- 1Department of Community and Behavioral Health, East Tennessee State University, Johnson City, TN, United States
- 2Department of Epidemiology and Biostatistics, East Tennessee State University, Johnson City, TN, United States
- 3School of Nursing, Thompson Rivers University, Kamloops, BC, Canada
- 4Department of Epidemiology and Biostatistics, Arnold School of Public Health, University of South Carolina, Columbia, SC, United States
- 5Department of Geriatrics, University of North Dakota School of Medicine and Health Sciences, Grand Forks, ND, United States
- 6Department of Psychology, University of Alaska, Anchorage, AK, United States
- 7College of Nursing, University of Central Florida, Orlanda, FL, United States
- 8Department of Health Behavior, Center for Community Health and Aging, Texas A&M University, College Station, TX, United States
Introduction: The adverse effects of social isolation and loneliness (SI/L) have been documented among older adults in rural communities and contribute to poor health outcomes, premature disability and mortality, and increased burden on the healthcare system. The identification of factors contributing to SI/L among older adults can build the foundation for rural policymakers and leaders to allocate resources and develop tailored strategies more efficiently. The purpose of this article is to describe findings from a needs assessment designed to understand local factors that contribute to SI/L among rural older adults in a county in Northeast Tennessee. Findings from the needs assessment will be used by local stakeholders to develop strategies to promote age-friendly initiatives.
Methods: Eighty-two older adults [ages 62 to 74 years (59%); non-Hispanic white (95%); female (71%)] from three senior apartment complexes in a Northeast Tennessee county completed an 87-item needs assessment survey. The evaluation of social isolation utilized Lubben’s 6-item Social Network Scale, while loneliness was assessed using the 3-item UCLA Loneliness Scale. Logistic regression analysis was used to identify predictors of SI/L. Given the limited sample size, statistical significance was considered at p < 0.10.
Results: The prevalence of social isolation and loneliness was 42% and 37%, respectively. Residing in the county <5 years [Adjusted OR (AOR): 3.35; 95% CI: 1.04–10.81; p = 0.04] and reporting resource-related barriers to aging-in-place (AOR: 6.56; 95% CI: 2.00–21.57; p = 0.004) were associated with increases in the odds of social isolation; whereas interest in intergenerational activities decreased the odds of social isolation (AOR: 0.19; 95% CI: 0.05–0.69; p = 0.01). Boredom (AOR: 4.06; 95% CI: 1.63–12.11; p = 0.01) and limited knowledge about community services (AOR: 4.61; 95% CI: 1.42–15.02; p = 0.01) quadrupled the odds of loneliness. Similarly, older adults who were frail (AOR: 2.69; 95% CI: 0.88–8.17; p = 0.08) and who rated their community livability as low (AOR: 3.35; 95% CI: 0.81–13.87; p = 0.09) were more likely to experience loneliness.
Discussion: This needs assessment provided important information about the individual and social drivers of SI/L among rural older adults in the community. Findings support the generation of localized data to support muti-partner efforts to design sustainable programs to address SI/L.
1 Introduction
The adverse effects of social isolation and loneliness (SI/L) have been documented among rural older adults and contribute to poor health outcomes, premature disability and mortality, and increased burden on the healthcare system (1–3). Older adults generally, and those in rural Appalachia specifically, rely on informal networks of family and friends to provide social support (4). However, many of these individuals experience structural barriers (e.g., geographic isolation, inadequate transportation services, sparse populations, and limited internet access) to connecting with family, friends, and neighbors (4–6). In addition, the Appalachian region is characterized as having multiple layers of vulnerability, such as a high proportion of older adults, limited availability of health and social services, and distinct cultural values that may inhibit health-seeking behaviors, a context referred to as “triple jeopardy” (4). Thus, older adults who tend to have more health problems and live in these rural areas face more challenges in accessing health and social services than their urban counterparts (7–9). These socio-structural barriers can reinforce existing health inequities, resulting in heightened vulnerability to SI/L.
Identifying factors that contribute to older adults’ SI/L can help rural policymakers and organizations target their resources and programming more effectively. However, the lack of local data is an ongoing challenge in these rural Appalachian communities (10, 11). Grassroots efforts may hold promise to address rural data gaps by generating local data, which can deepen stakeholders’ insights and strengthen efforts to implement specific, action-oriented solutions. This needs assessment reports on a local initiative to identify factors associated with SI/L among rural older adults aging-in-place in a Central Appalachian county within Northeast Tennessee.
2 Background and rationale
2.1 Social isolation and loneliness
SI/L have reached epidemic proportions in the U.S. (12). Although SI/L represent distinct concepts, they are often used interchangeably in the literature (1). While social isolation refers to an objective state of having few social relationships or infrequent social contact with others, loneliness reflects the individual’s subjective dissatisfaction with the frequency and closeness of relationships despite the actual interactions with others (3).
SI/L are associated with some similar and distinct negative health outcomes. These include heart disease, depression, anxiety, suicidality, dementia, frailty, nursing home admission, and premature disability and death (3, 13, 14). Studies estimate that SI/L are associated with a 26–29% increased risk of all-cause mortality (1). Recent research indicates that social isolation is a stronger predictor of all-cause mortality, while loneliness is more strongly associated with poor psychological well-being (2). Annually, social isolation results in $6.7 billion in additional Medicare spending (15).
Roughly 25% of older adults (ages 65 years and older) in the United States are socially isolated and 43% of adults ages 60 years and older feel lonely (3). Older adults are at increased risk of SI/L due to predisposing factors such as advanced age, lower educational attainment, living alone, chronic conditions, functional and cognitive impairment, smaller social networks, loss of family or friends, and retirement, among others (3). Some rural older adults have an even higher risk because they are more likely to live alone than their urban counterparts (16) and may not see or even communicate with another person for days at a time. Older adults in rural Appalachia may have greater susceptibility to the adverse health and psychological outcomes associated with SI/L due to underlying poor health status (7, 17) and limited access to behavioral and mental health services (4). Thus, it is important to take these factors into consideration when addressing SI/L in rural Appalachia (18).
2.2 Aging-in-place in Appalachia
Tennessee is home to more than 1.6 million residents over age 60 (19). Based on reports from America’s Health Rankings, Tennessee consistently falls in the bottom quartile of states for health outcomes among older adults over age 65 (20). Notable challenges include disease burden, limited access to clinical care and supportive social services, and risk of social isolation (20). In Tennessee, 52 out of 95 counties are in Central Appalachia. This region of Appalachia is predominately non-Hispanic White (21) and has experienced the largest growth in the older adult population in the region (22).
The Appalachian region is disproportionately burdened with poor social, economic, and health-related outcomes (22). Among 41 health indicators, the Appalachian region lags behind the U.S. on 33 of them, including seven of the 10 leading causes of death (7). Rural parts of the region have even greater risk for premature disability and mortality than urban areas (7). In this article, “rural” is defined as sparsely populated areas lying outside of urban centers (23) as defined by the United States Department of Agriculture Rural–Urban Commuting Area Codes (24). Many of the rural communities lack the infrastructure and resources to support healthy longevity (5, 7, 22). Consequently, rural older adults living in Appalachia often experience unique challenges to aging-in-place, which refers to having the ability to live safely and independently in one’s own home and community for as long as one chooses to do so (25). Rural older adults in these communities face a number of obstacles to social interactions, such as geographic isolation, environments that are not always walkable or socially conducive, a lack of economic resources, and restricted access to cellular and broadband Internet. Rural older adults are also more vulnerable to health problems because they are typically less mobile than their younger counterparts and more dependent on resources specific to their local community, creating difficulty in accessing mental health services among other medical services (26–28).
3 Context and essential elements of the needs assessment
Older adults are the fastest-growing age group in Tennessee. According to the Boyd Center for Business and Economic Research at the University of Tennessee, the proportion of individuals 65 and older will increase by almost 40% between 2020 and 2040 (29). Northeast Tennessee is aging even more rapidly than the rest of the state. Older adults in Northeast Tennessee have a higher burden of disease and disability compared to statewide averages. This is alarming because the patient-to-provider ratio in the eastern part of the state is 2.75 times higher than that in other parts of Tennessee. Older residents in Northeast Tennessee are also more likely to experience financial vulnerability, due in part to low educational attainment and a high number of grandparents raising grandchildren (19, 30). These cumulative disadvantages contribute to widening health inequities, particularly in persistently poor counties.
Given the significant risk for poor health outcomes among older Tennesseans, multi-partner efforts are needed to engage the local community in addressing key issues that impact this demographic (31). Multi-partner, grassroots initiatives are important in rural communities because they build on the existing infrastructure to foster collaboration, share resources, and address local concerns (32). This needs assessment builds on the efforts of a network of local service organizations working to promote healthy aging in counties within Northeast Tennessee. Because leaders in the network are familiar with the unique strengths and challenges of the community, they can more readily address emerging issues such as SI/L.
The needs assessment was designed to identify factors associated with SI/L and strategies to strengthen social connections among older adults. Network members selected one county as the needs assessment site because efforts were already underway to address the unmet needs of older adults. This county ranks in the bottom 50% of all counties in the state for health outcomes, health behaviors, and social and economic indicators (33). The county is also classified as rural (24) and is designated a health professional shortage area (34). The purpose of this article is to describe findings from the needs assessment related to the factors associated with SI/L.
4 Materials and methods
4.1 Needs assessment procedures
We conducted a needs assessment survey of older adults using purposive sampling in three affordable housing apartment complexes in a county within Northeast Tennessee between February and March 2023. This project was reviewed by the Institutional Review Board (IRB) at East Tennessee State University and deemed non-human subjects research because it was a needs assessment conducted for multi-stakeholder planning purposes to inform age-friendly initiatives. Participants were recruited via flyers distributed to residents of the apartments either in person or via mail. Residents were eligible to complete the survey if they were ages 62 years and older and spoke English. On the scheduled dates, two needs assessment team members returned to the apartments. While the university IRB deemed this needs assessment as non-human subjects research, our team took extra precautions to ensure respect and ethical considerations were addressed. During the resident engagement process, team members described the purpose of the needs assessment and received verbal consent from individuals prior to distributing the self-administered surveys. Only those who agreed to participate were given surveys to complete. Twelve individuals declined to participate in the needs assessment, and one individual did not meet the eligibility criteria. A total of 82 older adults completed the survey which took approximately 30 minutes to complete. Participants received $50 upon completion of the survey.
4.2 Measures
The 67-item survey was organized into the following seven thematic sections: general daily life; health status; socialization/recreation; relationships with others; neighborhood characteristics; programs and services for older adults; and sociodemographic characteristics.
4.2.1 Outcome variables
Two outcome variables were included in the analysis. Social isolation was measured using Lubben’s 6-item Social Network Sale (LSNS-6) (35). The LSNS-6 is a validated objective measure of social network size, including the number and frequency of contact with family and friends. Items are scored from 0 to 5 and summed to provide a total score ranging from 0 (higher risk) to 30 (lower risk). Risk of social isolation was defined as a score below 12 (35). For the present analysis, the Cronbach’s alpha was 0.87. Loneliness was measured with the 3-item UCLA Loneliness Scale, which measures three subjective aspects of loneliness: lack of companionship, feeling left out, and feeling isolated from others (36). There were three response options: 1 = hardly ever, 2 = some of the time, and 3 = often. Scores range from 3 to 9, with loneliness defined as having a composite score of 6 or more (37). Cronbach’s alpha was 0.87 in the present analysis.
4.2.2 Explanatory variables
We included 17 explanatory variables in the analysis. The selection of these variables was either well-established risk factors associated with SI/L, such as individual, neighborhood, and socio-cultural characteristics (3) or variables of interest to the researchers. The variables of interest to the researchers (e.g., interest in having more friends, activities, or intergenerational connections, knowledge about community services, and length of residence) were selected because of their potential connection to SI/L.
4.2.2.1 Neighborhood conditions
Resource-related barriers to aging-in-place were measured with three items: In the last 12 months have you: (1) put off going to the doctor because of transportation; (2) needed to see a doctor but could not because of cost; and (3) had trouble pay bills (utilities, phone, medicine) due to cost (1 = yes, 0 = no). Experiencing resource-related barriers to aging-in-place was defined as responding yes to all three items.
One item was used to measure the level of knowledge about community services. Participants rated their knowledge on a 4-point Likert scale, from 1 = very informed to 4 = no, I do not feel informed. Low levels of knowledge were defined as responding somewhat informed or no, I do not feel informed.
Community livability was assessed with two items. Participants indicated whether their community was safe (1 = yes, 0 = no) and a good place for people to live as they age (4-point Likert scale: 1 = excellent to 0 = poor). Low community livability was defined as responding no to the first item and fair or poor to the second item.
4.2.2.2 Interpersonal relationships and activities
Boredom, wanting more friends, wanting to participate in more activities, and interest in intergenerational activities (e.g., participating in activities with youth or young adults) were assessed with one item each (1 = yes, 0 = no).
Eighteen items were used to measure participants’ engagement in the following leisure time activities (38): (1) shop; (2) visit with family or friends in person; (3) visit with your neighbors in person; (4) exercise [walking, running, weights, etc]; (5) participate in a club or civic group; (6) go to church, Bible studies, prayer; (7) talk on the phone with family or friends; (8) talk on video call/internet with family or friends; (9) exchange text messages with family or friends; (10) provide help to family, friends or neighbors; (11) participate in activities at the senior center; (12) care for a pet; (13) do housework or home maintenance; (14) participate in a hobby alone in your house; (15) participate in hobbies with groups; (16) attend movies, sports, or community events; (17) volunteer or help in the community; and (18) use a computer iPad, tablet, or smartphone. Low leisure time activity was defined as responding rarely or never to more than nine items.
4.2.2.3 Frailty
We used 10 questions to assess frailty (39, 40). Frailty was defined as a yes response to six or more items assessing physical health and functional status: (1) 4 or more chronic conditions derived from the question “has a doctor ever told you that you have any of the following conditions? (check all that apply)” (41) [21-item list of common conditions affecting older adults]; (2) disability defined as having a disability or health problem that limits the individual from participating in activities (e.g., housework, driving, recreation) (42); (3) pain defined as having pain that interfered somewhat to very much with daily activities in the past 7 days (43); (4) polypharmacy defined as taking five or more medications daily (44); (5) limitations to activities of daily living defined as difficulty performing activities such as walking, bathing, dressing in the last 12 months (45); (6) limitations to instrumental activities of daily living defined as difficulty doing routine activities such as household chores or shopping in the past 12 months (45) (7) falls risk defined as having fallen or injured yourself in your home in the past 3 months (46); (8) emergency department or urgent care use defined as having used the emergency room or urgent care in the past 3 months (47); (9) currently uses home health services (48); (10) and needs or uses durable medical equipment (e.g., walkers, wheelchairs, lift chairs) (49).
4.2.3 Sociodemographic characteristics
Measured demographic characteristics included age, gender, race, education, marital status, number of people living in the household, annual income, education, and length of residence in the county. Age was recoded as a categorical variable (<80 and ≥ 80 years) because individuals 80 and older are at greatest risk for social isolation (50).
4.3 Analysis
We conducted bivariate analysis to identify potential risk factors associated with SI/L. Variables with a p-value of ≤0.20 (51) in the simple logistic regression models were included in multiple logistic models using stepwise-backward selection procedures. Through this process, variables were systematically eliminated based on their p-values until those remaining in the model had a significance level of 10% (52, 53). Variance inflation factors (VIF) were computed for each multiple logistic regression model to assess multicollinearity, and no evidence of multicollinearity between risk factors was found (all VIFs <1.20). The analysis used SAS (SAS 9.4, SAS Institute, Inc., Cary, NC).
5 Results
5.1 Descriptive statistics
The descriptive statistics are presented in Table 1. The needs assessment included 82 participants. Roughly 18% of the participants were ages 80 years and older. The majority were non-Hispanic white (95.1%), and nearly three-fourths (70.7%) were female. A little more than two-thirds (69.5%) reported incomes of $24,000 or less or had less than a high school degree or graduated from high school. Most participants lived in the county for 5 years or longer (75.6%), were unmarried (e.g., single, widowed, divorced) (92.6%), and lived alone (91.5%). One-in-three (37.8%) were frail.
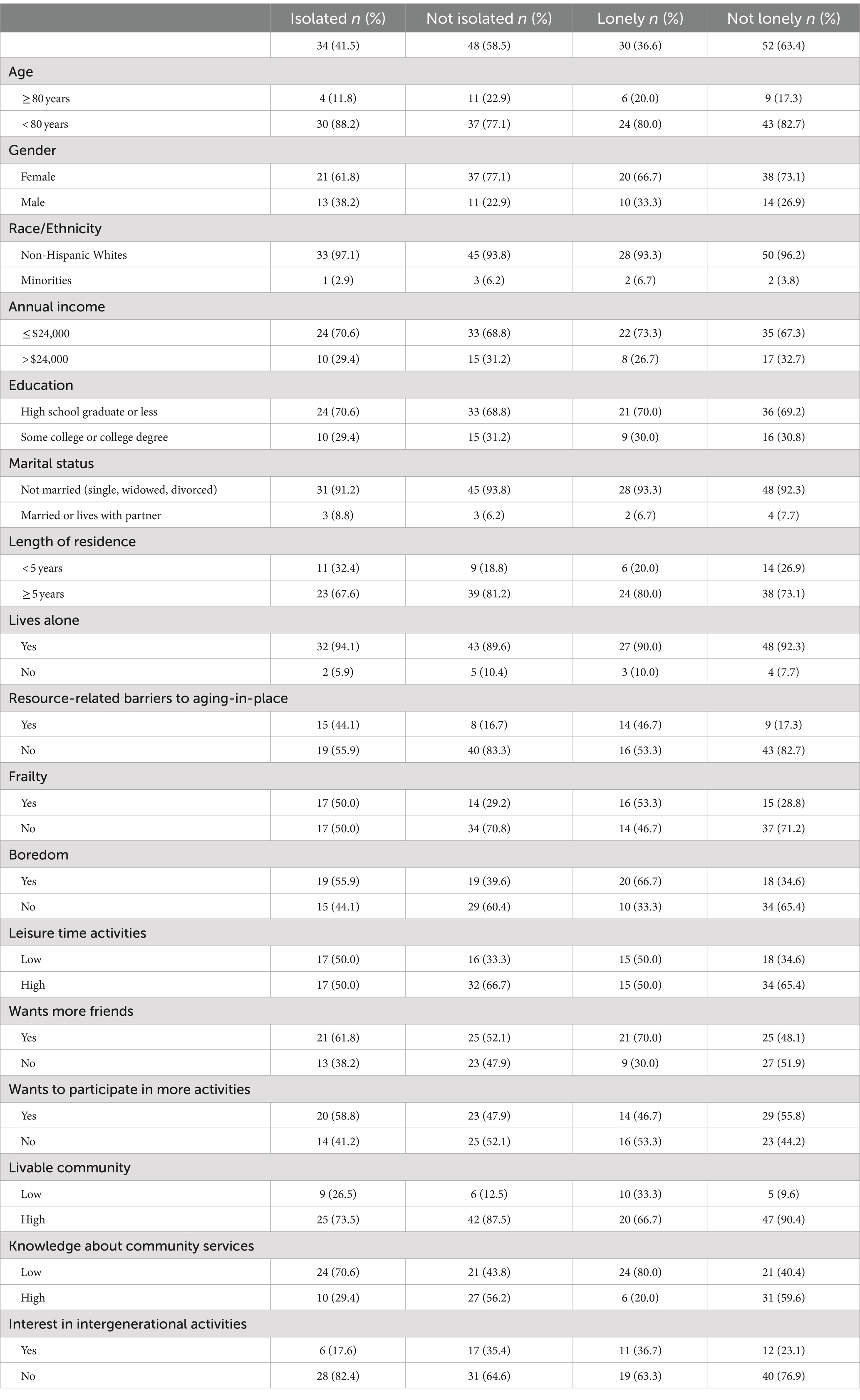
Table 1. Descriptive statistics for the sociodemographic characteristics, neighborhood conditions, and interpersonal relationships and activities.
As for neighborhood conditions, most participants rated the community livability as high (81.7%); whereas one-quarter reported resource-related barriers to aging-in-place (28.0%) and over half reported low levels of knowledge about community services (54.9%). Regarding interpersonal relationships and activities, almost half reported boredom (46.3%) and four-in-ten wanted to participate in more activities (40.2%). Although more than half of participants wanted more friends (56.1%), only one-quarter of participants were interested in opportunities for intergenerational engagement (28.0%).
5.2 Prevalence of social isolation and loneliness
Four-in-ten participants were socially isolated (41.5%) and over one-third of participants were lonely (36.6%).
5.3 Risk factors for social isolation and loneliness
Table 2 presents a summary of the outcomes from both simple and multiple logistic regression analyses conducted to identify predictors of social isolation and loneliness.
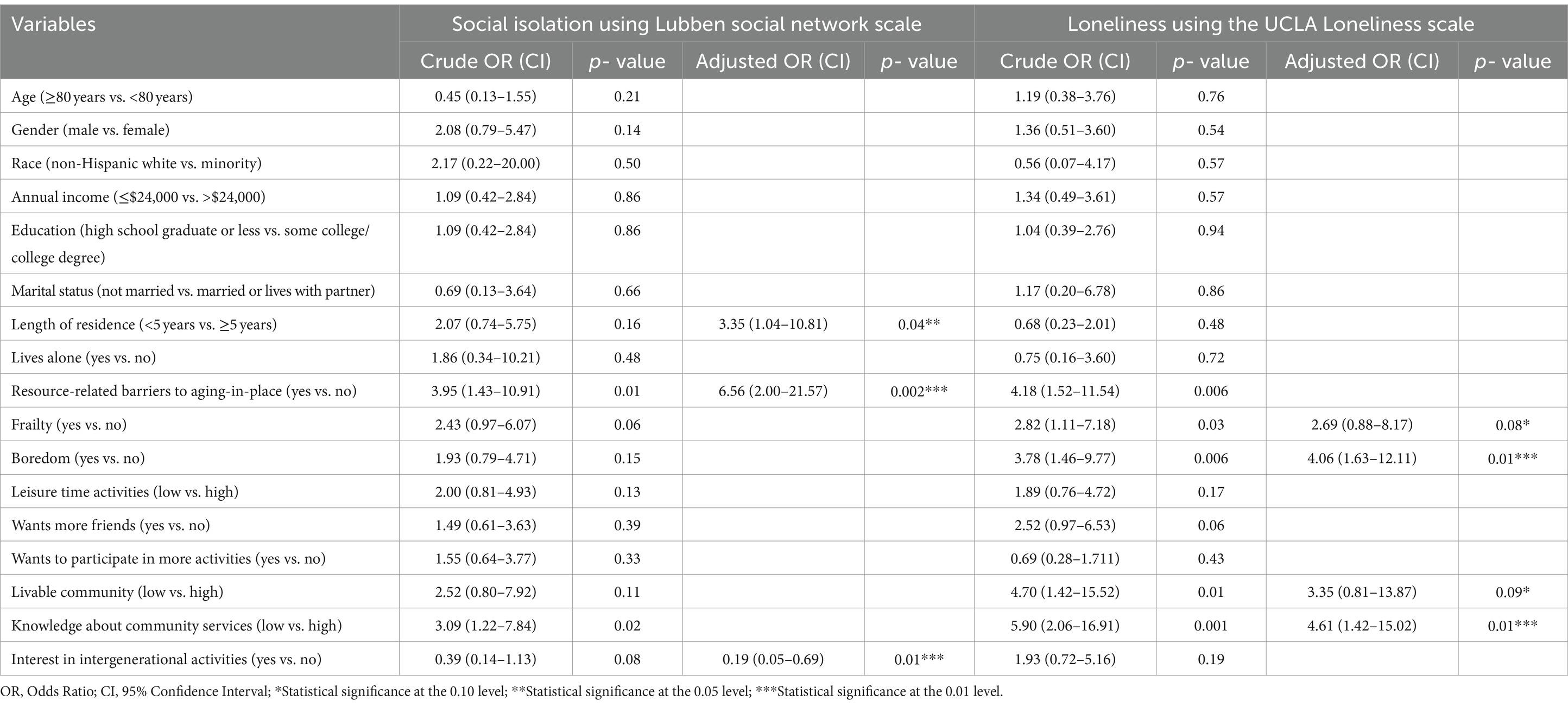
Table 2. Univariate and multivariate analyses to determine factors independently associated with social isolation and loneliness.
5.3.1 Social isolation
In the final adjusted model, we identified three significant predictors of social isolation. Participants who reported resource-related barriers to aging-in-place were 6.56 times more likely than those with no barriers to experience social isolation [95% CI (2.00–21.57), p = 0.002]. Participants living in the county for less than 5 years were 3.35 times more likely to experience social isolation compared to those residing in the county for longer term [95% CI (1.04–10.81), p = 0.04]. In contrast, the odds of social isolation were lower among older adults interested in intergenerational activities [Adjusted OR (AOR) = 0.19, 95% CI (0.05–0.69), p = 0.01] compared to those who were not interested in participating in activities with youth or young adults. The final adjusted model demonstrated good predictive ability (c-statistic, 0.746) (54, 55).
5.3.2 Loneliness
Four significant risk factors were identified via stepwise logistic regression. Participants who were frail were 2.69 times more likely than those without frailty to experience loneliness [95% CI (0.88–8.17), p = 0.08]. Reporting boredom quadrupled the likelihood of loneliness compared to those without boredom [AOR: 4.06, 95% CI (1.63–12.11), p = 0.01]. Likewise, participants with limited knowledge about community services were 4.61 times more likely than those with more knowledge to report being lonely [95% CI (1.42–15.02), p = 0.01]. Finally, older adults who rated their community livability as low were 3.35 times more likely to experience loneliness compared to those who rated their community livability as high [95% CI (0.81–13.87), p = 0.09]. The final adjusted model demonstrated good predictive ability (c-statistic, 0.811) (54, 55).
6 Discussion
This community needs assessment highlights a successful grassroots initiative to expand access to data about SI/L. The needs assessment also identifies factors associated with older adults’ SI/L, such as living in the county for less than 5 years, reporting resource-related barriers to aging-in-place, boredom, limited knowledge about community services, frailty, and perceived community livability. Local leaders and community stakeholders can use these data to guide policy and practice recommendations to support aging-in-place in the county.
6.1 Strength of the approach in a rural context
The approach merits several strengths in the rural context. First, the community needs assessment builds on existing efforts in the community to address the unmet needs of rural older adults. By proactively engaging local community leaders, many of whom are 65 years or older, in the process, our approach champions grassroots engagement and ownership of the initiative (10). Second, our approach leverages local capacity, resources, and readiness for change. Rural nonprofits often face financial, geographic, and staffing challenges that limit their reach and impact on rural older adults (10, 32). A network approach mobilizes multi-sectoral stakeholders and creates the necessary infrastructure to implement change initiatives to address the health and social needs of rural older adults (10). Last, our approach provides community leaders with access to local data to drive policies and the development of initiatives to better support rural older adults (10, 11). In national and statewide assessments, data on rural populations are often suppressed due to low response rates and small sample sizes. Grassroots initiatives have the advantage of having access to hard-to-reach populations, such as rural older adults, to aid networks and coalitions in making informed decisions for their communities.
6.2 Tailored strategies to address SI/L
A multifaceted approach is needed to address SI/L in this rural community (3). Findings from the needs assessment underscore the importance of addressing the built environment features to enhance access to healthcare services, transportation, broadband, information, and social engagement and volunteer opportunities (3, 56). Additionally, volunteer-led and home-based initiatives that enhance social contact via non-digital means are promising, low-cost approaches that this community can employ to reduce SI/L among rural older adults who have mobility issues, limited income, or lack access to transportation (57, 58).
The findings also highlight the significance of considering the length of residence in this community as a critical factor in understanding social isolation among older adults. Specifically, it reveals that newcomers to the area (i.e., those who have lived in the community for less than 5 years) are at a higher risk of experiencing social isolation. Similar findings have been reported elsewhere (59). This finding underscores the need for the development and implementation of initiatives, such as orientation programs aimed at healthcare staff and community organizations to facilitate a deeper understanding of “what matters” to older adults across various domains, including social, psychosocial, and spiritual determinants of their health and well-being. Orientation programs (60) can equip individuals with the necessary knowledge and tools to engage with older adults in a holistic manner, considering their individual preferences, values, and priorities. Such programs can also assist older adults with navigating the available resources and services in the community. Identifying community engagement opportunities and connecting older adults with those resources can help create a supportive environment that promotes social interactions, community engagement, emotional well-being, and a sense of purpose (3, 31). By incorporating the principles of such person-centered care, these programs may have potential to help professionals develop a comprehensive understanding of each older adult’s unique social support system and psychosocial needs (31).
6.3 Practical implications
By investing to build an ecosystem of support, rural communities can address the evolving health and social needs of older residents (60). The American Association of Retired Persons (AARP) Network of Age-Friendly Communities can guide local efforts. The age-friendly community movement builds on the World Health Organization’s eight domains of livability framework which was developed to guide communities in becoming more age-friendly, livable, and connected (61, 62). Despite having a growing proportion of older adults in Central Appalachia (22), age-friendly initiatives have been slow to emerge in the region (63).
Since implementing the needs assessment described in this article, efforts are now underway to work with the AARP State Office to obtain the designation as an Age-Friendly county. Network members will build upon the findings from the needs assessment and conduct listening sessions with the community. The goal is to explore key issues on a deeper level, assess community readiness for change, and identify leverage points and opportunities for improvement. By using a data-driven approach and guidance from evidence-based strategies, network members can tailor efforts to the needs of their community members. Other rural communities can learn practical lessons from this needs assessment to expand local efforts to promote healthy aging.
7 Limitations
Our project has several limitations including a small sample size and lack of generalizability of the findings since the data were derived from older adults in a single county. In addition, purposive recruitment and the characteristics of participants (e.g., female, unmarried/divorced, living alone) may partially explain the high percentage of social isolation in this population. We acknowledge the influence of employment on SI/L issues. Employment was not included in the analysis because residents who completed the needs assessment were not employed. Gender was captured in a binary way (male or female) and may not capture the gender diversity of participants. Lastly, a small sample size resulted in a lower precision during data analysis (e.g., wide confidence intervals).
8 Conclusion
Overall, this community needs assessment underscores the urgency of addressing SI/L among rural older adults in Central Appalachia and the importance of localized data to inform program development for this population. By implementing data-informed strategies and policies, rural communities can work toward promoting age-friendly initiatives to address SI/L among their older residents.
Data availability statement
The datasets presented in this article are not readily available because researchers are using the dataset to develop other manuscripts. Requests to access the datasets should be directed to Jodi Southerland, c291dGhlcmxhbmpsQGV0c3UuZWR1.
Ethics statement
The studies involving humans were approved by East Tennessee State University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the needs assessment was considered nonhuman subjects research.
Author contributions
JS: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. SZ: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. KD: Data curation, Investigation, Writing – original draft, Writing – review & editing. EM: Writing – original draft, Writing – review & editing. J-DB: Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing. JH: Writing – original draft, Writing – review & editing. SK: Writing – original draft, Writing – review & editing. AM: Writing – original draft, Writing – review & editing. MS: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Holt-Lunstad, J, Smith, TB, Baker, M, Harris, T, and Stephenson, D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
2. Hong, JH, Nakamura, JS, Berkman, LF, Chen, FS, Shiba, K, Chen, Y, et al. Are loneliness and social isolation equal threats to health and well-being? An outcome-wide longitudinal approach. SSM Popul Health. (2023) 23:1459. doi: 10.1016/j.ssmph.2023.101459
3. National Academies of Sciences Engineering and Medicine. Social isolation and loneliness in older adults: Opportunities for the health care system. Washington, DC: National Academies Press (2020).
4. Savla, J, Bivens, LR, Roberto, KA, and Blieszner, R. Where you age matters: Individual-And County-level predictors of formal and informal Care in Rural Appalachia. J Aging Health. (2019) 31:837–60. doi: 10.1177/0898264318761907
5. Henning-Smith, C, Tuttle, M, Tanem, J, Jantzi, K, Kelly, E, and Florence, LC. Social isolation and safety issues among rural older adults living alone: perspectives of meals on wheels programs. J Aging Soc Policy. (2022) 36:282–301. doi: 10.1080/08959420.2022.2081025
6. Lahr, M, and Henning-Smith, C. Barriers to aging in place in rural communities: Perspectives from state offices of rural health. Minneapolis, MN. (2021).
7. Hash, KM, Schreurs, BG, Tolley, SM, and Fiske, A. Health disparities in Appalachian and other rural communities. Int J Aging Hum Dev. (2023) 98:56–68. doi: 10.1177/00914150231171856
8. Reinhard, S, Harrell, R, Amero, CB, Flinn, B, Houser, A, Lingamfelter, P, et al. Innovation and opportunity: A state scorecard on long-term services and supports for older adults, people with disabilities, and family caregivers. Washington, DC. (2023).
9. Vipperman, A, Savla, J, Roberto, KA, and Burns, D. Barriers to service use among dementia family caregivers in rural Appalachia: implications for reducing caregiver overload. Prev Sci. (2023) 24:950–60. doi: 10.1007/s11121-022-01479-w
10. Guest, MA, Wolfe, M, Phillips, K, and Hook, J. Ensuring age-friendly public health in rural communities: Challenges, opportunities, and model programs background. (2023).
11. Scally, CP, Su, Y, and Mogan, A. Leveraging partnerships and data to improve rural health and well-being: A guidebook for rural practitioners. (2023).
12. Holt-Lunstad, J. Social connection as a public health issue: the evidence and a systemic framework for prioritizing the “social” in social determinants of health. Annu Rev Public Health. (2022) 43:193–213. doi: 10.1146/annurev-publhealth-052020-110732
13. DiNapoli, EA, Wu, B, and Scogin, F. Social isolation and cognitive function in Appalachian older adults. Res Aging. (2014) 36:161–79. doi: 10.1177/0164027512470704
14. Park, C, Majeed, A, Gill, H, Tamura, J, Ho, RC, Mansur, RB, et al. The effect of loneliness on distinct health outcomes: a comprehensive review and Meta-analysis. Psychiatry Res. (2020). doi: 10.1016/j.psychres.2020.113514
15. Flowers, L, Houser, A, Noel-Miller, C, Shaw, J, Bhattacharya, J, Schoemaker, L, et al. Medicare spends more on socially isolated older adults-AARP insight on the issues. (2017).
16. Schroeder, J, Henning-Smith, C, and Tuttle, M. Demographics and disability status of adults living alone in rural areas. (2021).
17. Glauber, R. Rural depopulation and the rural-urban gap in cognitive functioning among older adults. J Rural Health. (2022) 38:696–704. doi: 10.1111/jrh.12650
18. Henning-Smith, C. Meeting the social needs of older adults in rural areas. JAMA Health Forum. (2020) 1:1411. doi: 10.1001/jamahealthforum.2020.1411
21. United States Census Bureau. Central Appalachia. (2021). Available at: https://www.census.gov/library/visualizations/2021/demo/central-appalachia.html (Accessed January 18, 2024).
22. Pollard, K, Srygley, S, and Jacobsen, LA. The Appalachian region: A data overview from the 2017–2021 American community survey Chartbook. (2023).
24. United Stated Department of Agriculture. Rural-urban commuting area codes (2023). Available at: https://www.ers.usda.gov/data-products/rural-urbancommuting-area-codes/ (Accessed July, 24, 2023).
25. Centers for Disease Control and Prevention. Healthy places terminology (2009). Available at: http://www.cdc.gov/healthyplaces/terminology.htm (Accessed December 14, 2023).
26. Bacsu, J, McIntosh, T, Viger, M, Johnson, S, Jeffery, B, and Novik, N. Supporting older adults’ engagement in health-care programs and policies: findings from a rural cognitive health study. Home Health Care Serv Q. (2019) 38:209–23. doi: 10.1080/01621424.2019.1614505
27. Henning-Smith, C. The unique impact of COVID-19 on older adults in rural areas. J Aging Soc Policy. (2020) 32:396–402. doi: 10.1080/08959420.2020.1770036
28. Henning-Smith, C, Moscovice, I, and Kozhimannil, K. Differences in social isolation and its relationship to health by rurality. J Rural Health. (2019) 35:540–9. doi: 10.1111/jrh.12344
29. Boyd Center for Business and Economic Research. Tennessee population projections for 2021-2070 methodology, Executive Summary, and Notes. Boyd Center for Business and Economic Research, (2022).
30. Beatty, KE, Mathis, SM, McCurry, AR, Francisco, MM, Meit, M, and Wahlquist, AE. The association between grandparents as caregivers and overdose mortality in Appalachia and non-Appalachia counties. Front Public Health. (2023) 11:564. doi: 10.3389/fpubh.2023.1035564
31. Coalition to End Social Isolation and Loneliness. 2023–2024 policy priorities addressing the impact of social isolation and loneliness. (2023).
32. Walters, JE. Organizational capacity of nonprofit organizations in rural areas of the United States: a scoping review. Hum Serv Organ Manag Leadersh Gov. (2020) 44:63–91. doi: 10.1080/23303131.2019.1696909
33. University of Wisconsin Population Health Institute. County Health Rankings and Roadmaps 2023. (2023). Available at: www.countyhealthrankings.org (Accessed December 14, 2023).
34. Health Resources and Services Administration. Find shortage areas. (2023). Available at: https://data.hrsa.gov/tools/shortage-area (Accessed December 14, 2023).
35. Lubben, J, Blozik, E, Gillmann, G, Iliffe, S, Von, W, Kruse, R, et al. Performance of an abbreviated version of the Lubben social network scale among three European Community-dwelling older adult populations. Gerontologist. (2006) 46:503–13. doi: 10.1093/geront/46.4.503
36. Hughes, ME, Waite, LJ, Hawkley, LC, and Cacioppo, JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. (2004) 26:655–72. doi: 10.1177/0164027504268574
37. Chen, SW, Rice, S, Storey, K, Keglovits, M, Devine, M, Yan, Y, et al. COVID-19: factors predicting depressive symptoms in people aging with long-term physical disabilities. OTJR (Thorofare N J). (2023) 43:194–201. doi: 10.1177/15394492221107557
38. Research, B, and Consulting, I. Edmonton Seniors Coordinating Council, the City of Edmonton. 2015 Older Adult Needs Assessment, Final Report. (2015).
39. Lee, H, Lee, E, and Jang, IY. Frailty and comprehensive geriatric assessment. J Korean Med Sci. (2020) 35:e16. doi: 10.3346/jkms.2020.35.e16
40. Walston, J, Buta, B, and Xue, QL. Frailty screening and interventions: considerations for clinical practice. Clin Geriatr Med. (2018) 34:25–38. doi: 10.1016/j.cger.2017.09.004
41. Centers for Disease Control and Prevention. Behavioral risk factor surveillance system survey questionnaire. Atlanta: Centers for Disease Control and Prevention (2021).
42. Bouldin, ED, Vandenberg, A, Roy, M, Hege, A, Zwetsloot, JJ, and Howard, JS. Prevalence and domains of disability within and outside Appalachian North Carolina: 2013–2016 behavioral risk factor surveillance system. Disabil Health J. (2020) 13:879. doi: 10.1016/j.dhjo.2019.100879
43. Talaei-Khoei, M, Riklin, E, Merker, VL, Sheridan, MR, Jordan, JT, Plotkin, SR, et al. First use of patient reported outcomes measurement information system (PROMIS) measures in adults with neurofibromatosis. J Neuro-Oncol. (2017) 131:413–9. doi: 10.1007/s11060-016-2314-7
44. Varghese, D, Ishida, C, and Haseer Koya, H. Polypharmacy. Treasure Island, FL: Stat Pearls Publishing (2024).
45. Edemekong, PF, Bomgaars, DL, Sukumaran, S, and Schoo, C. Activities of daily living, in: Stat pearls. Treasure Island, FL: Stat Pearls Publishing (2024).
46. Saario, EL, Mäkinen, MT, Jämsen, ERK, Nikander, P, and Castrén, MK. Screening of community-dwelling older patients by the emergency medical services: an observational retrospective registry study. Int Emerg Nurs. (2021) 59:1078. doi: 10.1016/j.ienj.2021.101078
47. Tang, XR, Zarisfi, F, Pek, PP, Siddiqui, FJ, Malhotra, R, Kwan, YH, et al. Emergency department utilisation among older adults—protocol for a systematic review of determinants and conceptual frameworks. PLoS One. (2022) 17:e0265423. doi: 10.1371/journal.pone.0265423
48. Wallace, LG, Hirschman, KB, Huang, L, Cacchione, PZ, and Naylor, MD. Hospitalizations, emergency department visits, and home health use among older adults with sensory loss. J Aging Health. (2024) 36:133–42. doi: 10.1177/08982643231176669
49. West, BA, Bhat, G, Stevens, J, and Bergen, G. Assistive device use and mobility-related factors among adults aged ≥ 65 years. J Saf Res. (2015) 55:147–50. doi: 10.1016/j.jsr.2015.08.010
50. Kaye, LW. Older adults, rural living, and the escalating risk of social isolation. Public Policy Aging Rep. (2017) 27:139–44. doi: 10.1093/ppar/prx029
51. Bursac, Z, Gauss, CH, Williams, DK, and Hosmer, DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. (2008) 3:17. doi: 10.1186/1751-0473-3-17
52. Baghi, H, Noorbaloochi, S, and Moore, JB. Statistical and nonstatistical significance: implications for health care researchers. Qual Manage Healthc. (2007) 16:104–12. doi: 10.1097/01.QMH.0000267447.55500.57
53. Lang, PO, Meyer, N, Heitz, D, Dramé, M, Jovenin, N, Ankri, J, et al. Loss of independence in Katz’s ADL ability in connection with an acute hospitalization: early clinical markers in French older people. Eur J Epidemiol. (2007) 22:621–30. doi: 10.1007/s10654-007-9150-1
54. Rahmanian, PB, Kröner, A, Langebartels, G, Özel, O, Wippermann, J, and Wahlers, T. Impact of major non-cardiac complications on outcome following cardiac surgery procedures: logistic regression analysis in a very recent patient cohort. Interact Cardiovasc Thorac Surg. (2013) 17:319–27. doi: 10.1093/icvts/ivt149
55. Wall, JJS, Iqbal, J, Andrews, M, Teare, D, Ghobrial, M, Hinton, T, et al. Development and validation of a clinical risk score to predict mortality after percutaneous coronary intervention. Open Heart. (2017) 4:e000576. doi: 10.1136/openhrt-2016-000576
56. Williams, T, Lakhani, A, and Spelten, E. Interventions to reduce loneliness and social isolation in rural settings: a mixed-methods review. J Rural Stud. (2022) 90:76–92. doi: 10.1016/j.jrurstud.2022.02.001
57. Chua, CMS, Chua, JYX, and Shorey, S. Effectiveness of home-based interventions in improving loneliness and social connectedness among older adults: a systematic review and meta-analysis. Aging Ment Health. (2023) 28:1–10. doi: 10.1080/13607863.2023.2237919
58. Yu, DSF, Li, PWC, Lin, RSY, Kee, F, Chiu, A, and Wu, W. Effects of non-pharmacological interventions on loneliness among community-dwelling older adults: a systematic review, network meta-analysis, and meta-regression. Int J Nurs Stud. (2023) 144:4524. doi: 10.1016/j.ijnurstu.2023.104524
59. Ejiri, M, Kawai, H, Ishii, K, Oka, K, and Obuchi, S. Predictors of older adults’ objectively measured social isolation: a systematic review of observational studies. Arch Gerontol Geriatr. (2021) 94:357. doi: 10.1016/j.archger.2021.104357
60. Renaud, J, McClellan, SR, DePriest, K, Witgert, K, O’Connor, S, Abowd Johnson, K, et al. Addressing health-related social needs via community resources: lessons from accountable health communities. Health Aff. (2023) 42:832–40. doi: 10.1377/hlthaff.2022.01507
61. Levasseur, M, Dubois, MF, Généreux, M, Menec, V, Raina, P, Roy, M, et al. Capturing how age-friendly communities foster positive health, social participation and health equity: a study protocol of key components and processes that promote population health in aging Canadians. BMC Public Health. (2017) 17:4392. doi: 10.1186/s12889-017-4392-7
62. World Health Organization. National programmes for age-friendly cities and communities a guide. Geneva: World Health Organization (2023).
Keywords: social isolation, loneliness, rural, older adults, aging-in-place
Citation: Southerland JL, Zheng S, Dodson K, Mauck E, Bacsu J-DR, Brown MJ, Holloway J, Kim SM, Malatyali A and Smith ML (2024) Social isolation and loneliness prevention among rural older adults aging-in-place: a needs assessment. Front. Public Health. 12:1404869. doi: 10.3389/fpubh.2024.1404869
Edited by:
Shane Andrew Thomas, Federation University Australia, AustraliaReviewed by:
Albina Veltman, McMaster University, CanadaHashaam Akhtar, Yusra Institute of Pharmaceutical Sciences Islamabad, Pakistan
Copyright © 2024 Southerland, Zheng, Dodson, Mauck, Bacsu, Brown, Holloway, Kim, Malatyali and Smith. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jodi L. Southerland, c291dGhlcmxhbmpsQGV0c3UuZWR1
†ORCID: Juanita-Dawne R. Bacsu, https://orcid.org/0000-0002-2819-1617
Erin Mauck, https://orcid.org/0000-0002-2274-0275
Monique J. Brown, https://orcid.org/0000-0001-9552-244X
Jeremy Holloway, https://orcid.org/0000-0002-1441-3426
Steffi M Kim, https://orcid.org/0000-0003-0579-2492
Ayse Malatyali, https://orcid.org/0000-0002-6931-6914
Matthew Lee Smith, https://orcid.org/0000-0002-8232-9285
 Jodi L. Southerland
Jodi L. Southerland Shimin Zheng2
Shimin Zheng2 Erin Mauck
Erin Mauck Juanita-Dawne R. Bacsu
Juanita-Dawne R. Bacsu Monique J. Brown
Monique J. Brown Jeremy Holloway
Jeremy Holloway Steffi M. Kim
Steffi M. Kim Ayse Malatyali
Ayse Malatyali Matthew Lee Smith
Matthew Lee Smith