Methods
2.1 Ethics statement
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Medical Ethics Committee of the National University of Malaysia (Reference No. UKM PPI/111/8/JEP-2019-148) and the Department of Orang Asli Development, Ministry of Rural and Regional Development Malaysia. Participants were sensitised to the study objectives and procedures by the local health district personnel for the study participation.
2.2 Study area and population
The study was conducted in Pos Kuala Betis (latitude 4o53´22”N; longitude 101o45´30″E), a clustered rural resettlement of five villages (i.e., Angkek, Betak, Galas, Lambok and Podek) located at the Gua Musang district, Kelantan State, Peninsular Malaysia (Figure 1). The Temiar sub-ethnic of the Senoi was known to be the main indigenous OA in these villages. The present study is the first to assess the prevalence and severity of anaemia in the area and also builds on previous studies on malaria among these communities (25, 26). While the main economic activity was centred on agriculture, such as palm oil plantation, the livelihood of the villagers mainly depended on rubber-tapping, labourers, farmers and gathering and selling forest products (29).
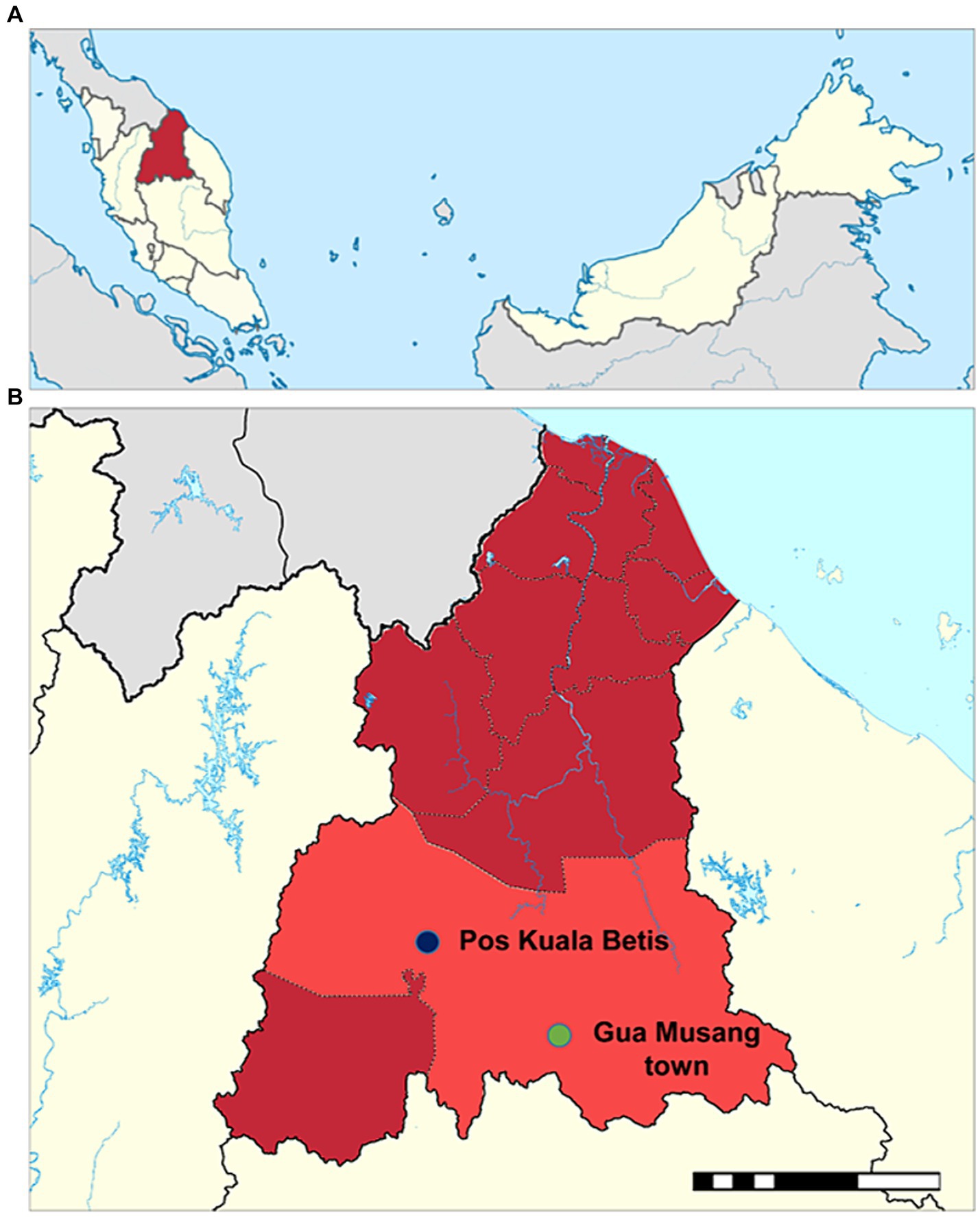
Figure 1. Map of the study setting. (A) Map of Malaysia showing the location of Kelantan State (dark red). (B) Map of Gua Musang district (light red) in Kelantan State showing the location of Pos Kuala Betis. The study in Pos Kuala Betis is located approximately 40 km from Gua Musang town.
2.3 Study design, sample size and sampling techniques
A community-based cross-sectional survey was carried out between June and July 2019 (29). All indigenous Temiar OA of both genders residing in the study villages and aged one and older were invited to take part in the study. The sample size for study participation was calculated using the following Cochran’s formula: N = z2p(1–p)/e2, where z is the confidence interval which is set at 95% (z-value of 1.96); (p) is the expected prevalence of anaemia of 68% from a previous study (23), and (e) is the allowed error margin which is set at 5%. In addition, contingencies were adjusted by adding another 30% of individuals, giving us a minimum of 435 participants to be sampled.
Participants were explained about the study protocol, and informed consent was documented. For the illiterate participant, informed consent was obtained in the presence of an independent literate witness. For children and adolescents below 18 years old, informed consent was obtained from parents or legal guardians. All participants were also informed of their right to withdraw from the study at any time without prior notice and prejudice. District healthcare providers and community leaders were purposely involved in the study to facilitate participation and cooperation among the community (29). Participants were divided into four groups following age stratification practices in Malaysia, namely infants and children (≤5 years), school-going children and adolescents (6–17 years), young adults (18–40 years) and older adults (>40 years). As a token of appreciation, the participants who contributed to the research were given some refreshments (e.g., snacks and drinks) at the end of the sampling activity.
2.4 Data collection
A structured questionnaire was used for collecting data that assessed factors associated with anaemia in the community. The questionnaire was developed from standard closed-ended questions adopted from a previous study by Munajat et al. (29). The questionnaire was written in English and then translated into Malay. A peripheral blood sample was obtained from each participant’s fingertip. The first and second droplets of blood were discarded after puncturing the side of the fingertip with a puncture needle, and blood was collected from the third drop. Hb level was measured with the HemoCue Hb 201 Analyzer (HemoCue, Sweden) and was expressed as g/L. Anaemia was classified as mild, moderate or severe based on the concentrations of Hb in the blood. According to WHO criteria (30), for children aged 6–59 months and pregnant women, anaemia is defined at Hb <110 g/L (100–109, 70–99, and < 70 g/L correspond to mild, moderate and severe anaemia, respectively). For children aged 5–11 years old, anaemia is defined as Hb <115 g/L, in which 110–114, 80–109, and < 80 g/L correspond to mild, moderate and severe anaemia, respectively. While for children 12–14 years old and non-pregnant women (15 years of age and above), anaemia is defined as Hb <120 g/L (110–119, 80–109, <80 g/L refers to mild, moderate and severe anaemia, respectively). Lastly, in men (15 years of age and above), anaemia is defined as Hb <130 g/L, in which 110–12.9, 80–109, <80 g/L correlate to mild, moderate and severe anaemia, reciprocally (30).
2.5 Statistical analysis
All survey data were double-entered into Microsoft Excel spreadsheets and cross-checked for errors. Data were processed and analysed using STATA/SE 13.1 statistical software package (StataCorp, United States). Differences in proportions were tested using the Chi-squared test or Fisher’s exact test. 95% confidence intervals (95% CI) were estimated to provide uncertainty surrounding the point estimates. Logistic regression analysis was used to identify factors associated with anaemia in the community. Gender, age group, and village were considered explanatory variables in the univariate analyses. The reference group for the logistic regression analysis was based on the lowest prevalence of anaemia in each category. All variables with a p-value of <0.50 from the likelihood ratio test in the univariate analyses were included in the multivariate logistic regression model, and stepwise backward elimination was used to identify the main risk factors for anaemia (31). A p < 0.05 was considered statistically significant.
3 Results
3.1 Characteristic of study participants
A total of 640 individuals from Pos Kuala Betis (representing 68% of the combined population in the five villages) participated in this study (Table 1). The surveillance coverage varied among villages from 50 to 90%, being mostly females (58%), and the age of participants ranged between 1 to 88 years old (mean [standard deviation; SD] age of 22.6 [17.8] years). A slight majority of the participants were school-age children and adolescents in the 6–17 age group (34.1%; 95% CI: 30.4–37.9). About 58% (95% CI: 54.1–61.8) of the participants reported enrolling in formal education at least once in their lifetime, with significant differences in education levels between the villages (p < 0.001). Most participants (44.4%; 95% CI: 39.7–49.2) were students with significant differences in each village (p = 0.028). The majority of employed participants (62.6%; 95% CI: 52.3–72.1) received less than Malaysian Ringgit (MYR) 500 (i.e., ≤USD105) per month. Of the entire participants, the majority 423 (86.7%; 95% CI: 83.3–89.6) had food security and significantly higher than those who experienced food insecurity between villages (p = 0.024).
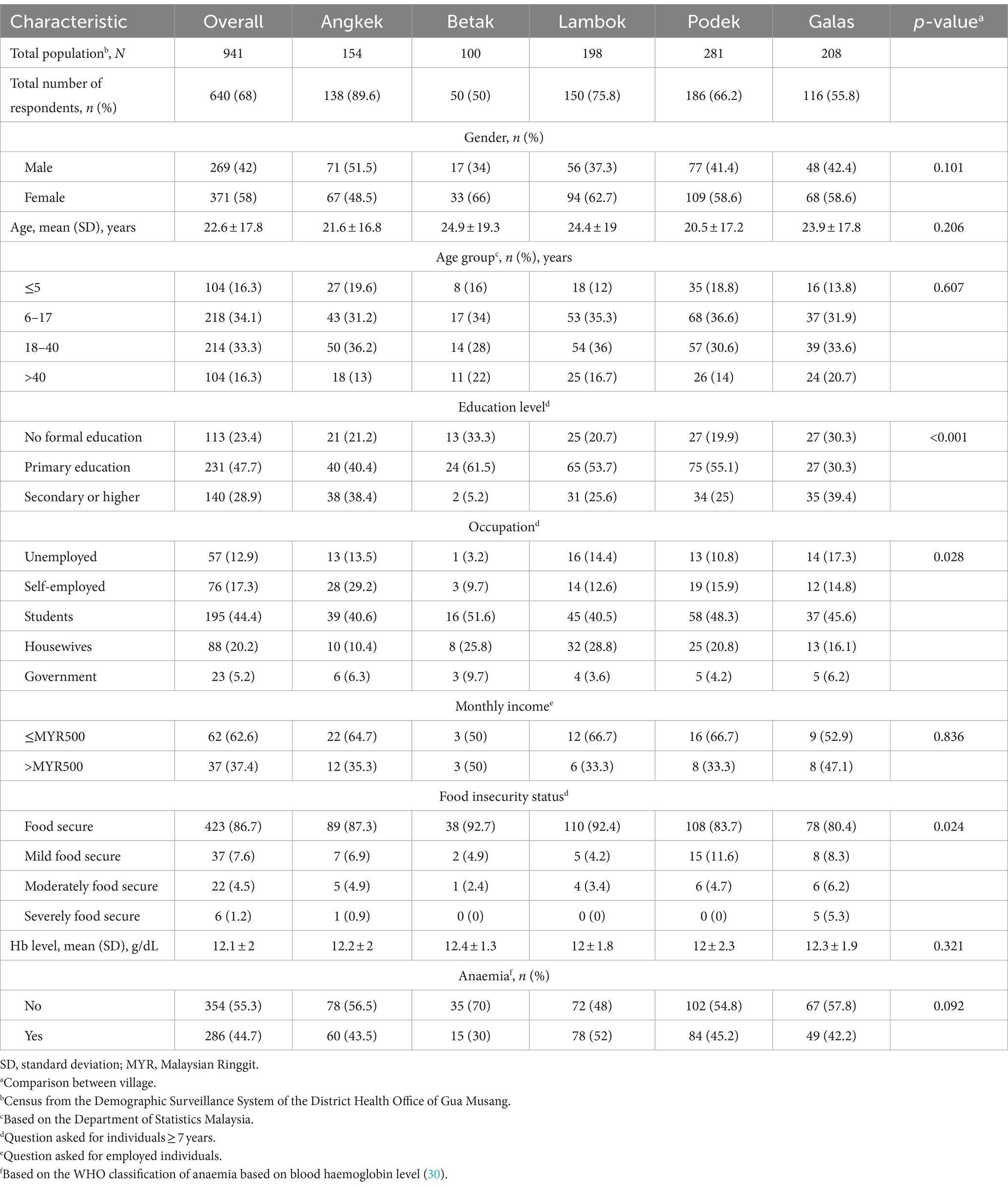
Table 1. Demographic characteristic and anaemia status of indigenous Temiar Orang Asli population in five settlements of Pos Kuala Betis, Kelantan, Malaysia.
3.2 Anaemia-specific prevalence
Of all participants, the overall mean haemoglobin level and prevalence of anaemia were 12.1 ± 2 g/dL and 44.7% (95% CI: 40.8–48.6) and not significantly different between villages (p > 0.05) (Table 1). The anaemia-specific prevalence among participants in Pos Kuala Betis is shown in Table 2. The prevalence of mild, moderate and severe anaemia was 42.7% (95% CI: 36.9–48.6), 50.7% (95% CI: 44.7–56.6) and 6.6% (95% CI: 4.1–10.2), respectively. Although the prevalence of anaemia was highest among females (57%; 95% CI: 51.2–62.8), no significant difference was observed between the three anaemia severity classifications (p = 0.691). Nevertheless, the prevalence of anaemia varied significantly by age group (p < 0.001) and was highest in the ≤5 group for both moderate anaemia (43.4%; 95% CI: 35.2–51.9) and severe anaemia (42.1%; 95% CI: 20.3–66.5), followed by the 6–17 age group for mild anaemia (39.3%; 95% CI: 30.6–48.6). Albeit no significant differences were observed between anaemia severity classifications, a high prevalence of anaemic individuals was observed in those living in Podek village, with primary education, monthly income ≤MYR500 and food security with 29.4% (95% CI: 24.2–35.1), 45.7% (95% CI: 38.4–53.1), 62.5% (95% CI: 40.6–81.2) and 87.4% (95% CI: 81.7–91.9), respectively. Interestingly, the prevalence of anaemia was highest among students (53.9%; 95% CI: 46.1–61.7), with a significant difference observed between the three anaemia severity classifications (p = 0.002).
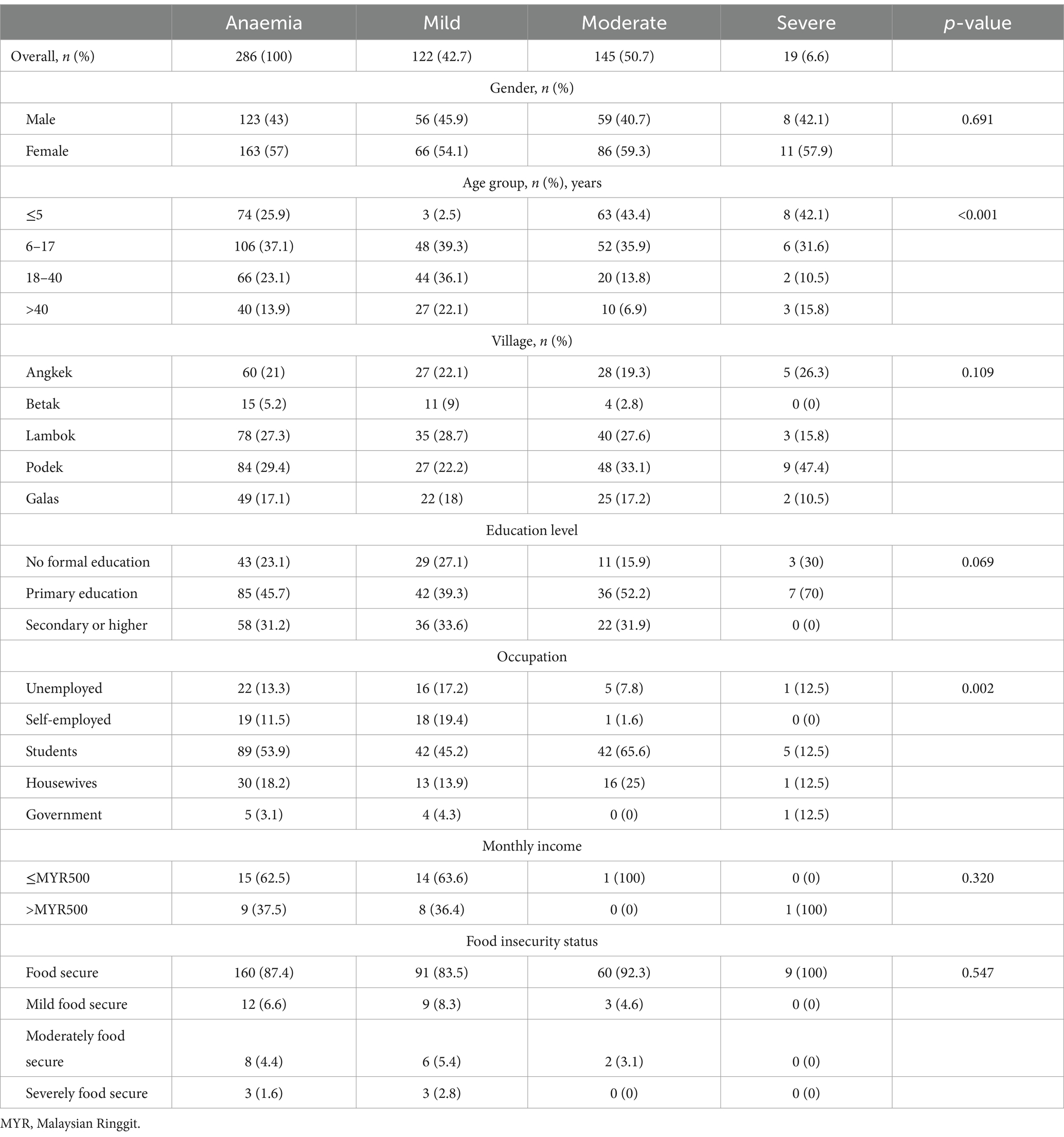
Table 2. Specific prevalence of anaemia among indigenous Temiar Orang Asli communities in Pos Kuala Betis, Kelantan, Malaysia.
3.3 Factor associated with anaemia
Results for all significant co-variables associated with anaemia in univariate analysis (p < 0.05) are provided in Table 3. These variables were further used to build multivariate models with stepwise forward selection. The final model in multivariate logistic regression showed that age groups of 6–17 (adjusted odds ratio [aOR] 0.38 [95% CI: 0.23–0.63], p < 0.001), 18–40 (aOR 0.18 [95% CI: 0.11–0.31], p < 0.001) and > 40 (aOR 0.25 [95% CI: 0.14–0.45], p < 0.001) were significantly associated with retaining the lower odds of anaemia in the population.
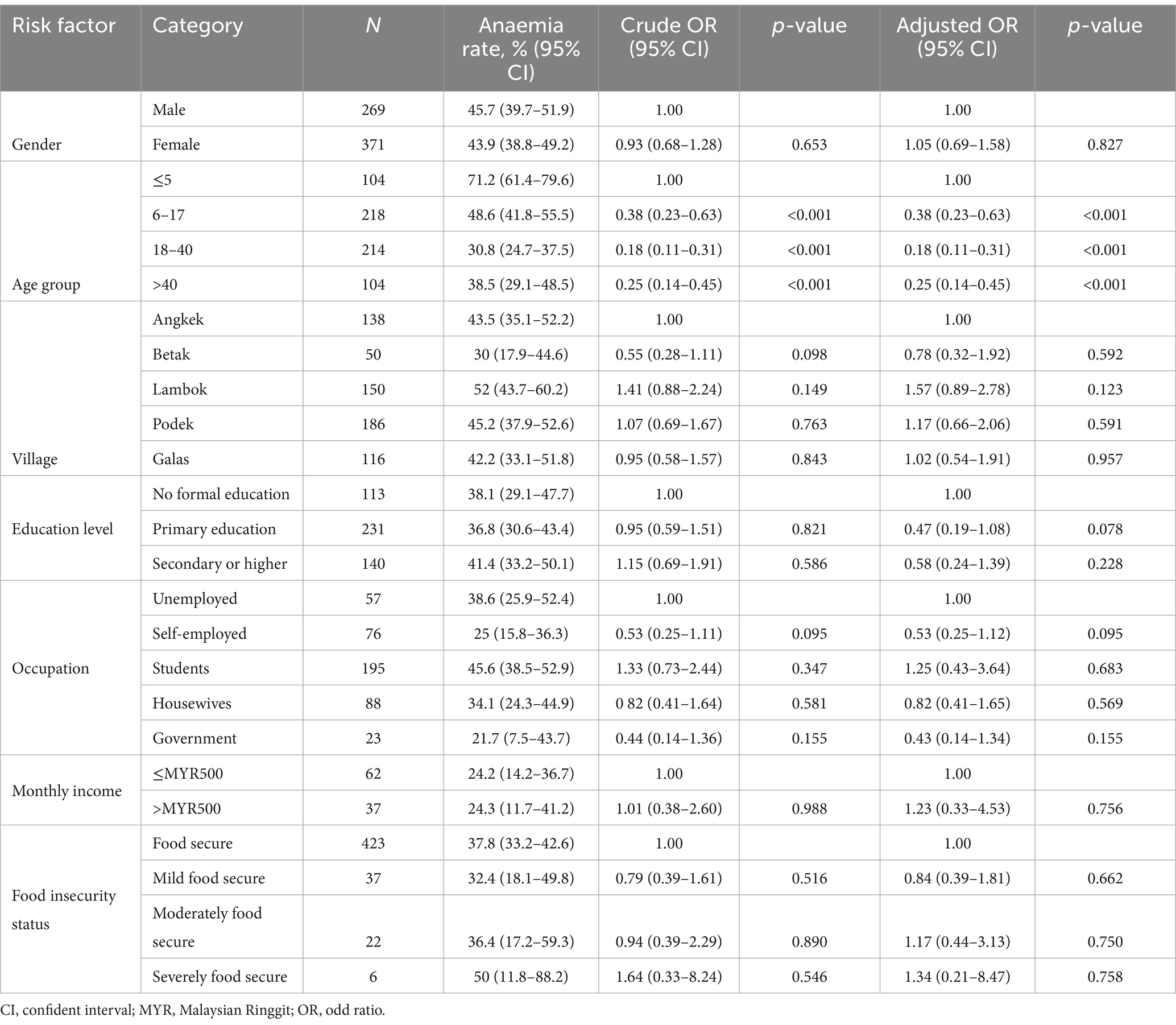
Table 3. Factors associated with anaemia among indigenous Temiar Orang Asli in Pos Kuala Betis, Kelantan, Malaysia.
4 Discussion
This study determined the current status and risk factors of anaemia among the Temiar sub-ethnic indigenous OA in Peninsular Malaysia. Overall, this study has shown a high anaemia prevalence of 44.7%, particularly among children and adolescents and considered a severe level (i.e., >40%) based on the ranges of anaemia among indigenous populations globally (11). Although this figure was two folds higher than the anaemia incidence among the general Malaysian population, i.e., 24.2% (32), the prevalence of anaemia among the Temiar OA was within similar ranges reported in other indigenous tribes in Malaysia, i.e., the Senoi and Semai in Peninsular Malaysia (16, 17), and Penan and Iban in Malaysian Borneo (33, 34). However, these findings were contrary to a recent study conducted among the present-day hunter-gatherer of indigenous Negritos OA, with an overall anaemia prevalence of 68.4% (23). As compared to the other main tribes, the prevalence of glucose-6 phosphate dehydrogenase (G6PD) deficiency was reported to be high among Negritos OA (i.e., 46.6%); hence this could further risk them to have haemolytic anaemia (35). Apart from that, the drastic nutritional transition from a traditional to a new modern lifestyle, relocation to an unfavourable location and inability to cope with a new environment among Negritos communities also contributed to the high prevalence of anaemia (23). The fact that a high prevalence of anaemia among indigenous populations is widely distributed in Malaysia suggests that common disparities in health among these diverse groups of people are attributed to a higher risk of anaemia.
The finding of this study demonstrated that the prevalence of anaemia was significantly higher in children and adolescents (i.e., ≤17 years, 55.9%) compared to adults (i.e., ≥18 years, 33.3%). This is consistent with earlier local studies conducted among OA in Peninsular Malaysia (15, 17). The variation in prevalence and severity of anaemia tends to be convex with age, increasing in childhood and decreasing in adulthood (33). This may be because the child’s exposure to being anaemic rises as he or she gets older. It is common for children to be more active, curious, and eager to learn new things in their surroundings. However, many of them are still unaware of personal and appropriate hygiene practices and the consequences of exposing themselves to infectious organisms due to their early age. Meanwhile, as in agreement with a previous study by Muslim et al. (23), gender stratification in this study showed no difference between the prevalence of anaemia between females and males, although it is well acknowledged that females tend to be more anaemic as a result of physiological differences (7, 36).
The present study also revealed that anaemia-specific prevalence of both moderate and severe anaemia was highest in children aged less than five years old with 43.4 and 42%, respectively. Besides, the odds of anaemia were lower in the 6–17 group when compared to those in the ≤5 group in the population. These scenarios agree with previous reports (15, 23, 27), whereby the younger children from the indigenous population in Malaysia had a higher prevalence of anaemia than older children. In the OA community, older children are usually enrolled in boarding schools provided by the government. It is postulated that a feeding intervention implemented in the boarding school could reflect the lower prevalence of anaemia among older children. Previous studies have shown that the contributing factors of anaemia among children of the indigenous population in Malaysia are largely due to poor dietary intake of iron, recurrent infections and low socioeconomic status (27, 28). Furthermore, preschoolers depend on their caregivers to provide food for most of the day. Because of that, a caregiver with a lack of knowledge of proper nutrition, low socioeconomic status, unemployment and low level of education attributed to childhood malnutrition. This issue deserves attention because chronic anaemia during childhood has been shown to be associated with retardation in physical development and cognition, while severe anaemia is responsible for more than half of the deaths in children under 5 years of age (37).
Local variation in anaemia prevalence was also observed among communities in the same clustered rural settlement. For example, the present study showed that anaemia prevalence in the five villages in Pos Kuala Betis ranged from 30 to 52%. The heterogeneity in anaemia prevalence within indigenous communities due to the difference in location and access to food has also been reported in other settings (38). Like many other indigenous communities globally (11), OA communities in Malaysia are often located in deeply remote areas with a lack of basic amenities such as piped water supply, electricity, toilet facility, garbage disposal service, as well as limited access to government health programs (21, 39). Tackling these issues could ultimately reduce intestinal parasitic transmission, subsequently lowering the prevalence of anaemia in OA communities.
A number of caveats should be considered in this study. First, this study lacks of potential sample representative. The participants were drawn from a single remote settlement, which may not fully capture the diversity and variability of the broader Temiar OA communities in Peninsular Malaysia. This limitation poses a challenge to the generalizability of our findings across the entire Temiar population. Furthermore, the reliance on a single settlement limits our ability to account for intra-community variations within the Temiar population. The sample may not encompass the full spectrum of age, gender, and socio-economic status distributions present in the wider community, potentially leading to biased estimates of anaemia prevalence and severity. To address these limitations in future research, it would be beneficial to include participants from multiple settlements across different regions. Second, although the cross-sectional nature of the research design was efficient and cost-effective, it has an inherent selection bias and does not allow causality to be established. While the cross-sectional approach allows for the identification of associations and prevalence at a specific point in time, it does not provide insights into the temporal sequence of events or the direction of these associations. This limitation is particularly important when considering the multifactorial nature of anaemia, where various factors such as infections, and socio-economic conditions may interplay. To gain a more comprehensive understanding of the factors contributing to anaemia in the Temiar population, longitudinal studies are essential. Third, the lack of data on micronutrient deficiencies, infectious diseases and genetic predispositions is important for understanding the causes of anaemia in the study population. While the study provides valuable data on the prevalence and severity of anaemia, it does not delve into the potential contributors to this condition. This omission hinders our ability to identify and address the specific causes of anaemia in this community. Micronutrient deficiencies, particularly of iron, vitamin B12, and folate, are well-known contributors to anaemia (5, 6). Without assessing the nutritional status of the participants, it is challenging to determine the extent to which these deficiencies may be driving the observed anaemia prevalence. Similarly, infectious diseases, including helminth infections, and chronic inflammatory conditions, can significantly impact haemoglobin levels and anaemia risk. The absence of data on the presence or prevalence of these infections in the study population limits our understanding of their role in anaemia aetiology. Fourth, the use of capillary blood instead of venous samples can also constitute a source of bias. At the moment when the surveyor pricks the skin and collects blood drops, the Hb can be diluted with extracellular fluid through manipulation of the subject’s finger (40). The choice of capillary sampling was primarily driven by practical considerations, including the ease of collection in remote field settings and the reduced discomfort for participants. However, it is important to acknowledge that this choice may limit the comparability of our results with studies that utilize venous blood samples. Nonetheless, this technique offers many practical advantages and does not affect the quality of diagnosis at the population level (41).
Despite these limitations, studying anaemia prevalence among the Temiar OA community is crucial for several reasons. This study highlights the health disparities faced by indigenous populations, who often have limited access to healthcare and nutritional resources. Understanding anaemia prevalence in this specific community can help prioritize public health efforts and allocate resources effectively to address their unique health challenges. Additionally, data from the present study provide a baseline for monitoring health trends over time and assessing the effectiveness of interventions aimed at improving nutritional and health outcomes. This research also raises awareness about the broader social determinants of health affecting the Temiar OA community, such as poverty, education, and food security, which are critical for developing comprehensive health policies. Ultimately, these studies are a vital step towards achieving health equity and improving the overall well-being not just of the Temiar OA community, but of all indigenous ethnic groups in the country.
In conclusion, anaemia constitutes a major health problem, particularly among the school-age children of the Temiar sub-ethnic indigenous OA communities in Peninsular Malaysia. The magnitude of anaemia in this study carries public health importance, particularly in planning programs for community health and could help develop intervention strategies and target high-risk subpopulations in this vulnerable population group. Furthermore, the high prevalence of anaemia among the Temiar OA community underscores the urgent need for targeted interventions that address potential nutritional deficiencies, improve healthcare access, and tackle underlying socioeconomic determinants of health. By implementing culturally sensitive strategies and engaging community stakeholders, public health efforts can effectively reduce anaemia prevalence and improve overall health outcomes among the indigenous communities. While the study provides valuable insights into anaemia prevalence and severity among the Temiar OA in a specific settlement, caution should be exercised when extrapolating these findings to the broader population. A more comprehensive approach involving multiple settlements and diverse demographic groups would enhance the robustness and generalizability of future research in this area. Further research also needs to be done to ascertain the exact cause of anaemia in this community.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of the National University of Malaysia. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
ZI: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WW: Investigation, Methodology, Writing – review & editing. MS: Investigation, Methodology, Writing – review & editing. NG: Investigation, Methodology, Writing – review & editing. NH: Investigation, Methodology, Writing – review & editing. SA: Investigation, Methodology, Project administration, Writing – review & editing. AM: Investigation, Methodology, Writing – review & editing. SC: Conceptualization, Investigation, Methodology, Validation, Writing – review & editing. MM: Conceptualization, Investigation, Methodology, Resources, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Faculty of Medicine, National University of Malaysia (grant number: GP-K019336) and the ASEAN Science Technology and Innovation Fund (ASTIF) (grant number: FF-2019-124) from the ASEAN Secretariat.
Acknowledgments
We would like to extend our gratitude to the communities and community leaders for their support and participation in the survey. We wish to sincerely thank all members of the field team.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization . Worldwide prevalence of anemia 1993–2005. Global Database on Anemia. Geneva: WHO (2008).
2. Masukume, G, Khashan, AS, Kenny, LC, Baker, PN, and Nelson, GSCOPE Consortium. Risk factors and birth outcomes of anemia in early pregnancy in a nulliparous cohort. PLoS One. (2015) 10:e0122729. doi: 10.1371/journal.pone.0122729
3. Xu, M, Papageorgiou, DP, Abidi, SZ, Dao, M, Zhao, H, and Karniadakis, GE. A deep convolutional neural network for classification of red blood cells in sickle cell anemia. PLoS Comput. Biol. (2007) 13:e1005746. doi: 10.1371/journal.pcbi.1005746
4. Janz, TG, Johnson, RL, and Rubenstein, SD. Anemia in the emergency department: evaluation and treatment. Emerg Med Pract. (2013) 15:1–5.
5. Allali, S, Brousse, V, Sacri, AS, Chalumeau, M, and de Montalembert, M. Anemia in children: prevalence, causes, diagnostic work-up, and long-term consequences. Expert Rev Hematol. (2017) 10:1023–8. doi: 10.1080/17474086.2017.1354696
6. Jamnok, J, Sanchaisuriya, K, Sanchaisuriya, P, Fucharoen, G, Fucharoen, S, and Ahmed, F. Factors associated with anemia and iron deficiency among women of reproductive age in Northeast Thailand: a cross-sectional study. BMC Public Health. (2020) 20:102. doi: 10.1186/s12889-020-8248-1
7. Clark, SF . Iron deficiency anemia. Nutr Clin Pract. (2008) 23:128–41. doi: 10.1177/0884533608314536
8. Lopez, A, Cacoub, P, Macdougall, IC, and Peyrin-Biroulet, L. Iron deficiency anemia. Lancet. (2016) 387:907–16. doi: 10.1016/S0140-6736(15)60865-0
10. Kay, A, Leidman, E, Lopez, V, Wilkinson, C, Tondeur, M, and Bilukha, O. The burden of anemia among displaced women and children in refugee settings worldwide, 2013–2016. BMJ Glob Health. (2019) 4:e001837. doi: 10.1136/bmjgh-2019-001837
11. Khambalia, AZ, Aimone, AM, and Zlotkin, SH. Burden of anemia among indigenous populations. Nutr Rev. (2011) 69:693–719. doi: 10.1111/j.1753-4887.2011.00437.x
12. United Nations Inter-Agency Support Group . The Health of Indigenous Peoples. Geneva: IASG (2007).
13. Bedford, KJA . Gombak Hospital, the Orang Asli hospital: Government healthcare for the indigenous minority of Peninsular Malaysia. Indo Malay World. (2009) 37:23–44. doi: 10.1080/13639810902743032
14. Mason, R, and Arifin, SM. The ‘Bumiputera policy’: Dynamics and dilemmas. Special issues of Orang Asli. J Malays Stud. (2005) 21:315–29.
15. Ahmed, A, Al-Mekhlafi, HM, Al-Adhroey, AH, Ithoi, I, Abdulsalam, AM, and Surin, J. The nutritional impacts of soil-transmitted helminths infections among Orang Asli schoolchildren in rural Malaysia. Parasit Vectors. (2012) 5:1–9. doi: 10.1186/1756-3305-5-119
16. Aini, UN, Al-Mekhlafi, MS, Azlin, M, Shaik, A, Sa'iah, A, Fatmah, MS, et al. Serum iron status in Orang Asli children living in endemic areas of soil-transmitted helminths. Asia Pac J Clin Nutr. (2007) 16:724–30.
17. Al-Mekhlafi, MH, Surin, J, Atiya, AS, Ariffin, WA, Mahdy, AK, and Abdullah, HC. Anemia and iron deficiency anemia among aboriginal schoolchildren in rural Peninsular Malaysia: an update on a continuing problem. Trans R Soc Trop Med Hyg. (2008) 102:1046–52. doi: 10.1016/j.trstmh.2008.05.012
18. Dian, ND, Rahim, MAFA, Chan, S, and Idris, ZM. Non-human primate malaria infections: a review on the epidemiology in malaysia. Int J Environ Res Public Health. (2022) 19:7888. doi: 10.3390/ijerph19137888
19. Idris, ZM, Zainal, FNS, Ching, LS, Azmin, A, Hamdan, Z, Kamaruzaman, UA, et al. Malaria in urban Kuala Lumpur, Malaysia from 2005 to 2017. Travel Med Infect Dis. (2021) 41:102055. doi: 10.1016/j.tmaid.2021.102055
20. Liew, JWK, Mahpot, RB, Dzul, S, Abdul Razak, HAB, Ahmad Shah Azizi, NAB, Kamarudin, MB, et al. Importance of proactive malaria case surveillance and management in Malaysia. Am J Trop Med Hyg. (2018) 98:1709–13. doi: 10.4269/ajtmh.17-1010
21. Lim, YAL, Romano, N, Colin, N, Chow, SC, and Smith, HV. Intestinal parasitic infections amongst Orang Asli (indigenous) in Malaysia: has socioeconomic development alleviated the problem? Trop Biomed. (2009) 26:110–22.
22. Muslim, A, Sofian, SM, Shaari, SA, Hoh, BP, and Lim, YAL. Prevalence, intensity and associated risk factors of soil transmitted helminth infections: A comparison between Negritos (indigenous) in inland jungle and those in resettlement at town peripheries. PLoS Negl Trop Dis. (2019) 13:e0007331. doi: 10.1371/journal.pntd.0007331
23. Muslim, A, Lim, YAL, Mohd Sofian, S, Shaari, SA, and Mohd Zain, Z. Nutritional status, hemoglobin level and their associations with soil-transmitted helminth infections between Negritos (indigenous) from the inland jungle village and resettlement at town peripheries. PLoS One. (2021) 16:e0245377. doi: 10.1371/journal.pone.0245377
24. Nasr, NA, Al-Mekhlafi, HM, Ahmed, A, Roslan, MA, and Bulgiba, A. Towards an effective control programme of soil-transmitted helminth infections among Orang Asli in rural Malaysia. Part 2: Knowledge, attitude, and practices. Parasit Vectors. (2013) 6:1–12. doi: 10.1186/1756-3305-6-28
25. Rahim, MAFA, Munajat, MB, Dian, ND, Seri Rakna, MIM, Wahid, W, Ghazali, N, et al. Naturally acquired antibody response to Plasmodium falciparum and Plasmodium vivax among indigenous Orang Asli communities in Peninsular Malaysia. Front Cell Infect Microbiol. (2023) 13:1165634. doi: 10.3389/fcimb.2023.1165634
26. Dian, ND, Muhammad, AB, Azman, EN, Eddie, NA, Azmi, NI, Yee, VCT, et al. Evidence of submicroscopic Plasmodium knowlesi mono-infection in remote indigenous communities in Kelantan, Peninsular Malaysia. Am J Trop Med Hyg. (2023) 109:1081–5. doi: 10.4269/ajtmh.23-0184
27. Ngui, R, Lim, YAL, Kin, LC, Chuen, CS, and Jaffar, S. Association between anemia, iron deficiency anemia, neglected parasitic infections and socioeconomic factors in rural children of West Malaysia. PLoS Negl Trop Dis. (2012) 6:e1550. doi: 10.1371/journal.pntd.0001550
28. Roslie, R, Yusuff, ASM, and Parash, MTH. The prevalence and risk factors of iron deficiency anemia among rural school children in Kudat, Sabah. Malaysian J Med Health Sci. (2019) 15:54–60.
29. Munajat, MB, Rahim, MAFA, Wahid, W, Seri Rakna, MIM, Divis, PCS, Chuangchaiya, S, et al. Perceptions and prevention practices on malaria among the indigenous Orang Asli community in Kelantan, Peninsular Malaysia. Malar J. (2021) 20:202–9. doi: 10.1186/s12936-021-03741-y
30. World Health Organization . Hemoglobin concentrations for the diagnosis of anemia and assessment of severity. Geneva, Switzerland: WHO (2011).
31. Idris, ZM, Chan, CW, Kongere, J, Gitaka, J, Logedi, J, Omar, A, et al. High and heterogeneous prevalence of asymptomatic and sub-microscopic malaria infections on islands in Lake Victoria. Kenya Sci Rep. (2016) 6:36958. doi: 10.1038/srep36958
32. Awaluddin, SM, Ahmad, NA, Naidu, BM, Mohamad, MS, Yusof, M, Razak, MA, et al. A population-based anemia screening using point-of care in estimating prevalence of anemia in Malaysian adults: findings from a Nationwide survey. J Community Med Health Educ. (2017) 7:2161–711. doi: 10.4172/2161-0711.1000513
33. Rajoo, Y, Ambu, S, Lim, YA, Rajoo, K, Tey, SC, Lu, CW, et al. Neglected intestinal parasites, malnutrition and associated key factors: a population based cross-sectional study among indigenous communities in Sarawak. Malaysia PloS One. (2017) 12:e0170174. doi: 10.1371/journal.pone.0170174
34. Sagin, DD, Ismail, G, Mohamad, M, Pang, EK, and Sya, OT. Anemia in remote interior communities in Sarawak, Malaysia. Southeast Asian J Trop Med Public Health. (2002) 33:373–7.
35. Ismail, E, Amini, F, Razak, A, Alwi, Z, and Farhour, R. Peninsular Malaysia’s Negrito Orang Asli and its theory of African origin. Sains Malaysiana. (2013) 42:921–6.
36. McLean, E, Cogswell, M, Egli, I, Wojdyla, D, and De Benoist, B. Worldwide prevalence of anemia, WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. (2009) 12:444–54. doi: 10.1017/S1368980008002401
37. Grantham-McGregor, S, and Ani, C. A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr. (2001) 131:649S–68S. doi: 10.1093/jn/131.2.649S
38. Diez-Ewald, M, Torres-Guerra, E, Layrisse, M, Leets, I, Vizcaíno, G, and Arteaga-Vizcaíno, M. Prevalence of anemia, iron, folic acid and vitamin B12 deficiency in two Bari Indian communities from western Venezuela. Investigacion Clinica. (1997) 38:191–201.
39. Khor, GL, and Zalilah, MS. The ecology of health and nutrition of Orang Asli (Indigenous people) women and children in Peninsular Malaysia. Tribes Tribals. (2008) 2:66–77.
40. Nambiema, A, Robert, A, and Yaya, I. Prevalence and risk factors of anemia in children aged from 6 to 59 months in Togo: analysis from Togo demographic and health survey data, 2013-2014. BMC Public Health. (2019) 19:215. doi: 10.1186/s12889-019-6547-1
Keywords: anaemia, prevalence, severity, indigenous Orang Asli, Malaysia
Citation: Idris ZM, Wahid W, Seri Rakna MIM, Ghazali N, Hassan NW, Abdul Manap SNA, Mohamed AI, Chuangchaiya S and Mohd Kasri MR (2024) Prevalence and severity of anaemia among the Temiar sub-ethnic indigenous Orang Asli communities in Kelantan, Peninsular Malaysia. Front. Public Health. 12:1412496. doi: 10.3389/fpubh.2024.1412496
Edited by:
Pozi Milow, University of Malaya, MalaysiaReviewed by:
Sarah Abdul Razak, University of Malaya, MalaysiaRomano Ngui, University of Malaysia Sarawak, Malaysia
Copyright © 2024 Idris, Wahid, Seri Rakna, Ghazali, Hassan, Abdul Manap, Mohamed, Chuangchaiya and Mohd Kasri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zulkarnain Md Idris, enVsa2FybmFpbi5tZGlkcmlzQHVrbS5lZHUubXk=
 Zulkarnain Md Idris
Zulkarnain Md Idris Wathiqah Wahid
Wathiqah Wahid Mohd Ikhwan Mukmin Seri Rakna2
Mohd Ikhwan Mukmin Seri Rakna2