- 1School of Ethnology and Sociology, Yunnan University, Kunming, China
- 2School of Medicine, Yunnan University, Kunming, China
- 3Yunnan Provincial Center for Population and Health Publicity and Education, Kunming, China
- 4School of Vocational and Continuing Education, Yunnan University, Kunming, China
- 5CAS Key Laboratory of Mental Health, Institute of Psychology, Chinese Academy of Sciences, Beijing, China
- 6Department of Psychology, University of Chinese Academy of Sciences, Beijing, China
Background: The health literacy of ethnic groups in remote areas of China is far from satisfactory. However, the health literacy of ethnic groups in China remains unclear. This study aimed to explore the health literacy of the “advancing directly” ethnic group and its influencing factors.
Methods: A cross-sectional study was conducted using a staged sampling method among the Wa ethnic group, who have rapidly transitioned directly from the traditional lifestyle of slash-and-burn cultivation to modern societies. We used the Health Literacy Questionnaire (HLQ) to assess health literacy. We defined low health literacy as less than 60% of the total score and adequate health literacy as more than 80% of the total score.
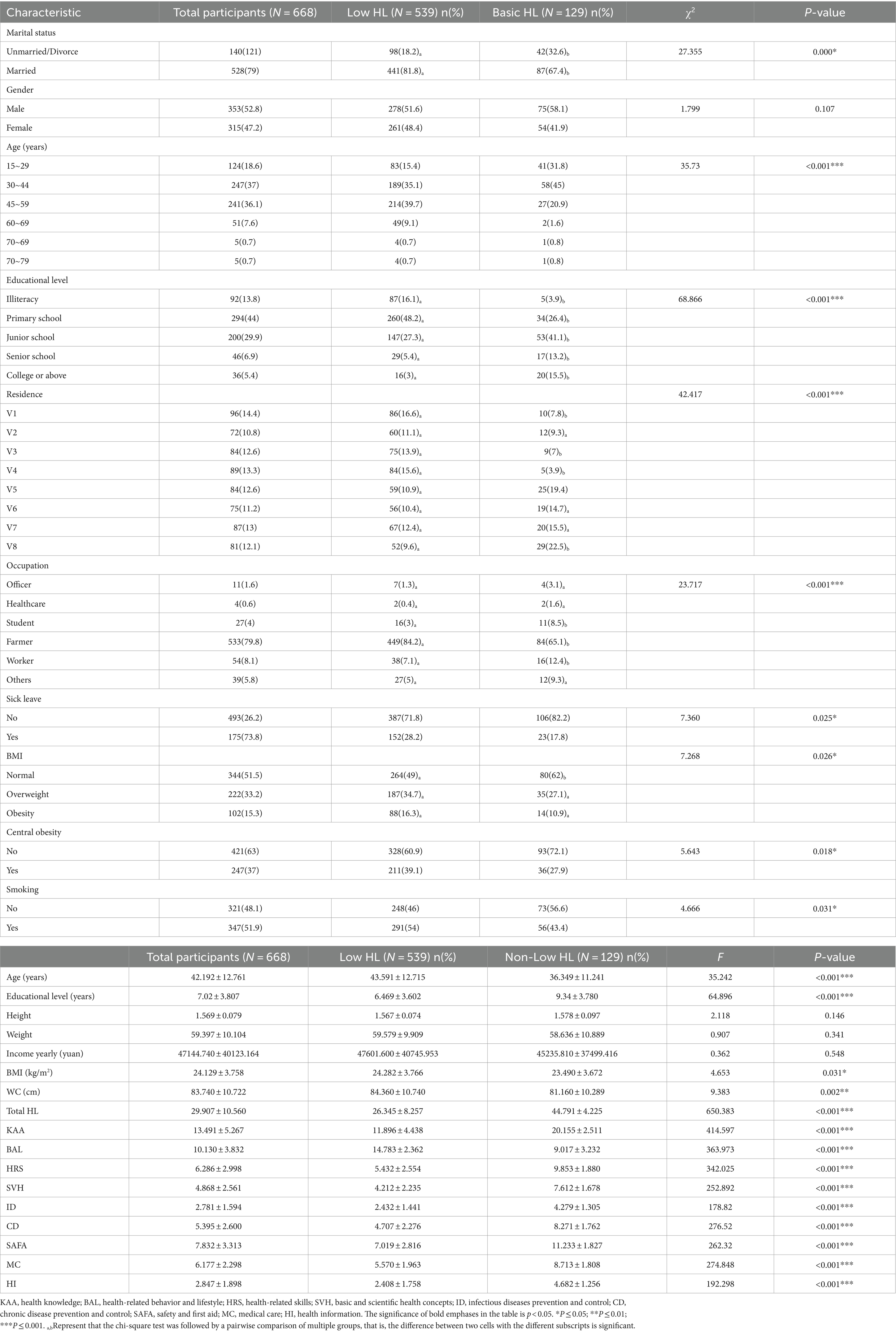
Results: A total of 668 individuals met the inclusion criteria and the mean age was 42.19 (SD 10.56) years. The mean HLQ total score was 29.9 (SD 10.56). The prevalence of adequate health literacy was 0.89%. There were significant differences between the low and the non-low health literacy groups in terms of gender, age, education, marital status, occupation, residing place, current smoking status, and waist circumference (all p < 0.05). Multiple linear regression analysis showed that women (t = 9·418, p < 0.001), older age (B = −0.0091, t = −2.644, p = 0.008), low educational level (B = 0.766, t = 6.018, p < 0.001), current smoking (B = −2.66, t = −3.038, p = 0.008), and residence far from township (B = −5.761, t = −4.1, p < 0.001) were associated with low HLQ total score.
Conclusion: Our findings suggest that the health literacy of the Wa ethnic group is far from favorable. It indicates the need for increased efforts in improving the health literacy of “advancing directly” ethnic groups.
1 Introduction
The World Health Organization (WHO) defines health literacy (HL) as personal knowledge and competence that enables individuals to acquire, understand, evaluate, and utilize information and services to promote their health and the health of those around them (1). There is increasing evidence that HL is a vital factor in health outcomes. Limited HL was related to increased hospitalization (2, 3), lower rates of medication adherence (2, 4), decreased acceptance of preventive interventions, increased health care costs (2, 5), poorer health status (6), and a higher rate of mortality among older adults (4). At the same time, lower HL can lead to communication barriers between healthcare providers and patients, impediments to citizens’ access to health information, and inefficient self-health management (6, 7). Moreover, HL followed a social gradient that reinforced existing inequalities, such as education and health resources, as well as economic development (8). HL is a better predictor of health status than age, education, income, occupation, and cultural context (8). Therefore, HL has been identified as a policy priority in the health strategy “Together for Health 2007–2013” in European Union (9), “Health 2023” in China (10), and the WHO 2030 Agenda for Sustainable Development (11).
In China, the Chinese Ministry of Health (MOH) issued the bulletin “Chinese Resident Health Literacy—Basic Knowledge and Skills (Trial)” in 2008 (12), the first government document to specify the HL of its citizens, and also developed a Health Literacy Questionnaire (HLQ) based on the HL evaluation indicators proposed by the WHO (12). Subsequently, starting in 2008, the standardized China Health Literacy Survey (CHLS) has been conducted every 2–3 years (13). The HL level of Chinese residents has steadily increased from 6.48% in 2008 to 25.4% in 2021, with 30.70% for urban residents and 22.02% for rural residents (14). However, these are huge urban–rural disparities and ethnic disparities in HL. Some studies from remote areas have reported that the HL level of rural residents was 7.94%—16.74 (15, 16). Adequate HL levels among ethnic groups range from 1.46 to 16.5% (17, 18). Moreover, reports on HL from ethnic groups in China remain inadequate (19).
Studies in Western countries have found growing evidence of lower levels of HL among ethnic groups (20, 21). Improving HL is beneficial for helping improve health inequalities among ethnic groups, and there are currently few studies in this area among Chinese ethnic groups (19), or in Western countries (20). In remote areas of China, the HL of ethnic groups is severely lacking (19). Nine of China’s 55 ethnic groups are known as “directly advancing” ethnic groups, such as the Wa, Dulong, Lisu, Jipo, and so on. Until 1960s, these ethnic groups maintained their traditional slash-and-burn farming lifestyles and only utilized their native language daily. They lived in family units, with social structures based on the family system, and their traditional lifestyle for centuries was relatively closed off. The Chinese government has been assisting in transforming their underdeveloped economic situation, particularly since 1994, through the implementation of poverty alleviation projects aimed at helping impoverished ethnic groups break the cycle of poverty (22), and these areas have seen tremendous improvements in the economy, education, and health. However, there is no HL data on “directly advancing” ethnic groups. To help fill the evidence gap, we surveyed the Wa ethnic group, one of the “directly advancing” ethnic groups in the southwest of China. The purpose of this study aimed to (1) estimate the HL level among the Wa ethnic group, and (2) assess risk factors for HL among the Wa ethnic group.
2 Materials and methods
2.1 Research design
This survey was conducted in Canyuan County, Yunnan Province, from December 2022 to February 2023. Canyuan County, the largest Wa ethnic group settlement in China, is situated on the border with Myanmar. The Wa ethnic group had preserved a slash-and-burn farming traditional lifestyle, heavily relying on family-based manual farming until 1960s.
2.2 Sample and setting
This was a cross-sectional study using a multi-stage cluster sampling method adopted in selecting the respondents. According to the principles of CHLS (13), the sample of the county was usually selected from six to eight administrative villages, and then two natural villages were selected from each administrative village. In this study, there were four stages for collecting the sampling. First, we randomly selected eight administrative villages from the 90 villages in Canyuan County. Second, two natural villages were selected from each administrative village, for a total of 16 natural villages. Third, using the systematic sampling method, 25 to 50 households randomly each natural village according to the size of the village. Finally, according to the KISH table (Kish Grid sampling), one household member was selected from each household. The sample size of respondents was calculated by the following formula (23). N = Z2P(1−P)/E2. Z is the significance level value (α = 0.05); P is the percentage of basic HL; E represents the maximum permissible error. The sample rate for monitoring the HL level of ethnic group residents in Yunnan province in 2019 was 12.21% (17); on this basis, a 95% confidence limit was set, with a relative error rate of no more than 20%, and E = 2%. Similarly, the minimum sample size was calculated as 525 using this formula. Meanwhile, the sample size was estimated as 577 based on a rejection rate of no more than 10%. In addition, the ideal sample size for a preliminary survey should be 5–10 times larger than the sample size in the questionnaire (24). The questionnaire consisted of 50 items; therefore, the sample size was consistent with the ideal sample size.
The inclusion criteria for this study were: (1) aged between 15 and 69; (2) local Wa ethnic residents; (3) lived in Canyuan County in the past 12 months. Exclusion criteria were: (1) providing unreliable results (n = 7); (2) unfinished interviews or difficulty in interviewing (n = 10); and (3) refusal to participate in this study (n = 3). The final sample consisted of 668 participants, including 353 males and 315 females. The questionnaire’s validity rate was 95%. Face-to-face interviews were conducted by trained interviewers because most respondents had low levels of education or were illiterate.
2.3 Ethical considerations
The study was approved by the Review Board (IRB) of the Institute of Psychology, Chinese Academy of Sciences (No. H18031), and was performed in accordance with the Declaration of Helsinki. Written informed consent was obtained prior to data collection.
2.4 Data collection and measurement
Demographic and socioeconomic variables were collected for all participants, including age, gender, marital status, ethnicity, education level, annual income, occupation, chronic disease, body mass index (BMI), and waist circumference (WC; in centimeters). The study used the WHO classification of general obesity and central obesity. General obesity is determined by BMI (kg/m2). WHO classifies BMI as: underweight = BMI < 18.5 kg/m2; normal = BMI 18.5–24.99 kg/m2; overweight = BMI 25–26.99 kg/m2; and obese = BMI 27 kg/m2 (25). In the Chinese classification, BMI is classified as underweight (BMI < 18), normal (18 ≤ BMI < 24), overweight (24 ≤ BMI < 28), or obese (BMI ≥ 28) (26). Central obesity was assessed by measuring waist circumference (WC). WC was measured at mid-breath at the level of the umbilicus with the participant in an upright position. In the WHO classification, the cut-off for central obesity is a WC of 88 cm (27). In this study, the threshold for central obesity was 90 cm WC for men and 85 cm WC for women (26).
Osborne et al. developed the Health Literacy Questionnaire (HLQ) (28), which has been translated into multiple languages for use with participants from non-English-speaking countries (29). In this study, data were obtained through face-to-face interviews, and a Chinese version of the HLQ (2022 edition) was developed by the MOH (12). It contains two parts. The first part includes mainly personal information on demographic characteristics and socioeconomic status. The second part includes 50 questions divided into 9 domains (3 aspects and 6 dimensions). The 3 aspects are health knowledge (KAA, 22 questions), health-related behaviors and lifestyles (BAL, 16 questions), and health-related skills (HRS, 12 questions). The 6 dimensions include basic and scientific health concepts (SVH, 8 questions), prevention and control of infectious diseases (ID, 6 questions), prevention and control of chronic disease (CD, 9 questions), safety and first aid (SAFA, 10 questions), medical care (MC, 11 questions), and health information (HI, 6 questions). The HL total score was calculated based on the sum of all 3 aspects or 6 dimensions. The HL total score ranged from 0 to 66. The full scores for KAA, BAL, and HRS were 28, 22, and 16, respectively, while the full scores for the 6 dimensions of SVH, ID, CD, SAFA, MC, and HI were 11, 7, 12, 14, 14, and 8, respectively. The classification was based on the 2022 Chinese criteria, a total score greater than or equal to 80% of the full score (total score ≥ 53) represents adequate HL. The cut-off points were 22, 18, and 13 for KAA, BAL, and HRS, respectively, and 9, 6,10, 11, 11, and 6 for the six dimensions of SVH, ID, CD, SAFA, MC, and HI, respectively (12). A score below 60% of the total score (score < 40) is represented as low of HL (30). Therefore, in our study, we defined the cut-off points for adequate health literacy (HL) and low HL as being equal to or greater than 53 and less than 40, respectively.
2.5 Statistical analysis
First, participants were divided into two categories: (1) low HL (a total score < 40) and (2) basic HL (a total score ≥ 40). Second, categorical and continuous variables are expressed as numbers (percentages) and mean ± SD, respectively, testing normally distributed (Kolmogorov–Smirnov one-sample test, all p’s > 0.05). Second, we used chi-square tests for categorical variables to compare the differences between the low of HL and basic HL groups and ANOVA for continuous variables. Also, the LSD test was used to compare the differences between the means of multiple groups. Third, multiple linear regression was used to predict the factors influencing HL. The total score of the HLQ scale was used as the dependent variable, and demographic and socioeconomic variables were used as the independent variables. We used SPSS version 26.0 for all statistical analyses. All p-values were 2-tailed, with a significance level ≤ 0.05. Bonferroni corrections were used to adjust for multiple comparisons. Coefficient values, 95% confidence intervals, odds ratios, and were used to quantify the strength of correlation.
3 Results
3.1 Participants’ demographic characteristics
Of the 668 participants, 353 (52.8%) were male, and the mean age (SD) was 42.2 (12.7) years, with an age range of 15–77 years old. 657(98.4%) were the Wa, 92 (13.8%) were illiterate, and 294(44%) had an elementary school education level. The mean annual income was 47144.74 ± 40123.164 Chinese Yuan. The mean BMI was 24.13 ± 3.76 kg/m2, ranging from 15.90 to 39.96 kg/m2, of which 222 (33.2%) were overweight (BMI ≥ 24 kg/m2) and 102 (15.3%) were obese (BMI ≥ 28 kg/m2). The mean WC was 83.74 ± 10.72 cm, ranging from 52 to 114 cm, of which 247 (37%) were centrally obese.
3.2 Prevalence of adequate HL and low HL in participants
The mean score of HL was 29.19 ± 10.56, ranging from 2 to 60. According to the cutoff point of a HL total score ≥ 53 for adequate HL, 6 (0.89%) had adequate HL. In the three aspects of the HL scale, 45 (6.73%), 14 (2.1%), and 9 (1.34%) had adequate knowledge of KAA, BAL, and HRS, respectively. In the six dimensions of the HL scale, MC24 (3.59%), ID33(4.94%), CD36(5.39%), HI 44(6.59%), SVH 60(8.98%), and SAFA140(20.96%), and achieved adequate levels in MC, ID, CD, HI, SVH, and SAFA, respectively. Based on a total HL score < 40 as the cutoff point for low HL, 538 (80.68%) had low knowledge of HL. The participants were then divided into low HL and basci HL.
3.3 Comparison of the characteristics of participants between low HL and basic HL groups
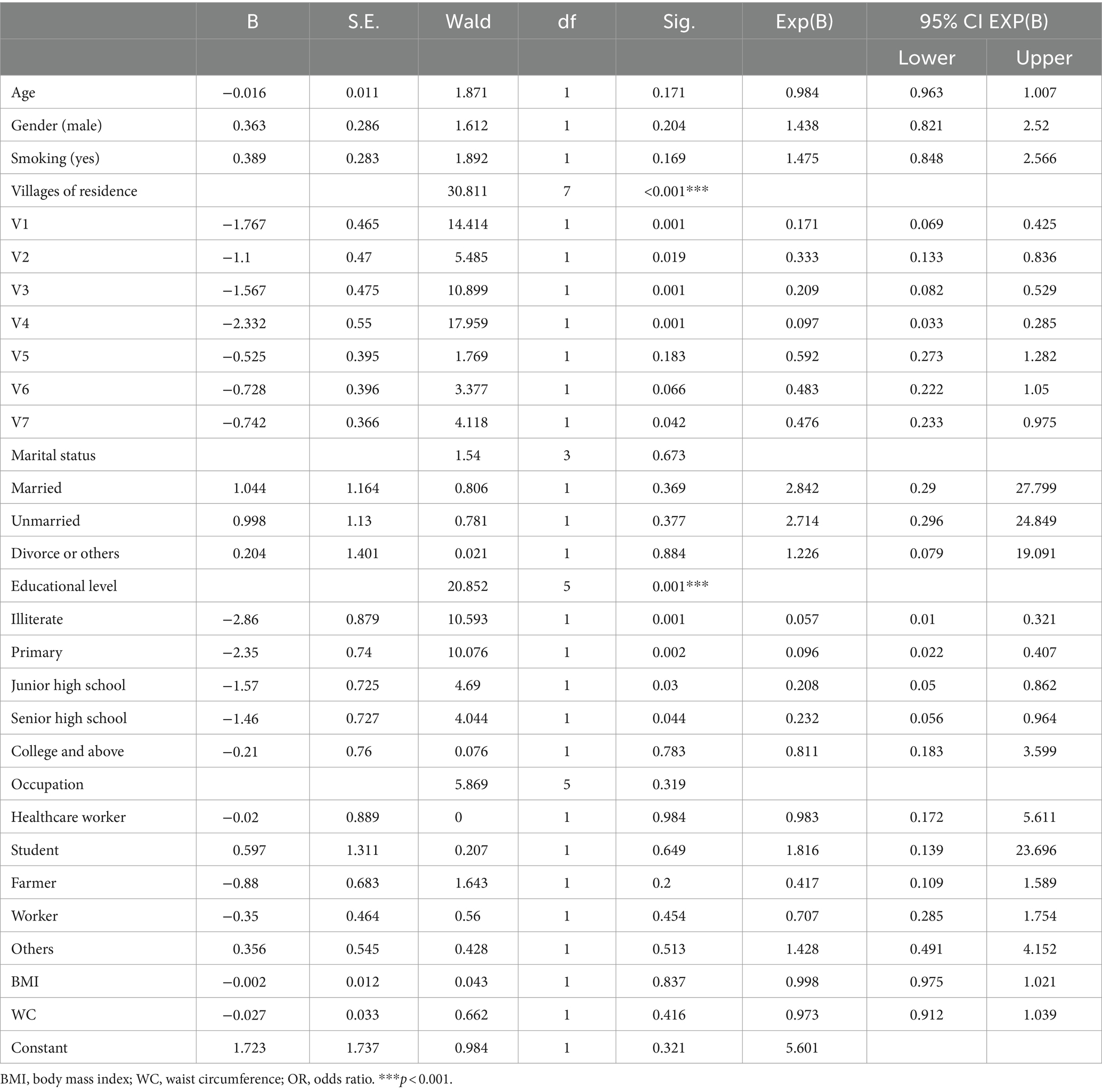
As shown in Table 1, we observed that participants in the low health literacy (HL) group (n = 538), who had a total score < 40, were older and had higher body mass index (BMI) and waist circumference (WC) compared to the basic HL group (n = 129), who had a score ≥ 40. After Bonferroni correction (p < 0.05/16 = 0.003), age and WC remained significant (all p’s < 0.01). Also, there were significant differences between the two groups in the following variables: married status, sick leave, current smoking, normal weight, central obesity, education level, occupation, and residence. Meantime, pair comparisons were made for variables larger than three categories, including education levels, occupation, and residence. After Bonferroni correction (p < 0.05/9 = 0.006), education level, occupation, residence, and marital status remained significant (all p’s < 0.01). There were no significant differences between the groups in terms of gender, height, weight, and annual income (all p > 0.05). Further binary logistic regression showed that risk factors for low HL included education level (Wald = 20.852, p = 0.001), and residence (Wald = 30.811, p < 0.001) (see Table 2).
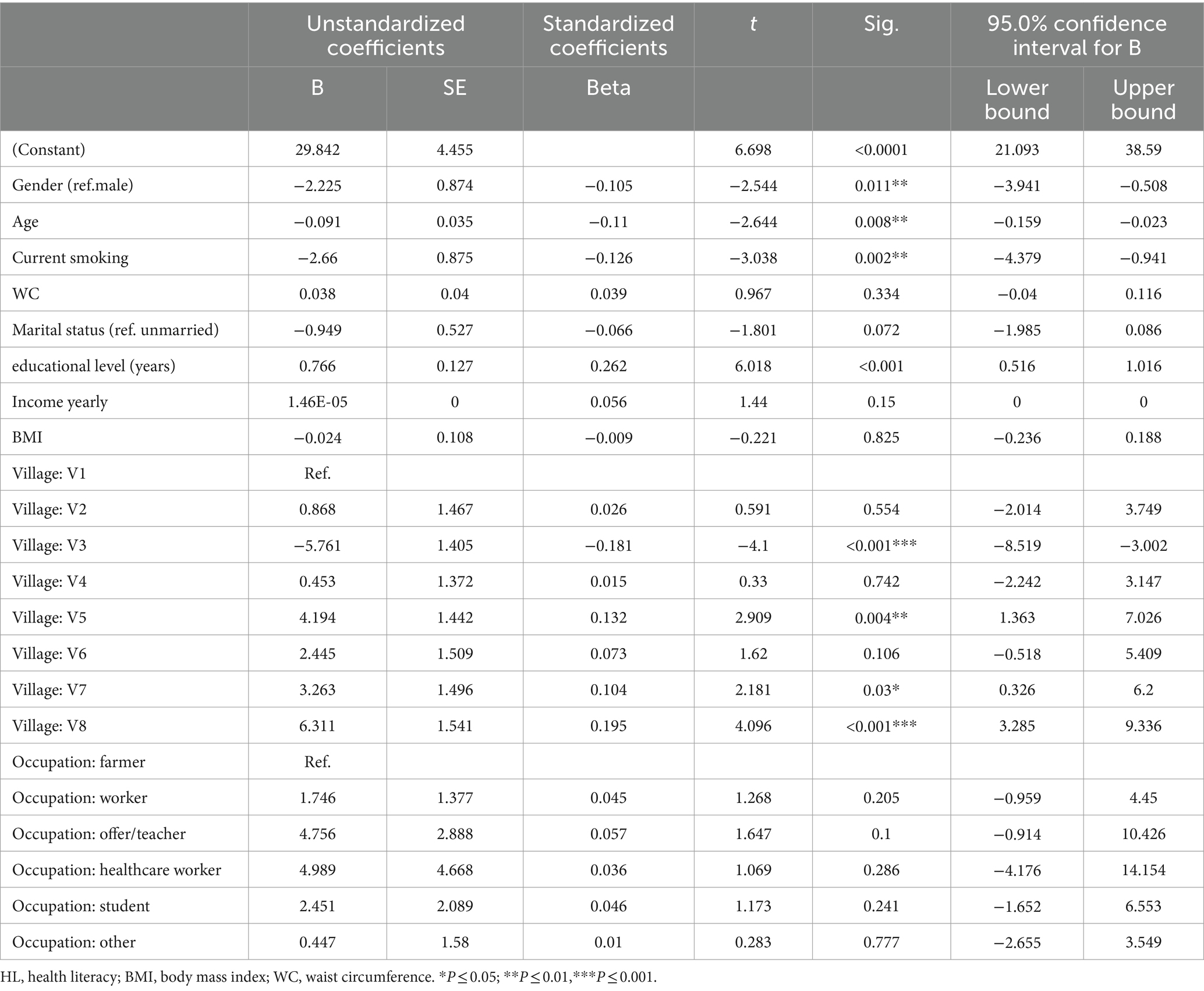
3.4 Relationship between HL and demographic characteristics
Table 3 summarizes the multiple linear regression models of HL predictors (F = 13.206, p < 0.0001, R2 = 0.290, adjusted R2 = 0.268). The model showed that HL significantly decreased with females (β = −2.225, t = −2.544, p = 0.0011), older age (β = −0.091, t = −2.644, p = 0.0008), current smoking (β = −2.66, t = −3.038 p = 0.019), and residence far from the local government office (β = −5.761, t = −4.1, p < 0.0001) and, however, HL significantly increased with residence closing to the local government office (β = 6.311, t = −4.096, p < 0.0001) and educational level (years) (β = 0.766, t = 0.262, p < 0.0001). However, no statistically significant differences were found in marital status, income yearly, BMI, WC, income yearly and occupation.
3.5 Comparison of HL among participants in different villages
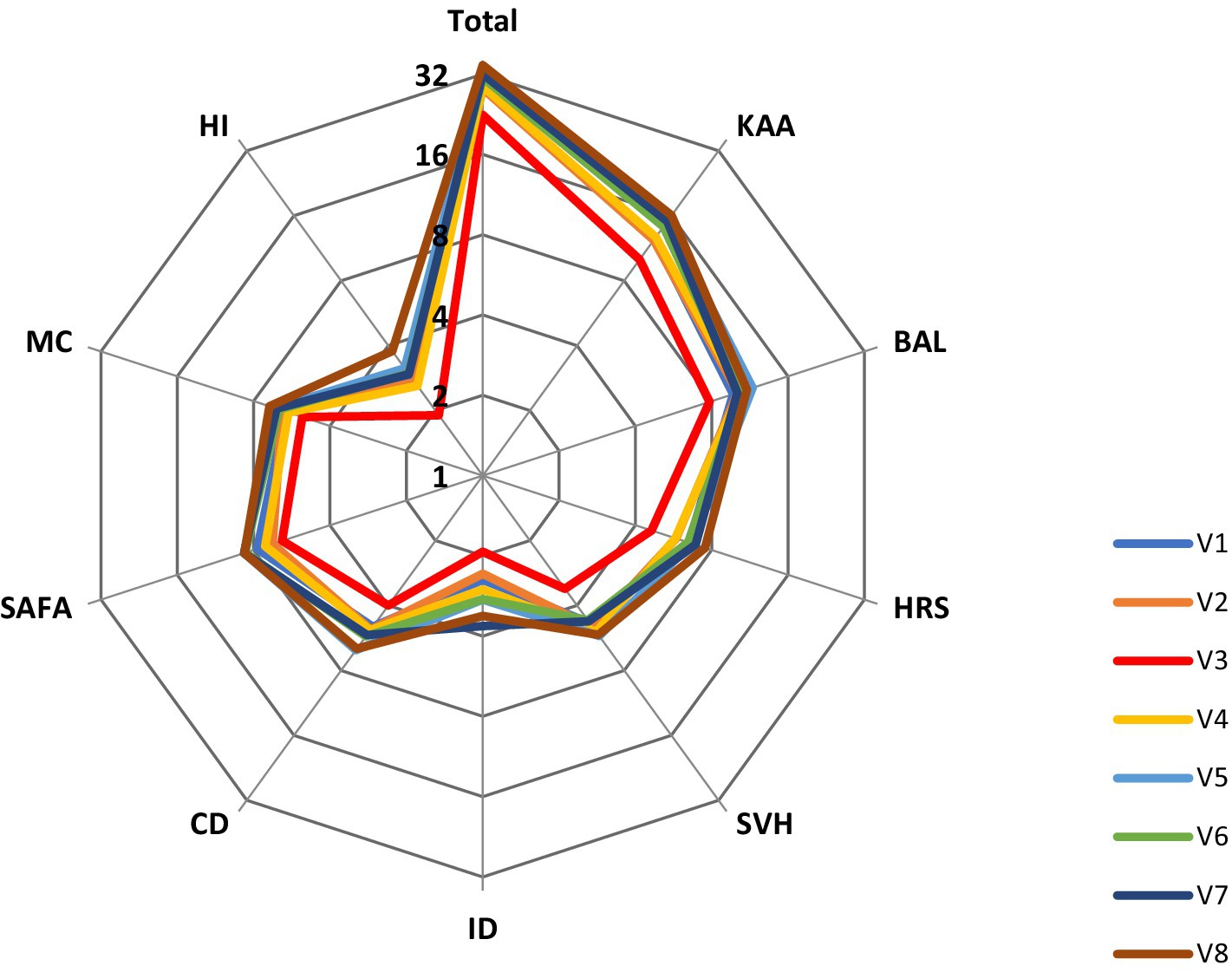
We used ANOVA to analyze the differences in the HL total and all subscale scores between villages. From V1 to V8, there were significant differences in the total score of HL between eight villages (F = 11.578, p < 0.001). Further, using the LSD-test, we found that the HL in village V3 was significantly lower than the other seven villages (mean difference = −5.778–12.080, p < 0.001) and the HL in village V8 was significantly higher than in the other V1–V4 villages (mean difference = 5.749–12.080, p < 0.001). In addition, the distance from the village to the government office (from V1 to V8) were 2.7, 6.5, 15.2, 13, 7.5, 10, 13, and 0.2 km, respectively. There was a significant negative correlation between village HL scores and the distance between villages and government offices (r = −0.541, p < 0.001). Figure 1 shows the HL total score and nine domain scores for different villages (V1–V8).
4 Discussion
To our knowledge, this is the first study to investigate the prevalence of HL and associated factors in the Wa ethnic group. Our findings are as follows: (1) the prevalence of low HL among the Wa ethnic group was by far the highest among Chinese ethnic groups; and (2) demographic variables, including gender, age, education level, current smoking, and residence were associated with the low HL.
Up to date, there has been only one survey of HL among the Dulong, a “directly advancing” ethnic group in China, with a rate 1.46% adequate HL (18). Compared to this previous report, our result showed that the Wa group had the lowest rate of adequate HL (0.89%). Pu et al. reported that the adequate level of health knowledge, health-related behaviors and lifestyles, and health-related skills among the Dolong were 2.11, 3.14, and 0.16%, respectively, while the Wa ethnic group had adequate HL rates of 6.73%, 2.1 and 1.34%, respectively (18). These results suggest that there was a significant lack of health-related skills among these two “directly advancing” ethnic groups, which may be a key point for health promotion interventions.
Two main reasons may contribute to the low level of HL among the “directly advancing” ethnic groups. First, the Wa ethnic group and Dulong lived in mountainous areas until 1960 and maintained a slash-and-burn farming lifestyle. Due to natural, environmental, social, and historical issue (31, 32), ethnic groups tend to have low levels of HL and health status. Numerous studies have shown that high socioeconomic status (32), good education, and good living and working environments (33) weaken their exposure to risk factors affecting health and increase the likelihood of acquiring HL (34). Second, low HL is associated with limited knowledge of screening, lack of desire to screen, and language skills (35, 36). In this study, most villagers, especially the older adult, had low Chinese language proficiency, and their responses to the questionnaire required translation. However, there were no words or phrases in the Wa ethnic group language to name disease terms such as cancer, hypertension, hepatitis B, and tuberculosis. Some information was more likely to be lost in translation during the survey. Specifically, of the eight villages, Nanlang village was the most backward, being far from the government office and health center, with no road access to the village until 2016. Villagers using bilingual or the Wa ethnic group language at home with limited Chinese proficiency. Respondents in Nanlang village had significantly lower HL than those in other villages.
Our results are consistent with existing studies on ethnic groups. For example, in the United States, 44.9% of low language proficient ethnic groups reported limited English proficiency, while only 13.8% of fluent English speakers had low HL (37). More than half of Chinese Americans with limited English proficiency had low HL and cancer screening rates due to health communication barriers (37). These findings suggest that the inclusion of language proficiency in multivariate study factors associated with HL is critical to understanding all screening factors for low HL across ethnic groups, as limited language proficiency may compound vulnerabilities such as educational attainment, underutilization or misuse of health care resources, and decreased HL (38). Therefore, language proficiency associated with HL should be quantified to better understand the predictors of low HL, to inform future interventions, and to remove appropriate barriers to HL (39). There is growing evidence that multifaceted, culturally and linguistically appropriate interventions enable respondents with lower levels of health literacy to be more responsive (40, 41) such as the use of colloquial language in screenings and interviews.
To further explore the risk factors for low HL in the Wa ethnic group, our results showed that demographic information, including age, gender, education level, and village location was significantly associated with low HL through linear regression models. Previous studies have shown that the most common demographic characteristics related to HL were education, age (31), gender (42), ethnicity (43), residence (44, 45), and income (45, 46). The meta-analysis study reported that of these variables, age, education, and race were the most consistently included in the regression equation (47). Nearly all of our respondents had a low level of education, with 87.7% having an elementary or middle school level. Illiteracy accounted for 13.8% of the population, and the mean age of illiterates was 52 ± 10.44 years, of which 62% were female. This is due to limited educational opportunities for Chinese seniors at a young age, resulting in low education levels and even illiteracy (48). Women typically have less access to higher education than men (49). An individual’s low educational background often leads to negative attitudes toward health management (50–53), affecting HL and impacting access to health care services.
Besides, several barriers, such as geography, distance (52), bad weather (29), and rural or urban (15), contribute to low levels of HL. Rural–urban differences in health information sources may be due to structural barriers, such as a shortage of rural specialists, inadequate online resources (51), and greater distance from the nearest health facility (53). Patients in rural areas are two to three times further away from medical appointments than those in urban areas, resulting in residents potentially having fewer opportunities to ask for or receive health information from specialists (54). Similarly, among our participants, those who were farther away from the township office (mean distance of 32 m) had lower HL than those closer to the township office (mean distance of 18 m). In each village studied, the township government office, health center, and other facilities are all centralized in the same or adjacent buildings. The township government office serves as a political, cultural, and informational center, providing many conveniences for villagers and offering health or political information resources. These results also illustrated that improving access to health information or other resources within the community is key to improving HL.
Few studies highlighted the relationship between BMI or WC and HL. Some studies have found a strong correlation between low HL and obesity (55), whereas others have shown that HL did not predict BMI (56). Similarly, our study showed that the association between BMI or WC and HL was statistically significant but not a risk predictor. 37 and 48.1% of our respondents who were centrally obese and smokers, respectively, had significantly lower HL than nonsmokers and nonobese individuals. Higher HL levels were associated with higher access to health information and lower risky habits, such as physical inactivity, smoking, and alcohol consumption (57, 58). These results may be explained by the strong relationship between a person’s BMI or WC and lifestyle, as those with low HL are more likely to have unhealthy diets and behaviors (59). Evidence suggests that effective interventions to improve HL in community settings may be to change unhealthy lifestyles (e.g., smoking, diet, and physical activity) (60). Therefore, we recommend that rural health professionals be trained to properly perform WC measurements and consider them an important and more accurate “vital sign” in screening goals to improve HL (61).
4.1 Strengths and limitations
This is the first study to examine the HL among the Wa ethnic group and its influencing factors. However, there are also several limitations. First, our study data came from the Wa ethnic group along the China-Burma border. Some compounding factors, such as economic, cultural, geographic environment, and health status conditions, were not taken into account; therefore, our results should be examined and carefully generalized to other studies from different cultural backgrounds. Second, the limited Chinese language proficiency of our participants may have influenced their responses to the HL questionnaire. Therefore, further research on HL among ethnic groups should consider using different data collection methods than survey studies. Finally, the data were measured by using a screening scale from a survey and thus it is difficult to avoid recall bias.
5 Conclusion and relevance for practice
In summary, this study is the first to examine HL among the Wa, a “directly advancing” ethnic group in China. Significant associations exist between low HL and age, gender, education level, place of residence, and current smoking. In particular, lower education level and residence far from the township were risk factors for low HL. These factors, including senior, female, smoking, low education, and living far from the township, have been identified as risk factors for HL. This finding helps to clarify the goals for improving HL and to develop problem-oriented health education among the Wa population.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Review Board (IRB) of the Institute of Psychology, Chinese Academy of Sciences (Beijing, China). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
WY: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing. YL: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. GZ: Conceptualization, Investigation, Project administration, Resources, Writing – original draft. YY: Formal analysis, Investigation, Project administration, Writing – original draft. YW: Investigation, Project administration, Writing – original draft. DL: Investigation, Project administration, Software, Writing – original draft. CL: Data curation, Investigation, Software, Writing – review & editing. KL: Data curation, Investigation, Software, Writing – original draft. JL: Investigation, Software, Writing – review & editing. YP: Investigation, Writing – review & editing. ML: Investigation, Writing – review & editing. BY: Investigation, Writing – review & editing. SZ: Investigation, Writing – review & editing. DM: Investigation, Writing – review & editing. XZ: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by grants from the “China Rural Social Survey” of Yunnan University, the National Key R&D Program of China (2017YFE0103700).
Acknowledgments
We are grateful to all respondents and researchers who participated in our current study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. Health promotion glossary of terms 2021. (2021). Available at: https://who.int/publications/i/item/9789240038349
2. Berkman, ND, Sheridan, SL, Donahue, KE, Halpern, DJ, Viera, A, Crotty, K, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess. (2011) 199:1–941.
3. Baker, DWGJ, Gazmararian, JA, Williams, MV, Scott, T, Parker, RM, Green, D, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. (2002) 92:1278–83. doi: 10.2105/AJPH.92.8.1278
4. Al Sayah, F, Majumdar, SR, Williams, B, Robertson, S, and Johnson, JA. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. (2013) 28:444–52. doi: 10.1007/s11606-012-2241-z
5. Dewalt, DA, Berkman, ND, Sheridan, S, Lohr, KN, and Pignone, MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. (2004) 19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x
6. Davis, TC, and Wolf, MS. Health literacy: implications for family medicine. Fam Med. (2004) 36:595–8.
7. Sudore, RL, Landefeld, CS, Perez-Stable, EJ, Bibbins-Domingo, K, Williams, BA, and Schillinger, D. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. (2009) 75:398–402. doi: 10.1016/j.pec.2009.02.019
8. Gilson, L, Doherty, J, Lowenson, R, and Francis, V. Challenging inequity through health systems. Final report. Knowledge Network on Health Systems. Technical Report. WHO Commission on the Social Determinants of Health. (2007) Available at: https://researchonline.lshtm.ac.uk/id/eprint/713
9. European Commission E. Together for health: a strategic approach for the EU, 2008–2013. (2007). Available at: https://ec.europa.eu/commission/presscorner/detail/en/IP_07_1571
10. National Health and Health Commission of the People’s Republic of China. “Health China 2030” planning outline. (2016). Available at: https://www.gov.cn/zhengce/2016-10/25/content_5124174.htm?eqid=ac00b02f000027f90000000464586447
11. WHO. The mandate for health literacy. (2017). Available at: https://www.who.int/teams/health-promotion/enhanced-wellbeing/ninth-global-conference/health-literacy
12. Ping, W, Qunan, M, and Xuanmao, T. Survey on the status of health literacy of Chinese resident. Chinese J Health Educ. (2010) 4:243–246. (in Chinese).
13. Li, YH, and Nic, XQ. Contrast analysis of 2008 and 2012 Chinese health literacy survey scheme. Chin J Health Educ. (2014) 2:176–7. doi: 10.16168/j.cnki.issn.1002-9982.2014.02.020
14. NHCoC. National health literacy level rises to 25.4% by 2021. Available at: https://wwwgovcn/xinwen/2022–06/08/content_5694585htm (2021).
15. Wang, W, Zhang, Y, Lin, B, Mei, Y, Ping, Z, and Zhang, Z. The urban-rural disparity in the status and risk factors of health literacy: a cross-sectional survey in Central China. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17113848
16. Li, Z, Tian, Y, Gong, Z, and Qian, L. Health literacy and regional heterogeneities in China: a population-based study. Front Public Health. (2021) 9:603325. doi: 10.3389/fpubh.2021.603325
17. Jiarong, Y, Mei, L, Lingqing, L, Chuanshi, P, and Yong, D. Analysis on status of health literacy among minority residents in Yunnan Province, 2019. Health Educ Health Promot. (2020) 15:10–4.
18. Liu Mei, PS, Jiarong, Y, Hongling, M, and Lingqing, L. Analysis on current situation and improvement path of health literacy of Dulong nationality residents. Health Educ Health Promot. (2022) 15:446–50. (in Chinese).
19. Hu, H, Liu, J, Liang, Y, and Xu, Y. Health literacy of ethnic minority in remote China: precise intervention is needed. Lancet Reg Health West Pac. (2021) 17:100322. doi: 10.1016/j.lanwpc.2021.100322
20. Sepassi, A, Garcia, S, Tanjasiri, S, Lee, S, and Bounthavong, M. Predicted health literacy disparities between immigrant and US-born racial/ethnic minorities: a Nationwide study. J Gen Intern Med. (2023) 38:2364–73. doi: 10.1007/s11606-023-08082-x
21. Blom, IM, Cohen, ES, Eshuis, LV, Woudstra, AJ, Snijder, MB, Kunst, AE, et al. Ethnic differences in health literacy among young adults in Amsterdam. Health Lit Res Pract. (2018) 2:e192–204. doi: 10.3928/24748307-20180926-01
22. China TSCo. Phase of poverty alleviation (1994-2000). Available at: https://wwwgovcn/ztzl/fupin/content_396638htm (1994).
23. Yang Cao, JC, Cao, J, and Qian, J. Application of Kish grid sampling in world health survey (China survey). Fudan Univ J Med Sci. (2004) 31:307–10. (in Chinese).
25. Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
26. Zhou, BFCooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. (2002) 15:83–96.
27. Bull, FC, Maslin, TS, and Armstrong, T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. (2009) 6:790–804. doi: 10.1123/jpah.6.6.790
28. Osborne, RH, Batterham, RW, Elsworth, GR, Hawkins, M, and Buchbinder, R. The grounded psychometric development and initial validation of the health literacy questionnaire (HLQ). BMC Public Health. (2013) 13:658. doi: 10.1186/1471-2458-13-658
29. Beauchamp, A, Buchbinder, R, Dodson, S, Batterham, RW, Elsworth, GR, McPhee, C, et al. Distribution of health literacy strengths and weaknesses across socio-demographic groups: a cross-sectional survey using the health literacy questionnaire (HLQ). BMC Public Health. (2015) 15:678. doi: 10.1186/s12889-015-2056-z
30. Mei, X, Zhong, Q, Chen, G, Huang, Y, and Li, J. Exploring health literacy in Wuhan, China: a cross-sectional analysis. BMC Public Health. (2020) 20:1417. doi: 10.1186/s12889-020-09520-9
31. Protheroe, J, Whittle, R, Bartlam, B, Estacio, EV, Clark, L, and Kurth, J. Health literacy, associated lifestyle and demographic factors in adult population of an English city: a cross-sectional survey. Health Expect. (2017) 20:112–9. doi: 10.1111/hex.12440
32. Sorensen, K, Pelikan, JM, Rothlin, F, Ganahl, K, Slonska, Z, Doyle, G, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Pub Health. (2015) 25:1053–8. doi: 10.1093/eurpub/ckv043
33. Yin, P, Zhang, M, Li, Y, Jiang, Y, and Zhao, W. Prevalence of COPD and its association with socioeconomic status in China: findings from China chronic disease risk factor surveillance 2007. BMC Public Health. (2011) 11:586. doi: 10.1186/1471-2458-11-586
34. Marshall, IJ, Wang, Y, Crichton, S, McKevitt, C, Rudd, AG, and Wolfe, CD. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. (2015) 14:1206–18. doi: 10.1016/S1474-4422(15)00200-8
35. Scott, TL, Gazmararian, JA, Williams, MV, and Baker, DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. (2002) 40:395–404. doi: 10.1097/00005650-200205000-00005
36. Papadakos, JK, Hasan, SM, Barnsley, J, Berta, W, Fazelzad, R, Papadakos, CJ, et al. Health literacy and cancer self-management behaviors: a scoping review. Cancer. (2018) 124:4202–10. doi: 10.1002/cncr.31733
37. Sentell, TL, Tsoh, JY, Davis, T, Davis, J, and Braun, KL. Low health literacy and cancer screening among Chinese Americans in California: a cross-sectional analysis. BMJ Open. (2015) 5:e006104. doi: 10.1136/bmjopen-2014-006104
38. Taylor, VM, Jackson, JC, Tu, SP, Yasui, Y, Schwartz, SM, Kuniyuki, A, et al. Cervical cancer screening among Chinese Americans. Cancer Detect Prev. (2002) 26:139–45. doi: 10.1016/S0361-090X(02)00037-5
39. Anderson, LM, Scrimshaw, SC, Fullilove, MT, Fielding, JE, and Normand, J. Culturally competent healthcare systems. A systematic review. Am J Prev Med. (2003) 24:68–79. doi: 10.1016/S0749-3797(02)00657-8
40. Paasche-Orlow, MK, and Wolf, MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. (2007) 31:19–26. doi: 10.5993/AJHB.31.s1.4
41. Tu, SP, Taylor, V, Yasui, Y, Chun, A, Yip, MP, Acorda, E, et al. Promoting culturally appropriate colorectal cancer screening through a health educator: a randomized controlled trial. Cancer. (2006) 107:959–66. doi: 10.1002/cncr.22091
42. Kelly, PA, and Haidet, P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. (2007) 66:119–22. doi: 10.1016/j.pec.2006.10.007
43. Montalto, NJ, and Spiegler, GE. Functional health literacy in adults in a rural community health center. W V Med J. (2001) 97:111–4.
44. Al-Tayyib, AA, Rogers, SM, Gribble, JN, Villarroel, M, and Turner, CF. Effect of low medical literacy on health survey measurements. Am J Public Health. (2002) 92:1478–80. doi: 10.2105/AJPH.92.9.1478
45. Bush, RA, Boyle, FM, and Ostini, R. Risks associated with low functional health literacy in Australian population. Comment Aust Med J. (2010) 192:479. doi: 10.5694/j.1326-5377.2010.tb03597.x
46. Gazmararian, JA, Baker, DW, Williams, MV, Parker, RM, Scott, TL, Green, DC, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. (1999) 281:545–51. doi: 10.1001/jama.281.6.545
47. Paasche-Orlow, MK, Parker, RM, Gazmararian, JA, Nielsen-Bohlman, LT, and Rudd, RR. The prevalence of limited health literacy. J Gen Intern Med. (2005) 20:175–84. doi: 10.1111/j.1525-1497.2005.40245.x
48. Wu, Y, Wang, L, Cai, Z, Bao, L, Ai, P, and Ai, Z. Prevalence and risk factors of low health literacy: a community-based study in Shanghai, China. Int J Environ Res Public Health. (2017) 14:628. doi: 10.3390/ijerph14060628
49. Alberti, TL, and Morris, NJ. Health literacy in the urgent care setting: what factors impact consumer comprehension of health information? J Am Assoc Nurse Pract. (2017) 29:242–7. doi: 10.1002/2327-6924.12452
50. Graetz, V, Rechel, B, Groot, W, Norredam, M, and Pavlova, M. Utilization of health care services by migrants in Europe-a systematic literature review. Br Med Bull. (2017) 121:5–18. doi: 10.1093/bmb/ldw057
51. Chen, X, Orom, H, Hay, JL, Waters, EA, Schofield, E, Li, Y, et al. Differences in rural and urban health information access and use. J Rural Health. (2019) 35:405–17. doi: 10.1111/jrh.12335
52. McIlhenny, CV, Guzic, BL, Knee, DR, Wendekier, CM, Demuth, BR, and Roberts, JB. Using technology to deliver healthcare education to rural patients. Rural Remote Health. (2011) 11:1798. doi: 10.22605/RRH1798
53. Xie, Y, Ma, M, Zhang, Y, and Tan, X. Factors associated with health literacy in rural areas of Central China: structural equation model. BMC Health Serv Res. (2019) 19:300. doi: 10.1186/s12913-019-4094-1
54. Chan, L, Hart, LG, and Goodman, DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. (2006) 22:140–6. doi: 10.1111/j.1748-0361.2006.00022.x
55. Li, JJ, Appleton, SL, Wittert, GA, Vakulin, A, McEvoy, RD, Antic, NA, et al. The relationship between functional health literacy and obstructive sleep apnea and its related risk factors and comorbidities in a population cohort of men. Sleep. (2014) 37:571–8. doi: 10.5665/sleep.3500
56. Adeseun, GA, Bonney, CC, and Rosas, SE. Health literacy associated with blood pressure but not other cardiovascular disease risk factors among dialysis patients. Am J Hypertens. (2012) 25:348–53. doi: 10.1038/ajh.2011.252
57. Suka, M, Odajima, T, Okamoto, M, Sumitani, M, Igarashi, A, Ishikawa, H, et al. Relationship between health literacy, health information access, health behavior, and health status in Japanese people. Patient Educ Couns. (2015) 98:660–8. doi: 10.1016/j.pec.2015.02.013
58. von Wagner, C, Knight, K, Steptoe, A, and Wardle, J. Functional health literacy and health-promoting behaviour in a national sample of British adults. J Epidemiol Community Health. (2007) 61:1086–90. doi: 10.1136/jech.2006.053967
59. Yang, SC, Luo, YF, and Chiang, CH. The associations among individual factors, eHealth literacy, and health-promoting lifestyles among college students. J Med Internet Res. (2017) 19:e15. doi: 10.2196/jmir.5964
60. Taggart, J, Williams, A, Dennis, S, Newall, A, Shortus, T, Zwar, N, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam Pract. (2012) 13:49. doi: 10.1186/1471-2296-13-49
Keywords: health literacy, associated factors, “directly advancing” ethnic groups, rural community, the Wa ethnic group
Citation: Yang W, Liu Y, Zhang G, Yao Y, Wang Y, Leng D, Li C, Liu K, Liu J, Pu Y, Li M, Yang B, Zhang S, Mu D and Zhang X (2024) Health literacy and associated factors in China: findings from the Wa ethnic group. Front. Public Health. 12:1407593. doi: 10.3389/fpubh.2024.1407593
Edited by:
Tianfeng He, Ningbo Municipal Center for Disease Control and Prevention, ChinaCopyright © 2024 Yang, Liu, Zhang, Yao, Wang, Leng, Li, Liu, Liu, Pu, Li, Yang, Zhang, Mu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wanqiu Yang, eWFuZ3dhbnFpdUB5bnUuZWR1LmNu; Xiangyang Zhang, emhhbmd4eUBwc3ljaC5hYy5jbg==
 Wanqiu Yang
Wanqiu Yang Yi Liu3
Yi Liu3 Xiangyang Zhang
Xiangyang Zhang